An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Surgical management of femoral neck fractures.
Zara Hayat ; Matthew Varacallo .
Affiliations
Last Update: August 4, 2023 .
- Continuing Education Activity
Femoral neck fractures (FNFs) are extremely common. FNFs demonstrate a bimodal distribution pattern, occurring secondary to low-energy falls in elderly patients and higher-energy traumatic mechanisms in younger patients. This activity reviews the key operative techniques and surgical management options, including the recent advances, for managing FNFs in the elderly and young populations. Intracapsular FNFs account for approximately 50% of all hip fractures. The majority of these fractures occur in elderly patients with underlying osteoporosis. This activity describes the pathophysiology of FNFs and emphasizes the importance of the interprofessional team in the preoperative workup of these patients to improve outcomes.
- Identify the anatomical structures involved in a femoral neck fracture.
- Describe the surgical techniques for managing a femoral neck fracture.
- Review the early and late complications of surgery to fix FNFs.
- Outline interprofessional team strategies for improving care coordination and communication to advance the preoperative workup of patients undergoing surgery and improve outcomes.
- Introduction
Femoral neck fractures (FNFs) are among the most common fractures in the elderly population, with a high mortality risk at one year, ranging up to 36%. [1] [2] Also, the management of such fractures entails a significant financial and societal burden.
These fractures demonstrate a bimodal distribution pattern secondary to low-energy falls in elderly patients and higher-energy traumatic mechanisms in younger patients. The majority of such fractures are seen in the elderly population, with risk factors including osteoporosis, female gender, smoking, and low BMI. [3] [4] This article reviews the key operative techniques and surgical management options for managing femoral neck fractures in the elderly and young populations.
- Anatomy and Physiology
Intracapsular femoral neck fractures account for approximately 50% of all hip fractures. The majority of these fractures occur in elderly patients with underlying osteoporosis. [5] [6]
Femoral neck fractures are differentiated from extracapsular hip fracture patterns based on anatomic location. The distinction between these fracture patterns is critical because intracapsular fractures demonstrate limited healing potential secondary to the absence of the periosteal layer, and the fracture is bathed in the surrounding synovial fluid. The hip joint capsule attaches to the intertrochanteric line anteriorly and the crest posteriorly. [7] There is a theoretical risk of compromised blood supply to the femoral head secondary to increased intra-articular pressures in the setting of an intracapsular FNF with preservation of the hip joint capsule. A tamponade effect that compromises femoral head perfusion has been demonstrated in previous studies. [8]
The arterial blood supply to the femoral head arises from three main sources. [9] [10] These are:
- The dominant contributing blood supply is from the MFCA by way of the lateral epiphyseal artery
- The LFCA supplies portions of the anterior and inferior femoral head
- Retinacular vessels branching from the circumflex arteries
- Ligamentum teres (predominant role in pediatric patients, minimal contribution in the adult patient)
- Minimal supply from the medullary canal and inferior gluteal artery
In addition to the tamponade effect mentioned above and its potential compromise to femoral head blood flow, patients with femoral neck fractures risk developing avascular necrosis (AVN) due to the retrograde blood supply and injury to the retinacular vessels. [11]
Implications for Treatment
Displaced intracapsular femoral neck fractures in the elderly are typically managed with hip reconstruction procedures. The femoral head and neck are replaced with a reconstruction prosthesis. These procedures typically include hip hemiarthroplasty or total hip arthroplasty (THA) procedures. Nondisplaced fractures can be managed with fixation using cannulated screw fixation.
In contrast, extracapsular fractures rarely compromise the arterial blood supply to the femoral head and neck and, thus, are commonly managed with various types of surgical fixation techniques. AVN of the femoral head is very rare following extracapsular fractures. [12]
- Indications
General Concepts
The elderly population often presents with femoral neck fractures in the setting of multiple medical comorbidities. Thus, this patient population requires a comprehensive and interprofessional approach to address all comorbidities and all mental and physical impairments. [13]
Surgery is nearly always indicated for patients presenting with an FNF. The goals of surgery include: [14]
- Pain control
- Restoration of mobility and function
- Achieve restoration of alignment and osseous healing (following surgical fixation techniques)
Nonoperative Management Considerations
In the setting of femoral neck fractures, nonoperative management is rarely indicated, given the devastatingly highly-associated complication rates. Nonoperative management is reserved only for a select subgroup of nonambulatory patients with significant medical comorbidities. [15]
Patients managed definitively with nonoperative treatment modalities are treated with pain control modalities. Patients often experience pain for several weeks, indicating the formation of a functional girdle stone. The goal of care is always based on a delicate balance in weighing the overall risks and benefits of surgical versus nonoperative management. In select patients that are deemed critically ill and at significant risk for perioperative complications with surgical management, the phases of patient care include initial pain/symptomatic control followed by attempts at mobilization once some callous formation is noted after a few weeks.
The risks associated with nonoperative management include increased rates of related complications, such as pulmonary dysfunction, pneumonia, urinary tract infections (UTIs), pressure sores (e.g., sacral decubitus ulcers), and venous thromboembolic events.
Indications for Specific Surgical Techniques
Hemiarthroplasty and Total Hip Arthroplasty (THA)
Replacement of the femoral head is indicated in displaced intracapsular femoral neck fractures, particularly in low-demand elderly patients. A THA is recommended for patients with these injuries in independent baseline ambulatory function or in patients with prior evidence of hip pain and/or radiographic evidence of degenerative arthritis. Due to increased chances of hip dislocation seen after THA is done for FNFs, advances in the implant type and modifications in the surgical technique have been described. [16] [17]
Cannulated Screws
Cannulated screw fixation is indicated in nondisplaced, intracapsular femoral neck fractures in elderly patients and displaced fractures in younger patients with ideal bone quality. The technique consists of inserting 3 or 4 cannulated screws in an inverted triangle or diamond configuration, respectively. While no difference in outcomes has been demonstrated comparing the utilization of three versus four screws, the literature notes superior results in surgical fixation configurations utilizing the inverted triangle placement compared to fractures fixed with only two cannulated screws. Recently, the biplane double-supported screw fixation (BDSF) method has been described for femoral neck fractures. [18] [19]
Critical utilization of partially threaded (long or short thread options) screw options should be pre-operatively planned before the commencement of the procedure. The surgeon should plan on optimizing the "lag by design" technique. Recently, a femoral neck system (FNS) implant has been described for the internal fixation of FNFs in young patients with theoretical biomechanical advantages compared to other implants. [20] [21]
Sliding Hip Screw (SHS)
The sliding hip screw fixation construct is comprised of a large, cancellous lag screw that passes from the lateral, proximal femur across the fracture site and ends near the apex position of the femoral head. The lag screw dynamically slides inside an incorporated metal sleeve, with the latter being connected to a fixation plate that subsequently is secured with multiple screws to the proximal femur. The compression mechanism is amenable for utilization for the following types of injuries:
- Stable, intertrochanteric hip fractures
- Basicervical FNF patterns
- SHS fixation is superior to cannulated screw fixation in younger patients with vertical fracture patterns
The fracture is amenable to compression as the transfer of weight-bearing forces propagates from the appendicular skeleton, through the pelvis, and through the femoral head and neck before the forces transmit distally. Thus, the SHS fixation construct allows for longitudinal sliding and compression as the patient ambulates postoperatively. Thus, the fracture compresses down as the lag screw slides into the barrel and further promotes healing. [22]
Intramedullary Nail (IMN)
Similar to the SHS in that one or multiple screw fixation elements extend from the lateral, proximal femur through the neck and end near the apex of the femoral head. Depending on the specific implant type, there are options to promote varying degrees of dynamic compression versus fixed angle constructs that can be tailored to the specific type of fracture pattern.
Critical differences in the indications for IMN versus SHS construct utilization include a shorter lever arm generated by using the IMN constructs, which are often favored in the setting of comminuted IT or subtrochanteric fracture patterns. Fractures involving the lateral wall of the proximal femur are, by definition, either reverse obliquity or transtrochanteric fracture patterns. These fracture patterns preclude the use of an SHS fixation device. [23]
Other potential benefits of IMN over SHS include the possible use of a smaller incision (assuming an open incision is not required to achieve an acceptable reduction of the fracture) and the maintenance of hip offset and lever arm as the IMN fixation results in a reduced sliding distance compared to the SHS. [24]
- Contraindications
Sliding hip screw fixation constructs are contraindicated in the following (unstable) fracture patterns:
- Reverse obliquity
- Transtrochanteric
- Comminuted fracture patterns with a large posteromedial fragment; imply a loss of the medial calcar buttress
- Fracture patterns with subtrochanteric extension [25]
All surgical procedures for femoral neck fractures require a standard orthopedic tray/set and should be carried out in an operating theatre equipped with laminar flow.
DHS/Cannulated Screws/IM Nails
All of them require the necessary implants, a radiolucent traction table or a flat Jackson operating table, an image intensifier, and a radiographic technician.
Hemiarthroplasty/THA
Standard operating table with necessary side supports, full set of implants, and, when applicable, the necessary instruments and materials allowing for incorporating cement fixation. Recently, the use of computer navigation and Robotics has been increasing for THAs. [26]
All operations require the following key personnel:
- Operating surgeon and assistant
- Anesthetist and ODP
- Scrub nurses
- Circulating staff
- Radiographer for SHS/cannulated screws/IM nail
- Preparation
The patient should have had a full history and examination, as well as appropriate anteroposterior (AP) and lateral radiographs of the hip and pelvis. They should consent and be marked in preparation for surgery. These patients tend to be elderly with numerous comorbidities. It is important that they are optimized pre-operatively. Healthcare providers need to pay particular attention to whether these patients are on any anti-coagulants, which may require reversal with Vitamin K and fresh frozen plasma (FFP in the case of warfarin). Available reversal agents vary by country and geographic region.
Routine pre-operative labs should be checked, including a complete blood count (CBC), a basic metabolic panel (BMP), and a type and screen/cross-match. Pre-operative medical service co-management may include additional consultation services depending on the degree and severity of pertinent medical comorbidities. Such patients should be appropriately optimized before posting for surgery; at the same time, the procedure should be expedited as the results are better when the surgery is done as early as possible. [27]
Other routine pre-operative workup elements include:
- Chest radiograph
- Electrocardiogram (ECG)
Patients should undergo review by the anesthetist and consideration for spinal versus general anesthetic.
Once in theatre, the WHO checklist should be completed, the patient positioned as detailed below, and appropriately prepped and draped.
Sliding Hip Screw/Cannulated Screws
The patient is placed supine on a radiolucent traction table. The foot on the side to be operated on is in a traction boot. The unaffected side is placed in the lithotomy position, strapped in a leg holder, and placed in a flexed, abducted, and externally rotated position to ensure the radiographic c-arm can access the fracture site appropriately. Gentle traction and internal rotation should be applied to reduce the fracture. Slight abduction may be needed to reduce any varus malalignment. Before prepping and draping, the fracture should be in near-anatomic alignment with radiographic confirmation. If closed reduction is not possible, open reduction may be necessary.
Correct lower extremity rotational alignment is imperative, and the patient should be positioned with the patella facing toward the ceiling. [25]
The positioning is the same as for DHS/cannulated screws, but it is important that the hip is in an adducted position. The torso can be pushed 10 to 15 degrees to the contralateral side to achieve this. The reduction is as above with traction and internal rotation with the image intensifier. Care should be taken not to rotate the pelvis when applying traction.
The patient is positioned in a lateral decubitus position with support over the anterior superior iliac spine and the sacrum. The pelvis should be at 90 degrees to the table. It is important to review the pre-operative radiographs and assess offset. This is the distance between the center of the femoral head and a line drawn down the middle of the femur. The femoral head size should also be checked and match the patient's own as closely as possible. [28]
- Technique or Treatment
Incision: A direct lateral approach is performed. The incision usually starts in line with the lesser trochanter, in line with the femur, and extends distally—next, a longitudinal incision through subcutaneous fat. The next layer is the fascia lata. This is incised in line with the skin incision to reveal vastus lateralis. The epimysium is incised. Vastus lateralis can be elevated off the lateral intermuscular septum but is more commonly split along its fibers.
Exposure of femur: A periosteal elevator (Bristow) is used to clear muscle from the bone, leaving a clear surface for the plate without soft tissue interposition. One or two self-retaining retractors may be helpful to gain adequate exposure for guidewire placement.
Guidewire: The kit typically includes a guidewire jig placed on the femoral shaft. It is important to ensure that the jig is placed centrally on the lateral shaft of the femur and can be checked by feeling how much bone there is anteriorly and posteriorly and adjusted accordingly. Regarding the AP placement of the wire, it is necessary to visualize where the tip of the guidewire will end up in the femoral head. The lesser trochanter usually marks the level of entry for a 135-degree angle plate. The tip should be within the subchondral bone. The position should be continually assessed using an image intensifier.
Measure: The included measuring device slides over the guidewire. It is important to ensure that it is sitting on the bone. Usually, 5 to 10 mm are deducted from the measurement.
Reaming: The guide wire is then over-drilled with a triple reamer. This creates a channel for both the lag screw and the barrel of the plate. Reaming is to the depth chosen for the screw. It is important to check on the radiograph that the third part of the reamer has engaged with the cortex of the bone and to ensure that the guide wire is not advancing into the pelvis.
Tap: In young patients or those with strong bones, it is beneficial to tap the bone.
Insert lag screw: The lag screw is then applied over the wire and screwed in using the attached handle. The final position of the handle should be parallel to the femur. This ensures the lag screw will slot into the plating barrel.
Apply plate and screws: The plate is then slid over the lag screw. The plate temper may be needed to ensure it is fully advanced. The guidewire can now be removed. The plate can be secured to the femur using a clamp. The screws are inserted next. The most distal one is conventionally done first. The 3.5-mm drill is used with the neutral drill guide to make the screw holes, drilling through both cortices. These are then measured using the depth gauge and the appropriate screw inserted.
Closure: Final AP and lateral radiographs should be obtained. The wound is washed, and closure is in layers. [29]
Reduction: Reduction is usually not needed for these, as screws are typically used for non-displaced fractures.
Incision: Similar to the DHS, a direct lateral approach is taken with a longitudinal incision made at the level of the lesser trochanter. This, however, is much smaller, usually around 5 cm.
Guidewire: The next step is to insert the three guidewires. This can be done using a guide or freehand, depending on the surgeon's preference and experience. The typical formation is an inverted triangle with one screw distally and two proximally. The entry point for the first guidewire should be no lower than the lesser trochanter; otherwise, there is the risk of causing a stress riser which may trigger a comminuted subtrochanteric fracture. Ideally, it should sit just above the calcar (on the AP view) and go up to the subchondral bone in the femoral head. The second guidewire is placed superiorly and posteriorly to the first one. On the lateral view, it should lie next to the posterior cortex. The third wire is placed superiorly and anteriorly to the first wire. Ideally, it should sit parallel to the second guidewire on the AP view. All three should be within 5 mm of the subchondral bone.
Measure and screw insertion: The measure is then used to ascertain which screw length will be used. Next, a cannulated drill is used to ream over the guidewires. This is usually from 5 to 10 mm short of the measured distance. Three partially threaded screws are then inserted before a wire driver is used to remove the guide wires. The screw measurement is usually the same as the original measurement of the guidewire. The threads of the screw should be beyond the fracture site to ensure that adequate compression takes place. The screws should be tightened together to ensure uniform compression. Depending on surgeon preference, washers may be used to further increase compression.
Closure: Final AP and lateral images should be taken, and the wound should be washed with normal saline. It should then be closed in layers. [29]
Hemiarthroplasty
Approach: There are numerous approaches to this operation. [30] One common approach is the anterolateral approach, also known as the modified Hardinge approach. A longitudinal incision centered over the greater trochanter is made. This is usually around 20 cm in length, curving posteriorly proximally. The layers encountered are subcutaneous fat, fascia lata, bursa, and then gluteus medius. The fascia lata is incised in line with the femur, following the line of the original incision, curving posteriorly. This is usually with a small incision centrally with a scalpel, and then, using scissors, the fascia lata is cut distally and then proximally. The fascia is then retracted using either a couple of self-retainers or a Charnley retractor. If the latter is used, the D shape created should point towards the knee. The trochanteric bursa is excised using forceps and scissors. Following this, the greater trochanter and attached muscles should be clearly visible, with gluteus medius proximally and vastus lateralis distally.
The assistant should then externally rotate the leg to put the gluteus medius on the stretch. The tip of the greater trochanter should be identified, and the gluteus medius fibers split. Be aware that the superior gluteal nerve is approximately 5 cm proximal to the tip of the greater trochanter.
The abductors (gluteus medius superficially and gluteus minimus underneath) are then detached from the greater trochanter using diathermy. This is typically done in an "s" or "omega" shape, leaving a sufficient cuff for repair at the end. It is sometimes necessary to split some of the vastus lateralis fibers as well.
Adequate dissection should reveal the capsule. A T-shaped incision is made in the capsule, staying close to the bone at the base of the femoral neck.
Dislocate hip: It is then necessary to dislocate the hip by externally rotating it. This should reveal the fractured neck as the leg is placed into the leg bag to enhance exposure.
Neck osteotomy: The next step is to make the neck cut. This is done with an oscillating saw at a 45-degree angle. The neck cut is typically measured from a line running between the superior aspect of the neck to 1cm proximal to the lesser trochanter but depends on the prosthesis to be used, particularly whether it has a collar or not.
Femoral head removal: This is done using the corkscrew, which is placed centrally in the head and then twisted in. The head is spun to detach it from the acetabulum and then can be removed. It may be necessary to use a mallet to help engage the corkscrew with the bone. If it is difficult to remove the femoral head, check the capsule cut is sufficient.
Femoral head measurement: This is done using the guide. If between sizes, most surgeons advise erring on the smaller side to minimize the risk of dislocation.
Prepare acetabulum: Ensure all soft tissue is removed; a bone nibbler can be used to remove any remaining soft tissue.
Femoral canal preparation: A Hohmann retractor is then used to expose the femoral calcar. The femur is prepared using a box chisel. This is typically placed as posterolaterally as possible and opens the femoral canal. A T-handled reamer is then inserted into the canal. While doing this, it can be helpful to place your other hand on the patient's knee to ensure it follows the anatomical axis. Reamers of increasing size are used until rotational movement is resisted. The femoral canal is then rasped. Particular attention is given to rasping the lateral side.
Trial: Trial the head and reduce the hip to assess size and stability with internal and external rotation with the hip flexed and extended. Assess for equal leg length. This is not always performed due to its intrinsic stability. If the hip is difficult to reduce, it may be because the stem is too proud, the offset is too great, or there is soft tissue obstruction. Dislocate the trial.
Cementing: Insert a cement restrictor (this may need to be sized depending on the kit used; typically 2 cm more than the length of the stem. The femoral canal is then washed using copious pulse lavage. Ribbon gauze is inserted into the femoral canal alongside a clean suction catheter. This will ensure the canal is dry and free from fat and blood, allowing the cement to interdigitate with the bone for solid fixation. At this point, the cement is prepared. The gauze is removed, and the cement is inserted into the canal using the cement gun. The nozzle should be inserted fully into the canal and by allowing the pressure of the cement to push the gun up proximally. Surgeon preference dictates whether the cement is pressurized.
Stem insertion and head attachment: The selected femoral stem is then inserted into the femoral canal. Be sure to remove all excess cement. It should ideally have 10 to 15 degrees of anteversion. Once the stem is in situ at the appropriate depth, avoid altering the degree of anteversion, as this can result in a varus stem which will compromise the outcome. The femoral head is then attached to the trunion, and the hip is reduced. This is done with gentle traction and a small degree of internal rotation. Stability should be assessed.
Closure: The wound is then washed and closed in layers (capsule, the abductors can be closed en masse, fascia lata, fat, skin). A double-layered closure of interrupted and then continuous sutures of the abductors may be of benefit to ensure a secure repair. [31]
Incision: A small (3 to 5 cm) lateral longitudinal incision is made proximal to the tip of the greater trochanter. This should be in line with the femoral shaft.
Entry point and guidewire: The entry point for the guidewire depends on the nail. Most use the tip of the trochanter (cephalomedullary nails) or the piriformis fossa (straight nails) as landmarks. Guidewire position should be checked using an image intensifier; the ideal position is central within the shaft on the AP view and in line with the middle of the femoral neck in the lateral view. It is important to avoid a too-lateral entry point as this will cause varus malalignment, which will predispose the implant to early failure.
Ream: Usually, a protection sleeve goes over the guidewire, which should sit flush with the greater trochanter. The femur should be renamed; it is suggested that this is done by hand in elderly patients with osteoporotic bone but can be done on power in younger patients.
Nail insertion: The nail is typically attached to a jig and is inserted manually over the wire. The depth of the nail as its inserted should be checked on the image intensifier. The lag screw must sit in the middle of the femoral neck with the tip in the center of the femoral head on AP and lateral views.
Lag screw guidewire: The guidewire is mounted on the jig. A small skin incision is then made. The drill sleeve should sit on the lateral cortex of the femur. The positioning of the screw is similar to that of the DHS, in line with the neck of the femur in the AP view with a slightly inferior position and centrally placed in the lateral view. It should go up to the subchondral bone. The tip apex distance should be less than 25 mm. The guidewire is then measured. The final measurement should be 5 to 10 mm less. The lateral cortex is then reamed. It is then locked using the jig.
Distal locking screw: Depending on the jig and whether it is a long or short nail, the distal locking screws may need to be done freehand using the 'perfect circles' technique. It is usually possible to use the selected hole on the jig for short nails. A stab incision is made in the skin, and both cortices are drilled using the drill bit and the protective sleeve. It is then measured, and a screw is inserted.
Closure: Final AP and lateral images are checked, and the wounds are washed. The closure is often surgeon-specific and can consist of multiple different suture options. The decision to repair the capsule and/or other periarticular tendinous structures is surgeon-dependent based on the preferred technique and the approach utilized. Strong suture options can generally be used in an interrupted or running-style closure. Once the deep layers are closed, 2-0 synthetic absorbable sterile surgical sutures composed of a copolymer can be used in an interrupted and buried stitch technique. Finally, the skin is closed utilizing staples, nylon, or running synthetic, absorbable sutures. Augmentation skin closure options include various types of skin glue or steri-strips. A sterile bandage is then applied.
Postoperative Plan
- Routine labs, including complete blood count (CBC) and BMP, are checked at various intervals following surgery, and the frequency will depend on the patient's overall condition and
- Formal radiographs depending on surgeon preference (essential post hemiarthroplasty to ensure the joint is reduced and in an ideal position
- Postoperative antibiotics as per hospital protocol
- Venous thromboembolism prophylaxis as per hospital protocol
- Mobilize full weight bearing as pain allows with physiotherapists (partial or touch weight bearing for cannulated screws and for comminuted fractures managed with an IM Nail)
- Follow-up depending on surgeon preference
- Complications
General Surgical Risks
- Infection (antibiotics are usually given at induction with two postoperative doses)
- Neurovascular injury
- Anesthetic risks
- MI/Stroke/Death
Specific Risks
Sepsis can occur in up to 20% of cases and can result from superficial or deep infection. Healthcare professionals believe the presence of hematoma increases this risk. [32] [33]
Fixation Failure
This is more likely to occur in patients with pathological bone, for example, as a result of rheumatoid arthritis or osteoporosis. It can occur as a result of technical errors while operating. Loosening or dislocation can occur following a hemiarthroplasty. [34]
It is estimated that there is a 4.5% risk of fracture in hemiarthroplasty procedures. They are most likely to occur on reduction of the hip and commonly affect the neck or greater trochanter. [35]
VTE/DVT/Blood clots
Fat Embolism
As discussed, this is a potential complication of pressurizing cemented stems and nailing. Hypoxia may be noted during pressurization or on the reduction of the hip. The risk can be minimized by adequate lavage and drying of the femoral canal.
Leg Length Discrepancy
This can occur with any of the procedures. A small difference can usually be managed with a shoe lift if problematic. [1]
Non-Union (DHS/IM nail)
Patients may re-present with groin or buttock pain approximately 12 months following fixation. Pain is worse on hip extension or with weight bearing. It is thought to affect up to 25% of displaced fractures and 5% of undisplaced fractures. Management is either with total hip replacement in the elderly or consideration for proximal femoral osteotomy in the young.
Dislocation
This is a specific complication of hemiarthroplasty. In general, THA for treating femoral neck fracture demonstrates a higher relative postoperative dislocation rate than patients undergoing an elective, primary THA procedure.
Avascular Necrosis
This can occur in up to 10% of undisplaced fractures and 30% to 45% of displaced fractures. Patients typically present with groin pain; there may be signs of sclerosis on radiographs. Management typically involves conversion to a total hip replacement, but alternatives such as osteotomy or core decompression may be considered in younger patients. [36]
There is an incidence of 5% to 30%. Varus malreduction following cannulated screw fixation correlates with fixation failure.
Fixation Failure Rates
- Rates stabilize by two years postoperative
- Forty-six percent following surgical fixation versus 8% following reconstruction techniques (THA or hemiarthroplasty)
- The failure rate is approximately 2% to 4%, respectively
- Overall failure rates are still higher in arthroplasty at a 10-year follow-up
Mortality is approximately 30% in the elderly in the first year following a fractured neck of the femur. [1]
- Clinical Significance
These are commonly performed procedures, and it is essential to understand and recognize that different fracture types and patient groups are better suited to the specific type of fixation/arthroplasty. There are some areas of debate on the finer points of the surgery, and these will be briefly considered.
Bipolar versus Unipolar Hemiarthroplasty
There is debate over the use of bipolar or unipolar implants. In bipolar implants, the femoral head is surrounded by a polyethylene liner within an acetabular shell within which it can move. Although a more expensive implant, studies suggest it confers benefits of reduced pain, less acetabular wear, and lower dislocation rates. It is also easier to convert to a total hip replacement should that be indicated in the future. Unipolar implants are simpler and less expensive. There is some evidence to suggest that over time the bipolar implant also loses movement at the inner bearing and eventually resembles a unipolar implant. [37]
Cemented versus Uncemented Hemiarthroplasty
Cemented implants give better functional and mobility-related outcomes. It also confers greater stability but does carry an increased risk of a fat embolism which can cause hypoxemia. Despite this, research suggests that cemented stems carry a higher overall survival rate. The cement acts as a grout, creating an interface to distribute the load between the smooth surface of the femoral stem and the irregularities of the bone surface. [38]
Uncemented implants carry a higher risk of periprosthetic fracture post and intra-operatively. [39] Stability is conferred from the impaction of the uncemented stem in the cancellous bone, but if the bone quality is poor, impaction will be impaired and stability reduced.
SHS Lag Screw Positioning
Tip apex distance is the sum of the distance from the tip of the screw to the apex of the femoral head on the AP and lateral views. Baumgaertner et al. [40] found that a tip apex distance of less than 20mm resulted in no occurrences of screw cut out. The aim is for a tip apex distance of less than 25 mm to minimize the risk of failure. On AP views, the law screw should be slightly inferior and slightly posterior on the lateral view. Eccentric placement is likely to cause a rotational failure of the construct. [41] The anterosuperior region is where bone quality is the poorest.
- Enhancing Healthcare Team Outcomes
Medical optimization of these patients pre-operatively and management of their medical co-morbidities postoperatively is vital for a good outcome. This could not be achieved without input from the orthogeriatric/medical teams. Physiotherapists and occupational therapists are also vital to safely mobilize these patients and ensure a safe discharge from the hospital. With proper physical therapy, most patients can regain function and muscle strength, but failure to comply with physical therapy can lead to disuse and numerous other complications. The primary care provider and nurse practitioner must continually follow these patients to ensure that they are ambulating without pain and not developing post-surgical complications. [Level 1 to 3 or 4]
All these disciplines must coordinate their activities, working as an interprofessional team, to achieve optimal patient outcomes with satisfactory rehabilitation and restoration of limb function. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Femoral neck fracture Image courtesy S Bhimji MD
Disclosure: Zara Hayat declares no relevant financial relationships with ineligible companies.
Disclosure: Matthew Varacallo declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Hayat Z, Varacallo M. Surgical Management of Femoral Neck Fractures. [Updated 2023 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Fractures in the elderly: when is hip replacement a necessity? [Clin Interv Aging. 2011] Review Fractures in the elderly: when is hip replacement a necessity? Antapur P, Mahomed N, Gandhi R. Clin Interv Aging. 2011; 6:1-7. Epub 2010 Dec 20.
- Outcomes following surgical management of femoral neck fractures in elderly dialysis-dependent patients. [Arch Orthop Trauma Surg. 2018] Outcomes following surgical management of femoral neck fractures in elderly dialysis-dependent patients. Puvanesarajah V, Amin R, Qureshi R, Shafiq B, Stein B, Hassanzadeh H, Yarboro S. Arch Orthop Trauma Surg. 2018 Jun; 138(6):757-764. Epub 2018 Feb 10.
- Classification of femoral neck fractures in the elderly as pathologic fractures. [Hip. 1983] Classification of femoral neck fractures in the elderly as pathologic fractures. Calandruccio RA. Hip. 1983; :9-33.
- Review Management of femoral neck fractures in the young patient: A critical analysis review. [World J Orthop. 2014] Review Management of femoral neck fractures in the young patient: A critical analysis review. Pauyo T, Drager J, Albers A, Harvey EJ. World J Orthop. 2014 Jul 18; 5(3):204-17. Epub 2014 Jul 18.
- A systematic review and meta-analysis of cemented and uncemented bipolar hemiarthroplasty for the treatment of femoral neck fractures in elderly patients over 60 years old. [Front Med (Lausanne). 2023] A systematic review and meta-analysis of cemented and uncemented bipolar hemiarthroplasty for the treatment of femoral neck fractures in elderly patients over 60 years old. Fu M, Shen J, Ren Z, Lv Y, Wang J, Jiang W. Front Med (Lausanne). 2023; 10:1085485. Epub 2023 Feb 2.
Recent Activity
- Surgical Management of Femoral Neck Fractures - StatPearls Surgical Management of Femoral Neck Fractures - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Open access
- Published: 09 February 2024
Incidence of dislocation and associated risk factors in patients with a femoral neck fracture operated with an uncemented hemiarthroplasty
- Britt Aaen Olesen 1 ,
- Susanne Faurholt Närhi 1 ,
- Thomas Giver Jensen 1 ,
- Søren Overgaard 1 , 2 ,
- Henrik Palm 1 &
- Michala Skovlund Sørensen 1
BMC Musculoskeletal Disorders volume 25 , Article number: 119 ( 2024 ) Cite this article
528 Accesses
Metrics details
Several factors might be associated with risk of dislocating following uncemented hemiarthroplasty (HA) due to femoral neck fracture (FNF). Current evidence is limited with great variance in reported incidence of dislocation (1–15%). Aim of this study was to identify the cumulative incidence of first-time dislocation following HA and to identify the associated risk factors.
We performed a retrospective cohort study of patients receiving an HA (BFX Biomet stem, posterior approach) at Copenhagen University Hospital, Bispebjerg, in 2010–2016. Patients were followed until death or end of study (dec 2018). Dislocation was identified by code extraction from the Danish National Patient Registry.
Variables included in the multivariate model were defined pre-analysis to include: age, sex and variables with a p -value < 0.1 in univariate analysis. A regression model was fitted for 90 days dislocation as the assumption of proportional hazard rate (HR) was not met here after.
We identified 772 stems (some patients occurred with both right and left hip) and 58 stems suffered 90 dislocations during the observation period, resulting in a 7% (CI 5–9) incidence of dislocation 90 days after index surgery. 55 of the 58 stems (95%) experienced the first dislocation within 90 days after surgery.
Only absence of dementia was identified as an independent protective factor in the cause-specific model (HR 0.46 (CI 0.23–0.89)) resulting in a 2.4-fold cumulative risk of experiencing a dislocation in case of dementia. Several other variables such as age, sex, various medical conditions, surgery delay and surgical experience were eliminated as statistical risk factors.
We found a decrease in survival probability for patients who experienced a dislocation during follow-up.
Conclusions
The incidence of first-time dislocation of HA (BFX Biomet stem, posterior approach) in patients with a hip fracture is found to be 7% 90 days after surgery. Due to the non-existing attribution bias, we claim it to be the true incidence. Dementia was among several variables identified as the only risk factor for dislocation.
In perspective, we may consider treating patients with dementia by other methods than HA e.g., HA with cement or with a more constrained solution. Also, a surgical approach that reduce the risk of dislocation should be considered.
Peer Review reports
Hemiarthroplasty (HA) is recommended for displaced femoral neck fracture (FNF) in elderly patients by most guidelines [ 1 , 2 ]. HA is associated with risk of dislocation, and previous studies show a number of factors that affects this risk such as: cognitive function, delay in surgery, unipolar vs bipolar implant head and surgical approach (anterolateral vs. posterior) [ 3 , 4 , 5 , 6 , 20 ]. Some of these risk factors can be explained by selection bias, and a retrospective cohort study that allows for adjustments should be performed. Such studies exist but their limitations are e.g., analysis of old implants with a unipolar head [ 7 ]. which is known to lead to an increased dislocation risk compared to the use of modern bipolar heads [ 8 , 9 ].
Furthermore, there is a great variance in reported incidence of dislocation at 1% to 15% [ 3 , 10 , 11 , 20 ]. If we truly want to compare implant performance between populations, we need to investigate the crude risk for dislocation, eliminating the influence of mortality on dislocation risk and thereby determining the unbiased incidence. Also, studies need to adjust for difference in baseline characteristics that might influence the risk of a patient experiencing dislocation of a HA. High quality studies of potential risk factors for dislocation of a HA in patients with FNF are, to the best of our knowledge, none existing for reported crude risk.
A true picture of these risk factors is needed if one wish to investigate the effect of a changed surgical technique or a new implant because the analysis must correct for them [ 12 ]. Thus, there is an urgent need to map the risk factors that influence the risk of dislocation of HA in patients with FNF, so we are able to evaluate the performance of the newest implants on the market.
The study aimed to: 1) calculate the cumulative incidence of first-time dislocation following uncemented hemiarthroplasty (uHA) in patients with FNF, and 2) identify the associated crude risk factors categorized as patient, surgeon, and implant-related.
Study design
The project was a retrospective cohort study of a consecutive patient population receiving an HA (BFX Biomet stem) at Copenhagen University Hospital Bispebjerg, Denmark in 2010–2016. The time period is determined by the period in which our department solely used BFX Biomet stem for HA in patients with FNF.
Patients were followed until occurrence of death or end of the study (31.12.18), whichever came first. The patients were identified by diagnostic and procedure ICD-10 codes (see Additional file 1 ) in our surgical planning system. Events (dislocation) were identified by diagnostic and procedure ICD-10 codes (see Additional file 2 ) extracted from Danish National Patient Registry (DNPR). These archives have a high validity for outcome measures for other diseases and events, but have not been validated for HA and dislocation codes [ 13 ]. Specifically, the DNPR provides nationwide longitudinal registration of detailed, survival, administrative and clinical data [ 13 ]. The DNPR extraction includes somatic contacts at both public and private hospitals in all of Denmark ensuring the completeness of the register. The DNPR enables a follow-up rate at almost 100% and thereby there were no censoring regarding inclusion of events, which it unique for this study.
To identify events (dislocation), we used a validated algorithm proposed by Hermansen et al., developed for locating dislocations of total hip arthroplasties (THA) based on codes from the DNPR [ 14 ]. Hermansen et al. found that a combination of the correct diagnoses and procedural codes increased the sensitivity from 63 to 91%. The algorithm thereby yields a sensitivity of 91% and positive predictive value of 93% and specificity greater than 99%. Even though the algorithm was developed on dislocations of THAs, we claim it to be applicable for dislocations of HAs because both patient groups were treated by the same department and personnel in our time period 2010–2018.
Identification of cohort
Patient files were reviewed for inclusion and exclusion criteria.
The inclusion criteria were:
1) Patients with FNF treated with HA (BFX Biomet stem).
The exclusion criteria were:
1) Previously hip fracture in the same hip
2) Pathological fracture
3) Perioperatively death
4) Age under 50 years
5) Hip dysplasia diagnosis
The baseline variables expected to be intriguing were found in multiple databases but primarily in the patient chart and to ensure data completeness some variables were supplementally identified from multiple databases (Danish Anesthesia Database (DAD) and Danish Interdisciplinary Register for Hip Fractures (RKKP hip fracture)).
Patient related variables
Age (years), sex (female, male), dementia (none, manifest deficiency reported in the admission record), chronic obstructive pulmonary disease (no, yes), American Society of Anesthesiologists (ASA) score (1 + 2, 3 + 4. Supplemented by DAD), Body Mass Index (BMI) (normal, obese, underweight. Supplemented by DAD and RKKP hip fracture), alcohol overuse (false, true), residence status (home, nursing home, ‘other’ which covered relief residence, rehabilitation, retirement community and group home for elderly), side of FNF (right, left. All classified as Garden stage 3–4), date of surgery, surgery delay (calculated in hours from the time between admission note with diagnostic X-ray and operation note), type of anesthesia (spinal, epidural, general anesthesia (GA). Supplemented by DAD. If more than one type of anesthesia were used (e.g., epidural and GA) it was noted as GA), date of death.
Surgeon related variables
Surgeon and supervisor experience (classified into ‘junior’ and ‘senior’ separated by 3 years of orthopedic surgical experience as described by Palm et al. [ 15 ]. and surgeons who advanced in training during study period was taken into account. The supervisor had to be present at the start of the operation for this expertise to count).
Implant related variables
Prostheses stem size and bipolar caput size. Unfortunately, these data included groups with less than 5 patients for some subgroups and therefore these variables have been discontinued due to the small test size.
Stem design
The BFX Biomet stem is uncemented for press-fit insertion. It comes in different sizes with a collar and is made of titanium-alloy. It is fully hydroxyapatite coated surface. The bipolar head is mounted over conus with a taper -1. The stems inserted was between size 7, 9, 11, 13, 15, 17. Implant head sizes used was between 42–52 mm.
Surgical technique
All stems were inserted by a posterior surgical approach. Whenever possible suture of the joint capsule and reinsertion of the rotators were performed by osteosuture or mainly to the soft tissue if trochanter major was used. We could not find convincing data on exactly how many operations included joint capsule suture and reinsertion of the rotators, as the standard operation description in the time period contained a description of this step and this was therefore rarely changed or omitted. In addition, some operation records could not be found and data could not be obtained from another source. Therefore, we decided not to include this as a variable.
Variables were considered normally distributed, thus mean and 95% confidence level are presented. Incidence was calculated by Aalen-Johansen estimator with death considered a competing event for dislocation. A subdistribution and a cause-specific Cox model was fitted to identify net and crude independent risk factors for dislocation. The results from these models were presented as hazard ratio (HR) with 95% confidence intervals (CIs). Variables included in the multivariate model was defined pre-analysis to include: age, sex, surgical experience and variables with a p -value < 0.1 in univariate analysis. A regression model was fitted for 90 days, as the assumption of proportional hazard rate was not met here after. Cumulative incidence function was used to identify risk of dislocation, and Grays test to identify any difference between strata. Kaplan Meier analysis was used for survival estimation and difference for survival in strata was evaluated by log-rank test.R3.2
Participants
The data extraction from our surgical planning system revealed that 812 patients received 848 BFX Biomet stems as treatment for a FNF in 2010–2016 at Copenhagen University Hospital Bispebjerg, Denmark. Thus 36 patients occurred twice with both right and left hip in the inclusion period, and this is why the term stem is used from now on instead of patients. In total 76 stems were excluded thus leaving 772 stems for further analysis, see Fig. 1 .
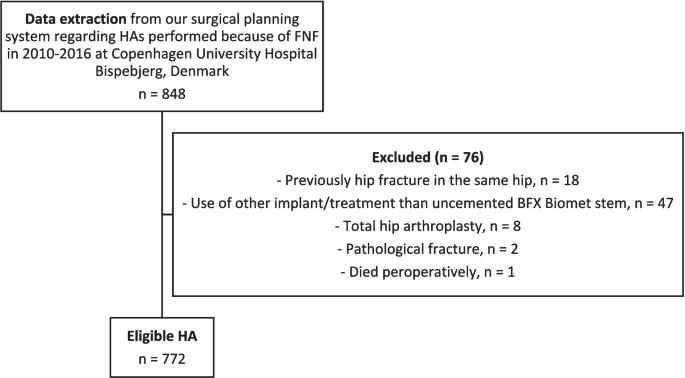
Flowchart providing an overview of data cleaning of the data extracted from our surgical planning system
Patient demographics
In general, patients without and with a dislocation exhibited similar distributions in terms of: age, year of surgery, sex, BMI, alcohol consumption, cases of chronic obstructive pulmonary disease, ASA score, surgery delay, highest surgeon or supervisor experience and type of anesthesia.
However, patients with a dislocation were more likely to: succumb to death, suffer from manifest dementia and live with some sort of assistance. See Table 1 for full information.
We identified 90 dislocations in 58 stems during the observation period. Mean time for first-time dislocation was 61 days (range: 0–1031 days). Fifty-five of the 58 patients (95%) experienced the first-time dislocation within 90 days after surgery. This resulting in an incidence of first-time dislocation of 7% (CI: 5–9%) 90 days after surgery, and this increasing to 8% (CI: 6–9%) 8 years after surgery. See Fig. 2 .
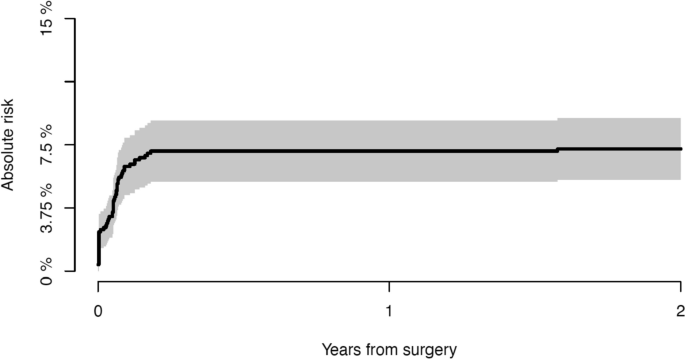
Cumulative incidence of experiencing a first-time dislocation within the first 2 years after surgery Risk factors.
- Risk factors
A regression model was fitted for 90 days as hazard rate was not found to be constant after this point including the pre-analysis defined variables. Dementia and residence status were found as independent risk factors in subdistribution model (dementia: HR 0.46 (CI: 0.22–0.92), residence ‘other’: HR 2.04 (CI: 1.00–4.14)). Only absence of dementia was identified as an independent protective factor in the cause-specific model (HR 0.46 (CI: 0.23–0.89)). Other variables that had a p -value < 0.1 in univariate analysis included: surgical experience, ASA score, sex, age and stem size. But the subdistribution model showed all of these to be without association with experiencing a dislocation. See Table 2 for full cause-specific model analysis. See Additional file 3 for both full subdistribution model and cause-specific model analysis.
Patients with manifest dementia showed a 2.4-fold cumulative risk of experiencing a dislocation. The risk of experiencing a dislocation among patients with dementia was 12% (CI: 8–16%) vs only 5% (CI: 3–7%) among patients without dementia at 90 days after surgery ( p < 0.001), see Fig. 3 .
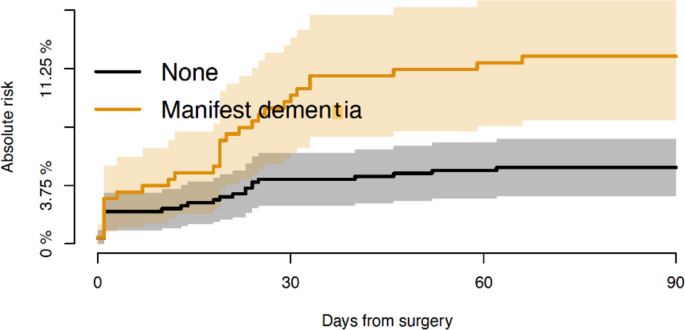
Absolute risk of dislocation for patients without and with dementia within 90 days after surgery
- Survival probability
Mean follow-up for patients alive at end of study was 73 months (range: 25–124), and 24 months (range: 0–101) for patients succumbed to disease during follow-up. Overall survival 1 year after surgery was 66% (CI: 62–69%). Survival 1 year after surgery for patients without and with a dislocation was respectively 68% (CI: 64–71) and 41% (CI: 29–54), ( p < 0.001). So generally, there was a decrease in survival observed for patients who experienced a dislocation during follow-up. See Fig. 4 .
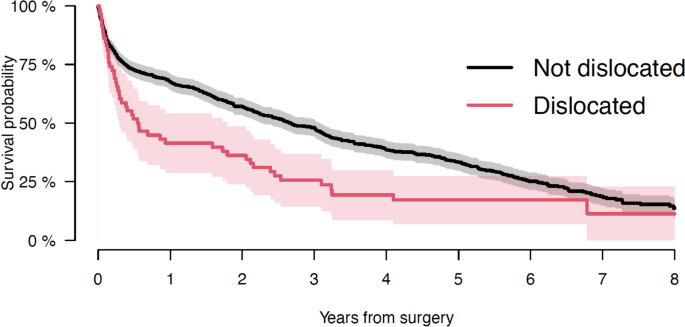
Survival probability of patients without and with dislocation of HA seen in years from surgery
In current study, we identified the cumulative incidence of first-time dislocation to be 7% (CI: 5–9%) 90 days after surgery for uncemented HA performed through a posterior approach. Our cohort comprised a complete population as the social health care system in our country eliminates bias in referral. Dislocations were identified from an algorithm by Hermansen et al. [ 14 ]. ensuring high validity from the DNPR. The DNPR contains all of our cohort except if the patient moved outside Denmark, which is extremely rare in this patient population. Due to these two aspects, we claimed our established 7% risk 90 days after surgery to be the true incidence of dislocation for patients undergoing HA with a BFX Biomet stem because of FNF performed with a posterior approach. Our findings suggested a shift in the incidence of dislocation with a cuff of at 90 days. We therefore hypothesize that causes for dislocation were different before and after the 90 days milestone. This 90 days phenomenon aligns with observations by Salem et al., who reported that 81% of dislocations in their study occurred in the first 6 weeks after surgery [ 16 ].
Manifest dementia emerged as the sole prognostic risk factor for dislocation, increasing the risk 2.4 times. Falsetto et al. [ 20 ] found that presence of dementia was associated with a 1.8-fold increased risk of dislocation comparable to our findings. This elevated risk found in people with dementia may be explained by patients being less able to understand and follow a postoperative mobility regime, they move more freely and risky because they do not understand the change in joint function and they have a high risk of recurrent falls [ 24 ].
We identified death as a competing risk factor for experiencing a dislocation. This is important as present literature does not account for the high mortality observed in this patient population and they report dislocation-free survival by net failure (Kaplan Meier estimates) [ 17 ]. making comparison of implant performance difficult as survival influence the risk of dislocation in different cohorts. Moreover, some of the known risk factors for dislocation can be explained by selection bias and present studies are limited by 1) univariate analysis methods used to identify the risk factors which do not adjust for confounding [ 18 ] and 2) attrition bias [ 19 ] both factors our study is not limited by.
The most surprising variable that was not identified as a risk factor was the surgical experience, but we found no correlation between low surgical training or absence of supervisor and risk of later dislocation. This is in coherence to other studies of FNF patients [ 28 ]. Even though the supervisor had to be present at the start of the operation for this expertise to count, we had to suspect a degree of underreporting which may explain this phenomenon. Previous studies have stated that surgeries performed by unsupervised junior surgeons were an independent risk factor for reoperation of the more complex FNFs [ 15 ].
We found an excess mortality in patients who experienced a dislocation of their HA compared to those without dislocation. The survival probability 1 year after surgery for patients not experiencing dislocation was 27% higher compared to patients experiencing dislocation. Due to the non-existing attrition bias because of thorough survival registries in our country, the validity of competing risk and survival analysis in this current study was unique. The decrease in survival may be explained by the fact that a dislocation triggers an admission and thus the risk of a nosocomial infection or the associated anaesthesia may affect the patient’s general health. Another explanation might by that the dislocation results in a temporary impairment of function. Falsetto et al. has similarly observed this trend and they explained it by the fragile patient group [ 20 ]. We advocate that in future studies a greater awareness of dislocations association to change in survival is in scope.
Limitations and strengths
An overall limitation of this study was underreporting. Even though we tried to complete the data of baseline variables by searching multiple databases and supplementing them with each other some data was just not recorded thus missing in the multivariate analysis. This may lead to underpower in analysis.
There was a potential underreporting of dislocation ICD-10 coding because a ‘closed reposition of dislocation’ code does not exist and because closed repositions could be performed in emergency departments without a hospital admission [ 21 ]. However, we feel confident that the validity of the DNPR coding shown for total hip replacement [ 14 ]. ensures a positive predictive value of 96.6% and a negative predictive value of 99.8% for our cohort as well and thereby limiting this reporting bias.
Another limitation was the opt-out of radiographic findings and thereby component positioning as this could have influenced the result as shown for total hip replacement surgery [ 21 ].
Regarding the study design the retrospective non-randomized design of this study limited the strength of evidence of our findings. But the population-based design was a strength, as no loss to inclusion limited our study and the results were thus applicable for a general Scandinavian population.
We exclusively used a posterior approach for stem insertion. Studies have shown this choice to increase the risk of dislocation compared to the direct anterior, anterolateral and the newer SPAIRE approach. The most common used approaches are the anterolateral and posterior [ 3 ]. where the anterolateral approach has a reported incidence of dislocation between 0 and 3,3% [ 3 ]. The direct anterior approach has an incidence between 0 and 2% [ 26 ]. The newer ‘Saving Piriformis And Internus, Repair of Externus’ approach is a muscle sparing mini-posterior approach and it has an incidence at 0,3% [ 27 ]. With this variance in dislocation incidence in mind our findings were only relatable to a population of patients undergoing the posterior surgical approach. However, in most cases in our cohort the operations included suture of the joint capsule and reinsertion of the rotators, which increases the stability of the prosthesis despite the posterior approach.
Also, as we only included a single stem (BFX Biomet) our results may not be valid for other stems. We did, however, provide the cumulative incidence of dislocation making our results a reliable reference for comparison of dislocation risk between stems in unrelated cohorts which is an advance and strength in this current study.
Perspectivation
In a clinical context, we wanted to use our findings to optimize the risk of experiencing a dislocation of a HA in patients with a FNF, and since dementia was the only risk factor, our focus lay here. Since patients with dementia often have been excluded from previous trials and the ageing population contains an increasing number of patients with dementia, it was of great importance to look at this patient group [ 22 , 23 ]. In perspective, we may consider to treat patients with dementia by other methods than HA e.g., HA with cement to allow for optimal stem insertion based on a trial reduction, or with a more constrained solution such as dual mobility cup [ 24 , 25 ]. Also, another surgical approach should be considered, as the posterior approach is known to massively increase the risk of dislocation [ 5 ].
The cumulative incidence of first-time dislocation of HA (BFX Biomet stem, posterior surgical approach) in patients with FNF is found to be 7% 90 days after surgery. Dementia is among several variables identified as the sole risk factor, and death is established as a competing risk factor for dislocation. We found an excess mortality in patients who experienced a dislocation of their HA compared to those without dislocation. We advocate that in future studies a greater awareness of dislocations association to change in survival is in scope.
In perspective, we may consider to treat patients with dementia by other methods than HA e.g., HA with cement or with a more constrained solution such as dual mobility cup. Also, another surgical approach should be considered, as the posterior approach is known to massively increase the risk of dislocation.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
American society of anesthesiologists’ score
Body mass index
Confidence interval
Danish Anesthesia Database
Danish National Patient Registry
- Femoral neck fracture
General anesthesia
Hemiarthroplasty
Hazard ratio
Danish Interdisciplinary Register for Hip Fractures
Total hip arthroplasties
Uncemented hemiarthroplasty
Palm H, Krasheninnikoff M, Jacobsen S. Surgical treatment of proximal femoral fracture. Ugeskr Laeger. 2006;168:2891–6.
PubMed Google Scholar
National Institute for Health and Care Excellence. Hip fracture: management. Clinical guideline [CG124] . National Institute for Health and Care Excellence, 2011.
Jones C, Briffa N, Jacob J, Hargrove R. The Dislocated Hip Hemiarthroplasty: Current Concepts of Etiological factors and Management. Open Orthop J. 2017;11:1200–12.
Article PubMed PubMed Central Google Scholar
Robertson GA, Wood AM. Hip hemi-arthroplasty for neck of femur fracture: What is the current evidence? World J Orthop. 2018;9(11):235–44.
Jobory A, Karrholm J, Hansson S, Akesson K, Rogmark C. Dislocation of hemiarthroplasty after hip fracture is common and the risk is increased with posterior approach: result from a national cohort of 25,678 individuals in the Swedish Hip Arthroplasty Register. Acta Orthop. 2021;92(4):413–8.
Jantzen C, Madsen CM, Lauritzen JB, Jorgensen HL. Temporal trends in hip fracture incidence, mortality, and morbidity in Denmark from 1999 to 2012. Acta Orthop. 2018;89(2):170–6.
Ninh CC, Sethi A, Hatahet M, Les C, Morandi M, Vaidya R. Hip dislocation after modular unipolar hemiarthroplasty. J Arthroplasty. 2009;24:768–74.
Article PubMed Google Scholar
Enocson A, Hedbeck CJ, Törnkvist H, Tidermark J, Lapidus LJ. Unipolar versus bipolar Exeter hip hemiarthroplasty: a prospective cohort study on 830 consecutive hips in patients with femoral neck fractures. Int Orthop. 2012;36:711–7.
Madanat R, Mäkinen TJ, Ovaska MT, Soiva M, Vahlberg T, Haapala J. Dislocation of hip hemiarthroplasty following posterolateral surgical approach: a nested case-control study. Int Orthop. 2012;36:935–40.
Zhang Y, Yao Z, Shi P, Wang C, Liu J, Yang Y, et al. Morphological risk factors associated with dislocation after bipolar hemiarthroplasty of the hip in patients with femoral neck fractures—a nested case-control study. J Orthop Surg Res. 2019;14:395.
Chan RN-W, Hoskinson J. Thompson prosthesis for fractured neck of femur. A comparison of surgical approaches. The Journal of Bone and Joint Surgery British volume. 1975;57(4):437–43.
Article CAS PubMed Google Scholar
Parker MJ. Lateral versus posterior approach for insertion of hemiarthroplasties for hip fractures: A randomised trial of 216 patients. Injury. 2015;46:1023–7.
Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–90.
Hermansen L, Viberg B, Overgaard S. Development of a diagnostic algorithm identifying cases of dislocation after primary total hip arthroplasty - based on 31,762 patients from the Danish Hip Arthroplasty Register. Acta Orthop. 2021;92(2):137–42.
Palm H, Jacobsen S, Krasheninnikoff M, Foss NB, Kehlet H, Gebuhr P, et al. Influence of surgeon’s experience and supervision on re-operation rate after hip fracture surgery. Injury. 2007;38(7):775–9.
Salem KMI, Shannak OA, Scammell BE, Moran CG. Predictors and outcomes of treatment in hip hemiarthroplasty dislocation. Orthopaedic surgery. 2014;96:446–51.
CAS Google Scholar
Sayers A, Evans JT, Whitehouse MR, Blom AW. Are competing risks models appropriate to describe implant failure? Acta Orthop. 2018;89(3):256–8.
Mukka S, Lindqvist J, Peyda S, Brodén C, Mahmood S, Hassany H, et al. Dislocation of bipolar hip hemiarthroplasty through a postero-lateral approach for femoral neck fractures: A cohort study. Int Orthop. 2015;39:1277–82.
Li L, Ren J, Liu J, Wang H, Sang Q, Liu Z, et al. What Are the Risk Factors for Dislocation of Hip Bipolar Hemiarthroplasty Through the Anterolateral Approach? A Nested Case-control Study. Clin Orthop Relat Res. 2016;474:2622–9.
Falsetto A, Dobransky J, Kreviazuk C, Papp S, Beaulé PE. Instability after hip hemiarthroplasty for femoral neck fracture: an unresolved problem. Can J Surg/J can chir. 2022;65(1):128–34.
Hermansen L, Viberg B, Hansen L, Overgaard S. “True” Cumulative Incidence of and Risk Factors for Hip Dislocation within 2 Years After Primary Total Hip Arthroplasty Due to Osteoarthritis. J Bone Joint Surg. 2021;103:295–302.
Hebert-Davies J, Laflamme G-Y, Rouleau D. Bias towards dementia: are hip fracture trials excluding too many patients? A systematic review Injury. 2012;43:1978–84.
Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112–7.
Kristoffersen MH, Dybvik E, Steihaug OM, Kristensen TB, Engesæter LB, Ranhoff AH, et al. Cognitive impairment influences the risk of reoperation after hip fracture surgery: results of 87,573 operations reported to the Norwegian Hip Fracture Register. Acta Orthop. 2020;91(2):146–51.
Adama P, Philippeb R, Ehlingera M, Rocheb O, Bonnometa F, Moléb D, et al. Dual mobility cups hip arthroplasty as a treatment for displaced fracture of the femoral neck in the elderly A prospective, systematic, multicenter study with specific focus on postoperative dislocation. Orthopaedics & Traumatology: Surgery & Research. 2012;98:296–300.
Google Scholar
Langlois J, Delambre J, Klouche S, Faivre B, Hardy P. Direct anterior Hueter approach is a safe and effective approach to perform a bipolar hemiarthroplasty for femoral neck fracture: outcome in 82 patients. Acta Orthop. 2015;86(3):358–62.
Hanly RJ, Sokolowski S, Timperley AJ. The SPAIRE technique allows sparing of the piriformis and obturator internus in a modified posterior approach to the hip. Hip Int. 2017;27(2):205–9.
Lagergren J, Strømrönnquist S, Wolf O, Mukka S, Möller M, Nåtman J, et al. The different strategies in treating displaced femoral neck fractures: mid-term surgical outcome in a register-based cohort of 1,283 patients aged 60–69 years. Acta Orthop. 2023;94:505–10.
Download references
Acknowledgements
We acknowledge all the surgeons who participated in this study making an effort in detailed describing the surgical intervention and recoding variables. We express a great gratitude to Mathilde Winther-Jensen and Marie Villumsen for statistical and epidemiological support making this study feasible. In addition, goes a thank you to the following databases: The Regions’ Clinical Quality Development Program (RKKP) with the databases ‘Danish Interdisciplinary Register for Hip Fractures’ and ‘Danish Anesthesia Database’.
Collection of some of the data came with a one-time fee, which was sponsored by the management at Copenhagen University Hospital, Bispebjerg and Frederiksberg, Department of Orthopaedic Surgery and Traumatology.
Author information
Authors and affiliations.
Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg and Frederiksberg, Nielsine Nielsens Vej 5, Staircase 6, 2. Floor, Copenhagen, NV, 2400, Denmark
Britt Aaen Olesen, Susanne Faurholt Närhi, Thomas Giver Jensen, Søren Overgaard, Henrik Palm & Michala Skovlund Sørensen
Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Blegdamsvej 3B, 2200, Copenhagen N, Denmark
Søren Overgaard
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by BAO and MSS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Britt Aaen Olesen .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval of the protocol was obtained from the ethics committee ‘Danish Patient Safety Authority’ (reference number 3–3013-2944/1) and general data protection regulation rules was ensured by ‘Capital Region of Denmark, Institutional Data Protection Agency’ (reference number P-2019–34). All methods were carried out in accordance with these guidelines and regulations. Furthermore, the study was reported in accordance with STROBE guidelines.
Regarding consent to participate does this retrospective cohort study contain human data from both alive and dead patients but the data is not personally identifiable data and no individual person’s data is used. Hence has this study been granted an exemption from requiring consent for publication. The ethics committee ‘Danish Patient Safety Authority’ (reference number 3–3013-2944/1) has given this consent waiver.
Consent for publication
Not applicable as this manuscript includes no identifiable information and/or media to an individual person.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., additional file 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Olesen, B., Närhi, S., Jensen, T. et al. Incidence of dislocation and associated risk factors in patients with a femoral neck fracture operated with an uncemented hemiarthroplasty. BMC Musculoskelet Disord 25 , 119 (2024). https://doi.org/10.1186/s12891-024-07237-z
Download citation
Received : 07 July 2023
Accepted : 28 January 2024
Published : 09 February 2024
DOI : https://doi.org/10.1186/s12891-024-07237-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Uncemented hip hemiarthroplasty
- Dislocation
- Posterior surgical approach
BMC Musculoskeletal Disorders
ISSN: 1471-2474
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 10 February 2017
A systematic review of undisplaced femoral neck fracture treatments for patients over 65 years of age, with a focus on union rates and avascular necrosis
- Dan-Feng Xu 1 ,
- Fang-Gang Bi 2 ,
- Chi-Yuan Ma 1 ,
- Zheng-Fa Wen 3 &
- Xun-Zi Cai 1
Journal of Orthopaedic Surgery and Research volume 12 , Article number: 28 ( 2017 ) Cite this article
15k Accesses
79 Citations
1 Altmetric
Metrics details
It remains unclear whether conservative treatment should be used to treat the common undisplaced femoral neck fractures that develop in the elderly. Herein, we systematically review the rates of union and avascular necrosis after conservative and surgical treatment of undisplaced femoral neck fractures.
We searched the EMBASE, PubMed, OVID, Cochrane Library, Web of Science, and Scopus databases for randomized controlled trials or observational studies that assessed the outcomes of conservative or surgical treatments of undisplaced femoral neck fractures. No language or publication year limitation was imposed. Statistical analyses were performed with the aid of the chi-squared test. We evaluated the quality of each publication and the risk of bias.
Twenty-nine studies involving 5071 patients were ultimately included; 1120 patients were treated conservatively and 3951 surgically. The union rates were 68.8% (642/933) and 92.6% (635/686) in the former and latter groups, respectively ( p < 0.001). The avascular necrosis rate in the conservatively treated group was 10.3% (39/380), while it was 7.7% (159/2074) in the surgically treated group ( p = 0.09).
Conclusions
Surgery to treat undisplaced femoral neck fractures was associated with a higher union rate and a tendency toward less avascular necrosis than conservative treatment.
A femoral neck fracture (FNF) is one of the most common and devastating injuries encountered by orthopedic surgeons. Over 150,000 femoral neck fractures occur every year in the USA, and this number will double by 2050 [ 1 – 3 ]. In the Garden classification, Garden I and II fractures describe undisplaced FNFs in older patients [ 4 – 6 ]. The treatment options are conservative (bed rest with or without traction) and surgical (internal fixation) [ 7 ]. Surgical treatment was reported to be optimal [ 8 ]. However, any surgery is associated with some risk. Patients undergoing conservative treatment enjoyed good outcomes in some studies [ 9 ].
Taha et al. found that conservative therapy afforded an undisplaced FNF union rate of only 44.3% [ 10 ]. Ma et al. and Buord et al. reported that the secondary displacement rates during conservative therapy were 41 and 33%, respectively [ 11 , 12 ]. However, Raaymakers et al. found that conservative treatment was successful in 85.9% of patients [ 9 ]. Surgery also seemed to be a good option, reducing secondary displacement and the non-union rate. Phillips et al. found that the union rate after surgery was 94.4% [ 13 ]. Chen et al. reported a union rate of 94.6% [ 14 ]. However, up to 22.5% of patients experienced avascular femoral head necrosis after surgery, and a fixation failure problem was also apparent [ 13 ].
Several retrospective studies have compared surgery and conservative therapy to treat undisplaced FNF. The three studies of Bentley et al., Manninger et al., and Cserhati et al. recommended surgical treatment of undisplaced FNFs; this was associated with earlier rehabilitation, lower complication rates, and higher functional scores [ 15 – 17 ]. However, of a total of 54 undisplaced FNF patients, Helbig et al. found that 24 (44%) developed no complications at all during conservative treatment whereas 28 (52%) required surgery because of early fracture dislocation [ 18 ]. No difference between conservative and operative treatment was evident in terms of survival rate, outcome score, or patient satisfaction.
The purpose of this systematic review was to assess all available clinical data on outcomes after surgery and conservative therapy to treat undisplaced FNFs; we mainly focused on the rates of bone union, secondary displacement, and avascular necrosis (AVN).
Literature search
The following sources of data were searched up to 1 October 2016 by three reviewers (DFX, CHZ, CHM): EMBASE, PubMed, OVID, Cochrane Library, Web of Science, Scopus, using the search strategy of (((femoral neck fracture [MeSH Terms]) OR (femoral neck fracture [Title/Abstract])) AND (“Garden I” OR “Garden II” OR “undisplaced” OR “non-displaced”)) with no limitation on the year or language of publication. Bibliographies of all the retrieved articles were hand-searched. In addition, we searched Clinical Trial Registry, Current Controlled Trials, Trials Central, Centre Watch, Google Scholar, multiple Websites of orthopedic associations, and conference proceedings for gray literatures. In the papers, we reviewed the references for any other papers we may not have found.
Selection criteria
The inclusion criteria for the studies were (1) patients with an undisplaced (Garden type I or Garden type II) femoral neck fracture; (2) primarily conservative treatment; (3) primarily surgical treatment; (4) the outcomes reported at least one of the following assessments: time to union, time to weight bearing, secondary displacement, non-union, AVN, and other complications; and (5) RCTs, non-randomized or quasi-randomized controlled trials, prospective cohort trials, or retrospective comparative studies.
The exclusion criteria were (1) displaced femoral neck fracture; (2) case report, reviews, biomechanical, animal study; (3) patients and fracture that had previously been reported; (4) follow-up <6 months; and (5) sample size of <10.
Data abstraction and analysis
Three reviews (DFX, FGB, CYM) extracted relevant data and checked the accuracy independently. Specially, study design and level of evidence, patient demographics (sample size, age, gender), mean follow-up time, loss to follow-up rate, intervention (technique and treatment protocol), and outcome measurements were all abstracted. The authors of the included trials were written to identify duplicate publication and uncertain data if necessary.
The weighted kappa for the agreement on the study quality between the investigators was 0.85 (95% confidence interval (CI), 0.77–0.93).
Assessment of trial quality
Two reviewers (DFX and ZFW) independently assessed the methodological quality of each trial with the modified Critical Appraisal Skills Programme (CASP) [ 19 ]. Each trial was scored with 12 questions, for which the score was 1 for “Yes” and 0 for “No” or “Can’t tell”. Disagreement was evaluated by means of kappa ( κ ) test and resolved by discussion.
Statistical analysis
All the results were combined and present as the mean value. The rates of union, secondary displacement and non-union, avascular necrosis, bed rest-related complications, 1 year mortality and reoperation could be combined for statistical analysis. Chi-square test and Fisher’s exact test were used to detect the difference of the latter two indices between the two treatment groups. The cutoff value of statistically significant difference was adjusted as α’ = α /[( k /2) + 1] = 0.05/[(4/2) + 1] = 0.017, where k was the number of groups. The pooling of the functional assessment data sets was not attempted because of the significant variability in the criteria. Statistical analyses were performed through STATA 12.0 (Stata Corp., College Station, TX, USA).
Study identification
The initial literature search yielded 1024 articles including 466 duplicates, after the removal of which 558 articles remained. Of these, 429 were excluded because they did not fulfill our selection or exclusion criteria based on evaluation of the titles and abstracts. The full texts of the remaining 129 papers were reviewed, and 31 [ 9 – 15 , 17 , 20 – 28 ] (Fig. 1 ) were finally included; these dealt with patients with undisplaced FNFs who were managed either non-operatively or operatively. After careful inspection, we found that >50% of the patients were lost to follow-up in the study of Manninger et al. [ 16 ] Additionally, in another study, patients in the surgical group had initially received conservative therapy [ 18 ]. We excluded both studies; 29 studies thus remained.
A PRISMA flowchart illustrated the selection of studies included in our systematic review
Patient characteristics and interventions
Table 1 shows the patient characteristics and the interventions used in all trials. There were 5 prospective cohort studies [ 9 , 12 , 23 , 27 , 29 ] and 24 retrospective cohort studies [ 10 – 15 , 17 , 20 – 22 , 24 – 26 , 28 , 30 – 40 ]. Of the 29 studies, 2 [ 15 , 17 ] compared both therapies, 7 [ 9 – 12 , 26 – 28 ] explored the outcomes of conservative treatment, and 20 [ 13 , 14 , 20 – 25 , 29 – 40 ] the outcomes of surgery. The surgical options included the use of cancellous screws, single Watson-Jones nails, placement of three Knowles pins, use of a dynamic hip screw, and Smith-Petersen nails. All trials recruited >10 patients. In total, 5071 cases were included, of which 1120 were conservatively and 3951 surgically treated. The vast majority of patients were female (female/male = 3211/1280). Four papers did not indicate the gender distributions [ 27 , 32 , 35 , 39 ]. The mean follow-up duration was >28.3 months. The frequency-weighted mean age was 75.0 ± 4.8 years for the conservatively treated group and 76.5 ± 4.1 years for the surgically treated group.
Tables 2 and 3 show the outcome measurements of all trials. All trials reported secondary displacement and/or non-union rates, and those of later AVN. Fourteen studies [ 9 – 11 , 13 – 15 , 20 , 25 – 28 , 33 , 34 , 40 ] reported union rates. These were 68.8% (642/933) in those receiving conservative treatment and 92.6% (635/686) in those receiving surgical treatment. The secondary displacement rate was 30.0% (334/1112) in conservatively treated patients compared to 0.57% (12/2124) in surgically treated patients. The AVN rate was 10.3% (39/380) in conservatively treated patients compared with 7.7% (159/2074) in surgically treated patients. The re-operation rate was 22.6% (157/696) in conservatively treated patients compared with 10.6% (336/3155) in surgically treated patients. Bed rest-related complications developed in 11.4% (27/237) of conservatively treated patients compared with 4.9% (106/2149) of surgically treated ones. The 1-year mortality was 14.7% (125/852) in conservatively treated patients compared with 18% (598/3318) in surgically treated ones.
Literature quality and the risk of bias
Most studies scored moderately in terms of methodological quality. The overall score was 7.38 ± 1.37, rendering the outcomes susceptible to the risk of bias (Table 4 ). The weighted kappa for agreement on trial quality between reviewers was 0.83 [95% CI (0.72–0.92)]. The biases included:
Selection bias: The fact that few trials were typical RCTs may cause major selection bias. Inconsistencies in evaluation of the type of undisplaced FNF and patient age may constitute other sources of bias.
Performance bias: This is attributable to the lack of rehabilitation programs. No consistent method was used for early weight-bearing facilitating recovery.
Attrition bias: A small number of trials exhibited considerable loss to follow-up. Most studies reported outcomes incompletely.
Detection bias: This may possibly be caused by non-standardized or undescribed follow-up schedules.
Reporting bias: This is an intrinsic weakness of retrospective cohort studies.
In detail, we restricted the type of FNF to undisplaced fractures. Most studies contained patients with both undisplaced and displaced fractures. It was difficult to isolate data on undisplaced FNF; we therefore established strict selection and exclusion criteria to reduce selection bias as much as possible. Furthermore, differences in surgical methods increased performance bias. Inconsistencies in follow-up and loss to follow-up also increased bias. Most studies were retrospective in nature, rendering reporting bias unavoidable.
Pooled analysis
As the measurements of patient characteristics and outcomes were consistent among the trials, we pooled these to derive mean values. Overall, surgically treated patients had a shorter time to weight-bearing and a shorter hospital stay. In addition, such patients had a higher union rate, lower rates of secondary displacement and non-union, and a lower rate of bed rest-related complications.
Significant differences were evident between the surgical and the conservative treatment groups in terms of the union rate ( p < 0.001), the rates of secondary displacement and non-union ( p < 0.001), and the rate of bed rest-related complications ( p < 0.001). A trend toward a difference in the AVN rate was also apparent ( p = 0.09).
To the best of our knowledge, this is the first systematic review to focus on the optimal treatment for undisplaced FNFs. We investigated whether conservative treatment was optimal for the common problem of undisplaced FNFs in the elderly. We developed explicit inclusion and exclusion criteria, assessed the methodological quality of all studies, explored the reproducibility of all selection and assessment criteria, performed quantitative analysis, and explored possible reasons for observed differences among studies. We found data paradox and confirmed the correct data of the original paper [ 20 ]. The validity of our findings is strengthened by the fact that we strictly followed the suggestions of the Cochrane Handbook for Systematic Reviews of Interventions (version 5.0.2) and the PRISMA 2009 checklist.
One of our most important findings is that fractures that were surgically treated had higher union rates and comparable non-union rates to those treated conservatively. Obviously, fixation affords stability and stiffness, directly enhancing the strength of the femoral neck [ 41 , 42 ]. Biomechanical studies have confirmed that fracture fixation and immobilization affect the pattern of skeletogenic stem cell differentiation into osteoblasts; mechanical fixation would obviously influence neovascularization [ 43 ]. Thus, fixation promotes bone union. In some studies [ 13 – 15 , 20 ], the union rates reached 90%. Fixation failure is a rare complication after surgery to treat undisplaced fractures. The fixation failure rate in our meta-analysis was only 3.3% (45/1366).
Conservative treatment is an option for undisplaced FNFs, the advantage being that surgery is avoided, but most studies revealed a significant risk of displacement during non-operative treatment. The risk varied from 14.1 to 55.7% [ 9 – 12 , 26 – 28 ]. Verheyen et al. [ 28 ] explored the rate of secondary displacement in 105 patients. Forty-eight patients (46%) were at risk of such displacement; the patient group had a high mean age. Secondary displacement was more common in patients aged >70 years, in agreement with the data of Raaymakers [ 27 ], who reported secondary instability in 41% of patients >70 years of age. In healthy patients <70 years of age, the value was 7%. Secondary displacement is very rare after surgical treatment.
AVN is a well-recognized complication of FNFs, caused by alterations in the blood supply [ 7 , 44 ]. AVN often develops 2–3 years after treatment. We found no significant difference between the two treatment groups in terms of AVN. However, AVN tended to be less common in surgical patients. Massive rupture of the retinacular vessels may occur when the femoral head is rotated during surgery; this may trigger AVN [ 45 ]. Thus, fixation potentially adversely affects the vascularity of the femoral head [ 46 ]. On the other hand, fixation prevents micromotion of the fracture site, facilitating vascularity. In Brodetti et al.’s cadaver experimental study [ 47 ], they inserted nails or screws into various sites to observe changes in blood supply; they found that such insertions were unlikely to contribute to further devascularization of the femoral head. Bentley et al. [ 15 ] followed up patients for >3 years and found that, although no AVN occurred in the first year, AVN did develop after 2 years in both groups. The incidence did not vary greatly between those who underwent conservative (14%) and surgical (18%) treatment. Hence, follow-up is very important to AVN detection.
Re-operation to deal with complications is a commonly reported outcome measure. After conservative treatment, re-operations were principally attributable to secondary displacement and latent AVN [ 11 , 28 ]. Non-union, fixation failure, and AVN were the most common reasons for re-operation after surgical treatment [ 7 ]. The re-operation rate differed significantly ( p < 0.01) between the two treatment options. Overall, the outcomes were better after surgery. It is true that patients are exposed to extra risks (including anesthesia and bleeding) during surgery. We found no evidence suggesting that complications associated with anesthesia and surgery outweighed the increased risk of fracture-healing complications characteristic of conservative treatment. On the contrary, surgical treatment significantly reduced the risk of fracture displacement and significantly increased the union rate. Patients undergoing re-operation generally underwent hemiarthroplasty or arthroplasty [ 7 , 11 ]. Overall, surgical treatment must be recommended.
Many clinical reports on treatment outcomes have focused on surgical rather than functional outcome measures. The objective functional results of various treatments are rarely assessed. The Harris hip score (HHS) is the most common modality used to assess hip function. In one study [ 40 ] on patients aged >60 years, Yih et al. reported an HHS of 84.2 ± 5.2 for those treated via insertion of dynamic hip screws and 82.6 ± 5.1 for those undergoing osteosynthesis using cannulated screws. Some studies employed fairly crude outcome measures (pain and mobility level documented in a rudimentary manner). In a recent study of 224 patients who completed self-evaluation questionnaires >3 years after internal fixation, Rogmark et al. found that 40% reported average to severe pain when walking and 25% pain at rest. [ 25 ] Functional results are rarely assessed in those treated conservatively. In one comparative study [ 17 ], Cserhati et al. recorded the levels of pain and mobility. Of 39 patients, 5.6% (10/39) reported poorer mobility status after conservative treatment compared with 45.2% (28/62) of those who underwent surgery; 51.3% (20/39) of patients reported severe or moderate pain when weight-bearing after conservative treatment compared with 61.3% (38/62) of those who underwent surgical treatment. It thus seems that conservative treatment afforded better outcomes. In terms of mortality, this was higher (68%; 83/122) after conservative treatment than the 50.4% (63/125) after surgical treatment. Therefore, the overall outcome is better after surgical treatment.
In terms of surgery, primary hemiarthroplasty of an undisplaced FNF is a possible alternative treatment. Parker et al. [ 37 ] randomized 692 patients with undisplaced FNFs to hemiarthroplasty (346 patients) or internal fixation (346 patients). Fixation was associated with a significantly reduced operative time (43 vs. 67 min), less blood loss, and a lower 1-year mortality rate (19 vs. 26%). The additional benefits of fixation were less pain at 1 year, less reduction in mobility, and a reduced dependence on walking aids. Re-operations were required by 5.5% (19/346) of the hemiarthroplasty group and 14.5% (50/346) of the fixation group. Hui et al. [ 32 ] and Sikand et al. [ 38 ] also evaluated re-operation and mortality levels. Internal fixation was associated with lower mortality but a greater need for re-operation, compared with hemiarthroplasty. The increased risk of mortality associated with hemiarthroplasty indicates that hemiarthroplasty cannot be recommended to treat an undisplaced FNF.
A precise diagnosis is important prior to choosing a treatment option. Radiography has certain limitations when used to distinguish FNF types, which can result in misdiagnosis. A patient may in fact have a displaced FNF but be diagnosed with an undisplaced one [ 6 , 10 ]. In addition, diagnoses using the Garden classification are very inconsistent. Zlowodzki et al. [ 48 ] surveyed the preferences of orthopedic surgeons in terms of FNF classification systems and asked whether they thought they could distinguish the four different Garden fracture types. Of all surgeons, 96% felt that they could distinguish between undisplaced (Garden I/II) and displaced (Garden III/IV) fractures. However, the Garden classification system exhibits great variability. Therefore, X-rays combined with a CT scan should be routinely used for diagnosis [ 6 ].
We reviewed the conservative treatments employed [ 9 – 12 , 15 , 17 , 26 – 28 ]. Careful nursing and optimal physician management allowed gradual mobilization to commence with exercises in bed, followed by partial weight-bearing, with the aid of crutches, for ≥8 weeks after fracture. The outcomes were satisfactory [ 9 , 15 ]. However, only a few patients adhered to their rehabilitative protocols in the long term. If a patient without a comorbid condition can guarantee good compliance, conservative treatment may also be recommended. In addition, patients with surgical risks must be treated conservatively.
Our work had certain limitations: (1) Most studies were retrospective in nature. Ignoring such studies would have underpowered our analyses and negatively affected the accuracy of our findings. A future strictly designed and adequately powered RCT is essential. (2) We pooled Garden I and Garden II FNFs; their prognoses did not differ greatly. A future study could compare treatment outcomes between patients with these two types of FNF. (3) We explored possible publication bias using Begg, Egger, and funnel plots. The included studies did not meet the standards required by these methods; it was thus difficult to evaluate publication bias.
Ideally, a randomized trial would reveal whether surgical or conservative treatment should be preferred for undisplaced FNFs. We suggest that future studies should prospectively compare the outcomes and complication rates of different internal fixation techniques and conservative methods.
Surgery to treat undisplaced FNFs was associated with a higher union rate and a tendency toward reduction in the AVN rate. Careful treatment and follow-up are essential. We suggest that CT should be routinely used to assist in precise diagnosis. Follow-up should be maintained for at least 2 years, allowing AVN detection (if AVN develops) and treatment.
Abbreviations
- Avascular necrosis
Femoral neck fractures
Harris hip score
Kannus P, Parkkari J, Sievanen H, Heinonen A, Vuori I, Jarvinen M. Epidemiology of hip fractures. Bone. 1996;18(1 Suppl):57s–63s.
Article CAS PubMed Google Scholar
Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407–13.
Cooper C, Campion G, Melton 3rd LJ. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285–9.
Thomsen NO, Jensen CM, Skovgaard N, Pedersen MS, Pallesen P, Soe-Nielsen NH, et al. Observer variation in the radiographic classification of fractures of the neck of the femur using Garden’s system. Int Orthop. 1996;20(5):326–9.
Lasanianos N, Kanakaris N, Giannoudis PV. An occult acetabular fracture preceding a femoral neck fracture. Orthopedics. 2009;32(8). doi: 10.3928/01477447-20090624-28 .
Melvin JS, Mataszewski P, Scolaro J, Baldwin K, Mehta S. The role of computed tomography in the diagnosis and management of femoral neck fractures in the geriatric patient. Orthopedics. 2011;34(2):87. doi: 10.3928/01477447-20101221-18 .
Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: current management. J Orthop Trauma. 2015;29(3):121–9.
Article PubMed Google Scholar
Miller BJ, Callaghan JJ, Cram P, Karam M, Marsh JL, Noiseux NO. Changing trends in the treatment of femoral neck fractures: a review of the american board of orthopaedic surgery database. J Bone Joint Surg Am. 2014;96(17):e149. doi: 10.2106/jbjs.m.01122 .
Raaymakers EL, Marti RK. Non-operative treatment of impacted femoral neck fractures. A prospective study of 170 cases. J Bone Joint Surg Br. 1991;73(6):950–4.
CAS PubMed Google Scholar
Taha ME, Audige L, Siegel G, Renner N. Factors predicting secondary displacement after non-operative treatment of undisplaced femoral neck fractures. Arch Orthop Trauma Surg. 2015;135(2):243–9. doi: 10.1007/s00402-014-2139-9 .
Ma S, Wang K, Tong Z, Zhang M, Wang W. Outcome of non-operative management in Garden I femoral neck fractures. Inj Int J Care Inj. 2006;37(10):974–8. doi: 10.1016/j.injury.2006.04.136 .
Article Google Scholar
Buord JM, Flecher X, Parratte S, Boyer L, Aubaniac JM, Argenson JN. Garden I femoral neck fractures in patients 65 years old and older: is conservative functional treatment a viable option? Orthop Traumatol. 2010;96(3):228–34.
Google Scholar
Phillips JE, Christie J. Undisplaced fracture of the neck of the femur: results of treatment of 100 patients treated by single Watson-Jones nail fixation. Injury. 1988;19(2):93–6.
Chen WC, Yu SW, Tseng IC, Su JY, Tul YK, Chen WJ. Treatment of undisplaced femoral neck fractures in the elderly. J Trauma Inj Infect Crit Care. 2005;58(5):1035–9. doi: 10.1097/01.ta.0000169292.83048.17 .
Bentley G, TREATMENT OF. Non-displaced fractures of the femoral-neck. Clin Orthop Relat Res. 1980;152:93–101.
Manninger J, Kazar G, Salacz T, Varga A. Conservative or surgical treatment of undisplaced (impacted) femoral neck fractures? Unfallchirurgie. 1990;16(3):116–21.
Cserhati P, Kazar G, Manninger J, Fekete K, Frenyo S. Non-operative or operative treatment for undisplaced femoral neck fractures: a comparative study of 122 non-operative and 125 operatively treated cases. Injury. 1996;27(8):583–8.
Helbig L, Werner M, Schneider S, Simank HG. Garden I femoral neck fractures: conservative vs operative therapy. Orthopade. 2005;34(10):1040–5.
No authors listed. Critical Appraisal Skills Programme UK Website. http://www.casp-uk.net . Date last accessed 31 May 2013.
Chiu FY, Lo WH, Yu CT, Chen TH, Chen CM, Huang CK. Percutaneous pinning in undisplaced subcapital femoral neck fractures. Inj Int J Care Inj. 1996;27(1):53–5. doi: 10.1016/0020-1383(95)00157-3 .
Article CAS Google Scholar
Han SK, Song HS, Kim R, Kang SH. Clinical results of treatment of garden type 1 and 2 femoral neck fractures in patients over 70-year old. Eur J Trauma Emerg Surg. 2015. doi: 10.1007/s00068-015-0528-6 .
PubMed Google Scholar
Kim JW, Byun S-E, Chang JS. The clinical outcomes of early internal fixation for undisplaced femoral neck fractures and early full weight-bearing in elderly patients. Arch Orthop Trauma Surg. 2014;134(7):941–6. doi: 10.1007/s00402-014-2003-y .
Lapidus LJ, Charalampidis A, Rundgren J, Enocson A. Internal fixation of garden i and II femoral neck fractures: posterior tilt did not influence the reoperation rate in 382 consecutive hips followed for a minimum of 5 years. J Orthop Trauma. 2013;27(7):386–90.
Manohara R, Liang S, Huang D, Krishna L. Cancellous screw fixation for undisplaced femoral neck fractures in the elderly. J Orthop Surg (Hong Kong). 2014;22(3):282–6.
Rogmark C, Flensburg L, Fredin H. Undisplaced femoral neck fractures-no problems? A consecutive study of 224 patients treated with internal fixation. Injury. 2009;40(3):274–6.
Jensen J, Hogh J. Fractures of the femoral neck. A follow-up study after non-operative treatment of Garden’s stage 1 and 2 fractures. Injury. 1983;14(4):339–42.
Raaymakers EL. The non-operative treatment of impacted femoral neck fractures. Injury. 2002;33 Suppl 3:C8–14.
Verheyen CC, Smulders TC, van Walsum AD. High secondary displacement rate in the conservative treatment of impacted femoral neck fractures in 105 patients. Arch Orthop Trauma Surg. 2005;125(3):166–8. doi: 10.1007/s00402-004-0791-1 .
Watson A, Zhang Y, Beattie S, Page RS. Prospective randomized controlled trial comparing dynamic hip screw and screw fixation for undisplaced subcapital hip fractures. ANZ J Surg. 2013;83(9):679–83. doi: 10.1111/j.1445-2197.2012.06256.x .
Bjorgul K, Reikeras O. Outcome of undisplaced and moderately displaced femoral neck fractures. Acta Orthop. 2007;78(4):498–504. doi: 10.1080/17453670710014149 .
Conn KS, Parker MJ. Undisplaced intracapsular hip fractures: results of internal fixation in 375 patients. Clin Orthop Relat Res. 2004;421:249–54.
Hui AC, Anderson GH, Choudhry R, Boyle J, Gregg PJ. Internal fixation or hemiarthroplasty for undisplaced fractures of the femoral neck in octogenarians. J Bone Joint Surg Br. 1994;76(6):891–4.
Lee YS, Chen SH, Tsuang YH, Huang HL, Lo TY, Huang CR. Internal fixation of undisplaced femoral neck fractures in the elderly: a retrospective comparison of fixation methods. J Trauma. 2008;64(1):155–62. doi: 10.1097/TA.0b013e31802c821c .
Makki D, Mohamed AM, Gadiyar R, Patterson M. Addition of an anti-rotation screw to the dynamic hip screw for femoral neck fractures. Orthopedics. 2013;36(7):e865–8. doi: 10.3928/01477447-20130624-15 .
Parker M, Cawley S, Palial V. Internal fixation of intracapsular fractures of the hip using a dynamic locking plate: two-year follow-up of 320 patients. Bone Joint J. 2013;95-b(10):1402–5. doi: 10.1302/0301-620x.95b10.31511 .
Parker MJ, Raghavan R, Gurusamy K. Incidence of fracture-healing complications after femoral neck fractures. Clin Orthop Relat Res. 2007;458:175–9. doi: 10.1097/BLO.0b013e3180325a42 .
Parker MJ, White A, Boyle A. Fixation versus hemiarthroplasty for undisplaced intracapsular hip fractures. Injury. 2008;39(7):791–5. doi: 10.1016/j.injury.2008.01.011 .
Sikand M, Wenn R, Moran CG. Mortality following surgery for undisplaced intracapsular hip fractures. Injury. 2004;35(10):1015–9. doi: 10.1016/j.injury.2004.01.004 .
Stromqvist B, Hansson LI, Nilsson LT, Thorngren KG. Hook-pin fixation in femoral neck fractures. A two-year follow-up study of 300 cases. Clin Orthop Relat Res. 1987;(218):58-62.
Yih-Shiunn L, Chien-Rae H, Wen-Yun L. Surgical treatment of undisplaced femoral neck fractures in the elderly. Int Orthop. 2007;31(5):677–82. doi: 10.1007/s00264-006-0243-3 .
Upasani V, Kishan S, Oka R, Mahar A, Rohmiller M, Pring M, et al. Biomechanical analysis of single screw fixation for slipped capital femoral epiphysis: are more threads across the physis necessary for stability? J Pediatr Orthop. 2006;26(4):474–8. doi: 10.1097/01.bpo.0000217732.24041.81 .
Miyanji F, Mahar A, Oka R, Pring M, Wenger D. Biomechanical comparison of fully and partially threaded screws for fixation of slipped capital femoral epiphysis. J Pediatr Orthop. 2008;28(1):49–52. doi: 10.1097/bpo.0b013e31815a5fa4 .
Zhao F, Zhou Z, Yan Y, Yuan Z, Yang G, Yu H, et al. Effect of fixation on neovascularization during bone healing. Med Eng Phys. 2014;36(11):1436–42. doi: 10.1016/j.medengphy.2014.07.002 .
Gierer P, Mittlmeier T. Femoral neck fracture. Unfallchirurg. 2015;118(3):259–70. doi: 10.1007/s00113-014-2729-6 .
Bachiller FG, Caballer AP, Portal LF. Avascular necrosis of the femoral head after femoral neck fracture. Clin Orthop Relat Res. 2002;399:87–109.
Linde F, Andersen E, Hvass I, Madsen F, Pallesen R. Avascular femoral head necrosis following fracture fixation. Injury. 1986;17(3):159–63.
Brodetti A. The blood supply of the femoral neck and head in relation to the damaging effects of nails and screws. J Bone Joint Surg. 1960;42-B:794–801.
Zlowodzki M, Bhandari M, Keel M, Hanson BP, Schemitsch E. Perception of Garden’s classification for femoral neck fractures: an international survey of 298 orthopaedic trauma surgeons. Arch Orthop Trauma Surg. 2005;125(7):503–5. doi: 10.1007/s00402-005-0022-4 .
Download references

Acknowledgements
We thank all the corresponding authors from the included trials for their kind assistance in obtaining additional data that contributed to our systematic review. The project was funded by the National Natural Science Foundation of China (81371954,81472113). All funding sources were independent and had no influence on the study design, the data extraction, analyses, interpretation of the data, writing of this article, or in the decision to submit the article for publication.
The study was funded by the National Natural Science Foundation of China (81371954, 81472113).
Availability of data and materials
All the data of the manuscript are presented in the paper or additional supporting files.
Authors’ contributions
All authors listed have made substantial contributions to the study. XZC conceived and designed the experiments, contributed reagents/materials/analysis tools. DFX and FGB wrote the manuscript and participated in performing the experiments and analyzing the data. CYM took part in performing the experiments. ZFW participated in the analysis of data. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The corresponding author has the right to grant on behalf of all authors and does grant on behalf of all authors, a worldwide licence to the publishers and its licensees in perpetuity, in all forms, formats and media (whether known now or created in the future), to (i) publish, reproduce, distribute, display, and store the contribution, (ii) translate the contribution into other languages, create adaptations, reprints, include within collections and create summaries, extracts and/or, abstracts of the contribution, (iii) create any other derivative work(s) based on the contribution, (iv) to exploit all subsidiary rights in the contribution, (v) the inclusion of electronic links from the contribution to third party material wherever it may be located; and (vi) licence any third party to do any or all of the above.
Author information
Authors and affiliations.
Department of Orthopaedic Surgery, The Second Affiliated Hospital, School of Medicine, Zhejiang University, Jie-fang Road 88, Hangzhou, 310009, People’s Republic of China
Dan-Feng Xu, Chi-Yuan Ma & Xun-Zi Cai
Department of Orthopaedic Surgery, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, 450001, People’s Republic of China
Fang-Gang Bi
Department of Orthopaedic Surgery, The Fourth Affiliated Hospital, School of Medicine, Zhejiang University, Yiwu, 322000, People’s Republic of China
Zheng-Fa Wen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Xun-Zi Cai .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Xu, DF., Bi, FG., Ma, CY. et al. A systematic review of undisplaced femoral neck fracture treatments for patients over 65 years of age, with a focus on union rates and avascular necrosis. J Orthop Surg Res 12 , 28 (2017). https://doi.org/10.1186/s13018-017-0528-9
Download citation
Received : 22 November 2016
Accepted : 03 February 2017
Published : 10 February 2017
DOI : https://doi.org/10.1186/s13018-017-0528-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Undisplaced femoral neck fracture
- Surgical treatment
- Conservative treatment
- Secondary displacement
Journal of Orthopaedic Surgery and Research
ISSN: 1749-799X
- Submission enquiries: [email protected]
Neck of femur fractures treated with the femoral neck system: outcomes of one hundred and two patients and literature review
- Original Paper
- Open access
- Published: 11 May 2022
- Volume 46 , pages 2105–2115, ( 2022 )
Cite this article
You have full access to this open access article
- Amit Davidson 1 , 3 ,
- Shlomo Blum 3 ,
- Elad Harats 3 ,
- Erick Kachko 4 ,
- Ahmad Essa 4 ,
- Ram Efraty 4 ,
- Amos Peyser 3 &
- Peter V. Giannoudis 1 , 2
6295 Accesses
19 Citations
Explore all metrics
Introduction
The recently developed femoral neck system (FNS) for treatment of femoral neck fractures (FNF), comprises theoretical biomechanical advantages compared to other implants. The aim of this study was to validate the safety and to report outcomes of patients treated with the FNS.
A retrospective multicentric analysis of patients treated by FNS with a minimum of three months of follow-up. Details analysed from three medical centres were operative duration, estimated blood loss, initial hospitalisation duration, fixation quality as well as complications and reoperation rate. Patients who had revision surgery were compared to all other patients to identify risk factors for failure. In addition, a literature review was performed to analyse data on FNS clinical implementation and patient’s outcomes. The two data sets were combined and analysed.
One-hundred and two patients were included in this study cohort with an average follow-up of seven months (range 3–27). Ten papers were included in the literature review, reporting data on 278 patients. Overall, 380 patients were analysed. Average age was 62.6 years, 52% of the fractures were classified as Gardens 1–2. Overall, the revision rate was 9.2% (14 patients diagnosed with cut-out of implant, 10 with AVN, 8 with non-union and 8 with hardware removal). For the 102 patients in the cohort risk factors for reoperation included patients age, surgeon seniority and inadequate placement of the implant.
This study shows that FNS is a safe treatment option for FNF. Intra-operative parameters and failure rates are comparable to previously reported rates for this implant and other frequently used implants.
Similar content being viewed by others
A comparison of outcomes of locking versus non-locking plate fixation for the distal fibula fractures: a systematic review and meta-analysis
Mandeep Singh Dhillon, Rajesh Kumar Rajnish, … Amit Srivastava
Internal Fixation Versus External Fixation in Orthopaedic Implantology

Biomechanical considerations on a CT-based treatment-oriented classification in radius fractures
W. Hintringer, R. Rosenauer, … H. Krimmer
Avoid common mistakes on your manuscript.
Femoral neck fractures (FNF) are common and account for over 50% of all hip fractures [ 1 ]. Standard treatment for FNF is surgical. The surgical treatment can be either internal fixation or arthroplasty, depending on bone quality, fracture severity and patient’s age [ 2 ]. Over the past decades, great effort has been put into deciphering specific biomechanical characteristics of FNF to develop an optimised fixation construct [ 3 ]. The recently developed femoral neck system (FNS), (DePuy Synthes, Raynham, MA, USA) comprises the theoretical mechanical advantages of combining compression and anti-rotation qualities during internal fixation. The effective solution the FNS design provides, involves the screw-plate construct, allowing stronger fixation, as well as a combination of blade and anti-rotation screw, that improves axial and rotational stability. Biomechanical studies have shown axial and rotational stability superiority of FNS implant over the traditional cannulated screws (CS) and the dynamic hip screw (DHS) [ 4 , 5 ]. In addition, the FNS is relatively a minimally invasive procedure which theoretically reduces blood loss and infection risk.
There are only few reports discussing the clinical implementation of FNS [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 ]. Studies are retrospective in nature and include small number of patients. Surgical workflow and surgeons experience operating with this implant were not evaluated. Moreover, intraoperative parameters such as duration of surgery and blood loss have not been fully explored. In addition, medium- and long-term patient’s outcomes, with relation to re-operation, mechanical failure and avascular necrosis (AVN) rates, are inconclusive.
While the FNS has mechanical superiority over the traditional implants in cadaveric experiments, it is crucial to evaluate the safety and report outcomes of this new implant.
The aim of this study therefore was to investigate the outcome of patients with FNF managed with FNS in our institutions and in the published literature. Moreover, we wish to validate the safety of this implant, and compare the outcome of patients treated with FNS to other implants. Our hypothesis was that the FNS implant would demonstrate if not better, analogous results to similar implants used for fixation of FNFs.
More specifically, the study’s objectives were as follows:
Analyse data obtained from three medical centres on patient treated by FNS regarding the operative duration, estimated blood loss and initial hospitalisation duration.
Assess patients’ medium- and long-term outcomes regarding AVN, mechanical failure, re-operation rates and the associated risk factors.
Perform literature review and analyse data reported on FNS clinical implementation and patient’s outcomes.
Compare the data collected on FNS to other implants published outcome and peri-operative parameters.
Patients and methods
Data on FNF patients treated with FNS from three different medical centres, between 01 March 2019 and 01 August 2021, was retrospectively collected and analysed. Institutional review board approval, from all institutes participating in the study, was obtained. Inclusion criteria for the study were patients with FNF treated with FNS and a minimum of three month post-operative follow-up. Exclusion criteria were open fractures, evidence of pathological fracture, skeletally immature patients and revision procedure for a failed fixation. Data was collected from electronic records of each institution and included patients’ demographics and recorded comorbidities. Comorbidities were defined as six distinct categories: cardiac, neurological, chronic kidney disease, chronic lung disease, diabetes mellitus and active malignancy. Data on the initial hospitalisation was collected regarding time from admission to surgery and length of hospital stay. In addition, operation time, estimated operative blood loss, which was estimated by the surgeon at the end of the procedure and surgeon seniority, qualified orthopaedic surgeon versus a trainee were recorded. Quality of reduction was evaluated by radiographic measurements performed on initial postoperative radiographs. Measurement of the tip apex distance (TAD) [ 16 ] and Parker ratio [ 17 ] in the anterior posterior and lateral radiographs was obtained. The rationale to add the Parkers ratio was that this measurement evaluates the importance of the position of the blade in the neck and not only the position of the tip of the blade.
Fracture classification and the radiographic measurements were performed by two of the authors. Fractures were classified according to the Garden classification [ 18 ]. Fractures were considered stable if classified as types 1 and 2 and unstable for types 3 or 4.
Treatment outcome for all patient was evaluated by collecting data from the follow-up records on, follow-up duration, reports of mechanical failure of implant (cut-out), nonunion (defined as no sign of union six months after surgery) and re-operations. Re-operated patients were evaluated for the diagnostic reason for the reoperation, time interval from primary surgery and the secondary procedure performed. Patients in the cohort were divided into two groups: group (1) underwent re-operation and group (2) did not require additional surgical procedure. Groups were compared for patients’ factors (demographics and comorbidities), fracture classification and surgical procedure-related collected data in order to evaluate specific risk factors for re-operation.
Data was collected from centres which had different implants for treatment of FNF. At one centre, FNS was the only construct used for FNF fixation, whereas at the other two centres either FNS, DHS or CS were applied for internal FNF fixation. The decision which implant to use was taken by the senior surgeon. Generally, elderly patients (aged above 65) suffering from a displaced fracture (Gardens 3–4), were treated by arthroplasty, whereas younger patients were treated by internal fixation, regardless to the displacement rate of the fracture, in all centres.
Systematic review of the literature
The medical search engine employed in this study was PubMed; medical subject headings words used included FNS, femoral neck system and femur fractures. Articles reporting on FNS clinical outcomes were collected and analysed. Inclusion criteria were papers reporting on patients treated with FNS for FNF which were published in English. Case reports, biomechanical studies and non-English publications were excluded. When available, data obtained in the literature review was collected for the variables described above.
For the statistical analysis of this study, contingency data were analysed using two-tailed χ 2 test or Fisher exact test, as appropriate. Continuous variables were compared using the Student’s t test.
In the systematic literature review section, literature mean numbers were calculated as weighted means, according to each sample size proportion out of all.
One hundred twenty-five patients treated with FNS were collected from three medical centres. However, twenty-three were excluded as they did not have at least three months of post-operative follow-up. In total, 102 patients (53 male) with a mean age of 62.9 years were included in this study. Data on demographics, fracture classification, surgical time, estimated blood loss, initial hospitalisation duration and patient comorbidities is presented in Table 1 . The average follow-up was seven months (range 3 to 27). Nine patients underwent revision surgery, out of which five were due to a failure of fixation and cut-out of the blade, three due to AVN and one as a result of fracture nonunion. All patients who required re-operation were treated by hip arthroplasty. The average time interval from the initial surgery to the revision surgery was 18 weeks, ranging from two to 36 weeks. Two patients were diagnosed with AVN by magnetic resonance imaging (MRI) but did not require surgical treatment as they were diagnosed with low-grade AVN stage and had minor clinical symptoms at their last follow-up examination. One patient, 93-year-old male, was diagnosed with mechanical failure of the implant (cut-out) six weeks post- operation. This patient was bedridden before the operation and suffered from major comorbidities, therefore he was treated non-operatively.
Results comparing patients who underwent revision surgery (9) to all other patients (93) are presented in Table 2 . Significant differences between the two groups were patient age, surgeon seniority and fixation quality assessed by radiographic measurements of the Lateral Parker ratio. No correlation to fracture stability was found.
Literature review revealed 16 articles which provided data on FNS-treated patients, however, six were excluded (two were written in Chinese [ 19 , 20 ], three were biomechanical articles [ 4 , 5 , 21 ] and one was a technical note [ 22 ]). From the ten eligible articles [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 ], data on 278 patients treated with FNS was collected and included in the final analysis. Table 3 summarises the number of patients, inclusion criteria, follow-up period, complications, re-operations rate and the main conclusions of the included articles. Data on demographics, fracture classification, surgical time, estimated blood loss, initial hospitalisation duration, follow-up duration and patient-reported comorbidities of the 278 patients described in the literature is presented in Table 1 . In addition, cumulative analysis on the above variables for all 380 patients treated with FNS (102 patients described in this study and 278 from the literature review), is presented in Table 1 . Finally, data regarding postoperative complications requiring revision surgery from the literature review and the 102 patients included in this paper is summarised and presented in Table 1 .
Radiographs and descriptions of three different patients from this study cohort are presented in Figs. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 .
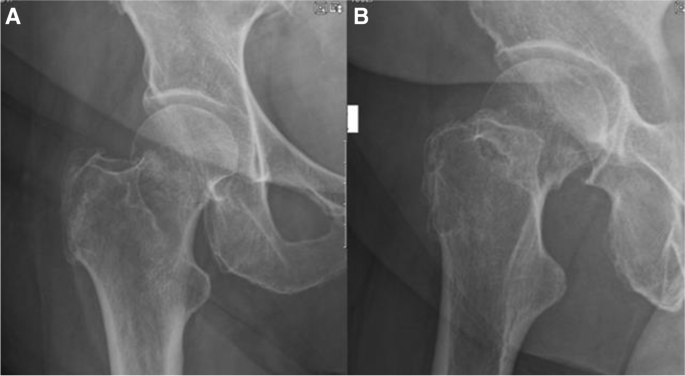
A , B AP and lateral radiographs showing intracapsular femur fracture of a 77-year-old female, which was admitted after a fall from standing height. Patient walks with no aids before the injury; her medical history consist of hypertension and dyslipidaemia
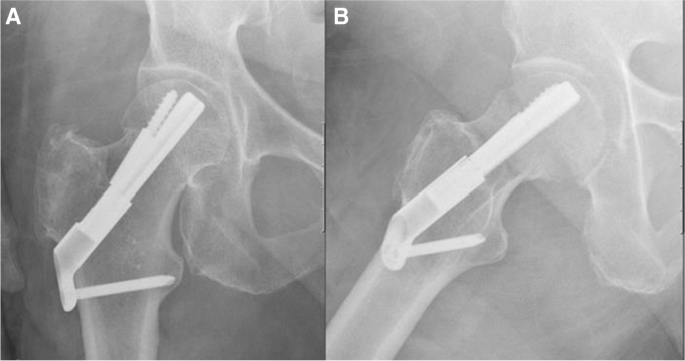
A , B AP and lateral radiographs postoperative day 1, demonstrating fixation of the fracture with FNS
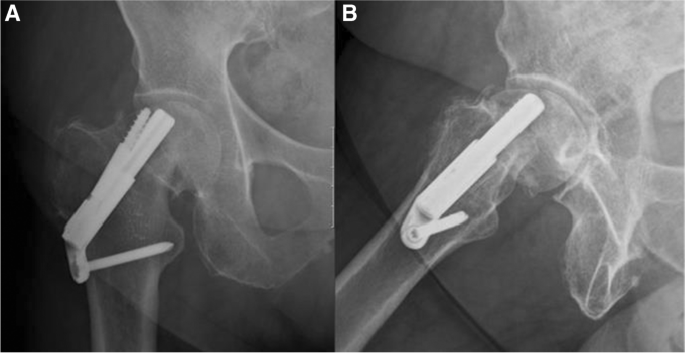
A , B AP and lateral radiographs 6 weeks after the surgical treatment. Radiographs demonstrate failure of fixation, cut-out of the implant. After the initial surgery, the patient was discharged home with instruction to full weight bear on the operated leg and was referred for physiotherapy treatment. Patient suffered from progressive hip pain and limp, walked short distance with the aid of a Zimmer frame. She was treated with revision surgery, hemiarthroplasty of the right hip
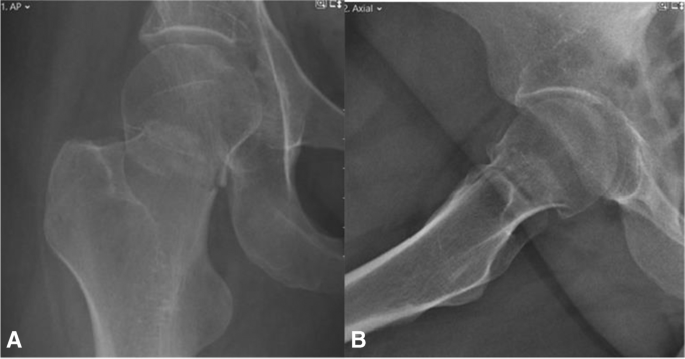
A , B AP and lateral radiographs showing intracapsular femur fracture (displaced, Garden 4) of a 39-year-old female. Past medical history consists of cerebral palsy, walks with a cane. Sustained an isolated injury to the right hip after falling from standing height

A , B AP and lateral radiographs post-operative day 1, demonstrating fixation of the fracture with FNS
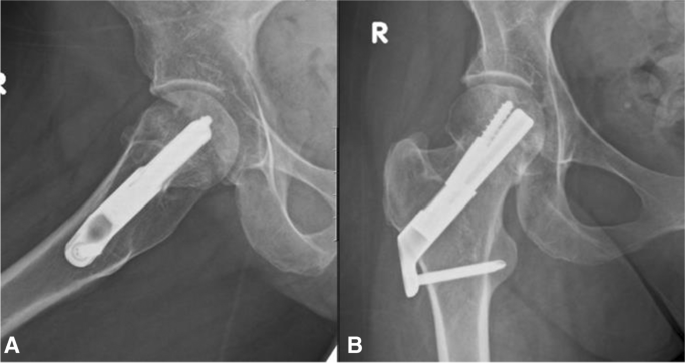
A , B AP and lateral radiographs from last follow-up 27 months after surgical treatment. Returned to her preinjury mobility status
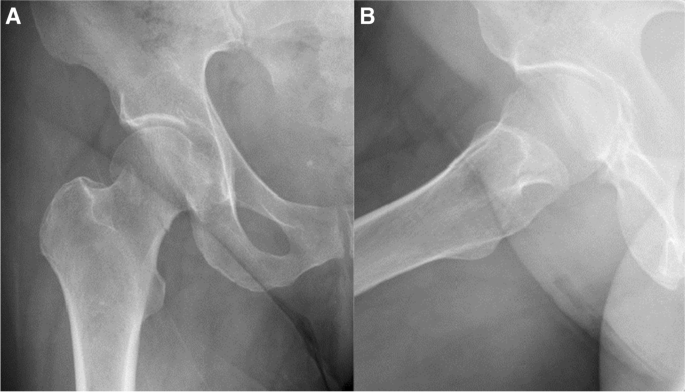
A , B AP and lateral radiographs showing right intracapsular femur fracture of a 71-year-old female. An isolated injury to the right hip after falling from own height when getting out of bed. Past medical history consists of chronic lymphocytic leukaemia, walks unaided
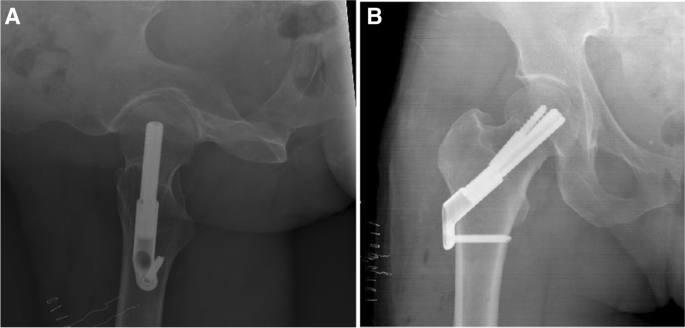
A , B AP and lateral radiographs from last follow-up, 24 months after the surgical treatment. Walks unaided, no complaints of chronic hip pain
In this study, we present data regarding 102 patients treated with FNS, and this represents the largest number of patients reported in literature to date. Adding data from previous publications enable us to analyse 380 patients treated with FNS. This study shows that FNS is a safe treatment option for FNF. Intraoperative parameters and clinical outcome of patients treated with FNS are comparable to those observed in other frequently used implants for fixation of FNF [ 23 , 24 ].
Reported reoperation rates of FNF vary; 8% for non-displaced fractures and up to 42% in displaced fractures have been reported [ 25 , 26 , 27 ]. In the FAITH study [ 24 ], a large randomised control study of FNF treated by different fixation constructs, the reoperation rate was 21%. Re-operation rate for all patients treated with FNS analysed in this study was 9.2%. In the literature review, one study showed reduced reoperation rate in the FNS group in comparison to the alternative implant [ 9 ]; in contrast, all other studies showed similar re-operation rates. The average follow-up period for this study was seven months (range 3–27). The relatively short follow-up period can be explained by the fact that the FNS was released only in 30 January 2019, and since then, it has been gradually used in our institutes. Generally, the majority of the reoperations of FNF occur in the first 12 months, in particular, re-operations related to fracture nonunion. The low number of nonunions, 1% (1/102), shown in our cohort, is an important finding and might reflect the biomechanical advantages of this implant. Longer follow-up would be ideal for exploring reoperation rates of FNFs. However, we believe that providing failure rates of a new implant, even before the desirable follow-up duration, can still provide useful information to both patients and clinicians.
Our study investigated intraoperative parameters of patients treated with FNS. The average operative time was 44 (range 21–95) minutes. This operative time is not dissimilar to other reported operative times for similar implants such as the Targon FN being 56 minutes [ 23 ]. Interestingly, three studies showed significant shorter operative time in the FNS group compared to the alternative implant [ 8 , 9 , 12 ]. One might have expected that a new implant would require longer operative time. The reported short operative time can be attributed to the low number of surgical steps in FNS which enhances procedural efficiency.
The average estimate blood loss for the FNS procedure was 47 (ml), an estimate, which is in the lower reported range for similar procedures. Fox et al. reported median intra-operative blood loss of 50 (ml) for CS and 200 (ml) for HA and DHS [ 28 ]. Other intra/peri-operative parameters which were reported for the FNS are reduced radiation exposure [ 7 , 14 , 15 ], shorter operation time [ 8 , 9 , 12 , 14 , 15 ], reduced initial hospitalisation and nonsurgical complication rate such as urinary tract infection and pneumonia [ 6 , 7 ], reduced femoral neck shortening [ 8 , 11 , 14 ] and improved functional outcome (Harris hip score) [ 11 , 14 ]. All these parameters demonstrate that the FNS is a relatively minimally invasive and operator-friendly implant.
Several predisposing factors are related to fixation failure in FNF, including female sex, increased BMI, older age, fracture type and suboptimal fracture reduction and implant positioning [ 24 ]. One of the objectives of this study was to identify risk factors for re-operation in patients treated with FNS. Our study found that patient’s age, surgeons’ seniority and precise surgical placement of implants were factors which affected the rate of re-operations. Only one other study evaluated risk factors for failure in patients treated with FNS and found patient age and presence of chronic lung disease as risk factors [ 10 ].
One of the limitations of this study is the short follow-up period. A longer follow-up period is necessary to effectively evaluate outcomes of FNF, preferably at 24 months. In addition, a larger cohort would enable assessment of the different fracture’s subgroups, displaced and non-displaced, and different patients age groups. A multi-centre randomised control study, with a long follow-up period, would be desirable to provide solid conclusions regarding the potential superiority of this implant in relation to the alternative treatment choices.
In conclusion, our hypothesis that the FNS implant would demonstrate analogous results to similar implants used for fixation of FNFs was confirmed. This study supports the view that FNS is a safe treatment option for FNF as shown in previously published literature.
Data availability
Raw data were generated from electronical records of the participating medical centres. Derived data supporting the findings of this study are available from the corresponding author [A.D] on request.
Physicians RCo (2017) National hip fracture database (NHFD) annual report 2017. In. RCP London.
Zelle BA, Salazar LM, Howard SL, Parikh K, Pape HC (2022) Surgical treatment options for femoral neck fractures in the elderly. Int Orthop. https://doi.org/10.1007/s00264-022-05314-3
Panteli M, Rodham P, Giannoudis PV (2015) Biomechanical rationale for implant choices in femoral neck fracture fixation in the non-elderly. Injury 46:445–452
Article Google Scholar
Stoffel K, Zderic I, Gras F, Sommer C, Eberli U, Mueller D, Oswald M, Gueorguiev B (2017) Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma 31:131–137
Schopper C (2018) Biomechanical evaluation of the femoral neck fracture fixation technique with the new implant FNS in comparison to DHS Blade. Universität Ulm, DHS Screw with antirotation screw and Three Cannulated Screws. In
Google Scholar
Cintean R, Pankratz C, Hofmann M, Gebhard F, Schutze K (2021) Early results in non-displaced femoral neck fractures using the femoral neck system. Geriatr Orthop Surg Rehabil 12:21514593211050150. https://doi.org/10.1177/21514593211050153
Article PubMed PubMed Central Google Scholar
He C, Lu Y, Wang Q, Ren C, Li M, Yang M, Xu Y, Li Z, Zhang K, Ma T (2021) Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet Disord 22:994. https://doi.org/10.1186/s12891-021-04888-0
Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S (2021) Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res 16:370. https://doi.org/10.1186/s13018-021-02517-z
Nibe Y, Matsumura T, Takahashi T, Kubo T, Matsumoto Y, Takeshita K (2021) A comparison between the femoral neck system and other implants for elderly patients with femoral neck fracture: a preliminary report of a newly developed implant. J Orthop Sci. https://doi.org/10.1016/j.jos.2021.04.016
Stassen RC, Jeuken RM, Boonen B, Meesters B, de Loos ER, van Vugt R (2021) First clinical results of 1-year follow-up of the femoral neck system for internal fixation of femoral neck fractures. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04216-0
Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G (2021) Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res 16:504. https://doi.org/10.1186/s13018-021-02659-0
Vazquez O, Gamulin A, Hannouche D, Belaieff W (2021) Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): short-term clinical and radiological outcomes. J Orthop Surg Res 16:477. https://doi.org/10.1186/s13018-021-02622-z
Zhou XQ, Li ZQ, Xu RJ, She YS, Zhang XX, Chen GX, Yu X (2021) Comparison of early clinical results for femoral neck system and cannulated screws in the treatment of unstable femoral neck fractures. Orthop Surg 13:1802–1809. https://doi.org/10.1111/os.13098
Zhang YZ, Lin Y, Li C, Yue XJ, Li GY, Wang B, Wang YQ, Zhu ZQ (2022) A comparative analysis of femoral neck system and three cannulated screws fixation in the treatment of femoral neck fractures: a six-month follow-up. Orthop Surg. https://doi.org/10.1111/os.13235
Niemann M, Braun KF, Ahmad SS, Stöckle U, Märdian S, Graef F (2022) Comparing perioperative outcome measures of the dynamic hip screw and the femoral neck system. Medicina (Kaunas) 58. https://doi.org/10.3390/medicina58030352
Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM (1995) The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. JBJS 77
Pervez H, Parker MJ, Vowler S (2004) Prediction of fixation failure after sliding hip screw fixation. Injury 35:994–998. https://doi.org/10.1016/j.injury.2003.10.028
Article PubMed Google Scholar
Garden RS (1961) Low-angle fixation in fractures of the femoral neck. The Journal of Bone and Joint Surgery British 43:647–663
Yan C, Wang X, Xiang C, Jiang K, Li Y, Chen Q, Deng C, Chen L (2021) Comparison of effectiveness of femoral neck system and cannulate compression screw in treatment of femoral neck fracture in young and middle-aged patients. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 35:1286–1292. https://doi.org/10.7507/1002-1892.202103099
Yang J, Zhou X, Li L, Xu L, Zhu W, Xu W, Xia R, Wang X, Wang G, Hua X, Xu X, Fang S (2021) Comparison of femoral neck system and inverted triangle cannulated screws fixations in treatment of Pauwels typle III femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 35:1111–1118. https://doi.org/10.7507/1002-1892.202102046
Fan Z, Huang Y, Su H, Jiang T (2021) How to choose the suitable FNS specification in young patients with femoral neck fracture: a finite element analysis. Injury 52:2116–2125. https://doi.org/10.1016/j.injury.2021.05.043
Cha Y, Song J-U, Yoo J-I, Park KH, Kim J-T, Park CH, Choy W-S (2021) Improved control over implant anchorage under the use of the femoral neck system for fixation of femoral neck fractures: a technical note. BMC Musculoskelet Disord 22:1–8
Parker MJ, Stedtfeld HW (2010) Internal fixation of intracapsular hip fractures with a dynamic locking plate: initial experience and results for 83 patients treated with a new implant. Injury 41:348–351. https://doi.org/10.1016/j.injury.2009.09.004
Nauth A, Creek AT, Zellar A, Lawendy A-R, Dowrick A, Gupta A, Dadi A, van Kampen A, Yee A, de Vries AC (2017) Fracture fixation in the operative management of hip fractures (FAITH): an international, multicentre, randomised controlled trial. The Lancet 389:1519–1527
Rogmark C, Carlsson A, Johnell O, Sernbo I (2002) A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur. Functional outcome for 450 patients at two years. J Bone Joint Surg Br 84:183–188. https://doi.org/10.1302/0301-620x.84b2.11923
Article CAS PubMed Google Scholar
Frihagen F, Nordsletten L, Madsen JE (2007) Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ 335:1251–1254. https://doi.org/10.1136/bmj.39399.456551.25
Oñativia IJ, Slullitel PA, Diaz Dilernia F, Gonzales Viezcas JM, Vietto V, Ramkumar PN, Buttaro MA, Piuzzi NS (2018) Outcomes of nondisplaced intracapsular femoral neck fractures with internal screw fixation in elderly patients: a systematic review. Hip Int 28:18–28. https://doi.org/10.5301/hipint.5000532
B. FN, H. K (2006) Hidden blood loss after surgery for hip fracture. The Journal of Bone and Joint Surgery British volume 88-B:1053–1059. https://doi.org/10.1302/0301-620x.88b8.17534
Download references
Author information
Authors and affiliations.
Academic Department of Trauma and Orthopaedic Surgery, School of Medicine, University of Leeds, Leeds, UK
Amit Davidson & Peter V. Giannoudis
NIHR Leeds Biomedical Research Center, Chapel Allerton Hospital, Leeds, UK
Peter V. Giannoudis
Department of Orthopaedic Surgery, Shaare Zedek Medical Center, Jerusalem, Israel
Amit Davidson, Shlomo Blum, Elad Harats & Amos Peyser
Department of Orthopaedic Surgery, Shamir (Assaf Harofeh) Medical Center, Zerifin, Israel
Erick Kachko, Ahmad Essa & Ram Efraty
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Amit Davidson .
Ethics declarations
Ethics approval.
This research study was conducted retrospectively from data obtained for clinical purposes. We consulted extensively with the IRB of SZMC and Asaf Harofeh medical centre who determined that our study did not need ethical approval. An IRB official waiver of ethical approval was granted from the IRB of SZMC, Asaf Harofeh medical centres (013–22-SZMC, ASF-0316–20).
Consent to participate
This is a retrospective anonymised data collecting data on patients treated for a common injury; the identity of the patients cannot be revealed. The ethic committee of the participating canters exempt this study form the need to obtain consent to participate.
Consent for publication
In this study, there is an X-ray image of one of the patients from the study cohort. This image purpose is to describe and visualise the paper subject. The X ray image is anonymised, and there is no concerns that the identity of this patient would be revealed. Following this journal instructions, there is no need in this case to perform informed consent from this specific patient.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Davidson, A., Blum, S., Harats, E. et al. Neck of femur fractures treated with the femoral neck system: outcomes of one hundred and two patients and literature review. International Orthopaedics (SICOT) 46 , 2105–2115 (2022). https://doi.org/10.1007/s00264-022-05414-0
Download citation
Received : 13 April 2022
Accepted : 22 April 2022
Published : 11 May 2022
Issue Date : September 2022
DOI : https://doi.org/10.1007/s00264-022-05414-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Femoral neck fractures
- Femoral neck system
- Revision rate
- Complications
- Risk factors
- Find a journal
- Publish with us
- Track your research
- Case report
- Open access
- Published: 07 June 2011
Proximal femoral fracture in a man resulting from modern clipless pedals: a case report
- James Parker 1 ,
- Neil Patel 1 &
- Ganesh Devarajan 1
Journal of Medical Case Reports volume 5 , Article number: 219 ( 2011 ) Cite this article
14k Accesses
5 Citations
2 Altmetric
Metrics details
Introduction
The use of clipless pedals amongst recreational cyclists has become increasingly popular in recent years. We describe a hip fracture, that was sustained due to inadequate set up of such pedals. To the best of our knowledge, this has only been described once before, and this was in the non-English language medical literature.
Case Report
A 38-year-old Caucasian man who was a club cyclist sustained a displaced intracapsular fracture of the hip whilst cycling. As a direct result of the incorrect set-up of his clipless pedals he was unable to release his feet whilst slowing to a halt. This resulted in a loss of balance and subsequent fall with a direct impact onto his left hip. The resulting fracture was managed successfully with early closed reduction and fixation. At six month review he was walking unaided without pain but, as yet, has been unable to return to cycling.
This case highlights the dangers of clipless pedals even in experienced cyclists, and underlines the importance of proper information for their correct setup to minimise the risk of potentially serious injuries, especially in the region of the hip.
Peer Review reports
Intra-capsular fractures of the femoral neck are extremely common in the elderly population and may be associated with relatively minor trauma. In the younger population, however, intra-capsular fractures are usually the result of high energy trauma with serious consequences of avascular necrosis of the femoral head.
We report a case of a displaced intra-capsular hip fracture in an otherwise fit and well 38-year-old Caucasian man as a direct result of his bicycle pedals being set too tight.
Case presentation
A previously healthy 38-year-old Caucasian man and competitive amateur cyclist sustained a displaced fracture of his left femoral neck following a fall from his racing bicycle whilst at rest. Having slowed gradually to a halt, our patient attempted to unclip his feet from the pedals. He was unable to unclip his feet and when the bicycle slipped on some ice, he was unable to remove his feet to steady himself. As a result he sustained a direct trauma to his left hip, resulting in a displaced intra-capsular fracture of the right femoral neck (Figure 1 , 2 ).

Pelvic radiograph view showing fracture to his left proximal femur .

Radiograph showing lateral view of his fractured left proximal femur .
Once other injuries had been excluded and adequate imaging had been obtained, our patient was admitted to our orthopedic ward and a closed reduction and internal fixation was performed later the same day. Reduction was obtained using the Leadbetter maneuver [ 1 ], and fixation performed with three 6.5 mm cannulated screws (Figure 3 , 4 ). The surgical treatment was completed within 12 hours of the injury. Subsequent to the fixation our patient progressed well with no immediate complications and was discharged two days following the injury. Toe touch weight bearing was commenced for a period of six weeks and, following satisfactory radiographs, partial weight bearing was allowed for a further six weeks.

Radiograph of his left hip six months after surgery .

Although our patient had no risk factors for osteoporosis, given the relatively low energy of the injury, a bone density scan was performed along with other metabolic bone disease screening tests. These were all within normal limits.
At a subsequent review four months after the injury, our patient had no pain in the hip, a good range of movement and is walking unaided. Radiographic appearances are satisfactory and show no evidence of avascular necrosis. Regular clinical and radiographic review is planned until two years after the injury.
To ensure efficient transfer of power from the rider to the cycle during cycling, good binding of the feet to the pedal is beneficial to prevent the foot from slipping and to allow a smooth cadence. Traditionally, this involved the use of cycling shoes with rudimentary cleats strapped into a pedal with toeclips. This, however, often required the cyclist to strap their feet so tightly that they had to physically loosen the straps by hand to disengage the pedal making it almost useless for anyone but the most proficient cyclists.
Clipless pedals were invented by Charles Hanson in 1895 but it wasn't until the 1980s that Look (France) applied downhill ski binding technology to pedals to produce the first widely used clipless pedals. The cleat is engaged by simply pushing down and forward on the pedal, or, with some designs, by twisting the cleat in sideways. Then, instead of loosening a toestrap or pulling a lever, the cyclist releases a foot from the pedal by twisting the heel outward. The force required to release the cleat from the pedal can be altered, by a tensioning mechanism, on the pedal. Competent cyclists, or those who have been using clipless pedal systems for a while, can usually find the right amount of tensioning to balance the need for quick release of the foot in an emergency against the foot disengaging the pedal while pedaling forcefully. This is usually done by trial and error. Those new to the pedals have no guide to the amount needed to tensioning the pedal. Unlike skiing, where beginners have the bindings adjusted based on weight and ability, there is no such guide readily available for bicycle pedals. As such users risk only finding out that they have over tightened the binding mechanism when they cannot release their foot in an emergency resulting in a fall and a potential injury [ 2 , 3 ].
Hip fractures are common in the elderly osteoporotic population following low energy falls. They can also occur in the young adult or even the child although they often involve a high energy type injury [ 4 ]. Intra-capsular femoral neck fractures have a high tendency (10-20%) to undergo non-union or avascular necrosis of the femoral head due to its blood supply [ 4 – 6 ]. The main blood supply to the femoral head in the adult is through the intra-osseous and capsular vessels, emanating mainly from the medial circumflex femoral artery, a branch of the profunda femoris artery. When a displaced intra-capsular fracture occurs, the blood supply to the femoral head is compromised. In the elderly, this is dealt with by replacement of the femoral head with a metal prosthesis (hemi-arthroplasty or total hip arthroplasty), with good functional outcomes [ 5 ]. However, in the active young patient, preservation of the femoral head offers a better functional outcome although survival of the head is not guaranteed [ 5 ]. It is, therefore, accepted practice that the fracture should be reduced and fixed as quickly as possible [ 4 , 5 ]. Should the fracture not heal or the head not survive then a total joint arthroplasty would then be needed. This would give the patient relief of pain but return to pre-injury activity levels is not guaranteed [ 7 ].
Hip fractures in the young are serious, but thankfully rare, injuries. They carry the potential for high long-term morbidity. The use of clipless pedals has become widespread over the last 20 years. Most injuries from clipless pedals are minor. We have described an extreme injury resulting from inappropriately tensioned pedals, which, to the best of our knowledge, has only been described once before in the non-English literature. It serves as a reminder of the importance of appropriate advice, especially from manufacturers and retailers, regarding the proper setup and dangers of using clipless pedals for the recreational cyclist. A system, similar to that used to adjust ski bindings, may help with the correct setup of such pedals.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Leadbetter GW: Closed reduction of fractures of the neck of the femur. J Bone Joint Surg (Am). 1938, 20: 108-113.
Google Scholar
Slootmans FC, Biert J, de Waard JW, de Waal Malefijt MC, Schoots FJ: Femoral neck fractures in bicyclists due to clipless pedals. Ned Tijdschr Geneeskd. 1995, 139 (22): 1141-1143. Dutch
CAS PubMed Google Scholar
Patel ND: Mountain bike injuries and clipless pedals: a review of three cases. Br J Sports Med. 2004, 38 (3): 340-341. 10.1136/bjsm.2002.003616.
Article CAS PubMed PubMed Central Google Scholar
Swiontkowski MF, Winquist RA, Hansen ST: Fractures of the femoral neck in patients between the ages of twelve and forty-nine years. J Bone Joint Surg Am. 1984, 66 (6): 837-846.
Gerber C, Strehle J, Ganz R: The treatment of fractures of the femoral neck. Clin Orthop. 1993, 292 (10): 77-86.
PubMed Google Scholar
Harty M: Blood Supply of the Femoral Head. Br Med J. 1953, 2 (4848): 1236-1237. 10.1136/bmj.2.4848.1236.
Palmer SJ, Parker MJ, Hollingworth MJ: The cost and implications of reoperation after surgery for fracture of the hip. J Bone Joint Surg (Br). 2000, 82 (6): 864-866. 10.1302/0301-620X.82B6.9974.
Article CAS Google Scholar
Download references
Author information
Authors and affiliations.
Hull and East Yorkshire NHS Trust, Hull Royal Infirmary, Anlaby Road, Hull, HU3 2JZ, UK
James Parker, Neil Patel & Ganesh Devarajan
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to James Parker .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
JP was the operating surgeon and prepared a significant part of the manuscript. NP prepared a significant part of the manuscript. GD is the senior surgeon and is responsible for the ongoing management of our patient and helped in retrieving the required information for the preparation of the manuscript. Both authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Parker, J., Patel, N. & Devarajan, G. Proximal femoral fracture in a man resulting from modern clipless pedals: a case report. J Med Case Reports 5 , 219 (2011). https://doi.org/10.1186/1752-1947-5-219
Download citation
Received : 03 July 2010
Accepted : 07 June 2011
Published : 07 June 2011
DOI : https://doi.org/10.1186/1752-1947-5-219
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Femoral Neck
- Femoral Head
- Avascular Necrosis
- Circumflex Femoral Artery
- Intracapsular Fracture
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Globally, approximately 1.3-2.2 million femoral neck fractures (FNFs) occur each year. 1 - 4 More than 50% of FNFs are intracapsular 5 and up to 80% are displaced. 6 The incidence is increasing and projected to be 3.9-7.3 million cases annually by 2050. 1 - 3, 7 - 9 Numbers of annual hip fracture cases treated are: UK 100,000, 4 ...
A case-based approach to the diagnosis and management of displaced femoral neck fractures. Discusses the current evaluation, science, techniques and common complications. A practical and user-friendly guide for orthopedic and trauma surgeons, residents and fellows. 4571 Accesses.
A displaced femoral neck fracture (FNF) in patients 55-70 years is a serious injury with a high risk of treatment failure and the optimal surgical treatment remains unclear. We aimed to describe characteristics of fracture patients compared to a sample from the normal population. Fifty patients aged 55-70 years with a displaced FNF were gender- and age- matched with a control group of 150 ...
vii Displaced femoral neck fractures are occurring more frequently and have a huge impact on our society. They are one of a few injuries in which similar patients treated in the same way can have
Fracture Pattern: Classification and Characteristics. Classification of FNF in a young patient is important for prognosis and treatment. The modified Garden classification differentiates FNFs as displaced or non-displaced (Figs. 2 and 3).Displaced fractures are at an increased risk of complications such as nonunion and osteonecrosis of the femoral head [10,11,12].
Study population. All patients signed informed consent from January 2020 to September 2021, which was approved by the ethics committee. The inclusion criteria were (1) the imaging diagnosis was femoral neck fracture, (2) the patient age ≤ 55 years old; (3) the follow-up time was longer than 12 months, (4) the fracture of the femoral neck was garden3 ~ 4 type.
In case of extremely vertical fracture patterns (Pauwels III), ... Orthopedic multidimensional prognostic index (ortho-mpi) in the elderly with hip or neck femur fracture: a pilot study. Arch Gerontol Geriatr, 58 (2014), ... Displaced femoral neck fractures in the young: significance of posterior comminution and raised intracapsular pressure ...
Femoral neck fracture (FNF) is the most common type of hip fracture in elderly patients; however, it also occurs in young patients as a result of high-energy trauma [1, 2].The number of patients with FNF continues to increase, and the number of patients with disabilities due to FNF is expected to increase to 21 million in the near future [].Owing to the high morbidity and mortality of FNF ...
Nondisplaced fractures can be managed with fixation using cannulated screw fixation. In contrast, extracapsular fractures rarely compromise the arterial blood supply to the femoral head and neck and, thus, are commonly managed with various types of surgical fixation techniques. AVN of the femoral head is very rare following extracapsular fractures.
2054 n engl j med 377;21 nejm.org November 23, 2017 The new england journal of medicine operative management.7 Mortality at 1 month after hip-fracture surgery approaches 10%.7 Pa- tients who ...
Anatomy. Physeal closure age 16. Neck-shaft angle 130° ± 7°. Anteversion 10° ± 7°. Calcar Femorale. Posteromedial dense plate of bone. Images from: Court-Brown, C. et al. Rockwood & Greens Fractures in Adults. Philadelphia: Lippincott Williams & Wilkins, 2014.
Hip fractures are a common type of fragility fracture, impacting 1.6 million individuals globally each year and more than 250,000 people annually in the United States [].The current estimates of hip fracture incidence are that it will continue increase, with the worldwide hip fracture burden expected to exceed six million by 2050 [2, 3].These fractures can lead to significant morbidity and ...
Hemiarthroplasty (HA) is recommended for displaced femoral neck fracture (FNF) in elderly patients by most guidelines [1, 2].HA is associated with risk of dislocation, and previous studies show a number of factors that affects this risk such as: cognitive function, delay in surgery, unipolar vs bipolar implant head and surgical approach (anterolateral vs. posterior) [3,4,5,6, 20].
Basicervical fractures are relatively rare compared to other femoral neck fractures, accounting for only 1.8-7.6% of all hip fractures. 3 There exists some heterogeneity in how basicervical fracture are defined, but one common definition is fractures of the base of the femoral neck that occur medially from the intertrochanteric line above the lesser trochanter. 4 There is currently limited ...
The general consensus on treating an undisplaced femoral neck fracture (FNF) with internal fixation (IF) ... comparison of internal fixation for undisplaced fracture with arthroplasty for displaced fracture: a population-based study from Danish National Registries. ... (case number 3-3013-1389/1). Statistics.
A femoral neck fracture (FNF) is one of the most common and devastating injuries encountered by orthopedic surgeons. Over 150,000 femoral neck fractures occur every year in the USA, and this number will double by 2050 [1-3].In the Garden classification, Garden I and II fractures describe undisplaced FNFs in older patients [4-6].The treatment options are conservative (bed rest with or ...
Introduction The recently developed femoral neck system (FNS) for treatment of femoral neck fractures (FNF), comprises theoretical biomechanical advantages compared to other implants. The aim of this study was to validate the safety and to report outcomes of patients treated with the FNS. Method A retrospective multicentric analysis of patients treated by FNS with a minimum of three months of ...
Intra-capsular femoral neck fractures have a high tendency (10-20%) to undergo non-union or avascular necrosis of the femoral head due to its blood supply [4-6]. The main blood supply to the femoral head in the adult is through the intra-osseous and capsular vessels, emanating mainly from the medial circumflex femoral artery, a branch of the ...