- Open access
- Published: 13 November 2019

Evidence-based models of care for the treatment of alcohol use disorder in primary health care settings: protocol for systematic review
- Susan A. Rombouts 1 ,
- James Conigrave 2 ,
- Eva Louie 1 ,
- Paul Haber 1 , 3 &
- Kirsten C. Morley ORCID: orcid.org/0000-0002-0868-9928 1
Systematic Reviews volume 8 , Article number: 275 ( 2019 ) Cite this article
7008 Accesses
3 Citations
Metrics details
Alcohol use disorder (AUD) is highly prevalent and accounts globally for 1.6% of disability-adjusted life years (DALYs) among females and 6.0% of DALYs among males. Effective treatments for AUDs are available but are not commonly practiced in primary health care. Furthermore, referral to specialized care is often not successful and patients that do seek treatment are likely to have developed more severe dependence. A more cost-efficient health care model is to treat less severe AUD in a primary care setting before the onset of greater dependence severity. Few models of care for the management of AUD in primary health care have been developed and with limited implementation. This proposed systematic review will synthesize and evaluate differential models of care for the management of AUD in primary health care settings.
We will conduct a systematic review to synthesize studies that evaluate the effectiveness of models of care in the treatment of AUD in primary health care. A comprehensive search approach will be conducted using the following databases; MEDLINE (1946 to present), PsycINFO (1806 to present), Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials (CENTRAL) (1991 to present), and Embase (1947 to present).
Reference searches of relevant reviews and articles will be conducted. Similarly, a gray literature search will be done with the help of Google and the gray matter tool which is a checklist of health-related sites organized by topic. Two researchers will independently review all titles and abstracts followed by full-text review for inclusion. The planned method of extracting data from articles and the critical appraisal will also be done in duplicate. For the critical appraisal, the Cochrane risk of bias tool 2.0 will be used.
This systematic review and meta-analysis aims to guide improvement of design and implementation of evidence-based models of care for the treatment of alcohol use disorder in primary health care settings. The evidence will define which models are most promising and will guide further research.
Protocol registration number
PROSPERO CRD42019120293.
Peer Review reports
It is well recognized that alcohol use disorders (AUD) have a damaging impact on the health of the population. According to the World Health Organization (WHO), 5.3% of all global deaths were attributable to alcohol consumption in 2016 [ 1 ]. The 2016 Global Burden of Disease Study reported that alcohol use led to 1.6% (95% uncertainty interval [UI] 1.4–2.0) of total DALYs globally among females and 6.0% (5.4–6.7) among males, resulting in alcohol use being the seventh leading risk factor for both premature death and disability-adjusted life years (DALYs) [ 2 ]. Among people aged 15–49 years, alcohol use was the leading risk factor for mortality and disability with 8.9% (95% UI 7.8–9.9) of all attributable DALYs for men and 2.3% (2.0–2.6) for women [ 2 ]. AUD has been linked to many physical and mental health complications, such as coronary heart disease, liver cirrhosis, a variety of cancers, depression, anxiety, and dementia [ 2 , 3 ]. Despite the high morbidity and mortality rate associated with hazardous alcohol use, the global prevalence of alcohol use disorders among persons aged above 15 years in 2016 was stated to be 5.1% (2.5% considered as harmful use and 2.6% as severe AUD), with the highest prevalence in the European and American region (8.8% and 8.2%, respectively) [ 1 ].
Effective and safe treatment for AUD is available through psychosocial and/or pharmacological interventions yet is not often received and is not commonly practiced in primary health care. While a recent European study reported 8.7% prevalence of alcohol dependence in primary health care populations [ 4 ], the vast majority of patients do not receive the professional treatment needed, with only 1 in 5 patients with alcohol dependence receiving any formal treatment [ 4 ]. In Australia, it is estimated that only 3% of individuals with AUD receive approved pharmacotherapy for the disorder [ 5 , 6 ]. Recognition of AUD in general practice uncommonly leads to treatment before severe medical and social disintegration [ 7 ]. Referral to specialized care is often not successful, and those patients that do seek treatment are likely to have more severe dependence with higher levels of alcohol use and concurrent mental and physical comorbidity [ 4 ].
Identifying and treating early stage AUDs in primary care settings can prevent condition worsening. This may reduce the need for more complex and more expensive specialized care. The high prevalence of AUD in primary health care and the chronic relapsing character of AUD make primary care a suitable and important location for implementing evidence-based interventions. Successful implementation of treatment models requires overcoming multiple barriers. Qualitative studies have identified several of those barriers such as limited time, limited organizational capacity, fear of losing patients, and physicians feeling incompetent in treating AUD [ 8 , 9 , 10 ]. Additionally, a recent systematic review revealed that diagnostic sensitivity of primary care physicians in the identification of AUD was 41.7% and that only in 27.3% alcohol problems were recorded correctly in primary care records [ 11 ].
Several models for primary care have been created to increase identification and treatment of patients with AUD. Of those, the model, screening, brief interventions, and referral to specialized treatment for people with severe AUD (SBIRT [ 12 ]) is most well-known. Multiple systematic reviews exist, confirming its effectiveness [ 13 , 14 , 15 ], although implementation in primary care has been inadequate. Moreover, most studies have looked primarily at SBIRT for the treatment of less severe AUD [ 16 ]. In the treatment of severe AUD, efficacy of SBIRT is limited [ 16 ]. Additionally, many patient referred to specialized care often do not attend as they encounter numerous difficulties in health care systems including stigmatization, costs, lack of information about existing treatments, and lack of non-abstinence-treatment goals [ 7 ]. An effective model of care for improved management of AUD that can be efficiently implemented in primary care settings is required.
Review objective
This proposed systematic review will synthesize and evaluate differential models of care for the management of AUD in primary health care settings. We aim to evaluate the effectiveness of the models of care in increasing engagement and reducing alcohol consumption.
By providing this overview, we aim to guide improvement of design and implementation of evidence-based models of care for the treatment of alcohol use disorder in primary health care settings.
The systematic review is registered in PROSPERO international prospective register of systematic reviews (CRD42019120293) and the current protocol has been written according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) recommended for systematic reviews [ 17 ]. A PRISMA-P checklist is included as Additional file 1 .
Eligibility criteria
Criteria for considering studies for this review are classified by the following:
Study design
Both individualized and cluster randomized trials will be included. Masking of patients and/or physicians is not an inclusion criterion as it is often hard to accomplish in these types of studies.
Patients in primary health care who are identified (using screening tools or by primary health care physician) as suffering from AUD (from mild to severe) or hazardous alcohol drinking habits (e.g., comorbidity, concurrent medication use). Eligible patients need to have had formal assessment of AUD with diagnostic tools such as Diagnostic and Statistical Manual of Mental Disorders (DSM-IV/V) or the International Statistical Classification of Diseases and Related Health Problems (ICD-10) and/or formal assessment of hazardous alcohol use assessed by the Comorbidity Alcohol Risk Evaluation Tool (CARET) or the Alcohol Use Disorders Identification test (AUDIT) and/or alcohol use exceeding guideline recommendations to reduce health risks (e.g., US dietary guideline (2015–2020) specifies excessive drinking for women as ≥ 4 standard drinks (SD) on any day and/or ≥ 8 SD per week and for men ≥ 5 SD on any day and/or ≥ 15 SD per week).
Studies evaluating models of care for additional diseases (e.g., other dependencies/mental health) other than AUD are included when they have conducted data analysis on the alcohol use disorder patient data separately or when 80% or more of the included patients have AUD.
Intervention
The intervention should consist of a model of care; therefore, it should include multiple components and cover different stages of the care pathway (e.g., identification of patients, training of staff, modifying access to resources, and treatment). An example is the Chronic Care Model (CCM) which is a primary health care model designed for chronic (relapsing) conditions and involves six elements: linkage to community resources, redesign of health care organization, self-management support, delivery system redesign (e.g., use of non-physician personnel), decision support, and the use of clinical information systems [ 18 , 19 ].
As numerous articles have already assessed the treatment model SBIRT, this model of care will be excluded from our review unless the particular model adds a specific new aspect. Also, the article has to assess the effectiveness of the model rather than assessing the effectiveness of the particular treatment used. Because identification of patients is vital to including them in the trial, a care model that only evaluates either patient identification or treatment without including both will be excluded from this review.
Model effectiveness may be in comparison with the usual care or a different treatment model.
Included studies need to include at least one of the following outcome measures: alcohol consumption, treatment engagement, uptake of pharmacological agents, and/or quality of life.
Solely quantitative research will be included in this systematic review (e.g., randomized controlled trials (RCTs) and cluster RCTs). We will only include peer-reviewed articles.
Restrictions (language/time period)
Studies published in English after 1 January 1998 will be included in this systematic review.
Studies have to be conducted in primary health care settings as such treatment facilities need to be physically in or attached to the primary care clinic. Examples are co-located clinics, veteran health primary care clinic, hospital-based primary care clinic, and community primary health clinics. Specialized primary health care clinics such as human immunodeficiency virus (HIV) clinics are excluded from this systematic review. All studies were included, irrespective of country of origin.
Search strategy and information sources
A comprehensive search will be conducted. The following databases will be consulted: MEDLINE (1946 to present), PsycINFO (1806 to present), Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials (CENTRAL) (1991 to present), and Embase (1947 to present). Initially, the search terms will be kept broad including alcohol use disorder (+synonyms), primary health care, and treatment to minimize the risk of missing any potentially relevant articles. Depending on the number of references attained by this preliminary search, we will add search terms referring to models such as models of care, integrated models, and stepped-care models, to limit the number of articles. Additionally, we will conduct reference searches of relevant reviews and articles. Similarly, a gray literature search will be done with the help of Google and the Gray Matters tool which is a checklist of health-related sites organized by topic. The tool is produced by the Canadian Agency for Drugs and Technologies in Health (CADTH) [ 20 ].
See Additional file 2 for a draft of our search strategy in MEDLINE.
Data collection
The selection of relevant articles is based on several consecutive steps. All references will be managed using EndNote (EndNote version X9 Clarivate Analytics). Initially, duplicates will be removed from the database after which all the titles will be screened with the purpose of discarding clearly irrelevant articles. The remaining records will be included in an abstract and full-text screen. All steps will be done independently by two researchers. Disagreement will lead to consultation of a third researcher.
Data extraction and synthesis
Two researchers will extract data from included records. At the conclusion of data extraction, these two researchers will meet with the lead author to resolve any discrepancies.
In order to follow a structured approach, an extraction form will be used. Key elements of the extraction form are information about design of the study (randomized, blinded, control), type of participants (alcohol use, screening tool used, socio-economic status, severity of alcohol use, age, sex, number of participants), study setting (primary health care setting, VA centers, co-located), type of intervention/model of care (separate elements of the models), type of health care worker (primary, secondary (co-located)), duration of follow-up, outcome measures used in the study, and funding sources. We do not anticipate having sufficient studies for a meta-analysis. As such, we plan to perform a narrative synthesis. We will synthesize the findings from the included articles by cohort characteristics, differential aspects of the intervention, controls, and type of outcome measures.
Sensitivity analyses will be conducted when issues suitable for sensitivity analysis are identified during the review process (e.g., major differences in quality of the included articles).
Potential meta-analysis
In the event that sufficient numbers of effect sizes can be extracted, a meta-analytic synthesis will be performed. We will extract effect sizes from each study accordingly. Two effect sizes will be extracted (and transformed where appropriate). Categorical outcomes will be given in log odds ratios and continuous measures will be converted into standardized mean differences. Variation in effect sizes attributable to real differences (heterogeneity) will be estimated using the inconsistency index ( I 2 ) [ 21 , 22 ]. We anticipate high degrees of variation among effect sizes, as a result moderation and subgroup-analyses will be employed as appropriate. In particular, moderation analysis will focus on the degree of heterogeneity attributable to differences in cohort population (pre-intervention drinking severity, age, etc.), type of model/intervention, and study quality. We anticipate that each model of care will require a sub-group analysis, in which case a separate meta-analysis will be performed for each type of model. Small study effect will be assessed with funnel plots and Egger’s symmetry tests [ 23 ]. When we cannot obtain enough effect sizes for synthesis or when the included studies are too diverse, we will aim to illustrate patterns in the data by graphical display (e.g., bubble plot) [ 24 ].
Critical appraisal of studies
All studies will be critically assessed by two researchers independently using the Revised Cochrane risk-of-bias tool (RoB 2) [ 25 ]. This tool facilitates systematic assessment of the quality of the article per outcome according to the five domains: bias due to (1) the randomization process, (2) deviations from intended interventions, (3) missing outcome data, (4) measurement of the outcome, and (5) selection of the reported results. An additional domain 1b must be used when assessing the randomization process for cluster-randomized studies.
Meta-biases such as outcome reporting bias will be evaluated by determining whether the protocol was published before recruitment of patients. Additionally, trial registries will be checked to determine whether the reported outcome measures and statistical methods are similar to the ones described in the registry. The gray literature search will be of assistance when checking for publication bias; however, completely eliminating the presence of publication bias is impossible.
Similar to article selection, any disagreement between the researchers will lead to discussion and consultation of a third researcher. The strength of the evidence will be graded according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach [ 26 ].
The primary outcome measure of this proposed systematic review is the consumption of alcohol at follow-up. Consumption of alcohol is often quantified in drinking quantity (e.g., number of drinks per week), drinking frequency (e.g., percentage of days abstinent), binge frequency (e.g., number of heavy drinking days), and drinking intensity (e.g., number of drinks per drinking day). Additionally, outcomes such as percentage/proportion included patients that are abstinent or considered heavy/risky drinkers at follow-up. We aim to report all these outcomes. The consumption of alcohol is often self-reported by patients. When studies report outcomes at multiple time points, we will consider the longest follow-up of individual studies as a primary outcome measure.
Depending on the included studies, we will also consider secondary outcome measures such as treatment engagement (e.g., number of visits or pharmacotherapy uptake), economic outcome measures, health care utilization, quality of life assessment (physical/mental), alcohol-related problems/harm, and mental health score for depression or anxiety.
This proposed systematic review will synthesize and evaluate differential models of care for the management of AUD in primary health care settings.
Given the complexities of researching models of care in primary care and the paucity of a focus on AUD treatment, there are likely to be only a few studies that sufficiently address the research question. Therefore, we will do a preliminary search without the search terms for model of care. Additionally, the search for online non-academic studies presents a challenge. However, the Gray Matters tool will be of guidance and will limit the possibility of missing useful studies. Further, due to diversity of treatment models, outcome measures, and limitations in research design, it is possible that a meta-analysis for comparative effectiveness may not be appropriate. Moreover, in the absence of large, cluster randomized controlled trials, it will be difficult to distinguish between the effectiveness of the treatment given and that of the model of care and/or implementation procedure. Nonetheless, we will synthesize the literature and provide a critical evaluation of the quality of the evidence.
This review will assist the design and implementation of models of care for the management of AUD in primary care settings. This review will thus improve the management of AUD in primary health care and potentially increase the uptake of evidence-based interventions for AUD.
Availability of data and materials
Not applicable.
Abbreviations
Alcohol use disorder
Alcohol Use Disorders Identification test
Canadian Agency for Drugs and Technologies in Health
The Comorbidity Alcohol Risk Evaluation
Cochrane Central Register of Controlled Trials
Diagnostic and Statistical Manual of Mental Disorders
Human immunodeficiency virus
10 - International Statistical Classification of Diseases and Related Health Problems
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols
Screening, brief intervention, referral to specialized treatment
Standard drinks
World Health Organization
WHO. Global status report on alcohol and health: World health organization; 2018.
The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016. a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012.
Article Google Scholar
WHO. Global strategy to reduce the harmful use of alcohol: World health organization; 2010.
Rehm J, Allamani A, Elekes Z, Jakubczyk A, Manthey J, Probst C, et al. Alcohol dependence and treatment utilization in Europe - a representative cross-sectional study in primary care. BMC Fam Pract. 2015;16:90.
Morley KC, Logge W, Pearson SA, Baillie A, Haber PS. National trends in alcohol pharmacotherapy: findings from an Australian claims database. Drug Alcohol Depend. 2016;166:254–7.
Article CAS Google Scholar
Morley KC, Logge W, Pearson SA, Baillie A, Haber PS. Socioeconomic and geographic disparities in access to pharmacotherapy for alcohol dependence. J Subst Abus Treat. 2017;74:23–5.
Rehm J, Anderson P, Manthey J, Shield KD, Struzzo P, Wojnar M, et al. Alcohol use disorders in primary health care: what do we know and where do we go? Alcohol Alcohol. 2016;51(4):422–7.
Le KB, Johnson JA, Seale JP, Woodall H, Clark DC, Parish DC, et al. Primary care residents lack comfort and experience with alcohol screening and brief intervention: a multi-site survey. J Gen Intern Med. 2015;30(6):790–6.
McLellan AT, Starrels JL, Tai B, Gordon AJ, Brown R, Ghitza U, et al. Can substance use disorders be managed using the chronic care model? review and recommendations from a NIDA consensus group. Public Health Rev. 2014;35(2).
Storholm ED, Ober AJ, Hunter SB, Becker KM, Iyiewuare PO, Pham C, et al. Barriers to integrating the continuum of care for opioid and alcohol use disorders in primary care: a qualitative longitudinal study. J Subst Abus Treat. 2017;83:45–54.
Mitchell AJ, Meader N, Bird V, Rizzo M. Clinical recognition and recording of alcohol disorders by clinicians in primary and secondary care: meta-analysis. Br J Psychiatry. 2012;201:93–100.
Babor TF, Ritson EB, Hodgson RJ. Alcohol-related problems in the primary health care setting: a review of early intervention strategies. Br J Addict. 1986;81(1):23–46.
Kaner EF, Beyer F, Dickinson HO, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007;(2):Cd004148.
O'Donnell A, Anderson P, Newbury-Birch D, Schulte B, Schmidt C, Reimer J, et al. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol. 2014;49(1):66–78.
Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165(9):986–95.
Saitz R. ‘SBIRT’ is the answer? Probably not. Addiction. 2015;110(9):1416–7.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj. 2015;350:g7647.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. Jama. 2002;288(14):1775–9.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. Jama. 2002;288(15):1909–14.
CADTH. Grey Matters: a practical tool for searching health-related grey literature Internet. 2018 (cited 2019 Feb 22).
Higgins JPT. Thompson SG. Quantifying heterogeneity in a meta-analysis. 2002;21(11):1539–58.
Google Scholar
Higgins JPT, Thompson SG, Deeks JJ. Altman DG. Measuring inconsistency in meta-analyses. 2003;327(7414):557–60.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed). 1997;315(7109):629–34.
Higgins JPT, López-López JA, Becker BJ, Davies SR, Dawson S, Grimshaw JM, et al. Synthesising quantitative evidence in systematic reviews of complex health interventions. BMJ Glob Health. 2019;4(Suppl 1):e000858–e.
Higgins, J.P.T., Sterne, J.A.C., Savović, J., Page, M.J., Hróbjartsson, A., Boutron, I., Reeves, B., Eldridge, S. (2016). A revised tool for assessing risk of bias in randomized trials. In: Chandler, J., McKenzie, J., Boutron, I., Welch, V. (editors). Cochrane methods. Cochrane database of systematic reviews, 10 (Suppl 1). https://doi.org/10.1002/14651858.CD201601 .
Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html ).
Download references
Acknowledgements
There is no dedicated funding.
Author information
Authors and affiliations.
Discipline of Addiction Medicine, Central Clinical School, Faculty of Medicine and Health, University of Sydney, Sydney, NSW, Australia
Susan A. Rombouts, Eva Louie, Paul Haber & Kirsten C. Morley
NHMRC Centre of Research Excellence in Indigenous Health and Alcohol, Central Clinical School, Faculty of Medicine and Health, University of Sydney, Sydney, NSW, Australia
James Conigrave
Drug Health Services, Royal Prince Alfred Hospital, Camperdown, NSW, Australia
You can also search for this author in PubMed Google Scholar
Contributions
KM and PH conceived the presented idea of a systematic review and meta-analysis and helped with the scope of the literature. KM is the senior researcher providing overall guidance and the guarantor of this review. SR developed the background, search strategy, and data extraction form. SR and EL will both be working on the data extraction and risk of bias assessment. SR and JC will conduct the data analysis and synthesize the results. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Kirsten C. Morley .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
PRISMA-P 2015 Checklist.
Additional file 2.
Draft search strategy MEDLINE. Search strategy.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Rombouts, S.A., Conigrave, J., Louie, E. et al. Evidence-based models of care for the treatment of alcohol use disorder in primary health care settings: protocol for systematic review. Syst Rev 8 , 275 (2019). https://doi.org/10.1186/s13643-019-1157-7
Download citation
Received : 25 March 2019
Accepted : 13 September 2019
Published : 13 November 2019
DOI : https://doi.org/10.1186/s13643-019-1157-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Model of care
- Primary health care
- Systematic review
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Case Report
- Open access
- Published: 08 November 2022
Alcohol use disorder with comorbid anxiety disorder: a case report and focused literature review
- Victor Mocanu 1 , 2 &
- Evan Wood ORCID: orcid.org/0000-0001-9412-6699 1 , 2
Addiction Science & Clinical Practice volume 17 , Article number: 62 ( 2022 ) Cite this article
4490 Accesses
1 Citations
1 Altmetric
Metrics details
Alcohol use disorder (AUD) and anxiety disorders (AnxD) are prevalent health concerns in clinical practice which frequently co-occur (AUD-AnxD) and compound one another. Concurrent AUD-AnxD poses a challenge for clinical management as approaches to treatment of one disorder may be ineffective or potentially counterproductive for the other disorder.
Case Presentation
We present the case of a middle-aged man with anxiety disorder, AUD, chronic pain, and gamma-hydroxybutyrate use in context of tapering prescribed benzodiazepines who experienced severe alcohol withdrawal episodes during a complicated course of repeated inpatient withdrawal management. After medical stabilization, the patient found significant improvement in symptoms and no return to alcohol use with a regimen of naltrexone targeting his AUD, gabapentin targeting both his AUD and AnxD, and engagement with integrated psychotherapy, Alcoholics Anonymous, and addictions medicine follow-up.
Proper recognition and interventions for AUD and AnxD, ideally with overlapping efficacy, can benefit individuals with comorbid AUD-AnxD. Gabapentin, tobacco cessation, and integrated psychotherapy have preliminary evidence of synergistic effects in AUD-AnxD. Meta-analysis evidence does not support serotoninergic medications (e.g. selective serotonin reuptake inhibitors) which are commonly prescribed in AnxD and mood disorders as their use has not been associated with improved outcomes for AUD-AnxD. Additionally, several double-blind placebo-controlled randomized trials have suggested that serotonergic medications may worsen alcohol-related outcomes in some individuals with AUD. Areas for future investigation are highlighted.
Introduction
Alcohol use disorder (AUD) is a prevalent health concern with a recent epidemiologic survey of the United States indicating a lifetime AUD prevalence of 29.1% and previous 12 month prevalence of 13.9% [ 1 ]. AUD portends an increased risk for diagnosis of a primary anxiety disorder (AnxD) [ 1 ], the definition of which, for the purposes of this case report, aligns with the most recent Canadian clinical practice guidelines for treatment of AnxD to include the DSM-IV umbrella of generalized anxiety disorder (GAD), social anxiety disorder (SAD), panic disorder, specific phobia, obsessive-compulsive disorder, and post-traumatic stress disorder (PTSD) [ 2 ]. A quarter or more of individuals with AUD qualify for dual diagnosis with a concurrent primary AnxD in cross-sectional studies [ 3 ]. Furthermore, individuals with comorbid AUD-AnxD fare worse in terms of severity, treatment response, and rate of relapse for both conditions [ 3 ]. Alcohol intoxication, withdrawal, and biopsychosocial consequences of AUD may all contribute to AnxD symptomatology and vice versa, some individuals with a primary AnxD may use alcohol as self-medication. Alternatively, these conditions may share a common neuropathophysiology influenced by environmental factors at the level of brain structures such as the amygdala and neurotransmitters including gamma aminobutyric acid (GABA), endogenous opioids, dopamine, and serotonin, with implications for clinical management [ 3 ].
We present a case report of an individual with comorbid AUD-AnxD and review literature for treatment options to aid clinicians in applying best current evidence for such individuals. Literature review consisted of relevant published studies extracted from author collections and PubMed search with no language or date restrictions for combinations of the following terms: alcohol, alcohol use disorder, anxiety, anxiety disorder, comorbidity, dual diagnosis. In addition, reference lists of selected articles were reviewed for eligible and relevant studies. We find that commonly used treatment options for either AUD or AnxD can have a range of positive and potentially negative impacts for AUD-AnxD which requires accurate understanding of evidence-based care in this area.
A middle-aged man with a longstanding but reportedly well managed history of anxiety disorder dating back to childhood presented for medicalized alcohol withdrawal management services. The individual had a workplace injury approximately 10 years prior that resulted in several spine fractures after which his anxiety deteriorated and he developed AUD. Around this time, an SSRI was trialed for AnxD over several months without benefit and ultimately discontinued. He did not endorse a history for a mood disorder, nor had he received a diagnosis as such. He went on to live with chronic pain and AUD-AnxD for half a decade at which point he had an accidental caustic ingestion resulting in an esophagectomy and jejunostomy tube feeding for one year. His AUD-AnxD subsequently deteriorated further resulting in a prescription of benzodiazepines which were taken for approximately one month until the patient experienced rebound anxiety, worsening of his AUD, and the emergence of gamma-hydroxybutyrate (GHB) use in the context of attempting to discontinue benzodiazepines. The individual sought care through an inpatient withdrawal management program where he had a number of repeated admissions complicated by alcohol withdrawal seizures. He was fortunately stabilized and benzodiazepines were tapered off at which point he was taking no other prescribed medications regularly. Prior to discharge, he was informed of AUD and AnxD treatment options. He was keen to engage with psychosocial supports while starting naltrexone 50 mg once daily and gabapentin 600 mg three times daily.
Eighteen months since discharge, he has found success engaging regularly with substance counselling, Alcoholics Anonymous, and outpatient addictions medicine as well as continuing with naltrexone and gabapentin, the majority of which were intended as synergistic treatments for AUD-AnxD (Fig. 1 ). He reports good health and no alcohol use, and although experiencing cravings, he describes feeling a shift from the sensation of “premeditated” or inevitable relapse as he had in previous attempts at reducing alcohol use.
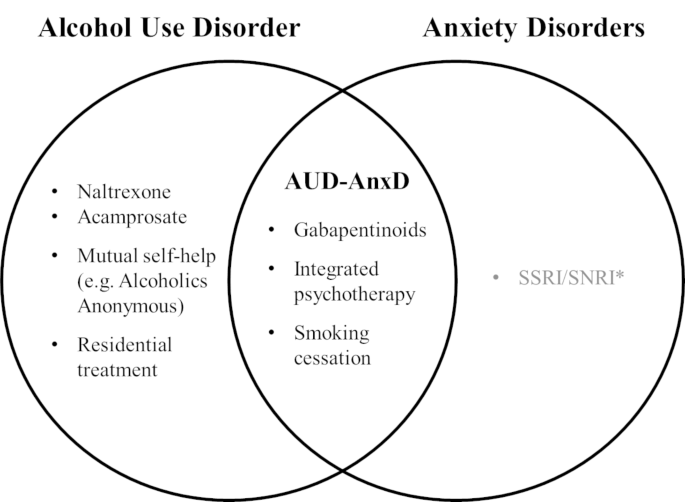
Venn diagram of current evidence-based interventions reviewed for alcohol use and anxiety disorders
AUD-AnxD indicates comorbid alcohol use disorder and anxiety disorder
* Caution to be exercised with serotoninergic agents given evidence for potential worsening of alcohol outcomes in comorbid AUD-AnxD
Patient perspective
Hi, I’m here to share with you a little bit of the trial and tribulations endured over the many years of addiction. I was an individual who had a seemingly normal life, but under this was a person with undiagnosed mental problems. I was always a drinker who could take or leave drugs, and kept steady employment and had a very loving partner, it wasn’t until an injury in 2009 when my pace with alcohol quickened and I noticed that my consumption was now an everyday affair. Slowly I developed shakes and my day would start with vomiting until I had alcohol of some variety introduced, this continued on for many years and I was now a product of full-blown alcoholism. There now was no job, no partner and very few things that resembled a person who was still an active part of society. I was in and out of hospitals for experiencing multiple seizures and would go weeks with no food or water and begun isolating. I would become so weak physically that I could not move, and would some days awake in with bruises and cuts from either sizing or pass out, I was never sure which. Then I would begin my process of detox recovery house or treatment only to get home and start the vicious cycle again, some time I could stay sober longer if I was using GHB. Nothing would stop my craving and I no longer felt human. I wanted to die… I am proud to inform you that of Dec 12 2020 I have been living a life of sobriety but continue to struggle with cravings, but I use Alcoholics Anonymous as a support and by surrounding like minded people I find myself sober today.
Alcohol use disorder and anxiety
AUD and AnxD are common clinical concerns with evidence-based treatment options. Clinicians should recognize that when two conditions such as AUD and AnxD co-occur, clinical management may require nuance and differ from an approach taken in the context of an individual disorder. As we discuss below, research specifically concerning concurrent AUD-AnxD is still rare despite its high prevalence so data must often be extrapolated. The best available evidence indicates that approaches for treating one disorder may be efficacious, ineffective, or in fact counterproductive for comorbid AUD-AnxD.
AUD treatments
It is critical to recognize and offer proper treatment for AUD even when the primary presenting concern of a client may be an AnxD and vice versa. Whether sequential treatment of AUD and then AnxD, or vice versa, could reduce polypharmacy and iatrogenic harms versus their concurrent treatment remains largely unexplored. Unhealthy alcohol use and AUD are associated with more severe AnxD and conversely abstinence from alcohol is associated with improvement of AnxD [ 3 , 4 ]. To that effect, longitudinal strategies to address AUD may improve AnxD by extension. As conveyed by the reflections of the individual described in the present report, motivational enhancement, formal psychotherapy, mutual self-help interventions such as Alcoholics Anonymous, and supportive settings such as residential treatment facilities, all highlighting the health benefits of reduction or cessation of alcohol use, can serve an important psychosocial role alongside appropriate evidence-based AUD pharmacotherapy [ 5 ]. Nevertheless, the question remains whether certain interventions have additional efficacy in AnxD beyond their efficacy for AUD.
Naltrexone and Acamprosate
Naltrexone is a first-line evidence-based pharmacotherapy which functions as a non-selective opioid antagonist, reducing the rewarding effects of alcohol use mediated by endogenous opioids and downstream neurotransmitters. Studies have demonstrated efficacy for reducing binge drinking (number needed to treat [NNT] = 12) as well as relapse to any alcohol use (NNT = 20) [ 5 ], which motivated our use of naltrexone in the case strongly featuring AUD. To our knowledge, no clinical trial has yet effectively addressed whether naltrexone treatment for AUD can improve a comorbid AnxD, nor an AnxD disorder in isolation.
Acamprosate, which modulates glutamate and GABA signaling disrupted by chronic alcohol use, is another first-line AUD medication effective in preventing relapse to any alcohol use (NNT = 12) [ 5 ]. In terms of comorbid AnxD, some preliminary data suggests benefit of acamprosate for augmentation in various AnxD at doses equivalent or lower than those used in AUD [ 6 ]. However, as with naltrexone, there is a paucity of data to confidently gauge the effect of these first-line AUD medications on a comorbid AnxD and further research would be valuable in this area.
Gabapentinoids
Gabapentinoids such as gabapentin and pregabalin also modulate glutamate and GABA signaling implicated in AnxD and AUD specifically by antagonism of voltage-gated calcium channels. For AUD, gabapentin can be used in the short-term to treat alcohol withdrawal symptoms and in the longer-term to reduce heavy drinking days although efficacy for other endpoints such as reduction in cravings is debated [ 7 ]. Importantly, the data suggest that a key element of clinical efficacy of gabapentin is appropriate patient selection, specifically those with more severe AUD and alcohol withdrawal symptoms. For example, a recent positive randomized clinical trial (RCT) of gabapentin in AUD, which excluded any major psychiatric condition besides PTSD, found that patients with less severe withdrawal tended to fare worse numerically on all indices of alcohol use compared to placebo, although not statistically significant [ 8 ]. To date, some literature exists to support using pregabalin during alcohol withdrawal but data for longer-term treatment of AUD is very limited [ 5 ]. Interestingly, a RCT comparing pregabalin versus naltrexone in subjects with AUD (approximately 15% with comorbid AnxD in each arm) suggested pregabalin was about as effective as naltrexone in terms of AUD outcomes and more effective in reducing phobic anxiety, a subscale of the particular psychiatric questionnaire used in the study [ 9 ]. Further research is needed in this area to better characterize the efficacy of gabapentinoids for treating AnxD specifically in individuals with AUD-AnxD.
The available evidence more strongly supports efficacy of gabapentinoids in treatment of isolated primary AnxD. Gabapentin may be effective for several types of AnxD, [ 2 ] although to our knowledge there is no high-quality data yet available to support gabapentin for treatment of GAD which is frequently encountered in clinical practice. On the other hand, pregabalin has extensive data demonstrating efficacy for GAD as well as SAD, so much so that national practice guidelines currently view pregabalin as a first-line agent for these two conditions [ 2 ].
In sum, the current evidence indicates gabapentinoids have a role in the treatment of both AUD and AnxD and this class of medications may hold promise for treatment of comorbid AUD-AnxD. This emerging evidence supported the prescription of gabapentin in the above case which we believe ultimately contributed to the substantial benefit the individual found with the regimen described. In the interim while further evidence accumulates, a pertinent consideration in the application of gabapentinoids remains the risk of misuse. Gabapentin misuse occurs in the general population, particularly those with substance use disorders, for a variety of reasons including self-medication (e.g. anxiety, pain, and drug withdrawal symptoms) as well as documented recreational use or self-harm [ 10 ]. Even in context of supportive evidence, clinicians should nevertheless be aware of these reports and potential for gabapentinoids to be misused or diverted in treatment of AUD, AnxD, or overlap AUD-AnxD.
Other studied AUD medications
Other medications which have received research attention for AUD include baclofen, topiramate, antipsychotics, and benzodiazepines [ 5 ]. The evidence base for these agents is even more limited and inconclusive in the realm of AUD and comorbid AUD-AnxD. For example, baclofen is a GABA-B agonist medication with a Cochrane systematic review finding conflicting evidence for AUD, comorbid anxiety, and lack of high-quality evidence for use in alcohol withdrawal [ 11 ].
AnxD pharmacotherapies
Psychotropics.
Regarding selective serotonin reuptake inhibitors (SSRIs), the prevalent pharmacologic treatment for AnxD [ 2 ], a Cochrane systematic review of RCTs for comorbid AUD-AnxD found modest improvements in anxiety measures but unreliable or even unhelpful effects on comorbid AUD [ 12 ]. At this juncture, we acknowledge SSRIs are also frequently prescribed according to clinical practice guidelines for treatment of mood disorders that can be challenging to distinguish clinically from AUD and AnxD, which are commonly comorbid [ 13 ]. Nevertheless, meta-analyses demonstrate a lack of benefit of SSRIs in the context of AUD with mood disorder with similar concerns of worsening outcomes [ 14 , 15 , 16 ]. Given the common co-presentation of anxiety and depression among individuals with AUD, the following discussion instead explores the literature from the perspective of AUD outcomes for individuals with any exposure to SSRI or other serotoninergic medications, such as the individual in our case report, regardless of the primary indication for their use. Notably, comorbid mood and anxiety disorders are frequently reported in the available studies and often served as the primary indication for SSRI use.
We note with interest the underappreciated phenomenon of enhanced serotoninergic neurotransmission exacerbating AUD for certain individuals. For example, a secondary analysis of a RCT studying naltrexone for individuals with AUD and comorbid mood and anxiety disorders found prescriptions for SSRI outside of study protocol during follow-up to be associated with worse drinking outcomes for participants randomized to placebo, an effect which was attenuated if participants received naltrexone [ 17 ]. More convincing evidence supporting the potential for harm also exists in several RCTs. In an RCT of the SSRI citalopram for AUD in which mood, AnxD, and both disorders were highly comorbid, participants consumed more alcohol on more days compared to placebo regardless of mood or anxiety measures [ 16 ]. Several trials have also evaluated sertraline in AUD and found that younger participants with more severe AUD in particular tend to fare worse when prescribed an SSRI [ 18 ], moderated in part by the presence of an allele of the serotonin transporter gene favoring greater serotonergic tone [ 18 ]. However, these data are complicated to apply in clinical practice since the predisposing allele may also be found in older participants who happen to develop AUD later in life. Based on allele prevalence in the general US population, Kranzler et al. extrapolated that approximately double the number of individuals with AUD on a population level would be adversely affected by unselected SSRI treatment rather than find benefit [ 18 ]. One small trial comparing combinations of venlafaxine and cognitive behavioral therapy (CBT) for AUD found the only effective treatment for reducing heavy drinking days to be CBT alone with placebo medication, suggesting that selective serotonin and norepinephrine reuptake inhibitors such as venlafaxine may likewise be unhelpful for AUD outcomes [ 19 ].
Trazodone, another psychotropic medication which modulates serotonin transmission, although used for mood disorders and insomnia rather than AnxD, should be addressed in context of AUD. Trazodone is occasionally prescribed with intent as an antidepressant and sleep aid for individuals with AUD but one RCT found a minimal short-term improvement in sleep quality, while also reporting reduced abstinent days, and increased severity of alcohol consumption following withdrawl of trazodone [ 20 ].
In sum, despite the evidence for first-line treatment of isolated AnxD or mood disorders with serotoninergic agents such as SSRIs, clinicians should reconsider and exercise caution in prescribing these medications for patients with comorbid AUD given current observational, RCT, and meta-analysis evidence demonstrating lack of benefit and potential of harm to alcohol use outcomes. In the interim, further investigation is needed to clarify which selected subpopulations in clinical practice would benefit from step-wise approach later involving serotoninergic agents or conversely serotonin antagonists [ 21 ]. Careful use of pharmacologic agents targeting AnxD, such as pregabalin or gabapentin, in tandem with other biopsychosocial strategies may have more of an evidence-based role to play since AnxD are frequently comorbid, have been reported to more frequently precede rather than follow AUD [ 3 ], and are associated with worsening of AUD [ 22 ], suggesting that effective treatment of AnxD may prevent AUD deterioration.
Tobacco cessation
Although not directly relevant to the individual described in our case report, tobacco use may impact clinical outcomes for individuals with AUD-AnxD. Research indicates that weekly smoking in youth is a risk factor for worsening of AUD [ 22 ], and tobacco cessation has been shown to improve anxiety symptoms for both individuals with and without psychiatric disorders [ 23 ]. For instance, a recent meta-analysis demonstrated that the nicotinic receptor partial agonist varenicline was safe and conferred a 25% lower risk of anxiety compared to placebo - likely a result of reduction and cessation in tobacco use [ 24 ]. However, data specific to AUD-AnxD clinical outcomes after tobacco cessation interventions is still limited and inconclusive to date [ 25 ]. In addition to other known broad health benefits such as reduced incidence of cardiovascular disease and cancer, the cessation of tobacco use may also play a synergistic role in treatment of AUD-AnxD.
Psychotherapies
Formal psychotherapy holds promise for addressing the propagating psychosocial factors of AUD and AnxD alone or in addition to pharmacotherapy. In the realm of AnxD, CBT can be equally or more effective than medication alone [ 2 ]. For comorbid AUD-AnxD, motivational interviewing and CBT are effective for both conditions, especially as longer-term modalities with more durable efficacy [ 26 ]. Such targeted and integrated psychotherapy might be particularly effective for individuals with AnxD attempting to self-medicate anxiety symptoms by using alcohol.
Teaching points
AnxD and AUD are prevalent health concerns which frequently co-occur and can compound one another as demonstrated in our report. Their co-occurrence requires a thoughtful approach to treatment given the evidence that treatments of one disorder have been shown to be ineffective or counterproductive for the other disorder (Fig. 1 ). Although evidence is scarce for synergistic treatments of comorbid AUD-AnxD, the literature supports overlapping efficacy of tobacco cessation, use of gabapentinoids, and integrated psychotherapy, the latter two of which were applied with success for the individual in this case report. While the first-line AUD pharmacotherapies naltrexone and acamprosate do not yet have evidence of concurrent benefit for AnxD, effectively treating AUD may yield downstream benefit for AnxD as suggested by treatment response in this report. Lastly, caution should be exercised with serotoninergic medications such as SSRIs as there appears to be underappreciated evidence suggesting that SSRIs are not of benefit in the context of AUD [ 12 ], and may actually worsen alcohol related outcomes for certain individuals [ 16 ]. Further investigation is needed to understand synergistic versus step-wise approaches to treatment of comorbid AUD-AnxD and identification of specific population subgroups which may derive benefit with serotoninergic agonists versus antagonists.
Data availability
Not applicable to case report.
Abbreviations
anxiety disorder
alcohol use disorder
comorbid alcohol use disorder and anxiety disorder
cognitive Behavioral Therapy
gamma aminobutyric acid
generalized anxiety disorder
gamma-hydroxybutyrate
post-traumatic stress disorder
randomized clinical trial
social anxiety disorder
selective serotonin reuptake inhibitors
Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry Aug. 2015;72(8):757–66. doi: https://doi.org/10.1001/jamapsychiatry.2015.0584 .
Article CAS Google Scholar
Katzman MA, Bleau P, Blier P, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry. 2014;14(Suppl 1):1. doi: https://doi.org/10.1186/1471-244X-14-S1-S1 .
Article Google Scholar
Anker JJ, Kushner MG. Co-Occurring Alcohol Use Disorder and Anxiety: Bridging Psychiatric, Psychological, and Neurobiological Perspectives. Alcohol Res. 2019;40(1)doi: https://doi.org/10.35946/arcr.v40.1.03 .
Driessen M, Meier S, Hill A, Wetterling T, Lange W, Junghanns K. The course of anxiety, depression and drinking behaviours after completed detoxification in alcoholics with and without comorbid anxiety and depressive disorders. Alcohol Alcohol . 2001 May-Jun. 2001;36(3):249–55. doi: https://doi.org/10.1093/alcalc/36.3.249 .
British Columbia Centre on Substance Use (BCCSU), B.C. Ministry of Health, B.C. Ministry of Mental Health and Addictions. Provincial Guideline for the Clinical Management of High-Risk Drinking and Alcohol Use Disorder. BCCSU; 2019. https://www.bccsu.ca/wp-content/uploads/2021/01/AUD-Guideline.pdf .
Hertzman M, Patt IS, Spielman LA. Open-label trial of acamprosate as a treatment for anxiety. Prim Care Companion J Clin Psychiatry. 2009;11(5):267. doi: https://doi.org/10.4088/PCC.08l00714 .
Article PubMed PubMed Central Google Scholar
Kranzler HR, Feinn R, Morris P, Hartwell EE. A meta-analysis of the efficacy of gabapentin for treating alcohol use disorder. Addiction. 2019;09(9):1547–55. doi: https://doi.org/10.1111/add.14655 . 114 ) .
Anton RF, Latham P, Voronin K, et al. Efficacy of Gabapentin for the Treatment of Alcohol Use Disorder in Patients With Alcohol Withdrawal Symptoms: A Randomized Clinical Trial. JAMA Intern Med. Mar 2020. doi: https://doi.org/10.1001/jamainternmed.2020.0249 .
Martinotti G, Di Nicola M, Tedeschi D, et al. Pregabalin versus naltrexone in alcohol dependence: a randomised, double-blind, comparison trial. J Psychopharmacol Sep. 2010;24(9):1367–74. doi: https://doi.org/10.1177/0269881109102623 .
Smith RV, Havens JR, Walsh SL. Gabapentin misuse, abuse and diversion: a systematic review. Addict 07. 2016;111(7):1160–74. doi: https://doi.org/10.1111/add.13324 .
Minozzi S, Saulle R, Rösner S. Baclofen for alcohol use disorder. Cochrane Database Syst Rev Nov. 2018;11:CD012557. doi: https://doi.org/10.1002/14651858.CD012557.pub2 .
Ipser JC, Wilson D, Akindipe TO, Sager C, Stein DJ. Pharmacotherapy for anxiety and comorbid alcohol use disorders. Cochrane Database Syst Rev Jan. 2015;1:CD007505. doi: https://doi.org/10.1002/14651858.CD007505.pub2 .
Beaulieu S, Saury S, Sareen J, et al. The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid substance use disorders. Ann Clin Psychiatry Feb. 2012;24(1):38–55.
Google Scholar
Agabio R, Trogu E, Pani PP. Antidepressants for the treatment of people with co-occurring depression and alcohol dependence. Cochrane Database Syst Rev. 2018;04:4:CD008581. doi: https://doi.org/10.1002/14651858.CD008581.pub2 .
Grant S, Azhar G, Han E, et al. Clinical interventions for adults with comorbid alcohol use and depressive disorders: A systematic review and network meta-analysis. PLoS Med. 2021;10(10):e1003822. doi: https://doi.org/10.1371/journal.pmed.1003822 . 18 ) .
Charney DA, Heath LM, Zikos E, Palacios-Boix J, Gill KJ. Poorer Drinking Outcomes with Citalopram Treatment for Alcohol Dependence: A Randomized, Double-Blind, Placebo-Controlled Trial. Alcohol Clin Exp Res Sep. 2015;39(9):1756–65. doi: https://doi.org/10.1111/acer.12802 .
Krystal JH, Gueorguieva R, Cramer J, Collins J, Rosenheck R, Team VCNS. Naltrexone is associated with reduced drinking by alcohol dependent patients receiving antidepressants for mood and anxiety symptoms: results from VA Cooperative Study No. 425, “Naltrexone in the treatment of alcoholism”. Alcohol Clin Exp Res Jan. 2008;32(1):85–91. doi: https://doi.org/10.1111/j.1530-0277.2007.00555.x .
Kranzler HR, Armeli S, Tennen H, et al. A double-blind, randomized trial of sertraline for alcohol dependence: moderation by age of onset [corrected] and 5-hydroxytryptamine transporter-linked promoter region genotype. J Clin Psychopharmacol Feb. 2011;31(1):22–30. doi: https://doi.org/10.1097/JCP.0b013e31820465fa .
Ciraulo DA, Barlow DH, Gulliver SB, et al. The effects of venlafaxine and cognitive behavioral therapy alone and combined in the treatment of co-morbid alcohol use-anxiety disorders. Behav Res Ther Nov. 2013;51(11):729–35. doi: https://doi.org/10.1016/j.brat.2013.08.003 .
Stein MD, Kurth ME, Sharkey KM, Anderson BJ, Corso RP, Millman RP. Trazodone for sleep disturbance during methadone maintenance: a double-blind, placebo-controlled trial. Drug Alcohol Depend Jan. 2012;120(1–3):65–73. doi: https://doi.org/10.1016/j.drugalcdep.2011.06.026 .
Johnson BA, Roache JD, Javors MA, et al. Ondansetron for reduction of drinking among biologically predisposed alcoholic patients: A randomized controlled trial. JAMA . 2000 Aug 23–30 2000;284(8):963 – 71. doi: https://doi.org/10.1001/jama.284.8.963 .
Conway KP, Swendsen J, Husky MM, He JP, Merikangas KR. Association of Lifetime Mental Disorders and Subsequent Alcohol and Illicit Drug Use: Results From the National Comorbidity Survey-Adolescent Supplement. J Am Acad Child Adolesc Psychiatry Apr. 2016;55(4):280–8. doi: https://doi.org/10.1016/j.jaac.2016.01.006 .
Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ (Clinical research ed) Feb 13. 2014;348:g1151. doi: https://doi.org/10.1136/bmj.g1151 .
Thomas KH, Martin RM, Knipe DW, Higgins JP, Gunnell D. Risk of neuropsychiatric adverse events associated with varenicline: systematic review and meta-analysis. BMJ Mar. 2015;12:350:h1109. doi: https://doi.org/10.1136/bmj.h1109 .
Kodl M, Fu SS, Joseph AM. Tobacco cessation treatment for alcohol-dependent smokers: when is the best time? Alcohol Res Health. 2006;29(3):203–7.
PubMed PubMed Central Google Scholar
Baker AL, Thornton LK, Hiles S, Hides L, Lubman DI. Psychological interventions for alcohol misuse among people with co-occurring depression or anxiety disorders: a systematic review. J Affect Disord Aug. 2012;139(3):217–29. doi: https://doi.org/10.1016/j.jad.2011.08.004 .
Download references
Acknowledgements
Not applicable.
This development of this article was not supported by any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and affiliations.
British Columbia Centre on Substance Use, 400-1045, V6Z 2A9, Howe St, Vancouver, BC, Canada
Victor Mocanu & Evan Wood
Department of Medicine, University of British Columbia, 2255 Wesbrook Mall, V6T 2A1, Vancouver, BC, Canada
You can also search for this author in PubMed Google Scholar
Contributions
VM and EW were involved in conception, design, planning, drafting, revision, and final approval of the manuscript. EW was directly involved in patient care and data collection.
Corresponding author
Correspondence to Evan Wood .
Ethics declarations
Ethics approval and consent to participate.
Per local University of British Columbia and Providence Health Care ethics boards, case reports do not meet the formal definition for research and ethics approval was waived.
Consent to publish
Written consent, manuscript feedback, and final approval was granted by the individual to present their anonymized information and reflection.
Competing interests
EW served as the Chief Medical Officer at Numinus Wellness, a Canadian company interested in medical application of psychedelic substances. Numinus Wellness was not involved in the conception, planning, writing or decision to submit this manuscript for publication. EW is supported by the Canadian Institutes of Health Research through the Canada Research Chairs Program. No other competing interests were declared.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mocanu, V., Wood, E. Alcohol use disorder with comorbid anxiety disorder: a case report and focused literature review. Addict Sci Clin Pract 17 , 62 (2022). https://doi.org/10.1186/s13722-022-00344-z
Download citation
Received : 27 June 2022
Accepted : 19 October 2022
Published : 08 November 2022
DOI : https://doi.org/10.1186/s13722-022-00344-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Comorbidity
- Dual diagnosis
- Treatment recommendations
Addiction Science & Clinical Practice
ISSN: 1940-0640
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Addictive Behaviour: Molecules to Mankind pp 260–291 Cite as
Alcohol Abuse in Society: Case Studies
- Adrian Bonner 3 &
- James Waterhouse 4
34 Accesses
The last three chapters have demonstrated how routine data may be collected from the health service and forensic medicine. These data present a view of the occurrence of alcohol and drug abuse in society which is generated from a ‘medical model’. As useful as this approach is, it does not take into account the nature and needs of specific groups. To do this a more ‘socially appropriate perspective’ can be used. The following case studies illustrate some of the problems resulting from methodological issues in this area of investigation and, in particular, from studies undertaken in short-term projects undertaken by graduate students. Important discussions relating to: ‘what level of consumption constitutes abuse ’ ‘alcohol usage by the elderly’, and ‘the effectiveness of health education’ will be introduced.
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Unable to display preview. Download preview PDF.
Anderson, P. (1984) ‘Alcohol Consumption of Undergraduates at Oxford University’, Alcohol and Alcoholism , 19:pp. 77–84.
Google Scholar
Black, D. and Weare, K. (1989) ‘Knowledge and Attitudes about Alcohol in 17- and 18-Year-Olds’, Health Education Journal , 48 (2):pp. 69–73.
Article Google Scholar
Cyster, R. and McEwen, J. (1987) ‘Alcohol Education in the Workplace’, Health Education Journal , 46 (4):pp. 156–61.
Davies, J. (1991) ‘Learning to Drink’, paper presented at a national conference on ‘Alcohol and Young People’, 8 October 1991, Queen Mother Conference Centre, Royal College of Physicians, Edinburgh.
Gillies, P. (1991) ‘What Can Education Achieve?’, paper presented at a national conference on ‘Alcohol and Young People’, 8 October 1991, Queen Mother Conference Centre, Royal College of Physicians, Edinburgh.
Grant, M. (1981) ‘Aims, Form and Content: First Steps in Developing a Taxonomy of Preventative Education in Drug and Alcohol Abuse’, in L. R. H. Drew et al . (eds), Man, Drugs, and Society: Current Perspectives (Canberra: Australian Foundation on Alcoholism and Drug Dependence).
Haack, M. (1988) ‘Stress and Impairment among Nursing Students’, Research in Nursing and Health , 11:pp. 125–34.
Haack, M. and Harford, T. (1984) ‘Drinking Patterns among Student Nurses’, The International Journal of the Addictions , 19 (5):pp. 577–83.
Hopkins, R., Maussa, A., Kearney, K. and Weisheit, R. (1988) ‘Comprehensive Evaluation of a Model Alcohol Education Curriculum’, Journal of Studies on Alcohol , 49 (1):pp. 38–50.
Hutchison, S. (1986) ‘Chemically Dependent Nurses: The Trajectory towards Self Annihilation’, Nursing Research , 35 (July/August):pp. 196–201.
Maussa, A., Hopkins, R., Weisheit, R., and Kearney, K. (1988) The Problematic Prospects for Prevention in the Classroom: Should Alcohol Education Programmes be Expected to Reduce Drinking by Youth?’, Journal of Studies in Alcohol , 49 (1):pp. 51–61.
Plant, M. (1991) ‘Heavy Drinkers: Are They Distinctive?’, paper presented at a national conference on ‘Alcohol and Young People’, 8 October 1991, Queen Mother Conference Centre, Royal College of Physicians, Edinburgh.
Plant, M. L., Plant, M. A. and Foster, J. (1991) ‘Alcohol, Tobacco and Illicit Drug Use Amongst Nurses: A Scottish Study’, Drug and Alcohol Dependence , 28:pp. 195–202.
Roberts, R. (1988) ‘Hiccups in Alcohol Education’, Health Education Journal , 47 (213):pp. 73–5.
Royal College of General Practitioners (1986) Alcohol: A Balanced View (London: Tavistock).
Saltz, R., and Elandt, D. (1986) ‘College Students Drinking Studies 1976–1985’, Contemporary Drug Problems (Spring):pp. 117–59.
Wallace, P., Brennan, P., and Haines, A. (1987) ‘Drinking Patterns in General Practice Patients’, Journal of the Royal College of General Practitioners , 37:pp. 354–7.
Weichsler, H. and McFadden, M. (1979) ‘Drinking among College Students in New England; Extent, Social Correlates and Consequences of Alcohol’, Journal of Studies on Alcohol , 40:pp. 969–99.
West, R., Drummond, C., and Eames, K. (1990) ‘Alcohol Consumption, Problem Drinking and Anti-Social Behaviour in a Sample of College Students’, British Journal of Addiction , 85:pp. 479–86.
Download references
Author information
Authors and affiliations.
Addictive Behaviour Centre Roehampton Institute, London, UK
Adrian Bonner ( Director )
School of Biological Sciences, School of Human Biology, University of Manchester, UK
James Waterhouse ( Senior Research Fellow, Lecturer in Physiology )
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Adrian Bonner ( Director ) ( Director )
James Waterhouse ( Senior Research Fellow, Lecturer in Physiology ) ( Senior Research Fellow, Lecturer in Physiology )
Copyright information
© 1996 Adrian Bonner and James Waterhouse
About this chapter
Cite this chapter.
Bonner, A., Waterhouse, J. (1996). Alcohol Abuse in Society: Case Studies. In: Bonner, A., Waterhouse, J. (eds) Addictive Behaviour: Molecules to Mankind. Palgrave Macmillan, London. https://doi.org/10.1007/978-1-349-24657-1_17
Download citation
DOI : https://doi.org/10.1007/978-1-349-24657-1_17
Publisher Name : Palgrave Macmillan, London
Print ISBN : 978-0-333-64556-7
Online ISBN : 978-1-349-24657-1
eBook Packages : Palgrave Social & Cultural Studies Collection Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

News & Events

National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Research insights into alcoholism and alcohol abuse highlighted in 10th special report.
Saturday, November 11, 2000
Secretary of Health and Human Services Donna E. Shalala has announced the availability of the 10th Special Report to the U.S. Congress on Alcohol and Health , produced by the National Institute on Alcohol Abuse and Alcoholism (NIAAA). The report highlights recent research advances on the causes, consequences, treatment, and prevention of alcohol addiction (alcoholism) and alcohol abuse.
The 492-page report, available in print and on the internet, documents the scope of alcohol’s impact on society. The effects range from violence to traffic crashes to lost productivity to illness and premature death—all of which, combined, cost our nation an estimated $184.6 billion per year. The report also conveys the rapid progress of research into the genetic and environmental factors that can lead to alcohol addiction. Scientists are using these insights to develop and test new ways of preventing and treating this disease. "Alcohol problems can yield to scientific investigation and medical intervention in the same way as other health conditions," writes DHHS Secretary Donna Shalala in the foreword.
The new report presents advances in alcohol research since 1997, when the last edition of Alcohol and Health was published. "This report reflects the tremendous growth in the scope of alcohol research," according to NIAAA Director Enoch Gordis, M.D. Contemporary alcohol research spans all life stages—from prenatal alcohol exposure to drinking problems in the elderly—and applies the latest methods of basic, epidemiological, clinical, behavioral, and social sciences research, often in multidisciplinary collaborations. The following research areas are among those detailed in the 10 th Report :
Genetics of alcoholism. Two studies have found evidence of genes on specific chromosomes influencing susceptibility to alcoholism. The ongoing Collaborative Study on the Genetics of Alcoholism (COGA), which involves 987 individuals from high-risk families, reported suggestive evidence of genes on chromosomes 1 and 7 involved in alcoholism. An early report from the study also reported weaker evidence of such a gene on chromosome 2. Another study from NIAAA’s Laboratory of Neurogenetics, based on 152 members of a southwestern Native American tribe, reported suggestive evidence for a gene influencing susceptibility to alcoholism on chromosome 11. Both studies reported finding evidence of a gene that was protective against alcoholism in a region of chromosome 4.
Heavy drinking during pregnancy and fetal brain development. Applying advances in neuroimaging and cellular and molecular biology, alcohol researchers are gaining an increasingly clear picture of the physical nature of alcohol-induced damage to the developing brain and the mechanisms that cause the damage. Imaging studies have demonstrated structural abnormalities in certain brain regions, whereas other regions seem to be spared. Research also shows that a number of deficits in cognitive and motor functions are linked to prenatal alcohol exposure, while other functions appear to remain intact. These studies, as well as basic research on the mechanisms of prenatal alcohol damage, support the notion that alcohol has specific, rather than global, effects on the developing brain.
Preventing underage drinking. One major study, the Community Trials Project, found that sales clerks in alcoholic beverage outlets were half as likely to sell alcohol to minors in communities with programs that trained clerks, enforced underage sales laws, and raised awareness of increased enforcement through the media. Another large study, Project Northland, showed that a multi-year program involving schools, parents, peers, policy-makers, and businesses can effectively reduce underage drinking—if the intervention begins before adolescents begin to use alcohol. The 10th Report also describes the search for the roots of alcohol problems in adolescence and later life stages, through multidisciplinary research on social, cultural, psychological, and biological influences.
Reducing alcohol-related traffic crashes. The 10 th Report presents many studies on the effectiveness of laws, public policies, community programs, and individual actions to deter drunk driving. A number of studies have focused on State laws that make it a criminal offense to drive with a blood alcohol concentration (BAC) over a certain limit, which in most States is 0.10 percent. New research shows that States that reduce the legal BAC limit to 0.08 percent experience a significant drop in fatal crashes related to alcohol, and that this decrease is distinct from the effects of other drunk driving measures.
Chronic alcohol use and the brain. Studies in animal models are revealing how changes in the brain from chronic alcohol consumption underlie such features of alcoholism as tolerance (lowered sensitivity to the intoxicating effects of alcohol), withdrawal, and craving. This work is helping scientists understand the biological basis for the motivation to drink too much and the mechanisms through which alcohol causes lasting damage to the brain in some individuals who consume alcohol heavily.
Damage to body organs. Research on how alcohol damages body organs is providing information that may be used in developing novel treatments. For example, a variety of evidence suggests that liver damage results from changes in immune function, suggesting the potential of immune-based treatments.
Helping patients to reduce alcohol use and related problems. When patients are found to be at-risk or problem drinkers, but not alcohol dependent, health care providers can significantly reduce alcohol use and related problems by providing a quick form of counseling called "brief intervention." Research shows that brief interventions delivered in primary care settings can decrease alcohol use for at least a year in persons who drink above recommended limits.
Medications for treating alcoholism. Advances in neuroscience have paved the way for medications that operate at the molecular level of brain processes that influence alcohol addiction. Studies show that the medication naltrexone and a similar compound, nalmefene, help reduce the chance of heavy drinking when abstinent individuals relapse; that a medication called acamprosate may prevent relapse; and that when patients with co-existing depression take antidepressants, their alcoholism treatment outcomes improve.
The report contains eight chapters: (1) Drinking Over the Life Span: Issues of Biology, Behavior and Risk, (2) Alcohol and the Brain: Neuroscience and Neurobehavior, (3) Genetic and Psychosocial Influences, (4) Medical Consequences, (5) Prenatal Exposure to Alcohol, (6) Economic and Health Services Perspectives, (7) Prevention, and (8) Treatment. Each chapter is divided into two to six subsections that can be downloaded individually in PDF format from the NIAAA website ( http://www.niaaa.nih.gov/ ). Bound copies of the entire 492-page report can also be ordered by writing to: National Institute on Alcohol Abuse and Alcoholism, Publications Distribution Center, P.O. Box 10686, Rockville, MD 20849-0686.
The NIAAA produced the 10 th Special Report to the U.S. Congress on Alcohol and Health with guidance from a distinguished editorial advisory board and contributions from some of the world’s leading alcohol researchers. A component of the National Institutes of Health, NIAAA funds more than 90 percent of the alcohol abuse and alcohol addiction (alcoholism) research in the United States.
About the National Institute on Alcohol Abuse and Alcoholism (NIAAA): The National Institute on Alcohol Abuse and Alcoholism (NIAAA), part of the National Institutes of Health, is the primary U.S. agency for conducting and supporting research on the causes, consequences, diagnosis, prevention, and treatment of alcohol use disorder. NIAAA also disseminates research findings to general, professional, and academic audiences. Additional alcohol research information and publications are available at www.niaaa.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
Contact info : NIAAA Press Office 301-443-2857 [email protected]
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
Study shows increase in serious alcohol-related complications early in pandemic
A new study in JAMA Health Forum shows increases in serious alcohol-related complications in 4 of 18 COVID-19 pandemic months studied (through September 2021), and suggests that women aged 40 to 64 years experienced increases of 33.3% to 56.0% in serious alcohol complication episodes in 10 of the 18 months.
The study is based on US national insurance claims data from March 2017 to September 2021, with researchers comparing prepandemic rates of serious alcohol-related problems to rates seen during pandemic months. A secondary outcome was the subset of episodes of alcohol-related liver disease (ALD).
Overall, in 4 of the 18 pandemic months beginning in March 2020, rates of serious alcohol-related issues were statistically higher than expected, the authors said, by 0.4 to 0.8 episodes per 100,000 people.
Middle-aged women most affected
Of the serious complications, 54% to 66% were ALD-related, 29% to 39% were alcohol withdrawal or alcohol-related mood disorders, 3% to 5% were alcohol-related cardiomyopathy, and 1% to 3% were alcohol-related gastritis with bleeding.
Middle-aged women experienced statistically significant increases in 10 of the 18 pandemic months (range of absolute and relative increases: 1.3 to 2.1 episodes per 100, 000 women; 33.3% to 56.0% increase), mostly of ALD complications.
The COVID-19 pandemic was associated with increased alcohol consumption, particularly among women, likely due to social isolation and stress.
" The COVID-19 pandemic was associated with increased alcohol consumption, particularly among women, likely due to social isolation and stress, " the authors write. " These findings imply a need for increased attention to alcohol use disorder (AUD) risk factors, alcohol use patterns, alcohol-related health effects, and related interventions, especially among women aged 40 to 64 years. "
Feds probe injuries from counterfeit Botox injections
Federal health officials and their state and local health partners are investigating reports of harmful reactions in women who received counterfeit or mishandled botulinum toxin (Botox) injections, with 19 injuries reported in nine states, the US Centers for Disease Control and Prevention (CDC) announced yesterday.
The reactions occurred following Botox injections from unlicensed and untrained people in non-healthcare settings, including homes and spas. The patients are from Colorado, Florida, Illinois, Kentucky, Nebraska, New Jersey, New York, Tennessee, and Washington.
Botox contains minute amounts of botulinum toxin, which comes from the bacterium Clostridium botulinum . The toxin, which in larger amounts can cause muscle paralysis, in very small amounts is used to smooth wrinkles and treat certain muscle conditions.
Examples of the patients' reactions include vision problems, drooping eyelids, difficulty swallowing, difficulty breathing, and general weakness. Nine were hospitalized, and four were treated with botulinum antitoxin owing to concerns that botulinum could spread beyond the injection site. Five people were tested for botulism, and all were negative.
All patients were women ages 25 to 59, and all but one received the injections for cosmetic purposes.
FDA says no link to approved products
Some women received counterfeit or unverified products, and investigators are still working to determine the sources. In a separate statement , the Food and Drug Administration (FDA) said it is working with AbbVie, the Botox manufacturer, to identify, investigate, and remove suspected counterfeit products. It added that there is no sign that the events were related to AbbVie's FDA-approved products.
The CDC urged people considering Botox injections to ensure that providers are licensed and trained and to ask if the product is approved by the FDA and obtained from a reliable source. "If in doubt, don’t get the injection," the agency added.
Canada reports more H5N5 avian flu virus detections in mammals, wild birds
Animal health officials in Canada have reported more highly pathogenic H5N5 avian flu detections in wild birds and mammals, according to recent notifications from the World Organization for Animal Health (WOAH).

In May 2023, the country reported the Eurasian H5N5 subtype in racoons found dead on Prince Edward Island, which followed sporadic detections of H5N5 in Canadian wild birds. At the time, WOAH warned of unprecedented genetic variability in avian flu subtypes in wild birds and poultry across the world, creating epidemiologic challenges.
The new detections in mammals also involved raccoons, which were found in February and March on Prince Edward Island and in Nova Scotia. The virus belongs to the same 2.3.4.4b clade as the H5N1 virus currently circulating in several world regions.
Canada also reported more H5N5 detections in wild birds , which involved crows found on Prince Edward Island in early January.
FDA to review 5-in-1 meningococcal vaccine candidate
British drugmaker GSK announced today that the US Food and Drug Administration (FDA) has accepted an application for review of the company's 5-in-1 meningococcal vaccine.
GSK's MenABCWY vaccine candidate will target the five groups of Neisseria meningitidis bacteria (meningococcal serogroups A, B, C, W, and Y) that cause most cases of invasive meningococcal disease (IMD) globally. It combines the antigenic components of GSK's well-established meningococcal vaccines, Bexsero and Menveo.
Simplified immunization
The company says combining the protection offered by these vaccines into a single vaccine will reduce the number of injections, simplify immunization, and help increase series completion. Just under 12% of US adolescents have had the required two doses of Bexsero, which provides protection against meningococcal group B, the most common group of IMD-causing bacteria in US adolescents and young adults. Menveo prevents IMD caused by meningococcal groups A, C, Y, and W-135.
Among those who contract IMD, one in six will die and one in five may suffer long-term consequences such as brain damage. Teens and young adults are among those at greatest risk of contracting it.
The Biologics License Application was submitted based on evidence from a multinational phase 3 randomized, controlled trial that involved 3,650 participants ages 10 to 25. MenABCWY met all primary end points in the trial, showing immunologic non-inferiority to one dose of Menveo and non-inferior immune responses against 110 diverse MenB invasive strains compared with two doses of Bexsero.
GSK says the FDA will make a decision on whether to approve the vaccine in February 2025.
In case you missed it
This week's top reads, wisconsin confirms another county affected by cwd in deer.
The 3-year-old buck was found dead in the town of Wautoma, within 10 miles of the Marquette and Portage county borders.
Avian flu virus detected in more Michigan dairy herds and on another large layer farm
Along with multiple detections now in dairy cows, avian flu has also hit 2 massive farms housing egg-laying hens in the state.

Vietnam reports its first human infection from H9 avian flu virus
The patient lived adjacent to a poultry market, but there were no reports of bird illnesses or deaths.
Avian flu detected in North Carolina dairy herd
Seven states have now reported the virus in dairy herds, with detections at 21 facilities.

Study: Pathogens that cause surgical infections may be coming from patients' skin
The study authors say the findings could have implications for infection-prevention strategies.
Blood donor study finds 21% incidence of long-term symptoms attributed to COVID-19
Among blood donors with prior SARS-CoV-2 infection, 23.6% reported long-term neurologic symptoms.

Study identifies inflammation and symptom patterns in long COVID
Inflammation of myeloid cells and activation of immune proteins that are part of the complement system stood out blood from long COVID patients, but it's not clear if that applies to all types of long COVID.
Avian flu virus detected in South Dakota dairy herd
Today's announcement raises the number of affected states to 8.
Three studies spotlight long-term burden of COVID in US adults
One study found that veterans were at 44% higher risk of a preventable hospitalization in the year after infection.

CDC: Spike in measles cases poses threat to US elimination status
Most imported cases this year occurred in US residents who were unvaccinated or had an unknown vaccination status.

Our underwriters
Unrestricted financial support provided by.

- Antimicrobial Resistance
- Chronic Wasting Disease
- All Topics A-Z
- Resilient Drug Supply
- Influenza Vaccines Roadmap
- CIDRAP Leadership Forum
- Roadmap Development
- Coronavirus Vaccines Roadmap
- Antimicrobial Stewardship
- Osterholm Update
- Newsletters
- About CIDRAP
- CIDRAP in the News
- Our Director
- Osterholm in the Press
- Shop Merchandise
- Discounts and promotions
- Delivery and payment
Cart is empty!
Case study definition

Case study, a term which some of you may know from the "Case Study of Vanitas" anime and manga, is a thorough examination of a particular subject, such as a person, group, location, occasion, establishment, phenomena, etc. They are most frequently utilized in research of business, medicine, education and social behaviour. There are a different types of case studies that researchers might use:
• Collective case studies
• Descriptive case studies
• Explanatory case studies
• Exploratory case studies
• Instrumental case studies
• Intrinsic case studies
Case studies are usually much more sophisticated and professional than regular essays and courseworks, as they require a lot of verified data, are research-oriented and not necessarily designed to be read by the general public.
How to write a case study?
It very much depends on the topic of your case study, as a medical case study and a coffee business case study have completely different sources, outlines, target demographics, etc. But just for this example, let's outline a coffee roaster case study. Firstly, it's likely going to be a problem-solving case study, like most in the business and economics field are. Here are some tips for these types of case studies:
• Your case scenario should be precisely defined in terms of your unique assessment criteria.
• Determine the primary issues by analyzing the scenario. Think about how they connect to the main ideas and theories in your piece.
• Find and investigate any theories or methods that might be relevant to your case.
• Keep your audience in mind. Exactly who are your stakeholder(s)? If writing a case study on coffee roasters, it's probably gonna be suppliers, landlords, investors, customers, etc.
• Indicate the best solution(s) and how they should be implemented. Make sure your suggestions are grounded in pertinent theories and useful resources, as well as being realistic, practical, and attainable.
• Carefully proofread your case study. Keep in mind these four principles when editing: clarity, honesty, reality and relevance.
Are there any online services that could write a case study for me?
Luckily, there are!
We completely understand and have been ourselves in a position, where we couldn't wrap our head around how to write an effective and useful case study, but don't fear - our service is here.
We are a group that specializes in writing all kinds of case studies and other projects for academic customers and business clients who require assistance with its creation. We require our writers to have a degree in your topic and carefully interview them before they can join our team, as we try to ensure quality above all. We cover a great range of topics, offer perfect quality work, always deliver on time and aim to leave our customers completely satisfied with what they ordered.
The ordering process is fully online, and it goes as follows:
• Select the topic and the deadline of your case study.
• Provide us with any details, requirements, statements that should be emphasized or particular parts of the writing process you struggle with.
• Leave the email address, where your completed order will be sent to.
• Select your payment type, sit back and relax!
With lots of experience on the market, professionally degreed writers, online 24/7 customer support and incredibly low prices, you won't find a service offering a better deal than ours.
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Robert’s story
Robert was living with an alcohol addiction and was homeless for over 25 years. He was well known in the local community and was identified as one of the top 100 A&E attendees at the Local General Hospital.
He drank all day every day until he would pass out and this was either in the town centre or just by the roadside. In addition, Robert was also incontinent and really struggled with any meaningful communication or positive decision making due to his alcohol usage. This often resulted in local services such as police, ambulance being called in to help. He had no independent living skills and was unable to function without alcohol.
In addition, and due to his lifestyle and presenting behaviours, Robert had a hostile relationship with his family and had become estranged from them for a long period of time.
Robert needed ongoing support and it was identified at the General Hospital that if he was to carry on “living” the way he currently was, then he wouldn’t survive another winter.
On the back of this, Robert was referred to Calico who organised a multi-disciplinary support package for him, which included support with housing as part of the Making Every Adult Matter programme.
After some initial challenges, Robert soon started to make some positive changes.
The intensive, multidisciplinary support package taught him new skills to support him to live independently, sustain his tenancy and make some positive lifestyle changes which in turn would improve his health and wellbeing.
This included providing daily visits in the morning to see Robert and to support him with some basic activities on a daily/weekly basis. This included getting up and dressed; support with shopping and taking to appointments; guidance to help make positive decisions around his associates; support about his benefits and managing his money. In addition, he was given critical support via accessing local groups such as RAMP (reduction and motivational programme) and Acorn (drugs and alcohol service), as well as 1 to 1 sessions with drugs workers and counsellors to address his alcohol addiction.
After six months Robert continued to do well and was leading a more positive lifestyle where he had greatly reduced his A&E attendance. He had significantly reduced his alcohol intake with long periods of abstinence and was now able to communicate and make positive decisions around his lifestyle.
Critically he had maintained his tenancy and continued to regularly attend local groups and other support for his alcohol addiction and had reconnected with some of his family members.
By being able to access these community resources and reduce his isolation he is now engaged in meaningful activities throughout the day and has been able to address some of his critical issues. A small but significant example is that Robert is now wearing his hearing aids which means that he can now interact and communicate more effectively.
Jump to navigation
- Bahasa Indonesia
- Bahasa Malaysia

New Cochrane Review finds Alcoholics Anonymous and 12-Step Facilitation programs help people to recover from alcohol problems

Newly updated evidence published in the Cochrane Library today compares Alcoholics Anonymous (AA) and clinically-related Twelve-Step Facilitation (TSF) programs with other treatments, such as cognitive behavioural therapy, to see if they help people who suffer from alcohol use disorders achieve sobriety or reduce the amount of alcohol that they consume.
Alcohol use disorder (AUD) is a prevalent, world-wide problem, and in some countries it is accelerating. ‘Alcoholics Anonymous’ (or AA for short) has been a popular treatment for alcohol use disorder for decades, but much debate has persisted on whether AA – and related 12-step clinical treatments designed to increase AA participation are effective.
AA are peer-led mutual-help groups. Twelve-step facilitation programs adopt some of the principles and techniques of AA and are delivered by clinicians. They are aimed at engaging people within AA during and after treatment for alcohol use disorder. Some of these programs follow a manual, so that the same treatment can be delivered at different times and places.
This Cochrane review looks at the effects of these programs on reducing alcohol consumption and the effects of heavy drinking (such as physical health, family, or employment problems), and enhancing long-term abstinence. The authors of the review also examined whether AA and TSF programs reduce healthcare costs compared to other treatments.
The previous Cochrane review published in 2006 was based on the eight available studies including a few thousand participants. The quantity and quality of the research has increased substantially since then. Twenty-seven studies are now included in this updated Cochrane review, comprising 10,565 people. The studies included in this update examined a range of programs that differed in their approach and intensity, and these were compared against other programs and different treatments for alcohol use disorder.
The authors found high certainty evidence that clinically delivered and manualized TSF programs designed to increase AA participation can lead to higher rates of continuous abstinence over months and years, when compared to other active treatment approaches such as cognitive behavioural therapy. The evidence suggests that 42 % of participants participating in AA would remain completely abstinent one year later, compared to 35% of participants receiving other treatments including CBT. This effect is achieved largely by fostering increased AA participation beyond the end of the TSF program.
When compared to the other treatment approaches Alcoholics Anonymous (AA)-based programs may perform just as well at reducing drinking intensity, negative alcohol-related consequences and addiction severity.
Dr. John Kelly, Elizabeth R. Spallin Professor of Psychiatry at Harvard Medical School and Director of the Massachusetts General Hospital Recovery Research Institute said, “Alcohol use disorder can be devastating for individuals and their families and it presents a significant, worldwide, costly public health problem. Alcoholics Anonymous is a well-known, free, mutual-help fellowship that helps people recover and improve their quality of life. One important finding from this review was that it does matter what type of TSF intervention people receive - better organized and well-articulated clinical treatments have the best result. In other words, it is important for clinical programs and clinicians to use one of the proven manualized programs to maximize the benefits from AA participation.”
“In terms of healthcare costs, policy makers will be interested that four of the five economics studies we identified showed considerable cost-saving benefits for AA and related 12-step clinical programs designed to increase AA participation, indicating these programs could reduce healthcare costs substantially.”
- Full Citation: Cochrane Database of Systematic Reviews: Kelly JF, Humphreys K, Ferri M. Alcoholics Anonymous and other 12-step programs for alcohol use disorder. Cochrane Database of Systematic Reviews 2020, Issue 3. Art. No.: CD012880
- Read interview with author, John Kelly
- For further information, contact [email protected]
- Follow us on twitter @cochranecollab
Advertisement
Supported by
Complications From Alcohol Use Are Rising Among Women
New research shows that alcohol-related liver disease and other health problems increased even more than expected among women ages 40 to 64 during the pandemic.
- Share full article

By Dani Blum
A new study adds to a mounting body of evidence showing that rising alcohol consumption among women is leading to higher rates of death and disease. The report, published Friday in the journal JAMA Health Forum , examined insurance claims data from 2017 to 2021 on more than 14 million Americans ages 15 and older. Researchers found that during the first year and a half of the coronavirus pandemic, women ages 40 to 64 were significantly more likely than expected to experience serious complications like alcohol-related cardiovascular and liver disease, as well as severe withdrawal.
The Background
Alcohol consumption in the United States has generally increased over the last 20 years , said Dr. Timothy Naimi, the director of the Canadian Institute for Substance Use Research at the University of Victoria. Dr. Naimi was a co-author on a recent paper that showed deaths from excessive alcohol use in the United States rose by nearly 30 percent between 2016 and 2021.
While men still die more often from drinking-related causes than women, deaths among women are climbing at a faster rate. “The gap is narrowing,” said Dr. Bryant Shuey, an assistant professor of medicine at the University of Pittsburgh and the lead author of the new study.
The Research
The study looked at serious health issues related to drinking, including alcohol-related liver and heart disease, inflammation of the stomach lining that led to bleeding, pancreatitis, alcohol-related mood disorders and withdrawal. Researchers compared insurance claims data for these complications with the rates they expected to see based on past prevalence of these conditions.
In nearly every month from April 2020 to September 2021, women ages 40 to 64 experienced complications from alcohol-related liver disease — a range of conditions that can develop when fat begins to accumulate in the liver — at higher rates than researchers predicted. If damage from drinking continues, scar tissue builds up in the liver and leads to a later stage of the disease, called cirrhosis. Some people with alcohol-related liver disease also develop severe liver inflammation, known as alcohol-associated hepatitis.
Rates of alcohol-related complications during the pandemic were also higher than predicted among men ages 40 to 64, but those increases were not statistically significant. But “men are not out of the woods” and still face health risks, Dr. Shuey said.
The Limitations
The study examined data only up until September 2021. Katherine Keyes, a professor of epidemiology at Columbia University who was not involved in the latest study, said she expected that alcohol use might keep rising among women — a pattern that could contribute to even more health issues.
And since the study relied on insurance claims, Dr. Shuey said it told an incomplete story. If someone is treated in the emergency room for an inflamed pancreas but doesn’t disclose a drinking history, for example, that instance may not be registered as an alcohol-related complication.
“The truth is, we’re probably underestimating this,” he said.
The Takeaways
These findings underscore how patterns of heavy drinking can translate into serious health consequences. Over the last 10 years, a growing number of American women — and particularly women in middle age — have reported binge-drinking, Dr. Keyes said.
“It used to be that 18- to 25-year-old males were the most likely to drink or the most likely to binge,” said Aaron White, a neuroscientist at the National Institute on Alcohol Abuse and Alcoholism. Now, binge drinking occurs more among people between the ages of 26 to 34, and is becoming more common among women. “Everything’s just getting pushed back later,” he said.
Demographic shifts can also help explain why women are drinking at higher rates, Dr. Keyes said. Women tend to marry and have children at later ages than in previous decades, so they spend more time in what Dr. Keyes calls a “high-risk period for heavy drinking.”
“People don’t realize the real health consequences these heavy drinking patterns can have,” she added.
These consequences take time to develop and often emerge between ages 40 and 60. Complications can occur after “years of heavy, persistent alcohol use,” Dr. Shuey said.
These longer-term increases in drinking predate the pandemic and might have increased the risk of health problems among women before Covid-19 hit. But higher levels of drinking during lockdowns may have exacerbated these issues or contributed to new complications, especially as women bore the brunt of family responsibilities, Dr. White said.
Even as research mounts on the harms of alcohol, many people might struggle to change their habits, Dr. White said.
“If you’ve been drinking wine with dinner every night for the last 20 years, just seeing a headline is not going to be enough to make you throw your wine away,” he said. “I think it’s going to be a slow cultural shift.”
Dani Blum is a health reporter for The Times. More about Dani Blum

Why Findings on Alcohol and Health Are So Confusing
Who is considered an abstainer matters..
Posted April 11, 2024 | Reviewed by Jessica Schrader
- What Is Alcoholism?
- Find counselling to overcome addiction
- Recent alcohol and health findings seem to contradict each other.
- How scientists classify abstainers and drinkers explains some of the contradictory results.
- Having more than two drinks a day increases your health risk.

If you've been perplexed by current findings on alcohol and health, there's a good reason. Results from recent scientific studies run the gamut from finding that modest alcohol consumption is better for your health than not drinking at all, to the World Health Organization stating that no level of alcohol is safe . How can there be such wide discrepancies in these findings? To understand why, I recently attended the National Academy of Sciences, Engineering, and Medicine public meeting, Review of Evidence on Alcohol and Health . Presenters illustrated several issues with how these studies are conducted that have led to the current confusion.
First, let’s cover the classic pattern of alcohol and health, which is something scientists call a J-shaped curve, in which low alcohol consumption (no more than zero to two drinks a day) has a lower risk of health problems than abstaining from alcohol. Health risks increase noticeably from low consumption to moderate and from moderate to high. While those of us who enjoy modest consumption of alcohol are happy to hear about such findings, the results are counterintuitive. Why would abstainers have worse outcomes than those with modest alcohol consumption?
As explained by Tim Stockwell, former director of the Canadian Institute for Substance Use Research at the University of Victoria, lifetime abstainers start out less healthy than their drinking peers, beginning at the legal drinking age. In early adulthood, lifetime abstainers tend to have more disabilities, worse health, and less income than young adults who consume alcohol. This difference in overall health status then increases with age. He noted, “The widening disparity in the health status of these groups leads to larger apparent health benefits from drinking alcohol for older adults.”
The classification of abstainer vs. drinker matters
Additionally, when people become unwell, they reduce or abstain from drinking. If they participate in an alcohol study, these people often are classified based on their current status as abstainers rather than as former drinkers. Indeed, Stockwell described how former drinkers at all levels have higher health risks than their current-drinker counterparts.
These selection biases can lead to the appearance of a health benefit from modest alcohol intake that does not exist. Stockwell and his colleagues demonstrated that longitudinal studies that exclude former and occasional drinkers from the abstainer category find that low-volume drinkers have an equivalent mortality risk as abstainers, whereas studies that do not take these biases into account find the "typical" reduced mortality risk for low volume drinkers compared to abstainers. Thus, the J-shaped curve goes away in studies that control for important selection biases.
Drinking regularly is not great for your health
While there has been controversy regarding the results pertaining to low-volume drinkers, the results for heavier volumes of drinking are consistent: The more you drink, the greater the health risk. How great is the risk? Compared to lifetime abstainers, medium-volume drinkers (averaging two to three drinks per day) have a 5% greater risk ; people who average three-to-four-and-a-half drinks per day have a 19% greater risk of all-cause mortality compared to lifetime abstainers; those who average 5 or more drinks per day have a 35% greater risk for all-cause mortality.
Unfortunately for women, their increased health risks begin at a lower volume of drinking than for men. Women face a significantly greater risk for all-cause mortality starting at an average of two-to-three drinks per day, whereas for men, a similar level of risk appears when averaging three-to-four-and-a-half drinks per day. When I asked Stockwell if this disparity is simply due to typical sex differences in body size, he said that it’s difficult to tell. For one thing, men and women tend to have different drinking patterns. Importantly, he noted that there fewer good alcohol and health studies have focused on women.
What does this mean for you?
What do these findings mean for everyday people? According to Stockwell, “It’s important to be skeptical of claims that modest alcohol consumption is good for health. Regardless of the type of alcoholic beverage, they all contain ethanol, which has toxic, addictive, and carcinogenic effects.” In other words, if you currently imbibe two or more drinks a day, you may want to consider making alcohol more of an occasional treat rather than a part of your daily routine.
de Gaetano, G, Costanzo, S. (2017). Alcohol and Health: Praise of the J Curves∗. Journal of the American College of Cardiology, 70 (8) 923 925. https://doi.org/10.1016/j.jacc.2017.07.710
Stockwell T, Zhao J, Clay J, Levesque C, Sanger N, Sherk A, Naimi T. (2024). Why do only some cohort studies find health benefits from low volume alcohol use? A systematic review and meta-analysis of study characteristics that may bias mortality risk estimates. Journal of the Study of Alcohol and Drugs . doi: 10.15288/jsad.23-00283.
World Health Organization (January 4, 2023). No level of alcohol consumption is safe for our health.
Zhao J, Stockwell T, Naimi T, Churchill S, Clay J, & Sherk A. (2023). Association Between Daily Alcohol Intake and Risk of All-Cause Mortality: A Systematic Review and Meta-analyses. JAMA Network Open. 6(3):e236185. doi:10.1001/jamanetworkopen.2023.6185

Quinn Kennedy, Ph.D., is the Director of Aging Research at neuroFit and CEO of QK Consulting.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Toxicol
- v.12(1); 2016 Mar

Case Presentations from the Addiction Academy
Joan r. laes.
Division of Addiction Medicine, Hennepin County Medical Center, 701 Park Avenue, Mail Code G5, Minneapolis, MN 55415 USA
Timothy Wiegand
University of Rochester Medical Center & Strong Memorial Hospital, Rochester, NY USA
In this article, a case-based format is used to address complex clinical issues in addiction medicine. The cases were developed from the authors’ practice experience, and were presented at the American College of Medical Toxicology Addiction Academy in 2015. Section I: Drug and Alcohol Dependence and Pain explores cases of patients with co-occurring pain and substance use disorders. Section II: Legal and Policy Issues in Substance Use Disorders highlights difficult legal and policy questions in addiction medicine. Section III: Special Populations and Addictive Disorders delves into the complexity of addiction in special populations (pregnant, pediatric, and geriatric patients).
Introduction
The case studies described in this article were presented as panel and small group discussion sessions at the American College of Medical Toxicology “Addiction Medicine Academy” symposium in March 2015. The individuals who participated in the panel and led the group sessions are listed in the appendix. These cases were developed based on the practice experiences of the author and faculty participating in the discussions. The ensuing discussions are described in the question and answer style of the group sessions.
The cases in Section I: Drug and Alcohol Dependence and Pain describe issues that arise in the treatment of pain in patients with a history of, or concerning features for, substance use disorder. In Section II. Legal and Policy Issues in Substance Use Disorders , addiction medicine legal and policy perspectives are discussed through case-based format. In Section III: Special Populations and Addictive Disorders , the cases highlight the complex clinical issues medical providers face in the management of addiction in special populations including pregnant women, pediatrics, and the elderly.
Section I: Drug and Alcohol Dependence and Pain
A 54-year-old woman with chronic pain due to inflammatory arthritis presents to the emergency department (ED) stating that she is having a “flare” of her arthritis, but is out of her Oxycontin® and immediate-release oxycodone. She is aware that it is too early to fill her prescriptions, but she insists that she will be traveling out of state and “really needs” her medications. She presents on a Saturday when her clinic is closed, and her primary care physician is “on vacation.”
Question: How do you Approach This Patient in the ED?
Due to the escalation of opioid misuse in the USA, many EDs have instituted guidelines limiting refills of opioid medications for chronic pain concerns, particularly when there is no objective evidence of for an acute etiology of changes in pain [ 1 ].
Additional steps to the approach of this patient include:
- Conducting an evaluation for medical conditions causing the change in symptoms.
- Reviewing the prescription monitoring program database if available in the state of practice.
- Determining how early the refill request is, and her recent pattern of opioid use.
- Considering non-narcotic therapies.
- Determining risk of withdrawal or adverse events if the medication is not refilled.
In this scenario, several “red flags” suggest that the patient has a substance use disorder. She is using her prescribed opioid analgesics inappropriately by taking extra doses, and has subsequently run out of medications early. She is also presenting to the emergency department rather than returning to her physician for refills. Additionally, her “off-hour” presentation occurs at a time when her prescribing physician cannot be reached for verification and direction. Most physicians that provide opioid prescriptions use a contract that includes information about early refills and use of non-prescribed medications and illicit drugs. Some hospitals or physician groups include patient opioid contracts in their electronic health record (EHR).
Case 1 Alternate Scenario
The patient then presents to her primary care physician of 1 year with objective painful conditions (inflammatory arthritis, severe osteoarthritis, knee replacement, and a hip fracture associated with chronic prednisone use). She requests continued opioid therapy for these conditions. While this patient has been under her PCP’s care, the physician has received concerning information regarding her use of alcohol; a Driving Under the Influence charge, spousal complaints about her drinking, and a discharge summary from the emergency department visit related to injuries sustained after a fall from “mixing her pills with her drinks.”
Question: How do you Approach Management of This Patient in the Primary Care Setting?
Alcohol misuse is a contraindication to the prescription of opioid therapy for pain. The combination of alcohol and opioids synergistically increases the potential for sedation; a recent study found that the misuse of alcohol was a common feature in prescription opioid-related ED visits [ 2 ]. Many physicians obtain an “informed consent agreement,” or a “pain contract,” as the standard of care for treating patients with opioids. These agreements detail the risks of chronic opioid therapy and outline guidelines for treatment, including warnings that patients should not be using alcohol or illicit drugs while receiving opioids. Many providers will monitor for alcohol use in patients receiving chronic opioids, incorporating urine ethyl sulfate or ethyl glucuronide testing for ethanol use.
Approaches to the management of patients who abuse alcohol in the setting of chronic opioid therapy vary. Strategies include limiting or tapering opioid therapies, referral to pain management specialists, or offering screening, assessment, brief intervention, and referral to treatment (SBIRT) for alcohol use disorder.
When chronic pain patients abuse alcohol or other substances, specific pain and addiction program referral is available in some areas. These programs include personalized treatment aimed at the substance use disorder, as well as the complex nexus of pain and addiction. Alternatives to opioid analgesics include non-opioid medications (muscle relaxants, NSAIDs), physical therapy, mindfulness, biofeedback, and relaxation techniques.
A 30-year-old woman with a history of recent intravenous (IV) drug use is admitted to the observation unit for IV antibiotics after the incision and drainage of an antecubital abscess. She has a history of opioid and cocaine dependence.
She receives IV morphine followed by IV hydromorphone for acute pain, as she had a significant debridement performed. After the procedure, she is demanding increasingly higher doses of IV opioids, and the observation unit team is becoming uneasy regarding the dose and frequency of opioid medications that she is receiving. The nursing staff raises concerns that she has tampered with her IV tubing and may be using her IV to “inject something.”
Question: How do you Approach This Patient with Respect to her Pain and her Behavior?
Given her history of opioid dependence, this patient is tolerant to opioids; her physiological requirements for analgesia are higher than expected when compared to an opioid-naïve patient. Careful assessment of physical and psychological indices of pain, and evaluation for other conditions that may be contributing to pain (i.e., recurrent infection, thrombosis, etc.) are indicated. Symptoms of opioid withdrawal should also be assessed. In this setting, it is essential to discuss the pain management plan with the patient in a non-judgmental manner that describes the course of treatment. Anxiety concerning withdrawal or unmanaged pain can drive requests for additional opioid medications or unusual behaviors during treatment. A common pitfall in the management of pain in opioid-dependent persons is a lack of consideration for analgesic needs above their baseline opioid tolerance. Healthcare providers are often concerned about the potential respiratory depression secondary to high opioid doses, without recognizing the tolerance to respiratory depression that opioid dependence confers; the “amount” of opioid has less importance in pain management than close clinical monitoring of patient response. Monitoring in patients receiving high-dose opioids must include vital signs and overall level of arousal and wakefulness, as well as other clinical assessments like oxygen saturation and end-tidal carbon dioxide measurement (capnography). These tools may indicate either insufficient or excessive opioid dose.
The treatment plan should be coordinated with the primary care provider with involvement of a pain specialist, if available. Opioid-tolerant patients may have a prolonged recovery after a painful illness or injury. Some healthcare systems have dedicated committees of multidisciplinary specialists, including psychiatry, pain management, addiction medicine, internal medicine, and emergency medicine providers to convene and discuss management of these difficult cases. When a patient truly does not respond to (or worsens with) opioid analgesia, opioid-induced hyperalgesia must be considered, which would improve with the decrease/cessation of opioids—notably, this a difficult concept to implement in a patient at risk of opioid withdrawal. In hospitalized patients, additional options include simultaneous treatment with agents that enhance or otherwise modify the opioid effect, such as ketamine [ 3 ] and alpha-2 agonists [ 4 ]. Delivery of adjunctive treatments such as nerve blocks or administration of intrathecal opioids singly or alongside other medications by appropriately trained providers can also provide relief to selected patients.
Specific strategies:
- Using a combination of long-acting and short-acting opioids, scheduling both the long- and short-acting opioids, and informing the patient regarding the schedule.
- Switching to oral formulations as soon as possible.
- Maximizing non-narcotic therapies.
- Considering initiation of methadone in the hospital for management of baseline tolerance and opioid use disorder, with referral to an addiction medicine program that incorporates opioid agonist treatment.
- Urine drug testing for concerns about IV use of illicit drugs, such as heroin, in the hospital.
- Consider buprenorphine for both pain and addiction in appropriate hospitalized patients. However, provider experience and knowledge of buprenorphine pharmacology is critical to the success of buprenorphine therapy in this setting.
A 27-year-old woman on buprenorphine-naloxone (Suboxone®) for treatment of opioid dependence is admitted to the hospital with severe abdominal pain due to a perforated gastric ulcer. She received hydromorphone in the ED, and is urgently taken to the operating room. Postoperatively, she is on a patient-controlled analgesic (PCA) pump containing fentanyl. Her last dose of buprenorphine-naloxone was 20 h prior to the surgery; her daily dose is 16 mg.
Question: How can Pain be Managed in Patients who are Taking Buprenorphine-Naloxone? What Adjustments to her Medication Regimen can be Recommended?
Whether the patient is on methadone or buprenorphine-naloxone for treatment of opioid use disorder, clarification of patient history is critical for making management decisions regarding pain, as well as continuation of therapy for opioid dependence. Important clinical actions include the following:
- Understanding the medication history. What was the medication schedule? Once or twice daily use? Recent dose changes? How often are doses missed? How many doses are directly observed?
- Obtaining consent to discuss management with prescribing provider.
- Reviewing the prescription monitoring program records, if available, noting that methadone from an opioid treatment program is not documented in the databases.
- Identifying any concomitant use of additional opioids or sedating medications (prescribed or non-prescribed).
The article “Acute Pain Management for Patients Receiving Maintenance Methadone or Buprenorphine Therapy” by Alford et al. [ 5 ] provides an excellent summary of options for pain management:
- Continue buprenorphine maintenance therapy and titrate short-acting analgesics. Doses required to provide analgesia are higher than expected and should be titrated to response. High-potency analgesics, such as fentanyl or hydromorphone, are suitable choices.
- Divide the pre-surgery daily buprenorphine dose every 6–8 h, with consideration of supplemental doses as needed for additional analgesia.
- Discontinue buprenorphine therapy and use a combination of long- and short-acting opioid analgesics, again noting that a higher dose is needed to meet both baseline opioid tolerance and analgesia requirements. The half-life of buprenorphine is approximately a day; expect that 1–2 days after last buprenorphine dose, other opioids will start to have more effect at the opioid receptor. The patient should be closely monitored during this time period. Convert back to buprenorphine by re-induction methods when pain is resolved.
- Discontinue buprenorphine and treat opioid dependence with methadone 20–40 mg. Use additional short-acting opioid analgesics to treat pain, with consideration to schedule doses. Note that this is only an option for hospitalized patients.
Any of the above treatment plans should include additional psychosocial support, such as mutual help groups, increased frequency of visits to their treating physician, or brief counseling sessions from a licensed alcohol and drug counselor or peer support specialist.
For buprenorphine re-induction, management should occur in tandem with the patient’s buprenorphine prescriber, especially if the plan is to restart buprenorphine as an outpatient. Buprenorphine re-induction can proceed in the hospital or at home, with an abbreviated version of a typical induction regimen. Once acute pain needs related to surgery have improved, discontinue short-acting opioids for 16–24 h depending on the opioid. Then, administer sequential doses of 2 mg buprenorphine up to previous maintenance dose over a 4-h period. If the pain persists, a more frequent dosing regimen (e.g., every 6–8 h) is indicated instead of the standard daily or twice daily dosing that most buprenorphine maintenance patients receive. The patient must follow up with his/her regular buprenorphine provider soon after hospital discharge.
Question: If This Patient was on Methadone Maintenance for Treatment of Opioid Use Disorder, How Should Pain be Managed?
Treatment of pain in patients maintained on methadone tends to be less complicated than those receiving buprenorphine-naloxone. Continue the patient’s methadone at the normal maintenance dose if she can tolerate oral medications. If the patient is not able to take medications by mouth, IV methadone is a viable alternative. Treat pain with additional short-acting opioids as needed; doses are likely to be higher than expected to provide analgesia in opioid-naïve patients.
Question: What Options are Available for Pain Management if This Patient was Being Treated With Oral Naltrexone for Opioid Use Disorder?
First, the provider must determine which form of naltrexone the patient is receiving (e.g., Revia® PO or Vivitrol® IM). If a painful condition can be anticipated (such as an elective surgery), the oral form of naltrexone should be discontinued for 2–3 days prior, or the last dose of intramuscular naloxone should be given 30 days beforehand. Administer opioids in typical doses after that time. If pain is unanticipated (e.g., trauma), rapidly acting potent opioids like fentanyl should be carefully titrated to patient response, including respiratory rate, level of awareness, and level of analgesia. This management strategy requires close monitoring; respiratory support and reversal agents must be available. A second option is the use of non-narcotic analgesics, like non-steroidal anti-inflammatory drugs, ketamine, or local/regional/general anesthesia.
Before resuming naltrexone after receiving opioid analgesics for pain, it is recommended the patient be abstinent from opioids for at least 3 to 5 days although this may need to be longer for patients given long-acting agents such as methadone, oxymorphone or that have been on a fentanyl patch. This is to mitigate any potential for precipitated withdrawal symptoms developing when the antagonist, naltrexone, is administered too closely after the full agonist used for pain.
The emergency department contacts a medical toxicologist with a question regarding a patient seen frequently for pain complaints. His outpatient providers have been managing his opioid therapies for chronic pain, but the patient often runs out of pills early, misses scheduled pills counts, or has non-prescribed substances identified on urine drug testing. The patient denies that he has an “addiction problem,” and states his increased use is due to uncontrolled pain. The provider asks whether these behaviors are due to addiction or pain, and if this patient should be referred to addiction medicine.
Question: How is Opioid use for Pain Versus Addiction Differentiated?
This is a difficult question. Clinicians will encounter this conundrum frequently when treating patients who receive chronic opioids. Separating behaviors related to unmanaged pain versus an opioid use disorder can be very challenging. The Diagnostics and Statistics Manual (DSM)-V criteria for opioid use disorder [ 6 ] (see Table Table1) 1 ) provide a useful framework. In addition to the DSM-V, several brief validated questionnaires are available to estimate the risk of opioid-related aberrant behaviors. The Opioid Risk Tool (ORT) is a five-question assessment that helps to identify patients at high risk for misuse that might benefit from other modalities of pain control besides opioids [ 7 ]. The ORT is primarily applicable to patients with chronic pain. The Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R) [ 8 ] is a slightly longer instrument which can also be used to predict opioid abuse in chronic pain patients. This tool includes aspects of self-report and observation as well as toxicology testing. The “Current Opioid Misuse Measure (COMM)” is a self-report assessment of past month aberrant medication-related behaviors [ 9 ]. The questions encapsulate signs and symptoms of inappropriate drug use, psychological issues, and compliance. Examples of aberrant behaviors include being more interested in opioids than other forms of treatment, seeking early refills, and requesting increasing doses of opioids. While the presence of aberrant behaviors can indicate a substance use disorder, patients may display aberrant behaviors for reasons other than addiction, such as misunderstanding instructions, seeking euphoria, using medications to deal with fear or stress, using medications to treat sleep problems, diverting medications for profit, coping with untreated psychiatric disorders, coping with undertreated pain, or general non-adherence. “Pseudoaddiction” is a controversial term of primarily historical significance thought to describe behaviors that mimicked those of addiction, but were actually due to severe, uncontrolled pain.
DSM-V criteria for substance use disorder
Section II. Legal and Policy Issues in Substance Use Disorders
A 20-year-old man is brought to the emergency department (ED) by his family for evaluation. His family reports that he failed out of school in his second year at a local community college. He admits to escalating struggles with prescription pain pills (prescription opioids), and then heroin use. He appears to be in opioid withdrawal; he describes anorexia and diarrhea, and is yawning and sweating on exam. He has a Clinical Opioid Withdrawal Scale (COWS) [ 10 ] (Fig. 1 ) score of 15, indicating moderate withdrawal. His provider orders clonidine, ondansetron, and 2/0.5 mg sublingual buprenorphine/naloxone, with a plan to observe him in the ED. The provider subsequently receives a concerned call from the hospital pharmacist.

Clinical opiate withdrawal scale
Question: The Pharmacist States That the Provider is Unable to Administer Buprenorphine in the ED Without an X-Waivered DEA Number. Is This Accurate?
In the ED setting, an X-waiver is not required. The distinction is that the providers are administering or dispensing buprenorphine, not prescribing it for outpatient use (please see Fig. 2 ). Under the Title 21 Code of Federal Regulations Section 1306.07 [ 11 ]: Administering or dispensing of narcotic drugs: “Nothing in this section shall prohibit a physician who is not specifically registered to conduct a narcotic treatment program from administering (but not prescribing) narcotic drugs to a person for the purpose of relieving acute withdrawal symptoms when necessary while arrangements are being made for referral to treatment. Not more than one day’s medication may be administered to the person or for the person’s use at one time. Emergency treatment may be carried out for not more than three days and may not be renewed or extended.” Section 1306.07 also declares that “This section is not intended to impose any limitations on a physician or authorized hospital staff to administer or dispense narcotic drugs in a hospital to maintain or detoxify a person as an incidental adjunct to medical or surgical treatment of conditions other than addiction or to administer or dispense narcotic drugs to persons with intractable pain in which no relief or cure is possible or none has been found with reasonable efforts.”

Title 21 Code of Federal Regulations 1306.07—Administering or Dispensing of Narcotic Drugs
This section of the Federal Regulations allows physicians in a hospital or ED to treat acute withdrawal with buprenorphine or methadone while the patient is attempting to access treatment. The patient may not receive more than 3 days of administered methadone in the emergency department or hospital unless there is a concomitant acute medical or surgical condition requiring treatment. Additionally, the patient may not be given a prescription for the medication upon discharge from the facility. For example, if the patient is hospitalized with an abscess, they may be treated for opioid withdrawal for the duration of their hospital encounter, but they may not be discharged with a prescription for methadone or buprenorphine. If a patient who is currently in a medication-assisted treatment program is hospitalized, their medication may be continued in the hospital, but they may not be discharged with a prescription. They must return to their prescribing provider for continued care. It is important to clarify their treatment plan with their provider and to verify the dose and schedule. Providers who administer buprenorphine in the ED for opioid withdrawal must follow standard buprenorphine induction guidelines [ 12 ]. An exception to the above rule exists when the treating provider is X-waivered (able to prescribe buprenorphine for the treatment of opioid dependence) and they are able to link the patient to either their own clinic or another provider who also has X-waiver certification and agrees to continue the buprenorphine prescription.
A provider is covering a county detoxification program (from alcohol and opioids) with 30 beds. The program is funded through the state’s Office of Alcohol and Substance Abuse Services, and operates under the Code of Federal Regulations (CFR) Title 42 Part 2 [ 13 ] guidelines regarding privacy and notification.
Question: What is CFR-42 Part 2?
Under federal law, there are restrictions concerning the use and disclosure of patient records pertaining to substance abuse treatment. CFR Title 42 Part 2 applies to any individual or entity that is federally assisted, and holds itself out as providing, and provides, alcohol or drug abuse diagnosis, treatment, or referral for treatment. Most drug and alcohol treatment programs are federally assisted. For-profit programs and private practitioners that do not receive federal assistance of any kind are not subject to the requirements of CFR Title 42 Part 2, unless the state licensing or certification agency requires them to comply. However, any clinician who uses a controlled substance for detoxification or maintenance treatment of a substance use disorder requires a federal Drug Enforcement Agency (DEA) registration, and becomes subject to the regulations through the DEA license. The restrictions under CFR Title 42 Part 2 apply to any information disclosed by a covered program that would identify a patient as a current or past alcohol or drug abuser, or as a participant in a covered program.
Case Continued
A woman calls the program, and identifies herself as the mother of one of the patients. She states that she does not want to intrude, but wants to confirm he actually made it to detox, saying “I just need to know if he’s there and safe.”
Question: Can the Provider Disclose his Presence at the Facility?
With limited exceptions, CFR Title 42 Part 2 requires patient consent for disclosures of protected health information even for the purposes of treatment, payment, or healthcare operations. Consent for disclosure must be documented in writing. Without consent, programs publicly identified as only a drug or alcohol diagnosis, treatment, or referral facility cannot disclose whether the person in question is a current or past patient. However, the regulations permit a provider to say that an identified individual is not, and never has been, a patient.
Case 6 Continued
Police arrive at the facility and state they have a warrant to arrest the patient. Apparently, his ex-girlfriend told the police that he was at this detoxification facility when they inquired about his location. The police will not discuss the charges, simply reiterating that they have an arrest warrant.
Question: What are the Obligations to Disclose Patient Information to Law Enforcement in This Setting?
If an immediate threat to the health and safety of an individual exists due to a medical emergency or crime on the program premises or against program personnel, information about a patient’s treatment may be disclosed without the patient’s consent to medical personnel in a medical emergency, or to law enforcement agencies. If there are threats to health and safety that do not involve medical emergencies or crimes on the program premises, reports can be made to law enforcement only if patient-identifying information is not disclosed. The restrictions do not apply to reporting incidents of child abuse or neglect to state authorities under state law; however, the restrictions continue to apply to the original alcohol or drug abuse records maintained by the program. Information may also be disclosed if there is both a court order to authorize disclosure, as well as a subpoena or similar legal mandate issued to compel disclosure. If presented with an arrest warrant, the healthcare provider cannot acknowledge the patient is on the premises unless the patient gives authorization, or if there is a court order authorizing disclosure. If law enforcement asks to speak with a patient, the provider may respond by informing them of a need to speak with supervisors, then discussing with the patient his willingness to provide written release if they are willing to speak with law enforcement.
A new patient presenting for buprenorphine-naloxone assisted treatment discloses that she is a PGY4 general surgery resident in a city 90 min away. She admits to intravenous heroin use (“20-30 bags a day”), along with cocaine and alprazolam. She reports that she is missing days of work due to heroin use, and has occasionally used heroin and cocaine while in the hospital, and before surgery just to “feel right.” She states that she presented to this distant provider because she did not want to be treated by anyone who might be affiliated with her training program.
Question: When is a Physician Considered “Impaired”? How Should Management of This Patient be Approached? Is There any Obligation to Notify Either the State Medical Board or her Residency Program Director?
When the health of the physician has declined to the point of causing interference with his or her ability to safely engage in professional activities, the physician is said to be impaired. Medical professionals have an obligation to intervene when it appears that the health of a colleague is compromised by addiction. In many states, it is legally permissible to report health professionals to the state’s impaired professionals program rather than to the professional licensing boards. Generally, impaired professional programs offer treatment programs while protecting confidentiality and the licensure of the professional. These programs also aim to prevent workplace safety concerns and harm to patients. Physicians caring for colleagues should not disclose patient information, except as required by law, ethical or professional obligation. Exceptions to the confidentiality of the physician and physician-patient relationship occur if the treating professional determines that the condition of the person constitutes a danger to public safety if the impaired colleague was to continue practice. In this case, the severity of the addiction with her self-reported use during patient care compels the treating physician to notify the state impaired professional program.
A 23-year-old woman attends an outpatient treatment program and office-based buprenorphine clinic. She has been doing well while maintained on 16 mg/day of buprenorphine. Recently though, she has missed group sessions and provided a urine for drug screening that tested positive for clonazepam and amphetamine. One of the other members in her group reported that they saw a “urine bottle fall out of her purse” as it spilled next to her chair in a group session; her counselor was unaware of this event.
Question: What are the Policies Regarding the use of Illicit Substances or Urine Adulteration or Substitution During Substance Abuse Treatment?
Policies should be determined by an individual provider or clinic. Typically, these policies provide balanced rules that seek to limit abuse, diversion, and harm from the administered medications, while providing the patient with direction, structure, and accountability. To increase awareness of program policies and expectations for patients, it is advisable to use special acknowledgment and treatment consent forms that describe program policies. Information regarding model buprenorphine policies and contracts for office-based buprenorphine programs are available from the Substance Abuse Mental Health Services Administration (SAMHSA) website [ 14 ].
Abnormal urine drug screens can be a first sign of dysfunction and relapse. The initial response is directed at helping the patient stabilize and recover their sobriety. For example, in many office-based buprenorphine programs, urine drug screens positive for non-prescribed or illicit substances prompt an increase in support services rather than a decrease (unlike a contract agreement for management of pain in primary care or specialty pain clinics). Increased support may include more therapeutic group attendance, individual counseling, referral to a more intensive treatment setting, or more frequent visits to the physician for medication management with enhanced accountability using observed dosing or additional “check-ins” with the patient’s counselor. Adulteration or substitution of urine is often considered a “positive urine drug screen.” Sometimes, if patients are not receiving enough of an opioid agonist to attenuate craving and withdrawal, dose increases can be helpful. This serves to both alleviate cravings for opioids, as well as limit the euphoria obtained from use.
The provider response also depends on the specific area of difficulty or conflict. Monitoring during buprenorphine treatment includes not only testing for illicit drug use in order to demonstrate effectiveness and sobriety, but also confirms compliance with the presence of buprenorphine, and adequate concentrations when levels or metabolite ratios are assayed. If there were signs that the patient was skipping doses or manipulating their dosing in order to use part way through a prescription, the response would be different. While providers avoid using a lower dose of a medication as a behavioral tool, limited circumstances (e.g., chronic non-compliance with treatment recommendations, or co-ingestion of sedatives or alcohol that can lead to overdose) may necessitate an “administrative” taper. Patients whose urine drug testing do not confirm appropriate buprenorphine levels may be diverting their medications. If there is concern for diversion of the medication, the response may be to limit the amount prescribed at one time, or to observe medication administration.
Responses to marijuana use, especially in states where medical marijuana or recreational marijuana is legal, vary widely. If the marijuana use does not interfere with treatment or the function of the patient, many programs do not address use as intensely as other drug use (such as heroin, non-prescribed opioids, or stimulants). Our panel would typically not sanction the patient for marijuana use, but direct more attention to counseling and focus on addressing the patient-reported motivation behind marijuana use. Patients who reported untreated pain as the reason behind marijuana use would be directed at alternative strategies to control the pain including mindfulness, physical therapy, yoga, and stretching. If the marijuana was used to regulate sleep or mood, the provider could recommend alternatives such as melatonin for insomnia, and confirm the patient has adequately addressed mental health resources.
Section III: Special Populations and Addictive Disorders
The toxicology service is consulted from the emergency department (ED) as the county jail staff has brought in a 21-year-old Hispanic woman who is 18 weeks pregnant. She was arrested on a warrant, and has been incarcerated for just over 24 h. During that time, she developed nausea, irritability, diaphoresis, anxiety, and yawning. She was noted to have stigmata of intravenous drug use (IVDU), and told the intake officers that she was going into heroin withdrawal.
Question: What is the Initial Approach to This Patient’s Care?
Heroin use during pregnancy is associated with fetal growth restriction, fetal death, and preterm labor [ 15 ]. Moreover, opioid withdrawal in pregnancy (especially during the first and third trimester) is associated with poor fetal outcomes, such as miscarriage and premature delivery [ 16 ]. Withdrawal symptoms in pregnant patients should be managed with medication. Initiation of methadone or buprenorphine is indicated during the acute care encounter, and can be initiated (or continued) by physicians even without a Drug Addiction Treatment Act (DATA) 2000 waiver (the waiver authority for physicians to prescribe buprenorphine in an office-based setting outside of a registered opioid treatment program). If a patient is hospitalized for reasons other than addiction (such as complications due to pregnancy, or delivery), physicians may administer opioids such as methadone or buprenorphine to initiate or continue maintenance treatment. Under these circumstances, the hospital treatment team does not require registration as an opioid treatment program, nor do they need a DATA 2000 waiver.
Pregnant patients must be connected to treatment resources prior to discharge from the ED or hospital. In most states, pregnant patients are prioritized for treatment; medication-assisted treatment programs will often initiate the intake process within 1–2 business days.
Question: What is the Safety of Methadone, Buprenorphine, or Buprenorphine-Naloxone Combination in Pregnancy and in Lactation?
Both buprenorphine and methadone, classified as category C drugs by the Food and Drug Administration, have been found in studies to be safe and effective when used in pregnant women [ 17 ]. While methadone has long been the standard of care for treatment of withdrawal and dependence in pregnancy, buprenorphine has a favorable profile, including less severe neonatal abstinence syndrome (NAS) after birth [ 17 ]. Additionally, buprenorphine has potential to be more accessible with both office-based settings and treatment programs, compared to methadone maintenance programs in clinic settings only. If buprenorphine is used, the induction can proceed after confirming that the patient is in withdrawal. The Clinical Opioid Withdrawal Scale (COWS) can be used to assess withdrawal symptoms, and to track improvement after treatment with methadone or buprenorphine.
In pregnancy, the buprenorphine-only formulation is recommended over the buprenorphine-naloxone co-formulation. Concerns have been raised about the safety of naloxone for the fetus. There are some data to suggest that naloxone causes maternal and fetal hormonal changes [ 4 ]; however, the clinical implications of this finding have not been demonstrated. There is additional concern over the possibility of inducing withdrawal if the mother injects buprenorphine-naloxone intravenously. Limited studies do suggest that the use of combination buprenorphine-naloxone is safe in pregnancy [ 18 ]; however, until the safety concerns have been adequately studied, patients on Suboxone® who become pregnant are recommended to transfer to buprenorphine-only formulations [ 15 ].
Post-partum, both buprenorphine and methadone are considered to be compatible with lactation [ 17 ]. Buprenorphine is excreted in breast milk; however, given the low oral bioavailability of buprenorphine, infant exposure is 10–20 % of available buprenorphine. The amount of methadone found in breast milk appears to be low (less than 1 % of the maternal dose) [ 19 ]. While studies do not demonstrate that buprenorphine in breast milk attenuates NAS, there are some reports describing attenuation in infants breast-fed by mothers taking methadone [ 6 ].
Question: What is the Approach to Diagnosis and Management of Neonatal Abstinence Syndrome (NAS)?
NAS is a generalized disorder characterized by signs and symptoms of irritability, gastrointestinal dysfunction, respiratory distress, and vomiting. NAS typically presents with 72 h after birth, in cases of in utero methadone or buprenorphine exposure; however, studies suggest that neonates exposed to buprenorphine require less medication and a shorter duration of treatment for NAS [ 20 ]. Many hospitals have protocols to treat NAS, using scale systems for severity and a combination of non-pharmacological and pharmacological treatments, with opioid and non-opioid medication options [ 21 ].
A 16-year-old boy is brought in to the Pediatric ED after his mother returned home and found him with slurred speech and “falling all over the kitchen!” He opens his eyes, sighs loudly, and turns away during the exam. The patient has been using marijuana, and has been caught drinking several times. When the patient is more awake, he and his mother have a loud and animated discussion about him “snorting her Xanax® again.” The mother asks for help with his continued drinking and drug use.
Question: What are Some Available Resources for Assessment and Treatment of Drug and Alcohol Abuse in Adolescents?
Adolescent substance use should be identified and addressed as early as possible. Drugs exert long-lasting effects on the developing brain [ 22 ]. The CRAFFT (Car, Relax, Alone, Forget, Friends, Trouble) questionnaire for alcohol and drug use disorders in adolescents (Fig. 3 ) is both validated and frequently used [ 23 ]. A total score of 2 or higher (5 questions, each “yes” is 1 point) indicates a positive screen and the need for additional assessment. Questions cover topics such as riding in a car with a driver under the influence of drugs or alcohol, using substances to relax or fit in or while alone, forgetting things while using substances, having others concerned about use, or getting into trouble while using alcohol or drugs.

CRAFFT questionnaire for alcohol and drug use disorders in adolescents
Adolescents can benefit from a drug abuse intervention, even if they are not “addicted” to a drug. Guides on treatment for adolescent substance use disorders indicate that motivational interviewing is a useful technique for discussing substance use, even with adolescents who are not interested in change or not ready to commit to change [ 24 ]. Treatment options include follow up with a primary care clinician, outpatient psychosocial addiction medicine treatment, family-based behavioral therapies, or pharmacological treatments. Several medications are approved by the FDA to treat addiction to opioids, alcohol, and nicotine. In most cases, though, little research has been conducted to evaluate the safety and efficacy of these medications for adolescents; however, some healthcare providers prescribe “off-label”, especially in older adolescents. Buprenorphine in particular has demonstrated potential efficacy in this population based on two research studies [ 25 , 26 ]. In some states, methadone is approved for adolescents between the ages of 16 and 18 after they have failed two other treatments, and with their parents’ approval.
The best approach to treatment includes supporting the adolescent’s life needs, such as those related to medical, psychological, and social well-being. Adolescents who abuse drugs frequently suffer from other conditions including depression, anxiety disorders, ADHD, oppositional defiant disorder, and conduct problems. Many adolescents who abuse drugs have a history of physical, emotional, and/or sexual abuse or other trauma. Tobacco use often accompanies other drug use and needs to be addressed as part of substance use disorder treatment [ 27 ]. Pharmacologic treatments for tobacco use disorder include bupropion, varenicline, or nicotine replacement therapies [ 28 ].
A 17-year-old boy is brought to the ED because his father states he has been “buying Suboxone® again, and I found it in his room!” The father is demanding that he be admitted to “detoxify” and referred to an inpatient treatment facility. The father refuses to take the patient home, saying, “I can’t have him around his younger brothers.” However, the father demands to be updated with information regarding his son’s care.
Question: How are Issues of Confidentiality Addressed for Adolescents With Substance Use Disorders?
Laws on various provisions can vary across states, including the definition of a minor (typically under age 18), the ability of a minor to consent to substance abuse treatment, parental notification of treatment, and the disclosure of medical records. HIPAA only allows parents to have access to the medical records of a minor child if that access does not conflict with a state or other confidentiality law. However, US Code §290dd-2 and 42 CFR Part 2.12 protect any information about an adolescent, if the adolescent has applied for or received any treatment related to his substance use disorder or referral services from a treatment program. Written consent from the adolescent is required to communicate with parents. Exceptions to the requirement for written consent can be made if the patient does not have the capacity to consent because of an extreme substance use disorder or a medical condition, or because disclosure is necessary due to substantial threat to the life or well-being of the adolescent or someone else.
A 66-year-old female presents to the ED somnolent and with myoclonus. Her sister found her unresponsive. She had an open bottle of Lyrica® (pregabalin) spilled on the bed, with other pills on her dresser and “around the room.” The patient has chronic kidney disease, diabetes mellitus, hypertension, chronic pain, and arthritis (status post-bilateral total knee arthroplasty), all of which has been “worsening” over the past month per her sister. She is arousable to painful stimuli, but confused and mumbling. She has myoclonus. Her respiratory rate is eight breaths per minute. Her creatinine is elevated to 2.3 mg/dL from baseline 1.4 mg/dL. She was in the ED the month prior for smoke inhalation after nearly burning her house down when “she fell asleep in a chair with her cigarette going.” She is on multiple medications, including long-acting morphine sulfate, pregabalin, gabapentin, cyclobenzaprine, metformin, glyburide, and lisinopril. She was also found with an empty bottle of her son’s tramadol.
Question: What Medication Regimen Changes are Warranted? What if the Patient is Resistant? For Example, if She States That She “Will Just Go to Another Doctor and Get the Same Pills…”
Benzodiazepines (especially those with long-acting metabolites and those metabolized by the CYP450 systems), antihistamines, and typical antipsychotics are among the medications not recommended for use in the elderly [ 29 ]. Opioid dose requirements decrease with age because of decreased gastrointestinal motility, decreased overall metabolism, decreased liver functioning, changes in kidney function, and changes in opioid receptor sensitivity. Due to decreased renal function, medications that have active metabolites or themselves are primarily excreted via the kidneys should be decreased or substituted: morphine sulfate, pregabalin, gabapentin. Care should be taken with glyburide, metformin, and lisinopril in the setting of decreased renal function. Cyclobenzaprine has sedating and anticholinergic effects and thus not recommended for extended use in the elderly population. Reasons that the patient may be taking her son’s tramadol should be explored, and subsequent management addressed. Before abruptly discontinuing medications, the potential for withdrawal should be addressed, as withdrawal may also cause delirium in the elderly.
Question: How are Elderly Patients Assessed for Substance Use Disorders?
Prescription drug abuse among older adults is prevalent; however, providers may be misled by their perceptions, and miss subtle clues that indicate substance misuse among the elderly. Concerning signs for substance abuse in the elderly include increased falls, increased daytime somnolence, self-medication, minor traffic accidents, and trauma without a known mechanism (bruises, scrapes, burns). Collateral reporting from family is often helpful. To screen the elderly for alcohol or substance use disorders, the CAGE [ 30 ] questionnaire or the Michigan Alcohol Screening Test [ 31 ] for older adults can be used. Providers should preface questions about alcohol or drug use with a link to a medical condition, and minimize use of stigmatizing terms. Providers should screen for cognitive functioning using an orientation, memory, and concentration test or the Mini Mental State Examination [ 32 ] with a drawn clock task; depression can be screened for using the Geriatric Depression Scale [ 33 ]. When planning for treatment, the ideal programs will involve the least intensive treatment options and cater to geriatric needs.
The management of co-occurring opioid use disorder and pain occurs frequently in both the emergency department as well as primary care settings. The treatment of chronic and acute pain with opioid therapies should be accompanied by careful monitoring for appropriate use of prescribed therapies and for the presence of relative contraindications to use of opioids therapies, such as alcohol misuse, diversion, or untreated opioid use disorder. Treatment of acute pain in patients receiving opioid-assisted therapy requires an informed plan by working with the patient and the healthcare providers involved in the care of the patient and knowledge of the pharmacokinetics and pharmacodynamics of opioids, including buprenorphine and methadone.
Understanding of policy and regulations surrounding treatment of substance use disorder is important for clinicians in a variety of clinical settings. In the emergency department or hospital setting, providers often encounter patients in opioid withdrawal; providers may use buprenorphine or methadone to treat withdrawal in these settings under CFR Section 1306.07. Special privacy protections at both the federal (42 CFR Part 2) and state level are afforded to patients with substance use disorders. These laws extend to the treatment of impaired physicians; however, there is an obligation to report to the appropriate regulatory bodies when there is a concern of danger to public health with continued practice. Policies at the clinic or provider level guide the approach to management of patients who continue to use illicit substances during substance use disorder treatment while simultaneously providing structure, direction, and balance for patients receiving treatment for their disorder.
Assessment and management of substance use disorders in pregnant, pediatric, or elderly requires an understanding of the unique needs of each population. Patients who are pregnant should be prioritized for treatment of substance use disorder due to the negative effects of illicit substances and withdrawal on both the mother and fetus. Adolescent substance use presents unique issues for confidentiality and treatment strategies. Elderly substance use requires careful clinical assessment and an understanding of the medical and social needs of this population. By using management strategies advised in the preceding cases, the clinician can develop a framework to navigate the complex management of addiction in these special populations.
JoAn R. Laes, MD
Petro Levounis, MD, MA, FASAM
Daniel L. Sudakin, MD, MPH, FACMT
Edwin A. Salsitz, MD, FASAM
Timothy Wiegand, MD, FACMT (Moderator)

IMAGES
VIDEO
COMMENTS
This case study presents the diagnosis and treatment of a male patient with an alcohol use disorder (AUD). Although medications are helpful in AUD, nurse practitioners must be cognizant when combining them with other approaches, such as therapy. Some clinicians prefer to control AUD use before treating other issues, under the theory that alcohol can obscure and aggravate underlying physical ...
A Case of Alcohol Abuse. The patient is a 65-year-old white woman, married for 35 years to an accountant. They have 5 grown children and 12 grandchildren. She taught elementary school for 28 years and has not worked since retiring 15 years ago.
This case is first of the kind depicting clinical features as well as withdrawal of combined volatile and moderate alcohol abuse. The feature of combined intoxication of the two abused substances makes it difficult for the clinician to reach a diagnosis. Our case report thus puts forward the scenario of increasing combined alcohol and volatile ...
current issue. current issue; browse recently published; browse full issue index; learning/cme
It is well recognized that alcohol use disorders (AUD) have a damaging impact on the health of the population. According to the World Health Organization (WHO), 5.3% of all global deaths were attributable to alcohol consumption in 2016 [].The 2016 Global Burden of Disease Study reported that alcohol use led to 1.6% (95% uncertainty interval [UI] 1.4-2.0) of total DALYs globally among females ...
Abstract. Alcohol is a major contributor to global disease and a leading cause of preventable death, causing approximately 88,000 deaths annually in the United States alone. Alcohol use disorder is one of the most common psychiatric disorders, with nearly one-third of U.S. adults experiencing alcohol use disorder at some point during their lives.
This case report discusses a 60-year-old male with severe alcohol use disorder who presented with a newly diagnosed AF with RVR, DCM, and cirrhosis. Our case demonstrates the consequential health risks of chronic alcoholism and highlights the significance of timely screening and early intervention for at-risk alcohol use.
Alcohol use disorder (AUD) is a prevalent health concern with a recent epidemiologic survey of the United States indicating a lifetime AUD prevalence of 29.1% and previous 12 month prevalence of 13.9% [].AUD portends an increased risk for diagnosis of a primary anxiety disorder (AnxD) [], the definition of which, for the purposes of this case report, aligns with the most recent Canadian ...
These data present a view of the occurrence of alcohol and drug abuse in society which is generated from a 'medical model'. As useful as this approach is, it does not take into account the nature and needs of specific groups. To do this a more 'socially appropriate perspective' can be used. The following case studies illustrate some of ...
Case Study Details. Jeff is a 66-year-old Caucasian man whose wife has encouraged him to seek treatment. He has never been in therapy before, and has no history of depression or anxiety. However, his alcohol use has recently been getting in the way of his marriage, and interfering with his newly-retired life.
The ongoing Collaborative Study on the Genetics of Alcoholism (COGA), which involves 987 individuals from high-risk families, reported suggestive evidence of genes on chromosomes 1 and 7 involved in alcoholism. An early report from the study also reported weaker evidence of such a gene on chromosome 2. Another study from NIAAA's Laboratory of ...
View Course. Henry drinks beer daily and has done so for the past 15 years. He drinks 5-6 cans on weekdays and 8-12 cans on the weekends, as well as liquor. Henry also smokes half a pack per day of cigarettes. He smoked marijuana as a teen, but took no other drugs. Henry's father "drank himself to death.".
A new study in JAMA Health Forum shows increases in serious alcohol-related complications in 4 of 18 COVID-19 pandemic months studied (through September 2021), and suggests that women aged 40 to 64 years experienced increases of 33.3% to 56.0% in serious alcohol complication episodes in 10 of the 18 months.. The study is based on US national insurance claims data from March 2017 to September ...
The above case is a composite of many clinical examples observed across mental health settings each day, illustrating the challenges clinicians face when evaluating psychiatric complaints in alcoholic patients. The questions facing the clinician in this example include: ... Journal of Studies on Alcohol. 1995; 56:218-225. ...
The ordering process is fully online, and it goes as follows: • Select the topic and the deadline of your case study. • Provide us with any details, requirements, statements that should be emphasized or particular parts of the writing process you struggle with. • Leave the email address, where your completed order will be sent to.
Study with Quizlet and memorize flashcards containing terms like Meet the client:, One of the simplest tools that a nurse can use to screen for alcoholism is the CAGE questionnaire. CAGE is an acronym that represents the four questions it contains. What is the first question that the nurse should ask Nick?, Nick answers "yes" to two of the four questions on the CAGE questionnaire.
Case studies; Robert's story; Robert's story. Robert was living with an alcohol addiction and was homeless for over 25 years. He was well known in the local community and was identified as one of the top 100 A&E attendees at the Local General Hospital. ... He had significantly reduced his alcohol intake with long periods of abstinence and was ...
Alcohol use disorder (AUD) is a prevalent, world-wide problem, and in some countries it is accelerating. 'Alcoholics Anonymous' (or AA for short) has been a popular treatment for alcohol use disorder for decades, but much debate has persisted on whether AA - and related 12-step clinical treatments designed to increase AA participation are ...
The Latest. A new study adds to a mounting body of evidence showing that rising alcohol consumption among women is leading to higher rates of death and disease. The report, published Friday in the ...
Journal of the Study of Alcohol and Drugs. doi: 10.15288/jsad.23-00283. World Health Organization (January 4, 2023). No level of alcohol consumption is safe for our health.
After removing duplicates, case studies, articles that were not published in English, and studies not conducted in humans, the remaining publications were reviewed to determine whether they met inclusion criteria, namely that the study examined vulnerabilities, consequences, and possible mechanisms for alcohol-induced blackouts.
HESI- Alcoholism Case Study. Nick Davis, a 42-year-old, is accompanied to the emergency room by the police who found him standing on a bridge and threatening to jump. He planned to jump off the bridge because his girlfriend moved out on him and he lost his job as a cook several days ago. Vital signs upon admission are BP 146/94, P 92, R 20, and ...
The case for alcohol could be weakened if adolescent drinking patterns became more mature in adulthood. ... The study analyses alcohol consumption among college students from a community health perspective. We aim to understand how the college-related environment shapes students' drinking behaviour. In particular, we assess the role of living ...
Provide an antiemetic. Matt reports feeling nauseous, so administering an antiemetic is advised. What is the therapeutic action of benzodiazepines? Potentiate effects of GABA. Benzodiazepines potentiate the effects of GABA, which has a calming effect. HESI case study [ADN240] "ALCOHOLISM".
Abstract. In this article, a case-based format is used to address complex clinical issues in addiction medicine. The cases were developed from the authors' practice experience, and were presented at the American College of Medical Toxicology Addiction Academy in 2015. Section I: Drug and Alcohol Dependence and Pain explores cases of patients ...
a. The client's partner states that moving out of their home caused the client to start drinking heavily. b. The client's partner removed hidden alcohol from the home and is now moving back to keep a close eye on the client. c. The client's partner brings two new pairs of jeans because the client only had one pair.