Principle One
Put patient's interests first, principle two, communicate effectively with patients, principle three, obtain valid consent, principle four, maintain and protect patients' information, principle five, have a clear and effective complaints procedure, principle six, work with colleagues in a way that is in patients' best interests, principle seven, maintain, develop and work within your professional knowledge and skills, principle eight, raise concerns if patients are at risk, principle nine, make sure your personal behaviour maintains patients' confidence in you and the dental profession.
- The 9 Principles
- 1 Put patients' interests first
- 2 Communicate effectively with patients
- 3 Obtain valid consent
- 4 Maintain and protect patients' information
- 5 Have a clear and effective complaints procedure
- 6 Work with colleagues in a way that is in patients' best interests
- 7 Maintain, develop and work within your professional knowledge and skills
- 8 Raise concerns if patients are at risk
- 9 Make sure your personal behaviour maintains patients' confidence in you and the dental profession

Make sure your personal behaviour maintains patients’ confidence in you and the dental profession
Patients expect:.
- That all members of the dental team will maintain appropriate personal and professional behaviour
- That they can trust and have confidence in you as a dental professional
- That they can trust and have confidence in the dental profession
Standards & their guidance
- 9.1.1 You must treat all team members, other colleagues and members of the public fairly, with dignity and in line with the law.
- 9.1.2 You must not make disparaging remarks about another member of the dental team in front of patients. Any concerns you may have about a colleague should be raised through the proper channels.
- 9.1.3 You should not publish anything that could affect patients’ and the public’s confidence in you, or the dental profession, in any public media, unless this is done as part of raising a concern. Public media includes social networking sites, blogs and other social media. In particular, you must not make personal, inaccurate or derogatory comments about patients or colleagues. See our guidance on social networking for more information.
- 9.1.4 You must maintain appropriate boundaries in the relationships you have with patients. You must not take advantage of your position as a dental professional in your relationships with patients.
- 9.2.1 If you know, or suspect, that patients may be at risk because of your health, behaviour or professional performance, you must consult a suitably qualified colleague immediately and follow advice on how to put the interests of patients first.
- 9.2.2 You must not rely on your own assessment of the risk you pose to patients. You should seek occupational health advice or other appropriate advice as soon as possible.
- 9.3.1 You must inform the GDC immediately if you are subject to any criminal proceedings anywhere in the world. See our guidance on reporting criminal proceedings for more information.
- 9.3.2 You must inform the GDC immediately if you are subject to the fitness to practise procedures of another healthcare regulator, either in the United Kingdom or abroad.
- 9.3.3 You must inform the GDC immediately if a finding has been made against your registration by another healthcare regulator, either in the United Kingdom or abroad.
- 9.3.4 You must inform the GDC immediately if you are placed on a barred list held by either the Disclosure and Barring Service or Disclosure Scotland.
- 9.4.1 If you receive a letter from the GDC in connection with concerns about your fitness to practise, you must respond fully within the time specified in the letter. You should also seek advice from your indemnity provider or professional association.
- Commissioners of health;
- other healthcare regulators;
- Hospital Trusts carrying out any investigation;
- the coroner or Procurator Fiscal acting to investigate a death;
- any other regulatory body;
- the Health and Safety Executive; and
- any solicitor, barrister or advocate representing patients or colleagues.
Learning Material & case studies
Case studies for principle 9.

Frequently Asked Questions
Further guidance.
- Social networking dos and don'ts
- Standards for the Dental Team
- Scenario 1 - Drink driving conviction
37 Wimpole Street London W1G 8DQ
www.gdc-uk.org
We want to make sure all of our services are accessible to everyone. Therefore if you would like a copy of these standards in a different format (for example, in large print or audio) or in a language other than English, please contact us.

Personal Development Planning

Working in a dental practice can be exciting, invigorating and rewarding. At the same time it can be very demanding as there is always a lot going on. The dental industry is one of continual learning – things are always changing, especially in medical terms – so it is vital to keep up. A dental nurse’s role has advanced more than ever in recent years, a dental nurse carries out a wide range of tasks. These include looking after patients, patient reassurance, safety precautions, being at the dentist’s side and preparing and sterilising equipment, the list goes on . In addition, of course, all of these tasks must be performed to very high standard. This is why it is so important to take time to reflect on your role, your tasks, your progress and then evaluate how you can develop yourself professionally.

Completing and utilising a Personal Development Plan (PDP) effectively can help support you on your road to progression and what you really want to achieve. It can give you, as an individual, structure, focusing on quality and accountability, which are significant considerations in terms of future goals not only for the individual, but for a dental practice too. A PDP is a method for identifying your developmental needs and devising the best solutions to achieve this development.
A PDP is part of Clinical Governance – the government requires that all NHS clinicians have and use a PDP. A PDP involves updating, revisiting, stimulating ideas, identifying strengths and weaknesses, and prioritising and planning for your future career.
Many people find the idea of reflecting, evaluating and making plans daunting and overwhelming. A word of advice, go through the process slowly and break it down. It will hugely benefit you if you make and stick to an effective PDP.
A PDP in other words is a ‘plan.’ This ‘plan’ demonstrates commitment to your professional development. It can be useful to break down what you need to learn and what you want to learn. This will encourage you to focus on what you want to achieve through this learning and it will force you to think specifically about how you are going to get to that point. You can create your own learning objectives and your PDP will therefore stands as a evidence of your learning and objectives.
A Personal Development Plan demonstrates to the General Dental Council (GDC) that you are committed to lifelong learning in your professional field. It also provides guidance and goals, in addition, assisting with continual professional development (CPD). A PDP has been defined as ‘a process by which we identify our educational needs, set ourselves some objectives in relation to these, undertake our educational activities and produce evidence that you have learned something useful.’ (Rughani, Franklin & Dickson. Personal Development Plans for Dentists. The new approach to continuing professional development. Oxon: Radcliffe Medical Press, 2003, p. 27)
Since August 2008, it was determined by the GDC that Dental Care Professionals (DCPs) have to complete 50 hours of verifiable CPD (in recommended subject areas) and 100 hours non-verifiable in a five-year cycle. Furthermore, it is now law for dental professionals to take part in CPD. The GDC introduced the CPD scheme to ensure patients the best possible treatment. CPD was put in place to ensure patients receive high quality care.

A PDP involves identifying your learning needs, it incorporates CPD activity and aims to improve your professional status. This means you can take control of your own learning and future career. The GDC require that you keep CPD records for five-years and you may be selected for audit. The GDC have declared, ‘As a registered dental professional you have a duty to keep our skills and knowledge up to date so you can give patients the best possible treatment and care. Continuing professional development (CPD) is compulsory, but ideally it should just set out a formal framework for what you are already doing.’ (GDC) A PDP is essential for an individual’s professional portfolio as well as requested by the GDC. A PDP will also be useful for job interviews.
Some practical advice
Before you start your PDP it is a good idea to make a spider diagram including the following topics: Learning and educational needs: how you will address these? Outcomes and Evidence: scribble down ideas and many of your first thoughts which surface when thinking about your career and job role. You can refer back to this. It will be useful as a draft and template.
Whilst drawing on your spider diagram it may be useful to reflect on the following:
• What are you good at? • What could you do better? • What do you think you could change to benefit your practice? • Do any patients make you feel uncomfortable or uneasy? • Has a patient asked you something you don’t know the answer to? • Have you ever needed to look anything up? • What issues have been raised in your appraisals? • Does your practice run effectively? The best it can? • What doesn’t run well in practice? • Have there been any significant events in practice? • What are the practice development priorities? How do they affect you?
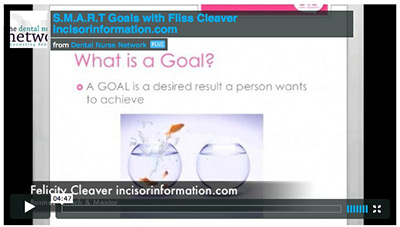
You might prefer to use a ‘Reflective Model’ which helps you to reflect and focus on something specific using the certain subtitles: Description: what happened? Feelings: what did you think or feel? Evaluation: was it good or bad? Analysis: what sense have you made of today? Conclusions: what else could have been done? Action plan: what will you do now? Gibbs (1988) stated that a Reflective Model will ‘help you reflect and focus on your thoughts today'.
The next stage is to begin your PDP. The key is to construct a simple, clear PDP and this can be achieved through a step by step approach.
SWOT analysis - open a word document, google document or pages document ( or DOWNLOAD one here ) and title it ‘SWOT analysis’. SWOT stands for STRENGHS (for example, team leader, update with CPD, good communication skills, good with elderly patients. This is an opportunity to sell yourself), WEAKNESSES (difficultly finding time for CPD or completing CPD, not recording CPD, lack of knowledge in specific areas. Address your weaknesses to help you overcome them), OPPORTUNITIES ( extended duties , supportive boss and colleagues, taking charge of PDP) and THREATS (new job, limited time, overwhelmed with learning new skills, poor communication with team). This gives you a chance to sit down and analyse your current situation. This can help you to work out your long term goals. You may want to do this with a colleague which may help.
The next part is to open a word document ( or DOWNLOAD one here ) and title it SMARTER GOAL 1, you may have more than one so the following pages you would label SMARTER GOAL 2, SMARTER GOAL 3, etc. This is where you can consider your goals, evaluate them, really think about them and make them smarter. You can identify your goals through appraisal, self-awareness, audit and reflection, etc. An occasion may occur when a patient asks you a question and you do not know the answer to it e.g ’ What are implants made of?' This realisation that you are not sure what to respond might highlight that you need to develop your knowledge on implants. Another example of goal may be to complete a certain number of CPD courses. In you PDP you should specifically state which CPD courses you want to undertake. You do not have to write 50 at once, you can build your PDP gradually.
Once you have determined a goal, you then make it smarter by addressing the following questions:
It is important to break your goals down. How will you achieve your goal? What will mark your success? What resources will you need? Set a date to complete the goal Too. You make these decisions and be as flexible as you want working towards what you want to achieve.
The next section of your PDP needs to be a record of your CPD ( DOWNLOAD Record sheet here ) . This includes both verifiable and non-verifiable CPD. This is just a case of compiling certificates, recording dates and sources.
Now you need to decide on how you are going to present you PDP and formulate your PDP portfolio. This can also include: your CV, references, appraisals.
Some practices have undergone annual appraisals and PDPs are involved in the final part of these appraisals. PDPs set out some of your planned, future learning. In this case, your appraiser will likely sign your PDP as satisfactory. Changes or suggestions may be given. The following year's appraisal will involve a review of the previous year's PDP.
The important thing to remember is that you must update your PDP constantly. You can change, alter and modify your goals and then you can add new needs as the year progresses. It is all about self-awareness and figuring out where your strengths and weaknesses lie. It is personal, so it is yours to do and decide what you want to do with. Its main aim is to help with your own development and this further benefits the practice and patients.
Remember Me
- Forgot Login?

Copyright © 2024 Dental Nurse Network. All Rights Reserved.
- News & blogs
- Search the register
Promoting professionalism
Developing our principles of professionalism .
We are currently working with dental professionals and patients to come to a shared understanding of what professionalism means in dentistry today. This work is being done to underpin the development of new principles of professionalism for UK dentistry.
Research has also been undertaken to support the work, Professionalism: a mixed-methods research study , was commissioned by the GDC to provide a comprehensive study of professionalism in healthcare and dentistry.
We have also worked with Community Research to conduct facilitated online sessions with dental professionals and patients to better understand the reasons why views on professionalism in some areas diverge. This work has included sharing stories of professionalism in dentistry and asking you to share with us your examples of professionalism - take a look at the details and get involved.
You can find out more about this work on our research pages and you can watch our recorded online session with the researchers from ADEE where we explored the findings in more detail.
The results were also the subject of a panel discussion at our Moving Upstream Conference 2020 . The expert panel, led by Professor Jonathan Cowpe, ADEE, discussed key points from the research including cultural and generational differences, and the challenges posed by social media.
Video: We asked delegates at our conference to also share their thoughts on what professionalism means to them - have a listen to what they told us.
The results of this work are now being used to inform the development of the principles of professionalism, and our review of the Standards for the dental team and its supporting guidance.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 03 November 2017
Service quality in dentistry: the role of the dental nurse
- M. T. Mindak
BDJ Team volume 4 , Article number: 17177 ( 2017 ) Cite this article
4809 Accesses
1 Citations
3 Altmetric
Metrics details
- Health services
- Quality of life
This From the archive article by M. T. Mindak was originally published in the BDJ on 23 November 1996 ( 181 : 363-368). Were dental nurses well motivated and satisfied with their roles 21 years ago? Did dentists’ and dental nurses’ perceptions of the dental nurse's role differ? Was there good communication within dental teams? Read on and see how 1995/6 compares to your experience in 2017.
Patients judge the dental service they receive by the interaction with the service providers - the dentist and his or her staff - as they are unable to judge the technical quality of the service. To perform well as a service provider, employees such as dental nurses have to be well motivated and satisfied with their position. A study of the role of the dental nurse in contributing to service quality in dentistry was carried out through interviews with dentists and nurses at 20 dental practices in the South Thames region in 1995. The results revealed that while dental staff believed that the role of the dental nurse was important in terms of the patient's view of the practice, perceptions of the nurse's role differed. The majority of dentists felt that the nurse's role should be to anticipate their needs, while the nurses’ opinions were evenly divided between putting the needs of the patient first or those of the dentist. Nurses also felt that their role was stressful and reported a lack of praise and recognition of their efforts by dentists. Few practices had written contracts or performance appraisals. The results indicated a lack of effective communication in many dental practices, producing role strain for the nurse and reducing job satisfaction. Increasing job satisfaction reduces staff turnover, resulting in more consistent service quality and reducing associated costs. In order to achieve this, several recommendations are made with the aim of improving communication between staff in dental practices.
The actions of health care representatives play a critical role in the public perception of any health care service. The provision of dental treatment provides a good example of this as a patient cannot judge the technical aspects of dentistry and so will judge the quality of the service provided by the quality of the interaction with the service providers - the dentist and his or her staff.
The dental nurse is an essential member of the dental team. The dentist and dental nurse need to have a clear understanding of their working relationship and the factors that affect it, in order to be effective in the process of service delivery. The importance of an effective interaction between dentist and dental nurse is further highlighted by the fact that there is a possibility, albeit rare, of that interaction working to save the life of a patient who has been taken ill during treatment.
The real benefit, however, in developing an improved working relationship between dentist and nurse, is in creating a more harmonious working environment. This, in turn, produces a more pleasant, friendly atmosphere for the patient, who perceives an improvement in the quality of service. As a result, the patient is more likely to stay with the practice and recommend it to friends and family.
There is a high turnover of dental staff. 1 This causes problems in delivering consistent service quality due to the disruption of routine for the dentist and loss of relationship continuity for patients when a staff member leaves. There is also the expense and time required to recruit and train a new member of staff. It is useful, therefore, to know what factors affect this turnover in order to try to reduce it. The aim of this study was to examine aspects of the role of the nurse in order to provide recommendations for reducing staff turnover and improving service quality in dental practices.
Materials and methods
A study was conducted by means of a series of qualitative interviews with dentists and nurses at 22 practices selected from the South Thames Health Authority region. Qualitative research was deemed to be the most appropriate method as the study was to be exploratory in nature, to ascertain general themes, which required a more flexible approach than would be possible by a standardised structured questionnaire.

It was decided to select 11 NHS practices and 11 private practices for the purposes of the study. The practices were chosen from three FHSAs from within the South Thames Health Authority region: Lambeth, Southwark and Lewisham FHSA, Bromley FHSA and Bexley and Greenwich FHSA. One hundred dental practices were initially selected, 50 practices from the NHS and 50 private practices.
Each practice was contacted by letter detailing the nature of the research. They were each then telephoned and asked if they wished to participate. Many practices did not wish to participate or else stated that the dates during which the study was being held (June to August 1995) were not convenient. The final sample of 22 practices (11 NHS and 11 private) was therefore, in part, self-selected.
The only selection criteria applied by the author were those of the practice being in one of the three FHSA areas, that the practice agreed to participate and that the interviewees consisted of one dentist and his or her own dental nurse and not a nurse who routinely worked with a colleague.
Pilot interviews were carried out at two additional dental practices in the London area to clarify the nature of the questions to be asked in the main study interviews. The main study interviews were conducted at the dental practices during July and August 1995. The vast majority took place during the practice lunch break and consisted of individual semi-structured interviews of approximately 20 to 30 minutes.
The interviewer first asked general closed questions regarding qualifications, hours worked and so on and then asked open-ended questions regarding the role of the dental nurse. Two sets of questions were used for the interview frameworks - one for the dentists and one for the dental nurses, but both followed the pattern of closed followed by open-ended questions. The interviews were conducted face-to-face with the author who travelled to each practice.
The dentist and his or her nurse were interviewed separately and encouraged to speak freely, being assured that the other members of the practice would not be informed of any comments made. All interviews were tape-recorded with individuals being informed of this prior to the interview and consent obtained. The taped interviews were then transcribed for analysis. Recurring themes and topics were then grouped together to produce the results.

Quantitative results
One dentist and his or her dental nurse were interviewed at each practice, a total of 40 individual interviews out of a possible 44. The results from two practices, ie four interviews, were deemed unsuitable for inclusion in the study. The reasons for this were that for one practice there was a mechanical fault with the tape recorder resulting in only half the interview being recorded, and in the other practice, the dentist concerned declined to continue with the interview and did not wish to answer the questions. This left a final sample of 20 practices - 10 NHS and 10 private.
Characteristics of the sample: dentists
AGE AND GENDER
The age range of dentists was from 27 to 58 years, with the majority between 30 and 40 years old. Four of the 20 dentists were female.
DATE OF DENTAL QUALIFICATION
The date of the dental qualification was naturally correlated with age and ranged from 1963 to 1991. Ten of the UK's 16 dental schools were represented, from all parts of the country. Two respondents had trained abroad - Nigeria and India.
TIME AT CURRENT PRACTICE
Time at current practice ranged from 11 months to 32 years, with 12 respondents being at the practice for more than two years. The majority of respondents were the practice owner and would therefore be expected to remain at the practice.
NUMBER OF STAFF AT THE PRACTICE
The number of staff was calculated to include part time staff as well as full time. The range was from two, where the nurse was also the full time receptionist (three practices), to one practice of 24 staff. The majority had four to six staff.
NUMBER OF PATIENTS SEEN PER DENTIST PER DAY
For NHS practices, this ranged from 18 patients (in two newly established practices) to around 40. The vast majority were in the range 25-30. In private practices the figures were rather lower; the range was 10-25, with most being around 15.
Characteristics of the sample: nurses
The range was from 16 to 57 years old. Two were over 50, three in their 40s and the remainder 39 or under. Two were teenagers. The average age of nurses in private practice was around nine years older (35 years) than that for NHS practices (26 years).
LENGTH OF TIME WORKED AS A DENTAL NURSE
This varied from eight months to, in one case, 39 years (the nurse having left school at 14). The sample was fairly evenly split between those who had worked as a nurse for 10 years or less and those who had worked as a nurse for more than 10 years.
For NHS practices, this ranged from two days to six years. Seven out of 10 nurses had been at the practice for two years or less. In private practice, the range was from 10 months to 15 years. Five nurses had been at the practice for two years or less and the other five for two years or more.
DENTAL NURSING CERTIFICATE
Six out of 20 nurses had a qualification, five in private practice and one in the NHS. Two further nurses in the NHS had taken the exam and failed, but did not intend to retake it. Two nurses in private practices were currently on the training course.
Qualitative results
All those involved in the study agreed that the role of the dental nurse was very important in terms of how the patient viewed the practice. The nurse was seen to be the patients’ confidante and provided reassurance:
‘It's always you they will ask’ (nurse aged 25, private practice)
‘If they’ve got a problem, I talk to them because at times they don’t want to talk to the dentist, so they talk to me and I can pass the message on to the dentist’ (nurse aged 30, NHS practice)
The study also produced other findings that can be grouped into three areas:
A difference in perceptions of the role of the dental nurse between nurses and dentists.
The lack of appreciation and acknowledgement of nurses’ efforts by dentists, as felt by nurses.
The lack of formalisation of the nurse's role in terms of written contracts or performance appraisal and the lack of regular staff meetings.
The difference in perceptions of the nurse's role
THE DENTISTS’ VIEW
The vast majority of the dentists (18 of 20) viewed the role of the dental nurse principally to be anticipating the dentist's needs: having instruments ready, the surgery clean and so on. They wanted the nurse to be able to think ahead for them:
‘You get to a stage where she's got it ready before you say anything and then when you get one stage further, you can ask for the wrong things and get the right things’ (male dentist aged 47, private practice)
Dentists felt that reliability was very important in fulfilling the nurse's role:
‘I’ve had situations where after being her for three or four months a nurse has taken her pay cheque on the Friday and then not come in on the Monday, without telling me that they’re not coming back’ (dentist aged 31, NHS practice)

Many of the dentists, 12 of 20, expressed a preference for older nurses rather than teenagers, and for those who had gained previous experience, saying that they found younger staff to be far less reliable in terms of timekeeping and attendance:
‘If I had a choice of someone to employ, I would happily go for someone in their late 20s onwards with children. We’ve found that with younger women, their attendance can be distinctly “iffy” and the merest sniffle, they’re off’ (dentist aged 39, private practice)
Dentists also felt that an empathetic and cheerful personality was important, not just for patients’ sake, but also for their own morale. All dentists said that an efficient and friendly nurse acted to greatly reduce the day to day stress of practice:
‘If you’ve got a very close relationship with that person (the dental nurse) for eight hours a day and if they’re not happy it can drain on you and affect the relationship with the patient’ (female dentist aged 30, NHS practice)
‘My stress level goes up enormously if she isn’t working with me ... she makes life a lot easier without a doubt’ (male dentist aged 35, private practice)
THE NURSES’ VIEW OF THEIR ROLE
In contrast to the dentists, dental nurses were divided as to their principal role: 10 nurses clearly stated that the patient was their first priority, while the other 10 said that the dentist's needs come first.
‘My role is actually thinking for the dentist’ (nurse aged 30, NHS practice)
‘I think for him, I’m one step ahead’ (nurse aged 31 private practice)
‘To help the patient feel as relaxed as possible’ (nurse aged 18, NHS practice)
‘Primarily, to make sure the patients feel comfortable and welcome’ (nurse aged 43, private practice)
Nurses also said that they saw a major part of their role to be acting as an intermediary between dentists and patients and that this could be very stressful. They said that patients saw them as representing the practice and would want explanations as to why an appointment was late, for example, while the dentists would be telling them to go out and keep the patient calm:
‘They (patients) quite often treat the nurse very differently to the dentist ... the patients have a real moan and then go into the surgery and be as nice as pie and you think “oooh”!’ (nurse aged 22, private practice)
The lack of appreciation
Many nurses, 11 of 20, reported problems in communicating with dentists. Areas of concern were principally the lack of definition of the nurses’ role by dentists and lack of appreciation by dentists for the nurses’ efforts. Nurses reported being given little instruction when joining a practice and were often expected to know what to do in the surgery:
‘He just expected everything there without telling you or asking you. Me sitting there not doing it because I don’t know what he needs and him probably thinking, “Oh she's just sitting there”, but it's not, it's because he's not actually explained what he needs and therefore I can’t mix it when I don’t know’ (nurse aged 24, NHS practice, describing life as a trainee at 17)
Most nurses, 14 of 20, reported being spoken to in a derogatory manner, which they felt indicated a lack of respect. This got worse when the dentist was under stress. Many understood that dentistry was stressful and wanted to help the dentist, but still wished to be spoken to courteously.
‘He was very rude, he used to swear at you and abuse you if you did things wrong’ (nurse aged 31, private practice)
‘I was a trainee and he was just very impatient and used to be sarcastic in front of patients and I didn’t like that because it made me look stupid’ (nurse aged 22, private practice)
Some dentists apparently coped with stress in unusual ways:
‘There was one guy, if he didn’t like things or things didn’t go his way or he couldn’t get a matrix band on, he’d throw tweezers at your ankles ... It wasn’t anything to do with the nurses, it was just his own pure frustration, but he was quite well known for it’ (nurse aged 43, private practice)
Dental nurses wanted their efforts recognised and acknowledged by the dentist and felt that this rarely occurred. When this did happen, it was much appreciated and was felt to contribute to a more pleasant atmosphere in the practice, which, nurses said, was noticed by the patients:
‘If the dentist appreciates what the nurse is doing, then the nurse gives her best to the dental surgeon. You’ve got to work as a team ... if you work as a team and you can be friends then the patient gets so much more out of that because the atmosphere is so different. I think a patient can feel an atmosphere when they go into a surgery. If they feel a good atmosphere, then they get good vibrations and they relax more’ (nurse aged 44, NHS practice)
A nurse with 24 years’ experience said of her employer, a dentist aged 39, in private practice:
‘I think really a dentist should include their nurse in the work or they can make them feel just like the washer-upper and I feel very included here ... he's terrific, absolutely terrific. This dentist will at the end of the day say “thank you”. That's not usual, normally they’re tools down and gone and leave you to clear up’.
Some dentists said they found managing staff difficult, especially in the first years of practice. Three of the four female dentists felt that the task was harder as a woman than for a man. Their nurses felt that female dentists were more sensitive in dealing with staff and would help the nurse more than a male dentist would.
RESPONSIBILITY AND EXPANSION OF THE ROLE OF THE DENTAL NURSE
At present, the role of the dental nurse is limited in terms of direct clinical interaction with the patient, in contrast to other countries such as the USA and New Zealand. Dentists and nurses were asked their views on the possible expansion of the nurse's role, as considered in the Nuffield Report. 2
Most dentists, 11 of 17 (three did not respond), were not in favour of the dental nurse taking on any clinical duties, apart from taking radiographs. Many did not see any real benefit of the nurse undertaking these tasks and expressed concern about the level of training for nurses that would be necessary to ensure patient safety. The majority of nurses however, expressed a desire to expand their role and mentioned the lack of a career path. Several nurses mentioned that being given responsibility made their job more enjoyable:
‘Having the responsibility brings our your best qualities because everybody's got a forte at something’ (nurse aged 31, private practice)
Six of the 20 had a dental nursing qualification, and five of these were in private practice. Many expressed a desire to expand their role with the patient and said they felt frustrated at not being able to do more in the surgery. Five of the 20 interviewed had made a definite decision to obtain further qualifications towards that end and had registered to train as a hygienist (1), dental therapist (2) oral health educator (1) and general medical nurse (1).
Four of the 20 nurses brought up the subject of their salary. They felt it was far too low for the job and felt unappreciated as a result. One nurse said:
‘You are risking yourself as much as dentists, with AIDS and all that, and their pay is good ... that makes me sick ... they sort themselves out and forget the nurses’ (nurse aged 24, NHS practice)
Some dentists seemed to be unaware of just how sensitive an issue this was. Nurses in private practice, not surprisingly, reported being paid more than in NHS practices and had left NHS practices as a result. Some private dentists said that they felt higher salaries to be a worthwhile investment to attract good staff.
The lack of a formalised role
WRITTEN CONTRACTS AND STAFF APPRAISAL
Only five practices in the survey had a written contract for staff and only one carried out a formal staff appraisal. Nurses said that they would welcome a regular appraisal of their performance, as some had just occasional comments made to them. Several complained of being readily criticised if they made a mistake, yet never praised when they performed well.
PRACTICE MEETINGS
Similarly, only five practices held practice meetings on a regular basis, while a few more held them on an occasional basis. The practices that did currently hold meetings found them to be valuable aids to communication and staff participation. Some nurses however, felt that little was achieved by meetings: they had attended them in the past and said that little attention was paid to their opinions or suggestions. In a lot of practices, both dentists and nurses did not see any need for meetings at all.
The results of the study should be interpreted with caution as this was a small and self-selecting sample. Nonetheless, several of the findings are relevant to dental practice management. It was evident from the study that there are problems in communication between the dentist and the dental nurse in many dental practices. These problems were manifested in the different perceptions as to what the role for the nurse actually entailed, in the way the required role was explained, the lack of written job descriptions, coupled with little positive feedback or appraisal, and a derogatory manner used in addressing the nurse. In addition, very few practices provided an opportunity for the nurse to raise problems, make suggestions or participate in decision making, by means of mechanisms such as a regular practice meeting. The lack of management skills training for dentists may well be a contributory factor here. These findings confirm previous research that has been carried out into job related for the dental nurse.
The consequences of poor communication
A lack of communication between and employer and employee results in several negative outcomes which researchers have found affect job satisfaction. 6 , 7 Two principal ones are role ambiguity and role conflict. Role ambiguity occurs where a role has not been clearly defined and responsibilities are ambiguous, as was clearly felt by the nurses in the study. Role conflict occurs when the employee is expected to carry out contradictory tasks, such as trying to please both patient and dentist. The stress nurses mentioned at being the ‘intermediary’ is well recognised in the literature, this position being described as the ‘boundary-spanning’ role ie the boundary between the organisation and the customer. Such roles have been associated with high degrees of stress for employees. 7
These factors result in role strain, which has been shown to decrease job satisfaction. Dentists stated that the main problems they had with dental nurses were poor timekeeping and absenteeism. Both these behaviours have been shown to be symptomatic of reduced job satisfaction.
Staff turnover
A reduction in job satisfaction is directly related to the employee's tendency to leave the organisation. 9 It is known that dental nurses have a high employment turnover, with the resultant increased costs and inconsistency of service quality for the dental practice as previously mentioned. Turnover of staff adversely affects the consumer's perception of the service, with the result that they will go elsewhere. So in order to provide and maintain service quality in the eyes of the consumer (the patient) staff turnover is to be avoided.
The results of this study show that a lack of communication between dentist and nurse could well be contributing to the high turnover rate. In order to reduce turnover of dental nurses and increase job satisfaction, positive steps should be taken to improve communication.
Recommendations
The process of good communication involves the processes of active listening - concentrating on exactly what a person is saying, not jumping to conclusions or assumptions; feedback on how the role was performed helps to clarify discussion and self-disclosure - an atmosphere of trust and openness should be established so that staff feel able to make comments and suggestions. 10
Many of the suggestions made below are not new. 11 - 16 However, this survey shows that they are still relevant and that improving communication is still necessary for many dental practices. Several of these improvements can be made immediately and the majority can be implemented at little or no financial cost.
Immediate changes in the dental practice
To make changes towards improving communication in the dental practice work, it is best to start with small and simple things that are easy to implement and are likely to succeed. Early success will encourage staff and reinforce the new approach.
ACHIEVING BETTER COMMUNICATION
Praise and recognition are powerful ‘motivators’. These are therefore ideal areas with which to start ( Tables 1 , 2 , 3 , 4 , and 5 ).
THE PRACTICE MEETING
Efforts to improve communication in the practice should involve all the staff, not just the nurse, and the suggestions below are relevant for all staff. In addition, practice meetings are a valuable tool.
Changes in the medium term
The initial approaches will start to improve communication in the practice and can be reinforced over the following few months by further measures - further clarify roles by written descriptions, build in praise and recognition and build up an atmosphere of trust by training and delegation.
Long term changes - recommendations for the profession
As we can see, these are relatively simply changes that can be carried out in a short period of time. However, for the profession as a whole, there remains the issue of training for both dentists and nurses which needs to take into account communication and interpersonal skills, which, as the study showed, are so necessary. In addition, the recommendations in the Nuffield Report 2 regarding the training of dental nurses, ie the introduction of a national training standard and statutory minimum qualification, should be implemented as soon as possible. A better career structure for dental nurses will act to retain and motivate staff, raise standards of care, improve service quality and thereby the patients’ view of the practice.
Bader J . Auxiliary turnover in 13 dental offices. J Am Dent Assoc 1982; 104 307–312.
Article Google Scholar
Nuffield Report. Education and training of personnel auxiliary to dentistry . Norwich, UK: The Nuffield Foundation 1993.
Locker D, Burman D, Otchere D . Work-related stress and its predictors among Canadian dental assistants. Community Dent Oral Epidemiol 1989; 17 263–266.
Blinkhorn A . Stress and the dental team: a qualitative investigation of the causes of stress in general dental practice. Dent Update 1992; 19 385–387.
PubMed Google Scholar
Craven R C, Blinkhorn A S, Roberts C . A survey of job stress and job satisfaction among DSAs in the north-west of England. Br Dent J 1995; 178 101–104.
Jackson S E, Schuler R S . A meta-analysis and conceptual critique of research on role ambiguity and role conflict in work settings. Organizational Behaviour and Human Decision Processes 1985; 36 16–49.
Netemeyer R, Burton S, Johnston M . A nested comparison of four models of the consequences of role perception variables. Organizational Behaviour and Human Decision Processes 1995; 61 77–93.
Shamir B . Between service and servility. Human Relations 1984; 33 : 741–756.
Bedian A, Armenakis A . A path analytic study of the consequences of role conflict and ambiguity. Academy of Management J 1981; 24 417–424.
Google Scholar
Hellriegal D, Slocum J Jr, Woodman R W . Organizational behaviour . 6th ed. St Paul, MN: West, 1992.
Cummings T G, Worley C G . Organizational development and change . St Paul, MN: West, 1993.
Schwartz S . Motivating the dental staff. Dent Clin North Am 1988; 32 35–45.
McKenzie S . Empowering your dental team. J Michigan Dent Assoc 1992; 74 36–38.
Manji I . Fair pay and then some: how to retain your staff. J Can Dent Assoc 1992; 58 : 895–896.
Butters J, Willis D . Satisfaction level of dental office personnel. Gen Dent 1993; May-June: 236–240.
Nacht E S . 13 ways to keep the staff motivated in your pediatric dental office. J Clin Pediatr Dent 1994; 18 163–164.
Download references
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Mindak, M. Service quality in dentistry: the role of the dental nurse . BDJ Team 4 , 17177 (2017). https://doi.org/10.1038/bdjteam.2017.177
Download citation
Published : 03 November 2017
DOI : https://doi.org/10.1038/bdjteam.2017.177
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Creating a new NHS England: Health Education England, NHS Digital and NHS England have merged. Learn more.

- Privacy and Cookies Policy

Reflection and Personal Development Plans
Home / About Us / Education and Training / Development Plans / Reflection and Personal Development Plans
The use of reflection has become a routine part of many professions such as teaching and nursing. In dentistry we have been slower to adopt it as way of highlighting development needs.
You might think, how can reflection help me, either to learn things or highlight an area that I need to develop further. How can reflection help to develop my own personal development plan?
There is evidence that engaging in Reflective Practice is associated with the improvement of the quality of care, stimulating personal and professional growth and closing the gap between theory and practice. There is a lot of literature on Reflective Practice. Davies (2012) has summarised a lot this and identifies that there are both benefits as well as limitations to reflective practice:
Benefits to Reflective Practice
- Increased learning from an experience or situation
- Promotion of deep learning
- Identification of personal and professional strengths and areas for improvement
- Identification of educational needs
- Acquisition of new knowledge and skills
- Further understanding of own beliefs, attitudes and values
- Encouragement of self-motivation and self-directed learning
- Could act as a source of feedback
- Possible improvements of personal and clinical confidence
Limitations of Reflective Practice
- Not all practitioners may understand the reflective process
- May feel uncomfortable challenging and evaluating own practice
- Could be time consuming
- May have confusion as to which situations/experiences to reflect upon
- May not be adequate to resolve clinical problems [this would point to a further learning need.]
Reflection is something we do every day we just don’t notice that were doing it much of the time. A lot has been written about reflection, but it can be best illustrated by an example:
You start a new job and have a new journey to work. Before your first day you think about the journey to work, which route to work will be best and how long will it take. This indicates what time you need to set off to arrive, at the time you want. As you have not done the journey before you may drive it before hand or allow extra time so you can allow for delays. This then becomes your daily commute. However on this drive there is a roundabout that always holds you up. One day you try a slightly different route and it works, you avoid the holdup and save five minutes on your journey Time. You have tried a new route and it worked, you have learnt something from trying something new. Another day there is a bad accident and your normal route is blocked so you have to take another one to try to get round it. You are forced to react to the situation.
These are examples of reflection and how it could help in professional practice. You try something out to overcome a problem you have and see if your idea improves the situation or not. Most of the time, we do this in our minds. In more ‘formal’ reflection, we take that a stage further and write in down. This separation helps us to consider what we are doing and consider our thought processes. It also means we can demonstrate this to others. [It will be part of revalidation with the GDC, when it comes.]
If we look at a Dental example: you have a number of new patients that have advanced periodontal disease, you would normally do quadrant scaling for these patients {which you were taught at Dental school}, some seem to be helped and others don’t seem to respond. In this situation you could carry on doing the same thing or start to reflect ‘I’m not sure this is the best way to treat them’. This might prompt you to go on a Periodontal update course and see if what you were taught at Dental school is still the current treatment being taught. It highlights a possible learning need.
In practice if we take the time to reflect on things that happens it can help us to identify areas we need to improve in our own practice. If you like Endodontics and get good results then it should not be a priority for your personal development plan. The temptation is to go on another endodontic course as you enjoy it. It may to the case that a Periodontal course would be more useful. This thought process can be developed by reflection. You are able to consider the areas of dentistry that you are comfortable with and get good results against those areas that you feel you could improve or feel you don’t have all the understanding to do well.
Lots of different ways of reflecting have been described, none of which is necessarily better or the correct way to do it. One way that is widely used is Gibbs reflection cycle [1988]
This page was last updated June 18th 2015 (9 years ago)
Pocket Dentistry
Fastest clinical dentistry insight engine.
- Dental Hygiene
- Dental Materials
- Dental Nursing and Assisting
- Dental Technology
- Endodontics
- Esthetic Dentristry
- General Dentistry
- Implantology
- Operative Dentistry
- Oral and Maxillofacial Pathology
- Oral and Maxillofacial Radiology
- Oral and Maxillofacial Surgery
- Orthodontics
- Pedodontics
- Periodontics
- Prosthodontics
- Gold Member
- Terms and Condition
4 Health and Safety in the Dental Workplace
Health and safety in the dental workplace.
- health and safety requirements relevant to both employers and employees
- the legislative and regulatory requirements of the dental workplace and its staff
- risk assessment in the dental workplace
- occupational hazards and their avoidance in the dental workplace
- the actions to take in various first aid scenarios
- general safety and security issues in the dental workplace
Health and Safety at Work Act (1974)
All dental workplaces, their staff and patients are covered by the provisions of the Health and Safety at Work Act (1974), as is any other workplace. In addition, other legislation is relevant to the dental workplace due to the potentially harmful nature of the equipment and chemicals used, as well as the occupational hazards associated with delivering dental treatment or working in the dental environment.
The Health and Safety legislation seeks to protect staff and patients while on the premises by making the staff aware of any potential hazards at work, and encouraging them to find the best ways of making their premises safer for all concerned. In legal terms, the employer has a statutory duty to ensure that, as far as is reasonably practicable, the health, safety and welfare at work of all employees and all visitors (including patients) are considered at all times. To do this, all the potential hazards first need to be identified, and then the likelihood of them actually causing harm to anyone must be determined. The chance that a particular workplace hazard could cause harm to someone is known as its risk, and the correct procedure to be followed by the employer (and their staff) to identify those hazards that could cause harm is called a risk assessment.
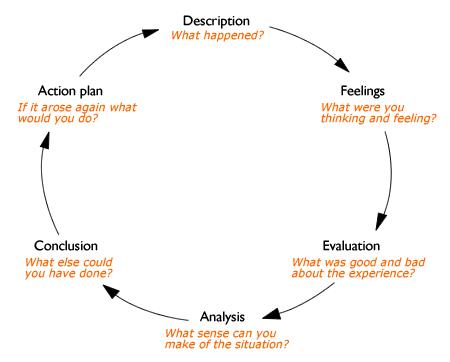
Compliance with the Health and Safety at Work Act is overseen and regulated by the Health and Safety Executive (HSE). This is a government body that provides guidance to employers on the correct enforcement of the Act, and investigates when any serious incidents occur in any workplace where someone suffers serious harm or is killed. Every dental workplace is required to be registered with the HSE.
Compliance with the additional legislation specific to the dental workplace is also required by the General Dental Council, under its Standards for Dental Professionals documentation.
To comply with the basic requirements of the Health and Safety at Work Act, every employer in the dental workplace must abide by the following requirements.
- Provide a working environment for employees that is safe, without risks to health, and adequate with regard to facilities and arrangements for their welfare at work.
- Maintain the place of work, including the means of access and exit, in a safe condition.
- Provide and maintain safe equipment, appliances and systems of work.
- Ensure all staff are trained in the safe handling and storage of any dangerous or potentially harmful items or substances.
- Provide such instruction, training and supervision as is necessary to ensure health and safety.
- Review the Health and Safety performance of all staff annually, be aware of and investigate any failures or concerns highlighted, when they occur.
- Display the official Health and Safety poster for all staff to refer to ( Figure 4.1 ).
To comply with these statutory obligations, dentists must keep their staff informed of all the safety measures adopted. Practices with five or more employees must produce a comprehensive Health and Safety policy and provide all staff with a copy. The policy will classify the practice Health and Safety procedures and name the persons responsible. It should also list the telephone numbers of all dental, administration and equipment maintenance contractors, the local HSE contact, and emergency services.
Role of the dental nurse
All dental nurses have a legal obligation to co-operate with their employers in carrying out the practice requirements in respect of these safety measures. They are designed to protect not only the staff and patients, but anybody else using or visiting the premises. In a large dental workplace, a dental nurse may be appointed as safety representative under the Act for the purpose of improving liaison within the practice about Health and Safety matters.
However, many dental nurses begin their careers as young trainees in the dental environment, so the following two sets of regulations are specifically important in protecting their welfare.
- Health and Safety (Young Persons) Regulations 1997
- Management of Health and Safety at Work Regulations 1999
Figure 4.1 Health and Safety poster.© Crown Copyright 2009. Published by the Health and Safety Executive (HSE).
These sets of regulations dictate that a risk assessment of the dental environment has to be carried out, with particular regard to the protection of younger staff members, by taking into account the following points.
- The risks to young people before they start work.
- The psychological or physical immaturity and inexperience of young people.
- Their lack of awareness of existing or potential risks to their health and safety.
- The fitting and layout of the practice and surgery, with regard to the safety of young people.
- The nature, degree and duration of any exposure to biological, chemical or physical agents within the work environment.
- The form, range, use and handling of dental equipment.
- The way in which processes and activities are organized.
- Any Health and Safety training given, or intended to be given.
A summary of the risk assessment details, covering the various types of work activity that a student dental nurse is likely to undertake, to ensure their safety in the dental workplace is shown in Table 4.1 . The risk assessment should take into account the likely activities that the student dental nurse will undertake while on the premises, and these are listed in the first column. To train effectively, they must always be involved in chairside assisting activities, so the potential areas of risk to the student during chairside working should then be considered – these are listed in the second column. The final column then needs to identify the methods required to ensure that the student is not exposed to these risks in the first place, and for each area it can be seen that suitable induction training is always required. This involves explaining why a certain activity is a risk to them, the provision of suitable training in the activity so that the risk is minimised as far as possible, and initial supervision when the activity is carried out for the first few times. Before dental nurses became registrants with the General Dental Council (GDC), and therefore before training and qualification were necessary, this supervision used to be referred to as ‘shadowing’ of a junior colleague by a senior colleague, until they were deemed able to carry out the activity unsupervised. The risk assessment procedure described here merely formalises the technique of shadowing.
Table 4.1 Risk assessment for student dental nurse
Full compliance with Health and Safety legislation for all dental workplaces, whether a practice, a clinic or a hospital department, involves all of the following.
- Fire Precaution (Workplace) Regulations (1999)
- Health and Safety (First Aid) Regulations (1981)
- Control of Substances Hazardous to Health (COSSH) (1994)
- Reporting of Injuries, Diseases and Dangerous Occurrences (RIDDOR) (1995)
- Environmental Protection Act (1990)
- Special Waste and Hazardous Waste Regulations (2005)
- Ionising Radiation Regulations (IRR) 1999
- Ionising Radiation (Medical Exposure) Regulations (IR(ME)R) 2000
- Occupational hazards
- General safety measures
- General security measures
Since 2010, additional regulations have been introduced in the specific areas of decontamination and infection control in the dental workplace, although their implementation currently varies throughout the UK. Referred to collectively as HTM 01-05, their detail is discussed in Chapter 8. Finally, since 2011 a system of mandatory registration with the Care Quality Commission (CQC) has been introduced for all providers of health and social care, including all dental workplaces. The CQC is a regulatory body which ensures that all registrants comply with essential standards of quality and safety when dealing with patients. The impact of CQC registration on the dental workplace, and its relevance to dental nurses, is discussed more fully in Chapter 3.
Risk assessment
As stated above, the whole purpose of the Health and Safety legislation is to protect everyone within the dental workplace (staff, patients and visitors) from coming to any harm while on the premises. This is achieved by carrying out a risk assessment of every potential hazard that could occur. The aim is not necessarily to eliminate every risk completely (this is likely to be impossible in most workplaces, including dental surgeries) but instead to minimise those risks identified as far as possible, so that there is little chance of them causing harm to anyone.
For example, various chemicals must be used in the dental workplace to carry out dental treatment successfully – these include decontamination solutions, x-ray processing solutions, and mercury in amalgam fillings; all are potentially harmful but only if mishandled. So knowledge of their correct storage and usage by staff, and protection from misuse by all others, are key factors in avoiding a hazardous event.
The steps involved in carrying out a risk assessment on a hazard, whatever its nature, should always follow the same pattern.
Although specialist knowledge of some hazards in the dental workplace is necessary to fully realise their potential for causing harm, many of the actions that should be followed to ensure the health and safety of everyone on the premises are common sense.
Table 4.2 Avoidance of hazards
Consider the scenarios and relevant common-sense actions in Table 4.2 . The table gives examples of various hazardous situations that may be encountered by patients and visitors to the dental workplace in the first column, in a similar way to those that may be encountered by the student dental nurse shown in Table 4.1 . The second column then suggests common-sense actions to take that will minimise the potential risk in the first place. So, for example, there are several potentially harmful chemicals used in dentistry that cannot be avoided, such as bleach-based cleaning agents. When used for their specific purpose, there is no risk but if used contrary to that purpose (such as being swallowed by a child), their potential to cause harm is huge. The common-sense action is to prevent the child from having access to the chemical at all times, by locking it away in a cupboard or storing it in a locked room away from the public access areas of the workplace. The differing design and layout of each workplace will require that an individual risk assessment is carried out for each one.
These scenarios are not exclusive to the dental workplace – they could occur anywhere at any time and to anyone. However, if they do occur in the dental workplace then they are not merely an unavoidable accident but have become an avoidable risk that should have been prevented from happening. In other words, someone is to blame. If the simple common-sense actions have not been carried out initially, then the employer is to blame. If, however, a risk assessment has resulted in the necessary preventive measures being put into place and someone has flouted them, such as by leaving a door or cupboard unlocked to avoid the inconvenience of having to keep unlocking it, then that person is to blame instead.
All members of staff have a legal obligation under the Health and Safety at Work Act to co-operate with their employer by following the policies and procedures put in place to protect all persons while on the premises. They must also take reasonable care for their own and others’ health and safety while on the premises. Failure to do so, as indicated above, will result in their possible investigation and prosecution by the HSE, and a fitness to practise hearing by the GDC, for those who are registrants.
The level of reasonable care expected to be taken for their own health and safety as an employee (and in line with ‘fitness to practise’ requirements by the GDC) requires all dental care professionals to abide by the following when in the dental workplace.
- Undergo suitable training in the use of dental materials and equipment.
- Always follow that training when using those materials and equipment.
- Always follow all policies in relation to health, safety and welfare issues.
- Never misuse any materials or equipment on the premises.
- In particular, never misuse or fail to use any materials or equipment that are specifically meant to reduce or eliminate hazardous risks.
- Always report any faults in procedures or equipment to a senior colleague immediately.
- Never enter certain designated ‘hazardous’ areas unless authorised to do so.
- Always report any suspected health problem that will affect their normal work to a senior colleague as soon as possible.
It is important, then, that a FULL risk assessment of the dental workplace is carried out and its findings reviewed on a regular basis, and that all staff follow the control measures that have been put into place, at all times. Advice and guidance are available on risk assessment generally, and in the dental workplace in particular, from both the HSE and from organisations such as the British Dental Association. Their website addresses for further information are:
- Health and Safety Executive: www.hse.gov.uk
- British Dental Association: www.bda.org .
Fire Precaution (Workplace) Regulations 1999
The above regulations were updated by the Regulatory Reform (Fire Safety) Order, which became law in 2006. This stipulates that the employer/owner of the premises (the dental workplace) must take reasonable steps to reduce the risk from fire, and to make sure that people on the premises can escape safely if there is a fire. They therefore require the employer/owner to risk assess the fire precautions that are needed for their own work premises, as these will vary from one workplace to another; a ground floor practice will be considered less dangerous to staff and patients in the event of a fire than one that is in a multistorey building, for instance.
A typical fire risk assessment should consider the following points, and in this order.
All dental workplaces then undergo a fire safety inspection, so that the premises can be formally recorded as having carried out the necessary risk assessment. Although several companies provide the means for this to be carried out by post, a visit by a suitably qualified inspector from the Fire Brigade will hold more weight if a fire does occur and the practice is held to account for its level of compliance.
The inspection will give advice with regard to the following.
- The number and positioning of smoke detectors.
- The number and positioning of fire extinguishers.
- Written records of staff training in the use of fire extinguishers.
- The types of fire extinguishers to be provided, with at least two types present in all workplaces.
Fire detection
The Regulatory Reform (Fire Safety) Order 2005 states that an electrical fire alarm system and/or an automatic detection system are only necessary on premises where these devices would be necessary to give warning in case of fire. The types of premises involved would be large workplaces, perhaps over several levels, where a fire breaking out in one area could go undetected by an ordinary smoke alarm or unnoticed by a person for some time. Hospital departments and health clinics are examples of places where these additional fire detection methods would be required.
In smaller workplaces (the majority of dental practices), a fire risk assessment should determine that adequate fire detection is provided by battery-operated smoke alarms around the premises ( Figure 4.2 ). The local fire station, or the fire inspector, will give advice on the number required and their suitable locations at key points throughout the premises. They should be tested on a regular basis to ensure they are functioning correctly, and a record kept of these test dates and results. Obviously, the battery should be changed as soon as it begins to fail, or the alarm changed if any malfunctions occur.
Figure 4.2 Smoke alarm.

Fire fighting
The main equipment available for use in fire fighting is the fire extinguisher ( Figure 4.3 ), although some premises will have additional equipment such as fire blankets and hoses. To determine which fire-fighting equipment should be available, the classification of fires is considered as follows.
- Class A fire – caused by the ignition of carbon-containing items such as paper, wood and textiles.
- Class B fire – caused by flammable liquids such as oils, solvents and petrol.
- Class C fire – caused by flammable gases such as domestic gas, butane, liquefied petroleum gas (LPG).
- Class D fire – caused by reactive metals that oxidise in air such as sodium and magnesium.
- Class E fire – caused by electrical components and equipment.
- Class F fire – caused by liquid fats such as used in kitchens and restaurants.
In the dental workplace, the likeliest causes of fire shown above suggest that extinguishers to fight classes A, B, C and E should be available. The content of each fire extinguisher varies depending on its recommended use, and is identifiable by a coloured label or specific wording on the label of the extinguisher. All extinguishers are coloured red so that they are easily visible, while the label and its wording describe the fire classification that it is suitable for, as follows.
- Red (water) extinguisher – for use on all except electrical fires.
- Black (carbon dioxide) extinguisher – for use on all fires.
- Blue (dry powder) extinguisher – for use on all fires.
Figure 4.3 Fire extinguisher.

The extinguishers must all be inspected and certificated by a competent person on an annual basis, and replaced as necessary. They should be located:
- within easy reach, ideally along escape routes
- in conspicuous positions (so not hidden by surrounding cupboards, for example)
- on wall mountings and signposted
- in a similar position on each level of the premises.
Evacuation and escape routes
During the risk assessment process, consideration should be given to whether, in the event of a fire, all persons on the premises could leave safely and reach a place of safety. There should be no possibility of anyone being cut off from escaping from the premises by either smoke or flames.
In particular, the following areas of fire safety must be complied with.
- Escape routes must be kept free from all obstructions to allow immediate evacuation from the premises if necessary. In particular, key-operated doors must be kept unlocked during normal working hours.
- Fire exits must lead directly to a place of safety, usually outside the building itself.
- They must be clearly marked by green ‘Fire Exit’ signs, with an accompanying pictogram of a running man ( Figure 4.4 ).
- Emergency lighting should be provided if necessary – this applies to hospitals rather than individual practices, and will have been identified during the fire risk assessment.
- Emergency doors should open manually in the direction of escape, and should not be operated electrically.
- Sliding or revolving doors should not be used as fire exits.
- All staff must be aware of the fire safety and evacuation process, and the procedure for evacuation should be practised at least annually.
- In addition, some staff should be charged with certain actions during the evacuation procedure, such as checking certain areas are clear or closing certain doors to contain the fire.
- Special consideration also needs to be given to the needs of disabled persons, and in small workplaces they should only be treated in ground-floor surgeries so that they can be easily evacuated from the premises.
Figure 4.4 Fire exit pictogram.

Figure 4.5 Fire escape poster.
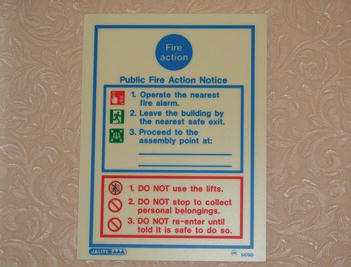
The culmination of the findings from the fire risk assessment will ultimately be the development of a written fire policy or an emergency plan. This is a legal requirement in workplaces with more than five employees, and must be available to all employees and to the fire inspector. It should detail what action everyone on the premises should take in the event of a fire, and may be covered by a simple ‘Fire Action’ poster displayed in the reception area ( Figure 4.5 ). Larger premises will be expected to provide more detail still, and a suitable emergency plan should cover the following points.
- Action to take in the event of a fire.
- Alarm warnings (klaxon, whistle, etc.).
- How to call rescue services.
- Evacuation arrangements, including details for disabled persons.
- Assembly point.
- Method of accounting for all persons (daylist, for example).
- Key escape routes.
- Location and use of fire-fighting equipment.
- Responsibilities of nominated persons.
- Power shutdown methods.
- Staff training.
Smoking in the workplace
Smoking in all enclosed workplaces is now prohibited throughout the UK. All enclosed workplaces, which include all types of dental workplace, must display a ‘No Smoking’ sign at each entrance ( Figure 4.6 ) and the sign must contain the following wording: ‘No smoking. It is against the law to smoke in these premises’. Before the ban, careless disposal of cigarettes was a significant cause of fires in the workplace, so future analysis of fires and their causes will hopefully show a reduction in their incidence.
Figure 4.6 ‘No Smoking’ sign.

Health and Safety (First Aid) Regulations 1981
In addition to the identification of the signs and symptoms of the medical emergencies that may occur in dental practice and their correct management (see Chapter 6), the whole dental team should be able to deal with basic first aid procedures too.
Under the First Aid Regulations, all workplaces must have adequate first aid provision available for all employees, although there is no legal requirement to provide first aid treatment and facilities for non-employees, including patients.
The risk assessment process carried out to comply with general Health and Safety requirements should identify the hazards and risks associated with the workplace itself, and the occupational hazards associated with the business of dentistry. The hazards and risks identified will determine the extent of the first aid provision that is required for the premises and the employees.
In line with clinical governance guidelines (see Chapter 3), every practice must comply with the following requirements.
- All staff must be trained and certificated in basic life support (see Chapter 6).
- All workplaces with more than five employees should have at least one person trained in emergency first aid.
- All practices must have a first aid kit available, besides the full range of emergency drugs and emergency oxygen cylinders required under clinical governance guidelines.
- All practices must have an accident book, which is used to record all except major accidental events that occur on the premises to staff, patients or visitors.
- In the event of a medical emergency, the dental team must be able to reassure and help the casualty until the professionals arrive, and this may include basic life support (BLS) to maintain life if necessary.
Figure 4.7 First aid box.

The first aid kit that must be present in the dental workplace should be placed in an easy-access and signposted location. Regulations stipulate that it should be a green box with a white cross on ( Figure 4.7 ), and should contain minimum requirements with regard to sterile dressings, eye pads, bandages, etc.
Specific training for emergency first aid is provided by various HSE-approved organisations, including the British Red Cross and St John Ambulance. The first aid emergencies that should be covered are as follows, and are summarised below.
Severe bleeding
Burns and scalds, electrocution.
- Bone fractures
- The first aid principle is to restrict the blood flow to the wound and encourage clotting to reduce blood loss .
- Arterial bleeding will spurt rhythmically and be cherry red in colour.
- Venous bleeding will gush quickly and be dark red or purple in colour.
- Capillary bleeding will ooze slowly and be dark red in colour.
- The required treatment is to raise the injured part above the level of the heart if possible, and apply direct pressure to the wound for up to 15 min using a clean dressing.
- Any foreign objects present should not be removed from the wound.
- As a last resort, severed arteries can be compressed against the underlying bone for up to 15 min, using a tourniquet.
- The casualty should be removed to hospital once the bleeding is under control, or the emergency services should be called if it cannot be controlled.
Possible causes of severe bleeding in the dental workplace include unexpected surgical trauma, traumatic falls, severe sharps injury, etc.
- A burn is an injury caused by dry heat, corrosive chemicals or irradiation.
- A scald is a wet burn caused by steam or hot liquids.
- The first aid principles are to prevent infection of the underlying tissues and to prevent clinical shock developing due to the loss of blood serum.
- The required treatment is to remove the casualty from the source of danger if possible, and to reassure them if they are still conscious.
- The injured part should be placed under cold water for a minimum of 10 min, to reduce blistering.
- Any restrictive jewellery should be removed before any swelling occurs, but clothing should be left in place as its removal may causing tearing of the tissues.
- Seek medical help for all but minor burns or scalds, and be prepared to carry out BLS if clinical shock develops in severe cases.
Possible causes of burns in the dental workplace include touching hot equipment or instruments, touching naked flames, various chemicals (etching gel, bleach products, other cleaning agents) and uncontrolled exposure to x-rays.
- The first aid principle is to limit the exposure of the casualty to the poison , and maintain life if necessary.
- Consult any available COSHH documentation for the required first aid advice.
- The required treatment is to remove the casualty from the source of the poison, without endangering other lives.
- Where vapours are the cause, provide good ventilation of the area immediately.
- Vomiting should not be induced, as caustic poisons will burn the digestive tract each time they pass through.
- Maintain the airway and carry out BLS if necessary.
- Seek urgent medical help.
Possible causes in the dental workplace include the ingestion or inhalation of various agents, such as corrosive chemicals (bleach products and acids), toxic chemicals (cleaning agents, processing chemicals, mercury), toxic vapours (processing chemicals, mercury, gases).
- This is caused by an electrical current passing through the body, causing burns and possibly affecting the electrical conduction of the heart itself.
- The first aid principle is to remove the casualty from the electrical source and maintain life until help arrives .
- The required treatment is to isolate the electrical supply if it is safe to do so, treat any surface burns and minimise the effects of clinical shock.
- The casualty should not be touched by the rescuer until the electrical source has been isolated, otherwise the rescuer could be electrocuted too.
- Carry out BLS if necessary.
Possible causes in the dental workplace are any faulty electrical equipment items, including portable appliances.
- A fracture is a break of a bone, either contained within the surrounding soft tissues or puncturing through them to cause a compound fracture, where the bone ends are visible and soft tissue damage is severe.
- The first aid principle is to prevent further tissue damage by restricting the movement of the casualty .
- The required treatment is to not move any injured part of the body, to cover any open skin wounds with clean dressings, and control bleeding as necessary.
Possible causes in the dental workplace are external trauma or a fall, although violent assault of a person may also be a cause.
Basic life support techniques and medical emergencies are covered in detail in Chapter 6.
Control of Substances Hazardous to Health (COSHH) 1994
Many of the chemicals and other hazardous substances used in the dental workplace can be harmful to a person’s health if they are misused or if adequate precautions are not taken to prevent access by unauthorised persons. However, without these substances the business of dentistry could not be carried out, so the continued use of the chemicals under safe conditions is the desired outcome. Again, the level of risk from any of the chemicals or substances involved, those who may be harmed and the necessary precautions to take are all determined by carrying out a risk assessment.
The risk assessment process to be followed in this case is determined by the COSHH regulations, which require all dental workplaces to carry out a risk assessment of all the chemicals and potentially hazardous substances used in the premises, to identify those that could harm or injure staff members. Harm may be caused if an accident occurs to expose personnel to an unusually large amount of a chemical, or if a chemical accidentally gains entry to the body (for example, by being inhaled), or merely just by the dangerous nature of even small amounts of a chemical (for example, mercury). The risk assessment process follows the usual steps but the written report produced must include every potential chemical hazard found, and the following specific information.
- The hazardous ingredient(s) it contains.
- The nature of the risk, ideally by indicating the risk category using recognised symbols ( Figure 4.8 ).
- The possible health effects of the hazardous ingredient(s).
- The precautions required for the safe handling of the product.
- Any additional hazard control methods required for its safe use.
- All necessary first aid measures required in the event of an accident involving the product.
Figure 4.8 Symbols of COSHH risk categories.
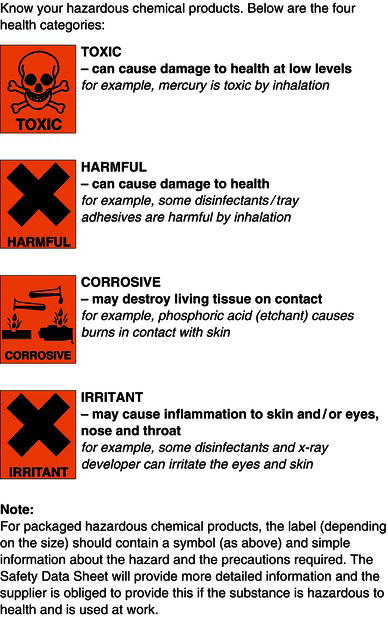
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- 2 The Dental Nurse
- 7 Microbiology and Pathology
- 8 Infection Control and Cleanliness
- 9 Head and Neck Anatomy and Physiology
- 16 Prosthodontics
- 12 Oral Health Assessment and Diagnosis
Stay updated, free dental videos. Join our Telegram channel
Comments are closed for this page.

VIDEdental - Online dental courses

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cochrane Database Syst Rev
One‐to‐one oral hygiene advice provided in a dental setting for oral health
Effective oral hygiene measures carried out on a regular basis are vital to maintain good oral health. One‐to‐one oral hygiene advice (OHA) within the dental setting is often provided as a means to motivate individuals and to help achieve improved levels of oral health. However, it is unclear if one‐to‐one OHA in a dental setting is effective in improving oral health and what method(s) might be most effective and efficient.
To assess the effects of one‐to‐one OHA, provided by a member of the dental team within the dental setting, on patients' oral health, hygiene, behaviour, and attitudes compared to no advice or advice in a different format.
Search methods
Cochrane Oral Health's Information Specialist searched the following databases: Cochrane Oral Health's Trials Register (to 10 November 2017); the Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 10) in the Cochrane Library (searched 10 November 2017); MEDLINE Ovid (1946 to 10 November 2017); and Embase Ovid (1980 to 10 November 2017). The US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform were also searched for ongoing trials (10 November 2017). No restrictions were placed on the language or date of publication when searching the electronic databases. Reference lists of relevant articles and previously published systematic reviews were handsearched. The authors of eligible trials were contacted, where feasible, to identify any unpublished work.
Selection criteria
We included randomised controlled trials assessing the effects of one‐to‐one OHA delivered by a dental care professional in a dental care setting with a minimum of 8 weeks follow‐up. We included healthy participants or participants who had a well‐defined medical condition.
Data collection and analysis
At least two review authors carried out selection of studies, data extraction and risk of bias independently and in duplicate. Consensus was achieved by discussion, or involvement of a third review author if required.
Main results
Nineteen studies met the criteria for inclusion in the review with data available for a total of 4232 participants. The included studies reported a wide variety of interventions, study populations, clinical outcomes and outcome measures. There was substantial clinical heterogeneity amongst the studies and it was not deemed appropriate to pool data in a meta‐analysis. We summarised data by categorising similar interventions into comparison groups.
Comparison 1: Any form of one‐to‐one OHA versus no OHA
Four studies compared any form of one‐to‐one OHA versus no OHA.
Two studies reported the outcome of gingivitis. Although one small study had contradictory results at 3 months and 6 months, the other study showed very low‐quality evidence of a benefit for OHA at all time points (very low‐quality evidence).
The same two studies reported the outcome of plaque. There was low‐quality evidence that these interventions showed a benefit for OHA in plaque reduction at all time points.
Two studies reported the outcome of dental caries at 6 months and 12 months respectively. There was very low‐quality evidence of a benefit for OHA at 12 months.
Comparison 2: Personalised one‐to‐one OHA versus routine one‐to‐one OHA
Four studies compared personalised OHA versus routine OHA.
There was little evidence available that any of these interventions demonstrated a difference on the outcomes of gingivitis, plaque or dental caries (very low quality).
Comparison 3: Self‐management versus professional OHA
Five trials compared some form of self‐management with some form of professional OHA.
There was little evidence available that any of these interventions demonstrated a difference on the outcomes of gingivitis or plaque (very low quality). None of the studies measured dental caries.
Comparison 4: Enhanced one‐to‐one OHA versus one‐to‐one OHA
Seven trials compared some form of enhanced OHA with some form of routine OHA.
Authors' conclusions
There was insufficient high‐quality evidence to recommend any specific one‐to‐one OHA method as being effective in improving oral health or being more effective than any other method. Further high‐quality randomised controlled trials are required to determine the most effective, efficient method of one‐to‐one OHA for oral health maintenance and improvement. The design of such trials should be cognisant of the limitations of the available evidence presented in this Cochrane Review.
Plain language summary
One‐to‐one oral hygiene advice for oral health
Review question
The aim of this review was to assess the effects of one‐to‐one oral hygiene advice, provided by a member of the dental team within the dental setting, on patients' oral health, hygiene, behaviour, and attitudes compared to no advice or advice in a different format.
Poor oral hygiene habits are known to be associated with high rates of dental decay and gum disease. The dental team routinely assess oral hygiene methods, frequency and effectiveness or otherwise of oral hygiene routines carried out by their patients; one‐to‐one oral hygiene advice is regularly provided by members of the dental team with the aim of motivating individuals and improving their oral health. The most effective method of delivering one‐to‐one advice in the dental setting is unclear. This review's aim is to determine if providing patients with one‐to‐one oral hygiene advice in the dental setting is effective and if so what is the best way to deliver this advice.
Study characteristics
Authors from Cochrane Oral Health carried out this review and the evidence is up to date to 10 November 2017. We included research where individual patients received oral hygiene advice from a dental care professional on a one‐to‐one basis in a dental clinic setting with a minimum of 8 weeks follow‐up.
In total, within the identified 19 studies, oral hygiene advice was provided by a hygienist in eight studies, dentist in four studies, dental nurse in one study, dentist or hygienist in one study, dental nurse and hygienist in one study, and dental nurse oral hygiene advice to the control group with further self‐administration of the intervention in one study. It was unclear in three of the studies which member of the dental team carried out the intervention. Over half of the studies (10 of the 19) were conducted in a hospital setting, with only five studies conducted in a general dental practice setting (where oral hygiene advice is largely delivered).
Key results
Overall we found insufficient evidence to recommend any specific method of one‐ to‐one oral hygiene advice as being more effective than another in maintaining or improving oral health.
The studies we found varied considerably in how the oral hygiene advice was delivered, by whom and what outcomes were looked at. Due to this it was difficult to readily compare these studies and further well designed studies should be conducted to give a more accurate conclusion as to the most effective method of maintaining or improving oral health through one‐to‐one oral hygiene advice delivered by a dental care professional in a dental setting.
Quality of the evidence
We judged the quality of the evidence to be very low due to problems with the design of the studies.
Summary of findings
Description of the condition.
Dental caries and periodontal disease are the two most prevalent dental conditions globally; both are largely preventable. The accumulation of dental plaque, a microbial biofilm on the tooth surface is a primary aetiological factor in both diseases ( Löe 1965 ; Löe 1972 ).
When the microbial biofilm is exposed to carbohydrate sources via the host's diet it can lead to the localised lowering of the pH which results in the chemical dissolution of the tooth surface ( Sheiham 2015 ). If this process goes undisturbed the caries process can lead to a lesion or 'cavity' in the exposed tooth. Although the affected carious tooth often remains asymptomatic in the early stages of the disease, the longer term consequences can be toothache, sepsis or ultimately tooth loss. Estimates of the prevalence of caries varies worldwide but the 2010 global burden of disease study estimated that untreated caries in permanent teeth was the most prevalent condition worldwide affecting an estimated 2.4 billion people ( Kassebaum 2015 ). Self‐care prevention strategies include: reducing free sugars intake; disruption of plaque biofilm (toothbrushing and interdental cleaning aids); using a fluoride dentifrice or fluoride mouthwash or both ( Marinho 2003 ; Marinho 2004a ; Marinho 2004b ; Marinho 2016 ). Self‐care strategies can be supplemented by professional interventions including fluoride gels and varnishes ( Marinho 2003 ; Marinho 2004a ; Marinho 2004b ).
The accumulation of dental plaque also results in the inflammation of the periodontium (supporting structures) of the teeth. The undisturbed plaque biofilm initially causes swelling, loss of texture, characteristic redness of the gingiva and liability to gingival bleeding (gingivitis). At this early stage the disease is reversible by the disruption of the dysbiotic pathogenic biofilm allowing a return to healthy periodontal tissues. Periodontal disease, like dental caries often goes unnoticed by patients at its earliest stages. If left undisturbed in susceptible patients, gingival inflammation can lead to the irreversible loss of supporting structures (periodontitis), which can present as gingival recession, sensitivity of the exposed root, tooth mobility, drifting of the teeth or ultimately tooth loss. Studies suggest that 50% to 90% of adults in the UK and USA have gingivitis. The global burden of disease study estimated that severe periodontitis affects approximately 11% of the global population or 743 million people worldwide ( Kassebaum 2014 ).
Oral self‐care prevention involves disruption of the plaque biofilm (toothbrushing and interdental cleaning aids) ( Poklepovic 2013 ; Yaacob 2014 ) and control of systemic risk factors (e.g. smoking) ( Tonetti 2017 ). There is evidence to suggest effective dental plaque control sustained over the longer term can achieve reduced experience of periodontal disease, dental caries and ultimately tooth mortality rates ( Axelsson 2004 ).
Description of the intervention
The patient's own oral self‐care is a crucial component of the prevention strategies for dental caries and periodontal disease. Ultimately the aim of oral hygiene advice (OHA) is to enable a patient to improve their own oral self‐care and consequently their oral health. To improve a patient's oral self‐care, OHA can be delivered in a variety of formats by any appropriately trained member of the dental team. The content of OHA can include: toothbrushing and toothpaste advice, interdental cleaning advice, mouthwash advice, denture hygiene advice and/or orthodontic fixed/removable appliance hygiene advice.
How the intervention might work
OHA may work through improving patient knowledge, attitudes, and behaviours. Helping patients to understand their disease process and the preventative actions required may motivate them to change their oral self‐care behaviours thus reducing their risk of oral disease. In addition, OHA may improve patients' confidence in carrying out oral self‐care and/or highlight barriers and enablers to facilitate improved oral self‐care. Adequate oral hygiene regimens help prevent dental caries and periodontal disease.
Why it is important to do this review
Current clinical guidance recommends that OHA should be reinforced regularly and tailored to individual patients' needs to attain sustainable benefits ( NICE 2015 ). Advice or information regarding toothbrushing is currently not uniformly provided to all patients. In England in 2009, 78% of adults reported receiving advice on cleaning their teeth and gums, an increase from 63% in 1998 ( Chadwick 2011 ). Within the child population, oral health advice varies widely in both content and to whom it is provided ( Tickle 2003 ) with younger children being less likely to receive advice than older children ( Tsakos 2015 ).
Although OHA is taught as an obligatory part of the undergraduate dental curriculum (given OHA frequently forms part of routine dental care), there remains uncertainty as to how, where and by whom OHA should be provided to be effective. Previously, the main focus of preventing oral disease has been to increase patient knowledge and awareness regarding oral health, with the hope that this would lead to improved oral health status ( Towner 1993 ). This has been superceded by oral health promotion, which aims not only to increase public knowledge, but also to utilise a multidisciplinary approach aimed at the underlying determinants of oral health ( WHO 1986 ; WHO 2003 ). A systematic review of oral health promotion concluded that the evidence for long‐term reduction in plaque and gingival bleeding outcomes, based on mainly short‐term interventions, was limited. There were also conflicting conclusions regarding the relative effectiveness of different types/styles of educational interventions employed ( Watt 2005 ). A recent systematic review of psychological approaches to behaviour change for improved plaque control in periodontal management concluded that interventions based on the use of goal setting, self‐monitoring and planning are effective in improving oral health‐related behaviours as assessed by oral health status ( Newton 2015 ), although these conclusions were based upon observational studies as well as randomised controlled trials.
Although there are a variety of healthcare professionals who may be involved in the delivery of OHA, both within the dental surgery and within the wider community setting, there does not appear to be any systematic reviews published previously which assess the effect of the individual providing OHA.
To assess the effects of one‐to‐one oral hygiene advice, provided by a member of the dental team within the dental setting, on patients' oral health, hygiene, behaviour, and attitudes compared to no advice or advice in a different format.
Criteria for considering studies for this review
Types of studies.
We included all randomised controlled trials (RCTs) in which participants who were provided with one‐to‐one oral hygiene advice (OHA) by a member of the dental team in the dental setting were compared to participants not provided with OHA. We also included RCTs which compared different formats (e.g. DVD, leaflet, video, etc.) of one‐to‐one OHA provided within the dental setting or OHA provided by different members of the dental team within the dental setting. We only included studies with a minimum follow‐up period of 8 weeks. The unit of randomisation could be individual participants, clusters of individuals, or dental setting.
Types of participants
We included studies that involved children (with or without guardian/parent) or adult participants who were fit and healthy or groups of individuals who had well defined medical conditions. Studies involving participants who wore a removable prosthesis or orthodontic appliance of any kind were excluded.
Types of interventions
We included studies that involved OHA being provided by any member of the dental team within the dental setting environment (i.e. within a general dental practice, community dental setting or dental hospital setting) on a one‐to‐one basis in which the comparator was no advice or advice in an alternative format or advice from a different member of the dental team. Dental team members included dentist, dental nurse, dental hygienist and dental therapist. Studies were included if the OHA took place alongside an intervention aiming to change dietary behaviour or smoking behaviour, although these multi‐intervention studies were planned to be subjected to a subgroup analysis if any such studies had met the inclusion criteria.
We excluded any studies where additional measures were provided to the intervention group but not the control group (e.g. dental prophylaxis, dental scaling, application or provision of fluoride containing products, provision of toothbrushes, etc.).
Types of outcome measures
Outcome measures considered in this review included clinical status, patient‐centred and economic factors. The outcome measure must have been assessed at least 8 weeks following the intervention.
Primary outcomes
Clinical status factors.
- Periodontal health (e.g. plaque levels, gingivitis, and probing depths).
- Caries (e.g. dmft/DMFT or other indices).
Secondary outcomes
Patient‐centred factors.
- Patient‐reported behaviour changes (e.g. toothbrushing/flossing/mouthwash use).
- Patient satisfaction with advice provided.
- Patient‐reported changes in knowledge, attitudes, and quality of life.
Economic factors
- Cost effectiveness.
Other outcomes
- Any adverse events due to OHA reported in the included trials.
Search methods for identification of studies
Cochrane Oral Health's Information Specialist conducted systematic searches in the following databases for RCTs and controlled clinical trials. There were no language, publication year or publication status restrictions:
- Cochrane Oral Health's Trials Register (searched 10 November 2017) ( Appendix 1 );
- Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 10) in the Cochrane Library (searched 10 November 2017) ( Appendix 2 );
- MEDLINE Ovid (1946 to 10 November 2017) ( Appendix 3 );
- Embase Ovid (1980 to 10 November 2017) ( Appendix 4 ).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 6 ( Lefebvre 2011 ).
Searching other resources
The following trial registries were searched for ongoing studies:
- US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 10 November 2017) ( Appendix 5 );
- World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 10 November 2017) ( Appendix 6 ).
Bibliographic references of identified RCTs and articles identified as relevant to the review retrieved in the electronic search were also searched (e.g. review articles and systematic reviews). In addition, emails were sent to authors of identified potentially eligible RCTs asking them for other known unpublished or ongoing research. Relevant sections of the reports were translated of non‐English publications identified from title, abstract, or keyword, to be of interest.
Selection of studies
The search was designed to be sensitive and included controlled clinical trials, these were filtered out early in the selection process if they were not randomised.
At least two review authors reviewed and analysed independently all reports identified by the search on the basis of title, keywords, and abstract (where this was available) to see if the study was likely to be relevant. Where it was not possible to classify an article based on title, keywords and abstract, we obtained the full article. The full report was obtained of all potentially eligible studies, and also of studies where the title/abstract provided insufficient information to make a decision on eligibility.
The review authors were not blinded with respect to report authors, journals, date of publication, sources of financial support, or results. The inclusion criteria, as outlined above, were applied and those studies deemed suitable for inclusion by at least two review authors were included. We contacted study authors for missing information or clarity regarding methods, results, etc. where required and feasible. We linked multiple publications of the same study under one single study title. Those studies excluded are cited with reasons for exclusion reported.
Two review authors independently and in duplicate assessed the eligibility of the non‐English language reports. Relevant sections of the reports were translated with the assistance of Cochrane Oral Health and non‐English reports that met the inclusion criteria had data extraction and risk of bias completed.
Data extraction and management
A data extraction form was designed and piloted prior to full use. At least two review authors independently extracted data from each of the potentially eligible studies; any disagreements between the two review authors undertaking data extraction was resolved by discussion and if necessary the involvement of a third review author. If necessary we contacted the study author, where possible, to clarify any unclear or inadequate characteristics before a final decision on inclusion was made. Data recorded included the following:
- general study information: authors, title, year research completed, year research published, country, ethics and consent process, financial support and conflicts of interest, country, contact address;
- methods: research objective, sample size calculation, allocation procedures, follow‐up period, degree of blindness in outcome assessment;
- participants: inclusion/exclusion criteria, age, medical factors, baseline periodontal health/caries status/behaviours/knowledge/attitudes/quality of life;
- intervention and comparators: type of OHA, format of OHA, advice duration, advice frequency, personnel providing advice;
- outcomes: primary and secondary outcomes and outcome measures.
Assessment of risk of bias in included studies
The risk of bias of included trials for the seven domains of random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential sources for bias was undertaken independently and in duplicate by at least two review authors as part of the data extraction process and in accordance with the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 ( Higgins 2011 ). Where possible, we contacted study authors for missing information or clarification of their study methods. Any disagreements were resolved by discussion between the review authors with Cochrane Oral Health being consulted where there was continuing disagreement.
We allocated the level of bias for each domain as high or low as per the criteria below; for those domains where insufficient information was available or not described in sufficient detail to allow a definitive judgement then the level of bias was recorded as unclear.
Random sequence generation
- Low: the investigators describe a random component in the sequence generation process such as referring to a random number table, using a computer random number generator, etc..
- High: the investigators describe a non‐random component in the sequence generation process. Usually, the description would involve some systematic, non‐random approach, (e.g. sequence generated by odd or even date of birth, etc.).
Allocation concealment
- Low: participants and investigators enrolling participants could not foresee assignment because an appropriate method was used to conceal allocation (e.g. central allocation, etc.).
- High: participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on using an open random allocation schedule, etc..
- Blinding of participants and personnel
- Low: no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding.
- High: no blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding.
- Blinding of outcome assessment
- Low: no blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding; blinding of outcome assessment ensured, and unlikely that the blinding could have been broken.
- High: no blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement is likely to be influenced by lack of blinding.
Incomplete outcome data
- Low: no missing outcome data; reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size; missing data have been imputed using appropriate methods.
- High: reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size; 'as‐treated' analysis done with substantial departure of the intervention received from that assigned at randomisation; potentially inappropriate application of simple imputation.
Selective reporting
- Low: the study protocol is available and all of the study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way.
- High: not all of this study's pre‐specified primary outcomes have been reported; one or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis; the study report fails to include results for a key outcome that would be expected to have been reported for such a study.
- Other potential sources for bias
- Low: the study appears to be free of other sources of bias.
- High: there is as least one important risk of bias, for example a potential source of bias related to the specific study design used.
We summarised the risk of bias as follows.
Measures of treatment effect
For continuous outcomes (e.g. plaque/gingivitis scores), where studies used the same scale, we used the mean values and standard deviations reported in the studies in order to express the estimate of effect of the intervention as mean difference (MD) with 95% confidence interval (CI). Where different scales were used, we expressed the treatment effect as standardised mean difference (SMD) and 95% CI.
For dichotomous outcomes (e.g. attachment loss/no attachment loss), we expressed the estimate of effect as a risk ratio (RR) with 95% CI. Had we included any cross‐over studies, we would have extracted appropriate data following the methods outlined by Elbourne 2002 , and would have used the generic inverse variance method to enter log RRs or MD/SMD and standard error into Review Manager 5 ( Review Manager 2014 ).
Unit of analysis issues
The participant was the unit of analysis. Had we included any cross‐over studies, these should have analysed data using a paired t‐test, or other appropriate statistical test, to take into account the paired nature of the data. Cluster‐RCTs should have analysed results taking account of the clustering present in the data, otherwise we would have used the methods outlined in Section 16.3.4 of the Cochrane Handbook for Systematic Reviews of Interventions in order to perform an approximately correct analysis ( Higgins 2011 ).
Dealing with missing data
We attempted, where feasible, to contact the author(s) of studies to obtain missing data or for clarification. We did not use any further statistical methods or carry out any further imputation to account for missing data.
Assessment of heterogeneity
Heterogeneity was assessed by examining the types of participants, interventions and outcomes in each study. It was agreed in advance that meta‐analysis would only be attempted if studies of similar comparisons reporting the same outcome measures were included in the review.
If it had been appropriate to perform meta‐analysis, we would have assessed the possible presence of heterogeneity visually by inspecting the point estimates and CIs on the forest plots; if the CIs had poor overlap then heterogeneity would have been considered to be present. We would also have assessed heterogeneity statistically using a Chi 2 test, where a P value < 0.1 would have been considered to indicate statistically significant heterogeneity. Furthermore, we would have quantified heterogeneity using the I 2 statistic. A guide to interpretation of the I 2 statistic given in Section 9.5.2 of the Cochrane Handbook for Systematic Reviews of Interventions is as follows ( Higgins 2011 ):
- 0% to 40%: might not be important;
- 30% to 60%: may represent moderate heterogeneity;
- 50% to 90%: may represent substantial heterogeneity;
- 75% to 100%: considerable heterogeneity.
Assessment of reporting biases
Assessment of reporting bias within studies has already been described in the section Assessment of risk of bias in included studies . Reporting biases can occur when reporting (or not reporting) research findings is related to the results of the research (e.g. a study that did not find a statistically significant difference/result may not be published). Reporting bias can also occur if ongoing studies are missed (but that may be published by the time the systematic review is published), or if multiple reports of the same study are published, or if studies are not included in a systematic review due to not being reported in the language of the review authors. If there had been more than 10 studies included in a meta‐analysis, we would have assessed the possible presence of reporting bias by testing for asymmetry in a funnel plot. If present, we would have carried out statistical analysis using the methods described by Egger 1997 for continuous outcomes and Rücker 2008 for dichotomous outcomes. However, we did attempt to limit reporting bias in the first instance by conducting a detailed, sensitive search, including searching for ongoing studies, and any studies not reported in English were translated by a member of Cochrane Oral Health.
Data synthesis
We would only have carried out a meta‐analysis where studies of similar comparisons reported the same outcomes. We would have combined MDs (we would have used SMD where studies had used different scales) for continuous outcomes, and would have combined RRs for dichotomous outcomes, using a fixed‐effect model if there were only two or three studies, or a random‐effects model if there were four or more studies.
We would have used the generic inverse variance method to include data from cross‐over studies in meta‐analyses as described in Section 16.4 of the Cochrane Handbook for Systematic Reviews of Interventions ( Elbourne 2002 ; Higgins 2011 ). Where appropriate, we would have combined the results from cross‐over studies with parallel group studies, using the methods described by Elbourne 2002 .
Subgroup analysis and investigation of heterogeneity
If it had been required, subgroup analyses would have been undertaken where OHA had taken place alongside an intervention aiming to change dietary behaviour or smoking behaviour, personnel providing advice and frequency of advice.
If there had been a number of similar studies, sensitivity analysis would have been considered to determine whether conclusions reached would be affected by different inclusion criteria. However, given the heterogeneity of studies included this was not required.
Presentation of main results
We produced a 'Summary of findings' table for each comparison. We included gingivitis, plaque and dental caries. We used GRADE methods (GRADE 2004), and the GRADEpro GDT online tool for developing 'Summary of findings' tables (www.guidelinedevelopment.org). We assessed the quality of the body of evidence for each comparison and outcome by considering the overall risk of bias of the included studies, the directness of the evidence, the inconsistency of the results, the precision of the estimates, and the risk of publication bias. We categorised the quality of each body of evidence as high, moderate, low, or very low.
Description of studies
See Characteristics of included studies ; Characteristics of excluded studies ; Characteristics of studies awaiting classification ; Characteristics of ongoing studies .
Results of the search
The literature search resulted in 15,188 references following de‐duplication. In addition, we also handsearched the references of seven relevant systematic reviews ( Harris 2012 ; Kay 1998 ; Kay 2016a ; Kay 2016b ; Khokhar 2016 ; Newton 2015 ; Yevlahova 2009 ) and two reviews ( Pastagia 2006 ; Watt 2005 ), identifying two further studies ( Hetland 1982 ; Little 1997 ). Four review authors screened the titles and abstracts against the inclusion criteria for this review, independently and in duplicate, and 15,076 references were found to be ineligible for this review (including four potentially eligible references but they had abstracts‐only published with no further information regarding the study available). Full‐text copies of the remaining references were obtained and examined independently and in duplicate, excluding 84 studies at this stage. Two studies are awaiting classification and four are ongoing. Nineteen studies reported in 24 papers met the inclusion criteria for this review. Handsearching of the references of included studies and correspondence from authors identified no further studies for inclusion. This process is illustrated in Figure 1 PRISMA flow diagram.

Study flow diagram.
Included studies
Characteristics of trial design and setting.
Nineteen studies met the inclusion criteria of the review and were included ( Characteristics of included studies ). All 19 studies were of parallel‐group design, 10 of which had two trial arms ( Aljafari 2017 ; Baab 1986 ; Bali 1999 ; Glavind 1985 ; Jönsson 2006 ; Jönsson 2009 ; Lepore 2011 ; López‐Jornet 2014 ; Münster Halvari 2012 ; Tedesco 1992 ), four of which had three arms ( Hetland 1982 ; Hoogstraten 1983 ; Memarpour 2016 ; Söderholm 1982 ), two of which had four arms ( Hugoson 2007 ; Weinstein 1996 ), and two of which had six arms ( Schmalz 2018 ; Van Leeuwen 2017 ). One study was a cluster‐randomised design with oral hygiene advice (OHA) randomised by cluster (routine or personalised OHA) and scale and polish treatment by parallel randomisation with three arms ( Ramsay 2018 ).
Ten of the included studies were conducted in hospital/graduate clinics ( Aljafari 2017 ; Baab 1986 ; Bali 1999 ; Jönsson 2006 ; Jönsson 2009 ; Lepore 2011 ; López‐Jornet 2014 ; Schmalz 2018 ; Söderholm 1982 ; Van Leeuwen 2017 ), four in a dental practice setting ( Glavind 1985 ; Hoogstraten 1983 ; Münster Halvari 2012 ; Ramsay 2018 ), one in public healthcare settings ( Memarpour 2016 ), one study involved one clinic in a public dental setting and the other a general dental practice ( Hugoson 2007 ), one was in a factory which had two dental units and chairs installed for the purpose of the study ( Hetland 1982 ), and two trials did not specify which dental setting they were conducted in ( Tedesco 1992 ; Weinstein 1996 ).
Fifteen of the studies were single centre with one study reporting two centres ( Hugoson 2007 ), one study with three centres ( Glavind 1985 ), one study with five centres ( Memarpour 2016 ), and one study with 63 centres ( Ramsay 2018 ).
Four studies were conducted in Sweden ( Hugoson 2007 ; Jönsson 2006 ; Jönsson 2009 ; Söderholm 1982 ), three in the USA ( Baab 1986 ; Lepore 2011 ; Tedesco 1992 ), two in the Netherlands ( Hoogstraten 1983 ; Van Leeuwen 2017 ), two in Norway ( Hetland 1982 ; Münster Halvari 2012 ), one in Germany ( Schmalz 2018 ), and one in Denmark ( Glavind 1985 ), Spain ( López‐Jornet 2014 ), Italy ( Weinstein 1996 ), England ( Aljafari 2017 ), Austria ( Bali 1999 ), Iran ( Memarpour 2016 ), and one study across the United Kingdom in Scotland and North East England ( Ramsay 2018 ).
Only seven studies mentioned sample size calculations ( Aljafari 2017 ; Jönsson 2009 ; Memarpour 2016 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Van Leeuwen 2017 ). Four of these studies achieved their sample sizes and had the required number of participants at follow‐up ( Memarpour 2016 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ). Jönsson 2009 reported their sample size calculation but noted that they did not recruit or follow up this number of participants; the original examiner could not continue to complete recruitment and a second examiner could not be recruited in time. The authors also noted that the original power analysis was based on an intervention that was less effective than the intervention investigated in their study. Aljafari 2017 reported that only 55% of the recruited sample completed the telephone follow‐up 3 months after the child's dental care under general anaesthetic; the authors recommended the results be interpreted with caution given the sample size calculation deemed a sample of 45 participants in each group would have been required to provide 80% power, at the 5% significance level, to detect effects of 0.6 and above. At 3‐month follow‐up there were 28 patients and 31 patients available from the intervention and control group, respectively ( Aljafari 2017 ). Van Leeuwen 2017 achieved their sample size in five of the six groups at 13 months such that the recruitment target was achieved at the 4‐month review for all groups, but not thereafter.
Eleven studies reported their funding source with six having received some form of public funding ( Aljafari 2017 ; Baab 1986 ; Hugoson 2007 ; Münster Halvari 2012 ; Ramsay 2018 ; Tedesco 1992 ), one with dental association research funds ( Glavind 1985 ), one with national health research and development funding ( Van Leeuwen 2017 ), one with a university grant ( Memarpour 2016 ), and one study reported joint funding sources between research council, public funding and the Pfizer oral care award ( Jönsson 2009 ). One study acknowledged Philips GmbH (Hamburg, Germany), CP GABA (GmbH, Hamburg, Germany), and GlaxoSmithKline Oral Health Care GmbH (Brühl, Germany) for providing materials for the study ( Schmalz 2018 ).
Characteristics of the participants
A total of 4232 participants were recruited, with numbers included in each trial ranging from 33 to 1877. Three studies investigated children with a mean age of 20 months, 3 years and six years old and age ranges from 1 year to 10 years old ( Aljafari 2017 ; Lepore 2011 ; Memarpour 2016 ). In the remaining adult population studies, the age range of the sample was reported in 15 studies with the mean age of adults ranging from 20 years to 58 years old and age range from 15 years to 91 years old ( Baab 1986 ; Bali 1999 ; Glavind 1985 ; Hetland 1982 ; Hoogstraten 1983 ; Jönsson 2006 ; Jönsson 2009 ; López‐Jornet 2014 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ; Weinstein 1996 ).
Two studies restricted their inclusion criteria to participants who were known to have a specific medical condition: diabetes ( Bali 1999 ) and hyposalivation ( López‐Jornet 2014 ).
The dental condition pre‐treatment required participants to be caries free in three studies ( Memarpour 2016 ; Schmalz 2018 ; Van Leeuwen 2017 ) and only those with caries were included in another study ( Aljafari 2017 ). Eight studies reported that the included individuals were only those with plaque present ( Glavind 1985 ) or those who had active or previously treated periodontal disease patients ( Baab 1986 ; Glavind 1985 ; Jönsson 2006 ; Jönsson 2009 ; Tedesco 1992 ; Van Leeuwen 2017 ; Weinstein 1996 ). One study reported including those individuals with healthy periodontal status, gingivitis or moderate periodontal disease ( Ramsay 2018 ). One study specified that there were to be no periodontal pockets ≥4.0 mm, as measured by a pocket probe, and/or serious bone loss visualized by digital X rays during the dental examination ( Münster Halvari 2012 ), and another specified there to be no periodontal attachment loss greater than 1.5 mm, radiographic evidence of bone loss greater than 25% (anterior/posterior bite‐wing radiographs or periapical radiographs), or previous periodontal therapy ( Tedesco 1992 ); another specified there to be no pockets of 4 mm to 5 mm in combination with gingival recession or pockets of ≥ 6 mm, as assessed according to the Dutch Periodontal Screening Index (DPSI) scores 3+ and 4 ( Van Leeuwen 2017 ).
Characteristics of the interventions
Intervention type.
A variety of interventions were used in the included studies, none of which were entirely identical.
- Two studies used self‐inspection/instruction manuals ( Baab 1986 ; Glavind 1985 ) with a further incorporating self‐assessment as part of the intervention ( Weinstein 1996 ).
- One study reported participants received one‐to‐one advice on toothbrushing technique ( Schmalz 2018 ).
- One used a computer game ( Aljafari 2017 ), one included instruction and viewing of an educational film ( Hoogstraten 1983 ), and another included showing patients a phase‐contrast slide of their own subgingival flora on a video monitor ( Tedesco 1992 ).
- One study reported the intervention group receiving once‐only professional individual oral hygiene instruction ( Van Leeuwen 2017 ), one with a three‐visit oral hygiene instruction program delivered on a once a week basis ( Hetland 1982 ), one with intensive patient education in oral hygiene with additional control examinations ( Bali 1999 ), another providing oral hygiene instruction in addition to a pamphlet and toothbrush ( Memarpour 2016 ), or similar instruction at a variable number of appointments ( Söderholm 1982 ).
- One study reported a motivational–behavioural skills protocol designed following principles of self‐efficacy theory ( López‐Jornet 2014 ).
- Six studies provided information tailored to the patients needs ( Bali 1999 ; Hugoson 2007 ; Jönsson 2009 ; Lepore 2011 ; Ramsay 2018 ; Weinstein 1996 ), one of which was with the addition of cognitive behavioural therapy ( Jönsson 2009 ), another including Social Cognitive Theory and Implementation Intention Theory ( Ramsay 2018 ) and another with the inclusion of positive social reinforcement ( Weinstein 1996 ).
- A negotiation and self‐selected goals method described as Client Self‐Care Commitment Model was reported in one study ( Jönsson 2006 ).
- A competency enhancing intervention in addition to standard autonomy‐supportive treatment was described in one study ( Münster Halvari 2012 ).
Member of dental team delivering intervention
It was unclear in three of the studies which member of the dental team carried out the intervention ( Bali 1999 ; López‐Jornet 2014 ; Weinstein 1996 ) but after reviewing the text the review authors were confident the intervention was undertaken by a member of the dental team. In the remainder of the studies the interventions were delivered by various members of the dental team.
- A hygienist delivered the intervention in eight of the studies ( Baab 1986 ; Hoogstraten 1983 ; Hugoson 2007 ; Jönsson 2006 ; Jönsson 2009 ; Münster Halvari 2012 ; Tedesco 1992 ; Van Leeuwen 2017 ).
- A dentist delivered the intervention in four studies ( Glavind 1985 ; Lepore 2011 ; Memarpour 2016 ; Schmalz 2018 ).
- A dentist or hygienist delivered the intervention in one study ( Ramsay 2018 ).
- A hygienist and dental nurse delivered the intervention in one study ( Söderholm 1982 ).
- A dental nurse delivered the intervention in one study ( Hetland 1982 ) and control OHA in another study ( Aljafari 2017 ).
- Further self‐administration of the intervention at home took place in one study ( Aljafari 2017 ).
Frequency of intervention
The frequency of the intervention varied with three studies reporting the intervention to be delivered on a one‐off basis ( Lepore 2011 ; Schmalz 2018 ; Van Leeuwen 2017 ).The remaining studies reported various intervention frequencies other than one study being unclear ( Hoogstraten 1983 ).
- Two studies reported two intervention visits ( Glavind 1985 ; Memarpour 2016 ).
- Two studies reported three intervention visits ( Hetland 1982 ; Jönsson 2006 ).
- Four studies reported four intervention visits ( Bali 1999 ; López‐Jornet 2014 ; Münster Halvari 2012 ; Tedesco 1992 ).
- Two studies reported five intervention visits ( Baab 1986 ; Söderholm 1982 ).
- One study reported three or six intervention visits ( Hugoson 2007 ).
One intervention was initially delivered in the clinic and then used at home as per the patients wishes ( Aljafari 2017 ), one study reported a median of nine intervention visits ( Jönsson 2009 ), and one reported reinforcement of OHA was provided at the discretion of the dentist/hygienist during the trial and recorded ( Ramsay 2018 ). The study by Weinstein 1996 varied in the frequency of intervention from three clinical visits with twice weekly phone call to periodontist to report self‐evaluated plaque score, 16 visits with OHA (twice weekly examinations by periodontist) or 16 visits with OHA (twice weekly examinations by periodontist) and daily completion of an oral hygiene task checklist.
Intensity of intervention
The intensity of the intervention was not reported in nine studies ( Baab 1986 ; Bali 1999 ; Jönsson 2006 ; Lepore 2011 ; Ramsay 2018 ; Schmalz 2018 ; Tedesco 1992 ; Weinstein 1996 ; Van Leeuwen 2017 ), two were largely administered at home ( Aljafari 2017 ; Glavind 1985 ), one remained unclear ( López‐Jornet 2014 ), and one varied between patients ( Jönsson 2009 ).
For those studies who did report the intensity of the intervention, the intensity varied considerably.
- Approximately 30 minutes to 40 minutes intervention noted in one study ( Hoogstraten 1983 ).
- Two intervention appointments of 30 minutes to 40 minutes each in one study ( Memarpour 2016 ).
- Forty‐five minutes for the first intervention visit, 30 minutes for the second intervention visit and 15 minutes for the third intervention visit in one study ( Hetland 1982 ).
- Approximately 45 minutes intervention was noted in one study ( Münster Halvari 2012 ).
- Between 120 minutes and 150 minutes was reported in two studies ( Hugoson 2007 ; Söderholm 1982 ).
Prophylaxis as part of intervention
Twelve studies reported some form of prophylactic measures at baseline ( Baab 1986 ; Glavind 1985 ; Hetland 1982 ; Hoogstraten 1983 ; Hugoson 2007 ; Jönsson 2006 ; Lepore 2011 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ). One study reported prophylactic measures throughout ( Jönsson 2009 ) and six did not report any prophylactic measures ( Aljafari 2017 ; Bali 1999 ; López‐Jornet 2014 ; Memarpour 2016 ; Van Leeuwen 2017 ; Weinstein 1996 ).
Characterictics of the outcomes
Primary outcomes ‐ clinical status, periodontal health.
Fifteen studies reported on the presence of gingivitis ( Baab 1986 ; Bali 1999 ; Glavind 1985 ; Hetland 1982 ; Hugoson 2007 ; Jönsson 2006 ; Jönsson 2009 ; Lepore 2011 ; López‐Jornet 2014 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ).
Of these studies:
- the gingival index by Löe and Sillness was used by seven studies ( Hetland 1982 ; Hugoson 2007 ; Jönsson 2006 ; Jönsson 2009 ; Münster Halvari 2012 ; Schmalz 2018 ; Tedesco 1992 );
- bleeding on probing was reported in five studies ( Baab 1986 ; Bali 1999 ; Glavind 1985 ; Ramsay 2018 ; Söderholm 1982 );
- gingival inflammation evaluated using the Papilla Bleeding Index (PBI) ( Lange 1977 ) was reported in one study ( Schmalz 2018 );
- one study ( Van Leeuwen 2017 ) reported that gingival health was assessed at six sites (mesio‐buccal, mid‐buccal, disto‐buccal, mesio‐lingual, mid‐lingual and disto‐lingual) around the selected quadrants by scoring bleeding on marginal probing (BOMP) on a scale of 0 to 2 (Lie 1998; Van der Weijden 1994);
- one study reported that gingival health was recorded but did not specify what scoring system was employed ( Lepore 2011 );
- one study reported a bleeding index was recorded but did not specify what scoring system was employed ( López‐Jornet 2014 ).
Probing depth
Four studies reported on probing depths ( Bali 1999 ; Jönsson 2006 ; Jönsson 2009 ; Ramsay 2018 ). One study reported on Community Periodontal Index of Treatment Needs (CPITN) score ( López‐Jornet 2014 ) with an additional study only reporting pocket depths of > 5 mm ( Söderholm 1982 ), and a further study only reporting on pocket depths > 4 mm ( Hetland 1982 ).
Plaque levels
Fifteen studies reported on plaque levels using various plaque indices ( Baab 1986 ; Bali 1999 ; Glavind 1985 ; Hetland 1982 ; Hugoson 2007 ; Jönsson 2006 ; Jönsson 2009 ; Lepore 2011 ; López‐Jornet 2014 ; Münster Halvari 2012 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ; Weinstein 1996 ).
- three studies ( Hugoson 2007 ; Münster Halvari 2012 ; Tedesco 1992 ) used the Löe and Sillness plaque index ( Löe 1963 ; Löe 1967 ) with a further two studies ( Jönsson 2006 ; Jönsson 2009 ) reporting the accumulation of plaque being recorded using Silness and Löe ( Silness 1964 );
- one study ( López‐Jornet 2014 ) reported a plaque extension index (PEI) following plaque disclosure using a 2% aqueous erythrosine solution. After rinsing once with water, plaque deposits were assessed using the Quigley and Hein index, modified by Turesky et al ( Turesky 1970 ), with scores from 0 to 5 with another study ( Van Leeuwen 2017 ) reporting a similar process by measuring plaque at six sites after disclosing with Mira‐2‐Ton® with scores also based on the modified Quigley and Hein (Quigley 1962) plaque index (QHPI) with a scale of 0 to 5. One study reported a similar method with plaque extension evaluated using the plaque index by Quigley and Hein (QHI) modified by Turesky et al after using a plaque disclosing agent (Mira‐2‐Ton®, Hager score 5 = plaque extending to the coronal third) in addition to recording the Marginal Plaque Index (MPI) by Deinzer et al to differentiate plaque extension at the gingival margin ( Deinzer 2014 ) ( Schmalz 2018 ). A further study also reported using the Turesky hygiene index ( Bali 1999 );
- two studies ( Baab 1986 ; Weinstein 1996 ) reported on presence or absence of disclosed plaque at the gingival margin ( O'Leary 1972 );
- two studies reported on the presence of disclosed plaque; one did not refer to a specific index ( Glavind 1985 ) and the other reported the percentage of tooth surfaces (mesial, buccal, distal and lingual) with plaque ( Söderholm 1982 );
- two studies reported that a plaque score was recorded but did not specify what scoring system was employed ( Hetland 1982 ; Lepore 2011 ).
Dental caries
Two studies reported on DMFT (number of decayed, missing or filled permanent teeth) ( Bali 1999 ; Hetland 1982 ). One study reported on dmft (number of decayed, missing or filled primary teeth) ( Memarpour 2016 ), and a further study reported on dental caries but appeared to use the terms DMFS (number of decayed, missing or filled permanent surfaces) and dmft interchangeably within the text of the primary paper ( Lepore 2011 ).
Secondary outcomes ‐ Patient‐centred factors
Patient‐reported behaviour changes.
Five studies reported on patient‐reported behaviour change regarding:
- time spent brushing and the number of oral hygiene aids used ( Baab 1986 );
- child's dietary habits, and the child's self‐reported snacking and toothbrushing practices ( Aljafari 2017 );
- oral health behaviour ( Ramsay 2018 );
- oral self‐care habits ( Jönsson 2006 );
- self‐reported brushing and flossing behaviours and self‐efficacy assessed via Oral Health Behavior Expectation Scale ( Tedesco 1992 ).
One of the studies specifically reported on patient‐reported health indices:
- the General Oral Health Assessment Index (GOHAI) and self‐rated oral health ( Jönsson 2009 ).
Patient satisfaction with advice provided
One study reported on patient satisfaction with provider of advice and patient satisfaction with advice format:
- parent and child satisfaction with their educational intervention ( Aljafari 2017 ).
Patient‐reported changes in knowledge, attitudes and quality of life
Five studies reported on patient‐reported changes in knowledge, attitudes and quality of life following provision of advice:
- child's dietary knowledge ( Aljafari 2017 );
- dental knowledge, attitude, behaviour, and fear of dental treatment ( Hoogstraten 1983 ; Jönsson 2009 );
- patient‐related dental quality of life and confidence in oral hygiene self‐efficacy ( Slade 1997 ) ( Ramsay 2018 );
- parents' knowledge and performance regarding oral health ( Memarpour 2016 );
- oral health‐related quality of life measure (OHQoL‐UK) ( Jönsson 2009 ).
One study used multiple psychological outcome measures including ( Münster Halvari 2012 ):
- autonomy orientation (Dental Care Autonomy Orientation Scale) adapted in the present study from the Exercise Causality Orientations Scale ( Rose 2001 ) and the General Causality Orientations Scale ( Deci 1985 );
- perceived autonomy support (6‐item version of the Health Care Climate Questionnaire ( Williams 1996 ));
- autonomous motivation for the dental project (Evaluation of Dental Project Scale ( Halvari 2006 ));
- autonomous motivation for dental home care (a 3‐item identified subscale of the Self‐Regulation for Dental Home Care Questionnaire ( Halvari 2012 ));
- perceived dental competence (Dental Coping Beliefs Scale ( Wolfe 1996 )) using the five items with the best factor loadings ( Halvari 2006 ) and two added items from a previous study ( Halvari 2010 );
- dental health behaviour assessed by a 4‐item formative composite scale ( Halvari 2010 ).
A further study ( Tedesco 1992 ) reported on the theory of reasoned action variables assessed via Theory of Reasoned Action Oral Health Scale ( Fishbein 1980 ).
Secondary outcome ‐ Economic factors
Only one study reported on economic net benefits of OHA ( Ramsay 2018 ).
No adverse events due to OHA were reported in the included trials.
Excluded studies
We excluded 84 studies from the review (see Characteristics of excluded studies ). Below is a summary of the reasons for excluding these studies (some studies were excluded for more than one reason).
- Thirty‐six studies did not take place in a dental setting.
- Eleven studies were not a randomised controlled trial.
- Nine studies the intervention was not delivered by a member of the dental team.
- Eight studies had less than 8 weeks follow‐up.
- Seven studies did not deliver the intervention on a one‐to‐one basis.
- Eleven studies had an additional intervention included in the intervention group but not the control group (e.g. fluoride application, prophylaxis, provision of an electric toothbrush).
- Three studies had no OHA provided or no OHA comparator.
- One study tested a model of behaviour only.
- One study compared manual versus powered toothbrushes.
- One study was not related to oral health education.
- In one study no pre‐treatment measures were completed.
Awaiting classification studies
The authors of two published trial protocols were contacted for further information but no reply was received ( Gao 2013 ; IRCT2014062618248N1 ).
Ongoing studies
The author of one ongoing trial confirmed that data collection was completed but data analysis was not complete at the current time ( ACTRN12605000607673 ).
Risk of bias in included studies
We assessed risk of bias based on the information reported in the included studies in the first instance. We subsequently contacted authors for further information for missing information or clarification. Two authors replied and provided information for two studies ( Aljafari 2017 ; Schmalz 2018 ).
We assessed nine studies to be at low risk of bias for this domain ( Aljafari 2017 ; Baab 1986 ; Hugoson 2007 ; Jönsson 2006 ; Jönsson 2009 ; López‐Jornet 2014 ; Memarpour 2016 ; Ramsay 2018 ; Van Leeuwen 2017 ). There were 10 studies that had insufficient information to make a judgement and we assessed them as at unclear risk of bias ( Bali 1999 ; Glavind 1985 ; Hetland 1982 ; Hoogstraten 1983 ; Lepore 2011 ; Münster Halvari 2012 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Weinstein 1996 ).
We assessed four studies to be at low risk of bias for this domain ( Aljafari 2017 ; Jönsson 2009 ; Ramsay 2018 ; Van Leeuwen 2017 ). None of the studies assessed were deemed to be at high risk of bias for this domain. There were 15 studies that had insufficient information to make a judgement and we assessed them as at unclear risk of bias ( Baab 1986 ; Bali 1999 ; Glavind 1985 ; Hetland 1982 ; Hoogstraten 1983 ; Hugoson 2007 ; Jönsson 2006 ; Lepore 2011 ; López‐Jornet 2014 ; Memarpour 2016 ; Münster Halvari 2012 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Weinstein 1996 ).
Blinding of participants and personnel (performance bias)
We assessed all 19 studies to be at unclear risk of bias for this domain ( Aljafari 2017 ; Baab 1986 ; Bali 1999 ; Glavind 1985 ; Hetland 1982 ; Hoogstraten 1983 ; Hugoson 2007 ; Jönsson 2006 ; Jönsson 2009 ; Lepore 2011 ; López‐Jornet 2014 ; Memarpour 2016 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ; Weinstein 1996 ). It is not possible to blind participants to this intervention and it is unclear the influence this would have on the risk of bias for this domain.
Blinding of outcome assessment (detection bias)
We assessed 13 studies to be at low risk of bias for this domain ( Aljafari 2017 ; Baab 1986 ; Hetland 1982 ; Hoogstraten 1983 ; Hugoson 2007 ; Jönsson 2006 ; Jönsson 2009 ; López‐Jornet 2014 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Söderholm 1982 ; Van Leeuwen 2017 ). There were six studies that had insufficient information to make a judgement and we assessed them as at unclear risk of bias ( Bali 1999 ; Glavind 1985 ; Lepore 2011 ; Memarpour 2016 ; Tedesco 1992 ; Weinstein 1996 ).
We assessed 11 studies to be at low risk of bias for this domain ( Glavind 1985 ; Jönsson 2006 ; Jönsson 2009 ; López‐Jornet 2014 ; Memarpour 2016 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ). We assessed two studies at high risk of bias for this domain ( Aljafari 2017 ; Bali 1999 ). There were six studies that had insufficient information to make a judgement and we assessed them as at unclear risk of bias ( Baab 1986 ; Hetland 1982 ; Hoogstraten 1983 ; Hugoson 2007 ; Lepore 2011 ; Weinstein 1996 ).
We assessed 16 studies to be at low risk of bias for this domain ( Aljafari 2017 ; Baab 1986 ; Glavind 1985 ; Hetland 1982 ; Hoogstraten 1983 ; Jönsson 2009 ; Lepore 2011 ; López‐Jornet 2014 ; Memarpour 2016 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ; Weinstein 1996 ). We assessed one study at high risk of bias for this domain ( Hugoson 2007 ). There were two studies that had insufficient information to make a judgement and we assessed them as at unclear risk of bias ( Bali 1999 ; Jönsson 2006 ).
Other potential sources of bias
We assessed 16 studies to be at low risk of bias for this domain ( Aljafari 2017 ; Bali 1999 ; Glavind 1985 ; Hetland 1982 ; Hugoson 2007 ; Jönsson 2006 ; Jönsson 2009 ; López‐Jornet 2014 ; Memarpour 2016 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ; Weinstein 1996 ). There were three studies that had insufficient information to make a judgement and we assessed them as at unclear risk of bias ( Baab 1986 ; Hoogstraten 1983 ; Lepore 2011 ).
Overall risk of bias
- We assessed none of the studies as being at low risk of bias.
- We assessed three studies as being at high risk of bias. These studies had at least one domain assessed as high risk of bias ( Aljafari 2017 ; Bali 1999 ; Hugoson 2007 ).
- We assessed 16 studies as being at unclear risk of bias. These studies had at least one domain judged to be at unclear risk of bias, but no domains judged to be at high risk of bias ( Baab 1986 ; Glavind 1985 ; Hetland 1982 ; Hoogstraten 1983 ; Jönsson 2006 ; Jönsson 2009 ; Lepore 2011 ; López‐Jornet 2014 ; Memarpour 2016 ; Münster Halvari 2012 ; Ramsay 2018 ; Schmalz 2018 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ; Weinstein 1996 ).
The results of the risk of bias assessments are presented graphically in Figure 2 and Figure 3 .

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Effects of interventions
See: Table 1 ; Table 2 ; Table 3 ; Table 4
Summary of findings for the main comparison
1 1 study at high risk and 1 at unclear risk of bias. 1 study small with contradictory results. Inconsistency between studies, unable to pool data. The number of appointments and intensity of the interventions would not be applicable in routine dental practice. Downgraded for risk of bias, inconsistency and indirectness. 2 1 study at high risk and 1 at unclear risk of bias. The number of appointments and intensity of the interventions would not be applicable in routine dental practice. Downgraded for risk of bias and indirectness. 3 2 unclear risk of bias studies. Inconsistency between studies, unable to pool data. The number of appointments and intensity of the interventions would not be applicable in routine dental practice. Downgraded for risk of bias and inconsistency and indirectness.
Summary of findings 2
1 4 unclear risk of bias studies. Inconsistency between studies, unable to pool data. Setting of 3 studies is secondary care, and intervention in 1 study (number of appointments and/or intensity required) is not applicable to routine dental practice. Downgraded for risk of bias, inconsistency and indirectness. 2 3 unclear risk of bias studies. Inconsistency between studies, unable to pool data. Setting of 3 studies is secondary care, and intervention in 1 study (number of appointments and/or intensity required) is not applicable to routine dental practice. Downgraded for risk of bias, inconsistency and indirectness. 3 1 unclear risk of bias study. No usable data. Setting not applicable to routine dental practice, so downgraded for indirectness.
Summary of findings 3
1 4 unclear risk of bias studies. Inconsistency between studies, unable to pool data. 3 studies were in secondary care and 3 of the interventions of 3 trials (number of appointments and/or intensity required) are not applicable to routine dental practice therefore we also downgraded for indirectness.
Summary of findings 4
1 1 study at high and 4 at unclear risk of bias. Unable to pool data. 2 of the included studies were in secondary care. Interventions of 4 trials (number of appointments and/or intensity) are not applicable in routine dental practice. Downgraded for risk of bias, inconsistency and indirectness. 2 1 study at high and 5 at unclear risk of bias. Unable to pool data. 2 of the included studies were in secondary care. Interventions of 5 trials (number of appointments and/or intensity) are not applicable in routine dental practice. Downgraded for risk of bias, inconsistency and indirectness. 3 1 high risk of bias study. Did not report usable data. Setting and intervention not applicable to routine dental care, therefore also downgraded for indirectness.
We have included 19 studies that investigated various forms and delivery methods of one‐to one oral hygiene advice (OHA) in a dental setting.
We have summarised data in additional tables, categorising trials to similar interventions groups where possible ( Table 5 ; Table 6 ; Table 7 ; Table 8 ).
CI = confidence interval; DMFT = number of decayed, missing or filled permanent teeth; GI = gingival index ( Löe 1963 ); MD = mean difference; n = number; OHA = oral hygiene advice; RR = risk ratio; SD = standard deviation.
CI = confidence interval; dmft = number of decayed, missing or filled primary teeth; GI = gingival index ( Löe 1963 ); MD = mean difference; modified QHI = Turesky Modified Quigley and Hein plaque index; n = number; OHA = oral hygiene advice; PI = plaque index ( Silness 1964 ); SD = standard deviation.
BOP = bleeding on probing; CI = confidence interval; DMFT = number of decayed, missing or filled permanent teeth; GI = gingival index ( Löe 1963 ); MD = mean difference; modified QHI = Turesky Modified Quigley and Hein plaque index; n = number; OHA = oral hygiene advice; O'Leary = disclosed plaque at the gingival margin ( O'Leary 1972 ); PI = plaque index ( Löe 1967 ); SD = standard deviation.
BOP = bleeding on probing; CI = confidence interval; GI = gingival index ( Löe 1963 ); MD = mean difference; modified QHPI = Quigley 1962 ; n = number; OHA = oral hygiene advice; PI = plaque index ( Löe 1967 ); SD = standard deviation.
Four studies compared any form of one‐to‐one OHA versus no OHA ( Hetland 1982 ; Hoogstraten 1983 ; Hugoson 2007 ; Memarpour 2016 ). Two of these studies reported outcomes of gingivitis and plaque levels ( Hetland 1982 ; Hugoson 2007 ). Two studies reported dental caries ( Hetland 1982 ; Memarpour 2016 ). The remaining study did not include clinical outcomes ( Hoogstraten 1983 ). Outcomes were reported up to 6 months in Hetland 1982 , 36 months in Hugoson 2007 , and 12 months in Hoogstraten 1983 and Memarpour 2016 .
The Hetland 1982 was a small study in adults that had contradictory results (very weak evidence) at 3 months and 6 months. There was a small difference favouring the control arm of no OHA at 3 months: mean difference (MD) 0.25, 95% confidence interval (CI) 0.05 to 0.45. At 6 months the small difference favoured the OHA intervention: MD ‐0.38, 95% CI ‐0.62 to ‐0.14.
The Hugoson 2007 study in adults showed very low‐quality evidence of a benefit for OHA at 12 months: MD ‐8.0, 95% CI ‐12.86 to ‐3.14; 24 months: MD ‐7.70, 95% CI ‐12.77 to ‐2.63; and 36 months: MD ‐9.10, 95% CI ‐14.03 to ‐4.17.
Both studies at all time points consistently showed low‐quality evidence of a benefit in plaque reduction for OHA. The Hetland 1982 showed a benefit of: MD ‐0.44, 95% CI ‐0.56 to ‐0.32 at 6 months; at 36 months the Hugoson 2007 study demonstrated a benefit of MD ‐13.10, 95% CI ‐19.97 to ‐6.23.
The Hetland 1982 study did not provide summary statistics or effect estimates, reporting only "small and statistically insignificant changes" between groups. The Memarpour 2016 study provided weak evidence of a benefit for OHA at 8 months: risk ratio (RR) 0.20, 95% CI 0.06 to 0.67; and 12 months: RR 0.14, 95% CI 0.05 to 0.39 (173 participants), but not at 4 months: RR 0.66, 95% CI 0.11 to 3.86. Overall, the evidence for dental caries was graded as very low‐quality evidence.
Four studies compared personalised OHA versus routine OHA ( Jönsson 2009 ; Lepore 2011 ; Ramsay 2018 ; Schmalz 2018 ). All four studies reported gingivitis as an outcome ( Jönsson 2009 ; Lepore 2011 ; Ramsay 2018 ; Schmalz 2018 ). Three of the studies that reported gingivitis also reported plaque levels as an outcome ( Jönsson 2009 ; Lepore 2011 ; Schmalz 2018 ). Only one of the studies reported dental caries ( Lepore 2011 ). Outcomes were reported up to 2 months ( Lepore 2011 ), 3 months ( Schmalz 2018 ), 12 months ( Jönsson 2009 ), and 36 months ( Ramsay 2018 ).
The large Ramsay 2018 study in adults showed little or no difference between groups at 36 months: MD ‐2.50, 95% CI ‐8.30 to 3.30.
The Jönsson 2009 study in adults showed weak evidence of a benefit for personalised OHA at 3 months: MD ‐0.25, 95% CI ‐0.31 to ‐0.19 and 12 months: MD ‐0.29, 95% CI ‐0.35 to ‐0.23.
The Lepore 2011 study in children reported "statistically significant (P < 0.05) improvement" for personalised OHA at 2 months but did not report usable data.
The Schmalz 2018 study showed little or no difference between groups at 3 months: MD ‐0.03, 95% CI ‐0.06 to 0.01.
Overall, the evidence for gingivitis was graded as very low‐quality evidence.
The Jönsson 2009 study in adults showed weak evidence of a benefit for personalised OHA at 3 months: MD ‐0.15, 95% CI ‐0.21 to ‐0.09 and 12 months: MD ‐0.17, 95% CI ‐0.22 to ‐0.12.
The Lepore 2011 study in children reported "statistically significant (P < 0.05) improvement" for personalised OHA but did not report usable data.
The Schmalz 2018 study showed little or no difference between groups at 3 months: MD ‐0.04, 95% CI ‐0.15 to 0.08.
Overall, the evidence for plaque levels was graded as very low‐quality evidence.
The Lepore 2011 study in children between the ages of 1 year and 6 years old reported "statistically significant (P < 0.05) improvement" for personalised OHA but did not report usable data. Overall, the evidence for dental caries was graded as very low‐quality evidence.
Five trials compared some form of self‐management with some form of professional OHA ( Aljafari 2017 ; Baab 1986 ; Glavind 1985 ; Jönsson 2006 ; López‐Jornet 2014 ). Four studies reported gingivitis and plaque levels ( Baab 1986 ; Glavind 1985 ; Jönsson 2006 ; López‐Jornet 2014 ). None of the studies reported dental caries. Outcomes were reported up to 2 months ( López‐Jornet 2014 ), 3 months ( Jönsson 2006 ), and 6 months ( Baab 1986 ; Glavind 1985 ).
The Baab 1986 study in adults reported "significant differences between groups at each observation were not found" but no usable data reported.
The Glavind 1985 study in adults reported "no statistically significant differences in gingival bleeding scores were found between the two treatment groups at any of the three examinations" but no usable data reported.
The Jönsson 2006 study in adults showed little or no difference between groups at 3 months: MD ‐0.01, 95 % CI ‐0.12 to 0.10.
The López‐Jornet 2014 study in adults with hyposalivation showed a benefit in gingivitis for professional OHA at 2 months: MD 12.30 95% CI 1.90 to 22.70.
Overall, the evidence for gingivitis was graded as very low quality.
The Baab 1986 study in adults reported "mean plaque scores did not differ significantly between groups" but no usable data reported.
The Glavind 1985 study in adults reported "no statistically significant differences were found between the two groups at any of the examination times" but no usable data reported.
The Jönsson 2006 study in adults showed a benefit in plaque reduction at 3 months for self‐management: MD ‐0.08, 95 % CI ‐0.15 to ‐0.01.
The López‐Jornet 2014 study in adults with hyposalivation showed a benefit in gingivitis for professional OHA at 2 months: MD ‐0.10 95% CI ‐0.18 to ‐0.02.
Overall, the evidence for plaque levels was graded as very low quality.
No studies were found that looked at dental caries.
Seven trials compared some form of enhanced OHA with some form of routine OHA ( Bali 1999 ; Hoogstraten 1983 ; Münster Halvari 2012 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ; Weinstein 1996 ). Five of the studies investigating enhanced OHA versus OHA reported gingivitis ( Bali 1999 ; Münster Halvari 2012 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ). Six of the studies investigating enhanced OHA versus routine OHA reported gingivitis ( Bali 1999 ; Münster Halvari 2012 ; Söderholm 1982 ; Tedesco 1992 ; Van Leeuwen 2017 ; Weinstein 1996 ). Only the Bali 1999 study reported dental caries. Outcomes were reported up to 2 months ( Weinstein 1996 ), 3 months ( Söderholm 1982 ), 5.5 months ( Münster Halvari 2012 ), 9 months ( Tedesco 1992 ), and 12 months ( Bali 1999 ; Hoogstraten 1983 ; Van Leeuwen 2017 ).
Two studies in adults did not report usable data ( Bali 1999 ; Tedesco 1992 ).
Three studies found little or no difference between groups across all time points ( Münster Halvari 2012 ; Söderholm 1982 ; Van Leeuwen 2017 ).
The Münster Halvari 2012 study showed low‐quality evidence of a benefit in reduction of gingivitis for enhanced OHA at 5.5 months: MD ‐0.32, 95% CI ‐0.36 to ‐0.28.
The Söderholm 1982 study reported little or no difference between groups at 3 months: MD 0.00, 95% CI ‐3.34 to 3.34.
The Van Leeuwen 2017 study reported little or no difference between groups at 12 months: MD ‐0.90, 95% CI ‐7.47 to 5.67.
Two studies ( Bali 1999 ; Tedesco 1992 ) in adults did not report usable data.
The Münster Halvari 2012 study in adults showed low‐quality evidence of a benefit in plaque reduction for enhanced OHA at 5.5 months: MD ‐0.39 95% CI ‐0.47 to ‐0.31.
The Söderholm 1982 study reported little or no difference between groups at 3 months: MD ‐2.90, 95% CI ‐11.56 to 5.76.
The Van Leeuwen 2017 study reported little or no difference between groups at all time points. The mean difference at 12 months was 0.03, 95% CI ‐0.12 to 0.18.
The Weinstein 1996 study included three intervention groups of enhanced OHA compared with the control OHA. Only one of the intervention groups (intervention group 3) showed a small benefit in plaque reduction at 2 months: MD ‐0.23, 95% CI ‐0.37 to ‐0.09.
The Bali 1999 study in adults investigated dental caries but did not report usable data.
Summary of main results
We have identified 19 studies suitable for inclusion to this review. A total of 4232 participants were recruited, with numbers included in each trial ranging from 33 to 1877. The member of the dental team delivering the oral hygiene advice (OHA) was a hygienist in eight studies, dentist in four studies, dental nurse in one study, dentist or hygienist in one study, dental nurse and hygienist in one study, and dental nurse OHA to the control group with further self‐administration of the intervention in one study. It was unclear in three of the studies which member of the dental team carried out the intervention.
Due to the heterogeneity of the studies with respect to participants, interventions, settings and outcome measures we were unable to pool the data. We summarised data by categorising similar interventions into comparison groups.
Four studies compared any form of one‐to‐one OHA versus no OHA and the results are summarised in Table 1 .
Two studies reported the outcome of gingivitis. Although one small study in adults had contradictory results at 3 months and 6 months, the other study in adults showed very low‐quality evidence of a benefit for OHA at all time points of 12 months, 24 months and 36 months.
Four studies compared personalised OHA versus routine OHA and the results are summarised in Table 2 .
Five trials compared some form of self‐management with some form of professional OHA and the results are summarised in Table 3 .
Seven trials compared some form of enhanced OHA with some form of routine OHA and the results are presented in Table 4 .
Overall completeness and applicability of evidence
Our search strategy was wide and retrieved 15,188 studies with a further two studies identified by handsearching. We identified 19 studies for inclusion having also handsearched the references from systematic reviews, reviews and those papers included. As such we are confident that the actions completed have resulted in a robust review of the evidence currently available. Furthermore, the evidence identified studies carried out in a number of dental settings, different countries, different age populations and healthy patients or those with specified medical or oral health conditions. In addition, there was a variety of dental care professionals who delivered a mixture of different interventions over a variety of time frames and frequencies. The sample size and length of follow‐up of included studies were also variable.
Regarding the applicability of the evidence, due to the heterogeneity of study design, study interventions and outcome measures it was not possible to carry out a meta‐analysis to determine if any specific intervention was more effective in maintaining or improving oral health, hygiene, behaviour, and attitudes compared to no advice or advice in a different format. There was also a dearth of high‐quality studies with low risk of bias. The majority of studies were carried out in secondary care, as such it may be difficult to extrapolate the evidence to the wider population as the majority of the general population access dental care in primary care. We also noted that the frequency and intensity of intervention varied significantly between studies with some reporting multiple intervention appointments, as many as median of nine ( Jönsson 2009 ), and up to 150 minutes intervention time. The follow‐up time was limited in most of the included studies. As such the applicability of the evidence is not largely generalisable.
The body of the evidence is very low quality as presented in Table 1 ; Table 2 ; Table 3 ; Table 4 .
Potential biases in the review process
The search strategy produced a large number of results with very few additional studies found via handsearching. However, while this process was deemed robust, it is possible that some small studies were not identified though we are confident that all larger studies were found.
We were not blinded to the names of authors, publications, institutions, etc. of studies at the time of reviewing which may have introduced bias to the review with conflict of interests declared in advance of the review process; the primary author had no conflict of interest and those who did declare conflicts of interest were not involved in reviewing any of the related data (i.e. the IQuaD Study ( Ramsay 2018 )).
Agreements and disagreements with other studies or reviews
In agreement with our review, a number of previous reviews have noted the variety of oral health promotion interventions investigated and the resultant heterogeneity in studies ( Kay 2016a ; Kay 2016b ; Watt 2005 ; Yevlahova 2009 ). Furthermore, due to the variable quality of studies and findings, it is not possible to estimate the intervention effect ( Watt 2005 ). As a result, direct comparisons between studies is difficult due to the lack of standardised and validated outcome measurement tools ( Kay 1998 ).
As previously stated, due to the variety of different outcomes and outcome measures used there is difficulty in assessing and summarizing the effect of interventions on plaque levels ( Watt 2005 ). Watt et al also commented that in the short term, i.e. up to 6 months‐post intervention, substantial reductions in plaque reduction can be expected following educational interventions but longer term studies are limited in number, so whether or not such short‐term improvements are maintained is impossible to determine ( Watt 2005 ) which has been echoed by others ( Kay 2016b ).
The systematic review by Kay et al, which focused on oral health promotion activities that could be delivered in the context of general dental practice, aimed to change individual's knowledge, attitudes or behaviours in order to influence their oral health, also noted that the quality of the studies were very variable. Furthermore, the authors similarly noted that "the outcome measures used to assess knowledge, behaviour and attitudes were ad‐hoc measures and therefore only very rarely allowed direct comparisons between studies and entirely obviated the possibility of meta‐analysing the data. Direct comparison between studies and/or meta‐analysis would have only been possible for studies that measured the same clinical outcomes, and then only if the interventions had been the same. This required level of similarity between studies was not reached" ( Kay 2016b ). The authors note that this is similar to a previous publication by the same authors ( Kay 2016a ).
One review concluded that there was evidence to show that motivational interviewing "may be useful in the dental surgery setting and this application should be researched further" ( Kay 2016b ). The current systematic review only found two studies suitable for inclusion on this topic ( López‐Jornet 2014 ; Münster Halvari 2012 ) and we did not think the available evidence allowed adequate comparisons.
Regarding previous review findings regarding OHA and dental caries prevention, Kay et al reported that "there is still no evidence that caries can be prevented by oral health promotion although this apparent lack of effect may be due, in part, to the short follow‐up (< 3 years) in the majority of studies" ( Kay 2016a ).
Implications for practice
There was insufficient high‐quality evidence to recommend any specific one‐to‐one oral hygiene advice (OHA) method as being effective in improving oral health or being more effective than any other method.
Implications for research
The quality of study reporting was variable with the use of CONSORT recommended for future studies (www.consort‐statement.org).
Many of the studies did not make the exact nature of the OHA intervention entirely clear; more detailed description of intervention(s) following the 'Criteria for Reporting the Development and Evaluation of Complex Interventions in health care: revised guideline (CReDECI 2)' ( Möhler 2015 ) would be of benefit to facilitate easier comparison.
Researchers conducting future studies should ensure that methods of randomisation are adequate and clearly reported along with ensuring allocation concealment, appropriate blinding and sample size determined at design stage. In addition, appropriate and validated patient‐centred outcome measures should be included in future studies along with the need to determine the cost effectiveness of interventions.
The vast majority of the studies had a short follow‐up; longer follow‐up periods would be beneficial to determine longer term effects of one‐to‐one OHA.
Given the vast majority of dental care is provided in a primary care environment, future studies within this environment that take into account the likely time and financial limitations such an environment are likely to impose (e.g. frequency and intensity of intervention), would be advantageous to allow future research to be applicable to the wider population with such interventions needing to be both clinically and financially effective and efficient.
Acknowledgements
We would like to extend our thanks to Anne Littlewood for completion of searches, and Luisa M Fernandez Mauleffinch for her editorial assistance and copy editing. We would also like to thank Anette Blümle, Dominic Lamont and Falk Schwendicke for their assistance with translation. Also, thanks to Craig Ramsay and Anne Marie Glenny for advice on thematic considerations, and Helen Worthington, Philip Riley, Paul Brocklehurst and Derek Richards for peer review comments.
Appendix 1. Cochrane Oral Health's Trials Register search strategy
From October 2012, searches were undertaken on Cochrane Register of Studies using the following search strategy: #1 ("dental health education" or "health promotion":TI,AB) AND (INREGISTER) #2 (("oral health" AND (instruct* or advice or advise* or educat* or teach* or train* or demonstrat* or supervis*)):TI,AB) AND (INREGISTER) #3 (("oral health" AND (behavior* or behaviour* or "patient compliance" or motivat*) AND (change OR changed OR changing or modify OR modified OR modification)) :TI,AB) AND (INREGISTER) #4 (attitude* AND "oral health") or (attitude AND "oral care") or (attitude AND "dental health") or (attitude AND "mouth hygiene") or (attitude AND "oral hygiene"):TI,AB) AND (INREGISTER) #5 (#1 or #2 or #3 or #4) AND (INREGISTER) Previous to October 2012, searches of the trials register were done using Procite software, using the following search strategy:
("dental health education" or "Health promotion" or ("oral health" AND (instruct* or advice or advise* or educat* or teach* or train* or demonstrat* or supervis*)) or behavior* or behaviour* or "patient compliance" or motivat* or ((behavior* OR behaviour*) AND (change OR changed OR changing or modify OR modified OR modification)) or "feedback device*" or "feed‐back device*" or (attitude* AND "oral health") or (attitude AND "oral care") or (attitude AND "dental health") or (attitude AND "mouth hygiene") or (attitude AND "oral hygiene"))
Appendix 2. Cochrane Central Register of Controlled Clinical Trials (CENTRAL) search strategy
#1 ORAL HEALTH/ #2 Exp STOMATOGNATHIC DISEASES/ #3 Exp HALITOSIS #4 ((dental or tooth or teeth or enamel or root*) AND (decay* or caries or carious or white next spot* or plaque or reminerali* or deminerali*)) #5 (periodont* or gingivitis or (gingiva* next inflamm*) or (gingiva* next bleed*) or (gingival next pocket*) or (periodont* next pocket*) or (periodont* near attachment) or (gingiva* near attachment) #6 stomatitis or (mouth next ulcer*) or (oral next ulcer*) or (oral next candidi*) or (aphthous next ulcer*) or (mouth near aphthae) or (oral near aphthae) or (mucositis near oral) or (mucositis near mouth) or xerostomi* #7 (oral next health) or (dental next health) or orthodontic* #8 ("tooth wear" or ((tooth or dental or teeth or enamel) and (erosion or abrasion))) #9 (halitosis or (mouth next odour*) or (mouth next odor*) or (mouth next malodour*) or (mouth next malodor*) or (oral next malodour) OR (oral next malodour) or (breath near malodour*) or (breath near odour*) or (breath near odor*)) #10 (bottle next caries) or (nursing next caries) or (bottle next decay*) or ((early next childhood) and (caries or decay*)) #11 MOUTH NEOPLASMS/ #12 (oral next cancer*) or ((gingival or mouth or lip* or tongue or (salivary next gland) or palatal or parotid or sublingual or submandibular) AND (cancer* or carcinoma* or neoplasm* or tumour* or tumor*)) #13 leukoplaki* #14 hairy next tongue #15 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 #16 Exp ORAL HYGIENE/ #17 Exp MOUTHWASHES/ #18 Exp DENTIFRICES/ #19 (oral next hygiene) or (mouth near care) or (dental near care) or (care near teeth) or (mouth next hygiene) or (plaque near control*) or (plaque near remov*) #20 toothbrush* or tooth‐brush* or toothpaste* or dentifrice* or mouthwash* or mouth‐wash* or mouthrinse* or mouth‐rinse* or fluoride* #21 ((interdental next clean*) or (inter‐dental next clean*) or (tooth near clean*) or (teeth near clean*) or (denture* near hygiene) or (denture* near clean*) or (tongue next scrap*) or (tongue next brush*) or (chewing next stick*) or (chewing next gum*) or (orthodontic next appliance near clean*)) #22 (chewing‐gum or sugar‐free next gum) #23 ((dental or tooth or teeth or interdental* or inter‐dental*) and floss*) #24 ((dental next plaque next index) or (dental next plaque next indices) or (DMF* next index) or (DMF next indices) or (dmf* next index) or (dmf* next indices) or (periodontal next index) or (periodontal next indices) or (oral next hygiene next index) or (oral next hygiene indices) or (gingival next index)) #25 #16 or #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 or #24 #26 Exp HEALTH EDUCATION DENTAL #27 Exp HEALTH PROMOTION #28 instruct* or advice or advise* or educat* or teach* or train* #29 (((health* near promot*)) and (dental or teeth or mouth or periodont* or gingival* or (oral next health))) #30 ((demonstrat* near toothbrush*) or (demonstrat* near "tooth brush*") or (demonstrat* near tooth‐brush*) or (demonstrat* near floss*) or (demonstrat*near "oral hygiene*") or (demonstrat* near "interdental cleaning") or (demonstrat* near wood‐stick*) or (demonstrat* near "wood stick*") or (demonstrat* near "interdental massag*")) #31 ((supervis* near toothbrush*) or (supervis* near floss*) or (supervis* near "oral hygiene") or (supervis* near "interdental cleaning") or (supervis* near wood‐stick*) or (supervis* near "wood stick*") or (supervis* near "interdental massag*")) #32 #26 or #27 or #28 or #29 or #30 or #31 #33 HEALTH BEHAVIOR/ #34 PATIENT COMPLIANCE/ #35 ADOLESCENT BEHAVIOR/ #36 MOTIVATION/ #37 ((behavior* OR behaviour*) AND (change OR changed OR changing or modify OR modified OR modification)) #38 “feed back device*” or “feedback device*” #39 (attitude* near (oral next health)) or (attitude near (oral next care)) or (attitude near (dental next health)) or (attitude near “mouth hygiene”) or (attitude near “oral hygiene”) #40 (((oral next hygiene) near improv*) or (“oral health” near improv*) or ("gingival health" near improv*) or ("periodontal health" near improv*) or ("periodontal condition" near improv*) or (caries near reduc*)) #41 #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 #42 ((#15 OR #25) AND (#32 OR #41))
Appendix 3. MEDLINE Ovid search strategy
1. ORAL HEALTH/ 2. exp Stomatognathic Diseases/ 3. exp HALITOSIS/ 4. ((dental or tooth or teeth or enamel or root$) and (decay$ or caries or carious or white spot$ or plaque or reminerali$ or deminerali$)).mp. 5. (periodont$ or gingivitis or "gingival$ inflamm$" or "gingival$ bleed$" or "gingival pocket$" or "periodont$ pocket$" or (periodont$ adj3 attachment) or (gingival$ adj3 attachment)).mp. 6. (stomatitis or "mouth ulcer$" or "oral ulcer$" or "oral candidi$" or "aphthous ulcer$" or (mouth adj3 aphthae) or (oral adj3 aphthae) or (mucositis adj3 oral) or (mucositis adj3 mouth)).mp. 7. ("oral health" or "dental health" or orthodontic$).mp. 8. ("tooth wear" or ((tooth or dental or teeth or enamel) and (erosion or abrasion))).mp. 9. (halitosis or "mouth odour$" or "mouth odor$" or "mouth malodour$" or "mouth malodor$" or "oral malodour$" or "oral malodour" or (breath adj3 malodour$) or (breath adj3 odour$) or (breath adj3 odor$)).mp. 10. (("bottle caries" or "nursing caries" or "bottle decay$" or "early childhood") and (caries or decay$)).mp. 11. exp Mouth Neoplasms/ 12. (("oral cancer$" or ((gingival or mouth or lip$ or tongue or salivary) adj (gland or palatal or parotid or sublingual or submandibular))) and (cancer$ or carcinoma$ or neoplasm$ or tumour$ or tumor$)).mp. 13. leukoplaki$.mp. 14. hairy tongue.mp. 15. or/1‐14 16. exp ORAL HYGIENE/ 17. exp MOUTHWASHES/ 18. exp DENTIFRICES/ 19. ("oral hygiene" or (mouth adj3 care) or (dental adj3 care) or (care adj3 teeth) or (mouth adj3 hygiene) or (plaque adj4 control$) or (plaque adj4 remov$)).mp. 20. (toothbrush$ or tooth‐brush$ or toothpaste$ or dentifrice$ or mouthwash$ or mouth‐wash$ or mouthrinse$ or mouth‐rinse$ or fluoride$).mp. 21. ("interdental clean$" or "inter‐dental clean$" or (tooth adj4 clean$) or (teeth adj4 clean$) or (denture$ adj4 hygiene) or (denture$ adj4 clean$) or "tongue scrap$" or (tongue adj3 brush$) or "chewing stick$" or "chewing gum$" or ("orthodontic appliance$" adj3 clean$)).mp. 22. (chewing‐gum or "sugar‐free gum").mp. 23. ((dental or tooth or teeth or interdental$ or inter‐dental$) and floss$).mp. 24. ("dental plaque index" or "dental plaque indices" or "DMF? index" or "DMF? indices" or "periodontal index" or "periodontal indices" or "oral hygiene index" or "oral hygiene indices" or "gingival index").mp. 25. or/16‐24 26. Health Education, Dental/ 27. exp Health Promotion/ 28. (instruct$ or advice or advise$ or educat$ or teach$ or train$).mp. 29. ((health$ adj3 promot$) and (dental or teeth or mouth or periodont$ or gingival$ or "oral health")).mp. 30. ((demonstrate$ adj4 toothbrush$) or (demonstrate$ adj4 "tooth brush$") or (demonstrat$ adj3 tooth‐brush$) or (demonstrate$ adj3 floss$) or (demonstrate$ adj3 "oral hygiene$") or (demonstrat$ adj3 "interdental cleaning") or (demonstrate$ adj3 wood‐stick$) or (demonstrate$ adj3 "wood stick$") or (demonstrate$ adj3 "interdental massage$")).mp. 31. ((supervise$ adj3 toothbrush$) or (supervise$ adj3 floss$) or (supervise$ adj3 "oral hygiene") or (supervise$ adj3 "interdental cleaning") or (supervise$ adj3 wood‐stick$) or (supervise$ adj3 "wood stick$") or (supervise$ adj3 "interdental massage$")).mp. 32. or/26‐31 33. HEALTH BEHAVIOR/ 34. PATIENT COMPLIANCE/ 35. ADOLESCENT BEHAVIOR/ 36. MOTIVATION/ 37. ((behavior$ or behaviour$) and (change or changed or changing or modify or modified or modification)).mp. 38. ("feed back device$" or "feedback device$").mp. 39. ((attitude$ adj3 "oral health") or (attitude adj3 "oral care") or (attitude adj3 "dental health") or (attitude adj3 "mouth hygiene") or (attitude adj3 "oral hygiene")).mp. 40. (("oral hygiene" adj3 improv$) or ("oral health" adj3 improv$) or ("gingival health" adj3 improv$) or ("periodontal health" adj3 improv$) or ("periodontal condition" adj3 improv$) or (caries adj3 reduc$)).mp. 41. or/33‐40 42. (15 or 25) and (32 or 41)
This subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials (RCTs) in MEDLINE: sensitivity‐maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) ( Lefebvre 2011 ).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. Embase Ovid search strategy
1 “oral health” 2 Exp MOUTH DISEASE/ 3 HALITOSIS/ 4 ((dental or tooth or teeth or enamel or root$) AND (decay$ or caries or carious or “white spot$” or plaque or reminerali$ or deminerali$)) 5 (periodont$ or gingivitis or “gingival$ inflamm$” or “gingival$ bleed$” or “gingival pocket$ or “periodont$ pocket$ or (periodont$ adj3 attachment) or (gingival$ adj3 attachment)) 6 stomatitis or “mouth ulcer$ or “oral ulcer$ or “oral candidi$ or “aphthous ulcer$” or (mouth adj3 aphthae) or (oral adj3 aphthae) or (mucositis adj3 oral) or (mucositis adj3 mouth) or xerostomi$ 7 “oral health” or “dental health” or orthodontic$ 8 ("tooth wear" or ((tooth or dental or teeth or enamel) and (erosion or abrasion))) 9 (halitosis or “mouth odour$” or “mouth odor$” or “mouth malodour$ or “mouth malodor$ or “oral malodour$” OR “oral malodour” or (breath adj3 malodour$) or (breath adj3 odour$) or (breath adj3 odor$)) 10 “bottle caries” or “nursing caries” or “bottle decay$” or (“early childhood”) and (caries or decay$)) 11 MOUTH TUMOR/ 12 (((oral next cancer$) or (gingival or mouth or lip$ or tongue or (salivary next gland) or palatal or parotid or sublingual or submandibular) AND (cancer$ or carcinoma$ or neoplasm$ or tumour$ or tumor$)) 13 leukoplaki$ 14 “hairy tongue” 15 OR/1‐14 16 “Mouth hygiene” 17 mouthwash$ 18 TOOTHPASTE/ 19 “oral hygiene” or (mouth adj3 care) or (dental adj3 care) or (care adj3 teeth) or (mouth adj3 hygiene) or (plaque adj4 control$) or (plaque adj4 remov$) 20 toothbrush$ or tooth‐brush$ or toothpaste$ or dentifrice$ or mouthwash$ or mouth wash$ or mouthrinse$ or mouth‐rinse$ or fluoride$ 21 (“interdental clean$” or “inter‐dental clean$ or (tooth adj4 clean$) or (teeth adj4 clean$) or (denture$ near hygiene) or (denture$ adj4 clean$) or “tongue scrap$” or (tongue adj3 brush$) or “chewing stick$” or “chewing gum$” or (“orthodontic appliance$” adj3 clean$)) 22 (chewing‐gum or sugar‐free next gum) 23 ((dental or tooth or teeth or interdental$ or inter‐dental$) and floss$) 24 (“dental plaque index” or “dental plaque indices” or “DMF$ index” or “DMF indices” or “dmf* index” or “dmf4 indices” or “periodontal index” or “periodontal indices” or “oral hygiene index” or (“oral hygiene indices”) or “gingival index”)) 25 OR/16‐24 26 DENTAL HEALTH EDUCATION/ 27 HEALTH PROMOTION/ 28 instruct$ or advice or advise$ or educat$ or teach$ or train$ 29 (((health$ adj3 promot$)) and (dental or teeth or mouth or periodont$ or gingival$ or “oral health”)) 30 ((demonstrate$ adj4 toothbrush$) or (demonstrate$ "tooth brush$") or (demonstrat$ adj3 tooth‐brush$) or (demonstrate$ adj3 floss$) or (demonstrate$ adj3 "oral hygiene$") or (demonstrat$ adj3 "interdental cleaning") or (demonstrate$ adj3 woodstick$) or (demonstrate$ adj3 "wood stick$") or (demonstrate$ near "interdental massage$")) 31 ((supervise$ adj3 toothbrush$) or (supervise$ adj3 floss$) or (supervise$ adj3 "oral hygiene") or (supervise$ adj3 "interdental cleaning") or (supervise$ adj3 wood‐stick$) or (supervise$ adj3 "wood stick$") or (supervise$ adj3 "interdental massage$")) 32 OR/26‐31 33 HEALTH BEHAVIOR/ 34 PATIENT COMPLIANCE/ 35 (adolescen$ adj3 (behavior or behaviour)) 36 MOTIVATION/ 37 ((behavior$ OR behaviour$) AND (change OR changed OR changing or modify OR modified OR modification)) 38 “feed back device$” or “feedback device$” 39 ((attitude$ adj3 “oral health”) or (attitude adj3 “oral care”) or (attitude adj3 “dental health”) or (attitude adj3 “mouth hygiene”) or (attitude adj3 “oral hygiene”) 40 ((“oral hygiene” adj3 improv$) or (“oral health” adj3 improv$) or ("gingival health" adj3 improv$) or ("periodontal health" adj3 improv$) or ("periodontal condition" adj3 improv$) or (caries adj3 reduc$)) 41 OR/33‐40 42 ((15 OR 25) AND (32 OR 41))
This subject search was linked to an adapted version of the Cochrane Centralised Search Project filter for identifying RCTs in Embase Ovid (see www.cochranelibrary.com/help/central‐creation‐details.html for information).
1. Randomized controlled trial/ 2. Controlled clinical study/ 3. Random$.ti,ab. 4. randomization/ 5. intermethod comparison/ 6. placebo.ti,ab. 7. (compare or compared or comparison).ti. 8. ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 9. (open adj label).ti,ab. 10. ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 11. double blind procedure/ 12. parallel group$1.ti,ab. 13. (crossover or cross over).ti,ab. 14. ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 15. (assigned or allocated).ti,ab. 16. (controlled adj7 (study or design or trial)).ti,ab. 17. (volunteer or volunteers).ti,ab. 18. trial.ti. 19. or/1‐18 20. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 21. 19 not 20
Appendix 5. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) search strategy
oral hygiene and advice oral hygiene and promotion
Appendix 6. World Health Organization International Clinical Trials Registry Platform search strategy
"oral hygiene" and advice "oral health" and advice "oral hygiene" and promotion "oral health" and promotion
Characteristics of studies
Characteristics of included studies [ordered by study id].
BOMP = bleeding on marginal probing; DH = dental hygienist; DMFS = number of decayed, missing or filled permanent surfaces; dmft = number of decayed, missing or filled primary teeth; DMFT = number of decayed, missing or filled permanent teeth; GA = general anaesthesia; ITT = intention to treat; OH = oral hygiene; OHA = oral hygiene advice; ppm = parts per million; PSR/PSI = periodontal screening; RCT = randomised controlled trial; SD = standard deviation; SE = standard error.
Characteristics of excluded studies [ordered by study ID]
Characteristics of studies awaiting assessment [ordered by study id], characteristics of ongoing studies [ordered by study id], differences between protocol and review.
We made the following amendments to the review.
- Controlled clinical trials were not included as per Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 ( Higgins 2011 ).
- Objective changed from 'To determine the benefits and harms of one‐to‐one oral hygiene ...' to 'To assess the effects of one‐to‐one oral hygiene...'.
- Oral infection removed from primary outcome clinical status factors.
- Periodontal health primary outcome clinical status factor to include plaque levels.
- Secondary outcomes patient‐centred factors compressed to:
- patient‐reported behaviour changes (e.g. toothbrushing/flossing/mouthwash use),
- patient satisfaction with advice provided,
- patient‐reported changes in knowledge, attitudes and quality of life.
- Additional databases searched:
- ClinicalTrials.gov (to November 2017),
- World Health Organization International Clinical Trials Registry Platform (to November 2017).
- Quality assessment completed as per Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 ( Higgins 2011 ).
- Data analysis guided by the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 ( Higgins 2011 ).
Contributions of authors
Janet E Clarkson (JC) conceived the idea for the review. JC, Francesca A Soldani (FS), Linda Young (LY), Kate Jones (KJ), and Tanya Walsh (TW) wrote the protocol. JC, FS, LY, KJ and Thomas Lamont (TL) designed the final review. FS co‐ordinated the review. FS, TL, KJ and LY screened abstracts. FS, TL, Rizwana Lala (RL) and KJ carried out data extraction. TL and FS compiled the characteristics of included studies tables. FS, TL, RL and KJ assessed the risk of bias for the included studies. TW provided statistical data advice. TL, FS and KJ drafted the background section. FS and TL drafted the body of the review. TW, KJ, RL, LY and JC commented on and edited the draft review.
Sources of support
Internal sources.
- No sources of support supplied
External sources
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oralhealth.cochrane.org/partnerships‐alliances). Contributors over the past year have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and the Swiss Society for Endodontology, Switzerland.
Declarations of interest
Janet E Clarkson, Linda Young and Thomas Lamont were all authors of Ramsay 2018 . They were not involved in the data extraction or risk of bias assessment of this trial. Janet E Clarkson is also Co‐ordinating Editor of Cochrane Oral Health. Francesca A Soldani: none known. Kate Jones: none known. Tanya Walsh: none known. Tanya Walsh is an Editor with Cochrane Oral Health. Rizwana Lala: none known.
References to studies included in this review
Aljafari 2017 {published and unpublished data}.
- Aljafari A, Gallagher JE, Hosey MT. Can oral health education be delivered to high‐caries‐risk children and their parents using a computer game? – A randomised controlled trial . International Journal of Paediatric Dentistry 2017; 27 ( 6 ):476‐85. [DOI: 10.1111/ipd.12286] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aljafari A, Rice C, Gallagher JE, Hosey MT. An oral health education video game for high caries risk children: study protocol for a randomized controlled trial . Trials 2015; 16 :237. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Baab 1986 {published data only}
- Baab D, Weinstein P. Longitudinal evaluation of a self‐inspection plaque index in periodontal recall patients . Journal of Clinical Periodontology 1986; 13 ( 4 ):313‐8. [ PubMed ] [ Google Scholar ]
Bali 1999 {published data only}
- Bali C, Gurdet C, Hauer G, Handler I, Fischer R. Evaluation of the effect of professional dental cleaning and education in dental hygiene in type 1 diabetic patients . Acta Medica Austriaca 1999; 26 ( 5 ):159‐62. [ PubMed ] [ Google Scholar ]
Glavind 1985 {published data only}
- Glavind L, Christensen H, Pedersen E, Rosendahl H, Attström R. Oral hygiene instruction in general dental practice by means of self‐teaching manuals . Journal of Clinical Periodontology 1985; 12 ( 1 ):27‐34. [ PubMed ] [ Google Scholar ]
Hetland 1982 {published data only}
- Hetland L, Midtun N, Kristoffersen T. Effect of oral hygiene instructions given by paraprofessional personnel . Community Dentistry and Oral Epidemiology 1982; 10 ( 1 ):8‐14. [ PubMed ] [ Google Scholar ]
Hoogstraten 1983 {published data only}
- Hoogstraten J, Moltzer G. Effects of dental health care instruction on knowledge, attitude, behavior and fear . Community Dentistry and Oral Epidemiology 1983; 11 ( 5 ):278‐82. [ PubMed ] [ Google Scholar ]
Hugoson 2007 {published data only}
- Hugoson A, Lundgren D, Asklöw B, Borgklint G. Effect of three different dental health preventive programmes on young adult individuals: a randomized, blinded, parallel group, controlled evaluation of oral hygiene behaviour on plaque and gingivitis . Journal of Clinical Periodontology 2007; 34 ( 5 ):407‐15. [ PubMed ] [ Google Scholar ]
- Hugoson A, Lundgren D, Asklöw B, Borgklint G. The effect of different dental health programmes on young adult individuals. A longitudinal evaluation of knowledge and behaviour including cost aspects . Swedish Dental Journal 2003; 27 ( 3 ):115‐30. [ PubMed ] [ Google Scholar ]
Jönsson 2006 {published data only}
- Jönsson B, Lindberg P, Oscarson N, Ohrn K. Improved compliance and self‐care in patients with periodontitis ‐ a randomized control trial . International Journal of Dental Hygiene 2006; 4 ( 2 ):77‐83. [DOI: 10.1111/j.1601-5037.2006.00175.x] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Jönsson 2009 {published data only}
- Jönsson B, Ohrn K. Evaluation of the effect of non‐surgical periodontal treatment on oral health‐related quality of life: estimation of minimal important differences 1 year after treatment . Journal of Clinical Periodontology 2014; 41 ( 3 ):275‐82. [ PubMed ] [ Google Scholar ]
- Jönsson B, Ohrn K, Lindberg P, Oscarson N. Cost‐effectiveness of an individually tailored oral health educational programme based on cognitive behavioural strategies in non‐surgical periodontal treatment . Journal of Clinical Periodontology 2012; 39 ( 7 ):659‐65. [DOI: 10.1111/j.1600-051X.2012.01898.x] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jönsson B, Ohrn K, Lindberg P, Oscarson N. Evaluation of an individually tailored oral health educational programme on periodontal health . Journal of Clinical Periodontology 2010; 37 ( 10 ):912‐9. [DOI: 10.1111/j.1600-051X.2010.01590.x] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jönsson B, Ohrn K, Oscarson N, Lindberg P. The effectiveness of an individually tailored oral health educational programme on oral hygiene behaviour in patients with periodontal disease: a blinded randomized‐controlled clinical trial (one‐year follow‐up) . Journal of Clinical Periodontology 2009; 36 ( 12 ):1025‐34. [DOI: 10.1111/j.1600-051X.2009.01453.x] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Lepore 2011 {published data only}
- Lepore LM, Yoon RK, Chinn CH, Chussid S. Evaluation of behavior change goal‐setting action plan on oral health activity and status . New York State Dental Journal 2011; 77 ( 6 ):43‐7. [PUBMED: 22338818] [ PubMed ] [ Google Scholar ]
López‐Jornet 2014 {published data only}
- López‐Jornet P, Fabio CA, Consuelo RA, Paz AM. Effectiveness of a motivational–behavioural skills protocol for oral hygiene among patients with hyposalivation . Gerodontology 2014; 31 ( 4 ):288–95. [DOI: 10.1111/ger.12037] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Memarpour 2016 {published data only}
- Memarpour M, Dadaein S, Fakhraei E, Vossoughi M. Comparison of oral health education and fluoride varnish to prevent early childhood caries: a randomized clinical trial . Caries Research 2016; 50 ( 5 ):433–42. [DOI: 10.1159/000446877] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Münster Halvari 2012 {published data only}
- Münster Halvari AE, Halvari H, Bjørnebekk G, Deci EL. Self‐determined motivational predictors of increases in dental behaviors, decreases in dental plaque, and improvement in oral health: a randomized clinical trial . Health Psychology 2012; 31 ( 6 ):777‐88. [DOI: 10.1037/a0027062] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Ramsay 2018 {published data only}
- Ramsay CR, Clarkson JE, Duncan A, Lamont TJ, Heasman PA, Boyers D, et al. Improving the Quality of Dentistry (IQuaD): a cluster factorial randomised controlled trial comparing the effectiveness and cost‐benefit of oral hygiene advice and/or periodontal instrumentation with routine care for the prevention and management of periodontal disease in dentate adults attending dental primary care . Health Technology Assessment 2018; 22 ( 38 ):1‐144. [DOI: 10.3310/hta22380] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Schmalz 2018 {published data only}
- Schmalz G, Kiehl K, Schmickler J, Rinke S, Schmidt J, Krause F, et al. No difference between manual and different power toothbrushes with and without specific instructions in young, oral healthy adults ‐ results of a randomized clinical trial . Clinical Oral Investigations 2018; 22 ( 3 ):1147‐55. [DOI: 10.1007/s00784-017-2200-5] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Söderholm 1982 {published data only}
- Söderholm G, Nobréus N, Attström R, Egelberg J. Teaching plaque control. I. A five‐visit versus a two‐visit program . Journal of Clinical Periodontology 1982; 9 ( 3 ):203‐13. [PUBMED: 6954162] [ PubMed ] [ Google Scholar ]
Tedesco 1992 {published data only}
- Tedesco LA, Keffer MA, Davis EL, Christersson LA. Effect of a social cognitive intervention on oral health status, behavior reports, and cognitions . Journal of Periodontology 1992; 63 ( 7 ):567‐75. [DOI: 10.1902/jop.1992.63.7.567] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Van Leeuwen 2017 {published data only}
- Leeuwen M, Rosema N, Versteeg PA, Slot DE, Hennequin‐Hoenderdos NL, Weijden GA. Effectiveness of various interventions on maintenance of gingival health during 1 year – a randomized clinical trial . International Journal of Dental Hygiene 2017; 15 ( 4 ):e16–e27. [ PubMed ] [ Google Scholar ]
Weinstein 1996 {published data only}
- Weinstein R, Tosolin F, Ghilardi L, Zanardelli E. Psychological intervention in patients with poor compliance . Journal of Clinical Periodontology 1996; 23 ( 3 Pt 2 ):283‐8. [DOI: 10.1111/j.1600-051X.1996.tb02090.x] [ PubMed ] [ CrossRef ] [ Google Scholar ]
References to studies excluded from this review
Albandar 1994 {published data only}.
- Albandar JM, Buischi YA, Mayer MP, Axelsson P. Long‐term effect of two preventive programs on the incidence of plaque and gingivitis in adolescents . Journal of Periodontology 1994; 65 ( 6 ):605‐10. [ PubMed ] [ Google Scholar ]
Aleksejūnienė 2018 {published data only}
- Aleksejūnienė J, Brukienė V. A cluster randomized theory‐guided oral hygiene trial in adolescents ‐ a latent growth model . International Journal of Dental Hygiene 2018; 16 ( 2 ):e23‐e30. [DOI: 10.1111/idh.12286] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Almomani 2006 {published data only}
- Almomani F, Brown C, Williams KB. The effect of an oral health promotion program for people with psychiatric disabilities . Psychiatric Rehabilitation Journal 2006; 29 ( 4 ):274‐81. [ PubMed ] [ Google Scholar ]
Almomani 2009 {published data only}
- Almomani F, Williams K, Catley D, Brown C. Effects of an oral health promotion program in people with mental illness . Journal of Dental Research 2009; 88 ( 7 ):648‐52. [ PubMed ] [ Google Scholar ]
Arrow 2013 {published data only}
- Arrow P, Raheb J, Miller M. Brief oral health promotion intervention among parents of young children to reduce early childhood dental decay . BMC Public Health 2013; 13 :245. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Arunakul 2012 {published data only}
- Arunakul M, Kuphasuk Y, Boonyathanasit R. Effectiveness of oral hygiene instruction media on periodontal health among hearing impaired children . Southeast Asian Journal of Tropical Medicine and Public Health 2012; 43 ( 5 ):1297‐303. [ PubMed ] [ Google Scholar ]
Arunakul 2015 {published data only}
- Arunakul M, Asvanund Y, Tantakul A, Mitrakul K, Srisatjaluk R, Vongsavan K. Effectiveness of an oral hygiene education program combined with fluoride mouthrinse among visually impaired students in Bangkok, Thailand . Southeast Asian Journal of Tropical Medicine and Public Health 2015; 46 ( 2 ):354‐9. [ PubMed ] [ Google Scholar ]
Axelsson 1981 {published data only}
- Axelsson P, Lindhe J. Effect of oral hygiene instruction and professional toothcleaning on caries and gingivitis in schoolchildren . Community Dentistry and Oral Epidemiology 1981; 9 ( 6 ):251‐5. [ PubMed ] [ Google Scholar ]
Bahri 2015 {published data only}
- Bahri N, Tohidinik HR, Bahri N, Iliati HR, Moshki M, Darabi F. Educational intervention to improve oral health beliefs and behaviors during pregnancy: a randomized‐controlled trial . Journal of the Egyptian Public Health Association 2015; 90 ( 2 ):41‐5. [ PubMed ] [ Google Scholar ]
Blinkhorn 1981 {published data only}
- Blinkhorn AS, Downer MC, Mackie IC, Bleasdale RS. Evaluation of a practice based preventive programme for adolescents . Community Dentistry and Oral Epidemiology 1981; 9 ( 6 ):275‐9. [ PubMed ] [ Google Scholar ]
Blinkhorn 2003 {published data only}
- Blinkhorn AS, Gratrix D, Holloway PJ, Wainwright‐Stringer YM, Ward SJ, Worthington HV. A cluster randomised, controlled trial of the value of dental health educators in general dental practice . British Dental Journal 2003; 195 ( 7 ):395‐400. [DOI: 10.1038/sj.bdj.4810566] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Brand 2013 {published data only}
- Brand VS, Bray KK, MacNeill S, Catley D, Williams K. Impact of single‐session motivational interviewing on clinical outcomes following periodontal maintenance therapy . International Journal of Dental Hygiene 2013; 11 ( 2 ):134‐41. [ PubMed ] [ Google Scholar ]
Brukienė 2012 {published data only}
- Brukienė V, Aleksejūnienė J. Is the authoritative parenting model effective in changing oral hygiene behavior in adolescents? . Health Education Research 2012; 27 ( 6 ):1081‐90. [ PubMed ] [ Google Scholar ]
Choi 2012 {published data only}
- Choi HS, Ahn HY. Effects of mothers involved in dental health program for their children . Journal of Korean Academy of Nursing 2012; 42 ( 7 ):1050‐61. [ PubMed ] [ Google Scholar ]
Clarkson 2009 {published data only}
- Clarkson JE, Young L, Ramsay CR, Bonner BC, Bonetti D. How to influence patient oral hygiene behavior effectively . Journal of Dental Research 2009; 88 ( 10 ):933‐7. [DOI: 10.1177/0022034509345627] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Crawford 1975 {published data only}
- Crawford AN, McAllan LH, Murray JJ, Brook AH. Oral hygiene instruction and motivation in children using manual and electric toothbrushes . Community Dentistry and Oral Epidemiology 1975; 3 ( 6 ):257‐61. [PUBMED: 1059513] [ PubMed ] [ Google Scholar ]
Daly 2009 {published data only}
- Daly CG. Prescribing good oral hygiene for adults . Australian Prescriber 2009; 32 ( 3 ):72‐5. [ Google Scholar ]
Davies 2007 {published data only}
- Davies GM, Duxbury JT, Boothman NJ, Davies RM. Challenges associated with the evaluation of a dental health promotion programme in a deprived urban area . Community Dental Health 2007; 24 ( 2 ):117‐21. [ PubMed ] [ Google Scholar ]
de Andrade Meyer 2010 {published data only}
- Andrade Meyer AC, Mello Tera T, Rocha JC, Jardini MA. Clinical and microbiological evaluation of the use of toothpaste containing 1% chlorhexidine and the influence of motivation on oral hygiene in patients with motor deficiency . Special Care in Dentistry 2010; 30 ( 4 ):140‐5. [ PubMed ] [ Google Scholar ]
Dermen 2014 {published data only}
- Dermen KH, Ciancio SG, Fabiano JA. A pilot test of motivational oral health promotion with alcohol‐dependent inpatients . Health Psychology 2014; 33 ( 4 ):392‐5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Džiaugytė 2017 {published data only}
- Džiaugytė L, Aleksejūnienė J, Brukienė V, Pečiulienė V. Self‐efficacy theory‐based intervention in adolescents: a cluster randomized trial‐focus on oral self‐care practice and oral self‐care skills . International Journal of Paediatric Dentistry 2017; 27 ( 1 ):37‐46. [ PubMed ] [ Google Scholar ]
Esfahanizadeh 2011 {published data only}
- Esfahanizadeh N. Dental health education programme for 6‐year‐olds: a cluster randomised controlled trial . European Journal of Paediatric Dentistry 2011; 12 ( 3 ):167‐70. [ PubMed ] [ Google Scholar ]
Ferrazzano 2008 {published data only}
- Ferrazzano GF, Cantile T, Sangianantoni G, Ingenito A. Effectiveness of a motivation method on the oral hygiene of children . European Journal of Paediatric Dentistry 2008; 9 ( 4 ):183‐7. [ PubMed ] [ Google Scholar ]
Franz‐Ritscherle 1983 {published data only}
- Franz‐Ritscherle A, Lange DE. Effectiveness of various audiovisual technics to improve oral hygiene behavior . Deutsche Zahnarztliche Zeitschrift 1983; 38 ( 9 ):811‐5. [ PubMed ] [ Google Scholar ]
Freitas‐Fernandes 2002 {published data only}
- Freitas‐Fernandes LB, Novaes AB Jr, Feitosa AC, Novaes AB. Effectiveness of an oral hygiene program for Brazilian orphans . Brazilian Dental Journal 2002; 13 ( 1 ):44‐8. [ PubMed ] [ Google Scholar ]
Gathece 2011 {published data only}
- Gathece LW, Wang'ombe JK, Ng'ang'a PM, Wanzala PN. Effect of health education on oral hygiene and gingival status of persons living with HIV attending comprehensive care centres in Nairobi, Kenya . African Journal of AIDS Research 2011; 10 ( 4 ):495‐500. [ PubMed ] [ Google Scholar ]
Glavind 1981 {published data only}
- Glavind L, Zeuner E, Attström R. Oral hygiene instruction of adults by means of a self‐instructional manual . Journal of Clinical Periodontology 1981; 8 ( 3 ):165‐76. [ PubMed ] [ Google Scholar ]
Glavind 1983 {published data only}
- Glavind L, Zeuner E, Attstrom R. Evaluation of various feedback mechanisms in relation to compliance by adult patients with oral home care instructions . Journal of Clinical Periodontology 1983; 10 ( 1 ):57‐68. [PUBMED: 6572635] [ PubMed ] [ Google Scholar ]
Godard 2011 {published data only}
- Godard A, Dufour T, Jeanne S. Application of self‐regulation theory and motivational interview for improving oral hygiene: a randomized controlled trial . Journal of Clinical Periodontology 2011; 38 ( 12 ):1099‐105. [ PubMed ] [ Google Scholar ]
Graehn 1984 {published data only}
- Graehn G. A health education program for pre‐school children. 1. Results on health knowledge, health behavior, and oral hygiene . Stomatologie der DDR 1984; 34 ( 4 ):226‐35. [ PubMed ] [ Google Scholar ]
Harnacke 2012 {published data only}
- Harnacke D, Mitter S, Lehner M, Munzert J, Deinzer R. Improving oral hygiene skills by computer‐based training: a randomized controlled comparison of the modified Bass and the Fones techniques . PLoS One 2012; 7 ( 5 ):e37072. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Harrison 2007 {published data only}
- Harrison R, Benton T, Everson‐Stewart S, Weinstein P. Effect of motivational interviewing on rates of early childhood caries: a randomized trial . Pediatric Dentistry 2007; 29 ( 1 ):16‐22. [ PubMed ] [ Google Scholar ]
Hietasalo 2009 {published data only}
- Hietasalo P, Seppa L, Lahti S, Niinimaa A, Kallio J, Aronen P, et al. Cost‐effectiveness of an experimental caries‐control regimen in a 3.4‐yr randomized clinical trial among 11‐12‐yr‐old Finnish schoolchildren . European Journal of Oral Sciences 2009; 117 ( 6 ):728‐33. [ PubMed ] [ Google Scholar ]
Ismail 2011 {published data only}
- Ismail AI, Ondersma S, Jedele JM, Little RJ, Lepkowski JM. Evaluation of a brief tailored motivational intervention to prevent early childhood caries . Community Dentistry and Oral Epidemiology 2011; 39 ( 5 ):433‐48. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Iwata 1981 {published data only}
- Iwata BA, Becksfort CM. Behavioral research in preventive dentistry: educational and contingency management approaches to the problem of patient compliance . Journal of Applied Behavior Analysis 1981; 14 ( 2 ):111‐20. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Jiang 2014 {published data only}
- Jiang EM, Lo EC, Chu CH, Wong MC. Prevention of early childhood caries (ECC) through parental toothbrushing training and fluoride varnish application: a 24‐month randomized controlled trial . Journal of Dentistry 2014; 42 ( 12 ):1543‐50. [ PubMed ] [ Google Scholar ]
Jönsson 2012 {published data only}
- Jönsson B, Baker SR, Lindberg P, Oscarson N, Ohrn K. Factors influencing oral hygiene behaviour and gingival outcomes 3 and 12 months after initial periodontal treatment: an exploratory test of an extended Theory of Reasoned Action . Journal of Clinical Periodontology 2012; 39 ( 2 ):138‐44. [ PubMed ] [ Google Scholar ]
Ju 2017 {published data only}
- Ju X, Brennan D, Parker E, Mills H, Kapellas K, Jamieson L. Efficacy of an oral health literacy intervention among Indigenous Australian adults . Community Dentistry and Oral Epidemiology 2017; 45 ( 5 ):413‐26. [ PubMed ] [ Google Scholar ]
Kakudate 2009 {published data only}
- Kakudate N, Morita M, Sugai M, Kawanami M. Systematic cognitive behavioral approach for oral hygiene instruction: a short‐term study . Patient Education and Counseling 2009; 74 ( 2 ):191‐6. [ PubMed ] [ Google Scholar ]
Kasaj 2004 {published data only}
- Kasaj A, Sculean A, Willershausen B. Study of the usefulness of the DetecTar System in improving patient compliance and oral hygiene . Parodontologie 2004; 15 ( 4 ):343‐53. [ Google Scholar ]
Langan 1976 {published data only}
- Langan MJ, Yearick ES. The effects of improved oral hygiene on taste perception and nutrition of the elderly . Journal of Gerontology 1976; 31 ( 4 ):413‐8. [ PubMed ] [ Google Scholar ]
Lee 2009 {published data only}
- Lee HK, Choi SH, Won KC, Merchant AT, Song KB, Jeong SH, et al. The effect of intensive oral hygiene care on gingivitis and periodontal destruction in type 2 diabetic patients . Yonsei Medical Journal 2009; 50 ( 4 ):529‐36. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Legler 1971 {published data only}
- Legler DW, Gilmore RW, Stuart GC. Dental education of disadvantaged adult patients: effects on dental knowledge and oral health . Journal of Periodontology 1971; 42 ( 9 ):565‐70. [ PubMed ] [ Google Scholar ]

Lim 1996 {published data only}
- Lim LP, Davies WI. Comparison of various modalities of "simple" periodontal therapy on oral cleanliness and bleeding . Journal of Clinical Periodontololgy 1996; 23 ( 6 ):595‐600. [ PubMed ] [ Google Scholar ]
Lim 1996b {published data only}
- Lim LP, Davies WI, Yuen KW, Ma MH. Comparison of modes of oral hygiene instruction in improving gingival health . Journal of Clinical Periodontology 1996; 23 ( 7 ):693‐7. [ PubMed ] [ Google Scholar ]
Little 1997 {published data only}
- Little SJ, Hollis JF, Stevens VJ, Mount K, Mullooly JP, Johnson BD. Effective group behavioral intervention for older periodontal patients . Journal of Periodontal Research 1997; 32 ( 3 ):315‐25. [ PubMed ] [ Google Scholar ]
Mahantesha 2015 {published data only}
- Mahantesha T, Nara A, Kumari PR, Halemani PK, Buddiga V, Mythri S. A comparative evaluation of oral hygiene using Braille and audio instructions among institutionalized visually impaired children aged between 6 years and 20 years: a 3‐month follow‐up study . Journal of International Society of Preventive and Community Dentistry 2015; 5 ( Suppl 2 ):S129‐32. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Makuch 2011 {published data only}
- Makuch A, Reschke K, Rupf S. Effective teaching of tooth‐brushing to preschool children . Journal of Dentistry for Children 2011; 78 ( 1 ):9‐12. [ PubMed ] [ Google Scholar ]
Mayer 2003 {published data only}
- Mayer MP, Paiva Buischi Y, Oliveira LB, Gjermo O. Long‐term effect of an oral hygiene training program on knowledge and reported behavior . Oral Health and Preventive Dentistry 2003; 1 ( 1 ):37‐43. [ PubMed ] [ Google Scholar ]
Meurman 2009 {published data only}
- Meurman P, Pienihäkkinen K, Eriksson AL, Alanen P. Oral health programme for preschool children: a prospective, controlled study . International Journal of Paediatric Dentistry 2009; 19 ( 4 ):263‐73. [ PubMed ] [ Google Scholar ]
Moltzer 1986 {published data only}
- Moltzer G, Hoogstraten J. The effect of three methods of dental health care instruction and dental knowledge, attitude, behaviour, and fear . Community Dental Health 1986; 3 ( 1 ):83‐9. [ PubMed ] [ Google Scholar ]
Moskovitz 2009 {published data only}
- Moskovitz M, Abud W, Ram D. The influence of an oral health education program provided in a community dental clinic on the prevalence of caries among 12‐14 year‐old children . Journal of Clinical Pediatric Dentistry 2009; 33 ( 3 ):259‐64. [ PubMed ] [ Google Scholar ]
Ohrn 2009 {published data only}
- Ohrn K, Sanz M. Prevention and therapeutic approaches to gingival inflammation . Journal of Clinical Periodontology 2009; 36 ( Suppl 10 ):20‐6. [ PubMed ] [ Google Scholar ]
Park 2011 {published data only}
- Park MS, Choi‐Kwon S. The effects of oral care education on caregivers' knowledge, attitude, & behavior toward oral hygiene for elderly residents in a nursing home . Journal of Korean Academy of Nursing 2011; 41 ( 5 ):684‐93. [ PubMed ] [ Google Scholar ]
Park 2015 {published data only}
- Park DY, Lee BJ, Kim BO, Yu SJ. Effect of the education interval and method on improving patients' plaque control ability . Journal of Korean Academy of Oral Health 2015; 39 ( 2 ):145‐51. [ Google Scholar ]
Patthoff 1981 {published data only}
- Patthoff DE, Horton AM Jr, Vecchio MB. Behavioral dentistry: a multiple‐baseline study incorporating contracting with patients . Perceptual and Motor Skills 1981; 53 ( 2 ):383‐6. [ PubMed ] [ Google Scholar ]
Picard 2014 {published data only}
- Picard AJ, Estrella MR, Boynton J, Maxwell A, Inglehart MR. Educating parents of children receiving comprehensive dental care under general anesthesia with visual AIDS . Pediatric Dentistry 2014; 36 ( 4 ):329‐35. [ PubMed ] [ Google Scholar ]
Pickrell 2007 {published data only}
- Pickrell JE, Heima M, Weinstein P, Coolidge T, Coldwell SE, Skaret E, et al. Using memory restructuring strategy to enhance dental behaviour . International Journal of Paediatric Dentistry 2007; 17 ( 6 ):439‐48. [ PubMed ] [ Google Scholar ]
Pine 2007 {published data only}
- Pine CM, Curnow MM, Burnside G, Nicholson JA, Roberts AJ. Caries prevalence four years after the end of a randomised controlled trial . Caries Research 2007; 41 ( 6 ):431‐6. [ PubMed ] [ Google Scholar ]
Plutzer 2008 {published data only}
- Plutzer K, Spencer AJ. Efficacy of an oral health promotion intervention in the prevention of early childhood caries . Community Dentistry and Oral Epidemiology 2008; 36 ( 4 ):335‐46. [ PubMed ] [ Google Scholar ]
Plutzer 2012 {published data only}
- Plutzer K, Spencer AJ, Keirse MJ. Reassessment at 6‐7 years of age of a randomized controlled trial initiated before birth to prevent early childhood caries . Community Dentistry and Oral Epidemiology 2012; 40 ( 2 ):116‐24. [ PubMed ] [ Google Scholar ]
Reinhardt 2010 {published data only}
- Reinhardt CH, Noack MJ, Wassmer G, Hurrelmann K, Klein K. A strategy for encouraging young adults' adoption of a preferred oral hygiene technique . Oral Health and Preventive Dentistry 2010; 8 ( 1 ):3‐8. [ PubMed ] [ Google Scholar ]
Roscher 2004 {published data only}
- Roscher T, Rösing CK, Gjermo P, Aass AM. Effect of instruction and motivation in the use of electric and manual toothbrushes in periodontal patients. A comparative study . Brazilian Oral Research 2004; 18 ( 4 ):296‐300. [ PubMed ] [ Google Scholar ]
Saengtipbovorn 2017 {published data only}
- Saengtipbovorn S. Efficacy of Motivational Interviewing in Conjunction with Caries Risk Assessment (MICRA) programmes in improving the dental health status of preschool children: a randomised controlled trial . Oral Health & Preventive Dentistry 2017; 15 ( 2 ):123‐9. [ PubMed ] [ Google Scholar ]
Sandeep 2014 {published data only}
- Sandeep V, Vinay C, Madhuri V, Rao VV, Uloopi KS, Sekhar RC. Impact of visual instruction on oral hygiene status of children with hearing impairment . Journal of the Indian Society of Pedodontics and Preventive Dentistry 2014; 32 ( 1 ):39‐43. [ PubMed ] [ Google Scholar ]
Sato 2008 {published data only}
- Sato T, Abe T, Ichikawa M, Fukushima Y, Nakamoto N, Koshikiya N, et al. A randomized controlled trial assessing the effectiveness of professional oral care by dental hygienists . International Journal of Dental Hygiene 2008; 6 ( 1 ):63‐7. [ PubMed ] [ Google Scholar ]
Schiffner 2007 {published data only}
- Schiffner U, Bahr M, Effenberger S. Plaque and gingivitis in the elderly: a randomized, single‐blind clinical trial on the outcome of intensified mechanical or antibacterial oral hygiene measures . Journal of Clinical Periodontology 2007; 34 ( 12 ):1068‐73. [DOI: 10.1111/j.1600-051X.2007.01150.x] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Schneider 1981 {published data only}
- Schneider HG, Friedländer B, Richter C, Unger E, Ziesenitz S, Bendrien S. Experience with plaque‐disclosing agents . Stomatologie der DDR 1981; 31 ( 12 ):904‐9. [ PubMed ] [ Google Scholar ]
Schneider 1982 {published data only}
- Schneider HG, Rasch K. The motivation of preschool children toward oral and dental hygiene . Stomatologie der DDR 1982; 32 ( 4 ):261‐5. [ PubMed ] [ Google Scholar ]
Schüz 2009 {published data only}
- Schüz B, Wiedemann AU, Mallach N, Scholz U. Effects of a short behavioural intervention for dental flossing: randomized‐controlled trial on planning when, where and how . Journal of Clinical Periodontology 2009; 36 ( 6 ):498‐505. [ PubMed ] [ Google Scholar ]
Seow 2003 {published data only}
- Seow WK, Cheng E, Wan V. Effects of oral health education and tooth‐brushing on mutans streptococci infection in young children . Pediatric Dentistry 2003; 25 ( 3 ):223‐8. [ PubMed ] [ Google Scholar ]
Sniehotta 2007 {published data only}
- Sniehotta FF, Araújo Soares V, Dombrowski SU. Randomized controlled trial of a one‐minute intervention changing oral self‐care behavior . Journal of Dental Research 2007; 86 ( 7 ):641‐5. [ PubMed ] [ Google Scholar ]
Söderholm 1982b {published data only}
- Söderholm G, Egelberg J. Teaching plaque control. II. 30‐minute versus 15‐minute appointments in a three‐visit program . Journal of Clinical Periodontology 1982; 9 ( 3 ):214‐22. [6954163] [ PubMed ] [ Google Scholar ]
Stenman 2012 {published data only}
- Stenman J, Lundgren J, Wennström JL, Ericsson JS, Abrahamsson KH. A single session of motivational interviewing as an additive means to improve adherence in periodontal infection control: a randomized controlled trial . Journal of Clinical Periodontology 2012; 39 ( 10 ):947‐54. [ PubMed ] [ Google Scholar ]
Stenman 2017 {published data only}
- Stenman J, Wennström JL, Abrahamsson KH. A brief motivational interviewing as an adjunct to periodontal therapy ‐ a potential tool to reduce relapse in oral hygiene behaviours. A three‐year study . International Journal of Dental Hygiene 2017 Aug 24 [Epub ahead of print]. [DOI: 10.1111/idh.12308] [ PubMed ] [ CrossRef ]
Strippel 2010 {published data only}
- Strippel H. Effectiveness of structured comprehensive paediatric oral health education for parents of children less than two years of age in Germany . Community Dental Health 2010; 27 ( 2 ):74‐80. [ PubMed ] [ Google Scholar ]
Tan 1978 {published data only}
- Tan HH, Saxton CA. Effect of a single dental health care instruction and prophylaxis on gingivitis . Community Dentistry and Oral Epidemiology 1978; 6 ( 4 ):172‐5. [ PubMed ] [ Google Scholar ]
Tan 1979 {published data only}
- Tan HH. Effect of dental health care instruction and prophylaxis on knowledge, attitude and behavior in Dutch military personnel . Community Dentistry and Oral Epidemiology 1979; 7 ( 5 ):252‐8. [ PubMed ] [ Google Scholar ]
Telford 1974 {published data only}
- Telford AB, Murray JJ. The effect of systematic chairside oral hygiene instruction on gingivitis and oral cleanliness in children . Community Dentistry and Oral Epidemiology 1974; 2 ( 2 ):50‐7. [PUBMED: 4528776] [ PubMed ] [ Google Scholar ]
Triana 1985 {published data only (unpublished sought but not used)}
- Triana Cue M, Nazco Ríos C. Gingival bleeding and motivation [Sangramiento gingival y motivación]. Revista Cubana de Estomatología 1985; 22 ( 2 ):118‐24. [ PubMed ] [ Google Scholar ]
Valle 2004 {published data only}
- Valle DD, Carvalho Vianna RB, Quintanilha LE, Abreu FV. Evaluation of an oral health promotion program using different indicators . Journal of Clinical Pediatric Dentistry 2004; 29 ( 1 ):87‐92. [ PubMed ] [ Google Scholar ]
Zanin 2007 {published data only}
- Zanin L, Meneghim MC, Assaf AV, Cortellazzi KL, Pereira AC. Evaluation of an educational program for children with high risk of caries . Journal of Clinical Pediatric Dentistry 2007; 31 ( 4 ):246‐50. [ PubMed ] [ Google Scholar ]
Zee 2006 {published data only}
- Zee KY, Lee DH, Corbet EF. Repeated oral hygiene instructions alone, or in combination with metronidazole dental gel with or without subgingival scaling in adult periodontitis patients: a one‐year clinical study . Journal of the International Academy of Periodontology 2006; 8 ( 4 ):125‐35. [ PubMed ] [ Google Scholar ]
Ziebolz 2009 {published and unpublished data}
- Ziebolz D, Herz A, Brunner E, Hornecker E, Mausberg RF. Individual versus group oral hygiene instruction for adults . Oral Health & Preventive Dentistry 2009; 7 ( 1 ):93‐9. [PUBMED: 19408821] [ PubMed ] [ Google Scholar ]
References to studies awaiting assessment
Gao 2013 {published data only}.
- Gao X, Lo EC, McGrath C, Ho SM. Innovative interventions to promote positive dental health behaviors and prevent dental caries in preschool children: study protocol for a randomized controlled trial . Trials 2013; 14 :118. [DOI: 10.1186/1745-6215-14-118] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
IRCT2014062618248N1 {unpublished data only}
- IRCT2014062618248N1. The effect of educational intervention based on Pender's Health Promotion Model on oral and dental health behaviors among high school students . apps.who.int/trialsearch/Trial3.aspx?trialid=IRCT2014062618248N1 (first received 25 October 2014).
References to ongoing studies
Actrn12605000607673 {unpublished data only}.
- ACTRN12605000607673. Oral Health Education Logan Programme (OHELP) [The effect of a personalised oral health education programme on clinical and molecular risk factors for oral and general health in an at risk population]. www.anzctr.org.au/ACTRN12605000607673.aspx (first received 12 September 2005).
ISRCTN24958829 {unpublished data only}
- ISRCTN24958829. Dental RECUR Trial [Comparison of a new with standard child and family primary care service to reduce the re‐occurrence of childhood dental caries (Dental RECUR Trial)]. www.isrctn.com/ISRCTN24958829 (first received 27 September 2013).
ISRCTN38542397 {unpublished data only}
- ISRCTN38542397. Is photographic evidence a valuable aide to oral hygiene advice in 9‐16 year olds? . www.isrctn.com/ISRCTN38542397 (first received 28 September 2007).
{"type":"clinical-trial","attrs":{"text":"NCT01118143","term_id":"NCT01118143"}} NCT01118143 {unpublished data only}
- NCT01118143. Oral health literacy tailored communication [Effects of communication tailored to oral health literacy level of adult dental patients: a randomized controlled trial]. clinicaltrials.gov/ct2/show/NCT01118143 (first received 6 May 2010).
Additional references
- Adair JG. The Hawthorne effect: a reconsideration of the methodological artifact . Journal of Applied Psychology 1984; 69 ( 2 ):334‐45. [ Google Scholar ]
Axelsson 2004
- Axelsson P, Nyström B, Lindhe J. The long‐term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance . Journal of Clinical Periodontology 2004; 31 ( 9 ):749‐57. [ PubMed ] [ Google Scholar ]
- Baab DA, Weinstein P. Oral hygiene instruction using a self inspection plaque index . Community Dentistry and Oral Epidemiology 1983; 11 ( 3 ):174‐9. [ PubMed ] [ Google Scholar ]
Bandura 1998
- Bandura A. Health promotion from the perspective of social cognitive theory . Psychology and Health 1998; 13 :623‐49. [ Google Scholar ]
- Bass CC. An effective method of personal oral hygiene . Journal of the Louisiana State Medical Society 1954; 106 ( 2 ):57‐73. [ PubMed ] [ Google Scholar ]
- Bass CC. An effective method of personal oral hygiene; part II . Journal of the Louisiana State Medical Society 1954; 106 ( 3 ):100‐12. [ PubMed ] [ Google Scholar ]
Björby 1967
- Björby Å, Löe H. The relative significance of different local factors in the initiation and development of periodontal inflammation. Scandinavian Symposium in Periodontology 1966 . Journal of Periodontal Research 1967; 2 ( 1 ):76‐7 (Abs No 20). [ Google Scholar ]
Chadwick 2011
- Chadwick B, White D, Lader D, Pitts N. 5: Preventive behaviour and risks to oral health ‐ a report from the Adult Dental Health Survey 2009 . Leeds: The Health and Social Care Information Centre; 2011 March .
Chapple 2008
- Chapple ILC, Hill K. Getting the message across to periodontitis patients: the role of personalised biofeedback . International Dental Journal 2008; 65 ( 5 Supplement 1 ):294‐306. [ Google Scholar ]
- Department of Health, British Association for the Study of Community Dentistry. Delivering Better Oral Health: an evidence‐based toolkit for prevention . London: Department of Health; 2009 April .
- Deci EL, Ryan RM. The general causality orientation scale: self‐determination in personality . Journal of Research in Personality 1985; 19 :109–34. [ Google Scholar ]
Deinzer 2014
- Deinzer R, Jahns S, Harnacke D. Establishment of a new marginal plaque index with high sensitivity for changes in oral hygiene . Journal of Periodontology 2014; 85 ( 12 ):1730‐8. [ PubMed ] [ Google Scholar ]
Dupont 1990
- Dupont WD, Plummer WD Jr. Power and sample size calculations. A review and computer program . Controlled Clinical Trials 1990; 11 ( 2 ):116‐28. [ PubMed ] [ Google Scholar ]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test . BMJ 1997; 315 ( 7109 ):629‐34. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross‐over trials: methodological issues . International Journal of Epidemiology 2002; 31 ( 1 ):140‐9. [ PubMed ] [ Google Scholar ]
Fishbein 1980
- Fishbein M, Azjen I. Understanding Attitudes and Predicting Social Behaviour . Englewood Cliffs: Prentice‐Hall, Inc., 1980. [ Google Scholar ]
Glavind 1979
- Glavind L, Attström R. Periodontal self‐examination. A motivational tool in periodontics . Journal of Clinical Periodontology 1979; 6 ( 4 ):238‐51. [ PubMed ] [ Google Scholar ]
Gollwitzer 1999
- Gollwitzer PM. Implementation intentions: strong effects of simple plans . American Psychologist 1999; 54 :493‐503. [ Google Scholar ]
Gründemann 2000
- Gründemann LJ, Timmerman MF, Ijzerman Y, Weijden GA, Weijden GA. Stain, plaque and gingivitis reduction by combining chlorhexidine and peroxyborate . Journal of Clinical Periodontology 2000; 27 ( 1 ):9‐15. [ PubMed ] [ Google Scholar ]
Halvari 2006
- Halvari A, Halvari H. Motivational predictors of change in oral health: an experimental test of self‐determination theory . Motivation and Emotion 2006; 30 :295‐305. [ Google Scholar ]
Halvari 2010
- Halvari AEM, Halvari H, Bjørnebekk G, Deci EL. Motivation and anxiety for dental treatment: testing a self‐determination theory model of oral self‐care behavior and dental clinic attendance . Motivation and Emotion 2010; 34 :15‐33. [ Google Scholar ]
Halvari 2012
- Halvari AEM, Halvari H, Bjørnebekk G, Deci EL. Motivation for dental home care: testing a self‐determination theory model . Journal of Applied Social Psychology 2012; 42 :1‐39. [ Google Scholar ]
Harris 2012
- Harris R, Gamboa A, Dailey Y, Ashcroft A. One‐to‐one dietary interventions undertaken in a dental setting to change dietary behaviour . Cochrane Database of Systematic Reviews 2012, Issue 3 . [DOI: 10.1002/14651858.CD006540.pub2] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011 . Available from handbook.cochrane.org .
- Holve S. An observational study of the association of fluoride varnish applied during well child visits and the prevention of early childhood caries in American Indian children . Maternal and Child Health Journal 2008; 12 Suppl 1 :64–7. [ PubMed ] [ Google Scholar ]
Hugoson 2003
- Hugoson A, Lundgren D, Asklöw B, Borgklint G. The effect of different dental health programmes on young individuals: a longitudinal evaluation of knowledge and behaviour including cost aspects . Swedish Dental Journal 2003; 27 ( 3 ):115‐30. [ PubMed ] [ Google Scholar ]
Kagihara 2009
- Kagihara LE, Niederhauser VP, Stark M. Assessment, management, and prevention of early childhood caries . Journal of the American Academy of Nurse Practitioners 2009; 21 ( 1 ):1–10. [ PubMed ] [ Google Scholar ]
Kassebaum 2014
- Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of severe periodontitis in 1990‐2010: a systematic review and meta‐regression . Journal of Dental Research 2014; 93 ( 11 ):1045‐53. [DOI: 10.1177/0022034514552491] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Kassebaum 2015
- Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of untreated caries: a systematic review and metaregression . Journal of Dental Research 2015; 94 ( 5 ):650‐8. [DOI: 10.1177/0022034515573272] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kay EJ, Locker D. A systematic review of the effectiveness of health promotion aimed at improving oral health . Community Dental Health 1998; 15 :132‐44. [ PubMed ] [ Google Scholar ]
- Kay E, Vascott D, Hocking A, Nield H, Dorr C, Barrett H. A review of approaches for dental practice teams for promoting oral health . Community Dentistry and Oral Epidemiology 2016; 44 ( 4 ):313‐30. [ PubMed ] [ Google Scholar ]
- Kay EJ, Vascott D, Hocking A, Nield H. Motivational interviewing in general dental practice: a review of the evidence . British Dental Journal 2016; 221 ( 12 ):785‐91. [ PubMed ] [ Google Scholar ]
Khokhar 2016
- Khokhar MA, Khokhar WA, Clifton AV, Tosh GE. Oral health education (advice and training) for people with serious mental illness . Cochrane Database of Systematic Reviews 2016, Issue 9 . [DOI: 10.1002/14651858.CD008802.pub3] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Kumarihamy 2011
- Kumarihamy SL, Subasinghe LD, Jayasekara P, Kularatna SM, Palipana PD. The prevalence of early childhood caries in 1–2 year olds in a semi‐urban area of Sri Lanka . BMC Research Notes 2011; 4 :336. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lang NP, Tonetti MS. Periodontal risk assessment (PRA) for patients in supportive periodontal therapy (STP) . Oral Health and Preventive Dentistry 2003; 1 ( 1 ):7–16. [ PubMed ] [ Google Scholar ]
- Lange DE, Plagmann H, Eenboom A, Promesberger A. Clinical methods for the objective evaluation of oral hygiene . Deutsche Zahnarztliche Zeitschrift 1977; 32 ( 1 ):44‐7. [ PubMed ] [ Google Scholar ]
- Lange DE. Odontologie in der Täglichen Praxis . Berlin: Quintessenz Verlag, 1986. [ Google Scholar ]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011 . Available from handbook.cochrane.org .
- Lie MA, Timmerman MF, Velden U, Weijden GA. Evaluation of 2 methods to assess gingival bleeding in smokers and non‐smokers in natural and experimental gingivitis . Journal of Clinical Periodontology 1998; 25 ( 9 ):695‐700. [ PubMed ] [ Google Scholar ]
Löe 1963
- Löe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity . Acta Odontologica Scandinavica 1963; 21 :533–51. [ PubMed ] [ Google Scholar ]
Löe 1965
- Löe H, Theilade E, Jensen SB. Experimental gingivitis in man . Journal of Periodontology 1965; 36 :177‐87. [ PubMed ] [ Google Scholar ]
Löe 1967
- Löe H. The Gingival Index, the Plaque Index and the Retention Index systems . Journal of Periodontology 1967; 38 ( 6 ):Suppl:610‐6. [ PubMed ] [ Google Scholar ]
Löe 1972
- Löe H, Fehr FR, Schiott CR. Inhibition of experimental caries by plaque prevention. The effect of chlorhexidine mouthrinses . Scandinavian Journal of Dental Research 1972; 80 ( 1 ):1‐9. [ PubMed ] [ Google Scholar ]
Magarey 2009
- Magarey A, Golley R, Spurrier N, Goodwin E, Ong F. Reliability and validity of the Children's Dietary Questionnaire; a new tool to measure children's dietary patterns . International Journal of Pediatric Obesity 2009; 4 ( 4 ):257‐65. [ PubMed ] [ Google Scholar ]
Mantilla Gómez 2001
- Mantilla Gómez S, Danser MM, Sipos PM, Rowshani B, Velden U, Weijden GA. Tongue coating and salivary bacterial counts in healthy/gingivitis subjects and periodontitis patients . Journal of Clinical Periodontolology 2001; 28 ( 10 ):970‐8. [ PubMed ] [ Google Scholar ]
Marinho 2003
- Marinho VCC, Higgins JPT, Logan S, Sheiham A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents . Cochrane Database of Systematic Reviews 2003, Issue 4 . [DOI: 10.1002/14651858.CD002782] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Marinho 2004a
- Marinho VCC, Higgins JPT, Sheiham A, Logan S. Combinations of topical fluoride (toothpastes, mouthrinses, gels, varnishes) versus single topical fluoride for preventing dental caries in children and adolescents . Cochrane Database of Systematic Reviews 2004, Issue 1 . [DOI: 10.1002/14651858.CD002781.pub2] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Marinho 2004b
- Marinho VCC, Higgins JPT, Sheiham A, Logan S. One topical fluoride (toothpastes, or mouthrinses, or gels, or varnishes) versus another for preventing dental caries in children and adolescents . Cochrane Database of Systematic Reviews 2004, Issue 1 . [DOI: 10.1002/14651858.CD002780.pub2] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Marinho 2016
- Marinho VCC, Chong LY, Worthington HV, Walsh T. Fluoride mouthrinses for preventing dental caries in children and adolescents . Cochrane Database of Systematic Reviews 2016, Issue 7 . [DOI: 10.1002/14651858.CD002284.pub2] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Mohebbi 2006
- Mohebbi SZ, Virtanen JI, Vahid‐Golpayegani M, Vehkalahti MM. Early childhood caries and dental plaque among 1‐3‐year‐olds in Tehran, Iran . Journal of the Indian Society of Pedodontics and Preventive Dentistry 2006; 24 ( 4 ):177‐81. [ PubMed ] [ Google Scholar ]
Mohebbi 2008
- Mohebbi SZ, Virtanen JI, Vahid‐Golpayegani M, Vehkalahti MM. Feeding habits as determinants of early childhood caries in a population where prolonged breastfeeding is the norm . Community Dentistry and Oral Epidemiology 2008; 36 ( 4 ):363‐9. [ PubMed ] [ Google Scholar ]
Möhler 2015
- Möhler R, Köpke S, Meyer G. Criteria for Reporting the Development and Evaluation of Complex Interventions in healthcare: revised guideline (CReDECI 2) . Trials 2015; 16 :204. [DOI: 10.1186/s13063-015-0709-y] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Newton 2015
- Newton TJ, Asimakopoulou K. Managing oral hygiene as a risk factor for periodontal disease: a systematic review of psychological approaches to behaviour change for improved plaque control in periodontal management . Journal of Clinical Periodontology 2015; 42 (Suppl 16) :S36‐S46. [ PubMed ] [ Google Scholar ]
- NICE. Oral health promotion: general dental practice. NICE guideline [NG30] . www.nice.org.uk/guidance/ng30 (accessed prior to 25 April 2018).
- Nyman S, Bratthall D, Böhlin E. The Swedish dental health program for adults . International Dental Journal 1984; 34 ( 2 ):130–4. [ PubMed ] [ Google Scholar ]
O'Leary 1972
- O'Leary TJ, Drake RB, Naylor JE. The plaque control record . Journal of Periodontology 1972; 43 ( 1 ):38. [ PubMed ] [ Google Scholar ]
Paraskevas 2005
- Paraskevas S, Versteeg PA, Timmerman MF, Velden U, Weijden GA. The effect of a dentifrice and mouth rinse combination containing amine fluoride/stannous fluoride on plaque and gingivitis: a 6‐month field study . Journal of Clinical Periodontology 2005; 32 ( 7 ):757‐64. [ PubMed ] [ Google Scholar ]
Pastagia 2006
- Pastagia J, Nicoara P, Robertson PB. The effect of patient‐centered plaque control and periodontal maintenance therapy on adverse outcomes of periodontitis . Journal of Evidence‐based Dental Practice 2006; 6 ( 1 ):25‐32. [ PubMed ] [ Google Scholar ]
Poklepovic 2013
- Poklepovic T, Worthington HV, Johnson TM, Sambunjak D, Imai P, Clarkson JE, et al. Interdental brushing for the prevention and control of periodontal diseases and dental caries in adults . Cochrane Database of Systematic Reviews 2013, Issue 12 . [DOI: 10.1002/14651858.CD009857.pub2] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Quigley 1962
- Quigley GA, Hein JW. Comparative cleansing efficiency of manual and power brushing . Journal of the American Dental Assocication 1962; 65 :26‐9. [ PubMed ] [ Google Scholar ]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5) . Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- Rice C, Hosey MT. Interactive oral health education – a randomised controlled trial . European Archives of Paediatric Dentistry 2008; 9 ( Suppl 2 ):20‐1 (Abs No O44). [ Google Scholar ]
- Rose EA, Markland D, Parfitt G. The development and initial validation of the Exercise Causality Orientations Scale . Journal of Sports Sciences 2001; 19 ( 6 ):445‐62. [ PubMed ] [ Google Scholar ]
Rugg‐Gunn 1979
- Rugg‐Gunn AJ, Macgregor ID, Edgar WM, Ferguson MW. Toothbrushing behaviour in relation to plaque and gingivitis in adolescent schoolchildren . Journal of Periodontal Research 1979; 14 ( 3 ):231‐8. [ PubMed ] [ Google Scholar ]
Rylander 1997
- Rylander H, Lindhe J. Chapter 15: Cause‐related periodontal therapy . Periodontology and Oral Implants . 3rd Edition. Copenhagen: Munksgaard, 1997:438‐60. [ Google Scholar ]
Rücker 2008
- Rücker G, Schwarzer G, Carpenter J. Arcsine test for publication bias in meta‐analyses with binary outcomes . Statistics in Medicine 2008; 27 ( 5 ):746‐63. [ PubMed ] [ Google Scholar ]
Schmalz 2017b
- Schmalz G, Müller M, Schmickler J, Rinke S, Haak R, Mausberg RF, et al. Influence of manual and power toothbrushes on clinical and microbiological findings in initial treatment of periodontitis ‐ a randomized clinical study . American Journal of Dentistry 2017; 30 ( 1 ):40‐6. [ PubMed ] [ Google Scholar ]
Schmickler 2014
- Schmickler J, Wurbs S, Wurbs S, Lange K, Rinke S, Hornecker E, et al. Influence of the utilization time of different manual toothbrushes on oral hygiene assessed during a 6‐month observation period: a randomized clinical trial . Journal of Periodontology 2014; 85 ( 8 ):1050–8. [ PubMed ] [ Google Scholar ]
Schmickler 2016
- Schmickler J, Wurbs S, Wurbs S, Kramer K, Rinke S, Hornecker E, et al. The influence of the utilization time of brush heads from different types of power toothbrushes on oral hygiene assessed over a 6‐month observation period: a randomized clinical trial . American Journal of Dentistry 2016; 29 ( 6 ):307‐14. [ PubMed ] [ Google Scholar ]
Schulz 2002
- Schulz KF, Grimes DA. Generation of allocation sequences in randomised trials: chance, not choice . Lancet 2002; 359 :515‐9. [ PubMed ] [ Google Scholar ]
Sheiham 2015
- Sheiham A, James WPT. Diet and dental caries: the pivotal role of free sugars reemphasized . Journal of Dental Research 2015; 94 ( 10 ):1341‐7. [ PubMed ] [ Google Scholar ]
Silness 1964
- Silness J, Löe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition . Acta Odontologica Scandinavica 1964; 22 :121‐35. [ PubMed ] [ Google Scholar ]
- Slade GD. Derivation and validation of a short‐form oral health impact profile . Community Dentistry and Oral Epidiemiology 1997; 25 ( 4 ):284‐90. [ PubMed ] [ Google Scholar ]
Tickle 2003
- Tickle M, Milsom KM, King D, Blinkhorn AS. The influences on preventive care provided to children who frequently attend the UK General Dental Service . British Dental Journal 2003; 194 ( 6 ):329‐32. [ PubMed ] [ Google Scholar ]
Tonetti 2017
- Tonetti MS, Jepsen S, Jin L, Otomo‐Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: a call for global action . Journal of Clinical Periodontology 2017; 44 ( 5 ):456‐62. [DOI: 10.1111/jcpe.12732] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Towner 1993
- Towner E. The history of dental health education: a case study of Britain . In: Schou L, Blinkhorn A editor(s). Oral Health Promotion . Oxford: Oxford University Press, 1993. [ Google Scholar ]
Tsakos 2015
- Tsakos G, Hill K, Chadwick B, Anderson T. Children's Dental Health Survey 2013. Report 1: Attitudes, behaviours and children's dental health England, Wales and Northern Ireland, 2013 . Leeds: The Health and Social Care Information Centre; 2015 March .
Turesky 1970
- Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analog of vitamin C . Journal of Periodontology 1970; 41 :41‐3. [ PubMed ] [ Google Scholar ]
Van der Velden 1979
- Velden U. Probing force and the relationship of the probe tip to the periodontal tissues . Journal of Clinical Periodontolology 1979; 6 ( 2 ):106‐14. [ PubMed ] [ Google Scholar ]
Van der Velden 2009
- Velden U. The Dutch periodontal screening index validation and its application in The Netherlands . Journal of Clinical Periodontology 2009; 36 ( 12 ):1018‐24. [ PubMed ] [ Google Scholar ]
Van der Weijden 1994
- Weijden GA, Timmerman MF, Saxton CA, Russell JI, Huntington E, Velden U. Intra‐/inter‐examiner reproducibility study of gingival bleeding . Journal of Periodontal Research 1994; 29 :236‐41. [ PubMed ] [ Google Scholar ]
- Watt RG, Marinho VC. Does oral health promotion improve oral hygiene and gingival health? . Periodontology 2000 2005; 37 :35‐47. [ PubMed ] [ Google Scholar ]
Weyant 2013
- Weyant RJ, Tracy SL, Anselmo TT, Beltrán‐Aguilar ED, Donly KJ, Frese WA, et al. Topical fluoride for caries prevention: executive summary of the updated clinical recommendations and supporting systematic review . Journal of the American Dental Association 2013; 144 ( 11 ):1279–91. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- World Health Organization. The Ottawa Charter for Health Promotion . www.who.int/healthpromotion/conferences/previous/ottawa/en/ (accessed prior to 25 April 2018).
- World Health Organization. Oral health surveys – basic methods, 4th edition . www.who.int/iris/handle/10665/41905 (accessed prior to 25 April 2018).
- World Health Organization. World Oral Health Report 2003 . www.who.int/oral‐health/publications/world‐oral‐health‐report‐2003/en/ (accessed prior to 25 April 2018).
Williams 1996
- Williams GC, Deci ED. Internalization of biopsychosocial values by medical students: a test of self‐determination theory . Journal of Personality and Social Psychology 1996; 70 :767–79. [ PubMed ] [ Google Scholar ]
Wilson 1992
- Wilson PH. Principles and Practice of Relapse Prevention . New York: Guildford Press, 1992. [ Google Scholar ]
- Wolfe GR, Stewart JM, Meader LA, Hartz GW. Use of dental coping beliefs scale to measure cognitive changes following oral hygiene interventions . Community Dentistry and Oral Epidemiology 1996; 24 ( 1 ):37–41. [ PubMed ] [ Google Scholar ]
Yaacob 2014
- Yaacob M, Worthington HV, Deacon SA, Deery C, Walmsley AD, Robinson PG, et al. Powered versus manual toothbrushing for oral health . Cochrane Database of Systematic Reviews 2014, Issue 6 . [DOI: 10.1002/14651858.CD002281.pub3] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Yevlahova 2009
- Yevlahova D, Satur J. Models for individual oral health promotion and their effectiveness: a systematic review . Australian Dental Journal 2009; 54 :190‐7. [ PubMed ] [ Google Scholar ]
References to other published versions of this review
Soldani 2008.
- Soldani FA, Young L, Jones K, Walsh T, Clarkson JE. One‐to‐one oral hygiene advice provided in a dental setting for oral health . Cochrane Database of Systematic Reviews 2008, Issue 4 . [DOI: 10.1002/14651858.CD007447] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]

LOG IN TO YOUR ACCOUNT
Not a member…join up now.
Home » Articles & News » Personal Presentation – an Overview
Personal Presentation – an Overview
- Young Professional
What is Personal Presentation and Why is It Important?
Personal presentation is a communication skill , and communication is one of five important life and work skills you can build as a Young Professional .
Personal presentation means the way you present yourself in everyday situations, and more stressful ones like job interviews. How you appear to the world can have a major impact on your ability to get a job. It’s said that an employer will make a judgement about you in the first 30 seconds after meeting you, which is then quite hard to change during the interview (though not impossible!). So it’s important to make a good impression.
You are your own brand, and what you do and say, as well as your appearance, is all part of that. This means dressing smartly, being clean and having good personal hygiene, and carrying yourself well. Presentation means making a strong first impression and appearing professional.
Whilst employers shouldn’t judge you on how you look, appearing neat and confident is important to show that you’ve made an effort. To be a professional you need to dress the part, which means appropriate clothing for your industry. It could be a suit and tie, or for some jobs particularly in the creative industries there’s more of a relaxed vibe. Whatever the dress code presenting yourself well means you’ve done your research and taken the time to fit in. Standing out can be good but you don’t want to be the only person in the office wearing trainers.
Developing and Demonstrating Good Self Presentation.
It’s fairly easy to improve your personal presentation. Start by looking into the sort of clothes people wear in your chosen industry. For an interview it’s good to wear a slightly smarter version of this. If in doubt it’s a safe bet to wear a suit or trousers/skirt and a blouse or smart top for an interview. Even in a casual role you want to show you take the job seriously at the interview. Make sure everything is clean, dry, and not wrinkled. Laying your outfit out the night before is a good idea, especially if you work in an office environment this will help you ensure you look the part every day.
Another part of personal presentation which isn’t as obvious is confidence. If you are confident people will be able to tell when you walk into a room, and will view you as well presented. If you don’t feel confident you can use the ‘fake it ’til you make it’ trick – stand tall, pull your shoulders back, make eye contact and smile. Tell yourself you are confident and you might find that soon you are.
You are a whole person, and as such everything you say or do in public counts towards the impression of you that others create. This includes social media, so make sure your accounts are presenting you in the best possible way. If you’ve got things on there you don’t think are particularly professional change your security settings, or remove them. It’s really important to make sure you’re aware of what you put out there!
Showing you have good personal presentation is as simple as turning up on time, dressed professionally and appropriately, and appearing confident and enthusiastic about the role. If you get that right you’ll make a great first impression, and can go on to talk about your excellent communication , teamwork and people skills – which all go towards presenting you in a positive way. If you use the STARRS method as well you’ll certainly impress.
Further reading:
- How Interviewers Know When To Hire You in 90 Seconds
- What really happens in the opening moments of a job interview
- Self-Presentation in Presentations
Getting life/work ready
Have you thought about boosting your life and work skills .
Developing the 5 most important skills for life and work is something you can do for free, in your own time. You can start building those skills with Youth Employment UK wherever you are on life’s journey. It can be a big help when you don’t know what to do next.
Boosting your Young Professional life and work skills means you can:
- Boost your confidence
- Feel like you’re taking charge of your life
- Find out more about yourself and what you genuinely want/need in life
- Give yourself more options – both now and later down the line
The 5 top life and work skills are:
- Communication
- Problem solving
- Self-management
- Self-belief
Tagged in: Young Professional
Discover Youth Friendly Employers

Give me more! I am a…
Email us at [email protected] or call 01536 513388.
Take Part In The Youth Voice Census
This national online survey is YOUR chance to say what matters to you and what support you want to get in life. Take part today!
Careers Advice
See All Careers Advice
Build Your Skills
Job Hunting Tips
Work Experience
Youth Friendly Places
Youth Friendly Employers
Career Guides
[su_button url="https://www.youthemployment.org.uk/careers-advice-help/cv-advice/" style="flat" background="#00aeef" size="6" radius="round" icon_color="#fff" color="#fff"]CV Tips [/su_button]
[su_button url="https://www.youthemployment.org.uk/careers-advice-help/interview-tips/" style="flat" background="#00aeef" size="6" radius="round" icon_color="#fff" color="#fff"]Interview Tips [/su_button]
[su_button url="https://www.youthemployment.org.uk/career-quiz/" style="flat" background="#00aeef" size="6" radius="round" icon_color="#fff" color="#fff"]Career Quiz [/su_button]
[su_button url="https://www.youthemployment.org.uk/careers-advice-help/choices/getting-a-job/" style="flat" background="#00aeef" size="6" radius="round" icon_color="#fff" color="#fff"]Job Hunting Tips [/su_button]
Build Skills + Confidence
Want a big boost in your life and work skills sign up to our free online young professional programme today.

Young Professional Programme
Get FREE skills training when you sign up. Get support with your personal confidence, positive attitude and coping with change!
Self Belief | Communication | Teamwork | Problem Solving | Self Management
FREE Online Courses
Boost your skills and careers confidence with FREE online courses . Complete them your own pace and get a certificate for your CV! Sign in as a Young Professional to get automatically enrolled.

Get Jobs + Experience
Find Opportunities

Looking for jobs and opportunities near you? Sign in as a Young Professional to see the latest jobs, apprenticeships, grad schemes, CV workshops, career events and early career opportunities in your area!
Latest Careers Help

IGCSE Results Day 2024 – Information For Students
- Home Education - Students
- Results Day

How To Get Your First Job in Tech for Unemployed Londoners – 14 Mar – London Digital Jobs and Skills Hub
- London Digital Jobs and Skills Hub
- Opportunities
Be Yourself
Mental Health
Stay Curious
Overcoming Barriers
For Students
Student Guides
For Teachers
Teacher Resources

Teachers - see how to use the Young Professional programme in your school or college, with lots of free teaching resources at your fingertips.


Relevant and engaging topics for dental nurses
Posted by: Dental Design 8th June 2022

The British Dental Conference and Dentistry Show (BDCDS) 2022 was a huge success! Dental nurses from across the country had the opportunity to get together once again and enjoy everything the show had to offer.
Among the highlights of the event, the Dental Nurses’ Forum was packed with expert speakers and enlightening topics, such as Hannah Grieves’ lecture titled “Stress management for dental nurses.” Delegates enjoyed this highly-relevant presentation, with one delegate commenting:
“Hannah was fantastic, very relatable and I’ll definitely be using the techniques and strategies discussed in the session!”
Another brilliant session was Rebecca Power’s “Dental health in pregnancy”, which highlighted vital statistics and information that every dental nurse needs to know. One delegate shared that it was “useful to hear about the different niches included in dental health during pregnancy”. Another delegate commented that Rebecca “showed good engagement with the audience and covered a range of learning objectives.”
Are you ready for next year’s BDCDS? We can’t wait to see you all again!
The British Dental Conference and Dentistry Show 2023 will be held on Friday 12 th and Saturday 13 th May, NEC Birmingham, co-located with DTS.
For more information, visit birmingham.dentistryshow.co.uk , or email [email protected]
Category: Featured Products , Promotional Features
No Comments
No comments yet.
Sorry, the comment form is closed at this time.
Join our Mailing List
Sign up to our newsletter and keep up to date on the latest happenings in the dental market.
Recent Posts
Shown below are the most recent articles from across the BDNJ website.
Protocol protection
BDIA Dental Showcase 2024 – Raising the standards of oral care
Connecting for social and professional enrichment
Leading orthodontists join forces to launch ‘Aligner Intelligence’
Eschmann recommended “unreservedly”
Dental Design Products

Published continually since 1959 and orginally the official magazine of the General Dental Practitioners Association , the editorial content of The Probe is of paramount importance and as such forms the backbone of the journal – it is the high quality, independent content of the magazine that ensures it is widely read by the profession and explains why The Probe consistently generates the highest levels of response for its advertisers among any UK dental journal.
Find out more
The UK’s leading magazine for oral health. Focusing on all areas of prevention, oral health and hygiene plus vital vCPD modules, Smile is a vital resource for hygienists wanting to stay at the forefront of clinical innovations in prevention.
An easy way to ensure your whole team is up to date with their CPD requirements. Online modules in all areas of required study which can be bought individually or in annual bundles.
I’d like to be informed of exclusive offers and other practice information YES
Dental nurse CV example
Everyone knows that first impressions count – and your CV acts as your first impression in the hunt for a rewarding dental nurse role.
Your CV needs to highlight why you’d make a great hire, to ensure you get noticed by recruiters and employers
To help you out, this guide will show you exactly what you need to include in a role-winning dental nurse CV.
It also comes with a tried-and-tested example dental nurse CV, to give you an idea of the high standard you should be aiming for.
Guide contents
Dental nurse CV example
- Structuring and formatting your CV
- Writing your CV profile
- Detailing work experience
- Your education
- Skills required for your dental nurse CV
CV templates

Whilst writing your own dental nurse CV, a professional and well-organised structure and format – as shown in the CV example above – should be your goal.
This high standard of presentation allows recruiters to easily navigate through the candidate’s experience, whilst allowing their key skills and achievements to stand out.
Read on to find out exactly how you can create a similar CV, which ultimately gets you hired.
Dental nurse CV structure & format
The written content of your CV is what will land you an interview… but if it’s hard to read, cluttered and disorganised, recruiters may skip your CV altogether.
Focusing on the structure and format of your CV from the get-go will mean that the finished product is clear, easy-to-navigate and oozes professionalism.
So, take a look at my suggested structure and formatting techniques in the image below:
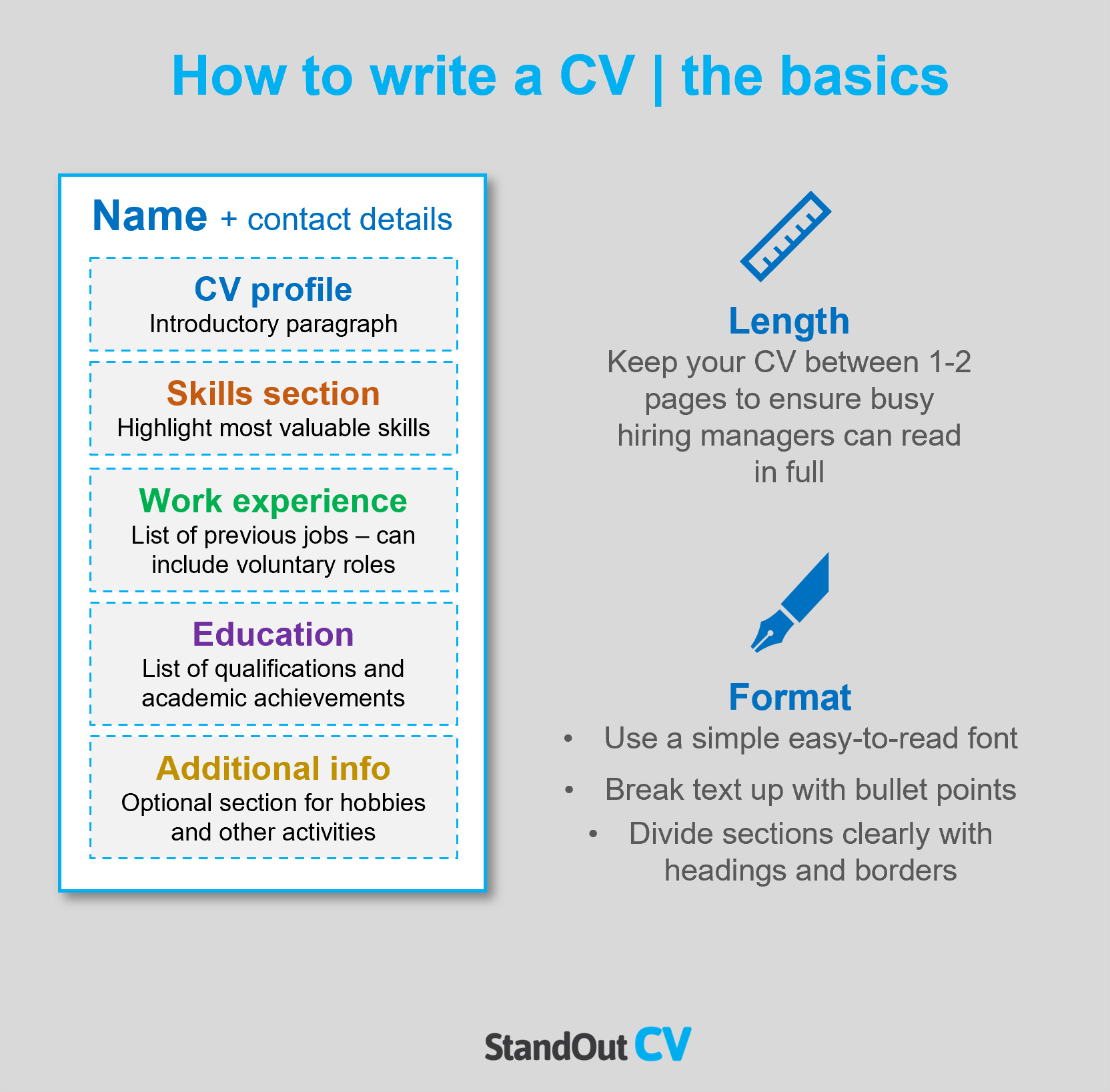
Formatting Tips
- Recruiters are busy and don’t have the time to read lengthy applications. The ideal CV length is a maximum of 2 pages of A4. If you’re just entering the job market, don’t worry if it’s shorter.
- Put yourself in the shoes of a recruiter – would you enjoy reading huge, chunky blocks of text? So, format your CV with plenty of bullet points, lists and columns, whilst making sure your sections are clearly defined with bold or underlined headers.
- Keep things simple. Black or dark grey text with a clear and legible font is best – there’s no need for multiple fonts or elaborate colour schemes.
- Don’t include a profile photo. It’s not only a waste of space but could actually work against you, as it’s illegal to factor age, gender, race or appearance into the recruitment process.
Quick tip: Employers will expect you to have a good standard of written communication, so use our quick-and-easy CV Builder to ensure your CV doesn’t contain any silly typos or grammatical mistakes.
Structuring your CV
By breaking up your information into the following sections, recruiters will be able to navigate your CV with ease:
- Contact details
- Profile – A 5-10 line summary which highlights your relevant experience, skills, qualification and dental certifications.
- Work experience / Career history – Starting with your current or most recent role, list your work history.
- Education – Detail your educational background, putting particular focus on qualifications related to the dental industry.
- Interest and hobbies – If you have any interesting hobbies which demonstrate transferable skills or qualities, you can include them in this optional section.
Keep on reading to learn exactly what to include in each of the CV sections mentioned above.
CV Contact Details
The first thing you list on your CV should be your contact details, including your:
- Phone number
- Email address
Quick Tip: You only need to share your basic contact details. Rather than a full address, just list your town or city, for example, ‘Brighton’.
Dental nurse CV Profile
Most dental nurse job adverts receive lots of applications, so your CV needs to immediately grab the recruiter’s attention.
Your CV profile (or personal statement for trainee roles) is a great way to do this. It’s the first thing they’ll read, so you can instantly prove that you’ve got the qualities they’re looking for and that it’s worth spending their valuable time reading your CV.
Aim to create a short, snappy, 5-10 line paragraph which summarises your relevant skills, experience and qualifications/certifications.
Tips to consider when creating your profile:
- Before you even think about writing, spend some time carrying out some research and analysing the job description . You should aim to match the requirements of the job description as closely as you can in your profile.
- Recruiters won’t be impressed if your profile is packed with meaningless clichés, such as ‘enthusiastic team player’ or ‘dedicated hard worker’. Focus on putting across your hard skills, knowledge, achievements and qualifications instead.
- A lengthy profile is a complete no-go. Keep it short and snappy, sharing just enough information to prove that you’re a candidate worth considering, whilst enticing the reader to find out more about you.
What to include in your dental nurse CV profile?
- Level of experience – Give recruiters a summary of your experience level, whether that’s 5 or 10 years in the industry, that you’re newly certified, or your hopes of becoming a trainee dental nurse.
- Relevant qualifications – Dental nurses in the UK are required to attain certification with the General Dental Council (GDC), so make sure to highlight this, or any other relevant qualifications, if you have them.
- Work experience – Whether you’ve worked as a community dental nurse, in a private clinic, or in the NHS, you’ll need to summarise your work experience so far. If this will be your first dental nurse role, give a quick summary of your working life so far but highlight the transferable skills you’ve picked up.
- Skills – Highlight your core dental nurse skills, such as sterilizing dental instruments, health and safety, note-taking and taking x-rays. Inexperienced candidates should highlight relevant transferable skills, such as organisation, interpersonal skills and working under pressure.
- Key achievements – How have you made an impact in your previous dental nursing roles? Whether you played a part in handling a pressured emergency, or received exceptional feedback from a patient, packing your profile with evidence-backed achievements is a great way to impress recruiters.
Core skills section
Another great way to hook the reader’s attention is to include a list of your core skills , which you’ll place right underneath your CV profile.
Use your industry research, paired with the requirements listed in the job description, to perfectly match yourself to the role.
This will help recruiters to gauge your suitability for the role at a single glance, without having to dig through your entire CV.
With this said, don’t be tempted to lie about your skills – if you can’t match them, don’t include them. For trainee roles, recruiters just want to see your potential – lying on your CV is never a good idea.
Work experience/Career history
By now, the reader will eager to find out more about your relevant experience and working capabilities.
Starting with your most recent (or current) role, list your work experience to date, focusing on the skills you used, your day-to-day duties and key results/achievements made.
If you’re an experienced dental nurse with numerous roles under your belt, focus the detail on your most recent positions.
Quick tip: If you’re applying for a trainee role or your first role after gaining a dental nurse qualification, don’t worry if this section is short. You can still include other, less relevant roles, but make sure to focus on pinpointing the transferable skills you’ve gained.
These might include:
- Interpersonal skills, with the ability to work well with a wide range of people
- Great organisational and multitasking skills, with experience of juggling a variety of tasks
- Working as part of a team or supporting another team member
- Working well under pressure or dealing with emergencies
- Computer literacy
Wherever possible, you should also try to give tangible examples of how you’ve used these skills.
Structuring your roles
Recruiters hate reading through large blocks of text, so it’s vital to structure your roles with their needs in mind.
Break up the content by using my simple 3-step role structure, as shown below:
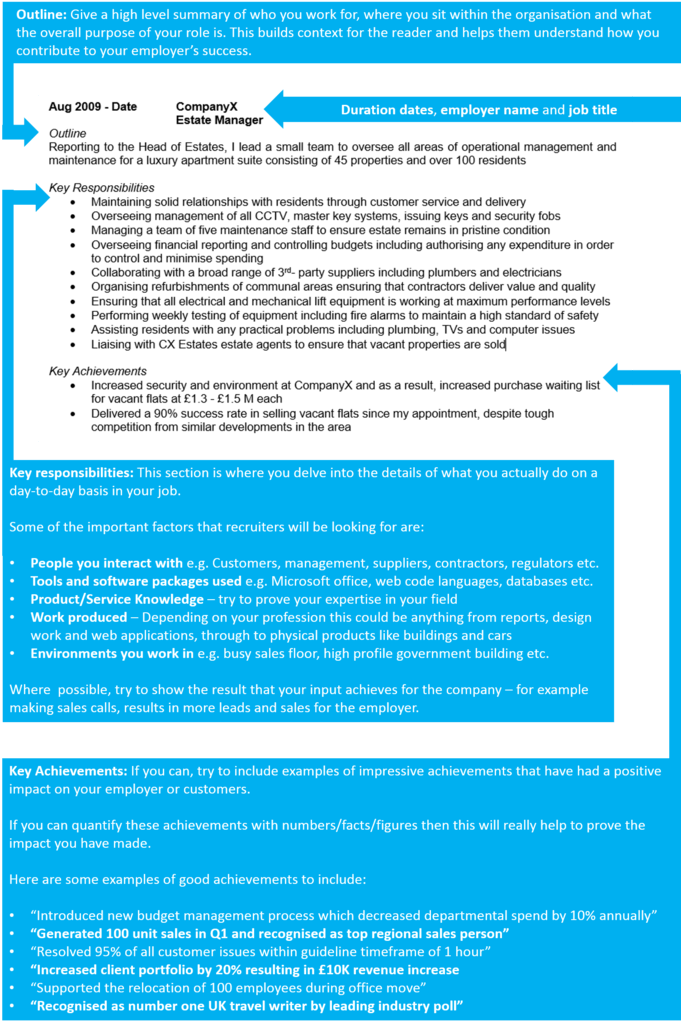
Start with a brief, 1-2 line overview of the role, describing the overriding purpose of your position, the type of company or organisation you worked for and who you supported in the role.
“Providing professional support to a team of 3 dentists within a busy private dental clinic, whilst providing ongoing care and advice to a range of patients with acute to chronic dental problems.”
Key responsibilities
Next, dive into the detail of your day-to-day duties within the role, using bullet points to aid readability.
- Setting up and sterilising dental instruments and equipmen t ready for patients.
- Taking notes to the patient’s dental record, direct from the dentist’s dictation.
- Provided essential support in procedures such as tooth extraction, dental prophylaxis and root canal.
- Ensuring that patients are as comfortable and as relaxed as possible during their treatment.
Key achievements
To prove the impact you made within your roles, note down some key results or achievements.
This could be a time you received exceptional feedback, won an award, improved processes, increase company sales or profits or played a vital part in an emergency procedure.
- Undertook sales training and increased product sales during patient visits, resulting in a sales boost of 25%.
- Received 97% positive customer comments during my time in the clinic.
- Received numerous unsolicited patient thank-you letters due to my empathetic and understanding nature.
- Decreased procedure set-up time by 25% in my first 3 months.
Now that you’ve given recruiters a round-up of your experience, they’ll be keen to find out about your qualifications/credentials.
You can train as a dental nurse with no prior experience or qualifications – just make sure you’re applying for a trainee role. You should still note down your highest qualifications in this section, such as your A-Levels or GCSEs.
Otherwise, dental nurses are required to be registered with the General Dental Council , which requires a formal qualification, such as a Foundation Degree in Dental Nursing .
So, highlight your registration and qualification details, noting the dates of competition and the institution/course provided you studied with.
Dental Nurse cover letter
Interests and hobbies
This is an optional section that should only be used if your hobbies and interests will add further depth to your CV.
For example, generic hobbies such as ‘socialising’ add no value to an application.
However, hobbies which display good communication or teamwork skills, or prove that you’re a committed and organised individual, may be worth including. This might be volunteering, being a part of a sports team, or following a creative pursuit such as playing an instrument.
Essential skills for your dental nurse CV
The required skillset for a dental nurse role will vary widely depending on the experience level – but generally, a qualified dental nurse will be expected to showcase the following hard skills:
Preparation – Preparing, sterilising and passing instruments to dentists and/or hygienists. Preparing and mixing dental materials.
Dental procedure support – Providing chairside support to dentists, therapists and hygienists during a range of dental procedures/treatments.
Patient support – Providing care, advice and reassurance to patients. Advising patients on oral hygiene.
Administration – Providing office support such as making appointments, taking payments and dealing with paperwork.
Health and safety – Ensuring that health and safety policies are adhered to and that all surgical areas and equipment are consistently cleaned and maintained. Undertaking infection control and decontamination procedures.
X-rays – Processing and filing x-rays.
Writing your dental nurse CV
Whether you’re looking to secure your first role as a dental nurse or are eager to step up into a senior role, an impactful CV is the key to success.
By following this guide, you’ll be able to write a CV which is highly tailored to the role, looks professional and seamlessly highlights why you’d make the perfect hire.
Remember to triple-check your CV before you send it off – it needs to be absolutely flawless.
Best of luck with your job search!
Appearances matter
Published: 03/06/2020

Eloise Meldrum considers professional self-image, dental nursing and patient perception
Self-image is very important in dentistry. Patients place their trust (and their oral health) in our hands so having a clean, professional and natural appearance is vitally important to promote and maintain that trust between any practice staff and its patients.
I like to promote a very professional image. I like to show patients and dentists that I am knowledgeable, committed and passionate about the industry. It’s important to show this to build a good relationship with both patient and dentist, so you show your drive, enthusiasm and professional pride.
The culture/brand of different practices do not necessarily impact how I present myself. I am always led by the GDC/ CQC standards in terms of professionalism, uniform, presentation and so on. The beauty of these standards is by adhering to them, you can be confident it will be acceptable in any practice.
As a locum, I usually wear just a black tunic, smart trousers and wipeable shoes. Other locums I have met have worn similar or the traditional scrubs. To be honest, I much prefer traditional scrubs. I have a selection of uniforms so would usually ask a practice for their preference so that I could match mine as closely as I can to theirs. Some practices have asked me to wear their scrubs which of course I’m always more than happy to do.
Keep a clean appearance, short and clean nails, no nail varnish, clean hair, tied up in a bun (most of the time) and clean uniforms daily. Minimal makeup and you can wear perfume but nothing over the top. We must remember that we are medical professionals so we need to represent our job description accurately. I always ask myself: ‘Would I be happy to be assisted by this person today?’ If the answer is ‘yes’ then that’s great! If it’s a ‘no’, then I will try to present myself better, for example to tie my hair a bit tighter etc.
I love grey, it communicates professionalism and is a bit of a different colour to see in the industry. I also loved the uniform I used to wear, which was a purple tunic and black trousers – very professional and different to the everyday navy. I’m not particularly fussy, and much more important is your overall presentation, cleanliness and professionalism.
Starring in a series of adverts for Belmont was an incredible experience. I am honoured to be chosen for the face of Belmont’s new Hygiene and Care Range, which will be seen all over the UK. It was all very enjoyable and I loved every moment. Belmont themselves were totally accommodating of me, ensuring I was comfortable and I appreciated being asked for my input on some photos due to my background in the industry. I never realised what went into photoshoots until I did this one, and I soon realised how much effort, care and attention goes into each photo, from the whole team photographer, model, to the team behind the camera with the vision.
Author: Eloise Meldrum
Please sign in or subscribe to continue reading.
The following article is restricted for Dental Nursing subscribers only. Please sign in to access the full article.
If you have any queries or require more information, Dental Nursing’s friendly customer services team is on hand to help. Call 01722 716997 or email [email protected] .
Subscribe to Dental Nursing below and get access to this article. Subscribing will enable you to:
- Update your knowledge in important areas of practice.
- Keep fully up-to-date with the latest developments taking place in clinical practice as they affect you.
- Access restricted content and our CPD platform.
Related articles

A warm congratulations
Mark Garner speaks with Amy Ciobanu about her passion for dental nursing and her recent winning of the ATU Dental Graduate Award.

Taking a look back
Claire Frisby reflects on her career.

Importance of appreciation
Preetee Hylton speaks with Shannon Wilkes about her dental nursing career and achievements.

Oral cancer ambassadors
Cancer charity invites dental nurses to become ambassadors.
.jpg?width=150&height=100&scale=canvas)
A crucial determinant of heal
A crucial determinant of health.

What I wish I could tell
What i wish i could tell my boss: ‘you made me feel so small’.

Fitness to Practise cases
New findings in gdc fitness to practise data.

Stress triggers in dentistry
When you need more than a stress ball.

Driving your development

Carving out your career path

1.8m not received treatment
Data shows 1.8 million people in scotland have not received dental treatment.

Oral mucosa 3D model
Researchers explore the mouth’s response to oral disease using a laboratory model.

Subscribe today
Get access to Dental Nursing's comprehensive CPD coverage ensuring that all dental nurses may achieve their full CPD requirements.
Click here for more information
- ALL MOSCOW TOURS
- Getting Russian Visa
- Top 10 Reasons To Go
- Things To Do In Moscow
- Sheremetyevo Airport
- Domodedovo Airport
- Vnukovo Airport
- Airports Transfer
- Layover in Moscow
- Best Moscow Hotels
- Best Moscow Hostels
- Art in Moscow
- Moscow Theatres
- Moscow Parks
- Free Attractions
- Walking Routes
- Sports in Moscow
- Shopping in Moscow
- The Moscow Metro
- Moscow Public Transport
- Taxi in Moscow
- Driving in Moscow
- Moscow Maps & Traffic
- Facts about Moscow – City Factsheet
- Expat Communities
- Groceries in Moscow
- Healthcare in Moscow
- Blogs about Moscow
- Flat Rentals
Healthcare in Moscow – Personal and Family Medicine
Emergency : 112 or 103
Obstetric & gynecologic : +7 495 620-41-70
About medical services in Moscow

Moscow polyclinic
Emergency medical care is provided free to all foreign nationals in case of life-threatening conditions that require immediate medical treatment. You will be given first aid and emergency surgery when necessary in all public health care facilities. Any further treatment will be free only to people with a Compulsory Medical Insurance, or you will need to pay for medical services. Public health care is provided in federal and local care facilities. These include 1. Urban polyclinics with specialists in different areas that offer general medical care. 2. Ambulatory and hospitals that provide a full range of services, including emergency care. 3. Emergency stations opened 24 hours a day, can be visited in a case of a non-life-threatening injury. It is often hard to find English-speaking staff in state facilities, except the largest city hospitals, so you will need a Russian-speaking interpreter to accompany your visit to a free doctor or hospital. If medical assistance is required, the insurance company should be contacted before visiting a medical facility for treatment, except emergency cases. Make sure that you have enough money to pay any necessary fees that may be charged.
Insurance in Russia

Travelers need to arrange private travel insurance before the journey. You would need the insurance when applying for the Russian visa. If you arrange the insurance outside Russia, it is important to make sure the insurer is licensed in Russia. Only licensed companies may be accepted under Russian law. Holders of a temporary residence permit or permanent residence permit (valid for three and five years respectively) should apply for «Compulsory Medical Policy». It covers state healthcare only. An employer usually deals with this. The issued health card is shown whenever medical attention is required. Compulsory Medical Policyholders can get basic health care, such as emergencies, consultations with doctors, necessary scans and tests free. For more complex healthcare every person (both Russian and foreign nationals) must pay extra, or take out additional medical insurance. Clearly, you will have to be prepared to wait in a queue to see a specialist in a public health care facility (Compulsory Medical Policyholders can set an appointment using EMIAS site or ATM). In case you are a UK citizen, free, limited medical treatment in state hospitals will be provided as a part of a reciprocal agreement between Russia and UK.
Some of the major Russian insurance companies are:
Ingosstrakh , Allianz , Reso , Sogaz , AlfaStrakhovanie . We recommend to avoid Rosgosstrakh company due to high volume of denials.
Moscow pharmacies

A.v.e pharmacy in Moscow
Pharmacies can be found in many places around the city, many of them work 24 hours a day. Pharmaceutical kiosks operate in almost every big supermarket. However, only few have English-speaking staff, so it is advised that you know the generic (chemical) name of the medicines you think you are going to need. Many medications can be purchased here over the counter that would only be available by prescription in your home country.
Dental care in Moscow

Dentamix clinic in Moscow
Dental care is usually paid separately by both Russian and expatriate patients, and fees are often quite high. Dentists are well trained and educated. In most places, dental care is available 24 hours a day.
Moscow clinics

«OAO Medicina» clinic
It is standard practice for expats to visit private clinics and hospitals for check-ups, routine health care, and dental care, and only use public services in case of an emergency. Insurance companies can usually provide details of clinics and hospitals in the area speak English (or the language required) and would be the best to use. Investigate whether there are any emergency services or numbers, or any requirements to register with them. Providing copies of medical records is also advised.
Moscow hosts some Western medical clinics that can look after all of your family’s health needs. While most Russian state hospitals are not up to Western standards, Russian doctors are very good.
Some of the main Moscow private medical clinics are:
American Medical Center, European Medical Center , Intermed Center American Clinic , Medsi , Atlas Medical Center , OAO Medicina .
Several Russian hospitals in Moscow have special arrangements with GlavUPDK (foreign diplomatic corps administration in Moscow) and accept foreigners for checkups and treatments at more moderate prices that the Western medical clinics.
Medical emergency in Moscow

Moscow ambulance vehicle
In a case of a medical emergency, dial 112 and ask for the ambulance service (skoraya pomoshch). Staff on these lines most certainly will speak English, still it is always better to ask a Russian speaker to explain the problem and the exact location.
Ambulances come with a doctor and, depending on the case, immediate first aid treatment may be provided. If necessary, the patient is taken to the nearest emergency room or hospital, or to a private hospital if the holder’s insurance policy requires it.
Our Private Tours in Moscow
Moscow metro & stalin skyscrapers private tour, moscow art & design private tour, soviet moscow historical & heritage private tour, gastronomic moscow private tour, «day two» moscow private tour, layover in moscow tailor-made private tour, whole day in moscow private tour, all-in-one moscow essential private tour, tour guide jobs →.
Every year we host more and more private tours in English, Russian and other languages for travelers from all over the world. They need best service, amazing stories and deep history knowledge. If you want to become our guide, please write us.
Contact Info
+7 495 166-72-69
119019 Moscow, Russia, Filippovskiy per. 7, 1
Mon - Sun 10.00 - 18.00

IMAGES
VIDEO
COMMENTS
Guidance. 9.1.1 You must treat all team members, other colleagues and members of the public fairly, with dignity and in line with the law.; 9.1.2 You must not make disparaging remarks about another member of the dental team in front of patients. Any concerns you may have about a colleague should be raised through the proper channels. 9.1.3 You should not publish anything that could affect ...
Front Office. Professional appearance in the workplace. Oct. 19, 2010. As an instructor for a dental assisting school, Tija Hunter, EFDA, has seen it all when it comes to appearance and dress. In this article, she tackles the subject of professional appearance and gives tips on how to project the right image in the dental profession.
Dental nurse 2017-2022 cycle PDP in place for remaining 4 years of my cycle to cover 35 hrs verifiable I have left. Mixed (NHS and private) general practice, part time. • Perform reception role when needed; • Perform sterilisation role when needed. • General population; • Large ethnic and cultural diversity. Personal development plan
dental disease and their application to patient management C 1.2* Describe and identify the clinical presentations of oral and dental diseases relevant to the role of a dental nurse and explain the principles underpinning their diagnosis, prevention, and treatment C 1.3 Explain the variance in disease presentation across diverse cultural and
A PDP is part of Clinical Governance - the government requires that all NHS clinicians have and use a PDP. A PDP involves updating, revisiting, stimulating ideas, identifying strengths and weaknesses, and prioritising and planning for your future career. Many people find the idea of reflecting, evaluating and making plans daunting and ...
CPD for dental professionals CPD is about keeping your professional skills and knowledge up to date.; Dental students and trainees Our dedicated hub for students and trainees will help and guide you along your journey to becoming a member of the dental team.; Dental education and training quality assurance We set the standards for dental education and training, and check to ensure those ...
Soft skills are used in personal and professional life. These soft skills help to organize, plan and manage, and track changes during the course of the growing dental practices. However, understanding of the soft skills in practice management, its simplicity and complex contexts of practice is essential.
Roles of the dental nurse with both environments: Patient comfort. Chair side assistance including moisture control, mixing of materials. Preparation of the clinical environment and equipment for a procedure. Maintaining and recording patient history. Extended duty dental nursing roles: Oral health advice.
The dental nurse is an essential member of the dental team. The dentist and dental nurse need to have a clear understanding of their working relationship and the factors that affect it, in order ...
Reflection and Personal Development Plans. The use of reflection has become a routine part of many professions such as teaching and nursing. In dentistry we have been slower to adopt it as way of highlighting development needs. You might think, how can reflection help me, either to learn things or highlight an area that I need to develop further.
Here are some reasons to consider your self-presentation as a professional: increases your ability to influence a customer. provides a representation of a brand or an organisation. increases the likelihood of building long-lasting relationships. encourages engagement from customers, which can improve sales.
5. Record the risk assessment findings - to prove compliance, to provide a reference for all users, to ensure all staff are fully informed of the potential hazards in the dental workplace. 6. Review the assessment process - on a regular basis to ensure that hazardous events or injuries do not occur.
Presentation of main results ... collected the baseline measures. A dental nurse‐educator allocated the participants according to the randomisation grid and administered the immediate post‐intervention measures. ... Patients were asked to examine the 6 teeth for disclosed plaque once each week following personal oral hygiene. During follow ...
Personal presentation is a communication skill, and communication is one of five important life and work skills you can build as a Young Professional. Personal presentation means the way you present yourself in everyday situations, and more stressful ones like job interviews. How you appear to the world can have a major impact on your ability ...
Dental nurses from across the country had the opportunity to get together once again and enjoy everything the show had to offer. Among the highlights of the event, the Dental Nurses' Forum was packed with expert speakers and enlightening topics, such as Hannah Grieves' lecture titled "Stress management for dental nurses.".
Trade waste includes items such as dental equipment (dental chairs, curing lights, portable suction units, etc.), as well as commercial electronic waste like computer screens, tele-visions, fluorescent lighting tubes and batteries. Figure 1.24 Blue-lidded sharps box. Figure 1.25 An orange hazardous waste sack.
CV templates Whilst writing your own dental nurse CV, a professional and well-organised structure and format - as shown in the CV example above - should be your goal.. This high standard of presentation allows recruiters to easily navigate through the candidate's experience, whilst allowing their key skills and achievements to stand out.
Call 01722 716997 or email [email protected] . Subscribe to Dental Nursing below and get access to this article. Subscribing will enable you to: Update your knowledge in important areas of practice. Keep fully up-to-date with the latest developments taking place in clinical practice as they affect you.
Here are the steps for writing a dental nurse CV: 1. Choose a template. Using a dental nurse example CV or template can help you structure your CV, ensuring it's easy to read. Look at various templates that match your level of experience or the presentation style you would like to use.
Dental care in Russia is usually paid for either separately or as an additional extra on a private healthcare insurance package. If you decide to go to a non-private dental clinic, you might need to take a Russian speaker with you. Dental clinics in Russia offer everything from preventative and restorative treatment to cosmetic treatment, and ...
These include 1. Urban polyclinics with specialists in different areas that offer general medical care. 2. Ambulatory and hospitals that provide a full range of services, including emergency care. 3. Emergency stations opened 24 hours a day, can be visited in a case of a non-life-threatening injury.
Job Types: Full-time, Part-time Related keywords: cna, nursing assistant, cna nursing assistant cna, certified nursing assistant, cna nursing assistant' ' Work Remotely. No; Job Type: Full-time. Pay: $17.00 - $19.00 per hour. Benefits: 401(k) Dental insurance; Flexible schedule; Health insurance; Paid time off; Vision insurance; Schedule: 8 ...
The EMC group is constituted of three distinct medical centers: The European Medical Center (EMC), the European Dental Center (EDC), and the Department of Assisted Fertility. All three centers are located in the heart of the city, close to each other, making it convenient for our patients, and physicians alike, to rotate between centers ...