- Research article
- Open access
- Published: 08 November 2012

Public health interventions in midwifery: a systematic review of systematic reviews
- Jenny McNeill 1 ,
- Fiona Lynn 1 &
- Fiona Alderdice 1
BMC Public Health volume 12 , Article number: 955 ( 2012 ) Cite this article
26k Accesses
20 Citations
10 Altmetric
Metrics details
Maternity care providers, particularly midwives, have a window of opportunity to influence pregnant women about positive health choices. This aim of this paper is to identify evidence of effective public health interventions from good quality systematic reviews that could be conducted by midwives.
Relevant databases including MEDLINE, Pubmed, EBSCO, CRD, MIDIRS, Web of Science, The Cochrane Library and Econlit were searched to identify systematic reviews in October 2010. Quality assessment of all reviews was conducted.
Thirty-six good quality systematic reviews were identified which reported on effective interventions. The reviews were conducted on a diverse range of interventions across the reproductive continuum and were categorised under: screening; supplementation; support; education; mental health; birthing environment; clinical care in labour and breast feeding. The scope and strength of the review findings are discussed in relation to current practice. A logic model was developed to provide an overarching framework of midwifery public health roles to inform research policy and practice.
Conclusions
This review provides a broad scope of high quality systematic review evidence and definitively highlights the challenge of knowledge transfer from research into practice. The review also identified gaps in knowledge around the impact of core midwifery practice on public health outcomes and the value of this contribution. This review provides evidence for researchers and funders as to the gaps in current knowledge and should be used to inform the strategic direction of the role of midwifery in public health in policy and practice.
Peer Review reports
The reproductive period offers maternity care providers the opportunity to maximise the health and well-being of women and their families potentially impacting on public health outcomes, both short and long term. Although all maternity care providers who engage with pregnant women are presented with such opportunities, it is the midwife that could have the most significant impact from regular contact and building of relationships through continuity of care. There are interventions that could be implemented by midwives, which potentially would have a public health impact but it is important such interventions are evidence based. Recognition of the importance of the relationship between public health and midwifery was highlighted when a general review of midwifery in the UK [ 1 ], named public health as one of five key areas of interest. While the review specifically focused on midwifery in the UK, the importance of preventative public health interventions during pregnancy and the postnatal period has been emphasized on a wider scale. Millennium Development Goal 5 focuses on improving maternal health specifying a secondary target aim to achieve universal access to reproductive health by 2015 [ 2 ]. Antenatal care and adolescent pregnancy are specifically mentioned as key to achieving this target, both of which are acknowledged widely, as areas of interest to public health [ 3 , 4 ]. Other areas of national and international interest, which impact on population health (both women and families), include rising caesarean section rates and other interventions during childbirth [ 5 – 7 ], the importance of positive parenting in the early postnatal period [ 8 ] and perinatal mental health [ 9 ]. Within these areas there is opportunity for evidence based public health interventions to be implemented with a view to potentially improving the long term health of women and families.
Aim of the review
This paper presents an update of a systematic review of systematic reviews conducted in 2009. The aim of the 2009 review was to evaluate the effectiveness of interventions relevant to the public health role of the midwife. The 2009 review was commissioned and conducted within the context of the Midwifery 2020 initiative. The final report of the Midwifery 2020 initiative (Delivering Expectations) and full report of the systematic review of reviews [ 10 ] are available freely online from: http://www.midwifery2020.org . A systematic review of systematic reviews was selected as the methodology, given the breadth of this topic area and the timescale of the project. This paper outlines the review methodology and builds on the original review findings by providing new and updated information about effective high quality public health interventions which could be implemented by midwives or other health care providers for women during pregnancy and the postnatal period who have a similar role, for example, public health nurses, obstetric nurses, labour and delivery nurses or health visitors.
The Preferred Reporting Items of Systematic reviews Meta-Analyses (PRISMA) guidelines was adhered to when conducting this review [ 11 ]. A systematic search strategy was formulated and definitive search terms used relative to key public health topics within midwifery following consultation with Expert Advisory Group members and Midwifery 2020 Public Health Work Stream members. Seven key areas were identified as relevant to the public health role of the midwife, which included: screening; vulnerable groups; breast feeding; mental health and wellbeing; education and support; childbirth and lifestyle factors. The complete list of search terms is available from McNeill et al. [ 10 ].
Search strategy
Databases searched included: MEDLINE, PubMed, EBSCO (CINAHL/British Nursing Index), MIDIRS Online Database, Web of Science, The Cochrane Library, CRD (NHS EED/DARE/HTA) and EconLit. Eligibility criterion included reviews published from 1999 onwards; English language publications and reviews originating from economically developed countries as indicated by membership of the Organisation for Economic Co-operation and Development (OECD). An additional search was conducted of the National Institute for Health and Clinical Excellence, UK (NICE) website to identify key publications or findings from systematic reviews within guidelines. Reference lists of identified reviews were manually searched for additional relevant reviews. The searches were initially conducted in November 2009 and updated in October 2010. The titles and abstracts were obtained and the decision process for eligibility was conducted by all members of the project team in collaboration (JM, FL & FA). Full text was obtained of all eligible reviews and those whose eligibility could not be discerned from reading the abstract. Eligible systematic reviews also had to publish a clearly identified search strategy or detail the reference databases used.
Data extraction
Data were extracted on: number of papers included in the review; methodological details; midwifery intervention; outcome measures and results. Data were systematically extracted using a data extraction form by individual project team members and verified by one other project team member. The project team subsequently met to discuss and achieve consensus regarding any contentious issues. A parallel process of developing a logic model to act as an overarching framework to inform forward planning was also conducted. Logic models are essentially a conceptual framework, which can be used for evidence‐based decision making and planning [ 12 ]. The model is composed of midwifery inputs and activities, producing a logical pathways to short, medium and long term public health outputs.
Quality assessment and effectiveness of reviews
It is important to consider both the type of evidence included in reviews i.e. was the review restricted to randomised trials only or were other types of studies included and also assess how well the review was conducted methodologically. As such, a two stage process was employed: initially the level of evidence was graded and secondly, the methodological quality was assessed. Recognised frameworks were used to support this process [ 13 , 14 ]. In the hierarchy of evidence, randomised controlled trials are perceived as the gold standard and as the aim of this paper is to present high quality evidence, an evidence grade was given to each review based on the Scottish Intercollegiate Guidelines Network [ 13 ] framework in order to distinguish between different levels of evidence. This framework grades the associated risk of bias based on the level of evidence in a hierarchal manner from a grade of 1++ (meta analysis and RCT evidence) through to 4 (expert opinion), as outlined in Table 1 . The SIGN framework was modified as this review was restricted to systematic reviews and therefore reviews could only be graded as 1++, 1+, 1- or 2++. This paper only presents evidence which was graded 1- or above; any review graded below 1- was not deemed eligible for inclusion. Following selection of the type of evidence, the second stage focused on the methodology of eligible reviews. Clarke [ 15 ] suggests the successful interpretation of results from systematic reviews should consider the methodological conduct of the review. The methodological quality of included reviews was assessed and rated as low, medium or high quality. Appraisal of methodological quality was based on Smith et al. [ 14 ], which contains similar elements to other tools used to assess review quality, for example, the AMSTAR tool [ 16 ]. Reviews were graded as high quality if they included evidence of a search strategy, selection and inclusion criterion, assessment of publication bias and assessment of heterogeneity. Reviews were rated as medium quality if no evidence of assessment of heterogeneity or publication bias was provided and low quality reviews were those which provided evidence of a search strategy only. Effectiveness of interventions was evaluated using a similar approach to van Sluijs et al. [ 17 ]. A differentiation was made between reviews which reported a statistically significant difference (P<0.05), therefore referred to as effective and those which reported no difference in effect between control and intervention group and are referred to as inconclusive or not effective (as appropriate). This paper focuses specifically on interventions which are evidenced by a statistically significant meta analysis or where the intervention is supported by a generally positive trend of results when a meta analysis was not possible. Reviews have been included where a small number of studies reported statistically significant positive effect of the intervention however the wider interpretation of these results is limited. As outlined previously, the aim of the original review was to identify any public health intervention relevant to midwifery. However for the purpose of this paper the focus was to report on public health interventions relating to midwifery that demonstrated a statistically significant effect in favour of the intervention (referred to subsequently as effective interventions for the sake of brevity). Reviews graded 1- or above and of high methodological quality which reported evidence of no effect, are not discussed in this paper. However, they have been summarised in Table 2 [ 18 – 23 ]. In the case of any disagreement regarding grading of evidence, quality appraisal of reviews or effectiveness of the intervention, consensus was reached by discussion between all three authors.
Data synthesis
A narrative review is provided for each of the systematic reviews and in table format the number and date range of papers included, intervention(s), primary outcome or other public health outcomes of interest, results (including key statistical findings e.g. p values or odds ratios) are described and whether the review included a meta analysis or not. It was not expected that a quantitative analyses would be conducted given the diversity of interventions across the broad subject of public health.
In total 214 systematic reviews were eligible of which 91 reported on effective interventions and 117 found no effect or were inconclusive. This paper only reports on high quality reviews with a level of evidence grading above 1-. Of the 91 systematic reviews which reported on effective interventions, 36 were identified which were graded as evidence level 1- or above and rated as high quality. The flow chart in Figure 1 presents the sequential process of identifying reviews eligible for inclusion in this paper. An overview of the key findings in relation to interventions demonstrating a statistically significant effect in favour of the intervention from good quality reviews will be presented in the following sections. A summary of included reviews is provided in Table 3 . The findings in this paper are presented chronologically through the reproductive period: preconceptual; antenatal; intranatal and postnatal. Within each section the reviews on similar broad topics have been further categorised: antenatal (screening; supplementation; support; education; mental health); intranatal (clinical care; environment); postnatal (breast feeding; mental health; education; support). The findings section also presents the logic model which was developed in parallel with the searching and analysis of reviews. Logic models enable the visualisation of how interventions or programmes work and the expected outcomes [ 24 ] and have been used to consider the strategic public health benefit of midwifery practice both in the short and long term [ 25 ].
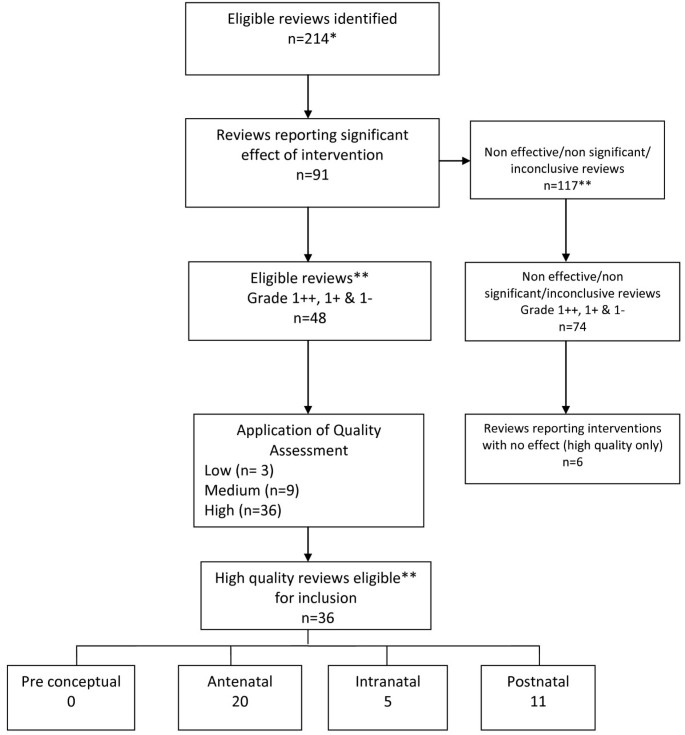
Identification of effective reviews of high quality *some reviews which were included at the request of funder have been excluded from this paper eg economic reviews (n=6) **non significant, non effective or inconclusive reviews, reviews graded 2++,2+ or 2- and medium or low quality reviews are not discussed in this paper.
Findings -effective interventions
Pre conceptual.
There were no high quality reviews that reported on effective interventions in the pre conceptual period.
The majority of reviews reporting effective interventions were relevant to the antenatal period (n=20). Included reviews have been grouped into screening, supplementation, support, education and mental health.
Reviews (n=4) related to screening reported on interventions relating to ultrasound [ 26 , 27 ], lower genital tract infection screening [ 28 ] and the use of decision making aids [ 29 ]. Bricker et al. [ 26 ] conducted a large Health Technology Assessment review on the clinical and cost effectiveness and women’s views of USS. The review comprised of three systematic reviews on routine ultrasound in early pregnancy, routine ultrasound in late pregnancy and routine Doppler ultrasound in pregnancy which were published in the Cochrane database around the time of Bricker et al. [ 26 ] however, all have since been updated or revised in the Cochrane database, one of which has been included in this paper. The final conclusions of Bricker et al. [ 26 ] indicated that a two stage regimen of USS in pregnancy, one in early pregnancy (booking USS) and a second anomaly USS around 20 weeks, was recommended. Whitworth et al. [ 27 ] reviewed the use of ultrasound for fetal assessment in early pregnancy and concluded that it reduces failure to detect multiple pregnancy (RR 0.07 95% CI 0.03-0.17) and accuracy of gestational dating may reduce the number of inductions of labour for post term gestation (RR 0.59; 95% CI 0.42-0.83). The authors also reported there was no reduction in adverse outcomes or health service use by mothers or infants and long term follow up did not indicate detrimental effect on children’s physical or mental development. The impact of antenatal screening for lower genital tract infection for preventing preterm delivery was reviewed by Sangkomkamhang et al . [ 28 ]. The review included one large RCT (n=4155), which indicated that preterm birth before 37 weeks was significantly lower in a group of women randomised to a screening programme before 20 weeks’ gestation (RR 0.55; 95% CI 0.41-0.75). The review provides evidence to suggest there may be some benefit to introducing a universal screening programme for lower genital tract infection; however the results are based on the findings of one study. O’Connor et al. [ 29 ] conducted a review on the use of decision aids for people facing screening decisions. The meta analysis indicated that the use of decision aids, such as leaflets or DVD’s are better than usual care and resulted in: greater knowledge (MD 15.2 out of 100; 95%CI 11.7 to 18.7), perception of risk (RR 0.6; 95% CI 0.5 to 0.8), lower decisional conflict related to feeling uninformed (MD −8.3 of 100; 95% CI −11.9 to −4.8), lower decisional conflict related to personal values (MD −6.4; 95% CI −10.0 to −2.7), reduced the proportion of people who were passive in decision making (RR 0.6; 95% CI 0.5-0.8) and reduced the proportion of people who remained undecided post intervention (RR 0.5; 95% CI 0.3-0.8). Although the results suggest decision aids are effective, the effect size was not consistent across studies and only three of the included studies related directly to antenatal screening.
Supplementation
Eight reviews [ 30 – 37 ] considered supplementation during pregnancy including iron, micronutrients, folic acid, calcium and Long Chain-Poly Unsaturated Fatty Acids (LC-PUFA’s). Two reviews [ 30 , 31 ] focused on folic acid supplementation, both of which concurred that the risk of neural tube defect was significantly reduced with supplementation: Blencowe et al., [ 30 ]; 70% reduction; 95% CI 35-86 and Lumley et al., [ 31 ]; RR 0.28; 95% CI 0.13-0.58. Iron supplementation during pregnancy was reviewed by Pena-Rosas and Viteri [ 32 ] who included 49 trials relating to the prevention of iron deficiency or anaemia at term. The authors concluded that daily iron supplementation was associated with increased haemoglobin before birth (MD 6.00; 95% CI 2.75-9.25) and reduced risk of anaemia at term (RR 0.46; 95% CI 0.29- 0.72) based on meta analyses of high quality trials only. Shah et al. [ 33 ] reviewed multi-micronutrient supplementation on pregnancy outcomes and reported there was a reduction in the risk of low birth weight amongst women given micronutrient supplementation (12 studies, RR 0.81; 95% CI 0.73-0.91) and iron-folic acid supplementation (RR 0.83; 95% CI 0.74-0.93) compared to placebo. The mean birth weight was higher (11 studies; WMD 54g; 95% CI 36-72g) in infants born to mothers who had micronutrient supplementation compared to iron-folic acid supplementation (no difference with placebo).
Calcium supplementation was the focus of three reviews [ 34 – 36 ]. Hofmeyr et al. [ 34 ] reported a reduction in pre-eclampsia (RR 0.68; 95% CI 0.57-0.81) and fewer babies born <2500g (RR 0.83; 95% CI 0.71-0.98). However the benefits seen were from small trials and not observed in the largest trial included. Hofmeyr et al. [ 35 ] reported that with supplementation a reduction in blood pressure (RR 0.7; 95% CI 0.57-0.86), pre-eclampsia (RR 0.48; 95% CI 0.33-0.69) and maternal death/morbidity (RR 0.80; 95% CI 0.65-0.97) was noted and advocated research to investigate calcium supplementation at community level. The most recent review [ 36 ] conducted by several of the same authors as Hofymeyr et al. [ 34 ] on calcium supplementation concluded that there was a reduced risk of increased blood pressure (RR 0.65; 95% CI 0.53-0.81) and preeclampsia (RR 0.45; 95% CI 0.31-0.65). The effect was greatest for high risk women (RR 0.22; 95% CI 0.12-0.42) and women with low baseline calcium (RR 0.36; 95% CI 0.20-0.65). Maternal death or serious morbidity was reduced (RR 0.80; 95% CI 0.65-0.97) although this was mostly in low risk women and women with low calcium and there was no effect on preterm births, stillbirth or death before discharge. Horvath et al. [ 37 ] reviewed the effect of advising high-risk pregnant women to take LC-PUFA supplementation on a number of pregnancy outcomes. The authors found a significantly lower rate of PTD <34 wks (RR 0.39; 95% CI 0.18-0.84) although this result was based on two trials (n=291). There was no effect on duration of pregnancy, PTD <37 wks, infant birth weight or the occurrence of IUGR. Although significant, the authors concluded that there was not enough evidence to recommend routine use of LC-PUFA supplements by high-risk women and that further research involving larger sample sizes was needed.
Three reviews [ 38 – 40 ] considered different types of supportive interventions for women during pregnancy. These ranged from using midwifery models of care to provision of emotional support to reduce the risk of preterm delivery or low birth weight infants. Hatem et al. [ 38 ] reviewed midwife led models of care versus other models of care and concluded that the majority of women should be offered midwifery led care. Women who had midwife led models of care were less likely to experience antenatal hospitalisation (RR 0.90; 95% CI 0.81-0.99), use of regional analgesia (RR 0.81; 95% CI 0.73-0.91), episiotomy (RR 0.82; 95% CI 0.77-0.88) and instrumental delivery (RR 0.86; 95% CI 0.78 to 0.96) and were more likely to experience no intrapartum analgesia/anaesthesia (RR 1.16; 95% CI 1.05-1.29), vaginal delivery (RR 1.04; 95% CI 1.02-1.06), to feel in control during childbirth (RR 1.74; 95% CI 1.32-2.30), attendance at birth by a known midwife (RR 7.84; 95% CI 4.15-14.81) and initiate breastfeeding (RR 1.35; 95% CI 1.03 to 1.76). In addition, women who were randomised to receive midwife-led care were less likely to experience fetal loss before 24 weeks’ gestation (RR 0.79; 95% CI 0.65-0.97). There was no difference between groups for birth by caesarean section (RR 0.96; 95% CI 0.87-1.06) and no statistically significant differences in fetal loss/neonatal death of at least 24 weeks (RR 1.01; 95% CI 0.67-1.53) or fetal/neonatal death overall (RR 0.83; 95% CI 0.70-1.00) and their babies were more likely to have a shorter length of hospital stay (mean difference in days: -2.00; 95% CI −2.15 to −1.85). Hodnett & Fredericks [ 39 ] assessed the value of emotional support to women who were judged, by a health professional, to be at increased risk of preterm delivery or having a low birth weight baby. No significant effect was detected for either outcome, however, women receiving support interventions were significantly less likely to undergo a caesarean section (RR 0.88; 95% CI 0.79-0.98) and were more likely to terminate their pregnancy (RR 2.96; 95% CI 1.42-6.17). There was also a trend towards improvement in maternal psychosocial outcomes although this was not significant. Denis & Kingston [ 40 ] reviewed the effect of telephone support during pregnancy and early postpartum period specifically on smoking, preterm birth, low birth weight, breast feeding and postpartum depression. The authors report a positive effect on breast feeding (3 trials; n=618; RR=1.18; 95% CI 1.05-1.33), low birth weight (3 trials; n=2,027; RR=0.78; 95% CI 0.63-0.97) and postpartum depression at 4 weeks (RR 0.24; 95% CI 0.06-1.00) and 8 weeks (RR 0.30; 95% CI 0.10-0.92), although all were from small numbers of trials and the finding on postpartum depression was from one pilot trial including 42 women.
Educational interventions in the antenatal period were the focus of four systematic reviews [ 41 – 44 ] that considered education about pelvic floor muscle training (PFMT) and promotion of smoking cessation in pregnancy Lumley et al. [ 41 ] reviewed the effect of interventions for promoting smoking cessation and included 72 studies of which 56 were RCT’s. Interventions to encourage cessation of smoking had a significant effect on the number of women smoking; 6 out of every 100 stopped, and a reduction in the number of cigarettes smoked by women was also evident. There was a significant reduction of smoking in late pregnancy (RR 0.94; 95% CI 0.93-0.96), reduction in LBW (RR 0.83; 95% CI 0.73 -0.95), preterm birth (RR 0.86; 95% CI 0.74-0.98) and an increase in mean birth weight (53.91g; 95% CI 10.44g - 95.38g). Naughton et al. , [ 42 ] reviewed the use of self help interventions for smoking and reported greater likelihood of quitting compared to usual care (13.2% v 4.9%; OR 1.83; 95% CI 1.23-2.73). The cost effectiveness of this method was also emphasised, however, further research is necessary to determine the intensity level of the intervention to maximise effectiveness. Hay-Smith et al. [ 43 ] and Lemos et al. [ 44 ] reviewed pelvic floor muscle training and concluded that for primigravida women PFMT was effective. Hay-Smith et al. [ 43 ] reported that women without prior incontinence were less likely to report incontinence in late pregnancy (RR 0.44; 95% CI 0.30-0.65) and up to 6 months postpartum (RR 0.71; 95% CI 0.52-0.97) similar to Lemos et al. [ 44 ] who reported significantly reduced development of urinary incontinence from 6 weeks to 3 months after delivery (OR 0.45; 95% CI 0.3-0.66; 4x RCT; n=675). Pregnant women with persistent incontinence 3 months after delivery and received PMFT were less likely to report urinary incontinence at 12 months post delivery (RR 0.79; 95% CI 0.70-0.90) and less likely to report faecal incontinence at 12 months (RR 0.52; 95%CI 0.31-0.87) [ 43 ].
Mental health
One review by Dennis & Creedy [ 45 ] considered interventions to prevent postnatal depression and all but one involved an intervention from a health professional. The authors reported that preliminary evidence suggests that intensive postnatal nursing home visits with at risk mothers assisted prevention of postpartum depression (RR 0.67; 95%CI 0.51-0.89).
Eligible systematic reviews relevant to the intranatal period yielded the smallest number in comparison to either the antenatal or postnatal periods. Five reviews [ 46 – 50 ] were included in this section and considered either clinical care during labour/delivery or the birthing environment.
Clinical care
Cluett & Burns [ 46 ] reviewed immersion in water for labour or birth (n=11) and reported from a meta analysis of 6 RCT’s. There was evidence to indicate that immersion in water for the first stage of labour significantly reduced the rate of epidural, spinal, paracervical analgesia and anaesthetic analgesia (478/1254 versus 529/1245; OR 0.82; 95% CI 0.70-0.98; p 0.025). However further research is required on other outcomes where there was no difference identified including assisted vaginal deliveries, C/S, perineal trauma, maternal infection, Apgar score < 7 at 5 mins, neonatal unit admissions or neonatal infection rates. Rabe et al. [ 47 ] reviewed delayed umbilical cord clamping and indicated from a meta analysis that there are benefits for both term and preterm infants. A delay of 30–120 seconds of cord clamping reduced the need for transfusions (RR 2.01; 95% CI 1.24-3.27, p=0.0049) and intraventricular haemorrhage (RR 1.74; 95% CI 1.08-2.81, p=0.022) in infants born <37 weeks [ 47 ]. Although the short term benefits are clear, further longitudinal work is needed to clarify the long term benefits.
Environment
The birth setting was the subject of four reviews although all were on different aspects. Hodnett et al. [ 48 ] reviewed the evidence regarding alternative versus conventional institutional settings for birth, which did not include any trials conducted in free standing birth centres. The review reported that for women allocated to the intervention (alternative setting) there was a significant increased likelihood of no analgesia/anaesthesia (RR 1.17; 95% CI 1.01-1.35), spontaneous vaginal delivery (RR 1.04; 95% CI 1.02-1.06), very positive views of care (RR 1.96; 95% CI 1.78-2.15), breastfeeding rates at 6–8 weeks (RR 1.04; 95% CI 1.02-1.06) and decreased episiotomy rate (RR 0.83; 95% CI 0.77-0.90). There was no effect on serious perinatal or maternal morbidity or mortality. Continuous support during childbirth was reviewed by Hodnett et al. [ 49 ]. The intervention involved one to one support during labour and found increased likelihood of shorter labour (WMD −0.43 hours; 95% CI −0.83 to −0.04), spontaneous vaginal delivery (RR 1.07; 95% CI 1.04 to 1.12) and were less likely to have intrapartum analgesia (RR 0.89; 95% CI 0.82- 0.96) or report dissatisfaction with childbirth experience (RR 0.73; 95% CI 0.65- 0.83). The authors only reported on outcomes where at least four trials were included in the meta analysis and highlighted that, generally, continuous intrapartum support was associated with greater benefits when it was not a member of hospital staff, when it began in early labour and in settings where epidural was not routinely available. Hodnett et al. [ 49 ] concluded that continuous support should be the norm rather than the exception for all women and further research is required as to the effectiveness of doula or lay support.
One review considered interventions aimed at reducing caesarean section rates [ 50 ]. Chaillet & Dumont [ 50 ] reported from a meta analysis that regular audit, detailed feedback regarding aspects of caesarean section performance (responsibility for decision making, rates, review of cases in clinical practice and multi faceted strategy approaches, such as development of guidelines, education of health professionals and women about vaginal birth after caesarean section (VBAC) were effective for reducing the caesarean section rate (RR 0.81; 95% CI 0.75-0.87). Details of relative risk for each type of strategy are included in Table 3 .
Eleven reviews [ 51 – 61 ] reporting on effective interventions related to the postnatal period. The reviews ranged across four areas: breast feeding; mental health; education and support.
Breast feeding
Reviews on this topic generally related to either support or promotion of breastfeeding. Britton et al. [ 51 ] reviewed the evidence in relation to support for breastfeeding mothers and key findings indicated that all forms of extra support for any breastfeeding (exclusive or partial) increased the duration of breastfeeding (RR 0.91; 95% CI 0.86-0.96) and the effect was greater for exclusive breastfeeding (RR 0.81; 95% CI 0.74-0.89). These findings were supported by Chung et al. [ 52 ] and Sikorski et al. [ 53 ]. Breastfeeding interventions included in both Britton et al. [ 51 ] and Chung et al. [ 52 ] involved formal or structured breastfeeding education, informal breastfeeding education or breastfeeding support either lay or professional. Chung et al. [ 52 ] from a meta analysis of 34 studies reported that breastfeeding interventions were effective in relation to increasing short term (1-3mths) and long-term (6-8mths) exclusive breastfeeding (RR 1.28; 95% CI 1.11-1.48 and RR 1.44; 95% CI 1.13-1.84) although statistically significant heterogeneity was noted for short term exclusive breast feeding (I 2 =55%; p= 0.006). The authors also highlighted an increased rate (22%) of any (RR 1.22; 95%CI 1.08-1.37) and exclusive (RR 1.65; 95%CI 1.03-2.63) short term breastfeeding with interventions that included a component of lay support. Sikorski et al. [ 53 ] reviewed additional support versus standard care and concluded that additional professional support was more beneficial than standard care for duration of any breastfeeding (RR 0.89, 95% CI 0.81-0.97; 10xRCT; n=19,696) and additional lay support was effective in reducing the cessation of exclusive breastfeeding (RR 0.66; 95% CI 0.49-0.89; 5xRCT; n=2530). Effect sizes for interventions with an antenatal education element (RR 0.85; 95% CI 0.70-1.04) were not statistically significant, while those with a postnatal element alone were (RR 0.80; 95% CI 0.80-0.96). Four trials using WHO/UNICEF training showed significant benefit in prolonging exclusive breastfeeding (RR 0.70; 95% CI 0.53-0.93), but were highly heterogeneous. The authors highlight the need to assess support in different settings especially with low rates, conduct economic analyses and use qualitative research to explore specific elements of support. Dyson et al. [ 54 ] focused on breastfeeding initiation rates and indicated from a meta analysis of five studies (n=582) that breastfeeding education had a significant effect on increasing initiation rates (RR 1.57, 95% CI 1.15-2.15, p=0.005) compared to standard care in low income groups although substantial statistical heterogeneity was noted (I 2 =53.4%). Early skin to skin contact was reviewed by Moore et al. [ 55 ] who reported statistically significant effects of early skin to skin on breastfeeding at one to four months post birth (OR 1.82, 95% CI 1.08-3.07) and breastfeeding duration (WMD 42.55, 95% CI −1.69 -86.79). In this review, data from more than two trials were only available for a small number of outcomes (8/64). Ahmed & Sands [ 56 ] reviewed breast feeding interventions. While the authors were unable to conduct a meta analysis they found from individual trials, statistically significant results relating to kangaroo care, peer counselling, in home breast milk measurement, and post discharge lactation support for improving breast feeding outcomes.
One review focused on improving maternal mental health and considered postnatal psychological and psychosocial interventions [ 57 ]. Dennis & Hodnett [ 57 ] reported that any psychosocial or psychological intervention compared to usual postpartum care was associated with a reduction in the likelihood of continued depression from their review of nine trials. Examples of psychosocial and psychological interventions reviewed included non-directive counselling, supportive interactions, delivered via telephone, home or clinic visits, or individual or group sessions in the postpartum period by a health professional or lay person, cognitive behavioural therapy and interpersonal psychotherapy.
Education and support
One review considered support for women in relation to weight reduction in the post partum period [ 58 ] focusing on the effect of diet or exercise or both for reducing weight after childbirth. They found that women who took part in a diet (1 trial; n=45; WMD −1.70 kg; 95% CI −2.08 to −1.32; z=8.73; p<0.00001), and women on a diet plus exercise programme (4 trials; n=169; WMD −2.89 kg; 95% CI −4.83 to −0.95; z=2.92; p<=0.00049), lost significantly more weight than women in the usual care. The authors also noted that there was no adverse effect on breastfeeding, although cautioned that further research is necessary to confirm this finding. Three reviews considered extra support for vulnerable groups of women in the form of home visiting or parenting interventions [ 59 – 61 ]. Corcoran & Pillai [ 59 ] reviewed rates in repeat pregnancy following the introduction of hospital-based programmes providing education and counselling to a sample of adolescent mothers. They found that although there was a 50% reduction in the odds of repeat pregnancy compared to comparison-control conditions at 19months (OR 0.474; 95% CI 0.322-0.695), the effect had dissipated by 31 months. All studies were US based and the majority conducted in low income groups (74%) and African Americans (60%). Two reviews focused on parenting interventions [ 60 , 61 ]. Pinquart and Teubert [ 60 ] reported small effects on parenting, parental stress, child abuse, health promoting behaviour, cognitive, social development, motor development, child mental health, parental mental health & couple adjustment from parenting education interventions. Vanderveen et al. [ 61 ] demonstrated an overall positive effect on neurodevelopment from early parental interventions (all involved teaching or enhancing parental skills) lasting up to 36 months. Meta analysis of twelve studies indicated higher cognitive scores at 12 months (WMD 5.57; 95% CI 2.29-8.86; p=0.0009), at 24 months (7 studies; WMD 7.59; 95% CI 5.01-14.31; p=0.0003) and at 36 months (2 studies; WMD 9.66; 95% CI 5.01-14.31; p=0.0001), but not at 5 yrs (3 studies p=0.24). The authors suggest further research is needed to clarify the most effective interventions and the long term effect.
Logic model
The parallel development of the logic model resulted in a summary model (Figure 2 ) provides a framework to visualise interventions across the perinatal period and the potential short, medium and long term impact on the health of women, their families and the community. Logic models display relationships between the core elements (context; inputs; outputs and outcomes) and the basic concept is to read from left to right, following a sequence of reasoning. An example of this is provision of education and information about screening in the antenatal period; an aspect of care where inequalities are known to occur [ 62 ]. The context in this example refers to the cultural, political, social circumstances in which the provision of screening is situated. Reading from left to right on the model indicates that the midwifery public health intervention is next so for example if a midwife provides information about antenatal screening for HIV (input), then uptake of screening may improve and at risk women will be identified earlier (outputs) and the effect will improve maternal and infant health during pregnancy. The medium and longer term outcomes are the resultant reduction in morbidity and or mortality in the local population.
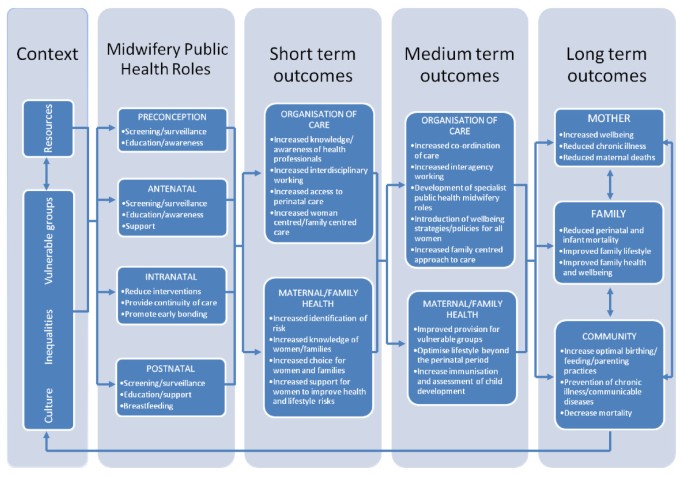
Summary Logic Model.
The focus of this paper is the development of the public health role of the midwife based on effective interventions and highlighting the short, medium and long term effects that these interventions could bring about. Any intervention must be considered within the context in which it is to be delivered as inequalities, resources, culture and vulnerable groups can influence the choice of intervention to best suit the population of women being served. The second column represents the inputs or activities; these are the interventions which are intended to bring about the change in outcomes. In relation to public health and midwifery these are interventions that may impact on public health primarily through education, screening and support. The outputs are the products or the targets of the service delivered and can been seen in the boxes entitled organisation of care under short and medium term outcomes. While the logic model provides a visual outline of midwifery public health roles, using this approach facilitates understanding of how public health programs can be planned and subsequently evaluated. Conducting the data synthesis in tandem with developing the logic model has also highlighted where the gaps in knowledge are and identified areas where midwives could potentially have a much greater role and subsequent impact on public health.
This paper sought to report on systematic reviews providing high quality evidence of effective interventions, in essence the ‘cream of the crop’. Reviews reporting on effective interventions were those which presented a statistically significant meta analysis or where the intervention was supported by a generally positive trend of results when a meta analysis was not possible to ensure the recommendations of the paper are based on strong evidence of good quality. There were a number of reviews included which presented statistically significant positive findings. However, in some cases these were limited by small numbers of participants or small numbers of trials included in the review. As a result of conducting the review and analyzing eligible systematic review evidence, three key areas for future consideration were identified including: recommendation and implementation of effective evidence; gaps in knowledge and developing the role of the midwife in public health which are discussed further in the following sections.
Recommendation and implementation of effective evidence
It is clear from this review of effective interventions, there are areas where evidence has been incorporated into guidelines and thus recommended for implementation into routine practice. However, it has also highlighted many areas where it has not. There has been extensive debate and commentary in the literature about knowledge transfer and translation of knowledge into practice, however, this paper confirms that despite the existence of good quality evidence, the gap remains. From this review, several effective interventions were identified, which are already recommended as routine practice, for example education about folic acid supplementation and pelvic floor muscle training to prevent or reduce the risk of urinary incontinence are advocated by current practice guidelines in the UK [ 63 ] and further afield [ 64 , 65 ]. However, to evaluate fully the extent to which guidelines have been applied it is essential to audit practice in order to provide evidence for knowledge transfer. To encourage implementation of NICE guidelines, audit support tools have been developed by NICE on antenatal care or diabetes in pregnancy for use at local level. Effective interventions were also identified which could easily be implemented by a midwife and could potentially impact on public health, such as education programs for parents of preterm infants and implementation of specific strategies to reduce caesarean section rates. Although there is recognition by health professionals these areas are important, this review provides definitive evidence and examples from systematic reviews, of interventions that are effective. Further consideration needs to be given to how to translate these effective interventions into practice using appropriate channels which are effective to facilitate knowledge transfer. These may include stronger collaborations between clinicians and academics and increasing the exposure students have to systematic reviews in education curricula at undergraduate level. Other effective interventions have been implemented on an ad hoc basis for example additional lay or professional support for breast feeding women and strategies to reduce caesarean section rates, which need to be included specifically in policy and strategy documents to ensure widespread implementation and thus contribute to an evidence based public health agenda to improve the health of women and families. Although this paper has focused on reporting effective interventions it is also important to take cognisance of those interventions that are not effective i.e. those which do not work and sometimes are deeply embedded into practice, for example, routine antenatal CTG for fetal assessment [ 20 ]. It was not possible to discuss reviews that demonstrated no effect within this current paper, however, Table 2 provides summary details of the areas where this was the case.
Gaps in knowledge
The review identified many gaps in systematic review literature relating to core midwifery practice, which potentially could impact on public health population goals. The UK Department of Health, Public Health Strategy [ 66 ] emphasizes the importance of improving maternal health and the subsequent impact on reducing infant mortality and premature births and yet this review identified limited systematic review evidence to support the implementation of midwifery interventions that could impact on perinatal morbidity and mortality. The review also highlighted it was difficult to accurately assess the potential public health impact in terms of effectiveness as some interventions were not well evaluated, evidenced by the large number of inconclusive reviews and reviews demonstrating no effect. The review of reviews identified some interventions that were effective but were limited in terms of methodological quality of included studies, for example, small numbers and design flaws, thus demonstrating the need for robust research and evaluation. One example of this is systematic review evidence in relation to weight management or obesity; a topic of growing concern to maternity care providers and yet the evidence from systematic reviews is limited in terms of quality. The systematic reviews included in the original review generally indicated that additional support related to diet or exercise for women in the postnatal period was effective, however, only one review was of a high quality. Another example of this is the evidence around home visiting for vulnerable groups of women in the postnatal period. While a significant body of research, including longitudinal studies has been published on parenting interventions indicating generally positive effects [ 67 , 68 ] the evidence from this current systematic review of reviews is mixed. Current early years governmental policy in the UK focuses on giving children the best start in life and various interventions have been, or are currently being rolled out, for example, SureStart and the Family Nurse Partnership, however the longer term impact on women and families remains to be seen. Logic models highlight the causal linkage between inputs, outputs and outcomes (24). This is illustrated very clearly in relation to support for parents in the form of parenting interventions (input) which can result in the short term outcome of increasing support for women to improve health and lifestyle; optimize lifestyle and child development beyond the immediate perinatal period (medium term) and in the long term improve family health and wellbeing for this generation and those to come.
Developing the role of the midwife in public health
In order for midwives to utilise their potential in relation to public health it is important not only to consider the interventions that could be implemented but also take cognisance of wider strategies and policy relating to public health. The logic model (Figure 2 ), which was developed as a parallel process to the review, provides an overarching framework that should be used by midwives to visualise their contribution to public health. The model illustrates possible future roles but also facilitates recognition of the current contribution of midwives to improving the health of women and their families as part of their core role. An example of this is how vulnerable women (either social or medical) could be identified in the antenatal period by midwives and a supportive or educational intervention implemented which would result in improved outcomes in the short term i.e. reduced pre term birth or improved birth weight. A medium term outcome of this intervention would focus on optimising lifestyle beyond the perinatal period for example collaborating with health visiting services to provide education and support that would potentially have a longer term outcome of improved family health and well being. The review did not identify any systematic reviews which specifically focused on interventions relating to midwifery public health roles, highlighting a gap in review evidence. Biro [ 69 ] suggests it may be challenging for midwives to think beyond individual women but ultimately necessary in order to meet the challenge of public health to improve population health. Reframing routine midwifery activities in a public health context, identifying midwives as public practitioners and building on existing activities, such as collaboration, organisation of care and interagency working are essential to clearly define the relationship between midwifery and public health. An earlier, wider review on health-led parenting interventions in pregnancy and the first three years of life [ 8 ] suggested that many interventions, particularly in relation to supporting parenting, could be provided as part of routine care and that although the optimal time to start programmes was not clear, there was some consensus that those initiated in the antenatal period were more effective. Development of the public health role of the midwife will also require strategic thinking and support from planners and commissioners of maternity services to ensure that midwives can influence policy and effectively implement public health strategies. This will involve dedicating time and resources to develop local policies, providing training for midwives and building good relationships with other healthcare disciplines to work together.
Limitations
There are a number of methodological challenges in using systematic review evidence which must be taken into account. It is difficult to summarise the evidence from systematic reviews as often there is significant diversity between interventions included in individual reviews or outcome measures used. In addition the results presented may be inconsistent between reviews or inconclusive, however, Smith et al. [ 14 ] suggest the strength of systematic reviews of reviews is that the best quality reviews can be highlighted in a single document. Systematic reviews are generally limited to published work and thus may be subject to publication bias. In addition, more recent, potentially conflicting, research may be available since the review was published or there may be effective interventions that have not been evaluated in a systematic review. A recent Cochrane overview of systematic reviews [ 70 ] highlighted that such reviews provide an accessible summary on the totality of the evidence in the area and minimised the need for referral to individual reviews, however suggested that readers may wish to do so for specific details. This review was similar in that it covered a broad scope of the evidence in relation to public health, providing a strategic overview while also providing a valuable resource for those who wish to consult individual reviews for additional specific details. In this paper, only high quality reviews (based on level of included evidence and methodology of review) reporting on effective interventions were included. While this provides reassurance regarding review findings, in that the conclusions are based on top level evidence, some interventions demonstrating effect may have been excluded because the review itself did not meet either the quality or level of evidence criteria for inclusion. In most cases this relates to areas worthy of future investigation, which need more robust evaluations. The search strategy utilised in the review was specifically focused on the public health role of the midwife and therefore incorporated key terms relative to key areas. However in doing so, some postnatal interventions, which extend beyond the role of the midwife, for example, parenting interventions that continue into early childhood may not have been included. In addition, due to the inclusion and exclusion criteria applied, it is possible that extensive broad reviews on particular topics have been excluded from this review due to the nature of evidence included within them, for example, the NICE Guideline on Antenatal and Postnatal Mental Health [ 9 ]. However, it is recognised these are valuable resources and contribute to wider understanding on specific subjects.
This paper has reported on high quality effective interventions identified from a larger systematic review on public health interventions that could be delivered primarily by midwives or maternity care providers. From the effective interventions identified it is clear that while some have been recommended for implementation into routine practice, others have not. This highlights the continuing gap between evidence and practice and the need for professionals and researchers to work better together to ensure specific interventions that are effective, are translated into practice and subsequently audited to provide evidence of knowledge translation. The public health role of the midwives has not been well researched or reviewed and the impact of everyday midwifery practice on longer term, holistic maternal and family well-being outcomes is poorly articulated in review literature. A shift in research, policy and practice is needed to fully articulate the public health role of the midwife. This systematic review of systematic reviews identifies a number of effective interventions that provide a useful starting point on which to build future practice. The logic model demonstrates the need to fill in major gaps in our knowledge on effective interventions to achieve both short and long term public health benefits for women and their families. Such benefits will remain elusive without investment in a collaborative, strategic approach to the role of public health in midwifery.
Advisory group members
Ms Liz Bannon , Senior Midwife, & Co Director of Maternity Services, Social Services, Family & Child Care Belfast Health and Social Care Trust, Belfast, Northern Ireland; Professor Debra Bick , Professor of Evidence Based Midwifery Practice, Kings College London, England; Dr Helen Cheyne , Nursing, Midwifery & Allied Professions Research Unit, University of Stirling, Scotland; Professor Mike Clarke , then Professor of Clinical Epidemiology & Director of UK Cochrane Centre, now Professor/Director of MRC Methodology Hub, Queen’s University Belfast; Ms Joanne Gluck , Consumer Representative; Professor Billie Hunter , Professor of Midwifery, Swansea University, Wales; Dr Dermot O’Riley , Centre of Excellence for Public Health Northern Ireland, Queen’s University Belfast, Northern Ireland.
Midwifery 2020 Programme: Midwifery 2020: Delivering Expectations. 2010, London: Midwifery 2020
Google Scholar
United Nations: The millennium development goals report 2008. 2008, New York: United Nations Department of Social and Economic Affairs
Thomson G, Dykes F, Singh G, Cawley L, Dey P: A public health perspective of women's experiences of antenatal care: An exploration of insights from a community consultation. Midwifery. 2012, 10.1016/j.midw.2012.01.002. Epub ahead of print
Whitehead E: Understanding the association between teenage pregnancy and intergenerational factors: a comparative and analytical study. Midwifery. 2009, 25: 147-154. 10.1016/j.midw.2007.02.004.
Article PubMed Google Scholar
Declercq E, Young R, Cabral H, Ecker J: Is a rising cesarean delivery rate inevitable? trends in industrialized countries, 1987 to 2007. Birth. 2011, 38 (2): 99-104. 10.1111/j.1523-536X.2010.00459.x.
Green J, Baston H: Have women become more willing to accept obstetric interventions and does this relate to mode of birth? data from a prospective study. Birth. 2007, 34 (1): 6-13. 10.1111/j.1523-536X.2006.00140.x.
Weaver J, Statham H, Richards M: Are there “Unnecessary” cesarean sections? perceptions of women and obstetricians about cesarean sections for nonclinical indications. Birth. 2007, 34 (1): 32-41. 10.1111/j.1523-536X.2006.00144.x.
Barlow J, Schrader McMillan A, Kirkpatrick S, Ghate D, Smith M, Barnes J: Health-led parenting interventions in pregnancy and early years. 2008, London: Department for Children, Schools and Families
National Collaborating Centre for Mental Health: Antenatal and postnatal mental health: The NICE guideline on clinical management and service guidance. NICE guideline CG45. 2007, London: The British Psychological Society & The Royal College of Psychiatrists
McNeill J, Lynn F, Alderdice F: Systematic review of reviews: the public health role of the midwife. 2010, Scotland: NHS Education for Scotland. Available online from, http://www.midwifery2020.org/Public%20Health/index.asp . Accessed 15th September 2012.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009, 339: b2535-10.1136/bmj.b2535.
Article PubMed PubMed Central Google Scholar
Chiappelli F, Cajulis OS: The logic model for evidence-based clinical decision making in dental practice. J Evid Based Dent Pract. 2009, 4: 206-210.
Article Google Scholar
Scottish Intercollegiate Guidelines Network: Systematic literature review. 2008, Available at: http://www.sign.ac.uk/guidelines/fulltext/50/ section6.htm. Accessed 27 March 2012,
Smith V, Devane D, Begley CM, Clarke M, Higgins S: A systematic review and quality assessment of systematic reviews of randomised trials of interventions for preventing and treating preterm birth. Eur J Obstet Gynecol Reprod Biol. 2009, 142: 3-11. 10.1016/j.ejogrb.2008.09.008.
Clarke M: Interpreting the results of systematic reviews. Semin Hematol. 2008, 45: 176-180. 10.1053/j.seminhematol.2008.04.002.
Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, Henry DA, Boers M: AMSTAR is a reliable and valid measurement toll to assess the methodological quality of systematic reviews. J Clin Epidemol. 2009, 62: 1013-1020. 10.1016/j.jclinepi.2008.10.009.
van Sluijs EMF, McMinn AM, Griffin SJ: Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007, 335: 703-707. 10.1136/bmj.39320.843947.BE.
Bricker L, Neilson JP, Dowswell T: Routine ultrasound in late pregnancy (after 24 weeks' gestation). Cochrane database of systematic reviews issue 4, . 2008, Chichester, UK: John Wiley & Sons
Carroli G, Piaggio G, Khan-Neelofur D: WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 2001, 357: 1565-1570. 10.1016/S0140-6736(00)04723-1.
Article CAS PubMed Google Scholar
Grivell RM, Wong L, Bhatia V: Regimens of fetal surveillance for impaired fetal growth. Cochrane database of systematic reviews issue 1. 2009, Chichester, UK: John Wiley & Sons
Kongnyuy EJ, Wiysonge CS, Shey MS: A systematic review of randomized controlled trials of prenatal and postnatal vitamin A supplementation of HIV-infected women. Int J Gynecol Obstet. 2009, 104: 5-8. 10.1016/j.ijgo.2008.08.023.
Article CAS Google Scholar
Rumbold A, Duley L, Crowther CA, Haslam Ross R: Antioxidants for preventing pre-eclampsia. Cochrane database of systematic reviews issue 1. 2008, Chichester, UK: John Wiley & Sons
Villar J, Carroli G, Khan-Neelofur D, Piaggio GGP, Gülmezoglu AM: Patterns of routine antenatal care for low-risk pregnancy. Cochrane database of systematic reviews issue 4. 2001, Chichester, UK: John Wiley & Sons
Kellogg Foundation WK: Logic model development guide. 2004, Michigan: WK Kellogg Foundation
Midwifery 2020: Public health workstream final report. 2012, available from http://www.midwifery2020.org/documents/2020/Public_Health.pdf . accessed 15th September,
Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, Martin MA: Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women's views. Health Technol Assess. 2000, 16: 1-193. 10.1017/S0266462300016111.
Whitworth M, Bricker L, Neilson JP, Dowswell T: Ultrasound for fetal assessment in early pregnancy. Cochrane database of systematic reviews issue 4. 2010, Chichester, UK: John Wiley & Sons
Sangkomkamhang US, Lumbiganon P, Prasertcharoensook W, Laopaiboon M: Antenatal lower genital tract infection screening and treatment programs for preventing preterm delivery. Cochrane database of systematic reviews issue 2. 2008, Chichester, UK: John Wiley & Sons
O’Connor AM, Bennett CL, Stacey D, Barry M, Col NF, Eden KB, Entwistle VA, Fiset V, Holmes-Rovner M, Khangura S, Llewellyn-Thomas H, Rovner D: Decision aids for people facing health treatment or screening decisions. Cochrane database of systematic reviews issue 3. 2009, Chichester, UK: John Wiley & Sons
Blencowe H, Cousens S, Modell B, Lawn J: Folic acid to reduce neonatal mortality from neural tube disorders. In J Epidemiol. 2010, 39: i110-i121. 10.1093/ije/dyq028.
Lumley J, Watson L, Watson M, Bower C: Periconceptional supplementation with folate and/or multivitamins for preventing neural tube defects. Cochrane database of systematic reviews issue 3. 2001, Chichester, UK: John Wiley & Sons
Pena-Rosas JP, Viteri FE: Effects and safety of preventive oral iron or iron+folic acid supplementation for women during pregnancy. Cochrane database of systematic reviews issue 4. 2009, Chichester, UK: John Wiley & Sons
Shah PS, Ohlsson A: Effects of prenatal multimicronutrient supplementation on pregnancy outcomes: a meta analysis. CMAJ. 2009, 180 (12): E99-E108. 10.1503/cmaj.081777.
Hofmeyr GJ, Roodt A, Atallah A, Duley L: Calcium supplementation to prevent pre-eclampsia: a systematic review. S Afr Med J. 2003, 93: 224-228.
CAS PubMed Google Scholar
Hofmeyr GJ, Duley L, Atallah A: Dietary calcium supplementation for prevention of pre-eclampsia and related problems: a systematic review and commentary. BJOG. 2007, 114: 933-943. 10.1111/j.1471-0528.2007.01389.x.
Hofmeyr GJ, Lawrie TA, Atallah AN, Duley L: Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane database of systematic reviews issue 8. 2010, Chichester, UK: John Wiley & Sons
Horvath A, Koletzko B, Szajewska H: Effect of supplementation of women in high-risk pregnancies with long-chain polyunsaturated fatty acids on pregnancy outcomes and growth measures at birth: a meta-analysis of randomized controlled trials. Br J Nutr. 2007, 98: 253-259. 10.1017/S0007114507709078.
Hatem M, Sandall J, Devane D, Soltani H, Gates S: Midwife-led versus other models of care for childbearing women. Cochrane database of systematic reviews issue 4. 2008, Chichester, UK: John Wiley & Sons
Hodnett ED, Fredericks S: Support during pregnancy for women at increased risk of low birth weight babies. Cochrane database of systematic reviews issue 3. 2003, Chichester, UK: John Wiley & Sons
Dennis C-L, Kingston D: A systematic review of telephone support for women during pregnancy and the early postpartum period. J Obstet Gynecol Neonatal Nurs. 2008, 37: 301-314. 10.1111/j.1552-6909.2008.00235.x.
Lumley J, Chamberlain C, Dowswell T, Oliver S, Oakley L, Watson L: Cochrane Database of Systematic Reviews. Interventions for promoting smoking cessation during pregnancy. 2009, Chichester, UK: John Wiley & Sons
Chapter Google Scholar
Naughton F, Prevost AT, Sutton S: Self-help smoking cessation interventions in pregnancy: a systematic review and meta-analysis. Addiction. 2008, 103: 566-579. 10.1111/j.1360-0443.2008.02140.x.
Hay-Smith J, Morkved S, Fairbrother KA, Herbison GP: Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane database of systematic reviews issue 4. 2008, Chichester, UK: John Wiley & Sons
Lemos A, Impieri De Souza A, Ferreira ALCG, Figueiroa JN, Cabral-Filho JE: Do perineal exercises during pregnancy prevent the development of urinary incontinence? A systematic review. Int J Urol. 2008, 15: 875-880. 10.1111/j.1442-2042.2008.02145.x.
Dennis C-L, Creedy DK: Psychosocial and psychological interventions for preventing postpartum depression. Cochrane database of systematic reviews issue 4. 2004, Chichester, UK: John Wiley & Sons
Cluett ER, Burns E: Immersion in water in labour and birth. Cochrane database of systematic ReviewsIssue 2. 2009, Chichester, UK: John Wiley & Sons
Rabe H, Reynolds GJ, Diaz-Rosello JL: Early versus umbilical cord clamping in preterm infants Cochrane database of systematic reviews issue 4. 2004, Chichester, UK: John Wiley & Sons
Hodnett ED, Gates S, Hofmeyr G, Justus SC: Continuous support for women during childbirth. Cochrane database of systematic reviews issue 3. 2007, Chichester, UK: John Wiley & Sons
Hodnett ED, Downe S, Walsh D, Weston J: Alternative versus conventional institutional settings for birth. Cochrane database of systematic reviews issue 9. 2010, Chichester, UK: John Wiley & Sons
Chaillet N, Dumont A: Evidence-based strategies for reducing cesarean section rates: a meta-analysis. Birth. 2007, 34: 53-64. 10.1111/j.1523-536X.2006.00146.x.
Britton C, McCormick FM, Renfrew MJ, Wade A, King SE: Support for breastfeeding mothers. Cochrane database of systematic reviews issue 1. 2007, Chichester, UK: John Wiley & Sons
Chung M, Raman G, Trikalinos T, Lau J, Ip S: Interventions in primary care to promote breastfeeding: an evidence review for the U.S. Preventive services task force. Ann Int Med. 2008, 149: 565-582.
Sikorski J, Renfrew MJ, Pindoria S, Wade A: Support for breastfeeding mothers: a systematic review. Paediatr Perinat Epidemiol. 2003, 17: 407-417. 10.1046/j.1365-3016.2003.00512.x.
Dyson L, McCormick FM, Renfrew MJ: Interventions for promoting the initiation of breastfeeding. Cochrane database of systematic reviews issue 2. 2008, Chichester, UK: John Wiley & Sons
Moore ER, Anderson GC, Bergman N: Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane database of systematic reviews issue 3. 2007, Chichester, UK: John Wiley & Sons
Ahmed AH, Sands LP: Effect of Pre- and postdischarge interventions on breast feeding outcomes and weight gain among premature infants. J Obstet Gynecol Neonatal Nurs. 2010, 39: 53-63. 10.1111/j.1552-6909.2009.01088.x.
Dennis C-L, Hodnett ED: Psychosocial and psychological interventions for treating postpartum depression. Cochrane database of systematic reviews issue 4. 2007, Chichester, UK: John Wiley & Sons
Amorim Adegboye AR, Linne YM, Lourenco PMC: Diet or exercise, or both, for weight reduction in women after childbirth Cochrane database of systematic reviews issue 3. 2007, Chichester UK: Cochrane Database of Systematic Reviews
Corcoran J, Pillai VK: Effectiveness of secondary pregnancy prevention programs: a meta-analysis. Res Soc Work Pract. 2007, 17: 5-18. 10.1177/1049731506291583.
Pinquart M, Tuebert D: Effects of parenting education with expectant and New parents: a meta analysis. J Fam Psychol. 2010, 24 (3): 316-327.
Vanderveen JA, Bassler D, Robertson CM, Kirpalani H: Early interventions involving parents to improve neurodevelopmental outcomes of premature infants: a meta-analysis. J Perinatol. 2009, 29: 343-351. 10.1038/jp.2008.229.
Alderdice F, McNeill J, Rowe R, Martin D, Dornan J: Inequalities in the reported offer and uptake of antenatal screening. Public Health. 2008, 122: 42-52. 10.1016/j.puhe.2007.05.004.
National Collaborating Centre for Women’s and Children’s Health: Antenatal care routine care for the healthy pregnant woman. 2008, London: RCOG Press
Wilson RD, on behalf of Genetics Committee of the Society of Obstetricians and Gynaecologists of Canada and The Motherisk Program, The Hospital for Sick Children Toronto, et al: Pre-conceptional vitamin/folic acid supplementation 2007: the Use of folic acid in combination with a multivitamin supplement for the prevention of neural tube defects and other congenital anomalies –guideline No. 201. J Obstet Gynaecol Can. 2007, 29 (12): 1003-1013.
Davies G, Wolfe L, Mottola M, MacKinnon C: Exercise in pregnancy and the post partum period –guideline No. 129. J Obstet Gynaecol Can. 2003, 25 (6): 516-522.
Department of Health: UK healthy lives, healthy people. 2010, London: HMSO
Olds D, Henderson CR, Chamberlin R, Tatelbaum R: Preventing Child Abuse and Neglect. Randomized Trial Nurse Home Visitation Pediatr. 1986, 78: 65-78.
CAS Google Scholar
Olds DL, Eckenrode J, Henderson CR, Kitzman H, Powers J, Cole R, Sidora K, Morris P, Pettitt LM, Luckeyet D: Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. JAMA. 1997, 27: 278 (8): 637-643.
Biro MA: What has public health got to do with midwifery? Midwives' role in securing better health outcomes for mothers and babies. Women Birth. 2010, 24 (1): 17-23.
Jones L, Othman M, Dowswell T, Alfirevic Z, Gates S, Newburn M, Jordan S, Lavender T, Neilson T: Pain management for women in labour: an overview of systematic reviews (review) Cochrane database of systematic reviews issue 3. 2012, Chichester, UK: John Wiley & Sons
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2458/12/955/prepub
Download references
Acknowledgements
We would like to thank all members of the Advisory Group for their contribution and guidance throughout the project. In addition, we would like to thank Midwifery 2020 for funding the original review and in particular, The Public Health Workstream Group who commissioned the original review.
Source of funding
The original review was funded by NHS Education for Scotland, Midwifery 2020, UK.
Author information
Authors and affiliations.
School of Nursing & Midwifery, Queen’s University Belfast, Medical Biology Centre, 97 Lisburn Road, Belfast, BT9 7BL, Ireland
Jenny McNeill, Fiona Lynn & Fiona Alderdice
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jenny McNeill .
Additional information
Competing interests.
The authors declare that they have no competing interest.
Authors’ contributions
JM extracted and interpreted data and wrote the first draft of the manuscript. FL conducted the searches of the literature, extracted and interpreted data and assisted with the manuscript. FA extracted and interpreted data and assisted with the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
McNeill, J., Lynn, F. & Alderdice, F. Public health interventions in midwifery: a systematic review of systematic reviews. BMC Public Health 12 , 955 (2012). https://doi.org/10.1186/1471-2458-12-955
Download citation
Received : 05 April 2012
Accepted : 29 October 2012
Published : 08 November 2012
DOI : https://doi.org/10.1186/1471-2458-12-955
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
- Public health
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Loading metrics
Open Access
Peer-reviewed
Research Article
Midwifery continuity of care: A scoping review of where, how, by whom and for whom?
Roles Data curation, Formal analysis, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing
Affiliations Maternal, Child, and Adolescent Health Program, Burnet Institute, Melbourne, Victoria, Australia, Mater Research, University of Queensland, Brisbane, Queensland, Australia
Roles Data curation, Formal analysis, Validation, Writing – review & editing
Affiliations Maternal, Child, and Adolescent Health Program, Burnet Institute, Melbourne, Victoria, Australia, Melbourne Medical School, University of Melbourne, Melbourne, Victoria, Australia
Roles Conceptualization, Funding acquisition, Methodology, Supervision, Validation, Writing – review & editing
Affiliation Department of Maternal, Newborn, Child, and Adolescent Health, World Health Organisation, Geneva, Switzerland
Roles Conceptualization, Funding acquisition, Methodology, Writing – review & editing
Roles Formal analysis, Methodology, Validation, Writing – review & editing
Affiliation Department of Women and Children’s Health, Kings College London, London, United Kingdom
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing
* E-mail: [email protected]
Affiliation Maternal, Child, and Adolescent Health Program, Burnet Institute, Melbourne, Victoria, Australia
- Billie F. Bradford,
- Alyce N. Wilson,
- Anayda Portela,
- Fran McConville,
- Cristina Fernandez Turienzo,
- Caroline S. E. Homer

- Published: October 5, 2022
- https://doi.org/10.1371/journal.pgph.0000935
- Peer Review
- Reader Comments
Systems of care that provide midwifery care and services through a continuity of care model have positive health outcomes for women and newborns. We conducted a scoping review to understand the global implementation of these models, asking the questions: where, how, by whom and for whom are midwifery continuity of care models implemented? Using a scoping review framework, we searched electronic and grey literature databases for reports in any language between January 2012 and January 2022, which described current and recent trials, implementation or scaling-up of midwifery continuity of care studies or initiatives in high-, middle- and low-income countries. After screening, 175 reports were included, the majority (157, 90%) from high-income countries (HICs) and fewer (18, 10%) from low- to middle-income countries (LMICs). There were 163 unique studies including eight (4.9%) randomised or quasi-randomised trials, 58 (38.5%) qualitative, 53 (32.7%) quantitative (cohort, cross sectional, descriptive, observational), 31 (19.0%) survey studies, and three (1.9%) health economics analyses. There were 10 practice-based accounts that did not include research. Midwives led almost all continuity of care models. In HICs, the most dominant model was where small groups of midwives provided care for designated women, across the antenatal, childbirth and postnatal care continuum. This was mostly known as caseload midwifery or midwifery group practice. There was more diversity of models in low- to middle-income countries. Of the 175 initiatives described, 31 (18%) were implemented for women, newborns and families from priority or vulnerable communities. With the exception of New Zealand, no countries have managed to scale-up continuity of midwifery care at a national level. Further implementation studies are needed to support countries planning to transition to midwifery continuity of care models in all countries to determine optimal model types and strategies to achieve sustainable scale-up at a national level.
Citation: Bradford BF, Wilson AN, Portela A, McConville F, Fernandez Turienzo C, Homer CSE (2022) Midwifery continuity of care: A scoping review of where, how, by whom and for whom? PLOS Glob Public Health 2(10): e0000935. https://doi.org/10.1371/journal.pgph.0000935
Editor: Ahmed Waqas, University of Liverpool, UNITED KINGDOM
Received: June 3, 2022; Accepted: September 5, 2022; Published: October 5, 2022
Copyright: © 2022 Bradford et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All data are in the Supporting information files.
Funding: This review was commissioned by the World Health Organization Department of Maternal, Newborn, Child and Adolescent Health and Ageing and funded through a grant received from Merck Sharp and Dohme Corp (MSD). CFT is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration (ARC) South London, a NIHR Global Health Research Group (NIHR133232) and a NIHR Development and Skills Award (NIHR301603). CSEH is supported by an Australian National Health and Medical Research Council Fellowship (APP1137745). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Continuity of care is a concept rooted in primary care involving the care of individuals (rather than populations) over time by the same care provider. It encompasses relational continuity, informational continuity and management continuity [ 1 ]. In the primary care setting, continuity of care has been shown to reduce mortality and hospitalisations, and increase patient satisfaction [ 2 ]. Continuity of care also has an important place in chronic care settings, such as palliative care [ 3 ].
In the maternal and newborn care setting, midwife-led continuity of care refers to a model whereby care is provided by the same midwife, or small team of midwives, during pregnancy, labour and birth, and the postnatal periods with referral to specialist care as needed [ 4 ]. Midwife-led also refers to a model of care which is provided there is a distinct occupational group of midwives [ 5 ] and the person is fully qualified, regulated and deployed only as a midwife. This contrasts to systems in many countries (most countries in Africa for and South East Asia for example) where nurse-midwives are rotated to either nursing or midwifery duties. Midwife-led continuity models in a small number of HICs have been associated with lower rates of preterm birth (24% reduction), and lower fetal loss before and after 24 weeks and neonatal deaths (16%) less likely to lose their babies overall (combined reduction in fetal loss and neonatal death) for women at low and mixed risk of complications compared to other models of care. In addition, women are less likely to experience interventions and more likely to report positive experiences of care [ 4 ]. A Cochrane review of reviews of interventions during pregnancy to prevent preterm birth also found that these models had clear benefit in reducing preterm birth and perinatal death [ 6 ]. Women prefer the personalised experience provided by such models, leading to trust between midwife and woman and empowerment of both women and midwives [ 7 ].
Models of care that provide continuity across the childbearing continuum are complex interventions, and the pathway of influence that produces these positive outcomes is unclear. A number of plausible hypotheses require further investigation. For example, it could be that midwives provide a mechanism that enables effective and equitable care to be provided by better coordination, navigation and referral; and/or that relational continuity and advocacy engenders trust and confidence between women and midwives, resulting in women feeling safer, less stressed and more respected [ 4 ]. Access to organisational infrastructure, innovative partnerships, and robust community networks has been found crucial to overcome barriers, address women’s, newborns’ and parents’ needs and ensure quality of care [ 8 ].
Inequity is a key driver of adverse perinatal outcome, both between and within countries. Some observational studies of midwife-led continuity of care models in socially and economically disadvantaged populations in high-income countries (HIC) have reported significant reductions in pre-term birth and caesarean sections in diverse cohorts of women in the United Kingdom [ 9 – 12 ]. In Australia, a study of maternity care during significant floods in Queensland showed that midwife-led continuity of care mitigated the social and emotional impacts of the floods [ 13 ]. Another Australian study showed reduced preterm births amongst Australian Aboriginal and Torres Strait Islander women who received midwife-led continuity of care [ 14 ]. These studies suggest that women who typically experience a greater burden of adverse perinatal outcome, may derive greater benefit from continuity of care. However, understanding how continuity per se may mitigate inequities in maternal and newborn health remains a research priority.
Despite evidence supporting midwife-led continuity of care and guidelines from the World Health Organization which recommend midwife-led continuity-of-care models for pregnant women in settings with well-functioning midwifery programmes [ 15 – 17 ] only a small proportion of women internationally have access to such care. The current evidence suggests that access to midwife-led continuity of care models is largely confined to a small number of HICs notably Australia, Canada, New Zealand and the United Kingdom [ 17 ] where a distinct occupational group of midwives has been a central part of the health systems for decades. Barriers to implementation of midwifery-led continuity of care exist across all country income levels and include a lack of local health system financing, shortage of personnel including administrative and other support staff [ 4 ]. It is not clear to what extent midwife-led continuity of care has been implemented in low- to middle-income countries (LMIC). Many LMICs have a model of predominantly nurse-midwives who are deployed to both nursing and midwifery duties, often preventing midwife-led continuity of care models. Advancing understanding around which countries have implemented continuity of care models for maternal and newborn health, how, for whom, and in what context, is crucial for successful implementation, scale-up and sustainability.
The overall aim of this review was to understand the global implementation of midwifery continuity of care, asking the questions: Where, how, by whom and for whom are midwifery continuity of care initiatives implemented?
Materials and methods
A scoping review was undertaken guided by the approach described by Arksey and O’Malley [ 18 ] and further defined by Levac and colleagues [ 19 ]. The following five steps were followed: i) identifying the research question; ii) identifying the relevant literature; iii) study selection, iv) charting the data; and v) collating, summarising and reporting the results.
We used the broad definition of midwifery from The Lancet Series on Midwifery as our starting point, that is, “skilled, knowledgeable, and compassionate care for childbearing women, newborn infants and families across the continuum from pre-pregnancy, pregnancy, birth, postpartum and the early weeks of life [ 20 ]. Midwifery continuity of care was defined as care delivered by the same known care provider or care provider team across two or more parts in the care continuum–antenatal, intrapartum, postnatal and neonatal periods. In some settings, continuity of care may be provided by cadre other than midwives, for example, nurses or physicians. Thus, eligible papers could include care providers that were midwives and non-midwives, such as, nurses, community health workers and physicians. We excluded reports on care primarily by traditional birth attendants (TBA).
Identifying the relevant literature—Search strategy and selection criteria
In order to develop the search strategy, a preliminary search of PubMed and Google scholar using the terms ‘midwifery or midwife-led continuity of care’ were used to locate key systematic and scoping reviews on the topic and identify relevant search terms for the systematic search strategy (see S1 Text for the search strategy). We then searched the following electronic databases: MEDLINE, CENTRAL, CINAHL, PsychINFO and Web of Science. A subject librarian reviewed search terms, keywords and strategies. In addition, we searched PubMed, Google Scholar, PROSPERO, Scopus and Dimensions and the WHO International Clinical Trials Registry platform. We conducted the search on the 20 February 2022 and included publications (peer reviewed studies and reports) in the past 10 years.
A key area of interest was implementation of continuity of midwifery care in LMICs but we recognised that reports of implementation may be published in formats other than peer reviewed publications. Eligible papers therefore included implementation studies or reports of implementation of midwifery continuity of care in the grey literature. We sourced grey literature through online searches on the websites of relevant professional groups, United Nations agencies and non-government organisations (NGO). We circulated a call for relevant materials through online list servs (email groups) and through midwifery contacts. The International Confederation of Midwives assisted by emailing all member associations asking for any relevant reports.
Eligible reports could report on midwifery continuity of care efforts in HICs and LMICs. Reports from implementation efforts by government programmes, private providers, professional organisations, NGOs and universities and research studies of any design were eligible for inclusion. Protocols that reported studies that were underway, but not concluded, were also eligible. Opinion pieces, editorials and other materials, which included details of midwifery continuity of care initiatives, were also eligible. Publications in any language were eligible. The search was limited to reports published in the last ten years (January 2012 to January 2022) to ensure the information was contemporary and therefore of greatest relevance to policy makers.
Reports identified through both peer-reviewed and grey literature databases were hand-searched for other potentially relevant studies. These included reference lists of relevant systematic reviews, and published conference abstracts, as well as any reports forwarded to authors in response to a call for notification of new or ongoing initiatives from key global stakeholder organisations, such as the International Confederation of Midwives.
Reports were excluded they if reported on midwifery continuity of care in general but did not report on a continuity of care practice initiative. We excluded systematic and literature reviews although their reference lists were searched for relevant primary studies.
Study selection
All reports identified through database searching were imported into Endnote referencing programme (Endnote 20, Clarivate Analytics, Philadelphia), and duplicates removed. Remaining citations (n = 5789) were uploaded into systematic review software Covidence (Covidence 2022, Veritas Health Innovations, Melbourne). Two authors independently conducted initial title and abstract screening and undertook full-text review. A third author screened a random selection of 10% of studies and discrepancies were discussed and resolved.
Charting the data
The following information was extracted for all included reports: country, income-level (as defined by the World Bank [ 21 ], study design (if applicable), setting (urban/rural and community-based or facility-based), novel or scaled-up initiative, model of care, level of continuity (antenatal and intrapartum, antenatal and postnatal, intrapartum and postnatal) and cadre of care providers, (e.g. mix of providers involved). We also collected information on the inclusion of priority population groups–these are groups of people who are persistently disadvantaged by existing systems of power with demographic features known to be associated with adverse perinatal outcomes, such as ethnic minorities, urban and remote women, socially disadvantaged, and Indigenous women. We have described these specific groups as priority rather than vulnerable populations [ 22 ]. Reporting of the scoping review findings follows the PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) format (see S1 Checklist ) and reference ( Fig 1 ) [ 23 ]. Appraisal of study quality or meta-analysis was not undertaken.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0000935.g001
In total, 6595 references were identified from electronic peer-reviewed databases, 821 duplicate records were removed prior to uploading to Covidence, a further 634 duplicates were removed by automation. Of the 5136 remaining references, 4728 did not meet the inclusion criteria. A further 256 references were excluded at the full-text stage as either: they did not describe continuity of care according to our pre-determined criteria (167); did not include primary source data (42); were duplicates (41); or did not have insufficient detail regarding the model of care (6). One hundred and fifty-two (152) peer-reviewed publications were eligible based on inclusion and exclusion criteria. A further 23 reports were identified following the grey literature search, bringing the total to 175 ( Fig 1 ). Details are listed in S1 Table .
Of the 175 individual reports, 152 (86.8%) were peer reviewed publications, 18 (10.3%) were conference abstracts, and the remaining five (3%) were published or unpublished reports. Reports primarily reported on birth outcomes (n = 54, 31%), women’s (including some partners’) views and experiences (n = 47, 27%) and midwives (including doctors) views and experiences (n = 33, 19%). There were 18 reporting on the model of care more broadly, including implementation challenges (n = 18, 10%), and 14 (7%) that were focussed on the experience of midwifery students providing continuity of care as part of their education. The majority of these student-focused reports were from Australia. Fewer reports focussed on the experience of midwifery managers (n = 3, 2%), while four were cost analyses (2%).
There were 163 unique studies including eight (4.9%) randomised or quasi randomised trials, 58 (38.5%) qualitative, 53 (32.7%) quantitative (cohort, cross sectional, descriptive, observational), 31 (19.0%) survey studies, and three (1.9%) health economics analyses. There were 10 practice-based accounts that did not include research.
‘The where’: Country and setting
Of the 175 included reports, the majority (n = 157, 90%) were from HICs and 18 (10%) from LMICs ( Table 1 ). Most were from Australia, (n = 71, 41%), followed by the United Kingdom (England, Scotland, Wales) (24, 14%), Sweden (13, 8%), Canada (8, 5%), Denmark (6, 4%), New Zealand (7, 4%), Japan (5, 3%), with less than five reports described initiatives conducted in Belgium, Finland, Germany, Greece, Ireland, Netherlands, Norway, Singapore, Switzerland and the United States of America (USA). In the LMICs, three from Palestine, three from China, two each from Bangladesh and Indonesia, and one from each of the remaining countries.
https://doi.org/10.1371/journal.pgph.0000935.t001
Overall, most midwifery continuity of care models were based in urban areas (n = 126, 72%). In HIC, three-quarters of services (n = 118, 75%) were urban-based, whereas in LMICs just under half (n = 8, 44%) were urban-based. Hospital or facility-based services were most common across all income levels (n = 124, 72% overall).
‘The how’: Describing the way continuity of care is provided
There were a number of different terms used to define the model of care, and the level of continuity provided across the continuum of care varied with no single term used. Overall, the most common terms were caseload midwifery (n = 63, 36%), midwifery-led continuity (n = 60, 34%), or team/midwifery group practice (n = 40, 23%). Most described services designed so that the same providers provided care across the continuum–antenatal, intrapartum and postnatal (n = 159, 91%). There were eight which described continuity only across the antenatal and postpartum periods [ 24 – 31 ] (excluding labour and birth), and five reported [ 32 – 36 ] (including 3 unique examples) where the continuity was provided only across antenatal and intrapartum periods without postpartum care.
In HICs, the most dominant approach is where small groups of midwives provide care for designated women, known as caseload midwifery or midwifery group practice in countries like Australia [ 37 ], the United Kingdom [ 9 ], Denmark [ 38 ], Sweden [ 39 ], and Singapore [ 40 ] where the number of midwives is usually two to four. In other countries, for example, Japan [ 41 ] and Switzerland [ 42 ], the approach is also called team midwifery and the number of midwives is five or more.
The continuity of care services were located as part of the usual hospital [ 37 , 43 ], in an alongside birth centre [ 44 – 46 ] or in a free-standing birth centre [ 47 ]. Some midwife-led continuity of care services were offered through homebirth practices, either as part of the hospital system [ 48 , 49 ] or as a private service [ 50 ]. Most services were based in urban areas but there were some examples from rural areas in Australia [ 51 – 53 ], Sweden [ 54 – 56 ] and Scotland [ 57 ] ( Table 2 ).
https://doi.org/10.1371/journal.pgph.0000935.t002
Although midwife-led continuity of care was available in a number of countries, mostly high-income with a cadre of midwives, in select facilities and locations, it was generally not scaled-up nationally. The exception being New Zealand, where the Lead Maternity Carer model is national allowing to midwives provide continuity of care to all women regardless of risk, in either caseloading or small community-based group practices, under a national funding arrangement and with medical or other collaboration when required [ 58 ].
In LMICs there was greater diversity in structure of arrangements for provision of midwifery continuity of care models. Models of care included a lead midwife delivering care across the continuum [ 59 , 60 ], midwives on-call for women during labour who they had previously seen for antenatal care [ 61 ], and a midwifery continuity of care team that ran in parallel with an obstetric team [ 62 ]. An initiative in Ethiopia involved the same midwife providing antenatal, intrapartum and postnatal care to the same women [ 63 , 64 ]. An initiative in Kenya involved midwifery care across the childbearing continuum, embedded within a family planning and HIV care service [ 65 ]. One initiative in China [ 66 ] facilitated continuity of care for women wishing to have a vaginal birth, where efforts were made for women to see the same midwife for intrapartum and postnatal care. In the Palestinian initiative [ 67 – 69 ], midwives were allocated geographical areas to provide antenatal and postnatal care for between 50–100 women. One initiative in Bangladesh [ 70 ] and another in Iran [ 71 ] involved teams of midwives providing care in a private midwifery clinic associated with two local hospitals.
Similar to HICs, continuity of care services were located as part of the usual hospital services (eg in Pakistan [ 59 , 72 ], China [ 61 ], Ethiopia [ 63 , 64 ], Palestine [ 67 – 69 ] or in community health centres or maternity clinics, for example in Bangladesh [ 60 , 70 ], Kenya [ 65 ] and Afghanistan [ 73 ]. Most services were based in urban or semi-urban areas but there were some examples from rural areas, for example, Palestine [ 67 – 69 ], Bangladesh [ 70 ], Afghanistan [ 73 ] and Indonesia [ 74 ].
Reports from China [ 62 ], Ethiopia [ 63 ], Iran [ 71 ], Kenya [ 65 ] and Pakistan [ 59 ] provided some degree of continuity of care across all antenatal, intrapartum and postnatal periods. Two reports, one from China [ 61 ] and the one from Kenya [ 65 ] provided care across antenatal and intrapartum. A study in China [ 66 ] involved the provision of midwife-led care at antenatal, intrapartum and postnatal time points, but continuity of care with the same/a known provider was only guaranteed at intrapartum and postnatal time points. S1 Table provides more details on each of the initiatives and S2 Table gives additional detail on models of care from LMICs.
The ‘by whom’: Providers of midwifery continuity of care
Midwives were the dominant provider of continuity of care across all settings. Services were mostly midwife-led with some reports including other cadre as well. Integration with existing services including systems for referral to obstetric services when needed was usual.
In HIC, almost all models of continuity of midwifery care involved care provided by midwives and/or midwifery students. A small number included midwives and other cadre. For example, programs with midwives and Aboriginal Health Workers (Indigenous health providers) [ 14 , 75 – 78 ]; collaborations with general practitioners, obstetricians or a social worker [ 44 , 79 – 81 ]. Just two examples did not include midwives; a model in Finland where continuity of care is provided by a nurse who takes care of the family from the pregnancy until the child reaches school age [ 26 , 82 ], and an example in Ireland [ 83 ], where continuity of care was provided by a privately practising obstetrician.
All except two of the continuity of care initiatives in LMICs were midwife-led. The initiative from Ghana [ 84 ] was provided by midwives, nurses and doctors while the one in Kenya [ 65 ] was provided by community based midwives who may have nursing or midwifery qualifications and other health professional with obstetric skills who reside in the community.
There were 16 reports which described midwifery students providing continuity of care, most of these were from Australia, Norway and Indonesia [ 74 , 85 – 101 ]. Midwifery students were placed with women, providing continuity of care to a defined number of women over their education program, as a way to engage them in this model of care [ 91 , 94 ].
The ‘for whom’: Priority groups for continuity of care initiatives
Of the 175 initiatives, 44 (25.5%) of these were implemented for women and newborns with risk of adverse outcomes ( Table 3 ). These included women from Indigenous communities, refugee and migrant populations, young mothers, women living in rural and remote areas, women who experience socioeconomic disadvantage, women with a history of substance abuse, chronic illness, and ethnic minority groups. The majority were from Australia [ 23 ], United Kingdom [ 9 ] and Canada [ 3 ]. There were four examples from LMICs, these were designed primarily for rural and remote communities in Palestine [ 67 – 69 ], Bangladesh [ 70 ], Afghanistan [ 73 ] and Kenya [ 84 ].
https://doi.org/10.1371/journal.pgph.0000935.t003
This scoping reviewed aimed to map where, how, by whom, and for whom are midwifery continuity of care models are being implemented globally. The majority of models identified were in HICs, largely in Australia and the United Kingdom. Notably, all countries where five or more continuity of midwifery care initiatives were identified in the last 10 years are high-income and provide free public healthcare to their citizens and have a distinct cadre of midwives which makes this possible (Australia, Canada, Denmark, Japan, New Zealand, Sweden, and United Kingdom). Only 18 initiatives were identified in LMICs.
There is a growing body of literature demonstrating beneficial effects of midwifery continuity of care [ 4 , 8 ]. Midwifery continuity of care is a complex, multi-faceted intervention and teasing out which elements impart benefit to recipients of care is difficult. We found that almost all papers included in this review, involved continuity of care initiatives led by midwives or midwifery students (with midwife supervision). This was despite casting the net wide to identify continuity of care initiatives provided by any health provider across two or parts of the maternal and newborn care continuum.
Reviews of continuity of care in maternal and newborn care have focused on midwife-led continuity of care compared with other models of care such as doctor-led and shared care models [ 4 , 102 ]. However, a previous integrative review of midwife-led care in LMICs, found that just over half of studies included in the review included only midwives, with other cadres of health professionals including nurses, nurse-midwives, doctors, traditional birth attendants and family planning workers [ 103 ]. Whilst there is scope for other non-midwife health providers to provide continuity of care, such as family physicians [ 104 ]and community health workers [ 105 ], which may particularly be of value in LMICs countries where there is a shortage of midwives [ 106 ], there are few studies or reports available about these continuity of care models and their benefits. Although other cadre are not precluded from providing continuity of care, this review has shown that in the global literature, continuity of care across the maternal and newborn continuum is reported to be almost exclusively provided by midwives and is a significant area of quality improvement and research interest for midwives.
An encouraging finding from this review was the significant proportion of initiatives in HICs which focussed on women and newborns with vulnerabilities related to social and economic determinants of health (23.2%). The evidence that such initiatives are feasible for a diverse range of priority groups across many countries could demonstrate recognition of the benefits of continuity of care in improving outcomes for those with greater social and economic barriers to good health outcomes. This has implications for future research in that previous studies exploring childbirth outcomes from midwifery continuity of care frequently involve low-risk women [ 4 ], or women who had self-selected to be part of a midwife-led care project and thus are more likely to experience a positive outcome. This review has revealed that initiatives in a range of settings involve groups acknowledged to be at increased risk of adverse outcome. Larger scale and robust studies of midwifery continuity of care initiatives involving populations who experience social and economic disadvantage, and/or are at increased obstetric risk are both feasible and desirable.
Implications for policy, practice, research
This review has revealed that most studies, or reports, on midwifery continuity of care describe models led by midwives within HICs. Despite the benefits of midwife-led continuity of care, none of these countries has managed to scale-up this approach to being the standard of care at a national level, other than New Zealand. This highlights the organisational challenges of widespread implementation and the importance of system-level reform to enable countries to transition to this model of care and to scale-up. This reform means having adequate funding, support to enable midwives to be educated, and regulated, to work to their full scope of practice including flexibility and autonomy, self-managed time, team space, telephone access, and being able to work safely in the community and having access to transport and referral services [ 8 , 107 ].
Fewer than 10% of initiatives included in this review were from LMICs and only one was a clinical trial. The greatest burden of maternal and newborn deaths and stillbirths exists in LMICs. In HICs, midwife-led continuity of care has potential to reduce preventable maternal and newborn mortality and morbidity and stillbirths, however system-level reform and ensuring an enabling environment is still key [ 44 ]. The lack of midwifery continuity of care initiatives in LMICs, highlights the need for greater investment to ensure well-functioning midwifery systems can be developed with monitoring, evaluation and research to understand the effect of different models and associated benefits and/or challenges in different contexts. Operational research that identifies the barriers, facilitators and blockages to implementing models of midwifery continuity of care is needed, including in settings where there are shortages of midwives. In order to facilitate transition to, and scale-up of, midwifery continuity of care in LMICs, key considerations include strengthening midwifery education and regulation and ensuring the presence of an enabling environment [ 66 , 73 ].
Future systematic and scoping review studies would be enhanced by clear reporting of midwifery continuity model type, implementation details (including on midwife competence, scope of practice, deployment) and degree of continuity achieved within published studies and reports. Establishment of a classification system for this purpose would also enhance implementation efforts. One example of a classification system in a country which has an identifiable cadre of midwives is the Maternity Care Classification System (MaCCS) which was developed to classify, record and report data about maternity models of care in Australia [ 108 , 109 ]. The MaCCS includes a series attributes including the target groups, profession of provider, the caseload size, the extent of planned continuity of care and the location of care to come up with 11 major model categories (see S3 Table for details) [ 110 ]. This classification system is now being included in all routine data systems in Australia so that, in the future, outcomes by model of care will be reported. While this is developed for one high-income country, an adaptation for global utility could be useful.
Measuring the extent to which continuity of care is achieved is the second key area. The health insurance industry in the USA has developed measures to assess patterns of visits to providers and therefore, the level of continuity of care [ 111 ]. The measures include the Bice-Boxerman Continuity of Care Index (measures the degree of coordination required between different providers during an episode), the Herfindahl Index (the degree of coordination required between different providers during an episode), the Usual Provider of Care (the concentration of care with a primary provider) and Sequential Continuity of Care Index (the number of handoffs of information required between providers). The Usual Provider of Care index has also been used to assess continuity of care in general practice in the UK, that is, to assess the proportion of a patient’s contacts that was with their most regularly seen doctor [ 112 ]. For example, if a patient had 10 general practitioner contacts, including six with the same doctor, then their usual provider of care index score would be 0.6. With the exception of one study, none of the papers in this review had applied such indexes. This is an important consideration for the future.
Strengths and limitations
This review provides a summary of midwifery continuity of care efforts globally. As countries look to strengthen midwifery and quality of care for women and newborns during pregnancy, childbirth and postnatal periods, understanding implementation in all resource settings is important. In this review the broad criteria for inclusion allowed for identifying the maximum number of implementation efforts in LMICs to be identified. Despite the efforts to reach out, and although no language filters were applied, search terms were in English thus we may have missed some ongoing efforts. We also did not measure, or account for, the skills and competencies in the different cadres providing care, or if they are always deployed as midwives or provide details about the profile/qualifications of the healthcare providers, the way the midwifery system function, if any affiliation to healthcare centres, support systems, health costs and coverage or safety outcome indicators as these were reported differently or not at all across the papers. Finally, in this review we were not able to reliably determine the extent to which women receiving care were able to see the same individual care provider. Relational continuity is a key element of continuity of care, and possible mechanism for beneficial effects, which requires repeat contact over time between individual care providers and recipients of care.
Conclusions
This review mapped midwifery continuity of care initiatives globally. The majority of initiatives identified were in HICs, with fewer identified in LMICs. Almost all initiatives identified in LMICs were led by midwives (some of whom worked in a model in which they were also deployed as nurses), despite our efforts to identify models led by other skilled health professionals. Almost no countries have managed to scale-up midwifery continuity of care to being the standard of care at a national level. This highlights the organisational challenges of widespread implementation and the importance of system-level reform to enable these models of care to scale-up. Nevertheless, examples of successful implementation of midwifery continuity of care in low-resource settings reported show that advances in this area are possible.
A number of initiatives identified in HICs focused on women and newborns at risk of adverse outcomes, demonstrating the value of midwifery continuity of care in populations who experience social and economic disadvantage and vulnerabilities. There is a need for further research on midwifery continuity of care models in LMICs, and strategies to facilitate transition to, and scale-up of, midwifery continuity of care initiatives globally.
Supporting information
S1 text. search strategy..
https://doi.org/10.1371/journal.pgph.0000935.s001
S1 Table. All included items.
https://doi.org/10.1371/journal.pgph.0000935.s002
S2 Table. Additional details from low- and middle-income countries.
https://doi.org/10.1371/journal.pgph.0000935.s003
S3 Table. Major model categories in MaCCS.
https://doi.org/10.1371/journal.pgph.0000935.s004
S1 Checklist. Preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews.
https://doi.org/10.1371/journal.pgph.0000935.s005
Acknowledgments
Thank you to Rana Islamiah Zahroh, PhD student and researcher at the University of Melbourne in Australia for assistance mapping the data. Thanks also to Rosemary Rowe, Subject Librarian at Faculty of Health, Victoria University of Wellington in New Zealand and to Allisyn Moran and Joao Paolo Souza (WHO) for useful feedback and advice.
- View Article
- PubMed/NCBI
- Google Scholar
- 5. World Health Organization. Global strategic directions for nursing and midwifery 2021–2025. Geneva: World Health Organization; 2021.
- 15. World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016.
- 16. World Health Organization. WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018.
- 17. World Health Organization. WHO recommendations on maternal and newborn care for a positive postnatal experience. Geneva: World Health Organization; 2022.
- 21. World Bank. World Development Indicators 2022. https://databank.worldbank.org/reports.aspx?source=world-development-indicators .
- 24. Cummins A, Griew K, Devonport C, Ebbett W, Catling C, Baird K. Exploring the value and acceptability of an antenatal and postnatal midwifery continuity of care model to women and midwives, using the Quality Maternal Newborn Care Framework. Women and Birth. 2021.
- 31. Health Synergy and Collaborative Business. Logan Community Maternity and Child Health Hubs Cost Analysis. Brisbane: Synergy Health and Business Collaborative; 2021.
- 35. Markesjö G. Women’s experience of pregnancy and childbirth in a continuity of care model. A qualitative study at Huddinge Hospital. Stockholm: Karolinska Institute; 2019.
- 36. Holroyd M. Midwives experiences of working within the project “Min Barnmorska”. Stockholm: Karolinska Institute; 2019.
- 63. Hailemeskel S, Alemu K, Christensson K, Tesfahun E, Lindgren H. Midwife-led continuity of care improved maternal and neonatal health outcomes in north Shoa zone, Amhara regional state, Ethiopia: A quasi-experimental study. Women and Birth. 2021.
- 70. Rahman S. Midwife led Care Centre in a Government Facility: Charikata Union Health and Family Welfare Centre (UH&FWC), Jaintiapur, Sylhet. 2021 Wednesday, Apr 20, 2022.
- 85. Baird K, Hastie C, Stanton P, Gamble J. Learning to be a midwife: Midwifery students’ experiences of an extended placement within a midwifery group practice. Women and Birth. 2021.
- 94. Newton M, Faulks F, Bailey C, Davis J, Vermeulen M, Tremayne A, et al. Continuity of care experiences: A national cross-sectional survey exploring the views and experiences of Australian students and academics. Women and Birth. 2021.
- 99. Tickle N, Gamble J, Creedy D. Clinical outcomes for women who had continuity of care experiences with midwifery students. Women and Birth. 2021.
- 106. UNFPA. State of the World’s Midwifery New York: United Nations Population Fund; 2021.
- 107. World Health Organization. Strengthening quality midwifery education for Universal Health Coverage 2030: framework for action. Geneva: World Health Organization; 2019.
- 108. Australian Institute of Health and Welfare. Maternity Care Classification System: Maternity Model of Care Data Set Specification national pilot report November 2014. Canberra: Australian Institute of Health and Welfare; 2014.
- Open access
- Published: 08 July 2020
A critical interpretive synthesis of the roles of midwives in health systems
- Cristina A. Mattison ORCID: orcid.org/0000-0001-7210-0690 1 ,
- John N. Lavis 2 ,
- Michael G. Wilson 2 ,
- Eileen K. Hutton 1 &
- Michelle L. Dion 3
Health Research Policy and Systems volume 18 , Article number: 77 ( 2020 ) Cite this article
9329 Accesses
17 Citations
12 Altmetric
Metrics details
Midwives’ roles in sexual and reproductive health and rights continues to evolve. Understanding the profession’s role and how midwives can be integrated into health systems is essential in creating evidence-informed policies. Our objective was to develop a theoretical framework of how political system factors and health systems arrangements influence the roles of midwives within the health system.
A critical interpretive synthesis was used to develop the theoretical framework. A range of electronic bibliographic databases (CINAHL, EMBASE, Global Health database, HealthSTAR, Health Systems Evidence, MEDLINE and Web of Science) was searched through to 14 May 2020 as were policy and health systems-related and midwifery organisation websites. A coding structure was created to guide the data extraction.
A total of 4533 unique documents were retrieved through electronic searches, of which 4132 were excluded using explicit criteria, leaving 401 potentially relevant records, in addition to the 29 records that were purposively sampled through grey literature. A total of 100 documents were included in the critical interpretive synthesis. The resulting theoretical framework identified the range of political and health system components that can work together to facilitate the integration of midwifery into health systems or act as barriers that restrict the roles of the profession.
Conclusions
Any changes to the roles of midwives in health systems need to take into account the political system where decisions about their integration will be made as well as the nature of the health system in which they are being integrated. The theoretical framework, which can be thought of as a heuristic, identifies the core contextual factors that governments can use to best leverage their position when working to improve sexual and reproductive health and rights.
Peer Review reports
Introduction
Midwives’ roles in sexual and reproductive health and rights (SRHR) continue to evolve and an understanding of the profession’s role in health systems is essential in creating evidence-informed policies. Countries across all income levels face challenges with providing high-quality SRHR and achieving effective coverage [ 1 ]. National or sub-national SRHR policies often do not include the midwifery workforce or account for the professions’ role in the provision of high-quality care [ 1 ]. The lack of conceptual clarity regarding the drivers of midwives’ roles within health systems, ranging from their regulation and scope of practice to their involvement in care, has resulted in significant variability both within and across countries on how the profession is integrated into health systems.
Research on midwifery care has demonstrated that the profession delivers high-quality SRHR services [ 1 , 2 , 3 ]. Care provided by midwives who are trained, licensed and regulated according to international standards is associated with improved health outcomes [ 3 , 4 , 5 , 6 , 7 ]. While midwifery care is associated with positive outcomes, it is an area that is under-researched [ 8 ]. This is particularly true in relation to how political and health system factors influence the profession’s role in health systems. As such, the roles of midwives in health systems are not clearly understood, which continues to challenge the profession’s ability to work effectively in collaborative and interprofessional settings.
Midwifery research is often dichotomised by the development status of the jurisdiction of focus — high-income countries (HICs) compared to low- and middle-income countries (LMICs). In HICs in general, midwives’ roles are focused on primary care to low-risk pregnant people through pregnancy, labour and a limited post-partum period [ 9 ]. In comparison, in LMICs, midwives’ scope of practice can be broader and extends to many aspects of SRHR [ 10 , 11 , 12 , 13 ]. International organisations (e.g. WHO, United Nations Population Fund and the International Confederation of Midwives) support an expanded approach to midwifery roles to include provision of a range of SRHR services (e.g. health counselling and education, prevention of mother-to-child HIV transmission, prevention and treatment of sexually transmitted infections, and provision of safe abortion where legal) [ 4 , 14 ].
Arguably one of the most crucial components of a health system is its health workforce, as highlighted by WHO’s framework of ‘building blocks’ to support health systems strengthening (service delivery, health workforce, health information systems, access to essential medicines, financing and governance) [ 15 ]. While midwifery is recognised as key to SRHR, there is a global shortage of the midwifery workforce [ 2 , 4 ]. Midwives who are educated and regulated according to international standards can provide 87% of a population’s essential SRHR, yet only 36% of the midwifery workforce is made up of such fully trained midwives, with a range of other health workers also delivering midwifery services [ 4 ]. The latter has been made possible by the range of roles that non-midwife health workers play in providing midwifery services [ 4 , 16 ].
The lack of understanding of the roles of midwifery in health systems has led to significant disparities within and across countries. A better understanding of the roles of midwives within the health system is desirable as they are a key component in the delivery of safe and effective SRHR and could possibly improve the cost-effectiveness of the delivery of these services [ 17 , 18 , 19 ]. There is growing recognition that, to strengthen health systems, decisions must be based on the best available research evidence [ 20 , 21 , 22 , 23 ]. Using the available research evidence to understand the roles of midwives across health systems, as well as the political and health system drivers, will yield important insights with the aim of adding to the evidence base that policy-makers can draw from.
The present study asks — across health systems, what are the factors that influence the roles of midwives within the health system? We present a theoretical framework to explain how political and health system factors influence the roles of midwives within the health system. It defines the political system as consisting of three main components, namely institutions, interests and ideas [ 24 ]. ‘Health system arrangements’ are made up of governance, financial and delivery arrangements, and implementation strategies [ 25 ]. Given the lack of theoretical development in the area, this paper, through a critical interpretive synthesis of the available literature, identifies the factors that act as barriers or facilitators to the roles of midwives.
A critical interpretive synthesis was used to develop the theoretical framework, which is an inductive approach to literature analysis. The approach uses conventional systematic review processes while incorporating qualitative inquiries to examine both the empirical and non-empirical literature [ 22 ]. Critical interpretive syntheses are best suited to developing theoretical frameworks that draw on a wide range of relevant sources and are particularly useful when there is a diverse body of literature that is not clearly defined, as is the case with literature related to the roles of midwives in health systems. Conventional systematic reviews have well formulated research questions at the outset, while a critical interpretive synthesis employs a compass question, which is highly iterative and responsive to the findings generated in the review process [ 26 ].
Literature search
The selection of the literature was carried out in phases (Fig. 1 ). The first phase consisted of a systematic search of electronic bibliographic databases. The searches were executed in consultation with a librarian, who provided guidance on developing keywords (along with Boolean operators) and MeSH (Medical Subject Heading), refining the search strategy, identifying additional databases and executing the searches. We searched the following electronic databases through to 14 May 2020: CINAHL, EMBASE, Global Health database, HealthSTAR, Health Systems Evidence, MEDLINE and Web of Science. The search strategy was first developed in the MEDLINE database, using keywords and MeSH. Similar search strings were used across databases, with minor adjustments made to ensure search optimisation. The searches in MEDLINE included midwi* AND (roles OR scope), midwi* AND delivery of health care (MeSH), midwi* AND patient satisfaction (MeSH), midwi* AND quality of health care (MeSH), and midwi* AND standards (MeSH).
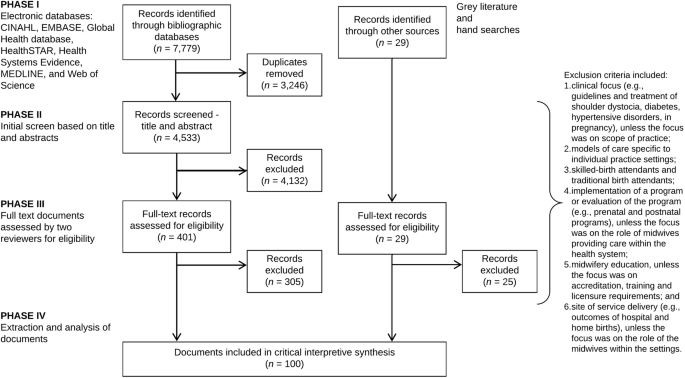
Literature search and study selection flow diagram
The second phase, complementary to the bibliographic database search, was a search of policy and health systems-related SRHR and midwifery organisation websites for relevant documents (e.g. World Health Assembly resolutions and United Nations Population Fund’s State of the World’s Midwifery reports). In addition, hand searches of reference lists from key publications were used to identify further relevant literature (e.g. 2014 Lancet Series on Midwifery). The final step in the literature search process was a purposive search to identify literature to fill the conceptual gaps that emerged.
Article selection
For inclusion, the documents had to relate specifically to trained midwives, with leeway in terms of title (e.g. certified nurse-midwives and certified midwives in the United States). Articles were included, that in addition to providing insight into the compass question, also (1) incorporated a range of perspectives across different countries; (2) integrated different concepts into one document; and (3) included perspectives on the compass question from other disciplines (e.g. geographic information system and other techniques to map the distribution of the midwifery workforce). In order to incorporate a broad range of documents, there were no limits placed on the searches such as regarding language or publication year.
An explicit set of exclusion criteria were developed by the research team to remove the documents that were not relevant to the aims of the study and did not link to the compass question. Exclusion criteria included documents (1) with a clinical focus (e.g. clinical guidelines, pharmacology, diagnostics, devices, surgery and/or treatment of shoulder dystocia, diabetes, hypertensive disorders, in pregnancy), unless the focus was on scope of practice (e.g. midwives working in expanded scopes); (2) focused on models of care that were specific to individual practices or hospitals and included those that were related to health system approaches; (3) relating to unskilled workers providing SRHR (e.g. traditional birth attendants); (4) focused on implementation of a programme or evaluation of the programme (e.g. prenatal and postnatal programmes), unless the focus was on the roles of midwives providing care within the health system; (5) focused on midwifery education, unless the focus was on accreditation, training and licensure requirements; and (6) focused on site of service delivery (e.g. outcomes of hospital and home births), unless the focus was on the roles of midwives within the different practice settings.
Once the series of searches were completed, an Endnote database was created to store and manage the results. All the duplicates were removed from the database and an initial review of the titles and abstracts was performed for each entry by the principal investigator (CAM) and records were classified as ‘possibly include’ or ‘exclude’. In the first stage of screening, records were marked as ‘possibly include’ if they provided insight into the study’s compass question. Full-text copies of the remaining records were retrieved and uploaded to Covidence, an online tool for systematic reviews, for final screening [ 27 ].
The last stage of screening involved two phases and consisted of full-text review by three reviewers (CAM, TD and KMB). Using Covidence, each reviewer examined the records independently to assess inclusion. Any discrepancies were discussed and resolved. The reviewers prioritised the inclusion of empirical articles where possible, including empirical qualitative studies, which are the types of articles most likely to address political and health system components.
Data analysis and synthesis
A coding structure was created to guide the data extraction. The areas of expertise of the authors (health systems and policy, clinical practice and political science) informed the selection of frameworks guiding the data extraction. The political system factors were informed through the 3i framework, which is a broad typology that recognises the complex interplay among institutions, interests, and ideas and provides a way of organising the many factors that can influence policy choices [ 24 , 28 , 29 , 30 ]. Institutions are made up of government structures (e.g. federal versus unitary government), policy legacies (e.g. the roles of past policies) and policy networks (e.g. relationships between actors around a policy issue). Interests can include a range of actors who may face (concentrated or diffuse) benefits and costs with particular courses of action, whereas ideas relate to peoples’ beliefs (including those based on research evidence) and values.
‘Health system arrangements’ were informed through an established taxonomy developed by the McMaster Health Forum that includes (1) governance arrangements (e.g. policy authority, organisational authority and professional authority); (2) financial arrangements (e.g. how systems are financed and health professionals remunerated); (3) delivery arrangements (e.g. how care meets consumers’ needs, who provides the care and where it is provided); and (4) implementation strategy (consumer- or provider-targeted strategies) [ 25 ]. The components of the framework for quality maternal and newborn care (practice categories, organisation of care, values, philosophy and health professionals) were incorporated into the health system arrangements coding structure to yield insights specific to midwifery care [ 3 ].
In addition to the frameworks that guided data extraction, further data was collected on publication year, study design and jurisdiction(s) of focus. A data extraction form was developed based on all of the concepts covered in the frameworks as well as the additional descriptive items.
The critical interpretive synthesis was conducted on the high value articles — those that yielded the most insight into the compass question. The reviewers prioritised the inclusion of empirical articles that were conceptually rich or integrated different concepts, filled disciplinary gaps, captured a breadth of perspectives across different countries or applied approaches outside of health. The articles were read by the principal investigator (CAM) and one- or two-page detailed summaries were created for each article. The summaries were coded using the qualitative software NVivo for Mac, which facilitates the organisation and coding of the data [ 31 ]. Coding was informed by the three key frameworks guiding the analysis and outlined above: 3i framework, ‘health system arrangements’ and components of the framework for quality maternal and newborn care.
Three steps were involved in the analysis for the critical interpretive synthesis. First, the summaries of the articles were coded based on the coding structure outlined in the data extraction form. Using a constant comparative method, emerging data were compared to previously collected data to find similarities and differences [ 32 , 33 ]. The approach included observations on the terms and concepts used to describe midwifery within the health system as well as relationships between the concepts. For example, how the role of midwives within the health system is influenced by policy legacies (i.e. institutions), which is related to problems with collaborative/interprofessional environments (i.e. delivery arrangements, skill mix and interprofessional teams). Second, all the data collected under each code was reviewed and more detailed notes of the concepts that emerged were included in the analysis. Lastly, themes were created for the concepts that emerged throughout the analysis.
Completeness of the findings was ensured through ongoing consultation with members of the research team. Central concepts and emerging themes of the study were discussed as a team and applied to current scholarship within the field of health systems and policy.
Search results and article selection
A total of 7779 records were identified through the searches of electronic bibliographic databases. Once duplicates were removed ( n = 3246), the remaining records ( n = 4533) were screened based on title, abstract and the explicit set of exclusion criteria outlined above, leaving 401 potentially relevant records. In addition to the electronic database search, 29 records were purposively sampled for inclusion through grey literature and hand searches. The remaining 401 documents from the electronic database searches and 29 documents from the grey literature and hand searches were assessed by the reviewers (CAM, TD and KMB) for inclusion using the full text. A total of 100 documents were included in the critical interpretive synthesis (Fig. 1 ).
Over three-quarters (79%) of the documents were published after 2010, with no documents published prior to 2000. Of the 100 documents, the majority were primary research ( n = 78), which were mostly qualitative research ( n = 24) and observational studies ( n = 24), followed by the ‘other’ category ( n = 18) (e.g. geographic information systems research), systematic reviews ( n = 15) and mixed methods ( n = 4), while 1 was a randomised control trial. The remaining documents were categorised as non-research ( n = 22), meaning that the approaches taken in the documents were either not systematic or that the methods were not reported transparently. Of the non-research documents, 8 were theoretical papers, 7 were reviews (non-systematic), 4 were ‘other’ (e.g. World Health Assembly resolutions, toolkits, etc.), and the remaining 3 were editorials. Forty-one of the documents focused on LMIC settings, followed by 35 on HIC settings, and 24 focused on both HIC and LMIC settings.
The results of the critical interpretive synthesis focused on the political and health system factors that influenced the roles of midwives within health systems. Table 1 focuses on the political system factors that emerged from the analysis and presents the relevant themes, relationships with other factors, and key examples from the literature of the factors that acted as either barriers or facilitators to the roles of midwives within the health system. Similarly, Table 2 focuses on the health system factors and presents the relevant themes, relationships with other factors, and key examples from the literature on the ‘health system arrangements’ that either acted as barriers or facilitators to the roles of midwives.
Three main findings emerged from the analysis on political system factors. First, within institutions, the effects of past policies regarding the value of midwives created interpretive effects, shaping the way midwifery care is organised in the health system. The legacies of these policies created barriers, which include SRHR policies that reinforced structural gender inequalities as well as, in a medical model, payment systems privileging physician-provided and hospital-based services [ 11 , 13 , 34 , 41 , 42 , 43 , 44 , 45 , 47 , 48 , 49 , 50 , 51 , 52 , 54 , 55 , 56 , 57 , 58 , 59 , 61 , 62 , 63 , 65 ].
Second, interest groups played an important role in either supporting or opposing the integration of midwifery in the health system. These groups can have direct or indirect influence and policies that provide concentrated benefits and diffuse costs for groups are more likely to move forward [ 24 ]. Interest groups advanced the integration of midwifery in the health system by (1) creating partnerships to improve SRHR [ 45 , 67 ]; (2) promoting regulation and accreditation (e.g. accreditation requirements, setting standards, policies and guidelines) [ 63 , 68 , 69 , 70 ]; (3) capacity-building including midwifery research [ 71 , 72 ]; (4) policy leadership and decision-making [ 43 ]; and (5) lobbying governments and advocacy [ 73 , 74 ]. Strong leadership from midwifery professional associations engaged in policy dialogue and decision-making has helped advance agendas related to universal health coverage and meeting health-related United Nations Sustainable Development Goals [ 8 , 63 , 66 , 71 , 90 ].
Third, the most relevant themes related to ideas that emerged from the analysis pertained to societal values regarding gender (women’s roles within society) as well as the medical model (historical medicalisation of the birth process and associated growth of physician-provided and hospital-based care). We recognise the importance of gender-inclusive language but have use the term ‘women’ in this publication to reflect how gender is referenced in the documents reviewed. Barriers created by societal values included (1) social construction of gender and the status of midwives in a given jurisdiction often reflected the value placed on women within society (i.e. ‘gender penalty’) [ 8 , 11 , 41 , 43 , 46 , 48 , 61 , 71 ]; (2) some cultures and beliefs did not allow women to receive care from men, yet there were few health professionals who were women due to lack of educational opportunities and societal values that restrict women from participating in the paid labour force [ 45 ]; and (3) health system priorities and shifting societal values favoured the medical model [ 41 , 48 , 49 , 50 , 75 , 78 , 99 , 100 , 101 ]. Examples of facilitators included Nordic health systems that value non-medical models and women-dominated professional groups [ 37 ], which respect the right to informed choice [ 86 ].
Within health system factors, the main themes that emerged from the literature are presented according to ‘health system arrangements’. First, within governance arrangements, regulation and accreditation mechanisms to support midwifery education programmes and institutional capacities were central to how midwives are integrated into health systems [ 63 , 70 , 93 , 107 ]. The lack of legislation to support regulatory activities [ 34 , 43 , 48 , 58 , 71 , 82 , 87 , 93 , 94 ] limited recognition and scope [ 38 , 87 ] and the ability for midwives to practice as an autonomous profession [ 80 ]. Globally, there was a general lack of knowledge regarding the International Confederation of Midwives’ Global Standards for Midwifery Education, which was a barrier to the provision of quality midwifery education [ 53 , 66 , 87 , 107 , 108 ]. Within financial arrangements, the literature focused primarily on how systems are financed, on the inclusion of midwifery services within financing systems and on the remuneration of midwives that is reflective of scope of practice [ 1 , 2 , 6 , 10 , 13 , 35 , 38 , 39 , 43 , 50 , 55 , 56 , 57 , 58 , 59 , 61 , 69 , 73 , 74 , 76 , 80 , 84 , 95 , 101 , 104 , 109 , 115 ]. Lastly, the main themes relating to delivery arrangements focused on (1) accessing midwifery care ranging from availability and timely access to workforce supply, distribution and retention; (2) by whom care is provided (e.g. task-sharing and interprofessional teams); and (3) where care is provided (e.g. hospital-based, integration of services and continuity of care) [ 3 , 4 , 6 , 7 , 9 , 10 , 11 , 12 , 13 , 34 , 35 , 36 , 37 , 38 , 39 , 43 , 45 , 46 , 48 , 50 , 51 , 54 , 55 , 58 , 59 , 61 , 62 , 69 , 73 , 74 , 76 , 77 , 79 , 86 , 94 , 96 , 97 , 99 , 100 , 104 , 105 , 110 , 116 , 117 , 118 , 120 , 121 , 122 ].
Theoretical framework
Figure 2 brings together the main findings from the critical interpretive synthesis and presents a theoretical framework, which can be thought of as a heuristic that can be used to map the key elements that influence midwives’ roles in a particular political and health system. The factors presented in the framework are not weighted but rather present the range of variables influencing the level of integration of the profession. The cumulative effects of the barriers presented on the right-hand side of the framework lead to health systems where the profession is disempowered and midwives exist on the margins with very limited capacity. Some of the variables and examples presented in the framework have context specificity to reflect findings from the critical interpretive synthesis (e.g. self-regulated profession, Indigenous self-government, Nordic maternity care systems, and payment systems privileging physician-provided and hospital-based services in some contexts).
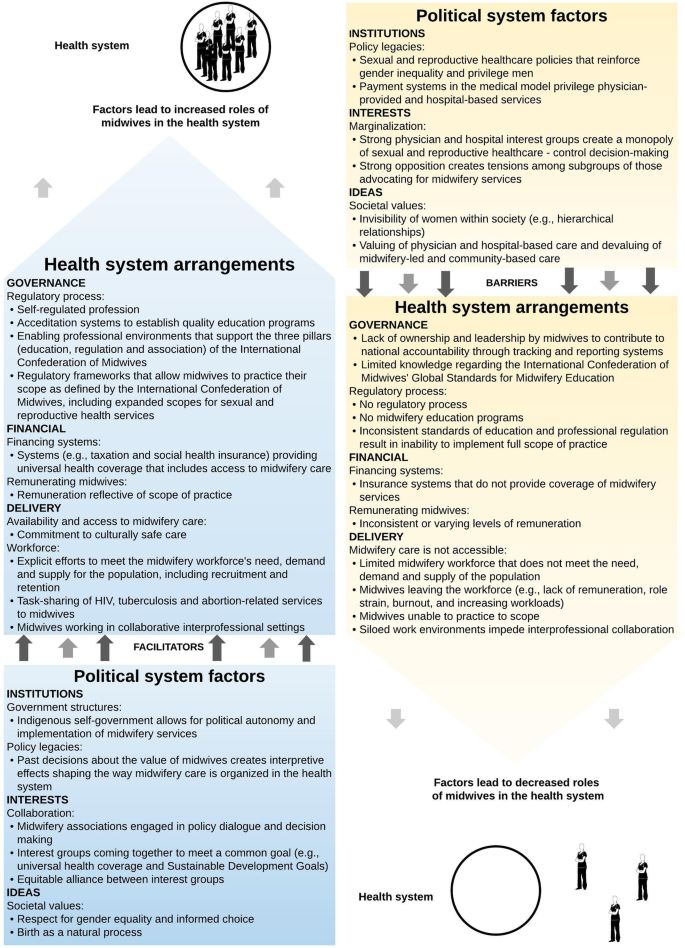
Theoretical framework of the political and health system factors that influence the roles of midwives within the health system
Principal findings
Similar to the concept of WHO’s health system ‘building blocks’, the political system factors presented in the theoretical framework form the bottom building block or the foundation for the ‘health system arrangements’, acting as either a barrier or facilitator. For example, favourable institutional factors (e.g. policy legacies that value midwifery as a profession), interests (e.g. collaborative interest groups coming together to reach a common goal) and ideas (e.g. societal values centring on gender equality and birth as a natural process) act as enablers to ‘health system arrangements’ that build on each other to support the integration of midwifery. Together, supportive political and health system factors lead to health systems where midwives practice to scope (i.e. trained, licensed and regulated according to international standards, working in collaborative/interprofessional settings with an established workforce). On the other hand, health systems that have many political and health system challenges will in turn have a limited midwifery workforce where midwives lack an institutional voice and representation in SRHR decision-making. Significant barriers limit the options available to the midwifery workforce and is most often reflected in siloed work settings with midwives working in the periphery of the health system.
Strengths and limitations of the study
The main strength of the study is the use of a critical interpretive synthesis. This is a relatively new systematic review methodology, which combines a rigorous systematic review of electronic bibliographic databases with iterative and purposive sampling of the literature to fill conceptual gaps. The approach incorporated a range of documents (empirical and non-empirical), which broadened the scope of the literature used to inform the theoretical framework.
The main limitation of the critical interpretive synthesis was that the search strategy may not have fully covered the diverse terminology used to refer to midwifery. However, the principal investigator (CAM) consulted with a librarian and team members to ensure that the search strategy was as inclusive as possible, which is also reflected by the high proportion of articles that were later excluded during the screening process. Meanwhile, the majority of articles retrieved from the searches were published after 2000, which could be related to the release of the Millennium Development Goals and subsequent Sustainable Development Goals, and the wider attention given to SRHR on global agendas.
Implications for policy and practice
Any changes to the roles of midwifery in health systems needs to take into account the political system where decisions about their integration will be made as well as the nature of the health system in which they are being integrated. The theoretical framework is a tool that helps to inform such changes by identifying the drivers of midwives’ roles that facilitate or constrain such integration. The study results have implications for policy-makers as, firstly, the theoretical framework can be used to conduct an assessment of the factors in order to strengthen the profession by identifying the facilitators that can be leveraged as well as the barriers that can be addressed to support change. For example, Sweden has favourable political system conditions (e.g. policy legacies of professionalisation of midwives dating back to the eighteenth century and an equitable alliance between midwifery and physician groups), which is reflected in the health system arrangements where midwives are the primary health professionals for low-risk pregnant people. In contrast, the United States has policy legacies of payment systems valuing physician-provided and hospital-based care, strong physician and hospital interest groups have created a monopoly over sexual and reproductive health services, and existing tensions within the profession between nurse midwives and midwives.
Moving forward, an implication for practice is that changes to further enhance the role of midwives would require different types of policy levers. In looking at growing midwifery in LMICs, governments can use the tool to understand how to best influence the integration of the profession. This information will provide valuable experience and understanding of the contextual factors so that governments can best leverage their position when working with bilateral and multilateral funders to improve SRHR. Conversely, in the example of the United States, the framework presented helps to explain why midwives play such a small role in sexual and reproductive health service delivery in the United States. The tool highlights that funding and regulatory levers would need to be pulled; yet, strong policy legacies and entrenched interests present significant barriers. Change would require spending political capital to modify existing structures within the health system.
While research evidence on the role of midwives in the provision of high-quality SRHR has increased and the 2014 Lancet Series on Midwifery was key to raising the profile of midwifery research, significant gaps in the literature persist. Structural gender inequalities are reflected in the low status of midwifery in some contexts, which leads to poor political and health systems supports to invest in quality midwifery care [ 43 ]. Our findings show that the research evidence related to the roles of midwives within health systems is relatively saturated in terms of delivery arrangements yet surprisingly little is known about governance and financial arrangements and about implementation strategies, which are key to effectively integrating midwifery and pushing the field forward in meaningful ways.
Availability of data and materials
All data generated or analysed during this study are included in this published article and summarised in Tables 1 and 2 .
Abbreviations
High-income countries
Low- and middle-income countries
- Sexual and reproductive health and rights
ten Hoope-Bender P, de Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. Lancet. 2014;384(9949):1226–35.
Article PubMed Google Scholar
Homer CS, Friberg IK, Dias MA, ten Hoope-Bender P, Sandall J, Speciale AM, et al. The projected effect of scaling up midwifery. Lancet. 2014;384(9948):1146–57.
Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet. 2014;384(9948):1129–45.
UNFPA. The State of the World’s Midwifery 2014. Geneva: United Nations Population Fund; 2014.
Google Scholar
Hutton EK, Cappelletti A, Reitsma AH, Simioni J, Horne J, McGregor C, et al. Outcomes associated with planned place of birth among women with low-risk pregnancies. CMAJ. 2016;188(5):E80–90.
Malott AM, Davis BM, McDonald H, Hutton E. Midwifery care in eight industrialized countries: how does Canadian midwifery compare? J Obstet Gynaecol Can. 2009;31(10):974–9.
Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev. 2013;8:CD004667.
Renfrew MJ, Ateva E, Dennis-Antwi JA, Davis D, Dixon L, Johnson P, et al. Midwifery is a vital solution-what is holding back global progress? Birth. 2019;46(3):396–9.
Malott AM, Kaufman K, Thorpe J, Saxell L, Becker G, Paulette L, et al. Models of organization of maternity care by midwives in Canada: a descriptive review. J Obstet Gynaecol Can. 2012;34(10):961–70.
Bartlett L, Weissman E, Gubin R, Patton-Molitors R, Friberg IK. The impact and cost of scaling up midwifery and obstetrics in 58 low- and middle-income countries. PLoS One. 2014;9(6):e98550.
Article PubMed PubMed Central CAS Google Scholar
Fauveau V, Sherratt DR, de Bernis L. Human resources for maternal health: multi-purpose or specialists? Hum Resour Health. 2008;6:21.
Article PubMed PubMed Central Google Scholar
Holcombe SJ, Berhe A, Cherie A. Personal beliefs and professional responsibilities: Ethiopian midwives’ attitudes toward providing abortion services after legal reform. Stud Fam Plan. 2015;46(1):73–95.
Article Google Scholar
Liljestrand J, Sambath MR. Socio-economic improvements and health system strengthening of maternity care are contributing to maternal mortality reduction in Cambodia. Reprod Health Matters. 2012;20(39):62–72.
ICM. International definition of the midwife. The Hague: International Confederation of Midwives; 2017. https://www.internationalmidwives.org/assets/files/definitions-files/2018/06/eng-definition_of_the_midwife-2017.pdf .
World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva: WHO; 2020. https://www.who.int/healthinfo/systems/WHO_MBHSS_2010_full_web.pdf .
Lopes SC, Titulaer P, Bokosi M, Homer CS, ten Hoope-Bender P. The involvement of midwives associations in policy and planning about the midwifery workforce: a global survey. Midwifery. 2015;31(11):1096–103.
Janssen PA, Mitton C, Aghajanian J. Costs of planned home vs. hospital birth in British Columbia attended by registered midwives and physicians. PLoS One. 2015;10(7):e0133524.
Reinharz D, Blais R, Fraser WD, Contandriopoulos A-P. Cost-effectiveness of midwifery services vs. medical services in Quebec. Can J Public Health. 2000;91(1):I12.
Article CAS PubMed PubMed Central Google Scholar
Schroeder E, Petrou S, Patel N, Hollowell J, Puddicombe D, Redshaw M, et al. Cost effectiveness of alternative planned places of birth in woman at low risk of complications: evidence from the Birthplace in England national prospective cohort study. BMJ. 2012;344:e2292.
Lavis J, Davies H, Oxman A, Denis JL, Golden-Biddle K, Ferlie E. Towards systematic reviews that inform health care management and policy-making. J Health Serv Res Policy. 2005;10(Suppl 1):35–48.
Lavis JN, Guindon GE, Cameron D, Boupha B, Dejman M, Osei EJ, et al. Bridging the gaps between research, policy and practice in low- and middle-income countries: a survey of researchers. CMAJ. 2010;182(9):E350–61.
Moat KA, Lavis JN, Abelson J. How contexts and issues influence the use of policy-relevant research syntheses: a critical interpretive synthesis. Milbank Q. 2013;91(3):604–48.
Wilson MG, Moat KA, Lavis JN. The global stock of research evidence relevant to health systems policymaking. Health Res Policy Syst. 2013;11:32.
Lazar H, Lavis JN, Forest P-G, Church J. Paradigm freeze: why it is so hard to reform health care in Canada. Montreal: McGill-Queen’s University Press; 2013.
Lavis JN, Wilson MG, Moat KA, Hammill AC, Boyko JA, Grimshaw JM, et al. Developing and refining the methods for a ‘one-stop shop’for research evidence about health systems. Health Res Policy Syst. 2015;13:10.
Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35.
Covidence. About us Australia: Covidence; 2017. https://www.covidence.org/about-us .
Hall PA. The role of interests, institutions, and ideas in the comparative political economy of the industrialized nations. In: Comparative politics: rationality, culture, and structure. Cambridge: Cambridge University Press; 1997. p. 174–207.
Oliver MJ, Pemberton H. Learning and change in 20th-century British economic policy. Governance. 2004;17(3):415–41.
Walsh JI. When do ideas matter? Explaining the successes and failures of Thatcherite ideas. Comp Political Stud. 2000;33(4):483–516.
QSR International. NVivo for Mac Australia: QSR International; 2017. http://www.qsrinternational.com/product/nvivo-mac .
Charmaz K. Constructing grounded theory. London: Sage; 2014.
Glaser BG, Strauss A. The discovery of ground theory. Chicago: Aldine; 1967.
Van Wagner V, Epoo B, Nastapoka J, Harney E. Reclaiming birth, health, and community: Midwifery in the Inuit villages of Nunavik, Canada. J Midwifery Womens Health. 2007;52(4):384–91.
Epoo B, Stonier J, Wagner VV, Harney E. Learning midwifery in Nunavik: community-based education for Inuit midwives. J Indigenous Wellbeing. 2012;10(3):283–99.
Wagner V, Osepchook C, Harney E, Crosbie C, Tulugak M. Remote midwifery in Nunavik, Quebec, Canada: outcomes of perinatal care for the Inuulitsivik Health Centre, 2000-2007. Birth Issue Perinat Care. 2012;39(3):230–7.
Wrede S, Benoit C, Einarsdottir T. Equity and dignity in maternity care provision in Canada, Finland and Iceland. Can J Public Health. 2008;99:S16–21.
DeMaria LM, Campero L, Vidler M, Walker D. Non-physician providers of obstetric care in Mexico: perspectives of physicians, obstetric nurses and professional midwives. Hum Resour Health. 2012;10:6.
Van Lerberghe W, Matthews Z, Achadi E, Ancona C, Campbell J, Channon A, et al. Country experience with strengthening of health systems and deployment of midwives in countries with high maternal mortality. Lancet. 2014;384(9949):1215–25.
Bogren M, Erlandsson K. Opportunities, challenges and strategies when building a midwifery profession. Findings from a qualitative study in Bangladesh and Nepal. Sex Reprod Healthc. 2018;16:45–9.
Temmar F, Vissandjee B, Hatem M, Apale A, Kobluk D. Midwives in Morocco: seeking recognition as skilled partners in women-centred maternity care. Reprod Health Matters. 2006;14(27):83–90.
Betron ML, McClair TL, Currie S, Banerjee J. Expanding the agenda for addressing mistreatment in maternity care: a mapping review and gender analysis. Reprod Health. 2018;15(1):143.
Filby A, McConville F, Portela A. What prevents quality midwifery care? A systematic mapping of barriers in low and middle income countries from the provider perspective. PLoS One. 2016;11(5):e0153391.
Witter S, Namakula J, Wurie H, Chirwa Y, So S, Vong S, et al. The gendered health workforce: mixed methods analysis from four fragile and post-conflict contexts. Health Policy Plann. 2017;32(Suppl. 5):v52–62.
Turkmani S, Currie S, Mungia J, Assefi N, Rahmanzai AJ, Azfar P, et al. ‘Midwives are the backbone of our health system’: lessons from Afghanistan to guide expansion of midwifery in challenging settings. Midwifery. 2013;29(10):1166–72.
Beek K, McFadden A, Dawson A. The role and scope of practice of midwives in humanitarian settings: a systematic review and content analysis. Hum Resour Health. 2019;17:5.
Devane D, Murphy-Lawless J, Begley CM. Childbirth policies and practices in Ireland and the journey towards midwifery-led care. Midwifery. 2007;23(1):92–101.
Brodie P. Addressing the barriers to midwifery--Australian midwives speaking out. Aust J Midwifery. 2002;15(3):5–14.
Christiaens W, Nieuwenhuijze MJ, de Vries R. Trends in the medicalisation of childbirth in Flanders and the Netherlands. Midwifery. 2013;29(1):e1–8.
Goodman S. Piercing the veil: the marginalization of midwives in the United States. Soc Sci Med. 2007;65(3):610–21.
Kennedy HP, Rousseau AL, Low LK. An exploratory metasynthesis of midwifery practice in the United States. Midwifery. 2003;19(3):203–14.
Mattison CA, Lavis JN, Hutton EK, Dion ML, Wilson MG. Understanding the conditions that influence the roles of midwives in Ontario, Canada’s health system: an embedded single-case study. BMC Health Serv Res. 2020;20(1):197.
Barger MK, Hackley B, Bharj KK, Luyben A, Thompson JB. Knowledge and use of the ICM global standards for midwifery education. Midwifery. 2019;79:102534.
James S, O'Brien B, Bourret K, Kango N, Gafvels K, Paradis-Pastori J. Meeting the needs of Nunavut families: a community-based midwifery education program. Circumpolar special issue: human health at the ends of the earth. Rural Remote Health. 2010;10(2):1355.
PubMed Google Scholar
Kildea S, Kruske S, Barclay L, Tracy S. ‘Closing the gap’: how maternity services can contribute to reducing poor maternal infant health outcomes for Aboriginal and Torres Strait Islander women. Rural Remote Health. 2010;10(3):1383.
CAS PubMed Google Scholar
Kreiner M. Delivering diversity: newly regulated midwifery returns to Manitoba, Canada, one community at a time. J Midwifery Women Health. 2009;54(1):e1–e10.
National Aboriginal Health Organization. Midwifery and aboriginal midwifery in Canada. Ottawa: National Aboriginal Health Organization; 2004.
Skye AD. Aboriginal midwifery: a model for change. Int J Indigenous Health. 2010;6(1):28–37.
Mavalankar D, Raman PS, Vora K. Midwives of India: missing in action. Midwifery. 2011;27(5):700–6.
Munabi-Babigumira S, Nabudere H, Asiimwe D, Fretheim A, Sandberg K. Implementing the skilled birth attendance strategy in Uganda: a policy analysis. BMC Health Serv Res. 2019;19:655.
Day-Stirk F, Fauveau V. The state of the world’s midwifery: making the invisible visible. Int J Gynecol Obstet. 2012;119:S39–41.
Hogberg U. The decline in maternal mortality in Sweden: the role of community midwifery. Am J Public Health. 2004;94(8):1312–20.
ten Hoope-Bender P, Lopes STC, Nove A, Michel-Schuldt M, Moyo NT, Bokosi M, et al. Midwifery 2030: a woman’s pathway to health. What does this mean? Midwifery. 2016;32:1–6.
Shakibazadeh E, Namadian M, Bohren MA, Vogel JP, Rashidian A, Pileggi VN, et al. Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. BJOG. 2018;125(8):932–42.
Article CAS PubMed Google Scholar
Oliver K, Parolin Z. Assessing the policy and practice impact of an international policy initiative: the state of the world’s midwifery 2014. BMC Health Serv Res. 2018;18(1):499.
World Health Organization. Nursing and Midwifery in the history of the World Health Organization 1948–2017. Geneva: WHO; 2017.
Spies LA, Garner SL, Faucher MA, Hastings-Tolsma M, Riley C, Millenbruch J, et al. A model for upscaling global partnerships and building nurse and midwifery capacity. Int Nurs Rev. 2017;64(3):331–44.
Chamberlain J, McDonagh R, Lalonde A, Arulkumaran S. The role of professional associations in reducing maternal mortality worldwide. Int J Gynecol Obstet. 2003;83(1):94–102.
Article CAS Google Scholar
Haththotuwa R, Senanayake L, Senarath U, Attygalle D. Models of care that have reduced maternal mortality and morbidity in Sri Lanka. Int J Gynaecol Obstet. 2012;119(Suppl 1):S45–9.
de Bernis L. Implementation of midwifery school accreditation mechanisms in Ivory Coast, Mali and Chad. Sante Publique. 2018;30:57–63.
Homer CSE, Castro Lopes S, Nove A, Michel-Schuldt M, McConville F, Moyo NT, et al. Barriers to and strategies for addressing the availability, accessibility, acceptability and quality of the sexual, reproductive, maternal, newborn and adolescent health workforce: addressing the post-2015 agenda. BMC Pregnancy Childbirth. 2018;18(1):55.
Nabirye RC, Kinengyere AA, Edwards G. Nursing and midwifery research output in Africa: a review of the literature. Int J Childbirth. 2018;8(4):236–41.
Koblinsky M, Matthews Z, Hussein J, Mavalankar D, Mridha MK, Anwar I, et al. Going to scale with professional skilled care... third in a series of five articles. Lancet. 2006;368(9544):1377–86.
World Health Organization. Munich declaration – nurses and midwives: a force for health. Intensive Crit Care Nurs. 2000;16(4):207–8.
Vedam S, Stoll K, MacDorman M, Declercq E, Cramer R, Cheyney M, et al. Mapping integration of midwives across the United States: impact on access, equity, and outcomes. PLoS One. 2018;13(2):e0192523.
Downe S, Finlayson K, Fleming A. Creating a collaborative culture in maternity care. J Midwifery Womens Health. 2010;55(3):250–4.
College of Midwives of Ontario. The Midwifery Scope of Practice: The College of Midwives of Ontario Submission to the Health Professions Regulatory Advisory Council. Toronto: College of Midwives of Ontario; 2008.
Hoope-Bender P, Renfrew MJ. Midwifery – a vital path to quality maternal and newborn care: the story of the Lancet series on midwifery. Midwifery. 2014;30(11):1105–6.
Scholmerich VL, Posthumus AG, Ghorashi H, Waelput AJ, Groenewegen P, Denktas S. Improving interprofessional coordination in Dutch midwifery and obstetrics: a qualitative study. BMC Pregnancy Childbirth. 2014;14:145.
Peterson C. Midwifery and the crowning of health care reform. J Midwifery Womens Health. 2010;55(1):5–8.
Bogren MU, Berg M, Edgren L, Ev T, Wigert H. Shaping the midwifery profession in Nepal - uncovering actors’ connections using a Complex Adaptive Systems framework. Sex Reprod Healthc. 2016;10:48–55.
Bogren MU, van Teijlingen E, Berg M. Where midwives are not yet recognised: a feasibility study of professional midwives in Nepal. Midwifery. 2013;29(10):1103–9.
Klopper HC, Madigan E, Vlasich C, Albien A, Ricciardi R, Catrambone C, et al. Advancement of global health: recommendations from the Global Advisory Panel on the Future of Nursing & Midwifery (GAPFON (R)). J Adv Nurs. 2020;76(2):741–8.
Binfa L, Pantoja L, Ortiz J, Gurovich M, Cavada G. Assessment of the implementation of the model of integrated and humanised midwifery health services in Santiago, Chile. Midwifery. 2013;29(10):1151–7.
Bergevin Y, Fauveau V, McKinnon B. Towards ending preventable maternal deaths by 2035. Semin Reprod Med. 2015;33(1):23–9.
Donnay F. Maternal survival in developing countries: what has been done, what can be achieved in the next decade. Int J Gynecol Obstet. 2000;70(1):89–97.
Castro Lopes S, Nove A, Hoope-Bender P, Bernis LD, Bokosi M, Moyo NT, et al. A descriptive analysis of midwifery education, regulation and association in 73 countries: the baseline for a post-2015 pathway. Hum Resour Health. 2016;14:37.
Bvumbwe T, Mtshali N. Nursing education challenges and solutions in Sub Saharan Africa: an integrative review. BMC Nurs. 2018;17:3.
Yalahow A, Hassan M, Foster AM. Training reproductive health professionals in a post-conflict environment: exploring medical, nursing, and midwifery education in Mogadishu, Somaila. Reprod Health Matters. 2017;25(51):114–23.
Ajuebor O, McCarthy C, Li Y, Al-Blooshi SM, Makhanya N, Cometto G. Are the global strategic directions for strengthening nursing and midwifery 2016–2020 being implemented in countries? Findings from a cross-sectional analysis. Hum Resour Health. 2019;17:54.
Nagle C, McDonald S, Morrow J, Kruger G, Cramer R, Couch S, et al. Informing the development midwifery standards for practice: a literature review for policy development. Midwifery. 2019;76:8–20.
Sandwell R, Bonser D, Hebert E, Kilroy K, Leshabari S, Mwanga F, et al. Stronger together: midwifery twinning between Tanzania and Canada. Glob Health. 2018;14(1):123.
West F, Homer C, Dawson A. Building midwifery educator capacity in teaching in low and lower-middle income countries. A review of the literature. Midwifery. 2016;33:12–23.
Colvin CJ, de Heer J, Winterton L, Mellenkamp M, Glenton C, Noyes J, et al. A systematic review of qualitative evidence on barriers and facilitators to the implementation of task-shifting in midwifery services. Midwifery. 2013;29(10):1211–21.
Sidebotham M, Fenwick J, Rath S, Gamble J. Midwives’ perceptions of their role within the context of maternity service reform: an appreciative inquiry. Women Birth. 2015;28(2):112–20.
McCarthy CF, Voss J, Verani AR, Vidot P, Salmon ME, Riley PL. Nursing and midwifery regulation and HIV scale-up: Establishing a baseline in East, Central and Southern Africa. J Int AIDS Soc. 2013;16:18051.
Jenkins GL. Burning bridges: policy, practice, and the destruction of midwifery in rural Costa Rica. Soc Sci Med. 2003;56(9):1893–909.
Fullerton J, Severino R, Brogan K, Thompson J. The International Confederation of Midwives’ study of essential competencies of midwifery practice. Midwifery. 2003;19(3):174–90.
Amelink-Verburg MP, Buitendijk SE. Pregnancy and labour in the Dutch maternity care system: what is normal? The role division between midwives and obstetricians. J Midwifery Women Health. 2010;55(3):216–25.
Homer CSE, Passant L, Brodie PM, Kildea S, Leap N, Pincombe J, et al. The role of the midwife in Australia: views of women and midwives. Midwifery. 2009;25(6):673–81.
Spendlove Z. Risk and boundary work in contemporary maternity care: tensions and consequences. Health Risk Soc. 2018;20(1–2):63–80.
Summer A, Walker D, Guendelman S. A review of the forces influencing maternal health policies in post-war Guatemala. World Med Health Policy. 2019;11(1):59–82.
Summer A, Walker D. Recommendations for sustainable midwifery in Guatemala. World Med Health Policy. 2018;10(4):356–80.
Kopacz L, Pawelec M, Pietras J, Karmowski A, Palczynski B, Karmowski M, et al. The Polish way to better midwifery or commercialization of maternity services? Adv Clin Exp Med. 2011;20(4):513–20.
Biro MA. What has public health got to do with midwifery? Midwives’ role in securing better health outcomes for mothers and babies. Women Birth. 2011;24(1):17–23.
Homer CSE, Passant L, Kildea S, Pincombe J, Thorogood C, Leap N, et al. The development of national competency standards for the midwife in Australia. Midwifery. 2007;23(4):350–60.
Luyben A, Barger M, Avery M, Bharj KK, O'Connell R, Fleming V, et al. Exploring global recognition of quality midwifery education: vision or fiction? Women Birth. 2017;30(3):184–92.
Zhu X, Yao JS, Lu JY, Pang RY, Lu H. Midwifery policy in contemporary and modern China: from the past to the future. Midwifery. 2018;66:97–102.
McNeill J, Lynn F, Alderdice F. Public health interventions in midwifery: a systematic review of systematic reviews. BMC Public Health. 2012;12:955.
Mainey L, O'Mullan C, Reid-Searl K, Taylor A, Baird K. The role of nurses and midwives in the provision of abortion care: a scoping review. J Clinical Nurs. 2020;29(9–10):1513–26.
Fullerton J, Butler MM, Aman C, Reid T, Dowler M. Abortion-related care and the role of the midwife: a global perspective. Int J Womens Health. 2018;10:751–62.
Massot E, Epaulard O. Midwives’ perceptions of vaccines and their role as vaccinators: the emergence of a new immunization corps. Vaccine. 2018;36(34):5204–9.
Van Hoover C, Holt L. Midwifing the end of life: expanding the scope of modern midwifery practice to reclaim palliative care. J Midwifery Women Health. 2016;61(3):306–14.
Alayande A, Mamman-Daura F, Adedeji O, Muhammad AZ. Midwives as drivers of reproductive health commodity security in Kaduna State, Nigeria. Eur J Contracept Reprod Health Care. 2016;21(3):207–12.
Ir P, Korachais C, Chheng K, Horemans D, Van Damme W, Meessen B. Boosting facility deliveries with results-based financing: a mixed-methods evaluation of the government midwifery incentive scheme in Cambodia. BMC Pregnancy Childbirth. 2015;15:170.
King TL, Laros RK, Parer JT. Interprofessional collaborative practice in obstetrics and midwifery. Obstet Gynecol Clin North Am. 2012;39(3):411–22.
Arias MG, Nove A, Michel-Schuldt M, Bernis L. Current and future availability of and need for human resources for sexual, reproductive, maternal and newborn health in 41 countries in Sub-Saharan Africa. Int J Equity Health. 2017;16(1):69.
Suleiman-Martos N, Albendin-Garcia L, Gomez-Urquiza JL, Vargas-Roman K, Ramirez-Baena L, Ortega-Campos E, et al. Prevalence and predictors of burnout in midwives: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(2):641.
Article PubMed Central Google Scholar
Nove A. The quality of midwifery education in six French-speaking sub-Saharan African countries. Sante Publique. 2018;30:45–55.
Renner RM, Brahmi D, Kapp N. Who can provide effective and safe termination of pregnancy care? A systematic review. BJOG. 2013;120(1):23–31.
Miyake S, Speakman EM, Currie S, Howard N. Community midwifery initiatives in fragile and conflict-affected countries: a scoping review of approaches from recruitment to retention. Health Policy Plan. 2017;32(1):21–33.
Sami S, Amsalu R, Dimiti A, Jackson D, Kenyi S, Meyers J, et al. Understanding health systems to improve community and facility level newborn care among displaced populations in South Sudan: a mixed methods case study. BMC Pregnancy Childbirth. 2018;18(1):325.
Download references
Acknowledgements
The authors would like to thank Kirsty Bourret and Tomasso D’Ovidio for their assistance with assessing documents for eligibility and inclusion in the review.
There are no sources of funding to declare for this research.
Author information
Authors and affiliations.
Department of Obstetrics and Gynecology, McMaster Midwifery Research Centre, 1280 Main St. West, HSC-4H26, Hamilton, ON, L8S 4K1, Canada
Cristina A. Mattison & Eileen K. Hutton
McMaster Health Forum, 1280 Main St West, MML-417, Hamilton, ON, L8S 4L6, Canada
John N. Lavis & Michael G. Wilson
Department of Political Science, McMaster University, 1280 Main St. West, KTH-533, Hamilton, ON, L8S 4M4, Canada
Michelle L. Dion
You can also search for this author in PubMed Google Scholar
Contributions
CAM conceived the study design with her supervisor, JNL, and was responsible for all data collection and analysis. JNL, EKH, MGW and MLD provided content expertise (health systems and health policy, clinical practice and political science) to inform the selection of frameworks guiding the data extraction. All authors contributed to the development of the conceptual framework and approved the final manuscript.
Corresponding author
Correspondence to Cristina A. Mattison .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mattison, C.A., Lavis, J.N., Wilson, M.G. et al. A critical interpretive synthesis of the roles of midwives in health systems. Health Res Policy Sys 18 , 77 (2020). https://doi.org/10.1186/s12961-020-00590-0
Download citation
Received : 27 January 2020
Accepted : 14 June 2020
Published : 08 July 2020
DOI : https://doi.org/10.1186/s12961-020-00590-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Political systems
- Health systems
- Critical interpretive synthesis
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 05 October 2023
Strengthening quality in sexual, reproductive, maternal, and newborn health systems in low- and middle-income countries through midwives and facility mentoring: an integrative review
- Rondi Anderson 1 ,
- Sojib Bin Zaman 2 ,
- Abdun Naqib Jimmy 3 ,
- Jonathan M Read 4 &
- Mark Limmer 1
BMC Pregnancy and Childbirth volume 23 , Article number: 712 ( 2023 ) Cite this article
1311 Accesses
3 Altmetric
Metrics details
There is an urgent global call for health systems to strengthen access to quality sexual, reproductive, maternal, newborn and adolescent health, particularly for the most vulnerable. Professional midwives with enabling environments are identified as an important solution. However, a multitude of barriers prevent midwives from fully realizing their potential. Effective interventions to address known barriers and enable midwives and quality sexual, reproductive, maternal, newborn and adolescent health are less well known. This review intends to evaluate the literature on (1) introducing midwives in low- and middle-income countries, and (2) on mentoring as a facilitator to enable midwives and those in midwifery roles to improve sexual, reproductive, maternal, newborn and adolescent health service quality within health systems.
An integrative systematic literature review was conducted, guided by the Population, Intervention, Comparison, Outcome framework. Articles were reviewed for quality and relevance using the Gough weight-of-evidence framework and themes were identified. A master table categorized articles by Gough score, methodology, country of focus, topic areas, themes, classification of midwives, and mentorship model. The World Health Organization health systems building block framework was applied for data extraction and analysis.
Fifty-three articles were included: 13 were rated as high, 36 as medium, and four as low according to the Gough criteria. Studies that focused on midwives primarily highlighted human resources, governance, and service delivery while those focused on mentoring were more likely to highlight quality services, lifesaving commodities, and health information systems. Midwives whose pre-service education met global standards were found to have more efficacy. The most effective mentoring packages were comprehensive, integrated into existing systems, and involved managers.
Conclusions
Effectively changing sexual, reproductive, maternal, newborn and adolescent health systems is complex. Globally standard midwives and a comprehensive mentoring package show effectiveness in improving service quality and utilization.
Trial registration
The protocol is registered in PROSPERO (CRD42022367657).
Peer Review reports
There is an urgent global call for increased availability of quality sexual, reproductive, maternal, newborn and adolescent health (SRMNAH) [ 1 ]. Literature finds that professional midwives with enabling environments are an effective solution [ 2 , 3 , 4 ]. The global standard for a midwife is delineated by the International Confederation Midwives (ICM). Although most countries are working toward attaining this standard, wide variation in the definition of midwife within countries remains.
Professional midwives have been found to improve quality in both high- and low-resource settings. However, barriers to practice are also noted [ 5 ]. Resistance to quality improvement within health systems is one barrier that can require complex system change to address [ 6 ]. In spite of clear World Health Organization (WHO) guidance on SRMNAH, there is a perpetuation of low quality–at times harmful–care in low- and middle- income countries (LMICs) [ 5 , 6 , 7 ]. The broad sweep of LMICs was chosen to reflect the ubiquitous nature of the problem, however contextual differences between and within countries are acknowledged and warrant further study [ 7 ]. The WHO 2021 publication from the Network for Improving Quality of Care for Maternal, Newborn and Child Health (or, the Quality of Care Network) outlines five functions for quality improvement, for LMICs [ 1 ]. The first one—onsite support—has been found to be effective in addressing resistance and influencing system change. The provision of onsite support can be key in supporting enabling environments for desired changes, thus it may be needed for midwives to reach their full potential.
Facility mentorship, a type of onsite support, is an increasingly popular approach for enabling quality SRMNAH in LMICs [ 8 , 9 ]. It comprises both clinical and facility-wide interventions aimed to capacitate and create enabling environments for quality care [ 10 , 11 ]. Through advocacy, modeling, and problem solving for the needed changes, quality improvements can be achieved.
Mentorship and midwifery have been found to be synergistic as midwives need enabling environments to achieve optimum results, and midwives’ expertise increases the success of mentorship [ 2 , 10 , 12 , 13 ]. This review intends to evaluate the bodies of literature on (1) introducing midwives and (2) facility mentoring to better understand facilitators and barriers to implementation of quality, evidence-based SRMNAH care. It aims to provide insight into effective methods of integrating midwives and their related services into health systems [ 14 ]. It is hoped that further refinement of our knowledge on this topic will support program efficacy and improve quality of care for the most vulnerable women. The research question was: what is the impact of deploying midwives, and of mentoring midwives, other cadres midwifery roles, managers, and support staff, on providing SRMNAH care in LMICs?
An integrative systematic literature review was performed with a narrative synthesis approach [ 15 ]. The details of the methodology have been published previously [ 16 ]. An initial scoping found abundant literature on midwives in high-resource countries and limited literature focused on LMICs. Very few articles from LMICs had a specific focus on the introduction of ICM-standard midwives, or on mentoring to support newly introduced midwives. For the purposes of this review, the term ‘midwife’ included all skilled health workers providing SRMNAH services and was not limited to midwives meeting ICM standards. Facility mentoring was defined as regular visits to health facilities to support providers, staff, faculty, and or managers. Mentors could engage in observation, guidance, feedback, and/or data collection, all with the intention of improving the quality and availability of SRMNAH services. Supplies and equipment as well as infrastructure support were not considered mentoring. An integrative systematic review was chosen as it encouraged the inclusion of diverse articles, thus allowing for a more robust comprehensive review [ 15 , 17 ].
Inclusion and exclusion criteria
The review was guided by the Population, Intervention, Comparison, Outcome (PICO) framework [ 18 ]. Inclusion and exclusion criteria are listed in Table 1 . The review included literature from the last 13 years (Jan 2010 to May 2023) that addressed systems strengthening in LMICs through the introduction of midwives, enabling environments for midwives, mentoring, and achieving quality of care. Reviews from the past thirteen years are thought to capture current contexts and issues [ 19 ]. Only articles published in English were included.
Information sources
The review was conducted in February of 2023. The literature was searched through Medline, EMBASE, and CINAHL. In addition to the database search, internet searches of published reports and gray literature, and hand searching of relevant reference lists were performed using a snowball approach. References were managed using an EndNote citation manager.
Search strategy
The review was carried out using a priori planned searches. It was inclusive of all literature that addressed the introduction of midwives and/or the use of mentoring to improve SRMNAH in LMICs, including qualitative experiences of those involved. Predetermined key concepts were searched with specific subject headings and the related Medical Subject Headings (MeSH) or thesaurus terms, as shown in Table 2 . The search was ConceptTerms1 AND ConceptTerms2 AND ConceptTerms3. Additionally, we conducted a systematic search of relevant gray literature sources using these search terms and key concepts to include gray literature in this review. After identifying relevant gray literature documents, such as government reports, conference proceedings, and institutional repositories, that align with this research topic, we critically assess their quality and relevance to our research question, applying the PICO inclusion and exclusion criteria. Finally, we synthesized the key findings from the selected gray literature sources alongside findings from peer-reviewed literature.
Study selection
The process of screening and reviewing abstracts and full-text articles based on eligibility criteria is presented in Fig. 1 [ 20 ]. After the initial titles were screened, the authors (RA, SBZ, ANJ) screened all abstracts against the inclusion and exclusion criteria. The full texts of all abstracts were then reviewed by the authors (RA, SBZ, ANJ).
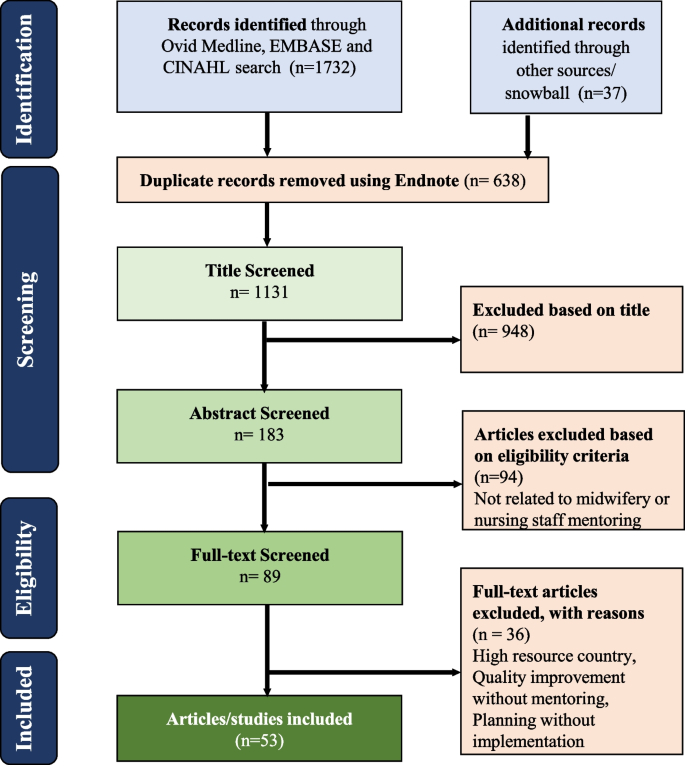
PRISMA flowchart of the literature review
Quality assessment
All selected articles were reviewed for quality and relevance. A combined, modified mixed-methods synthesis tool was used with the Gough (2007) weight-of-evidence framework [ 21 ]. The Gough tool guides quality evaluation using four themes: coherence and integrity, appropriateness for answering the question, relevance and focus, and overall assessment (Table 3 ). Using the tool, each theme was given a rating of high, medium, or low. These ratings then combine to form an overall rank. Author RA and SBZ independently reviewed and ranked the articles based on the above criteria, and results from the individual rankings were discussed. In case of discrepancies in rankings, the final decision was taken by the principal author (RA). All articles were included with recognition given their potential strengths and weaknesses.

Data analysis and presentation
As this was an integrative review, there were multiple types of research used. The articles were sorted by research types using five broad categories: 1) project intervention, 2) retrospective country analysis, 3) qualitative process description, 4) literature review, and 5) modeling study. This helped reduce risk of bias by at once evaluating a wide range of studies and distinguishing findings by their research approach.
A health systems building block framework was used to guide data extraction and analysis by the three authors (RA, SBZ and ANJ). Data from the articles were iteratively compared to identify common sub-themes relevant to the research question [ 17 ]. The sub-themes were coded and aggregated to identify emerging themes under the existing health system building blocks: national policies and administration, care quality, health-seeking behaviors, experiences and underlying motivators of staff, health outcomes, access to essential medicine, and information systems were identified (Table 4 ). Although the themes are distinct, they could also be described as steps in a process, tied to and dependent on each other. They are also aspects of the health systems building blocks.
Following theme identification, articles were categorized according to the building blocks. A master table and supplementary tables were created to classify each article according to its Gough score, country of focus, themes, building blocks and methodology. The table also categorized articles according to whether they were inclusive of midwives and or mentoring, if care providers met an international standard for midwives, and how mentoring was defined. To minimize risk of bias in the synthesis of findings, articles involving interventions (methodology type 1) were disaggregated to identify interventions most likely to be transferable. Disaggregation was based on their approaches to measuring outcomes and direction of change. Four outcomes measurement approaches were determined: 1) self-reported or before/after tested knowledge or skills; 2) observed quality improvement at clinical sites; 3) information system health outcome tracking; and 4) facility data on service utilization.
The results analysis is divided into three sections. We provide an overview of key characteristics, rankings and methodological approaches. We then present an analysis of the two main themes (a) midwives and/or both midwives and mentors and (b) mentoring, which emerged from the studies. Finally, we offer a comprehensive synthesis of the specific findings related to midwifery and mentorship according to the health system building blocks approach observed across the included studies.
Fifty-three articles were included in this review (Fig. 1 ) [ 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 ]. Tables 5 and 6 at the end of the article display all article data. Among them, 13 were ranked as high, 36 medium, and four low (Table 5 ). In addition, 18 focused on the introduction of midwives, 29 on mentoring, and six combined midwife introductions with mentoring. Ten articles described midwives meeting a global ICM standard while the others described a range of categories of staff who were called midwives or were providing maternity care. These included nurses, midwives not meeting ICM standards, midwives with unspecified education, general maternity staff (i.e., not midwives), and skilled birth attendants with unspecified education (Table 7 , also at end). Across both midwifery and mentoring articles, theme categories yielded overlap, with all articles aligning with multiple themes.
Among the articles focused on midwives and/or both midwives and mentors, seven assessed interventions, seven were retrospective country analyses, five were qualitative process descriptions, four were literature reviews, and one was a modeling study (Table 5 ). Key barriers were found across articles that limit midwives’ ability to provide quality care [ 2 , 12 , 39 , 66 , 74 ]. These included policies and work environments that relegated midwives to support roles and constrained their scope and opportunities for growth. For instance, midwives were found to have limited opportunities to attend normal births, and restrictions from managers on providing aspects of evidence-based care, including managing life threatening emergencies. In her integrative review of midwifery programs in LMICs, Schuldt (2019) noted that only one third of midwives were practicing to their full scope [ 12 ]. Despite the challenges, all midwives were providing aspects of midwifery care and many midwives were successfully expanding their roles and improving care quality [ 36 , 59 , 64 , 73 ]. Evidence-based policy and guidelines, supportive management, mentoring, and continuous professional development all enabled midwives’ performance. Practicing to their full competencies was more likely when midwives met a global standard and when facility mentoring was provided [ 59 , 60 , 64 , 73 ].
Of the articles that addressed mentoring (including mentoring of midwives), thirty evaluated mentoring interventions and five were literature reviews. Most mentors were project-based, providing support to government health facilities; some were government employees [ 23 , 36 , 40 , 44 , 45 , 61 , 62 ]. Except for one project that used international mentors, all mentors were national nurses, midwives, or doctors and all mentorship was conducted onsite [ 64 , 65 ]. Mentors largely received pre-mentoring training of up to a week, while some described only existing professional expertise. Three studies described a five week training [ 23 , 31 , 32 , 33 , 48 ]. Frequency of mentor visits and mentorship approaches varied across projects. Most mentors conducted from bi-weekly to bi-monthly visits ranging from a total of six facility visits to bi-weekly visits for over 18 months [ 27 , 43 , 48 , 52 ]. In two projects, mentors were deployed full time [ 69 , 74 ]. Most mentoring visits lasted one day and visit frequency was positively correlated with quality improvement [ 45 ]. While most mentoring focused on service delivery, three articles described mentoring as part of midwifery education to improve quality of classroom teaching and clinical teaching at practice sites [ 60 , 64 , 65 , 66 ]. Components of mentoring visits included group teaching, case studies, bedside teaching, assessing and advocating for supplies and equipment, establishing and reinforcing data systems, and providing problem solving support [ 23 , 30 , 36 , 40 , 44 , 45 , 47 , 61 , 62 ]. Checklists for mentors to guide their mentoring were mentioned in ten studies [ 49 , 50 , 51 , 58 , 69 ]. The mentoring programs that found improvements in outcomes mentored at least twice per month for at least a 3-month duration [ 49 , 51 ].
The six studies that described introducing midwives in education and practice with mentoring support found additional benefits of mentoring when introducing a new midwifery profession [ 32 , 33 , 34 , 35 , 36 , 37 ]. This was largely because of improved enabling environments. The benefits of combining mentoring with the deployment/strengthening of midwives include improved quality of care and improved service utilization. One study found statistically significant improvements in use of ANC cards and partographs over what was found with introducing midwives alone [ 60 ].
Across all 31 articles that described interventions, none achieved 100% of identified quality improvement goals. Nine articles highlighted gaps in achieving desired goals [ 37 , 38 , 41 , 43 , 46 , 47 , 69 , 70 , 71 ]. Outcomes measurement approaches with direction of change are delineated in Table 7 . Participant self-reported or researcher tested improvements in knowledge or skill, and researcher observed quality improvements were the most common approaches. Twenty-seven and 20 articles respectively showed improvements in outcomes using these approaches. Eleven articles reported improved outcomes using health facility data, eight reported increased service utilization, nine highlighted gaps in achieving desired goals, and one reported no improvement. Most intervention articles included baseline and endline observations and some were retrospective evaluations looking at sustainability. Notably, due to larger numbers of mentorship articles examining interventions, more rigorous outcomes measurement information is available on mentoring than on introducing midwives.
Across all articles, the most common building block themes were governance and leadership, and service delivery, with 31 and 28 articles aligning respectively (Table 6 ). Eleven or fewer articles aligned with access to essential medicine and supplies, data/ health information systems, finance, and health workforce. Studies examined 23 countries: Afghanistan, Bangladesh, Benin, Botswana, Burkina Faso, Cambodia, Ethiopia, India, Indonesia, Jordan, Kenya, Laos, Morocco, Malawi, Nepal, Pakistan, Peru, Rwanda, South Africa, Sri Lanka, Tanzania, Uganda and Zambia (Table 8 ) [ 33 , 37 , 39 , 40 , 41 , 43 , 44 , 47 , 52 , 58 , 62 , 64 , 65 , 69 , 70 , 71 , 73 , 74 , 75 ]. The following sections discuss the findings in further detail according to the health system building blocks, with midwifery and mentorship specific findings presented separately within each section.
Leadership and governance
The 33 articles that touched on leadership and governance discussed strengths and gaps. They aligned neatly with both the leadership and governance building block and the theme national policies and administration drawn from the review. Thirteen articles looked at the introduction of midwifery, and 18 looked at mentorship interventions. Another two looked at mentorship supporting midwives. Eight were rated high, 22 medium, and three low. The types of articles that addressed leadership and governance included intervention/ program interventions (17), retrospective country analysis (05), qualitative process review (05) and six literature reviews. Most articles on mentoring focused on local-level service delivery governance, including of managerial staff, and systems for overseeing implementation. Midwifery articles more commonly looked at national policies and guidelines. The articles broadly point to evidence-based leadership and governance that reflects ground realities being essential for midwives to practice to their full competencies. Workplace settings that are unsupportive to midwifery, a ground reality, significantly detracted from full scope midwifery and service quality, while supportive workplace settings fostered full scope practice and quality sexual, reproductive, maternal, newborn and adolescent health (SRMNAH) services. Supportive workplace settings typically involved manager engagement through various modes.
Strong leadership and clear global recommendations have helped shape national policies on midwifery and SRMNAH quality improvement [ 1 , 9 , 14 , 24 , 42 , 76 , 77 ] [ 1 , 54 , 61 ]. Global and national standards for midwives have brought stakeholders together and are an impetus to support midwifery in spite of competing interests [ 59 ]. Political will and multi-stakeholder collaboration were found essential for a quality midwifery profession [ 61 ]. Good governance of logistics and infrastructure were also identified as essential, though gaps were highlighted in adequate space for care provision, privacy for respectful care, and commodity availability [ 54 , 56 ]. Gaps in midwifery leadership were also noted. Lack of leadership by midwives of the midwifery profession may contribute to reduced political will for midwifery care. Country experience shows that professions other than midwives that are positioned as leaders of the midwifery profession sometimes do not fully understand midwives’ expertise and may compete with midwives for maternity care provision roles [ 12 ].
Policies that scale up education and deploy midwives closer to communities were found to have a positive impact on service utilization and health outcomes [ 68 ]. However, gaps in both of these policy areas were also noted. First, adherence to globally recommended midwifery competencies in education programs is often not abided by in countries [ 54 , 66 , 72 ]. Second, World Health Organization (WHO) workforce guidelines define the number of needed health care workers per population, but not the number of midwives needed [ 14 ]. Other gaps related to deployment policy were also identified. For instance, unsupportive workplaces resulted in constraints to optimal midwifery performance in studies in both Pakistan and Bangladesh [ 11 , 28 , 74 ]. In these contexts, midwives either did not perform their duties, or they operated under policies that restricted them from doing so. Governance that did not take into account the inputs needed to create an environment conducive to midwifery within workplace settings was associated with lesser success. One mentoring program that reported no improvement identified restrictive national policies as a barrier [ 28 ]. Across articles, few midwives reported supportive workplace settings, and some reported humiliation, including by their direct managers [ 12 , 39 , 65 , 72 ]. When managers were not fully involved, resistance to midwives in leadership roles, autonomous practice, and quality improvements in clinical care was found [ 60 , 74 , 78 ].
Conversely, local governance supporting midwife-friendly workplace settings improved midwives’ sense of competence and care quality. Webster et al. (2013) and Schuldt et al. (2020) found that midwives felt competent to provide midwife-led care in supportive workplace settings [ 29 , 59 ]. Importantly, involving onsite managers to strengthen ownership of midwifery and quality SRMNAH was identified as a priority in twenty-five articles utilizing a range of methods to measure outcomes [ 30 , 36 , 60 , 74 , 78 , 79 ]. Furthermore, support from managers for midwifery care and improved quality was better when on-site mentoring was present [ 30 , 36 , 60 ]. Seven articles found that initiating the well-known WHO quality improvement process, with a focus on SRMNAH, was an effective and easily accepted method of mentoring managers [ 30 , 36 , 49 , 52 , 58 , 60 , 69 , 79 ]. Taneja et al. (2021) describe initial handholding support and coaching for managers as part of the quality improvement process for SRMNAH in India [ 79 ].
Service delivery
Nearly all selected articles—47—addressed service delivery. Of these, 12 included the introduction of midwives, 29 included mentoring, and six included both (Table 7 ). The themes of care quality , service utilization and health outcomes mapped to the service delivery building block, with 39 articles addressing care quality. Due to their large number, articles addressing service delivery are discussed by theme. Of the service delivery articles, 31 were intervention evaluation, six reported retrospectively on the impact of national programs with a midwifery component (i.e., retrospective country analysis), two were qualitative process reviews, and eight were literature reviews.
Care quality
Among the 39 articles that had a focus on care quality, nine ranked high, 28 medium, and two low. Four included the introduction of midwives, 29 included mentoring, and six included both the introduction of midwives and also mentoring. Gaps in quality education and services were noted in most articles and both introducing ICM-standard midwives as well as mentoring enabled improvements [ 29 , 30 , 34 , 38 , 42 , 60 , 64 ].
Studies on introducing midwives reported that ICM-standard midwives improved service quality as defined by WHO maternity care guidelines. Improvements were seen in tertiary medical centers, sub-district hospitals, and non-governmental organization (NGO) supported facilities, as well as in clinical education for nurse, doctor and midwife students [ 60 , 64 , 74 , 78 ]. Analysis using logistic regression found that midwives significantly increased the number of women laboring in upright positions, delayed cord clamping, and immediate skin to skin contact after the birth [ 60 , 64 ].
The large number of mentorship focused studies found that mentorship contributed to quality improvements in midwifery education, comprehensive and respectful SRMNAH services, and emergency obstetric and neonatal care. Studies found gains made in quality education in both classroom and clinical teaching [ 60 , 61 , 65 , 66 ]. Midwifery educators identified that online mentoring helped them improve curriculum implementation [ 65 ]. Onsite mentoring improved teaching pedagogy, students' access to labs and libraries, and clinical teaching [ 64 ]. In addition, quality of care provided at clinical education sites improved after mentoring [ 60 , 61 , 64 ].
Comprehensive and respectful SRMNAH care quality showed improvements with mentoring in studies Afghanistan, Bangladesh, Rwanda, India, Nepal, Jordan, Botswana, Ethiopia, South Africa, Kenya, and Uganda [ 23 , 44 , 47 , 52 , 58 , 62 , 65 , 69 , 70 , 71 ]. An analysis of program data by Save the Children and UNFPA (2021) from 47 mentored health facilities with newly deployed midwives in Bangladesh, found improved respectful communication, partograph use, upright position for birth, and companionship as well as a notable increase in health facilities receiving obstetric emergencies coming from the community [ 64 ]. Using observation data, Anderson’s et al. (2022) mixed methods observational study found that midwives in Bangladesh without mentoring made quality improvements, but, with the addition of mentoring, use of ANC cards and partograph increased significantly [ 60 , 64 ].
Mentoring also contributed to better identification of high-risk pregnancies, improved diagnosis and treatment of STIs, better sterilization and cleanliness practices, and strengthened laboratory capacity to manage pregnancy and newborn-related emergencies in Rwanda [ 31 , 38 ]. Research in India, South Africa, Uganda, and Rwanda found that mentoring contributed to stronger newborn care services [ 23 , 30 , 38 , 39 ]. Despite the many documented benefits of mentoring, there is also evidence of care quality gaps remaining in programs that received mentorship. For example, Tiruneh et al. (2018) found improvements in newborn care in a study in Ethiopia, with the exception of newborn resuscitation [ 38 ] and Tripathi (2019) found little improvement in post-partum care and newborn resuscitation in India [ 35 ].
Service availability and utilization/ health seeking behaviors
Sixteen articles touched on service availability and/or utilization [ 22 , 24 , 34 , 38 , 42 , 50 , 64 , 73 , 74 ]. Three were ranked high, 11 medium, and two low. Eight were related to introducing midwifery, five assessed mentoring interventions, and three looked at mentors who supported mentors. For the most part, the introduction of midwives was associated with increased SRMNAH service availability and utilization. In a Lancet article, Van Lerberghe et al. (2014) found increased facility births with multi-pronged interventions that included educating and deploying midwives [ 24 ]. Vieira et al. (2012) and Speakman et al. (2014) found greater uptake of ANC and skilled birth attendance in studies in Indonesia and Afghanistan [ 26 , 27 ]. Tasnim et al. (2011) found increased ANC, facility birth, and postnatal care (PNC) following the introduction of ICM-standard midwives in Bangladesh [ 22 ]. Another study of ICM-standard midwives in Bangladesh found increases of 27%, 13% and 12% for ANC, facility birth, and PNC respectively [ 22 , 64 ]. However, other Bangladesh research looking at ICM-standard midwives using a different sample of hospitals found no difference in facility births nine months after a national deployment of ICM-standard midwives [ 60 ]. Studies that found gaps in enabling policies and/or workplace settings for midwives showed fewer increased in service utilization [ 28 , 50 ].
As discussed in the earlier sections, studies on mentorship interventions showed a consistent association between engaging managers in supportive workplace settings and care quality. Related to this, mentorship also influenced service availability and utilization. Two studies led by Anderson et al. (2022) and one led by Save the Children and UNFPA (2021) documented greater availability of cervical cancer screening, postpartum family planning, gender-based violence screening, and post abortion care with mentors supporting new midwives [ 60 , 64 , 74 ]. In research from Ethiopia, Uganda, and India, ANC and facility birth rates in their studies in Ethiopia, Uganda, and India in which mentors supported midwives. Tiruneh et al. (2018) found higher rates of care seeking for obstetric emergencies as service availability improved [ 38 ]. Namazzi et al. (2015) and Waiswa et al. (2021) found an increase of more than 20% in sick newborn care visits in Uganda [ 30 , 56 ]. Stephens et al.’s (2019) study saw a more than doubling of PAC service use including associated family after a mentoring intervention focused on service quality in Tanzania [ 50 ].
Health outcomes
Twelve articles reported health outcomes. Three ranked high, seven medium, and two low. Seven included the introduction of midwives and five had a mentoring intervention. Program interventions that were associated with improved health outcomes were thought to be the most likely to be transferable and thus were analyzed more closely to identify research methodology as well as intervention components. Ultimately, the goal of health care is to improve outcomes, and selected studies found improvements in health outcomes associated with midwife deployment [ 25 , 28 , 42 ].
Seven midwifery articles described improved outcomes with the introduction of midwives [ 24 , 25 , 26 , 27 , 29 , 43 ]. All were large national interventions that included many components in addition to midwives, making it difficult to ascribe attribution [ 24 , 26 , 43 , 49 ]. One was a multi-country study evaluating the introduction of skilled birth attendants (SBAs). It had mixed results but did find decreased neonatal morbidity in Latin America, the Caribbean and partially for Asia [ 25 ]. Vieira et al. (2012), Webster et al. (2013), The World Bank (2013), and Speakman et al. (2014) found significant reductions in maternal mortality in retrospective national analyses of national midwife deployments in five countries [ 26 , 27 , 29 , 42 ]. However, analyses of similar programs in India and Pakistan did not reduce maternal mortality [ 28 ]. The studies of projects in Indonesia and Bangladesh found that, when midwives were deployed, deaths from obstetric complications, particularly abortion, sepsis, and postpartum hemorrhage, fell over control groups of facilities that did not deploy midwives but rather used doctors and nurses in midwifery roles [ 22 , 60 , 64 , 74 ]. Bartlet et al.’s (2014) LIST modeling exercise estimated that under even a modest scale-up, midwifery services including family planning would reduce maternal, fetal, and neonatal deaths by 34% [ 67 ].
Neonatal outcomes were inconsistent in a systematic review assessing the protective effect of SBAs on neonatal mortality in nine LMICs [ 25 ]. Where SBAs were protective in Latin America, the protection was partial in Asia, and not at all in Africa. An article from Nigeria found that SBA rate was not associated with better neonatal outcomes. Meanwhile, Viera et al. (2012) found a reduction in under 5 mortality in Brazil [ 26 ].
Four of the five mentoring articles reported improved health outcomes. All were mentoring ICM-standard nurse-midwives or midwives [ 52 , 56 , 57 , 69 ]. In addition, all had comprehensive facility mentoring programs that visited at least twice monthly for at least three months, included managers, and strengthened data collection systems. Three were inclusive of training, two with simulation, and three provided medicine and equipment. However, certain outcomes did not improve. One study from Uganda notes declining MMR in project districts[ 56 ]. Studies from Uganda, Rwanda, and South Africa identify declining trends for stillbirths and or neonatal deaths[ 30 , 45 ]. In Uganda neonatal death was reduced from 30.1 to 19.6 deaths/1,000 live births. In addition, declines in neonatal morbidity including, asphyxia were found in Kenya, Uganda, and South Africa [ 57 ].
Health workforce
Like care quality, studies that addressed workforce comprised a relatively even split between focusing on introducing midwives and implementing mentorship programs. Seven examined midwife introduction and five mentorship; one addressed midwifery combined with mentorship. They were largely good quality with six and five rated as high and medium respectively. Two were given a low rating. The theme experiences of midwives and their support staff most aligned with the health workforce building block and is discussed in this section. [ 28 , 29 , 30 , 60 , 66 ]. Research quality varied and it was not always possible to discern whether attitudes were presumed or directly expressed.
Reports on midwives and other maternity staff and managers highlighted both positive and negative experiences. Some articles talked about midwives’ dissatisfaction with their workplace or feasibility to implement what was expected of them. Three studies reported midwives’ discomfort with their deployment status and the impact of those discomforts on their performance. Speakman et al. (2014) found that midwives in Afghanistan were less willing to work in military-controlled areas, stating fears about security and resistance from family [ 27 ]. Mumtaz et al. (2015) reported that newly deployed midwives in Pakistan stated difficulty in setting up private midwifery practices within rural communities, as distances made traveling prohibitive, particularly at night [ 28 ]. One study published in the Canadian Medical Association noted midwives' preference for positions with higher pay and not always choosing to serve the poorest [ 29 ].
Anderson et al.’s (2022) study found that midwives expressed un-elicited pride regarding their profession, particularly where midwives were enabled through mentoring. In this and other studies, midwives expressed a desire for professional autonomy, respect, and for midwifery to be a distinct profession [ 27 , 60 , 65 ]. In two of these studies, newly deployed ICM-standard midwives in Bangladesh expressed confidence and competence to provide quality SRMNAH services, while also expressing frustration with imposed limitations by managers and other maternity staff. Anderson et al. (2022) also found that some managers and nurses felt that midwives did not have the competence to practice autonomously or manage emergencies. Managers expressed those nurses’ felt competition with midwives and that this competition led to nurses questioning midwives’ competence.
Many articles on mentoring shared providers’, faculty’s, mentors’, and administrators’ appreciation of and knowledge gained from mentoring [ 52 , 56 , 57 , 69 ]. Mentees in the studies in Bangladesh, Uganda, and Karnataka expressed having increased confidence and feeling happy with the mentorship and what they had learned [ 30 , 60 , 66 ]. Studies in India and Bangladesh observed that mentoring contributed to better teamwork among maternity staff [ 60 ]. In Laos, a mentorship program designed for newly deployed inexperienced midwives was found to be well-received by hospital administrators [ 31 , 40 ]. Overall, mentoring led to positive experiences for maternity staff and maternity staff and managers were more appreciative of midwives when there was mentoring [ 60 ].
Access to essential medicine and supplies
While it was not one of the initial themes identified, eleven articles mentioned improving essential medicines [ 23 , 31 , 32 , 33 , 39 , 44 , 45 , 49 , 52 , 64 , 68 ]. All examined mentoring and two discussed program interventions that introduced midwives with mentorship. Four were rated high and seven medium. Anderson et al. (2022) and Save the Children and UNFPA (2021) addressed the impact of introducing midwives on medicine availability in their studies in Bangladesh [ 60 , 64 ]. In both of these articles, midwives alone did not make an impact on medicine availability. However, with mentoring, medicines became more available [ 60 , 64 ]. In an example from Anderson et al.’s (2022) observational study, oxytocin and MgSo4 availability was as low as 13% in facilities without midwives or mentorship, and as high as 81% in facilities with midwives and mentors [ 60 ]. Articles on mentoring interventions in India, South Africa, Rwanda and Uganda also reported a positive impact of mentoring on availability of essential medicines [ 23 , 30 , 31 , 39 , 44 , 45 , 49 , 52 , 64 ]. Improvements may be a result of capacitating health workers and supply chain staff to activate supply chain systems. They may also be the result of improved confidence of health care providers and managers to provide the needed care and thus ensure supplies.
Data systems
Ten articles reported on data or health information systems, also not an initial theme [ 23 , 30 , 31 , 32 , 36 , 37 , 39 , 51 , 56 , 58 , 69 ]. All ten looked at mentoring and reported strengthening data systems to track SRMNAH services. Articles emphasized the importance of using data to track implementation, such as a detailed clinical record which is sometimes called a case sheet [ 23 , 31 , 32 , 36 , 37 , 56 ]. Namazzi et al. (2015) describes assessing the status of the patient charts and registers at baseline and then having the MOH approve file folders for inpatients to standardize record-keeping and to facilitate data availability [ 30 ]. The introduction of individual client records allows for more detailed monitoring of patient care. Synergizing SRMNAH with existing quality improvement systems included increased emphasis on and of utilization of SRMNAH data for program monitoring [ 36 ]. Taneja from India describes involving government stakeholders to build on existing data systems to ensure data-based decision making within SRMNAH [ 79 ].
Health financing
Eight articles included a focus on health financing, which overlapped with the theme national policies and administration [ 23 , 24 , 26 , 27 , 28 , 29 , 43 , 68 ], Five related to midwifery and three included mentoring. Cost effective programs are essential in low-resource settings as even if projects are effective, sustainability is dependent on resources [ 56 ]. This review found that programs to introduce midwives and those supporting mentorship can be accomplished with minimal expenditure [ 23 , 31 ]. Midwifery models were noted to be significantly less costly then obstetrician led models for care [ 67 ]. Bartlett et al. (2014) found that midwifery models were almost twice as cost-effective as obstetric models ($2,200 versus $4,200 per death averted). The introduction of midwives as well as mentoring can also be implemented within existing government systems using government employees and thus add very little additional cost. However, mentoring projects using government staff sometimes encountered constraints on availability of mentors’ time. Yet, one of the most effective mentoring projects that impacted health was implemented through existing government staff [ 10 ]. Even if project mentors are used, research from India found mentoring only increased cost by $5.60 per pregnant woman, or around $460,000 annually for eight districts, making it a cost effective intervention [ 23 ].
This review underscores the significance of adhering to a global midwife definition and emphasizes the importance of onsite support in creating enabling environments. The health systems building blocks served as an effective framework for interpreting the results through the lenses of its various pillars. It is worth noting that the articles focusing on midwifery, as opposed to mentorship, had fewer intervention studies and more retrospective national and qualitative process research. This research gap limits our understanding of the effective steps required for implementation of successful midwifery programs, as has been mentioned in earlier literature [ 5 ]. Among the themes explored in the midwifery literature, governance and leadership emerged as a critical first step. However, there is a pressing need for implementation research that delves into the process and impact of introducing midwives in LMICs. Drawing insights from the literature on mentoring and quality improvement holds potential for guiding countries in devising effective midwife deployment strategies [ 42 ].
One notable gap identified in this review pertains to midwife leadership [ 59 ]. The significance of midwives leading the midwifery profession has been highlighted in other literature as well [ 80 ]. Competition between professions involved in maternal health—midwifery, medicine, and nursing—for leadership roles is recognized as a hindrance to midwives fully realizing their potential. Concerns associated with non-midwives leading midwives include potential conflicting self-interest and gaps in understanding. Midwives possess unique expertise in providing quality routine SRMNAH care to essentially healthy women and newborns. If midwives are not self-governing, their distinctive vision may not be fully implemented. Therefore, more research is needed to identify best practices for promoting midwives into leadership positions.
Although the majority of articles included in this review did not explicitly address the importance of globally standard midwives, those that did emphasized its priority. The literature on skilled birth attendants emphasizes the significance of expert maternity care providers and reiterates the components of globally standard midwives. However, gaps persist in countries' adherence to global recommendations [ 77 , 81 ]. Additionally, the scope of practice for midwives includes comprehensive sexual and reproductive health, as called for in the sustainable development goals. However, many non-standard midwives lack this expertise. Articles reporting changes in health outcomes consistently involved globally standard midwives, while those reporting no change often featured non-standard providers lacking basic knowledge. Further research is required to examine the impact and decision-making processes regarding the perpetuation of non-standard midwives within countries.
While all midwives provide aspects of midwifery care, this review identified significant gaps in their ability to perform to their full competencies. These gaps inevitably limit the contributions midwives can make. Enabling midwives to practice fully is particularly urgent in managing life-saving emergencies and is critical for ensuring quality respectful maternity care and comprehensive sexual and reproductive health. Frustrations regarding practice restrictions were expressed by professional midwives in this review, highlighting the importance of evidence-based leadership led by midwives themselves.
Essential medicines play a critical role in enabling environments for midwives. Notably, the findings indicate that midwives without mentoring did not impact the availability of medicine supplies. Weak supply chains are prevalent in LMICs, and stockouts of essential commodities pose significant barriers to delivering quality services. This underscores the essential role of mentoring or other forms of effective supportive supervision, particularly in this area [ 82 ]. The review suggests that mentoring involving managers and staff may help improve the availability of life-saving SRMNAH services. Further research is needed to identify the most effective methods for ensuring the availability of essential supplies and medicines through mentoring interventions.
The importance of data collection highlighted in the mentoring articles cannot be overstated. Midwives require effective monitoring of their performance to identify gaps and solve problems [ 83 ]. However, many countries still do not routinely use patient files, and the use of register books for storing patient information needed for macro data systems was noted. This review emphasizes the importance of effective gathering and utilization of information to ensure quality care and support at the micro-level. By highlighting gaps and facilitating feedback for improving care delivery, quality data at the micro-level is crucial.
The review found that evidence-based leadership and governance reflecting ground realities are essential. The 2018 WHO definition of Skilled Birth Attendant Standards emphasizes the importance of enabling environments [ 77 ]. The International Confederation of Midwives (ICM) defines an enabling environment for midwives as one that supports the necessary infrastructure, profession, and system-level integration for effective work performance [ 84 ]. Facility mentoring emerged as a critical factor in strengthening enabling environments and improving implementation quality [ 1 , 53 , 54 ]. Mentoring programs improve relationships between health system components and between staff and managers involved in care provision, aligning with the literature on addressing complex systems. Onsite facility mentoring, with frequent visits and involvement of all local authorities, integrated into all components of the related health system, proved to be the most effective approach. Further research is needed to determine best practices for mentoring approaches to inform program planners and policies that support workplace setting conducive to midwifery.
The facility mentoring findings in this review align closely with the WHO Quality Maternal Health Network guidelines, which emphasize on-site support, learning and sharing, measurement, community and stakeholder engagement, and program management as the key components for effective quality improvement in maternal health [ 76 ]. While WHO acknowledges the importance of management at the macro-level, this review highlights the criticality of on-site support for managers in facilitating sustainable change [ 85 ]. WHO may want to consider expanding its recommendations for managers to include micro-level support. The interventions evaluated in this review were further disaggregated by measures of success to deepen our understanding of known efficacy. Only a limited number of interventions assessed in-vivo changes in implementation. Self-reported changes or changes based on knowledge and skill were found to have limitations in effectively indicating implementation change, which reinforces the importance of on-site interventions [ 59 , 60 , 74 , 76 ]. Mentoring programs should consider incorporating methods that evaluate observed implementation changes.
Mentoring programs that demonstrated positive outcomes consisted of comprehensive packages including frequent visits, capacity building, manager involvement, and strengthening of data systems. These programs consistently mentored globally standard midwives. The high-performing programs prioritized on-site capacity building activities such as group teaching, case studies, bedside teaching, assessing and advocating for supplies and equipment, establishing and reinforcing data systems, and support for problem-solving. The use of checklists for mentors was also commonly observed in many studies (Fig. 2 ) [ 49 , 50 , 51 ].

Components of mentoring that drive outcomes
Several limitations of this review were identified. Firstly, the included studies exhibited diversity in their approaches, delivery methods, and outcomes, resulting in considerable heterogeneity. This heterogeneity is expected, given the inclusion of studies from different countries, diverse populations, and various public health interventions, but may lead to less accurate comparisons than a more homogeneous study. Secondly, the reliance on self-reporting of outcomes as the primary outcome method of measurement may introduce some bias, either through over- or under-reporting. Third, more nuance in terms of the most effective mentorship interventions would have given more insight, specifically the efficacy of internal versus external mentorship, but although the literature did find that frequency of mentoring contacts improved outcomes, more research is needed for more specific programmatic guidance. Finally, this review might be limited by the fact that we have employed a broad categorization for 'LMIC,' which leaves gaps in understanding specific country or region contexts.
This review highlights the importance of adhering to a global midwife definition and the role of onsite support in creating enabling environments. It identifies gaps in midwife leadership and emphasizes the need for more research to promote midwives into leadership positions. The review also underscores the significance of globally standard midwives and the challenges associated with non-standard midwives. Enabling midwives to practice to their full competencies is crucial for quality care provision leading to life saving and rights upholding, and access to essential medicine plays a critical role in creating supportive environments. Effective data collection and monitoring, as well as evidence-based leadership and governance, are essential for improving midwifery care. Onsite facility mentoring emerges as a critical component of strengthening enabling environments, and more research is needed to identify best practices for mentoring approaches.
Girls’ and women’s lives, and dignity depend on the availability of quality SRMNAH. To succeed in making the needed changes we need enabled, expert midwives. Midwifery literature has focused on the needed national governance and broad country understandings. There remains a need for follow up to ensure globally standard midwives are available for all girls and women. There is also a need for policy makers to include support for successful implementation. Current knowledge of health systems strengthening, and quality improvement, sheds light on the needed planning for midwives to ensure realization of their full potential. Mentoring is cost effective, and can be implemented within existing government systems. A comprehensive mentoring package inclusive of onsite capacity building of maternity staff, managers, data and procurement systems, will enable midwives to improve SRMNAH, and uphold rights for the most vulnerable.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to publication restrictions from journals but are available from the corresponding author on reasonable request.
Abbreviations
Sexual, reproductive, maternal, newborn and adolescent health
Low- and middle-income country
Quality improvement
International Confederation of Midwives
Skilled birth attendants
World Health Organization
World Health Organization. The Network for Improving Quality of Care for Maternal, Newborn and Child Health (Quality of Care Network). 2023. Available from: https://www.who.int/groups/Quality-of-care-network#:~:text=of%20Care%20Network . Accessed 1 Mar 2023.
Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet. 2014;384:1129–45.
PubMed Google Scholar
Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models of care compared with other models of care for women during pregnancy, birth and early parenting. Cochrane Database Syst Rev. 2016;4:CD004667.
Turkmani S, Currie S, Mungia J, Assefi N, Rahmanzai AJ, Azfar P, et al. ‘Midwives are the backbone of our health system’: lessons from Afghanistan to guide expansion of midwifery in challenging settings. Midwifery. 2013;29:1166–72.
Filby A, McConville F, Portela A. What prevents quality midwifery care? A systematic mapping of barriers in low and middle income countries from the provider perspective. PloS One. 2016;11:e0153391.
PubMed PubMed Central Google Scholar
Alenchery AJ, Thoppil J, Britto CD, de Onis JV, Fernandez L, Suman Rao P. Barriers and enablers to skin-to-skin contact at birth in healthy neonates-a qualitative study. BMC Pediatrics. 2018;18:1–10.
Google Scholar
Lencucha R, Neupane S. The use, misuse and overuse of the ‘low-income and middle-income countries’ category. BMJ Glob Health. 2022;7(6):e009067.
Starrs AM, Ezeh AC, Barker G, Basu A, Bertrand JT, Blum R, et al. Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher-Lancet Commission. Lancet. 2018;391:2642–92.
World Health Organization. Global strategic directions for nursing and midwifery 2021-2025 2021. Available from: https://apps.who.int/iris/bitstream/handle/10665/344562/9789240033863-eng.pdf . Accessed 2 Mar 2023.
Feyissa GT, Balabanova D, Woldie M. How effective are mentoring programs for improving health worker competence and institutional performance in Africa? A systematic review of quantitative evidence. J Multidiscip Healthc. 2019;12:989–1005.
Anderson R, Zaman SB. Improving the quality of maternity care through the introduction of professional midwives and mentoring in selected sub-district hospitals in bangladesh: a mixed method study protocol. Methods Protoc. 2022;5:84.
Glickman ME, Rao SR, Schultz MR. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol. 2014;67:850–7.
Chaturvedi S, Upadhyay S, De Costa A. Competence of birth attendants at providing emergency obstetric care under India’s JSY conditional cash transfer program for institutional delivery: an assessment using case vignettes in Madhya Pradesh province. BMC Pregnancy Childbirth. 2014;14:1–11.
UNFPA, World Health Organization & International Confederation of Midwives. The State of the World's Midwifery: A Universal Pathway. A Woman’s Right to Health 2014. Available from: https://www.unfpa.org/sites/default/files/pub-pdf/EN_SoWMy2014_complete.pdf . Accessed 2 Mar 2023.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health info Libr J. 2009;26:91–108.
Anderson R, Zaman SB, Limmer M. The impact of introducing midwives and also mentoring on the quality of sexual, reproductive, maternal, newborn, and adolescent health services in low- and middle-income Countries: an integrative review protocol. Methods Protoc. 2023;6:48.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52:546–53.
Eldawlatly A, Alshehri H, Alqahtani A, Ahmad A, Al-Dammas F, Marzouk A. Appearance of Population, Intervention, Comparison, and Outcome as research question in the title of articles of three different anesthesia journals: a pilot study. Saudi J Anaesth. 2018;12:283.
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. JBI Evid Implement. 2015;13:132–40.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89:873–80.
Gough D. Weight of evidence: a framework for the appraisal of the quality and relevance of evidence. Res Pap Educ. 2007;22:213–28.
Tasnim S, Rahman A, Rahman F, Kabir N, Islam F, Chowdhury S, et al. Implementing skilled midwifery services in Dhaka city urban area: Experience from community based safe motherhood project, Bangladesh. J Bangladesh Coll Phys Surg. 2011;29:10–5.
Jayanna K, Bradley J, Mony P, Cunningham T, Washington M, Bhat S, et al. Effectiveness of onsite nurse mentoring in improving quality of institutional births in the primary health centres of high priority districts of Karnataka, South India: a cluster randomized trial. PloS One. 2016;11:e0161957.
Van Lerberghe W, Matthews Z, Achadi E, Ancona C, Campbell J, Channon A, et al. Country experience with strengthening of health systems and deployment of midwives in countries with high maternal mortality. Lancet. 2014;384:1215–25.
Singh K, Brodish P, Suchindran C. A regional multilevel analysis: can skilled birth attendants uniformly decrease neonatal mortality? Matern Child Health J. 2014;18:242–9.
Vieira C, Portela A, Miller T, Coast E, Leone T, Marston C. Increasing the use of skilled health personnel where traditional birth attendants were providers of childbirth care: a systematic review. PloS One. 2012;7:e47946.
PubMed PubMed Central CAS Google Scholar
Speakman EM, Shafi A, Sondorp E, Atta N, Howard N. Development of the community midwifery education initiative and its influence on women’s health and empowerment in Afghanistan: a case study. BMC Womens Health. 2014;14:1–12.
Mumtaz Z, Levay A, Bhatti A, Salway S. Good on paper: the gap between programme theory and real-world context in Pakistan’s Community Midwife programme. BJOG. 2015;122:249–58.
PubMed CAS Google Scholar
Webster PC. Indonesia: the midwife and maternal mortality miasma. Can Med Assoc. 2013;185(2):E95-6.
Namazzi G, Waiswa P, Nakakeeto M, Nakibuuka VK, Namutamba S, Najjemba M, et al. Strengthening health facilities for maternal and newborn care: experiences from rural eastern Uganda. Glob Health Action. 2015;8:24271.
Fischer EA, Jayana K, Cunningham T, Washington M, Mony P, Bradley J, et al. Nurse mentors to advance quality improvement in primary health centers: lessons from a pilot program in Northern Karnataka India. Glob Health Sci Pract. 2015;3:660–75.
Bradley J, Jayanna K, Shaw S, Cunningham T, Fischer E, Mony P, et al. Improving the knowledge of labour and delivery nurses in India: a randomized controlled trial of mentoring and case sheets in primary care centres. BMC Health Serv Res. 2017;17:1–8.
CAS Google Scholar
Potty RS, Sinha A, Sethumadhavan R, Isac S, Washington R. Incidence, prevalence and associated factors of mother-to-child transmission of HIV, among children exposed to maternal HIV, in Belgaum district, Karnataka India. BMC Public Health. 2019;19:1–10.
Schwerdtle P, Morphet J, Hall H. A scoping review of mentorship of health personnel to improve the quality of health care in low and middle-income countries. Glob Health. 2017;13:1–8.
Tripathi S, Srivastava A, Memon P, Nair TS, Bhamare P, Singh D, et al. Quality of maternity care provided by private sector healthcare facilities in three states of India: a situational analysis. BMC Health Serv Res. 2019;19:1–9.
Manzi A, Nyirazinyoye L, Ntaganira J, Magge H, Bigirimana E, Mukanzabikeshimana L, et al. Beyond coverage: improving the quality of antenatal care delivery through integrated mentorship and quality improvement at health centers in rural Rwanda. BMC Health Serv Res. 2018;18:1–8.
Manzi A, Munyaneza F, Mujawase F, Banamwana L, Sayinzoga F, Thomson DR, et al. Assessing predictors of delayed antenatal care visits in Rwanda: a secondary analysis of Rwanda demographic and health survey 2010. BMC Pregnancy and Childbirth. 2014;14:1–8.
Tiruneh GT, Karim AM, Avan BI, Zemichael NF, Wereta TG, Wickremasinghe D, et al. The effect of implementation strength of basic emergency obstetric and newborn care (BEmONC) on facility deliveries and the met need for BEmONC at the primary health care level in Ethiopia. BMC Pregnancy Childbirth. 2018;18:1–11.
Horwood C, Haskins L, Phakathi S, McKerrow N. A health systems strengthening intervention to improve quality of care for sick and small newborn infants: results from an evaluation in district hospitals in KwaZulu-Natal South Africa. BMC Pediatr. 2019;19:1–12.
Catton HN. Developing a mentorship program in Laos. Front Public Health. 2017;5:145.
Thapa K, Dhital R, Karki YB, Rajbhandari S, Amatya S, Pande S, et al. Institutionalizing postpartum family planning and postpartum intrauterine device services in Nepal: role of training and mentorship. Int J Gynecol Obstet. 2018;143:43–8.
World Bank. Delivering the millennium development goals to reduce maternal and child mortality: a systematic review of impact evaluation evidence. 2013.
Haththotuwa R, Senanayake L, Senarath U, Attygalle D. Models of care that have reduced maternal mortality and morbidity in Sri Lanka. Int J Gynecol Obstet. 2012;119:S45–9.
Taneja G, Sarin E, Bajpayee D, Chaudhuri S, Verma G, Parashar R, et al. Care around birth approach: a training, mentoring, and quality improvement model to optimize intrapartum and immediate postpartum quality of care in India. Glob Health Sci Pract. 2021;9:590–610.
Barnhart DA, Spiegelman D, Zigler CM, Kara N, Delaney MM, Kalita T, et al. Coaching intensity, adherence to essential birth practices, and health outcomes in the BetterBirth Trial in Uttar Pradesh India. Glob Health Sci Pract. 2020;8:38–54.
Geldsetzer P, Mboggo E, Larson E, Lema IA, Magesa L, Machumi L, et al. Community health workers to improve uptake of maternal healthcare services: a cluster-randomized pragmatic trial in Dar es Salaam Tanzania. PLoS Med. 2019;16:e1002768.
Ngabonzima A, Kenyon C, Hategeka C, Utuza AJ, Banguti PR, Luginaah I, et al. Developing and implementing a novel mentorship model (4+ 1) for maternal, newborn and child health in Rwanda. BMC Health Serv Res. 2020;20:1–11.
Ngabonzima A, Kenyon C, Kpienbaareh D, Luginaah I, Mukunde G, Hategeka C, et al. Developing and implementing a model of equitable distribution of mentorship in districts with spatial inequities and maldistribution of human resources for maternal and newborn care in Rwanda. BMC Health Serv Res. 2021;21:1–12.
Haskins L, Chiliza J, Barker P, Connolly C, Phakathi S, Feeley A, et al. Evaluation of the effectiveness of a quality improvement intervention to support integration of maternal, child and HIV care in primary health care facilities in South Africa. BMC Public Health. 2020;20:1–12.
Stephens B, Mwandalima IJ, Samma A, Lyatuu J, Mimno K, Komwihangiro J. Reducing barriers to postabortion contraception: the role of expanding coverage of postabortion care in Dar es Salaam Tanzania. Glob Health Sci Pract. 2019;7:S258–70.
Marx Delaney M, Kalita T, Hawrusik B, Neal B, Miller K, Ketchum R, et al. Modification of oxytocin use through a coaching-based intervention based on the WHO Safe Childbirth Checklist in Uttar Pradesh, India: a secondary analysis of a cluster randomised controlled trial. BJOG. 2021;128:2013–21.
Magge H, Nahimana E, Mugunga JC, Nkikabahizi F, Tadiri E, Sayinzoga F, et al. The all babies count initiative: impact of a health system improvement approach on neonatal care and outcomes in Rwanda. Glob Health Sci Pract. 2020;8:000.
Hoover J, Koon AD, Rosser EN, Rao KD. Mentoring the working nurse: a scoping review. Hum Resour Health. 2020;18:1–10.
McFadden A, Gupta S, Marshall JL, Shinwell S, Sharma B, McConville F, et al. Systematic review of barriers to, and facilitators of, the provision of high-quality midwifery services in India. Birth. 2020;47:304–21.
Rao KD, Srivastava S, Warren N, Mayra K, Gore A, Das A, et al. Where there is no nurse: an observational study of large-scale mentoring of auxiliary nurses to improve quality of care during childbirth at primary health centres in India. BMJ Open. 2019;9:e027147.
Waiswa P, Wanduru P, Okuga M, Kajjo D, Kwesiga D, Kalungi J, et al. Institutionalizing a regional model for improving quality of newborn care at birth across hospitals in eastern Uganda: a 4-year story. Glob Health Sci Pract. 2021;9:365–78.
Oosthuizen SJ, Bergh A-M, Grimbeek J, Pattinson RC. Midwife-led obstetric units working ‘CLEVER’: Improving perinatal outcome indicators in a South African health district. S Afr Med J. 2019;109:95–101.
Feeley C, Crossland N, Betran AP, Weeks A, Downe S, Kingdon C. Training and expertise in undertaking assisted vaginal delivery (AVD): a mixed methods systematic review of practitioners views and experiences. Reprod Health. 2021;18:1–22.
Michel-Schuldt M, McFadden A, Renfrew M, Homer C. The provision of midwife-led care in low-and middle-income countries: an integrative review. Midwifery. 2020;84:102659.
Anderson R, Williams A, Jess N, Read JM, Limmer M. The impact of professional midwives and mentoring on the quality and availability of maternity care in government sub-district hospitals in Bangladesh: a mixed-methods observational study. BMC Pregnancy Childbirth. 2022;22:827.
Bogren M, Begum F, Erlandsson K. The historical development of the midwifery profession in Bangladesh. J Asian Midwives (JAM). 2017;4:65–74.
Bogren MU, van Teijlingen E, Berg M. Where midwives are not yet recognised: a feasibility study of professional midwives in Nepal. Midwifery. 2013;29:1103–9.
ten Hoope-Bender P, de Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. Lancet. 2014;384:1226–35.
Save the children and UNFPA. Brief: Integration of Midwifery Services into the Health System 2021. Available from: https://bangladesh.savethechildren.net/sites/bangladesh.savethechildren.net/files/library/SNMP%20Brief_Final_080221_1.pdf . Accessed 2 Mar 2023.
Erlandsson K, Doraiswamy S, Wallin L, Bogren M. Capacity building of midwifery faculty to implement a 3-years midwifery diploma curriculum in Bangladesh: a process evaluation of a mentorship programme. Nurse Educ Pract. 2018;29:212–8.
Bogren M, Erlandsson K, Byrskog U. What prevents midwifery quality care in Bangladesh? A focus group enquiry with midwifery students. BMC Health Serv Res. 2018;18:1–9.
Bartlett L, Weissman E, Gubin R, Patton-Molitors R, Friberg IK. The impact and cost of scaling up midwifery and obstetrics in 58 low-and middle-income countries. PloS One. 2014;9:e98550.
Dawson A, Nkowane A, Whelan A. Approaches to improving the contribution of the nursing and midwifery workforce to increasing universal access to primary health care for vulnerable populations: a systematic review. Hum Resour Health. 2015;13:1–23.
Namazzi G, Achola KA, Jenny A, Santos N, Butrick E, Otieno P, et al. Implementing an intrapartum package of interventions to improve quality of care to reduce the burden of preterm birth in Kenya and Uganda. Implement Sci commun. 2021;2:1–13.
Sangy MT, Duaso M, Feeley C, Walker S. Barriers and facilitators to the implementation of midwife-led care for childbearing women in low- and middle-income countries: a mixed-methods systematic review. Midwifery. 2023;122:103696.
Mwansisya T, Mbekenga C, Isangula K, Mwasha L, Mbelwa S, Lyimo M, et al. The impact of training on self-reported performance in reproductive, maternal, and newborn health service delivery among healthcare workers in Tanzania: a baseline-and endline-survey. Reprod Health. 2022;19:143.
Pappu NI, Öberg I, Byrskog U, Raha P, Moni R, Akhtar S, et al. The commitment to a midwifery centre care model in Bangladesh: An interview study with midwives, educators and students. PloS One. 2023;18: e0271867.
Brac University. Developing midwives: ten years of learning 2022. Accessed on 11 Feb 2023. Available from: https://bracjpgsph.org/assets/pdf/dmp/events/DEVELOPING%20MIDWIVES-TEN%20YEARS%20OF%20LEARNING_compressed.pdf .
Anderson R, Williams A, Emdadul Hoque DM, Jess N, Shahjahan F, Hossain A, et al. Implementing midwifery services in public tertiary medical college hospitals in Bangladesh: a longitudinal study. Women Birth. 2023;36(3):299–304.
Kieny M-P, Evans TG, Scarpetta S, Kelley ET, Klazinga N, Forde I, et al. Delivering quality health services: a global imperative for universal health coverage. Washington, DC: World Bank Group; 2018.
World Health Organization. Five functions to improve quality of care for maternal newborn and child health: knowledge brief 2021. Accessed on 27 May 2023. Available from: https://apps.who.int/iris/bitstream/handle/10665/350118/9789240039025-eng.pdf .
World Health Organization. Definition of skilled health personnel providing care during childbirth: the 2018 joint statement by WHO, UNFPA, UNICEF, ICM, ICN, FIGO and IPA: World Health Organization; 2018. Accessed on 28 May 2023. Available from: https://apps.who.int/iris/bitstream/handle/10665/272818/WHO-RHR-18.14-eng.pdf?ua=1 .
Elliott S, Murrell K, Harper P, Stephens T, Pellowe C. A comprehensive systematic review of the use of simulation in the continuing education and training of qualified medical, nursing and midwifery staff. JBI Evid Synth. 2011;9:538–87.
Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr. 2015;104:96–113.
Hewitt L, Dahlen HG, Hartz DL, Dadich A. Leadership and management in midwifery-led continuity of care models: a thematic and lexical analysis of a scoping review. Midwifery. 2021;98:102986.
Ten Hoope Bender P, Homer C, Matthews Z, Nove A, Sochas L, Campbell J, et al. The state of the world’s midwifery: a universal pathway, a woman’s right to health. 2014.
Bailey P, Paxton A, Lobis S, Fry D. The availability of life-saving obstetric services in developing countries: an in-depth look at the signal functions for emergency obstetric care. Int J Gynecol Obstet. 2006;93:285–91.
Ndabarora E, Chipps JA, Uys L. Systematic review of health data quality management and best practices at community and district levels in LMIC. Info Dev. 2014;30:103–20.
International Confederation of Midwives. Essential Competencies for Midwifery Practice, 2019 update 2019. Accessed on 11 Feb 2023. Available from: https://www.internationalmidwives.org/assets/files/general-files/2019/10/icm-competencies-en-print-october-2019_final_18-oct-5db05248843e8.pdf .
Reed JE, Green S, Howe C. Translating evidence in complex systems: a comparative review of implementation and improvement frameworks. Int J Qual Health Care. 2019;31:173–82.
Download references
Acknowledgements
Not applicable.
This research received no external funding.
Author information
Authors and affiliations.
The Faculty of Health and Medicine, Lancaster University, Lancaster, UK
Rondi Anderson & Mark Limmer
Department of Health Sciences, James Madison University, Harrisonburg, Virginia, USA
Sojib Bin Zaman
Environmental Science Department, Jahangirnagar University, Dhaka, Bangladesh
Abdun Naqib Jimmy
Lancaster Medical School, Lancaster University, Lancaster, UK
Jonathan M Read
You can also search for this author in PubMed Google Scholar
Contributions
RA conceived the design of this systematic review and drafted the first version of the manuscript. SBZ, ANJ, JMR, and ML has contributed substantially, providing inputs to the manuscript and revising it critically. All authors have reviewed and agreed to the submitted version of the manuscript.
Corresponding author
Correspondence to Rondi Anderson .
Ethics declarations
Ethics approval and consent to participate.
Not applicable
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Anderson, R., Zaman, S.B., Jimmy, A.N. et al. Strengthening quality in sexual, reproductive, maternal, and newborn health systems in low- and middle-income countries through midwives and facility mentoring: an integrative review. BMC Pregnancy Childbirth 23 , 712 (2023). https://doi.org/10.1186/s12884-023-06027-0
Download citation
Received : 30 June 2023
Accepted : 24 September 2023
Published : 05 October 2023
DOI : https://doi.org/10.1186/s12884-023-06027-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Maternity care
- Health systems strengthening
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Aromataris E, Pearson A. The Systematic Review. Am Jf Nurs. 2014; 114:(3)
Aromataris E, Riitano D. Systematic Reviews. Am J Nurs. 2014; 114:(5)49-56
Atsali E, Russell K. Hospital midwives' barriers when facilitating upright positions during a normal second stage of labour. Africa Journal of Nursing And Midwifery. 2018; 20:(1)
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006; 3:(2)77-101
Critical Appraisal Skills Programme. CASP Systematic Review Checklist. 2018. https://casp-uk.net (accessed 19 August 2020)
Deliktas A, Kukulu K. A meta-analysis of the effect on maternal health of upright positions during the second stage of labour, without routine epidural analgesia. Journal of Advanced Nursing. 2018; 74:(2)263-278
Gizzo S, Di GS, Noventa M, Bacile V, Zambon A, Nardelli GB. Women's choice of positions during labour: return to the past or a modern way to give birth? a cohort study in italy. Biomed Research International. 2014; 638093-638093
Green T. Exploring the influence that midwives have on women's position in childbirth: a review of the literature. Evidence Based Midwifery. 2015; 13:(4)132-137
Gupta JK, Sood A, Hofmeyr GJ, Vogel JP. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database of Systematic Reviews. 2017; 5:(5)
Hammond A, Homer CSE, Foureur M. Friendliness, functionality and freedom: Design characteristics that support midwifery practice in the hospital setting. Midwifery. 2017; 50:133-138
Huang J, Zang Y, Ren L, Li-Hua F, Lu H. A review and comparison of common maternal positions during the second-stage of labour. International Journal of Nursing Sciences. 2019; 6:(4)460-467
Lee N, Tracy S. Disturbances in the rhythm of labour (Chapter 36). In: Pairman S, Tracy SK, Dahlen HG, Dixon L (eds). Chatswood, Australia: Elsevier; 2019
Moher D, Liberatui A, Tetziaff J, Altman D. Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. PLoS Med. 2009; 6:(7)
Mselle L, Eustace L. Why do women assume a supine position when giving birth? The perceptions and experiences of postnatal mothers and nurse-midwives in Tanzania. BMC Pregnancy And Childbirth. 2020; 20:(1)
Munn Z, Tufanaru C, Aromataris E. JBI's Systematic Reviews: Data Extraction and Synthesis. American Journal Of Nursing. 2014; 114:(7)49-54
Musie M, Peu M, Bhana-Pema V. Factors hindering midwives' utilisation of alternative birth positions during labour in a selected public hospital. African Journal Of Primary Health Care & Family Medicine. 2019; 11:(1)
Porritt K, Gomersall J, Lockwood C. JBI's Systematic Reviews. American Journal Of Nursing. 2014; 114:(6)47-52
Robertson-Malt S. JBI's Systematic Reviews. American Journal Of Nursing. 2014; 114:(8)49-54
Stern C, Jordan Z, McArthur A. Developing the Review Question and Inclusion Criteria. American Journal Of Nursing. 2014; 114:(4)53-56
Tracy S. Interventions in pregnancy, labour and birth (Chapter 37). In: Pairman S, Tracy SK, Dahlen HG, Dixon L (eds). Chatswood, Australia: Elsevier; 2019
World Health Organization. WHO recommendation on birth position (for women without epidural analgesia). 2018. https://bit.ly/3sNv09T (accessed 15 February 2022)
Stand and deliver: an integrative review of the evidence around birthing upright
Laura Irvin
Registered midwife, Edith Cowan University, Western Australia
View articles
Annemarie De Leo
Midwifery lecturer, Edith Cowan University, Western Australia
View articles · Email Annemarie
Clare Davison
Lecturer in Midwifery and independent midwife, School of Nursing and Midwifery, Edith Cowan University, Western Australia

The benefits of upright birth positions are well-established in the literature, yet women are persistently challenged to assume the lithotomy or supine birth positions. This study aimed to explore what is known about women's capacity to assume upright birth positions in hospital environments, and its effect on physiological birth.
A structured five-step approach was employed to conduct an integrative review of the literature. The Cumulative Index to Nursing and Allied Health Literature and MEDLINE were searched for articles on women's position during labour and birth in hospital settings. Four articles were selected for inclusion and subjected to thematic analysis to elicit themes and subthemes.
Three core themes emerged from this review: ‘the biomedical model of care and workplace culture impact the positions women adopt during labour and birth’, ‘midwives' philosophy and views support physiological birth’ and ‘clinical settings are not conducive to physiological birth’.
Conclusions
Midwives are losing the skills and confidence to support women into upright birth positions. Improved education and training around upright birthing may see a rise in women adopting these positions in hospital environments.
A woman's physiological instinct to assume upright positions during labour and birth is increasingly challenged in hospital settings, despite recommendations from the World Health Organization (2018) that women should have the autonomy to adopt any position deemed safe and comfortable during birth. Acknowledged as an evidence-based practice, adopting upright birth positions is known to positively impact maternal and fetal birth outcomes ( Deliktas and Kukulu, 2018 ; Huang et al, 2019 ), yet labouring women are often encouraged into supine or semi-recumbent positions, which are known to increase the likelihood of epidurals and obstetric intervention ( Gizzo et al, 2014 ). While medical intervention is acknowledged to be beneficial at times, the risk of these becoming routine practices has undoubtedly influenced the normal processes of birth ( Gizzo et al, 2014 ; Lee and Tracy, 2019 ). Arguably, the rise in perineal trauma, prolonged labours ( Huang et al, 2019 ) and increased rates of assisted birth worldwide ( Atsali and Russel, 2018 ) are evidence that medical intervention during labour and birth are increasingly common practices.
This integrative review aimed to provide valuable insight into the factors that impact a woman's capacity to adopt upright birth positions in clinical settings, and also explores the influences of maternity staff in this context.
This review followed the recommendations of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) checklist ( Moher et al, 2009 ), the Critical Appraisal Skills Program (2018) checklists and a series of articles outlining the step-by-step approach to conducting systematic reviews published by the Joanna Briggs Institute ( Aromastaris and Pearson, 2014 ; Aromastaris and Riitano, 2014 ; Munn et al, 2014 ; Porritt et al, 2014 ; Robertson-Malt, 2014 ; Stern et al, 2014 ).
Search strategy
The focus of this search strategy was to locate published literature relevant to the review question ‘what factors prevent women from adopting upright birth positions in hospital settings?’ As outlined by Aromataris amd Pearson (2014) , a logic grid was developed to identify keywords derived from the review question ( Table 1 ).
When combined, these formulated a search string that was then entered into two accredited electronic databases: the Cumulative Index to Nursing and Allied Health Literature and MEDLINE. Following this, an extensive manual search by citation was conducted to retrieve additional literature that was not found in the initial search. This also included a search through the end reference lists of all articles meeting the inclusion criteria. The articles eligible for review had to have been peer-reviewed, published between 2014 and 2020 in English, with the full text available. The complete search and screening process is presented in Figure 1 .
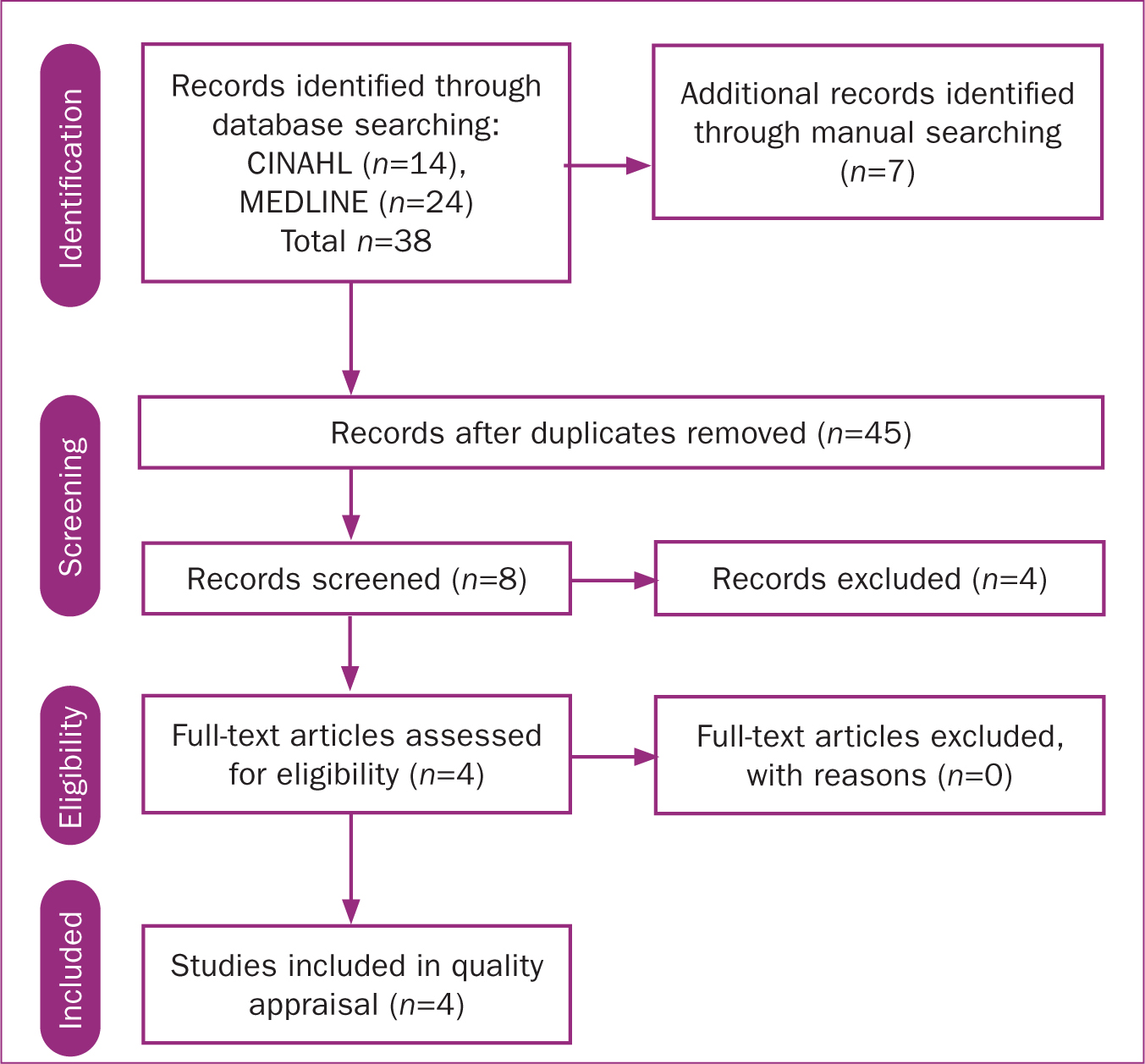
Critical appraisal
Critical appraisal was completed using the Critical Appraisal Skills Program (2018) checklist for qualitative research. The methodological rigor of each potential article was assessed against a set of 10 questions derived from three broad issues used to appraise the validity of a qualitative study. The first issue asks if the results are valid:
- Was there a clear statement of the aims of the research?
- Is a qualitative methodology appropriate?
- Was the design appropriate to address the aims?
- Was the recruitment strategy appropriate to the aims?
- Were the data collected in a way that addressed the research issue?
- Has the relationship between researcher and participants been adequately considered?
The second asks what the results were, by asking ‘have ethical issues been taken into consideration?’, ‘was the data analysis sufficiently rigorous?’ and ‘is there a clear statement of findings?’. The third asks whether the results will help locally, asking ‘how valuable is the research?’
Four articles were excluded as they did not adequately meet the checklist criteria, were deemed irrelevant or inappropriate to the review question and selection criteria or because they did not provide adequate descriptions of the study conducted. Four articles were retained for inclusion in this review ( Table 2 ).
Data extraction and analysis
Data extraction and thematic analysis was conducted using Braun and Clarke's (2006) approach. This involved initial familiarisation with the data, coding of key findings and grouping emergent themes and patterns into meaningful categories.
Three core themes emerged from the dataset, which were derived from five subthemes ( Table 3 ). The core themes were ‘the biomedical model of care and workplace culture impact the positions women adopt during labour and birth’, ‘midwives’ philosophy and views support physiological birth’ and ‘clinical settings are not conducive to physiological birth’. Together, these findings present the factors that both help and hinder women's capacity to assume upright positions in clinical settings and the impact this has on physiological birth.
The medical model of care and workplace culture impact labour and birth positions
The influence of the medical model of care within clinical settings were evident in all four articles included in this review ( Green, 2015 ; Atsali and Russell, 2018 ; Musie et al, 2019 ; Mselle and Eustace, 2020 ). Within these contexts, midwives were reportedly more likely not to offer women the choice of upright birth positions, even when requested by the woman ( Atsali and Russell, 2018 ). The medical model was also described as fragmented and led by obstetric policies, which were often unsupportive of physiological birth ( Atsali and Russell, 2018 ). Maternity staff were also noted to focus on delivering routine interventions such as cardiotocograph monitoring and vaginal examinations, which were used to persuade labouring women into supine positions or to remain on the bed ( Green, 2015 ; Atsali and Russell, 2018 ).
Workplace culture is seen as a barrier to physiological birth
Workplace culture was reported a barrier to upright birth in two of the included articles ( Atsali and Russell, 2018 ; Musie et al, 2019 ).
‘The conformity of midwives and women to hospital routines and practices [was] an important determinant of actual behaviour.’
( Atsali and Russell, 2018 )
‘I place the woman in the lithotomy position because it's what I find being done in the unit.’
( Musie et al, 2019 )
Despite some midwives acknowledging they were taught about optimal birth positions, midwives reported they did not use alternative birth positions.
‘I never practice alternatives [positions], I guess we just…adopted the [routine] culture.’
(Musie et al, 2018)
Green (2015) reported similar findings, suggesting midwives were more likely to support supine positions for clinical procedures and assessments during labour, such as routine cardiotocograph monitoring, as it was the norm for institutional policy.
Power and coercion were thought to dominate the practices and behaviour of midwives working in these contexts. This hierarchy impacted the culture of birth environments, at times leaving midwives struggling to be compliant and fearing consequences if they acted autonomously ( Atsali and Russell, 2018 ).
‘Midwives tend to work within a hierarchical system with the obstetrician at the top, followed by the senior midwife then the junior midwives and finally the women.’
All articles in this review included midwife participants who admitted to prioritising their own comfort over the woman's preference to adopt an upright position during birth ( Green, 2015 ; Atsali and Russell, 2018 ; Musie et al, 2019 ; Mselle and Eustace, 2020 ). This highlighted the potential for power imbalances between midwives and women.
‘My view on alternative birth positions is it can only be done if the midwife is comfortable with it.’
Similarly, Mselle and Eustace (2020) reported midwives felt more knowledgeable than women in regard to birth practices and as such determined the appropriate birth position.
‘It is difficult to allow [the woman] to use her preferred position because the midwife is the one who knows the best birthing position.’
( Mselle and Eustace, 2020 )
Midwives' philosophy and views support physiological birth
Midwives were recognised as being highly influential to labouring women, with women reporting midwives to be the most influential factor when considering birth positions ( Green, 2015 ; Atsali and Russell, 2018 ; Musie et al, 2019 ). As such, midwives' attitudes towards upright physiological birth are influences most likely to impact the positions women adopt during labour. While the skills and knowledge of midwives were at times recognised as a barrier to upright birth, so too was that of women, with a lack of knowledge about upright birth positions perceived by women to be a factor that further compounded this issue ( Musie et al, 2019 ).
Notably, midwives working within continuity of care services were more likely to encourage women to adopt the birth position of their choice ( Atsali and Russell, 2018 ). Midwifery-led models were also associated with information-sharing between women and midwives, which led to midwifery practices that accommodated women's preferences to adopt upright birth positions and information on the benefits of physiological birth ( Green, 2015 ).
Midwives are highly influential to pregnant and labouring women
The majority of articles included in this review recognised the midwife as influential to women adopting upright positions during birth ( Green, 2015 ; Atsali and Russell, 2018 ; Mselle and Eustace, 2020 ).
‘Women perceive midwives' influence as the most important factor when considering birth positions.’
( Green, 2015 )
Similarly, midwives were described to positively influence a woman's birth position by encouraging them to remain upright and being creative within the birth space ( Green, 2015 ).
Midwives' attitudes, skills and confidence are factors that influence physiological upright birth
This category highlights the influence of midwives' views towards upright birth and their confidence to support such practices. Atsali and Russell (2018) reported some midwives felt deficient in skills to confidently facilitate upright birth. Similarly, Musie et al (2019) suggested midwives lacked the confidence to support physiological birth because of limited training. Some midwives also reported they promoted supine birth as their preferred position, deeming this mode more convenient for managing obstetric complications ( Green, 2015 ; Atsali and Russell, 2018 ; Musie et al, 2019 ; Mselle and Eustace, 2020 ).
Women lack knowledge of physiological birth and antenatal education on birth positions is limited
Attending antenatal classes significantly contributed to women feeling better informed about upright birth positions, which increased women's preference to assume such positions during birth ( Green, 2015 ). Women's knowledge of the benefits of upright birth positions was further enhanced through continuity of care and discussion with their midwives ( Green, 2015 ). Other findings suggested women were not provided with information regarding upright birth positions during parent education sessions.
‘We did not receive any education on alternative birthing positions…but our friends tell us about different birthing positions.’
This was reportedly an issue for midwives as well, who commented on their increasing workloads, which impinged on the time midwives had to provide antenatal education, assessment and information sharing ( Musie et al, 2019 ).
Clinical settings are not conducive to physiological birth
A significant finding of this review suggested that midwives feel that clinical settings are not conducive to supporting upright physiological birth. The limited availability of equipment and resources (ie fit balls, birth stools, birth pools) to promote such practices in birth environments was also noted.
The design of clinical settings is not conducive to facilitating upright birth
A woman's birth environment can have a psychological impact on her labour and birth ( Atsali and Russell, 2018 ). Atsali and Russell (2018) and Green (2015) concurred, suggesting that hospital birth spaces were more likely to be designed with additional technologies to meet the needs of women requiring complex care, limiting room for both women and midwives to move.
The findings of this review confirm maternity care in clinical settings continues to be dominated by the medical model of care. This is evidenced by workplace cultures governed by risk-aversion, policies that at times may not reflect evidence-based practices and limited time to educate women and train midwives on positions that promote physiological birth. Midwives were found to significantly influence the positions women adopt during labour and birth, with midwives' views towards upright birth, and their skillsets to support such positions, directly impacting the provision of upright birth practices.
In this review, midwives' knowledge and experience of upright birth was varied, with an evident gap in both training and confidence to support women to birth in upright positions. This also influenced the education women receive antenatally, with most women and nurse-midwives reporting limited opportunities for discussion and education about optimal birth positions during antenatal appointments. These findings bring to light midwives' workloads and the limited capacity midwives and obstetric nurses have to adequately educate women on such practices in hospital settings. While midwifery-led care and other continuity of care models were recognised as facilitators of upright birth, the attitudes and skills of most nurse-midwives working in hospital settings were influenced by the medical model of care. This highlighted the use of routine intrapartum interventions that at times did not appear to be woman-centred, evidence-based or protective of physiological birth.
A substantial finding emphasises the importance of functional hospital birth spaces, with cluttered birthing rooms and limited access to resources highlighted as a core challenge for midwives wanting to support women to experience an upright physiological birth. This finding resonates with Hammond et al (2017) , who identified three key design characteristics that support midwifery practice: friendliness, functionality and freedom to move spontaneously and practice responsive midwifery care.
While the benefits of upright birth positions were well recognised in this review, so too were the risks associated with supine positions. Semi-recumbent and lithotomy positions were acknowledged to increase the risk of perineal trauma, maternal pain, prolonged labours, abnormal fetal heart rate patterns and the likelihood of assisted birth ( Atsali and Russel, 2018 ). This is consistent with work by Gupta et al (2017) , who reported women who used upright birth positions during labour were 25% less likely to experience an instrumental birth, 25% less likely to receive an episiotomy and, notably, experienced a significant reduction in pain during labour and birth. The use of oxytocics and schedule eight pain relief (eg epidural, morphine) was also increased, leading to additional risks for maternal and fetal wellbeing ( Tracy, 2019 ).
Limitations
Although every effort was made to ensure this review presents findings based on best available evidence, the authors acknowledge key issues arising from this review. It is possible that pertinent studies relevant to the phenomenon of interest were missed for inclusion, the findings were based on four articles and consequently may limit the transferability of evidence across different midwifery contexts or countries, and it is plausible that articles in languages other than English may have provided additional insight into the review findings.
This integrative review makes a valuable contribution to the body of evidence on the phenomenon of interest by highlighting key findings. An evidence-to-practice gap persists regarding the education midwives and women receive in the antenatal period on the benefits of adopting upright positions during labour and birth. Further development of policies that facilitate upright birth must be embedded into routine care practices in clinical areas and adequate education and training for midwives and obstetricians, as well as antenatal education programs for pregnant women, will raise awareness of upright birth positions and likely foster positive attitudes towards supporting upright birth in clinical practice.
- In hospital environments where birth occurs, midwives experience tensions between the medical model of care, adhering to clinical guidelines and practicing evidence-informed care.
- Normalising physiological birth for women in hospital environments is crucial for the future of evidence-based maternity services.
- For this to occur, the gap between clinical practice guidelines and evidence-based practice in birth environments must be addressed.
- Improving education and training for midwives, as well as pregnant women, will raise awareness of the benefits of upright birth positions and likely foster positive change in hospital birthing environments.
CPD reflective questions
- Do your workplace policies and guidelines reflect evidence-based practice, and do they align with your own midwifery philosophy?
- What practices can you identify in your workplace that require updating or improvement to align with latest evidence?
- What strategies can you employ to initiate the updating or improvement of evidence-based practice in your workplace?
- Does your workplace support evidence-based change, what helpers and hindrances can you identify?
- How can midwives ensure women remain the centre of all care in birth environments?
Systematic reviews in midwifery
Affiliation.
- 1 Department of Public Health, University of Aberdeen.
- PMID: 16734008
This paper highlights the key steps to follow when conducting a systematic review (see Box 2). Healthcare practitioners may be limited by time and resources when conducting literature reviews, however, a systematic and transparent approach should be adopted wherever possible. Further detailed guidance on conducting systematic reviews is available from the NHS Centre for Reviews and Dissemination (NHS CRD, 2001) and the Cochrane Reviewers' Handbook (Alderson et al, 2003).
Publication types
- Systematic Review
- Databases, Bibliographic
- Medical Subject Headings
- Midwifery / organization & administration*
- Nursing Methodology Research*
- Professional Competence*
- Review Literature as Topic*
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.10(3); 2023 Mar
An integrative review of supportive relationships between child‐bearing women and midwives
Hadeer almorbaty.
1 School of Nursing and Midwifery, College of Health Medicine and Well‐Being, The University of Newcastle, University Drive, Callaghan New South Wales, Australia
2 Nursing Department, Prince Sultan Military College of Health Sciences, Dhahran Saudi Arabia
3 Faculty of Health, Southern Cross University, Coffs Harbour New South Wales, Australia
Eileen Dowse
4 School of Nursing and Midwifery, College of Health Medicine and Well‐Being, The University of Newcastle, University Drive, Callaghan New South Wales, Australia
Sally Wai‐Chi Chan
5 Tung Wah College, Dhahran Hong Kong
Associated Data
The data that support the findings of this study are available in [repository name] at [URL/DOI], reference number [reference number]. These data were derived from the following resources available in the public domain: [list resources and URLs].
To review and evaluate the literature on the factors related to developing supportive relationships between women and midwives, including facilitators and barriers.
An integrative review.
The search used CINAHL, MEDLINE, Embase, EMcare, Maternity and Infant Care, PsycINFO, and Google Scholar from January 2009–June 2020. Two reviewers screened the eligible studies, and 2,399 records were identified. Quality was assessed with the mixed methods appraisal tool, and 14 articles were included.
The findings highlight that successful relationships require therapeutic communication, trust, respect, partnership, and shared decision‐making. Supportive relationships improve women′s satisfaction and birth outcomes, and continuity of care model is an enabling factor. Further research is required to understand supportive relationships in non‐continuity of care models and when different cultural backgrounds exist.
What Is Known About This Topic?
- The physical and emotional support midwives provide to child‐bearing women can contribute to positive child‐bearing experiences and birth outcomes.
- Not all women perceive their relationships with midwives as supportive.
- Organizational factors, such as staffing ratios and workload issues, may impede midwives' abilities to build supportive relationships with women.
- Continuity of care models facilitate the development of supportive relationships.
What Does This Paper Add?
- Midwives can facilitate the development of supportive relationships, through effective communication skills, mutual trust, respect, and partnership.
- Workplace culture within maternity units, affects midwives' abilities to develop and maintain supportive relationships with women.
- The socio‐cultural context in which women and midwives live and work further impacts their abilities to develop and maintain supportive relationships.
- There is a lack of knowledge about how supportive relationships are developed in maternity units, especially where continuity of care is not practised.
What Are the Implications for Practices and Policies?
- More research is needed to explore the best approach and most effective strategies for developing supportive relationships, within existing models of care.
- Further research is required to understand how the cultural identities of both women and midwives affect the development of supportive relationships.
1. INTRODUCTION
A key aspect of maternity care is a supportive relationship between the child‐bearing woman and her midwife or maternity nurse—the quality of this relationship is pivotal to safe maternity care and improving the woman′s experience (Agostini et al., 2015 ). Child‐bearing experiences can vary greatly among women. A poor experience can affect a woman′s physiological and psychological wellbeing during the immediate postpartum and long‐term periods (McInnes et al., 2020 ). Understanding how supportive relationships develop, between child‐bearing women and their midwives or maternity nurses during the child‐bearing period can help guide practices and improve maternity care.
2. BACKGROUND
The child‐bearing period can be one of the most significant times in a woman′s life. In this review, the ‘child‐bearing period’ refers to the pregnancy, labour, birth and postpartum period (i.e., up to 6 weeks following the birth) (Qi & Creedy, 2009 , p. 2). During this time, many physiological, psychological and emotional changes can affect the woman′s emotional and physical well‐being as well as the birth outcomes for her baby. A supportive relationship is a fundamental aspect of quality care for patients. In maternity care, supportive relationships between women and their midwives or maternity nurses are founded on mutual respect, shared power, and working in partnership to support women to engage in decision‐making regarding their care (World Health Organization, 2016 ).
The literature has used various terms for healthcare providers supporting child‐bearing women. In this review, “midwives” includes midwives and nurse‐midwives caring for women giving birth and their infants, and preparing them for self‐care and child care at home. It also includes registered or accredited nurses with a significant role in assessing and managing women′s progress in labour, where the provider attends the birthing room when the birth is close or there are serious complications. The exception is the “Results” section, where the original terminology from the reviewed articles is used for clarity.
Research has indicated that the physical and emotional support provided in a therapeutic relationship can contribute to positive child‐bearing experiences and birth outcomes, including reduced oxytocin requirements and perineal lacerations (Sehhatie et al., 2014 ), reduced elective caesarean births, lower healthcare costs (Tracy et al., 2014 ), reduced incidences of postpartum depression and increased levels of satisfaction with care (Backstrom et al., 2016 ; Goodwin et al., 2018 ). Furthermore, an effective supportive relationship can lower a woman′s stress levels and facilitate optimal conditions for the baby′s development (Buckley, 2015 ).
Literature has suggested that certain factors affect the development of supportive relationships, such as ethnic heterogeneity, socioeconomic differences, culture and preferences (Bradfield, Hauck, Duggan, et al., 2019 ; Goodwin et al., 2018 ). Other factors include the healthcare professional′s capacity for empathy, trust, and emotional support, and the hospital′s policies for the maternity care model such as continuity of care (COC) (Bradfield et al., 2019b ). COC is a model of midwifery care where the woman receives COC from a known midwife or known midwifery team throughout the child‐bearing period, and postpartum care may continue in the home (Homer, 2016 ).
The importance of woman–midwife relationships has been the focus of research on models of maternity care that implement COC in their health systems, such as the United Kingdom (UK) and New Zealand (NZ) (Bradfield et al., 2019d ; Homer, 2016 ). However, there is a paucity of summarized evidence focusing on facilitators and barriers to developing supportive relationships. An integrative review is required to synthesize the evidence on developing supportive relationships between child‐bearing women and midwives. Such understanding can help build supportive relationships, and thus improve the quality of maternity care and women′s child‐bearing experiences.
This review aims to evaluate the literature on the factors related to developing supportive relationships between women and midwives, including facilitators and barriers.
4.1. Design
An integrative literature review design was used to understand a particular phenomenon and produce new knowledge in social and behavioural sciences (Torraco, 2016 ). Its flexibility in combining diverse methodologies, and ability to contribute to evidence‐based practice can build knowledge and inform policymakers about a particular phenomenon in practice. This review adopted Whittemore and Knafl′s ( 2005 ) five‐stage process: (1) identifying the research questions; (2) conducting a comprehensive search of the literature; (3) evaluating the studies found; (4) analysing the studies included in the review; and (5) reporting and discussing the findings.
4.1.1. Research questions
- What are the perceived facilitators and barriers to developing supportive relationships during the child‐bearing period from women′s and midwives′ perspectives?
- What cultural factors might affect the process of developing supportive relationships during the child‐bearing period from women′s and midwives′ perspectives?
4.2. Comprehensive literature search
The literature search was limited to publications from January 2009–June 2020. The search included studies from the following databases: CINAHL, MEDLINE, EMbase, Emcare, Maternity and Infant Care, and PsycINFO. Google Scholar was used to find relevant studies. The keywords were: midwife*‐woman relationship, and matern* or midwife*, and facilitators or barriers and experience. Words were combined with AND or OR to focus or limit the search results. Synonyms of each keyword were generated via word expansion (see Table 1 ).
The keywords and synonyms used across all databases
The inclusion criteria included: (1) primary research studies on supportive relationships between women and midwives, or maternity nurses, using any research design; (2) studies published in the English or Arabic languages; and (3) studies published in peer‐review journals. The exclusion criteria included (1) studies not in the English or Arabic languages (due to a lack of translation resources); (2) publications other than primary research studies, such as meta‐analyses, dissertations, books, grey literature, conference abstract papers, reports, and commentaries; (3) studies focused on relationships with healthcare providers other than midwives or nurses; and (4) studies with a focus on a particular maternity or midwifery program, approach or care model.
4.3. Evaluating the studies
The initial search retrieved 2,399 sources. The duplicates were removed ( n = 1,193), and the relevant studies were manually screened. A total of 1,182 articles were excluded because of the study focus, leaving 24 studies for review. One article that aligned with the inclusion criteria was found in the reference list of one of the studies from the search. Therefore, the final review, included 25 studies, which were assessed for relevance, quality, and results concerning the research questions. A second reviewer (a supervisor from the research team) affirmed the eligibility of the included studies. Finally, a total of 14 articles were reviewed. The PRISMA diagram (see Figure 1 ) illustrates the review search steps and outcomes (Moher et al., 2009 ). All reviewers discussed and agreed on the review outcomes.

PRISMA diagram
4.3.1. Quality appraisal
The quality of the included studies was appraised using the mixed‐methods appraisal Tool (MMAT) (Hong et al., 2018 ). The MMAT allows a judgement of the methodological quality of studies for various research designs (qualitative, quantitative, and mixed‐methods studies). One study was judged as being of low quality. However, it was included because of its relevance to the research questions. Table 2 summarizes the included studies using MMAT criteria.
Summary of quality appraisal of qualitative, quantitative and mixed‐methods, using MMAT criteria
Note : S1 and S2 = screening questions (for all types of study design): S1, Are there clear research questions?; S2, Do the collected data allow to address the research questions? 1, 2, 3, 4, and 5 = Methodological quality criteria described below for each design, Qualitative: 1, Is the qualitative approach appropriate to answer the research question?; 2, Are the qualitative data collection methods adequate to address the research question?; 3, Are the findings adequately derived from the data?; 4, Is the interpretation of results sufficiently substantiated by data?; 5, Is there coherence between qualitative data sources, collection, analysis and interpretation? Quantitative, nonrandomized: 1, Are the participants representative of the target population?;2, Are measurements appropriate regarding both the outcome and intervention (or exposure)?; 3, Are there complete outcome data?; 4, Are the confounders accounted for in the design and analysis?; 5, During the study period, is the intervention administered (or exposure occurred) as intended? Mixed‐methods: 1, Is there an adequate rationale for using a mixed methods design to address the research question?; 2, Are the different components of the study effectively integrated to answer the research question?; 3, Are the outputs of the integration of qualitative and quantitative components adequately interpreted?; 4, Are divergences and inconsistencies between quantitative and qualitative results adequately addressed?; 5, Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? (Hong et al., 2018 ).
4.4. Analysing the studies
4.4.1. data extraction.
A data extraction form (see Table 3 ) was used to extract the data from the reviewed articles, including the study description, methods, and results. Thematic analysis was used to analyse the data for factors considered facilitators or barriers to developing supportive relationships. This involved reading the articles, searching for meaningful ideas, creating codes, identifying themes, organizing the themes, and naming them concisely to make sense for the reader (Braun & Clarke, 2006 ). Three main themes and nine sub‐themes were generated (see Table 4 ).
Extracted data of the included articles
Themes and sub‐themes generated
4.5. Reporting and discussing the findings
4.5.1. study characteristics.
Two studies were conducted in the United States of America, three in the UK, two in Sweden, one in Japan, one in East Africa, four in Australia and one in NZ. There were 762 participants in the reviewed studies, including 450 midwives, 78 maternity nurses, 172 child‐bearing women and 101 mothers. Of the participating women (i.e., 273 child‐bearing women and mothers), 22 participated in the studies during pregnancy, 17 were in either the pregnancy or postpartum period, 234 were in the postpartum period and one was in a neonatal intensive care unit (Shimizu & Mori, 2018 ).
5.1. Theme 1: Human interaction factors
Human interaction factors were mentioned in 14 studies. Four sub‐themes emerged: demonstrating trust and respect, recognizing midwives' attitudes and beliefs, developing partnerships and effective communication skills.
5.1.1. Demonstrating trust and respect
Six qualitative studies (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a , 2019b ; Madula et al., 2018 ; McInnes et al., 2020 ; Menage et al., 2020 ) described trust and respect as a facilitator of developing supportive relationships with women. In this review, ‘respect’ refers to how midwives differentiate the boundaries between professional and personal relationships, including accepting women′s choices (Nursing and Midwifery Board of Australia, 2018). “Trust” is defined as the part of a partnership with a woman that maintains equality and sharing (International Confederation of Midwives, 2017; Nursing and Midwifery Board of Australia, 2018).
Midwives stated that trust promoted the building of supportive relationships with women (Menage et al., 2020 ), and showing respect allowed them to form a strong connection, during a challenging time to engage, such as labour. In a study including 15 child‐bearing women, the importance of respect was reinforced—they experienced positive relationships with maternity nurses when they felt respected (Madula et al., 2018 ).
5.1.2. Recognizing midwives' attitudes and beliefs
“Attitudes” and ‘beliefs’ refer to modes feeling and thinking, which affect behaviour and, therefore, the ability to develop relationships (Bradfield et al., 2019a ; Carlton et al., 2009 ). Three qualitative studies (Backstrom et al., 2016 ; Bradfield et al., 2019a , 2019b ) reported that midwives' negative or positive feelings were important for their attitudes towards developing supportive relationships with women. Eight articles (Aschenbrenner et al., 2016 ; Backstrom et al., 2016 ; Bradfield et al., 2019a , 2019b ; Carlton et al., 2009 ; Goodwin et al., 2018 ; McInnes et al., 2020 ; Menage et al., 2020 ) discussed facilitators or barriers influencing midwives' or maternity nurses' attitudes. These included motivation, personality, preference, experience and knowledge (McInnes et al., 2020 ).
Experience and knowledge can empower midwives to manage challenges while building supportive relationships. The more educated and/or experienced the midwives/maternity nurses, the more their relationships were (Aschenbrenner et al., 2016 ; Bradfield et al., 2019a ; Carlton et al., 2009 ; Menage et al., 2020 ). Further, when a midwife′s and a woman′s personalities do not match, it could impede the supportive relationship (Backstrom et al., 2016 ; Bradfield et al., 2019a ). However, neither study discussed how the personalities might be mismatched.
5.1.3. Developing partnerships
Partnerships were discussed in 10 studies. Carlton et al. ( 2009 ) found that partnerships could be achieved when women and maternity nurses shared power. Partnerships include elements such as shared decision‐making (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a , 2019b ), mutual involvement (Shimizu & Mori, 2018 ) and healthcare professionals advocating for empowering the woman (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a , 2019b ; Davison et al., 2015 ; Shimizu & Mori, 2018 ). Empowering child‐bearing women is considered essential in supportive relationships (Menage et al., 2020 ). It is thought to occur when the midwife provides guidance (Crowther & Smythe, 2016 ) and advocates for the woman (Bradfield, Hauck, Duggan, et al., 2019 ). However, there were few details about when to share decision‐making and the relevant aspects of the care.
Two qualitative studies (Bradfield, Hauck, Duggan, et al., 2019 ; Davison et al., 2015 ) asserted that woman‐centred care could enhance positive and supportive relationships with women, facilitate shared decision‐making and improve their birth outcomes, enhancing women′s satisfaction with care and birthing experiences. Seven studies (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a ; Davison et al., 2015 ; Goodwin et al., 2018 ; McInnes et al., 2020 ; Menage et al., 2020 ; Shimizu & Mori, 2018 ) also reported that woman‐centred care that was tailored to the woman′s preferences facilitated supportive relationships .
Other studies identified positive relationships between women and midwives when women, their family members and significant others were involved in care planning (Bradfield et al., 2019a , 2019b ; Davison et al., 2015 ; Goodwin et al., 2018 ; Shimizu & Mori, 2018 ). Shimizu and Mori′s (2018) study was conducted in Japan with a small sample size ( N = 98 ). Although all study participants assessed their relationships with maternity nurses positively, Shimizu and Mori stated that it might not have been positive for those who did not participate. Furthermore, the women′s responses remained positive even when the questions did not apply. Finally, two studies (Bradfield et al., 2019a ; Goodwin et al., 2018 ) reported that some women refused to choose or build any relationships and preferred their own space.
5.1.4. Effective communication skills
Effective communication skills are fundamental in any relationship. Nine articles (Aschenbrenner et al., 2016 ; Backstrom et al., 2016 ; Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019b ; Carlton et al., 2009 ; Crowther & Smythe, 2016 ; Madula et al., 2018 ; Menage et al., 2020 ; Oscarsson & Stevenson‐Ågren, 2020 ) identified communication as an enabling practice for developing supportive relationships with women. In one study, midwives ( n = 31) described how they used basic communication skills, such as gaining rapport and providing verbal encouragement, to facilitate relationships development with women (Bradfield, Hauck, Duggan, et al., 2019 ). Further, Backstrom et al. ( 2016 ), Oscarsson and Stevenson‐Ågren ( 2020 ) and Menage et al. ( 2020 ) found that active listening skills are essential to developing supportive relationships. However, Madula et al. ( 2018 ) reported that a lack of interpersonal skills in midwives and maternity nurses was a common communication barrier leading to the women feeling frustrated about their unmet needs.
5.2. Theme 2: Cultural factors
Five studies (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a ; Carlton et al., 2009 ;Goodwin et al., 2018 ; Oscarsson & Stevenson‐Ågren, 2020 ) discussed cultural factors, focusing on individual′s beliefs and, their effects on the expectations and practices of women and midwives.
5.2.1. Women′s health beliefs
Bradfield et al., 2019a described the need for cultural safety, and understanding of women′s cultural backgrounds in the practice of maternity care, which requires trust and respect for other cultures. Two studies found that women and midwives valued supportive relationships, highlighting the importance of keeping this relationship non‐judgmental to facilitate its building, especially in women and midwives with different cultural beliefs (Goodwin et al., 2018 ; Oscarsson & Stevenson‐Ågren, 2020 ). Oscarsson and Stevenson‐Ågren ( 2020 ) reported that women′s health beliefs affected their child‐bearing practices, especially when they differed from midwives′ beliefs, all midwives in Oscarsson and Stevenson‐Ågren′s study were Swedish, which may have affected the results because cultural diversity can affect midwives′ perceptions and experiences. The study also did not report the cultural beliefs of immigrant women, although they were not homogenous. Furthermore, one study in the UK (Goodwin et al., 2018 ) claimed that midwives tended to negatively judge Pakistani women when they were unaware of their cultural practices and beliefs, such as shaving a newborn′s head. Unfamiliarity with women′s beliefs, priorities and expectations was a barrier to developing supportive relationships (Goodwin et al., 2018 ).
5.2.2. Family involvement
Goodwin et al. ( 2018 ) reported that family dynamics in some cultures (e.g., Pakistani) significantly influenced the relationships between maternity nurses and women. Maternity nurses and midwives explained that family members influenced some women′s decisions and the dominant family member was often the decision‐maker (Carlton et al., 2009 ; Goodwin et al., 2018 ; Oscarsson & Stevenson‐Ågren, 2020 ). Extra attention to cultural influence on building supportive relationships was considered as a facilitator (Goodwin et al., 2018 ). Conversely, one study described how some women preferred to handle the labour and birth alone and not involve their partners, preferring to handle the labour and birth alone (Bradfield, Hauck, Duggan, et al., 2019 ).
5.3. Theme 3: Organizational factors
Ten studies identified the organizational factors, such as the model of care, work‐load and resources, for developing supportive relationships with child‐bearing women. Three sub‐themes emerged: COC, time/workload and physical environment.
5.3.1. Continuity of care
Eight studies reported that (COC) facilitates developing supportive relationships with women. Healthcare model differ between countries, influencing the type and extent of COC the maternity team provides. This review included different healthcare systems in which the studies were conducted. Some studies mentioned COC in the health systems in the UK (McInnes et al., 2020 ; Menage et al., 2020 ), Australia (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a ; Davison et al., 2015 ), Sweden (Backstrom et al., 2016 ; Oscarsson & Stevenson‐Ågren, 2020 ), and NZ (Crowther & Smythe, 2016 ). Other studies have reported non‐COC in systems, in the United State of America (Carlton et al., 2009 ) and Australia (Bradfield et al., 2019b ).
Women and midwives in three qualitative studies (Backstrom et al., 2016 ; Bradfield et al., 2019b ; McInnes et al., 2020 ) reported that COC in maternity services facilitates supportive relationships and trust. Additionally, Oscarsson and Stevenson‐Ågren ( 2020 ) and Menage et al. ( 2020 ) suggested that midwives who cared for the same women throughout their pregnancies were more likely to build trusting relationships. However, midwives working in a birthing unit where COC was not practised expressed a feeling of disconnection with women (Bradfield et al., 2019b ). Women in one study (Davison et al., 2015 ) wanted COC and preferred private midwifery care because the relationship with their midwives was as supportive as they needed and they could be involved in shared decisions. This study was conducted in one location in Australia (from 2007–2013) when support for publicly funded home birth was still being developed.
5.3.2. Time and workload
The literature highlighted several work situations as barriers to supportive relationships with child‐bearing women; including lack of adequate time (Aschenbrenner et al., 2016 ; Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019b ; Carlton et al., 2009 ; Madula et al., 2018 ), heavy workloads (Aschenbrenner et al., 2016 ; Bradfield et al., 2019b ; Carlton et al., 2009 ; Menage et al., 2020 ), and staff shortages (Aschenbrenner et al., 2016 ; Carlton et al., 2009 ). Maternity nurses felt distracted by paperwork and technological interventions, such as electronic fetal monitoring and high‐risk protocols for all admitted women (Carlton et al., 2009 ). Carlton et al. ( 2009 ), Bradfield et al., 2019b and Crowther and Smythe ( 2016 ) found that midwives felt overloaded and often had to deal with staff shortages, which affected their abilities to provide care and develop relationships. Maternity nurses also reported a lack of time for developing supportive relationships with women due to their working conditions (Aschenbrenner et al., 2016 ; Carlton et al., 2009 ). Maternity nurses were challenged when they had to balance keeping electronic health records (EHRs) and women′s needs, such as electronic fetal monitoring (a part of HER), resulting in decreased time for building relationships (Aschenbrenner et al., 2016 ; Menage et al., 2020 ).
5.3.3. Physical environment
This sub‐theme refers to organizational facilitators and barriers to providing resources and support for midwives to develop supportive relationships, which midwives considered a significant challenge to staying connected with women (McInnes et al., 2020 ). For example, birthing unit design can influence how women feel. Birthing room environment s have varying levels of privacy, lighting, music or silence and hygiene facilities (Bradfield, Hauck, Duggan, et al., 2019 ). When the design matches a woman′s preferences, promotes a positive relationship between the woman and the midwife (Bradfield, Hauck, Duggan, et al., 2019 ; Menage et al., 2020 ). This can improve women′s physical and psychological comfort, enabling supportive relationships and positively affecting women′s feelings (Aschenbrenner et al., 2016 ; Bradfield, Hauck, Duggan, et al., 2019 ; Carlton et al., 2009 ; Menage et al., 2020 ).
6. DISCUSSION
This review has provided evidence on the factors related to developing supportive relationships between women and midwives. The findings indicated that midwives' relationships with child‐bearing women are critical and depend on human interaction, cultural and organizational factors. Each factor will be discussed as a facilitator or barrier to developing supportive relationships during the child‐bearing period from women′s and midwives′ perspectives.
6.1. Factors
6.1.1. human interaction.
Developing supportive relationships with child‐bearing women requires mutual trust, respect, partnerships and attitudes and effective communication skills, all of which are interrelated and facilitate relationships. Partnerships allow women to feel empowered to share decision‐making and make their own choices. They require provisions for involvement and advocacy (Bradfield, Hauck, Duggan, et al., 2019 ; Shimizu & Mori, 2018 ). Although some studies (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a , 2019b ; Davison et al., 2015 ; McInnes et al., 2020 ; Shimizu & Mori, 2018 ) identified involvement as a part of partnerships with child‐bearing women, there is insufficient information regarding the process for encouraging such involvement. Some studies focused on partnership as a maternity care approach, a foundational premise in developing supportive relationships (Bradfield et al., 2019a , 2019b ; Carlton et al., 2009 ). However, these studies did not demonstrate the steps necessary to build partnerships with women and thus, facilitate relationships. This area requires further research.
Appropriate shared decision‐making and women′s involvement were not always present in the reviewed studies (Bradfield et al., 2019a , 2019b ; Davison et al., 2015 ; Shimizu & Mori, 2018 ). Thus, there was little information about decision‐making processes, including how, when and the degree to which women were involved in decision‐making, which could be considered a barrier to building supportive relationships. Additionally, there was a lack of information about women′s understanding of empowerment, which may indicate their readiness to make their own decisions. While midwives should employ a woman‐centred care approach, empowering women to participate in joint decision‐making (Nursing and Midwifery Board of Australia, 2018), further research should clarify women′s understanding of empowerment.
Two studies reported described how midwives' or maternity nurses' attitudes, including their personalities, knowledge and experience, affected how they valued developing supportive relationships with women during childbirth (Bradfield et al., 2019a ; Carlton et al., 2009 ). Midwives need to gain women′s trust through positive attitudes and respect for their individual needs and culture.
These human interaction factors will have little success without effective communication skills, which are the basis of relationship development (Aschenbrenner et al., 2016 ; Backstrom et al., 2016 ; Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019b ; Carlton et al., 2009 ; Crowther & Smythe, 2016 ; Madula et al., 2018 ; Menage et al., 2020 ; Oscarsson & Stevenson‐Ågren, 2020 ). Positive communication between healthcare professionals and women facilitates trust, respect and support (Backstrom et al., 2016 ). Therapeutic communication should be supported and practised more often to meet women′s needs and facilitate relationship development (Fenton & Jones, 2015 ; World Health Organization, 2019 ).
6.1.2. Culture
The reviewed studies suggested some cultural factors, such as women′s health beliefs (Carlton et al., 2009 ; Goodwin et al., 2018 ), and family involvement (Oscarsson & Stevenson‐Ågren, 2020 ) that might inhibit the effective communication needed to support the connection between women and midwives. For example, some studies found women had a different view from that of midwives—while midwives often viewed the control of family members as a negatively dominant influence, some women viewed that as a kind of support (Goodwin et al., 2018 ). Such a situation requires that midwives understand cultural influences to maintain supportive relationships in a preferred way.
Further, women from different cultures might present with varying health demands (Tehsin et al., 2018 ), and the cultural barriers can affect supportive relationships. Understanding women′s beliefs and culture can help midwives understand the reasons behind health practices, promote acceptance and facilitate supportive relationships. Therefore, assessing women′s expectations of maternity care can benefit relationship development.
However, the relevant literature included of 14 articles published over the last 10 years, from seven countries, with primarily Western cultures. Few studies focused on cultural factors that affect how supportive relationships develop, indicating a substantial gap in the literature. Country‐specific studies are needed to explore cultural differences, views, expectations and health practices relevant to building relationships with child‐bearing women.
6.1.3. Organization
This review indicates that COC is crucial to meeting women′s. Findings demonstrated that women and midwives prefer to know each other before child birth, preferably meeting during the antenatal period (Bradfield et al., 2019a ), so their care can be continuous throughout the child‐bearing period (McInnes et al., 2020 ). The familiarity between women and midwives has helped midwives understand women′s needs and identify changes in health statuses throughout their visits. Simultaneously, it has helped women feel more comfortable with their midwives and develop trusting and positive relationships (McInnes et al., 2020 ). This finding was supported by recent Cochrane reviews, which established COC as the gold standard for midwifery care and suggested it should be practised much more widely (Homer et al., 2019 ; Sandall et al., 2016 ). However, further studies should address how supportive relationships are enabled within maternity care environments with a non‐COC model.
Findings have shown that midwives and maternity nurses are distracted by workloads due to documentation and technology interventions (Aschenbrenner et al., 2016 ). Developing a successful relationship requires a balance between all support aspects. Therefore, midwives desire enough time to build trust, respect and partnerships with women, particularly those from different cultures. They need extra time before, during and after meeting women to manage their increased workload (Kerr et al., 2014 ). One strategy for managing this challenge is more efficient documentation methods that enable more time and effort strengthening relationships with women (Kent & Morrow, 2014 ). Although the EHR might prompt workflows, several issues have been noted, such as ineffective time management and unexpected deficiencies in patient care and work flow (Abbey et al., 2012 ; Baumann et al., 2018 ). Thus, the effect of EHR on midwives' time needs more attention, suggesting staff training and EHR system modifications to increase the time available for women′s care (Coleman et al., 2021 ; Karp et al., 2019 ).
6.2. Strengths and limitations
This review integrated qualitative and quantitative studies to produce a holistic understanding of developing supportive relationships with child‐bearing women. However, it excluded non‐English and non‐Arabic studies, therefore, relevant data may have been omitted.
6.3. Recommendations
Future research should develop strategies to facilitate supportive relationships, particularly in non‐COC models. This review recommends that strengthening midwives' communication skills is essential. Future research should focus on how midwives share decision‐making power with women throughout the child‐bearing period, which is an important component of supportive relationships. Organizational support is a major factor affecting supportive relationships, and COC models are highly recommended. Further investigations should also address the effect cultural identity on relationship development and how women and midwives manage cultural differences.
7. CONCLUSION
This review highlighted that supportive relationships require therapeutic communication, trust, respect, partnership and shared decision‐making. Developing supportive relationships with women is easier in COC models of maternity care. However, little is known about developing and maintaining supportive relationships in non‐COC models. Further, working with women from different cultural backgrounds can affect developments, with additional considerations required to ensure women feel supported. However, it is unclear how supportive relationships are enabled within maternity care environments with differing cultural identity factors, demonstrating the need for further research.
7.1. Relevance to clinical trial
This study aimed to contribute substantially to evidence‐based decisions about the organizational barriers to building supportive relationships. These findings could be used to review or develop nursing and midwifery education curricula, guidelines and policies to enhance the knowledge, skills and practices used to build supportive relationships with child‐bearing women. Further, birthing outcomes can be improved, reducing health costs and increasing patient satisfaction. The importance of individualized care must be emphasized through the appropriate development of supportive relationships. This, will help midwives and maternity nurses understand and value women′s needs and ensure they have adequate time to build supportive relationships with women, provide woman‐centred care and ultimately improve women′s experiences during the child‐bearing period.
This review highlighted the importance of women′s involvement. Effective supportive relationships between child‐bearing women and midwives, increase women′s involvement and autonomy in caring for themselves and their infants in postpartum and during early childhood. Thus, there is a need to improve midwives′ skills concerning why, what and how to begin women′s involvement, suggesting that reflective supervision methods during home visiting could help maintain boundaries, observe one′s reactions and improving involvement (Tomlin et al., 2016 ).
Continuity of care focuses on building supportive relationships with women, which requires supportive leadership, and enables midwives to stay connected with maternity team (McInnes et al., 2020 ). Thus, further research is needed to examine relationships between all organizational levels in the maternity care. Additionally, there are few details on the strategies midwives and maternity nurses use to build these relationships. Thus, further research should address midwives' and maternity nurses' priorities and the actual time required to develop supportive relationships with child‐bearing women.
AUTHOR CONTRIBUTIONS
All the authors agreed and had a primary contribution to the following: conception and design, data appraisal, extraction, analysis, and reporting of findings. They affirmed their approval of the final version to be published.
FUNDING INFORMATION
This work was completed as a part of PhD research project at The University of Newcastle, University Drive, Callaghan, New South Wales 2308, Australia. Grant number HREC H‐2021‐0217. PhD candidate Hadeer Almorbaty has held a scholarship awarded by Prince Sultan Military College of Health Sciences, Medical Services Division, Armed Forces, Ministry of Defence, Kingdom of Saudi Arabia, for her PhD study at the University of Newcastle, Australia. There are no other funding sources for this project.
CONFLICT OF INTEREST
The authors have declared no conflict of interest.
ACKNOWLEDGEMENTS
We thank Debbie Booth, Senior Research Librarian (The University of Newcastle) for guidance in the literature search.
Almorbaty, H. , Ebert, L. , Dowse, E. , & Chan, S.‐C. (2023). An integrative review of supportive relationships between child‐bearing women and midwives . Nursing Open , 10 , 1327–1339. 10.1002/nop2.1447 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
DATA AVAILABILITY STATEMENT
- Abbey, M. , Chaboyer, W. , & Mitchell, M. (2012). Understanding the work of intensive care nurses: A time and motion study . Australia Critical Care , 25 ( 1 ), 13–22. [ PubMed ] [ Google Scholar ]
- Agostini, F. , Neri, E. , Salvatori, P. , Dellabartola, S. , Bozicevic, L. , & Monti, F. (2015). Antenatal depressive symptoms associated with specific life events and sources of social support among Italian women . Maternal and Child Health Journal , 19 ( 5 ), 1131–1141. 10.1007/s10995-014-1613-x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aschenbrenner, A. , Hanson, L. , Johnson, T. , & Kelber, S. (2016). Nurses' Own Birth Experiences influence Labor Support attitudes and behaviors . Journal of Obstetric, Gynecologic, & Neonatal Nursing , 45 ( 4 ), 491–501. 10.1016/j.jogn.2016.02.014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Backstrom, C. , Martensson, L. , Golsater, M. , & Thorstensson, S. (2016). "It′s like a puzzle": Pregnant women's perceptions of professional support in midwifery care . Women and Birth , 29 ( 6 ), e110–e118. 10.1016/j.wombi.2016.04.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baumann, L. A. , Baker, J. , & Elshaug, A. G. (2018). The impact of electronic health record system on clinical documentation times: A systematic review . Health Policy , 122 ( 8 ), 827–836. [ PubMed ] [ Google Scholar ]
- Bradfield, Z. , Hauck, Y. , Duggan, R. , & Kelly, M. (2019). Midwives' perceptions of being ‘With Woman’: A phenomenological study . BMC Pregnancy & Childbirth , 19 ( 1 ), 787–792. 10.1186/s12884-019-2548-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradfield, Z. , Hauck, Y. , Kelly, M. , & Duggan, R. (2019a). "It's what midwifery is all about": Western Australian midwives’ experiences of being ‘With Woman’ during labour and birth in the known midwife model . BMC Pregnancy & Childbirth , 19 ( 1 ), 29. 10.1186/s12884-018-2144-z [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradfield, Z. , Hauck, Y. , Kelly, M. , & Duggan, R. (2019b). Urgency to build a connection: Midwives' experiences of being ‘With Woman’ in a model where midwives are unknown . Midwifery , 69 , 150–157. 10.1016/j.midw.2018.11.014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradfield, Z. , Kelly, N. , Hauck, Y. , & Duggan, R. (2019d). Midwives ‘with Woman’ in the private obstetric model: Where divergent philosophies meet . Women & Birth , 32 ( 2 ), 157–167. [ PubMed ] [ Google Scholar ]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology . Qualitative research in psychology , 3 ( 2 ), 77–101. 10.1191/1478088706qp063oa [ CrossRef ] [ Google Scholar ]
- Buckley, S. (2015). Executive summary of hormonal physiology of childbearing: Evidence and implications for women, babies, and maternity care . The Journal of Perinatal Education , 24 ( 3 ), 145–153. 10.1891/1058-1243.24.3.145 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carlton, T. , Callister, L. , Christiaens, G. , & Walker, D. (2009). Labor and delivery nurses' perceptions of caring for childbearing women in nurse‐managed birthing units . MCN. The American Journal of Maternal/Child Nursing , 34 ( 1 ), 50–56. 10.1097/01.NMC.0000343866.95108.fa [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coleman, C. , Gotz, D. , Eaker, S. , James, E. , Bice, T. , Carson, S. , & Khairat, S. (2021). Analysing EHR navigation patterns and digital workflows among physicians during ICU pre‐rounds . Health Information Management Journal , 50 ( 3 ), 107–117. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crowther, S. , & Smythe, E. (2016). Open, trusting relationships underpin safety in rural maternity a hermeneutic phenomenology study . BMC Pregnancy & Childbirth , 16 , 370. 10.1186/s12884-016-1164-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davison, C. , Hauck, Y. , Bayes, S. , Kuliukas, L. , & Wood, J. (2015). The relationship is everything: Women′s reasons for choosing a privately practising midwife in Western Australia . Midwifery , 31 ( 8 ), 772–778. 10.1016/j.midw.2015.04.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fenton, C. , & Jones, L. K. (2015). Achieving cultural safety in Australian indigenous maternity care . International Journal of Health Sciences , 3 ( 1 ), 23–38. 10.15640/ijhs.v3n1a2 [ CrossRef ] [ Google Scholar ]
- Goodwin, L. , Hunter, B. , & Jones, A. (2018). The midwife‐woman relationship in a South Wales community: Experiences of midwives and migrant Pakistani women in early pregnancy . Health Expectations , 21 ( 1 ), 347–357. 10.1111/hex.12629 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Homer, C. S. (2016). Models of maternity care for midwifery continuity of care . Medical Journal of Australia , 205 ( 8 ), 370–374. [ PubMed ] [ Google Scholar ]
- Homer, C. , Brodie, P. , Sandall, J. , & Leap, N. (2019). Midwifery continuity of care: A practical guide . Elsevier Health Sciences. https://books.google.com.sa/books?id=kPaKDwAAQBAJ&lpg=PP1&pg=PP1#v=onepage&q&f=false [ Google Scholar ]
- Hong, Q. N. , Fàbregues, S. , Bartlett, G. , Boardman, F. , Cargo, M. , Dagenais, P. , Gagnon, M.‐P. , Griffiths, F. , Nicolau, B. , & O′Cathain, A. (2018). The mixed methods appraisal tool (MMAT) version 2018 for information pessionals and researchers . Education for Information , 34 ( 4 ), 285–291. 10.3233/EFI-180221 [ CrossRef ] [ Google Scholar ]
- Karp, E. L. , Freeman, R. , Simpson, K. N. , & Simpson, A. N. (2019). Changes in efficiency and quality of nursing electronic health record documentaion after implementaion of an adnission patient history essential data set . CIN: Computers, Informatics, Nursing , 37 ( 5 ), 260–265. [ PubMed ] [ Google Scholar ]
- Kent, P. , & Morrow, K. (2014). Better documentation improves patient care . Nursing Standard , 29 ( 14 ), 44–51. 10.7748/ns.29.14.44.e9267 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kerr, D. , Lu, S. , & McKinlay, L. (2014). Towards patient‐centred care: Perspectives of nurses and midwives regarding shift‐to‐shift bedside Handover . International Journal of Nursing Practice , 20 ( 3 ), 250–257. 10.1111/ijn.12138 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Madula, P. , Kalembo, F. W. , Yu, H. , & Kaminga, A. C. (2018). Healthcare provider‐patient communication: A qualitative study of women's perceptions during childbirth . Reproductive Health , 15 ( 1 ), 135. 10.1186/s12978-018-0580-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McInnes, R. J. , Aitken‐Arbuckle, A. , Lake, S. , Martin, C. H. , & MacArthur, J. (2020). Implementing continuity of midwife Carer – Just a friendly face? A realist evaluation . BMC Health Services Research , 20 ( 1 ), 1–15. 10.1186/s12913-020-05159-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Menage, D. , Bailey, E. , Lees, S. , & Coad, J. (2020). Women's lived experience of compassionate midwifery: Human and professional . Midwifery , 85 , 102662. 10.1016/j.midw.2020.102662 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. G. , & Group, P. (2009). Reprint—Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement . Physical Therapy , 89 ( 9 ), 873–880. 10.1093/ptj/89.9.873 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oscarsson, M. G. , & Stevenson‐Ågren, J. (2020). Midwives experiences of caring for immigrant women at antenatal care . Sexual & Reproductive Healthcare , 24 , 100505. 10.1016/j.srhc.2020.100505 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qi, A. M. , & Creedy, D. K. (2009). Central concepts in the midwife‐woman relationship in hospital and community settings . JBI Database of Systematic Reviews and Implementation Reports , 7 ( 34 ), 1–18. 10.11124/jbisrir-2009-587 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sandall, J. , Soltani, H. , Gates, S. , Shennan, A. , & Devane, D. (2016). Midwife‐led continuity models versus other models of care for childbearing women . Cochrane Database of Systematic Reviews(4) , 2016 , CD004667. 10.1002/14651858.CD004667.pub5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sehhatie, F. , Najjarzadeh, M. , Zamanzadeh, V. , & Seyyedrasooli, A. (2014). The effect of midwifery continuing care on childbirth outcomes . Iranian Journal of Nursing and Midwifery Research , 19 ( 3 ), 233–237. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shimizu, A. , & Mori, A. (2018). Maternal perceptions of family‐centred support and their associations with the mother‐nurse relationship in the neonatal intensive care unit . Journal of Clinical Nursing , 27 ( 7–8 ), e1589–e1599. 10.1111/jocn.14243 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tehsin, F. , Mohammed, A. O. , Lassoued, L. , Ali, S. I. , & al‐Kishi, A. M. (2018). Parturient satisfaction with intrapartum and postpartum care in a maternity referral hospital at Al Ahsa, Saudi Arabia . Journal of the Society of Obstetrics and Gynaecologists of Pakistan , 8 ( 3 ), 169–175. https://jsogp.net/index.php/jsogp/article/view/181/119 [ Google Scholar ]
- Torraco, R. J. (2016). Writing integrative literature reviews: Using the past and present to explore the future . Human Resource Development Review , 15 ( 4 ), 404–428. 10.1177/2F1534484316671606 [ CrossRef ] [ Google Scholar ]
- Tomlin, A. M. , Hines, E. , & Sturm, L. (2016). Relection in home visiting: The what, why, and a beginning step toward how . Infant Mental Health Journal , 37 ( 6 ), 617–627. [ PubMed ] [ Google Scholar ]
- Tracy, S. K. , Welsh, A. , Hall, B. , Hartz, D. , Lainchbury, A. , Bisits, A. , White, J. , & Tracy, M. B. (2014). Caseload midwifery compared to standard or private obstetric care for first time mothers in a ppublic teaching hospital in Australia: Across sectional study of cost and birth outcomes . BMC Pregnancy and Childbirth , 14 ( 1 ), 1–9. 10.1186/1471-2393-14-46 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Whittemore, R. , & Knafl, K. (2005). The integrative review: Updated methodology . Journal of Advanced Nursing , 52 ( 5 ), 546–553. 10.1111/j.1365-2648.2005.03621.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization . (2016). WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience . World Health Organization. https://www.who.int/publications/i/item/9789241549912 [ PubMed ] [ Google Scholar ]
- World Health Organization . (2019). Strengthening quality midwifery education for Universal Health Coverage 2030: Framework for action . World Health Organization. https://www.who.int/publications/i/item/9789241515849 [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
With the decrease in labor and birth interventions associated with. midwifery-led care, there is a strong possibility of reductions in health care costs. midwifery-led model of care. We use a global perspective of midwifery in this literature review to highlight the bene ts of a midwifery-led care model that enhances.
Midwives' practice of maternal positions throughout active second stage labour: an integrative review. An integrative review was considered suitable for this study, as this methodology allows inclusion of data from all types of literature to fully answer review questions (Whittemore and Knafl, 2005;...
This systematic review includes a comprehensive literature search of published scientific articles, in the English language, from January 1, 2000 to July 30, 2022, using the electronic databases which were deemed most relevant for the topics; CINAHL, EMBASE, and PubMed. ... One finding from the systematic review was that midwifery-led care ...
Midwifery is a research‐informed profession. However, a gap persists in the translation of best available evidence into practice settings, compromising gold standard maternity care and delaying the translation of new knowledge into everyday practice. ... Data abstraction from the literature included in this review was guided by the approach ...
A literature review to determine midwifery students' perceived essential qualities of preceptors to increase confidence and competence in the clinical environment Women Birth. 2022 May;35 ... As up to 50% of the midwifery program is taught in the clinical environment, an analysis of the preceptorship role in the context of midwifery student ...
A Literature Review of Midwifery-Led Care in Reducing Labor and Birth Interventions. 2018 Oct;22 (5):387-400. doi: 10.1016/j.nwh.2018.07.002. Epub 2018 Sep 6. Certified nurse-midwives are usually recognized as independently practicing advanced practice registered nurses because they provide maternity care to pregnant women in various states.
Certified nurse-midwives are usually recognized as independently practicing advanced practice registered nurses because they provide maternity care to pregnant women in various states. In the United States, certified nurse-midwives are historically underused. Culture favors physician-led care, with 90% of all births attended by physicians. Midwifery-led care is considered high-touch/low ...
Early assumptions from this literature review, lead us to recommend a reframing of midwifery care in terms of women's access to continuity of midwifery care models, improved education and training for midwives on facilitating IDM, and a consultation process with midwives when policy-makers introduce guidelines or recommendations that influence IDM.
This review aimed to examine the existing literature for insights, suggestions and knowledge gaps surrounding midwives' experiences of facilitating IDM, and provide meaningful recommendations for improvements in midwifery education, research, policy and practice, which benefit women, their families and midwives alike.
The Preferred Reporting Items of Systematic reviews Meta-Analyses (PRISMA) guidelines was adhered to when conducting this review [].A systematic search strategy was formulated and definitive search terms used relative to key public health topics within midwifery following consultation with Expert Advisory Group members and Midwifery 2020 Public Health Work Stream members.
There is an apparent push, in midwifery academia, toward systematic-styled literature reviews, even for those reviews foregrounding a qualitative research project. Commonly now, midwifery postgraduate students and researchers are persuaded that a "systematic-styled review" is the only (authoritative) kind of literature review that can be ...
Midwifery workplace culture in Australia: A national survey of midwives. 2020: Quantitative: 10.1016/j.wombi.2019.09.008: ... Although there are no equivalent reports to compare the findings from this review, literature is vast in explaining the impact of workplaces and working conditions on workers' health [88].
Using a scoping review framework, we searched electronic and grey literature databases for reports in any language between January 2012 and January 2022, which described current and recent trials, implementation or scaling-up of midwifery continuity of care studies or initiatives in high-, middle- and low-income countries.
A review of the literature. Midwifery. 2016;33:12-23. Article PubMed Google Scholar Colvin CJ, de Heer J, Winterton L, Mellenkamp M, Glenton C, Noyes J, et al. A systematic review of qualitative evidence on barriers and facilitators to the implementation of task-shifting in midwifery services.
ademia, toward systematic-styled literature reviews, even for those reviews foregrounding a qualitative research project. Commonly now, midwifery postgraduate students and researchers are persuaded that a "systematic-styled review" is the only (authoritative) kind of literature re-view that can be accomplished (or published). Coming to
This review intends to evaluate the literature on (1) introducing midwives in low- and middle-income countries, and (2) on mentoring as a facilitator to enable midwives and those in midwifery roles to improve sexual, reproductive, maternal, newborn and adolescent health service quality within health systems.
This review followed the recommendations of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) checklist (Moher et al, 2009), the Critical Appraisal Skills Program (2018) checklists and a series of articles outlining the step-by-step approach to conducting systematic reviews published by the Joanna Briggs Institute (Aromastaris and Pearson, 2014; Aromastaris and ...
Systematic reviews in midwifery. RCM Midwives2006 May;9 (5):186-8. This paper highlights the key steps to follow when conducting a systematic review (see Box 2). Healthcare practitioners may be limited by time and resources when conducting literature reviews, however, a systematic and transparent approach should be adopted wherever possible.
The aim of this scoping review is to synthesise and map what is reported in the international literature on the advanced scope of midwifery practice. This review has highlighted the many ways in which midwifery scope of practice has been framed and regulated globally, how the ICM competencies are interpreted and implemented, and the lack of ...
There is an apparent push, in midwifery academia, toward systematic‐styled literature reviews, even for those reviews foregrounding a qualitative research project. Commonly now, midwifery postgraduate students and researchers are persuaded that a "systematic‐styled review" is the only (authoritative) kind of literature review that can ...
COC is a model of midwifery care where the woman receives COC from a known midwife or known midwifery team throughout the child‐bearing period, ... Writing integrative literature reviews: Using the past and present to explore the future. Human Resource Development Review, 15 (4), 404-428. 10.1177/2F1534484316671606 ...
The major findings. synthesised from this review, are that; 1) midwifery decision-making in during birth is. socially negotiated involving hierarchies of sur veillance and control; 2) the role of ...
Findings. Decision-making is under-researched in midwifery and more specifically birth, as only 4 research articles met the inclusion criteria in this review. Three of the studies involved qualified midwives, and one involved student midwives. Two studies were undertaken in England, one in Scotland and one in Sweden.