- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Public Policy
- Public Administration
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

Vitamin A Deficiency: Health, Survival, and Vision
- Cite Icon Cite
- Permissions Icon Permissions
Many studies over the past decade and a half have indicated that vitamin A status is an important determinant of health. The World Bank now estimates that vitamin A intervention programs are some of the most cost-effective health strategies globally. This new book, written by leading investigators in the field, is the first to synthesize the many important studies to date. The authors identify and quantify the biological, clinical and public health impact of vitamin A deficiency on childhood growth, mortality and morbidity, including anemia and blindness. They deal with the epidemiologic and biological basis of these findings, and with the prevention and treatment of these disorders, particularly of measles, diarrhea and xeorophthalmia. Alternative approaches to identifying individuals and populations in need of intervention, alternative strategies for improving vitamin A and carotenoids, and the relationship between vitamin A and immunity are discussed. This comprehensive volume on a critically important and widespread nutritional deficiency will serve as a unique resource for nutritionists, physicians, public health workers and policy makers, and will be especially relevant to clinicians and researchers in international health.
Signed in as
Institutional accounts.
- GoogleCrawler [DO NOT DELETE]
- Google Scholar Indexing
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 12 September 2013
Review of the safety and efficacy of vitamin A supplementation in the treatment of children with severe acute malnutrition
- Lora L Iannotti 1 ,
- Indi Trehan 1 , 2 , 3 &
- Mark J Manary 1 , 2 , 4 , 5
Nutrition Journal volume 12 , Article number: 125 ( 2013 ) Cite this article
16k Accesses
9 Citations
6 Altmetric
Metrics details
World Health Organization (WHO) guidelines recommend for children with severe acute malnutrition (SAM), high-dose vitamin A (VA) supplements be given on day 1 of admission, and on days 2 and 14 in the case of clinical signs of vitamin A deficiency (VAD). Daily low-dose VA follows, delivered in a premix added to F-75 and F-100. This study aimed to systematically review the evidence for safety and effectiveness of high-dose VA supplementation (VAS) in treatment of children with SAM.
A comprehensive literature review was undertaken for all relevant randomized controlled trials (RCT) and observational studies from 1950 to 2012. Studies identified for full review were evaluated using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) methodology using a set of pre-defined criteria: indirectness; inconsistency; imprecision; and study limitations. A quality rating of high, moderate, or low was then assigned to each study, and only those attaining moderate to high were considered in making recommendations.
Of the 2072 abstracts screened, 38 met criteria for full review, and 20 were rated moderate to high quality. Only one study replicated the WHO VA protocol in children with SAM. Indirectness was a critical limitation, as studies were not exclusive to children with SAM. There was inconsistency across trials for definitions of malnutrition, morbidities, and ages studied; and imprecision arising from sub-group analyses and small sample sizes. Evidence showed improved outcomes associated with low-dose compared to high-dose VAS, except in cases presenting with signs of VAD, measles, and severe diarrhea or shigellosis. Adverse outcomes related to respiratory infection, diarrhea, and growth were associated with high-dose VAS in children who were predominantly adequately nourished. No adverse effects of the high dose were found in children with SAM in the trial that replicated the WHO VA guideline.
This is the first systematic review of the safety and efficacy of high-dose VAS in treatment of SAM. We recommend a low-dose VAS regimen for children with SAM, except in cases presenting with measles, severe diarrhea (shigellosis), and any indication of VAD. Further research is needed in exclusively malnourished children and to explore alternate delivery strategies.
Peer Review reports
Globally, vitamin A deficiency (VAD) affects 100–140 million children, 4.4 million of whom have xerophthalmia [ 1 , 2 ]. Coverage rates for full vitamin A supplementation (VAS) of children 6–59 months delivered through primary care have risen significantly over the last decade, reaching 88% for the least developed countries [ 3 ]. In recent years, alternative strategies to improve micronutrient nutrition have been increasingly applied for high-risk populations already supplemented with vitamin A (VA): micronutrient powders; fortification of staple foods; ready-to-use supplemental and therapeutic foods (RUSF and RUTF); and other food-based approaches.
Among the populations particularly vulnerable to VAD are children with severe acute malnutrition (SAM) [ 4 ]. The World Health Organization (WHO) currently recommends that for inpatient care of children with SAM, VA supplements be given on day 1 of admission unless there is clear evidence that VA was received in the last month [ 5 ]. Dosing guidelines are the following: 200,000 international units (IU) for children over 12 months of age, 100,000 IU for children 6–12 months, and 50,000 IU for children below 6 months. If clinical signs of vitamin A deficiency are present, then another age-specific, large dose is administered on day 2 and again, on day 14 [ 4 , 5 ]. Low-dose VA is then given as part of a vitamin mix added to F-75 or F-100 therapeutic milk formulations, or alternatively, as a proprietary multivitamin supplement or combined mineral-vitamin mix (CMV). There is a need to revisit these guidelines in the context of improved VA availability, but also in view of evidence showing the potential for harmful effects of such VAS dosages [ 6 ].
This systematic review aimed to assess the safety and effectiveness of VAS in children with SAM, with regards to mortality, nutritional recovery, and signs of symptomatic VAD [ 7 ]. A literature review was undertaken to search for all randomized controlled trials (RCT) and observational studies published from 1950 to March 2012. Databases searched included MEDLINE, EMBASE, and Google Scholar. The clinical trial registries at clinicaltrials.gov, pactr.org, and apps.who.int/trialsearch were also searched. Initial key words for the searches included “malnutrition”, “severe malnutrition”, “kwashiorkor”, “marasmus”, “vitamin A”, and “retinol”. A number of outcome measures were sought, including mortality, weight gain, nutritional recovery, and VAD. Further terms were added iteratively to the search based on results obtained from the initial searches.
Searches were also conducted to identify relevant publications and study documents produced by international health organizations such as the WHO and UNICEF. The titles and abstracts were scanned to identify relevant studies. The full text of relevant studies was obtained and the list of articles for inclusion further optimized based on an evaluation of the full text. Reference lists in relevant articles were also scanned manually and electronically to identify other studies that may have been missed in the original searches. Relevant publications that cited those previously identified articles were similarly sought.
Studies were included for full review based on relevance to the population of interest, study interventions, study design, outcome measures, and an assessment of the study’s methodological rigor and quality. These studies were then assessed and entered into a Grading of Recommendations, Assessment, Development and Evaluation (GRADE) table summarizing design, aim, outcomes, GRADE criteria assessment (indirectness, inconsistency, imprecision, and study limitations), and quality ranking (high, moderate, or low) [ 8 ].
Indirectness was judged based on study relevance to the review question in terms of the study population (children with SAM), intervention of interest (VAS), and outcome measures (mortality, recovery from SAM, signs of symptomatic VAD, and adverse outcomes due to supplementation) [ 9 ]. Consideration was given under this category to VA dosing relative the WHO protocol. Inconsistency was assessed by comparing point estimates and examining the heterogeneity of methods and statistical analyses [ 10 ]. Imprecision was based primarily on the 95% confidence interval with consideration of effect and sample sizes [ 11 ]. Potential biases (selection, recall, information/observation, misclassification) arising from failure to blind, losses in follow-up, inappropriate controls, and failure to adjust for confounding factors, among other problems, were considered under the study limitations (risk of bias) criteria [ 12 ].
Once these criteria were assessed, each study was assigned a quality ranking ranging from low to high. Only those studies with some degree of moderate or high ( i.e. , low-moderate, moderate, moderate-high, or high) quality ranking were included in this review for consideration in making recommendations on the use of VAS for the treatment of children with SAM.
Of the 2072 abstracts identified and screened, 38 were selected for full review (Figure 1 ). Twenty-two were of moderate- to high-quality, and were grouped into 3 categories and listed primary outcomes assessed: 1) previous reviews; 2) observational studies; and 3) randomized controlled trials (RCT).
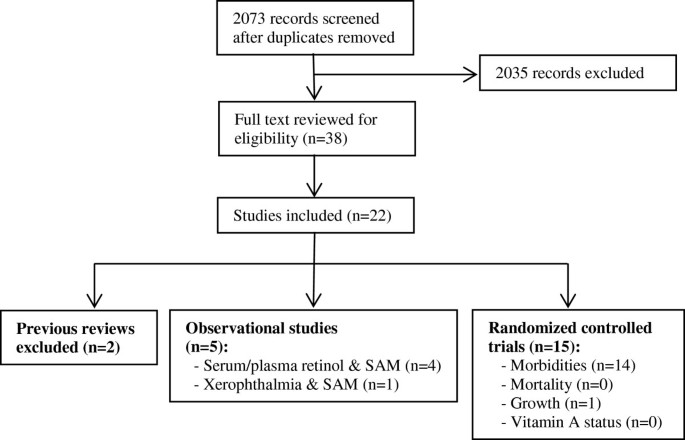
Flow diagram for studies included in review. The figure presents a flow diagram detailing the number of records screened and excluded, full-text articles reviewed, and ultimately, the number of studies included in the systematic review. The included observational and RCT studies are enumerated according to the primary outcome examined.
Previous reviews
Two previous reviews of VAS trials were identified; both considered malnourished children together with those not malnourished [ 7 , 13 ]. Preventive VAS reduced all-cause mortality by 25% and diarrhea-specific mortality by 30%. VA showed greater protection against morbidity and mortality in Asia than in Africa or Latin America [ 13 ]. An earlier review found that the severity of measles and diarrheal infections were reduced by VAS, but the risk of lower respiratory tract infection was increased in some trials [ 7 ]. Because the reviews did not provide new evidence for VA and management of SAM and all studies from the reviews were screened for this review, they were not included in the GRADE assessment.
Observational studies
Five observational studies were identified and assigned a GRADE quality ranking of low to moderate [ 14 – 18 ] (Additional file 1 : Table S1). These studies found significant associations between serum or plasma retinol concentrations and SAM [ 14 – 16 ]. Others established a link between VAD, SAM, and diarrhea. In Bangladesh, reduced serum retinol concentrations were associated with shigellosis and low weight-for-age Z-score [ 18 ]. Another case–control study in Bangladesh showed that the duration of diarrhea and SAM were independently associated with xerophthalmia [ 17 ].
Randomized controlled trials
Fifteen RCTs of moderate to high quality based on GRADE criteria were included in the systematic review on the safety and efficacy of high-dose VAS in children with SAM (Table 1 ). Issues of indirectness were present in all trials. Only one trial included children with SAM exclusively [ 19 ]. The remaining 14 included non-malnourished and malnourished children [ 20 – 33 ]. VA dosing also varied; only five trials administered the recommended high-dose on day 1 [ 19 , 26 , 30 , 31 , 33 ], while the remaining administered VA doses in varying quantities and forms. Only one trial followed the WHO protocol [ 19 ]; two compared high dose with daily low dose [ 26 , 33 ], and the remaining 12 compared high dose VAS with placebo [ 20 – 25 , 27 – 32 ].
Inconsistency across trials was observed with regards to the ages of children studied, ranging from birth to 14 years. Definitions of morbidity and malnutrition varied, as well as use of differing growth references and standards. Small sample sizes and rare events were the most common problems related to imprecision . Despite randomization, several studies also showed significant differences in baseline characteristics that elevated the risk of bias . Notably, these included baseline age and nutritional status differences with higher likelihoods of confounding [ 28 , 32 , 33 ].
Some key findings were identified across trials. First, low-dose VAS conferred more or similar health and recovery advantages when compared to high-dose supplementation in the treatment of malnourished children [ 19 , 26 , 33 ]. Second, high-dose VAS showed mixed results relative to placebo for infectious disease outcomes in children with and without SAM, showing benefit in some trials for children with severe diarrhea or shigellosis [ 27 , 31 ], measles [ 21 , 22 ], other acute respiratory infections [ 30 ], and undifferentiated fever [ 24 ]. However, in other trials, there was no benefit for children with acute respiratory infections or diarrhea [ 24 – 26 , 29 , 32 ]. There was also some evidence of improved growth outcomes associated with high-dose VAS among VA deficient children [ 20 ] and children with measles [ 22 ].
Finally, adverse effects were found to be associated with high-dose VAS in some trials, including an increased rate of respiratory illnesses [ 23 , 28 ] and diarrhea [ 26 , 31 ]. These findings appear primarily in samples or sub-samples of adequately nourished children. As noted previously, we identified only one RCT that included only severely malnourished children [ 19 ]. Some explicitly excluded children with marasmus, kwashiorkor, or all children with SAM [ 25 , 27 , 30 , 32 ], while the remaining included both malnourished and adequately nourished children. Among the five studies finding adverse events in association with VAS, two of these studies carried out sub-group analyses showing an increased risk of diarrhea among normally nourished children [ 31 ] and among children without edema [ 26 ]. One trial included only adequately nourished children [ 28 ], another found increased risk of ALRI in mainly adequately nourished children [ 23 ], and one included both malnourished and adequately nourished children, excluding children with SAM [ 32 ]. No adverse effects of the high-dose VAS were found in children with SAM in the trial that replicated the WHO VA guidelines [ 19 ].
Our systematic review of the literature using the GRADE methodology revealed only limited evidence that directly addresses the safety and effectiveness of high-dose VAS for children with SAM. Fourteen of the 15 RCTs identified for this review included both malnourished and non-malnourished children, thereby complicating the extrapolation of findings directly to efficacy and safety of VAS for SAM. There is sufficient evidence to recommend the use of high-dose VAS for children with SAM when presenting with measles, severe diarrhea (shigellosis), or evidence of VAD. The low-dose VAS regimen should be considered as the preferred protocol in other cases of malnourished children, given the potential for adverse events and similar recovery outcomes when compared to high-dose VAS. Higher quality prospective studies are still needed to directly examine VAD in children with SAM, applying more contemporary definitions of morbidity and malnutrition, and powered sufficiently to detect the critical outcomes of interest.
Observational studies demonstrated an association between SAM and VAD, but metabolic disruptions in SAM might preclude accurate measures of true VA status. Blood biomarkers of retinol concentrations were primarily used to indicate VA status [ 14 – 16 , 18 ]. Protein-energy malnutrition has been associated with reduced hepatic synthesis of retinol binding protein (RBP) and transthyretin used to transport VA in the body [ 34 , 35 ]. Thus, VA stores in the liver may not be mobilized appropriately in malnourished children and therefore not be reflected in blood biomarkers. Mitra showed that VA status improved from baseline to hospital discharge, even without VAS [ 18 ]. That study also showed that while urinary losses of retinol were associated with low retinol concentrations in children with dysentery, other inflammatory markers such as body temperature and serum α-1-acid glycoprotein and C reactive protein concentrations were more highly and negatively correlated with vitamin A status.
There is some evidence that diarrhea could be mediating this relationship, as revealed by independent associations between diarrhea, low WAZ, and VA levels [ 17 ]. Shigellosis , in particular, increases the risk of VAD [ 18 ]. A study in Brazil showed a possible interaction between SAM and low serum retinol concentrations for higher diarrheal morbidities [ 15 ]. Evidence from RCTs also finds that high-dose VAS may be beneficial for treating severely malnourished children in cases of severe diarrhea [ 27 , 31 ]. Again, the mechanism by which VA may be operating to mitigate severe diarrhea in SAM has not been elucidated, but it may be either through the repair of the gut epithelium or immune pathways that restore balance between T-cell subsets [ 36 ].
Two studies showed unequivocally the benefit of lose-dose (5000 IU daily until discharge) compared to a single high-dose (200,000 IU for children over 12 months or 100,000 IU for children under 12 months on day 1 of hospitalization) VAS regimen [ 26 , 33 ]. The low-dose regimen was more strongly correlated with lower incidence and shorter duration of respiratory disease [ 33 ] and a lower incidence of severe diarrhea [ 26 ]. A third study in Bangladesh also examined the administration of a lose-dose protocol in relation to a high-dose on day 1 followed by daily low doses until hospital discharge. [ 19 ]. That study did not find any differences in the two groups on a range of morbidity and nutrition recovery outcomes and adverse events. All children at baseline had diarrhea and while clinical signs of VAD were not apparent, baseline measures of VA status did indicate VAD in the sample. With regards to other morbidities, high-dose VAS was effective in reducing measles-specific respiratory illness [ 21 , 22 ], but showed mixed results with regards to non-measles pneumonia and other acute lower respiratory tract infections in children with SAM [ 23 – 25 , 28 – 30 , 32 , 37 , 38 ].
Only one trial identified in this review specifically included children who were HIV + [ 31 ]. Sub-group analyses stratified by HIV status showed a trend towards a protective effect of high-dose VAS on cough and rapid respiratory rate for HIV-infected children [RR 0.54 (0.24-1.20), p = 0.07], while children without HIV infection were at increased risk for these conditions [RR 1.47 (1.16-1.86), p = 0.001]. Because children infected with HIV are highly vulnerable to SAM and VAD, more research is needed to understand the optimal protocols for this population [ 39 ].
The evidence for growth outcomes in the follow-up period from hospital discharge was limited and somewhat dated [ 20 , 22 ]. One study showed that only among children who were VA deficient at baseline were there greater improvements in weight and MUAC in those who received high-dose VAS; this was not evident in the non-VA deficient children and high-dose VAS even reduced height gain among non-VA deficient girls [ 20 ]. Standard therapeutic foods designed for growth recovery in SAM may be a safer source of VA in certain cases. The foods contain VA as retinyl acetate, similar to VA supplements, in the following concentrations (per 100 g): F-75, 900 μg; F-100, 800 μg; and RUTF, 800–1100 μg. Thus, for a child weighing 5 kg, this would translate into 1,119 μg/d VA for F-75, or 1,544 μg/d VA for F-100, and 1,680 μg/d VA for RUTF. These quantities are comparable to the low-dose regimen of 5000 IU or 1500 μg retinol and are well below the high-dose recommendation of 100,000 IU or 30,000 μg/d VA that would be given to children under 12 mo. While these foods have not specifically been assessed as alternatives to VAS, the safety and efficacy of these products in the treatment of SAM is well-accepted [ 40 – 42 ]. Particularly in cases when a child’s VA status is unknown or adequate, therapeutic foods could thus serve as the delivery mechanism for low-dose VAS, though more research is needed.
Adverse effects found to be associated with high-dose VAS warrant more research. The most frequent negative outcome was an increased risk of acute respiratory infections [ 23 , 28 , 31 , 33 ]. There was also evidence of an increased risk of acute, non-severe diarrhea, mediated in part by nutritional status [ 26 , 31 , 32 ]. It should be noted that the adverse effects arising from high-dose VAS were found in samples or sub-samples that included primarily adequately nourished children. Heterogeneity in baseline characteristics and study design complicates comparisons across the various studies, but these safety issues should not be ignored. Excessive intake of preformed VA, notably in the absence of dietary fatty acids, may overwhelm the esterification process and introduce more harmful forms of VA into the child’s circulation [ 6 ]. Further along the metabolic pathway, VA presented to cell membranes in forms other than the RBP complex (as may be the case in SAM) can also lead to significant cellular damage [ 43 ]. Carotenoid forms of VA or lipid-based nutrient supplements such as RUTF, should be explored to minimize oxidative stress while still addressing VAD [ 44 ].
Conclusions
In the treatment of children with SAM, a high-dose VAS protocol can be safely recommended in cases presenting with measles, severe diarrhea (shigellosis), or symptoms of VAD. More research is needed to study this specific question in populations exclusively malnourished and to understand and prevent adverse outcomes related to high-dose VAS. We recommend exploration of alternative low-dose protocols and strategies beyond VAS, such as use of carotenoids or RUTF interventions, to address VA deficiency and associated health outcomes in the treatment of children with SAM.
Abbreviations
Acute lower respiratory infection
Grading of recommendations assessment development and evaluation
Mid-upper arm circumference
Randomized controlled trial
Ready-to-use therapeutic food
- Severe acute malnutrition
Vitamin A deficiency
- Vitamin A supplementation
Weight-for-age Z score
Weight-for-height Z score.
Black RE, Allen LH, Bhutta ZA, Caulfield LE, De Onis M, Ezzati M, Mathers C, Rivera J: Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008, 371: 243-260. 10.1016/S0140-6736(07)61690-0.
Article PubMed Google Scholar
West KP: Extent of vitamin A deficiency among preschool children and women of reproductive age. J Nutr. 2002, 132: 2857S-2866S.
CAS PubMed Google Scholar
UNICEF: The State of the World's Children 2012. 2012, New York: United Nations Children’s Fund
Google Scholar
WHO: Management of severe malnutrition: a manual for physicians and other senior health workers. 1999, Geneva: World Health Organization
Ashworth A, Khanum S, Jackson A, CS: Guidelines for the inpatient treatment of severely malnourished children. 2003, Geneva: World Health Organization
Penniston KL, Tanumihardjo SA, CS: The acute and chronic toxic effects of vitamin A. Am J Clin Nutr. 2006, 83: 191-201.
Villamor E, Fawzi WW: Vitamin A supplementation: implications for morbidity and mortality in children. J Infect Dis. 2000, 182: S122-133. 10.1086/315921.
Article CAS PubMed Google Scholar
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, et al: Grading quality of evidence and strength of recommendations. BMJ. 2004, 328: 1490-
Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Falck-Ytter Y, Jaeschke R, Vist G: GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol. 2011, 64: 1303-1310. 10.1016/j.jclinepi.2011.04.014.
Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA: GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011, 64: 1294-1302. 10.1016/j.jclinepi.2011.03.017.
Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, Devereaux PJ, Montori VM, Freyschuss B, Vist G: GRADE guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol. 2011, 64: 1283-1293. 10.1016/j.jclinepi.2011.01.012.
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y: GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). J Clin Epidemiol. 2011, 64: 407-415. 10.1016/j.jclinepi.2010.07.017.
Imdad A, Yakoob MY, Sudfeld C, Haider BA, Black RE, Bhutta ZA: Impact of vitamin A supplementation on infant and childhood mortality. BMC Publ Health. 2011, 11 Suppl 3: S20-
Article Google Scholar
Ashour MN, Salem SI, El-Gadban HM, Elwan NM, Basu TK: Antioxidant status in children with protein-energy malnutrition (PEM) living in Cairo, Egypt. Eur J Clin Nutr. 1999, 53: 669-673. 10.1038/sj.ejcn.1600830.
De Fatima Costa Caminha M, Da Silva Diniz A, Falbo AR, De Arruda IK, Serva VB, De Albuquerque LL, De Freitas Lola MM, Ebrahim GJ: Serum retinol concentrations in hospitalized severe protein-energy malnourished children. J Trop Pediatr. 2008, 54: 248-252. 10.1093/tropej/fmn018.
Donnen P, Brasseur D, Dramaix M, Vertongen F, Ngoy B, Zihindula M, Hennart P: Vitamin A deficiency and protein-energy malnutrition in a sample of pre-school age children in the Kivu Province in Zaire. Eur J Clin Nutr. 1996, 50: 456-461.
Mahalanabis D: Breast feeding and vitamin A deficiency among children attending a diarrhoea treatment centre in Bangladesh: a case–control study. BMJ. 1991, 303: 493-496. 10.1136/bmj.303.6801.493.
Article CAS PubMed PubMed Central Google Scholar
Mitra AK, Alvarez JO, Wahed MA, Fuchs GJ, Stephensen CB: Predictors of serum retinol in children with shigellosis. Am J Clin Nutr. 1998, 68: 1088-1094.
Sattar S, Ahmed T, Rasul CH, Saha D, Salam MA, Hossain MI: Efficacy of a high-dose in addition to daily low-dose vitamin A in children suffering from severe acute malnutrition with other illnesses. PloS ONE. 2012, 7: e33112-10.1371/journal.pone.0033112.
Donnen P, Brasseur D, Dramaix M, Vertongen F, Zihindula M, Muhamiriza M, Hennart P: Vitamin A supplementation but not deworming improves growth of malnourished preschool children in eastern Zaire. J Nutr. 1998, 128: 1320-1327.
Hussey GD, Klein M: A randomized, controlled trial of vitamin A in children with severe measles. N Engl J Med. 1990, 323: 160-164. 10.1056/NEJM199007193230304.
Coutsoudis A, Broughton M, Coovadia HM: Vitamin A supplementation reduces measles morbidity in young African children: a randomized, placebo-controlled, double-blind trial. Am J Clin Nutr. 1991, 54: 890-895.
Dibley MJ, Sadjimin T, Kjolhede CL, Moulton LH: Vitamin A supplementation fails to reduce incidence of acute respiratory illness and diarrhea in preschool-age Indonesian children. J Nutr. 1996, 126: 434-442.
Nacul LC, Kirkwood BR, Arthur P, Morris SS, Magalhaes M, Fink MC: Randomised, double blind, placebo controlled clinical trial of efficacy of vitamin A treatment in non-measles childhood pneumonia. BMJ. 1997, 315: 505-510. 10.1136/bmj.315.7107.505.
Si NV, Grytter C, Vy NN, Hue NB, Pedersen FK: High dose vitamin A supplementation in the course of pneumonia in Vietnamese children. Acta Paediatr. 1997, 86: 1052-1055. 10.1111/j.1651-2227.1997.tb14805.x.
Donnen P, Dramaix M, Brasseur D, Bitwe R, Vertongen F, Hennart P: Randomized placebo-controlled clinical trial of the effect of a single high dose or daily low doses of vitamin A on the morbidity of hospitalized, malnourished children. Am J Clin Nutr. 1998, 68: 1254-1260.
Hossain S, Biswas R, Kabir I, Sarker S, Dibley M, Fuchs G, Mahalanabis D: Single dose vitamin A treatment in acute shigellosis in Bangladesh children: randomised double blind controlled trial. BMJ. 1998, 316: 422-426. 10.1136/bmj.316.7129.422.
Stephensen CB, Franchi LM, Hernandez H, Campos M, Gilman RH, Alvarez JO: Adverse effects of high-dose vitamin A supplements in children hospitalized with pneumonia. Pediatrics. 1998, 101: E3-
Faruque AS, Mahalanabis D, Haque SS, Fuchs GJ, Habte D: Double-blind, randomized, controlled trial of zinc or vitamin A supplementation in young children with acute diarrhoea. Acta Paediatr. 1999, 88: 154-160. 10.1111/j.1651-2227.1999.tb01074.x.
Julien MR, Gomes A, Varandas L, Rodrigues P, Malveiro F, Aguiar P, Kolsteren P, Stuyft P, Hildebrand K, Labadarios D, Ferrinho P: A randomized, double-blind, placebo-controlled clinical trial of vitamin A in Mozambican children hospitalized with nonmeasles acute lower respiratory tract infections. Trop Med Int Health. 1999, 4: 794-800. 10.1046/j.1365-3156.1999.00493.x.
Fawzi WW, Mbise R, Spiegelman D, Fataki M, Hertzmark E, Ndossi G: Vitamin A supplements and diarrheal and respiratory tract infections among children in Dar es Salaam, Tanzania. J Pediatr. 2000, 137: 660-667. 10.1067/mpd.2000.110136.
Mahalanabis D, Lahiri M, Paul D, Gupta S, Gupta A, Wahed MA, Khaled MA: Randomized, double-blind, placebo-controlled clinical trial of the efficacy of treatment with zinc or vitamin A in infants and young children with severe acute lower respiratory infection. Am J Clin Nutr. 2004, 79: 430-436.
Donnen P, Sylla A, Dramaix M, Sall G, Kuakuvi N, Hennart P: Effect of daily low dose of vitamin A compared with single high dose on morbidity and mortality of hospitalized mainly malnourished children in Senegal: a randomized controlled clinical trial. Eur J Clin Nutr. 2007, 61: 1393-1399. 10.1038/sj.ejcn.1602671.
Jain MK, Mehta NJ, Fonseca M, Pai NV: Correlation of serum vitamin A and its transport protein (RBP) in malnourished and vitamin A deficient children. J Postgrad Med. 1990, 36: 119-123.
Rosales FJ, Ritter SJ, Zolfaghari R, Smith JE, Ross AC: Effects of acute inflammation on plasma retinol, retinol-binding protein, and its mRNA in the liver and kidneys of vitamin A-sufficient rats. J Lipid Res. 1996, 37: 962-971.
Semba RD, Ward BJ, Griffin DE, Scott AL, Natadisastra G, West KP, Sommer A, Muhilal: Abnormal T-cell subset proportions in vitamin-A-deficient children. Lancet. 1993, 341: 5-8. 10.1016/0140-6736(93)92478-C.
Daulaire NM, Starbuck ES, Houston RM, Church MS, Stukel TA, Pandey MR: Childhood mortality after a high dose of vitamin A in a high risk population. BMJ. 1992, 304: 207-210. 10.1136/bmj.304.6821.207.
Kjolhede CL, Chew FJ, Gadomski AM, Marroquin DP: Clinical trial of vitamin A as adjuvant treatment for lower respiratory tract infections. J Pediatr. 1995, 126: 807-812. 10.1016/S0022-3476(95)70416-7.
Trehan I, O’Hare BA, Phiri A, Heikens GT: Challenges in the Management of HIV-Infected Malnourished Children in Sub-Saharan Africa. AIDS Research and Treatment. 2012, 2012: 790786-
Article PubMed PubMed Central Google Scholar
Manary MJ, Sandige HL: Management of acute moderate and severe childhood malnutrition. BMJ. 2008, 337: 1227-1230. 10.1136/bmj.a1227.
Trehan I, Goldbach HS, LaGrone LN, Meuli GJ, Wang RJ, Maleta KM, Manary MJ: Antibiotics as part of the management of severe acute malnutrition. N Engl J Med. 2013, 368: 425-435. 10.1056/NEJMoa1202851.
WHO: Community-based management of severe acute malnutrition. 2007, Geneva: World Health Organization, World Food Programme, United Nations System Standing Committee on Nutrition, United Nations Children’s Fund
Creek KE, St Hilaire P, Hodam JR: A comparison of the uptake, metabolism and biologic effects of retinol delivered to human keratinocytes either free or bound to serum retinol-binding protein. J Nutr. 1993, 123: 356-361.
Celik M, Sermatov K, Abuhandan M, Zeyrek D, Kocyigit A, Iscan A: Oxidative status and DNA damage in chidren with marasmic malnutrition. J Clin Lab Anal. 2012, 26: 161-166. 10.1002/jcla.21505.
Yang H, De Onis M: Algorithms for converting estimates of child malnutrition based on the NCHS reference into estimates based on the WHO Child Growth Standards. BMC Pediatr. 2008, 8: 19-10.1186/1471-2431-8-19.
Download references
Acknowledgements
Funding was provided by the World Health Organization (WHO) to support the work of M. Manary and L. Iannotti.
Author information
Authors and affiliations.
Institute for Public Health/George Warren Brown School of Social Work, Washington University in St. Louis, Campus Box 1196, St. Louis, MO, 63130, USA
Lora L Iannotti, Indi Trehan & Mark J Manary
Department of Pediatrics, Washington University in St. Louis, 1 Childrens Pl, St Louis, MO, 63110, USA
Indi Trehan & Mark J Manary
Department of Paediatrics and Child Health, University of Malawi, Blantyre, Malawi
Indi Trehan
Department of Community Health, University of Malawi, Blantyre, Malawi
Mark J Manary
Children’s Nutrition Research Center, Baylor College of Medicine, Houston, Texas, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Lora L Iannotti .
Additional information
Competing interests.
There were no competing interests in this research.
Authors’ contributions
LLI, IT, and MJM contributed to the conception and design of the study. IT and MJM supervised the literature search and initial screening of studies. LLI carried out the full text review and initial GRADE assessment, followed by additional assessment from IT and MJM. All authors contributed to the analysis and interpretation of the compiled evidence. LLI drafted the manuscript with significant inputs received by IT and MJM. All authors have granted approval to this version of the manuscript.
Electronic supplementary material
12937_2013_711_moesm1_esm.doc.
Additional file 1: Table S1: Observational studies included in systematic review [ 45 ]. (DOC 68 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Iannotti, L.L., Trehan, I. & Manary, M.J. Review of the safety and efficacy of vitamin A supplementation in the treatment of children with severe acute malnutrition. Nutr J 12 , 125 (2013). https://doi.org/10.1186/1475-2891-12-125
Download citation
Received : 06 March 2013
Accepted : 21 August 2013
Published : 12 September 2013
DOI : https://doi.org/10.1186/1475-2891-12-125
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
Nutrition Journal
ISSN: 1475-2891
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Published: 28 March 2022
Vitamin A supplementation policy: A shift from universal to geographical targeted approach in India considered detrimental to health and nutritional status of under 5 years children
- Nimmathota Arlappa ORCID: orcid.org/0000-0001-5405-1872 1
European Journal of Clinical Nutrition volume 77 , pages 1–6 ( 2023 ) Cite this article
4814 Accesses
2 Citations
3 Altmetric
Metrics details
- Epidemiology
- Medical research
Evolvement of Vitamin A supplementation (VAS) programme in India: Universal coverage of children 6–59 months
Vitamin A is an essential fat-soluble micronutrient required for normal growth and development, maintenance of healthy mucosal membranes, reproductive health, immunity, and vision, especially for dark adaptation. Vitamin A deficiency (VAD) continues to be a major nutritional problem of public health concern in India, despite the implementation of a programme for vitamin A supplementation for over four decades. Although the incidence of clinical VAD in India has declined significantly over the period of time, the highest proportion of the world’s VAD children still lives in India [ 1 , 2 ]. The proportion of rural preschool children in India with Bitot’s spots, an objective clinical sign of VAD is reported to be over 0.5%, making VAD a public health problem [ 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 ]. A similar pattern of prevalence of sub-clinical VAD (serum retinol ≤ 0.70 µmol/L or ≤ 20 µg/dL) is also observed and confirms VAD to be a severe public health problem (≥ 20%) in India [ 4 , 5 , 6 , 7 , 8 , 9 , 11 , 14 ] Table 1 .
Taking into consideration the grave public health problem of VAD and nutritional blindness in India, the National Institute of Nutrition (NIN) carried out a series of clinical, biochemical, and field intervention studies in the 1960s [ 15 ]. Following this, a countrywide high dose (200000 IU) six-monthly Vitamin A Supplementation (VAS) program was recommended [ 16 , 17 ]. In 1970, the Government of India launched the “National program for prophylaxis against blindness in children due to vitamin A deficiency” targeting children 1–5 years [ 18 ]. Subsequently, the VAS programme was revisited in 1991 by the Indian experts in the context of emerging evidence of the impact of VAS on child mortality [ 19 ] and an India study on seroconversion of measles vaccine by the NIN [ 20 ]. The revised VAS programme included infants 6–11 months and was renamed as “Management of Vitamin A deficiency Programme”. In the early period of implementation, taking into consideration the supply of vitamin A solution and cost, the policy accorded a higher priority to administer VAS to the most vulnerable children aged 9–36 months. However, in 2006, with increased prevalence of VAD in 36–59 months children and no constraint on the supply of vitamin A solution, the Government of India expanded the target age group to meet the 1991 policy guidelines to 6–59 months [ 21 ]. The VAS is in operation in India as well as in more than 70 countries around the world and is recognised to be one of the most effective public health interventions ever undertaken [ 22 , 23 ]. Taking into consideration, the need for improving the coverage of six monthly administration of VAS In India, a biannual VAS strategy was piloted and scaled up in India [ 21 ].
Proposed policy shift from universal VAS coverage to targeting to the selected states: Questioning the rationale
Some studies carried out in India during the last two decades have reported a considerable decrease in the prevalence of Bitot’s Spots [ 24 , 25 , 26 ] and these findings have led to a constant opposition to the continuation of the universal VAS programme in India. The recommendation to discontinue the VAS programme by a selected group of experts has been persistent for over a decade despite the lack of state or nationally representative database that confirms substantial improvement in clinical, sub-clinical VAD or dietary vitamin A consumption among children under 5 years. In fact, after the NNMB-2003-05 rural survey in 8 states in India, no large-scale study has been carried out to measure sub-clinical vitamin A status in children [ 27 ]. Moreover, the dietary survey findings of the National Nutrition Monitoring Bureau (NNMB) surveys that were available also do not support discontinuation of VAS since the diets of children under 5 were reported to be extremely poor in vitamin A [ 25 , 26 ].
The argument by a select group of experts to discontinue universal Vitamin A Supplementation (VAS) for children 6–59 months under the national programme gained momentum following the release of the Comprehensive National Nutrition Survey (CNNS) report 2019 on micronutrients, including vitamin A status of young children and adolescents [ 28 ]. The Expert Group constituted by the Ministry of Health, Government of India recommended modification in the existing national programme and shifting the focus of VAS from universal coverage of children to a geographical targeted approach. This recommendation was primarily based on the CNNS findings of a low prevalence of sub-clinical VAD of 17.6% among children aged 1–4 years as assessed by the measure of serum retinol levels below 20 µg/dl and VAD as a severe public health problem (prevalence of ≥ 20%) only in 10 of the 30 states/union territories that were surveyed. An examination of the CNNS methodology, however, raises a number of questions on the prevalence of sub-clinical VAD among children reported by the CNNS, since there is a substantial gap in the design and the actual execution. Similarly, a substantial difference is noted in the CNNS methodology that prescribed the representative sample of children to be covered in various states and at the national level for estimation of various micronutrients including vitamin A and the actual number of children that were covered for estimation of serum retinol [ 28 ]. The CNN survey covered only 6694 children aged 1–4 years as against the 20,350 children proposed in the study methodology. Likewise, none of the 30 states/union territories surveyed met the target sample of children that was prescribed in the survey design. In about half of the states, the coverage was only around one-third of the proposed sample size, while the coverage was more than 75% of the proposed sample in only two of the 30 states- Odisha (80.5%) and Sikkim (76%) (Table 2 ). In such a situation of coverage of grossly inadequate sample size, valid estimation and inference on the prevalence of VAD are scientifically not correct. Such an inadequate sample could result in unduly large standard errors; inadequate power with the resulting inferences drawn being misleading. Moreover, the report on VAD situation does not represent the entire country and is limited to 28 states and two union territories (UTs). Similarly, the CNNS report has excluded serum retinol data of two states i.e. Rajasthan and Nagaland and the survey did not cover the six union territories. Therefore, the findings of the CNNS were derived from the grossly inadequate and non-representative sample for the country. Despite such apparent limitations in the CNNS survey, the Expert Committee recommends to discontinue the VAS programme in all the states and union territories except for 3 states with a high prevalence of VAD [ 24 ]. The rationale for zeroing on 3 states from the 10 states reported having VAD as a severe public health problem remains an enigma. On that account, the evidence is not sufficient to indicate a low prevalence of sub-clinical VAD to argue for modification of the existing VAS policy in India.
Assumption of vitamin A inadequacy is not convincing
In addition to the CNNS findings on VAD, the Expert Committee also substantiated their recommendation for change in vitamin A policy on the basis of dietary intake of vitamin A and fortification of oil and milk with vitamin A. These inferences on dietary vitamin A consumption were based on secondary data collected at two different time periods, a decade ago by the NNMB [ 25 ] and the National Sample Survey Office (NSSO) [ 29 ]. Likewise, it was also projected by the Expert Committee that the dietary inadequacy (≤ 70% of Recommended Dietary Allowances) of vitamin A will reduce substantially with the ongoing efforts by the country to fortify oil and milk with vitamin A [ 24 ]. There was no scientific data presented to support this assumption. Moreover, consumption of oil and milk used as food vehicles for fortification is rather low and the consumption of these food items differ widely in the various socio- economic groups. In fact, even if the fortification is 100%, the deficit intake will continue to be high as most rural, tribal, and peri-urban households in India purchase milk and oil from local vendors. As per the NNMB surveys, the intakes of oil and milk among the rural, tribal, and urban children in India are extremely poor [ 25 , 26 , 30 ] with the inadequacy (≤70% of Recommended Dietary Intakes) of intakes ranging from a low of 86.2 to a high of 100%. Likewise, the dietary inadequacy (≤ 70% of RDA) of vitamin A is also very high ranging from a low of 86.3% in rural children 4–6 years age to a high of 93.4% in urban children 1–3 years [ 25 , 26 , 30 ] Table 3 . The total available vitamin A gets further reduced due to the fact that the dietary source of vitamin A in the Indian diet is primarily from vegetarian source and the availability of vitamin A is rather low as compared with animal source of vitamin A. Provitamin A carotenoids from plant sources have lower relative absorption efficiency ranging from only 5% to 26% [ 31 ] and the ratio of conversion of provitamin A carotenoids to retinol in humans varies from 2:1 to 24:1 on a µg:µg basis [ 32 , 33 ]. While in contrast, pre-formed vitamin A (retinol) found only in animal-sourced foods is an active form of vitamin A with 70–90% bio-availability [ 34 , 35 ].
Therefore, it is scientifically inappropriate to argue for the modification of the existing vitamin A policy based on dietary data collected more than a decade ago. Moreover, the Expert Committee conveniently ignored the latest dietary data collected by the CNN survey (2016–18) that indicated extremely poor intake of dietary source of vitamin A, where only 5% of Indian children of 2–4 years reportedly consumed vitamin A-rich fruits and vegetables and the negligible proportion of them consumed animal source foods rich in vitamin A [ 24 , 28 ].
Presumption of Vitamin A hypervitaminosis has no basis
Besides the arguments stressing vitamin A deficiency is not a public health problem in the country and the dietary inadequacy of vitamin A is low, the Expert Committee has presented an additional viewpoint for the discontinuation of VAS programme. This argument pertains to the speculation and concerns that introduction of fortification of oils and milk with vitamin A combined with continuation of VAS would lead to hypervitaminosis among young children. No evidence is presented to support this rationale. Reports of acute toxicity have been reported only in case when erroneously an extremely high dose of VAS has been administered in a short period of time [ 36 ]. On the other hand, chronic toxicity has been reported only on long-term ingestion of vitamin A when the intake is higher than 10 times the recommended daily allowance [ 34 ]. Except for few reports of toxic effects in infants below six months, side effects of VAS are usually rare in children aged six months or older [ 37 , 38 , 39 ]. Penniston & Tanumihardjo substantiate that hypervitaminosis is not at all relevant to the age beyond 9 months with the recommended massive dose VAS for public health programmes or combination of interventions i.e., diet, fortified foods, and supplements [ 40 ]. In India, as indicated earlier, dietary intake of vitamin A, as well as the consumption of food vehicle selected for vitamin A fortification, is rather low and the issue of vitamin A toxicity remains totally hypothetical. Having a scientific basis is imperative for drawing such a conclusion and would require the use of an appropriate method such as application of sensitive biomarkers to assess the adverse impact of vitamin A supplement when combined with food fortification, the condition of hypervitaminosis cannot be detected by the mere measure of serum retinol concentrations [ 41 ].
Reflecting on Impact of VAS programmes in India: Imperative to ensure each and every child is protected from vitamin A deficiency
In public health programmes, the provision of micronutrient supplements such as vitamin A, iodine, and iron are viewed as a short-term strategy to reinforce dietary approaches to mitigate micronutrient deficiencies [ 42 ]. Administration of VAS is also recommended to be progressively phased out as soon as micronutrient-rich food-based interventions enable adequate consumption [ 43 , 44 ], and therefore, administration of VAS is not viewed to be a long-term strategy for prevention of VAD [ 45 ]. Several studies have supported a dietary modification (food-based) approach as a sustainable model for the prevention and control of multiple micronutrient deficiencies, particularly the VAD [ 46 , 47 , 48 , 49 ]. However, Sommer and Davidson have proposed that, based on dietary data and kinetic modelling, it is virtually impossible to correct widespread VAD by diet alone in developing countries, where populations remain dependent on conventional plant-based foods [ 50 ]. In Western societies, preformed vitamin A provides > 70% of daily vitamin A requirement [ 51 ] while people in developing countries meet 80–85% of their daily requirement of vitamin A from plant sources of foods [ 52 ]. Paradoxically VAD is common even in Indian children of affluent households when the source of vitamin A is predominantly from vegetarian diets [ 30 , 53 ]. If we consider this scientific evidence, it is impractical to assume children in India consume such amounts of fruits and vegetables, considering not only the access and cost but, the bioavailability and the rate of conversion of carotenoids to retinol.
Since the 1970s, food-based approaches have been an integral part of vitamin A deficiency control programme in India; but despite this, the dietary intakes of vitamin A have remained persistently low and have not changed much at all in the past four decades [ 49 ]. Thus, improving dietary intake of vitamin A through dietary diversification remains a challenge in India. Chronic poverty and ignorance, deep-rooted cultural and religious factors, as well as seasonal accessibility to micronutrient-rich foods, have longstanding impact on dietary intakes of vitamin A by Indian population. The unique requirements of caste and religion in India have further contributed to extreme variations in the diet; even among individuals living in geographic proximity [ 15 ].
In India, the introduction of the biannual fixed months VAS programme since mid 2000 has positively impacted VAS with coverage of children under 5 years for massive dose VAS reported to have increased from 25% in 2003–05 [ 27 ] to 60.2% in 2015–16 [ 54 ]. Recent NFHS-5 (2019–21) data also indicates a significant improvement in the percentage of children 9–36 months who received VAS in the preceding six months to be 71.2 % [ 55 ]. Such an improvement in coverage of children 6–59 months with VAS administration is possibly the reason for the low prevalence of sub-clinical VAD (17.6%) [ 34 ] and Bitot’s spots (0.3%) [ 25 ] in contrast to a high prevalence of Bitot’s spots (1.4%) [ 25 ] and sub-clinical VAD (21.5%) [ 28 ] in children aged 5–10years. Hence, the lower prevalence of VAD in children under 5 years as compared to that of 5–10 years old could definitely be attributed to the coverage under VAS. On the other hand, discontinuation of VAS when not replaced with adequate intake of vitamin A rich foods would possibly worsen the vitamin A status. Therefore, suspending the VAS programme prior to an improvement in dietary vitamin A intakes solely on the basis of nationally non-representative CNNS findings may reverse the progress in vitamin A status and lead to the re-emergence of blinding xerophthalmia [ 56 ]. This is also evident from an Indian study that reported corneal xerosis (0.3%) and corneal scars (0.5%) among children of Uttar Pradesh in 2011 [ 5 ]. Global Alliance for Vitamin A (GAVA) advocated that before scaling-back the existing VAS policy, countries should ascertain that the dietary intakes of vitamin A are adequate, the sub-clinical vitamin A status of children is optimal, and the prevalence of sub-clinical VAD among children 6–59 months is less than 10% [ 57 ]. Therefore, considering these recommendations of the GAVA, it is pertinent to judge the ground realities of vitamin A status in the country. From the available recent data, it is obvious that the diets of children are extremely poor in vitamin A and the prevalence of sub-clinical VAD among children is 17.6%, which cannot be considered low enough to revise the existing VAS policy in India [ 58 , 59 , 60 ].
Change of VAS Policy in India in the current situation is not conducive
It is imperative that prior to taking any decision on revision of India’s existing vitamin supplementation A policy, the Ministry of Health and Family Welfare (MoHFW) should appraise the ground realities of vitamin A status among children under 5 years in rural, tribal, urban and urban slums within the various states in India by undertaking a well-designed study with adequate state and nationally representative sample size using various parameters comprising serum retinol, Bitot’s spots and dietary vitamin A intake. Additionally, study with more sensitive biomarkers like relative dose response tests [ 58 ] is required to be undertaken in a sub-sample of children. In absence of such valid information, discontinuation of VAS programme in India implies denying children’s right to receive VAS until their vitamin A intake has improved optimally. Deprivation of vitamin A during formative years is detrimental to the growth and development of a child, resulting in morbidity and mortality [ 61 ]. In the Pandemic situation of Covid-19, we need to provide support in building immunity of children who are yet to receive vaccination against Covid-19 infection and may have lower intake of dietary vitamin A due to possible interruptions in the world’s largest ongoing supplementary feeding programme under the Integrated Child Development Services (ICDS) for children or poor food purchasing power. In such a grave situation, the significance of continuing the VAS policy of six monthly administration of vitamin A supplement to young children cannot be ignored.Universal coverage of all children 6–59 months with VAS in the current Covid-19 Pandemic situation needs high priority. The implications of the recommendation of Expert Committee to shift the existing universal coverage of VAS approach to a targeted geographical approach, with coverage limited to less than one tenth of the country could be devastating to the health of children, particularly those from poor and marginalised households. There is a need for substantial supportive scientific evidence. In absence of convincing rationale, the recommendation by selected experts to make changes in the existing VAS policy in India appears to be very similar to the well documented initial resistance by few scientists and experts who had strong opinions but not sufficient scientific basis to their claims for opposing the public health intervention of introduction of Bacille Calmette-Guerin (BCG) and many other novel vaccines across the globe [ 22 ].
Data availability
National Nutrition Monitoring Bureau published Technical Reports
https://www.nin.res.in/downloads.html
Comprehensive National Nutrition Survey (CNNS) National Report 2016-18
https://nhm.gov.in/WriteReadData/l892s/1405796031571201348.pdf
World Health Organization. Global prevalence of vitamin A deficiency in populations at risk: 1995–2005. WHO Global Database on Vitamin A Deficiency. Geneva: WHO; 2009.
West KP Jr. Extent of vitamin A deficiency among preschool children and women of reproductive age. J Nutr. 2002;132:2857–66.
Article Google Scholar
Panda L, Nayak S, Das T. Tribal Odisha eye disease study report 6. Opportunistic screening of vitamin A deficiency through School Sight Program in tribal Odisha (India). Indian J Ophthalmol. 2020;68:351–5.
Article PubMed PubMed Central Google Scholar
Awasthi S, Peto R, Read S, Clark S, Pande V, Bundy D, et al. Vitamin A supplementation every 6 months with retinol in 1 million pre-school children in north India: DEVTA, a cluster-randomised trial. Lancet 2013;381:1469–77.
Article CAS PubMed PubMed Central Google Scholar
Sachdeva S, Alam S, Beig FK, Khan Z, Khalique N. Determinants of vitamin A deficiency amongst children in Aligarh District, Uttar Pradesh. Indian Pediatr. 2011;48:861–6.
Article PubMed Google Scholar
Laxmaiah A, Nair MK, Arlappa N, Raghu P, Balakrishna N, Mallikharjuna Rao K, et al. Prevalence of ocular signs and subclinical vitamin A deficiency and its determinants among rural pre-school children in India. Public Health Nutr. 2012;15:568–77.
Arlappa N, Balakrishna N, Laxmaiah A, Brahmam GNV. Vitamin A deficiency disorders among the rural pre-school children of south India. Int J Nutr. 2016;2:1–11.
Arlappa N, Balakrishna N, Laxmaiah A, Brahmam GNV. Ocular manifestations of vitamin A deficiency among the rural pre-school children of north India. J Ophthalmic Sci. 2015;1:1–11.
Arlappa N, Balakrishna N, Laxmaiah A, Raghu P, Vikas, Madhavan Nair K, et al. Prevalence of vitamin A deficiency and its determinants among the rural pre-school children of Madhya Pradesh, India. Ann Hum Biol. 2011;38:131–6.
Article CAS PubMed Google Scholar
Arlappa N, Venkaiah K, Brahmam GNV. Severe drought and the vitamin A status of rural pre-school children in India. Disasters 2011;35:577–86.
Arlappa N, Balakrishna N, Laxmaiah A, Nair KM, Brahmam GN. Prevalence of clinical and sub-clinical vitamin A deficiency among rural preschool children of West Bengal, India. Indian Pediatr. 2011;48:47–9.
Arlappa N, Laxmaiah A, Balakrishna N, Harikumar R. Brahmam GNV.Clinical and sub-clinical vitamin A deficiency among rural pre-school children of Maharashtra, India. Ann Hum Biol. 2008;35:606–14.
Toteja GS, Singh P, Dhillon BS, Saxena BN. Vitamin A deficiency disorders in 16 districts of India. Indian J Pediatr. 2002;69:603–5.
Meshram II, Kumar BN, Venkaiah K, Longvah T. Subclinical vitamin A deficiency and anemia among women and preschool children from Northeast India. Indian J Community Med. 2020;45:371–4.
Arnold David. The ‘discovery’ of malnutrition and diet in colonial India. Indian Econ Soc Hist Rev. 1994;31:1–26.
Narsinga Rao. BS New Delhi: Allied Publishers; 2005. Development of nutrition science in India.
Gopalan C. Review of some current studies in the nutrition research laboratories, Hyderabad. Souvenir of golden jubilee celebrations of NRL. Hyderabad: Nutrition Research Laborotories; 1969. pp. 21–9.
New Delhi: Government of India Press. Maternal and child health scheme for prophylaxis against nutritional blindness in children caused by vitamin A deficiency. Family Planning Programme. Fourth Five-Year Plan Tech Inf: MCH No. 1970;2:1–22.
Google Scholar
Imdad A, Herzer K, Mayo-Wilson E, Yakoob MY, Bhutta ZA. Vitamin A supplementation for preventing morbidity and mortality in children from 6 months to 5 years of age. Cochrane Database Syst Rev. 2010;12:CD008524.
Bhaskaram P, Rao KV. Enhancement in seroconversion to measles vaccine with simultaneous administration of vitamin A in 9-months-old Indian infants. Indian J Pediatr. 1997;64:503–9.
Vir SC, Pandey RS Vitamin A prevention and control programme in India- past efforts and current status. In: Vir SC (eds). Public Health and Nutrition in Developing Countries. 1st ed. Woodenhead Publishers, New Delhi, 2011. pp 473–501
Wallace SK. Global health in conflict. Understanding opposition to vitamin A supplementation in India. Am J Public Health. 2012;102:1286–97.
Fawzi WW. The benefits and concerns related to vitamin A supplementation. J Infect Dis. 2006;193:756–9.
Reddy GB, Pullakhandam R, Gosh S, Boiroju NK, Tattari S, Laxmaiah A, et al. Vitamin A deficiency among children younger than 5 y in India:an analysis of national data sets to reflect on the need for vitamin A supplementation. Am J Clin Nutr. 2021;113:939–47.
National Nutrition Monitoring Bureau(NNMB).Diet and nutritional status of rural population, prevalence of hypertension and diabetes among adults and infant and young child feeding practices-3rd Repeat Survey. Report No.26. Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 2012.
National Nutrition Monitoring Bureau (NNMB).Diet and nutritional status of tribal population and prevalence of hypertension among adults-2nd Repeat Survey. Report No.25. Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 2009.
National Nutrition Monitoring Bureau (NNMB) Prevalence of vitamin A deficiency among rural pre-school children. Report No.23.Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 2006.
Comprehensive National Nutrition Survey (CNNS). CNNS National Report 2016-18.New Delhi: Ministry of Health and Family Welfare, Government of India, UNICEF and Population Council; 2019.
National Sample Survey Office (NSSO). Nutritional intake in India: 2011–12, NSS 68th round. New Delhi: National Statistical Organization, Government of India; 2014.
National Nutrition Monitoring Bureau (NNMB). Diet and nutritional status of urban population in India and prevalence of obesity, hypertension, diabetes and hyperlipidemia in urban men and women. Report No.27.Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 2017.
Institute of Medicine (IOM). Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Washington, DC: National Academies Press; 2001
Grune T, Lietz G, Palou A, Ross C, Stah W, Tang G, et al. Beta-carotene is an important vitamin A source for humans. J Nutr. 2010;140:2268S–2285S.
de Pee S, West CE, West CE, Muhilal, Karyadi D, Hautvast JG. Lack of improvement in vitamin A status with increased consumption of dark green leafy vegetables. Lancet 1995;346:75–81.
Penniston KL, Tanumihardjo SA. The acute and chronic toxic effects of vitamin A. Am J Clin Nutr. 2006;83:191–201.
Blomhoff R, Blomhoff HK. Overview of retinoid metabolism and function. J Neurobiol. 2006;66:606–30.
Olson JM, Ameer MA, Goyal A Vitamin A Toxicity. [Updated 2021 Aug 14]. In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2021.
Agoestina T, Humphrey JH, Taylor GA, Usman A, Subardja D, Hidayat S, et al. Safety of one 52‐µmol (50,000 IU) oral dose of vitamin A administered to neonates. Bull World Health Organ. 1994;72:859–68.
CAS PubMed PubMed Central Google Scholar
Baqui AH, de Francisco A, Arifeen SE, Siddique AK, Sack RB. Bulging fontanelle after supplementation with 25,000 IU of vitamin A in infancy using immunization contacts. Acta Paediatr. 1995;84:863–6.
de Francisco A, Chakraborty J, Chowdhury HR, Yunus M, Baqui AH, Siddique AK, et al. Acute toxicity of vitamin A given with vaccines in infancy. Lancet 1993;342:526–7.
Tanumihardjo SA, Russell RM, Stephensen CB, Gannon BM, Craft NE, Haskell MJ, et al. Biomarkers of Nutrition for Development (BOND)-Vitamin A Review. J Nutr. 2016;146:1816S–48S.
Food and Agriculture Organization of the United Nations/World Health Organization. International Conference on Nutrition. World Declaration and Plan of Action for Nutrition. Rome: FAO/WHO; 1992.
Greiner T Vitamin A: Moving the food-based approach forward. Ted Greiner Professor of Nutrition Department of Nutrition Hanyang University Seoul, South Korea. Rome: FAO. 2013;1–69. https://www.fao.org/fileadmin/user_upload/agn/pdf/Greiner_VITAMIN_A_Final.pdf (accessed 3 March 2022).
Sommer A, West KP Jr. Vitamin A deficiency: health, survival and vision. Oxford University Press, New York, 1996.
Delisle H. Vitamin A distribution in danger: should we worry? Lancet. 2018;392:631–2.
Latham M. The great vitamin A fiasco. World Nutr. 2010;1:12–45.
Srikantia SG. Vitamin A deficiency prevention programme. In: Gopalan C, ed.Combating Undernutrition. Basic Issues and Practical Approaches. New Delhi: Nutrition Foundation of India, Media Workshop, Special Publication Series. 1989; 3:353–6.
Gopalan C, Tamber B. Food-based approaches to prevent and control micronutrient malnutrition: Scientific evidence and policy implications. World Rev Nutr Diet. 2003;91:76–131.
Arlappa N. Vitamin A deficiency control measures: Importance of vitamin A supplementation as a public health policy in the Indian context. J Public Health Policy. 2013;34:538–48.
Sommer A, Davidson FR. Assessment and control of vitamin A deficiency: The Annecy accords. J Nutr. 2002;132:2845S–2851S.
US Department of Agriculture, Agricultural Research Service 2005- 2006 What we eat in America, NHANES Tasdableeee 1-8. 2008. http://www.ars.usda.gov/ba/bhnrc/fsrg (accessed 1 June 2021).
FAO/WHO Expert Consultation. Requirements of vitamin A, iron, folate and vitamin B 12 . FAO Food and Nutrition Series No.23, Rome, FAO;1988
Ramakrishnan U, Darnton-Hill I. Assessment and control of vitamin A deficiency disorders. J Nutr. 2002;132:2947S–2953S.
International Institute of Population Science. National Family Health Survey India 2015–2016: India fact sheet. Mumbai: Ministry of Health and Family Welfare, Government of India; 2016.
International Institute of Population Science. National Family Health Survey India 2019–2021: India fact sheet. Mumbai: Ministry of Health and Family Welfare, Government of India; 2021.
Thurnham DI. Vitamin A supplementation: Beneficial effects on mortality and morbidity in children aged six months to five years. Sight Life. 2011;25:38–49.
GAVA. Conditions for scaling back universal preschool vitamin A supplementation: policy brief. The Global Alliance for Vitamin A; 2019. http://www.gava.org/content/user_files/2019/05/GAVA-Brief-Scaling-Back-VAS-EN-May-10.pdf (accessed on 3 March 2022)
Sheftel J, Suri DJ, Tanumihardjo SA. Recommendations to adjust national vitamin A intervention policy must follow a consistent framework. Am J Clin Nutr 2021;113:1707–8.
Arlappa N. Sample size covered for serum vitamin A is not nationally representative: data are not suggestive for Targeted Vitamin A Supplementation Programme in India. Am J Clin Nutr 2021;113:1708–9.
Vir SC Plan to discontinue the vitamin A supplement programme is hasty. https://indianexpress.com/article/opinion/columns/vas-programme-vitamin-a-supplement-children-immunity-7538191/ (accessed on 3 March 2022)
Arlappa N, Ravikumar BP. Relevance of continuation of universal vitamin A supplementation program in India. Indian Pediatr. 2011;48:246–7.
CAS PubMed Google Scholar
Download references
Acknowledgements
I am extremely thankful to Dr. G.Sarika, Scientist-B, for her help in the review of literature.
Author information
Authors and affiliations.
Scientist-F, Division of Public Health Nutrition, ICMR-National Institute of Nutrition, Hyderabad, India
- Nimmathota Arlappa
You can also search for this author in PubMed Google Scholar
Contributions
NA conceptualised and prepared the perspective.
Corresponding author
Correspondence to Nimmathota Arlappa .
Ethics declarations
Competing interests.
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions

About this article
Cite this article.
Arlappa, N. Vitamin A supplementation policy: A shift from universal to geographical targeted approach in India considered detrimental to health and nutritional status of under 5 years children. Eur J Clin Nutr 77 , 1–6 (2023). https://doi.org/10.1038/s41430-022-01122-5
Download citation
Received : 02 June 2021
Revised : 03 March 2022
Accepted : 11 March 2022
Published : 28 March 2022
Issue Date : January 2023
DOI : https://doi.org/10.1038/s41430-022-01122-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Discontinuing five decades of vitamin a supplementation policy in india without valid scientific evidence: a step in haste.
European Journal of Clinical Nutrition (2023)
A vicious turn to the saga of vitamin A deficiency in India
- H. S. Sachdev
- G. B. Reddy
- A. V. Kurpad
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Signs and Symptoms of Vitamin D Deficiency
Many parts of your body rely on vitamin D for sustenance—including your bones, muscles, brain, and immune system . Most people have the vitamin D that their body needs, but as many as one in four adults in the U.S. are deficient and can experience symptoms such as muscle weakness, hair loss, and fatigue.
This is partly because vitamin D isn’t quite as easy to get naturally as some other nutrients. While your body makes some vitamin D when you are in the sun, this nutrient isn't easily found or abundant in Western diets.
Vitamin D deficiency can be hard to diagnose because it either produces no symptoms or its symptoms overlap with many other types of health conditions. The good news: a vitamin D deficiency is relatively easy to treat with supplements once your healthcare provider identifies that you're deficient.
Frequent Illness
Vitamin D bolsters the immune system, so if you’re constantly getting sick—or becoming seriously ill with even minor infections—a deficiency could be to blame. In fact, some research has found a link between higher disease severity in people in the ICU and low levels of vitamin D. This was examined again after the onset of COVID-19 , with studies showing that people with deficiencies may have had a higher risk of getting COVID and getting sicker from the virus.
Hair Loss
Vitamin D plays an important part in regulating the hair cycle, including the regeneration of new hair . That said, it’s possible that a deficiency could slow your hair growth process down. In fact, people with alopecia (an autoimmune disorder that causes hair loss ) have lower levels of vitamin D, and topical vitamin D treatments have been used to improve symptoms.
Bone Fractures
Because it’s a key nutrient in strengthening your bones , a vitamin D deficiency can cause osteomalacia in adults, or a condition that leads to the softening of the bones. This deficiency can also increase your risk of developing osteoporosis —a condition that causes a decrease in bone mass and density, making your bones more prone to breakage.
Muscle Pain and Weakness
Vitamin D promotes muscle function, so low levels of the vitamin may boost your likelihood of experiencing symptoms such as loss of muscle tone, atrophy, weakness, and pain . Due to the loss of muscle mass and strength, it's also possible to be more prone to experiencing falls.
The loss of muscle strength—and subsequent stress on the back and neck muscles—can lead to back pain. Lower back pain, in particular, is a common complaint among people with vitamin D deficiencies. Some experts suggest screening people with lower back pain for vitamin D deficiencies may be helpful, as treatment such as vitamin D supplements, can ease pain-related symptoms.
Fatigue
It’s unclear exactly why low vitamin D levels might lead to fatigue , but multiple studies have shown that people who take vitamin D supplements report an improvement in fatigue and an increase in overall energy levels.
The research is mixed on whether taking vitamin D supplements can improve existing symptoms of depression , but multiple studies have shown that people with a vitamin D deficiency may be at an increased risk of experiencing depressive episodes.
Symptoms in Children
A severe lack of vitamin D in children can lead to rickets, a condition that causes softening in developing bones. Many children get their vitamin D from the sun and from dairy products, but very young babies are typically not exposed to much sun and don’t consume dairy until they begin solid foods .
Rickets is especially common in breastfed babies. The condition may be even more common in babies if their breastfeeding parent also has a vitamin D deficiency . That's why healthcare providers recommend giving a vitamin D supplement to all babies, regardless of whether they're breastfed or fed by formulas. However, your baby may not need a vitamin D supplement if they are drinking at least 32 ounces of formula daily.
If your baby does develop rickets, they may experience the following symptoms:
- Bowed legs
- Changes in shape to the spinal curve, ribs, or breastbones
- Dental problems
- Stunted growth
- Loss of muscle tone
Although rickets is most common in young babies, older kids are also prone to having a vitamin D deficiency. About 15% of kids between the ages of one and 11 have a vitamin D deficiency, while 17% of adolescents don’t get enough vitamin D.
When to See a Healthcare Provider
If you or your child has symptoms of bone or hair loss, muscle pain, or fatigue, or are frequently becoming ill or experiencing bone fractures with no clear cause, make an appointment with a healthcare provider.
They can better assess your symptoms and order diagnostic measures (such as blood tests) to check your vitamin D levels, among other results from your bloodwork. If your results show that you have a vitamin D deficiency , your provider can recommend the right amount of vitamin D supplementation you will need to bring your levels back to normal.
Keep in mind: you should not self-treat a vitamin D deficiency, since too much vitamin D from supplements can have adverse side effects.
A Quick Review
Vitamin D is a vital nutrient for your bones, muscles, nerves, and immune system. Too little vitamin D can lead to fatigue, frequent illness or bone fractures, hair loss, and muscle and bone pain. In children, severe deficiency can cause rickets—a condition that leads to the softening of their bones.
A blood test can confirm if you have a vitamin D deficiency, so it's a good idea to see your healthcare provider for proper testing and diagnosis. If you have a deficiency, your healthcare provider can guide you in safely increasing your levels with vitamin D supplementation.
Frequently Asked Questions
What causes vitamin D to drop?
Vitamin D levels can become deficient if you don’t get enough exposure to sunlight, don’t consume enough of the vitamin in the foods you eat, or if you have a health condition that limits your ability to process or absorb vitamin D.
Does low vitamin D cause weight gain?
There is some evidence that people with vitamin D deficiency are more likely to become obese, possibly because excess fat prohibits the processing of the vitamins in the body. But there hasn’t been a direct correlation made between low vitamin D and weight gain and more research is still needed.
Does vitamin D affect sleep?
Vitamin D levels are often lower in people with sleep disorders, but researchers haven’t been able to demonstrate that vitamin D supplementation improves symptoms of sleep disorders or reduces their occurrence.
What happens when your vitamin D is very low?
Often, nothing noticeable happens. Most people with vitamin D deficiency are asymptomatic, but that doesn’t mean there aren't changes occurring within the body. Vitamin D is considered a “building block” for many body systems, so low levels can interfere with your body’s ability to produce strong and healthy bones, maintain proper muscle tone, fight infections, and regulate mood, energy, and sleep.
For more Health news, make sure to sign up for our newsletter!
Read the original article on Health .

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Review of the safety and efficacy of vitamin A supplementation in the treatment of children with severe acute malnutrition
Lora l iannotti.
1 Institute for Public Health/George Warren Brown School of Social Work, Washington University in St. Louis, Campus Box 1196, St. Louis, MO 63130, USA
Indi Trehan
2 Department of Pediatrics, Washington University in St. Louis, 1 Childrens Pl, St Louis, MO 63110, USA
3 Department of Paediatrics and Child Health, University of Malawi, Blantyre, Malawi
Mark J Manary
4 Department of Community Health, University of Malawi, Blantyre, Malawi
5 Children’s Nutrition Research Center, Baylor College of Medicine, Houston, Texas, USA
Associated Data
World Health Organization (WHO) guidelines recommend for children with severe acute malnutrition (SAM), high-dose vitamin A (VA) supplements be given on day 1 of admission, and on days 2 and 14 in the case of clinical signs of vitamin A deficiency (VAD). Daily low-dose VA follows, delivered in a premix added to F-75 and F-100. This study aimed to systematically review the evidence for safety and effectiveness of high-dose VA supplementation (VAS) in treatment of children with SAM.
A comprehensive literature review was undertaken for all relevant randomized controlled trials (RCT) and observational studies from 1950 to 2012. Studies identified for full review were evaluated using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) methodology using a set of pre-defined criteria: indirectness; inconsistency; imprecision; and study limitations. A quality rating of high, moderate, or low was then assigned to each study, and only those attaining moderate to high were considered in making recommendations.
Of the 2072 abstracts screened, 38 met criteria for full review, and 20 were rated moderate to high quality. Only one study replicated the WHO VA protocol in children with SAM. Indirectness was a critical limitation, as studies were not exclusive to children with SAM. There was inconsistency across trials for definitions of malnutrition, morbidities, and ages studied; and imprecision arising from sub-group analyses and small sample sizes. Evidence showed improved outcomes associated with low-dose compared to high-dose VAS, except in cases presenting with signs of VAD, measles, and severe diarrhea or shigellosis. Adverse outcomes related to respiratory infection, diarrhea, and growth were associated with high-dose VAS in children who were predominantly adequately nourished. No adverse effects of the high dose were found in children with SAM in the trial that replicated the WHO VA guideline.
This is the first systematic review of the safety and efficacy of high-dose VAS in treatment of SAM. We recommend a low-dose VAS regimen for children with SAM, except in cases presenting with measles, severe diarrhea (shigellosis), and any indication of VAD. Further research is needed in exclusively malnourished children and to explore alternate delivery strategies.
Globally, vitamin A deficiency (VAD) affects 100–140 million children, 4.4 million of whom have xerophthalmia [ 1 , 2 ]. Coverage rates for full vitamin A supplementation (VAS) of children 6–59 months delivered through primary care have risen significantly over the last decade, reaching 88% for the least developed countries [ 3 ]. In recent years, alternative strategies to improve micronutrient nutrition have been increasingly applied for high-risk populations already supplemented with vitamin A (VA): micronutrient powders; fortification of staple foods; ready-to-use supplemental and therapeutic foods (RUSF and RUTF); and other food-based approaches.
Among the populations particularly vulnerable to VAD are children with severe acute malnutrition (SAM) [ 4 ]. The World Health Organization (WHO) currently recommends that for inpatient care of children with SAM, VA supplements be given on day 1 of admission unless there is clear evidence that VA was received in the last month [ 5 ]. Dosing guidelines are the following: 200,000 international units (IU) for children over 12 months of age, 100,000 IU for children 6–12 months, and 50,000 IU for children below 6 months. If clinical signs of vitamin A deficiency are present, then another age-specific, large dose is administered on day 2 and again, on day 14 [ 4 , 5 ]. Low-dose VA is then given as part of a vitamin mix added to F-75 or F-100 therapeutic milk formulations, or alternatively, as a proprietary multivitamin supplement or combined mineral-vitamin mix (CMV). There is a need to revisit these guidelines in the context of improved VA availability, but also in view of evidence showing the potential for harmful effects of such VAS dosages [ 6 ].
This systematic review aimed to assess the safety and effectiveness of VAS in children with SAM, with regards to mortality, nutritional recovery, and signs of symptomatic VAD [ 7 ]. A literature review was undertaken to search for all randomized controlled trials (RCT) and observational studies published from 1950 to March 2012. Databases searched included MEDLINE, EMBASE, and Google Scholar. The clinical trial registries at clinicaltrials.gov, pactr.org, and apps.who.int/trialsearch were also searched. Initial key words for the searches included “malnutrition”, “severe malnutrition”, “kwashiorkor”, “marasmus”, “vitamin A”, and “retinol”. A number of outcome measures were sought, including mortality, weight gain, nutritional recovery, and VAD. Further terms were added iteratively to the search based on results obtained from the initial searches.
Searches were also conducted to identify relevant publications and study documents produced by international health organizations such as the WHO and UNICEF. The titles and abstracts were scanned to identify relevant studies. The full text of relevant studies was obtained and the list of articles for inclusion further optimized based on an evaluation of the full text. Reference lists in relevant articles were also scanned manually and electronically to identify other studies that may have been missed in the original searches. Relevant publications that cited those previously identified articles were similarly sought.
Studies were included for full review based on relevance to the population of interest, study interventions, study design, outcome measures, and an assessment of the study’s methodological rigor and quality. These studies were then assessed and entered into a Grading of Recommendations, Assessment, Development and Evaluation (GRADE) table summarizing design, aim, outcomes, GRADE criteria assessment (indirectness, inconsistency, imprecision, and study limitations), and quality ranking (high, moderate, or low) [ 8 ].
Indirectness was judged based on study relevance to the review question in terms of the study population (children with SAM), intervention of interest (VAS), and outcome measures (mortality, recovery from SAM, signs of symptomatic VAD, and adverse outcomes due to supplementation) [ 9 ]. Consideration was given under this category to VA dosing relative the WHO protocol. Inconsistency was assessed by comparing point estimates and examining the heterogeneity of methods and statistical analyses [ 10 ]. Imprecision was based primarily on the 95% confidence interval with consideration of effect and sample sizes [ 11 ]. Potential biases (selection, recall, information/observation, misclassification) arising from failure to blind, losses in follow-up, inappropriate controls, and failure to adjust for confounding factors, among other problems, were considered under the study limitations (risk of bias) criteria [ 12 ].
Once these criteria were assessed, each study was assigned a quality ranking ranging from low to high. Only those studies with some degree of moderate or high ( i.e. , low-moderate, moderate, moderate-high, or high) quality ranking were included in this review for consideration in making recommendations on the use of VAS for the treatment of children with SAM.
Of the 2072 abstracts identified and screened, 38 were selected for full review (Figure 1 ). Twenty-two were of moderate- to high-quality, and were grouped into 3 categories and listed primary outcomes assessed: 1) previous reviews; 2) observational studies; and 3) randomized controlled trials (RCT).

Flow diagram for studies included in review. The figure presents a flow diagram detailing the number of records screened and excluded, full-text articles reviewed, and ultimately, the number of studies included in the systematic review. The included observational and RCT studies are enumerated according to the primary outcome examined.
Previous reviews
Two previous reviews of VAS trials were identified; both considered malnourished children together with those not malnourished [ 7 , 13 ]. Preventive VAS reduced all-cause mortality by 25% and diarrhea-specific mortality by 30%. VA showed greater protection against morbidity and mortality in Asia than in Africa or Latin America [ 13 ]. An earlier review found that the severity of measles and diarrheal infections were reduced by VAS, but the risk of lower respiratory tract infection was increased in some trials [ 7 ]. Because the reviews did not provide new evidence for VA and management of SAM and all studies from the reviews were screened for this review, they were not included in the GRADE assessment.
Observational studies
Five observational studies were identified and assigned a GRADE quality ranking of low to moderate [ 14 - 18 ] (Additional file 1 : Table S1). These studies found significant associations between serum or plasma retinol concentrations and SAM [ 14 - 16 ]. Others established a link between VAD, SAM, and diarrhea. In Bangladesh, reduced serum retinol concentrations were associated with shigellosis and low weight-for-age Z-score [ 18 ]. Another case–control study in Bangladesh showed that the duration of diarrhea and SAM were independently associated with xerophthalmia [ 17 ].
Randomized controlled trials
Fifteen RCTs of moderate to high quality based on GRADE criteria were included in the systematic review on the safety and efficacy of high-dose VAS in children with SAM (Table 1 ). Issues of indirectness were present in all trials. Only one trial included children with SAM exclusively [ 19 ]. The remaining 14 included non-malnourished and malnourished children [ 20 - 33 ]. VA dosing also varied; only five trials administered the recommended high-dose on day 1 [ 19 , 26 , 30 , 31 , 33 ], while the remaining administered VA doses in varying quantities and forms. Only one trial followed the WHO protocol [ 19 ]; two compared high dose with daily low dose [ 26 , 33 ], and the remaining 12 compared high dose VAS with placebo [ 20 - 25 , 27 - 32 ].
Randomized controlled trials included in the systematic review
The table presents the included RCT studies in the review by date of publication, from most recent to oldest. For each study, the design, aim, quality assessment by GRADE criteria, findings, and GRADE rating are provided.
Inconsistency across trials was observed with regards to the ages of children studied, ranging from birth to 14 years. Definitions of morbidity and malnutrition varied, as well as use of differing growth references and standards. Small sample sizes and rare events were the most common problems related to imprecision . Despite randomization, several studies also showed significant differences in baseline characteristics that elevated the risk of bias . Notably, these included baseline age and nutritional status differences with higher likelihoods of confounding [ 28 , 32 , 33 ].
Some key findings were identified across trials. First, low-dose VAS conferred more or similar health and recovery advantages when compared to high-dose supplementation in the treatment of malnourished children [ 19 , 26 , 33 ]. Second, high-dose VAS showed mixed results relative to placebo for infectious disease outcomes in children with and without SAM, showing benefit in some trials for children with severe diarrhea or shigellosis [ 27 , 31 ], measles [ 21 , 22 ], other acute respiratory infections [ 30 ], and undifferentiated fever [ 24 ]. However, in other trials, there was no benefit for children with acute respiratory infections or diarrhea [ 24 - 26 , 29 , 32 ]. There was also some evidence of improved growth outcomes associated with high-dose VAS among VA deficient children [ 20 ] and children with measles [ 22 ].
Finally, adverse effects were found to be associated with high-dose VAS in some trials, including an increased rate of respiratory illnesses [ 23 , 28 ] and diarrhea [ 26 , 31 ]. These findings appear primarily in samples or sub-samples of adequately nourished children. As noted previously, we identified only one RCT that included only severely malnourished children [ 19 ]. Some explicitly excluded children with marasmus, kwashiorkor, or all children with SAM [ 25 , 27 , 30 , 32 ], while the remaining included both malnourished and adequately nourished children. Among the five studies finding adverse events in association with VAS, two of these studies carried out sub-group analyses showing an increased risk of diarrhea among normally nourished children [ 31 ] and among children without edema [ 26 ]. One trial included only adequately nourished children [ 28 ], another found increased risk of ALRI in mainly adequately nourished children [ 23 ], and one included both malnourished and adequately nourished children, excluding children with SAM [ 32 ]. No adverse effects of the high-dose VAS were found in children with SAM in the trial that replicated the WHO VA guidelines [ 19 ].
Our systematic review of the literature using the GRADE methodology revealed only limited evidence that directly addresses the safety and effectiveness of high-dose VAS for children with SAM. Fourteen of the 15 RCTs identified for this review included both malnourished and non-malnourished children, thereby complicating the extrapolation of findings directly to efficacy and safety of VAS for SAM. There is sufficient evidence to recommend the use of high-dose VAS for children with SAM when presenting with measles, severe diarrhea (shigellosis), or evidence of VAD. The low-dose VAS regimen should be considered as the preferred protocol in other cases of malnourished children, given the potential for adverse events and similar recovery outcomes when compared to high-dose VAS. Higher quality prospective studies are still needed to directly examine VAD in children with SAM, applying more contemporary definitions of morbidity and malnutrition, and powered sufficiently to detect the critical outcomes of interest.
Observational studies demonstrated an association between SAM and VAD, but metabolic disruptions in SAM might preclude accurate measures of true VA status. Blood biomarkers of retinol concentrations were primarily used to indicate VA status [ 14 - 16 , 18 ]. Protein-energy malnutrition has been associated with reduced hepatic synthesis of retinol binding protein (RBP) and transthyretin used to transport VA in the body [ 34 , 35 ]. Thus, VA stores in the liver may not be mobilized appropriately in malnourished children and therefore not be reflected in blood biomarkers. Mitra showed that VA status improved from baseline to hospital discharge, even without VAS [ 18 ]. That study also showed that while urinary losses of retinol were associated with low retinol concentrations in children with dysentery, other inflammatory markers such as body temperature and serum α-1-acid glycoprotein and C reactive protein concentrations were more highly and negatively correlated with vitamin A status.
There is some evidence that diarrhea could be mediating this relationship, as revealed by independent associations between diarrhea, low WAZ, and VA levels [ 17 ]. Shigellosis , in particular, increases the risk of VAD [ 18 ]. A study in Brazil showed a possible interaction between SAM and low serum retinol concentrations for higher diarrheal morbidities [ 15 ]. Evidence from RCTs also finds that high-dose VAS may be beneficial for treating severely malnourished children in cases of severe diarrhea [ 27 , 31 ]. Again, the mechanism by which VA may be operating to mitigate severe diarrhea in SAM has not been elucidated, but it may be either through the repair of the gut epithelium or immune pathways that restore balance between T-cell subsets [ 36 ].
Two studies showed unequivocally the benefit of lose-dose (5000 IU daily until discharge) compared to a single high-dose (200,000 IU for children over 12 months or 100,000 IU for children under 12 months on day 1 of hospitalization) VAS regimen [ 26 , 33 ]. The low-dose regimen was more strongly correlated with lower incidence and shorter duration of respiratory disease [ 33 ] and a lower incidence of severe diarrhea [ 26 ]. A third study in Bangladesh also examined the administration of a lose-dose protocol in relation to a high-dose on day 1 followed by daily low doses until hospital discharge. [ 19 ]. That study did not find any differences in the two groups on a range of morbidity and nutrition recovery outcomes and adverse events. All children at baseline had diarrhea and while clinical signs of VAD were not apparent, baseline measures of VA status did indicate VAD in the sample. With regards to other morbidities, high-dose VAS was effective in reducing measles-specific respiratory illness [ 21 , 22 ], but showed mixed results with regards to non-measles pneumonia and other acute lower respiratory tract infections in children with SAM [ 23 - 25 , 28 - 30 , 32 , 37 , 38 ].
Only one trial identified in this review specifically included children who were HIV + [ 31 ]. Sub-group analyses stratified by HIV status showed a trend towards a protective effect of high-dose VAS on cough and rapid respiratory rate for HIV-infected children [RR 0.54 (0.24-1.20), p = 0.07], while children without HIV infection were at increased risk for these conditions [RR 1.47 (1.16-1.86), p = 0.001]. Because children infected with HIV are highly vulnerable to SAM and VAD, more research is needed to understand the optimal protocols for this population [ 39 ].
The evidence for growth outcomes in the follow-up period from hospital discharge was limited and somewhat dated [ 20 , 22 ]. One study showed that only among children who were VA deficient at baseline were there greater improvements in weight and MUAC in those who received high-dose VAS; this was not evident in the non-VA deficient children and high-dose VAS even reduced height gain among non-VA deficient girls [ 20 ]. Standard therapeutic foods designed for growth recovery in SAM may be a safer source of VA in certain cases. The foods contain VA as retinyl acetate, similar to VA supplements, in the following concentrations (per 100 g): F-75, 900 μg; F-100, 800 μg; and RUTF, 800–1100 μg. Thus, for a child weighing 5 kg, this would translate into 1,119 μg/d VA for F-75, or 1,544 μg/d VA for F-100, and 1,680 μg/d VA for RUTF. These quantities are comparable to the low-dose regimen of 5000 IU or 1500 μg retinol and are well below the high-dose recommendation of 100,000 IU or 30,000 μg/d VA that would be given to children under 12 mo. While these foods have not specifically been assessed as alternatives to VAS, the safety and efficacy of these products in the treatment of SAM is well-accepted [ 40 - 42 ]. Particularly in cases when a child’s VA status is unknown or adequate, therapeutic foods could thus serve as the delivery mechanism for low-dose VAS, though more research is needed.
Adverse effects found to be associated with high-dose VAS warrant more research. The most frequent negative outcome was an increased risk of acute respiratory infections [ 23 , 28 , 31 , 33 ]. There was also evidence of an increased risk of acute, non-severe diarrhea, mediated in part by nutritional status [ 26 , 31 , 32 ]. It should be noted that the adverse effects arising from high-dose VAS were found in samples or sub-samples that included primarily adequately nourished children. Heterogeneity in baseline characteristics and study design complicates comparisons across the various studies, but these safety issues should not be ignored. Excessive intake of preformed VA, notably in the absence of dietary fatty acids, may overwhelm the esterification process and introduce more harmful forms of VA into the child’s circulation [ 6 ]. Further along the metabolic pathway, VA presented to cell membranes in forms other than the RBP complex (as may be the case in SAM) can also lead to significant cellular damage [ 43 ]. Carotenoid forms of VA or lipid-based nutrient supplements such as RUTF, should be explored to minimize oxidative stress while still addressing VAD [ 44 ].
Conclusions
In the treatment of children with SAM, a high-dose VAS protocol can be safely recommended in cases presenting with measles, severe diarrhea (shigellosis), or symptoms of VAD. More research is needed to study this specific question in populations exclusively malnourished and to understand and prevent adverse outcomes related to high-dose VAS. We recommend exploration of alternative low-dose protocols and strategies beyond VAS, such as use of carotenoids or RUTF interventions, to address VA deficiency and associated health outcomes in the treatment of children with SAM.
Abbreviations
ALRI: Acute lower respiratory infection; GRADE: Grading of recommendations assessment development and evaluation; MUAC: Mid-upper arm circumference; RCT: Randomized controlled trial; RUTF: Ready-to-use therapeutic food; SAM: Severe acute malnutrition; VA: Vitamin A; VAD: Vitamin A deficiency; VAS: Vitamin A supplementation; WAZ: Weight-for-age Z score; WHZ: Weight-for-height Z score.
Competing interests
There were no competing interests in this research.
Authors’ contributions
LLI, IT, and MJM contributed to the conception and design of the study. IT and MJM supervised the literature search and initial screening of studies. LLI carried out the full text review and initial GRADE assessment, followed by additional assessment from IT and MJM. All authors contributed to the analysis and interpretation of the compiled evidence. LLI drafted the manuscript with significant inputs received by IT and MJM. All authors have granted approval to this version of the manuscript.
Supplementary Material
Observational studies included in systematic review [ 45 ].
Acknowledgements
Funding was provided by the World Health Organization (WHO) to support the work of M. Manary and L. Iannotti.
- Black RE, Allen LH, Bhutta ZA, Caulfield LE, De Onis M, Ezzati M, Mathers C, Rivera J. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008; 371 :243–260. doi: 10.1016/S0140-6736(07)61690-0. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- West KP Jr. Extent of vitamin A deficiency among preschool children and women of reproductive age. J Nutr. 2002; 132 :2857S–2866S. [ PubMed ] [ Google Scholar ]
- UNICEF. The State of the World's Children 2012. New York: United Nations Children’s Fund; 2012. [ Google Scholar ]
- WHO. Management of severe malnutrition: a manual for physicians and other senior health workers. Geneva: World Health Organization; 1999. [ Google Scholar ]
- Ashworth A, Khanum S, Jackson A, CS. Guidelines for the inpatient treatment of severely malnourished children. Geneva: World Health Organization; 2003. [ Google Scholar ]
- Penniston KL, Tanumihardjo SA. CS. The acute and chronic toxic effects of vitamin A. Am J Clin Nutr. 2006; 83 :191–201. [ PubMed ] [ Google Scholar ]
- Villamor E, Fawzi WW. Vitamin A supplementation: implications for morbidity and mortality in children. J Infect Dis. 2000; 182 :S122–133. doi: 10.1086/315921. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D. et al. Grading quality of evidence and strength of recommendations. BMJ. 2004; 328 :1490. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Falck-Ytter Y, Jaeschke R, Vist G. GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol. 2011; 64 :1303–1310. doi: 10.1016/j.jclinepi.2011.04.014. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011; 64 :1294–1302. doi: 10.1016/j.jclinepi.2011.03.017. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, Devereaux PJ, Montori VM, Freyschuss B, Vist G. GRADE guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol. 2011; 64 :1283–1293. doi: 10.1016/j.jclinepi.2011.01.012. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias) J Clin Epidemiol. 2011; 64 :407–415. doi: 10.1016/j.jclinepi.2010.07.017. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Imdad A, Yakoob MY, Sudfeld C, Haider BA, Black RE, Bhutta ZA. Impact of vitamin A supplementation on infant and childhood mortality. BMC Publ Health. 2011; 11 Suppl 3 :S20. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ashour MN, Salem SI, El-Gadban HM, Elwan NM, Basu TK. Antioxidant status in children with protein-energy malnutrition (PEM) living in Cairo, Egypt. Eur J Clin Nutr. 1999; 53 :669–673. doi: 10.1038/sj.ejcn.1600830. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- De Fatima Costa Caminha M, Da Silva Diniz A, Falbo AR, De Arruda IK, Serva VB, De Albuquerque LL, De Freitas Lola MM, Ebrahim GJ. Serum retinol concentrations in hospitalized severe protein-energy malnourished children. J Trop Pediatr. 2008; 54 :248–252. doi: 10.1093/tropej/fmn018. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Donnen P, Brasseur D, Dramaix M, Vertongen F, Ngoy B, Zihindula M, Hennart P. Vitamin A deficiency and protein-energy malnutrition in a sample of pre-school age children in the Kivu Province in Zaire. Eur J Clin Nutr. 1996; 50 :456–461. [ PubMed ] [ Google Scholar ]
- Mahalanabis D. Breast feeding and vitamin A deficiency among children attending a diarrhoea treatment centre in Bangladesh: a case–control study. BMJ. 1991; 303 :493–496. doi: 10.1136/bmj.303.6801.493. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mitra AK, Alvarez JO, Wahed MA, Fuchs GJ, Stephensen CB. Predictors of serum retinol in children with shigellosis. Am J Clin Nutr. 1998; 68 :1088–1094. [ PubMed ] [ Google Scholar ]
- Sattar S, Ahmed T, Rasul CH, Saha D, Salam MA, Hossain MI. Efficacy of a high-dose in addition to daily low-dose vitamin A in children suffering from severe acute malnutrition with other illnesses. PloS ONE. 2012; 7 :e33112. doi: 10.1371/journal.pone.0033112. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Donnen P, Brasseur D, Dramaix M, Vertongen F, Zihindula M, Muhamiriza M, Hennart P. Vitamin A supplementation but not deworming improves growth of malnourished preschool children in eastern Zaire. J Nutr. 1998; 128 :1320–1327. [ PubMed ] [ Google Scholar ]
- Hussey GD, Klein M. A randomized, controlled trial of vitamin A in children with severe measles. N Engl J Med. 1990; 323 :160–164. doi: 10.1056/NEJM199007193230304. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coutsoudis A, Broughton M, Coovadia HM. Vitamin A supplementation reduces measles morbidity in young African children: a randomized, placebo-controlled, double-blind trial. Am J Clin Nutr. 1991; 54 :890–895. [ PubMed ] [ Google Scholar ]
- Dibley MJ, Sadjimin T, Kjolhede CL, Moulton LH. Vitamin A supplementation fails to reduce incidence of acute respiratory illness and diarrhea in preschool-age Indonesian children. J Nutr. 1996; 126 :434–442. [ PubMed ] [ Google Scholar ]
- Nacul LC, Kirkwood BR, Arthur P, Morris SS, Magalhaes M, Fink MC. Randomised, double blind, placebo controlled clinical trial of efficacy of vitamin A treatment in non-measles childhood pneumonia. BMJ. 1997; 315 :505–510. doi: 10.1136/bmj.315.7107.505. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Si NV, Grytter C, Vy NN, Hue NB, Pedersen FK. High dose vitamin A supplementation in the course of pneumonia in Vietnamese children. Acta Paediatr. 1997; 86 :1052–1055. doi: 10.1111/j.1651-2227.1997.tb14805.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Donnen P, Dramaix M, Brasseur D, Bitwe R, Vertongen F, Hennart P. Randomized placebo-controlled clinical trial of the effect of a single high dose or daily low doses of vitamin A on the morbidity of hospitalized, malnourished children. Am J Clin Nutr. 1998; 68 :1254–1260. [ PubMed ] [ Google Scholar ]
- Hossain S, Biswas R, Kabir I, Sarker S, Dibley M, Fuchs G, Mahalanabis D. Single dose vitamin A treatment in acute shigellosis in Bangladesh children: randomised double blind controlled trial. BMJ. 1998; 316 :422–426. doi: 10.1136/bmj.316.7129.422. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stephensen CB, Franchi LM, Hernandez H, Campos M, Gilman RH, Alvarez JO. Adverse effects of high-dose vitamin A supplements in children hospitalized with pneumonia. Pediatrics. 1998; 101 :E3. [ PubMed ] [ Google Scholar ]
- Faruque AS, Mahalanabis D, Haque SS, Fuchs GJ, Habte D. Double-blind, randomized, controlled trial of zinc or vitamin A supplementation in young children with acute diarrhoea. Acta Paediatr. 1999; 88 :154–160. doi: 10.1111/j.1651-2227.1999.tb01074.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Julien MR, Gomes A, Varandas L, Rodrigues P, Malveiro F, Aguiar P, Kolsteren P, Stuyft P, Hildebrand K, Labadarios D, Ferrinho P. A randomized, double-blind, placebo-controlled clinical trial of vitamin A in Mozambican children hospitalized with nonmeasles acute lower respiratory tract infections. Trop Med Int Health. 1999; 4 :794–800. doi: 10.1046/j.1365-3156.1999.00493.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fawzi WW, Mbise R, Spiegelman D, Fataki M, Hertzmark E, Ndossi G. Vitamin A supplements and diarrheal and respiratory tract infections among children in Dar es Salaam, Tanzania. J Pediatr. 2000; 137 :660–667. doi: 10.1067/mpd.2000.110136. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mahalanabis D, Lahiri M, Paul D, Gupta S, Gupta A, Wahed MA, Khaled MA. Randomized, double-blind, placebo-controlled clinical trial of the efficacy of treatment with zinc or vitamin A in infants and young children with severe acute lower respiratory infection. Am J Clin Nutr. 2004; 79 :430–436. [ PubMed ] [ Google Scholar ]
- Donnen P, Sylla A, Dramaix M, Sall G, Kuakuvi N, Hennart P. Effect of daily low dose of vitamin A compared with single high dose on morbidity and mortality of hospitalized mainly malnourished children in Senegal: a randomized controlled clinical trial. Eur J Clin Nutr. 2007; 61 :1393–1399. doi: 10.1038/sj.ejcn.1602671. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jain MK, Mehta NJ, Fonseca M, Pai NV. Correlation of serum vitamin A and its transport protein (RBP) in malnourished and vitamin A deficient children. J Postgrad Med. 1990; 36 :119–123. [ PubMed ] [ Google Scholar ]
- Rosales FJ, Ritter SJ, Zolfaghari R, Smith JE, Ross AC. Effects of acute inflammation on plasma retinol, retinol-binding protein, and its mRNA in the liver and kidneys of vitamin A-sufficient rats. J Lipid Res. 1996; 37 :962–971. [ PubMed ] [ Google Scholar ]
- Semba RD, Ward BJ, Griffin DE, Scott AL, Natadisastra G, West KP Jr, Sommer A. Muhilal. Abnormal T-cell subset proportions in vitamin-A-deficient children. Lancet. 1993; 341 :5–8. doi: 10.1016/0140-6736(93)92478-C. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Daulaire NM, Starbuck ES, Houston RM, Church MS, Stukel TA, Pandey MR. Childhood mortality after a high dose of vitamin A in a high risk population. BMJ. 1992; 304 :207–210. doi: 10.1136/bmj.304.6821.207. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kjolhede CL, Chew FJ, Gadomski AM, Marroquin DP. Clinical trial of vitamin A as adjuvant treatment for lower respiratory tract infections. J Pediatr. 1995; 126 :807–812. doi: 10.1016/S0022-3476(95)70416-7. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Trehan I, O’Hare BA, Phiri A, Heikens GT. Challenges in the Management of HIV-Infected Malnourished Children in Sub-Saharan Africa. AIDS Research and Treatment. 2012; 2012 :790786. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Manary MJ, Sandige HL. Management of acute moderate and severe childhood malnutrition. BMJ. 2008; 337 :1227–1230. doi: 10.1136/bmj.a1227. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Trehan I, Goldbach HS, LaGrone LN, Meuli GJ, Wang RJ, Maleta KM, Manary MJ. Antibiotics as part of the management of severe acute malnutrition. N Engl J Med. 2013; 368 :425–435. doi: 10.1056/NEJMoa1202851. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- WHO. Community-based management of severe acute malnutrition. Geneva: World Health Organization, World Food Programme, United Nations System Standing Committee on Nutrition, United Nations Children’s Fund; 2007. [ Google Scholar ]
- Creek KE, St Hilaire P, Hodam JR. A comparison of the uptake, metabolism and biologic effects of retinol delivered to human keratinocytes either free or bound to serum retinol-binding protein. J Nutr. 1993; 123 :356–361. [ PubMed ] [ Google Scholar ]
- Celik M, Sermatov K, Abuhandan M, Zeyrek D, Kocyigit A, Iscan A. Oxidative status and DNA damage in chidren with marasmic malnutrition. J Clin Lab Anal. 2012; 26 :161–166. doi: 10.1002/jcla.21505. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yang H, De Onis M. Algorithms for converting estimates of child malnutrition based on the NCHS reference into estimates based on the WHO Child Growth Standards. BMC Pediatr. 2008; 8 :19. doi: 10.1186/1471-2431-8-19. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Vitamin B12 deficiency-induced megaloblastic anemia in a pediatric patient with autism spectrum disorder with a chronically unbalanced diet
- Case Report
- Published: 25 March 2024
Cite this article
- Yuri Sawada 1 ,
- Kenichi Sakamoto ORCID: orcid.org/0000-0003-1499-538X 1 ,
- Atsushi Tsukamura 1 &
- Chihiro Sawai 1
36 Accesses
1 Altmetric
Explore all metrics
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by a lack of behavioral flexibility and stereotyped language. Food selectivity is common among children with ASD because of their persnickety nature. A prolonged unbalanced diet results in an increased risk of several diseases, such as iron deficiency anemia, scurvy, rickets, dry eye, and Wernicke encephalopathy. However, no cases of megaloblastic anemia have been reported to date. We report the case of an 11-year-old boy with ASD who developed megaloblastic anemia due to vitamin B12 deficiency. He had a prolonged history of selective eating for more than 10 years. His nutritional status on admission was poor, and he had low weight and short stature. His food selectivity was so strong that intervention to expand diet variety was unsuccessful. A developmental-behavioral pediatrician found that the patient had visual dominance and could take some medications when suffering from a minor illness. Nutritional supplements were selected after consultation with a nutritionist. Although compulsory treatment was necessary during the acute phase, the therapy was continued at home. With multidisciplinary intervention tailored to the patient and his parents’ characteristics, his nutritional status improved in a few months.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
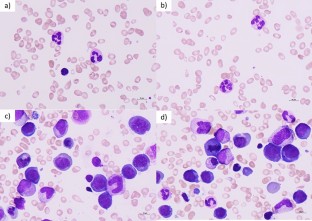
Similar content being viewed by others

Autism Spectrum Disorder in a Child with Propionic Acidemia

Vitamin B12 deficiency as a cause of severe neurological symptoms in breast fed infant – a case report
Cezary Dubaj, Katarzyna Czyż & Wanda Furmaga-Jabłońska

Overview of Nutritional Therapy for Autism Spectrum Disorder
Data availability.
The data supporting the findings of this study are not openly available because this manuscript has no associated data.
Hubbard KL, Anderson SE, Curtin C, Must A, Bandini LG. A comparison of food refusal related to characteristics of food in children with autism spectrum disorder and typically developing children. J Acad Nutr Diet. 2014;114:1981–7.
Article PubMed PubMed Central Google Scholar
Robea M-A, Luca A-C, Ciobica A. Relationship between vitamin deficiencies and co-occurring symptoms in autism spectrum disorder. Medicina. 2020;56:245.
Zimmer MH, Hart LC, Manning-Courtney P, Murray DS, Bing NM, Summer S. Food variety as a predictor of nutritional status among children with autism. J Autism Dev Disord. 2012;42:549–56.
Sharp WG, Berry RC, McCracken C, Nuhu NN, Marvel E, Saulnier CA, et al. Feeding problems and nutrient intake in children with autism spectrum disorders: a meta-analysis and comprehensive review of the literature. J Autism Dev Disord. 2013;43:2159–73.
Article PubMed Google Scholar
Elangovan R, Baruteau J. Inherited and acquired vitamin B12 deficiencies: which administration route to choose for supplementation? Front Pharmacol. 2022;13:972468.
Article CAS PubMed PubMed Central Google Scholar
Conti MV, Breda C, Basilico S, Luzzi A, Voto L, Santero S, et al. Dietary recommendations to customize canteen menus according to the nutritional and sensory needs of individuals with autism spectrum disorder. Eat Weight Disord. 2023;28:66.
Download references
Acknowledgements
Consent for publication of the case was obtained from the patient’s parents.
Author information
Authors and affiliations.
Department of Pediatrics, Shiga University of Medical Science, Seta Tsukinowa-cho, Otsu, Shiga, 520-2192, Japan
Yuri Sawada, Kenichi Sakamoto, Atsushi Tsukamura & Chihiro Sawai
You can also search for this author in PubMed Google Scholar
Contributions
Y.S. and K.S. designed the study. Y. S. drafted the manuscript. A.T. and C.S. reviewed the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Correspondence to Kenichi Sakamoto .
Ethics declarations
Conflict of interest.
The authors declare no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Sawada, Y., Sakamoto, K., Tsukamura, A. et al. Vitamin B12 deficiency-induced megaloblastic anemia in a pediatric patient with autism spectrum disorder with a chronically unbalanced diet. Int J Hematol (2024). https://doi.org/10.1007/s12185-024-03759-3
Download citation
Received : 04 December 2023
Revised : 11 March 2024
Accepted : 14 March 2024
Published : 25 March 2024
DOI : https://doi.org/10.1007/s12185-024-03759-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Megaloblastic anemia
- Vitamin B12 deficiency
- Unbalanced diet
- Autism spectrum disorder
- Find a journal
- Publish with us
- Track your research
Autoimmune Thyroiditis and Vitamin D
Affiliations.
- 1 Department of Pediatrics, School of Medicine, University of Navarra, 431008 Pamplona, Spain.
- 2 Navarrabiomed (Biomedical Research Center), 31008 Pamplona, Spain.
- 3 Department of Pediatrics, Navarra Hospital Complex, 31008 Pamplona, Spain.
- PMID: 38542128
- PMCID: PMC10969999
- DOI: 10.3390/ijms25063154
Hashimoto's thyroiditis (HT) is marked by self-tissue destruction as a consequence of an alteration in the adaptive immune response that entails the evasion of immune regulation. Vitamin D carries out an immunomodulatory role that appears to promote immune tolerance. The aim of this study is to elaborate a narrative review of the relationship between vitamin D status and HT and the role of vitamin D supplementation in reducing HT risk by modulating the immune system. There is extensive literature confirming that vitamin D levels are significantly lower in HT patients compared to healthy people. On the other hand, after the supplementation with cholecalciferol in patients with HT and vitamin D deficiency, thyroid autoantibody titers decreased significantly. Further knowledge of the beneficial effects of vitamin D in the prevention and treatment of autoimmune thyroid diseases requires the execution of additional randomized, double-blind, placebo-controlled trials and longer follow-up periods.
Keywords: Hashimoto thyroiditis; anti-thyroglobulin antibodies; anti-thyroid peroxidase; autoimmune thyroiditis; autoimmunity; immune cells; vitamin D; vitamin D deficiency; vitamin D supplementation.
Publication types
- Hashimoto Disease* / drug therapy
- Randomized Controlled Trials as Topic
- Vitamin D / therapeutic use
- Vitamin D Deficiency* / complications
- Vitamin D Deficiency* / drug therapy
- Vitamins / therapeutic use
Grants and funding

IMAGES
VIDEO
COMMENTS
Vitamin A is a fat-soluble vitamin essential in cell development, metabolism, immune competency, vision, and reproductive functions.[1][2] Vitamin A deficiency (VAD) is a highly prevalent health concern associated with substantial morbidity and mortality, mostly affecting young children in impoverished regions throughout the world. Insufficient intake of absorption leads to deficiency and ...
INTRODUCTION. Vitamin A is an essential component of the human diet. It is derived from vitamin-A-rich foods as well as from foods containing beta-carotene, composed of two retinol molecules. 1 Retinoic acid (RA) is the active metabolite of vitamin A and is a critical signaling molecule for both the developing and adult central nervous system (CNS). RA is synthesized more by the CNS than by ...
Assessment of the relative level of vitamin A nutriture in human populations when clinical signs and symptoms of deficiency or of toxicity are absent has presented methodological difficulties. Commonly used indicators include dietary intakes of the vitamin, serum levels, and dark adaptation, all of which have limitations in their precision, especially when applied to individuals and to young ...
Introduction. Vitamin A deficiency (VAD) is the leading cause of childhood blindness worldwide, despite being considered eradicated in developed countries [].There are certain populations, such as children with autism spectrum disorder, who are at risk for VAD [2-6].In areas with low prevalence of VAD, a delay in evaluation, diagnosis and management often occurs, leading to major systemic ...
Vitamin A deficiency (VAD) is a highly prevalent health concern associated with substantial morbidity and mortality, mostly affecting young children in impoverished regions throughout the world. Insufficient intake of absorption leads to deficiency and compromise of essential physiologic processes. Natural sources of vitamin A include dark ...
A literature review of the periods 2012 to 2018, focusing on vitamins A, B12, and D, calcium, iron and folate, was completed as these micronutrients are found to significantly affect the aging process. ... Effects of vitamin A deficiency include neurodegeneration, physiological function of steroid and thyroid hormones, and historically, vision ...
Vitamin A deficiency (VAD) is a widespread public health problem in the developing world and the ... Review studies, to be distinguished from meta-analyses, summarize evidence in the literature around specific questions without combining and analysing the primary data. Two reviews of vitamin A
Vitamin A deficiency is a major health risk for infants and children in low- and middle-income countries. This scoping review identified, quantified, and mapped research for use in updating nutrient requirements and upper limits for vitamin A in children aged 0 to 48 months, using health-based or modelling-based approaches. Structured searches were run on Medline, EMBASE, and Cochrane Central ...
This new book, written by leading investigators in the field, is the first to synthesize the many important studies to date. The authors identify and quantify the biological, clinical and public health impact of vitamin A deficiency on childhood growth, mortality and morbidity, including anemia and blindness.
WHO recommends vitamin A supplementation (VAS) programmes for children 6-59 months where vitamin A deficiency is a public health problem. However, resources for VAS are falling short of current ...
Methods: Critical review of the literature on the dietary gap in vitamin A intake and levels of wheat flour intake among risk groups as a basis for determining vitamin A fortificant levels.
Background: Vitamin A deficiency (VAD) is widely recognised as a major public health concern in low- and middle-income countries (LMICs). Despite various interventions implemented in many countries, a lack of reliable data is hindering progress. We aimed to consolidate available data and quantify estimates of the prevalence of VAD among children ≤18 years in LMICs.
nutrients Review Vitamin A Supplementation Programs and Country-Level Evidence of Vitamin A Deficiency James P. Wirth 1,*, Nicolai Petry 1, Sherry A. Tanumihardjo 2, Lisa M. Rogers 3, Erin McLean 4, Alison Greig 5, Greg S. Garrett 6, Rolf D. W. Klemm 7,8 and Fabian Rohner 1 1 GroundWork, 7306 Fläsch, Switzerland; [email protected] (N.P.); [email protected] (F.R.)
Objective: To evaluate the evidence that carotene-rich fruits and vegetables can overcome vitamin A deficiency. Design: Results of studies on the relationship between dietary carotenoids and vitamin A deficiency were evaluated critically. Results: Increased intake of fruits and vegetables has been shown to be related to improved vitamin A status in many cross-sectional, case-control and ...
Vitamin A deficiency (VAD) is widely recognised as a major public health concern across many low- and middle-income countries (LMICs) [].It is widely acknowledged as a leading micronutrient deficiency with adverse impacts on pregnancy, child growth and development [2,3].Approximately one-third of children under the age of five have VAD, contributing to approximately 2% of deaths in this age ...
Vitamin A is important for normal vision, the immune system, reproduction, and growth, development and helps to keep the heart, lungs, and other organs work properly [87]. Vitamin C is essential ...
Vitamin A (VA) is critical for many biological processes, including embryonic development, hormone production and function, the maintenance and modulation of immunity, and the homeostasis of epithelium and mucosa. Specifically, VA affects cell integrity, cytokine production, innate immune cell activation, antigen presentation, and lymphocyte trafficking to mucosal surfaces. VA also has been ...
Background World Health Organization (WHO) guidelines recommend for children with severe acute malnutrition (SAM), high-dose vitamin A (VA) supplements be given on day 1 of admission, and on days 2 and 14 in the case of clinical signs of vitamin A deficiency (VAD). Daily low-dose VA follows, delivered in a premix added to F-75 and F-100. This study aimed to systematically review the evidence ...
Status epilepticus secondary to hypocalcemia due to vitamin D deficiency is a rare presentation and is sparsely reported in the literature. 6 The presence of both PTC syndrome and status epilepticus is an exceedingly rare presentation of this common nutritional deficiency and we aim to describe it with this case report.
Vitamin A deficiency (VAD) continues to be a major nutritional problem of public health concern in India, despite the implementation of a programme for vitamin A supplementation for over four decades.
Background: Vitamin A deficiency (VAD) increases risk for morbidity and mortality. Food-based approaches offer one strategy to improve vitamin A status. Objective: This systematic review assessed evidence of the effects of food-based approaches on the vitamin A status of women and children under five years. Methods: VAD was defined as clinical ocular symptoms, such as loss of vision, and/or ...
A Quick Review. Vitamin B12 deficiency can lead to physical, psychological, and neurological symptoms. Physical symptoms of B12 deficiency may include diarrhea, fatigue, muscle weakness, lack of ...
A Quick Review. A deficiency in vitamin B6 can lead to mental health symptoms like depression, irritability, and brain fog. It can also cause sores, cracks, and swelling on the mouth or tongue, as ...
Besides the arguments stressing vitamin A deficiency is not a public health problem in the country and the dietary inadequacy of vitamin A is low, the Expert Committee has presented an additional viewpoint for the discontinuation of VAS programme. ... I am extremely thankful to Dr. G.Sarika, Scientist-B, for her help in the review of literature ...
A Quick Review . Vitamin D is a vital nutrient for your bones, muscles, nerves, and immune system. Too little vitamin D can lead to fatigue, frequent illness or bone fractures, hair loss, and ...
Abstract. An evidence-based systematic review of vitamin A by the Natural Standard Research Collaboration consolidates the safety and efficacy data available in the scientific literature using a validated and reproducible grading rationale. This paper includes written and statistical analysis of clinical trials, plus a compilation of expert ...
2.4 Literature review. We searched in PubMed, China National Knowledge Infrastructure, and Wanfang Database for articles published before June 2023. Articles selection criteria included: (1) case reports of PSAT1 variants, (2) the individual has both defined variants and clinical manifestations, and (3) language was limited to English and Chinese.
Globally, vitamin A deficiency (VAD) affects 100-140 million children, 4.4 million of whom have xerophthalmia [1,2]. ... A literature review was undertaken to search for all randomized controlled trials (RCT) and observational studies published from 1950 to March 2012. Databases searched included MEDLINE, EMBASE, and Google Scholar.
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by a lack of behavioral flexibility and stereotyped language. Food selectivity is common among children with ASD because of their persnickety nature. A prolonged unbalanced diet results in an increased risk of several diseases, such as iron deficiency anemia, scurvy, rickets, dry eye, and Wernicke encephalopathy ...
The aim of this study is to elaborate a narrative review of the relationship between vitamin D status and HT and the role of vitamin D supplementation in reducing HT risk by modulating the immune system. There is extensive literature confirming that vitamin D levels are significantly lower in HT patients compared to healthy people.