- Research article
- Open access
- Published: 24 October 2019

A scoping review of the literature on the current mental health status of physicians and physicians-in-training in North America
- Mara Mihailescu ORCID: orcid.org/0000-0001-6878-1024 1 &
- Elena Neiterman 2
BMC Public Health volume 19 , Article number: 1363 ( 2019 ) Cite this article
26k Accesses
56 Citations
11 Altmetric
Metrics details
This scoping review summarizes the existing literature regarding the mental health of physicians and physicians-in-training and explores what types of mental health concerns are discussed in the literature, what is their prevalence among physicians, what are the causes of mental health concerns in physicians, what effects mental health concerns have on physicians and their patients, what interventions can be used to address them, and what are the barriers to seeking and providing care for physicians. This review aims to improve the understanding of physicians’ mental health, identify gaps in research, and propose evidence-based solutions.
A scoping review of the literature was conducted using Arksey and O’Malley’s framework, which examined peer-reviewed articles published in English during 2008–2018 with a focus on North America. Data were summarized quantitatively and thematically.
A total of 91 articles meeting eligibility criteria were reviewed. Most of the literature was specific to burnout ( n = 69), followed by depression and suicidal ideation ( n = 28), psychological harm and distress ( n = 9), wellbeing and wellness ( n = 8), and general mental health ( n = 3). The literature had a strong focus on interventions, but had less to say about barriers for seeking help and the effects of mental health concerns among physicians on patient care.
Conclusions
More research is needed to examine a broader variety of mental health concerns in physicians and to explore barriers to seeking care. The implication of poor physician mental health on patients should also be examined more closely. Finally, the reviewed literature lacks intersectional and longitudinal studies, as well as evaluations of interventions offered to improve mental wellbeing of physicians.
Peer Review reports
The World Health Organization (WHO) defines mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.” [ 41 ] One in four people worldwide are affected by mental health concerns [ 40 ]. Physicians are particularly vulnerable to experiencing mental illness due to the nature of their work, which is often stressful and characterized by shift work, irregular work hours, and a high pressure environment [ 1 , 21 , 31 ]. In North America, many physicians work in private practices with no access to formal institutional supports, which can result in higher instances of social isolation [ 13 , 27 ]. The literature on physicians’ mental health is growing, partly due to general concerns about mental wellbeing of health care workers and partly due to recognition that health care workers globally are dissatisfied with their work, which results in burnout and attrition from the workforce [ 31 , 34 ]. As a consequence, more efforts have been made globally to improve physicians’ mental health and wellness, which is known as “The Quadruple Aim.” [ 34 ] While the literature on mental health is flourishing, however, it has not been systematically summarized. This makes it challenging to identify what is being done to improve physicians’ wellbeing and which solutions are particularly promising [ 7 , 31 , 33 , 37 , 38 ]. The goal of our paper is to address this gap.
This paper explores what is known from the existing peer-reviewed literature about the mental health status of physicians and physicians-in-training in North America. Specifically, we examine (1) what types of mental health concerns among physicians are commonly discussed in the literature; (2) what are the reported causes of mental health concerns in physicians; (3) what are the effects that mental health concerns may have on physicians and their patients; (4) what solutions are proposed to improve mental health of physicians; and (5) what are the barriers to seeking and providing care to physicians with mental health concerns. Conducting this scoping review, our goal is to summarize the existing research, identifying the need for a subsequent systematic review of the literature in one or more areas under the study. We also hope to identify evidence-based interventions that can be utilized to improve physicians’ mental wellbeing and to suggest directions for future research [ 2 ]. Evidence-based interventions might have a positive impact on physicians and improve the quality of patient care they provide.
A scoping review of the academic literature on the mental health of physicians and physicians-in-training in North America was conducted using Arksey and O’Malley’s [ 2 ] methodological framework. Our review objectives and broad focus, including the general questions posed to conduct the review, lend themselves to a scoping review approach, which is suitable for the analysis of a broader range of study designs and methodologies [ 2 ]. Our goal was to map the existing research on this topic and identify knowledge gaps, without making any prior assumptions about the literature’s scope, range, and key findings [ 29 ].
Stage 1: identify the research question
Following the guidelines for scoping reviews [ 2 ], we developed a broad research question for our literature search, asking what does the academic literature tell about mental health issues among physicians, residents, and medical students in North America ? Burnout and other mental health concerns often begin in medical training and continue to worsen throughout the years of practice [ 31 ]. Recognizing that the study and practice of medicine plays a role in the emergence of mental health concerns, we focus on practicing physicians – general practitioners, specialists, and surgeons – and those who are still in training – residents and medical students. We narrowed down the focus of inquiry by asking the following sub-questions:
What types of mental health concerns among physicians are commonly discussed in the literature?
What are the reported causes of mental health problems in physicians and what solutions are available to improve the mental wellbeing of physicians?
What are the barriers to seeking and providing care to physicians suffering from mental health problems?
Stage 2: identify the relevant studies
We included in our review empirical papers published during January 2008–January 2018 in peer-reviewed journals. Our exclusive focus on peer-reviewed and empirical literature reflected our goal to develop an evidence-based platform for understanding mental health concerns in physicians. Since our focus was on prevalence of mental health concerns and promising practices available to physicians in North America, we excluded articles that were more than 10 years old, suspecting that they might be too outdated for our research interest. We also excluded papers that were not in English or outside the region of interest. Using combinations of keywords developed in consultation with a professional librarian (See Table 1 ), we searched databases PUBMed, SCOPUS, CINAHL, and PsychNET. We also screened reference lists of the papers that came up in our original search to ensure that we did not miss any relevant literature.
Stage 3: literature selection
Publications were imported into a reference manager and screened for eligibility. During initial abstract screening, 146 records were excluded for being out of scope, 75 records were excluded for being outside the region of interest, and 4 papers were excluded because they could not be retrieved. The remaining 91 papers were included into the review. Figure 1 summarizes the literature search and selection.
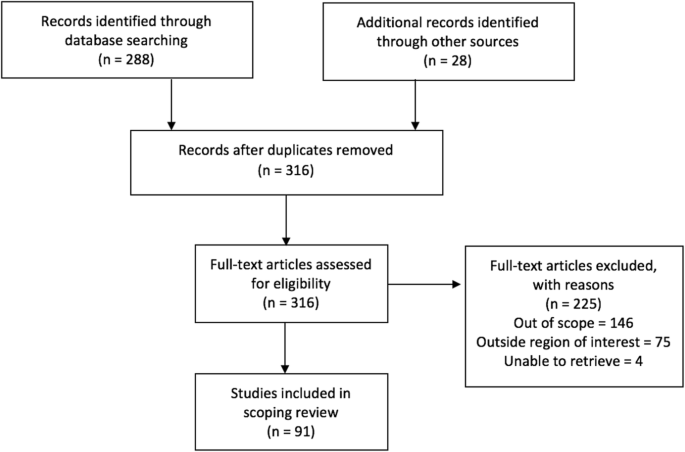
PRISMA Flow Diagram
Stage 4: charting the data
A literature extraction tool was created in Microsoft Excel to record the author, date of publication, location, level of training, type of article (empirical, report, commentary), and topic. Both authors coded the data inductively, first independently reading five articles and generating themes from the data, then discussing our coding and developing a coding scheme that was subsequently applied to ten more papers. We then refined and finalized the coding scheme and used it to code the rest of the data. When faced with disagreements on narrowing down the themes, we discussed our reasoning and reached consensus.
Stage 5: collating, summarizing, and reporting the results
The data was summarized by frequency and type of publication, mental health topics, and level of training. The themes inductively derived from the data included (1) description of mental health concerns affecting physicians and physicians-in-training; (2) prevalence of mental health concerns among this population; (3) possible causes that can explain the emergence of mental health concerns; (4) solutions or interventions proposed to address mental health concerns; (5) effects of mental health concerns on physicians and on patient outcomes; and (6) barriers for seeking and providing help to physicians afflicted with mental health concerns. Each paper was coded based on its relevance to major theme(s) and, if warranted, secondary focus. Therefore, one paper could have been coded in more than one category. Upon analysis, we identified the gaps in the literature.
Characteristics of included literature
The initial search yielded 316 records of which 91 publications underwent full-text review and were included in our scoping review. Our analysis revealed that the publications appear to follow a trend of increase over the course of the last decade reflecting the growing interest in physicians’ mental health. More than half of the literature was published in the last 4 years included in the review, from 2014 to 2018 ( n = 55), with most publications in 2016 ( n = 18) (Fig. 2 ). The majority of papers ( n = 36) focused on practicing physicians, followed by papers on residents ( n = 22), medical students ( n = 21), and those discussing medical professionals with different level of training ( n = 12). The types of publications were mostly empirical ( n = 71), of which 46 papers were quantitative. Furthermore, the vast majority of papers focused on the United States of America (USA) ( n = 83), with less than 9% focusing on Canada ( n = 8). The frequency of identified themes in the literature is broken down into prevalence of mental health concerns ( n = 15), causes of mental health concerns ( n = 18), effects of mental health concerns on physicians and patients ( n = 12), solutions and interventions for mental health concerns ( n = 46), and barriers to seeking and providing care for mental health concerns ( n = 4) (Fig. 3 ).
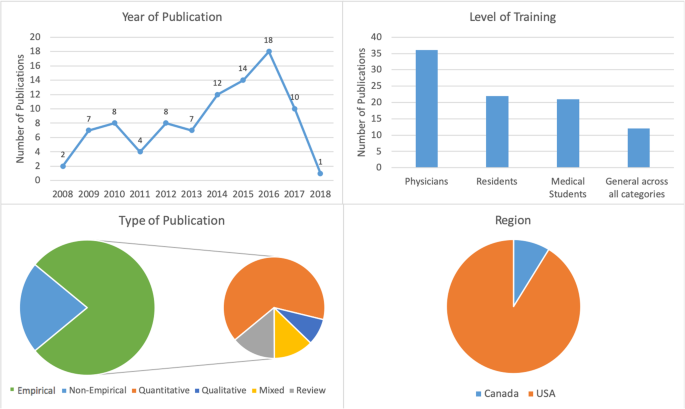
Number of sources by characteristics of included literature
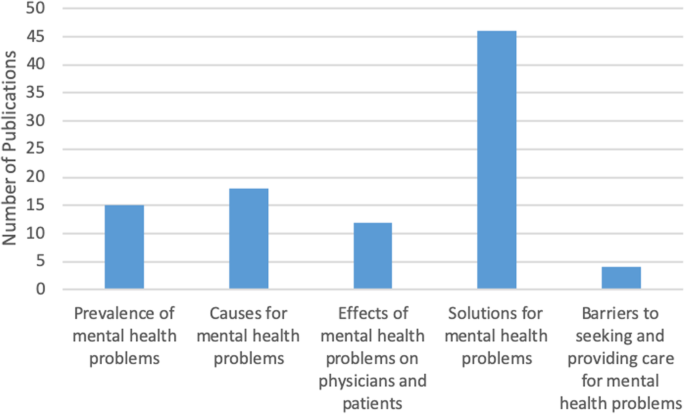
Frequency of themes in literature ( n = 91)
Mental health concerns and their prevalence in the literature
In this thematic category ( n = 15), we coded the papers discussing the prevalence of specific mental health concerns among physicians and those comparing physicians’ mental health to that of the general population. Most papers focused on burnout and stress ( n = 69), which was followed by depression and suicidal ideation ( n = 28), psychological harm and distress ( n = 9), wellbeing and wellness ( n = 8), and general mental health ( n = 3) (Fig. 4 ). The literature also identified that, on average, burnout and mental health concerns affect 30–60% of all physicians and residents [ 4 , 5 , 8 , 9 , 15 , 25 , 26 ].
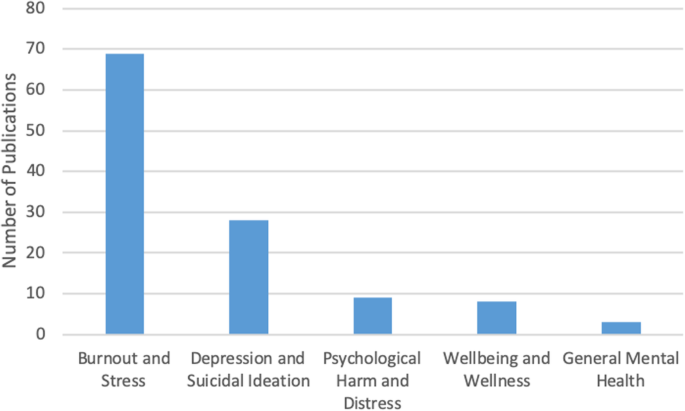
Number of sources by mental health topic discussed ( n = 91)
There was some overlap between the papers discussing burnout, depression, and suicidal ideation, suggesting that work-related stress may lead to the emergence of more serious mental health problems [ 3 , 12 , 21 ], as well as addiction and substance abuse [ 22 , 27 ]. Residency training was shown to produce the highest rates of burnout [ 4 , 8 , 19 ].
Causes of mental health concerns
Papers discussing the causes of mental health concerns in physicians formed the second largest thematic category ( n = 18). Unbalanced schedules and increasing administrative work were defined as key factors in producing poor mental health among physicians [ 4 , 5 , 6 , 13 , 15 , 27 ]. Some papers also suggested that the nature of the medical profession itself – competitive culture and prioritizing others – can lead to the emergence of mental health concerns [ 23 , 27 ]. Indeed, focus on qualities such as rigidity, perfectionism, and excessive devotion to work during the admission into medical programs fosters the selection of students who may be particularly vulnerable to mental illness in the future [ 21 , 24 ]. The third cluster of factors affecting mental health stemmed from structural issues, such as pressure from the government and insurance, fragmentation of care, and budget cuts [ 13 , 15 , 18 ]. Work overload, lack of control over work environment, lack of balance between effort and reward, poor sense of community among staff, lack of fairness and transparency by decision makers, and dissonance between one’s personal values and work tasks are the key causes for mental health concerns among physicians [ 20 ]. Govardhan et al. conceptualized causes for mental illness as having a cyclical nature - depression leads to burnout and depersonalization, which leads to patient dissatisfaction, causing job dissatisfaction and more depression [ 19 ].
Effects of mental health concerns on physicians and patients
A relatively small proportion of papers (13%) discussed the effects of mental health concerns on physicians and patients. The literature prioritized the direct effect of mental health on physicians ( n = 11) with only one paper focusing solely on the indirect effects physicians’ mental health may have on patients. Poor mental health in physicians was linked to decreased mental and physical health [ 3 , 14 , 15 ]. In addition, mental health concerns in physicians were associated with reduction in work hours and the number of patients seen, decrease in job satisfaction, early retirement, and problems in personal life [ 3 , 5 , 15 ]. Lu et al. found that poor mental health in physicians may result in increased medical errors and the provision of suboptimal care [ 25 ]. Thus physicians’ mental wellbeing is linked to the quality of care provided to patients [ 3 , 4 , 5 , 10 , 17 ].
Solutions and interventions
In this largest thematic category ( n = 46) we coded the literature that offered solutions for improving mental health among physicians. We identified four major levels of interventions suggested in the literature. A sizeable proportion of literature discussed the interventions that can be broadly categorized as primary prevention of mental illness. These papers proposed to increase awareness of physicians’ mental health and to develop strategies that can help to prevent burnout from occurring in the first place [ 4 , 12 ]. Some literature also suggested programs that can help to increase resilience among physicians to withstand stress and burnout [ 9 , 20 , 27 ]. We considered the papers referring to the strategies targeting physicians currently suffering from poor mental health as tertiary prevention . This literature offered insights about mindfulness-based training and similar wellness programs that can increase self-awareness [ 16 , 18 , 27 ], as well as programs aiming to improve mental wellbeing by focusing on physical health [ 17 ].
While the aforementioned interventions target individual physicians, some literature proposed workplace/institutional interventions with primary focus on changing workplace policies and organizational culture [ 4 , 13 , 23 , 25 ]. Reducing hours spent at work and paperwork demands or developing guidelines for how long each patient is seen have been identified by some researchers as useful strategies for improving mental health [ 6 , 11 , 17 ]. Offering access to mental health services outside of one’s place of employment or training could reduce the fear of stigmatization at the workplace [ 5 , 12 ]. The proposals for cultural shift in medicine were mainly focused on promoting a less competitive culture, changing power dynamics between physicians and physicians-in-training, and improving wellbeing among medical students and residents. The literature also proposed that the medical profession needs to put more emphasis on supporting trainees, eliminating harassment, and building strong leadership [ 23 ]. Changing curriculum for medical students was considered a necessary step for the cultural shift [ 20 ]. Finally, while we only reviewed one paper that directly dealt with the governmental level of prevention, we felt that it necessitated its own sub-thematic category because it identified the link between government policy, such as health care reforms and budget cuts, and the services and care physicians can provide to their patients [ 13 ].
Barriers to seeking and providing care
Only four papers were summarized in this thematic category that explored what the literature says about barriers for seeking and providing care for physicians suffering from mental health concerns. Based on our analysis, we identified two levels of factors that can impact access to mental health care among physicians and physicians-in-training.
Individual level barriers stem from intrinsic barriers that individual physicians may experience, such as minimizing the illness [ 21 ], refusing to seek help or take part in wellness programs [ 14 ], and promoting the culture of stoicism [ 27 ] among physicians. Another barrier is stigma associated with having a mental illness. Although stigma might be experienced personally, literature suggests that acknowledging the existence of mental health concerns may have negative consequences for physicians, including loss of medical license, hospital privileges, or professional advancement [ 10 , 21 , 27 ].
Structural barriers refer to the lack of formal support for mental wellbeing [ 3 ], poor access to counselling [ 6 ], lack of promotion of available wellness programs [ 10 ], and cost of treatment. Lack of research that tests the efficacy of programs and interventions aiming to improve mental health of physicians makes it challenging to develop evidence-based programs that can be implemented at a wider scale [ 5 , 11 , 12 , 18 , 20 ].
Our analysis of the existing literature on mental health concerns in physicians and physicians-in-training in North America generated five thematic categories. Over half of the reviewed papers focused on proposing solutions, but only a few described programs that were empirically tested and proven to work. Less common were papers discussing causes for deterioration of mental health in physicians (20%) and prevalence of mental illness (16%). The literature on the effects of mental health concerns on physicians and patients (13%) focused predominantly on physicians with only a few linking physicians’ poor mental health to medical errors and decreased patient satisfaction [ 3 , 4 , 16 , 24 ]. We found that the focus on barriers for seeking and receiving help for mental health concerns (4%) was least prevalent. The topic of burnout dominated the literature (76%). It seems that the nature of physicians’ work fosters the environment that causes poor mental health [ 1 , 21 , 31 ].
While emphasis on burnout is certainly warranted, it might take away the attention paid to other mental health concerns that carry more stigma, such as depression or anxiety. Establishing a more explicit focus on other mental health concerns might promote awareness of these problems in physicians and reduce the fear such diagnosis may have for doctors’ job security [ 10 ]. On the other hand, utilizing the popularity and non-stigmatizing image of “burnout” might be instrumental in developing interventions promoting mental wellbeing among a broad range of physicians and physicians-in-training.
Table 2 summarizes the key findings from the reviewed literature that are important for our understanding of physician mental health. In order to explicitly summarize the gaps in the literature, we mapped them alongside the areas that have been relatively well studied. We found that although non-empirical papers discussed physicians’ mental wellbeing broadly, most empirical papers focused on medical specialty (e.g. neurosurgeons, family medicine, etc.) [ 4 , 8 , 15 , 19 , 25 , 28 , 35 , 36 ]. Exclusive focus on professional specialty is justified if it features a unique context for generation of mental health concerns, but it limits the ability to generalize the findings to a broader population of physicians. Also, while some papers examined the impact of gender on mental health [ 7 , 32 , 39 ], only one paper considered ethnicity as a potential factor for mental health concerns and found no association [ 4 ]. Given that mental health in the general population varies by gender, ethnicity, age, and sexual orientation, it would be prudent to examine mental health among physicians using an intersectional analysis [ 30 , 32 , 39 ]. Finally, of the empirical studies we reviewed, all but one had a cross-sectional design. Longitudinal design might offer a better understanding of the emergence and development of mental health concerns in physicians and tailor interventions to different stages of professional career. Additionally, it could provide an opportunity to evaluate programs’ and policies’ effectiveness in improving physicians’ mental health. This would also help to address the gap that we identified in the literature – an overarching focus on proposing solutions with little demonstrated evidence they actually work.
This review has several limitations. First, our focus on academic literature may have resulted in overlooking the papers that are not peer-reviewed but may provide interesting solutions to physician mental health concerns. It is possible that grey literature – reports and analyses published by government and professional organizations – offers possible solutions that we did not include in our analysis or offers a different view on physicians’ mental health. Additionally, older papers and papers not published in English may have information or interesting solutions that we did not include in our review. Second, although our findings suggest that the theme of burnout dominated the literature, this may be the result of the search criteria we employed. Third, following the scoping review methodology [ 2 ], we did not assess the quality of the papers, focusing instead on the overview of the literature. Finally, our research was restricted to North America, specifically Canada and the USA. We excluded Mexico because we believed that compared to the context of medical practice in Canada and the USA, which have some similarities, the work experiences of Mexican physicians might be different and the proposed solutions might not be readily applicable to the context of practice in Canada and the USA. However, it is important to note that differences in organization of medical practice in Canada and the USA do exist, as do differences across and within provinces in Canada and the USA. A comparative analysis can shed light on how the structure and organization of medical practice shapes the emergence of mental health concerns.
The scoping review we conducted contributes to the existing research on mental wellbeing of American and Canadian physicians by summarizing key knowledge areas and identifying key gaps and directions for future research. While the papers reviewed in our analysis focused on North America, we believe that they might be applicable to the global medical workforce. Identifying key gaps in our knowledge, we are calling for further research on these topics, including examination of medical training curricula and its impact on mental wellbeing of medical students and residents, research on common mental health concerns such as depression or anxiety, studies utilizing intersectional and longitudinal approaches, and program evaluations assessing the effectiveness of interventions aiming to improve mental wellbeing of physicians. Focus on the effect physicians’ mental health may have on the quality of care provided to patients might facilitate support from government and policy makers. We believe that large-scale interventions that are proven to work effectively can utilize an upstream approach for improving the mental health of physicians and physicians-in-training.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
United States of America
World Health Organization
Ahmed N, Devitt KS, Keshet I, Spicer J, Imrie K, Feldman L, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. 2014;259(6):1041–53.
Article Google Scholar
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Atallah F, McCalla S, Karakash S, Minkoff H. Please put on your own oxygen mask before assisting others: a call to arms to battle burnout. Am J Obstet Gynecol. 2016;215(6):731.e1.
Baer TE, Feraco AM, Tuysuzoglu Sagalowsky S, Williams D, Litman HJ, Vinci RJ. Pediatric resident burnout and attitudes toward patients. Pediatrics. 2017;139(3):e20162163. https://doi.org/10.1542/peds.2016-2163 .
Article PubMed Google Scholar
Blais R, Safianyk C, Magnan A, Lapierre A. Physician, heal thyself: survey of users of the Quebec physicians health program. Can Fam Physician. 2010;56(10):e383–9.
PubMed PubMed Central Google Scholar
Brennan J, McGrady A. Designing and implementing a resiliency program for family medicine residents. Int J Psychiatry Med. 2015;50(1):104–14.
Cass I, Duska LR, Blank SV, Cheng G, NC dP, Frederick PJ, et al. Stress and burnout among gynecologic oncologists: a Society of Gynecologic Oncology Evidence-based Review and Recommendations. Gynecol Oncol. 2016;143(2):421–7.
Chan AM, Cuevas ST, Jenkins J 2nd. Burnout among osteopathic residents: a cross-sectional analysis. J Am Osteopath Assoc. 2016;116(2):100–5.
Chaukos D, Chad-Friedman E, Mehta DH, Byerly L, Celik A, McCoy TH Jr, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41(2):189–94.
Compton MT, Frank E. Mental health concerns among Canadian physicians: results from the 2007-2008 Canadian physician health study. Compr Psychiatry. 2011;52(5):542–7.
Cunningham C, Preventing MD. Burnout. Trustee. 2016;69(2):6–7 1.
PubMed Google Scholar
Daskivich TJ, Jardine DA, Tseng J, Correa R, Stagg BC, Jacob KM, et al. Promotion of wellness and mental health awareness among physicians in training: perspective of a national, multispecialty panel of residents and fellows. J Grad Med Educ. 2015;7(1):143–7.
Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA. 2011;305(19):2009–10.
Article CAS Google Scholar
Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. 2013;88(3):301–3.
Evans RW, Ghosh K. A survey of headache medicine specialists on career satisfaction and burnout. Headache. 2015;55(10):1448–57.
Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336(7642):488–91.
Fargen KM, Spiotta AM, Turner RD, Patel S. The importance of exercise in the well-rounded physician: dialogue for the inclusion of a physical fitness program in neurosurgery resident training. World Neurosurg. 2016;90:380–4.
Gabel S. Demoralization in Health Professional Practice: Development, Amelioration, and Implications for Continuing Education. J Contin Educ Health Prof 2013 Spring. 2013;33(2):118–26.
Google Scholar
Govardhan LM, Pinelli V, Schnatz PF. Burnout, depression and job satisfaction in obstetrics and gynecology residents. Conn Med. 2012;76(7):389–95.
Jennings ML, Slavin SJ. Resident wellness matters: optimizing resident education and wellness through the learning environment. Acad Med. 2015;90(9):1246–50.
Keller EJ. Philosophy in medical education: a means of protecting mental health. Acad Psychiatry. 2014;38(4):409–13.
Krall EJ, Niazi SK, Miller MM. The status of physician health programs in Wisconsin and north central states: a look at statewide and health systems programs. WMJ. 2012;111(5):220–7.
Lemaire JB, Wallace JE. Burnout among doctors. BMJ. 2017;358:j3360.
Linzer M, Bitton A, Tu SP, Plews-Ogan M, Horowitz KR, Schwartz MD, et al. The end of the 15-20 minute primary care visit. J Gen Intern Med. 2015;30(11):1584–6.
Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of burnout on self-reported patient care among emergency physicians. West J Emerg Med. 2015;16(7):996–1001.
Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422.
McClafferty H, Brown OW. Section on integrative medicine, committee on practice and ambulatory medicine, section on integrative medicine. Physician health and wellness. Pediatrics. 2014;134(4):830–5.
Miyasaki JM, Rheaume C, Gulya L, Ellenstein A, Schwarz HB, Vidic TR, et al. Qualitative study of burnout, career satisfaction, and well-being among US neurologists in 2016. Neurology. 2017;89(16):1730–8.
Peterson J, Pearce P, Ferguson LA, Langford C. Understanding scoping reviews: definition, purpose, and process. JAANP. 2016;29:12–6.
Przedworski JM, Dovidio JF, Hardeman RR, Phelan SM, Burke SE, Ruben MA, et al. A comparison of the mental health and well-being of sexual minority and heterosexual first-year medical students: a report from the medical student CHANGE study. Acad Med. 2015;90(5):652–9.
Ripp JA, Privitera MR, West CP, Leiter R, Logio L, Shapiro J, et al. Well-being in graduate medical education: a call for action. Acad Med. 2017;92(7):914–7.
Salles A, Mueller CM, Cohen GL. Exploring the relationship between stereotype perception and Residents’ well-being. J Am Coll Surg. 2016;222(1):52–8.
Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry. 2013;37(3):158–64.
Sikka R, Morath J, Leape L. The quadruple aim: care, health, cost and meaning in work. BMJ Qual Saf. 2015;24(10):608–10. https://doi.org/10.1136/bmjqs-2015-004160 .
Tawfik DS, Phibbs CS, Sexton JB, Kan P, Sharek PJ, Nisbet CC, et al. Factors Associated With Provider Burnout in the NICU. Pediatrics. 2017;139(5):608. https://doi.org/10.1542/peds.2016-4134 Epub 2017 Apr 18.
Turner TB, Dilley SE, Smith HJ, Huh WK, Modesitt SC, Rose SL, et al. The impact of physician burnout on clinical and academic productivity of gynecologic oncologists: a decision analysis. Gynecol Oncol. 2017;146(3):642–6.
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272.
Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry. 2015;39(1):47–54.
Woodside JR, Miller MN, Floyd MR, McGowen KR, Pfortmiller DT. Observations on burnout in family medicine and psychiatry residents. Acad Psychiatry. 2008;32(1):13–9.
World Health Organization. (2001). Mental disorders affect one in four people.
World Health Organization. Promoting mental health: concepts, emerging evidence, practice (Summary Report). Geneva: World Health Organization; 2004.
Download references
Acknowledgements
Not Applicable.
Not Applicable
Author information
Authors and affiliations.
Telfer School of Management, University of Ottawa, 55 Laurier Ave E, Ottawa, ON, K1N 6N5, Canada
Mara Mihailescu
School of Public Health and Health Systems, University of Waterloo, 200 University Avenue West, Waterloo, ON, N2L 3G1, Canada
Elena Neiterman
You can also search for this author in PubMed Google Scholar
Contributions
M.M. and E.N. were involved in identifying the relevant research question and developing the combinations of keywords used in consultation with a professional librarian. M.M. performed the literature selection and screening of references for eligibility. Both authors were involved in the creation of the literature extraction tool in Excel. Both authors coded the data inductively, first independently reading five articles and generating themes from the data, then discussing their coding and developing a coding scheme that was subsequently applied to ten more papers. Both authors then refined and finalized the coding scheme and M.M. used it to code the rest of the data. M.M. conceptualized and wrote the first copy of the manuscript, followed by extensive drafting by both authors. E.N. was a contributor to writing the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mara Mihailescu .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Mihailescu, M., Neiterman, E. A scoping review of the literature on the current mental health status of physicians and physicians-in-training in North America. BMC Public Health 19 , 1363 (2019). https://doi.org/10.1186/s12889-019-7661-9
Download citation
Received : 29 April 2019
Accepted : 20 September 2019
Published : 24 October 2019
DOI : https://doi.org/10.1186/s12889-019-7661-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Mental illness
- Medical students
- Scoping review
- Interventions
- North America
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Recommendation 22 Literature Review Summary
- Mental health literacy encompasses knowledge about mental health symptoms, interventions, and resources available, as well as positive attitudes and willingness to intervene when others are struggling.
- Literacy campaigns targeted at mental health have been positively received in post-secondary institutions, though it is unclear how they might affect behavioural outcomes.
- Mental health training can improve knowledge, attitudes and self-efficacy. However, improvements often diminish over time, and it is unclear how actual gatekeeping behaviours are affected.
- Barriers to participating in training programs include lack of awareness, time constraints, resource limitations, and uncertainty about the benefits of training.
Literature Review Findings
Mental health literacy is broadly defined as knowledge of mental health symptoms, interventions, and resources available, as well as positive attitudes and self-efficacy toward helping others in need. Many students were aware of counselling services and symptoms related to depression, but fewer recognized other campus resources and types of mental health conditions. Health promotion and prevention of mental health issues were under-recognized; students only endorsed help-seeking actions when symptoms were severe. Additionally, students experiencing high levels of depression and distress were less likely to recognize symptoms of mental illness than others.
Various mental health literacy campaigns have been implemented in post-secondary settings. Feedback collected through focus groups and surveys tended to be positive, though response rates were often low and outcomes following exposure were minimal. Campaigns utilizing visual promotion materials are more effective when they are designed appealingly and with a student audience in mind. There is also a need for campaigns targeted at groups at higher risk of experiencing mental distress, such as LGBTQ+ and racialized student groups.
Mental health training programs are associated with short-term increases in self-reported knowledge, attitudes, and self-efficacy. However, there is mixed evidence supporting changes to actual behaviours; (quasi-)experimental studies found few differences in skills following training. Training programs that included components such as experiential learning exercises and scenarios tailored to post-secondary settings were the most effective at improving outcomes. Limitations of studies on training programs include low participation and response rates, lack of long-term follow-up assessments, and the use of instruments that have not been empirically validated.
Faculty, staff and students described barriers to participating in training programs, such as lack of awareness about training opportunities, limited time and resources, and uncertainty about the benefits of training given the role of the person. Support from peers and leaders in the community was a strong enabling factor for participating in training.
Implications for Practice
Mental health literacy campaigns need to be embedded into a larger policy and service framework that emphasizes health promotion and prevention as well as intervention and crisis management. Tailored campaigns for high risk groups, such as minority student populations and those experiencing high levels of mental distress, are recommended.
As part of a mental health literacy strategy, training programs need to be available to all members of the university community. Training programs that are specialized for post-secondary settings, incorporate experiential exercises, and which receive institutional resources and ongoing support, are likely to have the most impact.

- Contact Waterloo
- Maps & Directions
- Accessibility
The University of Waterloo acknowledges that much of our work takes place on the traditional territory of the Neutral, Anishinaabeg and Haudenosaunee peoples. Our main campus is situated on the Haldimand Tract, the land granted to the Six Nations that includes six miles on each side of the Grand River. Our active work toward reconciliation takes place across our campuses through research, learning, teaching, and community building, and is co-ordinated within the Office of Indigenous Relations .
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 75, NO. 4 CURRENT ISSUE pp.307-398
- March 01, 2024 | VOL. 75, NO. 3 pp.203-304
- February 01, 2024 | VOL. 75, NO. 2 pp.107-201
- January 01, 2024 | VOL. 75, NO. 1 pp.1-71
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
E-Mental Health: A Rapid Review of the Literature
- Shalini Lal , Ph.D. , and
- Carol E. Adair , Ph.D.
Search for more papers by this author
The authors conducted a review of the literature on e-mental health, including its applications, strengths, limitations, and evidence base.
The rapid review approach, an emerging type of knowledge synthesis, was used in response to a request for information from policy makers. MEDLINE was searched from 2005 to 2010 by using relevant terms. The search was supplemented with a general Internet search and a search focused on key authors.
A total of 115 documents were reviewed: 94% were peer-reviewed articles, and 51% described primary research. Most of the research (76%) originated in the United States, Australia, or the Netherlands. The review identified e-mental health applications addressing four areas of mental health service delivery: information provision; screening, assessment, and monitoring; intervention; and social support. Currently, applications are most frequently aimed at adults with depression or anxiety disorders. Some interventions have demonstrated effectiveness in early trials. Many believe that e-mental health has enormous potential to address the gap between the identified need for services and the limited capacity and resources to provide conventional treatment. Strengths of e-mental health initiatives noted in the literature include improved accessibility, reduced costs (although start-up and research and development costs are necessary), flexibility in terms of standardization and personalization, interactivity, and consumer engagement.
Conclusions
E-mental health applications are proliferating and hold promise to expand access to care. Further discussion and research are needed on how to effectively incorporate e-mental health into service systems and to apply it to diverse populations.
Innovations in information and communication technology (ICT) are transforming the landscape of health service delivery. This emerging field, often referred to as “e-health,” includes key features, such as electronic, efficient, enhancing quality, evidence based, empowering, encouraging, education, enabling, extending, ethics, and equity ( 1 ). E-health is a broader concept than telehealth (and telemedicine), which involves the use of ICT to connect patients and providers in real time across geographical distances ( 2 ) for the delivery of typical care and where the use of real-time video is the main modality ( 3 ).
Interest is also increasing in the application of ICT in mental health care. For example, the first international e-mental health summit was held in 2009 in Amsterdam, and a summit-specific issue of the Journal of Medical Internet Research was published ( 4 ). Christensen and colleagues ( 5 ) defined e-mental health as “mental health services and information delivered or enhanced through the Internet and related technologies.” However, there is no agreement on a field-specific definition. Some scholars consider e-mental health to include only initiatives delivered directly to mental health service users ( 6 ) and only on the Internet ( 6 , 7 ) (as opposed to, for example, delivery via stand-alone computers or video seminars). Others adopt a wider definition that includes frontline delivery activities related to screening, mental health promotion and prevention, provision of treatment, staff training, administrative support (for example, patient records), and research ( 4 ).
Because of the growth of the e-mental health field, it is difficult for policy makers and practitioners to stay abreast of available applications and the evidence for their effectiveness. In response to a request from a Canadian executive-level policy maker, we conducted a rapid review of the literature on e-mental health. In this article, we report briefly on the review methods and summarize key findings.
Rapid reviews are an emerging type of knowledge synthesis used to inform health-related policy decisions and discussions, especially when information needs are immediate ( 8 – 11 ). Rapid reviews streamline systematic review methods—for example, by focusing the literature search ( 8 ) while still aiming to produce valid conclusions. The requirements for the review, which was undertaken with a two-week deadline, were for a short (maximum eight pages) but in-depth synthesis of the current state of the science on the topic. The personnel available was one senior (doctoral-level) mental health services researcher (CEA). Later, a second (doctoral-level) mental health services researcher (SL) validated the conclusions by screening all titles and abstracts, extracting and synthesizing additional data, and reviewing the findings.
The overarching review question was: What is currently known on the topic of e-mental health? (Even though telepsychiatry is typically included in e-mental health definitions, we did not include this subtopic because its literature is already well developed with several systematic reviews and reviews of reviews.)
Several secondary questions were developed and refined as the review progressed: What types of e-mental health initiatives have been developed? What are the strengths and benefits of e-mental health? What are the concerns with and barriers to use of e-mental health? What is the state of the evidence for the effectiveness of e-mental health? How has e-mental health been integrated in service systems and policy?
The rapid review method used is similar to Khangura and colleagues’ ( 10 ) seven-step process. Briefly, the search focused on English, peer-reviewed full abstracts in MEDLINE from 2005 to 2010 and used the MESH terms mental disorders and internet and the following non-MESH key words: e-mental health, e-therapy, computer, computer-based therapy, computer-based treatment, web-based therapy, web-based treatment. We excluded search terms related to telehealth because that is a distinct, and well-established subset of the e-health field that mainly considers the use of telecommunications to connect service providers and patients across geographical distances ( 3 ) (as opposed to delivering automated, self-management interventions, for example). The search was run in MEDLINE because of time constraints and because it is the most widely searched database for health-related topics, has comprehensive coverage (more than 5,500 journals), and has substantial capture of the content of health services research and overlap with similar sources.
The initial search (December 2010) yielded 158 titles or abstracts. Similar keywords were also used in a brief on-line grey literature search, which retrieved additional relevant documents, such as a list of in-progress trials, a policy report, and recent conference proceedings. Two experts on e-mental health were also contacted by e-mail for comment on the appropriateness of the identified literature and additional articles. Final searches focused on the work of prominent authors (for example, Christensen, Hickie, and Titov). These searches yielded an additional 50 titles and abstracts, resulting in 208 titles and abstracts screened for duplicates and relevancy.
Further details on the rapid review method and our search and selection strategy are provided in an online data supplement to this article.
General description of the literature
The screening process resulted in 115 documents, which were reviewed. Of these, 108 (94%) had been peer reviewed. Publication dates were from 2000 to 2010, with most (N=91, 79%) published between 2007 and 2010, which confirmed an expected increase in the volume of literature on the topic over time. Of the 115 documents, 59 (51%) reported primary empirical studies, of which 25 (42%) were conducted in the United States, 13 (22%) in Australia, and seven (12%) in the Netherlands.
Types of e-mental health initiatives
The review identified e-mental health applications addressing four areas of mental health service delivery: information provision ( 6 , 12 ); screening, assessment, and monitoring ( 13 – 20 ); intervention ( 21 – 24 ); and social support ( 25 ). Many applications addressed several areas of mental health service delivery concurrently ( 26 – 29 ). [A table listing examples of these e-mental health programs and initiatives is provided in the online data supplement . It summarizes information on the purpose of the application, the health conditions and populations targeted, and the components and technologies used.]
With respect to information provision, there is an identified need to ensure the quality of information about mental health. Therefore, tools such as the Brief DISCERN ( 13 ) have been developed to help users assess the quality of mental health–related content on Web sites.
Screening and assessment tools have been available for many years on stand-alone computers, but more recent developments are Internet-based screening tools to provide broader access to individuals for self-assessment (particularly to underserved or hard-to-reach groups) or for use by professionals in specific settings (for example, primary care) ( 30 ). For example, Diamond and colleagues ( 16 ) described an Internet-based behavioral health screening tool for adolescents and young adults in primary care. It requires minimal time to complete; addresses a broad spectrum of psychiatric symptoms, risk behaviors, and patient strengths; is automatically scored online; and allows results to be integrated into the patient’s electronic medical record and into system-level performance measurement.
Social support in e-mental health occurs through several types of Web-based formats, including discussion groups, bulletin boards, chat rooms, blogs, and social media. For example, Scharer ( 25 ) reported on a pilot study that examined the effectiveness of an online electronic bulletin board to provide social support to parents of children with mental illness. Parents made use of the bulletin board over a four-month period, actively posting messages to each other about their children’s illness or about the group.
E-mental health interventions were classified in our review by stage (promotion, prevention, early intervention, active treatment, maintenance, and relapse prevention), type of relationship (for example, between a professional and a consumer, between consumers, and between professionals), and treatment or therapy modality (for example, cognitive-behavioral therapy [CBT] and psychoeducation). Treatments identified were self-led or led by a therapist or were a combination (for example, self-led and therapist guided). Interventions were provided as the primary therapy or adjunct to conventional in-person therapy and were delivered to individuals or groups or both. For example, MoodGYM is an exemplary Web-based, interactive intervention that has been developed and evaluated in several randomized controlled trials ( 27 , 31 – 33 ). Its purpose is to enhance coping skills in relation to depression, and it includes assessments, workbooks, games, online exercises, and feedback. MoodGYM is freely available to the public and has been translated into several languages.
Most of the interventions studied were situated on a specific point of the continuum of care (for example, prevention, mental health promotion, or intervention) and used a single format; however, a few incorporated several types of approaches. For example, Tillfors and colleagues ( 34 ) investigated whether an Internet-delivered self-help intervention in conjunction with minimal e-mail contact was as effective as adding in-person group sessions to the Internet intervention. They found that adding in-person group sessions did not result in significant differences in outcomes.
Typically, e-mental health interventions mimicked traditional treatment approaches in that they often addressed single disorders; none were designed for individuals with comorbid mental and substances use disorders. The most frequent disorders addressed by the 59 empirical studies were depression or anxiety (18 studies, 31%). Several interventions focused on mental health promotion or prevention, including early identification (eight studies, 14%). Most interventions were developed specifically for adults (40 studies, 68%), followed by interventions targeting adolescents or young adults (11 studies, 19%). Recent e-mental health initiatives reflect the shift in the mid-2000s to Web 2.0 technologies (that is, more interactive, multimedia, and user-driven technologies) ( 35 ).
Strengths and benefits
Many authors believe that e-mental health has enormous potential to address the gap between the identified need for mental health services in the population and the limited capacity and resources to provide conventional treatment services ( 13 , 30 ). Strengths of e-mental health initiatives noted in the literature include improved accessibility, reduced costs (although start-up and research and development costs are necessary), flexibility in terms of standardization and personalization, interactivity, and consumer engagement ( 5 , 30 , 34 – 38 ). E-health technologies are considered to be particularly promising for rural and remote populations. They are also promising for subpopulations that have other barriers to access (attitudinal, financial, or temporal) or that avoid treatment because of stigma. For example, by using Internet-based social support, individuals can share their perspectives freely while preserving their anonymity. Further details and examples of benefits are summarized in a box on the next page.
Concerns and barriers
Some concerns and barriers are associated with using e-mental health. There are concerns that e-mental health will replace important and needed conventional services; divert attention away from improvements to or funding for conventional services; and be costly to develop, deploy, and evaluate ( 5 ). Another issue raised in the literature is related to the financial interests of developers and researchers, which may produce a risk of publication bias ( 39 ). Others have highlighted the limited evidence base for interventions, lack of quality control and care standards, and slow uptake by or reluctance among health care professionals ( 39 , 40 ). Some question the ability of professionals to establish therapeutic relationships on line and the feasibility of online treatment for certain population groups (for example, patients with severe depression) ( 39 ). Emmelkamp ( 39 ) described “technological phobia,” whereby professionals may be unfamiliar with technology and anxious about its use in professional care. Concerns have also been expressed about the potential to further marginalize individuals who have physical, financial, or cognitive barriers in terms of access to conventional services. Finally, some are concerned that the availability of e-mental health services may lead some individuals to postpone seeking needed conventional care or that some will receive inappropriate or harmful care when there is insufficient quality control over content ( 7 ).
Ethical and liability concerns have been cited. For example, when participants are from outside the regulatory jurisdiction, ethical responsibilities cannot be met; other concerns are that participants cannot be reliably identified and that privacy cannot be guaranteed for typed or recorded communications ( 5 , 34 , 37 , 38 , 41 ). To address these issues, several professional organizations (for example, the American Psychological Association) have developed guidelines ( 38 ), and an international organization to set standards has been established—the International Society for Mental Health Online. Even so, adherence has been found to be lacking, and concerns remain ( 7 , 39 , 42 , 43 ). At the same time, remedies for the above-mentioned concerns are emerging. Technology for the protection of security and confidentiality has improved, and some efforts are being made to review Web site content for quality ( 35 , 44 , 45 ). In Australia, a Web portal called Beacon has been set up that provides quality ratings for mental health Web sites and recommends evidence-based interventions ( 46 ).
Consumer engagement, reach, and response
A handful of recent studies have shed some light on the role of e-mental health providing prevention or intervention programming for particular groups of individuals, such as youths, socioeconomically diverse populations, rural and remote populations, the general public, and patients. One study investigated the preferences for e-mental health services in an online Australian sample (N=218) ( 47 ). Among individuals in the general population who were already using the Internet, a large majority (77%) expressed a preference for face-to-face services, but less than 10% indicated that they would not use e-mental health services. The authors highlighted the importance of raising public awareness, knowledge, and understanding about e-mental health services. More than 50% of the sample expressed the need to learn more about e-mental health services and about issues related to confidentiality.
More than 90% of youths now use the Internet, and it is seen as a promising medium for reaching that age group ( 28 , 48 ). In a large population-based sample of 2,000 young people aged 12 to 25 in Australia, 77% reported seeking information about mental health problems whether or not they had the problem themselves ( 49 ). In another study among military personnel, who are predominantly younger males, one-third of 352 respondents who reported that they were not willing to talk to a counselor in person indicated that they would be willing to use technology to address their concerns ( 50 ).
Preliminary research has also indicated that mental health service users value the use of e-mental health. A qualitative study of 36 participants found that their primary motive for Internet use was to access social support and their secondary motive was for information ( 51 ). Respondents noted that hearing about other individuals’ experiences helped them to feel less isolated and more hopeful. Respondents also liked the convenience, privacy, and anonymity of the Internet. On the other hand, several authors have documented low access to and use of the Internet among persons with more serious mental illnesses, such as those with co-occurring substance use and serious mental illness ( 52 , 53 ). Cost, lack of training, and impairment (in cognition, concentration, executive function, and motor control) can present barriers for individuals with serious mental illness, further disenfranchising them from services ( 54 ). However, evidence is emerging that with a user-friendly interface, high levels of engagement and positive outcomes can be obtained in online interventions for individuals with serious mental illnesses such as schizophrenia and their families ( 26 ). Nonetheless, access to and attitudes toward technology, as well as socioeconomic factors, need to be taken into account in planning Internet-based interventions for specific population groups ( 55 ).
Evidence base for e-mental health
Although evaluation of some interventions is limited, an encouraging amount of rigorous research is available, depending on the developmental stage of the intervention. Research on Web-based interventions has both opportunities and challenges. Studies are relatively inexpensive to conduct, and large samples can be used. Interventions are easily standardized, randomized or controlled designs are feasible (often with wait list controls), and data are easily collected. Challenges include low rates of completion because of the relative ease with which participants can drop out of studies. In addition, it is difficult to study both the intervention and the mode of delivery; contamination of the control group is possible because participants can access similar services elsewhere on the Web; the ability to conduct double-blind studies is limited; and biases related to using self-report measures are a problem ( 56 – 58 ). Increasingly, resources for optimizing practice and evaluation are available; for example, guidelines for program design and for study methods have been published ( 36 , 59 ).
In the past five years, several reviews, including systematic reviews and meta-analyses of randomized controlled trials, have documented the progress made; effectiveness has been demonstrated in particular for interventions (both therapist assisted and self-directed) addressing depression and anxiety disorders ( 57 , 59 , 60 ). For example, a systematic review of meta-analyses of the efficacy of Internet-based self-help for depression and anxiety disorders reported that these interventions are effective and that effect sizes are comparable to those observed in similar interventions delivered in person ( 60 ). Systematic reviews of Internet-based CBT interventions (prevention and treatment) for anxiety and depression among adults have found that they are as effective as or more effective than treatment as usual ( 57 ). Preliminary evidence has also been reported for the effectiveness of Internet-based interventions to address issues such as stress, insomnia, and substance abuse ( 61 ). There are still some interventions for which evidence is weak or contrary, such as one CBT-based program for individuals with obsessive-compulsive disorder ( 62 ), and not all studies evaluating the effectiveness of Internet-based interventions for depression and anxiety have found positive results ( 62 , 63 ). Lower effect sizes have generally been found for interventions targeting alcohol and smoking cessation compared with those for anxiety and depression ( 61 ). There are some indications that programs work best for individuals with mild to moderate disorders; however, this group has been the focus of most research. Despite the popularity of online support groups, concerns about the encouragement of maladaptive behaviors, or support for continuing such behaviors, have surfaced—for example, in a recent survey of members of an eating disorders forum ( 64 ).
Systematic reviews are also beginning to appear that address e-health interventions for children and youths. For example, Stinson and colleagues ( 65 ) found that symptoms improved in seven of nine identified self-management interventions. A recent narrative review of Internet-based prevention and treatment programs for anxiety and depression among children and adolescents concluded that there was early support for effectiveness but a need for more rigorous research as well as interventions specifically targeting children ( 66 ). Recent innovations, such as those that embed prevention and early-intervention content in online games, need more evaluation. A study of one such program found a nonsignificant worsening effect on support seeking, avoidance, and resilience outcomes, especially among males ( 29 ). An interactive fantasy gaming approach has also been developed by Sally Merry, M.D., of Auckland, New Zealand (personal communication, Merry S, Dec. 2010). A recently published randomized controlled trial demonstrated its effectiveness among adolescents seeking help for depression in primary care settings ( 67 ).
In the area of substance use and abuse, a systematic review of Internet-based interventions for young people found small positive effects for programs aimed at alcohol abuse; the effects were of similar magnitude to those of brief in-person interventions, but the Internet-based interventions had the advantage of much broader delivery ( 68 ). However, programs aimed at preventing subsequent development of alcohol-related problems among those who were nondrinkers at baseline were generally not effective.
More research is needed on individual or subgroup predictors of differential outcomes of e-mental health interventions ( 21 , 69 ). Moreover, even though there is some preliminary evidence supporting the lower cost of using e-mental health approaches, true cost-effectiveness studies are just beginning to appear in the literature ( 70 ).
E-mental health, systems, and policy
Most of the literature reviewed described the development, implementation, and evaluation of single interventions in isolation. One very important question that has been given limited attention is how e-mental health interventions might best be situated in relation to an array of related services for a broad population. In a rare exception, van Straten and colleagues ( 71 ) discussed a stepped-care approach for depression in primary care wherein interventions advance from watchful waiting through self-guided but supported intervention (including Web-based formats), brief face-to-face psychotherapy, and finally longer-term face-to-face psychotherapy with consideration of antidepressant medication. To ensure continuity of care, a care manager monitors patient status at all levels and makes decisions about necessary transitions. Treatments at all levels are evidence based. These authors described trials of two different e-mental health interventions, including one for younger adults, and most important, how they fit within the full stepped-care model. Data on cost-effectiveness of the full model are unavailable, but the authors suggested that the incidence of new cases of depression and anxiety could be halved by introducing this model.
Andrews and Titov ( 72 ) described the promotion of Internet-based treatment programs (a virtual clinic) connected to a hospital in Sydney, Australia. The programs are considered to be cost-effective alternatives to medication or face-to-face CBT treatment. Programs are offered for major depression, social phobia, panic disorder, and generalized anxiety disorder. Programs are available free or at very low cost directly to the public; general practitioners and other mental health professionals can use these programs in addition to or instead of conventional care. Trial results show high levels of patient adherence and strong reductions in symptoms with very little investment of clinician time. The authors discuss how e-mental health programs might fit in a broader health service delivery context (for example, in U.S. health maintenance organizations, health care trusts in the United Kingdom, and regional health authorities in Canada). They suggest that the programs could be the first level of treatment for the proportion of the population that desires Internet-based treatment; however, with the support of a small team, individuals who need more support could be identified and referred for more intensive intervention.
An approach that reaches out to the total population but that is not fully connected to conventional services has been described by Bennett and colleagues ( 27 ). At its center is “e-hub,” which is an online self-help mental health service available free to the public. The service provides automated Web interventions for several needs, such as symptoms of depression, anxiety, and social anxiety, and an online bulletin board. Programs focus on the prevention and early-intervention end of the spectrum. There is no therapist involvement in the interventions, and the bulletin board is moderated by trained consumers under the supervision of a clinical psychologist. Interested individuals can contact the e-hub by e-mail. The organizers report a high volume of use by individuals with and without mental disorders, some over a lengthy period. The service is considered most suitable for those who prefer to receive help anonymously, prefer self-help, or reside in rural or remote areas. Quality control processes are included.
No peer-reviewed articles had a central focus on policy-level discussions about e-mental health. However, the gray literature search yielded one major report on the topic from Australia, E-Mental Health in Australia: Implications of the Internet and Related Technologies for Policy ( 5 ). Although the report was published in 2004, much of the content is relevant for other countries, because many are only at the beginning stages of e-mental health implementation. The report describes the advantages of e-mental health initiatives and barriers to implementation (as described above). Five major recommendations for moving forward are included related to access, ethical issues, quality and effectiveness, technology, and funding.
Articles and studies identified by the rapid review but not discussed here are listed in References ( 73 – 103 ).
The purpose of this rapid review was to synthesize and describe what is currently known on the topic of e-mental health. On the basis of the findings, several considerations for future research and practice in the field of e-mental health are evident. First, it is important to consider the fit of e-mental health initiatives within the context of the existing service system and to ensure that they complement—and not detract from—needs for direct care. Second, it is important to select interventions and initiatives on the basis of available evidence regarding both design features and effectiveness and to build research and evaluation into any new initiatives. Third, it is important to consider the needs of the population as well as the greatest potential for benefit when choosing or investing in e-mental health initiatives—for example, the intervention’s suitability for a diverse group of participants (in age, ethnocultural status, literacy, and disability) should be considered. Fourth, it is important to ensure that ethical and quality issues are addressed. Fifth, the extent to which interventions have or can be applied in cross-cultural and international contexts is an important consideration. Sixth, the involvement of consumers, as well as other relevant key stakeholder groups (such as families and caregivers, service providers, and policy makers), in the development and deployment of initiatives is paramount. Seventh, further research is needed in relation to conditions other than common disorders, such as psychotic disorders. Eighth, more rigorously conducted research is needed, such as randomized controlled trials, and it is important to understand which groups of individuals will benefit the most from such interventions and to take into account cross-cultural and international factors (for example, cultural adaptations).
It is important to acknowledge the limits of rapid review. They include focusing the search on one electronic database source (although we used the database that contains by far the largest number of health and medical journals). The search was also complemented by gray literature searches on the Internet, focused author searches, and brief key-informant consultations. A second limitation of our review is that only one author (CEA) initially screened the titles and abstracts from the total set of documents retrieved, although this author is knowledgeable about the content area and has experience conducting systematic reviews. However, the second author (SL) rescreened all extracted titles and abstracts from the total set. This rescreening uncovered additional nuances in various content areas, identified further studies for review, and provided the opportunity for incorporating more detailed information in this article (for example, technologies and components of e-mental health initiatives described in the online data supplement ). Some minor errors in the initial review were also uncovered. Although the initial review was well received by its sponsors and was reported to inform key policy discussions, the effectiveness of rapid reviews in terms of their ultimate impact on health policy decisions and service outcomes remains to be systematically considered.
This rapid review identified a small but rich set of information on the topic of e-mental health, which was found to be highly useful for its specific intended policy discussion. The apparent promise and pitfalls of e-mental health and the increasing interest of policy makers in its potential for service system transformation indicate that careful monitoring of the evidence base is warranted.
Acknowledgments and disclosures
While conducting this review, Dr. Lal was partially supported by a postdoctoral fellowship from Knowledge Translation Canada. Dr. Adair conducted the initial review while under contract with the Mental Health Commission of Canada. The authors acknowledge Jayne Barker, Ph.D., and Janice Popp, M.S.W., for their assistance in refining the research questions to serve a policy purpose. The views expressed herein are solely those of the authors.
The authors report no competing interests.
1 Eysenbach G : What is e-health? Journal of Medical Internet Research 3:E20, 2001 Crossref , Medline , Google Scholar
2 Sood S, Mbarika V, Jugoo S, et al. : What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings . Telemedicine and e-Health 13:573–590, 2007 Crossref , Medline , Google Scholar
3 Wade VA, Karnon J, Elshaug AG, et al. : A systematic review of economic analyses of telehealth services using real time video communication . BMC Health Services Research 10:233, 2010 Crossref , Medline , Google Scholar
4 Riper H, Andersson G, Christensen H, et al. : Theme issue on e-mental health: a growing field in Internet research . Journal of Medical Internet Research 12:e74, 2010 Crossref , Medline , Google Scholar
5 Christensen H, Griffiths K, Evans K : E-Mental Health in Australia: Implications of the Internet and Related Technologies for Policy . Canberra, Commonwealth Department of Health and Ageing, 2002 Google Scholar
6 Lambousis E, Politis A, Markidis M, et al. : Development and use of online mental health services in Greece . Journal of Telemedicine and Telecare 8(suppl 2):51–52, 2002 Crossref , Medline , Google Scholar
7 Ybarra ML, Eaton WW : Internet-based mental health interventions . Mental Health Services Research 7:75–87, 2005 Crossref , Medline , Google Scholar
8 Watt A, Cameron A, Sturm L, et al. : Rapid reviews versus full systematic reviews: an inventory of current methods and practice in health technology assessment . International Journal of Technology Assessment in Health Care 24:133–139, 2008 Crossref , Medline , Google Scholar
9 Ganann R, Ciliska D, Thomas H : Expediting systematic reviews: methods and implications of rapid reviews . Implementation Science 5:56, 2010 Crossref , Medline , Google Scholar
10 Khangura S, Konnyu K, Cushman R, et al. : Evidence summaries: the evolution of a rapid review approach . Systematic Reviews 1:10, 2012 Crossref , Medline , Google Scholar
11 Konnyu KJ, Kwok E, Skidmore B, et al. : The effectiveness and safety of emergency department short stay units: a rapid review . Open Medicine 6:e10–e16, 2012 Medline , Google Scholar
12 Santor DA, Poulin C, LeBlanc JC, et al. : Online health promotion, early identification of difficulties, and help seeking in young people . Journal of the American Academy of Child and Adolescent Psychiatry 46:50–59, 2007 Crossref , Medline , Google Scholar
13 Khazaal Y, Chatton A, Cochand S, et al. : Brief DISCERN, six questions for the evaluation of evidence-based content of health-related Websites . Patient Education and Counseling 77:33–37, 2009 Crossref , Medline , Google Scholar
14 Becker J, Fliege H, Kocalevent R-D, et al. : Functioning and validity of a Computerized Adaptive Test to measure anxiety (A-CAT) . Depression and Anxiety 25:E182–E194, 2008 Crossref , Medline , Google Scholar
15 Chinman M, Hassell J, Magnabosco J, et al. : The feasibility of computerized patient self-assessment at mental health clinics . Administration and Policy in Mental Health and Mental Health Services Research 34:401–409, 2007 Crossref , Medline , Google Scholar
16 Diamond G, Levy S, Bevans KB, et al. : Development, validation, and utility of Internet-based, behavioral health screen for adolescents . Pediatrics 126:e163–e170, 2010 Crossref , Medline , Google Scholar
17 Donker T, van Straten A, Marks I, et al. : A brief Web-based screening questionnaire for common mental disorders: development and validation . Journal of Medical Internet Research 11:e19, 2009 Crossref , Medline , Google Scholar
18 Gringras P, Santosh P, Baird G : Development of an Internet-based real-time system for monitoring pharmacological interventions in children with neurodevelopmental and neuropsychiatric disorders . Child: Care, Health and Development 32:591–600, 2006 Crossref , Medline , Google Scholar
19 Gualtieri CT : An Internet-based symptom questionnaire that is reliable, valid, and available to psychiatrists, neurologists, and psychologists . Medscape General Medicine 9:3, 2007 Medline , Google Scholar
20 Heron KE, Smyth JM : Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments . British Journal of Health Psychology 15:1–39, 2010 Crossref , Medline , Google Scholar
21 Spek V, Nyklícek I, Cuijpers P, et al. : Predictors of outcome of group and Internet-based cognitive behavior therapy . Journal of Affective Disorders 105:137–145, 2008 Crossref , Medline , Google Scholar
22 Bergström J, Andersson G, Ljótsson B, et al. : Internet- versus group-administered cognitive behaviour therapy for panic disorder in a psychiatric setting: a randomised trial . BMC Psychiatry 10:54, 2010 Crossref , Medline , Google Scholar
23 Khanna MS, Kendall PC : Computer-assisted cognitive behavioral therapy for child anxiety: results of a randomized clinical trial . Journal of Consulting and Clinical Psychology 78:737–745, 2010 Crossref , Medline , Google Scholar
24 Khanna MS, Kendall PC : Computer-Assisted CBT for Child Anxiety: the Coping Cat CD-ROM . Cognitive and Behavioral Practice 15:159–165, 2008 Crossref , Google Scholar
25 Scharer K : An Internet discussion board for parents of mentally ill young children . Journal of Child and Adolescent Psychiatric Nursing 18:17–25, 2005 Crossref , Medline , Google Scholar
26 Rotondi AJ, Anderson CM, Haas GL, et al. : Web-based psychoeducational intervention for persons with schizophrenia and their supporters: one-year outcomes . Psychiatric Services 61:1099–1105, 2010 Link , Google Scholar
27 Bennett K, Reynolds J, Christensen H, et al. : e-hub: an online self-help mental health service in the community . Journal of Medical Internet Research 192(suppl):S48–S52, 2010 Google Scholar
28 Burns JM, Durkin LA, Nicholas J : Mental health of young people in the United States: what role can the Internet play in reducing stigma and promoting help seeking? Journal of Adolescent Health 45:95–97, 2009 Crossref , Medline , Google Scholar
29 Shandley K, Austin D, Klein B, et al. : An evaluation of “Reach Out Central”: an online gaming program for supporting the mental health of young people . Health Education Research 25:563–574, 2010 Crossref , Medline , Google Scholar
30 Farrell SP, Mahone IH, Zerull LM, et al. : Electronic screening for mental health in rural primary care: implementation . Issues in Mental Health Nursing 30:165–173, 2009 Crossref , Medline , Google Scholar
31 Christensen H, Griffiths KM, Jorm AF : Delivering interventions for depression by using the Internet: randomised controlled trial . British Medical Journal 328:265, 2004 Crossref , Medline , Google Scholar
32 O’Kearney R, Gibson M, Christensen H, et al. : Effects of a cognitive-behavioural Internet program on depression, vulnerability to depression and stigma in adolescent males: a school-based controlled trial . Cognitive Behaviour Therapy 35:43–54, 2006 Crossref , Medline , Google Scholar
33 Hickie IB, Davenport TA, Luscombe GM, et al. : Practitioner-supported delivery of Internet-based cognitive behaviour therapy: evaluation of the feasibility of conducting a cluster randomised trial . Medical Journal of Australia 192(suppl):S31–S35, 2010 Crossref , Medline , Google Scholar
34 Tillfors M, Carlbring P, Furmark T, et al. : Treating university students with social phobia and public speaking fears: Internet delivered self-help with or without live group exposure sessions . Depression and Anxiety 25:708–717, 2008 Crossref , Medline , Google Scholar
35 Ginn S : Evidence based mental health and Web 2.0 . Evidence-Based Mental Health 13:69–72, 2010 Crossref , Medline , Google Scholar
36 Coyle D, Doherty G, Matthews M, et al. : Computers in talk-based mental health interventions . Interacting with Computers 19:545–562, 2007 Crossref , Google Scholar
37 Christensen H, Hickie IB : Using e-health applications to deliver new mental health services . Medical Journal of Australia 192(suppl):S53–S56, 2010 Medline , Google Scholar
38 Alleman JR : Online counseling: the Internet and mental health treatment . Psychotherapy 39:199–209, 2002 Crossref , Google Scholar
39 Emmelkamp PM : Technological innovations in clinical assessment and psychotherapy . Psychotherapy and Psychosomatics 74:336–343, 2005 Crossref , Medline , Google Scholar
40 Christensen H, Griffiths K : The internet and mental health practice . Evidence-Based Mental Health 6:66–69, 2003 Crossref , Medline , Google Scholar
41 Perecherla S : Web matters . Evidence-Based Mental Health 12:4–6, 2009 Crossref , Medline , Google Scholar
42 Humphreys K, Winzelberg A, Klaw E : Psychologists’ ethical responsibilities in Internet-based groups: issues, strategies, and a call for dialogue . Professional Psychology, Research and Practice 31:493–496, 2000 Crossref , Medline , Google Scholar
43 Recupero P, Rainey SE : Forensic aspects of e-therapy . Journal of Psychiatric Practice 11:405–410, 2005 Crossref , Medline , Google Scholar
44 Taylor C, Luce K : Computer- and Internet-based psychotherapy interventions . Current Directions in Psychological Science 12:18–22, 2003 Crossref , Google Scholar
45 Christensen H, Hickie IB : E-mental health: a new era in delivery of mental health services . Medical Journal of Australia 192(suppl):S2–S3, 2010 Medline , Google Scholar
46 Santhiveeran J : Compliance of social work e-therapy websites to the NASW Code of Ethics . Social Work in Health Care 48:1–13, 2009 Crossref , Medline , Google Scholar
47 Klein B, Cook S : Preferences for e-mental health services amongst an online Australian sample . Electronic Journal of Applied Psychology 6:27–38, 2010 Google Scholar
48 Horgan A, Sweeney J : Young students’ use of the Internet for mental health information and support . Journal of Psychiatric and Mental Health Nursing 17:117–123, 2010 Crossref , Medline , Google Scholar
49 Burns JM, Davenport TA, Durkin LA, et al. : The Internet as a setting for mental health service utilisation by young people . Journal of Medical Internet Research 192(suppl):S22–S26, 2010 Google Scholar
50 Wilson JA, Onorati K, Mishkind M, et al. : Soldier attitudes about technology-based approaches to mental health care. Cyberpsychology and Behavior 11:767–769, 2008 Crossref , Medline , Google Scholar
51 Powell J, Clarke A : Investigating Internet use by mental health service users: interview study . Studies in Health Technology and Informatics 129:1112–1116, 2007 Medline , Google Scholar
52 Borzekowski DLG, Leith J, Medoff DR, et al. : Use of the Internet and other media for health information among clinic outpatients with serious mental illness . Psychiatric Services 60:1265–1268, 2009 Link , Google Scholar
53 Clayton S, Borzekowski D, Himelhoch S, et al. : Media and internet ownership and use among mental health outpatients with serious mental illness . American Journal of Drug and Alcohol Abuse 35:364–367, 2009 Crossref , Medline , Google Scholar
54 Nicholson JRA, Rotondi AJ : The Internet, health promotion, and community participation . Psychiatric Services 61:96–97, 2010 Link , Google Scholar
55 Yellowlees P, Marks S, Hilty D, et al. : Using e-health to enable culturally appropriate mental healthcare in rural areas . Telemedicine Journal and e-Health 14:486–492, 2008 Crossref , Medline , Google Scholar
56 Eysenbach G : Issues in evaluating health websites in an Internet-based randomized controlled trial . Journal of Medical Internet Research 4:E17, 2002 Crossref , Medline , Google Scholar
57 Kaltenthaler E, Parry G, Beverley C, et al. : Computerised cognitive-behavioural therapy for depression: systematic review . British Journal of Psychiatry 193:181–184, 2008 Crossref , Medline , Google Scholar
58 Christensen H, Griffiths KM, Farrer L : Adherence in Internet interventions for anxiety and depression . Journal of Medical Internet Research 11:e13, 2009 Crossref , Medline , Google Scholar
59 Smit F, Riper H : E-Mental Health: Presence and Future . Utrecht, Netherlands, Innovation Centre of Mental Health and Technology, 2010 Google Scholar
60 Van’t Hof E, Cuijpers P, Stein DJ : Self-help and Internet-guided interventions in depression and anxiety disorders: a systematic review of meta-analyses . CNS Spectrums 14(suppl 3):34–40, 2009 Crossref , Medline , Google Scholar
61 Amstadter AB, Broman-Fulks J, Zinzow H, et al. : Internet-based interventions for traumatic stress-related mental health problems: a review and suggestion for future research . Clinical Psychology Review 29:410–420, 2009 Crossref , Medline , Google Scholar
62 Computerised Cognitive Behaviour Therapy for Depression and Anxiety (review) . London, National Institute for Health and Clinical Excellence, 2008 Google Scholar
63 Griffiths KM, Farrer L, Christensen H : The efficacy of Internet interventions for depression and anxiety disorders: a review of randomised controlled trials . Medical Journal of Australia 192(suppl):S4–S11, 2010 Crossref , Medline , Google Scholar
64 Ransom DC, La Guardia JG, Woody EZ, et al. : Interpersonal interactions on online forums addressing eating concerns . International Journal of Eating Disorders 43:161–170, 2010 Medline , Google Scholar
65 Stinson J, Wilson R, Gill N, et al. : A systematic review of Internet-based self-management interventions for youth with health conditions . Journal of Pediatric Psychology 34:495–510, 2009 Crossref , Medline , Google Scholar
66 Calear AL, Christensen H : Review of Internet-based prevention and treatment programs for anxiety and depression in children and adolescents . Medical Journal of Australia 192(suppl):S12–S14, 2010 Crossref , Medline , Google Scholar
67 Merry SN, Stasiak K, Shepherd M, et al. : The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: randomised controlled non-inferiority trial . British Medical Journal 344:e2598, 2012 Crossref , Medline , Google Scholar
68 Tait RJ, Christensen H : Internet-based interventions for young people with problematic substance use: a systematic review . Medical Journal of Australia 192(suppl):S15–S21, 2010 Crossref , Medline , Google Scholar
69 Postel M, De Haan H, De Jong C : E-therapy for mental health problems: a systematic review . Telemedicine and e-Health 14:707–714, 2008 Crossref , Medline , Google Scholar
70 Woolderink M, Smit F, van der Zanden R, et al. : Design of an Internet-based health economic evaluation of a preventive group-intervention for children of parents with mental illness or substance use disorders . BMC Public Health 10:470, 2010 Crossref , Medline , Google Scholar
71 van Straten A, Seekles W, Beekman ATF, et al. : Stepped care for depression in primary care: what should be offered and how? Medical Journal of Australia 192(suppl 11):S36–S39, 2010 Crossref , Medline , Google Scholar
72 Andrews G, Titov N : Is Internet treatment for depressive and anxiety disorders ready for prime time? Medical Journal of Australia 192(suppl):S45–S47, 2010 Crossref , Medline , Google Scholar
73 Barnes DE, Yaffe K, Belfor N, et al. : Computer-based cognitive training for mild cognitive impairment: results from a pilot randomized, controlled trial . Alzheimer Disease and Associated Disorders 23:205–210, 2009 Crossref , Medline , Google Scholar
74 Swanton R, Collin P, Burns J, et al. : Engaging, understanding and including young people in the provision of mental health services . International Journal of Adolescent Medicine and Health 19:325–332, 2007 Crossref , Medline , Google Scholar
75 Carroll KM, Ball SA, Martino S, et al. : Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT . American Journal of Psychiatry 165:881–888, 2008 Link , Google Scholar
76 Crilly J, Lewis J : Internet-based psychiatric interventions: applications for rural veterans at risk for suicide. Presented at the International Conference on Society and Information Technology, Orlando, Fla, April 6–9, 2010 Google Scholar
77 Cukrowicz KC, Smith PN, Hohmeister HC, et al. : The moderation of an early intervention program for anxiety and depression by specific psychological symptoms . Journal of Clinical Psychology 65:337–351, 2009 Crossref , Medline , Google Scholar
78 Deegan PE, Rapp C, Holter M, et al. : A program to support shared decision making in an outpatient psychiatric medication clinic . Psychiatric Services 59:603–605, 2008 Link , Google Scholar
79 Deegan PE : A Web application to support recovery and shared decision making in psychiatric medication clinics . Psychiatric Rehabilitation Journal 34:23–28, 2010 Crossref , Medline , Google Scholar
80 Deitz DK, Cook RF, Billings DW, et al. : A Web-based mental health program: reaching parents at work . Journal of Pediatric Psychology 34:488–494, 2009 Crossref , Medline , Google Scholar
81 Freeman E, Barker C, Pistrang N : Outcome of an online mutual support group for college students with psychological problems. Cyberpsychology and Behavior 11:591–593, 2008 Crossref , Medline , Google Scholar
82 Golkaramnay V, Bauer S, Haug S, et al. : The exploration of the effectiveness of group therapy through an Internet chat as aftercare: a controlled naturalistic study . Psychotherapy and Psychosomatics 76:219–225, 2007 Crossref , Medline , Google Scholar
83 Horgan D : Www.DoctorsHealth.com.au . Australian and New Zealand Journal of Psychiatry 42:173–174, 2008 Medline , Google Scholar
84 Clarke G, Eubanks D, Reid E, et al. : Overcoming Depression on the Internet (ODIN) (2): a randomized trial of a self-help depression skills program with reminders . Journal of Medical Internet Research 7:e16, 2005 Crossref , Medline , Google Scholar
85 Matano RA, Koopman C, Wanat SF, et al. : A pilot study of an interactive Web site in the workplace for reducing alcohol consumption . Journal of Substance Abuse Treatment 32:71–80, 2007 Crossref , Medline , Google Scholar
86 Kessler D, Lewis G, Kaur S, et al. : Therapist-delivered Internet psychotherapy for depression in primary care: a randomised controlled trial . Lancet 374:628–634, 2009 Crossref , Medline , Google Scholar
87 Klein B, Richards J : A brief Internet-based treatment for panic disorder . Behavioural and Cognitive Psychotherapy 29:113–117, 2001 Crossref , Google Scholar
88 Klein B, Mitchell J, Gilson K, et al. : A therapist-assisted Internet-based CBT intervention for posttraumatic stress disorder: preliminary results . Cognitive Behaviour Therapy 38:121–131, 2009 Crossref , Medline , Google Scholar
89 Klinger E, Bouchard S, Légeron P, et al. : Virtual reality therapy versus cognitive behavior therapy for social phobia: a preliminary controlled study . Cyberpsychology and Behavior 8:76–88, 2005 Crossref , Medline , Google Scholar
90 Lange A, Rietdijk D, Hudcovicova M, et al. : Interapy: a controlled randomized trial of the standardized treatment of posttraumatic stress through the Internet . Journal of Consulting and Clinical Psychology 71:901–909, 2003 Crossref , Medline , Google Scholar
91 Lin C-C, Bai Y-M, Liu C-Y, et al. : Web-based tools can be used reliably to detect patients with major depressive disorder and subsyndromal depressive symptoms . BMC Psychiatry 7:12, 2007 Crossref , Medline , Google Scholar
92 Linke S, Murray E, Butler C, et al. : Internet-based interactive health intervention for the promotion of sensible drinking: patterns of use and potential impact on members of the general public . Journal of Medical Internet Research 9:e10, 2007 Crossref , Medline , Google Scholar
93 McCrone P, Knapp M, Proudfoot J, et al. : Cost-effectiveness of computerised cognitive-behavioural therapy for anxiety and depression in primary care: randomised controlled trial . British Journal of Psychiatry 185:55–62, 2004 Crossref , Medline , Google Scholar
94 Perini S, Titov N, Andrews G : Clinician-assisted Internet-based treatment is effective for depression: randomized controlled trial . Australian and New Zealand Journal of Psychiatry 43:571–578, 2009 Crossref , Medline , Google Scholar
95 Piasecki TM, Hufford MR, Solhan M, et al. : Assessing clients in their natural environments with electronic diaries: rationale, benefits, limitations, and barriers . Psychological Assessment 19:25–43, 2007 Crossref , Medline , Google Scholar
96 Rabiner DL, Murray DW, Skinner AT, et al. : A randomized trial of two promising computer-based interventions for students with attention difficulties . Journal of Abnormal Child Psychology 38:131–142, 2010 Crossref , Medline , Google Scholar
97 Ritterband LM, Thorndike FP, Gonder-Frederick LA, et al. : Efficacy of an Internet-based behavioral intervention for adults with insomnia . Archives of General Psychiatry 66:692–698, 2009 Crossref , Medline , Google Scholar
98 Ruggiero KJ, Resnick HS, Acierno R, et al. : Internet-based intervention for mental health and substance use problems in disaster-affected populations: a pilot feasibility study . Behavior Therapy 37:190–205, 2006 Crossref , Medline , Google Scholar
99 Spence SH, Holmes JM, March S, et al. : The feasibility and outcome of clinic plus Internet delivery of cognitive-behavior therapy for childhood anxiety . Journal of Consulting and Clinical Psychology 74:614–621, 2006 Crossref , Medline , Google Scholar
100 Titov N, Andrews G, Johnston L, et al. : Shyness programme: longer term benefits, cost-effectiveness, and acceptability . Australian and New Zealand Journal of Psychiatry 43:36–44, 2009 Crossref , Medline , Google Scholar
101 van Spijker BAJ, van Straten A, Kerkhof AJFM : The effectiveness of a Web-based self-help intervention to reduce suicidal thoughts: a randomized controlled trial . Trials 11:25, 2010 Crossref , Medline , Google Scholar
102 Van Voorhees BW, Fogel J, Reinecke MA, et al. : Randomized clinical trial of an Internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: 12-week outcomes . Journal of Developmental and Behavioral Pediatrics 30:23–37, 2009 Crossref , Medline , Google Scholar
103 Wims E, Titov N, Andrews G, et al. : Clinician-assisted Internet-based treatment is effective for panic: a randomized controlled trial . Australian and New Zealand Journal of Psychiatry 44:599–607, 2010 Crossref , Medline , Google Scholar
- Internet-Based Cognitive-Behavioral Therapy for Individuals Experiencing Panic Attacks: A Scoping Literature Review Journal of Psychosocial Nursing and Mental Health Services, Vol. 62, No. 4
- New in Town—An internet-based self-efficacy intervention for internal migrants: A randomized controlled trial 7 March 2024 | PLOS ONE, Vol. 19, No. 3
- Traditional versus virtual partial hospital programme for eating disorders: Feasibility and preliminary comparison of effects 7 September 2023 | European Eating Disorders Review, Vol. 32, No. 2
- The Effects of Using Psychotherapeutic e-Mental Health Interventions on Men’s Depression and Anxiety: Systematic Review and Meta-Analysis 9 August 2023 | Current Psychology, Vol. 43, No. 10
- A Lost Frontier or a New Gateway to Global Climate Action? The Afghan Leadership and the Revival of Afghanistan’s Mineral Sector 11 February 2024 | India Quarterly: A Journal of International Affairs, Vol. 80, No. 1
- Intersecting identities, diverse masculinities, and collaborative development: Considerations in creating online mental health interventions that work for men Comprehensive Psychiatry, Vol. 129
- Diagnostic applications and benefits of virtual reality for sexual aversion 2 February 2024 | The Journal of Sexual Medicine, Vol. 21, No. 2
- Exploring the attitudes of young people toward catfish impersonating and feigning illness on social media
- Cognitive behavioural therapy self-help intervention preferences among informal caregivers of adults with chronic kidney disease: an online cross-sectional survey 4 January 2023 | BMC Nephrology, Vol. 24, No. 1
- Digital interventions for substance use disorders in young people: rapid review 17 February 2023 | Substance Abuse Treatment, Prevention, and Policy, Vol. 18, No. 1
- A self-guided Internet-based intervention for individuals with chronic pain and depressive symptoms: study protocol of a randomized controlled trial 11 July 2023 | Trials, Vol. 24, No. 1
- Australian Psychologists Experiences with Digital Mental Health: a Qualitative Investigation 16 August 2022 | Journal of Technology in Behavioral Science, Vol. 8, No. 4
- The effect of smartphone-based monitoring and treatment including clinical feedback versus smartphone-based monitoring without clinical feedback in bipolar disorder: the SmartBipolar trial—a study protocol for a randomized controlled parallel-group trial 12 September 2023 | Trials, Vol. 24, No. 1
- Be a Mom Coping with Depression: a Feasibility Study of a Blended Cognitive-Behavioral Intervention for Postpartum Depression 16 August 2023 | International Journal of Cognitive Therapy, Vol. 16, No. 4
- Parents' acceptability of blended psychological interventions for children with emotional disorders Internet Interventions, Vol. 34
- Lockdown during the early phase of Covid-19 – effects on specialized mental health services and vocational activities for patients with psychotic disorders 3 August 2023 | Nordic Journal of Psychiatry, Vol. 77, No. 8
- A Brief Wellbeing Training Session Delivered by a Humanoid Social Robot: A Pilot Randomized Controlled Trial 12 October 2023 | International Journal of Social Robotics, Vol. 6
- Crossover of the dimensions of work-family and family-work conflict in couples: Protocol for a qualitative study 28 September 2023 | PLOS ONE, Vol. 18, No. 9
- Active transport to school and health-enhancing physical activity: a rapid review of European evidence 31 May 2023 | Cities & Health, Vol. 7, No. 5
- Evaluating the Usability of a Serious Game for Nutritional Education with Children with ADHD
- Potential implementers’ perspectives on the development and implementation of an e-mental health intervention for caregivers of adults with chronic kidney disease: a qualitative study (Preprint) 2 August 2023 | JMIR Human Factors
- How to e-mental health: a guideline for researchers and practitioners using digital technology in the context of mental health 7 August 2023 | Nature Mental Health, Vol. 1, No. 8
- Evaluation of Psychometric Properties of the Acceptability of ICT Use for Mental Health Care Questionnaire 20 June 2022 | International Journal of Mental Health and Addiction, Vol. 21, No. 4
- Improving older adults' autobiographical memory through video‐conferencing intervention during COVID‐19 1 August 2023 | International Journal of Geriatric Psychiatry, Vol. 38, No. 8
- Stepping up to COVID-19: A Clinical Trial of a Telepsychology Positive Parenting Program Targeting Behavior Problems in Children With Neurological Risk 14 June 2023 | Journal of Pediatric Psychology, Vol. 48, No. 6
- Suicidal Ideation Amongst University Students During the COVID-19 Pandemic: Time Trends and Risk Factors 6 December 2022 | The Canadian Journal of Psychiatry, Vol. 68, No. 7
- Loving-kindness and walking meditation with a robot: Countering negative mood by stimulating creativity International Journal of Human-Computer Studies, Vol. 12
- Videoconferencing versus face‐to‐face psychotherapy: Insights from patients and psychotherapists about comparability of therapeutic alliance, empathy and treatment characteristics 17 May 2022 | Counselling and Psychotherapy Research, Vol. 23, No. 2
- Experiences of a Digital Mental Health Intervention from the Perspectives of Young People Recovering from First-Episode Psychosis: A Focus Group Study 8 May 2023 | International Journal of Environmental Research and Public Health, Vol. 20, No. 9
- The impact of COVID‐19 on school‐age children 1 December 2022 | Psychology in the Schools, Vol. 60, No. 5
- Implementation of eMental health technologies for informal caregivers: A multiple case study 24 March 2023 | Frontiers in Digital Health, Vol. 5
- Assessment of App Store Description and Privacy Policy to Explore Ethical and Safety Concerns Associated with the Use of Mental Health Apps for Depression 14 January 2023 | Indian Journal of Psychological Medicine, Vol. 45, No. 2
- The effectiveness of an internet-based support program on maternal self-efficacy, postpartum depression and social support for primiparous women during the COVID-19 pandemic: Randomized controlled trial 9 February 2023 | Frontiers in Public Health, Vol. 11
- “I don’t think they’re as culturally sensitive”: a mixed-method study exploring e-mental health use among culturally diverse populations 30 June 2022 | Journal of Mental Health, Vol. 32, No. 1
- The Potential of Internet-Based Psychological Interventions for Perinatal Depression Prevention and Treatment 30 November 2022
- A blended psychological intervention for postpartum depression: acceptability and preferences in women presenting depressive symptoms 21 August 2021 | Journal of Reproductive and Infant Psychology, Vol. 41, No. 1
- Workplace Wellness, Mental Health Literacy, and Usage Intention of E-Mental Health amongst Digital Workers during the COVID-19 Pandemic International Journal of Mental Health Promotion, Vol. 25, No. 1
- Family Intervention in Psychosis: A Case 26 April 2023
- New Technologies (Tele-Health and Other Trends) Directed in Neurology and Psychiatric Disorders in Home Care 13 June 2023
- mHealth Early Intervention to Reduce Posttraumatic Stress and Alcohol Use After Sexual Assault (THRIVE): Feasibility and Acceptability Results From a Pilot Trial 4 July 2023 | JMIR Formative Research, Vol. 7
- Smartphone-Based Treatment in Psychiatry: A Systematic Review 1 January 2023
- Digital Health Secondary Prevention Using Co-Design Procedures: Focus Group Study With Health Care Providers and Patients With Myocardial Infarction 30 October 2023 | JMIR Cardio, Vol. 7
- User profiles of electronic ecological momentary assessment in outpatient child and adolescent mental health services Spanish Journal of Psychiatry and Mental Health, Vol. 16, No. 1
- e-Mental health
- Time in schizophrenia: a link between psychopathology, psychophysics and technology 12 August 2022 | Translational Psychiatry, Vol. 12, No. 1
- E-Mental-Health aftercare for children and adolescents after partial or full inpatient psychiatric hospitalization: study protocol of the randomized controlled DigiPuR trial 26 August 2022 | Trials, Vol. 23, No. 1
- Recruitment, adherence and attrition challenges in internet-based indicated prevention programs for eating disorders: lessons learned from a randomised controlled trial of ProYouth OZ 4 January 2022 | Journal of Eating Disorders, Vol. 10, No. 1
- Guidelines for conducting rapid reviews in psychology research 22 December 2022 | Journal of Psychology in Africa, Vol. 32, No. 6
- Family Intervention in Severe Mental Disorder: An Online Intervention Format in Psychosocial Rehabilitation Centers 6 October 2022 | Journal of Psychosocial Rehabilitation and Mental Health, Vol. 23
- Online intervention to prevent postnatal depression and anxiety in Chilean new mothers: Protocol for a feasibility trial 27 October 2022 | Health Informatics Journal, Vol. 28, No. 4
- A Blended Cognitive–Behavioral Intervention for the Treatment of Postpartum Depression: A Case Study 12 April 2022 | Clinical Case Studies, Vol. 21, No. 5
- Compassionate Technology: A Systematic Scoping Review of Compassion as Foundation for Blended and Digital Mental Health Interventions (Preprint) 8 September 2022 | JMIR Mental Health
- Regional and rural clients’ presenting concerns and experiences of care when engaging with an online substance use counseling service 26 February 2022 | Addiction Research & Theory, Vol. 30, No. 5
- Personal experience of Latin American therapists on their clinical practice during the COVID-19 pandemic ( Experiencia personal de terapeutas latinoamericanos sobre su práctica clínica durante la pandemia por COVID-19 ) 20 December 2022 | Studies in Psychology, Vol. 43, No. 3
- Potential and Pitfalls of Mobile Mental Health Apps in Traditional Treatment: An Umbrella Review 25 August 2022 | Journal of Personalized Medicine, Vol. 12, No. 9
- Implementation of E-Mental Health Interventions for Informal Caregivers of Adults with Chronic Diseases: A Mixed-Methods Systematic Review with Qualitative Comparative Analysis and Thematic Synthesis (Preprint) 15 August 2022 | JMIR Mental Health
- Acceptability and satisfaction with emma, a smartphone application dedicated to suicide ecological assessment and prevention 11 August 2022 | Frontiers in Psychiatry, Vol. 13
- Attitudes toward innovative mental health treatment approaches in Germany: E-mental health and home treatment 15 July 2022 | Frontiers in Psychiatry, Vol. 13
- Technology-Based Interventions to Improve Help-Seeking for Mental Health Concerns: A Systematic Review 21 September 2021 | Indian Journal of Psychological Medicine, Vol. 44, No. 4
- Online and Offline Intervention for the Prevention of Postpartum Depression among Rural-to-Urban Floating Women: Study Protocol for a Randomized Control Trial 29 June 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 13
- Theory of Planned Behavior 29 December 2021 | Journal of Nervous & Mental Disease, Vol. 210, No. 7
- Development of Flow State Self-Regulation Skills and Coping With Musical Performance Anxiety: Design and Evaluation of an Electronically Implemented Psychological Program 17 June 2022 | Frontiers in Psychology, Vol. 13
- Differences in mobility patterns according to machine learning models in patients with bipolar disorder and patients with unipolar disorder Journal of Affective Disorders, Vol. 306
- What Comes after the Trial? An Observational Study of the Real-World Uptake of an E-Mental Health Intervention by General Practitioners to Reduce Depressive Symptoms in Their Patients 19 May 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 10
- Gaming My Way to Recovery: A Systematic Scoping Review of Digital Game Interventions for Young People's Mental Health Treatment and Promotion 7 April 2022 | Frontiers in Digital Health, Vol. 4
- Supporting Relatives Prior to Caregiver Burden—Preventive E-Mental Health Short Intervention for Family Members of Individuals with Parkinsonism in an Early Phase of the Disease: Protocol for a Feasibility Study 26 March 2022 | Brain Sciences, Vol. 12, No. 4
- COVID Feel Good: Evaluation of a Self-Help Protocol to Overcome the Psychological Burden of the COVID-19 Pandemic in a German Sample 7 April 2022 | Journal of Clinical Medicine, Vol. 11, No. 8
- The impact of COVID-19 on addiction treatment in New Zealand Addictive Behaviors, Vol. 127
- School counselling during COVID-19: an initial examination of school counselling use during a 5-week remote learning period 1 December 2020 | Pastoral Care in Education, Vol. 40, No. 1
- e-Mental Health and Health Informatics 7 November 2022
- Pollutant extraction from water and soil using Montmorillonite clay-polymer composite: A rapid review Materials Today: Proceedings, Vol. 60
- User experience and acceptance of patients and healthy adults testing a personalized self-management app for depression: A non-randomized mixed-methods feasibility study 7 April 2022 | DIGITAL HEALTH, Vol. 8
- Immersive Reality Experience Technology for Reducing Social Isolation and Improving Social Connectedness and Well-being of Children and Young People Who Are Hospitalized: Open Trial 25 March 2022 | JMIR Pediatrics and Parenting, Vol. 5, No. 1
- Egyptian Students Open to Digital Mental Health Care: Cross-Sectional Survey 21 March 2022 | JMIR Formative Research, Vol. 6, No. 3
- Acceptability of Web-Based Mental Health Interventions in the Workplace: Systematic Review 11 May 2022 | JMIR Mental Health, Vol. 9, No. 5
- Design of a Game-Based Training Environment to Enhance Mental Health Care Professionals’ Skills in Using e–Mental Health: Multiple Methods User Requirements Analysis 27 July 2022 | JMIR Serious Games, Vol. 10, No. 3
- Meeting the Unmet Needs of Individuals With Mental Disorders: Scoping Review on Peer-to-Peer Web-Based Interactions 5 December 2022 | JMIR Mental Health, Vol. 9, No. 12
- Motive-Oriented, Personalized, Internet-Based Interventions for Depression: Nonclinical Experimental Study 13 September 2022 | JMIR Formative Research, Vol. 6, No. 9
- A Web-Based Positive Psychology App for Patients With Bipolar Disorder: Development Study 19 September 2022 | JMIR Formative Research, Vol. 6, No. 9
- Incorporating health information technology/information communication technology into prevention and treatment of mental health disorders Annals of Indian Psychiatry, Vol. 6, No. 2
- The effectiveness of e-healthcare interventions for mental health of nurses 24 June 2022 | Medicine, Vol. 101, No. 25
- The effects of non-clinician guidance on effectiveness and process outcomes of digital mental health interventions: A systematic review and meta-analysis (Preprint) 31 December 2021 | Journal of Medical Internet Research
- Clinical Staging for Youth Mental Disorders: Progress in Reforming Diagnosis and Clinical Care Annual Review of Developmental Psychology, Vol. 3, No. 1
- Is Mental Illness like Any Other Medical Illness? Causal Attributions, Supportive Communication and the Social Withdrawal Inclination of People with Chronic Mental Illnesses in China 26 August 2020 | Health Communication, Vol. 36, No. 14
- Accessibility of mental health support in China and preferences on web-based services for mood disorders: A qualitative study Internet Interventions, Vol. 26
- A randomized controlled trial on a self-guided Internet-based intervention for gambling problems 22 June 2021 | Scientific Reports, Vol. 11, No. 1
- ICan, an Internet-based intervention to reduce cannabis use: study protocol for a randomized controlled trial 6 January 2021 | Trials, Vol. 22, No. 1
- Associations between the cortisol awakening response and patient-evaluated stress and mood instability in patients with bipolar disorder: an exploratory study 1 March 2021 | International Journal of Bipolar Disorders, Vol. 9, No. 1
- TourHeart—An Online Stratified Stepped Care Mental Health Platform: Qualitative Evaluation from Multiple Stakeholders’ Perspectives (Preprint) 18 November 2021 | JMIR Human Factors
- A mixed methods exploration of “Creativity in Mind”, an online creativity-based intervention for low mood and anxiety 19 May 2021 | Journal of Mental Health, Vol. 30, No. 6
- Targeting hostile attributions in inclusive schools through online cognitive bias modification: A randomised experiment Behaviour Research and Therapy, Vol. 146
- eSano – An eHealth Platform for Internet- and Mobile-based Interventions
- Alien Attack: A Non-Pharmaceutical Complement for ADHD Treatment 11 October 2021 | Entropy, Vol. 23, No. 10
- Integrating eHealth within a Transforming Mental Healthcare Setting: A Qualitative Study into Values, Challenges, and Prerequisites 29 September 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 19
- Technology Enhanced Health and Social Care for Vulnerable People During the COVID-19 Outbreak 10 September 2021 | Frontiers in Human Neuroscience, Vol. 15
- Evaluation of the effectiveness of online mental health first aid guidelines for helping someone experiencing gambling problems 21 May 2020 | Advances in Mental Health, Vol. 19, No. 3
- The COVID PIVOT – Re-orienting Child and Youth Mental Health Care in the Light of Pandemic Restrictions 22 March 2021 | Psychiatric Quarterly, Vol. 92, No. 3
- Research on the Characteristics and Usefulness of User Reviews of Online Mental Health Consultation Services: A Content Analysis 27 August 2021 | Healthcare, Vol. 9, No. 9
- Stakeholders’ views on online interventions to prevent common mental health disorders in adults implemented into existing healthcare systems in Europe 7 July 2021 | European Journal of Public Health, Vol. 31, No. Supplement_1
- The Interplay between Social and Ecological Determinants of Mental Health for Children and Youth in the Climate Crisis 26 April 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 9
- A Participatory Design of Conversational Artificial Intelligence Agents for Mental Healthcare Application (Preprint) 29 April 2021 | JMIR Formative Research
- Disclosure of suicidal thoughts during an e-mental health intervention: relational ethics meets actor-network theory 1 December 2019 | Ethics & Behavior, Vol. 31, No. 3
- Community Mental Health Care Delivery During the COVID-19 Pandemic: Practical Strategies for Improving Care for People with Serious Mental Illness 19 June 2020 | Community Mental Health Journal, Vol. 57, No. 3
- Establishing the content validity of an online depression screening tool for South Africa 26 October 2021 | African Journal of Psychological Assessment, Vol. 3
- Analysis of topics and characteristics of user reviews on different online psychological counseling methods International Journal of Medical Informatics, Vol. 147
- Virtually Real, But Not Quite There: Social and Economic Barriers to Meeting Virtual Reality’s True Potential for Mental Health 17 February 2021 | Frontiers in Virtual Reality, Vol. 2
- The Practice-Based Implementation (PBI) Network: Technology (Tech) into Care pilot 28 November 2019 | Translational Behavioral Medicine, Vol. 11, No. 1
- How digital health solutions align with the roles and functions that support hospital to home transitions for older adults: a rapid review study protocol 25 February 2021 | BMJ Open, Vol. 11, No. 2
- Digital systemic practices in Europe: a survey before the Covid‐19 pandemic 9 September 2020 | Journal of Family Therapy, Vol. 43, No. 1
- Screening and supporting the mental health of student physiotherapists during the COVID-19 pandemic International Journal of Therapy and Rehabilitation, Vol. 28, No. 1
- A Decision Support System for the Prediction of Drug Predisposition Through Personality Traits 1 January 2022
- Defining Rapid Reviews: a systematic scoping review and thematic analysis of definitions and defining characteristics of rapid reviews Journal of Clinical Epidemiology, Vol. 129
- The emergence of digital mental health in low-income and middle-income countries: A review of recent advances and implications for the treatment and prevention of mental disorders Journal of Psychiatric Research, Vol. 133
- Digital Health Applications in Mental Health Care for Immigrants and Refugees: A Rapid Review Telemedicine and e-Health, Vol. 27, No. 1
- Priority Given to Technology in Government-Based Mental Health and Addictions Vision and Strategy Documents: Systematic Policy Review 5 May 2021 | Journal of Medical Internet Research, Vol. 23, No. 5
- Multimodule Web-Based COVID-19 Anxiety and Stress Resilience Training (COAST): Single-Cohort Feasibility Study With First Responders 7 June 2021 | JMIR Formative Research, Vol. 5, No. 6
- A Digital Health Innovation to Prevent Relapse and Support Recovery in Youth Receiving Specialized Services for First-Episode Psychosis: Protocol for a Pilot Pre-Post, Mixed Methods Study of Horyzons-Canada (Phase 2) 7 December 2021 | JMIR Research Protocols, Vol. 10, No. 12
- Using Information and Communication Technologies (ICT) for Mental Health Prevention and Treatment 8 January 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 2
- mHealth for Illness Self-Management for People With Schizophrenia
- Les interventions psychosociales destinées aux personnes composant avec un premier épisode psychotique : une revue narrative et critique Santé mentale au Québec, Vol. 46, No. 2
- Daily mobility patterns in patients with bipolar disorder and healthy individuals Journal of Affective Disorders, Vol. 278
- Video Consultation Consumer Home-based Assessment Tool (VC-CHAT) 22 July 2020 | Australian & New Zealand Journal of Psychiatry, Vol. 54, No. 12
- Healthcare professionals’ perspectives on mental health service provision: a pilot focus group study in six European countries 6 March 2020 | International Journal of Mental Health Systems, Vol. 14, No. 1
- Patient-evaluated cognitive function measured with smartphones and the association with objective cognitive function, perceived stress, quality of life and function capacity in patients with bipolar disorder 30 October 2020 | International Journal of Bipolar Disorders, Vol. 8, No. 1
- Exploring meaning in life through a brief photo-ethnographic intervention using Instagram: a Bayesian growth modelling approach 5 October 2020 | International Review of Psychiatry, Vol. 32, No. 7-8
- Added value or added burden? A qualitative investigation of blending internet self-help with face-to-face cognitive behaviour therapy for depression 5 February 2020 | Psychotherapy Research, Vol. 30, No. 8
- A Blended Cognitive–Behavioral Intervention for the Treatment of Postpartum Depression: Study Protocol for a Randomized Controlled Trial 20 November 2020 | International Journal of Environmental Research and Public Health, Vol. 17, No. 22
- eHealth Treatments for Compulsive Overeating: a Narrative Review 23 May 2020 | Current Addiction Reports, Vol. 7, No. 3
- Social robots as treatment agents: Pilot randomized controlled trial to deliver a behavior change intervention Internet Interventions, Vol. 21
- Computer incursion in psychiatry via e-mental health: Innovation and implications to keep in mind RIVISTA SPERIMENTALE DI FRENIATRIA, No. 2
- The Cultural Adaptation of Step-by-Step: An Intervention to Address Depression Among Chinese Young Adults 7 July 2020 | Frontiers in Psychiatry, Vol. 11
- A Web-based Psychoeducation Program for People with Pathological Dissociation: Development and Pilot Testing 29 April 2020 | Journal of Evidence-Based Social Work, Vol. 17, No. 4
- Be a Mom’s Efficacy in Enhancing Positive Mental Health among Postpartum Women Presenting Low Risk for Postpartum Depression: Results from a Pilot Randomized Trial 29 June 2020 | International Journal of Environmental Research and Public Health, Vol. 17, No. 13
- Mitigating the psychological effects of social isolation during the covid-19 pandemic 21 May 2020 | BMJ
- Automatically generated smartphone data and subjective stress in healthy individuals – a pilot study 27 December 2019 | Nordic Journal of Psychiatry, Vol. 74, No. 4
- Utilization of e-mental-health and online self-management interventions of patients with mental disorders—A cross-sectional analysis 20 April 2020 | PLOS ONE, Vol. 15, No. 4
- Applying gender-based analysis plus to Employee Assistance Programs: A Canadian perspective 26 March 2020 | Journal of Workplace Behavioral Health, Vol. 35, No. 2
- Feasibility of perinatal mood screening and text messaging on patients’ personal smartphones 15 June 2019 | Archives of Women's Mental Health, Vol. 23, No. 2
- YouTube as a New Medium for Dementia Education Among Chinese Americans 22 October 2019 | Community Mental Health Journal, Vol. 56, No. 3
- Implementation of e‐mental health for depression and anxiety: A critical scoping review 16 January 2020 | Journal of Community Psychology, Vol. 48, No. 3
- Perspectives of Young Adults on Receiving Telepsychiatry Services in an Urban Early Intervention Program for First-Episode Psychosis: A Cross-Sectional, Descriptive Survey Study 3 March 2020 | Frontiers in Psychiatry, Vol. 11
- Client experiences of blending a coping-focused therapy for auditory verbal hallucinations with smartphone-based ecological momentary assessment and intervention Internet Interventions, Vol. 19
- Hypomania/Mania by DSM-5 definition based on daily smartphone-based patient-reported assessments Journal of Affective Disorders, Vol. 264
- Using Persuasive Systems Design Model to Evaluate “Cuida tu Ánimo”: An Internet-Based Pilot Program for Prevention and Early Intervention of Adolescent Depression Telemedicine and e-Health, Vol. 26, No. 2
- Global research priorities for youth mental health 20 January 2020 | Early Intervention in Psychiatry, Vol. 14, No. 1
- User-Oriented Interface for Monitoring Affective Diseases in Patients with Bipolar Disorder Using Mobile Devices 28 May 2020
- eMental health service use among Australian youth: a cross-sectional survey framed by Andersen's model Australian Health Review, Vol. 44, No. 6
- A Decade of Ubiquitous Computing Research in Mental Health IEEE Pervasive Computing, Vol. 19, No. 1
- <p>Understanding Interactions Between Caregivers and Care Recipients in Person-Centered Dementia Care: A Rapid Review</p> 1 September 2020 | Clinical Interventions in Aging, Vol. Volume 15
- Digital Game Interventions for Youth Mental Health Services (Gaming My Way to Recovery): Protocol for a Scoping Review 24 June 2020 | JMIR Research Protocols, Vol. 9, No. 6
- Evaluation of Electronic Mental Health Implementation in Northern Territory Services Using the Integrated “Promoting Action on Research Implementation in Health Services” Framework: Qualitative Study 26 May 2020 | JMIR Mental Health, Vol. 7, No. 5
- Forecasting Mood in Bipolar Disorder From Smartphone Self-assessments: Hierarchical Bayesian Approach 1 April 2020 | JMIR mHealth and uHealth, Vol. 8, No. 4
- Role of a Digital Return-To-Work Solution for Individuals With Common Mental Disorders: Qualitative Study of the Perspectives of Three Stakeholder Groups 16 September 2020 | JMIR Formative Research, Vol. 4, No. 9
- Potential of Mobile Technology to Relieve the Urgent Mental Health Needs in China: Web-Based Survey 7 July 2020 | JMIR mHealth and uHealth, Vol. 8, No. 7
- Integrating People, Context, and Technology in the Implementation of a Web-Based Intervention in Forensic Mental Health Care: Mixed-Methods Study 26 May 2020 | Journal of Medical Internet Research, Vol. 22, No. 5
- Youth Experiences With Referrals to Mental Health Services in Canada: Protocol for a Web-Based Cross-Sectional Survey Study 24 March 2020 | JMIR Research Protocols, Vol. 9, No. 3
- Repetitive Transcranial Magnetic Stimulation With and Without Internet-Delivered Cognitive-Behavioral Therapy for the Treatment of Resistant Depression: Protocol for Patient-Centered Randomized Controlled Pilot Trial 27 October 2020 | JMIR Research Protocols, Vol. 9, No. 10
- Connected Mental Health: Systematic Mapping Study 28 August 2020 | Journal of Medical Internet Research, Vol. 22, No. 8
- Conditional cash transfers: A critical review 25 October 2019 | Development Policy Review, Vol. 38, No. 1
- Postpartum Mental Health Care for Mothers of Multiples: A Qualitative Study of New Mothers’ Treatment Preferences 1 May 2020 | Journal of Psychiatric Practice, Vol. 26, No. 3
- Reporting guidelines on remotely collected electronic mood data in mood disorder (eMOOD)—recommendations 7 June 2019 | Translational Psychiatry, Vol. 9, No. 1
- A self-guided Internet-based intervention for individuals with gambling problems: study protocol for a randomized controlled trial 23 January 2019 | Trials, Vol. 20, No. 1
- Group art activities and arts therapies for people using substances: A rapid review of the literature Nordic Journal of Arts, Culture and Health, Vol. 1, No. 1
- Common themes and emerging trends for the use of technology to support mental health and psychosocial well-being in limited resource settings: A review of the literature Psychiatry Research, Vol. 281
- Examining the usage, user experience and perceived impact of an Internet-based cognitive behavioural therapy program for adolescents with anxiety: Results from a randomized controlled trial (Preprint) 7 August 2019 | JMIR Mental Health
- Characteristics of stakeholder involvement in systematic and rapid reviews: a methodological review in the area of health services research 15 August 2019 | BMJ Open, Vol. 9, No. 8
- The association between mixed symptoms, irritability and functioning measured using smartphones in bipolar disorder 28 March 2019 | Acta Psychiatrica Scandinavica, Vol. 139, No. 5
- Key steps for a mental health and addictions performance measurement framework for Canada 10 February 2019 | Healthcare Management Forum, Vol. 32, No. 2
- E-mental health: Promising advancements in policy, research, and practice 10 February 2019 | Healthcare Management Forum, Vol. 32, No. 2
- Using rapid reviews to strengthen health policy and systems and progress towards universal health coverage 5 February 2019 | BMJ Global Health, Vol. 4, No. 1
- , Vol. 1192
- Clinical Child and Family Psychology Review, Vol. 22, No. 2
- Transitioning to adulthood: A glance at the education system Children and Youth Services Review, Vol. 96
- Internet Interventions, Vol. 18
- Cost-Effectiveness Evaluations of Psychological Therapies for Schizophrenia and Bipolar Disorder: A Systematic Review 22 July 2019 | International Journal of Technology Assessment in Health Care, Vol. 35, No. 4
- Journal of Consumer Health on the Internet, Vol. 23, No. 1
- CoDesign, Vol. 15, No. 3
- Translational Behavioral Medicine
- Kann eine Online-Intervention für Depressionen emotionale Probleme und Schmerzen lindern? Eine randomisiert-kontrollierte Studie 26 July 2019 | Verhaltenstherapie, Vol. 29, No. 3
- PLOS ONE, Vol. 14, No. 5
- Journal of Medical Internet Research, Vol. 21, No. 3
- JMIR Mental Health, Vol. 6, No. 10
- JMIR Formative Research, Vol. 3, No. 2
- JMIR Mental Health, Vol. 6, No. 7
- Journal of Medical Internet Research, Vol. 21, No. 10
- Medical Journal of Australia, Vol. 211, No. S7
- www.psychopap.com : améliorer l’accès à la psychothérapie par le transfert des connaissances aux patients et aux futurs thérapeutes 11 November 2020 | Santé mentale au Québec, Vol. 44, No. 2
- OpenSIMPLe: A real-world implementation feasibility study of a smartphone-based psychoeducation programme for bipolar disorder Journal of Affective Disorders, Vol. 241
- Be a Mom: Formative Evaluation of a Web-Based Psychological Intervention to Prevent Postpartum Depression Cognitive and Behavioral Practice, Vol. 25, No. 4
- Working adults’ well‐being: An online self‐help goal‐based intervention 23 March 2018 | Journal of Occupational and Organizational Psychology, Vol. 91, No. 3
- European Psychiatric Association (EPA) guidance on forensic psychiatry: Evidence based assessment and treatment of mentally disordered offenders 1 January 2020 | European Psychiatry, Vol. 51
- Michael S. Dunbar , Ph.D. ,
- Lisa Sontag-Padilla , Ph.D. ,
- Courtney A. Kase , M.P.H. ,
- Rachana Seelam , M.P.H. ,
- Bradley D. Stein , M.D., Ph.D.
- Internet- and Mobile-Based Psychological Interventions: Applications, Efficacy, and Potential for Improving Mental Health European Psychologist, Vol. 23, No. 2
- Academic Pediatrics, Vol. 18, No. 1
- Asian Journal of Psychiatry, Vol. 38
- Internet Interventions, Vol. 12
- Internet Interventions, Vol. 14
- Seminars in Oncology Nursing, Vol. 34, No. 3
- International Journal of Forensic Mental Health, Vol. 17, No. 1
- Journal of Technology in Human Services, Vol. 36, No. 4
- Journal of Workplace Behavioral Health, Vol. 33, No. 3-4
- IOP Conference Series: Materials Science and Engineering, Vol. 407
- Health & Social Care in the Community, Vol. 26, No. 4
- Effectiveness and impact of networked communication interventions in young people with mental health conditions: A rapid review 21 March 2018 | DIGITAL HEALTH, Vol. 4
- Trials, Vol. 19, No. 1
- International Journal of Bipolar Disorders, Vol. 6, No. 1
- PLOS ONE, Vol. 13, No. 2
- PLOS ONE, Vol. 13, No. 6
- Korean Journal of Journalism & Communication Studies, Vol. 62, No. 6
- Journal of Medical Internet Research, Vol. 20, No. 10
- JMIR Human Factors, Vol. 5, No. 1
- Journal of Medical Internet Research, Vol. 20, No. 8
- JMIR Mental Health, Vol. 5, No. 2
- JMIR Research Protocols, Vol. 7, No. 4
- Etyczne aspekty prowadzenia terapii online: analiza wybranych stron internetowych 1 January 2018 | Annales Universitatis Paedagogicae Cracoviensis. Studia de Cultura, Vol. 4, No. 10
- International Journal of Integrated Care, Vol. 18, No. 4
- Adaptive coping strategies of affected family members of a relative with substance misuse: A qualitative study 8 September 2017 | Journal of Advanced Nursing, Vol. 74, No. 1
- Introduction of e-mental health in national health systems – A health professionals' perspective Health Policy and Technology, Vol. 6, No. 4
- Online ethics: where will the interface of mental health and the internet lead us? 6 August 2017 | International Journal of Bipolar Disorders, Vol. 5, No. 1
- There's No Time like the Present: Improving the Current System of Care for Low-Income Substance Abusers with Comorbid Health Conditions 3 May 2018 | Families in Society: The Journal of Contemporary Social Services, Vol. 98, No. 4
- Arts on prescription in Scandinavia: a review of current practice and future possibilities 16 November 2016 | Perspectives in Public Health, Vol. 137, No. 5
- Internetnutzung bei depressiven Patienten 7 August 2017 | NeuroTransmitter, Vol. 28, No. 7-8
- Effects of a web-based follow-up intervention on self-efficacy in obesity treatment for women 13 April 2017 | Wiener klinische Wochenschrift, Vol. 129, No. 13-14
- A Mapping Study on the Internet and Suicide Crisis, Vol. 38, No. 4
- People, processes, and systems: An observational study of the role of technology in rural youth mental health services 23 November 2016 | International Journal of Mental Health Nursing, Vol. 26, No. 3
- E-mental health and the veterinary profession Journal of the American Veterinary Medical Association, Vol. 250, No. 11
- Integrative Approach to Child and Adolescent Mental Health 24 May 2017
- User profiles of an electronic mental health tool for ecological momentary assessment: MEmind 9 March 2017 | International Journal of Methods in Psychiatric Research, Vol. 26, No. 1
- E-mental Health for Elderly: Challenges and Proposals for Sustainable Integrated Psychological Interventions in Primary Care 31 January 2017 | Frontiers in Psychology, Vol. 8
- Contemporary Family Therapy, Vol. 39, No. 4
- Academic Psychiatry, Vol. 41, No. 6
- Journal of Technology in Behavioral Science, Vol. 2, No. 1
- Asian Journal of Psychiatry, Vol. 25
- Behaviour Research and Therapy, Vol. 88
- Current Perspectives on e-Mental-Health Self-Help Treatments: Exploring the “Black Box” of Public Views, Perceptions, and Attitudes Toward the Digitalization of Mental Health Care 17 June 2017
- International Journal of Forensic Mental Health, Vol. 16, No. 2
- Social Work in Mental Health, Vol. 15, No. 6
- BMC Medical Informatics and Decision Making, Vol. 17, No. 1
- BMC Health Services Research, Vol. 17, No. 1
- Implementation Science, Vol. 12, No. 1
- PLOS ONE, Vol. 12, No. 7
- JMIR Human Factors, Vol. 4, No. 1
- Journal of Medical Internet Research, Vol. 19, No. 8
- JMIR Mental Health, Vol. 4, No. 2
- JMIR Mental Health, Vol. 4, No. 1
- JMIR Mental Health, Vol. 4, No. 3
- JMIR Research Protocols, Vol. 6, No. 12
- Journal of Mental Health, Vol. 26, No. 1
- Frontiers in Psychology, Vol. 8
- What E-Mental Health Can Offer to Saudi Arabia Using an Example of Australian E-Mental Health
- The Applicability of Currently Available Adults ADHD Treatment Tools
- Electronic self-monitoring of mood using IT platforms in adult patients with bipolar disorder: A systematic review of the validity and evidence 15 January 2016 | BMC Psychiatry, Vol. 16, No. 1
- Delivering the session 28 December 2016
- Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder 11 August 2016 | The Canadian Journal of Psychiatry, Vol. 61, No. 9
- Are There Other Options? 19 May 2016 | Journal of Health Management, Vol. 18, No. 2
- Using e-Mental Health Services for the Benefit of Consumers in Saudi Arabia 22 March 2016
- Journal of Child and Family Studies, Vol. 25, No. 10
- International Journal of Medical Informatics, Vol. 94
- Nurse Education Today, Vol. 37
- Systematic Reviews, Vol. 5, No. 1
- Rehabilitation Research, Policy, and Education, Vol. 30, No. 3
- Journal of Medical Internet Research, Vol. 18, No. 1
- Journal of Medical Internet Research, Vol. 18, No. 5
- Journal of Medical Internet Research, Vol. 18, No. 4
- Journal of Medical Internet Research, Vol. 18, No. 6
- JMIR Mental Health, Vol. 3, No. 2
- JMIR Research Protocols, Vol. 5, No. 4
- LA CYBERTHÉRAPIE DANS LE TRAITEMENT DE L’HYPERPHAGIE BOULIMIQUE : RECENSION DE LA LITTÉRATURE 12 June 2017 | Revue québécoise de psychologie, Vol. 37, No. 1
- Psychiatric Apps: Patient Self-Assessment, Communication, and Potential Treatment Interventions
- The Affordable Care Act, Accountable Care Organizations, and Mental Health Care for Older Adults Harvard Review of Psychiatry, Vol. 23, No. 5
- Shalini Lal , Ph.D. ,
- Jennifer Dell'Elce , B.A. , and
- Ashok K. Malla , M.B.B.S., F.R.C.P.C.
- Current Psychiatry Reports, Vol. 17, No. 11
- Contemporary Clinical Trials, Vol. 44
- Internet Interventions, Vol. 2, No. 2
- Games for Health Journal, Vol. 4, No. 6
- BMC Health Services Research, Vol. 16, No. 1
- Journal of Medical Internet Research, Vol. 17, No. 5
- JMIR Mental Health, Vol. 2, No. 2
- International Review of Psychiatry, Vol. 27, No. 6
- Journal of Mental Health, Vol. 24, No. 5
- IEEE Transactions on Affective Computing, Vol. 5, No. 3
- Journal of Medical Internet Research, Vol. 16, No. 10
- International Journal of Environmental Research and Public Health, Vol. 11, No. 10

- Open access
- Published: 02 May 2022
Rethinking mental wellness among adolescents: an integrative review protocol of mental health components
- Zaida Orth ORCID: orcid.org/0000-0002-2895-0417 1 &
- Brian van Wyk ORCID: orcid.org/0000-0003-1032-1847 1
Systematic Reviews volume 11 , Article number: 83 ( 2022 ) Cite this article
5977 Accesses
4 Citations
1 Altmetric
Metrics details
Adolescents have been overlooked in global public health initiatives as this period is generally considered to be the healthiest in an individual’s life course. However, the growth of the global adolescent population and their changing health profiles have called attention to the diverse health needs of adolescents. The increased attention toward adolescent health has accentuated existing gaps as global health reports have emphasised that there is a continued need for valid and reliable health data. In this context, evidence has shown that mental health issues constitute one of the greatest burdens of disease for adolescents. This integrative review aims to unpack the meaning of mental wellness among adolescents and its associated constructs by analysing and synthesising empirical and theoretical research on adolescent mental wellness. In doing this, we will develop a working definition of adolescent mental wellness that can be used to develop an instrument aimed at measuring adolescent mental wellness.
The integrative review is guided by the five steps described by Whittemore and Knafl. A comprehensive search strategy which will include carefully selected terms that correspond to the domains of interest (positive mental health/mental wellness) will be used to search for relevant literature on electronic databases, grey literature and government or non-governmental organisations (NGO) websites. Studies will be included if they describe and/or define general mental wellness in adolescent populations aged 10–19. The screening and reporting of the review will be conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Data from the integrative review will be analysed using narrative framework synthesis for qualitative and quantitative studies.
This integrative review aims to search for and synthesise current research regarding adolescent mental wellness to identify how wellness is being described and conceptualised. We aim to identify gaps and to contribute to a more comprehensive definition of mental wellness which can aid in the development of an age- and culturally appropriate measure of adolescent mental wellness.
Peer Review reports
In 2016, adolescents (10–19 years) were estimated at 1.2 billion (18%) of the world population, making them the largest population of adolescents in history [ 1 , 2 ]. Adolescents have been largely overlooked in global health and social policies, because this period is generally considered to be the healthiest in an individual’s life-course [ 2 ], and the unique health problems associated with adolescence have been misconstrued or ignored in favour of more pressing public health concerns [ 3 ]. However, changing health profiles of adolescents in both developed and developing countries have called attention to the diverse health needs of adolescents [ 1 ]. According to the World Health Organization (WHO), more than 1.1 million adolescents died in 2016—mostly from preventable or treatable causes [ 4 ]. Therefore, the considerable gains from global investments in child and maternal health programmes would yield fewer long term benefits without simultaneous investments in adolescent health [ 5 , 6 ].
According to the life course approach, all stages of an individual’s life are intricately intertwined and interconnected with each other, and other people in society including past, present and future generations of their families [ 7 ]. In other words, evidence has shown that early life experiences, including events experienced in the pre-conception phase, play a role in determining the developmental origins and trajectories of health and wellness or disease across an individual’s life course [ 7 ]. From this perspective, it is understood that the health and wellness of individuals, as well as communities, depend on interactions oscillating between multiple risk and protective factors throughout one’s life. Based on this, early and appropriate interventions during child and adolescent years are shown to be the most effective prevention strategies to promote optimal public health and human development [ 5 , 6 , 8 ]. Additionally, following the life course approach, it is argued that these early investments in child and adolescent health will yield a triple dividend as they will grow into healthier adults who can contribute positively to society, as well as the health and development of the next generation [ 2 , 9 ].
Globally, mental health issues constitute one of the greatest burdens of disease for adolescents. According to the WHO, in 2016 mental health conditions accounted for 16% of the global burden of disease and injury for adolescents, with depression being identified as one of the leading causes of illness and disability, followed by suicide as the second leading cause of death in adolescents and self-harm the third [ 4 , 9 ]. UNICEF propagates that half of all lifetime mental disorders have onset during adolescence [ 10 ]. The recent inclusion of adolescents on the global health agenda as a target group for intervention represents a key step toward reducing the global burden of disease attributed to mental health disorders and reducing preventable deaths [ 2 , 10 , 11 , 12 , 13 ]. However, due to the previous neglect of mental health as a public health issue, efforts to address adolescent mental health are met with various challenges.
Currently, there is a lack of data concerning mental health conditions among adolescents, especially those living in low- and middle-income countries (LMICs) [ 11 ]. The lack of a body of quality evidence can affect the way adolescents are represented in national policies, as well as the ways in which government and healthcare officials respond to treatment and prevention [ 2 , 14 ]. According to WHO, a 2014 review of health policy documents from 109 countries showed that 84% have given some attention to adolescents, with three-quarters of them addressing sexual and reproductive health; one-third addressing tobacco and alcohol use, and one-quarter focusing on mental health [ 1 ]. In LMICs, efforts to improve child and adolescent mental health services (CAMHS) are hindered by a lack of specific CAMHS policies, resources and, fewer child and adolescent psychiatrists and other mental health professionals [ 12 , 13 ]. Furthermore, studies from developed countries have suggested that while CAMHS and policies are in place, there is a lack of mental health service uptake among children and adolescents due to various attitudinal, stigma-related, and structural barriers to accessing mental health services [ 14 ]. These challenges and barriers to CAMHS in both LMICs and higher-income countries are particularly apparent among adolescents living with a chronic disorder or disease [ 15 , 16 ]. Mental health conditions are increasingly recognised in children and adolescents with chronic disorders. Studies have shown that living with a chronic health condition is associated with increased risk of developing comorbid physical and mental health problems, which in turn influence treatment adherence and quality of life [ 16 , 17 , 18 ].
Another recurring obstacle for integrating mental health into global public health initiatives and frameworks is the lack of consensus of a definition of mental health [ 19 ]. Despite the growth of mental health and wellness research in recent decades, the question of how mental wellness should be defined remains largely unresolved [ 20 ]. This has given rise to broad and ambiguous definitions which, consequently, result in concepts such as mental health, mental wellness and mental wellbeing being used interchangeably. Currently, the term ‘mental health’ is often used as a euphemism to refer to mental illness, referring to conditions that adversely affect cognition, emotion and behaviour (i.e. depression and anxiety) [ 21 ]. This use reflects in the literature as the majority of adolescent mental health research adopts the dominant pathological view of health by focusing on mental health disorders such as psychiatric disorders, general mental health disorders, emotional and behavioural problems and psychological distress [ 22 , 23 ]. Similarly, global health initiatives such as AAH-HA! focus majorly on the burden of disease of mental disorders by reporting on self-harm, depressive disorders, childhood behavioural disorders and anxiety [ 3 ]. This dominant pathological view of mental health persists despite the contributions of positive health and wellbeing research which argues that wellness and illness are not two ends of the same continuum as previously thought, rather these constructs represent two independent continua [ 19 , 23 ]. In other words, the absence of mental illness does not necessarily indicate a state of mental health/wellness [ 1 , 23 , 24 ]. Therefore, it is imperative to consider both mental wellness and mental illness in research, and to move away from the previous ‘absence of disease’ model to one that emphasises positive psychological functioning for mental health [ 23 , 24 ]. In this model, wellness refers to the degree one feels positive about life, and one’s capacity to manage one’s feelings, behaviours, and limitations [ 23 ]. From this model, addressing adolescent mental wellness is seen as more than treating and mitigating the burden of disease of mental illness, rather it is also useful in maintaining lifelong mental and physical wellness and preventing the development of mental disorders [ 23 ]. Adolescents in particular experience multiple physical, social, and emotional changes, which can positively or negatively impact on their mental wellness. Therefore, interventions at this stage are crucial as research shows that providing psychosocial support and mental health promotion, such as psycho-education and community empowerment, facilitates the development of mental wellness (positive mental health) which is protective against psychopathology (mental illness) [ 9 , 24 ].
There is a need to develop accurate and culturally appropriate measures of mental wellness to support research endeavours that aim to improve adolescent mental health. Therefore, there is a greater necessity to clarify what is being measured, and how the resulting data from the measure should be interpreted to undertake fair and valid assessments. As such, developing a definition of mental wellness should encompass more than the description of wellness itself (as is the case with current definitions) to a clear and definite statement of the exact meaning of the construct.
To this end, this integrative review forms part of a larger study which aims to unpack the meaning of mental wellness among adolescents and its associated constructs by analysing and synthesising relevant literature and empirical and theoretical research on adolescent mental wellness. In doing this, we aim to use this information to develop and conceptualise adolescent mental wellness as a construct. Additionally, by focusing on conceptualising mental wellness, we hope to provide clarity regarding the way concepts such as mental wellness are used in the literature by clearly distinguishing between mental health (as a euphemism for mental illness) and mental wellness as a positive state of mental health. We aim to develop an instrument which can measure mental wellness as an indicator of general mental health and wellness among adolescents.
Methodology
The integrative review has been identified as a unique tool in healthcare for synthesising investigations available on a given topic or phenomena and for directing practise based on scientific knowledge [ 25 ]. The existing body of literature on mental health among adolescents is varied and complex as there are many concepts associated with mental health research ranging from positive aspects such as ‘resilience’ and ‘self-efficacy’ to negative aspects such as ‘depression’ and ‘anxiety’. As such, it is not possible for one study to capture all the dimensions associated with mental health. However, by adopting the integrative review method, we will be able to include the various sources and methodologies used in research to summarise existing empirical and theoretical literature associated with [positive] mental wellness concepts to better understand and conceptualise mental wellness among adolescents. The integrative review method proposed by Whittemore and Knafl [ 26 ] will be used: (1) problem identification, (2) literature search, (3) data evaluation, (4) data analysis, and (5) presentation of the integrative review.
Problem identification
The problem identification stage is a crucial first step in an integrative review. Therefore, we aim to approach this as a phase in itself. This means, going beyond the initial research questions to fully develop a framework of the problem and all its related variables. In this section, we describe some approaches we will use to identify the problem which the integrative review will address. As previously mentioned, our interest lies in understanding how mental wellness is conceptualised among adolescents, to aid in the conceptualisation and development of a mental wellness instrument for adolescent populations. Based on our initial reading of the literature, we have identified two recurring issues in this regard: firstly, there is a lack of validated mental wellness instruments for adolescents; and secondly, despite a growing body of research, the question of how mental wellness should be defined remains largely unresolved. Based on this, we have proposed to follow two research questions to aid us in identifying the problem.
How is the concept of mental wellness defined in research involving adolescents?
What indicators of mental wellness are being explored/investigated in research?
These two questions allow us to investigate how research has approached the study of mental wellness, what variables were of interest and how these were defined. To answer these questions, we will follow an iterative approach to gather and assess the available information to present a clear identification of the problem and all the variables of interest. To this end, we are currently conducting a systematic review of mental health instruments used in research with adolescent populations [ 21 ].
Understanding how mental wellness has been defined in research is an important part of our problem identification, as it will show us what theories and/or definitions of mental wellness are dominant, and which are missing. As Dodge et al. [ 20 ] argued, current definitions of wellness are more descriptive in the sense that they describe aspects of wellness rather than the construct itself. This lack of definition poses a problem in measurement development as the definition of a construct ultimately influences how it is being measured and how the resulting data should be interpreted. Therefore, to further aid our problem identification, we will compare the data from the systematic review with data from qualitative interviews exploring mental wellness among adolescents living with HIV (ALHIV). As previously mentioned, this review forms part of a larger study aimed at developing an instrument to measure mental wellness among adolescents. We have chosen to include the interviews with ALHIV for the problem identification stage as we want to develop an instrument that can measure mental wellness among healthy populations and those living with a chronic illness such as HIV. This is necessary as Manderscheid et al. [ 23 ] argue that a dual emphasis on mental and physical health is essential as studies have shown that positive health may influence biological functioning. This information will be used to identify the problem of the integrative review (Fig. 1 ). Using the information from the problem identification phase, we will move on to the second phase to conduct a literature search of mental health concepts used in research with adolescent populations.
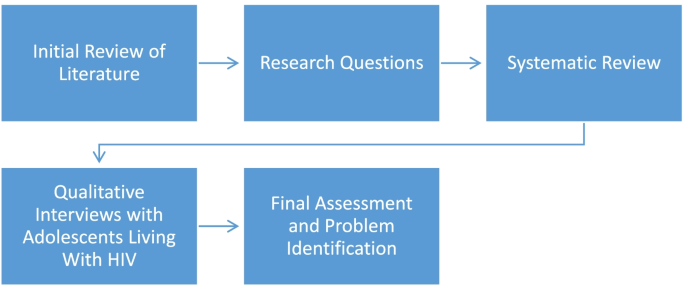
Steps followed to identify the problem for an integrative review
Literature search
A comprehensive search strategy which will include carefully selected terms that correspond to the domains of interest (mental health/mental wellness) will be used to search for relevant literature on electronic databases, grey literature and government or non-governmental organisations (NGO) websites. A systematic database search will be performed using Ebscohost (Psycharticles, Academic Search Premier, SocIndex), Educational Resource Information Center (ERIC), Medical Literature Analysis Retrieval System Online (MEDLINE) and Sabinet. A list of initial keywords has been identified for the search strategy: ((adolescen* OR teenage* OR young people OR youth) [AND] (“psychological wellbeing” OR “mental health wellbeing” OR “mental wellness” OR “mental health”). As the integrative review allows for a more iterative process, the list of keywords will be modified as the initial search reveals more relevant and refined search terms.
Inclusion and exclusion criteria
Studies will be included if they describe and/or define mental wellness in adolescent populations. As the interest lies in conceptualising mental wellness for adolescents, only studies dealing with general mental health, wellbeing and wellness will be included. In other words, studies focused on mental disorders or mental illnesses among adolescents will be excluded. For this review, studies will be included for all adolescents aged 10–19 who have not been diagnosed with a mental illness or disorder. Eligible studies will include qualitative, quantitative, and mixed-method studies published from 2000 to 2022. The time period of the search strategy was chosen due to the paucity of research in this area [ 3 , 22 , 27 ]. Furthermore, the prioritization of adolescent health and the focus on adolescent-friendly services occurred after 2000 [ 28 ].
Screening and selection process
Study selection.
The PICOT mnemonics (Table 1 ) for reviews will be used to guide study selection.
The above-mentioned criteria and search strategy will be used to search the databases. The screening and reporting of the review will be conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline and checklist [ 29 ]. The number of hits for each database will be recorded and the citations will be exported to Mendeley citation software. Following this, two reviewers will screen all the titles and abstracts to assess which articles are appropriate for inclusion. The full-text articles of the included abstracts will be downloaded and reviewed again to determine which articles should be included for the final assessment [ 30 ]. Any discrepancies between the two reviewers will be resolved by a third party. Additionally, based on the information retrieved from the screening, the researcher may modify the search to include other relevant sources.
Data evaluation
In this integrative review, the primary sources will include both empirical and theoretical literature - which increases the complexity of evaluating the quality of the included sources [ 26 ]. According to Whittmore and Knafl [ 26 ], integrative reviews using diverse sampling frames may adopt an approach to data evaluation that is similarly used in historical research. In this case, the authenticity, methodological quality, informational value, and representativeness of the available sources should be discussed in the final report. To minimise bias, the two reviewers will utilise two existing quality criteria instruments to evaluate the different types of data [ 26 ]. Firstly, the Mixed Methods Appraisal Tool (MMAT) (Additional file 1 : Appendix A) will be used to assess the methodological quality of the studies as it allows for summarising the overall quality across a range of study designs [ 31 ]. Secondly, the SFS scoring system version E (Additional file 1 : Appendix B) will be used to assess the quality of the methodologies of the included articles [ 32 ]. The SFS scoring system version E is appropriate as it allows for screening of both quantitative and qualitative research and allows for the appraisal of the definitions of constructs being investigated [ 32 ].
Data analysis
Once the selection of included articles has been finalised, we will extract the relevant data into a Microsoft Excel document to organise the information and prepare for the data synthesis. The Excel sheet will include information regarding the purpose of the study, study characteristics, results, and appraisal of the study as well as any other supporting information. All data will be cross-checked for quality purposes.
Data from the integrative review will be analysed using narrative framework synthesis for qualitative and quantitative studies. Framework synthesis begins with a tentative framework that can either be borrowed from previous studies or can be developed from key concepts [ 26 , 33 ]. With framework synthesis, the included studies are coded according to the developing framework in an iterative process until the body of evidence can be presented coherently.
In the final stage, the findings from the review will be discussed and presented in either tabular or diagrammatic form. Additionally, the limitations of the review will be discussed as well as recommendations for future research.
This integrative review aims to synthesise current literature on adolescent mental wellness to identify the ways in which this is being described and applied in research. The purpose of this is to identify gaps and to contribute to the conceptualisation of a more comprehensive definition of mental wellness which can aid in the development of an age- and culturally appropriate measure of adolescent mental wellness. Such measures are much needed in adolescent health research as it may be used to better understand the mental wellness needs of adolescents and contribute to the development of interventions and programmes aimed at improving psychological wellbeing and/or mental wellness of adolescents.
Strengths and limitations
According to our knowledge, this protocol describes the first integrative review to investigate and describe how mental wellness is defined in research among adolescents. Understanding how mental wellness among adolescents has been conceptualised is necessary to identify what are the strengths and limitations of such definitions. This will allow researchers to rethink what mental wellness means to adolescents and how this can and should be measured in research. A limitation of this study is related to the search strategy, notably around the time span (2000–2022) and the identification of grey literature, as not all possible sources of literature may be accessed.
Availability of data and materials
Not applicable.
Abbreviations
Adolescents living with HIV
Antiretroviral therapy
Child and Adolescent Mental Health
Low- and middle-income countries
Mixed Methods Appraisal Tool
SFS Scoring System
United Nations International Children’s Emergency Fund
World Health Organization
World Health Organization. Health for the world’s adolescents: a second chance in the second decade. 2014. Available from: https://www.who.int/maternal_child_adolescent/documents/second-decade/en/
Google Scholar
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387:2423–78. https://doi.org/10.1016/S0140-6736(16)00579-1 .
Article PubMed PubMed Central Google Scholar
World Health Organization. Global accelerated action for the health of adolescents (AA-HA!) guidance to support country implementation. 2017. Available from: http://www.who.int/maternal_child_adolescent/topics/adolescence/framework-accelerated-action/en/ .
World Health Organization. Adolescents: health risks and solutions. 2014. Available from: http://www.who.int/mediacentre/factsheets/fs345/en/ .
James S, Pisa PT, Imrie J, Beery MP, Martin C, Skosana C, et al. Assessment of adolescent and youth friendly services in primary healthcare facilities in two provinces in South Africa. BMC Health Serv Res. 2018;18:1–10. https://doi.org/10.1186/s12913-018-3623-7 .
Article CAS Google Scholar
Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet. 2012;379:1630–40. https://doi.org/10.1016/S0140-6736(12)60072-5 .
Article PubMed Google Scholar
World Health Organization. The life-course approach: from theory to practice. Case stories from two small countries in Europe. 2018. Available from: http://www.euro.who.int/__data/assets/pdf_file/0004/374359/life-course-iceland-malta-eng.pdf?ua=1 .
Armstrong A, Nagata JM, Vicari M, Irvine C, Cluver L, Sohn AH, et al. A global research agenda for adolescents living with HIV. J Acquir Immune Defic Syndr. 2018;78:S16–21. https://doi.org/10.1097/QAI.0000000000001744 .
World Health Organization. Adolescent mental health, 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health .
UNICEF. Measurement of mental health among adolescents at the population level (MMAP): conceptual framework and the roadmap to the measurement of mental health, 2018. Available from: https://data.unicef.org/wp-content/uploads/2018/11/Conceptual-framework-and-Roadmap-19-july.pdf .
Guthold R, Moller AB, Azzopardi P, Ba MG, Fagan L, Baltag V, et al. The Global Action for Measurement of Adolescent health (GAMA) initiative—rethinking adolescent metrics. J Adolesc Health. 2019;64:697–9. https://doi.org/10.1016/j.jadohealth.2019.03.008 .
Mokitimi S, Schneider M, de Vries PJ. Child and adolescent mental health policy in South Africa: history, current policy development and implementation, and policy analysis. Int J Ment Health Syst. 2008;12(36):1–15. https://doi.org/10.1186/s13033-018-0213-3 .
Article Google Scholar
Juengsiragulwit D. Opportunities and obstacles in child and adolescent mental health services in low- and middle-income countries: a review of the literature. WHO South-East Asia J Public Health. 2015;4:110. https://doi.org/10.4103/2224-3151.206680 .
Campo JV, Bridge JA, Fontanella CA. Access to mental health services implementing an integrated solution. JAMA Pediatr. 2015;169:299–300. https://doi.org/10.1001/jamapediatrics.2014.3558 .
Sawyer SM, Drew S, Yeo MS, Britto MT. Adolescents with a chronic condition: challenges living, challenges treating. Lancet. 2007;369:1481–9. https://doi.org/10.1016/S0140-6736(07)60370-5 .
Delamater AM, Guzman A, Aparicio K. Mental health issues in children and adolescents with chronic illness. Int J Hum Rights Healthc. 2017;10:163–73. https://doi.org/10.1108/IJHRH-05-2017-0020 .
Duffus SH, Cooper KL, Agans RP, Jain N. Mental health and behavioral screening in pediatric type 1 diabetes. Diabetes Spectr. 2019;32:171–5. https://doi.org/10.2337/ds18-0053.22 .
Lee S, Chung NG, Choi JY. Comparison of resilience and quality of life between adolescent blood cancer survivors and those with congenital heart disease: a cross sectional study. Health Qual Life Outcomes. 2020;18:1–7. https://doi.org/10.1186/s12955-020-01487-w .
Manwell LA, Barbic SP, Roberts K, Durisko Z, Lee C, Ware E, et al. What is mental health? Evidence towards a new definition from a mixed methods multidisciplinary international survey. BMJ Open. 2015;5:1–11. https://doi.org/10.1136/bmjopen-2014-007079 .
Dodge R, Daly AP, Huyton J, Sanders LD. The challenge of defining wellbeing. Int J Wellbeing. 2012;2:222–35. https://doi.org/10.5502/ijw.v2i3.4 .
Orth Z, Van Wyk B. Adolescent mental wellness: a systematic review protocol of instruments measuring general mental health and well-being. BMJ Open. 2020;10:37237. https://doi.org/10.1136/bmjopen-2020-037237 .
Vreeman RC, Mccoy BM, Lee S. Review article mental health challenges among adolescents living with HIV. J Int AIDS Soc. 2017;20:100–9. https://doi.org/10.7448/IAS.20.4.21497 .
Manderscheid RW, Ryff CD, Freeman EJ, Mcknight-eily LR, Dhingra S, Strine TW. Evolving definitions of mental illness and wellness. Prev Chronic Dis. 2010;7:5–10 http://www.cdc.gov/pcd/issues/2010/jan/09_0124.htm .
Keyes CLM. Promoting and protecting mental health as flourishing. Am Psychol. 2005:95–108. https://doi.org/10.1037/0003-066X.62.2.95 .
De Souza MT, De Carvalho R. Integrative review: what is it? How to do it? Einstein. 2010;8:102–7. https://doi.org/10.1590/S1679-45082010RW1134 .
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53. https://doi.org/10.1111/j.1365-2648.2005.03621 .
Sherr L, Cluver LD, Toska E, He E. Differing psychological vulnerabilities among behaviourally and perinatally HIV infected adolescents in South Africa–implications for targeted health service provision. AIDS Care. 2018;30:92–101. https://doi.org/10.1080/09540121.2018.1476664 .
Article CAS PubMed Google Scholar
World Health Organization. Promoting mental health: concepts, emerging evidence, practice (summary report). Geneva: World Health Organization; 2004.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
Eggar M, Smith GD, Altman DG. Systematic reviews in health care: meta analysis in context. 2nd ed. London: BMJ Publishing Group; 2001.
Book Google Scholar
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34:285–91. https://doi.org/10.3233/EFI-180221 .
Smith MR, Franciscus G, Swartbooi C, Munnik E, Jacobs W. The SFS scoring system. In: Smith MR (Ed., Chair). Symposium on methodological rigour and coherence: deconstructing the quality appraisal tool in systematic review methodology, conducted at the 21 st National Conference of the Psychological Association of South Africa. South Africa; 2015.
Snilstveit B, Oliver S, Vojtkova M. Narrative approaches to systematic review and synthesis of evidence for international development policy and practice. J Dev Eff. 2012;4:409–29. https://doi.org/10.1080/19439342.2012.710641 .
Download references
Acknowledgements
ZO is supported by the National Research Foundation, grant number (118160). Additionally, the authors would like to acknowledge funding form the Belgian Development Cooperation, through the Institute of Tropical Medicine Antwerp. Any opinion, finding and conclusion or recommendation expressed in this material is that of the authors and not the funders.
Author information
Authors and affiliations.
School of Public Health, University of the Western Cape, Bellville, 7535, South Africa
Zaida Orth & Brian van Wyk
You can also search for this author in PubMed Google Scholar
Contributions
ZO conceived the idea, developed the research question and study methods, and contributed meaningfully to the drafting and editing; she also approved the final manuscript. BvW aided in developing the research question and study methods, contributed meaningfully to the drafting and editing, and approved the final manuscript.
Corresponding author
Correspondence to Zaida Orth .
Ethics declarations
Ethics approval and consent to participate.
This integrative review forms part of the corresponding author’s PhD work and has been approved by the University of the Western Capes’ Biomedical Science Research Ethics Committee.
Ethics Reference Number: BM19/9/18
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix a..
Mixed Methods Appraisal Tool (MMAT). Appendix B. SFS Scoring System (Version E). Appendix C. PRISMA-P Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Orth, Z., van Wyk, B. Rethinking mental wellness among adolescents: an integrative review protocol of mental health components. Syst Rev 11 , 83 (2022). https://doi.org/10.1186/s13643-022-01961-0
Download citation
Received : 05 October 2020
Accepted : 15 April 2022
Published : 02 May 2022
DOI : https://doi.org/10.1186/s13643-022-01961-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescent mental health
- Mental wellness
- Integrative review
- Positive psychology
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Advertisement
Social and environmental variables as predictors of mania: a review of longitudinal research findings
- Open access
- Published: 14 March 2022
- Volume 2 , article number 7 , ( 2022 )
Cite this article
You have full access to this open access article
- Sheri L. Johnson ORCID: orcid.org/0000-0002-9945-4816 1 &
- Benjamin Z. S. Weinberg ORCID: orcid.org/0000-0002-9761-541X 1
4672 Accesses
2 Citations
Explore all metrics
Considerable evidence suggests that psychosocial variables can shape the course of bipolar disorder. Here, though, we focus on the more specific idea that the social environment can predict the course of mania. We systematically review evidence from longitudinal studies concerning how social support, family interactions, traumatic life events, and recent life events relate to the age of onset, the frequency of episode recurrence, and the severity of manic symptoms. Although we find some evidence that the course of mania can be worsened by social environmental factors, the links are specific. Among social variables, some studies indicate that conflict and hostility are predictive, but more general social relationship qualities have not been found to predict mania. Some research indicates that childhood trauma, and recent life events involving goal attainment or sleep disruption can predict mania. Taken together, the profile of variables involving recent exposure that are most predictive include those that are activating, reward-related, or sleep-disrupting, which fits with general psychological hypotheses of behavioral activation and sleep disruption as important for mania. We discuss gaps in the literature, and we note future directions for research, including the need for more integrative, longitudinal research on a fuller range of social and biological risk variables.
Similar content being viewed by others

Dynamic contextual influences on social motivation and behavior in schizophrenia: a case-control network analysis
Varsha D. Badal, Emma M. Parrish, … Eric Granholm

Contributions of the social environment to first-onset and recurrent mania
S E Gilman, M Y Ni, … R H Perlis
Longitudinal Study of Life Events, Well-Being, Emotional Regulation and Depressive Symptomatology
Eiríkur Örn Arnarson, Ana Paula Matos, … W. Edward Craighead
Avoid common mistakes on your manuscript.
1 Introduction
Bipolar spectrum disorders are defined by manic symptoms of varying duration and intensity. The DSM differentiates three major types of bipolar disorders. Bipolar I disorder is defined by at least one lifetime episode of mania. Bipolar II disorder is defined by milder hypomanic episodes as well as episodes of major depression. Cyclothymia is defined by chronic fluctuations between depressive and manic symptoms that do not meet the criteria for hypomanic or manic episodes [ 1 ].
Bipolar disorder is well-established as a genetically driven illness. Nonetheless, social and environmental factors can influence the onset, course, and outcomes of this disorder. Here, we focus on how such variables may inform the course of manic symptoms, including onset, severity, and recurrence of manic or hypomanic episodes. Notwithstanding that depression is common among those with bipolar disorder [ 2 ] and is important for quality of life and functional outcomes within bipolar disorder [ 3 , 4 ], we focus here on mania for a few reasons. First, manic symptoms are the defining feature of bipolar spectrum disorders. Second, many individuals with bipolar disorder never experience depression [ 2 ]. Third, given the evidence that depression and mania within bipolar disorder have separable genetic contributions [ 5 ], and fluctuate independently in an uncorrelated manner [ 6 ], there have been calls to consider whether mania and depression can be considered to be separable syndromes within bipolar disorder [ 7 ]. Taken together, it seems important to consider whether the social environment has direct contributions to the course of mania, and to examine which facets of the social environment are relevant.
We focus specifically on longitudinal studies that test whether socioenvironmental factors can predict change in mania parameters over time. This is not to minimize the bidirectionality of these effects—substantial evidence indicates that manic episodes exert profound influence on employment, finances, and relationships [ 3 ]. For example, bipolar spectrum disorders are related to high levels of functional impairment, unemployment, homelessness, and legal difficulties and to lower likelihood of becoming and staying married [ 8 , 9 , 10 , 11 ], and high rates of relationship dissatisfaction [ 12 , 13 ]. Deficits in social support appear to worsen with manic episodes [ 14 ], with longer illness duration [ 15 ], with inter-episode subsyndromal symptoms [ 16 , 17 ], and when individuals experience more internalized stigma concerning their bipolar disorder [ 18 ]. Given the evidence that difficult contexts can emerge consequent to symptoms, estimating the causal influence of social environmental factors on the course of disorder requires prospective research that controls for symptom levels at baseline.
In addition to the direction of effects, mania may shape how one interprets social circumstances, in that when manic, people may be less sensitive to negative information [ 19 ]. Where possible, we will highlight objective ratings of the social environment that have been used to supplement subjective ratings.
We consider several facets of mania here: age of onset, recurrence, and increases in the severity of manic symptoms. Where available, we consider evidence concerning the age of onset—a variable of particular merit in considering whether the social environmental features were present before manic episodes began. After onset, that the median time between manic episodes for those with bipolar I disorder is about one year [ 20 ]. Given the low frequency of mania recurrence, statistical power is often greater in analyses of symptom severity than for recurrence. Not surprisingly, then, many of the studies in the field focus on changes in symptom severity.
2 Methodological approach
PRISMA guidelines for systematic review were followed to conduct this review [ 21 ]. The PRISMA checklist is attached as Appendix A , and the PRISMA flowchart is included as Fig. 1 . To consider the links of social environmental variables with the course of mania, we conducted a PsycINFO search for the terms (“Life events OR social support OR trauma OR violence OR family OR interpersonal OR environmental OR stress OR victimization OR expressed emotion OR marital satisfaction OR adversity OR life stress OR perceived criticism OR family interaction”) and (“mania OR manic”). In a second search, we sought articles that included the social terms, the words “hypomania OR hypomanic”, and were not covered in the first search. Both searches were restricted to longitudinal and prospective human studies. Because the first author had conducted a comprehensive review in 2016 [ 22 ], we first limited our searches to articles published since 2014. Upon editorial suggestion, we conducted a third search for articles published before 2014. The PsycINFO searches identified 573 articles (440 for mania, 37 additional articles for hypomania, and 96 for articles preceding 2014). B. W., S. J., and an assistant reviewed the articles to assess inclusion criteria, including whether it included (a) information specific to mania, including timing or presence of manic/hypomanic onset, presence or timing of manic/hypomanic relapse, and severity of manic/hypomanic symptoms over time; (b) social environmental variables (e.g., social, family, marital, trauma, adversity, or life events), and (c) analyses of how social environmental variables prospectively predicted mania-related variables. Environmental variables that were less clearly tied to the social domain, such as religiosity or exposure to in utero nicotine, were excluded from review, as were composite measures of functioning without specific indices such as family function or social support. S. J. and B. W. jointly reviewed articles where there were questions about inclusion. After review of these criteria, 53 articles were selected for systematic review. Most articles were excluded because they provided no longitudinal analyses of social variables. We also reviewed the references discussed in these articles, and we looked for relevant articles in previous reviews of life events [ 23 , 24 ], expressed emotion [ 25 ] and broad predictors of mania [ 26 ]. We emailed authors who previously published regarding social factors in bipolar disorder to request articles, which yielded eight articles for potential inclusion. After more careful review, 30 articles (several of which contributed information about more than one social or mania parameter) were identified as assessing how social variables longitudinally predicted mania parameters; we describe findings from each of these below. Table 1 shows summary information for each of these studies.
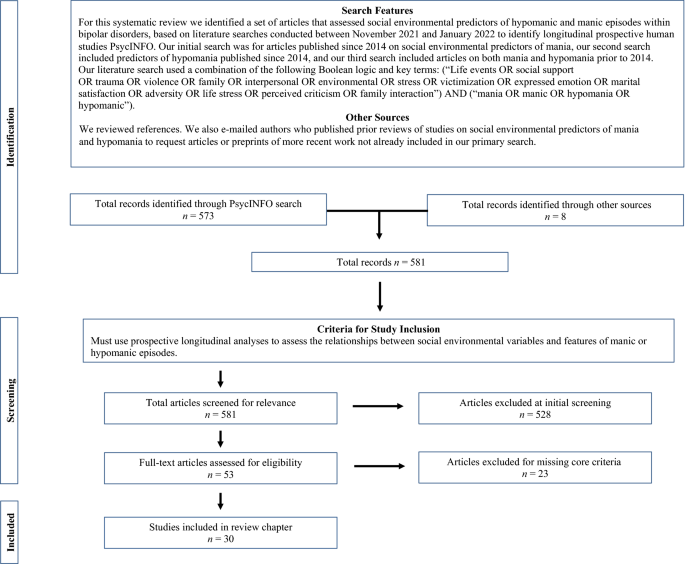
PRISMA-style flow diagram showing the search criteria, selection of studies, inclusion criteria, and exclusion rationale of studies for systematic review
3 Evidence concerning the social environment as a predictor of the course of mania
We begin by discussing the influence of social support, then discuss the more specific domain of family functioning. After discussing this literature on relationships, we consider the effects of traumatic events and life events.
3.1 Social support
The term “social support” has been used to refer to emotional and material resources provided by a person’s social network. In general, social support has been found to be more predictive than social network size for mental health outcomes [ 27 ].
Relative to controls, people with bipolar disorder report low availability and adequacy of social support, even between episodes of illness [ 28 ]. In prospective studies, social support has been found to predict increases in depression over time [ 29 , 30 , 31 ]. In contrast, multiple indices of social support—including indices of social strain, satisfaction with social support or the degree of behavioral support received –have been shown to be unrelated to manic symptom severity, to manic relapse, or to hospitalization for mania [ 16 , 29 , 31 , 32 , 33 ]. In contrast, in the Zurich study, among 38 participants who developed hypomanic episodes by age 30, endorsement of conflict with friends at age 22, preceding onset, was significantly higher than among the 377 individuals without hypomanic episodes [ 34 ]. Thus, based on a single study, conflict within relationships appears to be predictive of hypomanic episodes, but findings of multiple studies indicate that general social support variables are not predictive of the course of manic symptoms.
3.2 Family factors
Multiple facets of family relationships have been considered in relation to bipolar disorder. These include questionnaires and observer ratings to assess family function or specific facets of family function. One domain that has received particular attention is expressed emotion (EE), which is defined by observer ratings of criticism, hostility or emotional over-involvement from family members towards the person with bipolar disorder during a standardized interview in which the patient is not present [ 35 ].
Multiple facets of family function have not been found to predict the course of mania, despite significant effects on depression course observed in most of these studies. More specifically, observer ratings of family functioning were not found to predict changes in mania over a 1-year period among persons with bipolar I disorder [ 31 ]. Similarly, parent and child ratings of family cohesion and family adaptability were not found to predict significant change in manic symptoms among adolescents with bipolar disorder followed for 2 years [ 36 ]. Among youths ages 5 to 17 diagnosed with bipolar spectrum disorder, self-ratings of family function, communication, and problem-solving on the Family Assessment Device [ 37 ] did not predict change in interview-based mania ratings [ 38 ]. EE has also been found not to significantly predict manic symptoms over time [ 39 , 40 ].
A different pattern emerges when researchers have examined more specific aspects of family function, in that mirroring the social support literature, family conflict and parental criticism do appear to be predictive of mania in several studies. In a study of adolescents diagnosed with bipolar disorder enrolled in a treatment trial and followed for two years, parent and adolescent reports of family conflict both predicted more prolonged manic symptoms, and improvement in family conflict was associated with greater decline in manic symptoms [ 36 ]. Similarly, parental criticism, as rated by observers watching a standardized family interview, was the only facet of EE found to predict greater manic symptoms among children diagnosed with bipolar disorder [ 41 ]. In one study, self-ratings of severity of distress over, but not severity of, parental criticism predicted change in manic symptoms [ 42 ].
Effects of family conflict were not consistent when considered in one younger sample of preadolescent and early adolescent youth who had experienced manic episodes. In that sample, when either mothers or children reported a low degree of maternal warmth toward the child, this predicted greater risk of relapse of manic/hypomanic symptoms within a 2-year [ 43 ], 4-year [ 44 ], and 8-year follow-up [ 45 ]; in the same study, neither paternal warmth nor maternal criticism predicted relapse. As noted above, statistical power to examine relapse timing may be lower than the power to examine severity of manic symptoms, which could help explain the null findings for maternal criticism. Alternatively, the studies above, which focused on adolescents, might have captured a more ideal developmental period for studying family conflict, given the naturalistic increases in parent–child conflict during that time period. Given positive effects for warmth in this study but not in other research, though, further research is warranted.
Taken together, findings of several studies indicate that parent–child conflict, parental criticism, and distress over parental criticism may contribute to more severe (hypo)manic symptoms among adolescents with bipolar spectrum disorders. The findings regarding conflict and criticism are distinct from a set of null findings regarding more general facets of relationships (with the exception of one study identifying maternal, but not paternal warmth as a predictor). One intriguing possible explanation for this specific profile of effects is that conflict and criticism are agitating, which could relate more directly to triggering high activation symptoms of mania.
3.3 Childhood Traumatic events
About half of people diagnosed with bipolar disorder report a history of severe childhood abuse [ 46 ], and childhood trauma exposure is correlated with many different indicators of severity of bipolar disorder [ 47 ]. More specific to mania, large-scale studies indicate that among those diagnosed with bipolar spectrum disorder, early abuse and trauma are correlated with an earlier age of onset [ 46 , 48 ], and more severe manic symptoms during adolescence [ 49 ].
Trauma has been suggested to influence inflammatory responses, which in turn, are implicated in symptom levels. Consistent with this idea, in one study, a genetic polymorphism tied to innate immune response, the TT genotype of the toll-like receptor 2 (TLR2) rs3804099, implicated in innate immune response to pathogens, was related to a stronger effect of self-rated sexual abuse on age of onset in bipolar disorder [ 50 ].
Some prospective research on trauma in bipolar disorder is available. In the general population, trauma did not significantly predict manic symptoms over time, highlighting the import of studying samples that are vulnerable to mania [ 51 ]. When researchers have focused on those who have already experienced manic episodes, trauma was found to predict more rapid mania recurrence among those with first episode psychotic mania [ 52 ] and greater likelihood of hypomanic symptoms among adolescents diagnosed with bipolar spectrum disorder [ 53 ]. Findings from the Course and Outcome of Bipolar Youth (COBY) study are particularly notable, as researchers completed interviews to assess symptoms and trauma within a large sample of 375 youths and young adults diagnosed with bipolar spectrum disorder, and they assessed trauma with parent and self-report measures [ 54 ]. Controlling for covariates, lifetime history of abuse per parent and child report was related to 1. 4 times the risk of hypomanic episodes over time but was not related significantly to full-blown manic episodes.
The effects of trauma may be particularly pernicious when exposure occurs during childhood as compared to adulthood. When researchers coded trauma exposure across the lifetime including recent trauma, trauma exposure did not predict significant changes in manic symptoms [ 55 ]. In a second study, lifetime trauma exposure also did not predict manic episodes, although did predict the likelihood of depressive symptoms during manic episodes (mixed episodes) [ 56 ]. In one study which directly compared childhood vs. adult abuse, childhood, but not adulthood, physical abuse prospectively predicted severity of mania across a one-year follow-up [ 57 ]. Taken together, three studies indicate that early trauma exposure appears meaningful for the prediction of hypomanic or manic episodes among those with bipolar spectrum disorder, in samples defined by bipolar spectrum disorders and by psychotic mania, with findings of one study suggesting effects specific to hypomania (as compared to mania).
3.4 Recent life events
Although many studies have focused on life events in bipolar disorder, most rely on self-report scales, which have lower validity and reliability than interview measures do [ 58 ]. It also is difficult to rule out the possibility that prodromal symptoms contributed to stressors when using self-report measures. For example, a person who develops heightened confidence and impulsivity during a manic episode may spend large sums of money, creating significant financial stress. Thus, the causality of findings that stress levels and relationship problems are correlated with manic severity [ 59 ] can be difficult to interpret. Here, then, we focus on studies that use the Bedford College Life Event and Difficulty Schedule [ 60 ] or other interview measures to differentiate life events triggered by illness characteristics from those that appear to be independent of illness.
Prospective studies using life event interviews indicate that independent, negative life events, and chronic recent stressors predict increases in bipolar depression and delayed recovery from episodes of depression, but not mania [ 28 , 55 , 61 ]. Within negative life events, loss and danger events both related to depressive, but not manic symptoms, across an 8-month follow-up period [ 62 ].
Although negative life stressors do not appear related to mania, other facets of life events do appear related. For example, findings of several studies indicate that life events which involve goal attainment, such as getting married, having a child, or completing a degree, precede increases in manic symptoms [ 63 ]. In an initial study, goal-attainment life events predicted increases in manic but not depressive symptoms after controlling for baseline symptoms among persons with bipolar I disorder. This effect is observed despite removing events that are potentially caused by symptoms. These findings have been replicated in bipolar I disorder [ 61 ] and bipolar spectrum disorder [ 64 ]. Goal attainment events, which involve motivated pursuit of a desired goal, appear more powerful than more general positive events [ 63 ]. Among those with bipolar spectrum disorder who experienced life events related to goal pursuit, those with more perfectionistic, goal-striving cognitive styles showed more increase in hypomanic symptoms and more frequent hypomanic episodes during a three-year follow-up period [ 65 , 66 ]. In each of these studies, the effects of goal attainment events appeared to be specific, in that such events were not significantly related to change in depressive symptoms.
Some research has examined mechanisms through which life events involving goal attainment become translated into symptoms. Unlike negative life events, goal attainment life events do not appear related to hair cortisol levels [ 67 ]. In a daily monitoring study, people with bipolar disorder were found to become more active and energized, relative to controls, after initial progress toward a goal [ 68 ]. Increases in goal engagement (setting new goals and spending time pursuing goals) have been found to predict increases in manic symptoms over several months among those diagnosed with bipolar I disorder [ 69 ]. Hence, increases in activity and goal pursuit may at least partially mediate the effects of goal attainment on mania. Some work has shown that national profiles of cultural values related to goal striving and individualism correlate with the prevalence levels of bipolar diagnoses [ 70 ]. This work fits with a broader set of findings on increased activity of the behavioral activation system as implicated in the onset of manic episodes [ 71 ].
Mania also has been found to relate to life events that involve schedule disruption. The influential social zeitgeber theory proposes that people with mood disorders may be particularly vulnerable to events that disrupt social rhythms, as these have the potential to trigger disturbances in sleep [ 72 ]. This builds from the extensive evidence that those with bipolar disorder show dysregulation in their sleep and circadian rhythm profiles [ 73 ]. Social rhythms are defined as daily routines that involve consistent timing (e. g., routines in timing of sleeping, eating, exercise, and social interactions) and thus help entrain natural circadian rhythms. Those with bipolar disorder have been found to have diminished social rhythms in their daily routine, and lower levels of social rhythm have been shown to predict the onset of bipolar spectrum disorder [ 74 ]. According to social zeitgeber theory, events that disrupt social rhythms—such as travel across time zones, loss of a spouse, or unemployment—can trigger disturbances in sleep and the sleep–wake cycle, which in turn, precipitate relapse among people with bipolar disorder [ 72 ]. Consistent with theory, social rhythm disrupting events have been shown to be more common before manic than depressive episodes within bipolar disorder [ 75 , 76 ]. In one prospective study, events that specifically disrupted sleep predicted increases in hypomanic symptoms, whereas more general schedule disruptions due to life events were not predictive of change in hypomanic symptoms [ 77 ].
4 Conclusions
A growing number of studies have examined the effects of the social environment on the course of mania within bipolar disorder. Findings indicate that more general facets of relationship quality, such as measures of social support, family function, or expressed emotion, do not appear to predict change in manic symptom severity over time in most studies, and yet findings of several studies indicate that conflicts with friends and family and parental criticism predict change in (hypo)manic symptoms. Measures of recent negative life events do not predict increases in mania over time, and yet findings of several studies indicate that early trauma exposure predicts increases in manic symptoms and greater risk of hypomanic recurrence over time. Goal attainment life events have been found to predict increases in manic symptoms in several studies, and cultures with higher rates of goal striving and individualism show higher prevalence of bipolar disorder. Consistent with the large literature linking sleep and circadian disruption to mania, sleep-disrupting life events have been found to predict change in manic symptoms within one study. Overall, then, findings of this small literature indicate that specific aspects of the social environment appear to be important for predicting the course of mania, including family conflict and criticism, early trauma, and recent life events involving goal attainment or sleep disruption.
The profile of variables that appear predictive, as compared to those with null effects, suggests some intriguing future directions. The relatively larger effects for early trauma may reflect the import of events occurring during critical periods for brain development [ 78 ]. In considering the influence of more recent social experiences, specificity appears to matter. Speculatively, social relationship variables that could trigger agitation may be important to consider. Within the domain of life events, mania effects appear specific to life events related to activation and sleep disruption. Taken together, the profile of these effects suggests the potential importance of early exposure and of recent risk variables that are that are activating, reward-related, or sleep-disrupting. This is intriguing, given that two major hypotheses of psychological contributors to mania involve dysregulation in the behavioral activation system involved in reward pursuit—believed to involve hyperactivation as a consequence of excessive goal pursuit [ 71 ] and dysregulation in sleep and circadian rhythms [ 73 ]. Nonetheless, it is important to note that some of the social variables predictive of mania, such as trauma and sleep disruption, also appear transdiagnostically important; without further research, it is difficult to know whether any mania-specific mechanisms are involved.
5 Limitations and future directions
Despite evidence for the import of the social environment for mania onset, recurrence, and severity, only a small number of studies are available to consider each social domain covered here, and we were unable to identify any data on some key facets of the social environment. For example, although cross-sectional evidence suggests that being married is correlated with diminished symptoms, including fewer manic episodes among men [ 79 ] , we were unable to identify longitudinal studies of marital status or marital relationship quality in relation to mania. Major national differences in prevalence also suggest the likelihood of strong cultural influences on the course of bipolar disorder [ 80 ]. More work is warranted to understand the mechanisms driving these cultural effects.
More work is also needed to consider whether findings generalize across forms of disorder, and the range of mania-related symptom outcomes that can be predicted. Many of the samples studied include individuals with a broad range of bipolar spectrum disorders, and analyses did not differentiate those with bipolar I from those with bipolar II or cyclothymic disorders. Given increasing evidence for genetic differentiation in the forms of disorder [ 81 ], examining effects within subtypes will be an important goal for future research. It is also the case that most studies were only statistically powered to examine change in the level of manic symptoms, and not the onset or recurrence of disorder. Hence it will be important for future studies to consider more specific analyses of the types of disorder and the types of manic outcome variables that are tied to these social variables.
We also express caution, in that interpersonal domains are intricately inter-related, and most studies reviewed here examine only a small slice of the interpersonal world. As one example, within couples where one partner was diagnosed with bipolar spectrum disorder, higher relationship satisfaction predicted higher perceived social support, and vice versa [ 82 ]. Parental criticism of adolescents with bipolar disorder was also tied to greater family conflict [ 41 ]. Broader batteries encompassing multiple facets of the social environment will be important for disentangling these effects.
Beyond the need to disentangle social variables, there is a profound need to integrate social and biological risk factors in studies of bipolar disorder, given the estimates of 80% or higher heritability for bipolar disorder [ 5 ], and the evidence that exposure to early trauma can trigger long-lasting neural changes [ 78 ]. Findings of one study show that trauma effects on mania may be heightened among those with genetic polymorphisms related to inflammation [ 50 ]; these integrative studies are particularly important.
We are optimistic that currently underway studies will fill many of the gaps in current knowledge of social variables. That is, promising work has begun with large samples of those at risk for bipolar disorder, to gather self-rated measures of trauma, life stress, social support and marital satisfaction along with other key biological and personality risk variables to prospectively track conversion into the disorder [ 83 , 84 ]. We urge careful attention to specific dimensions in analyses of those datasets.
6 Implications
The early evidence described here that the social environment can shape the severity of mania fits with the evidence that psychological interventions, when added as adjuncts to medication, can help reduce symptoms of bipolar disorder. Large-scale research indicates that cognitive behavioral, psychoeducation, and family interventions can improve outcomes in bipolar disorder, including mania [ 85 ]. In keeping with the treatment outcome findings, several national standards for the treatment of bipolar disorder suggest providing psychotherapy as standard adjunctive care for bipolar disorder [ 86 , 87 ].
With greater attention to the nature of diagnoses and manic outcomes, current findings could also inform treatment development. Given that mania severity is tied to more specific facets of the social environment, such as conflict or criticism rather than global relationship quality, or sleep disruption rather than general life events, one goal might be to examine how well psychosocial interventions can address these narrower facets of the social environment. To date, some work suggests that family interventions may be particularly helpful in reducing the duration of depressive and manic episodes among those with more serious family impairment [ 88 ] and those experiencing higher EE [ 89 ]. Research, though, suggests that family-focused therapies more readily enhance positive communications than reduce EE among families of those with bipolar disorder [ 90 , 91 ]. Might a treatment focused specifically on family criticism provide more robust mania effects? Given that distress in response to family criticism can predict change in manic symptoms, work showing that psychological intervention can reduce amygdala reactivity to emotion stimuli provides one promising approach to this issue [ 92 ]. We also reported findings from a single study showing a role of events disrupting sleep. Although in need of replication, this finding has intriguing parallels with research documenting that intervention targeting insomnia can reduce manic symptoms [ 93 ]. Targeted intervention work provides the unique opportunity to examine experimentally how change in these key risk factors can promote better outcomes.
In sum, the small research base on social environmental predictors of mania suggests a profile of findings with intriguing clinical implications. Despite the need for more replication, for more careful examination of generalizability across bipolar diagnoses, and for integrative, prospective research, there is evidence that the social environment has an influence on the onset, severity, and recurrence of mania. That is, multiple studies indicate that early adversity and recent social challenges of patients could help shape the severity of mania. Several interventions are available to address social risk factors, including interpersonal/social rhythm psychotherapy and family-focused therapy. By considering social risk variables, clinicians can consider how to tailor treatment to address these key issues.
Data availability (data transparency)
Not applicable.
Code availability (software application or custom code)
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. American Psychiatric Association; 2013. https://doi.org/10.1176/appi.books.9780890425596 .
Angst J, Rössler W, Ajdacic-Gross V, Angst F, Wittchen HU, Lieb R, et al. Differences between unipolar mania and bipolar-I disorder: Evidence from nine epidemiological studies. Bipolar Disord. 2019;21:437–48. https://doi.org/10.1111/bdi.12732 .
Article PubMed Google Scholar
Gitlin MJ, Miklowitz DJ. The difficult lives of individuals with bipolar disorder: a review of functional outcomes and their implications for treatment. J Affect Disord. 2017;209:147–54. https://doi.org/10.1016/j.jad.2016.11.021 .
Khafif TC, Belizario GO, Silva M, Gomes BC, Lafer B. Quality of life and clinical outcomes in bipolar disorder: an 8-year longitudinal study. J Affect Disord. 2021;278:239–43. https://doi.org/10.1016/j.jad.2020.09.061 .
McGuffin P, Rijsdijk F, Andrew M, Sham P, Katz R, Cardno A. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch Gen Psychiatry. 2003;60:497–502. https://doi.org/10.1001/ARCHPSYC.60.5.497 .
Johnson SL, Morriss R, Scott J, Paykel E, Kinderman P, Kolamunnage-Dona R, et al. Depressive and manic symptoms are not opposite poles in bipolar disorder. Acta Psychiatr Scand. 2011;123:206–10. https://doi.org/10.1111/j.1600-0447.2010.01602.x .
Article CAS PubMed Google Scholar
Joffe RT, Young LT, MacQueen GM. A two-illness model of bipolar disorder 1. Bipolar Disord. 1999;1:25–30. https://doi.org/10.1034/J.1399-5618.1999.10107.X .
Suppes T, Leverich GS, Keck PE, Nolen WA, Denicoff KD, Altshuler LL, et al. The Stanley Foundation Bipolar Treatment Outcome Network. II. Demographics and illness characteristics of the first 261 patients. J Affect Disord. 2001;67:45–59. https://doi.org/10.1016/S0165-0327(01)00432-3 .
Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RMA, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch Gen Psychiatry. 2007;64:543–52. https://doi.org/10.1001/archpsyc.64.5.543 .
Article PubMed PubMed Central Google Scholar
Folsom DP, Hawthorne W, Lindamer L, Gilmer T, Bailey A, Golshan S, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162:370–6. https://doi.org/10.1176/APPI.AJP.162.2.370 .
Quanbeck CD, Stone DC, Scott CL, McDermott BE, Altshuler LL, Frye MA. Clinical and legal correlates of inmates with bipolar disorder at time of criminal arrest. J Clin Psychiatry. 2004;65:198–203. https://doi.org/10.4088/JCP.V65N0209 .
Whisman MA. Marital distress and DSM-IV psychiatric disorders in a population-based national survey. J Abnorm Psychol. 2007;116:638–43. https://doi.org/10.1037/0021-843X.116.3.638 .
Sheets ES, Miller IW. Predictors of relationship functioning for patients with bipolar disorder and their partners. J Fam Psychol. 2010;24:371–9. https://doi.org/10.1037/a0020352 .
Koenders MA, Giltay EJ, Spijker AT, Hoencamp E, Spinhoven P, Elzinga BM. Stressful life events in bipolar I and II disorder: Cause or consequence of mood symptoms? J Affect Disord. 2014;161:55–64. https://doi.org/10.1016/j.jad.2014.02.036 .
Romans SE, McPherson HM. The social networks of bipolar affective disorder patients. J Affect Disord. 1992;25:221–8. https://doi.org/10.1016/0165-0327(92)90079-L .
Eidelman P, Gershon A, Kaplan K, McGlinchey E, Harvey AG. Social support and social strain in inter-episode bipolar disorder: Social support, strain, bipolar disorder. Bipolar Disord. 2012;14:628–40. https://doi.org/10.1111/j.1399-5618.2012.01049.x .
Morriss R, Lobban F, Riste L, Davies L, Holland F, Long R, et al. Clinical effectiveness and acceptability of structured group psychoeducation versus optimised unstructured peer support for patients with remitted bipolar disorder (PARADES): a pragmatic, multicentre, observer-blind, randomised controlled superiority trial. Lancet Psychiatry. 2016;3:1029–38. https://doi.org/10.1016/S2215-0366(16)30302-9 .
Cerit C, Filizer A, Tural Ü, Tufan AE. Stigma: a core factor on predicting functionality in bipolar disorder. Compr Psychiatry. 2012;53:484–9. https://doi.org/10.1016/j.comppsych.2011.08.010 .
Lembke A, Ketter TA. Impaired recognition of facial emotion in mania. Am J Psychiatry. 2002;159:302–4. https://doi.org/10.1176/appi.ajp.159.2.302 .
Coryell W, Endicott J, Maser JD, Mueller T, Lavori P, Keller M. The likelihood of recurrence in bipolar affective disorder: the importance of episode recency. J Affect Disord. 1995;33:201–6. https://doi.org/10.1016/0165-0327(94)00091-M .
PRISMA-S Group, Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, et al. PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev 2021;10:39. https://doi.org/10.1186/s13643-020-01542-z .
Johnson SL, Gershon A, McMaster KJ. Environmental Risk and Protective Factors in Bipolar Disorder. In: DeRubeis RJ, Strunk DR, editors. The Oxford Handbook of Mood Disorders. Oxford: Oxford University Press; 2017. p. 131–41.
Google Scholar
Alloy LB, Abramson LY, Urosevic S, Nusslock R, Jager-Hyman S. Course of early-onset bipolar spectrum disorders during the college years: a behavioral approach system dysregulation perspective. In: Miklowitz DJ, Cicchetti D, editors. Understanding Bipolar Disorders & Developing Psychopathology Perspective. The Guilford Press: New York; 2010. p. 166–91.
Alloy LB, Titone MK, Ng TH, Bart CP. Stress in Bipolar Disorder. In: Harkness KL, Hayden EP, editors. The Oxford Handbook of Stress and Mental Health. Oxford: Oxford University Press; 2020. p. 126–54.
Hooley JM, Rosen LR, Richters JE. Expressed Emotion: Toward Clarification of a Critical Construct. In: Miller GA, editor. The Behavioral High-Risk Paradigm in Psychopathology. New York: Springer; 1995. p. 88–120.
Chapter Google Scholar
Johnson SL, Cuellar AK, Peckham AD. Risk factors for bipolar disorder. In: Handook of Depression. 3rd Ed, New York: The Guilford Press; 2014, p. 315–33.
Sarason IG, Sarason BR, Pierce GR. Social support: the search for theory. J Soc Clin Psychol. 1990;9:133–47. https://doi.org/10.1521/jscp.1990.9.1.133 .
Article Google Scholar
Cohen AN, Hammen C, Henry RM, Daley SE. Effects of stress and social support on recurrence in bipolar disorder. J Affect Disord. 2004;82:143–7. https://doi.org/10.1016/J.JAD.2003.10.008 .
Johnson SL, Meyer B, Winett C, Small J. Social support and self-esteem predict changes in bipolar depression but not mania. J Affect Disord. 2000;58:79–86. https://doi.org/10.1016/S0165-0327(99)00133-0 .
Johnson SL, Winett CA, Meyer B, Greenhouse WJ, Miller I. Social support and the course of bipolar disorder. J Abnorm Psychol. 1999;108:558–66. https://doi.org/10.1037/0021-843X.108.4.558 .
Weinstock LM, Miller IW. Psychosocial predictors of mood symptoms one year following acute phase treatment of bipolar i disorder. Compr Psychiatry. 2010;51:497–503. https://doi.org/10.1016/j.comppsych.2010.02.001 .
Johnson L, Lundström O, Åberg-Wistedt A, Mathé AA. Social support in bipolar disorder: Its revelance to remission and relapse. Bipolar Disord. 2003;5:129–37. https://doi.org/10.1034/j.1399-5618.2003.00021.x .
Koenders MA, Giltay EJ, Hoencamp E, Elzinga BM, Spinhoven P, Spijker AT. The bidirectional impact of perceived and enacted support on mood in bipolar outpatients: a two-year prospective study. Compr Psychiatry. 2015;60:59–67. https://doi.org/10.1016/j.comppsych.2015.03.009 .
Wicki W, Angst J. The Zurich study. Eur Arch Psychiatry Clin Neurosci. 1991;240:339–48. https://doi.org/10.1007/BF02279764 .
Falloon IRH, Emotion E. Expressed Emotion in Families By Julllan Leff and Christine Vaughn. Br J Psychiatry. 1985;1987(151):281–281. https://doi.org/10.1192/S0007125000216541 .
Sullivan AE, Judd CM, Axelson DA, Miklowitz DJ. Family functioning and the course of adolescent bipolar disorder. Behav Ther. 2012;43:837–47. https://doi.org/10.1016/j.beth.2012.04.005 .
Miller IW, Epstein NB, Bishop DS, Keitner GI. The McMaster Family assessment device: reliability and validity. J Marital Fam Ther. 1985;11:345–56. https://doi.org/10.1111/j.1752-0606.1985.tb00028.x .
Townsend LD, Demeter CA, Youngstrom E, Drotar D, Findling RL. Family conflict moderates response to pharmacological intervention in pediatric bipolar disorder. J Child Adolesc Psychopharmacol. 2007;17:843–51. https://doi.org/10.1089/cap.2007.0046 .
Kim EY, Miklowitz DJ. Expressed emotion as a predictor of outcome among bipolar patients undergoing family therapy. J Affect Disord. 2004;82:343–52. https://doi.org/10.1016/j.jad.2004.02.004 .
Yan LJ, Hammen C, Cohen AN, Daley SE, Henry RM. Expressed emotion versus relationship quality variables in the prediction of recurrence in bipolar patients. J Affect Disord. 2004;83:199–206. https://doi.org/10.1016/j.jad.2004.08.006 .
Weintraub MJ, Posta F, Arevian AC, Miklowitz DJ. Using machine learning analyses of speech to classify levels of expressed emotion in parents of youth with mood disorders. J Psychiatr Res. 2021;136:39–46. https://doi.org/10.1016/j.jpsychires.2021.01.019 .
Miklowitz DJ, Wisniewski SR, Miyahara S, Otto MW, Sachs GS. Perceived criticism from family members as a predictor of the one-year course of bipolar disorder. Psychiatry Res. 2005;136:101–11. https://doi.org/10.1016/j.psychres.2005.04.005 .
Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry. 2002;159:927–33. https://doi.org/10.1176/appi.ajp.159.6.927 .
Geller B, Tillman R, Craney JL, Bolhofner K. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype. Arch Gen Psychiatry. 2004;61:459–67. https://doi.org/10.1001/archpsyc.61.5.459 .
Geller B, Tillman R, Bolhofner K, Zimerman B. Child bipolar I disorder: Prospective continuity With adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch Gen Psychiatry. 2008;65:1125–33. https://doi.org/10.1001/archpsyc.65.10.1125 .
Garno JL, Goldberg JF, Ramirez PM, Ritzler BA. Impact of childhood abuse on the clinical course of bipolar disorder. Br J Psychiatry J Ment Sci. 2005;186:121–5. https://doi.org/10.1192/BJP.186.2.121 .
Daruy-Filho L, Brietzke E, Lafer B, Grassi-Oliveira R. Childhood maltreatment and clinical outcomes of bipolar disorder. Acta Psychiatr Scand. 2011;124:427–34. https://doi.org/10.1111/J.1600-0447.2011.01756.X .
Post RM, Altshuler LL, Kupka R, Mcelroy SL, Frye MA, Rowe M, et al. Verbal abuse, like physical and sexual abuse, in childhood is associated with an earlier onset and more difficult course of bipolar disorder. Bipolar Disord. 2015;17:323–30. https://doi.org/10.1111/BDI.12268 .
Du Rocher ST, Youngstrom EA, Martinez M, KogosYoungstrom J, Scovil K, Ross J, et al. Physical and sexual abuse and early-onset bipolar disorder in youths receiving outpatient services: Frequent, but not specific. J Abnorm Child Psychol. 2021;43:453–63. https://doi.org/10.1007/s10802-014-9924-3 .
Oliveira J, Etain B, Lajnef M, Hamdani N, Bennabi M, Bengoufa D, et al. Combined effect of TLR2 gene polymorphism and early life stress on the age at onset of bipolar disorders. PLoS ONE. 2015. https://doi.org/10.1371/journal.pone.0119702 .
Tijssen MJA, Van Os J, Wittchen HU, Lieb R, Beesdo K, Wichers M. Risk factors predicting onset and persistence of subthreshold expression of bipolar psychopathology among youth from the community: Predicting persistence of bipolar symptoms. Acta Psychiatr Scand. 2010;122:255–66. https://doi.org/10.1111/j.1600-0447.2010.01539.x .
Daglas R, Conus P, Cotton SM, Macneil CA, Hasty MK, Kader L, et al. The impact of past direct-personal traumatic events on 12-month outcome in first episode psychotic mania: trauma and early psychotic mania. Aust N Z J Psychiatry. 2014;48:1017–24. https://doi.org/10.1177/0004867414545672 .
Leverich GS, McElroy SL, Suppes T, Keck PE, Denicoff KD, Nolen WA, et al. Early physical and sexual abuse associated with an adverse course of bipolar illness. Biol Psychiatry. 2002;51:288–97. https://doi.org/10.1016/S0006-3223(01)01239-2 .
Pascual MA, Levenson JC, Merranko J, Gill MK, Hower H, Yen S, et al. The effect of traumatic events on the longitudinal course and outcomes of youth with bipolar disorder. J Affect Disord. 2020;274:126–35. https://doi.org/10.1016/j.jad.2020.05.131 .
Article PubMed Central Google Scholar
Gershon A, Johnson SL, Miller I. Chronic stressors and trauma: prospective influences on the course of bipolar disorder. Psychol Med. 2013;43:2583–92. https://doi.org/10.1017/S0033291713000147 .
Meade CS, McDonald LJ, Graff FS, Fitzmaurice GM, Griffin ML, Weiss RD. A prospective study examining the effects of gender and sexual/physical abuse on mood outcomes in patients with co-occurring bipolar I and substance use disorders. Bipolar Disord. 2009;11:425–33. https://doi.org/10.1111/j.1399-5618.2009.00682.x .
Nolen WA, Luckenbaugh DA, Altshuler LL, Suppes T, McElroy SL, Frye MA, et al. Correlates of 1-year prospective outcome in bipolar disorder: results from the Stanley foundation bipolar network. Am J Psychiatry. 2004;161:1447–54. https://doi.org/10.1176/appi.ajp.161.8.1447 .
McQuaid JR, Monroe SM, Roberts JE, Johnson SL, Garamoni GL, Kupfer DJ, et al. Toward the standardization of life stress assessment: Definitional discrepancies and inconsistencies in methods. Stress Med. 1992;8:47–56. https://doi.org/10.1002/smi.2460080107 .
Kim EY, Miklowitz DJ, Biuckians A, Mullen K. Life stress and the course of early-onset bipolar disorder. J Affect Disord. 2007;99:37. https://doi.org/10.1016/J.JAD.2006.08.022 .
Brown GW, Harris TO, editors. Life events and illness. New York: Guilford Press; 1989.
Johnson SL, Cuellar AK, Ruggero C, Winett-Perlman C, Goodnick P, White R, et al. “Life events as predictors of mania and depression in bipolar I disorder”: Correction to Johnson et al. (2008). J Abnorm Psychol. 2008;117:698. https://doi.org/10.1037/a0013417 .
Hosang GM, Uher R, Maughan B, McGuffin P, Farmer AE. The role of loss and danger events in symptom exacerbation in bipolar disorder. J Psychiatr Res. 2012;46:1584–9. https://doi.org/10.1016/j.jpsychires.2012.07.009 .
Johnson SL, Sandrow D, Meyer B, Winters R, Miller I, Solomon D, et al. Increases in manic symptoms after life events involving goal attainment. J Abnorm Psychol. 2000;109:721–7. https://doi.org/10.1037/0021-843X.109.4.721 .
Article CAS PubMed PubMed Central Google Scholar
Nusslock R, Abramson LY, Harmon-Jones E, Alloy LB, Hogan ME. A goal-striving life event and the onset of hypomanic and depressive episodes and symptoms: Perspective from the behavioral approach system (BAS) dysregulation theory. J Abnorm Psychol. 2007;116:105–15. https://doi.org/10.1037/0021-843X.116.1.105 .
Francis-Raniere EL, Alloy LB, Abramson LY. Depressive personality styles and bipolar spectrum disorders: prospective tests of the event congruency hypothesis. Bipolar Disord. 2006;8:382–99. https://doi.org/10.1111/j.1399-5618.2006.00337.x .
Gerstein RK. The long-term course of bipolar spectrum disorder: applications of the behavioral approach system (BAS) model. 2011. http://doi.org/ https://doi.org/10.34944/dspace/1270
Staufenbiel SM, Koenders MA, Giltay EJ, Elzinga BM, Manenschijn L, Hoencamp E, et al. Recent negative life events increase hair cortisol concentrations in patients with bipolar disorder. Stress. 2014;17:451–9. https://doi.org/10.3109/10253890.2014.968549 .
Fulford D, Johnson SL, Llabre MM, Carver CS. Pushing and coasting in dynamic goal pursuit: coasting is attenuated in bipolar disorder. Psychol Sci. 2010;21:1021–7. https://doi.org/10.1177/0956797610373372 .
Lozano BE, Johnson SL. Can personality traits predict increases in manic and depressive symptoms? J Affect Disord. 2001;63:103–11. https://doi.org/10.1016/S0165-0327(00)00191-9 .
Johnson KR, Johnson SL. Cross-national prevalence and cultural correlates of bipolar i disorder. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1111–7. https://doi.org/10.1007/S00127-013-0797-5 .
Johnson SL, Edge MD, Holmes MK, Carver CS. The behavioral activation system and mania. Annu Rev Clin Psychol. 2012;8:243–67. https://doi.org/10.1146/annurev-clinpsy-032511-143148 .
Ehlers CL, Kupfer DJ, Frank E, Monk TH. Biological rhythms and depression: The role of zeitgebers and zeitstorers. Depression. 1993;1:285–93. https://doi.org/10.1002/DEPR.3050010602 .
Murray G, Harvey A. Circadian rhythms and sleep in bipolar disorder. Bipolar Disord. 2010;12:459–72. https://doi.org/10.1111/j.1399-5618.2010.00843.x .
Shen GHC, Alloy LB, Abramson LY, Sylvia LG. Social rhythm regularity and the onset of affective episodes in bipolar spectrum individuals. Bipolar Disord. 2008;10:520–9. https://doi.org/10.1111/J.1399-5618.2008.00583.X .
Malkoff-Schwartz S, Frank E, Anderson BP, Hlastala SA, Luther JF, Sherrill JT, et al. Social rhythm disruption and stressful life events in the onset of bipolar and unipolar episodes. Psychol Med. 2000;30:1005–16. https://doi.org/10.1017/S0033291799002706 .
Malkoff-Schwartz S, Frank E, Anderson B, Sherrill JT, Siegel L, Patterson D, et al. Stressful life events and social rhythm disruption in the onset of manic and depressive bipolar episodes: a preliminary investigation. Arch Gen Psychiatry. 1998;55:702–7. https://doi.org/10.1001/ARCHPSYC.55.8.702 .
Sylvia LG, Alloy LB, Hafner JA, Gauger MC, Verdon K, Abramson LY. Life events and social rhythms in bipolar spectrum disorders: a prospective study. Behav Ther. 2009;40:131–41. https://doi.org/10.1016/j.beth.2008.04.003 .
Stevens JS, van Rooij SJH, Jovanovic T. Developmental contributors to trauma response: the importance of sensitive periods, early environment, and sex differences. Curr Top Behav Neurosci. 2018;38:1–22. https://doi.org/10.1007/7854_2016_38 .
Lieberman DZ, Massey SH, Goodwin FK. The role of gender in single vs married individuals with bipolar disorder. Compr Psychiatry. 2010;51:380–5. https://doi.org/10.1016/j.comppsych.2009.10.004 .
Post R, Altshuler L, Kupka R, McElroy S, Frye MA, et al. More pernicious course of bipolar disorder in the United States than in many European countries: Implications for policy and treatment. J Affect Disord. 2014;160:27–33. https://doi.org/10.1016/j.jad.2014.02.006 .
Guzman-Parra J, Streit F, Forstner AJ, Strohmaier J, González MJ, Gil Flores S, et al. Clinical and genetic differences between bipolar disorder type 1 and 2 in multiplex families. Transl Psychiatry. 2021;11:1–10. https://doi.org/10.1038/s41398-020-01146-0 .
Boyers GB, Simpson RL. Social support and relationship satisfaction in bipolar disorder. J Fam Psychol. 2018;32:538–43. https://doi.org/10.1037/fam0000400 .
Pfennig A, Leopold K, Martini J, Boehme A, Lambert M, Stamm T, et al. Improving early recognition and intervention in people at increased risk for the development of bipolar disorder: Study protocol of a prospective-longitudinal, naturalistic cohort study (Early-BipoLife). Int J Bipolar Disord. 2020. https://doi.org/10.1186/s40345-020-00183-4 .
Trivedi MH, Chin Fatt CR, Jha MK, Cooper CM, Trombello JM, Mason BL, et al. Comprehensive phenotyping of depression disease trajectory and risk: Rationale and design of Texas Resilience Against Depression study (T-RAD). J Psychiatr Res. 2020;122:22–32. https://doi.org/10.1016/j.jpsychires.2019.12.004 .
Miklowitz DJ, Efthimiou O, Furukawa TA, Scott J, McLaren R, Geddes JR, et al. Adjunctive psychotherapy for bipolar disorder: a systematic review and component network meta-analysis. JAMA Psychiat. 2021;78:141–50. https://doi.org/10.1001/jamapsychiatry.2020.2993 .
National Collaborating Centre for Mental Health (UK). Bipolar Disorder: The NICE Guideline on the Assessment and Management of Bipolar Disorder in Adults, Children and Young People in Primary and Secondary Care. London: The British Psychological Society and The Royal College of Psychiatrists; 2014.
Hirschfeld RMA, Bowden CL, Gitlin MJ, Keck PE, Suppes T, Thase ME, et al. Practice guideline for the treatment of patients with bipolar disorder. 2nd ed. Arlington: American Psychiatric Association; 2002.
Miller IW, Keitner GI, Ryan CE, Uebelacker LA, Johnson SL, Solomon DA. Family treatment for bipolar disorder: family impairment by treatment interactions. J Clin Psychiatry. 2008;69:732–40. https://doi.org/10.4088/JCP.v69n0506 .
Miklowitz DJ, Axelson DA, George EL, Taylor DO, Schneck CD, Sullivan AE, et al. Expressed emotion moderates the effects of family-focused treatment for bipolar adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48:643–51. https://doi.org/10.1097/CHI.0b013e3181a0ab9d .
Eisner LR, Johnson SL. An acceptance-based psychoeducation intervention to reduce expressed emotion in relatives of bipolar patients. Behav Ther. 2008;39:375–85. https://doi.org/10.1016/j.beth.2007.11.001 .
Miklowitz DJ, George EL, Richards JA, Simoneau TL, Suddath RL. A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. Arch Gen Psychiatry. 2003;60:904–12. https://doi.org/10.1001/archpsyc.60.9.904 .
Garrett AS, Miklowitz DJ, Howe ME, Singh MK, Acquaye TK, Hawkey CG, et al. Changes in brain activation following psychotherapy for youth with mood dysregulation at familial risk for bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2015;56:215–20. https://doi.org/10.1016/j.pnpbp.2014.09.007 .
Harvey AG, Soehner AM, Kaplan KA, Hein K, Lee J, Kanady J, et al. Treating insomnia improves mood state, sleep, and functioning in bipolar disorder: a pilot randomized controlled trial. J Consult Clin Psychol. 2015;83:564–77. https://doi.org/10.1037/a0038655 .
Download references
Acknowledgements
The authors thank Nandini A. Rajgopal for help with the literature search. Support for this manuscript preparation was provided by the National Institute of Mental Health (NIMH) R01 MH110477.
Preparation of this manuscript was supported by NIMH R01, MH110477.
Author information
Authors and affiliations.
Department of Psychology, University of California, 2121 Berkeley Way West, MC 2010, Berkeley, CA, 94720-2010, USA
Sheri L. Johnson & Benjamin Z. S. Weinberg
You can also search for this author in PubMed Google Scholar
Contributions
SJ and BW collaborated on the literature search and summary, SJ drafted the manuscript, and BW edited the manuscript and prepared tables. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Sheri L. Johnson .
Ethics declarations
Ethical standards and consent to participants, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix A: Prisma checklist
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Johnson, S.L., Weinberg, B.Z.S. Social and environmental variables as predictors of mania: a review of longitudinal research findings. Discov Ment Health 2 , 7 (2022). https://doi.org/10.1007/s44192-022-00010-5
Download citation
Received : 06 January 2022
Accepted : 07 February 2022
Published : 14 March 2022
DOI : https://doi.org/10.1007/s44192-022-00010-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bipolar disorder
- Social support
- Life events
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Public Health
Promoting University Students' Mental Health: A Systematic Literature Review Introducing the 4M-Model of Individual-Level Interventions
Bhavana nair.
1 Guidance & Counseling Office, Student Services & Registration, Mohammed Bin Rashid University of Medicine and Health Sciences (MBRU), Dubai, United Arab Emirates
Farah Otaki
2 Strategy & Institutional Excellence, Mohammed Bin Rashid University of Medicine and Health Sciences (MBRU), Dubai, United Arab Emirates
Associated Data
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Objective: The purpose of this study is to systematically review recently published individual student-level interventions aimed at alleviating the burden of mental health challenges faced by the students and/ or at equipping them with coping mechanism that will foster their resilience.
Methods: This study relied on a systematic literature review. PubMed dataset was used; the search was confined to the following period: July 2016-December 2020.
Results: A total of 1,399 records were identified by the electronic search, out of which 40 studies were included in this study. The authors inductively identified four overlapping categories of interventions across all included articles, and coded them as follows: Mindfulness, Movement, Meaning, and Moderator. Accordingly, each study was linked to at least one of four overlapping categories based on the nature of the intervention(s) under investigation, leading to differing assortments of categories.
Conclusions: The 4M-Model generated by this study encourages focusing on devising holistic, university-based interventions that embrace the individuality of students to improve their mental health through elements of mindfulness, movement, meaning, and moderator. Through this focused approach, university counselors are enabled to design interventions that address students' physical, psychological, emotional, and social needs.
Introduction
There has been a positive paradigm shift in the way our world and its citizens are perceiving the concept of mental health. Mental health is a state of well-being that allows individuals to enjoy and maintain relationships as well as handle stress in a healthy manner without compromising on productivity ( 1 ).
A large body of literature on tertiary education students highlights the importance of maintaining mental health with evidence relating it to educational attainment and productivity ( 2 ), social relationships, engagement on campus, and quality of life ( 3 ), and placement performance ( 4 ). Poor mental health has also been linked with lower retention within a programme, grade point averages, and graduation rates among university students ( 5 ). Counseling, psychoeducation, and mental health services on campuses are no longer deemed as merely supportive but rather an integral component necessary to empower students. These services are integral to help students develop skills such as psychological flexibility ( 6 ) which in turn influences mental health ( 1 ).
The current generation of university students is vastly different from previous generations, especially in their attitudes and beliefs toward their mental health needs. Well-being is a dynamic concept of interlinked physical, social, and psychological dimensions which is constantly changing depending on intrinsic and extrinsic environments and motivations ( 7 ). It is not only the demographics of the current generation of university students that has changed considerably from the past ( 8 ), but so have their attitudes and beliefs toward their needs, including mental health ( 3 ). This population is considered high risk because most mental health problems are triggered before the age of 24 ( 9 ). There is enough evidence to link personal and academic stressors to mental health ( 10 – 12 ). Contemporary tertiary education is striving to attain and maintain cultures of excellence, similar to traditional universities in the past ( 13 ). However, there has been a shift to turn modern day campuses into high stakes competitive testing environments with well-intended emphasis on preparing students to become part of the global economy. This change has influenced the context in which modern universities function. There are a set of challenges that contemporary universities face that extend beyond the earlier tertiary educational institutions and there is an assumption that students are coming to college “overwhelmed and more damaged than those of previous years” ( 14 ).
Although good citizenship has always been an important foundation of all educational institutions, with the dynamic social landscape that the universities are set within, there seems to be a tendency to lead students to fixate on extrinsic factors such as: results and Grade Point Averages, over intrinsic interest such as innovative learning, and expansion of lateral thinking ( 13 ). When the priority is grades, it manifests itself in excessive hours of focused studying, and in negative coping behaviors, such as: inadequate sleep and addictive behaviors, which could potentially affect the well-being of the student. Often, in this pursuit of academic excellence, there is the danger of ignoring the social, emotional, and psychological problems that modern students are now increasingly facing.
There is enough research that indicates that students are experiencing more mental health disorders in contemporary times and are less resilient than students in the past ( 8 ), with lower levels of frustration tolerance ( 15 ). Anxiety and depression are most prevalent among tertiary students ( 16 ). There is a rise in the number of college students with a diagnosable psychological disorder ( 17 ) with some students at greater risk than others of experiencing stress and mental health problems ( 18 ). There has been also a shift in the severity of the problems by students seeking counseling services over the past decade. It is no longer just presenting challenges of adjustment and individuation ( 19 ), or benign hormonal developmental problems associated with the age that prompts students to seek counseling. Students are presenting with severe psychological problems ( 20 ) with a sizeable number of them on psychiatric medication to help them function better on campus ( 15 ).
A common narrative through an exhaustive body of literature highlights the barriers to seeking help for mental health problems by students on campus due to stigma ( 21 ), scepticism about treatment efficacy ( 22 ), and a belief that their emotional problems will not be completely understood. This leads to a sense of social isolation as the students restrain from reaching out for help ( 21 ). Two contributing factors to inadequate help-seeking are the stigma of having a mental health problem and the personal characteristics of the individual student ( 20 ). A fear of negative consequences on academic records ( 23 ) is another common barrier among university students. Interestingly, students resist seeking help because they do not perceive their condition to require intervention or do not perceive it as a priority among their other commitments. They also have the tendency to normalize stress as part of university life, expecting it “will go away with time,” and prefer to handle their problems on their own ( 24 ).
More recent research indicates that students also rely on informal sources of help-seeking from non-professionals, particularly peer groups ( 25 ). Students report having no inhibitions about having open discussions about their mental health problems via social-networking websites ( 26 ). This resonates with the network episode model of help-seeking that emphasizes the social network as an integral, contemporary support in enhancing knowledge and attitudes toward seeking help ( 27 ). However, there is also a significant increase in the number of students with major psychological problems seeking counseling services on campus ( 3 ) challenging the stigma connected with help-seeking. The newer generation's familiarity with psychosocial support services and openness toward seeking them are putting mental health at the core of self-care, much like diet and exercise ( 26 ).
Along with rapid social changes and expectations, the dilution of traditional family anchors (that is the changes to family systems which include busy yet isolated lifestyles, social media pressures, a living free from parental influence which is very common to this age group, and forced separation from families in the pursuit of dream destinations for education) all compounding to the considerable degree of stress that students report upon ( 18 ). Considering all these transitions, focusing on the support that is available to young people on campus is increasingly becoming a necessity. This is not only a personal benefit for students but a national and international investment that could also result in considerable economic benefit ( 28 ) as these students stand to become contributors to the global economy.
A wealth of research exists which highlights the effectiveness of changing organizational factors that influence mental health ( 29 , 30 ). However, there is limited research on person-centric mental health strategies used in university settings ( 31 ). A Systematic Literature Review that was conducted by Fernandez et al. focused on evaluating the effect of setting-based interventions that stimulated and improved the mental health and well-being of university students and employees ( 32 ). That review constitutes an asset for universities seeking to adopt setting-based strategies that were proven efficacious. Yet, given the highspeed in which the higher education ecosystem has been evolving, there is an evident need for a more up-to-date review. Also, despite the importance of modifying the environment for it to become more nurturing for university students' mental health, this needs to be in conjunction with embracing the individuality of each student. Accordingly, the purpose of this study is to bridge this gap through providing a review of the literature on recently published individual student-level interventions that aim to alleviate the burden of mental health challenges faced by the students and/or help them with coping mechanisms that will foster their resilience.
We conducted a systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines ( 33 ). The protocol of the systematic review was published in PROSPERO, a database of prospectively registered systematic reviews in health and social care (CRD42021227862).
Search Strategy
To complement the work of Fernandez et al., focusing on the recent literature, the search period was confined to July 2016 through December 2020 ( 32 ). PubMed database was used. The search strategy used, with its key words and Boolean logic, is available as an online resource. It was structured as follows:
- Subjects: student or resident.
- Location: higher education, university, college, or tertiary education.
- State-of-being : mental health.
- Challenges faced by subjects : psychosocial, anxiety, depression, burnout, stress, peer-pressure, social media pressure, bullying, eating disorder, perfectionism, or learning difficulties.
- Intervention to address the challenges : psychotherapy, mindfulness, Counseling, support group, yoga, breathing, art therapy, awareness, resilience, gratitude, affirmations, or peer-Counseling.
Pure qualitative studies were excluded. We included all quantitative studies, so long as they contained information on the impact of the intervention. These included those using experimental (i.e., randomized controlled trials) or observational (i.e., controlled trials without randomization, and pre-post and time series) approaches. Duplicated papers were excluded. Studies were screened for inclusion in three phases:
- BN and FO went over all the abstracts, together, to remove the articles that certainly did not meet the inclusion criteria.
- The full text of all the remaining abstracts were reviewed independently by BN and FO. The results were discussed. Any discrepancies were investigated and reflected upon until reaching consensus.
- Finally, all remaining articles were thoroughly reviewed for summarizing purposes based on a preset template: research study objective, context, design, method, sample, intervention, and main conclusion.
Articles were included if:
- a) Empirical/applied (i.e., theoretical studies or systematic reviews, and studies using secondary data were excluded),
- b) Conducted in one or more university,
- c) Aimed at evaluating, the immediate or long-term effect of an intervention on the mental health status of students,
- d) Included global measures of mental health and well-being,
- e) Had the university counselor involved in the intervention,
- f) Involved full-time students, and
- g) Was written in English.
Quality Assessment
The quality of each of the included articles was evaluated considering the internal and external validity. For the internal validity (risk of bias), each study's methodological quality was assessed using the criteria introduced by Jadad et al. ( 34 ). As for the external/ ecological validity of the included studies, it was assessed using the criteria developed by Green and Glasgow ( 35 ). This quality assessment was not used to exclude articles. Yet, the results of the assessment were thoroughly reflected upon as an evaluative measure of the review output.
Data Analysis
The interventions referred to in the included studies were analyzed by the researchers using the framework of Braun and Clarke ( 36 ). The intention was to inductively build a general interpretation of all included studies, in alignment with the paradigm of constructivism ( 37 , 38 ). The assumption was that reality is socially-constructed. This required thoroughly reflecting upon the interventions investigated in the included studies. The process of exploratory reflection adapted was spiral, where the researchers' observations kept getting revisited which culminated into the development of an evidence-driven model. Since the constructivism paradigm gives precedence to thoroughness and insightfulness over extensiveness and generalizability ( 39 ), the decision was made upfront, as abovementioned, for this search to be limited to a single database ( 40 ). As for the purpose of the qualitative meta-synthesis, it was to create a dynamic individual-level intervention framework that is holistic and context-specific ( 41 ). All articles were categorized based on the nature of the intervention(s) under investigation. It is all narratively presented in the results section.
A total of 1,399 records were identified by the electronic search. Two researchers (BN and FO) reviewed all the abstracts of the resulting papers to identify ones that fitted the inclusion criteria. Based on that, a total of 1,178 articles were excluded. The full text of all remaining 220 articles were extracted and thoroughly reviewed by the two researchers (110 by each). Accordingly, 133 articles were excluded. The remaining 87 articles underwent another round of assessment by both researchers together. Out of these 87 articles, 47 papers were excluded: four studies did not meet the eligibility criteria of having an intervention in them, 31 studies did not include assessing the effectiveness of an intervention,10 studies were not exclusively on university students, and 1 was not on full-time students. Also, one study was excluded because it was not counselor-led but outsourced. Out of the initially identified 1399 articles, 40 articles were finally included in the study ( Figure 1 ).

PRISMA flow-diagram. Promoting university students' mental health: a systematic literature review introducing the 4M-Model of individual-level interventions, Dubai, United Arab Emirates, 2020.
Of the 40 studies, nine studies were conducted in USA, eight in United Kingdom, four in Canada, three in Australia, five in Germany, four in China, and one in each of Turkey, Hungary, Israel, Ireland, Japan, South Korea and Netherlands. The quality of evidence is very high in terms of internal validity because most of the studies ( 25 ) employed RCT, five studies used a quasi-experimental method, two had a cross sectional design, and eight studies utilized a pre-post design without a control group.
The external validity of the papers could be considered low/ moderate. Since most of the studies indicated the experience of only one institution; generalization of the findings is limited. The only exceptions were one study that was conducted in Israel which included three institutions and one conducted in UK which included eight universities. After thoroughly reflecting upon the interventions under investigation across all 40 resulting studies, the authors qualitatively synthesized a holistic framework. This involved inductively identifying four overlapping categories of interventions. Each category was in turn coded with a label that appeared to be most fit to the encapsulated interventions and that is in harmony with the codes of the rest of the categories (i.e., alliteration).
Accordingly, each study was linked to at least one of four overlapping categories based on the nature of the intervention(s) under investigation ( Table 1 ). The first category, coded as Mindfulness, included individual-level interventions that used mindfulness as a strategy to promote mental health. Mindfulness, in this context, refers to any intervention that aims to promote living in the moment or “now” and adopting acceptance and a non-judgmental attitude to guide action. The popular Mindfulness Based Stress Reduction (MBSR) curriculum was used in four studies ( 8 , 42 – 45 ). Mindfulness Based Cognitive Therapy (MBCT) which focuses on reframing thoughts along with becoming aware of the nature and quality of them was found to also be effective in two studies ( 46 , 47 ). In three studies, the intervention(s) made use of imagery and self-guidance ( 48 – 51 ), whereas two other studies explored the effectiveness of Acceptance and Commitment Therapy (ACT) ( 6 ) to improve the psychological flexibility, school engagement, and mental health among University students.
Distribution of the output of the systematic literature review depending on the nature of the intervention(s) under investigation.
Promoting university students' mental health: a systematic literature review introducing the 4M-Model of individual-level interventions, Dubai, United Arab Emirates, 2020 .
The second category of studies was coded as Movement and included individual-level interventions which have a predominant physical element and solicit change in bodily sensations including but not limited to yoga, fitness, dance, kickboxing, and aerobics and breathing exercises. While Tong et al. ( 52 ) exclusively looked at the effect of Yoga and Fitness on mental health, five sets of researchers ( 8 , 42 , 43 , 45 , 46 ) looked at breathing and simple yoga as part of their mindfulness course. Sleep was studied in connection to mental health in two studies ( 53 , 54 ) as it has been found to be a precursor to many mental health problems with insomnia and the quality of sleep put on top of the list affecting sleep hygiene. Behavioral activation, a personalized therapeutic tool mainly used in the treatment of depression targeting behaviors that feed into the condition, was found to be effective in three studies that were reviewed ( 55 – 57 ) involving students with mild depression. The goal of Behavioral Activation is engaging in enjoyable activities with a part of the process focusing on getting past obstacles that may impede that enjoyment. One study included peer-led support ( 56 ) and online delivery of the course ( 57 ), where both appeared to be efficacious. Only one study by Chalo et al. ( 58 ) used Biofeedback intervention, that involved measuring students' quantifiable bodily functions to convey information to them in real-time as a solution to help students manage their physiological response to anxiety and stress.
The third category was coded as Meaning and included studies that investigate individual-level interventions that focus on the counselor addressing connections and associations between variables and enabling the student to reframe cognitions. Psychoeducation was widely utilized with cognitive training as the most common ( 54 , 59 – 63 ). Eustis et al. ( 49 ) focused their study on the student's self-awareness, while Demir and Ercan ( 64 ) explored communication techniques among students. In addition, three studies explored the feasibility of having courses embedded within the curriculum ( 38 , 48 , 50 ) to improve the mental health of students, while nine studies explored the effect of elective courses that aimed at stress reduction ( 18 , 43 , 50 , 56 , 58 , 65 – 69 ).
The last category of studies was coded as Moderator which referred to any element of support that was deployed in conjunction with the counselor, in an individual-level intervention, that acts as a moderator between the student and the counselor. Pet therapy was explored in three studies ( 70 – 72 ) to assess well-being, and an extensive use of the computer to deliver courses such as ACT, Psychoeducation, and Cognitive Behavior Therapy (CBT) which are all traditionally effective in psychotherapy, were found to be efficacious online in 10 studies ( 44 , 50 , 57 , 61 , 73 – 78 ) highlighting the significance of the potential of web-based interventions to impart psychotherapy to a wider audience.
This literature review showed that elements of Mindfulness were a major part of the 23 studies, Meaning was predominant in 24 studies, while Movement was an important feature in 17 studies. An element of support complementary to the therapist, either in the form of a pet (canine) or a web/phone application (i.e., Moderator), was part of 16 interventions. Commonly used approaches were Mindfulness based therapies, ACT, Cognitive Behavior Therapy, and Psychoeducation. The duration of the interventions investigated in the included studies ranged between 1 and 12 weeks, with most of the studies spanning between 6 and 8 weeks. Nine studies had just one element, and only one study ( 49 ) had all the four elements included ( Figure 2 ), which the authors perceived as a “lucky find.”

The 4M-Model generated from this study's qualitative synthesis, visually illustrated as a four-leaf clover which is a symbol of luck. Promoting university students' mental health: a systematic literature review introducing the 4M-Model of individual-level interventions, Dubai, United Arab Emirates, 2020.
Thirty-one studies had overlapping elements indicating that these elements are not mutually exclusive and rather interlinked and are blended with the intention of enhancing the effectiveness of a program.
The output of this Systematic Literature Review revealed diverse interventions. Most of these interventions were hybrid versions of existing evidence-based interventions. A few of the identified articles reflected upon contextualized home-grown interventions. There appeared to be a lack of consensus on a common model/ approach to effectively improve the mental health and wellness of university students ( 61 ) who are known to have their own set of challenges. Hence, this paper provides an outline of practices that have been deployed in this direction, illustrating them from a holistic perspective. Elements of mindfulness, meaning, movement, and use of a moderator were seen to overlap in the studies. The blending of these elements was proven to be effective in improving metacognitive awareness, emotional regulation ( 79 ), concentration, and mental clarity ( 80 ), and decreasing emotional reactivity ( 81 ) and rumination (through disengagement with persistent negative thoughts) ( 82 ) and in turn reducing depression, stress, and anxiety ( 83 ). It has also shown to foster social connectedness and the ability to express oneself in various social situations ( 84 ) thereby reducing stress and anxiety and increasing patience, gratitude, and body awareness ( 85 ). With so many elements that need to be taken into consideration, the researchers have attempted to comprehend the output of this review from the field theory point-of-view where the “organism and environment are perceived as part of an interacting field” ( 86 ).
Moreover, Counseling strategies and interventions are meant to emphasize on the growth of an individual. The human potential for self-actualization, a concept understood by Abraham Maslow as a change process that aims at making a person “aware of what is going on inside himself” [Maslow, as cited in Seaman ( 87 ), p. 3] is core to Counseling interventions, which is where the four elements blend to become crucial to the process of self-awareness and eventually self-growth.
The results of the study indicate that self-awareness through mindfulness is an important foundation upon which all other elements build up to improve mental health of students. This was not a surprising find because this is in alignment with the results of many previously conducted studies ( 88 , 89 ). Mindfulness seems to be the new mantra and has been intensively researched ( 90 ). However, despite a substantial amount of theoretical work conducted to merge Buddhist and Western conceptual viewpoints to psychotherapy ( 91 ), there is minimal literature on how it can translate to practice making this review an important addition to the limited knowledge around the topic of psychological interventions that have been found to be effective among university students. MBSR has proven to reduce stress and anxiety among university students by fostering insight and concentration along with physiologic relaxation ( 92 ). Teaching students to live in the present moment by reframing thoughts (i.e., MBCT) has been found to be effective in reducing depression ( 93 ). It also lessens the risk of relapse with comparable efficacy to antidepressant medication ( 94 ) which, in itself, is a breakthrough for psychotherapy. ACT which focuses on acceptance has been found to improve coping, self-regulation, psychological flexibility, and school engagement ( 6 ). Counseling young adults, in particular students at the university level, would benefit by basing it on Engel's biopsychosocial viewpoint which includes taking into consideration the hormonal changes (biological), identity crisis, and the challenges arising from intimacy and isolation (psychological) which have been hypothesized in Eric Erickson's psychosocial stages of development for this age group. The new age technological challenges of peer-pressure over social media sites and the demands of fitting in and changing family dynamics (sociological) also need to be taken into consideration when conceptualizing a Counseling program for this target group.
Moreover, this transition stage between adolescence and adulthood, also referred to as “emerging adulthood” ( 95 ), is considered to be a period of accepting responsibility for one's actions and livelihood, developing belief systems and values independent of parental and external influences, and establishing relationships with parents on equal grounds. Young university students who are still financially dependent and living with parents during this period are arbitrarily considered to be adolescents if adult responsibilities are not yet accessed. These intangible markers gradually develop. The entailed process could last many years until the corresponding responsibilities are effectively adopted. As such, the range between adolescence and adulthood becomes wider than typically defined, stretching from the beginning of puberty to the early twenties ( 96 ).
Counseling has been traditionally associated as a profession that requires the physical presence of a minimum of two people in a professional relationship to talk through and process experiences to gain insight and understanding. However, in this review, it is evident that web-based interventions seem to produce an equally effective result ( 97 ) as observed in 16 studies of the literature review which could be utilized as a complementary medium widening the scope of practice of counselors and psychotherapists. This could also help in minimizing the stigma associated with getting undesirably labeled and help in reducing psychological self-restraint which has been termed as ‘online disinhibition effect' ( 98 ). Web-based mental health interventions also are becoming a preferred medium for students to gain services and information ( 99 ) as they accommodate their busy schedules ( 100 ).
Another observation was that even though most of the interventions were conducted only for a short period of time, the effectiveness of the interventions was established. Embedding interventions within the curriculum has been suggested ( 101 ) which makes this review even more pertinent for innovations in curriculum planning. This may also help in alleviating the stigma that is attached to Counseling services which is often a barrier that prevents students from reaching out for help ( 102 ). This aligns with Vygotsky's notion of Zone of Proximal Development ( 103 ) which refers to pedagogical support being beneficial for activities, in this context, psychoeducation of positive behaviors that facilitate help seeking behaviors before they can start using them independently.
The above observations prompted the researchers to recognize that the four identified elements when combined would result in a holistic approach of addressing the individual from a biopsychosocial point-of-view. This was depicted in the form of the 4M-Model to guide counselors to develop and implement university-level interventions that could help to reduce stress, anxiety, and depression as well as improve emotion regulation and self-awareness to address the mental health needs of young adults. It would be worthwhile for future research studies to validate the suggested 4M-Model through a similar systematic review of the literature relying on a combination of databases ( 104 ). The analysis in this case would be deductive where the model conceived from this study can be used as a preset template. Also, for validation purposes, it is recommended to conduct follow-up studies aimed at evaluating the efficaciousness of a tailor-made assortment of interventions that can be linked to all elements of the 4M-Model. For that purpose, it would be useful to adapt a mixed methods approach to research, where quantitative and qualitative findings will be integrated to obtain a holistic perspective of the output, outcome, and impact of such university-based, individual-student level mental health initiatives.
Findings of this review reveal the 4M-Model that happen to address all aspects of holistic well-being: physical, psychological, emotional, and social. Effectiveness of the varied interventions that have been reviewed in this study indicate that if a comprehensive approach toward intervention including mindfulness, movement, moderator, and meaning is adapted, then it would not only help students to be supported in a holistic manner but would help counselors plan and execute their programs in a focused approach to address the needs of any university student population who are increasingly overwhelmed and burned out with the stressors from their outside worlds as well as from within. The findings from the review add to the growing evidence for the urgent need of an intervention model that can serve as a directive for counselors and students.
Data Availability Statement
Author contributions.
BN and FO conceptualized the study, conducted the review, performed the qualitative meta-synthesis, and prepared and approved the manuscript. Both authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to extensd their gratitude to three of their colleagues: Dr. Lisa Jackson, Dr. Leigh Powell, and Ms. Mersiha Kovacevic, for their active role, and valuable reflections and feedback in reviewing the complete manuscript.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 18 March 2024
The impact of mindfulness apps on psychological processes of change: a systematic review
- Natalia Macrynikola 1 ,
- Zareen Mir 2 ,
- Tishmattie Gopal 3 ,
- Erica Rodriguez 4 ,
- Sunnie Li 4 ,
- Milann Cox 5 ,
- Gloria Yeh 1 &
- John Torous 1
npj Mental Health Research volume 3 , Article number: 14 ( 2024 ) Cite this article
1031 Accesses
8 Altmetric
Metrics details
- Health care
Mindfulness-based interventions (MBIs) have demonstrated therapeutic efficacy for various psychological conditions, and smartphone apps that facilitate mindfulness practice can enhance the reach and impact of MBIs. The goal of this review was to summarize the published evidence on the impact of mindfulness apps on the psychological processes known to mediate transdiagnostic symptom reduction after mindfulness practice. A literature search from January 1, 1993, to August 7, 2023 was conducted on three databases, and 28 randomized controlled trials involving 5963 adults were included. Across these 28 studies, 67 outcome comparisons were made between a mindfulness app group and a control group. Between-group effects tended to favor the mindfulness app group over the control group in three psychological process domains: repetitive negative thinking, attention regulation, and decentering/defusion. Findings were mixed in other domains (i.e., awareness, nonreactivity, non-judgment, positive affect, and acceptance). The range of populations examined, methodological concerns across studies, and problems with sustained app engagement likely contributed to mixed findings. However, effect sizes tended to be moderate to large when effects were found, and gains tended to persist at follow-up assessments two to six months later. More research is needed to better understand the impact of these apps on psychological processes of change. Clinicians interested in integrating apps into care should consider app-related factors beyond evidence of a clinical foundation and use app databases to identify suitable apps for their patients, as highlighted at the end of this review.
Similar content being viewed by others

Microdosing with psilocybin mushrooms: a double-blind placebo-controlled study
Federico Cavanna, Stephanie Muller, … Enzo Tagliazucchi

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers
Joseph M. Rootman, Pamela Kryskow, … Zach Walsh

The serotonin theory of depression: a systematic umbrella review of the evidence
Joanna Moncrieff, Ruth E. Cooper, … Mark A. Horowitz
Introduction
Mindfulness-based interventions (MBIs) have demonstrated efficacy in improving a range of clinical outcomes, such as depression and anxiety 1 . In a rigorous randomized controlled trial, mindfulness-based stress reduction (MBSR) was even found to be non-inferior to antidepressant medication 2 . However, MBI delivery and impact remain limited by various factors, two important ones being barriers to access and difficulties with sustained engagement. That is, for many individuals, MBIs remain inaccessible for the same reasons that mental health treatment remains inaccessible, including cost, stigma, a shortage of clinicians, and various logistical barriers (e.g., lack of transportation, lack of childcare) 3 , 4 . In addition, MBIs necessitate practice outside of session, which contributes to outcomes 5 ; however, many struggle to sustain a consistent mindfulness practice on their own outside of in-person sessions.
Technology can bridge the gap in both of these situations. Mindfulness apps can provide an alternative when in-person MBIs are inaccessible, and integrating mindfulness apps into in-person treatment can facilitate practice and increase intervention impact 6 , 7 . Yet most commercially available mindfulness apps have not been scientifically evaluated 8 , and most mental health apps struggle to keep users engaged 9 . Related, uptake of mindfulness apps is low in treatment, despite interest from clinicians 10 and their patients 11 , 12 . One commonly cited barrier is a lack of knowledge about which apps are credible and effective 13 . To address these barriers and stimulate more research into building the mindfulness app evidence base, we conducted a systematic review to assess these apps’ effectiveness in shifting psychological processes of change related to mindfulness.
Recent reviews suggest that mindfulness app effects on clinical outcomes are often inconsistent. For example, one review found generally small app effects on depression and contradictory results for anxiety 14 . However, the common approach of evaluating app effects on such distal psychological outcomes as psychiatric disorders is problematic because app intervention periods tend to be too brief for these types of outcomes to demonstrate significant and consistent change. A recent meta-analysis of 23 mindfulness app evaluations found that only nine studies used intervention periods that adhered to the recommended eight weeks of such MBIs as MBSR and MBCT 15 . Therefore, a more suitable approach to reviewing mindfulness app efficacy may be to focus on the more proximal processes of change, or mechanisms, that have been empirically demonstrated to explain the effects of mindfulness practice on more distal psychological outcomes. Temporally, mechanisms shift first 16 ; thus, focusing on these intermediary outcomes may provide a clearer picture of the efficacy of mindfulness apps.
Adopting a mechanisms-as-outcomes approach has three additional benefits. First, the knowledge gained from such an approach can lead to more targeted apps, which may enhance their efficacy. Second, current evidence suggests that mHealth app engagement in the general public falls to near zero after two weeks 9 . Given this reality, it is key to understand whether the brief periods in which apps tend to be evaluated have any impact on mechanistic targets. If they do not, it will be important to focus efforts on sustaining engagement for longer in the hopes of seeing a substantial impact on these important targets. Third, this approach provides valuable insights for clinicians specializing in evidence-based treatments as many of the mechanisms of mindfulness practice (e.g., emotion regulation) are also the transdiagnostic mechanisms targeted in such therapies 17 , 18 . Therefore, knowledge gained from this approach can aid clinicians in evaluating such apps as potential complements to ongoing treatment goals.
To date, no mindfulness app review of which we are aware has focused on the mechanisms of mindfulness training as outcomes. Thus, a systematic review is warranted to investigate the evidence of mindfulness app effects on the mechanistic processes through which mindfulness training has been demonstrated to influence transdiagnostic symptom change 19 .
This systematic review was conducted according to PRISMA guidelines 20 and registered on the International Platform of Registered Systematic Review and Meta-Analysis Protocols (#202350017). To identify mechanisms of mindfulness practice, we first searched for papers that proposed likely mechanisms based on a thorough rationale. We searched for these papers in Pubmed (using the keywords “mindful*” in the Title field, and “mechanism” or “mediat*” in the Text field). This method yielded four theory papers 21 , 22 , 23 , 24 , from which we extracted the proposed mechanisms. For each proposed mechanism, we then searched the literature for empirical support (obtained through mediation analysis). Our list of theoretically and empirically supported mechanisms of mindfulness practice appears in Table 1 . (For an overview of corresponding theories, see eTable 1 ).
To be included in this review, a study had to (a) be a randomized controlled trial design, (b) evaluate a mindfulness-based mobile app, (c) assess change in one or more of our identified mechanisms using a validated, reliable measure, (d) focus on adults (≥18 years), and be (e) peer-reviewed and (f) written in English. A mindfulness-based app was defined as any app that was designed for the sole purpose of facilitating mindfulness practice. We excluded studies on Web-only or text-based interventions, as we were most interested in apps for their accessibility and scalability. To avoid sample biases, we also excluded studies of non-smartphone technology (e.g., VR, wearables, tablet apps), which are not yet widely adopted. We also excluded studies on adolescents because many mindfulness apps limit use to adults in their terms and conditions, and because some recent evidence suggests that mindfulness practice may affect adolescents differently than it does adults 25 . Finally, regarding validated measures, we made an exception for ecological momentary assessment (EMA) studies, which tend to use few items to reduce participant burden.
An electronic literature search was performed by the first author on October 26, 2022, on Pubmed, APA PsycINFO, and Web of Science. The search was updated on August 7, 2023. (For search strategy, see eTable 2 ). Studies identified were divided among four pairs of reviewers (NM & ZM, NM & TG, NM & ER, NM & SL). Reviewers independently assessed studies based on title and abstract and gave inclusion/exclusion recommendations, which were subsequently compared; any disagreements were resolved through discussion in each pair, consulting JT if consensus could not be reached. The same process was followed for full-text review, data extraction, and quality assessment (QA). The Quality Assessment Tool for Quantitative Studies, which has evidence of validity and reliability 26 , guided the quality assessment process. The tool outlines assessment criteria for eight domains of bias. Overall QA ratings and domain-specific section ratings for each study appear in eTable 3 and eTable 4 , respectively.
The range of clinical and methodological characteristics in the studies included in this review prevented a meta-analysis, and we employed a narrative synthesis of the data. We first grouped studies by thematic similarity. Within each group, we assessed studies by findings, searching for similarities and differences. When findings were contradictory within a group of studies, we examined potential contributors (e.g., differences across studies in sample and study characteristics, such as control group strength, type of app evaluated, and measurement instruments). The results of this process are described in the subsequent sections.
A PRISMA flow diagram summarizing the results of our study selection process appears in eFigure 1 . In total, data was collected from 5963 adults across 28 studies that varied widely in terms of location. The mean age across 23 studies that reported it was ~33 ( SD = 8.98). Only 17 studies described the racial/ethnic composition of the sample; samples were predominantly White, and none were nationally representative. Approximately 79% identified as female (across the 24 studies that reported on female gender) and 19% as male (across the 17 studies that reported on male gender). Only one study reported on sexual orientation. See Table 2 for detailed sample characteristics.
Study characteristics
Studies assessed Headspace ( n = 12), VGZ Mindfulness Coach ( n = 3), Unwinding Anxiety ( n = 2), Healthy Minds Program ( n = 2), Calm ( n = 1), Stop, Breathe & Think ( n = 1), Craving to Quit ( n = 1), MediTrain ( n = 1), Balloon App ( n = 1), REM Volver a Casa ( n = 1), Spirits Healing ( n = 1), Wildflowers ( n = 1), and Mindfulness ( n = 1). These apps are available on both Apple and Android phones, except two: one offered on iPhones only (Mindfulness app 19 ) and one that was commercially available at the time of investigation but now appears to be defunct (Wildflowers app 27 ). (For more details on these apps, see eTable 7 ).
Most studies prescribed a specific dose, or amount, of app-delivered mindfulness practice ( n = 20), ranging from 10 minutes a day ( n = 9), several exercises a day ( n = 5), daily ( n = 3) or weekly ( n = 1), or beginning at 10–20 minutes daily and gradually increasing use ( n = 2). (For more details on app features designed to facilitate mindfulness practice, see eTable 7 ).
All 28 studies had at least one control group. Active control groups tended to be digital in nature, with most involving non-mindfulness apps ( n = 10), one offering a WeChat-based health consultation, one a multimedia stress-related psychoeducation website, and one in-person MBSR. Non-mindfulness apps used to control for cognitive expectancies and attention included emotion self-monitoring apps ( n = 3), cognitive training apps such as the 2048 app and the Peak app ( n = 2), apps delivering other psychological interventions such as behavioral activation and progressive muscle relaxation ( n = 2), a list-making app ( n = 1), a music app ( n = 1), and directions to split time equally among three apps (i.e., Duolingo, Tai Chi app, or logic games) identified in a prior study as matched in cognitive outcome expectancy ( n = 1). Passive control group participants were either waitlisted ( n = 15), offered treatment as usual ( n = 2), or provided with no intervention ( n = 1). See Table 3 .
The average intervention phase lasted ~5.46 weeks ( SD = 2.23). In all studies, participants were asked to train with the mindfulness app on their own (rather than in a controlled lab environment). Outcomes were measured with pre- and post-intervention self-report questionnaires in all studies but three. These three studies used objective behavioral tasks to measure outcomes, with one administering a gamified app remotely 28 and two administering cognitive tasks in a lab environment 27 , 29 . Only 10 studies included follow-up assessments (i.e., assessments taking place at least one month after the end of the intervention period) to examine whether changes in the outcomes of interest to this review were sustained in the long term. (See Table 3 ).
App engagement metrics reported varied widely. Some reported engagement in terms of average number of minutes of app use (total or per day or week), average days practiced, and average number of app sessions/exercises completed (total or per day). As such, it was difficult to determine patterns of engagement across studies. To identify patterns, we grouped studies with similar metrics by intervention length and computed ratios based on the two metrics most often reported. Results indicated that engagement was generally low (see eTable 5 ).
Methodological quality
Overall, study quality was rated as moderate to weak, with all studies having some concerns (see eTable 3 ). Most studies minimized measurement, allocation, and detection bias, as they assessed outcomes with valid and reliable measures or tasks, used appropriate allocation methods, and ensured research staff were blinded to condition. Bias tended to arise in terms of selection, attrition, and lack of attention on minimizing potential confounders. Most studies used self-referred convenience samples from one setting, and attrition rates ranged from moderate (i.e., 21%–40%) to high (i.e., >40%), with an average of 23% (SD = 13%) across studies. Most studies did not adjust for important confounders (see eTable 4 note). In addition, 12 studies were underpowered. Implementation bias was difficult to detect, as most studies did not report the percentage of participants who received the allocated intervention as it was intended (i.e., recommended dose of app use).
Outcomes and findings
Across 28 studies, 67 outcome comparisons were made between the intervention and control group. Of these 67 comparisons, 35 (53%) revealed a between-group difference favoring the intervention group. Of the 35 between-group effects favoring the intervention group, most were found when the mindfulness app was evaluated against a passive ( n = 28; 65%) versus an active ( n = 7; 30%) control group. (Note: Passive, or inactive, control groups involved either waitlisting participants, or offering them treatment as usual or no intervention. Active control groups offered participants a comparable task to engage in, such as a non-mindfulness app.) Effect sizes tended to be moderate to large across domains, and gains from using mindfulness apps were generally sustained at follow-up. (See Table 4 ). Results by outcome domain appear in Table 4 and Fig. 1 .
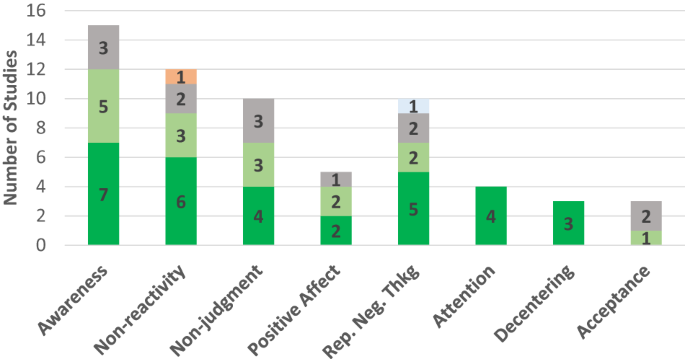
Dark green represents a between-group effect favoring the mindfulness app group; orange represents a between-group effect favoring the control group. Light green denotes studies that found no between-group effect (i.e., both groups improved or within-group effect favoring the mindfulness app group present); gray denotes studies that found no between-group effect (i.e., neither group improved or within-group effect favoring the control group). Light blue represents no between-group effect but unclear whether both or neither group improved. Rep. Neg. Thkg = Repetitive Negative Thinking.
Awareness . The most frequently examined outcome was awareness, assessed in 15 comparisons and measured with the Acting With Awareness subscale of the Five Facet Mindfulness Questionnaire (FFMQ 30 ) 31 , 32 , 33 , 34 , 35 , 36 or of its short-form version (FFMQ-SF 37 ) 38 , 39 , 40 , a one-item measure based on the FFMQ Acting With Awareness subscale in an experience sampling study 41 , the Acceptance subscale of the Philadelphia Mindfulness Scale (PHLMS 42 ) 43 , the Multidimensional Assessment of Interoceptive Awareness (MAIA 44 ) 45 , or the Interoceptive Respiration Task 27 . Findings were mixed, with about half the studies ( n = 7) finding an effect favoring the intervention group (small to large effect sizes), five finding that both groups improved, and three that neither improved. Studies that found an effect favoring the intervention (versus those that did not) used passive control groups and tended to have samples with a greater female composition (see eTable 6 ). The four studies that used active control groups found that either both groups improved 39 , 41 or neither did 27 , 36 .
Nonreactivity was assessed in 12 comparisons and measured with the nonreactivity subscale of the Five Facet Mindfulness Questionnaire (FFMQ 31 ) in all but two studies that instead used the nonreactivity subscale from its 24-item short-form version (FFMQ-SF 37 ) 38 , 40 . Findings were mixed, with six comparisons yielding an effect favoring the mindfulness app (medium to large effect sizes) 34 , 35 , 38 , 39 , 45 , 46 , three showing that both groups improved 33 , 39 , 40 , two that neither did 36 , 40 , and one yielding an effect favoring the control group 30 . All six comparisons that yielded an effect favoring the mindfulness app were made with passive control groups and tended to have samples with a greater female composition. Two studies that used active control groups found that either both groups improved 39 or neither did 36 . The study finding an effect favoring the control group had a very small sample size and was underpowered 30 . No consistent associations between intervention length and outcomes were apparent across studies.
Non-judgment was assessed in 10 comparisons, using the non-judging of inner experience subscale from either the Five Facet Mindfulness Questionnaire (FFMQ 31 ) or its short-form version (FFMQ-SF 37 ). Findings were mixed, with four finding an effect favoring the mindfulness app 30 , 34 , 35 , 39 , three that both groups improved 36 , 39 , 40 , and three that neither improved 33 , 40 , 47 . Only two studies used active control groups, both finding that both groups improved 36 , 39 .
Positive affect was examined in five studies and measured with the Positive and Negative Affect Scale 48 , 49 or one-item measures in EMA studies 36 , 50 , 51 . Findings were mixed, with two finding an effect favoring the intervention group 48 , 49 , two that both groups improved 36 , 51 , and one that neither group improved. 52 All five studies used an active control group, although in two, control groups were non-equivalent 48 , 52 . Two of the three that found no between-group differences were underpowered 51 , 52 , and in one, the intervention app dose varied across participants, with some receiving it for 40 days and some for 60 51 . The two studies that found a between-group difference had samples with a greater female composition.
Repetitive negative thinking . Ten comparisons assessed repetitive negative thinking styles, including worry ( n = 7), perseverative thinking ( n = 2), and rumination ( n = 1). Worry was assessed with the Penn State Worry Questionnaire. Three studies found an effect favoring the intervention group, with small to large effect sizes 45 , 46 , 53 , and one of these had an active control group 53 . Two studies that found that neither group improved were underpowered 52 , 54 . Studies that found a between-group difference (versus none) had samples with a greater female composition.
Two studies examined perseverative thinking 32 , 55 , assessing it with the Perseverative Thinking Questionnaire (PTQ 56 ), a measure of both worry and rumination, and using a waitlist control group. Both studies found an effect favoring the mindfulness app. Only one study examined rumination directly 53 , measuring it with the brooding subscale of the Ruminative Response Scale (RRS 57 ); no significant between-group differences were found.
Attention regulation was evaluated in only three studies (that yielded four group comparisons) and measured with behavioral tasks, including the Centre for Research on Safe Driving-Attention Network Test (CRSD-ANT 58 ) 27 , which is a validated briefer version of the Attention Network Test (ANT 59 ); the validated sustained attention task Test of Variables of Attention (TOVA 60 ) 29 ; and a gamified sustained attention task (“Go Sushi Go”) 28 based on the validated Sustained Attention to Response Task (SART 61 ). All four yielded an effect favoring the intervention group, with effect sizes ranging from small to large. All studies used an active control group.
Decentering/defusion was examined in three studies. Two 32 , 55 used the Drexel Defusion Scale 62 and one 36 the decentering subscale of the Toronto Mindfulness Scale 63 . All three found a between-group difference favoring the intervention group; one had an active control group 36 .
Acceptance/psychological flexibility was examined in three studies and measured with the acceptance subscale of the Philadelphia Mindfulness Scale (PHLMS 64 ) 43 , or with the English 65 or Dutch 52 version of the Acceptance and Action Questionnaire—II (AAQ-II 66 ). No between-group differences were found; one study that used an active control group of a behavioral activation app found that both groups improved 65 . Two other studies found that neither group improved 43 , 52 , although one was underpowered 52 .
Finally, only one study each examined self-regulation, reappraisal, suppression, values , and extinction , with one study examining the first three against a waitlist control group 67 using the Self-Regulation Scale 68 and the German version of the Emotion Regulation Questionnaire 69 . This study found a between-group effect favoring the app group for self-regulation and reappraisal, but not suppression. One study assessed behavioral enactment of values 30 with the Valuing Questionnaire 70 and used a waitlist control group; results favored the intervention over the control group. The study that examined extinction 71 used a two-day lab-based aversive Pavlovian conditioning and extinction procedure and a waitlist control group. Results showed that after using the mindfulness app for 4 weeks, the intervention (versus waitlist control) group had greater retention of extinction learning, as demonstrated by less spontaneous recovery of conditioned threat responses one day after extinction training.
Mediation analysis
Only two studies conducted mediation analysis with a psychological disorder as an outcome. One study found that worry partially mediated the relationship between mindfulness practice and anxiety 45 and the other that worry fully mediated the association between mindfulness training and worry-related sleep disturbance 46 .
Heterogeneity & certainty of evidence
The range of populations in which apps were evaluated and inconsistent app engagement likely contributed to heterogeneity in findings. Methodological quality was also a likely contributor to inconsistent findings, as quality was moderate to low across studies. In the awareness domain, for example, of studies that found no between-group differences, one was underpowered, 27 one used a single-item measure that did not correlate highly with the full measure 41 , another had a 45% dropout rate 39 , and in another, data came from only 4% of eligible patients who enrolled 43 . Such methodological weaknesses, found across domains, likely increased the heterogeneity of findings and lower confidence that the lack of effects was due to a lack of app efficacy.
Methodological weaknesses also lower the certainty of evidence in domains with more consistent findings. In most domains, when effects favoring the mindfulness apps were found, most or all were from studies with passive, rather than active, control groups. In only two domains did all studies use active control groups: positive affect and attention regulation. However, in the positive affect domain, studies finding an effect favoring the mindfulness app group had relatively high attrition rates (38% and 35%), lowering confidence in findings. (For context, the average attrition rate in a recent meta-analysis of mHealth studies was 24%; 72 objectively, attrition rates of up to 20% are considered ideal, and those nearing 40% are deemed to be high as they risk introducing bias 26 ).
The domain of attention regulation was the strongest set of studies. All studies in this domain employed not just an active digital control group but also objective task measures to assess outcomes, increasing the certainty of evidence, although more studies are needed in this domain.
This systematic review identified 28 RCTs that evaluated a mindfulness app and examined as an outcome at least one theoretically and empirically supported mechanism of mindfulness practice. By focusing on mechanisms, this review aimed to provide a more nuanced understanding of the psychological impact of mindfulness apps. Overall, more research is needed in most outcome domains assessed in this review. Effects tended to favor the mindfulness app (versus control) group in the domains of attention regulation, repetitive negative thinking, and decentering/defusion, and findings were mixed in the domains of awareness, nonreactivity, non-judgment, positive affect, and acceptance/psychological flexibility. Various methodological issues, population characteristics, and app engagement problems likely contributed to the heterogeneity of findings.
The attention regulation domain was the strongest set of research studies. Results favoring the mindfulness app group in this domain are promising and consistent with other findings suggesting that in-person MBIs have positive effects on executive function 73 , 74 . They are also consistent with other study findings suggesting that those with (versus without) meditation experience exhibit greater cognitive flexibility 75 .
A trend that became apparent across most sets of studies is that studies with more female participants tended to more consistently find effects favoring the mindfulness app group. This trend is in line with other recent findings suggesting that females (versus males) may benefit more from mindfulness-based interventions 14 , 76 , 77 , 78 . Some have suggested that this difference may be due to the fact that mindfulness targets rumination, a problematic emotion regulation strategy more often used by females than males; in contrast, men tend to more often use distraction, and the focus on the present-moment experience that mindfulness training requires may initially increase negative affect for men 76 . Based on this finding, more research into these potential gender differences is warranted. If this finding is indeed replicated, gender-specific modifications in app delivery for males (e.g., emphasis on non-judgmental observation of experience) may be beneficial.
Another likely moderator of mixed findings was app engagement. Engagement metrics reported across studies varied widely, and it was difficult to assess overall engagement across the majority of studies. From the available metrics, however, engagement appeared to be generally low. The lack of consensus on engagement metrics is a recognized challenge in the mHealth space 79 , 80 , as is the difficulty sustaining engagement over time 81 . Notably, some studies that found no between-group differences found a mindfulness app effect at higher engagement rates 38 , 40 . Such findings are in line with evidence of a dose-response relationship between home practice and outcomes in in-person MBIs, which also demonstrate problems with adherence to at-home mindfulness practice, as data suggests that MBI participants complete, on average, only about 64% of the assigned amount of home practice 5 . This nevertheless amounts to a much higher rate of daily practice than seen in the studies of mindfulness apps in this review, underscoring the importance of incorporating strategies to increase app engagement so that the efficacy of these apps can be better evaluated.
It is also worth noting two other potential contributors to heterogeneity that relate to broader issues in the field. There is a lack of consensus on the definition of mindfulness, and the resulting diverse mindfulness conceptualizations 82 may lead to different teams emphasizing different aspects of mindfulness practice during intervention implementation—differences that may have contributed to heterogeneity in outcomes. In addition, despite more mechanism-driven research into in-person MBIs over the past decade, these mechanisms are not yet well understood 83 , with some leading mindfulness mechanism theories at times yielding mixed support 84 . A better understanding of the transdiagnostic factors through which in-person MBIs impact change in mental health outcomes will lead not just to more refined mHealth interventions but also stronger evidence for the theories informing these interventions.
Limitations of body of evidence and future directions
To advance this literature, we propose several future directions and research recommendations. First, future studies replicating these findings should employ strategies that foster app engagement. Sustained app engagement is key to obtaining accurate estimates of apps’ impact on various outcomes. In addition, although the use of incentives is acceptable in (and in line with the goals of) earlier stages of research, it is not a scalable strategy for real-world dissemination. Selecting theory-based strategies (e.g., goal-setting features, support) and building them into an app’s design, even in earlier stages of research, paves the way toward creating efficacious apps that have a greater likelihood of successful dissemination.
Related, more fine-grained details on app engagement would likely aid in resolving some of the inconsistent findings. Even mindfulness apps have a variety of features, some of which do not necessarily strengthen practice (e.g., soothing sounds or music that several apps offered, as seen in eTable 7 ). Better understanding how participants were using apps could help clarify why app use, in some cases, was less impactful. In addition, some people stop engaging with apps as they achieve their mental health goals, a phenomenon referred to in the literature as “e-attainment.” 85 Thus, in some cases, discontinuation could be associated with positive outcomes, as some may have stopped using the app because mindfulness practice became a part of their routines. Thus, assessing reasons for app discontinuation can also help clarify inconsistent outcomes.
Second, future studies should better control for digital placebo effects. Many of the studies that found app effects used passive control groups, which provides encouraging evidence but does not rule out the possibility that improvements were due to simply using an app rather than to the mindfulness-specific aspects of the app. At the same time, active control groups should be chosen with careful consideration. For example, one study used a progressive muscle relaxation app as an active control and found no between-group differences in positive affect 51 . This finding may be expected, however, as relaxation has also been found to increase positive affect 86 .
Third, future studies should carefully consider the measurement of mindfulness-related constructs. There is growing concern that the conceptualization of mindfulness—and thus its measurement—is culturally biased, with some evidence suggesting that such widely used measures as the FFMQ may not actually perform well in non-Western populations 87 . Without this awareness, researchers risk continuing to build a body of evidence based on mindfulness definitions that are not necessarily universally accessible. Fortunately, alternative, more culturally relevant measures are starting to be developed 88 . In addition, although objective outcome measures are often not widely available, when they are, they should be used in future studies. Some examples of objective outcome measures include app-based cognitive games that are gamified versions of validated neuropsychological paradigms 28 , implicit tasks (e.g., the IPANAT for positive affect 89 ), wearables to measure physiological reactivity (which, when combined with self-reported arousal, can be a measure of experiential avoidance 90 ), or rumination induction tasks 91 to assess whether participants who have been practicing mindfulness more are better able to exit such repetitive negative thinking states. Confidence in findings from self-report measures can be strengthened by the addition of objective measures.
With respect to study population, future studies should evaluate apps in nationally representative samples to increase the generalizability of findings. However, studies should also continue to evaluate apps in specific populations but test population-specific, theory-driven hypotheses about specific mechanisms most pertinent to that population. Doing so can help inform ways to tailor app delivery to each population to better target mechanisms. Related, greater empirical focus is needed on evaluating mindfulness apps in minoritized populations, who continue to be underrepresented in mHealth research 92 —a trend that also became apparent in the studies included in this review. Some evidence suggests that being African American is associated with lower odds of accessing and continuing to use a leading commercially available mindfulness app 93 , and lower educational attainment is also associated with lower odds of app access 93 . It is critical that future research studies focus on minoritized populations to avoid perpetuating disparities and introducing new ones in the form of digital inequities.
In addition, most studies did not report on implementation details, including details on how mindfulness was explained to participants. Yet how an intervention is introduced affects engagement and outcomes 94 , 95 , and calls have been made for mindfulness intervention studies to report on the explicit instruction given to participants regarding mindfulness 82 . This is especially important, given evidence that core aspects of mindfulness practice are often misunderstood by the general public 96 and given the different conceptualizations of mindfulness 82 that may lead to differences in intervention design and implementation. Better reporting on instruction details may elucidate some heterogeneity in findings. Researchers can also focus on other aspects of delivery beyond instructions, such as tailoring recommendations regarding timing and practice. For example, in samples of socioeconomically disadvantaged individuals facing multiple daily stressors, special attention could be placed on creating a tailored practice schedule. This discussion would help integrate mindfulness practice into their daily routine and better relate the practice to their specific challenges (e.g., constant worry regarding financial strain). This strategy may increase app relevance to each population’s contextual factors and heighten the app’s impact on hypothesized mechanisms.
Finally, moderators should be conceptualized and measured. While heterogeneity is often viewed as a signal of low efficacy, it is, in fact, normal and expected 97 . Aside from main and mediating effects, it is also important to consider when and for whom app effects are strengthened or weakened. Population-specific moderator hypotheses can relate to technology (e.g., app features), the individual (e.g., beliefs about technology), and their context (e.g., app integration into lifestyle). Special consideration should be paid to gender differences to increase our understanding of how gender influences mindfulness app outcomes. Overall, there has been little empirical focus on individual differences in the broader MBI literature too 98 , a gap that needs to be addressed in both of these areas of research.
Guidance for clinicians: integrating apps into care
Although this review focuses on mindfulness apps’ clinical foundation, it is important to note that evidence of efficacy is just one of the five factors clinicians need to consider when selecting apps to recommend to patients. The other four factors are described in the APA app evaluation model 99 , a framework for helping clinicians choose suitable apps: accessibility (e.g., app cost, offline features), privacy and safety (i.e., data protection), app usability, and data integration toward the therapeutic goal (e.g., can app data be easily shared with the provider?) 99 . To ease the process of evaluating these factors, clinicians can use an app database, such as mindapps.org, a constantly updated database designed to make the APA framework easily actionable for public use. Using such tools can leave clinicians empowered to integrate mindfulness apps that may improve outcomes into care.
Limitations
Several limitations of this review are worth noting. First, we did not extend the search into gray literature, which may bias results to only published evidence. Second, despite efforts to be inclusive of mindfulness mechanisms, we neglected to include self-compassion, one mechanism that has also been theoretically and empirically supported 100 . Future research should extend the focus on this important potential intermediary outcome of mindfulness app use. Third, our review did not focus on SMS-based interventions, which are also promising digital mental health tools that can enhance the impact of MBIs 101 and thus warrant future empirical attention. Finally, given that our research question focused on discrete mechanistic targets that theories suggest would change after the onset of mindfulness practice, we excluded studies that only reported on composite measures of mindfulness (e.g., FFMQ, MAAS). Given that these scales measured several of our constructs of interest together, they were deemed out of the scope of this review. Although this limitation was partially addressed by a recent meta-analysis on composite measures of mindfulness as an outcome of mindfulness app interventions 14 , whether included studies examined mindfulness as a mechanism was not reported. Thus, a future review on this topic may be potentially fruitful.
Mindfulness-based mobile apps can not only enhance mental health treatment but also offer scalable solutions to address barriers to in-person MBI access. The literature on the psychological impact of mindfulness apps is still nascent and suggests that mindfulness-based apps are promising, especially for regulating attention, reducing repetitive negative thinking, and promoting decentering/defusion. Continuing to elucidate mindfulness apps’ impact on processes of change that account for transdiagnostic symptom reduction is crucial in optimizing app design to enhance app efficacy and truly realize the potential of these apps as viable complements to routine care.
Data availability
While most of the data generated during this study are included in this published article, additional data on outcome measures and app engagement metrics extracted from each study is available from the corresponding author upon request.
Creswell, J. D. Mindfulness interventions. Annu. Rev. Psychol. 68 , 491–516 (2017).
Article PubMed Google Scholar
Hoge, E. A. et al. Mindfulness-based stress reduction vs escitalopram for the treatment of adults with anxiety disorders: a randomized clinical trial. JAMA Psychiatry 80 , 13–21 (2023).
Wilhelm, S. et al. Efficacy of app-based cognitive behavioral therapy for body dysmorphic disorder with coach support: initial randomized controlled clinical trial. Psychother. Psychosom. 91 , 277–285 (2022).
Harvey, A. G. & Gumport, N. B. Evidence-based psychological treatments for mental disorders: modifiable barriers to access and possible solutions. Behav. Res. Ther. 68 , 1–12 (2015).
Article PubMed PubMed Central Google Scholar
Parsons, C. E., Crane, C., Parsons, L. J., Fjorback, L. O. & Kuyken, W. Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: a systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav. Res. Ther. 95 , 29–41 (2017).
Ben-Zeev, D., Buck, B., Meller, S., Hudenko, W. J. & Hallgren, K. A. Augmenting evidence-based care with a texting mobile interventionist: pilot randomized controlled trial. Psychiatr. Serv. 71 , 1218–1224 (2020).
Austin, S. F., Jansen, J. E., Petersen, C. J., Jensen, R. & Simonsen, E. Mobile app integration into dialectical behavior therapy for persons with borderline personality disorder: qualitative and quantitative study. JMIR Ment. Health 7 , e14913 (2020).
Schultchen, D. et al. Stay present with your phone: a systematic review and standardized rating of mindfulness apps in european app stores. Int.J. Behav. Med. 28 , 552–560 (2021).
Baumel, A., Muench, F., Edan, S. & Kane, J. M. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J. Med. Internet Res. 21 , e14567 (2019).
Schueller, S. M., Washburn, J. J. & Price, M. Exploring mental health providers’ interest in using web and mobile-based tools in their practices. Internet Interv. 4 , 145–151 (2016).
Noel, V. A., Acquilano, S. C., Carpenter-Song, E. & Drake, R. E. Use of mobile and computer devices to support recovery in people with serious mental illness: survey study. JMIR Ment. Health 6 , e12255 (2019).
Torous, J., Friedman, R. & Keshavan, M. Smartphone ownership and interest in mobile applications to monitor symptoms of mental health conditions. JMIR mHealth and uHealth 2 , e2994 (2014).
Google Scholar
Morton, E., Torous, J., Murray, G. & Michalak, E. E. Using apps for bipolar disorder—an online survey of healthcare provider perspectives and practices. J. Psychiatr. Res. 137 , 22–28 (2021).
Tan, Z. Y. A., Wong, S. H., Cheng, L. J. & Lau, S. T. Effectiveness of mobile-based mindfulness interventions in improving mindfulness skills and psychological outcomes for adults: a systematic review and meta-regression. Mindfulness 13 , 2379–2395 (2022).
Article Google Scholar
Gal, E., Stefan, S. & Cristea, I. The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: a meta-analysis of randomized controlled trials. J. Affect. Disord. 279 , 131–142 (2021).
Kazdin, A. E. Mediators and mechanisms of change in psychotherapy research. Annu. Rev. Clin. Psychol. 3 , 1–27 (2007).
Linehan, M. M. Cognitive-behavioral treatment of borderline personality disorder. xvii, 558 (Guilford Press, 1993).
Farchione, T. J. et al. Unified protocol for transdiagnostic treatment of emotional disorders: a randomized controlled trial. Behav. Ther. 43 , 666–678 (2012).
Gu, J., Strauss, C., Bond, R. & Cavanagh, K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol. Rev. 37 , 1–12 (2015).
Article CAS PubMed Google Scholar
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann. Intern. Med. 151 , W–65 (2009).
Shapiro, S. L., Carlson, L. E., Astin, J. A. & Freedman, B. Mechanisms of mindfulness. J. Clin. Psychol. 62 , 373–386 (2006).
Hölzel, B. K. et al. How does mindfulness meditation work? proposing mechanisms of action from a conceptual and neural perspective. Perspect. Psychol. Sci. 6 , 537–559 (2011).
Garland, E. L., Farb, N. A., R. Goldin, P. & Fredrickson, B. L. Mindfulness broadens awareness and builds eudaimonic meaning: a process model of mindful positive emotion regulation. Psychol. Inq. 26 , 293–314 (2015).
Lindsay, E. K. & Creswell, J. D. Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clin. Psychol. Rev. 51 , 48–59 (2017).
Yuan, J. P. et al. Gray matter changes in adolescents participating in a meditation training. Front. Hum. Neurosci. 14 , 319 (2020).
Thomas, B. H., Ciliska, D., Dobbins, M. & Micucci, S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid. Based Nurs. 1 , 176–184 (2004).
Walsh, K. M., Saab, B. J. & Farb, N. A. Effects of a mindfulness meditation app on subjective well-being: active randomized controlled trial and experience sampling study. JMIR Ment. Health 6 , e10844 (2019).
Axelsen, J. L., Meline, J. S. J., Staiano, W. & Kirk, U. Mindfulness and music interventions in the workplace: assessment of sustained attention and working memory using a crowdsourcing approach. BMC Psychol. 10 , 108 (2022).
Ziegler, D. A. et al. Closed-loop digital meditation improves sustained attention in young adults. Nat. Hum. Behav. 3 , 746–757 (2019).
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J. & Toney, L. Using self-report assessment methods to explore facets of mindfulness. Assessment 13 , 27–45 (2006).
Levin, M. E., Hicks, E. T. & Krafft, J. Pilot evaluation of the stop, breathe & think mindfulness app for student clients on a college counseling center waitlist. J. Am. Coll. Health 70 , 165–173 (2022).
Hirshberg, M. J. et al. A randomized controlled trial of a smartphone-based well-being training in public school system employees during the COVID-19 pandemic. J. Educ. Psychol. 114 , 1895–1911 (2022).
Yang, E., Schamber, E., Meyer, R. M. L. & Gold, J. I. Happier healers: randomized controlled trial of mobile mindfulness for stress management. J. Altern. Complement. Med. 24 , 505–513 (2018).
van Emmerik, A. A. P., Berings, F. & Lancee, J. Efficacy of a mindfulness-based mobile application: a randomized waiting-list controlled trial. Mindfulness 9 , 187–198 (2018).
Huberty, J. et al. Efficacy of the mindfulness meditation mobile app “calm” to reduce stress among college students: randomized controlled trial. JMIR Mhealth Uhealth 7 , e14273 (2019).
Haliwa, I., Ford, C. G., Wilson, J. M. & Shook, N. J. A mixed-method assessment of a 10-day mobile mindfulness intervention. Front. Psychol. 12 , 722995 (2021).
Bohlmeijer, E., ten Klooster, P. M., Fledderus, M., Veehof, M. & Baer, R. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment 18 , 308–320 (2011).
Rich, R. M., Ogden, J. & Morison, L. A randomized controlled trial of an app-delivered mindfulness program among university employees: effects on stress and work-related outcomes. IJWHM 14 , 201–216 (2021).
Orosa-Duarte, Á. et al. Mindfulness-based mobile app reduces anxiety and increases self-compassion in healthcare students: a randomised controlled trial. Med. Teach. 43 , 686–693 (2021).
Kubo, A. et al. A randomized controlled trial of mhealth mindfulness intervention for cancer patients and informal cancer caregivers: a feasibility study within an integrated health care delivery system. Integr. Cancer Ther. 18 , 153473541985063 (2019).
Sala, M., Roos, C. R., Brewer, J. A. & Garrison, K. A. Awareness, affect, and craving during smoking cessation: an experience sampling study. Health Psychol. 40 , 578–586 (2021).
Bishop, S. R. et al. Mindfulness: a proposed operational definition. Clin. Psychol. Sci. Pract. 11 , 230–241 (2004).
Ainsworth, B. et al. A feasibility trial of a digital mindfulness-based intervention to improve asthma-related quality of life for primary care patients with asthma. J. Behav. Med. 45 , 133–147 (2022).
Mehling, W. E. et al. The multidimensional assessment of interoceptive awareness (MAIA). PLoS One 7 , e48230 (2012).
Article ADS CAS PubMed PubMed Central Google Scholar
Roy, A. et al. Clinical efficacy and psychological mechanisms of an app-based digital therapeutic for generalized anxiety disorder: randomized controlled trial. J. Med. Internet Res. 23 , e26987 (2021).
Gao, M. et al. Targeting anxiety to improve sleep disturbance: a randomized clinical trial of app-based mindfulness training. Psychosom. Med. 84 , 632–642 (2022).
Rich, A. et al. Evaluation of a novel intervention to reduce burnout in doctors-in-training using self-care and digital wellbeing strategies: a mixed-methods pilot. BMC Med. Educ. 20 , 294 (2020).
Sun, Y. et al. Effectiveness of smartphone-based mindfulness training on maternal perinatal depression: randomized controlled trial. J. Med. Internet Res. 23 , e23410 (2021).
Howells, A., Ivtzan, I. & Eiroa-Orosa, F. J. Putting the ‘app’ in happiness: a randomised controlled trial of a smartphone-based mindfulness intervention to enhance wellbeing. J. Happiness Stud. 17 , 163–185 (2016).
Versluis, A., Verkuil, B., Spinhoven, P., Brosschot, F. & Effectiveness, J. of a smartphone-based worry-reduction training for stress reduction: a randomized-controlled trial. Psychol. Health 33 , 1079–1099 (2018).
Low, T., Conduit, R., Varma, P., Meaklim, H. & Jackson, M. L. Treating subclinical and clinical symptoms of insomnia with a mindfulness-based smartphone application: a pilot study. Internet Interv. 21 , 100335 (2020).
Versluis, A., Verkuil, B., Spinhoven, P. & Brosschot, J. F. Feasibility and effectiveness of a worry-reduction training using the smartphone: a pilot randomised controlled trial. Br. J. Guid. Counc. 48 , 227–239 (2020).
Taylor, H., Cavanagh, K., Field, A. P. & Strauss, C. Health care workers’ need for headspace: findings from a multisite definitive randomized controlled trial of an unguided digital mindfulness-based self-help app to reduce healthcare worker stress. JMIR Mhealth Uhealth 10 , e31744 (2022).
Abbott, D., Lack, C. W. & Anderson, P. Does using a mindfulness app reduce anxiety and worry? a randomized-controlled trial. J. Cogn. Psychother. 37 , 26–42 (2023).
Goldberg, S. B. et al. Testing the efficacy of a multicomponent, self-guided, smartphone-based meditation app: three-armed randomized controlled trial. JMIR Ment. Health 7 , e23825 (2020).
Ehring, T. et al. The perseverative thinking questionnaire (PTQ): validation of a content-independent measure of repetitive negative thinking. J. Behav. Ther. Exp. Psychiatry 42 , 225–232 (2011).
Nolen-Hoeksema, S. & Morrow, J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta earthquake. J. Pers. Soc. Psychol. 61 , 115–121 (1991).
Weaver, B., Bédard, M. & McAuliffe, J. Evaluation of a 10-minute version of the attention network test. Clin. Neuropsychol. 27 , 1281–1299 (2013).
Fan, J., McCandliss, B. D., Sommer, T., Raz, A. & Posner, M. I. Testing the efficiency and independence of attentional networks. J. Cogn. Neurosci. 14 , 340–347 (2002).
Greenberg, L. M. TOVA continuous performance test manual (The TOVA Company, 1996).
Robertson, I. H., Manly, T., Andrade, J., Baddeley, B. T. & Yiend, J. ‘Oops!’: performance correlates of everyday attentional failures in traumatic brain injured and normal subjects. Neuropsychologia 35 , 747–758 (1997).
Forman, E. M. et al. The Drexel defusion scale: a new measure of experiential distancing. J. Context. Behav. Sci. 1 , 55–65 (2012).
Lau, M. A. et al. The toronto mindfulness scale: development and validation. J. Clin. Psychol. 62 , 1445–1467 (2006).
Cardaciotto, L., Herbert, J. D., Forman, E. M., Moitra, E. & Farrow, V. The assessment of present-moment awareness and acceptance: the philadelphia mindfulness scale. Assessment 15 , 204–223 (2008).
Ly, K. H. et al. Behavioural activation versus mindfulness-based guided self-help treatment administered through a smartphone application: a randomised controlled trial. BMJ Open 4 , e003440 (2014).
Bond, F. W. et al. Preliminary psychometric properties of the acceptance and action questionnaire–ii: a revised measure of psychological inflexibility and experiential avoidance. Behav. Ther. 42 , 676–688 (2011).
Schulte‐Frankenfeld, P. M. & Trautwein, F. App‐based mindfulness meditation reduces perceived stress and improves self‐regulation in working university students: a randomised controlled trial. Appl. Psychol. Health Well Being 14 , 1151–1171 (2022).
Diehl, M., Semegon, A. B. & Schwarzer, R. Assessing attention control in goal pursuit: a component of dispositional self-regulation. J. Pers. Assess. 86 , 306–317 (2006).
Abler, B. & Kessler, H. ERQ - emotion regulation questionnaire - deutsche Fassung. https://doi.org/10.23668/psycharchives.402 (2011).
Smout, M., Davies, M., Burns, N. & Christie, A. Development of the valuing questionnaire (VQ). J. Context. Behav. Sci. 3 , 164–172 (2014).
Bjorkstrand, J. et al. The effect of mindfulness training on extinction retention. Sci. Rep. 9 , 19896 (2019).
Linardon, J. & Fuller-Tyszkiewicz, M. Attrition and adherence in smartphone-delivered interventions for mental health problems: a systematic and meta-analytic review. J. Consult. Clin. Psychol. 88 , 1–13 (2020).
Tang, Y.-Y. et al. Short-term meditation training improves attention and self-regulation. Proc. Natl. Acad. Sci. 104 , 17152–17156 (2007).
Zeidan, F., Johnson, S. K., Diamond, B. J., David, Z. & Goolkasian, P. Mindfulness meditation improves cognition: evidence of brief mental training. Conscious. Cogn. 19 , 597–605 (2010).
Hodgins, H. S. & Adair, K. C. Attentional processes and meditation. Conscious. Cogn. 19 , 872–878 (2010).
Rojiani, R., Santoyo, J. F., Rahrig, H., Roth, H. D. & Britton, W. B. Women benefit more than men in response to college-based meditation training. Front. Psychol. 20 , 551 (2017).
de Vibe, M. et al. Mindfulness training for stress management: a randomised controlled study of medical and psychology students. BMC Med. Educ. 13 , 107 (2013).
Roos, C. R., Stein, E., Bowen, S. & Witkiewitz, K. Individual gender and group gender composition as predictors of differential benefit from mindfulness-based relapse prevention for substance use disorders. Mindfulness 10 , 1560–1567 (2019).
Lipschitz, J. M. et al. Digital mental health interventions for depression: scoping review of user engagement. J. Med. Internet Res. 24 , e39204 (2022).
Ng, M. M., Firth, J., Minen, M. & Torous, J. User engagement in mental health apps: a review of measurement, reporting, and validity. Psychiatr. Serv 70 , 538–544 (2019).
Amagai, S., Pila, S., Kaat, A. J., Nowinski, C. J. & Gershon, R. C. Challenges in participant engagement and retention using mobile health apps: literature review. J. Med. Internet Res. 24 , e35120 (2022).
Van Dam, N. T. et al. Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect. Psychol. Sci. 13 , 36–61 (2018).
Alsubaie, M. et al. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin. Psychol. Rev. 55 , 74–91 (2017).
Simione, L., Raffone, A. & Mirolli, M. Acceptance, and not its interaction with attention monitoring, increases psychological well-being: Testing the monitor and acceptance theory of mindfulness. Mindfulness 12 , 1398–1411 (2021).
Sanatkar, S. et al. Using cluster analysis to explore engagement and e-attainment as emergent behavior in electronic mental health. J. Med. Internet Res. 21 , e14728 (2019).
Unger, C. A., Busse, D. & Yim, I. S. The effect of guided relaxation on cortisol and affect: stress reactivity as a moderator. J. Health Psychol. 22 , 29–38 (2017).
Karl, J. A. et al. The cross-cultural validity of the five-facet mindfulness questionnaire across 16 countries. Mindfulness 11 , 1226–1237 (2020).
Ng, S. & Wang, Q. Measuring mindfulness grounded in the original Buddha’s discourses on meditation practice. In: Assessing Spirituality in a Diverse World (eds. Ai, A. L., Wink, P., Paloutzian, R. F. & Harris, K. A.) 355–381 (Springer International Publishing, 2021). https://doi.org/10.1007/978-3-030-52140-0_15 .
Quirin, M., Kazén, M. & Kuhl, J. When nonsense sounds happy or helpless: the implicit positive and negative affect test (IPANAT). J. Pers. Soc. Psychol. 97 , 500–516 (2009).
Leonidou, C. & Panayiotou, G. Can we predict experiential avoidance by measuring subjective and physiological emotional arousal? Curr. Psychol. 41 , 1–13 (2021).
Hilt, L. M. & Pollak, S. D. Getting out of rumination: comparison of three brief interventions in a sample of youth. J. Abnorm. Child Psychol. 40 , 1157–1165 (2012).
Adu-Brimpong, J., Pugh, J., Darko, D. A. & Shieh, L. Examining diversity in digital therapeutics clinical trials: descriptive analysis. J. Med. Internet Res. 25 , e37447 (2023).
Jiwani, Z. et al. Examining equity in access and utilization of a freely available meditation app. npj Ment. Health Res. 2 , 10 (2023).
Breitenstein, S. M. et al. Implementation fidelity in community-based interventions. Res. Nurs. Health 33 , 164–173 (2010).
Borghouts, J. et al. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. J. Med. Internet Res. 23 , e24387 (2021).
Choi, E., Farb, N., Pogrebtsova, E., Gruman, J. & Grossmann, I. What do people mean when they talk about mindfulness? Clin. Psychol. Rev. 89 , 102085 (2021).
Bryan, C. J., Tipton, E. & Yeager, D. S. Behavioural science is unlikely to change the world without a heterogeneity revolution. Nat. Hum. Behav. 5 , 980–989 (2021).
Farias, M., Wikholm, C. & Delmonte, R. What is mindfulness-based therapy good for?. Lancet Psychiatry 3 , 1012–1013 (2016).
Lagan, S. et al. Actionable health app evaluation: translating expert frameworks into objective metrics. npj Digit. Med. 3 , 1–8 (2020).
Baer, R. A. Self-compassion as a mechanism of change in mindfulness- and acceptance-based treatments. in Assessing mindfulness and acceptance processes in clients: Illuminating the theory and practice of change 135–153 (Context Press/New Harbinger Publications, 2010).
Watson, T., Simpson, S. & Hughes, C. Text messaging interventions for individuals with mental health disorders including substance use: a systematic review. Psychiatry Res. 243 , 255–262 (2016).
Download references
Author information
Authors and affiliations.
Beth Israel Deaconess Medical Center & Harvard Medical School, Boston, MA, USA
Natalia Macrynikola, Gloria Yeh & John Torous
Teacher’s College, Columbia University, New York, NY, USA
Hunter College, City University of New York, New York, NY, USA
Tishmattie Gopal
Northeastern University, Boston, MA, USA
Erica Rodriguez & Sunnie Li
Penn State College of Medicine, Hershey, PA, USA
You can also search for this author in PubMed Google Scholar
Contributions
N.M. conceptualized the review, led each part of the process of the review (i.e., screening, full-text review, data extraction, QA), and wrote and edited substantial portions of the manuscript. Z.M., T.G., E.R., S.L., and M.C. were involved in screening, full-text review, data extraction, QA, writing, and editing. G.Y. provided consultation and editing to the manuscript. J.T. contributed to the review conceptualization, consulted on all parts of the review process, and edited the manuscript. All authors read and approved the final version of the manuscript. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Corresponding author
Correspondence to Natalia Macrynikola .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Esupplement, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Macrynikola, N., Mir, Z., Gopal, T. et al. The impact of mindfulness apps on psychological processes of change: a systematic review. npj Mental Health Res 3 , 14 (2024). https://doi.org/10.1038/s44184-023-00048-5
Download citation
Received : 26 May 2023
Accepted : 08 December 2023
Published : 18 March 2024
DOI : https://doi.org/10.1038/s44184-023-00048-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 01 December 2023
Compassion fatigue in healthcare providers: a scoping review
- Anna Garnett 1 ,
- Lucy Hui 2 ,
- Christina Oleynikov 1 &
- Sheila Boamah 3
BMC Health Services Research volume 23 , Article number: 1336 ( 2023 ) Cite this article
2539 Accesses
2 Altmetric
Metrics details
The detrimental impacts of COVID-19 on healthcare providers’ psychological health and well-being continue to affect their professional roles and activities, leading to compassion fatigue. The purpose of this review was to identify and summarize published literature on compassion fatigue among healthcare providers and its impact on patient care. Six databases were searched: MEDLINE (Ovid), PsycINFO (Ovid), Embase (Ovid), CINAHL, Scopus, Web of Science, for studies on compassion fatigue in healthcare providers, published in English from the peak of the pandemic in 2020 to 2023. To expand the search, reference lists of included studies were hand searched to locate additional relevant studies. The studies primarily focused on nurses, physicians, and other allied health professionals. This scoping review was registered on Open Science Framework (OSF), using the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) extension to scoping review. From 11,715 search results, 24 met the inclusion criteria. Findings are presented using four themes: prevalence of compassion fatigue; antecedents of compassion fatigue; consequences of compassion fatigue; and interventions to address compassion fatigue. The potential antecedents of compassion fatigue are grouped under individual-, organization-, and systems-level factors. Our findings suggest that healthcare providers differ in risk for developing compassion fatigue in a country-dependent manner. Interventions such as increasing available personnel helped to minimize the occurrence of compassion fatigue. This scoping review offers important insight on the common causes and potential risks for compassion fatigue among healthcare providers and identifies potential strategies to support healthcare providers’ psychological health and well-being.
• What do we already know about this topic? The elevated and persistent mental stress associated with the COVID-19 pandemic predisposed healthcare providers (HCP) to various psychological conditions such as compassion fatigue. Declines in health providers’ mental health has been observed to negatively impact their professional performance and the quality of patient care.
• How does your research contribute to the field? This review provides an overview of the prevalence of compassion fatigue among HCPs across the globe during the COVID-19 pandemic. The main risk factors for compassion fatigue include younger age, female sex, being either a physician or a nurse, high workload, extensive work hours, and limited access to personal protective equipment (PPE). Negative behavioral intention towards patients has been identified to be a consequence of compassion fatigue. Interventions such as the provision of emotional support, increased monitoring for conditions such as stress and burnout, and increasing available personnel helped to minimize the occurrence of compassion fatigue.
• What are your research’s implications towards theory, practice, or policy? While the public health emergency associated with the COVID-19 pandemic has ended, the impact on human health resources persists. The findings of this review can inform policy decisions and implementation of evidence-based strategies to prevent, manage, and lessen the negative effects of compassion fatigue on HCPs and its subsequent impacts on patient care.
Peer Review reports

Introduction
The 2019-novel coronavirus disease (COVID-19) outbreak spread rapidly and by January 30 th , 2022 was formally proclaimed a global health emergency despite being first identified just over a month prior [ 1 ]. Although there have been five other global health emergencies associated with disease outbreaks since 2009, none has matched the scale and scope of the COVID-19 pandemic [ 2 ]. In the short-term the rapid increase in patients requiring acute care services presented unprecedented challenges for health systems. Care provision and infection control strategies were hampered by capacity limitations, staffing shortfalls and supply chain challenges [ 3 ]. As a result, healthcare providers (HCPs) encountered mounting levels of strain which have continued with little reprieve for the duration of and beyond the global COVID-19 pandemic. Limited access to personal protective equipment (PPEs) exacerbated transmission of the virus, compounding healthcare providers’ fears of contracting and spreading COVID-19 among their peers, patients and families [ 4 , 5 , 6 , 7 ]. HCPs also contracted COVID-19, became seriously ill and died with global estimates of HCP death between January 2020 and May 2021 being over 100,000. With time, the number of absences, extended sick leaves and staff turnovers increased [ 7 , 8 ]. The combination of short staffing, frequent changes to workflow and continuous care provision to patients who were gravely ill and had high mortality amplified the toll on health care providers [ 8 , 9 ]. While no longer a global health emergency, there continue to be COVID-19 cases and deaths. As of July 14, 2023 there were 767,972,961 COVID-19 cases and 6,950,655 deaths globally [ 10 ].
HCPs around the globe who treated severe COVID-19 cases, a process which necessitated in-depth compassionate engagement, became vulnerable to developing compassion fatigue as a result of their continued and in-depth involvement in the care of these severely ill patients and their families [ 11 ]. Compassion fatigue is defined as a composite of two measurements: burnout (sustained employment-related stress that compromises an individual’s desire to work) and secondary trauma (the development of traumatic symptoms resulting from the protracted exposure to the suffering of others) [ 12 , 13 ]. An individual experiencing compassion fatigue has a reduced ability for showing compassion to others, resulting from the prolonged exposure to witnessing the suffering of others without being able to relieve one’s anguish despite having the desire to do so [ 9 ]. Individuals experiencing compassion fatigue may express a range of behaviors such as increased work absences or declines in the ability to engage in work-related tasks such as decision-making. Burnout and secondary trauma are suggested to be mediated by compassion satisfaction—the pleasure that comes from helping behavior [ 11 , 12 ].
As the pandemic shifts from being a global health emergency to an endemic disease, there continues to be concern for HCP health and well-being [ 14 , 15 , 16 ]. The increased and chronic nature of the stress experienced during and beyond the COVID-19 pandemic has heightened HCPs risk for a range of negative psychological impacts such as depression, fearfulness, grief and post-traumatic stress disorder (PTSD) [ 17 ]. Prior infectious disease outbreaks (SARS-CoV-1, H1N1, MERS-CoV, Ebola) are also associated with an increased prevalence of declining mental health in HCPs [ 18 ]. A growing body of research on the COVID-19 pandemic highlights the range of psychological symptoms HCPs developed following their sustained exposure to COVID-19 including burnout, feelings of isolation, insomnia, grief, emotional exhaustion, depression, post-traumatic stress and depersonalization, some of which have persisted over time [ 14 , 17 , 19 , 20 , 21 , 22 ]. The consequences of HCPs’ declining psychological health and well-being has had impacts on the quality of patient care and indirectly on patient outcomes through inadequate staffing [ 18 ]. Compromises in HCPs’ ability to provide optimal clinical care can have serious consequences, including the worsening of patient conditions and the increased transmission of the infection from patients to others in the hospital [ 18 ]. In addition, compassion fatigue may be exacerbated by the COVID-19 pandemic, potentially leading to moral injury, decreased productivity, increased turnover, and reduced quality of care [ 23 ]. Moreover, a growing body of literature suggests that challenges across health systems will persist although COVID-19 is no longer a global health emergency [ 24 , 25 ]. As such, it is important to have a fulsome understanding of COVID-19’s toll on HCPs and tailor health system strategies accordingly.
As health care systems continue to experience a health human resources crisis, it is important to identify and understand the prevalence of compassion fatigue, identify contributing factors, and increase understanding of the consequences and actions that can be taken to address compassion fatigue among HCPs. While there has been in an increase in the body of published literature on the health and well-being of HCPs since the onset of the COVID-19 pandemic, there continues to be a knowledge gap mapping the incidence of compassion fatigue, its resultant impact on HCP well-being, and its potential influence on patient care provision [ 11 , 17 ]. A comprehensive review of the literature on compassion fatigue among HCPs can inform policy and practice initiatives to improve the current health human resources crisis experienced by many health systems. It may also aid in identifying prospective research foci.
The purpose of this scoping review was to synthesize and provide a synopsis of the literature on compassion fatigue among HCPs during the COVID-19 pandemic and to understand its broader impact. The review was guided by the following question: What is the current state of knowledge on compassion fatigue among HCPs over the course of COVID-19?
Project registration
This scoping review was registered under Open Science Framework. A project outline was submitted including the study hypotheses, design, and data collection procedures. The DOI for the registered project is as follows: https://doi.org/10.17605/OSF.IO/F4T7N . In addition, a scoping review protocol for this review has been published in a peer-reviewed journal ( https://doi.org/10.1136/bmjopen-2022-069843 ).
Study design
A systematic scoping review strategy was chosen to explore the existing body of literature pertaining to the research topic. The objective of a scoping review is to identify relevant literature on a given topic, without focusing on evaluating research quality or conducting a thorough analysis of selected studies, as systematic reviews typically do. Current gaps in research and directions for future research can be identified by means of summarizing emerging literature on compassion fatigue in HCPs.
The current scoping review used two methodological tools, namely the Arksey and O’Mally scoping review framework as well as the Joanna Briggs Institute Critical Appraisal Tools. The Arksey and O’Malley framework comprises five stages, which include: (1) formulating the research question; (2) identifying relevant studies; (3) selecting studies for inclusion; (4) extracting and organizing the data; and (5) collating, summarizing, and reporting the findings [ 26 ]. While scoping reviews typically do not require article appraisal, all articles were evaluated by one author (CO) using the methodology established by the Joanna Briggs Institute (JBI) to enhance the overall quality of the review [ 27 ]. No articles were excluded based on their quality, in accord with the Arksey and O’Malley framework [ 26 ].
Stage I: Identifying the research question(s)
The research objective and question were drafted by the authors (AG, LH, CO, SB) and can be found in the previous section under “Research aim”.
Stage II: Identifying relevant studies
As outlined by the JBI methodology, a three-step approach was used to identify relevant studies. These steps include: (1) conducting a preliminary search of at least two suitable databases; (2) identifying relevant keywords and index terms to perform a secondary search across all chosen databases; and (3) manually examining the reference lists of the included articles to discover additional relevant studies [ 28 ] (p11) .
Preliminary literature search
To establish the criteria for inclusion and exclusion, an initial and restricted search was conducted on the subject of interest. The preliminary literature exploration encompassed three scholarly electronic databases: MEDLINE (Ovid), Scopus, and Web of Science. The search employed the keywords “compassion fatigue” and incorporated the timeframe March 1, 2020, to June 15, 2022, so that the most impactful waves of the COVID-19 pandemic were represented in the included literature, resulting in 1519, 2489, and 2246 studies, from the respective databases. These three databases were selected due to their likelihood of yielding results relevant to the research topic. To construct a comprehensive search strategy, a collection of keywords and index terms were identified from the titles and abstracts of relevant articles. The search strategy was further refined in collaboration with a social science librarian.
Structured search strategy
A systematic search was conducted across six scholarly electronic databases: MEDLINE (Ovid), Embase (Ovid), CINAHL, Scopus, and Web of Science. These databases were deliberately chosen to encompass a broad range of relevant findings within the current knowledge landscape regarding the research topic. The systematic search of the literature commenced once the scoping review was peer reviewed and revisions were addressed by the authors. Using the selected vocabulary and Boolean connectors as shown in Table 1 , a string of relevant search terms was developed. The search strategy was adapted accordingly for each individual database (e.g., Medical Subject Headings [MeSH] terms for MEDLINE [Ovid]). In the final stage of the search strategy, the reference lists of all included studies were manually examined to identify additional relevant studies.
Inclusion criteria
The inclusion criteria for this review was formulated using the PCC (Population, Concept, Context) mnemonic developed by JBI (Table 1 ). The participants included in this review were HCPs who were employed across healthcare systems during the COVID-19 pandemic (e.g., physicians, registered nurses, nurse practitioners, physician assistants, and licensed clinical social workers). The concept explored in this review focused on compassion fatigue among HCPs working in healthcare systems during the COVID-19 pandemic. The context of the study encompassed various care settings where HCPs carry out their professional activities across different clinical specialties (e.g., surgery, critical care, palliative care), as well as clinical settings (e.g., inpatient and outpatient). For the purposes of this scoping review, formal healthcare settings were broadly classified as those that provided health services and were situated within and administered by healthcare institutions.
This scoping review only included articles published in English. A time filter was applied to encompass studies conducted between 2020 to 2023, spanning the period from the onset of the COVID-19 pandemic to the present. A range of study designs were included in the review (i.e., experiments, quasi-experimental studies, analytical observational studies, descriptive observational studies, mixed-methods studies, and qualitative studies).
Exclusion criteria
Through the past two decades, compassion fatigue has been defined in different ways, sometimes being considered synonymous with burnout and secondary traumatic stress, or as an outcome resulting from both components [ 12 , 13 ]. Yet recently, it has been suggested that compassion fatigue is a focal concept related to the management of traumatic situations whereas burnout is a general concept that may have multiple contributors [ 26 ]. Due to the conceptual ambiguity surrounding compassion fatigue, articles that solely examine the components of compassion fatigue, such as burnout and secondary trauma, without directly addressing compassion fatigue itself, were excluded from consideration.
Studies that failed to meet the inclusion criteria or lacked full-text availability were excluded from the review. Additionally, editorials, letters to the editor, commentaries, and reviews were also excluded as they did not offer sufficient information for addressing the research questions.
Stage III: Study selection
After the full database searches were conducted, all identified citations were compiled and uploaded into Covidence. Any duplicate citations were automatically excluded.
Three reviewers (LH, CO, AG) independently screened the titles and abstracts of the identified studies to assess their eligibility according to the pre-established inclusion and exclusion criteria. Subsequently, the full texts of 736 selected studies were evaluated to arrive at the final list of articles for data extraction. The reasons for excluding specific studies were documented. Throughout the process, any disagreements that arose at each stage of study selection were resolved through discussions with a third reviewer (AG, SB).
The outcomes of the study selection process were presented in a flow diagram adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) guidelines (Fig. 1 ) [ 29 ]. Additionally, all the included studies underwent an assessment of their risk of bias (quality) using established critical appraisal tools from the Joanna Briggs Institute (JBI) for Evidence Synthesis [ 30 ]. Although not mandatory for scoping reviews, appraisals of study quality will contribute to the subsequent implications and future steps stemming from this scoping review [ 31 ]. The JBI provides critical appraisal checklists for various study designs, encompassing experimental, quasi-experimental, randomized controlled trials, observational, and qualitative study designs. One reviewer (CO) conducted the assessments of all the included studies, and a second reviewer (AG) verified the evaluations. Any discrepancies that arose were discussed and resolved in consultation with both reviewers. In line with the methodology of scoping reviews, no studies were excluded based on their quality assessments, ensuring a comprehensive understanding of the current state of the literature on compassion fatigue among HCPs during the COVID-19 pandemic. A summary of the quality assessments were presented in the results section of the review, while the full appraisals can be found in Additional file 1 .
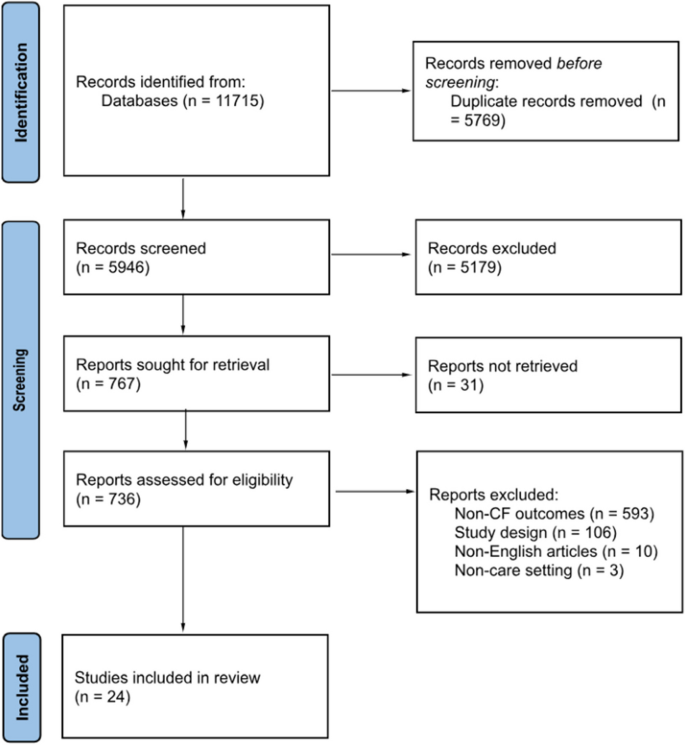
PRISMA flow chart [ 28 ]
Stage IV: Data extraction
To facilitate data extraction aligned with the research objectives, a data-extraction template was developed by one reviewer (LH). This template encompassed various aspects of the included studies (i.e., authors, publication year, study populations, country, study design, aims, sample size, assessment instruments, risk factors, protective factors, consequences of compassion fatigue, and measures to prevent/manage/reduce compassion fatigue). Utilizing Covidence, two independent reviewers (LH, CO) extracted the relevant data from the studies included in the final list of citations.
Stage V: Risk of bias
Standardized tools developed by the Joanna Briggs Institute for respective study types were used to assess risk of bias (quality) for all studies included in the review [ 27 ]. The study appraisals were conducted by one reviewer (CO) and reviewed by another reviewer (AG). Any discrepancies were discussed and resolved together. While no studies were excluded based on the appraisal scores to ensure a comprehensive presentation of the available literature on compassion fatigue among healthcare providers, the findings for the risk of bias assessments are summarized in the results section and the full appraisals are presented in Additional file 1 .
Stage VI: Collating, summarizing, and reporting the results
To summarize and synthesize the findings, the study followed a three-step approach proposed by Levac et al. [ 32 ]: (1) collating and analyzing the collected data; (2) reporting the results and outcomes to address the study objectives; and (3) discussing the potential implications that findings hold for future research and policy considerations [ 31 ]. The review process adhered to the PRISMA Extension for Scoping Reviews checklist, which provided guidance for conducting the review and reporting the findings [ 26 ].
Search results
Figure 1 displays the PRISMA-ScR flowchart of the scoping review search strategy. The search and reference list initially yielded 11,715 studies. Of these, 5769 were excluded as duplicates. Following the title and abstract screening of the remaining studies, 5179 studies were excluded as they met the exclusion criteria. Finally, the full-texts of the remaining 736 studies were screened, and 712 were excluded as they did not meet the inclusion criteria. In total, 24 eligible studies were included in the review for further analysis.
Risk of bias of included studies
The complete assessment of risk of bias of all 24 included studies is available in Additional file 1 . Within the two mixed-methods studies risk of bias primarily stemmed from the quantitative strand of the studies with a lack of clarity provided about study inclusion criteria, study setting, and identification of confounding factors [ 29 ]. Other sources of bias in other quantitative studies were vagueness around the criteria used for outcome measurement [ 30 ] and only one study identified potential cofounding factors along with strategies to manage them [ 31 ]. Further shortcomings related to the failure to provide transparency around the use of valid and reliable outcome measures [ 23 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Within qualitative studies not all provided information about the researchers’ theoretical stance [ 29 , 41 , 43 ] and two studies did not provide documentation of ethics approval for the conducted research [ 43 , 44 ]. One included case report met most assessment criteria for risk of bias although more description of assessment, post-assessment condition and adverse events were warranted [ 45 ].
Characteristics of studies
Study characteristics are presented in Table 2 . Of the 24 eligible studies, 18 studies used quantitative methods [ 23 , 30 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 46 , 47 , 48 , 49 , 50 , 51 ], 3 studies used qualitative methods [ 43 , 44 , 45 ], and the remaining studies used mixed-methods approaches [ 29 , 41 , 52 ]. Additionally, 13 studies focused on the antecedents of compassion fatigue [ 23 , 29 , 33 , 34 , 35 , 36 , 40 , 41 , 42 , 45 , 46 , 47 , 48 ] and 5 studies examined the consequences of compassion fatigue [ 30 , 37 , 43 , 44 , 49 ]. Six studies were conducted in the United States, with the others being conducted in a range of countries including Ecuador, Spain, United Kingdom, Italy, Greece, Turkey, Iran, Uganda, Taiwan, Japan, Philippines, China, and India. These studies primarily focused on nurses, physicians, and other allied health professionals. The study samples included both male and female HCPs. Only one study focused exclusively on female HCPs [ 43 ].
A variety of assessment tools were used to measure compassion fatigue across included studies. Common tools included Compassion Fatigue Short Scale (CFSS) [ 33 , 47 , 48 ], Compassion Fatigue Scale (CFS) [ 30 , 49 ], Professional Quality of Life Scale Version 5 (ProQoL 5) [ 23 , 29 , 29 , 31 , 35 , 36 , 38 , 39 , 40 , 41 , 42 , 50 , 51 ], Work-Related Quality of Life Scale (WRQoL) [ 46 ], and Compassion Fatigue and Satisfaction Self-Test (CFST) [ 37 , 52 ] (Table 3 ).
The time period of the study period shows that most of the studies were conducted in the first six months of 2020, coinciding with the World Health Organization’s declaration of the COVID-19 outbreak as a pandemic [ 54 ]. No studies included in the review were conducted between March 2021 and May 2023 (Fig. 2 ).
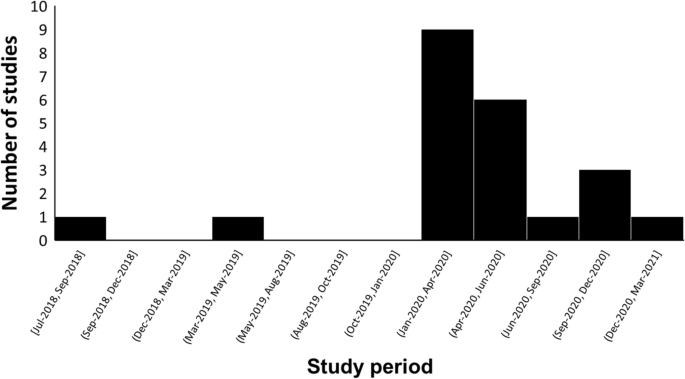
The time trend of study periods on compassion fatigue in HCPs during the COVID-19 pandemic
Findings were synthesized and presented using the following 4 themes: (1) prevalence of compassion fatigue, (2) antecedents of compassion fatigue (individual-Level, organizational-Level, and systems-level factors), (3) consequences of compassion fatigue, and (4) interventions for compassion fatigue.
Theme 1: Prevalence of compassion fatigue
Of the studies reviewed, five measured the prevalence of compassion fatigue among HCPs during the COVID-19 pandemic [ 23 , 30 , 31 , 36 , 41 ]. In a study conducted in Spain, 306 out of 506 (60.4%) HCPs reported high levels of compassion fatigue while 170 (33.6%) showed moderate levels of compassion fatigue (ProQoL 5: M = 19.9, SD = 7.6) [ 36 ]. In a sample composed of 395 Ugandan frontline nurses, 49.11% of the nurses reported high levels of compassion fatigue, while 29.6% experienced moderate levels of compassion fatigue [ 23 ]. Over half of the nurses in the study (54.94%) reported direct exposure to COVID-19 cases. A study conducted in Greece found that in a sample of 105 nurses, the majority of nurses (51.4%) experienced moderate levels of compassion fatigue (ProQoL 5: M = 22.26, SD = 6.76) [ 41 ]. In a Taiwanese study of 503 HCPs, the majority of the participants (63.2%) experienced low levels of compassion fatigue (ProQoL 5: M = 20.9, SD = 7.6) [ 31 ]. Finally, in a Filipino sample composed of 270 frontline nurses, 61.4% of the nurses reported low levels of compassion fatigue (CFS: M = 2.213, SD = 0.979) [ 30 ].
Theme 2: Antecedents of compassion fatigue
Individual-level factors.
Age and sex were key factors associated with compassion fatigue among participant HCPs. Younger HCPs with less experience were more likely to experience mental health issues and conflicting feelings with regards to providing care to COVID-19 patients [ 23 , 29 , 44 , 46 ]. Seven studies included in the review determined that female HCPs were more likely than male HCPs to experience compassion fatigue [ 23 , 35 , 36 , 38 , 40 , 50 , 52 ]. Physicians were also reported to have higher levels of compassion fatigue compared to nurses in three studies [ 36 , 38 , 39 ]. While nursing assistants had higher levels of compassion fatigue when compared to nurses in one study (ProQol 5: Nursing assistants = 29.15 ± 6.94; Nurse = 25.68 ± 5.87) [ 29 ]. Furthermore, the risk was higher in permanent workers compared to temporary workers (ProQoL 5: Permanent = 2.48 ± 1.29; Temporary = 2.11 ± 1.15; P -value < 0.05) [ 35 ]. One included study determined that marital status and education levels were not correlated with compassion fatigue [ 23 ]. Psychiatric comorbidities such as past trauma, burnout, stress, anxiety, and depression exacerbated HCPs’ psychological well-being across a number of included studies [ 31 , 33 , 36 , 38 , 39 , 41 , 49 , 50 ]. Other psychological factors such as excessive empathetic engagement, sensitive sensory processes, and overidentification from frequent witnessing of patient suffering and deaths were found to aggravate the development of compassion fatigue [ 34 , 39 , 45 ]. The inability to cope with the rapidly evolving landscape of healthcare provision and a lack of self-care contributed to increased burden and blurring of role boundaries between professional and private lives [ 29 , 41 , 43 , 44 , 51 , 52 ]. One study that used Compassion Fatigue and Satisfaction Self-Tests and a questionnaire of personal and professional characteristics found that feelings of underappreciation, insufficient compensations, and social isolation incurred psychological burden on pediatric sub-specialists [ 52 ]. Additionally, a decrease in occupational hardiness, as measured by the Occupational Hardiness Questionnaire, increased the risk of compassion fatigue among HCPs in two studies [ 42 , 50 ]. Negative outcomes to the HCPs’ families and concerns revolving around their patients’ families also predicted higher risk of experiencing compassion fatigue [ 45 , 48 , 52 ]. Finally, HCPs’ fear of COVID-19 with regards to infection and transmission was identified as a predictor of compassion fatigue [ 29 , 40 , 43 , 44 , 47 ].
Two studies identified social support from family, friends, peers, and hospital leadership as a crucial protective factor for compassion fatigue [ 43 , 52 ]. Coping mechanisms such as venting and exercising were found to help alleviate stress among HCPs [ 44 ]. Psychological qualities such as compassion satisfaction, professional satisfaction, resilience, vigor, and hardiness were found to help protect the psychological health of HCPs as well as reducing turnover intention and increasing perceived quality of care [ 30 , 34 , 36 , 37 , 39 , 40 , 42 , 46 , 50 ]. Self-care, self-awareness of limitations, and self-regulation of emotions were crucial for reducing risk of compassion fatigue in two studies comprised of physicians and nurses [ 44 , 50 ]. Lastly, spirituality, religiosity, and meditation also served as protective factors in three studies on compassion fatigue in HCPs [ 41 , 44 , 51 ].
Organizational-level factors
In five of the articles reviewed, increased workload [ 23 , 29 , 44 , 45 ], long working hours [ 23 , 29 , 44 , 45 ], and increased number of patients [ 50 ] were identified as common predictors of compassion fatigue. Furthermore, providing direct care to COVID-19 patients, which were often emotionally challenging cases, exacerbated the psychological risks to HCPs [ 23 , 36 , 46 , 48 , 50 ]. Chronic exposure to a dynamic work environment also increased the risk of compassion fatigue among HCPs [ 29 ]. Lack of access to suitable PPEs and lack of foresight from management and human resources teams regarding infection control guidelines contributed to HCPs’ distress [ 29 ]. Adjusting to the discomfort caused by wearing PPEs presented as a challenge to maintaining the efficiency of work activities [ 29 ]. Lastly, in two studies, HCPs identified that while there were plenty of wellness resources provided by healthcare organizations to support mindfulness, there was a lack of practical and pragmatic resources for social and emotional support, work-life balance, and remuneration [ 23 , 43 ].
Positive work conditions, such as a visible presence and engagement by leadership and management, as well as a positive work culture allowing HCPs to seek help without fear of judgment was found to be important protective factors against the development of compassion fatigue [ 44 ]. The social aspects of teamwork facilitated the sharing of feelings of trauma which in turn contributed to resilience and improved psychological well-being among HCPs in three studies [ 41 , 43 , 44 ]. One study observed that workplace wellness activities and a sense of feeling valued can prevent high levels of compassion fatigue [ 52 ]. Words of appreciation from supervisors boosted morale for some HCPs [ 44 ]. Attention to workplace safety in the form of PPEs and early access to vaccines alleviated the fear of infection [ 44 ]. Finally, two studies determined that adequate preparation and education to handle COVID-19 cases and increased autonomy decreased the risk of compassion fatigue and increased professional fulfillment [ 42 , 44 ].
Systems-level factors
Significant and frequently changing public health measures over the course of the pandemic presented a challenge as they were disruptive to workflow and resulted in uncertainty, feelings of inadequacy, and distress among HCPs across a range of geographical contexts [ 29 , 41 , 43 , 49 ]. Increases in the incidence of COVID-19 cases also contributed to a rise in the number of hospital admissions, aggravating HCPs’ workload [ 35 ]. Social-distancing policies precluded informal team interactions, such as sharing meals together, which posed a risk to HCPs’ psychological well-being by decreasing social support [ 43 , 52 ]. Transitions to tele-health also increased social isolation [ 43 ]. A theme that emerged was the negative impact of stigma on HCPs, with their proximity to contagion, as a possible risk factor [ 35 , 41 ]. Aggressive behaviors and verbal abuse from patients were sources of emotional stress for some HCPs [ 44 ]. Finally, negative peer pressure was identified as a barrier to HCPs engaging in self-care as they felt pressure to conform to sociocultural norms of an expected level of dedication [ 44 ]. In contrast to the impacts of stigma, a positive perception of one’s own profession is related to increased commitment and decreased compassion fatigue [ 46 ].
Theme 3: Consequences of compassion fatigue
The findings of one study suggested that compassion fatigue associated with HCP’s professional practice impacted their private lives, predicting greater parental burnout ( r = 0.542), child abuse ( r = 0.468), child neglect ( r = 0.493), spouse conflict ( r = 0.340), and substance abuse ( r = 0.298) [ 48 ]. This study identified factors such as direct care of COVID-19 patients ( r = 0.255), exposure to patient death and suffering due to COVID-19 ( r = 0.281), and family income loss due to COVID-19 ( r = 0.366) as risk factors for compassion fatigue [ 48 ]. Additionally, at an organizational-level, two studies conducted in 2020 and 2021 observed that Turkish and Filipino HCPs who reported compassion fatigue also reported lower job satisfaction and reduced professional commitment [ 30 , 46 ]. Consequently, elevated compassion fatigue also increased organizational turnover intent among Filipino HCPs (β = 0.301, P -value = 0.001) [ 30 ]. A study conducted in China found that compassion fatigue predicted negative behavioral intentions towards treating COVID-19 patients, as measured by the Attitude, Subjective Norms, and Behavioral Intention of Nurses toward Mechanically Ventilated Patients (ASIMP) questionnaire [ 33 ]. This suggests that quality of care may be adversely impacted [ 33 ]. Finally, an American study observed that compassion fatigue among HCPs was associated with deteriorating workplace culture [ 52 ].
- Patient care
The provision of care during the pandemic was impacted by the general lack of preparation for handling novel tasks experienced by many HCPs [ 23 ]. Findings from one study found that many HCPs (73%) experienced a shift in their clinical practice setting, for example, from in-personal care to virtual telehealth consults as a result of the pandemic [ 43 ]. HCPs also experienced an increase in the need to provide palliative care as a result of the negative health impacts of COVID-19, something they may have had limited prior experience with [ 43 ]. In a case study conducted in Japan, the physician reported feeling inexperienced with handling the psychological impact of the pandemic experienced by not only the patients but also the patients’ family [ 45 ]. The consequences of not being able to provide optimal care was found to exacerbate feelings of guilt, powerlessness, and frustration in HCPs [ 41 , 43 ]. In turn, study findings suggest that worsening compassion fatigue may reduce the quality of care provided by HCPs because it has been found to be a significant predictor of negative behavioral intention [ 30 , 33 , 40 , 52 ].
Theme 4: Interventions for compassion fatigue
Two studies in Japan and Uganda investigated potential interventions to support HCPs experiencing COVID-19 related compassion fatigue. On an individual-level, regularly engaging in self-care activities such as expressions of gratitude as well as learning how to recognize signs and symptoms of compassion fatigue were identified as crucial first steps in its management [ 45 , 52 ]. Emotional support from colleagues and mental health specialists was found to be effective in improving the mental health of a Japanese physician experiencing compassion fatigue [ 45 ]. Findings of two studies identified the need for a systematic approach to monitor the progression of psychological symptoms and providing tailored resources in a timely manner to HCPs to help ameliorate compassion fatigue and its consequences [ 29 , 45 ]. Suggested strategies included: facilitating regular consultations with each department [ 45 , 52 ], increasing the staffing number of HCPs in busy departments [ 23 , 45 ], and providing PPEs and vaccines in a timely manner [ 23 , 52 ]. Lastly, findings from two studies in Uganda and the United States suggested that increased remuneration may prevent or minimize compassion fatigue [ 23 , 52 ].
Key findings
This scoping review sought to provide a comprehensive summary of the literature published between January 2020 and May 2023 on the impact of the COVID-19 pandemic on compassion fatigue among HCPs and its subsequent impact on patient care. Most of the included studies were conducted in 2020 and used cross-sectional study designs. Given that the COVID-19 outbreak was declared a global health emergency in early 2020 [ 1 ], cross-sectional study designs were well-placed to provide prompt and important insights on compassion fatigue across the HCP population. Review findings were presented using four themes addressing the prevalence, antecedents, consequences, and consequences of compassion fatigue in HCPs. The prevalence of compassion fatigue was observed to vary across countries. The negative psychological outcomes reported by included studies were precipitated by individual-level factors such as age and occupational role; organizational-factors such as lack of access to PPE; and systems-level factors such as loss of social engagement and stigma. The consequences of compassion fatigue impacted HCPs’ personal and professional roles. Findings suggest an urgent need for policy makers, health managers, and team leaders to develop and implement strategies that target the potential root causes of compassion fatigue in HCPs.
Prevalence of compassion fatigue
Among the five studies that measured prevalence of compassion fatigue, results were highly variable across countries [ 23 , 30 , 31 , 36 , 41 ]. This may be attributed to differences in preparedness for infection containment and variability among health systems’ preparation and ability to respond to supply chain issues [ 53 ]. Taiwan provides an example of how digital technologies were adopted to improve disease surveillance and monitor medical supply chains [ 55 ]. Using the stringent Identify-Isolate-Inform model in conjunction with public mask-wearing and physical distancing, the spread of the disease was effectively contained in Taiwan [ 53 ]. Consequently, despite not enforcing lockdowns, Taiwan blocked the first wave of cases and slowed down subsequent outbreaks, which may contribute to the observed low prevalence of compassion fatigue among HCPs [ 56 ]. In the Philippines, responses to disease outbreaks varied across different municipalities and provinces [ 57 ]. Effective containment measures such as strict border control and early lockdowns in addition to plentiful medical supplies and personnel allowed certain regions to mount a strong response to this public health emergency, subsequently resulting in the observed low prevalence of compassion fatigue among HCPs [ 57 ]. In Uganda, there were generally low levels of preparedness with regards to the infection identification, PPE supply, access to hand-washing facilities, and establishment of isolation facilities [ 58 ]. This may have contributed to an overwhelmed healthcare system and overworked HCPs as the surge of cases was exacerbated by the shortage of disease containment resources [ 58 ]. In April 2020, Spain experienced the second highest infection incidence in the world [ 59 ]. The Spanish health system was overwhelmed by the abundance of patients due to lack of HCPs [ 60 ], hospital capacity, and material supplies [ 59 ]. An increase in compassion fatigue among HCPs was also observed in recent studies from Italy and Canada [ 61 , 62 ]. Overall, the various strategies used to address the resultant COVID-19-related public health crisis presented distinctive challenges to HCPs in different countries. Caution must be taken when interpreting the study findings given the contextual differences across various healthcare systems. The psychological burden and prevalence of compassion fatigue subsequently varied depending on the context.
Antecedents of compassion fatigue
The findings of this review suggest that individual characteristics such as age and occupational role are significant contributing factors to the development of compassion fatigue during COVID-19 [ 63 ]. Specifically, older HCPs were less likely to experience compassion fatigue than younger HCPs according to regression analyses [ 23 , 29 , 44 , 46 ]. This observation may be attributed to their increased work experience. Resilience was also positively linearly related to age [ 64 ]. Factors identified as potential contributors to the observed age-related advantage in wellbeing were access to job resources, better job security, work-life balance, and coping skills [ 64 ]. The compounding of stressors such as an increase in workload during the COVID-19 pandemic could have exacerbated the psychological health of younger HCPs. In the context of telework, older employees tended to create clear boundaries between work and non-work responsibilities [ 64 ]. The rise in telework among HCPs was mostly a consequence of the COVID-19 pandemic which may have increased the psychological burden on younger HCPs [ 65 ]. In addition, a study examining demographic predictors of resilience in nurses reported that younger nurses had less exposure to stress, and thus have fewer opportunities to develop skills in stress management [ 66 ]. As a result of these factors, the younger HCPs were at high risk for compassion fatigue during the COVID-19 pandemic. Interestingly, three of the included studies in this review also observed that physicians were at a higher risk of compassion fatigue compared to nurses [ 36 , 38 , 39 ]. This difference may be attributed to the burden of responsibility in relation to breaking bad news, a task that is often the physicians’ responsibility [ 67 ]. A study examining compassion fatigue in HCPs determined that conflict arising during patient interactions placed HCPs at a risk for compassion fatigue [ 68 ]. Delivery of bad or uncertain news also predicted a greater mental health burden in HCPs [ 68 ].
At the organizational level, findings from the studies included in this review identified that a lack of access to PPE was a contributor to compassion fatigue in HCPs during COVID-19 [ 29 , 52 ]. Specifically, one study reported that the fear of infection and transmission to patients, family, and friends added to the concern of HCPs working in high-risk environments [ 69 ]. This finding can potentially be explained by the increased vulnerability that HCPs experience following a lag in the provision of PPE. Several organizational factors were determined as potential barriers to the distribution of PPE; the unprecedented nature of the pandemic presented challenges for maintaining domestic inventories [ 70 ]. Disruptions to the PPE global supply chain also amplified the equipment shortage [ 70 ]. This finding highlights the importance of monitoring and ensuring that domestic health supplies are adequately stocked.
At the system level, loss of social engagement [ 43 , 52 ] and stigma [ 35 , 41 ] were identified in the studies included in the review as antecedents to compassion fatigue. Public policies such as social-distancing and occupancy capacity limits negatively impact social interactions which may explain the loss of social engagement in addition to worsening mental health well-being in HCPs [ 71 ]. As certain practices transition to telehealth, other studies have found increased mental fatigue and difficulty with maintaining empathetic rapport, which has important implications on patient care [ 72 , 73 ]. In addition, other studies have found that given the proximity of their role to contagion, stigma towards HCPs from patients increased during COVID-19 [ 74 , 75 ]. Consequently, the combinatorial experience of being socially isolated and stigmatized may worsen mental health outcomes [ 76 ]. This points to a need for increased access to support services for HCPs such as virtual communities.
Consequences of compassion fatigue
Review findings suggest that compassion fatigue impacted the private and professional lives of HCPs. The risk for parental burnout has increased across many occupations during the pandemic [ 77 ]. Factors related to low levels of social support, lack of leisure time, and greater parental responsibilities in face of education disruptions adds to the psychological burden of parents [ 77 ]. HCPs were placed in a unique position having to work in highly stressful environments while also balancing household responsibilities and increased challenges related to childcare [ 48 , 78 ]. This finding highlights a need for the provision of child support services for HCPs or a reduction in workload to alleviate the burden of parental and homecare responsibilities particularly in times of public health crises.
Beyond their private lives, this review has found that decreases in HCPs’ professional commitment due to compassion fatigue, may endanger the quality of patient care delivered [ 79 ]. In particular, this may be attributed to the surge in palliative care cases during the pandemic in conjunction with an unprepared workforce, creating psychological stress for HCPs [ 80 ]. In a study examining palliative care preparedness during the pandemic, a lack of core palliative care training and expertise among frontline HCPs [ 81 ] meant many felt emotionally unprepared to address cases with seriously ill patients [ 45 ]. An increased frequency of breaking bad news to patients’ families was associated with negative psychological outcomes [ 82 ]. Providing training on relevant communication skills may protect HCPs from compassion fatigue [ 83 , 84 ].
Implications
The findings of this review highlight the urgency to provide support for HCPs who may be at risk for compassion fatigue which could have subsequent impacts on the provision of patient care [ 85 ]. To address the antecedents of compassion fatigue, this scoping review has identified a need for increased staffing, recruitment, and retention efforts on the part of hospital human resources departments [ 23 , 45 ]. Interventions suggested by studies included in the review encompass the monitoring of psychological well-being among HCPs to inform timely provision of resources [ 29 , 45 ]. Specifically, structured debriefing, training on self-care routine, reduced workload, and normalization of trauma-related therapy are essential interventions [ 86 ]. Additionally, a study identified that fostering collaborative workplace culture encourages social and emotional support among staff [ 45 ]. Certain hospitals have adopted “wobble rooms” as a private unwinding and venting space for employees [ 87 ]. Studies have observed that interventions aimed at improving the well-being of HCPs resulted in enhanced quality and safety of care being delivered [ 75 ].
Strengths and limitations
There are both strengths and limitations in this review. Although some literature reviews focused on the psychological health status of HCPs (e.g., burnout, anxiety, depression), very few studies have specifically explored compassion fatigue. Reviews that considered the impact of the COVID-19 pandemic on HCPs were even more limited. It is known that compassion is a cornerstone of quality health care improvement and increases successful medical outcomes [ 88 , 89 , 90 ]. Nevertheless, prolonged exposure to distressing events by HCPs, such as patient death and suffering, results in the absorption of negative emotional responses and leads to the development of compassion fatigue [ 91 ]. This scoping review presents an extensive exploration of the current body of literature on compassion fatigue among HCPs during the COVID-19 pandemic. Another strength in this study lies in the transparency and reproducibility of the methodology. The scoping review protocol has been published in a peer-reviewed journal to establish high methodological standards for the final scoping review [ 92 ]. Additionally, the study plan was pre-registered with Open Science Framework to ensure commitment to the methodology. Double extraction was performed to ensure that a comprehensive descriptive summary of the studies was achieved.
Some limitations include the short time frame chosen for the included studies that were published since the COVID-19, which may have constrained the breadth and quality of the studies. Longitudinal studies may not be captured in the review as this study methodology requires a prolonged period of time to yield meaningful observations. More data is needed to support conclusions on the impact of compassion fatigue on patient care. Additionally, none of the studies included in the review were conducted between March 2021 and May 2023, which may miss out on meaningful trends in levels of compassion fatigue in HCPs. This scoping review only included literature published in English so studies published in other languages were not assessed. Additionally, no comparisons of compassion fatigue were made among the HCP groups in spite of potentially relevant differences such as patient exposure. There was also a lack of allied health profession representation, with the majority of the study population being nurses or physicians. Lastly, grey literature was not included in this scoping review which may delimitate the information included in the scoping review.
There were recurring themes related to limitations in the included research studies. Several studies identified sampling issues including small sample sizes, restricted sample frame, low response rate, and selection error [ 23 , 29 , 31 , 38 , 39 , 40 , 41 , 42 , 43 , 47 , 50 , 51 , 83 ]. Other studies have called for investigations into how different sociodemographic factors, other psychiatric diseases, health care settings, and workplace environment impact compassion fatigue in HCPs [ 38 , 39 , 47 , 48 , 83 ]. One study observed a lack of homogeneity in the sample due to an overrepresentation of female HCPs in the sample [ 38 ]. Lastly, many studies employed a cross-sectional study design which limits the interpretation of the data in terms of causality [ 23 , 30 , 31 , 34 , 42 , 47 , 48 , 50 ]. While there are limitations to the study, a comprehensive summary of existing literature may be useful to inform future research and policies.
Future research is needed to examine the longitudinal impacts of COVID-19 on compassion fatigue in HCPs. Moreover, research in this area could be strengthened by including a consultation phase with external experts on compassion fatigue to improve the robustness of the scoping review.
Conclusions
The COVID-19 pandemic presented a unique set of challenges to healthcare systems across the globe. This scoping review indicated that the prevalence of compassion fatigue was inconsistent across countries and may reflect the variability of pandemic preparedness among the individual countries. Primary risk factors for the development of compassion fatigue included being younger, female, a physician or nurse, and having limited access to PPE in conjunction with an excessive workload and prolonged work hours. The negative impacts of compassion fatigue were experienced at the individual and organizational level. The findings suggest there is a systemic need to assess, monitor and support health professionals’ well-being particularly during conditions of protracted health crises such as a pandemic. In addition, many health systems and sectors are facing a profound health human resources crisis and therefore ongoing efforts must be made to improve workplace environments and increase recruitment and retention efforts. Lastly, pandemic planning must include provisions to support health providers’ ability to safely do their jobs while also minimizing negative impacts to their health and well-being.
Availability of data and materials
All the material presented in the manuscript is owned by the authors and/or no permissions are required.
Coronavirus disease (COVID-19) pandemic. Accessed 16 Jan 2023. https://www.who.int/europe/emergencies/situations/covid-19
Wilder-Smith A, Osman S. Public health emergencies of international concern: a historic overview. J Travel Med. 2020;27(8):taaa227. https://doi.org/10.1093/jtm/taaa227 .
Article PubMed Google Scholar
Gristina GR, Piccinni M. COVID-19 pandemic in ICU. limited resources for many patients: approaches and criteria for triaging. Minerva Anestesiol. 2021;87(12):1367–79. https://doi.org/10.23736/S0375-9393.21.15736-0 .
Chaka EE, Mekuria M, Melesie G. Access to Essential personal safety, availability of personal protective equipment and perception of healthcare workers during the COVID-19 in public hospital in West Shoa. Infect Drug Resist. 2022;15:2315–23. https://doi.org/10.2147/IDR.S344763 .
Article PubMed PubMed Central Google Scholar
Gholami M, Fawad I, Shadan S, et al. COVID-19 and healthcare workers: a systematic review and meta-analysis. Int J Infect Dis. 2021;104:335–46. https://doi.org/10.1016/j.ijid.2021.01.013 .
Article CAS PubMed PubMed Central Google Scholar
Schug C, Geiser F, Hiebel N, et al. Sick Leave and Intention to Quit the Job among Nursing Staff in German Hospitals during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(4):1947. https://doi.org/10.3390/ijerph19041947 .
Lancet T. COVID-19: protecting health-care workers. Lancet Lond Engl. 2020;395(10228):922. https://doi.org/10.1016/S0140-6736(20)30644-9 .
Article Google Scholar
Beck E, Daniels J. Intolerance of uncertainty, fear of contamination and perceived social support as predictors of psychological distress in NHS healthcare workers during the COVID-19 pandemic. Psychol Health Med. Published online July 6, 2022:1–13. https://doi.org/10.1080/13548506.2022.2092762.
Nikeghbal K, Kouhnavard B, Shabani A, Zamanian Z. Covid-19 effects on the mental workload and quality of work life in Iranian nurses. Ann Glob Health. 2021;87(1):79. https://doi.org/10.5334/aogh.3386.
WHO Coronavirus (COVID-19) Dashboard. Accessed 16 Jan 2023. https://covid19.who.int
Lluch C, Galiana L, Doménech P, Sansó N. The Impact of the COVID-19 pandemic on burnout, compassion fatigue, and compassion satisfaction in healthcare personnel: a systematic review of the literature published during the first year of the pandemic. Healthcare. 2022;10(2):364. https://doi.org/10.3390/healthcare10020364 .
Salmond E, Salmond S, Ames M, Kamienski M, Holly C. Experiences of compassion fatigue in direct care nurses: a qualitative systematic review. JBI Evid Synth. 2019;17(5):682. https://doi.org/10.11124/JBISRIR-2017-003818 .
Sinclair S, Raffin-Bouchal S, Venturato L, Mijovic-Kondejewski J, Smith-MacDonald L. Compassion fatigue: A meta-narrative review of the healthcare literature. Int J Nurs Stud. 2017;69:9–24. https://doi.org/10.1016/j.ijnurstu.2017.01.003 .
Majid U, Hussain SAS, Zahid A, Haider MH, Arora R. Mental health outcomes in health care providers during the COVID-19 pandemic: an umbrella review. Health Promot Int. 2023;38(2):daad025. https://doi.org/10.1093/heapro/daad025 .
Rahmani F, Hosseinzadeh M, Gholizadeh L. Complicated grief and related factors among nursing staff during the Covid-19 pandemic: a cross-sectional study. BMC Psychiatry. 2023;23(1):73. https://doi.org/10.1186/s12888-023-04562-w .
Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic. Accessed July 6, 2023. https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic
Ghahramani S, Kasraei H, Hayati R, Tabrizi R, Marzaleh MA. Health care workers’ mental health in the face of COVID-19: a systematic review and meta-analysis. Int J Psychiatry Clin Pract. 2022;0(0):1–10. https://doi.org/10.1080/13651501.2022.2101927 .
Article CAS Google Scholar
Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J Clin Nurs. 2020;29(21–22):4217–26. https://doi.org/10.1111/jocn.15454 .
Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Occup Environ Health. 2021;94(6):1345–52. https://doi.org/10.1007/s00420-021-01695-x .
Iddrisu M, Poku CA, Mensah E, Attafuah PYA, Dzansi G, Adjorlolo S. Work-related psychosocial challenges and coping strategies among nursing workforce during the COVID-19 pandemic: a scoping review. BMC Nurs. 2023;22(1):210. https://doi.org/10.1186/s12912-023-01368-9 .
Yang BJ, Yen CW, Lin SJ, et al. Emergency nurses’ burnout levels as the mediator of the relationship between stress and posttraumatic stress disorder symptoms during COVID-19 pandemic. J Adv Nurs. 2022;78(9):2861–71. https://doi.org/10.1111/jan.15214 .
Fukushima H, Imai H, Miyakoshi C, Naito A, Otani K, Matsuishi K. The sustained psychological impact of coronavirus disease 2019 pandemic on hospital workers 2 years after the outbreak: a repeated cross-sectional study in Kobe. BMC Psychiatry. 2023;23(1):313. https://doi.org/10.1186/s12888-023-04788-8 .
Amir K, Okalo P. Frontline nurses’ compassion fatigue and associated predictive factors during the second wave of COVID-19 in Kampala. Uganda Nurs Open. 2022;9(5):2390–6. https://doi.org/10.1002/nop2.1253 .
Calkins K, Guttormson J, McAndrew NS, et al. The early impact of COVID-19 on intensive care nurses’ personal and professional well-being: a qualitative study. Intensive Crit Care Nurs. 2023;76:103388. https://doi.org/10.1016/j.iccn.2023.103388 .
Sexton JB, Adair KC, Proulx J, et al. Emotional exhaustion among US health care workers before and during the COVID-19 Pandemic, 2019–2021. JAMA Netw Open. 2022;5(9):e2232748. https://doi.org/10.1001/jamanetworkopen.2022.32748 .
Slatten LA, David Carson K, Carson PP. Compassion fatigue and burnout what managers should know. Health Care Manag. 2011;30(4):325–33. https://doi.org/10.1097/HCM.0b013e31823511f7 .
Martin J. © Joanna Briggs Institute 2017 Critical Appraisal Checklist for Systematic Reviews and Research Syntheses. Published online 2017.
PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation | Annals of Internal Medicine. Accessed 16 Jan 16 2023. https://www.acpjournals.org/doi/full/ https://doi.org/10.7326/M18-0850?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
Moreno-Mulet C, Sansó N, Carrero-Planells A, et al. The Impact of the COVID-19 Pandemic on ICU healthcare professionals: a mixed methods study. Int J Environ Res Public Health. 2021;18(17):9243. https://doi.org/10.3390/ijerph18179243 .
Labrague LJ, de los Santos JAA. Resilience as a mediator between compassion fatigue, nurses’ work outcomes, and quality of care during the COVID-19 pandemic. Appl Nurs Res. 2021;61:151476.
Su PA, Lo MC, Wang CL, et al. The correlation between professional quality of life and mental health outcomes among hospital personnel during the Covid-19 pandemic in Taiwan. J Multidiscip Healthc. 2021;14:3485–95. https://doi.org/10.2147/JMDH.S330533 .
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5:69. https://doi.org/10.1186/1748-5908-5-69 .
Cheng J, Cui J, Yu W, Kang H, Tian Y, Jiang X. Factors influencing nurses’ behavioral intention toward caring for COVID-19 patients on mechanical ventilation: a cross-sectional study. PLoS ONE. 2021;16(11):e0259658. https://doi.org/10.1371/journal.pone.0259658 .
Pérez-Chacón M, Chacón A, Borda-Mas M, Avargues-Navarro ML. Sensory processing sensitivity and compassion satisfaction as risk/protective factors from burnout and compassion fatigue in healthcare and education professionals. Int J Environ Res Public Health. 2021;18(2):611. https://doi.org/10.3390/ijerph18020611 .
Ramaci T, Barattucci M, Ledda C, Rapisarda V. Social Stigma during COVID-19 and its Impact on HCWs Outcomes. Sustainability. 2020;12(9):3834. https://doi.org/10.3390/su12093834 .
Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Cabrera-Troya J, Carmona-Rega MI, Ortega-Galán ÁM. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs. 2020;29(21–22):4321–30. https://doi.org/10.1111/jocn.15469 .
Kase SM, Gribben JL, Guttmann KF, Waldman ED, Weintraub AS. Compassion fatigue, burnout, and compassion satisfaction in pediatric subspecialists during the SARS-CoV-2 pandemic. Pediatr Res. 2022;91(1):143–8. https://doi.org/10.1038/s41390-021-01635-y .
Article CAS PubMed Google Scholar
Carmassi C, Dell’Oste V, Bertelloni CA, et al. Gender and occupational role differences in work-related post-traumatic stress symptoms, burnout and global functioning in emergency healthcare workers. Intensive Crit Care Nurs. 2022;69:103154. https://doi.org/10.1016/j.iccn.2021.103154 .
Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Carmona-Rega MI, Sánchez-Ruiz MJ, Ortega-Galán ÁM. Professional quality of life, self-compassion, resilience, and empathy in healthcare professionals during COVID-19 crisis in Spain. Res Nurs Health. 2021;44(4):620–32. https://doi.org/10.1002/nur.22158 .
Yılmaz A, Bay F, Erdem Ö, Özkalp B. The professional quality of life for healthcare workers during the COVID-19 Pandemic in Turkey and the influencing factors. Bezmialem Sci. 2022;10(3):361–9. https://doi.org/10.14235/bas.galenos.2021.5837 .
Missouridou E, Mangoulia P, Pavlou V, et al. Wounded healers during the COVID-19 syndemic: Compassion fatigue and compassion satisfaction among nursing care providers in Greece. Perspect Psychiatr Care. 2022;58(4):1421–32. https://doi.org/10.1111/ppc.12946 . Published online September 10, 2021.
Zakeri MA, Rahiminezhad E, Salehi F, Ganjeh H, Dehghan M. compassion satisfaction, compassion fatigue and hardiness among nurses: a comparison before and during the COVID-19 Outbreak. Front Psychol. 2022;12:815180. https://doi.org/10.3389/fpsyg.2021.815180 .
Austin EJ, Blacker A, Kalia I. “Watching the tsunami come”: a case study of female healthcare provider experiences during the COVID-19 pandemic. Appl Psychol Health Well-Being. 2021;13(4):781–97. https://doi.org/10.1111/aphw.12269 .
Kong KYC, Ganapathy S. Are we in control of our demons?: understanding compassion satisfaction, compassion fatigue and burnout in an asian pediatric emergency department in a pandemic. Pediatr Emerg Care. 2022;38(3):e1058. https://doi.org/10.1097/PEC.0000000000002656 .
Nishihara T, Ohashi A, Nakashima Y, Yamashita T, Hiyama K, Kuroiwa M. Compassion fatigue in a health care worker treating COVID-19 patients: a case report. Biopsychosoc Med. 2022;16(1):10. https://doi.org/10.1186/s13030-022-00239-0 .
Kaya ŞD, Mehmet N, Şafak K. Professional commitment, satisfaction and quality of life of nurses during the COVID-19 Pandemic in Konya. Turkey Ethiop J Health Sci. 2022;32(2):393–404. https://doi.org/10.4314/ejhs.v32i2.20 .
Kottoor AS, Chacko N. Role of entrapment in relation between fear of Covid-19 and compassion fatigue among nurses. Int J Behav Sci. 2022;15(4):250–5. https://doi.org/10.30491/ijbs.2022.288846.1573 .
Stevenson MC, Schaefer CT, Ravipati VM. COVID-19 patient care predicts nurses’ parental burnout and child abuse: Mediating effects of compassion fatigue. Child Abuse Negl. 2022;130:105458. https://doi.org/10.1016/j.chiabu.2021.105458 .
Hochwarter W, Jordan S, Kiewitz C, et al. Losing compassion for patients? The implications of COVID-19 on compassion fatigue and event-related post-traumatic stress disorder in nurses. J Manag Psychol. 2022;37(3):206–23. https://doi.org/10.1108/JMP-01-2021-0037 .
Cuartero-Castañer ME, Hidalgo-Andrade P, Cañas-Lerma AJ. professional quality of life, engagement, and self-care in healthcare professionals in Ecuador during the COVID-19 Pandemic. Healthcare. 2021;9(5):515. https://doi.org/10.3390/healthcare9050515 .
Spiridigliozzi S. Exploring the relationship between faith and the experience of burnout, compassion fatigue, and compassion satisfaction for hospice workers during a global pandemic: a multidisciplinary study. Dr Diss Proj. Published online April 1, 2022. https://digitalcommons.liberty.edu/doctoral/3572
Gribben JL, Kase SM, Guttmann KF, Waldman ED, Weintraub AS. Impact of the SARS-CoV-2 pandemic on pediatric subspecialists’ well-being and perception of workplace value. Pediatr Res. Published online January 20, 2023:1–7. https://doi.org/10.1038/s41390-023-02474-9.
Chien LC, Beÿ CK, Koenig KL. Taiwan’s Successful COVID-19 mitigation and containment strategy: achieving quasi population immunity. Disaster Med Public Health Prep.:1–4. https://doi.org/10.1017/dmp.2020.357.
Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Bio-Medica Atenei Parm. 2020;91(1):157–60. https://doi.org/10.23750/abm.v91i1.9397 .
Kuo S, Ou HT, Wang CJ. Managing medication supply chains: Lessons learned from Taiwan during the COVID-19 pandemic and preparedness planning for the future. J Am Pharm Assoc. 2021;61(1):e12–5. https://doi.org/10.1016/j.japh.2020.08.029 .
Cheng HY, Liu DP. Early Prompt Response to COVID-19 in Taiwan: Comprehensive surveillance, decisive border control, and information technology support. J Formos Med Assoc. Published online November 11, 2022. https://doi.org/10.1016/j.jfma.2022.11.002.
S. Talabis DA, Babierra AL, H. Buhat CA, Lutero DS, Quindala KM, Rabajante JF. Local government responses for COVID-19 management in the Philippines. BMC Public Health. 2021;21:1711. https://doi.org/10.1186/s12889-021-11746-0 .
Rashid N, Nazziwa A, Nanyeenya N, Madinah N, Lwere K. Preparedness, identification and care of COVID-19 cases by front line health workers in selected health facilities in mbale district uganda: a cross-sectional study. East Afr Health Res J. 2021;5(2):144–50. https://doi.org/10.24248/eahrj.v5i2.665 .
Alfonso Viguria U, Casamitjana N. Early Interventions and Impact of COVID-19 in Spain. Int J Environ Res Public Health. 2021;18(8):4026. https://doi.org/10.3390/ijerph18084026 .
Rodríguez-Almagro J, Hernández-Martínez A, Romero-Blanco C, Martínez-Arce A, Prado-Laguna MD, García-Sanchez FJ. Experiences and Perceptions of Nursing Students during the COVID-19 Crisis in Spain. Int J Environ Res Public Health. 2021;18(19):10459.
Dodek PM, Cheung EO, Burns KEA, et al. Moral distress and other wellness measures in Canadian critical care physicians. Ann Am Thorac Soc. 2021;18(8):1343–51. https://doi.org/10.1513/AnnalsATS.202009-1118OC .
Franza F, Basta R, Pellegrino F, Solomita B, Fasano V. The role of fatigue of compassion, burnout and hopelessness in healthcare: experience in the time of covid-19 outbreak. Psychiatr Danub. 32.
Coşkun Şimşek D, Günay U. Experiences of nurses who have children when caring for COVID-19 patients. Int Nurs Rev. 2021;68(2):219–27. https://doi.org/10.1111/inr.12651 .
Scheibe S, De Bloom J, Modderman T. Resilience during crisis and the role of age: involuntary telework during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(3):1762. https://doi.org/10.3390/ijerph19031762 .
Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc JAMIA. 2020;27(7):1132–5. https://doi.org/10.1093/jamia/ocaa072 .
Afshari D, Nourollahi-darabad M, Chinisaz N. Demographic predictors of resilience among nurses during the COVID-19 pandemic. Work. 2021;68(2):297–303. https://doi.org/10.3233/WOR-203376 .
Monden KR, Gentry L, Cox TR. Delivering bad news to patients. Proc Bayl Univ Med Cent. 2016;29(1):101–2.
Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: a review of current literature. J Nurs Scholarsh. 2016;48(5):456–65. https://doi.org/10.1111/jnu.12229 .
Alharbi J, Jackson D, Usher K. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs. 2020;29(15–16):2762–4. https://doi.org/10.1111/jocn.15314 .
Cohen J, van der Meulen Rodgers Y. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Prev Med. 2020;141:106263.
Institute of Professional Psychology, Bahria University Karachi Campus, Karachi, Pakistan, Waris Nawaz M, Imtiaz S, Quaid-i-Azam University Islamabad, Islamabad, Pakistan, Kausar E, Institute of Professional Psychology, Bahria University Karachi Campus, Karachi, Pakistan. self-care of frontline health care workers: during covid-19 pandemic. Psychiatr Danub. 2020;32(3–4):557–62. https://doi.org/10.24869/psyd.2020.557 .
Mano MS, Morgan G. Telehealth, social media, patient empowerment, and physician burnout: seeking middle ground. Am Soc Clin Oncol Educ Book Am Soc Clin Oncol Annu Meet. 2022;42:1–10. https://doi.org/10.1200/EDBK_100030 .
Myronuk L. Effect of telemedicine via videoconference on provider fatigue and empathy: Implications for the Quadruple Aim. Healthc Manage Forum. 2022;35(3):174–8. https://doi.org/10.1177/08404704211059944 .
Abuhammad S, Alzoubi KH, Al‐Azzam S, et al. Stigma toward healthcare providers from patients during COVID‐19 era in Jordan. Public Health Nurs Boston Mass. Published online March 25, 2022: https://doi.org/10.1111/phn.13071
Nashwan AJ, Valdez GFD, AL-Fayyadh S, et al. Stigma towards health care providers taking care of COVID-19 patients: a multi-country study. Heliyon. 2022;8(4):e09300. https://doi.org/10.1016/j.heliyon.2022.e09300 .
Shiu C, Chen WT, Hung CC, Huang EPC, Lee TSH. COVID-19 stigma associates with burnout among healthcare providers: evidence from Taiwanese physicians and nurses. J Formos Med Assoc Taiwan Yi Zhi. 2022;121(8):1384–91. https://doi.org/10.1016/j.jfma.2021.09.022 .
Griffith AK. Parental burnout and child maltreatment during the COVID-19 Pandemic. J Fam Violence. 2022;37(5):725–31. https://doi.org/10.1007/s10896-020-00172-2 .
Çakmak G, Öztürk ZA. Being both a parent and a healthcare worker in the pandemic: who could be exhausted more? Healthcare. 2021;9(5):564. https://doi.org/10.3390/healthcare9050564 .
Cavanagh N, Cockett G, Heinrich C, et al. Compassion fatigue in healthcare providers: a systematic review and meta-analysis. Nurs Ethics. 2020;27(3):639–65. https://doi.org/10.1177/0969733019889400 .
Boufkhed S, Harding R, Kutluk T, Husseini A, Pourghazian N, Shamieh O. What is the preparedness and capacity of palliative care services in Middle-Eastern and North African Countries to Respond to COVID-19? a rapid survey. J Pain Symptom Manage. 2021;61(2):e13–50. https://doi.org/10.1016/j.jpainsymman.2020.10.025 .
Gelfman LP, Morrison RS, Moreno J, Chai E. Palliative care as essential to a hospital system’s pandemic preparedness planning: how to get ready for the next wave. J Palliat Med. 2021;24(5):656–8. https://doi.org/10.1089/jpm.2020.0670 .
Messerotti A, Banchelli F, Ferrari S, et al. Investigating the association between physicians self-efficacy regarding communication skills and risk of “burnout.” Health Qual Life Outcomes. 2020;18:271. https://doi.org/10.1186/s12955-020-01504-y .
Gribben JL, Kase SM, Waldman ED, Weintraub AS. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric critical care physicians in the United States. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2019;20(3):213–22. https://doi.org/10.1097/PCC.0000000000001803 .
Sengupta M, Roy A, Gupta S, Chakrabarti S, Mukhopadhyay I. Art of breaking bad news: a qualitative study in Indian healthcare perspective. Indian J Psychiatry. 2022;64(1):25–37. https://doi.org/10.4103/indianjpsychiatry.indianjpsychiatry_346_21 .
Cross LA. Compassion fatigue in palliative care nursing: a concept analysis. J Hosp Palliat Nurs. 2019;21(1):21. https://doi.org/10.1097/NJH.0000000000000477 .
Paiva-Salisbury ML, Schwanz KA. Building compassion fatigue resilience: awareness, prevention, and intervention for pre-professionals and current practitioners. J Health Serv Psychol. 2022;48(1):39–46. https://doi.org/10.1007/s42843-022-00054-9 .
Jun 8, information 2020 | For more, Corpuz-Bosshart contact L. ‘Wobble room’ provides time-out for COVID-19 frontliners. UBC News. Published June 8, 2020. Accessed 17 Jan 2023. https://news.ubc.ca/2020/06/08/making-a-difference-wobble-room-provides-time-out-for-covid-19-frontliners/
Gupta N, Dhamija S, Patil J, Chaudhari B. Impact of COVID-19 pandemic on healthcare workers. Ind Psychiatry J. 2021;30(Suppl 1):S282–4. https://doi.org/10.4103/0972-6748.328830 .
Menon GR, Yadav J, Aggarwal S, et al. Psychological distress and burnout among healthcare worker during COVID-19 pandemic in India—a cross-sectional study. PLoS ONE. 2022;17(3):e0264956. https://doi.org/10.1371/journal.pone.0264956 .
Nishimura Y, Miyoshi T, Sato A, et al. Burnout of healthcare workers amid the COVID-19 Pandemic: a follow-up study. Int J Environ Res Public Health. 2021;18(21):11581. https://doi.org/10.3390/ijerph182111581 .
Jemal K, Hailu D, Mekonnen M, Tesfa B, Bekele K, Kinati T. The importance of compassion and respectful care for the health workforce: a mixed-methods study. J Public Health. 2023;31(2):167–78. https://doi.org/10.1007/s10389-021-01495-0 .
Hui L, Garnett A, Oleyniov C, Boamah S. Compassion fatigue in health providers during the COVID-19 pandemic: A scoping review protocol. BMJ Open. 2023;13:e069843. https://doi.org/10.1136/bmjopen-2022-069843 .
Download references
Acknowledgements
I declare that the authors have no competing interests as defined by BMC, or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Author information
Authors and affiliations.
Arthur Labatt Family School of Nursing, Western University, London, ON, Canada
Anna Garnett & Christina Oleynikov
Medical Sciences, Western University, London, ON, Canada
School of Nursing, McMaster University, Hamilton, ON, Canada
Sheila Boamah
You can also search for this author in PubMed Google Scholar
Contributions
AG is responsible for conception and design of the review. AG, LH, CO & SB contributed to the acquisition and analysis of the data. AG, LH & SB interpreted the data. LH drafted the manuscript and AG was a major contributor to the final version of the manuscript. AG, LH, CO & SB read, provided feedback and approved the final manuscript
Corresponding author
Correspondence to Anna Garnett .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was not required because this manuscript is a review of published literature.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Critical appraisals of included articles.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Garnett, A., Hui, L., Oleynikov, C. et al. Compassion fatigue in healthcare providers: a scoping review. BMC Health Serv Res 23 , 1336 (2023). https://doi.org/10.1186/s12913-023-10356-3
Download citation
Received : 07 August 2023
Accepted : 20 November 2023
Published : 01 December 2023
DOI : https://doi.org/10.1186/s12913-023-10356-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Compassion fatigue
- Healthcare provider
- Psychological health
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

- Previous Article
- Next Article
Literature review: The importance of maintaining mental health in facing the Covid-19 pandemic
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Reprints and Permissions
- Cite Icon Cite
- Search Site
Rahma Afifah , Salma Salsabila Az Zahra , Tasya Azalia , Samsul Arifin , F. Faisal; Literature review: The importance of maintaining mental health in facing the Covid-19 pandemic. AIP Conf. Proc. 4 April 2024; 3048 (1): 020025. https://doi.org/10.1063/5.0201953
Download citation file:
- Ris (Zotero)
- Reference Manager
At the end of 2019, the coronavirus or COVID-19, which attacks the respiratory system and can spread quickly, was first discovered in the city of Wuhan, China. There are many impacts caused by COVID-19, one of which affects the psychological health of the community and individuals. The purpose of this literature review is to find out the importance of maintaining mental health in the face of the COVID-19 pandemic. The world community, including Indonesia, has panicked since the World Health Organization (WHO) declared the status of this virus as a pandemic, coupled with the news about the spread of COVID-19 which seemed scary. In tackling this pandemic, the government implemented a lockdown and Large-Scale Social Restrictions (PSBB) which caused significant changes in people’s lifestyles. This also disrupts the economic activities of companies that cause employee layoffs. This situation also causes economic stress and emotional stress such as stress, hopelessness, disappointment, anxiety, restlessness, fear of uncertainty, confusion, post-traumatic stress disorder (PTSD), boredom, and so on. Factors that affect mental health include social isolation and distance, the global economic recession, and physical distancing. Children and adolescents are considered a subgroup that is more prone to experiencing anxiety and stress. Research reveals that mental health is as closely related to an individual’s physical health as it is during the face of COVID-19. Mental health has an important role in maximizing health because the body’s immunity is also influenced by mental health. Therefore, it is important for every individual to maintain his mental health.
Citing articles via
Publish with us - request a quote.
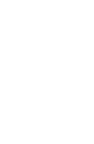
Sign up for alerts
- Online ISSN 1551-7616
- Print ISSN 0094-243X
- For Researchers
- For Librarians
- For Advertisers
- Our Publishing Partners
- Physics Today
- Conference Proceedings
- Special Topics
pubs.aip.org
- Privacy Policy
- Terms of Use
Connect with AIP Publishing
This feature is available to subscribers only.
Sign In or Create an Account
- Systematic Review
- Open access
- Published: 04 April 2024
Effectiveness and cost-effectiveness of community-based mental health services for individuals with severe mental illness in Iran: a systematic review and meta-analysis
- Mozhgan Taban 1 ,
- Sara Nooraeen 2 ,
- Kiarash Tanha 3 ,
- Maziar Moradi-Lakeh 4 &
- Seyed Kazem Malakouti 5
BMC Psychiatry volume 24 , Article number: 256 ( 2024 ) Cite this article
7 Altmetric
Metrics details
Severe mental illness (SMI) imposes a substantial worldwide burden of disability, highlighting the need for comprehensive and adaptable mental health services. This study aims to assess the efficacy and cost-effectiveness of community-based mental health services (CBMHS) in reducing relapse and rehospitalization rates among individuals with SMI in Iran.
A systematic review and meta-analysis were conducted. Medline, EMBASE, ISI, SCOPUS, and ProQuest were searched until December 2022. We focused on randomized controlled trials, quasi-experimental studies, or economic studies related to individuals with SMI. Out of 127 articles, 17 were selected for a full-text review. The primary outcomes were the severity of psychopathology, rehospitalization rates, and the mental health of caregivers. We also examined community-based interventions and their impact on various outcomes. Data extraction and risk of bias assessment were performed, and critical appraisal was conducted using JBI checklists. Meta-analysis was carried out using STATA software. (PROSPERO registration. CRD42022332660).
Rehospitalization rates among patients who received CBMHS were significantly lower, with an odds ratio of 2.14 (95% CI: 1.44 to 3.19), indicating a 2.14 times lower likelihood than those who received treatment as usual. A reduction in psychopathology accompanied this, SMD: -0.31, 95% CI: -0.49 to -0.13, I2 = 40.23%). Moreover, there was a notable improvement in social skills (SMD: -0.7, 95% CI: -0.98 to -0.44, I2 = 0.00%). The burden on caregivers also decreased (SMD: -0.55, 95% CI: -0.99 to -0.1, I2 = 63.2). The Incremental Cost-Effectiveness Ratio (ICER) for QUALY was acceptable, albeit with a wide range of 613 to 8400 Dollars.
CBMHS has demonstrated effectiveness and efficiency in Iran as a developing country. Additionally, it shows promise in mitigating the shortage of acute psychiatry beds. Using multiple data collection tools poses a limitation regarding data consolidation and conducting a meta-analysis.
Peer Review reports
Introduction
Severe mental illness (SMIs) is a prevalent global cause of disability. In 2019, mental disorders contributed to approximately 418 million disability-adjusted life years (DALYS), accounting for 16% of global DALYS. This represents a significant increase compared to previous estimates. The World Health Organization's (WHO) Action Plan (2013–2030) emphasizes establishing inclusive and adaptable community-based mental health and social care services. The goal is to empower individuals affected by these disorders to exercise their full human rights and gain timely access to culturally appropriate, high-quality healthcare and social support. This approach promotes recovery, enables individuals to achieve optimal well-being, actively participate in society and employment, and eliminates stigmatization and discrimination [ 1 ].
Although medication is essential for symptom control and relapse prevention, it is insufficient to address the social needs of patients with severe mental illness. In recent years, there has been notable progress in pharmacotherapy, particularly in managing the acute phase of the disorder, which has subsequently increased the inclination toward providing community-based mental health services (CBMHS) [ 2 , 3 ]. The various aspects of psychiatric disorders, including their health, familial, social, and economic dimensions, also highlight the different CBMHS, such as home visits, outpatient services, community-based rehabilitation, psychological training, family therapy, and other methods. Additionally, it acknowledges the financial burden that SMIs place on families and governments, with an estimated economic impact of approximately USD 5 trillion in 2019 [ 4 ].
Based on the findings of the Iranian Mental Health Survey (IranMHS) conducted in 2011, nearly a quarter of the population experiences psychiatric disorders, of which 3 to 5 presents suffer severe illness [ 5 ]. Furthermore, it emphasizes that these conditions are the leading cause of disability among individuals aged 10 to 40 in Iran [ 6 ].
Studies demonstrate that the provision of CBMHS effectively reduces relapse and rehospitalization rates in patients and alleviates the burden on families. Additionally, by lowering hospitalization and daycare costs, the economic burden associated with SMIS is reduced. However, offering these services in Low- and Middle-Income Countries (LMICS) encounters obstacles related to social, cultural, and financial factors [ 7 ]. In Iran, notable attention has been given to providing comprehensive, integrated, and responsive mental health services in community settings [ 8 ]. Conducted in Iran, it demonstrated a 67% reduction in hospitalization rates after individuals received CBMHS [ 9 ]. There are numerous studies conducted worldwide that have demonstrated the effectiveness and cost–benefit of community-based services [ 10 , 11 , 12 , 13 ]. However, in parallel with the expansion of community-based services, long-term hospitalization and asylum-like services were expanded nationwide in the last two decades. Our intention in this study was not to evaluate these services at the global level, but we checked whether this system works in Iran's cultural, social, and economic conditions, and maybe this Rio systematic is useful for mental health policymakers and shows that the development of these services requires It takes more effort. For this reason, we focused on Iranian studies.
To address the knowledge gap, we conducted a systematic review and meta-analysis of Randomized Clinical Trials (RCTs), quasi-experimental studies, or economic studies to evaluate the cost-effectiveness and cost benefit effectiveness of CBMHS in reducing relapse and rehospitalization rates among patients with SMIs. The findings of this study may have implications not only for future research in Iran but also for neighboring countries.
Eligibility criteria
RCTs, quasi-experimental studies, or economic studies conducted on specific outcomes such as clinical relapse, rehospitalization, cost, and the severity of psychopathology, were included. The intervention on individuals with a diagnosis of psychotic spectrum disorder (schizophrenia, schizophreniform, and other long-lasting psychotic disorders), Bipolar Mood Disorders (BMD), or severe refractory major depression were considered were considerd.
Amongst them, studies with any community-based intervention, including home-visit services (by professionals or peers and family members), telephone follow-up, family psychoeducation, and skill training, and the studies which aim the caregivers' knowledge, burden, and mental conditions as by proxy groups to have an impact on SMI clinical outcome were included.
Rehospitalization, relapses, clinical condition and severity of the symptoms, treatment adherence, economic outcomes including QALYS, CER (Cost-Effectiveness Ratio), social functioning, quality of life, and family knowledge were outcomes of interest.
Exclusion criteria were any studies performed on individuals with substance use disorders, intellectual disability, brain trauma, or; the intervention model was not transparent and did not have a follow-up interval.
The study protocol had been approved by the Ethics Committee of the Iran University of Medical Sciences (code: IR.IUMS.REC.1400.733) and registered in PROSPERO. (CRD42022332660, available here: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022332660 .)
Search strategy
We systematically reviewed the published literatures on the intervention models for SMIs in Iran. This review includes all RCTs, quasi-experimental studies, or economic studies reporting on the effectiveness and cost-effectiveness of community-based care and interventions designed to promote social engagement among individuals with SMI.
The search was conducted for articles published in English using databases such as Medline, EMBASE, ISI, SCOPUS, and ProQuest. Additionally, peer-reviewed papers in the Persian language, were accessed via Iranian websites including SID, MAGIRAN, and Iran doc. Our search terms (keywords and Mesh terms) reflected central concepts: severe mental illness, models of intervention, outcome, and relapse. We limited our search to publications in English and Persian available in full text. If the full text was not available, the authors were contacted. publications included in the study were published until December 2022, the complete search strategy can be found in the Supplementary Material 1 : Appendix.
Since this study aimed to estimate the effectiveness of CBMHS, and some of the included articles used alternative versions of the questionnaires, we excluded the data from alternative versions. We extracted the relevant data by carefully studying the tables and text.
Screening and data extraction
Two independent reviewers (S.N., M.T.) assessed article titles and abstracts to exclude unrelated records. The full text of the remaining studies was also reviewed independently by S.N. and M.T., with unrelated articles being excluded. Any disagreements were resolved through discussion and judgment by the principal investigator (SK.M.).
A pre-designed data sheet was completed for each of the included studies. Data extraction from each included paper was performed by two independent authors (S.N., M.T.) based on the author's name, publication year, journal name, study population, city of the study population, sex, sample size, type of intervention, and tools.
Risk of bias assessment
The relevant JBI critical appraisal checklist regarding the study designs (i.e., RCT, quasi-experimental, and economic evaluation) was used to evaluate the articles. JBI critical appraisal Checklist for RCTs has 13 questions evaluating different methodological aspects of an RCT, including randomization, concealed allocation, blinding, follow-up, and analysis (all versions of JBI available: https://jbi.global/critical-appraisal-tools ) .
Statistical analysis
To ensure comparable results, we calculated Standardized Mean Differences (SMD) and 95% confidence interval between the intervention and control groups [ 10 ]. SMDs were calculated, where available, to assess the intervention's effectiveness during the follow-up period (i.e., a pre-post comparison in the experimental group) and to measure the differences between the experimental and control groups at the follow-up time (i.e., calculated as the post–pre-experimental mean minus the post–pre control mean). The odds ratio and 95% confidence interval were calculated to compare the rehospitalization rate between the groups.
The data were analyzed using STATA, version 17.0 (STATA Corporation, College Station, TX, USA). The statistical heterogeneity between the studies was assessed using the I2 statistic, which was able to measure the inconsistency across the results of the studies and describe the proportion of the total variations based on their estimates due to the presence of heterogeneity rather than sampling errors. A random-effects model was used if heterogeneity was observed (the I2 values > 50).
Seventy-one articles were selected through the English-language website, and fifty-six Persian-language articles were selected through the Iranian website. After removing duplicates, 115 articles remained. In the next steps, the titles and abstracts were reviewed, and 84 articles were excluded. The full text of thirty-one articles was reviewed, of which 14 unrelated articles were excluded. Finally, 17 English and Persian articles were included in the study (Fig. 1 ).
PRISMA flow chart to illustrate the article search and selection process
Critical appraisal and risk of bias assessment
The results of the risk of bias and critical appraisal in the qualitative assessment of the articles are as follows. We have 8 experimental articles that meet the inclusion criteria for our study. These articles were selected based on their relevance to our research question and their adherence to our predetermined criteria for experimental design. We evaluated the articles based on the JBI critical appraisal checklist (Fig. 2 ). Question four (Were participants blind to treatment assignment?) And question five (Were those delivering treatment blind to treatment assignment?) Were not applicable for most of the studies as in the communicate based intervention it is not feasible for the participants and the person who deliver the services to be blind of interventions. The rest of the items were enough qualified to rely on the results (Fig. 2 ). The result of the quasi experimental and economy studies checklists depicted in the Supplementary Material 1 :Appendix.
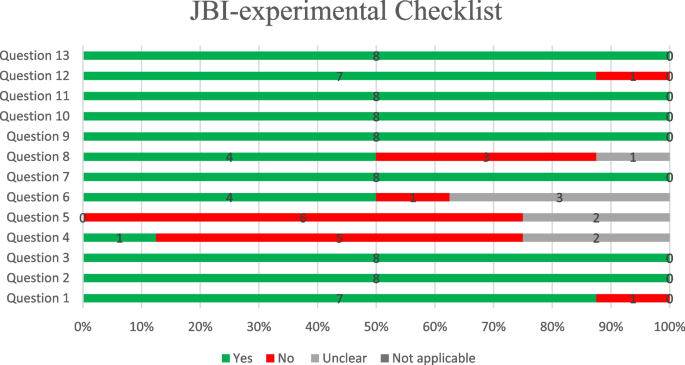
Quality assessment of experimental studies
The demographic characteristics of included articles
Demographic characteristics of included articles revealed Table 1 .
The results of intervention comparing before and after 12-months follow-up presented. The findings related to the tools used in intervention studies are presented in Table 2 . As noted, most tools reported a weak level of heterogeneity(I 2 ), so the meta-analysis has not been performed. The meta-analysis was conducted for rehospitalization, PANSS (Positive and Negative Syndrome Scale) as a psychopathology assessment tool and KELS (Kohlman Evaluation of Living Skills of the patients) and FEIS variables indicating psychological distress in caregivers.
The rehospitalization rate
One of the study's primary goals was to evaluate the effect of any CBMHS on rehospitalization after the index discharge. The CBMHS included home-visit and telephone follow-ups, the rehospitalization rate among patients who received CBMHS (with a total of 595 participants in both intervention and control groups) was 2.14 times lower compared to those who received treatment as usual (OR: 2.14,95%CI: 1.44, 3.19). Mohebi [ 17 ] was the only article that used Medication Adherence Rating Scale (MARS) to evaluate the compliance of the patient with treatment (SMD: 3.15, CI: 95% 2.31, 3.98). The result of the meta-analysis of rehospitalization among four studies showed in Fig. 3 . There was not any publication bias. It shown as Fig. 4 .
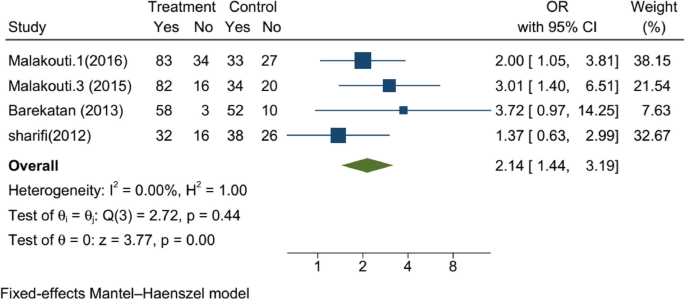
The result of the meta-analysis of rehospitalization among four studies
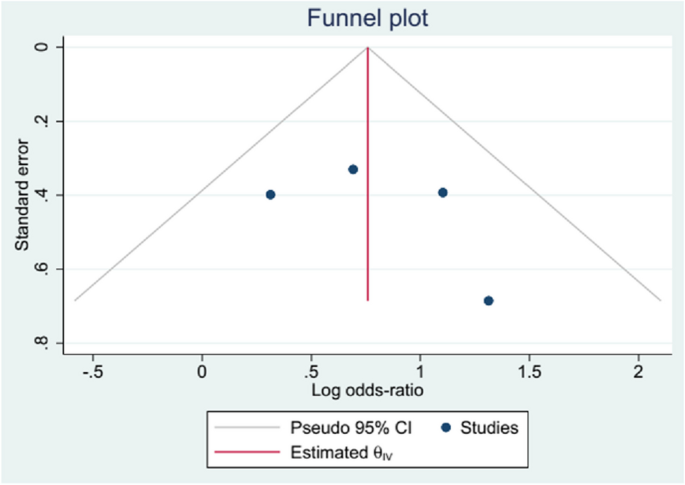
Funnel plot, publication bias for rehospitalization in studies
Severity of psychopathology
Out of 17 studies, 5 used PANSS to evaluate the effect of intervention on psychopathology, whose data were amenable to analysis (with a total of 669 participants in both intervention and control groups). Meta-analysis shows that after 12 months of intervention, CBMHS are successful in reducing significantly of the severity of psychopathology (SMD: -0.31, 95%CI: -0.49 to -0.13, I 2 = 40.23%). Akbari [ 18 ] was the only one that used ANSQ -Anderson Negative Symptoms- (SMD: -0.581, 95%CI: -1.312, 0.149). The meta-analysis of the studies for PANSS showed in Fig. 5 .
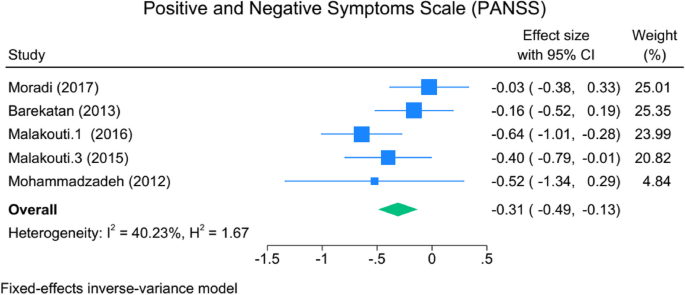
The meta-analysis of the studies for PANSS
The result of meta-analysis on the YOUNG (evaluating the severity of Bipolar mood disorder) shows significant difference by implementing the intervention (SMD: -0.764, 95% CI: -1.274, -0.253, I 2 = 85.22%), however the heterogeneity among four studies were not acceptable.
Upon visual examination of the funnel plot, no significant signs of asymmetry were observed (located in the Supplementary Material 1 : Appendix).
Social skills as secondary outcomes of the study could be considered as one of the outcomes of any intervention that aims to help the patient to be as independent as possible in the family and society. Just two studies used KELS to evaluate the social skills of the patients. The result of KELS shows a high effect size (SMD: -0.7, 95%CI: -0.98 to -0.44, I2 = 0.00%), and the community-based interventions are more promising. The same result was revealed by the study of Shahmiri (2014) by Matson evaluation of social skills (MESS) (SMD: -0.877, 95%CI: -1.749, 0.041) (lower scores indicating better functioning).
The tools of ACIS Assessment of Communication and Interaction Skills (mean difference 1.747 (CI: 1.08, 2.41).) Higher scores indicate better skills, such as DSK Dehbozorgi's social skills (SMD: 0.835, 95%CI: 0.088, 1.581). (Lower scores indicate lower social skills).
The burden of the caregivers was evaluated by FEIS (evaluating the burden of the caregivers) in the meta-analysis (not shown in the article). It shows that again in the two articles, the effect size was -0.55 (SMD: -0.55, 95%CI: -0.99, -0.1, I2 = 63.2) (in favor of community-based services.
For the CSQ, which evaluated the satisfaction of the clients from the services, there were not any significant differences with the control group. In the study of Sharifi [ 14 ], the quality of life of (WHOQOL) patients has been improved marginally (SMD:-0.246, 95%CI: -0.500, 0.007) ( P = 0.057). However, in the study of Hojati- Abad [ 27 ] WQOLCQ (Wisconsin Quality of Life Client Questionnaire (SMD: 0.798, 95%CI: 0.29, 5, 1.301), there was not any significant difference.
Economic evaluation studies
For economic evaluation we considered tow indexes reported incremental cost-effectiveness ratios (ICER) [ 28 ] and Quality-Adjusted Life Year (QUALY) [ 29 , 30 ], which is are more common indexes economic evaluation.
The QALY serves as a metric for assessing the worth of health outcomes. As health is contingent upon both lifespan and well-being, the QALY was formulated as an endeavor to amalgamate the value of these attributes into a solitary index. In the field of mental health, improving the quality of life for patients and reducing the burden of the disease not only for the patients themselves but also for their families and society as a whole. QALYs can be integrated with medical expenses to derive a final universal measure of cost/QALY. This parameter facilitates the comparison of the cost-effectiveness of various treatments without bias.
In numerous healthcare systems, determinations regarding the reimbursement and availability of new medications hinge upon health technology assessments. These assessments, involve the evaluation of an ICER. Decision-makers then weigh the ICER against a predetermined benchmark for cost-effectiveness, referred to as the cost-effectiveness threshold (CET), in order to ascertain whether reimbursement should be granted or withheld [ 28 ].
We identified two reports that met our inclusion criteria concerning economic evaluations of community-based interventions to improve the mental health of individuals with SMI [ 13 , 21 ]. In both studies were included QUALY and ICER.
Malakouti et al. ICER for aftercare home services following the discharge of individuals with SMI. Their analysis was based on a 12-month follow-up of participants in a clinical trial conducted between 2007 and 2008. They found that the ICER was 5.7 million Rials (IRR) per QALY when using general practitioners (GPs) as care providers during home visits and 5.0 million IRR per QALY when replacing GPs with nurses [ 13 ]. In a separate study, Moradi-Lakeh et al. conducted a cost-utility analysis of aftercare services following the discharge of individuals hospitalized for SMI. Their analysis was based on a clinical trial performed from 2012 to 2014, with a 20-month follow-up. They reported an ICER of US$8,399 (95% CI: 8,178–8,620) per QALY for the intervention [ 13 ]. It is worth noting that the services provided by the second study were more comprehensive. In these two studies showed that community-based interventions can be useful in terms of cost–benefit and cost-effectiveness.
While the ICER measures in these two studies differed considerably (partly due to a significant fluctuation in IRR-USD exchange rates $1 = 935 to 10,402 IRR, and other services provided by the second study included the expenses of general psychologists, supervising psychiatrists, as well as the costs of weekly co-ordination meetings of home visit teams, costs of classes for caregivers' education, training of social skills), both were found to be below the World Health Organization's recommended threshold for cost-effectiveness of health interventions [ 13 , 21 ]. The second study aimed to provide the cheapest and most effective intervention and evaluated the feasibility of providing such CBMHS. However, from $ 613 to $8400, it is feasible to provide such services while considering the exchange and inflation rates.
Out of 127 English and Persian language articles which were conducted in IRAN, seventeen met the eligibility criteria for inclusion in the systematic review and meta-analysis. community-based services effectively reduced rehospitalizations by 2times. reduction in psychopathology with moderate effect sizes. economic cost-effectiveness, with ICER values falling below the recommendations set by the WHO s.
Community psychiatry was launched in the USA in 1970 [ 31 ], community psychiatry was launched in the USA in 1970 [ 31 ] Reducing hospitalization, enabling individuals to have an active social life in society [ 32 ], and providing holistic care are among the main goals of community psychiatry community psychiatry was launched in the USA in 1970 [ 31 ].
CBMHS, including home visits, telephone follow-ups, case management systems, intensive care systems, and other CBMHS developed in different societies, have emerged and expanded to address this new challenge [ 32 ]. Even in a crisis, CBMHS mobile crisis intervention can reduce the number of readmissions [ 33 ]. Providing and connecting discharged patients to community services as soon as possible is a critical issue to prevent readmission [ 34 ].
On the other hand, the evidence shows that the direct daily costs for community-based social psychiatric care were about half the costs of inpatient treatment over the entire period [ 34 , 35 ]. However, reducing the number of readmissions depends on the intensity of community services, and it may yield different results in some societies [ 36 ].
Some reasons may be nominated for reduction of rehospitalization [ 37 , 38 ]. However, compared with the developed societies, we need to examine this issue from a dual perspective. First, in addition to having social activities and supporting the patients to have an almost independent life, second, the shortage of psychiatric beds is an essential matter in our country's mental health services. According to the according recommended assesment, we should have forty more than 56 thousand psychiatric beds in Iran [ 39 , 40 ] which falls behindrrrr. With the best estimation, we have thirty thousand psychiatric beds, of which fifty percent belong to the Welfare Organization for long-term hospitalization and rehabilitation [ 40 ]. Therefore, an extension of CBMHS psychiatry could help the patient and their family but also help the national mental health service to compensate for the shortage of facilities. Exacerbating the severity of psychopathology could increase the odd behaviors and tension in the family, leading to the patient's hospitalization [ 41 , 42 ]. Reducing the severity of psychopathology, as revealed in the study results as the severity of PANSS and YMRS in the current study, could be helpful. Increasing adherence to medication due to frequent contact (in person or by telephone) encourages the patient to comply with the treatment, which is the main reason for reducing the severity of psychopathology.
Having a long-duration mental health stability state without exacerbation of the symptoms, in addition to psychoeducation and behavioral rehearsal, which is part of community-based intervention, could provide suitable opportunities for the patient to retrieve his/her behavioral skills or learn new skills, which are necessary for independent living [ 43 , 44 ]. Social skills, evaluated by KELS and MESS, showed promising outcomes for CBMHS with remarkable effect size. However, gaining social skills requires intense and close supervision, which any community-based intervention may not obtain, as shown by the study of Jamshidi [ 25 ]; the results of this study are controversial ACIS.
The burden and mental health of the caregivers for chronic diseases such as schizophrenia, bipolar mood disorder, and dementia are essential in mental health services. Given that in developing countries [ 45 , 46 ], taking care of patients is on the shoulders of the families, providing aftercare services and regular contact with the patient and the caregivers could help them overcome the long-lasting problems in their family. The reduction of burden and improvement of the mental health condition of the caregivers show that such services have a positive impact on them [ 44 ].
Satisfaction with the services and quality of life, which did not exhibit significant differences from the control group in our study, remains a topic of extensive debate. Satisfaction and quality of life depend on physical and mental health and suitable living conditions such as housing, jobs, and income, which are not fulfilled by community-based services and are beyond the scope of these services and require intersectoral collaboration [ 12 , 21 , 38 ].
The challenge of the studies performed in Iran as CBMHS was using multiple tools with similar goals to evaluate corresponding variables. This hinders the ability to compare and analyze the results effectively. For instance, the study employed four different tools to measure life skills. Also, despite the history of CBMHS in Iran, there is a lower publication rate for the results of these interventions and programs. The expectation of having more articles that evaluate this specific area emphasizes the need for attention to be given to this issue.
The findings of community-based studies in Iran, although rare, showed that in line with international studies, this type of service is compatible and effective in Iran's economic, social, and cultural conditions. Even though there are challenges regarding patient satisfaction and organizational interdepartmental cooperation. These findings emphasize that community-based services not only in Iran but also in similar countries should be preferred over long-term inpatient services.
Availability of data and materials
This is an evidence synthesis study, all data is available from the primary research studies, or can be circulated from the corresponding author.
Singh OP. Comprehensive mental health action plan 2013–2030: we must rise to the challenge. Indian J Psychiatry. 2021;63:5415–7.
Article Google Scholar
Ojha SP, Pant SB. Community based rehabilitation for task shifting in mental health. J Psychosoc Rehabil Ment Health. 2018;5:109–10.
Keegan J. Community-based mental health care: bridging the gap between community care and primary care. Aust N Z J Ment Health Nurs. 1998;7(3):95–102.
CAS PubMed Google Scholar
Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. EClinicalMedicine. 2022;54.
Sharifi V, Amin-Esmaeili M, Hajebi A, Motevalian A, Radgoodarzi R, Hefazi M, et al. Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian Mental Health Survey, 2011. Arch Iran Med. 2015;18(2):76–84.
PubMed Google Scholar
Forouzanfar MH, Sepanlou SG, Shahraz S, Dicker D, Naghavi P, Pourmalek F, et al. Evaluating causes of death and morbidity in Iran, global burden of diseases, injuries, and risk factors study 2010. Arch Iran Med. 2014;17(5):304–20.
Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental health service provision in low-and middle-income countries. Health Serv Insights. 2017;10:1178632917694350.
PubMed PubMed Central Google Scholar
Sharifi V, Abolhasani F, Farhoudian A, Amin-Esmaeili M. Community mental health centers in Iran: planning evidence-based services. Iran J Psychiatry Clin Psychol. 2014;19(3):163–76.
Google Scholar
Malakouti SK, Nojomi M, Panaghi L, Chimeh N, Mottaghipour Y, Joghatai MT, et al. Case-management for patients with schizophrenia in Iran: a comparative study of the clinical outcomes of mental health workers and consumers’ family members as case managers. Community Ment Health J. 2009;45:447–52.
Article PubMed Google Scholar
Andrade C. Mean difference, Standardized Mean Difference (SMD), and their use in meta-analysis: as simple as it gets. J Clin Psychiatry. 2020 2020/09//; 81(5):[20f13681 p.]. Available from: http://europepmc.org/abstract/MED/32965803. https://www.psychiatrist.com/read-pdf/11349 . https://doi.org/10.4088/JCP.20f13681 .
Barekatain M, Maracy MR, Rajabi F, Baratian H. Aftercare services for patients with severe mental disorder: a randomized controlled trial. J Res Med Sci. 2014;19(3):240–5.
Malakouti SK, Nojomi M, Mirabzadeh A, Mottaghipour Y, Zahiroddin A, Kangrani HM. A comparative study of nurses as case manager and telephone follow-up on clinical outcomes of patients with severe mental illness. Iran J Med Sci. 2016;41(1):19–27.
Moradi-Lakeh M, Yaghoubi M, Hajebi A, Malakouti SK, Vasfi MG. Cost-effectiveness of aftercare services for people with severe mental disorders: an analysis parallel to a randomised controlled clinical trial in Iran. Health Soc Care Community. 2017;25(3):1151–9.
Sharifi V, Tehranidoost M, Yunesian M, Amini H, Mohammadi M, Jalali RM. Effectiveness of a low-intensity home-based aftercare for patients with severe mental disorders: a 12-month randomized controlled study. Community Ment Health J. 2012;48(6):766–70.
Babokani ZS, Ghazanfari A, Ahmadhi R, Chorami M. The comparison of the effectiveness of behavioral activation and psychosocial on mental cognitive functions in women with chronic schizophrenia. Q J Psychol Stud. 2020;15(4):91–108.
Malakouti SK, Chimeh N, Panaghi L, AhmadAbadi Z, Nojomi M. The effectiness of two case management methods on mental health, knowledge, and burden of schizophernics. Family Member Fam Res. 2009;5(17):29–42.
Mohebi P, Fallahi-Khoshknab M, Rahgoi A, Tabrizi K, Khodaei-Ardakani M-R. Effect of the community re-entry program on medication adherence in patients with bipolar disorder type I. Iran J Rehabil Res Nurs. 2017;3:58–65.
Akbari M, Saeidi S. The effectiveness of psychosocial rehabilitation in reducing negative symptoms and improving social skills of chronic schizophrenia patients. Shenakht J Psychol Psychiatry. 2017;4(3):21–35.
Fayyazi Bordbar MR, Soltanifar A, Talaei A. Short-term family-focused psycho-educational program for bipolar mood disorder in Mashhad. Iran J Med Sci. 2009;34.
Ahmadi A, Farahbakhsh K, Moatamedy A, Khodaei M, Safi MH. The effectiveness of family psychological training on prevention of recurrence of symptoms in patients with schizophrenia spectrum disorders. Iran J Psychiatr Nurs. 2020;8(3):93–103.
Malakouti SK, Mirabzadeh A, Nojomi M, Ahmadi Tonkaboni A, Nadarkhani F, Mirzaie M, et al. Clinical outcomes and cost effectiveness of two aftercare models provided by general physicians and nurses to patients with severe mental illness. Med J Islam Repub Iran. 2015;29:196.
Shahmir E, Talebizadeh M, Jafarifard S. The effectiveness of the returning to society program in improving the social skills of schizophrenic patients. Thoughts Behav Clin Psychol. 2014;9(31):27–36.
Mohammadzadeh Nanehkaran S, Karbalaie Noori A, Hosseini SA. Effect of Community Re-entry Program (CRM) in patients with schizophrenia. Arch Rehabil. 2013;14(2):22–8.
Fallahi-Khoshknab M. Effectiveness of Psychiatric Nursing Home Care Services for Psychiatric Status in Schizophrenics. Arch Rehabil. 2007;8:77–81.
Jamshidi F, Shayan A, Forouhari S, Taherkhani H, Seyedi M. The effect of community Re-entry program (CRP) on social function of patients with chronic mental disorders. Acta Med Mediterr. 2016;32(Specia):1311–6.
Dashtbozorgi B, Ghadirian F, Khajeddin N, Karatni K. Effect of family psychoeducation on the level of adaptation and improvement of patients with mood disorders. Iran J Psychiatry Clin Psychol. 2009;15(2):193–200.
Hojjati-Abed E, Karbalaaei-nouri A, Rafiei H, Karimlou M. The efficacy of psychosocial occupational therapy services on quality of life of chronic pschiatric patents. Arch Rehabil. 2010;11(1):0.
Berdud M, Ferraro J, Towse A. A theory on ICER pricing and optimal levels of cost-effectiveness thresholds: a bargaining approach. Front Health Serv. 2023;3:1055471.
Article PubMed PubMed Central Google Scholar
Prieto L, Sacristán JA. Problems and solutions in calculating quality-adjusted life years (QALYs). Health Qual Life Outcomes. 2003;1:80.
Rand LZ, Kesselheim AS. Controversy over using quality-adjusted life-years in cost-effectiveness analyses: a systematic literature Review. Health Aff (Millwood). 2021;40(9):1402–10.
Dean C, Phillips J, Gadd E, Joseph M, England S. Comparison of community based service with hospital based service for people with acute, severe psychiatric illness. Br Med J. 1993;307(6902):473–6.
Article CAS Google Scholar
Kisely S, Yu D, Maehashi S, Siskind D. A systematic review and meta-analysis of predictors and outcomes of community treatment orders in Australia and New Zealand. Aust N Z J Psychiatry. 2021;55(7):650–65.
Guo S, Biegel DE, Johnsen JA, Dyches H. Assessing the impact of community-based mobile crisis services on preventing hospitalization. Psychiatr Serv. 2001;52(2):223–8.
Article CAS PubMed Google Scholar
Haywood TW, Kravitz HM, Grossman LS, Cavanaugh JL, Davis JM, Lewis DA. Predicting the" revolving door" phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. Am J Psychiatry. 1995.
Bachrach LL. Deinstitutionalisation: promises, problems and prospects. Ment Health Serv Eval. 1996:3–18.
Sytema S, Burgess P, Tansella M. Does community care decrease length of stay and risk of rehospitalization in new patients with schizophrenia disorders? A comparative case register study in Groningen, The Netherlands; Victoria, Australia; and South-Verona. Italy Schizophr Bull. 2002;28(2):273–81.
Joynt KE, Sarma N, Epstein AM, Jha AK, Weissman JS. Challenges in reducing readmissions: lessons from leadership and frontline personnel at eight minority-serving hospitals. Jt Comm J Qual Patient Saf. 2014;40(10):435–7.
Phillips MS, Steelesmith DL, Campo JV, Pradhan T, Fontanella CA. Factors associated with multiple psychiatric readmissions for youth with mood disorders. J Am Acad Child Adolesc Psychiatry. 2020;59(5):619–31.
Allison S, Bastiampillai T, Licinio J, Fuller DA, Bidargaddi N, Sharfstein SS. When should governments increase the supply of psychiatric beds? Mol Psychiatry. 2018;23(4):796–800.
Malakouti SK, Keshavarz Akhlaghi A, Shirzad F, Rashedi V, Khlafbeigi M, Moradi Lakeh M, et al. Urban mental health initiative: developing interdisciplinary collaboration, the role of the family physician in management of severe mentally ill patients. Iran J Psychiatry Clin Psychol. 2021;27(1):104–19.
Hinojosa-Marqués L, Domínguez-Martínez T, Barrantes-Vidal N. Family environmental factors in at-risk mental states for psychosis. Clini Psychol Psychother. 2022;29(2):424–54.
Kuhney FS, Miklowitz DJ, Schiffman J, Mittal VA. Family-based psychosocial interventions for severe mental illness: social barriers and policy implications. Policy Insights Behav Brain Sci. 2023;10(1):59–67.
de Pablo GS, De Micheli A, Nieman DH, Correll CU, Kessing LV, Pfennig A, et al. Universal and selective interventions to promote good mental health in young people: systematic review and meta-analysis. Eur Neuropsychopharmacol. 2020;41:28–39.
Estrada-Fernández ME, Gil-Lacruz M, Gil-Lacruz AI, Viñas-López A. The impact of community care: burden and quality of life of the informal caregivers of patients with severe mental disorder. J Community Psychol. 2022;50(1):487–501.
Ofovwe CE, Osasona SO. Burden of caregiving among caregivers of patients with severe mental illnesses in Benin City. Nigeria Afr Health Sci. 2022;22(2):657–67.
Ahmadzadeh Asl M, Shojaee A, Shariati B, Rasoolian M, Rashedi V. A comparative study on the burden of disease of schizophrenia, bipolar disorder type I, and autism spectrum disorder on the family caregivers in Iran. Arch Rehabil. 2021;22(3):320–41.
Download references
Acknowledgements
Not applicable.
The current study has been financially supported by the Iran University of Medical Sciences (Registration number: IR.IUMS.REC. 1400–1-99–21128). The funders had no role in the study implementation, data collection and analysis, or interpretation of study results.
Author information
Authors and affiliations.
Mental Health Research Center, Psychosocial Health Research Institute, Iran University of Medical Sciences, Tehran, Iran
Mozhgan Taban
Department of Psychiatry and Psychology, Mayo Clinic, Rochester, MN, USA
Sara Nooraeen
Oxford Vaccine Group, Department of Pediatrics, University of Oxford, Oxford, U.K.
Kiarash Tanha
Gastrointestinal and Liver Disease Research Center (GILDRC), Iran University of Medical Sciences, Tehran, Iran
Maziar Moradi-Lakeh
Geriatric Mental Health Research Center, School of Behavioral Sciences and Mental Health, Iran University of Medical Sciences, Tehran, Iran
Seyed Kazem Malakouti
You can also search for this author in PubMed Google Scholar
Contributions
Conceived the project (SKM); Developed the protocol (SKM, SN, KT, MT); Carried out the searches (SN, MT, KT), carried out the synthesis (MT, SN), Interpreted the findings (SKM, MT, KT), drafted the manuscript (SKM, MT), approved the manuscript (SKM). SKM is the guarantor of this review. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Seyed Kazem Malakouti .
Ethics declarations
Ethics approval and consent to participate.
The study protocol had been approved by the Ethics Committee of the Iran University of Medical Sciences (code: IR.IUMS.REC.1400.733) and about consent and participate: Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Taban, M., Nooraeen, S., Tanha, K. et al. Effectiveness and cost-effectiveness of community-based mental health services for individuals with severe mental illness in Iran: a systematic review and meta-analysis. BMC Psychiatry 24 , 256 (2024). https://doi.org/10.1186/s12888-024-05666-7
Download citation
Received : 10 November 2023
Accepted : 07 March 2024
Published : 04 April 2024
DOI : https://doi.org/10.1186/s12888-024-05666-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Effectiveness
- Cost-effectiveness
- Community-based mental health services
- Severe mental illness
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
Revolutionizing the Study of Mental Disorders
March 27, 2024 • Feature Story • 75th Anniversary
At a Glance:
- The Research Domain Criteria framework (RDoC) was created in 2010 by the National Institute of Mental Health.
- The framework encourages researchers to examine functional processes that are implemented by the brain on a continuum from normal to abnormal.
- This way of researching mental disorders can help overcome inherent limitations in using all-or-nothing diagnostic systems for research.
- Researchers worldwide have taken up the principles of RDoC.
- The framework continues to evolve and update as new information becomes available.
President George H. W. Bush proclaimed the 1990s “ The Decade of the Brain ,” urging the National Institutes of Health, the National Institute of Mental Health (NIMH), and others to raise awareness about the benefits of brain research.
“Over the years, our understanding of the brain—how it works, what goes wrong when it is injured or diseased—has increased dramatically. However, we still have much more to learn,” read the president’s proclamation. “The need for continued study of the brain is compelling: millions of Americans are affected each year by disorders of the brain…Today, these individuals and their families are justifiably hopeful, for a new era of discovery is dawning in brain research.”

Still, despite the explosion of new techniques and tools for studying the brain, such as functional magnetic resonance imaging (fMRI), many mental health researchers were growing frustrated that their field was not progressing as quickly as they had hoped.
For decades, researchers have studied mental disorders using diagnoses based on the Diagnostic and Statistical Manual of Mental Disorders (DSM)—a handbook that lists the symptoms of mental disorders and the criteria for diagnosing a person with a disorder. But, among many researchers, suspicion was growing that the system used to diagnose mental disorders may not be the best way to study them.
“There are many benefits to using the DSM in medical settings—it provides reliability and ease of diagnosis. It also provides a clear-cut diagnosis for patients, which can be necessary to request insurance-based coverage of healthcare or job- or school-based accommodations,” said Bruce Cuthbert, Ph.D., who headed the workgroup that developed NIMH’s Research Domain Criteria Initiative. “However, when used in research, this approach is not always ideal.”
Researchers would often test people with a specific diagnosed DSM disorder against those with a different disorder or with no disorder and see how the groups differed. However, different mental disorders can have similar symptoms, and people can be diagnosed with several different disorders simultaneously. In addition, a diagnosis using the DSM is all or none—patients either qualify for the disorder based on their number of symptoms, or they don’t. This black-and-white approach means there may be people who experience symptoms of a mental disorder but just miss the cutoff for diagnosis.
Dr. Cuthbert, who is now the senior member of the RDoC Unit which orchestrates RDoC work, stated that “Diagnostic systems are based on clinical signs and symptoms, but signs and symptoms can’t really tell us much about what is going on in the brain or the underlying causes of a disorder. With modern neuroscience, we were seeing that information on genetic, pathophysiological, and psychological causes of mental disorders did not line up well with the current diagnostic disorder categories, suggesting that there were central processes that relate to mental disorders that were not being reflected in DMS-based research.”
Road to evolution
Concerned about the limits of using the DSM for research, Dr. Cuthbert, a professor of clinical psychology at the University of Minnesota at the time, approached Dr. Thomas Insel (then NIMH director) during a conference in the autumn of 2008. Dr. Cuthbert recalled saying, “I think it’s really important that we start looking at dimensions of functions related to mental disorders such as fear, working memory, and reward systems because we know that these dimensions cut across various disorders. I think NIMH really needs to think about mental disorders in this new way.”
Dr. Cuthbert didn’t know it then, but he was suggesting something similar to ideas that NIMH was considering. Just months earlier, Dr. Insel had spearheaded the inclusion of a goal in NIMH’s 2008 Strategic Plan for Research to “develop, for research purposes, new ways of classifying mental disorders based on dimensions of observable behavior and neurobiological measures.”
Unaware of the new strategic goal, Dr. Cuthbert was surprised when Dr. Insel's senior advisor, Marlene Guzman, called a few weeks later to ask if he’d be interested in taking a sabbatical to help lead this new effort. Dr. Cuthbert soon transitioned into a full-time NIMH employee, joining the Institute at an exciting time to lead the development of what became known as the Research Domain Criteria (RDoC) Framework. The effort began in 2009 with the creation of an internal working group of interdisciplinary NIMH staff who identified core functional areas that could be used as examples of what research using this new conceptual framework looked like.
The workgroup members conceived a bold change in how investigators studied mental disorders.
“We wanted researchers to transition from looking at mental disorders as all or none diagnoses based on groups of symptoms. Instead, we wanted to encourage researchers to understand how basic core functions of the brain—like fear processing and reward processing—work at a biological and behavioral level and how these core functions contribute to mental disorders,” said Dr. Cuthbert.
This approach would incorporate biological and behavioral measures of mental disorders and examine processes that cut across and apply to all mental disorders. From Dr. Cuthbert’s standpoint, this could help remedy some of the frustrations mental health researchers were experiencing.
Around the same time the workgroup was sharing its plans and organizing the first steps, Sarah Morris, Ph.D., was a researcher focusing on schizophrenia at the University of Maryland School of Medicine in Baltimore. When she first read these papers, she wondered what this new approach would mean for her research, her grants, and her lab.
She also remembered feeling that this new approach reflected what she was seeing in her data.
“When I grouped my participants by those with and without schizophrenia, there was a lot of overlap, and there was a lot of variability across the board, and so it felt like RDoC provided the pathway forward to dissect that and sort it out,” said Dr. Morris.
Later that year, Dr. Morris joined NIMH and the RDoC workgroup, saying, “I was bumping up against a wall every day in my own work and in the data in front of me. And the idea that someone would give the field permission to try something new—that was super exciting.”
The five original RDoC domains of functioning were introduced to the broader scientific community in a series of articles published in 2010 .
To establish the new framework, the RDoC workgroup (including Drs. Cuthbert and Morris) began a series of workshops in 2011 to collect feedback from experts in various areas from the larger scientific community. Five workshops were held over the next two years, each with a different broad domain of functioning based upon prior basic behavioral neuroscience. The five domains were called:
- Negative valence (which included processes related to things like fear, threat, and loss)
- Positive valence (which included processes related to working for rewards and appreciating rewards)
- Cognitive processes
- Social processes
- Arousal and regulation processes (including arousal systems for the body and sleep).
At each workshop, experts defined several specific functions, termed constructs, that fell within the domain of interest. For instance, constructs in the cognitive processes domain included attention, memory, cognitive control, and others.
The result of these feedback sessions was a framework that described mental disorders as the interaction between different functional processes—processes that could occur on a continuum from normal to abnormal. Researchers could measure these functional processes in a variety of complementary ways—for example, by looking at genes associated with these processes, the brain circuits that implement these processes, tests or observations of behaviors that represent these functional processes, and what patients report about their concerns. Also included in the framework was an understanding that functional processes associated with mental disorders are impacted and altered by the environment and a person’s developmental stage.
Preserving momentum
Over time, the Framework continued evolving and adapting to the changing science. In 2018, a sixth functional area called sensorimotor processes was added to the Framework, and in 2019, a workshop was held to better incorporate developmental and environmental processes into the framework.;
Since its creation, the use of RDoC principles in mental health research has spread across the U.S. and the rest of the world. For example, the Psychiatric Ratings using Intermediate Stratified Markers project (PRISM) , which receives funding from the European Union’s Innovative Medicines Initiative, is seeking to link biological markers of social withdrawal with clinical diagnoses using RDoC-style principles. Similarly, the Roadmap for Mental Health Research in Europe (ROAMER) project by the European Commission sought to integrate mental health research across Europe using principles similar to those in the RDoC Framework.;
Dr. Morris, who has acceded to the Head of the RDoC Unit, commented: “The fact that investigators and science funders outside the United States are also pursuing similar approaches gives me confidence that we’ve been on the right pathway. I just think that this has got to be how nature works and that we are in better alignment with the basic fundamental processes that are of interest to understanding mental disorders.”
The RDoC framework will continue to adapt and change with emerging science to remain relevant as a resource for researchers now and in the future. For instance, NIMH continues to work toward the development and optimization of tools to assess RDoC constructs and supports data-driven efforts to measure function within and across domains.
“For the millions of people impacted by mental disorders, research means hope. The RDoC framework helps us study mental disorders in a different way and has already driven considerable change in the field over the past decade,” said Joshua A. Gordon, M.D., Ph.D., director of NIMH. “We hope this and other innovative approaches will continue to accelerate research progress, paving the way for prevention, recovery, and cure.”
Publications
Cuthbert, B. N., & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine , 11 , 126. https://doi.org/10.1186/1741-7015-11-126
Cuthbert B. N. (2014). Translating intermediate phenotypes to psychopathology: The NIMH Research Domain Criteria. Psychophysiology , 51 (12), 1205–1206. https://doi.org/10.1111/psyp.12342
Cuthbert, B., & Insel, T. (2010). The data of diagnosis: New approaches to psychiatric classification. Psychiatry , 73 (4), 311–314. https://doi.org/10.1521/psyc.2010.73.4.311
Cuthbert, B. N., & Kozak, M. J. (2013). Constructing constructs for psychopathology: The NIMH research domain criteria. Journal of Abnormal Psychology , 122 (3), 928–937. https://doi.org/10.1037/a0034028
Garvey, M. A., & Cuthbert, B. N. (2017). Developing a motor systems domain for the NIMH RDoC program. Schizophrenia Bulletin , 43 (5), 935–936. https://doi.org/10.1093/schbul/sbx095
Kozak, M. J., & Cuthbert, B. N. (2016). The NIMH Research Domain Criteria initiative: Background, issues, and pragmatics. Psychophysiology , 53 (3), 286–297. https://doi.org/10.1111/psyp.12518
Morris, S. E., & Cuthbert, B. N. (2012). Research Domain Criteria: Cognitive systems, neural circuits, and dimensions of behavior. Dialogues in Clinical Neuroscience , 14 (1), 29–37. https://doi.org/10.31887/DCNS.2012.14.1/smorris
Sanislow, C. A., Pine, D. S., Quinn, K. J., Kozak, M. J., Garvey, M. A., Heinssen, R. K., Wang, P. S., & Cuthbert, B. N. (2010). Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology , 119 (4), 631–639. https://doi.org/10.1037/a0020909
- Presidential Proclamation 6158 (The Decade of the Brain)
- Research Domain Criteria Initiative website
- Psychiatric Ratings using Intermediate Stratified Markers (PRISM)
- Open access
- Published: 06 December 2022
What improves access to primary healthcare services in rural communities? A systematic review
- Zemichael Gizaw 1 ,
- Tigist Astale 2 &
- Getnet Mitike Kassie 2
BMC Primary Care volume 23 , Article number: 313 ( 2022 ) Cite this article
13k Accesses
9 Citations
1 Altmetric
Metrics details
To compile key strategies from the international experiences to improve access to primary healthcare (PHC) services in rural communities. Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities.
All published and unpublished qualitative and/or mixed method studies conducted to improvement access to PHC services were searched from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar. Articles published other than English language, citations with no abstracts and/or full texts, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We assessed the methodological quality of the included studies using mixed methods appraisal tool (MMAT) version 2018 to minimize the risk of bias. Data were extracted using JBI mixed methods data extraction form. Data were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes.
Our analysis of 110 full-text articles resulted in ten key strategies to improve access to PHC services. Community health programs or community-directed interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, working with traditional healers, working with non-profit private sectors and non-governmental organizations including faith-based organizations are the key strategies identified from international experiences.
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies can play roles in achieving universal health coverage and reducing disparities in health outcomes among rural communities and enabling them to get healthcare when and where they want.
Peer Review reports
Introduction
Universal health coverage (UHC) is used to provide expanding services to eliminate access barriers. Universal health coverage is defined by the world health organization (WHO) as access to key promotional, preventive, curative and rehabilitative health services for all at an affordable rate and ensuring equity in access. The term universal has been described as the State's legal obligation to provide healthcare to all its citizens, with particular attention to ensuring that all poor and excluded groups are included [ 1 , 2 , 3 ].
Strengthening primary healthcare (PHC) is the most comprehensive, reliable and productive approach to improving people's physical and mental wellbeing and social well-being, and that PHC is a pillar of a sustainable health system for UHC and health-related sustainable development goals [ 4 , 5 ]. Despite tremendous progress over the last decades, there are still unaddressed health needs of people in all parts of the world [ 6 , 7 ]. Many people, particularly the poor and people living in rural areas and those who are in vulnerable circumstances, face challenges to remain healthy [ 8 ].
Geographical and financial inaccessibility, inadequate funding, inconsistent medication supply and equipment and personnel shortages have left the reach, availability and effect of PHC services in many countries disappointingly limited [ 9 , 10 ]. A recent Astana Declaration recognized those aspects of PHC need to be changed to adapt adequately to current and emerging threats to the healthcare system. This declaration discussed that implementation of a need-based, comprehensive, cost-effective, accessible, efficient and sustainable healthcare system is needed for disadvantaged and rural populations in more local and convenient settings to provide care when and where they want it [ 8 ].
Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities. The findings of this systematic literature review can be used by healthcare professionals, researchers and policy makers to improve healthcare service delivery in rural communities.
Methodology
Research question.
What improves access to PHC services in rural communities? We used the PICO (population, issue/intervention, comparison/contrast, and outcome) construct to develop the search question [ 11 ]. The population is rural communities or remote communities in developing countries who have limited access to healthcare services. Moreover, we extended the population to developed countries to capture experiences of both developing and developed countries. The issue/intervention is implementation of different community-based health interventions to access to essential healthcare services. In this systematic review, we focused on PHC health services, mainly essential or basic healthcare services, community or public health services, and health promotion or health education. Primary healthcare is “a health care system that addressed social, economic, and political causes of poor health promotes health though health services at the primary care level enhances health of the community” [ 12 ]. Comparison/contrast is not appropriate for this review. The outcome is improved access to essential healthcare services.
Outcome measures
The outcome of this review is access to PHC services, such as preventive, promotive, curative, rehabilitative, and palliative health services which are affordable, convenient or acceptable, and available to all who need care.
Criteria for considering studies for this review
All published and unpublished qualitative and/or mixed method studies conducted to improve access to PHC services were included. Government and international or national organizations reports were also included. Different organizations whose primary mission is health or promotion of community health were selected. We included articles based on these eligibility criteria: context or scope of studies (access to PHC services), article type (primary studies), and publication language (English). Articles published other than English language, citations with no abstracts and/or full texts, reviews, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We didn’t use time of publication for screening.
Information sources and search strategy
We searched relevant articles from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar to access all forms of evidence. An initial search of MEDLINE was undertaken followed by analysis of the text words contained in the title and abstract, and of the index terms used to describe articles. We used the aforementioned performance indicators of PHC delivery and the PICO as we described above to choose keywords. A second search using all identified keywords and index terms was undertaken across all included databases. Thirdly, references of all identified articles were searched to get additional studies. The full electronic search strategy for MEDLINE, a major database we used for this review is included as a supplementary file (Additional file 1 : Appendix 1).
Study selection and assessment of methodological quality
Search results from different electronic databases were exported to Endnote reference manager version 7 to remove duplication. Two independent reviewers (ZG and BA) screened out records. An initial screening of titles and abstracts was done based on the PICO criteria and language of publication. Secondary screening of full-text papers was done for studies we included at the initial screening phase. We further investigated and assessed records included in the full-text articles against the inclusion and exclusion criteria. We sat together and discussed the eligibility assessment. The interrater agreement was 90%. We resolved disagreements by consensus for points we had different rating. We used the PRISMA flow diagram to summarize the study selection processes.
Methodological quality of the included studies was assessed using mixed methods appraisal tool (MMAT) version 2018 [ 13 ]. As it is clearly indicated in the user guide of the MMAT tool, it is discouraged to calculate an overall score from the ratings of each criterion. Instead, it is advised to provide a more detailed presentation of the ratings of each criterion to better inform quality of the included studies. The rating of each criterion was, therefore, done as per the detail explanations included in the guideline. Almost all the included full text articles fulfilled the criteria and all the included full text articles were found to be better quality.
Data extraction
We independently extracted data from papers included in the review using JBI mixed methods data extraction form. This form is only used for reviews that follow a convergent integrated approach, i.e. integration of qualitative data and qualitative data [ 14 ]. The data extraction form was piloted on randomly selected papers and modified accordingly. One reviewer extracted the data from the included studies and the second reviewer checked the extracted data. Disagreements were resolved by discussion between the two reviewers. Information was extracted from each included study on: list of authors, year of publication, study area, population of interest, study type, methods, focus of the studies, main findings, authors’ conclusion, and limitations of the study.
Synthesis of findings
The included full-text articles were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes. Themes are strategies mentioned or discussed in the included records to improve access to PHC services. Themes were identified manually by reading the included records again and again. We then synthesized each theme by comparing the discussion and conclusion of the included articles.
Systematic review registration number
The protocol of this review is registered in PROSPERO (the registration number is: CRD42019132592) to avoid unplanned duplication and to enable comparison of reported review methods with what was planned in the protocol. It is available at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019132592 .
Schematic of the systematic review and reporting of the search
We used PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 checklist [ 15 ] for reporting of this systematic review.
Study selection
The search strategy identified 1148 titles and abstracts [914 from PubMed (Table 1 ) and 234 from other sources] as of 10 March 2022. We obtained 900 after we removed duplicated articles. Following assessment by title and abstract, 485 records were excluded because these records did not meet the criteria as mentioned in the method section. Additional 256 records were discarded because the records did not discuss the outcome of interest well and some records were systematic reviews. The full text of the remaining 159 records was examined in more detail. It appeared that 49 studies did not meet the inclusion criteria as described in the method section. One hundred ten records met the inclusion criteria and were included in the systematic review or synthesis (Fig. 1 ).
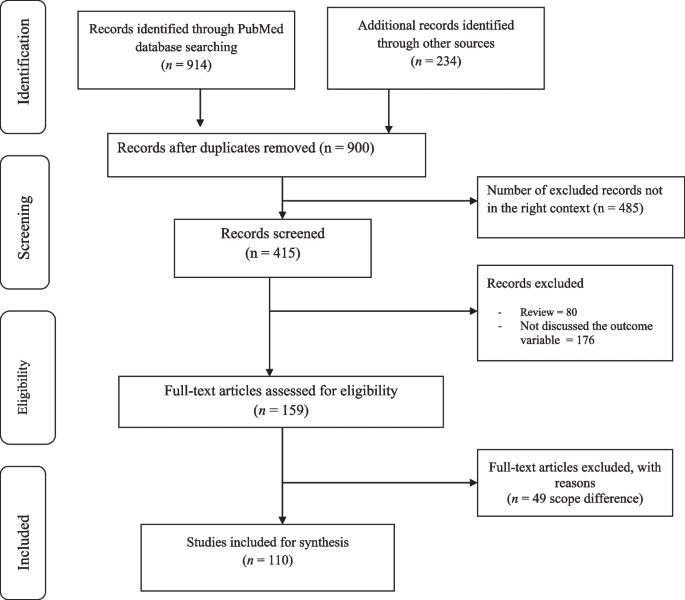
Study selection flow diagram
Of 900 articles resulting from the search term, 110 (12.2%) met the inclusion criteria. The included full-text articles were published between 1993 and 2021. Ninety-two (83.6%) of the included full-text articles were research articles, 5(4.5%) were technical reports, 3 (2.7%) were perspective, 4 (3.6%) was discussion paper, 3(2.7%) were dissertation or thesis, 2 (1.8%) were commentary, and 1 (0.9) was a book. Thirty-six (33%) and 29 (26%) of the included full-text articles were conducted in Africa and North America, respectively (Fig. 2 ).
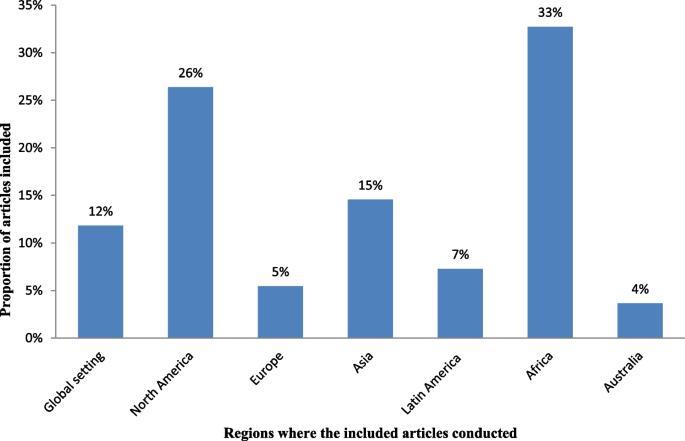
Regions where the included full-test articles conducted
Key strategies identified
The analysis of 110 full-text articles resulted in 10 themes. The themes are key strategies to improve access to PHC services in rural communities. The key strategies identified are community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, promoting the role of traditional medicine, working with non-profit private sectors and non-governmental organizations (NGOs) including faith-based organizations (Table 2 ).
Description of strategies
a. Community health programs or community-directed healthcare interventions
Twenty-four (21.8%) of the full-text articles included in this review discussed that community health programs (CHPs) or community-directed healthcare interventions are best strategies to provide basic health and medical care close to the community to increase access and coverage of essential health services. Community health programs are locally based health promotion, disease prevention, and treatment programs available typically to communities in need and community-directed intervention strategy is an approach in which communities themselves direct the planning and implementation of intervention delivery. Rural communities, especially, in developing countries have no access to healthcare facilities in the near distance and have less chance to receive healthcare from doctors, health officers, nurses or midwives. In response to this critical problems, many countries have been investing heavily in community based primary health care to bring services to rural and remote areas where most of the population lives. Community health programs include construction of health posts or community health centers close to the community and deployment of community health workers (CHWs), such as health extension workers, to reach-out every village, who play a prominent role as the gatekeepers of healthcare in rural communities. Community-directed healthcare intervention is an approach in which communities themselves direct the planning and implementation of healthcare interventions. Community participation remains crucial in the identification of health problems, planning or designing of health interventions and implementation of the interventions, which enhances need-based and demand-driven provision of health services while promoting sustainability and ownership (Additional file 2 : Appendix 2, Table A1).
b. School-based primary healthcare
In this review, 9 of 110 (8.2%) of the included full-text articles pointed out that school-based healthcare services can be effective to improve access to PHC services. School-based health services are health programs that offer health care to children and youth either in a school or on school grounds and usually staffed according to school community needs and resources. School-based health services provide a variety of healthcare services to underserved children, youth and vulnerable populations in a convenient and accessible environment. Access to comprehensive health services via schools leads to improved access to healthcare (Additional file 3 : Appendix 3, Table A2).
c. Student-led healthcare services
In this review, 5 of 110 (4.5%) of the full-text articles discussed that the use of medical and health science students as healthcare service providers can minimize problems related with shortage of health professionals in rural healthcare system and can play appreciable roles to minimize healthcare service access problems in rural communities. Student-led healthcare services are developed through consultation between universities and local health providers and are purposefully designed clinical placements with a focus on clinical educational activities for pre-registration students. Student-led clinics link students, healthcare professionals, community-based organizations, universities, and communities. In this approach, students can gain practical experience in an interdisciplinary setting and through exposure to a community with unique and severe needs (Additional file 4 : Appendix 4, Table A3).
d. Outreach services or mobile clinics
In this systematic literature review, 18 of 110 (16.4%) of the included studies discussed that outreach services or mobile clinics in primary care and rural hospital settings can improve access to PHC services in rural communities. Mobile outreach service is defined as healthcare services provided by a mobile team of trained providers, from a higher-level health facility to a lower-level health facilities or locally available community facilities that are not used for clinical services, such as schools, health posts, or other community structures. Outreach services improve access to specialists and hospital-based services, strengthen connections between specialists and PHC providers, and give the benefits of consultations in primary care settings. Specialist outreach services have the potential to overcome access barriers faced by disadvantaged rural and remote communities. Furthermore, a community-based mobile clinics can be effective in uncovering illness and in directing patients to a healthcare home (Additional file 5 : Appendix 5, Table A4).
e. Family health program
Four (3.6%) of the included full-text articles discussed that family health program (FHP) is highly cost-effective tool for improving access to healthcare services for deprived areas (such as rural communities). Family health program means the program is a program designed to provide primary care as well as the prevention and early treatment of communicable and non-communicable diseases in defined populations by deploying interdisciplinary healthcare teams include physicians, nurses, nurse assistants, and full-time community health agents. It has evolved into a robust approach to providing primary care for defined populations by deploying interdisciplinary healthcare teams. The nucleus of each team includes a physician, a nurse, a nurse assistant, and full-time community health agents. This approach is effective on improving access to healthcare and eliminating health disparities (Additional file 6 : Appendix 6, Table A5).
f. Empanelment
This systematic review of literature identified that empanelment (also known as rostering) is a best strategy to proactively provide coordinated primary healthcare towards achieving universal health coverage. Empanelment is a continuous, iterative set of processes that identify and assign populations to facilities, care teams, or primary care providers who have a responsibility to know their assigned population. It enables health systems to improve health outcomes and to reduce costs. Empanelment establishes a point of care for individuals and simultaneously holds primary healthcare providers and care teams accountable for actively managing care for a specific group of individuals (Additional file 7 : Appendix 7, Table A6).
g. Community health funding schemes
In this systematic review of literature, 11 (10%) of the included articles discussed that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare services in low-income rural communities. Community-based health insurance schemes are usually voluntary and characterized by community members pooling funds to offset the cost of healthcare. Moreover, this approach is effective to mobilize domestic resources for health at low income levels. For low-income countries, community health financing has modest ability to increase the total amount of funds for healthcare. Properly structured community health financing system can significantly improve efficiency, reduce the cost of healthcare, improve quality and health outcomes, and pool risks. Community-financing schemes could improve preventive services and reduce the incidence of diseases. It could also improve people’s access to healthcare and the quality of services, thus improving their health status. Community health financing could also improve risk pooling and reduce health-induced impoverishment. Community health insurance has potential positive impacts on health and social security (Additional file 8 : Appendix 8, Table A7).
h. Telemedicine
In this review, 13 of 110 (11.8%) articles discussed that telemedicine is one of the solutions for rural subspecialty healthcare delivery. Telemedicine can be defined as the use of technology (computers, video, phone, messaging) by a medical professional to diagnose and treat patients in a remote location. The provision of subspecialty services using telemedicine to a remote and medically underserved population provides improved access to subspecialty care. Telemedicine brings sustainable healthcare to rural populations. Use of information and communication technologies in support of health and health-related fields, including healthcare services, health surveillance, health education, and health research has the potential to greatly improve health service efficiency, expand or scale up treatment delivery to thousands of patients in the rural populations (Additional file 9 : Appendix 9, Table A8).
i. Promoting the role of traditional medicine
Seven (6.4%) of the included articles showed that incorporating traditional healers into public health system addresses healthcare needs of people with limited access to allopathic medicine. Traditional medicine is the sum total of the knowledge, skill, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness. Knowledge about traditional medicine has a catalyzing effect in meeting health sector development objectives. Integrating traditional medicine into national health systems in combination with national policy and regulation for products, practices and providers can enhance access to PHC services in remote populations (Additional file 10 : Appendix 10, Table A9).
j. Working with non-profit private sectors and non-governmental organizations
In this systematic review, 15 of 110 (13.6%) of the included articles revealed that working with non-profit private sectors and NGOs strengthens the healthcare system. Involving the non-profit private sectors, faith-based organizations (FBOs), and NGOs for health system strengthening eventually contributes to create a healthcare system reflecting an increased efficiency, more equity and good governance in health. International and local NGOs have endeavored to fill the gaps in access to healthcare services, research and advocacy. Non-profit private sectors and NGOs have a key role in improving health in low- and middle-income countries. With networks that reach even the most remote communities, many FBOs are well positioned to promote demand and access for healthcare services. Partnership among FBOs is critical in increasing access to healthcare services, and ensuring sustainability by influencing behaviors at the community, family and individual level. Faith-based organizations play an integral role in the healthcare system by increasing health seeking behaviors and delivering supportive services that address common access and cultural barriers (Additional file 11 : Appendix 11, Table A10).
This systematic literature review found that community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telehealth, integrative medicine, and working with non-profit private sectors and NGOs are key strategies to improve access to PHC services in rural communities. The identified strategies address the four major pillars of primary healthcare (i.e., community participation, inter-sectoral coordination, appropriate technology, and support mechanism made available) [ 126 ]. Moreover, the identified strategies are effective to improve access to healthcare services to rural communities. Moreover, the identified strategies are effective to solve shortage of manpower and to build knowledge and skill of the local health workforces in rural healthcare system. The ability of a healthcare system to meet health needs of the population depends largely on the knowledge, skills, motivation and deployment of the people responsible for organizing and delivering health services. The results of this review can strengthen the health information system, which are core elements of the healthcare system that ensure community engagement through dissemination and use of timely and reliable health information to rural populations. This review also suggests strategies to narrow down the health disparities among rural populations, which is wide in most Least and Middle Income Countries (LMICs). Healthcare services are usually disproportionately concentrated in major urban areas. As a result, rural communities face growing health disparities, largely attributed to weak policies, inefficiencies, poor leadership, and governance in healthcare system.
This review identified that community health programs or community-directed healthcare interventions address health disparities by ensuring equitable access to health resources in communities where health equity is limited by socioeconomic and geographical factors. Community health programs include identifying and prioritizing public health problems in a specific geographic area; designing and implementing public health interventions (such as establishing community health centers, mobile clinics, and outreach programs); providing services (such as health education, screenings, social support, and counseling), and deploying community health workers to promote healthy behaviors; advocating for improved care for populations at risk; and working with stakeholders to address community healthcare needs [ 16 , 17 , 18 , 127 , 128 , 129 , 130 ]. The community-oriented PHC model which is socially responsive medicine makes a healthcare system more rational, accountable, appropriate, and socially relevant to the public. Consequently, this model serves as a paradigm for reforming healthcare systems. Community-directed interventions can be considered as a realistic means to increase accessibility of interventions at community-level in rural areas [ 32 , 33 , 34 , 35 , 36 , 37 , 38 ]. This approach is best in situations where there are cultural barriers to implement interventions because this strategy is effective to develop ownership in the community. In-service and on-the-job training for community health workers, close supervision and government support, and program evaluation is very important to strengthen the community health program [ 131 , 132 , 133 ].
This review identified that school-based PHC services are effective strategies to improve access to PHC services. School-based health services provide a variety of healthcare services to children, youth and vulnerable populations in a convenient and accessible environment which indirectly improve leadership and governance. Science teachers and home room teachers play important roles to implement this strategy. It impacts on delivering preventive care such as immunizations, managing chronic illnesses and providing reproductive health services for adolescents. Comprehensive health services via schools improve access to healthcare information [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. Access to school around the world increased drastically in the last century [ 134 ]. This high schooling rate is a good opportunity to provide healthcare services to school learners in accessible places and to disseminate health messages to families. Prior researches suggest that school-based healthcare services increase access to healthcare by increasing utilization of primary care, prevention services, and health maintenance visits [ 135 , 136 ]. Including science teachers, home room teachers, school principals, students, communities, community health workers, and other interested parties in the school-based healthcare system as main actors or promoters must be considered to sustain the impact. Health and education sectors should work in collaboration with the above-mentioned actors to plan, implement and monitor the progress. School-based healthcare services are preferable in situations when there is high schooling rate and limited access to healthcare institutions. This strategy is also an alternative way in areas where the health seeking behavior of the community is low.
The use of medical and health science students in rural healthcare system was identified as a key strategy to minimize health inequalities in rural communities due to shortages in health workforce and distribution of healthcare resources [ 49 , 50 , 51 , 52 , 53 ]. Student-led health intervention is an alternative approach to provide essential healthcare services to the community where there is shortage of healthcare workers [ 137 , 138 ]. Students will have opportunities to learn professional skills and competencies while they are providing healthcare services to the community. Moreover, benefits for student learning include increased communication, collaboration, and leadership skills [ 53 , 139 ]. Student-led health intervention also enables increased access to services, more time for assessments and treatments, increased depth of health teaching, holistic and integrated healthcare, and free health supports [ 140 , 141 , 142 , 143 ]. However, the use of medical and health science students in the rural healthcare system may have ethical and competency issues. Supporting strategies such as close supervision, preparing clear protocols, and including senior experts in the team should be considered.
This systematic review of literature found that outreach services or mobile clinics can improve access to PHC service delivery in rural populations [ 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 ]. In developing countries, the highest proportion of people lives in rural areas where doctor services are not available. Rural communities travel to major cities to get specialist services. This reflects a desire for closer integration between primary and secondary care. Specialist outreach services or mobile clinics have become one of the effective solution to solve health disparities, to improve access to healthcare services, and to build capacity of local healthcare workforces. This strategy is preferable in situations when there are high loads in tertiary or referral level hospitals and when there is high patient leakage in the referral system [ 63 , 64 , 65 , 66 , 67 , 68 , 69 ]. However, the implementation may not be easy. It needs well established healthcare system and budget. Moreover, the efficiency of care may be lower compared with hospital-based cares and the effect on patients’ health outcomes might be small [ 56 , 57 , 61 ] . Irregular specialist visits in rural areas may not have real impacts unless the services are sustainable with a strong commitment at national and local levels. Outreach activities should be included in health policies with strong leadership, healthcare financing, and private initiatives must be encouraged to maintain the activities over time.
This review revealed that FHP is highly effective tool for improving health for rural communities. The FHP has provided a new, more robust model of primary healthcare services designed to provide accessible, first contact, comprehensive, and whole person care that is coordinated with other healthcare services. It has positive results to improved availability, access to, and use of health services, and improved health indicators, such as reduced infant mortality, improved detection of cases of neglected diseases, and reduced health disparities [ 73 , 144 , 145 , 146 ]. The FHP deploys interdisciplinary healthcare teams. The team includes a physician, a nurse, a nurse assistant, and full-time community health agents. Family health teams are organized geographically. The teams are responsible for delivering public health interventions [ 72 , 74 ]. Family health program is an alternative strategy in rural healthcare system in situations when there are inequities in access to care; when there is high hospitalization rate; when there is low health seeking behavior in the community; and when there is poor case detecting and reporting system. Despite these remarkable achievements, the FHP has some challenges include difficulties in the recruitment and retention of doctors trained appropriately to deliver primary healthcare, large variations in quality of local care, patchy integration of primary care services with existing secondary and tertiary care, and slow adoption of FHP in large population [ 147 ].
In this review, empanelment has been identified as a best strategy to deliver coordinated primary healthcare towards achieving universal health coverage [ 76 , 77 , 78 , 79 ]. The goal of empanelment is provide people-centered healthcare services based on their needs to ensure that every established patient receives optimal care, whether he/she regularly visits healthcare centers. Major activities in this approach include assignment of all patients to a healthcare provider panel; update panel assignments on a regular basis; and use panel data to educate, and track patients [ 79 ]. Empanelment enables healthcare systems to improve patient experiences, reduce costs, and improve health outcomes. Empanelment is an effective strategy to deliver four key functions: first-contact accessibility, continuity, comprehensiveness, and coordination [ 148 ]. Effective empanelment requires responsibility for the health of a target population, including providing healthcare services based on their health status, which is an important step in moving towards people-centered integrated healthcare [ 79 ].
This review identified that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare in low-income rural communities. Moreover, this approach is effective to mobilize domestic resources for health at low income levels [ 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 ]. Community-based health insurance is an emerging strategy to provide financial protection against the cost of illness. It is an effective strategy to improve access to quality health services for low-income rural households [ 149 ]. Existence of social capital in the community is a determinant factor for the effectiveness of CBHI as social capital has a positive effect on the community's demand for insurance [ 150 , 151 ]. Moreover, solidarity and trust between the members are the key principles for the good functioning of a CBHI. Solidarity and trust stir-up members who are susceptible to risk to put together their resources for common use [ 149 , 152 , 153 ]. Affordability of premiums or contributions, technical arrangements made by the scheme management, timing of collecting the contributions, trust in the integrity and competence of the managers of the CBHI, The quality of care offered through the CBHI, accessible across different population groups are some of the determinant factors to be considered to increase people’s decision to join the CBHI schemes [ 154 , 155 ].
In this review, telemedicine has been identified as one of the many possible solutions for rural subspecialty healthcare delivery. Telemedicine is a vital technological tool to increase healthcare access, improve care delivery systems, engage in culturally competent outreach, health workforce development, and health information system [ 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 ]. Telemedicine can be a great alternative to the traditional healthcare system in situations like diagnoses of common medical problems; inquiries about various medical issues for home treatments; post-treatment check-ins or follow-up for chronic care; holidays, weekends, late night or any other situation when regular medical care is not possible; patient inability to leave the house; patients who lack regular access to relevant medical expertise in their geographic area ; and etc. However, technological issues are challenges when dealing with telemedicine, especially in developing countries. General problems of Internet connectivity and access to infrastructure can minimize benefits of this strategy. Costs associated with technology can also be a barrier. Furthermore, health technology requires human capacity to use it. Therefore, strengthening the information communication technologies (ICT) and human capacity building on ICT are important to address the health needs of the rural communities.
This systematic review of literature identified that promoting the role of TM solves problems of access to allopathic medicine. Integration of TM in health system will result in increased coverage and access to healthcare services. The role of complementary and alternative medicine for health is undisputed particularly in light of its role in health promotion and well-being. It also supports local health workforces [ 104 , 105 , 106 , 107 , 108 , 109 ]. Incorporating traditional healers into the public health system addresses healthcare needs [ 156 , 157 ]. However, integrating TM to the public healthcare system is challenging. It is a general belief that TM defies scientific procedures in terms of objectivity, measurement, codification and classification [ 157 ]. If integrated, who provides training to medical doctors on the ontology, epistemology and the efficacies of TM in modern medicine [ 157 ]. Due to these, some scholars suggest that both TM and modern medicine be allowed to operate and develop independent of one another [ 158 , 159 ]. Another fundamental challenge to TM is the widespread reported cases of fake healers and healings [ 157 ]. Generally, this strategy is more of feasible in areas where formal trainings on integrative medicine are available. Even though the integration is challenging, the health sector can use traditional healers as health educators or health promoters by providing training and continuous support. It can be also possible to use traditional healers as facilitators in the community-directed approaches. In general TM can be used in the primary healthcare system where no access to allopathic medicine and when conventional medicine is ineffective in treatment of disease [ 160 ].
Working with non-profit private sectors and NGOs has been identified as effective strategies to strengthen the healthcare system in developing countries [ 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 ]. Since governments in developing countries are challenged to meet the health needs of their populations because of financial constraints, limited human resources, and weak health infrastructure; the private sector (especially the non-profit private sectors) and non-governmental organizations can help expand access to healthcare services through its resources, expertise, and infrastructure. However, the presence of an NGO in the operation, may contribute to unrealistic expectations of health services, affecting perceptions of the latter negatively [ 113 ]. Moreover, reports have it that besides other issues in many instances NGOs allocated funds only to disease specific projects (vertical programming) rather than to broad based investments (horizontal programming) [ 161 ]. There are also concerns that donor expenditures in developing countries are not only unsustainable but may be considered as inadequate considering the enormous healthcare burden [ 161 , 162 , 163 , 164 ]. To avoid unrealistic expectations and dissatisfaction, and to increase and sustain the population’s trust in the organization, NGOs should operate in a manner that is as integrated as possible within the existing structure and should work close to the population it serves, with services anchored in the community. Moreover, faith-based organizations contribute in health such as disease prevention, health education or promotion, and community health development beyond psychological and spiritual care [ 119 , 120 , 121 , 122 , 123 , 124 ]. Religious organizations can reach all segments of rural populations. Therefore, integrating PHC services, especially health education and promotion, diseases prevention and community health development with religious organizations intensifies delivery of healthcare services. Working with FBOs is a best way in situations where cultural and faith-based barriers are common and in areas, where access problems are often related to lack of providers. However, religious organizations need intensive training on health promotion and health system to enable them to respond to local contexts within the framework of national policies. Moreover, there should be strong partnership with government agenesis to sustain the effort [ 165 , 166 , 167 , 168 ].
Contribution of this review
Various studies reported one or more strategies to improve access to primary healthcare services. However, the strategies reported by individual studies are not compiled together and there is lack of pooled evidence on effective strategies to improve access to healthcare system. This systematic literature review was, therefore, conducted to compile effective strategies to improve access to healthcare services in rural communities. The review suggests key strategies to improve access to PHC services in rural communities. These suggested strategies are implementable in countries that suffer from shortage of health workers and healthcare financing because all the strategies used locally available opportunities. The local healthcare system needs, therefore, scan the available opportunities in the locality for implementing the suggested strategies and needs to integrate the strategies in the healthcare system to sustain the impacts. Healthcare providers, researchers and policy makers could use the results of this systematic literature review to increase access to healthcare services in hard-to-reach areas. As the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional, and geographical challenges to adopt the identified strategies. Moreover, some of the experiences only come from one or two countries. Therefore, strategy developers and implementers need to consider these contextual challenges or variation during adopting and implementing different strategies.
Strengths and limitations of the study
As a strength, this systematic review explores international (both developed and developing countries) best experiences on primary healthcare service delivery and identified ten key approaches to improve access to PHC services in rural communities. We also searched relevant published or unpublished articles, dissertations or theses, discussion papers, and perspectives from a wide range of sources, such as MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar.
As a limitation, we entirely relied on electronic databases to search relevant articles. We didn’t include locally available printed out records. We also applied limits for language. We excluded articles published other than English language. We believed we could get more relevant articles if we had access to records available in prints and if we include articles published other than English language. Furthermore, since the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional and geographical challenges to adopt the identified strategies. There was also limited evidence for some articles, especially reports to rate their methodological quality. Readers should also note that our review might missed some important work in improving access to PHC services and the identified strategies are not the only strategies to improve access to PHC services. There might be other effective strategies which are not included in this review. In addition generalizability might be affected since some of the experiences only come from one or two countries. Moreover, this review focuses on access not quality of care delivered.
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies are effective to improve access to healthcare services in rural or remote communities. They can also play roles in achieving UHC and reducing disparities in health outcomes and increase access to rural communities to get healthcare when and where they want. Therefore, incorporating these key strategies suggested by this review in to the healthcare system is useful to enhance PHC services and to minimize impacts of health disparity in rural communities. However, the identified strategies may not be easy to implement. Increasing number and capacity of human resource for health; strengthening the healthcare financing system; improving medicine and supplies; working in different partners and communities; establishing monitoring and evaluation system; strong and committed leadership; and encouraging private initiatives must be considered to implement and maintain these strategies over time. Moreover, policy makers, program planners and implementers who want to utilize findings of this review should be aware that these are not the only effective strategies to improve access to primary healthcare services.
Availability of data and materials
All the extracted data are included in the manuscript.
Abbreviations
Community-based health insurance
Faith-based organizations
Family health program
Information communication technologies
Mixed methods appraisal tool
Non-governmental organizations
- Primary healthcare
Primary Health Care Performance Initiative
Population, phenomena of interest and context)
Traditional medicine
Universal health coverage
Hampton MB, Kettle AJ, Winterbourn CC. Inside the neutrophil phagosome: oxidants, myeloperoxidase, and bacterial killing. Blood. 1998;92(9):3007–17.
Article CAS Google Scholar
Kirby M. The right to health fifty years on: Still skeptical? Health Hum Rights. 1999;4(1):6–25.
O’Connell T, Rasanathan K, Chopra M. What does universal health coverage mean? The Lancet. 2014;383(9913):277–9.
White F. Primary health care and public health: foundations of universal health systems. Med Princ Pract. 2015;24(2):103–16.
Article Google Scholar
Sanders D, Nandi S, Labonté R, Vance C, Van Damme W. From primary health care to universal health coverage—one step forward and two steps back. The Lancet. 2019;394(10199):619–21.
Brezzi M, Luongo P. Regional Disparities In Access To Health Care. 2016.
Google Scholar
Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94(10):1675–8.
Walraven G. The 2018 Astana declaration on primary health care, is it useful? J Glob Health. 2019;9(1).
Gillam S. Is the declaration of Alma Ata still relevant to primary health care? BMJ (Clinical research ed). 2008;336(7643):536–8.
Tollman S, Doherty J, Mulligan JA. General Primary Care. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, editors. Disease Control Priorities in Developing Countries. Washington: World Bank The International Bank for Reconstruction and Development/The World Bank Group; 2006. Available at https://www.ncbi.nlm.nih.gov/books/NBK11789/pdf/Bookshelf_NBK11789.pdf .
Stern C, Jordan Z, McArthur A. Developing the review question and inclusion criteria. AJN The Am J Nurs. 2014;114(4):53–6.
World Health Organization. losing the gap in a generation. Commission on Social Determinants of Health FINAL REPORT. 2008. Available at https://www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf . Accessed on 22 March 2022.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, GagnonM-P GF, Nicolau B, O’Cathain A. Mixed methods appraisal tool (MMAT), version 2018. Canada: IC Canadian Intellectual Property Office, Industry; 2018. Available at https://mixedmethodsappraisaltoolpublicpbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf .
JBI Manual for Evidence Synthesis. Appendix 8.1 JBI Mixed Methods Data Extraction Form following a Convergent Integrated Approach. Available at https://jbi-global-wiki.refined.site/space/MANUAL/3318284375/Appendix+8.1+JBI+Mixed+Methods+Data+Extraction+Form+following+a+Convergent+Integrated+Approach . Accessed on 12 August 2021.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Glob Health. 2019;15(1):1–11.
Admassie A, Abebaw D, Woldemichael AD. Impact evaluation of the Ethiopian health services extension programme. J Dev Eff. 2009;1(4):430–49.
Yitayal M, Berhane Y, Worku A, Kebede Y. The community-based Health extension Program significantly improved contraceptive utilization in West gojjam Zone, ethiopia. J Multidiscip Healthc. 2014;7:201.
Croke K, Mengistu AT, O’Connell SD, Tafere K. The impact of a health facility construction campaign on health service utilisation and outcomes: analysis of spatially linked survey and facility location data in Ethiopia. BMJ Glob Health. 2020;5(8):e002430.
Arwal S. Health Posts in Afghanistan. J Gen Practice. 2015;3(213):2.
Negussie A, Girma G. Is the role of Health Extension Workers in the delivery of maternal and child health care services a significant attribute? The case of Dale district, southern Ethiopia. BMC Health Serv Res. 2017;17(1):1–8.
Than KK, Mohamed Y, Oliver V, Myint T, La T, Beeson JG, Luchters S. Prevention of postpartum haemorrhage by community-based auxiliary midwives in hard-to-reach areas of Myanmar: a qualitative inquiry into acceptability and feasibility of task shifting. BMC Pregnancy Childbirth. 2017;17(1):1–10.
Medhanyie A, Spigt M, Kifle Y, Schaay N, Sanders D, Blanco R, GeertJan D, Berhane Y. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res. 2012;12(1):1–9.
Sakeah E, McCloskey L, Bernstein J, Yeboah-Antwi K, Mills S, Doctor HV. Can community health officer-midwives effectively integrate skilled birth attendance in the community-based health planning and services program in rural Ghana? Reprod Health. 2014;11(1):1–13.
Sarmento DR. Traditional birth attendance (TBA) in a health system: what are the roles, benefits and challenges: a case study of incorporated TBA in Timor-Leste. Asia Pac Fam Med. 2014;13(1):1–9.
Rahmawati R, Bajorek B. Peer Reviewed: A Community Health Worker-Based Program for Elderly People with Hypertension in Indonesia: A Qualitative Study, 2013. Prev Chronic Dis. 2015;12:E175.
Feltner FJ, Ely GE, Whitler ET, Gross D, Dignan M. Effectiveness of community health workers in providing outreach and education for colorectal cancer screening in Appalachian Kentucky. Soc Work Health Care. 2012;51(5):430–40.
Hughes MM, Yang E, Ramanathan D, Benjamins MR. Community-based diabetes community health worker intervention in an underserved Chicago population. J Community Health. 2016;41(6):1249–56.
Panday S, Bissell P, Van Teijlingen E, Simkhada P. The contribution of female community health volunteers (FCHVs) to maternity care in Nepal: a qualitative study. BMC Health Serv Res. 2017;17(1):1–11.
Datiko DG, Lindtjørn B. Health extension workers improve tuberculosis case detection and treatment success in southern Ethiopia: a community randomized trial. PLoS ONE. 2009;4(5):e5443.
le Roux KW, Almirol E, Rezvan PH, Le Roux IM, Mbewu N, Dippenaar E, Stansert-Katzen L, Baker V, Tomlinson M, Rotheram-Borus M. Community health workers impact on maternal and child health outcomes in rural South Africa–a non-randomized two-group comparison study. BMC Public Health. 2020;20(1):1–14.
Witmer A, Seifer SD, Finocchio L, Leslie J, O’Neil EH. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85(8 Pt 1):1055–8.
Wright RA. Community-oriented primary care. The cornerstone of health care reform. Jama. 1993;269(19):2544–7.
Makaula P, Bloch P, Banda HT, Mbera GB, Mangani C, de Sousa A, Nkhono E, Jemu S, Muula AS. Primary Health Care in rural Malawi - a qualitative assessment exploring the relevance of the community-directed interventions approach. BMC Health Serv Res. 2012;12:328.
Katabarwa MN, Habomugisha P, Richards FO Jr, Hopkins D. Community-directed interventions strategy enhances efficient and effective integration of health care delivery and development activities in rural disadvantaged communities of Uganda. Trop Med Int Health : TM & IH. 2005;10(4):312–21.
Madon S, Malecela MN, Mashoto K, Donohue R, Mubyazi G, Michael E. The role of community participation for sustainable integrated neglected tropical diseases and water, sanitation and hygiene intervention programs: A pilot project in Tanzania. Soc Sci Med. 1982;2018(202):28–37.
Okeibunor JC, Orji BC, Brieger W, Ishola G, Otolorin E, Rawlins B, Ndekhedehe EU, Onyeneho N, Fink G. Preventing malaria in pregnancy through community-directed interventions: evidence from Akwa Ibom State, Nigeria. Malaria J. 2011;10:227.
Brieger WR, Sommerfeld JU, Amazigo UV. The Potential for Community-Directed Interventions: Reaching Underserved Populations in Africa. Int Q Community Health Educ. 2015;35(4):295–316.
Braimah JA, Sano Y, Atuoye KN, Luginaah I. Access to primary health care among women: the role of Ghana’s community-based health planning and services policy. Prim Health Care Res Dev. 2019;20:e82.
Kaplan DW, Brindis CD, Phibbs SL, Melinkovich P, Naylor K, Ahlstrand K. A comparison study of an elementary school–based health center: effects on health care access and use. Arch Pediatr Adolesc Med. 1999;153(3):235–43.
Allison MA, Crane LA, Beaty BL, Davidson AJ, Melinkovich P, Kempe A. School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics. 2007;120(4):e887–94.
Keeton V, Soleimanpour S, Brindis CD. School-based health centers in an era of health care reform: Building on history. Curr Probl Pediatr Adolesc Health Care. 2012;42(6):132–56.
Brindis CD, Klein J, Schlitt J, Santelli J, Juszczak L, Nystrom RJ. School-based health centers: Accessibility and accountability. J Adolesc Health. 2003;32(6):98–107.
Hutchinson P, Carton TW, Broussard M, Brown L, Chrestman S. Improving adolescent health through school-based health centers in post-Katrina New Orleans. Child Youth Serv Rev. 2012;34(2):360–8.
Paschall MJ, Bersamin M. School-based health centers, depression, and suicide risk among adolescents. Am J Prev Med. 2018;54(1):44–50.
Minguez M, Santelli JS, Gibson E, Orr M, Samant S. Reproductive health impact of a school health center. J Adolesc Health. 2015;56(3):338–44.
Gibson EJ, Santelli JS, Minguez M, Lord A, Schuyler AC. Measuring school health center impact on access to and quality of primary care. J Adolesc Health. 2013;53(6):699–705.
Bozigar M. A Cross-Sectional Survey to Evaluate Potential for Partnering With School Nurses to Promote Human Papillomavirus Vaccination. Prev Chronic Dis. 2020;17:E111.
Suen J, Attrill S, Thomas JM, Smale M, Delaney CL, Miller MD. Effect of student-led health interventions on patient outcomes for those with cardiovascular disease or cardiovascular disease risk factors: a systematic review. BMC Cardiovasc Disord. 2020;20(1):1–10.
Atuyambe LM, Baingana RK, Kibira SP, Katahoire A, Okello E, Mafigiri DK, Ayebare F, Oboke H, Acio C, Muggaga K. Undergraduate students’ contributions to health service delivery through communitybased education. BMC Med Educ. 2016;16:123.
Stuhlmiller CM, Tolchard B. Developing a student-led health and wellbeing clinic in an underserved community: collaborative learning, health outcomes and cost savings. BMC Nurs. 2015;14(1):1–8.
Campbell DJ, Gibson K, O’Neill BG, Thurston WE. The role of a student-run clinic in providing primary care for Calgary’s homeless populations: a qualitative study. BMC Health Serv Res. 2013;13(1):1–6.
Simpson SA, Long JA. Medical student-run health clinics: important contributors to patient care and medical education. J Gen Intern Med. 2007;22(3):352–6.
Gruen RL, O’Rourke IC, Bailie RS, d’Abbs PH, O’Brien MM, Verma N. Improving access to specialist care for remote Aboriginal communities: evaluation of a specialist outreach service. Med J Aust. 2001;174(10):507–11.
Gruen RL, Weeramanthri T, Bailie R. Outreach and improved access to specialist services for indigenous people in remote Australia: the requirements for sustainability. J Epidemiol Community Health. 2002;56(7):517–21.
Gruen RL, Bailie RS, Wang Z, Heard S, O’Rourke IC. Specialist outreach to isolated and disadvantaged communities: a population-based study. The Lancet. 2006;368(9530):130–8.
Bond M, Bowling A, Abery A, McClay M, Dickinson E. Evaluation of outreach clinics held by specialists in general practice in England. J Epidemiol Community Health. 2000;54(2):149–56.
Irani M, Dixon M, Dean JD. Care closer to home: past mistakes, future opportunities. J R Soc Med. 2007;100(2):75–7.
Bailey JJ, Black ME, Wilkin D. Specialist outreach clinics in general practice. BMJ (Clinical research ed). 1994;308(6936):1083–6.
De Roodenbeke E, Lucas S, Rouzaut A, Bana F. Outreach services as a strategy to increase access to health workers in remote and rural areas. Geneva: WHO; 2011.
Bowling A, Stramer K, Dickinson E, Windsor J, Bond M. Evaluation of specialists’ outreach clinics in general practice in England: process and acceptability to patients, specialists, and general practitioners. J Epidemiol Community Health. 1997;51(1):52–61.
Spencer N. Consultant paediatric outreach clinics–a practical step in integration. Arch Dis Child. 1993;68(4):496–500.
Aljasir B, Alghamdi MS. Patient satisfaction with mobile clinic services in a remote rural area of Saudi Arabia. East Mediterr Health J. 2010;16(10):1085–90.
Lee EJ, O’Neal S. A mobile clinic experience: nurse practitioners providing care to a rural population. J Pediatr Health Care. 1994;8(1):12–7.
Cone PH, Haley JM. Mobile clinics in Haiti, part 1: Preparing for service-learning. Nurse Educ Pract. 2016;21:1–8.
Diaz-Perez Mde J, Farley T, Cabanis CM. A program to improve access to health care among Mexican immigrants in rural Colorado. J Rural Health. 2004;20(3):258–64.
Hill C, Zurakowski D, Bennet J, Walker-White R, Osman JL, Quarles A, Oriol N. Knowledgeable Neighbors: a mobile clinic model for disease prevention and screening in underserved communities. Am J Public Health. 2012;102(3):406–10.
Edgerley LP, El-Sayed YY, Druzin ML, Kiernan M, Daniels KI. Use of a community mobile health van to increase early access to prenatal care. Matern Child Health J. 2007;11(3):235–9.
Peters G, Doctor H, Afenyadu G, Findley S, Ager A. Mobile clinic services to serve rural populations in Katsina State, Nigeria: perceptions of services and patterns of utilization. Health Policy Plan. 2014;29(5):642–9.
Neke NM, Gadau G, Wasem J. Policy makers’ perspective on the provision of maternal health services via mobile health clinics in Tanzania—Findings from key informant interviews. PLoS ONE. 2018;13(9):e0203588.
Padmadas SS, Johnson FA, Leone T, Dahal GP. Do mobile family planning clinics facilitate vasectomy use in Nepal? Contraception. 2014;89(6):557–63.
Macinko J, Harris MJ. Brazil’s family health strategy—delivering community-based primary care in a universal health system. N Engl J Med. 2015;372(23):2177–81.
Macinko J, Lima Costa MF. Access to, use of and satisfaction with health services among adults enrolled in Brazil’s Family Health Strategy: evidence from the 2008 National Household Survey. Tropical Med Int Health. 2012;17(1):36–42.
Dourado I, Oliveira VB, Aquino R, Bonolo P, Lima-Costa MF, Medina MG, Mota E, Turci MA, Macinko J. Trends in primary health care-sensitive conditions in Brazil: the role of the Family Health Program (Project ICSAP-Brazil). Medical care. 2011;49:577–84.
Aquino R, De Oliveira NF, Barreto ML. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health. 2009;99(1):87–93.
Chong P-N, Tang WE. Transforming primary care—the way forward with the TEAMS2 approach. Fam Pract. 2019;36(3):369–70.
Primary Health Care Performance Initiatives (phcpi). Improvement strategies model: Population health management: Empanelment. Available at https://improvingphc.org/sites/default/files/Empanelment%20-%20v1.2%20-%20last%20updated%2012.13.2019.pdf . Accessed on 18 March 2022.
McGough P, Chaudhari V, El-Attar S, Yung P. A health system’s journey toward better population health through empanelment and panel management. Healthcare. 2018;6(66):1–9.
Bearden T, Ratcliffe HL, Sugarman JR, Bitton A, Anaman LA, Buckle G, Cham M, Quan DCW, Ismail F, Jargalsaikhan B. Empanelment: A foundational component of primary health care. Gates Open Res. 2019;3:1654.
Hsiao WC. Unmet health needs of two billion: is community financing a solution? 2001.
Wang W, Temsah G, Mallick L. The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health Policy Plan. 2017;32(3):366–75.
Atnafu DD, Tilahun H, Alemu YM. Community-based health insurance and healthcare service utilisation, North-West, Ethiopia: a comparative, cross-sectional study. BMJ Open. 2018;8(8):e019613.
USAID. Ethiopia’s Community-based Health Insurance: A Step on the Road to Universal Health Coverage. Available at https://www.hfgproject.org/ethiopias-community-based-health-insurance-step-road-universal-health-coverage/ . Accessed on 18 March 2022.
Blanchet NJ, Fink G, Osei-Akoto I. The effect of Ghana’s National Health Insurance Scheme on health care utilisation. Ghana Med J. 2012;46(2):76–84.
CAS Google Scholar
Nshakira-Rukundo E, Mussa EC, Nshakira N, Gerber N, von Braun J. Impact of community-based health insurance on utilisation of preventive health services in rural Uganda: a propensity score matching approach. Int J Health Econ Manag. 2021;21(2):203–27.
Mwaura JW, Pongpanich S. Access to health care: the role of a community based health insurance in Kenya. Pan Afr Med J. 2012;12(1):35.
Jutting JP. The Impact Of Health Insurance On The Access To Health Care And Financial Protection In Rural Developing Countries: The Example of Senegal. HNP discussion paper series;. World Bank, Washington, DC. © World Bank. 2011. https://openknowledge.worldbank.org/handle/10986/13774 . License: CC BY 3.0 IGO.
Balamiento NC. The impact of social health insurance on healthcare utilization outcomes: evidence from the indigent program of the Philippine National Health Insurance. International Institute of Social Studies. 2018. Available at https://thesis.eur.nl/pub/46445/Balamiento,%20Neeanne_MA_2017_18%20_ECD.pdf . Accessed 30 Nov 2022.
Farrell CM, Gottlieb A. The effect of health insurance on health care utilization in the justice-involved population: United States, 2014–2016. Am J Public Health. 2020;110(S1):S78–84.
Thuong NTT. Impact of health insurance on healthcare utilisation patterns in Vietnam: a survey-based analysis with propensity score matching method. BMJ Open. 2020;10(10):e040062.
Custodio R, Gard AM, Graham G. Health information technology: addressing health disparity by improving quality, increasing access, and developing workforce. J Health Care Poor Underserved. 2009;20(2):301–7.
Meier CA, Fitzgerald MC, Smith JM. eHealth: extending, enhancing, and evolving health care. Annu Rev Biomed Eng. 2013;15:359–82.
Anstey Watkins JOT, Goudge J, Gomez-Olive FX, Griffiths F. Mobile phone use among patients and health workers to enhance primary healthcare: A qualitative study in rural South Africa. Soc Sci Med. 1982;2018(198):139–47.
Kuntalp M, Akar O. A simple and low-cost Internet-based teleconsultation system that could effectively solve the health care access problems in underserved areas of developing countries. Comput Methods Programs Biomed. 2004;75(2):117–26.
Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, Ruggiero KJ. mHealth: a mechanism to deliver more accessible, more effective mental health care. Clin Psychol Psychother. 2014;21(5):427–36.
Bashshur RL, Shannon GW, Krupinski EA, Grigsby J, Kvedar JC, Weinstein RS, Sanders JH, Rheuban KS, Nesbitt TS, Alverson DC, et al. National telemedicine initiatives: essential to healthcare reform. Telemed J E Health. 2009;15(6):600–10.
Norton SA, Burdick AE, Phillips CM, Berman B. Teledermatology and underserved populations. Arch Dermatol. 1997;133(2):197–200.
Raza T, Joshi M, Schapira RM, Agha Z. Pulmonary telemedicine–a model to access the subspecialist services in underserved rural areas. Int J Med Informatics. 2009;78(1):53–9.
Shouneez YH. Smartphone hearing screening in mHealth assisted community-based primary care. UPSpace Institutional Repository, Department of Liberary Service. Dissertation (MCommPath)--University of Pretoria. 2016. Available at http://hdl.handle.net/2263/53477 . Accessed 17 Mar 2022.
Marcin JP, Ellis J, Mawis R, Nagrampa E, Nesbitt TS, Dimand RJ. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics. 2004;113(1 Pt 1):1–6.
Olu O, Muneene D, Bataringaya JE, Nahimana M-R, Ba H, Turgeon Y, Karamagi HC, Dovlo D. How can digital health technologies contribute to sustainable attainment of universal health coverage in Africa? A perspective. Front Public Health. 2019;7:341.
Ryan MH, Yoder J, Flores SK, Soh J, Vanderbilt AA. Using health information technology to reach patients in underserved communities: A pilot study to help close the gap with health disparities. Global J Health Sci. 2016;8(6):86.
Buckwalter KC, Davis LL, Wakefield BJ, Kienzle MG, Murray MA. Telehealth for elders and their caregivers in rural communities. Fam Community Health. 2002;25(3):31–40.
WHO Regional Committee for Africa. Promoting the role of traditional medicine in health systems: a strategy for the African Region. World Health Organization. Regional Office for Africa. Available at http://www.who.int/iris/handle/10665/95467. .
Mishra SR, Neupane D, Kallestrup P. Integrating complementary and alternative medicine into conventional health care system in developing countries: an example of Amchi. J Evid-Based Complementary Altern Med. 2015;20(1):76–9.
Mbwambo ZH, Mahunnah RL, Kayombo EJ. Traditional health practitioner and the scientist: bridging the gap in contemporary health research in Tanzania. Tanzan Health Res Bull. 2007;9(2):115–20.
Poudyal AK, Jimba M, Murakami I, Silwal RC, Wakai S, Kuratsuji T. A traditional healers’ training model in rural Nepal: strengthening their roles in community health. Trop Med Int Health : TM & IH. 2003;8(10):956–60.
Payyappallimana U. Role of Traditional Medicine in Primary Health Care: An Overview of Perspectives and Challenges. Yokohama J Social Sciences. 2009;14(6):723–43.
Kange’ethe SM. Traditional healers as caregivers to HIV/AIDS clients and other terminally challenged persons in Kanye community home-based care programme (CHBC), Botswana. SAHARA J. 2009;6(2):83–91.
Habtom GK. Integrating traditional medical practice with primary healthcare system in Eritrea. J Complement Integr Med. 2015;12(1):71–87.
Ejaz I, Shaikh BT, Rizvi N. NGOs and government partnership for health systems strengthening: a qualitative study presenting viewpoints of government, NGOs and donors in Pakistan. BMC Health Serv Res. 2011;11(1):1–7.
Wu FS. International non-governmental actors in HIV/AIDS prevention in China. Cell Res. 2005;15(11):919–22.
Biermann O, Eckhardt M, Carlfjord S, Falk M, Forsberg BC. Collaboration between non-governmental organizations and public services in health–a qualitative case study from rural Ecuador. Glob Health Action. 2016;9(1):32237.
Mercer A, Khan MH, Daulatuzzaman M, Reid J. Effectiveness of an NGO primary health care programme in rural Bangladesh: evidence from the management information system. Health Policy Plan. 2004;19(4):187–98.
Baqui AH, Rosecrans AM, Williams EK, Agrawal PK, Ahmed S, Darmstadt GL, Kumar V, Kiran U, Panwar D, Ahuja RC. NGO facilitation of a government community-based maternal and neonatal health programme in rural India: improvements in equity. Health Policy Plan. 2008;23(4):234–43.
Ricca J, Kureshy N, LeBan K, Prosnitz D, Ryan L. Community-based intervention packages facilitated by NGOs demonstrate plausible evidence for child mortality impact. Health Policy Plan. 2014;29(2):204–16.
Ahmed N, DeRoeck D, Sadr-Azodi N. Private sector engagement and contributions to immunisation service delivery and coverage in Sudan. BMJ Glob Health. 2019;4(2):e001414.
Edimond BJ. The Contribution of Non-Governmental Organizations in Delivery of Basic Health Services in Partnership with Local Government. Doctoral Dissertation, Uganda Martyrs University. 2014.
Chand S, Patterson J: Faith-Based Models for Improving Maternal and Newborn Health. IMA World Health and ActionAid International USA, 2007 Available at https://imaworldhealthorg/wp-content/uploads/2014/06/faith_based_models_for_improving_maternal_and_newborn_health.pdf
Magezi V. Churchdriven primary health care: Models for an integrated church and community primary health care in Africa (a case study of the Salvation Army in East Africa). HTS Teologiese Studies/ Theological Studies. 2018;74(2):4365.
Villatoro AP, Dixon E, Mays VM. Faith-based organizations and the Affordable Care Act: Reducing Latino mental health care disparities. Psychol Serv. 2016;13(1):92–104.
Levin J. Faith-based initiatives in health promotion: history, challenges, and current partnerships. American journal of health promotion : AJHP. 2014;28(3):139–41.
Green A, Shaw J, Dimmock F, Conn C. A shared mission? Changing relationships between government and church health services in Africa. Int J Health Plann Manage. 2002;17(4):333–53.
Bandy G, Crouch A. Building from common foundations : the World Health Organization and faith-based organizations in primary healthcare. World Health Organization; 2008. Available at https://apps.who.int/iris/handle/10665/43884 . Accessed 16 Mar 2022.
Zahnd WE, Jenkins WD, Shackelford J, Lobb R, Sanders J, Bailey A. Rural cancer screening and faith community nursing in the era of the Affordable Care Act. J Health Care Poor Underserved. 2018;29(1):71–80.
Wagle K. Primary Health Care (PHC): History, Principles, Pillars, Elements & Challenges. Global Health, 2020. Available at https://www.publichealthnotes.com/primary-health-care-phc-history-principles-pillars-elements-challenges/ . Accessed 4 June 2022.
Bhatt J, Bathija P. Ensuring access to quality health care in vulnerable communities. Acad Med. 2018;93(9):1271.
Arvey SR, Fernandez ME. Identifying the core elements of effective community health worker programs: a research agenda. Am J Public Health. 2012;102(9):1633–7.
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. Community health needs assessment: potential for population health improvement. Popul Health Manag. 2016;19(3):178–86.
Chudgar RB, Shirey LA, Sznycer-Taub M, Read R, Pearson RL, Erwin PC. Local health department and academic institution linkages for community health assessment and improvement processes: a national overview and local case study. J Public Health Manag Pract. 2014;20(3):349–55.
Desta FA, Shifa GT, Dagoye DW, Carr C, Van Roosmalen J, Stekelenburg J, Nedi AB, Kols A, Kim YM. Identifying gaps in the practices of rural health extension workers in Ethiopia: a task analysis study. BMC Health Serv Res. 2017;17(1):1–9.
Lehmann U, Sanders D. Community health workers: what do we know about them. The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers Geneva: World Health Organization; 2007. Available at https://www.hrhresourcecenter.org/node/1587.html . Accessed 17 Mar 2022.
Chen N, Raghavan M, Albert J, McDaniel A, Otiso L, Kintu R, West M, Jacobstein D. The community health systems reform cycle: strengthening the integration of community health worker programs through an institutional reform perspective. Global Health: Sci Practice. 2021;9(Supplement 1):S32–46.
Roser M, Ortiz-Ospina E: Global rise of education. Our World in Data 2017. Available at https://ourworldindata.org/global-rise-of-education . Accessed on 29 May 2019.
Santelli J, Morreale M, Wigton A, Grason H. School health centers and primary care for adolescents: a review of the literature. J Adolesc Health. 1996;18(5):357–66.
Wade TJ, Mansour ME, Guo JJ, Huentelman T, Line K, Keller KN. Access and utilization patterns of school-based health centers at urban and rural elementary and middle schools. Public Health Reports. 2008;123(6):739–50.
Johnson I, Hunter L, Chestnutt IG. Undergraduate students’ experiences of outreach placements in dental secondary care settings. Eur J Dent Educ. 2012;16(4):213–7.
Ndira S, Ssebadduka D, Niyonzima N, Sewankambo N, Royall J. Tackling malaria, village by village: a report on a concerted information intervention by medical students and the community in Mifumi Eastern Uganda. Afr Health Sci. 2014;14(4):882–8.
Frakes K-a, Brownie S, Davies L, Thomas JB, Miller M-E, Tyack Z. Capricornia Allied Health Partnership (CAHP): a case study of an innovative model of care addressing chronic disease through a regional student-assisted clinic. Aust Health Rev. 2014;38(5):483–6.
Frakes KA, Brownie S, Davies L, Thomas J, Miller ME, Tyack Z. The sociodemographic and health-related characteristics of a regional population with chronic disease at an interprofessional student-assisted clinic in Q ueensland C apricornia A llied H ealth P artnership. Aust J Rural Health. 2013;21(2):97–104.
Frakes K-A, Tyzack Z, Miller M, Davies L, Swanston A, Brownie S. The Capricornia Project: Developing and implementing an interprofessional student-assisted allied health clinic. 2011.
Frakes K-A, Brownie S, Davies L, Thomas J, Miller M-E, Tyack Z. Experiences from an interprofessional student-assisted chronic disease clinic. J Interprof Care. 2014;28(6):573–5.
Schutte T, Tichelaar J, Dekker RS, van Agtmael MA, de Vries TP, Richir MC. Learning in student-run clinics: A systematic review. Med Educ. 2015;49(3):249–63.
Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. The Lancet. 2011;377(9779):1778–97.
Rocha R, Soares RR. Evaluating the impact of community-based health interventions: evidence from Brazil’s Family Health Program. Health Econ. 2010;19(S1):126–58.
Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ (Clinical research ed). 2014;349:g4014.
Harris M. Brazil’s Family Health Programme: A cost effective success that higher income countries could learn from. BMJ: Br Med J. 2010;341(7784):1171–2.
Starfield B. Is primary care essential? The lancet. 1994;344(8930):1129–33.
Donfouet HPP, Mahieu P-A. Community-based health insurance and social capital: a review. Heal Econ Rev. 2012;2(1):1–5.
Zhang L, Wang H, Wang L, Hsiao W. Social capital and farmer’s willingness-to-join a newly established community-based health insurance in rural China. Health Policy. 2006;76(2):233–42.
Donfouet HPP. Essombè J-RE, Mahieu P-A, Malin E: Social capital and willingness-to-pay for community-based health insurance in rural Cameroon. Global J Health Sci. 2011;3(1):142.
Grunau J. Exploring people’s motivation to join or not to join the community-based health insurance’Sina Passenang’in Sotouboua, Togo. 2013.
Gitahi JW. Innovative Healthcare Financing and Equity through Community Based Health Insurance Schemes (CBHHIS) In Kenya. United States International University-Africa Digital Repository. Available at http://erepo.usiu.ac.ke/11732/3654 . Accessed 18 May 2022.
Carrin G, Waelkens MP, Criel B. Community-based health insurance in developing countries: a study of its contribution to the performance of health financing systems. Tropical Med Int Health. 2005;10(8):799–811.
Umeh CA, Feeley FG. Inequitable access to health care by the poor in community-based health insurance programs: a review of studies from low-and middle-income countries. Global Health: Science And Practice. 2017;5(2):299–314.
Odebiyi AI. Western trained nurses’ assessment of the different categories of traditional healers in southwestern Nigeria. Int J Nurs Stud. 1990;27(4):333–42.
Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med : AJTCAM. 2011;8(5 Suppl):115–23.
Taye OR. Yoruba Traditional Medicine and the Challenge of Integration. The J Pan Afr Studies. 2009;3(3):73–90.
Konadu K. Medicine and Anthropology in Twentieth Century Africa: Akan Medicine and Encounters with (Medical) Anthropology. African Studies Quarterly. 2008;10(2 & 3).
Benzie IF, Wachtel-Galor S: Herbal medicine: biomolecular and clinical aspects. 2nd Ed. 2011. Available at https://www.crcpress.com/Herbal-Medicine-Biomolecular-and-Clinical-Aspects-Second-Edition/Benzie-Wachtel-Galor/p/book/9781439807132 . Accessed 21 May 2022.
Ejughemre U. Donor support and the impacts on health system strengthening in sub-saharan africa: assessing the evidence through a review of the literature. Am J Public Health Res. 2013;1(7):146–51.
Seppey M, Ridde V, Touré L, Coulibaly A. Donor-funded project’s sustainability assessment: a qualitative case study of a results-based financing pilot in Koulikoro region. Mali Globalization and health. 2017;13(1):1–15.
Shaw RP, Wang H, Kress D, Hovig D. Donor and domestic financing of primary health care in low income countries. Health Systems & Reform. 2015;1(1):72–88.
Gotsadze G, Chikovani I, Sulaberidze L, Gotsadze T, Goguadze K, Tavanxhi N. The challenges of transition from donor-funded programs: results from a theory-driven multi-country comparative case study of programs in Eastern Europe and Central Asia supported by the Global Fund. Global Health: Science and Practice. 2019;7(2):258–72.
Ascroft J, Sweeney R, Samei M, Semos I, Morgan C. Strengthening church and government partnerships for primary health care delivery in Papua New Guinea: Lessons from the international experience. Health policy and health finance knowledge hub Working paper series. 2011(16).
Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–34.
Olivier J, Wodon Q. The role of faith-inspired health care providers in Sub-Saharan Africa and public private partnerships: Strengthening the Evidence for faith-inspired health engagement in Africa, Volume 1. Health, Nutrition and Population (HNP) Discussion Paper Series 76223v1. Available at https://documents1.worldbank.org/curated/en/851911468203673017 . Accessed 20 May 2022.
Schumann C, Stroppa A, Moreira-Almeida A. The contribution of faith-based health organisations to public health. Int Psychiatry. 2011;8(3):62–4.
Download references
Acknowledgements
The author would like to thank IPHC- E for funding this review.
This review was funded by International Institute for Primary Health Care- Ethiopia (IPHC- E).
Author information
Authors and affiliations.
Department of Environmental and Occupational Health and Safety, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Zemichael Gizaw
International Institute for Primary Health Care- Ethiopia, Ethiopian Public Health Institute, Addis Ababa, Ethiopia
Tigist Astale & Getnet Mitike Kassie
You can also search for this author in PubMed Google Scholar
Contributions
ZG prepared the manuscript. TA and GMK critically reviewed the protocol and manuscript. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Zemichael Gizaw .
Ethics declarations
Ethics approval and consent to participate.
Systematic review does not required ethics approval.
Consent for publication
This manuscript does not contain any individual person’s data.
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: .
Searchstrategy. MEDLINE (PubMed).
Additional file 2: Appendix 2: Table A1.
Description of full-text articles which discussed community health programs or community-directed interventions as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 3:
Appendix 3: Table A2. Description of full-text articles which discussed school-based healthcareservices as a strategy to improve PHCservice delivery in rural communities.
Additional file 4:
Appendix 4: Table A3. Description of full-text articles which discussed student-led healthcareservices as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 5: Appendix 5: Table A4
. Descriptionof full-text articles which discussed outreach services or mobile clinics as astrategy to improve PHC service delivery in ruralcommunities.
Additional file 6:
Appendix 6: Table A5. Description of full-text articles which discussed family health program as astrategy to improve PHC service delivery in rural,communities.
Additional file 7:
Appendix 7: Table A6. Description of full-text articles whichdiscussed empanelment as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 8:
Appendix 9: Table A8. Description of full-text articles which discussed telemedicine or mobile healthas a strategy to improve PHC service delivery in ruralcommunities.
Additional file 9:
Appendix 8: Table A7. Description of full-text articles which discussed community health funding schemes as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 10:
Appendix 10: Table A9. Description of full-text articles which discussed promoting the role of workingwith traditional healers as a strategy toimprove PHC service delivery in rural communities.
Additional file 11:
Appendix 11: Table A10. Description of full-text articles which discussed working with non-profitprivate sectors and non-governmental organizations as a strategy to improve PHC service delivery in rural communities.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gizaw, Z., Astale, T. & Kassie, G.M. What improves access to primary healthcare services in rural communities? A systematic review. BMC Prim. Care 23 , 313 (2022). https://doi.org/10.1186/s12875-022-01919-0
Download citation
Received : 09 August 2022
Accepted : 18 November 2022
Published : 06 December 2022
DOI : https://doi.org/10.1186/s12875-022-01919-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Access to PHC services
- Rural communities
- Key strategies to improve access to PHC services
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]

The Michigan Daily
One hundred and thirty-three years of editorial freedom
The tell-tale mind: Psychosis and mental health in literature
Share this:.
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)

Content warning: mentions of suicide, sexual assault and mental illness.
Lady Macbeth stands in a trance, staring at the blood upon her hands: a contamination that will plague her palms forever. The unnamed narrator of Edgar Allan Poe’s “ The Tell-Tale Heart ” sits in perpetual paranoia, spiraling as he listens to the ever-growing heartbeat under his floorboards pulsate beneath him. One by one, the doomed Lisbon sisters find themselves drowning in a depressive haze until it eventually becomes all-consuming under the societal pressures of girlhood and family. Throughout history and literature, two eternally interlinked topics, the human psyche has been an inescapable topic. To readers, there is nothing more fascinating, tragic, frightening or relevant than the depth of the human mind.
We can trace literary themes of madness back to times of mythology and oral stories, from the demise of Oedipus to the divinity of Apollo’s prophecy . Mental complexity and insanity were described poetically; the tragedy of the human mind was hauntingly beautiful. In times before mental health was studied in depth, the loss of control over one’s mind was the ultimate form of defeat, and the literature of this time reflected these sentiments.
Over the years, the depiction of mental health in literature has shifted . In the modern day, we are equipped with the necessary knowledge of mental health conditions that allows us to analyze these works through a lens of science and psychology that was not available when they were first written. A contemporary lens adds an extra dimension to literature that now stands as a product of its time.
An early example of mental illness in literature occurs in Charlotte Perkins Gilman’s 1892 short classic, “ The Yellow Wallpaper ,” which follows a woman who, after the birth of her child, is locked in a room lined with yellow wallpaper. It’s implied that she has been diagnosed with “hysteria,” which in the context of modern medicine can often be recognized as the misogynistic placeholder for postpartum depression . Though the disorder has always been common in women, the taboo around women’s mental health at the time made it difficult to diagnose and treat, leading to the condition’s most commonly prescribed solution: isolation from society. This so-called “treatment,” however, often did nothing but worsen the patient’s emotional turmoil.
Continuing into the next century, mental asylums became an even worse fate for those struggling with mental illness. Treatment in these institutions commonly took the form of unethical shock therapies and lobotomies — both of which were prevalent throughout the 20th century. Works of literature around this time similarly reflected the horrors of mental asylums, brought on by misinformation and dated medical tactics. One of the earliest examples, the 1962 novel by Ken Kesey, “One Flew Over the Cuckoo’s Nest” features the famous Nurse Ratched and her cruelty towards the men in the asylum. The novel explores themes of power dynamics, mental illness, isolation and rebellion, coalescing into a definitive critique of society as recounted by the most unreliable of narrators. Frustratingly enough, the image of this asylum is the perfect example of how deeply our perceptions of mental illness have changed. One of the characters in the novel, Dale Harding, finds himself in the asylum due to his “homosexual tendencies,” revealing the discriminatory and intolerant nature of psychology at the time. Even the treatments themselves have changed course; lobotomies and other unethical practices have ceased as ethics have come to play a greater role in the mental health system and the treatments themselves have been proven ineffective.
After the publication of “One Flew Over the Cuckoo’s Nest,” Sylvia Plath’s “ The Bell Jar ” — arguably one of the most famous literary depictions of mental illness — was published in England. The reader follows the narrator, Esther Greenwood, as she navigates life as a student in New York and the debilitating mental breakdown she later experiences. Plath’s depiction of mental illness in this novel is widely considered to be semi-autobiographical , as it is said to draw from the author’s own struggles. In fact, due to how closely the story mirrored her real life, Plath originally published the novel under the pseudonym “ Victoria Lucas .” It was not published under her real name or in the United States until after her death in 1963 (with the book’s U.S. publication following in 1971). As a result, the story remains incredibly accessible — and even relatable — to a modern audience, as Esther’s diagnosis is synonymous with what we would now call bipolar disorder and depression. The novel doesn’t set out to be a direct critique of the taboo around mental health at the time, but looking at the writing through a modern lens reveals the widespread impact this novel had by making its readers feel heard and understood.
Though this time in literary history was a turning point for accurate representation of mental illness, there were still quite a few flaws with the way in which it was depicted and perceived — namely rooted in misogyny and racism — which continued to change with time. Stories released in the last thirty years have shown the most drastic change when it comes to addressing mental health. From John Green’s depiction of OCD in “ Turtles All the Way Down ” to Kate Elizabeth Russel’s intense descriptions of the psychological turmoil following grooming and assault in “ My Dark Vanessa, ” the literary scope of this subject has shifted widely and for the better. The taboo around mental health, though still present, does not limit authors to the same extent, and those represented in media are no longer antagonized for the mental illnesses they have.
In 1999, the novel “ The Perks of Being a Wallflower ” by Stephen Chbosky hit shelves and became an international bestseller, known for its imaginative and realistic teenage characters and their everyday struggles with mental health. The narrator, Charlie, is a self-isolated teenager who undergoes his own coming-of-age; throughout the story, he experiences both the horrifying traumas and the spontaneously wonderful parts of growing up. Not only does Chbosky address the stigma that surrounds mental health with this book, he lays all of it out on the table for the reader to analyze without any ambiguity or shame.
As new books are released every year, mental health continues to be a prevalent topic of conversation, one that upcoming works of literature will hopefully continue to incorporate into their work. With time, such discussions have been handled with less nonchalance and more mindfulness about the subject’s sensitivity, and we hope to see that trend continue. The same way each human comes with their own complexities, so does each character. Literature is meant to be supplementary to our lives; it reveals the innermost parts of ourselves as we read. By carefully understanding what has made each person the way they are, the author is providing attentive care to their craft, which equates to care for the reader. Even before diagnoses were directly stated in works, a piece of the author’s self and humanity is left in their characters, making them that much more flawed and interesting. From Lady Macbeth to Charlie, their minds are connected to the author’s ink — a truth that prevails beyond the confines of an era of time.
Daily Arts Writer Archisha Pathak can be reached at [email protected] .
Related articles

The use and impact of surveillance-based technology initiatives in inpatient and acute mental health settings: A systematic review
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Jessica L. Griffiths
- For correspondence: [email protected]
- ORCID record for Katherine R. K. Saunders
- ORCID record for Una Foye
- ORCID record for Anna Greenburgh
- ORCID record for Antonio Rojas-Garcia
- ORCID record for Brynmor Lloyd-Evans
- ORCID record for Sonia Johnson
- ORCID record for Alan Simpson
- Info/History
- Supplementary material
- Preview PDF
Background: The use of surveillance technologies is becoming increasingly common in inpatient mental health settings, commonly justified as efforts to improve safety and cost-effectiveness. However, the use of these technologies has been questioned in light of limited research conducted and the sensitivities, ethical concerns and potential harms of surveillance. This systematic review aims to: 1) map how surveillance technologies have been employed in inpatient mental health settings, 2) identify any best practice guidance, 3) explore how they are experienced by patients, staff and carers, and 4) examine evidence regarding their impact. Methods: We searched five academic databases (Embase, MEDLINE, PsycInfo, PubMed and Scopus), one grey literature database (HMIC) and two pre-print servers (medRxiv and PsyArXiv) to identify relevant papers published up to 18/09/2023. We also conducted backwards and forwards citation tracking and contacted experts to identify relevant literature. Quality was assessed using the Mixed Methods Appraisal Tool. Data were synthesised using a narrative approach. Results: A total of 27 studies were identified as meeting the inclusion criteria. Included studies reported on CCTV/video monitoring (n = 13), Vision-Based Patient Monitoring and Management (VBPMM) (n = 6), Body Worn Cameras (BWCs) (n = 4), GPS electronic monitoring (n = 2) and wearable sensors (n = 2). Twelve papers (44.4%) were rated as low quality, five (18.5%) medium quality, and ten (37.0%) high quality. Five studies (18.5%) declared a conflict of interest. We identified minimal best practice guidance. Qualitative findings indicate that patient, staff and carer perceptions and experiences of surveillance technologies are mixed and complex. Quantitative findings regarding the impact of surveillance on outcomes such as self-harm, violence, aggression, care quality and cost-effectiveness were inconsistent or weak. Discussion: There is currently insufficient evidence to suggest that surveillance technologies in inpatient mental health settings are achieving the outcomes they are employed to achieve, such as improving safety and reducing costs. The studies were generally of low methodological quality, lacked lived experience involvement, and a substantial proportion (18.5%) declared conflicts of interest. Further independent coproduced research is needed to more comprehensively evaluate the impact of surveillance technologies in inpatient settings, including harms and benefits. If surveillance technologies are to be implemented, it will be important to engage all key stakeholders in the development of policies, procedures and best practice guidance to regulate their use, with a particular emphasis on prioritising the perspectives of patients.
Competing Interest Statement
AS and UF have undertaken and published research on BWCs. We have received no financial support from BWC or any other surveillance technology companies. All other authors declare no competing interests.
Clinical Protocols
https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=463993
Funding Statement
This study is funded by the National Institute for Health and Care Research (NIHR) Policy Research Programme (grant no. PR-PRU-0916-22003). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. ARG was supported by the Ramon y Cajal programme (RYC2022-038556-I), funded by the Spanish Ministry of Science, Innovation and Universities.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
The template data extraction form is available in Supplementary 1. MMAT quality appraisal ratings for each included study are available in Supplementary 2. All data used is publicly available in the published papers included in this review.
View the discussion thread.
Supplementary Material
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
- Addiction Medicine (316)
- Allergy and Immunology (617)
- Anesthesia (159)
- Cardiovascular Medicine (2277)
- Dentistry and Oral Medicine (279)
- Dermatology (201)
- Emergency Medicine (370)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (798)
- Epidemiology (11578)
- Forensic Medicine (10)
- Gastroenterology (678)
- Genetic and Genomic Medicine (3577)
- Geriatric Medicine (336)
- Health Economics (616)
- Health Informatics (2305)
- Health Policy (913)
- Health Systems and Quality Improvement (864)
- Hematology (335)
- HIV/AIDS (752)
- Infectious Diseases (except HIV/AIDS) (13154)
- Intensive Care and Critical Care Medicine (757)
- Medical Education (359)
- Medical Ethics (100)
- Nephrology (389)
- Neurology (3348)
- Nursing (191)
- Nutrition (507)
- Obstetrics and Gynecology (651)
- Occupational and Environmental Health (645)
- Oncology (1756)
- Ophthalmology (524)
- Orthopedics (209)
- Otolaryngology (284)
- Pain Medicine (223)
- Palliative Medicine (66)
- Pathology (438)
- Pediatrics (1002)
- Pharmacology and Therapeutics (422)
- Primary Care Research (406)
- Psychiatry and Clinical Psychology (3062)
- Public and Global Health (5989)
- Radiology and Imaging (1221)
- Rehabilitation Medicine and Physical Therapy (714)
- Respiratory Medicine (811)
- Rheumatology (367)
- Sexual and Reproductive Health (352)
- Sports Medicine (316)
- Surgery (386)
- Toxicology (50)
- Transplantation (170)
- Urology (142)

IMAGES
VIDEO
COMMENTS
A scoping review of the academic literature on the mental health of physicians and physicians-in-training in North America was conducted using Arksey and O'Malley's [] methodological framework.Our review objectives and broad focus, including the general questions posed to conduct the review, lend themselves to a scoping review approach, which is suitable for the analysis of a broader range ...
Scope of Mental Health Promotion and Prevention in the Current Situation. Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses (18, 36-42).There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe ...
Consequently, there is a high probability of missing critical related publications published in non-English languages. Finally, as the review depended mainly on the available literature from the aforementioned sources, which showed marked variability in their design and covered diverse ideas under the central theme, the different weights for ...
Reviews the extant literature on mental health and well-being. • Identifies the antecedents and consequences of employees' mental health and well-being. • Highlights the gaps in the existing literature and under researched areas. • Presents the findings as well as the future research directions at three interconnected levels.
Literature Review Findings. Mental health literacy is broadly defined as knowledge of mental health symptoms, interventions, and resources available, as well as positive attitudes and self-efficacy toward helping others in need. Many students were aware of counselling services and symptoms related to depression, but fewer recognized other ...
Four studies measured the effect of gender in the relationship between social media-related variables and mental health outcomes. ... Although the results of this systematic review contributed to the existing literature in a way of providing considerable evidence for the mental health impact of social media use by focussing on not only the ...
This scope review maps out the literature on the association between social support and mental health by focusing on recovery from mental health problems, and the features of social support and community mental health services. The scope begins with the notion that social support plays a substantial role in attaining and maintaining good mental ...
Abstract. The COVID-19 pandemic is a major health crisis affecting several nations, with over 720,000 cases and 33,000 confirmed deaths reported to date. Such widespread outbreaks are associated with adverse mental health consequences. Keeping this in mind, existing literature on the COVID-19 outbreak pertinent to mental health was retrieved ...
As e-mental health applications proliferate, the Internet is increasingly viewed as a potentially transformative tool that will broaden access to effective mental health services. This "rapid review" of the literature found an encouraging amount of rigorous research supporting the effectiveness of e-mental health applications, even therapist-assisted cognitive-behavioral therapy for ...
The integrative review has been identified as a unique tool in healthcare for synthesising investigations available on a given topic or phenomena and for directing practise based on scientific knowledge [].The existing body of literature on mental health among adolescents is varied and complex as there are many concepts associated with mental health research ranging from positive aspects such ...
This review aims to build on previous reviews by synthesising and appraising athlete mental health literature including intervention studies, consensus statements, position statements, and grey literature, offering the most comprehensive applied review to date. ... Henriksen et al., Citation 2020) to conducting a systematic review of related ...
This article reviews research related to mental health in students with disabilities, with a focus on understanding potential pathways between disability and mental health difficulties and examining the evidence for effective universal and targeted interventions. ... Dosen A., Buitelaar J.K., & Janzing J.G.E. (2011). Depression in Down syndrome ...
Chapter 2. REVIEW OF RELATED LITERATURE AND STUDIES. This chapter presents the relevant literature and studies that the researcher. considered in strengthening the claim and importance of the ...
Mental health literacy: A review of what it is and why it matters. Abstract. An increasing amount of scholarly work has attempted to understand the reasons for poor. rates of help-seeking for ...
Evaluations of mental health and suicide-related educational campaigns are relatively rare and generally methodologically weak, which limits definitive conclusions. Recent reviews have concluded that suicide prevention and so-called "mental health literacy" campaigns can make short-term improvements in
This literature review can be used as an evidence base by those in public health and the clinical setting and can be used to inform targeted interventions. 2. Materials and Methods. We conducted a review of the literature on the biological, psychological, and social determinants of depression in the last 4 years.
This literature review focused on the mental health and coping strategies of healthcare workers amidst pandemic. Coronavirus disease 2019 (COVID-19) has produced a worldwide health catastrophe ...
Considerable evidence suggests that psychosocial variables can shape the course of bipolar disorder. Here, though, we focus on the more specific idea that the social environment can predict the course of mania. We systematically review evidence from longitudinal studies concerning how social support, family interactions, traumatic life events, and recent life events relate to the age of onset ...
Objective: The purpose of this study is to systematically review recently published individual student-level interventions aimed at alleviating the burden of mental health challenges faced by the students and/ or at equipping them with coping mechanism that will foster their resilience. Methods: This study relied on a systematic literature review. . PubMed dataset was used; the search was ...
Third, our review did not focus on SMS-based interventions, which are also promising digital mental health tools that can enhance the impact of MBIs 101 and thus warrant future empirical attention ...
The detrimental impacts of COVID-19 on healthcare providers' psychological health and well-being continue to affect their professional roles and activities, leading to compassion fatigue. The purpose of this review was to identify and summarize published literature on compassion fatigue among healthcare providers and its impact on patient care. Six databases were searched: MEDLINE (Ovid ...
Research reveals that mental health is as closely related to an individual's physical health as it is during the face of COVID-19. Mental health has an important role in maximizing health because the body's immunity is also influenced by mental health. Therefore, it is important for every individual to maintain his mental health.
Background Severe mental illness (SMI) imposes a substantial worldwide burden of disability, highlighting the need for comprehensive and adaptable mental health services. This study aims to assess the efficacy and cost-effectiveness of community-based mental health services (CBMHS) in reducing relapse and rehospitalization rates among individuals with SMI in Iran. Method A systematic review ...
Introduction. Mental health and mental illness have been contested concepts for decades, if not centuries. Scholars from medical and non-medical disciplines, such as psychiatry, psychology, biology, neurology, philosophy, sociology, and medical history have tried to answer questions about the essence of mental health, the cause of mental health problems, and how to classify or operationalize them.
The Research Domain Criteria framework (RDoC) was created in 2010 by the National Institute of Mental Health. The framework encourages researchers to examine functional processes that are implemented by the brain on a continuum from normal to abnormal. This way of researching mental disorders can help overcome inherent limitations in using all ...
How does mental health affect the academic performance of university students? This paper provides a comprehensive literature review of the existing research on this topic, covering various ...
This systematic literature review found that community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telehealth, integrative medicine, and working with ...
The tell-tale mind: Psychosis and mental health in literature. Design by Evelyn Mousigian. Content warning: mentions of suicide, sexual assault and mental illness. Lady Macbeth stands in a trance, staring at the blood upon her hands: a contamination that will plague her palms forever. The unnamed narrator of Edgar Allan Poe's " The Tell ...
Background: The use of surveillance technologies is becoming increasingly common in inpatient mental health settings, commonly justified as efforts to improve safety and cost-effectiveness. However, the use of these technologies has been questioned in light of limited research conducted and the sensitivities, ethical concerns and potential harms of surveillance. This systematic review aims to ...