Generalized Anxiety Disorder in Very Young Children: First Case Reports on Stability and Developmental Considerations
Affiliation.
- 1 Department of Psychiatry and Behavioral Sciences, Tulane University School of Medicine, 1430 Tulane Ave., #8448, New Orleans, LA 70112, USA.
- PMID: 30345136
- PMCID: PMC6174746
- DOI: 10.1155/2018/7093178
Generalized anxiety disorder (GAD) is purported to start in early childhood but concerns about attenuation of anxiety symptoms over time and the development of emerging cognitive and emotional processing capabilities pose multiple challenges for accurate detection. This paper presents the first known case reports of very young children with GAD to examine these developmental challenges at the item level. Three children, five-to-six years of age, were assessed with the Diagnostic Infant and Preschool Assessment twice in a test-retest reliability study. One case appeared to show attenuation of the worries during the test-retest period based on caregiver report but not when followed over two years. The other two cases showed stability of the full complement of diagnostic criteria. The cases were useful for demonstrating that the current diagnostic criteria appear adequate for this developmental period. The challenges of accurate assessment of young children that might cause missed diagnoses are discussed. Future research on the underlying dysregulation of negative emotionality and long-term follow-ups are needed to better understand the etiology, treatment, and course of GAD in this age group.

Publication types
- Case Reports

- Membership & Supporters
- Facebook Support
- Social Events
- Support Groups
- Fact sheets
- Health Tips
- Personal Stories
- Books & CD's
- Lectures & Workshops
- Participate in Research
- Who does what?
- Find a Therapist
- Product Search
- Shopping Cart
- Terms & Conditions
Hannah, an anxious child
Hannah (not a real person) was a 10-year-old girl from a close, supportive family who was described as 'anxious from birth'. She had been a shy, reserved young girl at pre-school, but she integrated well in grade 1 and began making friends and succeeding academically. She complained several times of severe abdominal pain that was worst in the morning and never present at night. She had missed about 20 days of school during the previous year because of the pain. She also avoided school excursions, fearing the bus would crash. She had difficulty falling asleep and frequently asked her parents for their reassurance.
Hannah was worried that she and members of her family might die. She was unable to sleep at all before a test. She could not tolerate having her parents on a different floor of the house from herself, and she insisted on securing the house to an unnecessary extent in the evenings, fearing intruders. Her insecurity, need for constant reassurance, and school absenteeism were frustrating and upsetting for her parents.
Hannah had no personal history of traumatic events. She exhibits symptoms typical of childhood anxiety disorder, which is thought to occur in about 10% of children, equally in boys and girls before puberty. This type of disorder is diagnosed when anxiety is sufficient to interfere with daily functioning, for example Hannah's school attendance and sleep. These effects can increase and interfere to a progressively greater extent with age-appropriate functioning at home, at school and with peers, and also places sufferers at risk of developing mood disorders or substance abuse disorders in the future.
Many children experience fears; fears that are developmentally normal. Children with anxiety disorders, however, experience persistent fears or other symptoms of anxiety for months. Children can experience all the anxiety disorders experienced by adults. However, they can also experience separation anxiety disorder and selective mutism (failure to speak in certain social situations, thought to be related to social anxiety), which are unique to children. The duration of Hannah's difficulties and the symptoms, including inability to sleep, attend school regularly, go on school excursions, or face tests without extreme distress are all developmentally inappropriate, suggesting an anxiety disorder.
There is a range of common symptoms seen in anxious children. Symptoms involving thoughts include worrying, requests for reassurance, 'what if.' questions, and upsetting obsessive thoughts. Common symptoms involving behaviours include difficulty in separation, avoiding feared situations, tantrums when faced with fear, 'freezing' or mutism in feared situations, and repetitive rituals, or compulsions. Common symptoms involving feelings include panic attacks, hyperventilation, stomachaches, headaches and insomnia.
To screen quickly for one or more anxiety disorders in children, four questions are often useful:
- Does the child worry or ask for parental reassurance almost every day?
- Does the child consistently avoid certain age-appropriate situations or activities, or avoid doing them without a parent?
- Does the child frequently have stomachaches, headaches, or episodes of hyperventilation?
- Does the child have daily repetitive rituals?
These questions address the main thoughts, behaviours and feelings related to anxiety seen in children.
Megan Rodgers wishes to acknowledge an article entitled 'Childhood Anxiety Disorders' written by Dr Manassis, a Staff Psychiatrist at the Hospital for Sick Children and the Center for Addiction and Mental Health in Toronto, Ontario, on which this article is based.
Written by Megan Rodgers ADAVIC Volunteer June 2004
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Call for papers
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 32, Issue 6
- Very early family-based intervention for anxiety: two case studies with toddlers
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5603-6959 Dina R Hirshfeld-Becker 1 , 2 ,
- Aude Henin 1 , 2 ,
- Stephanie J Rapoport 1 ,
- Timothy E Wilens 2 , 3 and
- Alice S Carter 4
- 1 Child CBT Program, Department of Psychiatry , Massachusetts General Hospital , Boston , Massachusetts , USA
- 2 Department of Psychiatry , Harvard Medical School , Boston , Massachusetts , USA
- 3 Division of Child and Adolescent Psychiatry, Department of Psychiatry , Massachusetts General Hospital , Boston , Massachusetts , USA
- 4 Department of Psychology , University of Massachusetts Boston , Boston , Massachusetts , USA
- Correspondence to Dr Dina R Hirshfeld-Becker; dhirshfeld{at}partners.org
Anxiety disorders represent the most common category of psychiatric disorder in children and adolescents and contribute to distress, impairment and dysfunction. Anxiety disorders or their temperamental precursors are often evident in early childhood, and anxiety can impair functioning, even during preschool age and in toddlerhood. A growing number of investigators have shown that anxiety in preschoolers can be treated efficaciously using cognitive–behavioural therapy (CBT) administered either by training the parents to apply CBT strategies with their children or through direct intervention with parents and children. To date, most investigators have drawn the line at offering direct CBT to children under the age of 4. However, since toddlers can also present with impairing symptoms, and since behaviour strategies can be applied in older preschoolers with poor language ability successfully, it ought to be possible to apply CBT for anxiety to younger children as well. We therefore present two cases of very young children with impairing anxiety (ages 26 and 35 months) and illustrate the combination of parent-only and parent–child CBT sessions that comprised their treatment. The treatment was well tolerated by parents and children and showed promise for reducing anxiety symptoms and improving coping skills.
- childhood anxiety disorders
- preschoolers
- cognitive behavioural therapy
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/gpsych-2019-100156
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Anxiety disorders affect as many as 30% of children and adolescents and contribute to social and academic dysfunction. These disorders or their temperamental precursors 1 are often evident in early childhood, with 10% of children ages 2–5 already exhibiting anxiety disorders. 2 Anxiety symptoms in toddlerhood 3 and preschool age 4 show moderate persistence and map on to the corresponding Diagnostic and Statistic Manual anxiety disorders. 5 6 Well-meaning parents, particularly those with anxiety disorders themselves, may respond to a child’s distress around separating from parents or being around unfamiliar children by decreasing the child’s exposure to these situations, for example, by not having the child start preschool or by not leaving the child with a childcare provider to go to work or socialise. In the short term, such responses may impair concurrent family function, strain the parent–child relationship, and reduce the child’s opportunity for increased autonomy, learning and social development. 7 These avoidant strategies may initiate a trajectory where the child takes part in fewer and fewer activities, leading to social and academic dysfunction. 8
Members of our research team began championing the idea of early intervention with young anxious children over two decades ago, with the aim of teaching children and their parents cognitive–behavioural strategies to manage anxiety before their symptoms became too debilitating. 8 Although cognitive–behavioural therapy (CBT) has since emerged as the psychosocial treatment of choice for treating and preventing anxiety, 9 10 at that time, most protocols that had been empirically tested were aimed at children ages 7 through early adolescence, with only a few enrolling children as young as age 6. 11 We developed and tested a parent–child CBT intervention (called ‘Being Brave’) and reported efficacy in children as young as 4 years. 12 13 The treatment involved teaching parents about fostering adaptive coping and implementing graduated exposures to feared situations, and modelling how to teach children basic coping skills and conduct exposures with reinforcement. In parallel, a growing number of investigators confirmed that anxiety in preschoolers could be treated efficaciously using CBT administered either by training parents to apply CBT strategies with their children or through direct intervention with children. 14 15 Early family-based intervention using cognitive–behavioural strategies was shown to reduce rates of later anxiety and to attenuate the onset of depression in adolescence in girls. 16
The question remains as to whether early intervention can be extended even younger. With few exceptions, 17 18 most investigators do not offer direct CBT for anxiety to children under age 3 or 4, 15 and none to our knowledge have treated anxiety disorders with CBT in children under age 2.7. 15 However, we reasoned that since toddlers can also present with impairing symptoms, and since behaviour strategies can be feasibly applied even in preschoolers with poor language ability, 19 it ought to be possible to apply family-based CBT for anxiety to toddlers as well. We therefore present two cases of anxious children, ages 26 and 35 months, treated with parent and child CBT.
Recruitment
Parents of children ages 21–35 months were recruited for a pilot intervention study (a maximum of three cases) using advertisements to the community. To be included, children had to be rated by a parent as above a standard deviation on the Early Childhood Behavior Questionnaire Fear or Shyness Scale 20 and could not have global developmental delays, autism spectrum disorder or a primary psychiatric disorder other than anxiety.
Children were evaluated for behavioural inhibition using a 45 min observational protocol. 21 Parents completed a structured diagnostic interview about the child (Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime) that has been used with parents of children as young as 2 years; 22 23 an adapted Coping Questionnaire, 24 in which parents assessed the child’s ability to cope with their six most feared situations; and questionnaires assessing child symptoms (Child Behavior Checklist 1-1/2-5 (CBCL), 25 subscales from the Infant Toddler Social Emotional Assessment (ITSEA) 26 ), family function (Family Life Impairment Scale 27 ) and parental stress (Depression Anxiety Stress Scale 28 ). These assessments were repeated following the intervention, with the exception of the behavioural observation for the child initially rated ‘not inhibited’. The clinician rated the global severity of the child’s anxiety on a 7-point severity scale (Clinician Global Impression of Anxiety 29 ) at baseline and rated global severity and improvement of anxiety postintervention. Participant engagement in session and adherence to between-session assignments were rated by the clinician at each visit, and parents completed a post-treatment questionnaire rating the intervention.
Children were treated by the first author, a licensed child psychologist, using the ‘Being Brave’ programme. 13 It includes six parent-only sessions, eight or more parent–child sessions and a final parent-only session on relapse prevention. An accompanying parent workbook reinforces the information presented. Parent-only sessions focus on factors maintaining anxiety; monitoring the child’s anxious responses and their antecedents and consequences; restructuring parents’ anxious thoughts; identifying helpful/unhelpful responses to child anxiety; modelling adaptive coping; playing with the child in a non-directive way; protecting the child from danger rather than anxiety; using praise to reinforce adaptive coping; and planning and implementing graduated exposure. Child–parent sessions teach the child basic coping skills; and focus on planning, rehearsing and performing exposure exercises, often introduced as games, with immediate reinforcement. All parent–child sessions were preserved from the original protocol, but two sessions teaching the child about the CBT model, relaxation and coping plans were omitted, as were two sessions in which the (older) child does a summary project and celebrates gains. Up to six child–parent sessions focusing on exposure practice were included.
In the cases that follow, identifying details are disguised to protect participants’ privacy. Parents of both children provided written consent for the publication of de-identified case reports.
Background information
‘J’ was a 35-month-old girl, the third of three children of married parents. She had congenital medical problems requiring multiple surgeries, and she continued to undergo regular follow-up procedures. J met the criteria for separation anxiety disorder with marked severity, mild social phobia and mild specific phobia. Although she was able to attend her familiar day care if handed directly to a teacher and attend a gymnastics class with a friend while her mother waited in the hall, J showed great distress if apart from her mother at home. If her mother left her sight (eg, to use the bathroom), J would sob, cry and try to open the door to get in. If her mother went out and left her with a family member, J would fuss, cry and try to come along, and would continually ask to video-call her, so her mother would cut her outings short. J also had fears of doctors’ visits, of riding in the car seat, and of walking independently up and down a staircase at home. She would approach new children only with assistance from her mother, and she was afraid to take part in gymnastics performances.
J also had some mood symptoms possibly related to her medical issues. She would intermittently have days when she was much more clingy, had uncharacteristically low energy, would want to be held, and would say ‘ow, ow’ if put down to stand. She also had difficulty staying asleep and would periodically wake up with respiratory difficulties.
‘K’ was a 26-month-old boy, the only child of married parents. He met the criteria for moderate separation anxiety disorder. Although able to go to a day care he had been attending since infancy, he showed distress at drop-off particularly at the start of each week, crying for 15 min. He feared being apart from his mother in the house: he could not tolerate his mother leaving the room even to change clothes and would cry if his mother left the playroom while K played with his father. He would get distressed if his father took him on outings without his mother. He could not be dropped off at a childcare centre at his parents’ gym, leading to their avoiding exercise. He slept in his own crib, rocked to sleep by a parent, but would wake in a panic (alert but distressed) two to three times per month, crying for over an hour until his parents took him into their bed. K also was very particular about where objects were placed in the playroom and would fuss if they were put in the wrong place. He got anxious about deviations in routine (eg, taking a different path on a walk) and had trouble throwing things away (eg, used Band-Aids).
Intervention Feasibility and Outcomes
To demonstrate feasibility, the application of the treatment protocol with both participants is summarised in table 1 . Both participants completed the treatment, in 11 and 10 sessions, respectively. For each, session engagement was rated ‘moderately’ or ‘completely engaged’ at all but one session, and homework adherence was rated as ‘moderate work’ to ‘did everything assigned’ at all but one session.
- View inline
Application of treatment protocol with both participants
The quantitative results of the treatment are presented in table 2 . Both children were rated by the clinician as having shown ‘much improvement’ (Clinician Global Impression of Anxiety-Improvement 1 or 2), and both showed changes in quantitative measures of anxiety and family function. In both families, parents rated their satisfaction with the treatment as ‘extremely satisfied’, and felt that they would ‘definitely’ recommend the intervention to a friend. They rated all strategies introduced in the intervention as ‘very-’ or ‘moderately helpful’ and rated the change in their ability to help their child handle anxiety as ‘moderately-’ to ‘very much improved’.
Quantitative changes in diagnoses, coping ability, symptoms and family function in both participants
These pilot cases demonstrate the feasibility and acceptability of parent–child CBT for toddlers with anxiety disorders. The two participating families completed the treatment protocol and were consistently engaged with in-session exercises and adherent to between-session skills practice. The cases demonstrate that basic coping skills and exposure practice can be conducted with toddlers.
Although efficacy cannot be determined from uncontrolled case studies, the cases did show promising preliminary results. Both children showed a decrease in number of anxiety disorders, both were rated by the clinician (and parents) as either ‘moderately-’ or ‘much improved’ in their overall anxiety, and both showed increases in their parent-rated ability to cope with their most feared situations. Participant 2 improved on all symptom measures as well. Most significantly, his ITSEA general anxiety, separation distress, inhibition to novelty, negative emotionality, compliance and social relatedness scores and his CBCL total score, internalising score and somatic complaints scale score normalised from clinical to non-clinical range. Participant 1 had a more complicated clinical presentation, and whereas her diagnoses and coping scores improved, her parent-rated symptom scores were more mixed, perhaps related to medical problems which impacted sleep. Beyond changes in the children’s behaviour, family life impairment was reduced for both families, and parental stress was decreased out of clinical range for participant 1. Notably, both children also showed gains in areas of competence, including prosocial peer relations and mastery motivation.
This work extends previous research demonstrating that very young children experience impairing levels of anxiety that are amenable to CBT. Previous studies have found that CBT is as efficacious with older preschool-age children with anxiety disorders as it is with school-aged youth, 14 15 with approximately two-thirds of treated youth demonstrating clinically significant improvement. There is increasing recognition that anxiety disorders start early in childhood, and that there are significant advantages to intervening proximally to their onset, before anxiety symptoms crystallise and impairment accumulates. For example, one study of 1375 consecutive referrals (mean age 10.7) to a paediatric psychopharmacology clinic found that the median age of onset of a child’s first anxiety disorder was 4 years. 30 Children seeking treatment for anxiety often present in middle childhood, for symptoms which began much earlier, exposing the child and family to undue stress for years. By teaching parents and very young children skills to manage anxiety, we hope to give families important tools to navigate the developmental transitions inherent in this age range, and to help children develop a sense of mastery during a critical developmental period. Of course, a larger controlled trial is needed to further evaluate this intervention and its efficacy over time.
Assessing and treating toddlers require a developmentally informed approach. Anxiety and other symptoms may present differently in younger children, and because of limited language and cognitive abstraction capabilities toddlers are not as able to describe their fears and worries. Because some forms of anxiety (eg, separation anxiety, stranger anxiety) are normative, determination of clinically significant levels of anxiety requires an understanding of typical development in toddlerhood and the ability to conduct a detailed assessment with parents and the child using measures normed for this age group (such as the ITSEA and CBCL 1-1/2-5). Similarly, implementing CBT with toddlers and preschoolers requires age-appropriate modifications of empirically supported techniques. The adaptations we used included increased parental involvement in planning exposures, decreased focus on child cognitive restructuring (beyond framing the practice as ‘being brave’ and redirecting the child’s attention to rewarding aspects of the situation), and adaptations to exposure exercises to maximise child participation and motivation (practising at times when the child was rested and not irritable, incorporation of games and reinforcers, and allowing the child maximal choice about when/how to carry out the exposure). The cases we presented demonstrate that existing interventions can be effectively adapted and implemented with children as young as 2 years of age. By sharing the information gleaned from our research, we hope to inform providers who may be less familiar with treating children in this age range and increase their confidence in intervening with very young children.
Acknowledgments
The authors acknowledge Jordan Holmen for assistance with data checking.
- Hirshfeld-Becker DR ,
- Biederman J ,
- Henin A , et al
- Briggs-Gowan MJ ,
- Carter AS ,
- Bosson-Heenan J , et al
- Finsaas MC ,
- Bufferd SJ ,
- Dougherty LR , et al
- Spence SH ,
- McDonald C , et al
- Briggs-Gowan MJ , et al
- Biederman J
- Cowdrey FA , et al
- Banneyer KN ,
- Price K , et al
- Labellarte MJ ,
- Ginsburg GS ,
- Walkup JT , et al
- Mazursky H , et al
- Yang L , et al
- Kennedy SJ ,
- Ingram M , et al
- Bezonsky R , et al
- Chronis-Tuscano A ,
- O'Brien KA , et al
- Driscoll K ,
- Schonberg M ,
- Carter AS , et al
- Putnam SP ,
- Gartstein MA ,
- Rothbart MK
- Rosenbaum JF ,
- Hirshfeld-Becker DR , et al
- Kaufman J ,
- Birmaher B ,
- Brent D , et al
- Axelson DA , et al
- Kendall PC ,
- Hudson JL ,
- Gosch E , et al
- Achenbach TM
- Jones SM , et al
- Lovibond PF ,
- Lovibond SH
- Hammerness P ,
- Harpold T ,
- Petty C , et al
- Hembree-Kigin T ,
Dina Hirshfeld-Becker earned her undergraduate degree from Harvard and her doctorate in clinical psychology from Boston University, and completed post-doctoral training at Massachusetts General Hospital. Dr Hirshfeld-Becker is currently co-founder and co-director of the Child Cognitive Behavioral Therapy (CBT) Program in the Department of Psychiatry at MGH and an associate professor of psychology in the Department of Psychiatry at Harvard Medical School. The Child CBT Program offers short-term empirically supported CBT with youths ages 3-24, research in novel treatment adaptations, and clinical training in CBT, including on-line training courses. She pioneered the development and empirical evaluation of one of the first manualized cognitive-behavioral intervention protocols for anxiety in 4- to 7-year-old children, the “Being Brave” program, and has been exploring its use with children with autism spectrum disorder and with younger toddlers and their parents. Dr Hirshfeld-Becker has published numerous articles, reviews, and chapters. Her main research interests include the etiology, development, and treatment of childhood psychiatric disorders, particularly anxiety disorders, and in the study of early risk factors for these disorders.
Contributors DRHB designed the study with input from ASC, AH and TEW. DRHB developed the intervention and treated the cases, and DRHB, SJR and AH collected, scored, analysed and tabulated the data. DRHB wrote the first draft of the manuscript, SJR drafted parts of the Results section, and AH made significant additions to the Discussion section. AH, ASC and TEW revised the manuscript critically for important intellectual content. DRHB incorporated all of their edits and finalised the document. All authors approved the final version and are accountable for ensuring accuracy and integrity of the work.
Funding This work was supported by a private philanthropic donation by Mrs. Eleanor Spencer.
Competing interests DRHB and AH receive or have received research funding from the National Institutes of Health (NIH). ASC reports receipt of royalties from MAPI Research Trust on the sale of the ITSEA, one of the instruments included in the manuscript. TEW receives or has received grant support from the NIH (NIDA), and is or has been a consultant for Alcobra, Neurovance/Otsuka, Ironshore and KemPharm. TEW has published a book, Straight Talk About Psychiatric Medications for Kids (Guilford Press); and co/edited books: ADHD in Adults and Children (Cambridge University Press), Massachusetts General Hospital Comprehensive Clinical Psychiatry (Elsevier), and Massachusetts General Hospital Psychopharmacology and Neurotherapeutics (Elsevier). TEW is co/owner of a copyrighted diagnostic questionnaire (Before School Functioning Questionnaire), and has a licensing agreement with Ironshore (BSFQ Questionnaire). TEW is Chief of the Division of Child and Adolescent Psychiatry, and (Co)Director of the Center for Addiction Medicine at Massachusetts General Hospital. He serves as a clinical consultant to the US National Football League (ERM Associates), US Minor/Major League Baseball, Phoenix House/Gavin Foundation and Bay Cove Human Services.
Patient consent for publication Parental/guardian consent obtained.
Ethics approval All procedures were approved by our hospital’s institutional review board (Partners Human Research Committee, 2018P000376), and parents provided informed consent for themselves and their child.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
GAD-Specific Cognitive Behavioral Treatment for Children and Adolescents: A Pilot Randomized Controlled Trial
- Original Article
- Open access
- Published: 25 April 2019
- Volume 43 , pages 1051–1064, ( 2019 )
Cite this article
You have full access to this open access article
- Sean Perrin ORCID: orcid.org/0000-0002-5468-4706 1 , 2 nAff3 ,
- Denise Bevan 1 nAff4 ,
- Susanna Payne 1 &
- Derek Bolton 1 , 2
13k Accesses
14 Citations
6 Altmetric
Explore all metrics
Cognitive behavioral therapy (CBT) designed to target generalized anxiety disorder (GAD) in youth was examined in a pilot feasibility trial. Participants (aged 10–18 years) were randomized to either 10 weeks of individual CBT (n = 20) or supported wait-list (n = 20). Diagnostic status (primary outcome) was assessed blindly at post-treatment for both groups, and at a 3-month follow-up for treated participants. Two participants failed to complete CBT and retained their GAD during the trial. Intention-to-treat analyses revealed large between-group differences in favor of CBT at post-treatment for remission from GAD (80% vs 0%) and comorbid disorders (83% vs 0%), and for all secondary outcomes (child and parent-reported). All gains were maintained at 3-month follow-up in the CBT group. Consistent with the treatment model, significant pre- to post-treatment reductions in several cognitive processes were found for CBT but not wait-listed participants, with these gains maintained at follow-up. Further investigations are warranted. Trial registry: ISRCTN.com Identifier ISRCTN50951795
Similar content being viewed by others
Cognitive Behavior Therapy and Metacognitive Therapy: Moderators of Treatment Outcomes for Children with Generalized Anxiety Disorder
Monika Walczak, Sonja Breinholst, … Barbara Hoff Esbjørn

Evaluation of Cognitive-Behavioral Therapy Efficacy in the Treatment of Separation Anxiety Disorder in Childhood and Adolescence: a Systematic Review of Randomized Controlled Trials
Ludovica Giani, Marcella Caputi, … Simona Scaini
Effectiveness of an Individualized Case Formulation-Based CBT for Non-responding Youths with Anxiety Disorders
Irene Lundkvist-Houndoumadi, Mikael Thastum & Esben Hougaard
Avoid common mistakes on your manuscript.
Introduction
Generalized Anxiety Disorder (GAD) is a chronic condition characterized by excessive and uncontrollable worry about a number of events and activities, accompanied by > 3 somatic symptoms (one for children) and clinically significant distress or impairment for no less than 6 months [American Psychological Association (American Psychiatric Association (APA), 2013 ]. The 12-month prevalence of GAD in children and adolescents aged 6–18 years (hereafter youth) in the community is 1–3%, with affected individuals experiencing high rates of comorbidity, functional impairments, and a chronic course (Copeland et al. 2014 ). GAD is also one of the most commonly occurring comorbid disorders in youth seeking treatment for anxiety (Kendall et al. 2010 ). The evidence for the efficacy of transdiagnostic and GAD-specific treatments for GAD in youth is now briefly reviewed.
Cognitive behavioral therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs) are the two most studied treatments for youth with GAD, either as a primary disorder or comorbid to another anxiety disorder (Wang et al. 2017 ). The most frequently evaluated CBT approaches, including the coping cat (CC) program (Kendall 1990 ), are transdiagnostic for anxiety disorders, not disorder-specific. The preponderance of transdiagnostic CBT programs for childhood anxiety reflects a general consensus that while specific anxiety disorders can be identified in youth, comorbidity is the rule rather than exception, and can be effectively treated with a broad-based protocol focused on ‘anxiety’ (cf., Hudson et al. 2015 ; Kendall et al. 2010 ; Waite and Creswell 2014 ).
Meta-analytic studies find that SSRIs and transdiagnostic CBT programs are superior to no treatment for youth with anxiety disorders, most frequently a combination of GAD, separation anxiety disorder, social anxiety disorder, and specific phobias (James et al. 2013 ; Wang et al. 2017 ). Approximately 60% achieve remission from at least one of their comorbid anxiety disorders, with gains maintained up to 36-weeks. As outcomes for GAD are not reported, the effectiveness of transdiagnostic approaches for this this condition remain unclear (Ewing et al. 2015 ). However, there is some evidence for the efficacy of the transdiagnostic approach Cool Kids (Lyneham et al. 2003 ). Hudson et al. ( 2015 ) combined data from controlled and uncontrolled trials (at total of 848 participants) of this approach and observed a 57.6% remission rate for GAD at 3–12 months post-treatment. This is consistent with response rates for GAD reported in several early cases studies involving treatments based on the CC approach (Eisen and Silverman 1993 , 1999; Kane and Kendall 1989 ).
An empirical question arises whether outcomes for childhood GAD specifically can be improved by drawing upon models of GAD, most often developed with adults, to modify existing transdiagnostic CBT programs, or to develop new GAD-specific treatments. As an example of the former, Waters et al. (Waters et al. 2008 ) administered five sessions of CC (Kendall 1990 ) followed by five sessions of interpersonal therapy for adolescent depression (IPT-A; Mufson et al. 1994 ), to four adolescents with a primary diagnosis of GAD. All four participants were free of GAD at post-treatment, with clinically significant improvements on self-report measures of trait anxiety, depression, and interpersonal skills. The authors added IPT-A interventions based on the observation that excessive reassurance seeking from family members is common in those with GAD, and that interpersonal difficulties (generally) are more frequent in individuals with GAD compared to those with other anxiety disorders, and are associated with poorer outcomes from traditional CBT (Borkovec et al. 2002 , 2003 ; Uhmann et al. 2010 ).
As an alternative approach to modifying existing transdiagnostic CBT programs for childhood anxiety, efforts have been made to develop and test GAD-specific CBT approaches (reviewed below) that draw upon a model of worry and GAD in adults (Laval model), developed by Dugas et al. ( 1998 ). Central to the model is the trait-like phenomenon intolerance of uncertainty (IU), originally described as “cognitive, emotional and behavioral reactions to uncertainty in everyday life situations” (Freeston et al. 1994 , p. 792). The definition has evolved over time to include: “an individual’s dispositional incapacity to endure the aversive response triggered by the perceived absence of salient, key, or sufficient, information, and sustained by the associated perception of uncertainty” (Carleton 2016 , p. 31). When confronted with uncertainty, persons high in IU may engage strategies that make bouts of excessive worrying more likely or more difficult to stop (Dugas et al. 1998 ). These strategies, also mentioned in other models of GAD, include: a tendency to view uncertain outcomes as ‘threats’ that will either be difficult to prevent or to cope with if they occur ( Negative Problem Orientation –NPO); the use of distraction and suppression to reduce intrusive images of the feared outcomes and distress ( Cognitive Avoidance –CA); and dysfunctional appraisals about the nature of worries, including the belief that worrying may be necessary to prevent or lessen the impact of the feared outcomes ( Positive Beliefs About Worry –PBW).
There is now a growing body of research on the applicability of the Laval model, and in particular—the central role played by IU, to the severity of childhood worry and anxiety. Laugesen et al. ( 2003 ) found that scores on measures of IU, CA, PBW, and NPO contributed significantly to the variance in total worry, with scores on the four measures correctly classifying 72.8% of adolescents (aged 14–18 years) into moderate and high worry groups. Using measures of IU, CA, and PBW, Fialko et al. ( 2012 ) fit a path model wherein IU acted as a higher-order vulnerability factor for CA and PBW, with the three variables together influencing the severity of self-reported worry and anxiety in adolescents (aged 13–19 years). The model fit in children (aged 7–12 years) had a similar hierarchical structure but without positive beliefs about worry. Donovan et al. ( 2016 ) found that IU, CA, NPO, PBW, and negative beliefs about worry accounted for 59% of the variance in worry in children (aged 8–12 year). However, only negative beliefs about worry and CA were unique predictors, accounting for 25% and 14% of the variance. In a longitudinal study of adolescents (mean age 12.5 years), Dugas et al. ( 2012 ) found that IU and worry interacted in a bidirectional and reciprocal relationship, with changes in IU producing changes in worry and vice versa. A recent meta-analysis of 31 studies examining the relationship between IU and worry, found that IU accounted for 39.7% of the variance in child worry and 35% of the variance in child anxiety (Osmanagaoglu et al. 2018 ). This (non-exhaustive) review, suggests that processes from the Laval model of worry may be important targets for intervention in the treatment of youth with GAD.
As originally developed for use with adults, the GAD-specific treatment based on the Laval model involved modules targeting IU, PBW, NPO, and CA through worry-awareness training, exposure to situations involving uncertainty, modification of maladaptive beliefs about worries and the nature of everyday problems, and imaginal exposure to the content of worries (Dugas and Robichaud 2007 ). Trials of this treatment in adults report remission rates from GAD in the range of 70–88%, with gains maintained up to 24-months (Ladouceur et al. 2000 , 2004 ; Dugas et al. 2003 , 2010 ). Consistent with the assumptions of the Laval model of worry, changes in IU during treatment for adults with GAD has been found to be associated with changes in worry; whether the treatment was based on the Laval model (Ladouceur et al. 2000 ) or not (Bomyea et al. 2015 ; Torbit and Laposa 2016 ).
To date, three case series have been conducted that evaluate GAD-specific CBT approaches that target the four cognitive processes from the Laval model. Leger et al. ( 2003 )administered an average of 13.2 sessions of CBT to four adolescents (aged 14–18 years; no drop-outs), 43% of whom were free of their GAD diagnosis at post-treatment, declining to 28.6% at the 12-month follow-up. Payne et al. ( 2011 ) modified this treatment for use with children and younger adolescents. After an average of 9.7 sessions (and no drop-outs), 81% of the 16 participants (aged 7–17 years) were free of their GAD diagnosis, with 59% losing their comorbid anxiety and depressive disorders, and large effect size reductions in child-reported worry and anxiety. Wahlund et al. ( 2019 ) administered a 12-session, IU-focused CBT program to 12 adolescents (aged 13–18 years; no drop-outs) with excessive worry, nine of whom had GAD. The adolescent-focused sessions were supplemented by an internet-delivered program for parents designed to teach them about worry, IU, and helpful parenting behaviors. At post-treatment, 58.3% of the adolescents were rated as much or very much improved by independent clinicians, rising to 66% at the three-month follow-up. Moderate to large effect sizes were observed for adolescent-and parent-reported worry, anxiety, depression and global functioning at post-treatment (maintained at follow-up). Moderate to large effect-size reductions were also reported for self-report measures of IU, NPO, CA, and PBW, although the pre-to-post-treatment changes for PBW were non-significant.
To date, there has been one RCT of a GAD-specific treatment for youth. Holmes et al. ( 2014 ) evaluated the efficacy of a group-based, child- and parent-focused, CBT program targeting the four cognitive processes from the Laval model, as well as perfectionism and sleep difficulties. Participants were 42 children aged 7–12 years with a primary diagnosis of GAD, randomized to 10-weeks of the group treatment plus two 90-min booster sessions, or a 12-week wait-list. Parents completed a parallel, 7-session group. Three of the 20 participants (15%) in the CBT condition dropped out. Based on intention-to-treat analyses, 52.9% of the children in the CBT group were free of their GAD (and 17.6% free of all diagnoses) at post-treatment, rising to 80% at three-month follow-up. None of the children in the wait-list group lost their GAD or comorbid diagnoses. At post-treatment, there were no significant within-subject or between-group changes on child-report measures of IU, CA, NPO, and PBW. However, at follow-up, and relative to baseline, significant reductions in the moderate to large range were observed for treated participant’s scores on the measures of IU, CA, NPO–but not PBW.
The current study was designed as a randomized controlled, pilot feasibility trial with the primary aim of assessing the tolerability and efficacy of a child-friendly adaptation of the GAD-specific CBT approach described in Dugas and Robichaud ( 2007 ). This would be only the second randomized control trial of a GAD-specific treatment with children and the first to include adolescents. As such, the design incorporated a delayed-treatment (wait-list) condition as the control group. Based on the results of a previous uncontrolled trial of the current treatment approach (Payne et al. 2011 ), as well as outcomes reported in the literature for GAD-specific treatments for youth (described above), we anticipated that the current treatment would be well tolerated (i.e., < 10% drop-outs), and would yield differences in GAD remission relative to wait-list controls in excess of 50% at post-treatment. Based on the results from the two GAD-specific treatment trials that administered measures of IU, CA, NPO, and PBW (Holmes et al. 2014 ; Wahlund et al. 2019 ), we anticipated moderate to large effect-size differences for the four cognitive measures between CBT and wait-list at post-treatment, and between pre-treatment and post-treatment/follow-up for treated participants.
Participants
The 40 participants (aged 10–18 years) were recruited from standard referrals to the 10 child and adolescent mental health services and a specialist child anxiety disorders clinic affiliated with the South London and Maudsley NHS Foundation Trust (United Kingdom). The Trust serves a catchment area of approximately 1.3 million inhabitants from diverse socioeconomic and ethnic backgrounds. Referrals may be initiated by the parent (or adolescent), family doctor, school, or social services; all clinical care is free of charge.
Inclusion criteria for the trial were as follows: (1) Aged 10–18 years; (2) referred for treatment of anxiety; (3) a current, primary diagnosis of DSM-IV GAD; (4) no other psychiatric problems in need of more urgent treatment (including self-injurious thoughts/behaviors or substance use/abuse); (5) no concurrent psychological or pharmacological treatment for any disorder; and (6) the absence of moderate to severe learning difficulties as evidenced in the medical or school records or as reported by the referrer/parent at the pre-trial screening. No other inclusion/exclusion criteria were applied. All participants were fluent in English.
The study was planned as a Phase 0/1 RCT with the participants randomly allocated, in equal proportions (no stratification), to either 10 weeks of either individual, GAD-specific cognitive behavior therapy (CBT) or a supported wait-list (WL). Participants in both groups completed primary and secondary outcome measures at pre- and post-treatment/wait-list. Wait-listed participants who still required treatment at the end of the 10-week wait-list were provided immediate treatment in the clinic, either the GAD-specific CBT tested in this trial or another appropriate treatment (these data are not included in this study). CBT participants (only) were reassessed at a 3-month follow-up.
Following referral, an initial phone screening was carried out to determine if the primary complaint was GAD, and if positive, written information about the trial was sent to the family, along with a date for a face-to-face assessment with the trial coordinator. All participants attended the face-to-face assessment with at least one parent. If all inclusion criteria were met at the face-to-face assessment, the trial coordinator contacted the lead author who accessed an online, random allocation programme created by King’s College London Clinical Trials Unit for the purposes of this trial. The trial coordinator revealed the allocation to the family and told them they could withdraw from the trial at any time without negatively impacting their access to treatment. At all stages, clinical need overrode the trial protocol.
Figure 1 presents the CONSORT diagram of participant flow through the trial. Complete data were available for 38 of the 40 study participants (95%). All WL participants (n = 20) completed the 10-week wait-list, including all diagnostic interviews, secondary outcome measures, and cognitive process measures at pre- and post-wait-list. All but two of the CBT participants (both adolescents) completed treatment. One CBT participant dropped out after four sessions because they wanted to focus on social anxiety and not GAD, and another was removed from the trial after four sessions because of the onset of suicidal thoughts in response to a family crisis that began after the trial treatment had commenced. This crisis was unrelated to the participant’s GAD or treatment. While both non-completers were out of the trial, they continued to receive treatment in the clinic where the trial was carried out. The investigators were aware that they continued to suffer from GAD at the time that their (per-protocol) post-treatment and 3-month follow-up assessments would have occurred. Thus, their pre-treatment data (all) was carried forward to post-treatment and follow-up. Data for all primary, secondary, and cognitive process measures administered at pre-, post-treatment, and 3-month-follow-up were available for the remaining 18 CBT participants.
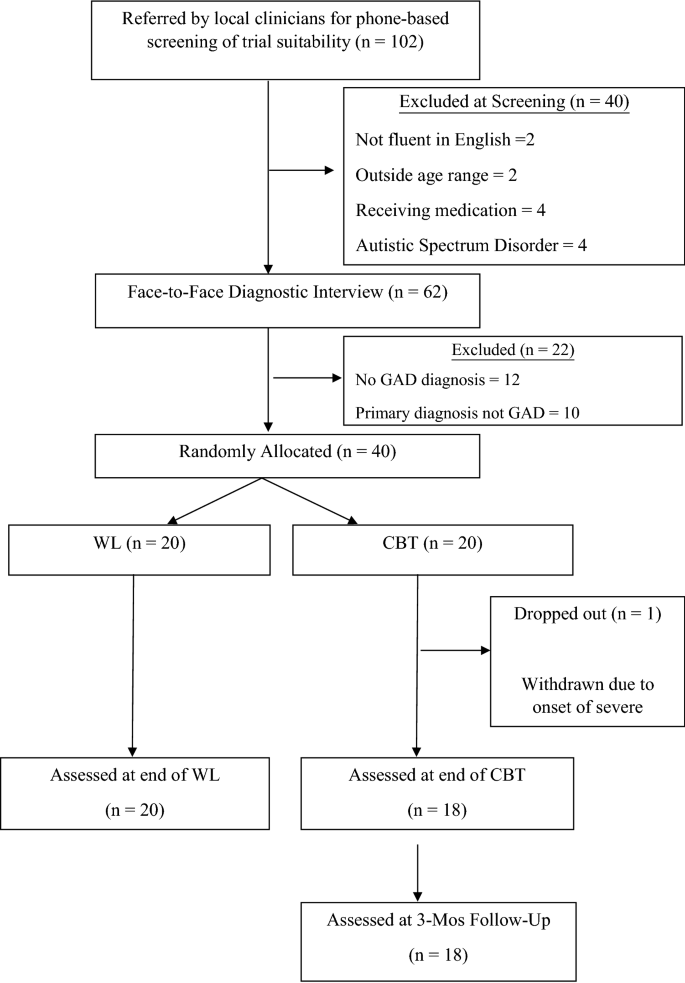
CONSORT flow chart
Primary Outcome
The primary outcome was defined as the difference in the proportion of participants with a GAD diagnosis in the CBT versus WL groups at post-treatment/wait-list. GAD was assessed with the Anxiety Disorders Interview Schedule for DSM-IV, Child and Parent Report Version (ADIS-C/P; Silverman and Nelles 1998 ). All participants, and at least one parent/primary caregiver, were interviewed separately with ADIS-C/P and the information combined to arrive at the diagnostic profile and the clinician’s separate severity ratings (0–8) for GAD and any comorbid disorders. ADIS-C/P interviews were carried out by fully qualified, doctoral-level clinical psychologists with extensive training in the use of the ADIS-C/P in clinical and research contexts. Assessors of the primary outcome at post-treatment, and for CBT participants only—the 3-month follow-up, were independent of the trial and the clinic where the trial was carried out. The assessors were blinded to the participant’s treatment allocation and history. Participants (and their parents) were given written instructions just prior to the post-treatment/wait-list and follow-up assessments not to disclose their treatment history.
Secondary Outcomes
In order to assess a broader range of outcomes than remission from GAD, several child-, parent-, and clinician-completed measures of symptoms, overall functioning, and quality of life, were administered to all participants at pre- and post-treatment/wait-list, and for CBT participants (only) at the 3-month-follow-up. The secondary outcome measures have been validated for use with children and adolescents, have excellent psychometric properties, and are routinely used in trials of anxiety disordered youth. The secondary outcome measures were as follows: (1) Worry Severity (child-report): Penn State Worry Questionnaire for Children (PSWQ-C; Chorpita et al. 1997 ); (2) Anxiety/GAD Symptoms (child and parent-report): Screen for Child Anxiety Related Emotional Disorders—Child and Parent Report Version (SCARED-C/P; Birmaher et al. 1997 ); (3) Depression (child and parent-report): Mood and Feelings Questionnaire-Child and Parent Report Versions (MFQ-C/P; Angold et al. 1995 ); (4) Conduct Problems, Peer Difficulties, Overall Impairment (parent-report): Strengths and Difficulties Questionnaire-Parent Version (SDQ-P; Goodman 1997 ); (5) Global Functioning (clinician-report): Children’s Global Assessment Scale (CGAS; Shaffer et al. 1983 ); and (6) Quality of Life (child- report): Pediatric Quality of Life Enjoyment and Satisfaction Questionnaire (PQ- LES-Q; Endicott et al. 2006 ).
Cognitive Processes from the Laval Model of Worry
At the time this trial was planned, measures of the four cognitive processes from the Laval model of worry (IU, CA, NPO, PBW), adapted and formally validated for use with children and adolescents, did not exist. For the purposes of this trial, a five-item version of each of the four self-report measures used by Dugas et al. ( 1998 ) to assess IU, CA, NPO, and PBW in adults were created (Fialko et al. 2009 ; Fialko et al. 2012 ). Briefly, for each of the four scales, five items were chosen from the original questionnaire based on these items having the highest item-total correlations, or item-subscale/factor loadings for measures with subscales. The five-item scales were then given to clinically-referred and non-referred children and adolescents, and small changes made to increase comprehensibility. The five-item measures of IU, CA, and PBW were also administered to 515 British youth (aged 7–19 years) and found to have high levels of internal consistency, similar factor structures as the full-length originals, and to correlate (positively) in the moderate to large range with self-reported worry and anxiety (Fialko et al. 2012 ). Swedish-language versions of the same five-item cognitive process measures used in this trial were found to be sensitive to the effects of an IU-focused CBT program for excessive worry in adolescents (aged 13–18 years) (Wahlund et al. 2019 ).
Intolerance of Uncertainty (IU) was assessed using the child-report, Brief Intolerance of Uncertainty Scale (Brief-IUS; Fialko et al. 2012 ). The scale is comprised of the following five-items from the 27-item IUS for adults (Freeston et al. 1994 ): Not knowing what may happen next makes my life horrible; I can’t be relaxed if I don’t know what will happen tomorrow; When I am not sure about something, I can’t get on with it; When I am not sure what will happen next, I can’t do things very well; Not knowing what may happen next can make me scared or sad. Each item is rated on a 5-point scale (1 = Not all like me; 5 = Completely like me); higher total scores indicate higher IU. The internal reliability coefficients for the Brief-IUS for the 40 participants in this study were: pre-treatment/wait-list α = .89; post-treatment/wait-list α = .95.
Cognitive Avoidance (CA) was assessed using the Brief Cognitive Avoidance Questionnaire (Brief-CAQ; Fialko et al. 2012 ), comprised of the following 5-items from the 25-item CAQ for adults (Sexton and Dugas 2008 ): There are things that I would rather not think about; I have thoughts that I try to avoid; To avoid thinking about things that upset me, I force myself to think about something else; I avoid doing anything that reminds me of things I don’t want to think about; When I have a scary picture in my mind, I say things to myself in my head to replace the picture. Each item is rated on a 5-point scale (1 = Never; 5 = always); higher total scores indicate higher CA. Internal reliability coefficients for the Brief-CAQ for the 40 participants in this study were: pre-treatment/wait-list α = .83; post-treatment/wait-list α = .90.
Positive Beliefs About Worry (PBW) were assessed using the Brief Why Worry Scale-II (Brief-WW-II; Fialko et al. 2012 ) comprised of the following 5-items from the 25-item WW-II for adults (Holowka et al. 2000 ): If I worry in advance, I will be less upset if something bad happens; Worrying can stop bad things from happening; Worrying helps me find a better way to do things; Worry helps me to get started on things I must do; The fact that I worry shows that I am a good person. Each item is rated on a 5-point scale (1 = Not all true of me; 5 = Completely true of me); higher total scores indicate higher PBW. Internal reliability coefficients for the Brief-WW-II for the 40 participants in this study were: pretreatment/wait-list α = .77; post-treatment/wait-list α = .79.
Negative Problem Orientation (NPO) was measured with the Brief Negative Problem Orientation Questionnaire (Brief-NPOQ, unpublished measure), comprised of five-items drawn from the 12-item NPOQ for adults (Robichaud and Dugas, 2005 ): I often doubt my ability to solve problems; Often my problems seem unmanageable; When I try to solve a problem I often question my own ability; I often get the impression that my problems can’t be solved; My first reaction to a problem is to question my own ability . Each item is rated on a 5-point scale (1 = Not all true of me; 5 = Completely true of me); higher scores indicate higher NPO. This scale has not been formally validated. However, the five items overlap with those from five-item measure of NPO used in the trial by Holmes et al. ( 2014 ), which found the NPO measure to be sensitive to the effects of a GAD-specific treatment based on the Laval model in children (aged 7–12 years). Internal reliability coefficients for the scale in the 40 participants in the present study were: pre-treatment/wait-list α = .93; post-treatment/wait-list α = .96.
Treatment Protocol
Cognitive behavioral therapy for gad.
The treatment was a child-friendly adaptation of the CBT for GAD approach described in Dugas and Robichaud ( 2007 ). As described by Dugas and Robichaud ( 2007 ), treatment proceeds sequentially through six stages/modules: (1) worry awareness training; (2) planned exposure to uncertainty; (3) modification of dysfunctional beliefs about worry; (4) modified problem-solving training; (5) imaginal exposure to unpleasant images or worries; and 6) relapse prevention. The treatment was successfully piloted with seven adolescents (aged 14–18 years) with GAD by Leger et al. ( 2003 ).
The modular approach and same interventions as described in Dugas and Robichaud ( 2007 ) were retained in the current trial, but the treatment was modified with the aims of making it less abstract and more engaging for children and younger adolescents who might not immediately grasp the relevant processes/concepts (IU, CA, NPO, PBW). To achieve these aims, the therapist would always use language commensurate with the young person’s age and vocabulary. Second, at the start of each module, therapist-led explanations about the cognitive processes and module were kept very brief, always confined to the beginning of a single session. It was explained to the young person that they would learn the relevant concepts more easily through the discussion of a recent worry, behavioral experiments, and imaginal exercises.
Third, the therapist would then elicit a concrete, specific and personalized example of the young person’s worrying from the past week, and use this example to help them notice “real-time” instances of the cognitive process to be targeted in that module, or if necessary because the child could not identify the cognitive process relevant to that module, a cognitive process from another module. For example, if during an exploration of concrete episodes of worry during the third module, the child was unable to identify any dysfunctional beliefs about their worries, the therapist could shift the focus to appraisals about uncertainty, negative problem orientation, cognitive avoidance, or their tolerance for uncertainty and distress related to feared outcomes. In practice, most participants (regardless of age) were able to progress through the modules as described in Dugas and Robichaud ( 2007 ). However, some participants (both children and adolescents) were not able to identify dysfunctional beliefs about worry, and rather than repeatedly engaging the participant in Socratic questioning or other exercises to elicit such beliefs, the therapist had the flexibility to move to the next or previous modules as needed.
Just prior to session 1, the child completed the self-report measure of worry (PSWQ-C), followed by a discussion about the nature of worry/GAD and its treatment, the role played by the four cognitive processes play in the maintenance of worry/GAD, and the importance of self-guided exposure to situations involving uncertainty. Thereafter, each session began with the child completing the worry measure and a brief review of their progress over the past week. From session two onwards, the therapist proceeded through the modules in the sequence described above, but in every session the therapist would elicit a concrete episode of worry from the past week that was then tied to behavioral experiments and imaginal exposures, as described in Dugas and Robichaud ( 2007 ), and with the purpose of: (a) increasing awareness about worry; (b) increasing tolerance for uncertainty; (c) reducing cognitive avoidance; (c) modifying positive beliefs about worry; (d) helping the young person distinguish between genuine problems from worries and to modify negative beliefs about their ability to solve their problems; and (e) testing the young person’s tolerance for uncertainty and feelings of fear in the event of a possible but unlikely feared outcome.
Homework tasks largely followed those described in Dugas and Robichaud ( 2007 ): (1) increasing worry awareness by pausing several times each day to reflect upon, write down, and distinguish between worries about current problems versus hypothetical situations; (2) to plan confrontations each day with situations that involve uncertainty and normally trigger worries (e.g. raising your hand in class when you are not 100% sure of the answer); (3) reducing requests for reassurance from parents/others; (4) practicing behavioral experiments to test dysfunctional beliefs about IU, CA, NPO, and PBW; and (5) engaging in self-guided exposures to the content of worries to test their ability to tolerate uncertainty and the distress. Homework assignments were always discussed in session and reflected experiments/exposures practiced in the session.
Parents were invited to join session one and asked to provide praise/rewards to their child for attempting to complete homework assignments. They were not asked to guide the child in homework exercises or to challenge their child’s maladaptive beliefs about uncertainty, the likelihood of feared outcomes, the child’s problem-solving abilities, or the worries themselves. The concept of secondary gain was introduced such that requests from the child for reassurance about worries can sometimes result in parents trying to alleviate their child’s distress through the provision of rewards or allowing the child to escape from activities that may have prompted a bout of excessive worrying. The child and parents were encouraged to be aware of these contingencies, and the parents to refrain from rewarding avoidance and reassurance seeking. No further guidance was provided to the parents about dealing with their child’s worries or reassurance-seeking.
Sessions 2–10 were one-to-one with the participant, not all of whom were brought to the clinic by their parents for every session. Where there was time and the child agreed, the parents were invited to join for the last 5–10 min of the session to discuss progress. If the therapist or parents wanted a separate meeting one could be scheduled, however, no such meetings were requested by the parents or deemed necessary by the trial therapists. Prior to the start of session 5 (mid-treatment), the child and parents completed several of the baseline symptom questionnaires and progress in treatment discussed with the child and parent separately and together during the session.
Therapist Training and Treatment Adherence
All treatment was provided by two of the authors (Payne and Bevan) under the supervision of the lead author. Both trial therapists were fully qualified doctoral-level clinical psychologists at the time of the trial. Their core professional training focused on cognitive and behavioral interventions. Both had 2–3 years of post-doctoral experience providing CBT interventions to children and/or adults with GAD and other anxiety disorders, under supervision from internationally recognized experts in CBT for child/adult anxiety.
Prior to the trial, Payne and the lead author attended a 1-day clinical workshop by Dugas on the CBT for GAD approach described in Dugas and Robichaud ( 2007 ). After the treatment manual was adapted by the authors for use with children and adolescents (described above), it was successfully piloted with 16, clinically-referred youth (aged 7–18 years) with a primary diagnosis of GAD (Payne et al. 2011 ), with Payne as the sole therapist under the supervision of the lead author. Prior to treating cases in the current trial, Bevan was provided with training in the treatment model/manual by Payne and the lead author, and then observed Payne treat five young people with GAD using the manual. Bevan then treated five youth with GAD who were not included in the current trial using the treatment manual under observation/supervisions from Payne and the lead author.
Treatment adherence was monitored through supervision with the lead author with reference to the trial manual. When permission was given by the participant/parent, a video was made of the therapy session for the purposes of supervision. The videos were used in supervision to facilitate therapist adherence to the manual. Video-recordings were not available for all sessions and were not formally rated for adherence.
Treatment Credibility and Engagement
At the end of session 2, CBT participants were given a 4-item measure of treatment credibility and therapeutic engagement to complete at home and return to the trial coordinator by post. The participants were told the therapist would not see the completed measure or be informed of the child’s views. The measure was developed for the purpose of this trial and based on the widely-used, 6-item Credibility Expectancy Questionnaire developed by Devilly and Borkovec ( 2000 ) used in clinical trials with adults. Prior to the trial, the 4-item measure was administered to 10 children and adolescents (aged 10–14) receiving CBT for an anxiety disorder and feedback obtained on the comprehensibility of the items and the rating scale. As a result of the feedback we added the phrase (‘makes sense’) to the first item (see below). The first three questions address treatment credibility: “Does this treatment seem logical (make sense) to you?” (1 = Not at all, 10 = Makes complete sense); “How certain are you that this treatment will be helpful for your problems?” (1 = Not at all certain, 10 = Completely certain); “How confident would you feel recommending this treatment to a friend with the same type of problems as you?” (1 = Not at all confident, 10 = Completely confident).
The last question addresses therapeutic engagement: “Some people think that the following things are important in therapy sessions: (1) Your therapist is warm and supportive; (2) Your therapist is helping you; (3) You and your therapist get on well; (4) You feel your therapist listens to what you have to say and treats what you say as important; (5) You and your therapist are working together as a team; (6) You and your therapist share the same way of thinking about the problem; (7) You feel that what your therapist is suggesting will be helpful. Overall, how much do you think this has been happening in your sessions so far? Please circle the number that you think is closest to how you feel” (1 = Not at all, 10 = Very much) .”
At the end of session 2, CBT participants rated the therapy as: logical/sensible (M = 8.0, SD = 1.5, Min/Max = 5/10); likely to succeed (M = 8.3, SD = 1.6, Range = 6/10); recommendable to a friend with the same problem (M = 8.5, SD = 1.5, Range = 4/10); and the therapist as warm/engaged (M = 8.9, SD = 1.0, Range = 7/10). The internal reliability coefficient for total scores on the 4-item scale in the treated participants (N = 20) was α = .78.
Wait-List Condition
At the time of allocation, wait-listed participants were provided information about the prevalence of worry and GAD, 10 copies of the self-report measure of worry (PSWQ-C), along with pre-paid envelopes addressed to the trial coordinator, and the date of their first treatment appointment after the 10-week wait-list ended. No information about causes or maintaining factors in relation to worry/GAD, or anxiety broadly, were discussed or presented in written form. The wait-listed participants were asked to complete the worry measure at the end of each week and to return it by post to the trial coordinator. No other measures were completed by the wait-listed participants during weeks 2–9 of the wait-list. The participant and their parents were told that they would receive one phone call per week from the trial coordinator to ask them how they were coping, to remind them of the date of the upcoming treatment appointment, and to complete/return the weekly worry measure. No advice about managing worries or any other difficulties were provided during these phone calls.
Statistical Analyses
Sample size was calculated a priori based on the difference between the proportion of participants in the CBT and WL group with GAD being > 50%, with < 10% drop-outs. To achieve a proportional difference this size, with 80% power, and p = 0.05, required a minimum of 14 participants per group. To account for possible drop-outs, recruitment was set at 20 participants per group. All analyses and reporting were planned on the ‘intention-to-treat’ (ITT) principle. Data for the primary outcome variable was missing for only two trial participants both in the CBT group. However, as both continued to receive treatment from the clinic where the trial was carried out, their status with respect to the primary outcome was known to the authors. With this information, and in consultation with a clinical trials unit, we used a last-observation-carried-forward strategy (LOCF).
For categorical outcomes, 2 × 2 chi squares were used to assess the proportion of CBT and WL participants remitted from their GAD diagnosis (primary outcome) and any comorbid disorders (secondary outcome) at post-treatment. For the remaining secondary outcomes (continuous), we were primarily interested in group differences at post-treatment and carried out one-way analyses of covariance (ANCOVA) with group (CBT vs WL) as the between factor, post-treatment scores as the dependent variable, and pre-treatment scores on the same measure as the covariate.
Within-subject analyses were carried out for participants in the CBT group as they underwent a further assessment at 3-month follow-up. The presence versus absence of GAD and any comorbid disorders at post-treatment versus 3-month-follow-up were examined using 2 × 2 chi squares. For all continuously-measured secondary outcomes and the cognitive process measures, one-way, repeated measure analyses of variance (ANOVA) with three timepoints (pre-, post-treatment, 3-month follow-up), and simple contrasts, were carried out. Between-group and within-subject effect sizes for all (continuous) outcomes and cognitive process measures are reported as partial eta-squared (ɳ 2 = sum of squares for the measure/sum of squares for the measure + sum of squares for error). Partial eta squared (ɳ 2 ) = .02, .13 and .26 reflect small, medium, and large effect sizes (Cohen 1988 ).
Baseline Characteristics of CBT and WL Participants
Table 1 presents the baseline characteristics separately for participants in the CBT and WL groups. Between-group comparisons for the CBT and WL on the baseline characteristics in Table 1 were evaluated using 2 × 2 Chi squares and t-tests. No significant between-group differences were observed for any of the listed variables (or for the mean number of disorders), except that more CBT participants had comorbid Separation Anxiety Disorder (χ 2 (1) = 4.8, p = .028).
Not reported in Table 1 , there were no between-group differences in respect of the proportion of participants aged 10-12 years (CBT = 55%; WL = 35%) or the mean number of current DSM-IV diagnoses (including GAD) (CBT = 1.7 (SD = .73); WL = 1.6 (SD = .59). Youth with moderate to severe learning difficulties were excluded from the study. Two participants had a statement of special educational need, one tied to a comorbid diagnosis of ADHD (randomized to CBT) and one tied to a motor disorder (randomized to WL). No other participants had a diagnosis of neurodevelopmental disorder or statement of educational need. No standardized measure of socioeconomic status was used in the study. Reflecting the socioeconomic diversity of the catchment area from which all participants were recruited, 10 of the 40 participants (25%) were living in a home where the parents were receiving either income or housing benefits (6 in CBT, 4 in WL).
Primary and Secondary Outcomes (Assessor/Clinician-Rated)
Table 2 present the proportion of participants in the CBT and WL groups meeting criteria for GAD at pre- and post-treatment (primary outcome), and for CBT participants (only) at the 3-month follow-up, and secondary assessor/clinician-rated secondary outcomes. At post-treatment/WL, CBT participants were more likely than WL participants to have remitted from their GAD diagnosis, as well from the comorbid disorders that were preset at pre-treatment/WL. Significant between group differences at post-treatment/WL, in the large range ( ɳ 2 > .26), were found for assessor’s blinded ratings of GAD severity (ADIS-C/P) and clinician-rated global functioning (CGAS). Age and gender of the participant at pre-treatment were unrelated to likelihood of remission GAD (or comorbid diagnoses) at post-treatment or 3-month follow-up for treated participants.
Within-subject analyses were carried out for the CBT participants (pre-, post-treatment, and follow-up). As noted above, significant pre-to-post treatment reductions were observed in the proportion of CBT participants with a GAD diagnosis. No further changes occurred in this variable between post-treatment and month follow-up. Significant time effects, in the large range, were observed for GAD severity (ADIS-C/P; F(2,18) = 44.8, p = .000, ɳ 2 = .78) and Global functioning (CGAS: F(2,18) = 34.6, p = .000, ɳ 2 = .77). Post-hoc comparisons (Bonferroni) revealed significant differences between pre- and post-treatment, between pre-treatment and follow-up only (all p’s = .000).
Secondary Outcomes (Child/Parent-Report)
Table 3 presents results for the secondary outcomes (child- and parent-reports). Significant differences, in the large range of effect sizes, were observed between the CBT and WL groups at post-treatment/WL for all secondary outcomes except conduct problems (parent-report). The results of the within subject analyses for CBT participants on the child/parent-report secondary outcomes and cognitive measures are not reported in Table 3 . A significant effect for time was observed for all child-reported outcomes, including: worry (PSWQ-C: F(2, 18) = 61.1, p = .000, ɳ 2 = .76); total anxiety (SCARED-C: F(2, 38) = 39.8, p = .000, ɳ 2 = .67); GAD symptoms (SCARED-C-GAD: F(2, 38) = 37.0, p = .000, ɳ 2 = .61); depression (MFQ-C: F(2, 38) = 24.4, p = .000, ɳ 2 = .60); and quality of life (PQ-LES-Q: F(2,38) = 26.9, p = .000, ɳ 2 = .59). Post-hoc comparisons (Bonferroni) revealed significant differences between pre- and post-treatment, and between pre-treatment and follow-up only (all p’s = .000).
Significant time effects were also observed for parent-reported, secondary outcomes including: total anxiety (SCARED-P Total: F(2, 38) = 29.1, p = .000, ɳ 2 = .61); GAD symptoms (SCARED-P-GAD: F(2, 38) = 20.5, p = .000, ɳ 2 = .52); depression (MFQ-P: F(2, 38) = 20.5, p = .000, ɳ 2 = .52); difficulties with peers (SDQ-P-Peer: F(2, 38) = 31.1, p = .000, ɳ 2 = .62); overall impairment (SDQ-P-Impairment: F(2, 38) = 30.9, p = .000, ɳ 2 = .62). No time effect was found for parent-reported conduct problems (SDQ-P-Behavioral: F(2, 38) = 2.5, p = .09, ɳ 2 = .12). Again, post hoc comparisons (Bonferroni) revealed significant differences between pre- and post-treatment, and between pre-treatment and follow-up only (all p’s = .000).
Cognitive Process Measures
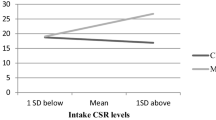
Table 4 presents results for the cognitive process measures (child-report). Significant differences, in the large range of effect sizes, were observed between the CBT and WL groups at post-treatment/WL for intolerance of uncertainty, cognitive avoidance, and negative problem orientation, but not positive beliefs about worry. For the within-subject analyses (not reported in Table 4 ) for the CBT participants, significant effects for time was observed for intolerance of uncertainty (Brief-IUS: F(2, 18) = 19.9, p = .000, ɳ 2 = .62), cognitive avoidance (Brief-CAQ: F(2, 18) = 10.9, p = .001, ɳ 2 = .41), and negative problem orientation (Brief-NPO: F(2, 18) = 19.4, p = .000, ɳ 2 = .61), but not positive beliefs about worry (Brief-WW-II: F(2, 18) = 7.1, p = .06, ɳ 2 = .27). For intolerance of uncertainty, cognitive avoidance, and negative problem orientation, post hoc comparisons (Bonferroni) revealed significant differences between pre- and post-treatment, and between pre-treatment and follow-up only (all p’s = .000).
This study was designed as a randomized controlled, pilot feasibility trial with the aim of assessing the tolerability and efficacy of an individual, child-focused, GAD-specific CBT under randomized controlled conditions. The treatment is based on (and targets) four cognitive processes from the Laval model of worry: intolerance of uncertainty, cognitive avoidance, negative problem orientation, and positive beliefs about worry. The secondary aim was to assess whether changes in these four processed occurred for the treated versus the wait-listed participants. This is only the second controlled trial of GAD-specific CBT with children and the first with adolescents. It is the third trial to report change scores on measures of the four cognitive processes from the Laval model.
The treatment was well tolerated with only two non-completers, both adolescents. One of whom removed themselves from the trial because they wanted to focus more on their symptoms of social anxiety disorder. The other was removed from the trial due to an acute onset suicidal depression relating to a family crisis, not their GAD diagnosis or treatment. Using a measure developed for this trial, the participants reported that the treatment was highly credible, and they felt able to engage well with their therapist. Including the present study, three trials have been carried out with children between seven and 12 years of age using GAD-specific CBT targeting the four cognitive processes from the Laval model, with less than 15% drop-outs, and high rates of recovery (Holmes et al. 2014 ; Payne et al. 2011 ). While further research is needed, the findings from the three trials suggest that children and adolescents are able to engage with a treatment focused largely on cognitive processes associated with worry and GAD severity.
For the primary outcome variable, measured according to intention-to-treat, a large and significant difference was observed between the CBT and wait-listed participants for GAD remission (80% vs 0%, respectively) There was a slight but non-significant increase in the proportion of CBT participants with GAD at follow-up (85%), suggesting that improvements at the diagnostic threshold level were largely maintained. These findings are similar to the intention-to-treat outcomes for GAD remission reported for post-treatment in our uncontrolled pilot of the same treatment (81%; Payne et al. 2011 ), and at the 3 month-follow up (80%; intention-to-treat) in the randomized controlled trial of a group-based treatment (Holmes et al. ( 2014 ). The present findings for GAD remission rates are also comparable to those reported in trials of adults with GAD treated with the CBT approach (Dugas and Robichaud 2007 ) on which the current treatment is based (70–88%; Ladouceur et al. 2000 , 2004 ; Dugas et al. 2003 , 2010 ).
Consistent with Payne et al. ( 2011 ) and Holmes et al. ( 2014 ), the effects of the present treatment were not limited to remission from GAD. Significant reductions were observed in the rate of comorbid disorders, as well as moderate to large effects for child- and parent-reported worry, anxiety, depression, peer problems, overall impairment, and quality of life. These gains were maintained at the 3-month follow-up for treated participants.
The present study was also designed to assess whether changes in GAD and worry would be accompanied by changes in the four cognitive processes that are targeted in treatment. Consistent with the Laval model, and expectation, treated participants experienced large reductions in IU, cognitive avoidance, and negative problem orientation. However, no significant changes were found for positive beliefs about worry. The same pattern of findings for the four cognitive processes were reported by both Holmes et al. ( 2014 ) and Wahlund et al. ( 2019 ). This trial was not designed to test for mediation and so it not possible to conclude that changes in the primary or secondary outcomes occurred because of changes in IU, cognitive avoidance, or negative problem orientation, or that the interventions themselves were responsible for any observed changes in these processes. What the present findings, and those of previous GAD/IU-focused treatments with youth, do suggest is that trials capable of assessing whether changes in the four cognitive processes mediate outcomes are warranted.
The absence of findings for positive beliefs about worry in the present trial requires further comment. It is possible that the lack of change in this process during treatment, not just in this trial but also in Holmes et al. ( 2014 ) and Wahlund et al. ( 2019 ), reflects a problem with the way that positive beliefs about worry were measured. Both this trial and Wahlund et al. ( 2019 ), used a 5-item version of the 25-item, Why Worry Scale-II scale for adults (Holowka et al. 2000 ). Holmes et al. ( 2014 ) used a 6-item subscale from the Metacognitions Questionnaire for Children (Bacow et al. 2009 ). While scores on these measures of positive beliefs about worry correlate in the moderate to large range with child- and adolescent-reported worries and anxiety (Bacow et al. 2009 ; Fialko et al. 2012 ), it is possible that neither scale is sufficiently sensitive to positive beliefs about worry for treatment purposes. At present, there is no consensus in the literature on the measurement of IU, cognitive avoidance, negative problem orientation, or positive beliefs about worry (in adults or children). Further, scale development, and validation with children and adolescents, is necessary before any conclusions can be drawn about the importance of targeting positive beliefs about worry in young people with GAD.
As a pilot examination of the tolerability and efficacy of a GAD-specific treatment for youth, the study benefitted from several strengths, including: a randomized controlled design; a manualized treatment; primary outcomes based on blinded, structured diagnostic interviews; a broad range of standardized, secondary outcome measures obtained from multiple informants; and the use of measures designed to assess processes assumed to underlie change in treatment. This is only the second randomized controlled trial of a GAD-specific treatment carried out with children and the first with adolescents. Nevertheless, the findings must be viewed within the context of certain limitations. While a comparison with wait-list controls, and a brief follow-up for treated participants, are appropriate design elements for a pilot feasibility trial, studies involving active treatment and placebo controls, and longer follow-ups are are needed to properly estimate the efficacy of the present treatment. Second, while the treatment was manualized, and the therapists trained and supervised in its use, no formal treatment adherence protocol was followed. Third, inter-rater reliability ratings were not obtained for the diagnostic assessments. Fourth, the treatment credibility and cognitive process measures were developed specifically for this trial and required further examination of their validity in clinical samples. Finally, treatment was delivered in a specialist anxiety disorders clinic by experienced therapists receiving weekly supervision. The treatment should also be evaluated in routine care settings where most anxiety disordered children are seen.
In conclusion, the present findings add to a small body of literature suggesting that GAD-specific CBT treatments are acceptable to children as young as 7 years and adolescents up to 19 years. In uncontrolled and controlled trials involving wait-list controls, these treatments appear to yield high rates of remission from GAD and comorbid disorders, as well as moderate to large reductions in worry, anxiety, depressive symptoms, and overall functioning. The findings also add to a small body of evidence suggesting that IU, cognitive avoidance, negative problem orientation, and positive beliefs are associated with the severity of worry, anxiety and GAD in youth, and important targets for further investigation in a clinical context.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: APA.
Google Scholar
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: APA.
Book Google Scholar
Angold, A., Costello, E. J., Messer, S. C., Pickles, A., Winder, F., & Silver, D. (1995). The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research, 5, 237–249.
Bacow, T. L., Pincus, D. B., Ehrenreich, J. T., & Brody, L. R. (2009). The metacognitions questionnaire for children: Development and validation in a clinical sample of children and adolescents with anxiety disorders. Journal of Anxiety Disorders, 23 (6), 727–736.
Article PubMed Google Scholar
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., et al. (1997). The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry, 4, 545–553.
Article Google Scholar
Bomyea, J., Ramsawh, H., Ball, T. M., Taylor, C. T., Paulus, M. P., Lang, A. J., et al. (2015). Intolerance of uncertainty as a mediator of reductions in worry in a cognitive behavioral treatment program for generalized anxiety disorder. Journal of Anxiety Disorders, 33, 90–94.
Article CAS PubMed PubMed Central Google Scholar
Borkovec, T. D., Newman, M. G., Pincus, A. L., & Lytle, R. (2002). A component analysis of cognitive-behavioral therapy for generalised anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology, 70, 288–298.
Article CAS PubMed Google Scholar
Borkovec, T. D., Newman, M. G., & Castonguay, L. G. (2003). Cognitive behavioural therapy for generalized anxiety disorder with integrations from interpersonal and experiential therapies. CNS Spectrums, 8, 382–389.
Carleton, R. N. (2016). Into the unknown: A review and synthesis of contemporary models involving uncertainty. Journal of Anxiety Disorders, 39, 30–43.
Chorpita, B. F., Tracey, S. A., Brown, T. A., Colica, T. J., & Barlow, D. H. (1997). Assessment of worry in children and adolescents: An adaptation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 35, 569–581.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences . New Jersey: Routledge.
Copeland, W. E., Angold, A., Shanahan, L., & Costello, E. J. (2014). Longitudinal patterns of anxiety from childhood to adulthood: The great smoky mountains study. Journal of the American Academy of Child and Adolescent Psychiatry, 53 (1), 21–33.
Devilly, G. J., & Borkovec, T. D. (2000). Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy and Experimental Psychiatry, 31, 71–86.
Donovan, C. L., Holmes, M. C., & Farrell, L. J. (2016). Investigation of the cognitive variables associated with worry in children with generalised anxiety disorder and their parents. Journal of Affective Disorders, 192, 1–7.
Dugas, M., & Robichaud, M. (2007). Cognitive-behavioural therapy for generalized anxiety disorder . New York: Routledge.
Dugas, M. J., Gagnon, F., Ladouceur, R., & Freeston, M. H. (1998). Generalized anxiety disorder: A preliminary test of a conceptual model. Behavior Research and Therapy, 36, 215–226.
Article CAS Google Scholar
Dugas, M. J., Ladouceur, R., Leger, E., Freeston, M. H., Langlois, F., Provencher, M. D., et al. (2003). Group cognitive-behavioral therapy for generalized anxiety disorder: Treatment outcome and long-term follow-up. Journal of Consulting and Clinical Psychology, 4, 821–825.
Dugas, M. J., Brillon, P., Savard, P., Turcotte, J., Gaudet, A., Ladouceur, R., et al. (2010). A randomized clinical trial of cognitive-behavioural therapy and applied relaxation for adults with generalized anxiety disorder. Behavior Therapy, 41 (1), 46–58.
Dugas, M. J., Laugesen, N., & Bukowski, W. M. (2012). Intolerance of uncertainty, fear of anxiety, and adolescent worry. Journal of Abnormal Child Psychology, 40 (6), 863–870.
Eisen, A., & Silverman, W. K. (1993). Should I relax or change my thoughts? A preliminary examination of cognitive therapy, relaxation training, and their combination with overanxious children. Journal of Cognitive Psychotherapy, 7, 265–279.
Eisen, A. R., & Silverman, W. K. (1999). Prescriptive treatment for generalized anxiety disorder in children. Behavior Therapy, 29 (1), 105–121.
Endicott, J., Nee, J., Yang, R., & Wohlberg, C. (2006). Pediatric quality of life enjoyment and satisfaction questionnaire (PQ-LES-Q): Reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry, 45 (4), 401–407.
Ewing, D. L., Monsen, J. J., Thompson, E. J., Cartwright-Hatton, S., & Field, A. (2015). A meta-analysis of transdiagnostic cognitive behavioural therapy in the treatment of child and young person anxiety disorders. Behavioural & Cognitive Psychotherapy, 43 (5), 562–577.
Fialko, L. (2009). Cognitive variables associated with worry in young people aged 7-18 (Doctoral dissertation). Institute of Psychiatry, Psychology & Neuroscience, King’s College London.
Fialko, L., Bolton, D., & Perrin, S. (2012). Applicability of a cognitive model of worry to children and adolescents. Behaviour Research and Therapy, 50 (5), 341–349.
Freeston, M. H., Rhéaume, J., Letarte, H., Dugas, M. J., & Ladouceur, R. (1994). Why do people worry? Personality and Individual Differences, 17, 791–802.
Goodman, R. (1997). The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38, 581–586.
Holmes, M. C., Donovan, C. L., Farrell, L. J., & March, S. (2014). The efficacy of a group- based, disorder-specific treatment program for childhood GAD: A randomized controlled trial. Behavior Research and Therapy, 61, 122–135.
Holowka, D. W., Dugas, M. J., Francis, K., & Laugesen, N. (2000). Measuring beliefs about worry: A psychometric evaluation of the Why Worry - II Questionnaire. Poster presented at the Association for Advancement of Behavior Therapy’s 34th Annual Convention, New Orleans, LA.
Hudson, J. L., Rapee, R. M., Lyneham, H. J., McLellan, L. F., Wuthrich, V. M., & Schniering, C. A. (2015). Comparing outcomes for children with different anxiety disorders following cognitive behavioural therapy. Behavior Research and Therapy, 72 (9), 30–37.
James, A. C., James, G., Cowdrey, F. A., Soler, A., & Choke, A. (2013). Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Systematic Review . https://doi.org/10.1002/14651858.CD004690.pub3 .
Kane, M. T., & Kendall, P. C. (1989). Anxiety disorders in children: A multiple-baseline evaluation of a cognitive-behavioral treatment. Behavior Therapy, 20, 499–508.
Kendall, P. C. (1990). The coping cat manual . Ardmore PA: Workbook Publishing.
Kendall, P. C., Compton, S. N., Walkup, J. T., Birmaher, B., Albano, A. A., Sherrill, J., et al. (2010). Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders, 24 (3), 360–365.
Article PubMed PubMed Central Google Scholar
Ladouceur, R., Dugas, M., Freeston, M. H., Leger, E., Gagnon, F., & Thibodeau, N. (2000). Effectiveness of a new cognitive-behavioral treatment for generalized anxiety disorder: Evaluation in a controlled clinical trial. Journal of Consulting and Clinical Psychology, 68, 957–964.
Ladouceur, R., Léger, É., Dugas, M., & Freeston, M. (2004). Cognitive-behavioral treatment of generalized anxiety disorder (GAD) for older adults. International Psychogeriatrics, 16 (2), 195–207.
Laugesen, N., Dugas, M. J., & Bukowski, W. M. (2003). Understanding adolescent worry: The application of a cognitive model. Journal of Abnormal Child Psychology, 31, 55–64.
Leger, E., Ladouceur, R., Dugas, M. J., & Freeston, M. H. (2003). Cognitive-behavioural treatment of generalized anxiety disorder among adolescents: A case series. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 327–330.
Lyneham, H. J., Abbott, M. J., Wignall, A., & Rapee, R. M. (2003). The cool kids anxiety treatment program . Sydney, Australia: MUARU, Macquarie University.
Mufson, L., Moreau, D., & Weissman, M. M. (1994). Modification of interpersonal psychotherapy with depressed adolescents (IPT-A): Phase I and phase II studies. Journal of the American Academy of Child and Adolescent Psychiatry, 33 (5), 695–705.
Osmanağaoğlu, N., Creswell, C., & Dodd, H. F. (2018). Intolerance of uncertainty, anxiety, and worry in children and adolescents: A meta-analysis. Journal of Affective Disorders, 225, 80–90.
Payne, S., Bolton, D., & Perrin, S. (2011). A pilot investigation of cognitive therapy for generalized anxiety disorder in children aged 7-17 years. Cognitive Therapy & Research, 25 (2), 171–178.
Robichaud, M., & Dugas, M. J. (2005). Negative problem orientation (Part I): Psychometric properties of a new measure. Behaviour Research and Therapy, 43 (3), 391–401.
Sexton, K. A., & Dugas, M. J. (2008). The cognitive avoidance questionnaire: Validation of the english translation. Journal of Anxiety Disorders, 22 (3), 355–370.
Shaffer, D., Gould, M. S., Brasic, J., Ambrosini, P., Fisher, P., Bird, H., et al. (1983). A children’s global assessment scale (CGAS). Archives of General Psychiatry, 40 (11), 1228–1231.
Silverman, W., & Nelles, W. (1998). The anxiety disorders interview schedule for children. Journal of the American Academy of Child and Adolescent Psychiatry, 27, 772–778.
Torbit, L., & Laposa, J. M. (2016). Group CBT for GAD: The role of change in intolerance of uncertainty in treatment outcomes. International Journal of Cognitive Therapy, 9 (4), 356–368.
Uhmann, S., Beesdo-Baum, K., Becker, E. S., & Hoyer, J. (2010). Specificity of interpersonal problems in generalized anxiety disorder versus other anxiety disorders and depression. Journal of Nervous & Mental Disorders, 198 (11), 846–851.
Wahlund, T., Andersson, E., Jolstedt, M., Perrin, S., Vigerland, S., & Serlachius, E. (2019). Intolerance of uncertainty-focused treatment for adolescents with excessive worry-a pilot feasibility study. Cognitive & Behavioral Practice.
Waite, P., & Creswell, C. (2014). Children and adolescents referred for treatment of anxiety disorders: Differences in clinical characteristics. Journal of Affective Disorders, 167 (100), 326–332.
Wang, Z., Whiteside, S. P., Sim, L., Farah, W., Morrow, A. S., Alsawas, M., et al. (2017). Comparative effectiveness and safety of cognitive behavioral therapy and pharmacotherapy for childhood anxiety disorders: A systematic review and meta-analysis. JAMA Pediatrics, 171 (11), 1049–1056.
Waters, A. M., Donaldson, J., & Zimmer-Gembeck, M. J. (2008). Cognitive-behavioural therapy combined with an interpersonal-skills component in the treatment of generalised anxiety disorder in adolescent females: A case series. Behaviour Change, 25 (1), 35–43.
Download references
Acknowledgements
The authors express their sincere gratitude to the participating families. We would like to thank the reviewers for their comments on an earlier version of the manuscript.
This work was supported by a grant from the National Institute of Health Research to S. Perrin and D. Bolton (NIHR; 0808-17094), and with additional supports from the Guy’s & St Thomas’ Charity (EFT 120604), and the NIHR Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Author information
Sean Perrin
Present address: Department of Psychology, Lund University, Box 213, 221 00, Lund, Sweden
Denise Bevan
Present address: Cumberledge Intermediate Care Centre, Southend-on-Sea, UK
Authors and Affiliations
South London & Maudsley NHS Foundation Trust, London, UK
Sean Perrin, Denise Bevan, Susanna Payne & Derek Bolton
Institute of Psychiatry Psychology & Neuroscience, King’s College London, London, UK
Sean Perrin & Derek Bolton
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sean Perrin .
Ethics declarations
Conflict of interest.
Sean Perrin, Denise Bevan, Susanna Payne, and Derek Bolton declare that they have no conflicts of interest.
Ethical Approval
This study was approved by the National Health Service Research Ethics Committee (ref: 09/H0720/127) and Institutional Review Board of the South London and Maudsley NHS Foundation Trust. All procedures were performed in accordance with the ethical standards of the institution, the research ethics committee, and the 1964 Helsinki declaration, and its later amendments, on research with human subjects.
Informed Consent
Written informed consent was obtained from the participants and at least one parent or legal guardian. No financial incentive was offered for participation.
Animal Rights
No animals studies were carried out by the authors for this article.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Perrin, S., Bevan, D., Payne, S. et al. GAD-Specific Cognitive Behavioral Treatment for Children and Adolescents: A Pilot Randomized Controlled Trial. Cogn Ther Res 43 , 1051–1064 (2019). https://doi.org/10.1007/s10608-019-10020-3
Download citation
Published : 25 April 2019
Issue Date : December 2019
DOI : https://doi.org/10.1007/s10608-019-10020-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Generalized anxiety disorder
- Cognitive behavior therapy
- Laval model
- Intolerance of uncertainty
- Adolescents
- Find a journal
- Publish with us
- Track your research
Internet Explorer is no longer supported
Please upgrade to Microsoft Edge , Google Chrome , or Firefox .
Lo sentimos, la página que usted busca no se ha podido encontrar. Puede intentar su búsqueda de nuevo o visitar la lista de temas populares.
Get this as a PDF
Enter email to download and get news and resources in your inbox.
Share this on social
Generalized anxiety disorder in kids.
When near-constant worry affects your child’s well-being
Writer: Shelley Flannery
Clinical Experts: Emily Gerber, PhD , Jerry Bubrick, PhD
What You'll Learn
- How is generalized anxiety disorder different from other forms of anxiety?
- What do kids with generalized anxiety disorder worry about?
- How can we help kids with generalized anxiety disorder?
Most kinds of anxiety focus on a particular worry — fear of heights, separating from parents, speaking in public, things like germs or spiders. But some kids are anxious about many things. They have what’s called generalized anxiety disorder or GAD.
Kids with GAD worry about everything, and it often takes the form of “what ifs”:
“What if we run out of gas?
“What if mom loses her job?
“What if a hurricane blows away our house?
“What if I get a bad grade?”
Kids with GAD tend to imagine the worst happening, and their anxiety may not be triggered by anything in particular. They may be irritable and have trouble sleeping.
Kids with GAD also tend to be perfectionists. They may put enormous pressure on themselves to perform well — more than their teachers or parents — and may avoid doing things because they’re worried about not doing them well enough. They may have anxious stomachaches and headaches and spend a lot of time in the school nurse’s office.
It’s important to get help for kids with GAD because all that worry can lead to depression, and it also leads, for teenagers, to substance use —drinking alcohol or smoking pot to ease their anxiety.
Treatment for GAD includes cognitive behavior therapy (CBT), in which kids learn to recognize irrational thinking and replacing it with more logical, healthy ways of thinking. An alternative is acceptance and commitment therapy (ACT), which teaches kids to acknowledge and accept the anxious thoughts they’re having and commit to moving forward despite them. Parents also learn how to avoid enabling their child’s anxiety and instead support their overcoming it.
Severe GAD may be treated with a combination of therapy and medication, usually an antidepressant called an SSRI.
For a lot of kids with anxiety, excessive worry is triggered by a specific situation, such as being away from their parents, public speaking, heights or a scary animal. But kids who worry excessively about numerous things may have generalized anxiety disorder.
Generalized anxiety disorder (GAD) is characterized as constant worry about lots of different things that aren’t really threats and/or overreacting to minor threats. It’s the most common type of anxiety disorder among children and teens.
Unlike with a phobia, which has a specific trigger — spiders, needles, dogs, airplanes, clowns, etc. — children with GAD worry about a variety of everyday situations.
“Kids with generalized anxiety disorder worry about all the same things that other kids worry about,” says Emily Gerber, PhD , the senior director of the Anxiety Disorders Center at the Child Mind Institute’s San Francisco Bay Area clinic, “but they worry more often and more intensely.”
There doesn’t even necessarily have to be anything that triggers it, adds Dr. Gerber. “It’s sort of always there.”
Si gns of GAD
“Kids with GAD are chronic worriers,” says Jerry Bubrick, PhD, a senior clinical psychologist at the Child Mind Institute. “There’s no area that they don’t worry about, but the typical areas of worry are usually around health of themselves or their family, money, and safety and stability.”
Kids with GAD worry about the “what if’s,” adds Dr. Bubrick.
“What if we run out of gas?”
“What if mom loses her job?”
“What if a hurricane blows away our house?”
They tend to imagine the worst happening, and seek reassurance from parents that it won’t.
Dr. Bubrick has seen kids, for example, who are super worried if a big storm is coming in. Then, if nothing bad happens, they’re worried about another storm coming. What if we’re not as prepared next time? They’re glued to the weather reports with excessive worry.
Dr. Gerber describes a child who developed GAD during the pandemic. “His aunt was in the ICU for a while during COVID, and so he started to become overly concerned about everybody around him,” she says. “He was constantly asking, ‘Are they going to be okay?’ and didn’t want anyone to go out because he was so worried they would get sick.”
Other signs of GAD in children and teens include:
- Restlessness or feeling on edge
- Apprehensiveness
- Indecisiveness
- Being easily fatigued, especially at the end of the school day
- Irritability
- Trouble sleeping
- Difficulty concentrating or feeling their mind go “blank”
- Catastrophizing or always expecting the worst
Kids with GAD are perfectionists
Most kids feel anxious about their performance in school from time to time and may worry about an upcoming test or presentation. A child with GAD, however, is likely to take that worry to an extreme, and study obsessively even though they already know the material.
“There’s one 9-year-old in particular I’m thinking of whose parents are very ambitious and so he only wants to get A-pluses at school,” Dr. Gerber says. “He has this terrible fear that if he submits an assignment and it’s anything less than perfect, his life is going to be ruined. As a result, he’s developed some avoidant behaviors. He either is distressed or he’s so avoidant that he completely forgets about the assignment.”
Dr. Bubrick adds that some kids with GAD are such perfectionists that they don’t want to do anything unless they can be the best at it. “They will think, ‘If I can’t be the best at something, then why try? If I can’t be a rock star, then why take guitar lessons?’ “
They may have anxious stomachaches and headaches and spend a lot of time in the school nurse’s office.
Who’s at risk?
GAD can develop in children as early as 5 but is most frequently diagnosed in adolescents. It tends to affect girls more than boys, but all genders can develop the disorder. Kids with sensitive temperaments are more likely than others to develop generalized anxiety.
The largest predictor of GAD in children and teens is family history. Kids who have one parent with any kind of anxiety disorder are more likely to have generalized anxiety than other kids; those with two parents with anxiety are significantly more at risk. Experts believe the risk stems from a combination of biology and learned behaviors — seeing how a parent deals with stress and worry and emulating that behavior.
And if there’s one thing kids today have an abundance of, it’s stress. Rates of anxiety had already been on the rise when COVID-19 hit the U.S. in March 2020. The pandemic accelerated the development of the disorder in many young people. Between 2016 and 2020, anxiety rates among kids had increased from 7.1% to 9.2%, according to a study published in JAMA Pediatrics whereas a review published just a year later in the Journal of Psychiatric Research reported rates of anxiety among kids were between 19% and 24%.
“The pandemic was a major anxiety trigger for a lot of Americans, especially kids, who rely on school for most of their socialization,” Dr. Gerber says. “And unfortunately, we have yet to see rates of GAD slow down. We’re still seeing kids with anxiety levels parents say they’ve not seen before.”
When GAD goes untreated
Without treatment, GAD typically worsens over time. If you suspect your child might have generalized anxiety disorder, it’s a good idea to get them evaluated. The sooner GAD is diagnosed and treated, the fewer long-term complications your child will develop.
“The danger is that if GAD isn’t treated and kids don’t learn how to cope with anxiety in safe and effective ways, it can continue to erode their functioning,” Dr. Gerber says. “It really can become chronic and is a strong predictor of depression and other disorders later in life.”
Another real concern, particularly for adolescents and teens, is substance use.
“There are a lot of kids — when they haven’t gotten treatment — who will self-medicate and start drinking alcohol or smoking pot to ease their anxiety,” Dr. Gerber says. “But a lot of times, the opposite happens. It might be a relief initially, but if they don’t learn to cope with the discomfort and develop skills for dealing with their feelings, then the anxiety will continue to increase and often so will the substance use.”
Treatment options
Most instances of GAD can be treated with psychotherapy in the form of cognitive behavior therapy (CBT) or acceptance and commitment therapy (ACT).
With CBT, children and teens are taught their worries are not based in fact and learn ways to cope with anxious thoughts when they arise. Exposure therapy, a CBT technique commonly used in the treatment of anxiety, involves triggering a child’s anxiety a little at a time, in a safe and controlled setting, until the anxiety subsides. Once a child has learned to tolerate the anxiety without avoiding it, the anxiety diminishes.
There’s a limit to what you can do with exposure therapy for kids with GAD, who are worried about so many things, notes Dr. Bubrick. “You can’t do exposures for everything all the time. So, we do a lot of cognitive work instead. We do a lot of challenging thinking, getting kids to recognize that irrational thinking and replacing it with more logical, rational versions of those thoughts. So, it’s really having the kids learn a different way to think.”
Teens, particularly those who have prior experience with CBT, may benefit from ACT, a form of mindfulness therapy closely related to CBT. With ACT, a teen would learn to acknowledge and accept the anxious thoughts they’re having and commit to moving forward despite them. ACT helps kids step back and observe their anxiety, Dr. Gerber adds. “Rather than trying to stop it, they’re, in a way, making friends with it, treating it like an uninvited guest who’s tolerable, if not exactly welcome.”
Mild to moderate GAD can often be treated in anywhere from 10 and 20 therapy sessions. Severe GAD is treated with combination psychotherapy and medication for anxiety disorders , usually an antidepressant called an SSRI.
“The medication might allow them to progress more quickly in the therapy because they can tolerate the intensity of the worry or the anxiety better,” Dr. Gerber adds.
What parents can do
While GAD tends to run in families, it’s important not to blame yourself for your child’s anxiety and instead focus on helping them work past their worries.
“A lot of times parents will feel like they did something wrong,” Dr. Gerber says. “In reality, many factors go into a kid developing GAD. I like to tell them ‘You’re not the problem, but you can be a big part of the solution.’”
That involves getting your child the treatment they need and working with your child’s therapist to learn how to best support your child outside of the clinician’s office. Step one is to avoid inadvertently reinforcing anxious behavior. Parents can unintentionally accommodate fears by providing reassurance or allowing kids to avoid things that trigger their anxiety.
“It’s quite natural for parents to want to provide reassurance or accommodate a child when they’re upset,” Dr. Gerber says. “But by doing that, you’re sending the message that there is something to be worried about.”
As an example, Dr. Gerber says she once had a patient who was scared to come downstairs for fear something bad would happen. His well-meaning parents “got a mini fridge and plugged it in next to his room so he only had to peek out and grab a juice box when he wanted something to drink,” she says. “But that’s not helpful in the long run.”
On the other hand, it can be equally harmful to ignore or dismiss anxious thoughts since, “the more you try to avoid or accommodate anxiety, the stronger it gets,” Dr. Gerber says.
One relatively new approach to helping kids with GAD or other kinds of anxiety involves a therapist working with parents alone — not directly with the children. It’s called Supportive Parenting for Anxious Child Emotions , or SPACE, and it teaches parents how to change their own behavior in order to help their child overcome anxiety.
If parents have anxiety themselves, it can also help for them to get support or treatment, she adds. In turn, they’ll be better equipped to help their child with it as well.
Was this article helpful?
Explore popular topics, subscribe to our newsletters.
" * " indicates required fields

Don’t Miss Out
Sign up for more articles and parenting tips direct to your inbox.
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Generalized Anxiety Disorder in Children and Adolescents
, MD, Sidney Kimmel Medical College of Thomas Jefferson University
Symptoms and Signs
Generalized anxiety disorder is a persistent state of heightened anxiety and apprehension characterized by excessive worrying, fear, and dread. Physical symptoms can include tremor, sweating, multiple somatic complaints, and exhaustion. Diagnosis is by clinical criteria. Treatment is often with relaxation therapy, sometimes combined with drug therapy.
(See also Overview of Anxiety Disorders in Children and Adolescents Overview of Anxiety Disorders in Children and Adolescents Anxiety disorders are characterized by fear, worry, or dread that greatly impairs the ability to function normally and that is disproportionate to the circumstances at hand. Anxiety may result... read more and Generalized Anxiety Disorder Generalized Anxiety Disorder Generalized anxiety disorder is characterized by excessive anxiety and worry about a number of activities or events that are present more days than not for ≥ 6 months. The cause is unknown,... read more in adults.)
Children with generalized anxiety disorder have multiple and diffuse worries, which are exacerbated by stress. These children often have difficulty paying attention and may be hyperactive and restless. They may sleep poorly, sweat excessively, feel exhausted, and complain of physical discomfort (eg, stomachache, muscle aches, headache).
During the COVID-19 pandemic, the abrupt and dramatic disruption in routines—such as school closure and isolation from extended family, peers, teachers, cultural and religious groups—increased anxiety in nearly all children. Living in constrained spaces with family members for weeks to months, parental job loss, and general uncertainty about the future increased stress as well ( 1 Symptoms and signs reference Generalized anxiety disorder is a persistent state of heightened anxiety and apprehension characterized by excessive worrying, fear, and dread. Physical symptoms can include tremor, sweating... read more ).
Symptoms and signs reference
1. Mental Health and Coping During the Coronavirus (COVID-19) Pandemic . Centers for Disease Control and Prevention. Accessed May 12, 2023.
Psychiatric assessment
Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) criteria
Generalized anxiety disorder is diagnosed in children and adolescents who have prominent and impairing anxiety symptoms that are not focused enough to meet criteria for a specific disorder such as social anxiety disorder Social Anxiety Disorder in Children and Adolescents Social anxiety disorder is a persistent fear of embarrassment, ridicule, or humiliation in social settings. Typically, affected children avoid situations that might provoke social scrutiny ... read more or panic disorder Panic Disorder in Children and Adolescents Panic disorder is characterized by recurrent, frequent (at least once/week) panic attacks. Panic attacks are discrete spells lasting about 20 minutes; during attacks, children experience somatic... read more . Generalized anxiety disorder is also an appropriate diagnosis for children who have a specific anxiety disorder, such as separation anxiety Separation Anxiety and Stranger Anxiety Separation anxiety is fussing and crying when a parent leaves the room. Some children scream and have tantrums, refuse to leave their parents' side, and/or have nighttime awakenings. Separation... read more , but also have other significant anxiety symptoms above and beyond those of the specific anxiety disorder.
Specific criteria include the presence of each of the following:
Excessive anxiety and worry that patients have difficulty controlling
Symptoms present on more days than not for ≥ 6 months
Symptoms cause significant distress or impair functioning socially or at school
In addition, the above criteria must be accompanied by ≥ 1 of the following:
Restlessness or a keyed-up or on-edge feeling
Being easily fatigued
Difficulty concentrating
Irritability
Muscle tension
Sleep disturbance
Occasionally, generalized anxiety disorder can be confused with attention-deficit/hyperactivity disorder (ADHD) Attention-Deficit/Hyperactivity Disorder (ADD, ADHD) Attention-deficit/hyperactivity disorder (ADHD) is a syndrome of inattention, hyperactivity, and impulsivity. The 3 types of ADHD are predominantly inattentive, predominantly hyperactive/impulsive... read more because generalized anxiety disorder can cause difficulty paying attention and can result in psychomotor agitation (ie, hyperactivity). However, in ADHD, children also have difficulty concentrating and feel restless when they are not anxious. Some children have both ADHD and an anxiety disorder.
Relaxation therapy
Sometimes anxiolytic medications, usually selective serotonin reuptake inhibitors (SSRIs)
Because the focus of symptoms is diffuse, generalized anxiety disorder is especially challenging to treat with behavioral therapy. Relaxation training is often more appropriate.
Children with generalized anxiety disorder have multiple and diffuse worries, rather than a single, specific one.
Diagnose generalized anxiety disorder when symptoms cause significant distress to the child or impair social or academic functioning socially and the child has ≥ 1 specific symptoms (eg, restlessness, a keyed-up or on-edge feeling).
Relaxation therapy may help; if children have severe anxiety or do not respond to psychotherapeutic interventions, consider anxiolytic medications (preferably SSRIs).

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada) — dedicated to using leading-edge science to save and improve lives around the world. Learn more about the MSD Manuals and our commitment to Global Medical Knowledge.
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Manual

- IN THIS TOPIC
- Second Opinion

Generalized Anxiety Disorder (GAD) in Children and Teens
What is generalized anxiety disorder in children and teens.
Generalized anxiety disorder (GAD) is a mental health problem. A child with GAD has a lot of worry and fear that seems to have no real cause. The worry may be more intense than the situation calls for. Children or teens with GAD often worry about many things, such as:
Future events
Past behaviors
Social acceptance
Family matters
Their personal abilities
School performance
All children and teens have some anxiety. It is a normal part of growing up. But sometimes worries and fears don’t go away. They may interfere with a child’s normal activities. In these cases, an anxiety disorder may be present.
What causes GAD in a child or teen?
Experts believe GAD is caused by both biological and environmental factors. A child may inherit a tendency to be anxious. An imbalance of 2 chemicals in the brain (norepinephrine and serotonin) most likely plays a part.
A child can also learn anxiety and fear from family members and others. For example, a child with a parent who is afraid of thunderstorms may learn to fear thunderstorms. A traumatic event may also cause GAD. This can include things such as the death of a parent, a divorce, or a serious family accident or illness.
Which children and teens are at risk for GAD?
Children who have parents with an anxiety disorder are more likely to have GAD. Children who seem more restrained as toddlers may be at more risk for GAD.
What are the symptoms of GAD in a child or teen?
Unlike adults with GAD, children and teens often don’t realize that their anxiety is more intense than the situation calls for. Children and teens with GAD often need a lot of reassurance from the adults in their life.
Symptoms may be a bit different for each child. But the most common symptoms of GAD are:
Many worries about things before they happen
Many worries about friends, school, or activities
Almost constant thoughts and fears about the child’s safety or the parents’ safety
Refusing to go to school
Frequent stomachaches, headaches, or other physical complaints
Muscle aches or tension
Sleep problems
Lots of worry about sleeping away from home
Clingy behavior with family members
Feeling as though there is a lump in the throat
Extreme tiredness (fatigue)
Lack of concentration
Being easily startled
Being grouchy
Inability to relax
The symptoms of GAD may seem like other health problems. Make sure your child sees his or her healthcare provider for a diagnosis.
How is GAD diagnosed in a child or teen?
Before a mental health referral is made, your child's healthcare provider will want to rule out any other health problems. Once this is done, a child psychiatrist or other mental health expert can diagnose GAD. He or she will do a mental health assessment of your child. It may include a complete emotional and social history, interviews with you and your child, and standardized testing.
How is GAD treated in a child or teen?
Children and teens with GAD can’t just pull themselves together and get better. They often need treatment. In many cases, treatment is key to recovery. Untreated, GAD can get worse or become a long-term problem. Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
Treatment for GAD may include:
Cognitive behavioral therapy. This helps a child learn how to better manage anxiety. The goal is also to help a child master the situations that may lead to the anxiety.
Medicines. Antidepressant or anti-anxiety medicine may help some children feel calmer.
Family therapy. Parents play a vital role in any treatment.
School input. A child’s school may also be included in care.
How can I help prevent GAD in my child or teen?
Experts don’t know how to prevent GAD in children. If you see signs of GAD in your child, you can help by getting an evaluation as soon as possible. Early treatment can ease symptoms and enhance your child’s normal development. It can also improve his or her quality of life.
How can I help my child or teen live with GAD?
As a parent, you play a key role in your child’s treatment. Here are things you can do to help:
Keep all appointments with your child’s healthcare provider.
Reassure your child. With GAD, your child may not realize his or her worry is more intense than the situation calls for. Your child will need more reassurance from you and other adults.
Talk with your child’s healthcare provider about other providers who will be included in your child’s care. Your child may get care from a team that may include counselors, therapists, social workers, psychologists, teachers, and psychiatrists. Your child’s care team will depend on his or her needs and how serious GAD is.
Tell others about your child’s GAD. Work with your child’s healthcare provider and school to create a treatment plan. Remind teachers that your child will need extra reassurance.
If GAD greatly interferes with your child’s ability to succeed in school, he or she may be eligible for specific protections and reasonable accommodations under the Americans with Disabilities Act (ADA) or Section 504 of the Civil Rights Act. Ask your school's principal or your child’s teacher for more information.
Reach out for support from local community services. Being in touch with other parents who have a child with GAD may be helpful.
When should I call my child’s healthcare provider?
Call the healthcare provider right away if your child:
Feels extreme depression, fear, anxiety, or anger toward him or herself or others
Feels out of control
Hears voices that others don’t hear
Sees things that others don’t see
Can’t sleep or eat for 3 days in a row
Shows behavior that concerns friends, family, or teachers, and others express concern about this behavior and ask you to get help
GAD may increase a child’s risk for suicide. Threats of suicide are a cry for help. Always take such statements, thoughts, behaviors, or plans very seriously. Any child who expresses thoughts of suicide should be evaluated right away.
Call 911 if your child has suicidal thoughts, a suicide plan, and the means to carry out the plan.
Key points about GAD in children and teens
Generalized anxiety disorder (GAD) is a mental health problem. A child with GAD has a lot of worry and fear that seems to have no real cause.
A child with GAD may worry about things such as future events, past behaviors, and family matters.
The child may not realize his or her worry is more intense than the situation calls for
GAD is caused by both biological and environmental factors.
A mental health evaluation is needed to diagnose GAD.
Treatment includes therapy and medicines.
Tips to help you get the most from a visit to your child’s healthcare provider:
Know the reason for the visit and what you want to happen.
Before your visit, write down questions you want answered.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
Ask if your child’s condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if your child does not take the medicine or have the test or procedure.
If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Related Links
- Brain and Behavior Center
- Child and Adolescent Mental Health
- Traumatic stress changes brains of boys, girls differently
- Pediatric Cardiology
- Our Services
- Chiari Malformation Center at Stanford Medicine Children's Health
Connect with us:
Download our App:
- Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.

Generalized Anxiety Disorder Case Study: James
A paper on case studies.

If you are seeking help in this area, please let one of our therapists know. Theravive has thousands of licensed counselors available to help you right away. The following article may have multiple collaborators and thus, parts of it may not represent the official positions of Theravive.
Generalized anxiety disorder, (GAD) is a traumatic illness, and is hard to understand unless you are experiencing it yourself. While specific anxiety disorders are complicated by panic attacks or other features of the disorder, GAD has no specific focus. (Durand, 2007 p.130). The person constantly worries about everyday life; not being able to figure out what to do with their worries. All the while making themselves and everyone around them miserable. (p.130). The worries seem to take over control of one's life, almost to the point of not being able to function at all.
It seems that GAD tends to run in families based on studies conducted, and seems to happen more to women than men. (Durand, 2007 p.132). And evidence shows that GAD may be proved to be just as heritable, the same as other anxiety disorders. (p.133). The textbook states that this disorder originated in 1980, however therapists were working with patients with anxiety way before the criteria was developed. (p.133). For many years, clinicians believed that people who were generally anxious just didn't seem to have anything specific to focus on, thus calling it the 'free floating' disorder. (p.133).
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) has specific criteria that characterized GAD. As stated in our textbook, the features are:
• Excessive anxiety and worry for 6 months or more about a number of events or activities. • Difficulty in controlling the worry. • At least three of these symptoms: (1) restlessness of feeling all keyed up; (2) becoming fatigues easily; (3) difficulty concentrating; (4) irritability; (5) muscle tension; (6) sleep disturbance. • Significant distress or impairment. • Anxiety is not limited to one specific issue. (Durand, 2007 p.131).
Generalized anxiety disorder has been studied using various criteria. The National Comorbidity Survey (NCS) focused on noninstitutionalized American civilians ages 15 to 54. The results were reported and found there was a clear predominance of women with GAD, with a 2:1 female/male ratio. It was lowest among the younger age group but increased with age. (NA, 1997). 'There was a significant regional difference in GAD as well, with a higher lifetime prevalence in the Northeast than in other parts of the country.' (1997). Studies have shown that many people could not really pinpoint a clear age of onset of GAD or an onset dating back to childhood. (Barlow, 1993 p.156). There have also been twin studies which conclude that GAD is somewhat greater for identical female twins than for non-identical twins, but only if one twin already had generalized anxiety disorder. (Durand, 2007 p.132). But later researched showed that what seemed to be inherited was the ability to become anxious rather than GAD itself. (p.132). It's amazing to know that people with GAD seem to show less responsiveness on most physiological measures, such as heart rate, blood pressure, skin conductance and respiration rate than do people with other anxiety disorders. (p.133).
Although it seems to prove that GAD is quite common, I am amazed that more people don't have this disorder. I think that many people have general anxieties on a daily basis, but most people are able to handle them successfully. I did not realize that most people with GAD have usually had symptoms of anxiety or feelings of being worried throughout life, but just didn't know when it all started. The criterion has changed over the years as well as doctors have become more knowledgeable about this disorder. I first had knowledge of this disease in 1997 when I noticed strange things happening.
He was not really watching as he stared directly at the television set. I would notice that he had no expressions at all; nothing during the humorous scenes, or the dramatic ones. He once told me that it was as if he was someone else, watching himself try to crawl out of his own skin. That was 10 years ago when I was married to this man who was suffering from generalized anxiety disorder. I didn't understand and I really didn't want to. I thought he was just being lazy and unmotivated. Although this disorder seems to be simple to others, it is quite alarming to the person who is suffering from it, and the onset is rather quick, whereas, treatments are difficult. Everyone experiences anxiety, but in most people, it does not last for months at a time.
The case study I am choosing is about James who is a doctor suffering from generalized anxiety disorder. At 31 years of age and living in New York, he is unemployed because of his constant anxiety, even at the thought of working. He now lives with his parents off a small trust fund set up for him by an uncle. Although he was an overachiever throughout his academic career, James is having a hard time keeping it together, while his parents are somewhat supportive but disappointed with his medical career. Let's see what we can learn about this horrible and crippling disorder. 'Generalized anxiety disorder is associated with irregular neurotransmitters in the brain. Neurotransmitters are chemicals that carry signals across nerve endings. Neurotransmitters that seem to involve anxiety include norepinephrine, GABA (gamma-aminobutyric acid), and serotonin.' (na, 2001). So it was thought that reduced levels of GABA initiated excessive anxiety, although neurotransmitters are much to complex to be interpreted that simply. (Durand, 2007 p.45).
The brain is a very fascinating and intricate part of who we are and if the brain is not functioning properly, then our reactions to certain situations are not in balance. This is why some people still believe that undeniable psychological disorders are said to be caused by biochemical imbalances. (Durand, 2007 p.50). So in James' case, his brain was not functioning right and he was experiencing an unnatural balance of change within his various neurotransmitters, causing him to become anxious, easily irritated, distracted and quite tense. He also complained of headaches, body aches and pains and always feeling tired.
Genetics does play a major role is determining whether a person will or will not have a psychological disorder. The textbook states that the research is beginning to acknowledge genes that relate to some psychological disorders. (Durand, 2007 p.70). I feel that genetics does contribute to some disorders, but I also think that the environment and society can cause debilitating stress to induce certain disorders, such as anxiety. If the gene linked to the disorder is dormant, a stress related incident can bring it to the surface, thus bringing on the disorder. My research has shown that there are brain abnormalities indicated with generalized anxiety disorder. A study of 30 patients displayed that compared to 20 healthy volunteers, 11 patients had significant brain abnormalities mainly in the right temporal lobe. (Nutt, 2003 p.209). The temporal lobe controls the processes of recognizing various sights and sounds and long term memory storage. (Durand, 2007 p.48). However there are two temporal lobes on each side of the brain, located at the level of the ears. The lobes help a person distinguish one sound from another as well as one smell from the other. The right lobe controls visual memory while the left lobe controls verbal memory. (Johnson, 2006) So this would explain why James kept making mistakes because he was probably having a hard time remembering simple procedures.
The first thing James would need to do would be to seek professional help and see if he has this disorder, although being a medical doctor, he may have self diagnosed himself, however he should see a psychiatrist. There are no laboratory tests that can determine if a person has anxiety or a mental illness, but a doctor will perform a battery of tests to weed out other illnesses, such as an overactive thyroid gland, which can produce anxiety and its symptoms. (NA, 2007 WebMD). James' next plan of attack would be to discuss the different types of medications that are available for providing relief from this disorder. Since James has generalized anxiety disorder, which has been called a 'free-floating' disorder because of his constant worrying and nervousness, as stated earlier, he would need a medication that treats low levels of GABA. (Roberts, ch.17 p.6). The textbook states that the drub benzodiazepine (minor tranquilizers) is the most frequently prescribed. (Durnad, 2007 p.134). The drug is used for short-term relief and can be hard to stop taking because of dependence issues. One such drug in particular is called Xanax, which is shown to enhance the function of GABA in the brain. It also slows down the central nervous system. This drug is extremely addicting; it's the drug my ex-husband did not want to give up, so we got a divorce.
There is also evidence that antidepressants can be used for GAD and may be a better choice. (p.134) The most common antidepressants are prozac and zoloft. 'These drugs are shown to affect the concentration and activity of the neurotransmitter serotonin, a chemical in the brain thought to be linked to anxiety disorders.' (na, 2004). Some of these drugs that I have researched for GAD, are also used for treating migraines, because I was prescribed some for headaches. No wonder I was always in a good mood, even though it felt like my head was about to explode.
Because the drugs prescribed for this disorder are recommended to be taken for short periods of time, therapy should be initialized as well. The side effects of these drugs are: Xanax (benzodiazepines): drowsiness, fatigue, decreased concentration, confusion, blurred vision, pounding or irregular heartbeat, impaired coordination, short term memory problems, dizziness. (Smith et al, 2006).
Prozac (Selective Serotonin reuptake inhibitors): nausea, insomnia, headaches, decreased sex drive, dizziness, weight gain or loss, nervousness, sweating, drowsiness/fatigue, dry mouth, diarrhea or constipation, skin rashes. (Smith et al, 2006) These medications offer so many side effects, it's a wonder anyone wants to take them at all. But I guess for the person who is suffering from anxiety attacks or generalized anxiety disorder, the side effects may be a welcomed relief There are also natural remedies to help with GAD such as valerian root and kava kava, which has been treating anxiety for years, but the results are not well documented. (Smith et al, 2006) Some natural remedies can actually make anxiety worse and taking supplements may interact with the prescription anxiety medications, so it's a good idea to discuss this with a doctor.
Another approach to treatment is to help James with therapy sessions to try to figure out why he is experiencing all this anxiety and worry. One session may include showing James pictures of things that may make him anxious and then teaching him how to relax deeply to fight his tension. It's called cognitive behavioral treatment, developed in the early 1990s, and is quite successful; however we need both medications and therapy to treat GAD. (Durand, 2007 p.134).
Acupuncture, which is one medical treatment that does no harm to the body, only releases energy and gets it moving in the system; (NA, 2007) biofeedback, which is the ability to allow the patient hear or see feedback of their body's physiological state while relaxing;(Grohol, 2004) and hypnotherapy shown as an appropriate treatment modality for those individuals who are highly suggestible, have also been used to treat anxiety. (Grohol, 2004).
So which treatments work the best? That is hard to say because everyone is different and will react differently to each treatment. As stated in the textbook, a combined treatment of therapy and medications suggested there were no advantages for both, and that people did better in the long run when having psychological treatments only. (Durand, 2007 p.144). So it's suggested to start with psychological treatment first and then followed by drug treatments for the patients who are not responding to therapy. (p.144).
How does environment influence our behavior? Do we imitate what we see around us? Are we simply looking for acceptance, thereby, acting or saying what we think society expects? Who decides what acceptable behavior is? Although the environment may affect a person's behavior, there are many other elements to explore that influence the way we are.
James is coping with generalized anxiety disorder, as was stated earlier. At 31, he is allowing this disorder to control his life which is leading to being emotionally and physically drained. Although he realizes that he is an intelligent and capable person, he knows to avoid any situation that may exacerbate the anxieties that he is experiencing. With minimal support from his family and friends, James feels that he is dealing with this all alone and just wants to lead a normal life. Perhaps the stress and strain of becoming a doctor led to James' anxiety disorder as it may have been dormant within his genetic makeup, and is now just surfacing.
Many people develop generalized anxiety disorder (GAD) during adolescence, but do not seek professional help until they are adults. (NA, 2001). When they do finally get help, they claim they have been anxious and nervous all their lives. (2001). These people cannot just 'get over it' but society seems to not grasp that concept. Some of the environmental influences that could lead to general anxiety are: • Work. This would affect James immensely because his whole life has been based around his becoming a doctor. Even his father wanted him to follow in his footsteps and have a prestigious career. • School. Although James did not experience anxieties until after he graduated from medical school, I'm sure he still felt anxious with tests and schoolwork. • Relationships. This would be dealing with James' parents as they are somewhat supportive but disappointed that his career has not been progressing. He also lost his relationship with his girlfriend of three years because of the stress. • Health. Because James is dealing with this disorder, his health is rapidly declining. He is having headaches, body aches and pains and is always tired. His emotional health is affected as well with feelings of laziness and worthlessness. • Financial. James is realizing that if he cannot work, he cannot earn a paycheck. He is living off a small trust fund set up for him by his great uncle, but that won't last forever. All of these things are considered threats and can cause James to worry excessively which is interfering with his life.
Is the environment to blame for James' anxiety or is it more biological? I think that genetics and the environment work together to produce this disorder. I feel that if a person is genetically prone to have anxiety and fear; if the person never leaves the house, then what does he/she have to worry about? The environment has to play a role in the mobility of this disorder. If James were to isolate himself from the world, he would still have anxiety; however he would not be able to face his fears, thus restricting his life. His thought process would be 'what if this happened, or what if that happened?' He would always be having threatening thoughts and images playing over and over in his mind. (Alloy, 2006 p.189).
Our textbook states that GAD generally runs in families, which I mentioned earlier. (Durand, 2007 p.132). With all the research and studies that are performed, it will show that generalized anxiety disorder is inherited. So genetics and biology has to be the most important because people who aren't suffering from anxiety will react more favorable to a stressful situation, than someone who is suffering from GAD. It seems that we all have to face the same environmental influences, but the threat of each situation interacts with the biological aspect of a person, thus bringing on the symptoms of the disorder. (p.133).
James needs to be treated by a psychiatrist, not a family physician. He needs to be seen by someone who deals with psychological disorders daily and is educated with the treatments available. Psychological treatments work better in the long run and work just as well as prescription medication. Our textbook states that, 'as we learn more about generalized anxiety, we may find that helping people with this disorder to focus on what is actually threatening is useful.' (Durand, 2007 p.134).
Research has indicated that psychological treatments work very well for children who suffer from GAD. (Durand, 2007 p.135). But I feel that unless a child is diagnosed early in life, the treatments won't be as effective. I'm sure that James was experiencing some form of anxiety as a child, but children are difficult to diagnose, and if the parents don't know what to look for, they won't know the child needs help. But children respond to cognitive-behavioral treatments along with family therapy. (p.135).
I feel that psychosocial treatments would be the best way to start with a patient. In James' case, I think he should start with therapy for at least three months. He needs to confront the fear, phobias and anxieties head on to figure out what's making him feel emotionally and physically drained. I would also suggest to James that he should educate and read everything he can on this disorder. Having this knowledge will benefit him so he may get the most out of his treatments. If I had a disorder, I would want to know everything about it. And I would be asking a million questions. Sometimes I feel that everyone in society could use some form of therapy to deal with the stressors of life.
Next, I would try medications in addition to therapy to help James with possible other symptoms of GAD, such as depression. (Smith et al, 2006). The medication, however, would only be used on a temporary basis, as addiction can occur. My ex-husband was on medication for his GAD, but he was not seeing anyone for therapy. I think that was the biggest problem. He was increasing his dosage without telling his doctor, thus becoming extremely dependent on the drugs. As a doctor, James should know that some of the medications used for GAD are very addictive and hopefully would only be used as directed.
There are certain beliefs about thoughts and thought processes that are included in cognitive forms. (Papageorgiou, 2004 p.228). 'There are two types of worries; Type 1 and Type 2. Type 1 worries deal with external daily events such as the welfare of a partner, and non-cognitive internal events such as concerns about bodily sensations. Type 2 worries are focused on the nature and occurrence of thoughts themselves such as worrying that worry will lead to insanity. It's basically worry about worry.' (Wells, 1997 p.202). The cognitive model claims that the varieties of worry are typically type 2 worries in which the patients negatively appraise the activity of worrying. (p 202). I feel that the cognitive psychological model best applies to understanding and treating this disorder. I believe that by using cognitive therapies and similar research studies, we can begin to know what it takes to treat the people who are suffering with better results now and in the future. There are new medications that can help people with GAD, but there are side effects that may be too harsh or severe. I believe that more psychosocial therapies may need to be developed in order to help these people, so they can live a normal life without medications, because of the problems they present to the body.
I believe that James could once again become a successful doctor if and when he gets his generalized anxiety disorder under control. The treatments are available; all he has to do is seek them out. I feel that with therapy coupled with medications would benefit James tremendously. Eventually he will be able to stop taking the medications and perhaps enjoy a fairly normal life. The good news is that only 4% of the population meets the criteria for GAD during a given one-year period. However it is still one of the most common anxiety disorders. (Durand, 2007 p.132). . My research for this paper has helped me so far in understanding what a person is going through with crippling anxiety. It's not something that a person can just 'get over' and I know I wanted to tell my ex-husband that many, many times. However, he became addicted to the prescriptions drugs, and became a drug addict in about two weeks. Because of my first hand experience with this disorder, I chose to do my projects on it.
References N.A. (1997) Retrieved Oct. 20, 2007 from The Natural History of Generalized Anxiety Disorder website: www.medscape.com N.A. (2001). Retrieved Sept. 16, 2007 from General Anxiety Disorder website: http://www.mentalhealthchannel.net N.A. (2004). Retrieved Sept. 13, 2007 from Anxiety Disorders Association of America website: http://www.adaa.org N.A. (2007) Retrieved Sept. 17, 2007 from Anxiety Panic Guide website: http://www.webmd.com N.A. (2007). Retrieved Oct. 21, 2007 from Acupuncture for Generalized Anxiety Disorder website: www.revelutionhealth.com Barlow, D. (1993) Clinical Handbook of Psychological Disorders: A step-by-step treatment Manual 3rd ed. Guilford Press Retrieved Oct. 20, 2007 from libsys.uah.edu. Durand, V. & Barlow, D. (2007) Essentials of Abnormal Psychology: Mason, OH. Thomson/Wadsworth Publishing. Grohol, J. (2004) Retrieved Oct. 20, 2007 from generalized anxiety disorder treatment website: www.psychentral.com/disorders Johnson, G. (2006) Retrieved Sept. 15, 2007 from A Guide to Brain Anatomy website: http://www.waiting.com/brainanatomy Nutt, D. & Ballenger, J. (2003). Anxiety Disorders. Malden, Ma: Blackwell Publishers Retrieved Sept. 18, 2007 from Net library search: libsys.uah.edu Papageorgiou, C. & Wells, A. (2004). Depressive Rumination Nature, Theory and Treatment. Hoboken, NJ: John Wiley & Sons, LTD. Roberts, M. (nd). Introductory Guide to Psychology Kaplan University Class SS-124 Alloy, L. & Riskind, J. (2006). Cognitive Vulnerability to Emotional Disorders. Mahwah, NJ: Lawrence Erlbaum Associates Inc. Smith, M., Kemp, G., Larson, H., Jaffe, J., Segal, J. (2006). Retrieved Oct.8, 2007 from Anxiety Attacks and Disorders website: http://www.helpguide.org Wells, A. (1997). Cognitive therapy of Anxiety Disorders: A practice manual and conceptual guide. Chichester, NY: John Wiley & Sons, LTD.

Our purpose is to help people everywhere find great counselors and psychologists. Everyone can have a new start in life.
Theravive does not provide medical advice, diagnosis, or treatment.
Read here for more info.
- Open access
- Published: 02 April 2024
Psychometric properties of the GAD-7 (General Anxiety Disorder-7): a cross-sectional study of the Peruvian general population
- David Villarreal-Zegarra ORCID: orcid.org/0000-0002-2222-4764 1 , 4 ,
- Rubi Paredes-Angeles ORCID: orcid.org/0000-0003-3669-4932 4 ,
- Nikol Mayo-Puchoc ORCID: orcid.org/0000-0002-6182-7605 4 ,
- Enoc Arenas-Minaya ORCID: orcid.org/0000-0001-9577-6212 5 ,
- Jeff Huarcaya-Victoria ORCID: orcid.org/0000-0003-4525-9545 2 &
- Anthony Copez-Lonzoy ORCID: orcid.org/0000-0003-4761-4272 3 , 4
BMC Psychology volume 12 , Article number: 183 ( 2024 ) Cite this article
165 Accesses
Metrics details
Anxiety disorders are among the main mental health problems worldwide and are considered one of the most disabling conditions. Therefore, it is essential to have measurement tools that can be used to screen for anxiety symptoms in the general population and thus identify potential cases of people with anxiety symptoms and provide them with timely care. Our aim was to evaluate the psychometric properties of the General Anxiety Disorder-7 scale (GAD-7) in the Peruvian population.
Our study was a cross-sectional study. The sample included people aged 12 to 65 years in Peru. Confirmatory factor analysis, analysis of measurement invariance, convergent validity with the Patient Health Questionnaire-9 (PHQ-9) and internal consistency analysis were performed.
In total, 4431 participants were included. The one-factor model showed the best fit (CFI = 0.994; TLI = 0.991; RMSEA = 0.068; WRMR = 1.567). The GAD-7 score showed measurement invariance between men and women and between age groups (adults vs. adolescents) (ΔCFI < 0.01). The internal consistency of the one-factor model was satisfactory (ω = 0.90, α = 0.93). The relationship between depressive symptoms (PHQ-9) and anxiety symptoms (GAD-7) presented a moderate correlation ( r = 0.77).
Conclusions
Our study concluded that the GAD-7 score shows evidence of validity and reliability for the one-factor model. Furthermore, because the GAD-7 score is invariant, comparisons can be made between groups (i.e., by sex and age group). Finally, we recommend the use of the GAD-7 for the general population in the Peruvian context.
Peer Review reports
Introduction
Anxiety disorders (ADs) are among the main mental health problems worldwide and are considered among the most disabling mental health problems; they were among the 25 leading causes of mental health burden worldwide in 2019 [ 1 ]. The number of ADs has been increasing; in 2015, the estimated incidence of anxiety disorders worldwide was 3.6% (264 million), with a greater proportion of women [ 2 ]. The region of the Americas represented 21% (57.22 million) of all cases, and in Peru, 5.7% of people had AD [ 2 ]. In 2020, before COVID-19, the estimated global incidence of AD reached 298 million, and after the pandemic, the incidence increased by 25.6%, reaching an estimated global prevalence of 374 million. This increase was also greater for women (27.9%; 51.8 million) than for men (21.7%; 24.4 million). In addition, these percentages vary according to country, with an increase greater than 36.4% in AD occurring in Peru [ 3 ].
In this sense, it is necessary to have instruments with good psychometric properties that are brief and screening for easy, fast, and timely risk assessment of this disorder in the population. The most common instruments for measuring anxious symptoms include the Generalized Anxiety Disorders-7 (GAD-7); Beck Anxiety Inventory (21 items) [ 4 ]; the Hospital Anxiety and Depression Scale-Anxiety Subscale (7 items) [ 5 ]; the Depression, Anxiety and Stress Scale-Anxiety Subscale (7 items) [ 6 ]; State-Trait Anxiety Inventory (20 items) [ 7 ]; and the Zung Self-rating Anxiety Scale (20 items) [ 8 ]. These instruments are most commonly used with adults and adolescents, as older adults have different criteria for anxiety [ 9 ].
The GAD-7 is one of the instruments with the fewest number of items and was created according to diagnostic criteria from the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV), to detect generalized anxiety disorders [ 10 ]. Additionally, it is widely used in the clinical field [ 11 , 12 ], demonstrating good performance and adequate diagnostic accuracy [ 11 ]. Similarly, this instrument has shown good results in different populations and situations, such as in university students [ 13 , 14 ], adolescents [ 15 ], older adults [ 16 ], and health workers [ 17 ]; in virtual evaluations [ 18 ]; and because it is used for screening, it is also useful for obtaining prevalence estimates in the general population [ 19 , 20 ].
Despite being widely used, the GAD-7 has some heterogeneity in terms of its dimensionality. Most studies agree that the original one-factor model works well [ 16 , 21 , 22 , 23 ]; however, some studies report some modifications to this factorial structure, considering errors correlated between somatic items [ 24 , 25 ]. Other studies have considered a two-factor model, distinguishing cognitive-emotional aspects from somatic ones [ 26 , 27 ], and another study has suggested using a second-order model, taking cognitive-emotional and somatic elements as first-order factors [ 28 ]. However, to date, there is no consensus on the most appropriate factor structure for the GAD-7, but the one-factor model is the most widely used [ 35 , 36 ].
Another important property is measurement invariance, understood as the equivalence (in psychometric terms) of a construct across groups, which has the same meaning as those groups and is a prerequisite for comparing group means [ 29 ]. This property is not always reported, and the results of measurement invariance studies of GAD-7 scores according to age and sex have some discrepancies. Some studies have shown that invariance is achieved by sex and age [ 26 ], while in other studies, invariance is violated [ 30 ]; therefore, if this property is not verified in a population, comparisons between sex or age groups can lead to biased results and interpretations. Despite the available evidence, there are gaps in the knowledge of which variables GAD-7 is invariant and which are not. Therefore, this is still an open area of research.
Additional evidence of validity reported for the GAD-7 is its relationship with other variables, which are strongly related to depressive symptoms and are generally measured by the PHQ-9 [ 24 , 28 , 31 ]. This relationship is consistent with what is expected between depressive and anxiety disorders, both of which are considered common mental disorders due to their high prevalence and comorbidity [ 2 ].
The GAD-7 is a widely researched and useful tool for detecting potential cases of anxiety symptoms. Despite its usefulness, evidence regarding its factor structure and its invariance between groups is mixed. This highlights the need for further research to clarify these aspects. Given the importance of confirming adequate psychometric properties before using an instrument in a specific population, our study aims to: (1) Analyze the factorial structure of the original GAD-7 in the Peruvian population; (2) Evaluate GAD-7 measurement invariance based on sex and age; (3) Report the relationship with other variables (depressive symptoms); and (4) Estimate the reliability of the GAD-7. Our central hypotheses are that the GAD-7 has a strong factor structure, is invariant across gender and age groups, has a strong relationship with depressive symptoms, and has optimal levels of reliability.
Study design
Secondary data from six studies were obtained before and during the COVID-19 pandemic, and a cross-sectional design was used to evaluate the psychometric properties and validity of the GAD-7 in teenagers and adults in Lima, Peru.
Peru is a middle-income Latin American country that has had several problems in its health system since before the outbreak of COVID-19. The Peruvian government decreed of a state of sanitary emergency (March 16, 2020) to mitigate the spread of the infection, and a suppressive strategy was adopted (social isolation or quarantine). Moreover, the suspension of activities such as economic, academic, transport, and recreational activities was stipulated, and only essential activities related to the supply of products and services for public health were maintained [ 32 , 33 ].
Evidence indicates that the mental health impacts (e.g., anxiety, depression, posttraumatic stress) caused by strict health measures in low-income and middle-income countries have a significant mental impact, which contributes to a slow recovery toward normality [ 34 ].
Participants
The following six datasets were used to analyze the data of patients who met the inclusion criteria: (1) aged 12 years to 65 years. (2) Patients had complete data on the GAD-7 score, sex, and age. (3) Participants must have agreed to participate in the study first after providing informed consent. For those under 18 years of age, only those participants whose parents provided consent for their children to participate were considered (informed consent). We excluded participants with implausible data (i.e., age > 99 years). Nonprobabilistic sampling was performed for all the datasets.
Measurement
Anxiety symptoms.
The General Anxiety Disorder-7 scale (GAD-7) is a 7-item self-report Likert scale that was developed to assess the severity of anxiety disorders based on the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). This self-report measures the indicators of anxiety symptomatology in the last 2 weeks. Each item is rated on a 4-point Likert-type scale (0 = not at all; 1 = several days; 2 = more than half the day; 3 = nearly every day) [ 10 ]. To identify possible cases of general anxiety disorder (GAD), some studies considered using a cutoff range of 10 points because this cutoff provides a high balance between sensitivity and specificity [ 35 , 36 ]. We use the Spanish version of GAD-7 by Soto-Balbuena and collaborators [ 22 ].
Depressive symptoms
The Patient Health Questionnaire-9 (PHQ-9) is a 9-item Likert scale developed to measure the severity of depressive symptoms; this scale was designed from the nine diagnostic criteria from the DSM-IV. The instrument reports the indicators of depressive symptomatology over the past 2 weeks. Its response options were 4-point Likert-type scales (0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day) [ 37 ]. According to other studies, a standard cutoff score of 10 or above can be used for screening to detect moderate depressive symptoms [ 37 , 38 ]. The PHQ-9 has been validated in a Peruvian population sample, where it presented optimal validity and reliability values [ 39 ].
Participants were recruited through an online Google Forms form, which was distributed to potential participants through networking via instant messaging applications such as WhatsApp and Telegram, as well as social media platforms such as Facebook and Instagram. Participants received no economic incentives or rewards. Participation was voluntary, and they accepted informed consent before the evaluation process began.
Statistical methods
All the analyses were performed in RStudio [ 40 ] using the packages lavaan [ 41 ], semTool [ 42 ] and semPlot [ 43 ].
Descriptive analysis
A descriptive analysis of participant characteristics was also conducted (mean, standard deviation, percentage, and frequency). The prevalence of anxious and depressive symptoms was based on the cut-off of 10 points or more for the GAD-7 and PHQ-9, respectively. In addition, we performed a descriptive analysis of the items using mean, standard deviation, skewness, and kurtosis.
Confirming factor analysis
We used one-factor, two-factor, and second-order factor models to assess the factorial structure of GAD-7 scores. All the models use the weighted least squares means and variance adjusted (WLSMV) estimator because of its ability to provide a good option for modeling categorical or ordered data [ 44 , 45 ]. Additionally, a polychoric correlation matrix was calculated. Therefore, to evaluate the model fit, the weighted root mean square residual (WRMR), the comparative fit index (CFI), and the root mean square error of approximation (RMSEA) along with 90% confidence intervals (90% CIs) were used. A reasonably good fit is recommended following the following criteria: (a) WRMR < 1 or below; (b) RMSEA < 0.08 or below; and (c) CFI and TLI > 0.95 or above [ 46 , 47 ]. This analysis was performed to determine the best factor structure of the GAD-7.
Invariance between groups
Testing for measurement invariance involves testing a series of hierarchically nested models to assess whether the instrument is stable between two or more groups; thus, comparisons can be made between them [ 48 ]. Comparisons were made between sex groups (male and female) and ages (adolescents and adults). To compare models with more restrictions against models with fewer restrictions, we used ΔCFI and ΔRMSEA as variants of the comparative fit index and the root means the square error of approximation, respectively. Thus, ΔCFI values < 0.01 and ΔRMSEA values < 0.015 provide evidence for measurement invariance [ 29 , 49 ]. In addition, we assessed other fit indices, such as the CFI and RMSEA, along with 90% confidence intervals. This analysis was performed to determine whether the GAD-7 showed measurement invariance between groups, allowing comparisons to be made between these groups.
Convergent validity
To examine convergent validity, the GAD-7 and the PHQ-9 total scores were correlated. Due to its concordance with other samples, the GAD-7 score was hypothesized to be strongly correlated with depression indicators (PHQ-9) [ 24 , 28 , 31 ]. This correlation was determined by Pearson’s r (r). A large ( r > 0.70), moderate ( r > 0.50) or small ( r > 0.30) ratio was determined based on the size of the correlation coefficient [ 50 ].
Reliability
Internal consistency analyses were performed using two coefficients: the ordinal alpha (α) and categorical omega (ω) coefficients. Both are acceptably reliable when the coefficient values are greater than 0.80 [ 50 ]. In addition, we performed a test item correlation analysis.
Ethics aspects
The institutional research ethics committee of the Instituto Peruano de Orientación Psicológica approved the study protocol.
Characteristics of the participants
Initially, we found 5048 records in the different datasets, and we eliminated 617 records after applying the inclusion criteria (12.2%). Therefore, the study included a total sample of 4431 participants. The sample consisted of 1929 men (43.5%) and 2502 women (56.5%), and the ages ranged from 11 to 65 years (M = 28.9 years; SD = 12.8). Furthermore, 3581 were adults (80.8%), and 850 were adolescents (19.2%). Additionally, 3653 patients were evaluated during the COVID-19 pandemic (82.4%), and 778 were evaluated before the pandemic (17.6%). In terms of prevalence, we found that 20.8% of participants presented anxious symptoms ( n = 922) and that 29.5% had depressive symptoms ( n = 1307). In addition, the raw scores of the GAD-7 and their measures of skewness and kurtosis are presented (see Table 1 ).
Confirmatory factor analysis
Our study evaluated different factor models based on previous studies. Based on this, we determined that all the models evaluated achieved optimal goodness-of-fit indices (see Table 2 ). The model with two correlated factors exhibited a very high correlation (Φ > 0.90). Therefore, we believe that both factors overlap, which means that it is not considered a parsimonious model and should be discarded. According to the second-order models, the two specified factors had loads very close to one concerning their general factor. This is why it is not considered a stable model, since both specific dimensions can actually be part of a one factor model.
Our study considers the one-factor model more appropriate because it is more parsimonious and requires fewer assumptions. In addition, all factor loadings were greater than 0.71 (see Fig. 1 ). This decision was made because the other two models present overlap and the one-factor model is the most used and stable model found in other studies.
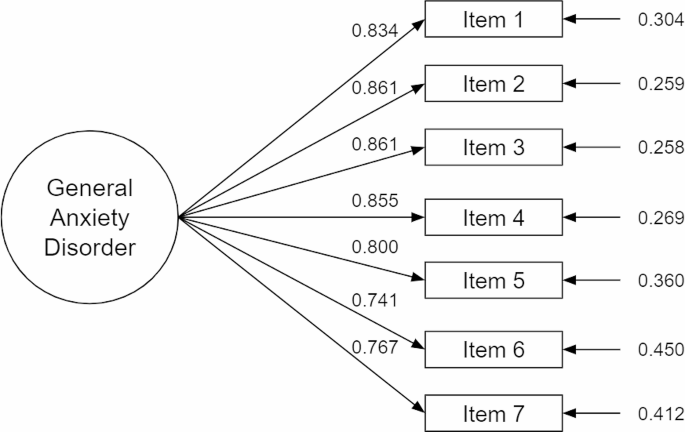
One-factor model of the GAD-7 score
Measurement invariance analysis between sex and age revealed that both groups were invariant, so comparisons could be made between each of these groups. Total scores can be compared between males and females or between age groups (adults vs. adolescents) as the ΔCFI and ΔRMSEA values remain at appropriate levels (see Table 3 ). In addition, the CFI and RMSEA values remained adequate for the configural, metric, and strong models. The configural level suggested that the different groups (men vs. women, and adults vs. adolescents) presented an equivalent factor structure, i.e., a seven-item, one-dimensional model. The metric level indicated that the different groups had equivalent factor loadings, and the strong level suggested that there were equivalent thresholds between the groups.
The internal consistency of the one-factor model was satisfactory (ω = 0.90; α = 0.93). The item-test correlation analysis indicated that, even if one item within the GAD-7 were eliminated, the internal consistency coefficient alpha would remain adequate in all cases (see Table 1 ). Therefore, eliminating one item would not affect the reliability of the scale.
A moderate correlation was shown between depressive symptoms and anxiety symptoms ( r = 0.77), as other studies have shown. Therefore, it can be inferred that the instrument has convergent validity.
Main findings and interpretation
Our study validates a brief tool for measuring anxious symptoms, which represents a valuable resource for the development of mental health research and a potential screening tool in the primary care setting in Peru. Our study concluded that the GAD-7 score is valid and reliable according to the one-factor model. Internal structure validity evidence for the GAD-7 suggests that its seven items can be summed to obtain a total score. In addition, our study revealed that comparisons can be made between groups according to factors such as sex and age. For example, a comparison of GAD-7 scores can be made between men and women. Similarly, evidence of convergent validity indicates that the GAD-7 score in the Peruvian context is strongly related to depressive symptoms, which has been found in different studies, suggesting that the instrument behaves consistently with other studies. Finally, the GAD-7 score for the one-factor model presented optimal reliability values.
Our study revealed that the GAD-7 score has one factor. This finding is consistent with results reported in previous studies [ 21 , 23 , 51 ]. Other studies have suggested two-factor or higher-order models, but these results are not necessarily contradictory because these highly related dimensions are part of the same overall construct, anxiety symptoms [ 27 ]. Therefore, although somatic and cognitive-emotional factors are theoretically valid, they do not seem to be distinguishable at the empirical level in the general population [ 27 ].
A one-factor model indicates that the GAD-7 can use a total score and establish cutoff points with sensitivity and specificity values [ 36 ]. In addition, a Peruvian study also found adequate levels of sensitivity and specificity for GAD-7 with a cut-off of 10 points or more [ 52 ]. However, for models with two or more factors, sensitivity and specificity analyses must be performed for each factor. We did not find any sensitivity or specificity studies for the two-factor models of the GAD-7 score. Therefore, the one-factor model is more commonly used and studied.
Our results showed invariance of the GAD-7 score across sex and age. Although few studies have explored the invariance of the GAD-7 score, similar findings were obtained by [ 26 ], who found invariance across sex, age and marital status, level of education, and employment situation in Spanish primary care patients. Likewise, another study reported invariance regarding sex, strata, and linguistic background in a sample of patients after traumatic brain injury [ 23 ]. A study that included a Peruvian sample also reported invariance of the GAD-7 score and other short versions across sexes; however, only university students were considered [ 51 ]. The interpretation of our results suggests that, for the different groups, participants perceive the existence of a single factor consisting of seven items (configural invariance), indicating that the items have equivalent factor loadings, and therefore the items contribute equally to the construct (metric invariance). In addition, the thresholds of these items show equivalent values across groups, allowing for comparisons between groups (strong invariance) [ 29 ].
At the level of convergent validity, the GAD-7 score showed a moderate correlation with the PHQ-9 score, which measures depressive symptoms. These findings are consistent with the results of several studies that have shown a direct relationship between moderate and strong strength [ 23 , 24 , 27 , 31 ]. At the level of reliability, other studies have also shown that the GAD-7 has adequate internal consistency values for one-factor models [ 24 , 31 , 53 ].
Public health implications
In Peru, there are no clinical practice guidelines for the assessment, diagnosis or treatment of anxiety disorders. Our study allows the GAD-7 to be used as a scale to detect depressive symptoms in the general population. Because of its brevity, we recommended their use in future Peruvian clinical practice guidelines on anxiety from the Ministry of Health or Social Health Insurance (EsSalud). Considering that there are currently a study evaluating the sensitivity and specificity of different cut-offs for GAD-7 in the Peruvian population [ 52 ].
Strengths and limitations
The main strength of our study is the large sample size. Our study has several limitations. First, our study was not probability-based, so it cannot be generalized to other populations. Second, our study does not propose a cutoff point for determining whether participants have anxiety symptoms. Third, it was not possible to assess invariance with other groups of interest, such as marital status, chronic illness or economic status.
Conclusions and recommendations
Data availability.
Access to data will only be by convincing request.To review the manuscript we have enabled a link to our dataset https://zenodo.org/records/10600793 .
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Article Google Scholar
World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. 2017.
Santomauro DF, Herrera AMM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–12.
Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–7.
Article PubMed Google Scholar
Zigmond AS, Snaith RP. The Hospital anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70.
Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression anxiety stress scales (DASS) with the Beck Depression and anxiety inventories. Behav Res Ther. 1995;33:335–43.
Spielberger C, Gorsuch R, Lushene R, Vagg P, Jacobs G. Manual for the State-Trait Anxiety Inventory (Form Y1– Y2). 1983.
Zung WWK. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–9.
Balsamo M, Cataldi F, Carlucci L, Fairfield B. Assessment of anxiety in older adults: a review of self-report measures. Clin Interv Aging. 2018;13:573–93.
Article PubMed PubMed Central Google Scholar
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092.
Clover K, Lambert SD, Oldmeadow C, Britton B, King MT, Mitchell AJ, et al. Apples to apples? Comparison of the measurement properties of hospital anxiety and depression-anxiety subscale (HADS-A), depression, anxiety and stress scale-anxiety subscale (DASS-A), and generalised anxiety disorder (GAD-7) scale in an oncology setting using Rasch analysis and diagnostic accuracy statistics. Curr Psychol. 2020. https://doi.org/10.1007/s12144-020-00906-x .
Motolese F, Rossi M, Albergo G, Stelitano D, Villanova M, Di Lazzaro V et al. The psychological impact of COVID-19 pandemic on people with multiple sclerosis. Front Neurol. 2020;11.
Alghadir A, Manzar MD, Anwer S, Albougami A, Salahuddin M. Psychometric properties of the generalized anxiety disorder scale among Saudi University male students. Neuropsychiatr Dis Treat. 2020;16:1427–32.
Byrd-Bredbenner C, Eck K, Quick V. Psychometric properties of the generalized anxiety Disorder-7 and generalized anxiety disorder-Mini in United States University students. Front Psychol. 2020;11.
Tiirikainen K, Haravuori H, Ranta K, Kaltiala-Heino R, Marttunen M. Psychometric properties of the 7-item generalized anxiety disorder scale (GAD-7) in a large representative sample of Finnish adolescents. Psychiatry Res. 2019;272:30–5.
Shrestha S, Ramos K, Fletcher TL, Kraus-Schuman C, Stanley MA, Ramsey D, et al. Psychometric properties of worry and anxiety measures in a sample of African American and caucasian older adults. Aging Ment Health. 2020;24:315–21.
Liang Y, Wu K, Zhou Y, Huang X, Zhou Y, Liu Z. Mental Health in Frontline Medical Workers during the 2019 Novel Coronavirus Disease Epidemic in China: a comparison with the General Population. Int J Environ Res Public Health. 2020;17:6550.
Peters L, Peters A, Andreopoulos E, Pollock N, Pande RL, Mochari-Greenberger H. Comparison of DASS-21, PHQ-8, and GAD-7 in a virtual behavioral health care setting. Heliyon. 2021;7.
Galindo-Vázquez O, Ramírez-Orozco M, Costas-Muñiz R, Mendoza-Contreras LA, Calderillo-Ruíz G, Meneses-García A. Symptoms of anxiety, depression and self-care behaviors during the COVID-19 pandemic in the general population. Gac Med Mex. 2020;156:298–305.
PubMed PubMed Central Google Scholar
Stocker R, Tran T, Hammarberg K, Nguyen H, Rowe H, Fisher J. Patient Health Questionnaire 9 (PHQ-9) and general anxiety disorder 7 (GAD-7) data contributed by 13,829 respondents to a national survey about COVID-19 restrictions in Australia. Psychiatry Res. 2021;298:113792.
Jordan P, Shedden-Mora MC, Löwe B. Psychometric analysis of the generalized anxiety disorder scale (GAD-7) in primary care using modern item response theory. PLoS ONE. 2017;12:e0182162.
Soto-Balbuena C, Rodríguez-Muñoz MF, Le H-N. Validation of the generalized anxiety disorder screener (GAD-7) in Spanish pregnant women. Psicothema. 2021;33:164–70.
PubMed Google Scholar
Teymoori A, Real R, Gorbunova A, Haghish EF, Andelic N, Wilson L, et al. Measurement invariance of assessments of depression (PHQ-9) and anxiety (GAD-7) across sex, strata and linguistic backgrounds in a european-wide sample of patients after traumatic brain Injury. J Affect Disord. 2020;262:278–85.
Johnson SU, Ulvenes PG, Øktedalen T, Hoffart A. Psychometric properties of the General anxiety disorder 7-Item (GAD-7) scale in a Heterogeneous Psychiatric Sample. Front Psychol. 2019;10.
Zhou Y, Xu J, Rief W. Are comparisons of mental disorders between Chinese and German students possible? An examination of measurement invariance for the PHQ-15, PHQ-9 and GAD-7. BMC Psychiatry. 2020;20:480.
Moreno E, Muñoz-Navarro R, Medrano LA, González-Blanch C, Ruiz-Rodríguez P, Limonero JT, et al. Factorial invariance of a computerized version of the GAD-7 across various demographic groups and over time in primary care patients. J Affect Disord. 2019;252:114–21.
Stochl J, Fried EI, Fritz J, Croudace TJ, Russo DA, Knight C, et al. On dimensionality, Measurement Invariance, and suitability of Sum scores for the PHQ-9 and the GAD-7. Assessment. 2020. 1073191120976863.
Doi S, Ito M, Takebayashi Y, Muramatsu K, Horikoshi M. Factorial Validity and Invariance of the 7-Item generalized anxiety disorder scale (GAD-7) among populations with and without self-reported Psychiatric Diagnostic Status. Front Psychol. 2018;9.
Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90.
Hinz A, Klein AM, Brähler E, Glaesmer H, Luck T, Riedel-Heller SG, et al. Psychometric evaluation of the generalized anxiety disorder screener GAD-7, based on a large German general population sample. J Affect Disord. 2017;210:338–44.
Sawaya H, Atoui M, Hamadeh A, Zeinoun P, Nahas Z. Adaptation and initial validation of the Patient Health Questionnaire– 9 (PHQ-9) and the generalized anxiety disorder– 7 questionnaire (GAD-7) in an arabic speaking Lebanese psychiatric outpatient sample. Psychiatry Res. 2016;239:245–52.
Gonzales-Castillo JR, Varona-Castillo L, Dominguez-Morante MG, Ocaña-Gutierrez VR. Pandemia De La COVID-19 y las Políticas De Salud Pública en El Perú: marzo-mayo 2020. Rev Salud Pública. 2020;22:1–9.
Presidencia de Consejo de Ministros. Decreto Supremo N° 044-2020-PCM. 2020. https://www.gob.pe/institucion/pcm/normas-legales/460472-044-2020-pcm . Accessed 22 May 2021.
Kola L, Kohrt BA, Hanlon C, Naslund JA, Sikander S, Balaji M, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. 2021;8:535–50.
Kroenke K, Spitzer L, Williams RBW, Monahan JO, Löwe P. B. Anxiety disorders in Primary Care: prevalence, impairment, Comorbidity, and detection. Ann Intern Med. 2007.
Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Levis B, Benedetti A, Thombs BD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 2019;365.
Villarreal-Zegarra D, Copez-Lonzoy A, Bernabé-Ortiz A, Melendez-Torres GJ, Bazo-Alvarez JC. Valid group comparisons can be made with the Patient Health Questionnaire (PHQ-9): a measurement invariance study across groups by demographic characteristics. PLoS ONE. 2019;14:e0221717.
R Core Team. R: A language and environment for statistical computing. 2021.
Rosseel Y. Lavaan: an R Package for Structural equation modeling. J Stat Softw. 2012;48:1–36.
Jorgensen TD, Pornprasertmanit S, Schoemann AM, Rosseel Y, Miller P, Quick C et al. semTools: Useful Tools for Structural Equation Modeling. 2022.
Epskamp S, Stuber S, Nak J, Veenman M, Jorgensen TD, semPlot. Path Diagrams and Visual Analysis of Various SEM Packages’ Output. 2022.
Brown TA. Confirmatory factor analysis for applied research. New York, NY, US: The Guilford; 2006.
Google Scholar
Flora DB, Curran PJ. An Empirical Evaluation of Alternative Methods of Estimation for Confirmatory Factor Analysis with Ordinal Data. Psychol Methods. 2004;9:466–91.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6:1–55.
Yun C-Y, Muthen B. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes. Doctoral dissertation. University of California; 2002.
Sousa KH, West SG, Moser SE, Harris JA, Cook SW. Establishing measurement invariance: English and Spanish Paediatric Asthma Quality of Life Questionnaire. Nurs Res. 2012;61:171–80.
Chen FF. Sensitivity of goodness of fit indexes to lack of Measurement Invariance. Struct Equ Model Multidiscip J. 2007;14:464–504.
Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med. 2018;18:91–3.
Franco-Jimenez RA, Nuñez-Magallanes A. Propiedades psicométricas del GAD-7, GAD-2 Y GAD-Mini en universitarios peruanos. Propósitos Represent. 2022;10:e1437–1437.
Villarreal-Zegarra D, Barrera-Begazo J, Otazú-Alfaro S, Mayo-Puchoc N, Bazo-Alvarez JC, Huarcaya-Victoria J. Sensitivity and specificity of the Patient Health Questionnaire (PHQ-9, PHQ-8, PHQ-2) and general anxiety disorder scale (GAD-7, GAD-2) for depression and anxiety diagnosis: a cross-sectional study in a Peruvian hospital population. BMJ Open. 2023;13:e076193.
Shih Y-C, Chou C-C, Lu Y-J, Yu H-Y. Reliability and validity of the traditional Chinese version of the GAD-7 in Taiwanese patients with epilepsy. J Formos Med Assoc Taiwan Yi Zhi. 2022;121:2324–30.
Download references
Acknowledgements
Not applicable.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Universidad César Vallejo, Escuela de Medicina, Trujillo, Peru
David Villarreal-Zegarra
Escuela Profesional de Medicina Humana, Universidad Privada San Juan Bautista, Filial Ica, Ica, Peru
Jeff Huarcaya-Victoria
Universidad San Ignacio de Loyola, Lima, Peru
Anthony Copez-Lonzoy
Instituto Peruano de Orientación Psicológica, Lima, Peru
David Villarreal-Zegarra, Rubi Paredes-Angeles, Nikol Mayo-Puchoc & Anthony Copez-Lonzoy
Universidad Nacional Mayor de San Marcos, Lima, Peru
Enoc Arenas-Minaya
You can also search for this author in PubMed Google Scholar
Contributions
David Villarreal-Zegarra: Formal analysis, methodology, supervision, validation, writing– original version, and approval of the final version. Rubi Paredes-Angeles: conceptualization, formal analysis, methodology, validation, writing– original version. Nikol Mayo: conceptualization, methodology, validation, writing– original version, and approval of the final version. Enoc: Methodology, Validation, Writing– Original version, Approval of the final version. Jeff Huarcaya-Victoria: Conceptualization, approval of the final version. Anthony Copez-Lonzoy: Conceptualization, Methodology, Validation, Writing– Review & Editing, Supervision, Approval of the final version.
Corresponding author
Correspondence to Anthony Copez-Lonzoy .
Ethics declarations
Ethics approval and consent to participate.
The institutional research ethics committee of the Instituto Peruano de Orientación Psicológica approved the study protocol. Informed consent to participate was obtained from all the participants, for participants below 16 years, informed consent was obtained from their legal guardians.
Consent for publication
Conflict of interest.
The authors report no conflicts of interest when conducting the study, analyzing the data, or writing the manuscript.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Villarreal-Zegarra, D., Paredes-Angeles, R., Mayo-Puchoc, N. et al. Psychometric properties of the GAD-7 (General Anxiety Disorder-7): a cross-sectional study of the Peruvian general population. BMC Psychol 12 , 183 (2024). https://doi.org/10.1186/s40359-024-01688-8
Download citation
Received : 31 January 2024
Accepted : 26 March 2024
Published : 02 April 2024
DOI : https://doi.org/10.1186/s40359-024-01688-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychometrics
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Shanghai Arch Psychiatry
- v.28(1); 2016 Feb 25
Language: English | Chinese
Case report of a child's anxiety disorder precipitated by tremors from a distant earthquake that was extensively covered in local news stories
当地新闻对远距离地震所致非破坏性震感的过度报道促发儿童焦虑障碍的病例报告, m.s. bhatia.
Department of Psychiatry, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi, India
Earthquakes are relatively common natural disasters in many parts of the world, but research about the mental health effects of earthquakes remains limited. Individuals experiencing an earthquake often suffer significant loss and are at increased risk for developing mental disorders. However, the prevalence of mental disorders following less dramatic or non-destructive earthquake phenomena is unknown. We report the case of a 10-year-old girl who came to a psychiatric outpatient department with a 2-week history of severe, disabling anxiety symptoms precipitated by non-destructive tremors from a distant earthquake that received extensive coverage in the local press. Her condition did not meet criteria for any of the specific anxiety-related disorders, so the non-specific DSM-5 category 'Other Specified Anxiety Disorder' was considered most appropriate. Her symptoms resolved over 4 weeks when treated with both a benzodiazepine and a selective serotonin reuptake inhibitor.
地震是世界上许多地区比较常见的自然灾害,但地震对心理健康影响的研究还很有限。经历地震的人往往遭受重大损失,患精神障碍的风险增加。然而,规模不大、非破坏性地震现象所致精神障碍的患病率还是未知的。本文报告了一名就诊于精神科门诊的10岁女孩,她出现严重影响功能的焦虑症状已2周,其诱因是经历了一场较远地区的地震,而在当地仅有非破坏性震感,媒体却过度报道。她的情况不符合任何特定的焦虑相关障碍,因此最合适的诊断是精神障碍诊断与统计手册第五版 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, DSM-5) 非特异性分类中的“ 其它特定焦虑障碍”。经过一种苯二氮䓬类药物和一种选择性5- 羟色胺再摄取抑制剂的治疗,患者的症状4周后消失。
中文全文
本文全文中文版从2016年5月25日起在 http://dx.doi.org/10.11919/j.issn.1002-0829.215077 可供免费阅览下载
1. Introduction
Earthquakes are among the most common and most devastating natural disasters known to mankind, but much still needs to be understood about the mental health consequences of earthquakes and about the risk factors that increase the likelihood of a mental disorder following a major earthquake. [1] Numerous mental health conditions are known to occur after earthquakes, events that often result in significant losses for many members of the affected communities. [1] Major earthquakes have been associated with an increased prevalence of major depression (MDD), anxiety disorders, post-traumatic stress disorders (PTSD), [2] sleep disorders, [3] and other neurological complaints such as dizziness. [4] The estimated prevalence of MDD among earthquake survivors is approximately 12% and that of PTSD is 8%. [5] Female survivors have higher rates of most psychiatric disorders following earthquakes than male survivors. Other factors that increase the risk of mental disorders following an earthquake include being divorced or widowed, having a low education, and experiencing significant damage to one's home. [5] A survey that investigated the psychological reactions and recovery process of children and adolescents who had experienced a major earthquake found that fear- and anxiety-related mental disorders occurred earlier and resolved more quickly than depressive disorders and psychophysical symptoms. [6]
Most research studies on the mental health effects of earthquakes focus on survivors living in communities that were severely affected by the earthquake.[ 5 , 7 ] Few studies assess the mental health effects on communities that are further from the earthquakes' epicenters where residents experience minor trembling and aftershocks but no structural damage or injury. Non-destructive earthquake tremors and aftershocks are known to cause episodes of dizziness, presumably due to a disturbance in the brain's equilibrium mechanisms, [8] but there have been no reports of the prevalence of major mental disorders among individuals who experience such nondestructive earthquake phenomena.
We report a case of a 10-year-old girl who came to our outpatient psychiatry department with symptoms of anxiety after experiencing a non-destructive earthquake tremor caused by a distant earthquake.
2. Case report
A 10-year-old girl was brought to our outpatient psychiatry department with symptoms of anxiety that began after experiencing an earthquake tremor while sitting in her Delhi home two weeks earlier. The epicenter of the earthquake was in Afghanistan where there was severe destruction and loss of life, but Delhi had only experienced minor tremors with no loss of life or property. The girl had seen coverage of the earthquake in news reports and became fearful that a major earthquake would occur in Delhi. She refused to leave her home and became afraid of anything that moved. When taken out of her home by family members, she became anxious when seeing moving motor vehicles and even when seeing leaves move on trees. Family members tried to reassure her that no earthquake was occurring and that the movements around her were normal, but she was not convinced and believed that she was experiencing another earthquake tremor. In the two weeks before coming to the outpatient department, she had stopped attending school and playing outdoors with her friends. Continually apprehensive about earthquakes, she was unable to study. She repeatedly scanned the walls, furniture, and appliances in her home, asking family members for reassurance that they were not moving due to an earthquake. She refused to sit in front of a fan or air conditioner and asked that others switch them off. Her sleep became disturbed; she woke multiple times during the night and cried out with fear that an earthquake was occurring. Her parents reported that she had no significant past history of psychological problems and was previously well-adjusted. There was no family history of any psychiatric disorder.
The mental status examination at the time of her first clinic visit found that she was conscious and oriented to time, place, and person. She was well-groomed and had no abnormal perceptions, but her affect was anxious and she was preoccupied with the possibility of the occurrence of an earthquake. Her general physical examination was normal. Her routine laboratory tests (including blood profile; liver, kidney, and thyroid function tests; electrocardiogram; and urine test) were all within normal limits.
We taught her relaxation exercises and prescribed alprazolam 0.25 mg once daily. However, at the two-week follow-up visit she showed little improvement, so the alprazolam was augmented with escitalopram 10 mg daily. At the 4-week follow-up visit, 2 weeks after starting the escitalopram, she reported significant improvement: she no longer felt afraid of moving objects, was able to play outdoors with her friends, and was able to return to school.
3. Discussion
This case report is unique in that the young girl's anxiety was precipitated by experiencing only the tremors of an earthquake without suffering any actual physical damage or loss. Apparently her emotional response to this relatively mild exposure to the earthquake was intensified by news reports of major destruction at the earthquake's epicenter. Her symptoms were quite severe and disabling, but they had only lasted for 2 weeks at the time of first evaluation, so she did not fit neatly into any of the currently available specific diagnostic categories.
The International Classification of Diseases-Tenth Revision (ICD 10) [9] criteria for Acute Stress Reaction stipulate that symptoms from transient stressors must diminish in less than 8 hours and symptoms from persistent stressors must diminish within 48 hours; but in our case the symptoms persisted and became progressively worse for 2 weeks following the initial stressor. The corresponding diagnosis in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [10] is 'Acute Stress Disorder'; the required duration is 3 days to a month, which fits our case, but there must be a precipitating event that is life threatening and repeated exposure by television and other media is explicitly excluded so, again, our case does not fit these criteria. PTSD symptoms need to persist for at least a month and the symptoms of Generalized Anxiety Disorder (GAD) need to persist for 6 months, so neither diagnosis was appropriate for this patient.
Given the severity of the symptoms and the degree of disability, the patient merited a psychiatric diagnosis despite not meeting criteria of PTSD or any of the specific anxiety disorders. After excluding the other possible diagnoses, the remaining diagnosis was 'Other Specified Anxiety Disorder, ' a non-specific DSM 5 category that covers situations in which significant anxiety is present with associated social dysfunction, but the individual does not meet criteria of any other specific condition.
Treatment was tailored according to the needs of the case as no standardized guidelines exist for the management of Other Specified Anxiety Disorder. Her severe, disabling anxiety was not controlled after two weeks of relaxation exercises and monotherapy with a benzodiazepine (alprazolam), so a selective serotonin reuptake inhibitor (SSRI) was added (escitalopram). After two weeks on this combined treatment with a benzodiazepine and a SSRI, her symptoms improved dramatically and her social functioning returned to normal. In an earlier report [11] we described a similar case of a 19-year-old male who suffered from debilitating anxiety that was only controlled after treatment with a SSRI.
Research is needed to explore how earthquakes and other major disasters affect the mental health of those who only indirectly witness the events via news reports or who experience only minimal physical effects, such as non-destructive earthquake tremors and aftershocks.
Professor M.S Bhatia obtained a bachelor degree of medicine in 1982 from Maulana Azad Medical College in Delhi University and an MD in psychiatry in 1987 from Lady Hardinge Medical University in Delhi University, New Delhi. He currently is a professor and the head of the Department of Psychiatry, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi, India. He also is an editor of the Delhi Psychiatry Journal, field editor of the Indian Journal of Psychiatry, an executive member of the Indian Psychiatric Society (North Zone) and the Indian Association for Social Psychiatry, a member of the World Psychiatric Association, the World Association of Social Psychiatry, and the World Federation for Biological Psychiatry. His research interests are psychopharmacology, cultural psychiatry, consultation liaison psychiatry, and somatoform disorders.
Funding Statement
No funding was received to prepare this case report.
Conflict of interest statement:The authors report no conflict of interest related to this case report.
Informed consent:The patient's father provided written informed consent for the publication of this case report.

Personalize Your Experience
Log in or create an account for a personalized experience based on your selected interests.
Already have an account? Log In
Free standard shipping is valid on orders of $45 or more (after promotions and discounts are applied, regular shipping rates do not qualify as part of the $45 or more) shipped to US addresses only. Not valid on previous purchases or when combined with any other promotional offers.
Register for an enhanced, personalized experience.
Receive free access to exclusive content, a personalized homepage based on your interests, and a weekly newsletter with topics of your choice.
Home / Parenting, Kids & Teens / Could my child’s social challenges actually be signs of social anxiety disorder?
Could my child’s social challenges actually be signs of social anxiety disorder?
An excerpt from Anxiety Coach
Please login to bookmark

Anxiety Coach by Mayo Clinic child psychologist Stephen P. Whiteside, Ph.D, L.P, takes Mayo Clinic’s safe, rapid, effective Exposure Therapy program for children and teens suffering from anxiety disorders, OCD and phobias, and adapts it from a supervised clinical setting to the family home in an easy to follow self help guide for parents and kids. In the following excerpt from Anxiety Coach , Stephen Whiteside helps parents figure out if their child’s social challenges are actually signs of social anxiety disorder, what sets off social anxiety, why a child avoids triggering situations and finally presents a simple case study of a 16 year old girl with social anxiety disorder, who went on to be successfully treated with Exposure therapy.
What is social anxiety disorder ?
The term social anxiety disorder fits when children are overly nervous about interacting with other people, particularly peers. Kids with social anxiety are afraid they will make mistakes when talking or will say or do something that could lead other people to think of them negatively. Feeling nervous leads kids to avoid situations that involve talking with or hanging out with or even being around other kids. When children with social anxiety disorder consistently avoid social situations, it means they miss out on fun activities, like sports, or don’t do things they need to do, like give a class presentation. Over time, missing out on these important activities can cause other problems. Social anxiety disorder is one of the most common reasons families come to our clinic.
How do we know it’s social anxiety disorder?
Social anxiety disorder is different from typical shyness in the degree of anxiety that kids experience and how much their fears cause problems. There is nothing wrong with being shy or introverted; I myself was pretty shy as a child. Being nervous giving presentations at school or starting a new activity is also a very normal, common experience. As I mentioned earlier, it’s important not to unnecessarily label your child’s behavior as a problem. If they are content with the way they are living their life and they are doing the school and social activities they need to, that’s a solid sign that all is well. However, when fears of embarrassment are so upsetting that they get in the way of living everyday life, that’s when we call it social anxiety disorder and recommend treatment. There are times in our clinic when kids and parents disagree on whether social anxiety is a problem. This usually happens in two scenarios. Since many social interactions for kids occur in school, without parents there to witness their child’s difficulties, parents have only the impression they get from seeing their child function in the family setting, whether that’s at home or in public. In these cases, parents may not realize how much their teens or kids are struggling socially. Other times, it’s the reverse, and kids are so upset by their social difficulties that they deny they are nervous and instead say they are simply not interested in spending time with other kids, and what is wrong with that conscious choice, if they are making it? In that and similar kinds of cases, we need to focus on the three jobs we expect from kids and teens—being successful in school, with friends, and at home—and if there are problems in those areas, we can explore how social anxiety might be getting in the way. In addition to situations and activities, for some kids social anxiety is set off by memories of awkward social situations or physical feelings of anxiety or embarrassment, like blushing or sweating, which lead to the same withdrawal and avoidance as social anxiety that relates to real-time, everyday scenarios.
What sets off my child’s social anxiety?
Social anxiety is typically set off by things in the world around us, most often situations in which kids need to talk to their peers or other people or when they may be observed by others. There are many different types of social situations and not all will give your child feelings of anxiety. Some children get more nervous in performance situations— reading aloud in class, acting in a school play, singing in a school musical, answering a question in class, competing in a basketball game, playing in a school concert, or giving a presentation in class. Others might get more nervous in unstructured social situations, like initiating conversations, meeting other kids at the start of a new school year, joining a club, finding people to sit with during lunch, or making small talk in the hallways between classes. And then there are kids whose anxiety is set off by talking to adults, especially in public situations such as the school principal, a teacher, or a sports coach. These children may also be nervous to order food at restaurants, ask questions of store clerks, or check out with you at the grocery store. Sometimes children feel nervous simply being in public where people may be watching and observing them. For many kids with social anxiety, all of the above may set off their anxiety.
Expectations that make social situations scary
Once you’ve identified the situations that set off your child’s anxiety, the next thing to do is pinpoint the expectations that cause your child to feel nervous in these situations when most of their peers enjoy them or feel only somewhat uncomfortable. As we have learned, there are two main expectations that drive fear and worry— something bad will happen and I won’t be able to handle this —both apply to kids with social anxiety. A core component of social anxiety is the fear of being judged negatively. However, the type of feared judgment often differs based on the situation in which kids feel anxious. Kids who get nervous speaking in performance situations may have expectations that they will make mistakes, perform poorly, and be judged as not good enough, smart enough, or talented enough. Kids who are more nervous about talking to peers may be more afraid that they will do something embarrassing and everyone will think they’re uncool or unlikable. And when kids are nervous around authority figures they are typically concerned about getting in trouble, being a burden, or irritating others. For many children with social anxiety, expectations can occur in any combination of the above. Despite the importance of expecting negative judgment in social anxiety, it’s important to note that some kids don’t describe these specific worries. Younger kids especially are more likely to simply say that talking to others is scary and they don’t know why. Teens may add that they know it’s unlikely that people will laugh at them or be mean but that they still feel nervous. If this is the case, you might describe the child’s expectation as believing they can’t handle talking to people or they have to avoid being around people to feel okay.
Avoidance of social situations
Next, we need to identify what avoidance strategies your child uses to stay away from the situations they fear and in doing so, miss out on the opportunity to learn that these situations are not as bad as they expect them to be. The most common form of avoidance for kids with social anxiety disorder is partial physical avoidance, which is when kids can’t completely avoid a situation but try to avoid as much of it as possible when they are in the midst of it. For example, these kids can’t avoid going to class, but when in class, they are careful never to raise their hand to answer a question asked by a teacher. Or because of anxiety around playing on the school football team, a teen might arrive at practice at the last minute and rush home quickly afterward to avoid the banter and socializing among teammates in the locker room. Partial avoidance due to social anxiety can also include a child keeping their head down while walking in the hallways between classes at school, avoiding eye contact to make sure no one talks to them, or purposefully reading a book before class to put up a wall against being greeted by fellow classmates. As many parents of socially anxious children know, full avoidance of anxiety-provoking activities can also occur. Complete avoidance involves not signing up for sports, clubs, and other extracurricular activities. Or not attending school dances or sporting events. Or eating lunch in the library. It may grow to include staying home from school on days there is a presentation due or even transitioning to online school or homeschooling. Kids with social anxiety may also often rely on others to help avoid feared social interactions. As we saw earlier, parents may be asked to order food in restaurants or communicate with teachers.
Social anxiety disorder, a case study
Meet 16-year-old Maria, a smart, likable teenager and a successful figure skater. She and her parents agreed that she had always been shy, but it hadn’t been a problem because she’d maintained a core group of friends since kindergarten. In restaurants, she’d appear nervous, and her parents would order for her, but they weren’t overly concerned about it. None of this was a problem until she entered middle school. With that transition, she began to struggle. Her core friends connected with new faces and added new friends, while Maria stayed on the sidelines, feeling shy. She felt even more nervous in class when she didn’t yet know many of the other students and, with seven different classes a day, there wasn’t much of a chance to get to know her teachers. In this new environment, she came to dread presentations, yet was too nervous to ask for help. Under pressure across the board, some of her grades began to slip. When Maria began to complain that she felt too sick to go to school on days she had a class where there was always a lot of student participation, her parents brought her in to Mayo Clinic for help. During the initial assessment, Maria readily acknowledged that in social situations she was afraid she would say the wrong thing and look ridiculous in front of other kids who all seemed to be calm, outgoing, and happy to make new friends and expand their social circle. She had always felt comfortable with figure skating because so much of it involved working on her own without having to make conversation with the other skaters. However, now that they were getting older and spending more time chit chatting before and after practice, she was struggling with these interactions and feeling awkward. What she feared most was doing something foolish that would lead her peers to laugh at her and, as a result, see no value in being friends with her. Although she outright avoided some school activities and relied on her parents to order for her at restaurants, most of her avoidance strategies involved finding ways to dodge direct conversation when at school or during activities by looking busy, avoiding eye contact, or leaving early. It had reached a point where she felt left out and was considering quitting. After our clinical assessment, a diagnosis of social anxiety disorder was agreed upon and she went on to be rapidly and successfully treated with Exposure therapy.

Relevant reading
I’m a Paramedic
A lively, illustrated introduction to the essential work of paramedics as community helpers and health heroes.

My Life Beyond Sickle Cell Disease
A graphic nonfiction story with a kid’s-eye view of living with, and beyond, sickle cell disease.

Discover more Parenting, Kids & Teens content from articles, podcasts, to videos.
Want more children’s health and parenting information? Sign up for free to our email list.
Children’s health information and parenting tips to your inbox.
Sign-up to get Mayo Clinic’s trusted health content sent to your email. Receive a bonus guide on ways to manage your child’s health just for subscribing.
You May Also Enjoy

Privacy Policy
We've made some updates to our Privacy Policy. Please take a moment to review.

IMAGES
VIDEO
COMMENTS
Two treatment studies have been conducted with very young anxious children but GAD was mixed with other anxiety disorders [4, 17]. One assessment study has been conducted with two- to five-year-old children to describe differences of children with GAD compared to selective mutism, but test-retest stability of diagnoses was not tested and ...
Generalized anxiety disorder (GAD) is purported to start in early childhood but concerns about attenuation of anxiety symptoms over time and the development of emerging cognitive and emotional processing capabilities pose multiple challenges for accurate detection. This paper presents the first know …
Hannah, an anxious child. This article presents a case study of an anxious child, and highlights some common symptoms for parents and teachers to be watchful for. The case study involves a fictitious identity; any resemblance to a real person is completely coincidental. Hannah (not a real person) was a 10-year-old girl from a close, supportive ...
Treatment of Generalized Anxiety Disorder: A Case Study of a 17 Year-Old Male An Empirically Supported Treatment Case Study Submitted to the Faculty of the Psychology Department of ... Noah is the only biological child of both parents who divorced when Noah was 14 years old. His mother currently works in administration and father worked as a ...
The QEEG study provides important information about the specificity of brain waves of people with generalized anxiety disorder; therefore, it enables the preliminary and quick diagnosis of ...
Figure Box 1. Generalized anxiety disorder (GAD) is one of the most common mental health disorders among children, affecting an estimated 2% to 10%. 1-3 Despite this high prevalence, few affected children are properly diagnosed or receive adequate mental health care. 4 Although GAD in children may remit spontaneously, it also can cause severe social, academic, and emotional impairment or ...
For example, one study of 1375 consecutive referrals (mean age 10.7) to a paediatric psychopharmacology clinic found that the median age of onset of a child's first anxiety disorder was 4 years.30 Children seeking treatment for anxiety often present in middle childhood, for symptoms which began much earlier, exposing the child and family to ...
Cognitive behavioral therapy (CBT) designed to target generalized anxiety disorder (GAD) in youth was examined in a pilot feasibility trial. Participants (aged 10-18 years) were randomized to either 10 weeks of individual CBT (n = 20) or supported wait-list (n = 20). Diagnostic status (primary outcome) was assessed blindly at post-treatment for both groups, and at a 3-month follow-up for ...
Between 2016 and 2020, anxiety rates among kids had increased from 7.1% to 9.2%, according to a study published in JAMA Pediatrics whereas a review published just a year later in the Journal of Psychiatric Research reported rates of anxiety among kids were between 19% and 24%.
Clinical case scenarios: Generalised anxiety disorder (2011) 4 Case scenario 1: Mary Presentation Mary is aged 42 years, divorced with two children, employed part time and cares for her mother who has Alzheimer's disease. Past history Mary has no significant past medical history, although she frequently makes
This case report describes cognitive-behavioral treatment (CBT) with a 7-year-old girl diagnosed with generalized anxiety disorder (GAD) and specific phobia (fear of vomiting). Developmental history was significant for excessive worry, pervasive anxiety, and complaints of stomach discomfort.
Generalized anxiety disorder is diagnosed in children and adolescents who have prominent and impairing anxiety symptoms that are not focused enough to meet criteria for a specific disorder such as social anxiety disorder Social Anxiety Disorder in Children and Adolescents Social anxiety disorder is a persistent fear of embarrassment, ridicule, or humiliation in social settings.
This case study follows an 8-year-old Caucasian female who presented with symptoms of Generalized Anxiety Disorder (GAD). Given this child's age but advanced cognitive skills, careful selection of an appropriate treatment was made.
Generalized anxiety disorder (GAD) is a mental health problem. A child with GAD has a lot of worry and fear that seems to have no real cause. The worry may be more intense than the situation calls for. Children or teens with GAD often worry about many things, such as: Future events. Past behaviors. Social acceptance.
Abstract. This article presents the clinical case of a 38-year-old man with generalized anxiety disorder (GAD). "William" reports longstanding excessive and uncontrollable worry about a number of daily life events, including minor matters, his family, their health, and work. In addition, he endorses chronic symptoms of restlessness and ...
Case Study Details. Phil is a 67-year-old male who reports that his biggest problem is worrying. He worries all of the time and about "everything under the sun.". For example, he reports equal worry about his wife who is undergoing treatment for breast cancer and whether he returned his book to the library. He recognizes that his wife is ...
The case study I am choosing is about James who is a doctor suffering from generalized anxiety disorder. At 31 years of age and living in New York, he is unemployed because of his constant anxiety, even at the thought of working. He now lives with his parents off a small trust fund set up for him by an uncle.
Generalized anxiety disorder (GAD) is purported to start in early childhood but concerns about attenuation of anxiety symptoms over time and the development of emerging cognitive and emotional processing capabilities pose multiple challenges for accurate detection. This paper presents the first known case reports of very young children with GAD to examine these developmental challenges at the ...
Anxiety disorders (ADs) are among the main mental health problems worldwide and are considered among the most disabling mental health problems; they were among the 25 leading causes of mental health burden worldwide in 2019 [].The number of ADs has been increasing; in 2015, the estimated incidence of anxiety disorders worldwide was 3.6% (264 million), with a greater proportion of women [].
1. Introduction. Earthquakes are among the most common and most devastating natural disasters known to mankind, but much still needs to be understood about the mental health consequences of earthquakes and about the risk factors that increase the likelihood of a mental disorder following a major earthquake. Numerous mental health conditions are known to occur after earthquakes, events that ...
In the following excerpt from Anxiety Coach, Stephen Whiteside helps parents figure out if their child's social challenges are actually signs of social anxiety disorder, what sets off social anxiety, why a child avoids triggering situations and finally presents a simple case study of a 16 year old girl with social anxiety disorder, who went ...