
Schizophrenia
Apr 14, 2013
780 likes | 1.52k Views
Schizophrenia. Features, Diagnosis, Epidemiology, Etiology, Treatment, Neurochemistry Jack Foust, MD Assistant Professor, Department of Psychiatry and Behavioral Sciences Medical University of South Carolina. Features of Schizophrenia - Positive Symptoms. Hallucinations
Share Presentation
- moghaddam b et al
- hallucinations
- environmental influences
- less likely
- temporal lobe structures
- res brain res rev

Presentation Transcript
Schizophrenia • Features, Diagnosis, Epidemiology, Etiology, Treatment, Neurochemistry • Jack Foust, MD • Assistant Professor, Department of Psychiatry and Behavioral Sciences • Medical University of South Carolina
Features of Schizophrenia - Positive Symptoms • Hallucinations • Disorganized speech/thinking/behavior • Delusions
(from The Hour of the Wolf, directed by Ingmar Bergman)
Features of Schizophrenia - Negative Symptoms • Affective flattening • Alogia • Avolition • Anhedonia • Social Withdrawal
Features of Schizophrenia - Cognitive Deficits • Attention • Memory • Executive functions (organization, planning)
Schizophrenia - DSM Diagnostic Criterion “A” • Characteristic Sxs (2 + for 1 month) • delusions • hallucinations • disorganized speech • grossly disorganized or catatonic behavior • negative Sxs (flat affect, alogia, avolition) • (Only one element required if delusions bizarre, • or hallucinations commentary 2 voices conversing )
Schizophrenia - DSM Diagnostic Criteria B - F • Social/occupational dysfunction (decline) • Duration - 6 months total, 1 month “A” Sxs • Exclusion - SAFD, mood d/o • Exclusion - sub abuse, gen med condition • PDD/Autism - at least 1 month delusions or hallucinations
Schizophrenia - Comorbid Conditions • Depression • Anxiety • Aggression • Substance use disorder
Schizophrenia: Who is at Risk? • Lifetime prevalence • Epidemiologic Catchment Area Study: 1.3% • National Comorbidity Survey: 0.7% • Demographic characteristics • Age - typical onset late teens/early twenties • Gender - earlier age of onset among men • Marital status - less likely to be married
Schizophrenia: Who is at Risk? • Predisposing factors • Season of birth • Pregnancy and birth complications • Genetic background • Precipitating factors • Stress • Substance Abuse
“In addition to interfering with normal brain development, heavy marijuana use in adolescents may also lead to an earlier onset of schizophrenia in individuals who are genetically predisposed” Dr Sanjiv Kumra, Albert Einstein College of Medicine
“Carriers of the COMT valine158 allele were most likely to exhibit psychotic symptoms and to develop schizophreniform disorder if they used cannabis. Cannabis use had no such adverse influence on individuals with two copies of the methionine allele.” Caspi A, et al. Biological Psychiatry.2005; 57:1117-1127.
Genetic Risk Factors
Etiology: Neurodevelopmental Hypothesis • Possible insult during gestation, environmental influences • Disturbance in normal brain maturation • Reduced size medial temporal lobe structures - amygdala, hippocampus • Disturbed cytoarchitecture in hippocampus, entorhinal cortex
Treatment: Psychosocial Interventions • Supportive therapy • Behavioral family therapy • Family education • Social skills training • Community support • Lower relapse; improved functioning, compliance and social adjustment
Treatment: Antipsychotics • Used to treat psychotic disorders, such as schizophrenia, mania, psychotic depression • Include both “typicals” (Haldol) and “atypicals” (Clozaril, Risperdal)
Typical Antipsychotics • Chlopromazine (Thorazine) - prototype • Thioridazine (Mellaril) • Fluphenazine (Prolixin) • Haloperidol (Haldol)
Typical Antipsychotics: Drug/Receptor Effects • Antidopaminergic (D2) • Anticholinergic • Antihistaminic • Anti-alpha 1
Effects of Typical Antipsychotics • Four dopamine pathways • Mesocortical (negative symptoms) • Mesolimbic (positive symptoms) • Nigrostriatal (EPS, TD) • Tuberoinfundibular (hyperprolactinemia)
Guillin O and Laruelle M. Cellscience Reviews. 2005; 2:79-107
DA Receptor Distribution • D1- prefrontal cortex, striatum • D5 - hippocampus and entorhinal cortex • D2 – striatum, low concentration in medial temporal structures (hippocampus, entorhinal cortex, amygdala), thalamus, prefrontal cortex • D3 – striatum and ventral striatum • D4 - prefrontal cortex and hippocampus (have not been detected in the striatum)
Side Effects of Typical Neuroleptics • Extra-pyramidal syndrome (EPS) • Tardive dyskinesia (TD) • Neuroleptic malignant syndrome (NMS) • Prolactin elevation
Extra-Pyramidal Syndrome (EPS) • Acute dystonia • Akathesia • Muscle rigidity • Bradykinesia • Treatment – typically treated with anticholinergic compounds (Cogentin, Benadryl, Artane), Beta-blockers
Tardive Dyskinesia(TD) • 25-year continuous exposure risk: 68% in Yale Incidence Study • Annual incidence: 5% • Risk factors • Increased age • African-American race • Dose and duration of drug exposure • Early and severe EPS
Neuroleptic Malignant Syndrome (NMS) • Potentially fatal complication of neuroleptic Tx • Temperature dysregulation: T >104°F/40°C • Muscle rigidity • Elevated CPK • Elevated WBC • Associated with TaqI A polymorphism in DRD2 • Tx: withdraw neuroleptics, cooling, dantrolene, bromocriptine (DA agonist)
Summary: Limitations of Typical Antipsychotics • Limited efficacy against negative symptoms • A substantial portion of patients (25% to 40%) respond poorly to treatment • EPS occurs at clinically effective doses • Side effects other than EPS (such as NMS) • Liable to cause tardive dyskinesia • Serum prolactin elevation
Advantages of Typical Antipsychotics • No blood monitoring • Efficacious for positive symptoms • Parenteral and depot preparations available • Low-cost
Antipsychotics: Atypical • Clozapine (Clozaril) - prototype • Risperidone (Risperdal) • Olanzepine (Zyprexa) • Quetiapine (Seroquel) • Ziprasidone (Geodon) • Aripiprazole (Abilify)
Atypical Antipsychotics: Clinical and Drug/Receptor Characteristics • Clinically display less EPS, more effective against negative symptoms, some improvement in cognition • Balanced D2/D1 antagonism • Strong 5HT2 antagonists
Serotonin-Dopamine Antagonists and TD: Hypothesized “Site-Specific” Neuromechanisms Psychosis EPS and TD Limbic Cortical Caudate/Putamen A10 A9 Ventral Tegmental Area Substantia Nigra Dopamine/5HT Antagonist Conventional Antipsychotic Agents
Atypical Antipsychotics
Antipsychotic Receptor Affinities • Haloperidol (Haldol)
Antipsychotic Receptor Affinities • Clozapine (Clozaril)
Antipsychotic Receptor Affinities • Risperidone (Risperdal)
Antipsychotic Receptor Affinities • Olanzepine (Zyprexa)
Antipsychotic Receptor Affinities • Quetiapine (Seroquel)
Ziprasidone (Geodon) • High affinity (antagonist) for D2, D3, 5HT2a, 5HT2c, 5HT1d • High affinity (agonist) for 5HT1a • Inhibits re-uptake of 5HT and NE • Moderate affinity for H1, α1 • Low affinity for D1, α2 • Negligible affinity for M1
Ziprasidone (Geodon), cont. • Positive symptoms improved (PANSS) • Negative symptoms improved (PANSS) • Depressive symptoms improved (MADRS) • Low EPS (5HT2a/D2, 5HT1a) • Low weight gain (H1) • Low sexual dysfunction • Minimal CYP450, CBC, LFT or CV effects (some QTc prolongation)
Neurotransmitter Systems Implicated in Schizophrenia Dopamine Acetylcholine Serotonin Norepinephrine GABA Neuropeptides Glutamate
Dopamine Hypothesis • Induction or worsening of psychotic symptoms with dopamine agonists • Amelioration of psychotic symptoms with antipsychotic drugs that are D2-receptor antagonists
Serotonin (5HT) Hypothesis • M-CPP (m-chlorophenylpiperazine) selective 5HT receptor agonist worsens psychotic symptoms • Pretreatment with ritanserin (5HT antagonist) attenuates psychotic symptoms
Glutamate Hypothesis • Psychotomimetic effects of phencyclidine (PCP), a potent N-methyl-D-aspartate (NMDA) type glutamate receptor antagonist - mimics negative, positive and disorganization symptoms • Possible beneficial effects of cycloserine, glutamate receptor agonist
Glutamate, Dopamine, Ketamine • “Subanesthetic doses of ketamine, a noncompetitive NMDA receptor antagonist, impair prefrontal cortex (PFC) function in the rat and produce symptoms in humans similar to those observed in schizophrenia.” • “These findings suggest that ketamine may disrupt dopaminergic neurotransmission in the PFC as well as cognitive functions associated with this region, in part, by increasing the release of glutamate, thereby stimulating postsynaptic non-NMDA glutamate receptors.” Moghaddam B et al. J Neurosci 1997; 17: 2921-2927.
Aghajanian GK, Marek GJ. Brain Res Brain Res Rev 2000; 31:302-312.
Neuronal Circuits in Schizophrenia • Thalamic nuclei relay sensory information to pyramidal neurons in limbic cortex and neocortex through glutaminergic excitatory afferents • Excessive response of pyramidal neurons is putative mechanism of psychosis (overstimulation) Freedman R. Schizophrenia. NEJM. 2003; 349:1738-1749.
- More by User
A group of severe disorders characterized by… disorganized and delusional thinking disturbed perceptions inappropriate emotions and behaviors. Schizophrenia. Often linked to the neurotransmitter dopamine. How Prevalent is Schizophrenia?.
3.27k views • 14 slides
Schizophrenia. Chapter 16. Schizophrenia. Fascinated and confounded healers for centuries One of most severe mental illnesses 1/3 of population 2.5% of direct costs of total budget $46 billion in indirect costs. History of Schizophrenia.
1.51k views • 55 slides
Schizophrenia. Tutorial (6/7/06) O.Arikawe. Definition: Splitting of psychic functions . Incidence : Low incidence but relatively high prevalence Annual incidence using current diagnostic criteria is 0.17 and 0.54 per 1000 population. Types. Acute and chronic
515 views • 16 slides
Schizophrenia. Schizophrenia: The Facts. Affects about .8% of Americans are afflicted Throughout the world over 24 million people suffer from this disease Strikes most commonly in early twenties Affects men and women equally “split mind”. 2. Symptoms of Schizophrenia.
368 views • 11 slides
Schizophrenia. Definition. Schizophrenia is a mental illness that effects the brain that makes the person view reality abnormally. This can consist of delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior. Types.
339 views • 7 slides
Schizophrenia. Chapter 11. Schizophrenia. Positive Symptoms: Type I Delusions Persecutory Delusions of Reference Grandiose Delusions. Schizophrenia. Hallucinations Disorganized Thoughts and Speech Disorganized or Catatonic Behavior http://www.wimp.com/schizophrenicsymptoms/.
368 views • 14 slides
Schizophrenia. By Garren Richardson. What is Schizophrenia?. Schizophrenia is a psychological disorder classified separately from other disorders because it is not easily categorized as an anxiety or mood disorder
376 views • 10 slides
Schizophrenia. The Unwell Brain. Disturbance in the Neurochemistry. The first discovery in the mid 1950s was that chronic usage of large daily doses of Amphetamines could produce a psychosis that was virtually indistinguishable from schizophrenia.
289 views • 12 slides

Schizophrenia. Schizophrenia. Two or more of the following, each present for a significant portion of the time during a 1-month period** Delusions Hallucinations Disorganized speech Grossly disorganized or catatonic behavior Negative symptoms . Schizophrenia.
959 views • 20 slides
Schizophrenia. By Rebecca Stipp. History. Definition. a severe mental disorder characterized by some, but not necessarily all, of the following features: emotional blunting, intellectual deterioration, social isolation, disorganized speech and behavior, delusions, and hallucinations.
268 views • 10 slides
Schizophrenia. What is schizophrenia?. Most disabling and chronic of all mental illnesses Psychosis: type of mental illness- cannot distinguish reality from imagination Psychotic episodes Distorts: Thinking (may believe others are controlling their thoughts) Expression of emotions
294 views • 14 slides
Schizophrenia. Definition Psychotic disorder Thought Disorder Loose associations “Split” from reality NOT split or multiple personality. Symptoms of Schizophrenia. Positive Symptoms Loose associations Word salad Delusions Hallucinations Negative Symptoms Poverty of speech content
538 views • 24 slides
SCHIZOPHRENIA
SCHIZOPHRENIA. Andy Cortez Julian Cruz Period 05. Peter Green. He is the founder of Fleetwood Mac, a famous band He was diagnosed with schizophrenia in the mid 70’s Spent time in psychiatric hospitals and went through electroconvulsive therapy
343 views • 7 slides
Schizophrenia. Unfolding Case Study By Amanda Eymard , DNS, RN and Linda Manfrin-Ledet , DNS, APRN. Assigned Reading to be completed prior to case study. Prior to conducting this unfolding case study, students should read the following:
3.84k views • 82 slides
Schizophrenia. Lecture of 2-14-07. Symptoms. Psychosis Lack of touch with reality Delusions Erroneous beliefs Hallucinations False sensory perceptions Too much dopamine or not enough glutamate. Paranoid Schizophrenia. Delusions of grandeur Believe they are special with special powers
393 views • 22 slides
Schizophrenia. Stacy Zeigler. NIMH. Schizophrenia is a chronic, severe, and disabling brain disorder Affects 1.1% of the U.S. population age 18 and older in a given year.
753 views • 60 slides
Schizophrenia. A group of severe disorders characterized by disorganized and delusional thinking, disturbed perceptions, and inappropriate emotions and behaviours. Those with paranoid tendencies are particularly prone to delusions of persecution.
1.5k views • 7 slides
Schizophrenia. Lyudmyla T. Snovyda. Schizophrenia -.
987 views • 36 slides
Schizophrenia. www.psychlotron.org.uk. Schizophrenia is not a multiple personality A psychotic disorder involving a break with reality Many different manifestations with a few shared features. Schizophrenia diagnosis. Positive Symptoms:
852 views • 24 slides

Schizophrenia. Tiffany Becker Denise Keown Heather Baltz. Overview of Schizophrenia. What is schizophrenia? Schizophrenia behaviors Does schizophrenia affect the brain? What causes schizophrenia? Who gets schizophrenia? Early Onset Schizophrenia Schizophrenia Facts.
1.09k views • 37 slides

Rochelle Blumenstock. Schizophrenia. Etiology. Genetics 10% chance of developing the disorder if you have an immediate relative with it 40-65% chance of both twins being diagnosed with the disorder No single gene associated Many rare genetic mutations . Environment
346 views • 17 slides
schizophrenia
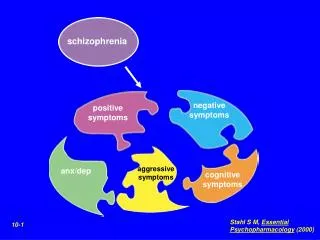
schizophrenia. negative symptoms. positive symptoms. aggressive symptoms. anx/dep. cognitive symptoms. Stahl S M, Essential Psychopharmacology (2000). 10-1. Positive Symptoms of Schizophrenia. Negative Symptoms of Schizophrenia. Stahl S M, Essential Psychopharmacology (2000). 10-20.
640 views • 14 slides
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.7(6); Nov-Dec 2018
Very early-onset psychosis/schizophrenia: Case studies of spectrum of presentation and management issues
Jitender aneja.
1 Department of Psychiatry, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
Kartik Singhai
Karandeep paul.
Schizophrenia occurs very uncommonly in children younger than 13 years. The disease is preceded by premorbid difficulties, familial vulnerability, and a prodromal phase. The occurrence of positive psychotic symptoms such as delusions and hallucinations depends on the level of cognitive development of child. Furthermore, at times it is very difficult to differentiate the psychopathology and sustain a diagnosis of schizophrenia in view of similarities with disorders such as autism, mood disorders, and obsessive compulsive disorders. Here, we present three case studies with varying presentation of childhood-onset psychosis/schizophrenia and associated management issues.
Introduction
Schizophrenia is a chronic severe mental illness with heterogeneous clinical profile and debilitating course. Research shows that clinical features, severity of illness, prognosis, and treatment of schizophrenia vary depending on the age of onset of illness.[ 1 , 2 ] Hence, age-specific research in schizophrenia has been emphasized. Although consistency has been noted in differentiating early-onset psychosis (onset <18 years of age) and adult-onset psychosis (onset >18 years), considerable variation is observed with regard to the age of childhood-onset schizophrenia or very early-onset psychosis/schizophrenia (VEOP/VEOS).[ 2 , 3 ] Most commonly, psychosis occurring at <13 years of age has been considered to be of very early onset and that between 13 and 17 years to be of adolescent onset.[ 4 ] Furthermore, VEOS has been considered to be rare and shown to have differing clinical features (including positive and negative symptoms, cognitive decline, and neuroimaging findings), course, and outcome when compared with that of early-onset or adult-onset schizophrenia.[ 3 ] Progress in acknowledgement of psychotic disorders in children in the recent times has led primary care physicians and paediatricians to increasingly serve as the principal identifiers of psychiatrically ill youth. In recent years, there has been substantial research in early intervention efforts (e.g., with psychotherapy or antipsychotic medicines) focused on the early stages of schizophrenia and on young people with prodromal symptoms.[ 5 ] Here, we report a series of cases with very early onset of psychosis/schizophrenia who had varying clinical features and associated management issues.
Case Reports
A 14-year-old boy, educated up to class 6, belonging to a family of middle socioeconomic status and residing in an urban area was brought with complaints of academic decline since 3 years and hearing voices for the past 2 years. The child was born out of a nonconsanguineous marriage, an unplanned, uneventful, but wanted pregnancy. The child attained developmental milestones as per age. From his early childhood, he was exposed to aggressive behavior of his father, who often attempted to discipline him and in this pursuit at times was abusive and aggressive toward him. Marital problems and domestic violence since marriage lead to divorce of parents when the child attained age of 10 years.
The following year, the child and the mother moved to maternal grandparents’ home and his school was also changed. Within a year of this, a decline in his academic performance with handwriting deterioration, and irritable and sad behaviour was noted. Complaints from school were often received by the mother where the child was found engaged in fist fights and undesirable behavior. He also preferred solitary activities and resented to eat with the rest of the family. In addition, a decline in performance of daily routine activities was seen. No history suggestive of depressive cognitions at that time was forthcoming. A private psychiatrist was consulted who treated him with sodium valproate up to 400 mg/day for nearly 2 months which led to a decline in his irritability and aggression. But the diagnosis was deferred and the medications were gradually tapered and stopped. Over the next 1 year, he also started hearing voices that fulfilled dimensions of commanding type of auditory hallucinations. He suspected that family members including his mother collude with the unknown persons, whose voices he heard and believed it was done to tease him. He eventually dropped out of school and was often found awake till late night, seen muttering to self, shouting at persons who were not around with further deterioration in his socialization and self-care. Another psychiatrist was consulted and he was now diagnosed with schizophrenia and treated inpatient for 2 weeks with risperidone 3 mg, olanzapine 2.5 mg, and oxcarbazepine 300 mg/day with some improvement in his symptoms. Significant weight gain with the medication lead to poor compliance which further led to relapse within 3 months of discharge. Frequent aggressive episodes over the next 1 year resulted in multiple hospital admissions. He was brought to us with acute exacerbation of symptoms and was receiving divalproex sodium 1500 mg/day, aripiprazole 30 mg/day, trifluperazine 15 mg/day, olanzapine 20 mg/day, and lorazepam injection as and when required. He was admitted for diagnostic clarification and rationalization of his medications. He had remarkable physical features of elongated face with large ears. Non-cooperation for mental state examination, and aggressive and violent behavior were noted. He was observed to be muttering and laughing to self. His mood was irritable, speech was laconic, and he lacked insight into his illness. We entertained a diagnosis of very early-onset schizophrenia and explored for the possibilities of organic psychosis, autoimmune encephalitis, and Fragile X syndrome. The physical investigations done are shown in Table 1 . Further special investigations in the form of rubella antibodies (serum IgG = 64.12 U/mL, IgM = 2.44 U/mL) and polymerase chain reaction for Fragile X syndrome (repeat size = 24) were normal. His intelligence quotient measured a year ago was 90, but he did not cooperate for the same during present admission. Initially, we reduced the medication and only kept him on aripiprazole 30 mg/day and added lurasidone 40 mg twice a day and discharged him with residual negative symptoms only. However, his hallucinations and aggression reappeared within 2 weeks of discharge and was readmitted. This time eight sessions of bilateral modified electroconvulsive therapy were administered and he was put on aripiprazole 30 mg/day, chlorpromazine 600 mg/day, sodium divalproex 1000 mg/day, and trihexyphenidyl 4 mg/day. The family was psychoeducated about the illness, and mother's expressed emotions and overinvolvement was addressed by supportive psychotherapy. Moreover, an activity schedule for the child was made, and occupational therapy was instituted. Dietary modifications in view of weight gain were also suggested. In the past 6 months, no episodes of violence came to our notice, though irritability on not meeting his demands is persistent. However, poor socialization, lack of motivation, apathy, weight gain subsequent to psychotropic medications, and aversion to start school are still unresolved. Influence of his multiple medications on bone marrow function is an impending issue of concern.
Details of investigations done in the three children

An 11-year-old boy, educated up to class 3, belonging to a rural family of lower socioeconomic status was brought with complaints of academic decline since 2 years, repetition of acts, irritability since a year, and adoption of abnormal postures since 6 months. He was born out of a nonconsanguineous marriage, uneventful birth, and pregnancy. He was third in birth order and achieved developmental milestones at an appropriate age. Since 2 years, he would not attend to his studies, had poor attention, and difficult memorization. He attributed it to lack of friends at school and asked for school change. There was no history of low mood, depressive cognitions, conduct problems, or bullying and he performed his daily routine like his premorbid self at that time. Since a year, he was observed to repeat certain acts such as pacing in the room from one end to another, continuously for up to 1–2 h, with intermittent stops and often insisted his mother to follow the suit, stand nearby him, or else he would clang on her. He prohibited other family members except his mother near him and would accept his meals only from her. He repeatedly sought assurance of his mother if he had spoken everything right. He also washed his hands repeatedly, up to 10–20 times at one time, and was unable to elaborate reason for the same. His mood during that period was largely irritable with no sadness or fearfulness. He mostly wore the same set of clothes, would be forced to take bath or get nails/hair trimmed, and efforts to these were often met with aggression from the patient. Eventually, he stopped going to school and his family sought faith healing. Within the next 5–6 months, his illness worsened. Fixed gaze, reduced eye blinking, smiling out of context, diminished speech, and refusal to eat food were the reasons for which he was brought to us. His physical examination was unremarkable and his mental state examination using the Kirby's method showed an untidy and ill-kempt child, with infrequent spontaneous acts, and occasional resentment for examination. He had an expressionless face, with occasional smiling to self, negativism, and mutism. No rigidity in any of the limb was observed. He was diagnosed with catatonic schizophrenia and probable obsessive compulsive disorder (vs mannerisms). We performed a battery of physical investigation to rule out organic psychosis [ Table 1 ]. He responded to injection lorazepam with which catatonia melted away. He was also prescribed olanzapine up to 15 mg/day, fluoxetine 20 mg/day, and dietary modification and lactulose for constipation. The family left against medical advice with 50%–60% clinical improvement [rating on Bush Francis Catatonia Rating scale (BFCRS) reduced from 10 to 4]. He relapsed within a month of discharge, initially with predominance of the probable obsessive compulsive symptoms. Fluoxetine was further increased to up to 60 mg/day. But within the next 2 months, the catatonic symptoms reappeared and he was readmitted. He had received olanzapine up to 25 mg/day, which was replaced with risperidone. In view of nonresponse to intravenous lorazepam, we administered him five sessions of modified bilateral Electro-convulsive therapy (ECT) (rating on BFCRS reduced from 8 to 0). The family was psychoeducated about the child's illness and the need for continuous treatment was emphasized. He was discharged with up to 80%–90% improvement. At follow-ups, he started participating at farm work of the family, took care of self, with some repetition of acts such as washing of hands, and denied any associated anxiety symptoms. However, efforts to re-enroll in school had been futile as the child did not agree for it. He has been maintaining at the same level since 6 months of discharge.
A 7-year-old girl, student of second class, belonging to a high socioeconomic status family living in an urban locality was brought with complaints of academic decline, irritability, and abnormal behavior for the past 9 months. The child was born out of a nonconsanguineous marriage, is first in order, and was a wanted child. Maternal health during pregnancy was normal, but the period of labor was prolonged beyond 18 h, so a lower segment caesarean section was performed. There was no history of birth-related complications and the child's birth weight was 2.80 kg. The child attained developmental milestones as per age. The child had a temperament characterized by high activity levels, below average threshold of distractibility, average ability to sustain attention and persist, easy to warm up, adaptation to new situations, and regular bowel and bladder habits. She was enrolled in school at the age of 4 years and progressed well till 9 months back when a decline in her academic interest was observed by her class teacher. Deterioration of her handwriting skills and avoidance of group activities in school were observed. Similarly, at home persistent irritable behavior was seen and her play activities with her siblings reduced. However, her biofunctions were normal during this period.
One month prior to visiting us, she started insisting on wearing the same dress. She wore the same colored or at times the same dress which she would not take off even at bed or bath time. In addition, a change in her mood from largely irritable to cheerful was noted. Her activity levels were increased and it would be difficult to make her sit quietly in class. Her speech output was more than her usual self and she talked incessantly. Her sleep duration also decreased and she started getting up 3–4 h earlier than her usual routine. In view of these symptoms, her family made first contact with us. Her physical examination was normal and mental state examination revealed her to be cheerful, overactive, and difficult to interrupt. She sang and danced during the interview. We diagnosed her with acute mania on the basis of clinical evaluation and assessment on MINI Kid 6.0.[ 6 ] The details of her physical examination are depicted in Table 1 . She was initially treated with olanzapine 5 mg/day which was later on increased to 10 mg/day. However, no response was observed with it in the next 2 weeks, so it was cross tapered with sodium valproate which was built up to 400 mg/day. She improved by nearly 50%, but her mood still remained cheerful/irritable. She did not resume her school and was brought irregularly for the follow-up. Within the next 2 months, she also started muttering to herself and made certain abnormal gestures. She often feared staying alone, or while going to bed insisted the lights to be kept on and ask someone to accompany her in the toilet unlike her previous self. When asked, she reported seeing a lady in white clothes, with no other details. She stopped asking for food on her own and remained lost in her fantasy world. However, her interest in dressing and appreciating herself in mirror persisted. Her mood during this period was mostly labile and often changed from cheerful to sad or irritable. As per the family, the medications were continued as advised. So in view of the emerging picture, the diagnosis was revised to schizo-affective disorder, and in addition to hike in dose of sodium valproate to 500 mg/day, risperidone 2 mg/day was also added. However, even after 8 weeks of treatment with this combination with hike of risperidone to 4 mg/day, there was no relief. The child is still symptomatic, does not go to school, and has significant dysfunction. Psychosocial intervention in the form of psychoeducation, activity scheduling for the child, and occupational therapy has been instituted in addition to the existing treatment regimen, but results are yet to be seen.
The older concept of neurodegenerative etiology of schizophrenia has been superseded by evolving neurodevelopmental nature of this disease. The latter has been attributed to initiation of the underlying pathophysiological processes long before the onset of clinical disease and interaction of the various genetic and environmental factors. The more accommodating theorist propose schizophrenia to be of neurodevelopmental in origin which in turn speeds the process of neurodegeneration.
On clinical front, VEOS is associated with a more insidious onset, prominent negative symptoms, auditory hallucinations, poorly formed delusions which is in part due to less developed cognitive abilities.[ 7 ] The presence of history of speech and language delay as well as motor development deficits have been observed in major studies on childhood-onset schizophrenia, be it the Maudsley early-onset schizophrenia project or the NIMH study.[ 8 , 9 ] Premorbid deficits in social adjustments and presence of autistic symptoms have also been shown. Moreover, the early onset of psychosis is associated with poor prognosis, worse overall functioning, and multiple hospitalizations.[ 7 ] The duration of untreated psychosis in childhood-onset psychosis has been shown to be smaller in hospital-based studies[ 10 ] and larger in community settings.[ 11 ] In addition, the presence of comorbidities and an organic etiology or history of maternal illness during pregnancy is a common finding in VEOS.[ 10 ] In addition, obsessive compulsive symptoms are frequently observed in first-episode drug-naive schizophrenia patients and have a poorer outcome, more severe impairment of social behavior, and lower functioning.[ 12 ] However, in many instances it is very difficult to differentiate the obsessive compulsive symptoms from the motor symptoms of schizophrenia such as stereotypy and mannerisms and varying degree of insight.[ 13 ]
In the present case series, all the children had an insidious onset of illness, with initial symptom of academic decline, and poorly formed psychotic symptoms/psychotic-like experiences. All the children reported here had dropped out of school, showed a shift in their interests, withdrew from social circle, appeared to be distant, had impaired self-care, and often lacked concern for others along with a range of mood disturbances. All these symptoms fit into the classical description of prodromal symptoms of schizophrenia.[ 14 ] In contrast to available evidence, no history of motor, speech, or language delay was noted in any of the child. Furthermore, no history suggestive of autistic features or problems in social adjustments prior to onset of illness was forthcoming.
However, the diagnosis of schizophrenia could be clearly made in the first case, while the second child had predominant catatonic and probably obsessive compulsive symptoms. It is difficult to ascertain the diagnosis of schizophrenia on the basis of presence of only catatonic symptoms and no delusions and hallucinations or negative symptoms as required by Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition or International Classification of Diseases, Tenth Revision. However, it is very difficult to sustain any other diagnosis for the second child. In the third child, the illness has been evolving and the clinical picture changed from predominant mood symptoms to psychotic-like experiences at later stage. Therefore, at present a diagnosis of schizo-affective disorder is entertained. We could not find any possible organic etiology in any of the three cases with the best of our efforts.
With provision of pharmacological and psychosocial treatment in accordance to the available treatment guidelines,[ 15 ] remission was not achieved in two of the three children. Currently, the available evidence also suggests that the prognosis of childhood-onset schizophrenia is mainly poor as it disrupts the social and cognitive development and thus nearly two-third of children do not achieve remission.[ 16 ] On a positive note, we have been able to retain all the children in treatment.
Other issues faced by the families of three children and the treating team are briefly discussed below. In countries like India, where significant expenses are born by patients/family, associated stigma, limited social services, and the anti-psychotic related adverse effects raise the burden of care exponentially. In 2/3 index patients, the family bore the costs of special investigations, which was not possible in the second child and led to financial difficulties for the single mother of the first child. Adding on, the availability of rehabilitation services for children with major mental illnesses is scarce in various parts of our country. Furthermore, we successfully used ECT for management of acute disturbance in two of the three patients prior to the notification of Mental Health Care Act, 2017 that prohibits its use in minors. The case series also put forward a strong case for strengthening and sensitizing primary care physicians and pediatricians in identifying and treating cases of VEOP, since they are more likely to be the first points of contact with patients of the discussed age group. In view of the duration of untreated psychosis being a very eloquent prognostic factor for VEOP and the symptomatology of the same showing significant heterogeneity, armoring primary care physicians and pediatricians with the right skills to identify, treat, or refer patients with VEOP, especially in the prodromal period, might profoundly contribute in decreasing the morbidity and improving prognosis. Citing this lacuna which could be filled and used to our advantage, Stevens et al .[ 17 ] elaborated and discussed various questions which practitioners might find useful.
Childhood-onset schizophrenia is a rare occurrence. The current case series highlights differing clinical presentation of VEOS/VEOP in children and adolescents. Certain other issues pertinent to the management of VEOS/VEOP are also touched upon in this article. With the early recognition of childhood mental health illnesses, we need to build and strengthen ample child and adolescent mental health services in India.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Acknowledgement
The authors thank Dr. Sonam Arora, MD, DNB (Pathology), for providing assistance in laboratory investigations and article writing.
Customer Reviews

260 King Street, San Francisco
Updated Courtyard facing Unit at the Beacon! This newly remodeled…
Finished Papers
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Pilot study shows ketogenic diet improves severe mental illness
A small clinical trial led by Stanford Medicine found that the metabolic effects of a ketogenic diet may help stabilize the brain.
April 1, 2024 - By Nina Bai

A study led by researchers at Stanford Medicine showed that diet can help those with serious mental illness. nishihata
For people living with serious mental illness like schizophrenia or bipolar disorder, standard treatment with antipsychotic medications can be a double-edged sword. While these drugs help regulate brain chemistry, they often cause metabolic side effects such as insulin resistance and obesity, which are distressing enough that many patients stop taking the medications.
Now, a pilot study led by Stanford Medicine researchers has found that a ketogenic diet not only restores metabolic health in these patients as they continue their medications, but it further improves their psychiatric conditions. The results, published March 27 in Psychiatry Research , suggest that a dietary intervention can be a powerful aid in treating mental illness.
“It’s very promising and very encouraging that you can take back control of your illness in some way, aside from the usual standard of care,” said Shebani Sethi , MD, associate professor of psychiatry and behavioral sciences and the first author of the new paper.
Making the connection
Sethi, who is board certified in obesity and psychiatry, remembers when she first noticed the connection. As a medical student working in an obesity clinic, she saw a patient with treatment-resistant schizophrenia whose auditory hallucinations quieted on a ketogenic diet.
That prompted her to dig into the medical literature. There were only a few, decades-old case reports on using the ketogenic diet to treat schizophrenia, but there was a long track record of success in using ketogenic diets to treat epileptic seizures.
“The ketogenic diet has been proven to be effective for treatment-resistant epileptic seizures by reducing the excitability of neurons in the brain,” Sethi said. “We thought it would be worth exploring this treatment in psychiatric conditions.”
A few years later, Sethi coined the term metabolic psychiatry, a new field that approaches mental health from an energy conversion perspective.

Shebani Sethi
In the four-month pilot trial, Sethi’s team followed 21 adult participants who were diagnosed with schizophrenia or bipolar disorder, taking antipsychotic medications, and had a metabolic abnormality — such as weight gain, insulin resistance, hypertriglyceridemia, dyslipidemia or impaired glucose tolerance. The participants were instructed to follow a ketogenic diet, with approximately 10% of the calories from carbohydrates, 30% from protein and 60% from fat. They were not told to count calories.
“The focus of eating is on whole non-processed foods including protein and non-starchy vegetables, and not restricting fats,” said Sethi, who shared keto-friendly meal ideas with the participants. They were also given keto cookbooks and access to a health coach.
The research team tracked how well the participants followed the diet through weekly measures of blood ketone levels. (Ketones are acids produced when the body breaks down fat — instead of glucose — for energy.) By the end of the trial, 14 patients had been fully adherent, six were semi-adherent and only one was non-adherent.
The participants underwent a variety of psychiatric and metabolic assessments throughout the trial.
Before the trial, 29% of the participants met the criteria for metabolic syndrome, defined as having at least three of five conditions: abdominal obesity, elevated triglycerides, low HDL cholesterol, elevated blood pressure and elevated fasting glucose levels. After four months on a ketogenic diet, none of the participants had metabolic syndrome.
On average, the participants lost 10% of their body weight; reduced their waist circumference by 11% percent; and had lower blood pressure, body mass index, triglycerides, blood sugar levels and insulin resistance.
“We’re seeing huge changes,” Sethi said. “Even if you’re on antipsychotic drugs, we can still reverse the obesity, the metabolic syndrome, the insulin resistance. I think that’s very encouraging for patients.”
The participants reported improvements in their energy, sleep, mood and quality of life.
The psychiatric benefits were also striking. On average, the participants improved 31% on a psychiatrist rating of mental illness known as the clinical global impressions scale, with three-quarters of the group showing clinically meaningful improvement. Overall, the participants also reported better sleep and greater life satisfaction.
“The participants reported improvements in their energy, sleep, mood and quality of life,” Sethi said. “They feel healthier and more hopeful.”
The researchers were impressed that most of the participants stuck with the diet. “We saw more benefit with the adherent group compared with the semi-adherent group, indicating a potential dose-response relationship,” Sethi said.

Alternative fuel for the brain
There is increasing evidence that psychiatric diseases such as schizophrenia and bipolar disorder stem from metabolic deficits in the brain, which affect the excitability of neurons, Sethi said.
The researchers hypothesize that just as a ketogenic diet improves the rest of the body’s metabolism, it also improves the brain’s metabolism.
“Anything that improves metabolic health in general is probably going to improve brain health anyway,” Sethi said. “But the ketogenic diet can provide ketones as an alternative fuel to glucose for a brain with energy dysfunction.”
Likely there are multiple mechanisms at work, she added, and the main purpose of the small pilot trial is to help researchers detect signals that will guide the design of larger, more robust studies.
As a physician, Sethi cares for many patients with both serious mental illness and obesity or metabolic syndrome, but few studies have focused on this undertreated population.
She is the founder and director of the metabolic psychiatry clinic at Stanford Medicine.
“Many of my patients suffer from both illnesses, so my desire was to see if metabolic interventions could help them,” she said. “They are seeking more help. They are looking to just feel better.”
Researchers from the University of Michigan; the University of California, San Francisco; and Duke University contributed to the study.
The study was supported by Baszucki Group Research Fund, the Kuen Lau Fund and the Obesity Treatment Foundation.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Artificial intelligence
Exploring ways AI is applied to health care

Constant customer Assistance
- Admission/Application Essay
- Annotated Bibliography
- Argumentative Essay
- Book Report Review
- Dissertation
Reset password
Email not found.
Customer Reviews
offers a great selection of professional essay writing services. Take advantage of original, plagiarism-free essay writing. Also, separate editing and proofreading services are available, designed for those students who did an essay and seek professional help with polishing it to perfection. In addition, a number of additional essay writing services are available to boost your customer experience to the maximum!
Advanced writer
Add more quality to your essay or be able to obtain a new paper within a day by requesting a top or premium writer to work on your order. The option will increase the price of your order but the final result will be totally worth it.
Top order status
Every day, we receive dozens of orders. To process every order, we need time. If you’re in a great hurry or seek premium service, then choose this additional service. As a result, we’ll process your order and assign a great writer as soon as it’s placed. Maximize your time by giving your order a top status!
SMS updates
Have you already started to write my essay? When it will be finished? If you have occasional questions like that, then opt-in for SMS order status updates to be informed regarding every stage of the writing process. If you’re pressed for time, then we recommend adding this extra to your order.
Plagiarism report
Is my essay original? How do I know it’s Turnitin-ready? Very simple – order us to attach a detailed plagiarism report when work is done so you could rest assured the paper is authentic and can be uploaded to Turnitin without hesitating.
1-page summary
World’s peace isn’t riding on essay writing. If you don’t have any intent on reading the entire 2000-word essay that we did for you, add a 1-page summary to your order, which will be a short overview of your essay one paragraph long, just to be in the loop.

Finished Papers

Customer Reviews
First, you have to sign up, and then follow a simple 10-minute order process. In case you have any trouble signing up or completing the order, reach out to our 24/7 support team and they will resolve your concerns effectively.
Customer Reviews
- Member Login
- How it Works
- Top Writers
- Terms & conditions
- Privacy policy
- Referral program
From a high school essay to university term paper or even a PHD thesis


We are inclined to write as per the instructions given to you along with our understanding and background research related to the given topic. The topic is well-researched first and then the draft is being written.
- Article Sample
- Terms & Conditions
- Privacy Policy

Know Us Better
- Knowledge Base
- Referencing Styles
- Know Our Consultance
- Revision and Refund Policy
- Terms Of Use
We do not tolerate any form of plagiarism and use modern software to detect any form of it
Customer Reviews
Finished Papers
Some FAQs related to our essay writer service
Our Service Is Kept Secret
We are here to help you with essays and not to expose your identity. Your anonymity is our priority as we know it is yours. No personal data is collected on our service and no third parties can snoop through your info. All our communication is encrypted and stays between you and your writer. You receive your work via email so no one will have access to it except you. We also use encrypted payment systems with secure gateways for extra security.
Finished Papers
Rebecca Geach

What We Guarantee
- No Plagiarism
- On Time Delevery
- Privacy Policy
- Complaint Resolution

Finished Papers

How can I be sure you will write my paper, and it is not a scam?
DRE #01103083
Finished Papers
Gain efficiency with my essay writer. Hire us to write my essay for me with our best essay writing service!
Enhance your writing skills with the writers of penmypaper and avail the 20% flat discount, using the code ppfest20.
Need a personal essay writer? Try EssayBot which is your professional essay typer.
- EssayBot is an essay writing assistant powered by Artificial Intelligence (AI).
- Given the title and prompt, EssayBot helps you find inspirational sources, suggest and paraphrase sentences, as well as generate and complete sentences using AI.
- If your essay will run through a plagiarism checker (such as Turnitin), don’t worry. EssayBot paraphrases for you and erases plagiarism concerns.
- EssayBot now includes a citation finder that generates citations matching with your essay.

Customer Reviews
- Admission/Application Essay
- Annotated Bibliography
- Argumentative Essay
- Book Report Review
- Dissertation

IMAGES
VIDEO
COMMENTS
The Case: Darius is a 27-year-old man who has just been admitted to your inpatient service team. This is Darius' fourth admission in the past 2 years, but first in nearly 11 months. Darius was working most recently at a big box retailer stocking shelves but has had to leave his job over the past month.
At least one of these must be (1), (2), or (3): Delusions. Hallucinations. Disorganized speech (e.g., frequent derailment or incoherence). Grossly disorganized or catatonic behavior. Negative symptoms (i.e., diminished emotional expression or avolition). Decreased functioning 2.6 months of symptoms with 1 month meeting criterion A. 3.Not ...
Schizophrenia. Unfolding Case Study By Amanda Eymard , DNS, RN and Linda Manfrin-Ledet , DNS, APRN. Assigned Reading to be completed prior to case study. Prior to conducting this unfolding case study, students should read the following: 3.83k views • 82 slides. Schizophrenia. Schizophrenia. Lecture of 2-14-07. Symptoms.
Introduction. Schizophrenia is a chronic severe mental illness with heterogeneous clinical profile and debilitating course. Research shows that clinical features, severity of illness, prognosis, and treatment of schizophrenia vary depending on the age of onset of illness.[1,2] Hence, age-specific research in schizophrenia has been emphasized.Although consistency has been noted in ...
Schizophrenia is a chronic and severe mental disorder characterized by distortions in thinking, perception, emotions, language, sense of self, and behaviour. This report presents the role of clinical pharmacists in the management of a patient diagnosed with schizophrenia with symptoms of paranoia. A gainfully employed young African male adult reported to be roaming around town moving from one ...
predominance. Schizophrenia is socioeconomic burden with suicidal rate of 10% and expense of .021.65% o- f GDP spent on treatment. -morbid factors associated with Other co Schizophrenia are diabetes, Obesity, HIV infection many metabolic disorders etc. Clinically, schizophrenia is a syndrome of variables symptoms, but profoundly disruptive,
Case Study On Schizophrenia Slideshare - Emilie Nilsson #11 in Global Rating ID 19300. 4.7/5. I accept. REVIEWS HIRE. 26 Customer reviews. 100% Success rate 4.8. Case Study On Schizophrenia Slideshare: 12 Customer reviews. Affiliate program. Refer our service to your friend ...
A small clinical trial led by Stanford Medicine found that the metabolic effects of a ketogenic diet may help stabilize the brain. April 1, 2024 - By Nina Bai. A study led by researchers at Stanford Medicine showed that diet can help those with serious mental illness. nishihata. For people living with serious mental illness like schizophrenia ...
Case Study On Schizophrenia Slideshare. 7 Customer reviews. ID 4817. We value democratic peace and support Ukraine in its fight for freedom and democratic development. We also encourage you to support Ukraine in its defense of democracy by donating at #StandWithUkraine. 1 (888)814-4206 1 (888)499-5521.
1404Orders prepared. Feb 22, 2021. Case Study On Schizophrenia Slideshare, Cheap University Essay Writing Services Au, Essay On Goddess Durga, Professional Admission Paper Editing Service Us, Aim Of Case Study Method, Write A Essay Who Is Jesus, Literature Review Computer Science Research. Business and Finance.
Case Study On Schizophrenia Slideshare - 26 Customer reviews. Give Yourself up to Extra Pleasures. Total orders: 9156. Direct communication with a writer. Our writers always follow the customers' requirements very carefully. Level: Master's, University, College, PHD, High School, Undergraduate. 4629 Orders prepared. THREE. Services .
Schizophrenia Case Study Slideshare, Popular Literature Review Proofreading For Hire, Popular College Biography Topics, Thesis About Financial Literacy In The Philippines, Help With Marketing Research Paper, Parts Of Speech In Diagram, How To Keep From Getting Depressed
Now the customer can delegate any service and it will be carried out in the best possible way. Writing essays, abstracts and scientific papers also falls into this category and can be done by another person. In order to use this service, the client needs to ask the professor about the topic of the text, special design preferences, fonts and ...
View Property. ID 10820. Case Study On Schizophrenia Slideshare, Religion And Peace Hsc Essay, Kimberleigh Zolciak Resume, 31 Contest Essay May, Apa Paper Numbering, Essay Formalia Hhu, Cheap Cv Writer For Hire For School. ©2022 .
San Francisco CA 94123. 1 (888)814-4206 1 (888)499-5521. Feb 07, 2021. Package Plan. Social Sciences. REVIEWS.
The writers of PenMyPaper have got a vast knowledge about various academic domains along with years of work experience in the field of academic writing. Thus, be it any kind of write-up, with multiple requirements to write with, the essay writer for me is sure to go beyond your expectations. Some most explored domains by them are: Healthcare. Law.
Case Study On Schizophrenia Slideshare - EssayService uses secured cookies. Read more. Health Category. THREE. 4.8/5. Nursing Business and Economics Management Healthcare +108. 13 Customer reviews. Case Study On Schizophrenia Slideshare: Harry. Level: College, University, Master's, High School, PHD, Undergraduate.