An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Diabetes Spectr
- v.34(4); 2021 Nov


Literature Review of Type 2 Diabetes Management and Health Literacy
The purpose of this literature review was to identify educational approaches addressing low health literacy for people with type 2 diabetes. Low health literacy can lead to poor management of diabetes, low engagement with health care providers, increased hospitalization rates, and higher health care costs. These challenges can be even more profound among minority populations and non-English speakers in the United States.
A literature search and standard data extraction were performed using PubMed, Medline, and EMBASE databases. A total of 1,914 articles were identified, of which 1,858 were excluded based on the inclusion criteria, and 46 were excluded because of a lack of relevance to both diabetes management and health literacy. The remaining 10 articles were reviewed in detail.
Patients, including ethnic minorities and non-English speakers, who are engaged in diabetes education and health literacy improvement initiatives and ongoing follow-up showed significant improvement in A1C, medication adherence, medication knowledge, and treatment satisfaction. Clinicians considering implementing new interventions to address diabetes care for patients with low health literacy can use culturally tailored approaches, consider ways to create materials for different learning styles and in different languages, engage community health workers and pharmacists to help with patient education, use patient-centered medication labels, and engage instructors who share cultural and linguistic similarities with patients to provide educational sessions.
This literature review identified a variety of interventions that had a positive impact on provider-patient communication, medication adherence, and glycemic control by promoting diabetes self-management through educational efforts to address low health literacy.
Diabetes is the seventh leading cause of death in the United States, and 30.3 million Americans, or 9.4% of the U.S. population, are living with diabetes ( 1 , 2 ). For successful management of a complicated condition such as diabetes, health literacy may play an important role. Low health literacy is a well-documented barrier to diabetes management and can lead to poor management of medical conditions, low engagement with health care providers (HCPs), increased hospitalizations, and, consequently, higher health care costs ( 3 – 5 ).
The Healthy People 2010 report ( 6 ) defined health literacy as the “degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” Diabetes health literacy also encompasses a wide range of skills, including basic knowledge of the disease state, self-efficacy, glycemic control, and self-care behaviors, which are all important components of diabetes management ( 3 – 5 , 7 ). According to the Institute of Medicine’s Committee on Health Literacy, patients with poor health literacy are twice as likely to have poor glycemic control and were found to be twice as likely to be hospitalized as those with adequate health literacy ( 8 ). Associations between health literacy and health outcomes have been reported in many studies, the first of which was conducted in 1995 in two public hospitals and found that many patients had inadequate health literacy and could not perform the basic reading tasks necessary to understand their treatments and diagnoses ( 9 ).
Evaluation of health literacy is vital to the management and understanding of diabetes. Several tools for assessing health literacy have been evaluated, and the choice of which to use depends on the length of the patient encounter and the desired depth of the assessment. One widely used literacy assessment tool, the Test of Functional Health Literacy in Adults (TOFHLA), consists of 36 comprehension questions and four numeric calculations ( 10 ). Additional tools that assess patients’ reading ability include the Rapid Estimate of Adult Literacy in Medicine (REALM) and the Literacy Assessment for Diabetes. Tests that assess diabetes numeracy skills include the Diabetes Numeracy Test, the Newest Vital Sign (NVS), and the Single-Item Literacy Screener (SILS) ( 11 ).
Rates of both diabetes and low health literacy are higher in populations from low socioeconomic backgrounds ( 5 , 7 , 12 ). People living in disadvantaged communities face many barriers when seeking health care, including inconsistent housing, lack of transportation, financial difficulties, differing cultural beliefs about health care, and mistrust of the medical professions ( 13 , 14 ). People with high rates of medical mistrust tend to be less engaged in their care and to have poor communication with HCPs, which is another factor HCPs need to address when working with their patients with diabetes ( 15 ).
The cost of medical care for people with diabetes was $327 billion in 2017, a 26% increase since 2012 ( 1 , 16 ). Many of these medical expenditures are related to hospitalization and inpatient care, which accounts for 30% of total medical costs for people with diabetes ( 16 ).
People with diabetes also may neglect self-management tasks for various reasons, including low health literacy, lack of diabetes knowledge, and mistrust between patients and HCPs ( 7 , 15 ).
These challenges can be even more pronounced in vulnerable populations because of language barriers and patient-provider mistrust ( 17 – 19 ). Rates of diabetes are higher among racial and ethnic minority groups; 15.1% of American Indians and Alaskan Natives, 12.7% of Non-Hispanic Blacks, 12.1% of Hispanics, and 8% of Asian Americans have diagnosed diabetes, compared with 7.4% of non-Hispanic Whites ( 1 ). Additionally, patient-provider relationship deficits can be attributed to challenges with communication, including HCPs’ lack of attention to speaking slowly and clearly and checking for patients’ understanding when providing education or gathering information from people who speak English as a second language ( 15 ). White et al. ( 15 ) demonstrated that patients with higher provider mistrust felt that their provider’s communication style was less interpersonal and did not feel welcome as part of the decision-making process.
To the authors’ knowledge, there is no current literature review evaluating interventions focused on health literacy and diabetes management. There is a pressing need for such a comprehensive review to provide a framework for future intervention design. The objective of this literature review was to gather and summarize studies of health literacy–based diabetes management interventions and their effects on overall diabetes management. Medication adherence and glycemic control were considered secondary outcomes.
Research Design and Methods
Search strategy.
A literature review was conducted using the PubMed, Medline, and EMBASE databases. Search criteria included articles published between 2015 and 2020 to identify the most recent studies on this topic. The search included the phrases “diabetes” and “health literacy” to specifically focus on health literacy and diabetes management interventions and was limited to original research conducted in humans and published in English within the defined 5-year period. Search results were exported to Microsoft Excel for evaluation.
Study Selection
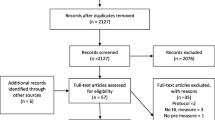
Initial screening of the articles’ abstracts was conducted using the selection criteria to determine which articles to include or exclude ( Figure 1 ). The initial search results were reviewed for the following inclusion criteria: original research (clinical trials, cohort studies, and cross-sectional studies) conducted in human subjects with type 2 diabetes in the United States, and published in English between 2015 and 2020. Articles were considered to be relevant if diabetes was included as a medical condition in the study and an intervention was made to assess or improve health literacy. Studies involving type 1 diabetes or gestational diabetes and articles that were viewpoints, population surveys, commentaries, case reports, reviews, or reports of interventions conducted outside of the United States were excluded from further review. The criteria requiring articles to be from the past 5 years and from the United States were used because of the unique and quickly evolving nature of the U.S. health care system. Articles published more than 5 years ago or from other health care systems may have contributed information that was not applicable to or no longer relevant for HCPs in the United States. Articles were screened and reviewed independently by both authors. Disagreements were resolved through discussion to create the final list of articles for inclusion.

PRISMA diagram of the article selection process.
Data Extraction
A standard data extraction was performed for each included article to obtain information including author names, year of publication, journal, study design, type of intervention, primary outcome, tools used to assess health literacy or type 2 diabetes knowledge, and effects of intervention on overall diabetes management, glycemic control, and medication adherence.
A total of 1,914 articles were collected from a search of the PubMed, MEDLINE, and EMBASE databases, of which 1,858 were excluded based on the inclusion and exclusion criteria. Of the 56 articles that met criteria for abstract review, 46 were excluded because of a lack of relevance to both diabetes management and health literacy. The remaining 10 studies identified various diabetes management interventions, including diabetes education tools such as electronic medication instructions and text message–based interventions, technology-based education videos, enhanced prescription labels, learner-based education materials, and culturally tailored interventions ( 15 , 20 – 28 ). Figure 1 shows the PRISMA diagram of the article selection process, and Table 1 summarizes the findings of the article reviews ( 15 , 20 – 28 ).
Findings of the Article Reviews (15,20–28)
SAHLSA, Short Assessment of Health Literacy for Spanish Adults.
Medical mistrust and poor communication are challenging variables in diabetes education. White et al. ( 15 ) examined the association between communication quality and medical mistrust in patients with type 2 diabetes. HCPs at five health department clinics received training in effective health communication and use of the PRIDE (Partnership to Improve Diabetes Education) toolkit in both English and Spanish, whereas control sites were only exposed to National Diabetes Education Program materials without training in effective communication. The study evaluated participant communication using several tools, including the Communication Assessment Tool (CAT), Interpersonal Processes of Care (IPC-18), and the Short Test of Functional Health Literacy in Adults (s-TOFHLA). The authors found that higher levels of mistrust were associated with lower CAT and IPC-18 scores.
Patients with type 2 diabetes are also likely to benefit from personalized education delivery tools such as patient-centered labeling (PCL) of prescription drugs, learning style–based education materials, and tailored text messages ( 24 , 25 , 27 ). Wolf et al. ( 27 ) investigated the use of PCL in patients with type 2 diabetes and found that patients with low health literacy who take medication two or more times per day have higher rates of proper medication use when using PCL (85.9 vs. 77.4%, P = 0.03). The objective of the PCL intervention was to make medication instructions and other information on the labels easier to read to improve medication use and adherence rates. The labels incorporated best-practice strategies introduced by the Institute of Medicine for the Universal Medication Schedule. These strategies prioritize medication information, use of larger font sizes, and increased white space. Of note, the benefits of PCL were largely seen with English speakers. Spanish speakers did not have substantial improvement in medication use or adherence, which could be attributed to language barriers ( 27 ).
Nelson et al. ( 25 ) analyzed patients’ engagement with an automated text message approach to supporting diabetes self-care activities in a 12-month randomized controlled trial (RCT) called REACH (Rapid Education/Encouragement and Communications for Health) ( 25 ). Messages were tailored based on patients’ medication adherence, the Information-Motivation-Behavioral Skills model of health behavior change, and self-care behaviors such as diet, exercise, and self-monitoring of blood glucose. Patients in this trial were native English speakers, so further research to evaluate the impact of the text message intervention in patients with limited English language skills is still needed. However, participants in the intervention group reported higher engagement with the text messages over the 12-month period ( 25 ).
Patients who receive educational materials based on their learning style also show significant improvement in their diabetes knowledge and health literacy. Koonce et al. ( 24 ) developed and evaluated educational materials based on patients’ learning style to improve health literacy in both English and Spanish languages. The materials were made available in multiple formats to target four different learning styles, including materials for visual learners, read/write learners, auditory learners, and kinesthetic learners. Spanish-language versions were also available. Researchers were primarily interested in measuring patients’ health literacy and knowledge of diabetes. The intervention group received materials in their preferred learning style and language, whereas the control group received standard of care education materials. The intervention group showed significant improvement in diabetes knowledge and health literacy, as indicated by Diabetes Knowledge Test (DKT) scores. More participants in the intervention group reported looking up information about their condition during week 2 of the intervention and showed an overall improvement in understanding symptoms of nerve damage and types of food used to treat hypoglycemic events. However, the study had limited enrollment of Spanish speakers, making the applicability of the results to Spanish-speaking patients highly variable.
Additionally, findings by Hofer et al. ( 22 ) suggest that patients with high A1C levels may benefit from interventions led by community health workers (CHWs) to bridge gaps in health literacy and equip patients with the tools to make health decisions. In this study, Hispanic and African American patients with low health literacy and diabetes not controlled by oral therapy benefited from education sessions led by CHWs. The CHWs led culturally tailored support groups to compare the effects of educational materials provided in an electronic format (via iDecide) and printed format on medication adherence and self-efficacy. The study found increased adherence with both formats, and women, specifically, had a significant increase in medication adherence and self-efficacy. One of the important aspects of this study was that the CHWs shared cultural and linguistic characteristics with the patients and HCPs, leading to increased trust and satisfaction with the information presented ( 22 ).
Kim et al. ( 23 ) found that Korean-American participants benefited greatly from group education sessions that provided integrated counseling led by a team of nurses and CHW educators. The intervention also had a health literacy component that focused on enhancing skills such as reading food package labels, understanding medical terminology, and accessing health care services. This intervention led to a significant reduction of 1–1.3% in A1C levels in the intervention group. The intervention established the value of collaboration between CHW educators and nurses to improve health information delivery and disease management.
A collaboration between CHW educators and pharmacists was also shown to reinforce diabetes knowledge and improve health literacy. Sharp et al. ( 26 ) conducted a cross-over study in four primary care ambulatory clinics that provided care for low-income patients. The study found that patients with low health literacy had more visits with pharmacists and CHWs than those with high health literacy. The CHWs provided individualized support to reinforce diabetes self-management education and referrals to resources such as food, shelter, and translation services. The translation services in this study were especially important for building trust with non-English speakers and helping patients understand their therapy. Similar to other studies, the CHWs shared cultural and linguistic characteristics with their populations, which helped to overcome communication-related and cultural barriers ( 23 , 26 ).
The use of electronic tools or educational videos yielded inconclusive results with regard to medication adherence. Graumlich et al. ( 20 ) implemented a new medication planning tool called Medtable within an electronic medical record system in several outpatient clinics serving patients with type 2 diabetes. The tool was designed to organize medication review and patient education. Providers can use this tool to search for medication instructions and actionable language that are appropriate for each patient’s health literacy level. The authors found no changes in medication knowledge or adherence, but the intervention group reported higher satisfaction. On the other hand, Yeung et al. ( 28 ) showed that pharmacist-led online education videos accessed using QR codes affixed to the patients’ medication bottles and health literacy flashcards increased patients’ medication adherence in an academic medical hospital.
Goessl et al. ( 21 ) found that patients with low health literacy had significantly higher retention of information when receiving evidence-based diabetes education through a DVD recording than through an in-person group class. This 18-month RCT randomized participants to either the DVD or in-person group education and assessed their information retention through a teach-back strategy. The curriculum consisted of diabetes prevention topics such as physical exercise, food portions, and food choices. Participants in the DVD group had significantly higher retention of information than those in the control (in-person) group. The authors suggested this may have been because participants in the DVD group have multiple opportunities to review the education material.
Management of type 2 diabetes remains a challenge for HCPs and patients, in part because of the challenges discussed in this review, including communication barriers between patients and HCPs and knowledge deficits about medications and disease states ( 29 ). HCPs can have a positive impact on the health outcomes of their patients with diabetes by improving patients’ disease state and medication knowledge.
One of the common themes identified in this literature review was the prevalence of culturally tailored diabetes education interventions. This is an important strategy that could improve diabetes outcomes and provide an alternative approach to diabetes self-management education when working with patients from culturally diverse backgrounds. HCPs might benefit from using culturally tailored educational approaches to improve communication with patients and overcome the medical mistrust many patients feel. Although such mistrust was not directly correlated with diabetes management, it was noted that patients who feel mistrustful tend to have poor communication with HCPs ( 20 ). Additionally, Latino/Hispanic patients who have language barriers tend to have poor glycemic control ( 19 ). Having CHWs work with HCPs might mitigate some patient-provider communication barriers. As noted earlier, CHWs who share cultural and linguistic characteristics with their patient populations have ongoing interactions and more frequent one-on-one encounters ( 12 ).
Medication adherence and glycemic control are important components of diabetes self-management, and we noted that the integration of CHWs into the diabetes health care team and the use of simplified medication label interventions were both successful in improving medication adherence ( 23 , 24 ). The use of culturally tailored education sessions and the integration of pharmacists and CHWs into the management of diabetes appear to be successful in reducing A1C levels ( 12 , 26 ). Electronic education tools and educational videos alone did not have an impact on medication knowledge or information retention in patients with low health literacy, but a combination of education tools and individualized sessions has the potential to improve diabetes medication knowledge and overall self-management ( 20 , 22 , 30 ).
There were several limitations to our literature review. We restricted our search criteria to articles published in English and studies conducted within the United States to ensure that the results would be relevant to U.S. HCPs. However, these limitations may have excluded important work on this topic. Additional research expanding this search beyond the United States and including articles published in other languages may demonstrate different outcomes. Additionally, this literature review did not focus on A1C as the primary outcome, although A1C is an important indicator of diabetes self-management. A1C was chosen as the method of evaluating the impact of health literacy interventions in patients with diabetes, but other considerations such as medication adherence, impact on comorbid conditions, and quality of life are also important factors.
The results of this work show that implementing health literacy interventions to help patients manage type 2 diabetes can have beneficial results. However, such interventions can have significant time and monetary costs. The potential financial and time costs of diabetes education interventions were not evaluated in this review and should be taken into account when designing interventions. The American Diabetes Association estimated the cost of medical care for people with diabetes to be $327 billion in 2017, with the majority of the expenditure related to hospitalizations and nursing home facilities ( 16 ). Another substantial cost of diabetes that can be difficult to measure is treatment for comorbid conditions and complications such as cardiovascular and renal diseases.
Interventions designed to address low health literacy and provide education about type 2 diabetes could be a valuable asset in preventing complications and reducing medical expenditures. Results of this work show that clinicians who are considering implementing new interventions may benefit from the following strategies: using culturally tailored approaches, creating materials for different learning styles and in patients’ languages, engaging CHWs and pharmacists to help with patient education, using PCLs for medications, and engaging education session instructors who share patients’ cultural and linguistic characteristics.
Diabetes self-management is crucial to improving health outcomes and reducing medical costs. This literature review identified interventions that had a positive impact on provider-patient communication, medication adherence, and glycemic control by promoting diabetes self-management through educational efforts to address low health literacy. Clinicians seeking to implement diabetes care and education interventions for patients with low health literacy may want to consider drawing on the strategies described in this article. Providing culturally sensitive education that is tailored to patients’ individual learning styles, spoken language, and individual needs can improve patient outcomes and build patients’ trust.
Article Information
Duality of interest.
No potential conflicts of interest relevant to this article were reported.
Author Contributions
Both authors conceptualized the literature review, developed the methodology, analyzed the data, and wrote, reviewed, and edited the manuscript. R.A. collected the data. K.M. supervised the review. K.M. is the guarantor of this work and, as such, has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
Portions of this research were presented at the Washington State University College of Pharmacy and Pharmaceutical Sciences Honors Research Day in April 2019.
Literature Review of Type 2 Diabetes Management and Health Literacy
Affiliation.
- 1 Washington State University College of Pharmacy and Pharmaceutical Sciences, Spokane, WA.
- PMID: 34866874
- PMCID: PMC8603116
- DOI: 10.2337/ds21-0014
Objective: The purpose of this literature review was to identify educational approaches addressing low health literacy for people with type 2 diabetes. Low health literacy can lead to poor management of diabetes, low engagement with health care providers, increased hospitalization rates, and higher health care costs. These challenges can be even more profound among minority populations and non-English speakers in the United States.
Methods: A literature search and standard data extraction were performed using PubMed, Medline, and EMBASE databases. A total of 1,914 articles were identified, of which 1,858 were excluded based on the inclusion criteria, and 46 were excluded because of a lack of relevance to both diabetes management and health literacy. The remaining 10 articles were reviewed in detail.
Results: Patients, including ethnic minorities and non-English speakers, who are engaged in diabetes education and health literacy improvement initiatives and ongoing follow-up showed significant improvement in A1C, medication adherence, medication knowledge, and treatment satisfaction. Clinicians considering implementing new interventions to address diabetes care for patients with low health literacy can use culturally tailored approaches, consider ways to create materials for different learning styles and in different languages, engage community health workers and pharmacists to help with patient education, use patient-centered medication labels, and engage instructors who share cultural and linguistic similarities with patients to provide educational sessions.
Conclusion: This literature review identified a variety of interventions that had a positive impact on provider-patient communication, medication adherence, and glycemic control by promoting diabetes self-management through educational efforts to address low health literacy.
© 2021 by the American Diabetes Association.
Advertisement
Health literacy in type 2 diabetes patients: a systematic review of systematic reviews
- Review Article
- Published: 11 November 2017
- Volume 55 , pages 1–12, ( 2018 )
Cite this article
- Rosario Caruso 1 ,
- Arianna Magon 1 ,
- Irene Baroni 1 ,
- Federica Dellafiore 1 ,
- Cristina Arrigoni 2 ,
- Francesco Pittella 3 &
- Davide Ausili ORCID: orcid.org/0000-0001-5212-6463 4
8275 Accesses
83 Citations
18 Altmetric
Explore all metrics
Aim To summarize, critically review, and interpret the evidence related to the systematic reviews on health literacy (HL) amongst type 2 diabetes mellitus (T2DM). Methods The methodology for this study consisted of a systematic review of systematic reviews, using the PRISMA statement and flowchart to select studies, and searching on PubMed, CINAHL, Scopus, and Cochrane. The search covered the period between January 2006 and June 2016. Results From the 115 identified record by the queries, only six systematic reviews were included, following a quality evaluation using AMSTAR. The included systematic reviews content was analyzed by the independent work of two authors, using a narrative synthesis approach. The findings of this study (i.e., main themes) are areas of consensus and gaps in knowledge. Areas of consensus are HL definition, HL measurement tools, and the relationship between T2DM patient knowledge (or literacy) and his/her HL. The gaps in knowledge were the assessment of the relations between HL and health outcomes and self-efficacy, the gender differences, the effectiveness of interventions to improve HL, the cost-effectiveness study of interventions to improve HL, and the understanding of the influence of organizational environment on HL. Conclusion This review provides a current state of knowledge to address clinical practice and research proposals. HL could be useful to personalize patients' follow-up and it should be routinely assessed in its three dimensions (i.e. functional, interactive and critical) to enhance patients' ability to cope with clinical recommendations. Future research should be mainly aimed to test the effectiveness of evidence-based interventions to improve HL amongst T2DM patients.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Hospital falls prevention with patient education: a scoping review
Hazel Heng, Dana Jazayeri, … Meg E. Morris
Establishing the efficacy of interventions to improve health literacy and health behaviours: a systematic review
Ronie Walters, Stephen J. Leslie, … Trish Gorely


Understanding the role of the paramedic in primary care: a realist review
Georgette Eaton, Geoff Wong, … Kamal R. Mahtani
IDF (2015) IDF Diabetes Atlas 7th edn., vol 144. http://www.diabetesatlas.org/
Ogurtsova K, da Rocha Fernandes JD, Huang Y et al (2017) IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 128:40–50. https://doi.org/10.1016/j.diabres.2017.03.024
Article CAS PubMed Google Scholar
Guariguata L, Whiting DR, Hambleton I et al (2014) Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 103:137–149. https://doi.org/10.1016/j.diabres.2013.11.002
Ausili D, Bulgheroni M, Ballatore P et al (2017) Self-care, quality of life and clinical outcomes of type 2 diabetes patients: an observational cross-sectional study. Acta Diabetol. https://doi.org/10.1007/s00592-017-1035-5
Google Scholar
Eichler K, Wieser S, Brügger U (2009) The costs of limited health literacy: a systematic review. Int J Public Health 54:313–324. https://doi.org/10.1007/s00038-009-0058-2
Article PubMed PubMed Central Google Scholar
Al Sayah F, Johnson ST, Vallance J (2016) Health literacy, pedometer, and self-reported walking among older adults. Am J Public Health 106:327–333. https://doi.org/10.2105/AJPH.2015.302901
Article PubMed Google Scholar
Osborn CY, Cavanaugh K, Wallston KA, Rothman RL (2010) Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun 15:146–158. https://doi.org/10.1080/10810730.2010.499980
Hamer S, Collinson G (2014) Achieving evidence-based practice: a handbook for practitioners, 2nd edn. Elsevier, Amsterdam
Friis K, Lasgaard M, Osborne RH, Maindal HT (2016) Gaps in understanding health and engagement with healthcare providers across common long-term conditions: a population survey of health literacy in 29 473 Danish citizens. BMJ Open 6:e009627. https://doi.org/10.1136/BMJOPEN-2015-009627
Powell CK, Hill EG, Clancy DE (2007) The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ 33:144–151. https://doi.org/10.1177/0145721706297452
Rothman RL, DeWalt DA, Malone R et al (2004) Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. Jama 292:552–557. https://doi.org/10.1001/JAMA.292.14.1711
Article Google Scholar
Loke YK, Hinz I, Wang X, Salter C (2012) Systematic review of consistency between adherence to cardiovascular or diabetes medication and health literacy in older adults. Ann Pharmacother 46:863–872. https://doi.org/10.1345/aph.1Q718
Nielsen-Bohlman L, Panzer AM, Kindig DA (2004) Health literacy. National Academies Press, Washington, DC. https://doi.org/10.17226/10883
Nutbeam D (2008) The evolving concept of health literacy. Soc Sci Med 67:2072–2078. https://doi.org/10.1016/j.socscimed.2008.09.050
Green JA, Mor MK, Shields AM et al (2013) Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. Am J Kidney Dis 62:73–80. https://doi.org/10.1053/j.ajkd.2012.12.014
Bailey SC, Brega AG, Crutchfield TM et al (2014) Update on health literacy and diabetes. Diabetes Educ 40:581–604. https://doi.org/10.1177/0145721714540220
McNaughton CD, Jacobson TA, Kripalani S (2014) Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Couns 96:165–170. https://doi.org/10.1016/j.pec.2014.05.007
Hahn EA, Burns JL, Jacobs EA et al (2015) Health literacy and patient-reported outcomes: a cross-sectional study of underserved English- and Spanish-speaking patients with type 2 diabetes. J Health Commun 20:4–15
Matsuoka S, Tsuchihashi-Makaya M, Kayane T et al (2016) Health literacy is independently associated with self-care behavior in patients with heart failure. Patient Educ Couns. https://doi.org/10.1016/j.pec.2016.01.003
PubMed Google Scholar
Ishikawa H, Takeuchi T, Yano E (2008) Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care 31:874–879. https://doi.org/10.2337/dc07-1932
Heisler M, Piette JD, Spencer M et al (2005) The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care 28:816–822. https://doi.org/10.2337/diacare.28.4.816
Asche C, LaFleur J, Conner C (2011) A review of diabetes treatment adherence and the association with clinical and economic outcomes. Clin Ther 33:74–109. https://doi.org/10.1016/j.clinthera.2011.01.019
Gao J, Wang J, Zheng P et al (2013) Effects of self-care, self-efficacy, social support on glycemic control in adults with type 2 diabetes. BMC Fam Pract 141(14):1090–1101. https://doi.org/10.1186/1471-2296-14-66
Caruso R, Arrigoni C, Magon A et al (2017) Health determinants in Italian type 2 diabetes mellitus (T2DM) patients: a critical gender differences analysis. J Res Gend Stud 7:93–108. https://doi.org/10.22381/JRGS7220176
Mårtensson L, Hensing G (2012) Health literacy—a heterogeneous phenomenon: a literature review. Scand J Caring Sci 26:151–160. https://doi.org/10.1111/j.1471-6712.2011.00900.x
Al Sayah F, Majumdar SR, Williams B et al (2013) Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med 28:444–452. https://doi.org/10.1007/s11606-012-2241-z
Smith V, Devane D, Begley CM, Clarke M (2011) Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol 111(11):1–7. https://doi.org/10.1186/1471-2288-11-15
Becker L, Oxman A (2008) Overviews of reviews. In: Higgins J, Green S (eds) Cochrane Handbook for Systematic Reviews of Interventions Cochrane B Series. Wiley, Chippenham, pp 607–631
Chapter Google Scholar
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Shea BJ, Grimshaw JM, Wells GA et al (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 71(7):1085–1086. https://doi.org/10.1186/1471-2288-7-10
Banerjee M, Capozzoli M, McSweeney L, Sinha D (1999) Beyond kappa: a review of interrater agreement measures. Can J Stat 27:3–23. https://doi.org/10.2307/3315487
Popay J, Roberts H, Sowden A (2006) Guidance on the conduct of narrative synthesis in systematic reviews. A Product from the ESRC Methods Programme. Institute for Health Research, Lancaster University, pp 1–92. http://www.lancaster.ac.uk/shm/research/nssr/research/dissemination/publications.php
Al Sayah F, Williams B, Johnson JA (2013) Measuring health literacy in individuals with diabetes: a systematic review and evaluation of available measures. Health Educ Behav 40:42–55. https://doi.org/10.1177/1090198111436341
Davey J, Holden CA, Smith BJ (2015) The correlates of chronic disease-related health literacy and its components among men: a systematic review. BMC Public Health 15:589. https://doi.org/10.1186/s12889-015-1900-5
Fransen MP, von Wagner C, Essink-Bot M-L (2012) Diabetes self-management in patients with low health literacy: ordering findings from literature in a health literacy framework. Patient Educ Couns 88:44–53. https://doi.org/10.1016/j.pec.2011.11.015
Nutbeam D (2000) Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int 15:259–267. https://doi.org/10.1093/heapro/15.3.259
Bandura A (2001) Social cognitive theory: an agentic perspective. Annu Rev Psychol 52:1–26. https://doi.org/10.1146/annurev.psych.52.1.1
Parschau L, Fleig L, Koring M et al (2013) Positive experience, self-efficacy, and action control predict physical activity changes: a moderated mediation analysis. Br J Health Psychol 18:395–406. https://doi.org/10.1111/j.2044-8287.2012.02099.x
Sarkar U, Fisher L, Schillinger D (2006) Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care 29:823–829. https://doi.org/10.2337/diacare.29.04.06.dc05-1615
Arrigoni C, Caruso R, Campanella F et al (2015) Investigating burnout situations, nurses’ stress perception and effect of a post-graduate education program in health care organizations of northern Italy: a multicenter study. G Ital Med Lav Ergon 37:39–45
Caruso R, Fida R, Sili A, Arrigoni C (2016) Towards an integrated model of nursing competence: an overview of the literature reviews and concept analysis. Prof Inferm 69:35–43. https://doi.org/10.7429/pi.2016.691035
Cavanaugh K, Huizinga M, Wallston K (2008) Association of numeracy and diabetes control. Ann Int 148:737–746. https://doi.org/10.7326/0003-4819-148-10-200805200-00006
Vassy JL, O’Brien KE, Waxler JL et al (2012) Impact of literacy and numeracy on motivation for behavior change after diabetes genetic risk testing. Med Decis Mak 32:606–615. https://doi.org/10.1177/0272989X11431608
White RO, DeWalt DA, Malone RM et al (2010) Leveling the field: addressing health disparities through diabetes disease management. Am J Manag Care 16:42–48
PubMed PubMed Central Google Scholar
Mbaezue N, Mayberry R, Gazmararian J et al (2010) The impact of health literacy on self-monitoring of blood glucose in patients with diabetes receiving care in an inner-city hospital. J Natl Med Assoc 102:5–9
Karter AJ, Subramanian U, Saha C et al (2010) Barriers to Insulin initiation. Diabetes Care 33:733–735. https://doi.org/10.2337/dc09-1184
Bains SS, Egede LE (2011) Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther 13:335–341. https://doi.org/10.1089/dia.2010.0160
Caruso R, Pittella F, Zaghini F et al (2016) Development and validation of the nursing profession self-efficacy scale. Int Nurs Rev 63:455–464. https://doi.org/10.1111/inr.12291
WHO (2015) Death and DALY estimates for 2004 by cause for WHO member states: persons, all ages. World Health Organization, Geneva
Baker P, Dworkin SL, Tong S et al (2014) The men’s health gap: men must be included in the global health equity agenda. Bull World Health Organ 92:618–620. https://doi.org/10.2471/BLT.13.132795
Kemppainen V, Tossavainen K, Turunen H (2013) Nurses’ roles in health promotion practice: an integrative review. Health Promot Int 28:490–501. https://doi.org/10.1093/heapro/das034
Whiting DR, Guariguata L, Weil C, Shaw J (2011) IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 94:311–321. https://doi.org/10.1016/j.diabres.2011.10.029
Download references
This study was funded by local research funds of the IRCCS Policlinico San Donato, a Clinical Research Hospital partially funded by the Italian Ministry of Health.
Author information
Authors and affiliations.
Health Professions Research and Development Unit, IRCCS Policlinico San Donato University Hospital, San Donato Milanese, MI, Italy
Rosario Caruso, Arianna Magon, Irene Baroni & Federica Dellafiore
Hygiene Section, Department of Public Health, Experimental and Forensic Medicine, University of Pavia, Pavia, Italy
Cristina Arrigoni
Nursing Degree Course, University of Milan, Section of IRCCS Policlinico San Donato University Hospital, San Donato Milanese, MI, Italy
Francesco Pittella
Department of Medicine and Surgery, University of Milano-Bicocca, Via Cadore 48, 20900, Monza, Italy
Davide Ausili
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Davide Ausili .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Human and animal rights
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
Not applicable.
Additional information
Managed by Massimo Porta.
Appendix 1. Queries used for the systematic review of systematic reviews search
Rights and permissions.
Reprints and permissions
About this article
Caruso, R., Magon, A., Baroni, I. et al. Health literacy in type 2 diabetes patients: a systematic review of systematic reviews. Acta Diabetol 55 , 1–12 (2018). https://doi.org/10.1007/s00592-017-1071-1
Download citation
Received : 04 October 2017
Accepted : 03 November 2017
Published : 11 November 2017
Issue Date : January 2018
DOI : https://doi.org/10.1007/s00592-017-1071-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health literacy
- Type 2 diabetes mellitus
- Diabetes mellitus
- Systematic review
- Diabetes knowledge
- Health outcomes
- Find a journal
- Publish with us
- Track your research
- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- E-Collections
- Virtual Roundtables
- Author Videos
- Author Guidelines
- Submission Site
- Open Access Options
- About The European Journal of Public Health
- About the European Public Health Association
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Terms and Conditions
- Explore Publishing with EJPH
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
- < Previous
Health Literacy in Diabetes management: A priority in health care
- Article contents
- Figures & tables
- Supplementary Data
D do Ó, J Raposo, A Goes, I Loureiro, Health Literacy in Diabetes management: A priority in health care, European Journal of Public Health , Volume 30, Issue Supplement_5, September 2020, ckaa166.478, https://doi.org/10.1093/eurpub/ckaa166.478
- Permissions Icon Permissions
Glycemic control and self-management of diabetes are influenced by a range of factors, including health literacy - the ability to access, understand, appraise, and use health information. This study explored associations between domains of health literacy (HL), glycemic control and perceived general health in people with diabetes.
Cross-sectional study, with 453 people with diabetes,attending the Portuguese Diabetes Association (APDP). We collected information on HL, demographics, glycemic control and self-perception of health. HL was assessed using the Health Literacy Questionnaire. Descriptive and correlational analysis were performed.
85.4% consider Feeling understood and supported by healthcare providers but only 54.1% have the Ability to actively engage with healthcare providers and 27.8% feel the Ability to find good health information,66.5% consider Having sufficient information to manage my health but only 38.7% are Understanding health information well enough to know what to do and 28.5% refer the Ability to find good health information. Higher HL scores were associated with better glycemic control and more positive perception of general health(GH) across the following domains: Having sufficient information to manage my health, Appraisal of health information, Ability to find good health information, Actively managing my health and social support for health. The domains Ability to actively engage with healthcare providers and Navigating the healthcare system were also associated with more positive perception of GH. Associations achieved either p < 0.001 or p < 0.05. Considering HL levels, a statistically significant negative association was found with the levels of HbA1c and positive association with perceived general health, even for functional HL.
The results emphasize the importance of improving the level of HL of people with diabetes in order to improve glycemic control and the perceive General Health
Health literacy is critical for diabetes self-management.
People with diabetes need to understand and use health information to promote well-being and diabetes control.
- diabetes mellitus
- diabetes mellitus, type 2
- health personnel
- hemoglobin a, glycosylated
- personal satisfaction
- social support
- glycemic control
- health care systems
- health literacy
- self-management
- self-perception
Email alerts
Citing articles via.
- Contact EUPHA
- Recommend to your Library
Affiliations
- Online ISSN 1464-360X
- Print ISSN 1101-1262
- Copyright © 2024 European Public Health Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

IMAGES
VIDEO
COMMENTS
Objective. The purpose of this literature review was to identify educational approaches addressing low health literacy for people with type 2 diabetes. Low health literacy can lead to poor management of diabetes, low engagement with health care providers, increased hospitalization rates, and higher health care costs.
Abstract. Objective: The purpose of this literature review was to identify educational approaches addressing low health literacy for people with type 2 diabetes. Low health literacy can lead to ...
A literature review identified a variety of interventions that had a positive impact on provider-patient communication, medication adherence, and glycemic control by promoting diabetes self-management through educational efforts to address low health literacy. Objective The purpose of this literature review was to identify educational approaches addressing low health literacy for people with ...
diabetes mellitus type 2, glucose control and clinical trials, health literacy, self-management Highlights • Health literacy (H)L-driven interventions were effective in controlling glyce-mic levels and improving diabetes self-management outcomes. Received: 2 May 2023 Accepted: 3 June 2023 DOI: 10.1111/1753-0407.13436
Aim To summarize, critically review, and interpret the evidence related to the systematic reviews on health literacy (HL) amongst type 2 diabetes mellitus (T2DM). Methods The methodology for this ...
Diabetes is a global health problem. Approximately 463 million people had diabetes worldwide in 2019, and this number is estimated to reach 700 million by 2045 [].Type 2 diabetes accounts for about 90% of all diabetes cases [].These people need to perform ongoing self-management in their daily lives, such as physical exercise, healthy diets, emotional coping, taking medication, self-monitoring ...
Abstract. Objective: The purpose of this literature review was to identify educational approaches addressing low health literacy for people with type 2 diabetes. Low health literacy can lead to poor management of diabetes, low engagement with health care providers, increased hospitalization rates, and higher health care costs. These challenges ...
Diabetes imposes an increasing health and economic burden on individuals living with it and their societies worldwide. Glycemic control is necessary to reduce morbidity and mortality of type 2 diabetes mellitus (T2DM). Self-management is the primary tool for managing diabetes. Health literacy (HL) is the primary driver of self-management ...
The impact of health literacy on diabetes self-management education ... Lipman RD (2016) Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. ... Diabetes self-management in patients with low health literacy: Ordering findings from literature in a health literacy ...
Aim To summarize, critically review, and interpret the evidence related to the systematic reviews on health literacy (HL) amongst type 2 diabetes mellitus (T2DM). Methods The methodology for this study consisted of a systematic review of systematic reviews, using the PRISMA statement and flowchart to select studies, and searching on PubMed, CINAHL, Scopus, and Cochrane. The search covered the ...
The HL scale used in this study was developed with reference to the multidimensional Functional, Communicative and Critical Health Literacy (CHL) scale, Citation 23 which includes the three constructs of HL introduced by Nutbeam, and was used to assess HL skills and measure HL for patients with type 2 diabetes. The questionnaire included 14 ...
Glycemic control and self-management of diabetes are influenced by a range of factors, including health literacy - the ability to access, understand, appraise, and use health information. This study explored associations between domains of health literacy (HL), glycemic control and perceived general health in people with diabetes.
The aim of this study was to explore the relationship between health literacy and diabetes self-management and control among adults living with type 2 diabetes. Methods. ... levels when compared to persons who were not affected by T2DM. 17 This is of concern as the results of a systematic review indicate that persons with low health literacy ...
The purpose of this review is to summarise the existing evidence about the association of health literacy (HL) with type 2 diabetes mellitus self-management. ... randomised control trials of type 2 diabetes mellitus (T2DM) self-management and HL published between 2009 and 2018. ... 2016 20 literature review [ti] OR this systematic review [tw ...
Diabetes mellitus is a global problem; currently, 463 million people live with diabetes, comprising 9.3% of the global adult population [1]. Type 2 diabetes is the most common type of diabetes, comprising nearly 90% of all diabetes [1]. The disease progression is associated with complications, as it depends on the management of the disease [2]. Although type 2 diabetes management enhanced ...
Introduction: Obtaining, understanding, interpreting, and acting on health information enables people with diabetes to engage and make health decisions in various contexts. Hence, inadequate health literacy (HL) could pose a problem in making self-care decisions and in self-management for diabetes. By applying multidimensional instruments to assess HL, it is possible to differentiate domains ...
This cross-sectional Path analysis study aimed to investigate the effect of HLOC and diabetes health literacy on QOL in 564 patients with type 2 diabetes between October 2021 and February 2022.