- Search Menu
- Animal Research
- Cardiovascular/Pulmonary
- Health Services
- Health Policy
- Health Promotion
- History of Physical Therapy
- Implementation Science
- Integumentary
- Musculoskeletal
- Orthopedics
- Pain Management
- Pelvic Health
- Pharmacology
- Population Health
- Professional Issues
- Psychosocial
- Advance Articles
- COVID-19 Collection
- Featured Collections
- Special Issues
- PTJ Peer Review Academies
- Author Guidelines
- Submission Site
- Why Publish With PTJ?
- Open Access
- Call for Papers
- Self-Archiving Policy
- Promote your Article
- About Physical Therapy
- Editorial Board
- Advertising & Corporate Services
- Permissions
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Case description and methods, case report.
- < Previous
Combined Clinical and Home Rehabilitation: Case Report of an Integrated Knowledge-to-Action Study in a Dutch Rehabilitation Stroke Unit
All authors provided concept/idea/project design. Ms Nanninga, Dr Postema, Ms van Twillert, and Dr Lettinga provided writing. Ms Nanninga provided data collection. Ms Nanninga, Ms van Twillert, and Dr Lettinga provided data analysis. Ms Nanninga and Dr Lettinga provided project management. Ms Nanninga provided fund procurement. Ms Nanninga and Dr Schönherr provided patients and institutional liaisons. Dr Schönherr provided facilities/equipment. Dr Schönherr, Ms van Twillert, and Dr Lettinga provided consultation (including review of manuscript before submission). The authors gratefully acknowledge Stichting Beatrixoord NN for providing financial support for the present work. Special thanks go to the patients and therapists of the multidisciplinary rehabilitation team participating in this project.
- Article contents
- Figures & tables
- Supplementary Data
Christa S. Nanninga, Klaas Postema, Marleen C. Schönherr, Sacha van Twillert, Ant T. Lettinga, Combined Clinical and Home Rehabilitation: Case Report of an Integrated Knowledge-to-Action Study in a Dutch Rehabilitation Stroke Unit, Physical Therapy , Volume 95, Issue 4, 1 April 2015, Pages 558–567, https://doi.org/10.2522/ptj.20130495
- Permissions Icon Permissions
There is growing awareness that the poor uptake of evidence in health care is not a knowledge-transfer problem but rather one of knowledge production. This issue calls for re-examination of the evidence produced and assumptions that underpin existing knowledge-to-action (KTA) activities. Accordingly, it has been advocated that KTA studies should treat research knowledge and local practical knowledge with analytical impartiality. The purpose of this case report is to illustrate the complexities in an evidence-informed improvement process of organized stroke care in a local rehabilitation setting.
A participatory action approach was used to co-create knowledge and engage local therapists in a 2-way knowledge translation and multidirectional learning process. Evidence regarding rehabilitation stroke units was applied in a straightforward manner, as the setting met the criteria articulated in stroke unit reviews. Evidence on early supported discharge (ESD) could not be directly applied because of differences in target group and implementation environment between the local and reviewed settings. Early supported discharge was tailored to the needs of patients severely affected by stroke admitted to the local rehabilitation stroke unit by combining clinical and home rehabilitation (CCHR).
Local therapists welcomed CCHR because it helped them make their task-specific training truly context specific. Key barriers to implementation were travel time, logistical problems, partitioning walls between financing streams, and legislative procedures.
Improving local settings with available evidence is not a straightforward application process but rather a matter of searching, logical reasoning, and creatively working with heterogeneous knowledge sources in partnership with different stakeholders. Multiple organizational levels need to be addressed rather than focusing on therapists as sole site of change.
Physical therapy subscribes to the ideal of evidence-based practice, but how do we achieve that ideal? The health care sector, including physical therapy, has difficulty in applying and achieving widespread uptake of evidence in local practices. 1 – 4 Despite the ever greater technologies available for critically assembling, appraising, and synthesizing the relevant studies of interest on any given topic, therapists still experience difficulties when applying the results of systematic reviews and related guidelines to their routine daily practice. 2 They complain about the poor quality in terms of relevance and fit of the evidence produced by researchers. Researchers, in turn, point to therapists who insist on doing it in their own experience-based way. There is growing recognition that the research-practice gap thus experienced is really a problem of knowledge production rather than one of knowledge transfer. 5 – 7 Research goes unused because researchers fail to address the most important problems facing patients, therapists, and decision makers. 8
The research-practice gap is increasingly articulated in terms of concern about the relative neglect of external validity when it comes to clinical epidemiological research. It is a sine qua non that researchers need to eliminate the possibility of bias in order to provide high-quality evidence. The focus of the research community is on the methodological quality of the clinical trials rather than on the usefulness of their results. 1 , 8 – 11 A drawback that ensues from the stringent rating of research proposals and publications in terms of the rigor of their internal validity control is the creation of a rather “sterile” evidence base. 1 Because clinical trials require such tight criteria when it comes to the interventions and selection of participants, they are likely to end up not having a very high external validity. 1 Much more space, therefore, should be devoted to issues of external validity, 1 , 8 – 11 engaged scholarship, 5 , 6 and the conduct of knowledge translation work in a disinterested way. 12
This case report illustrates the complexities involved in an evidence-informed improvement process in a local rehabilitation stroke unit. It is an integrated knowledge-to-action (KTA) process that draws on a sociologically informed way of considering what sciences are and do. 12 , 13 In such a conception of science, research knowledge is not privileged over practical knowledge. 12 – 14 Translation is conceived in our KTA process as a 2-way knowledge exchange between knowledge producers and users. 6 , 8 , 12 Both forms of knowledge are thereby considered as being distinct but equally valued knowledge practices.
Target Setting
The target setting was the stroke unit of a Dutch rehabilitation center to which patients with multifaceted problems are admitted for multidisciplinary rehabilitation after discharge from an acute stroke unit. The multidisciplinary team consists of physiatrists, physical therapists, occupational therapists, nutritionists, speech therapists, psychologists, social workers, and nursing staff specializing in stroke rehabilitation. A medical and team manager coordinate the multidisciplinary team's work.
Identified Problem
This KTA project started with a request from the head of the department to improve the local service with the best evidence available in the whole chain of care. The request stemmed from his concern that home- and community-based rehabilitation were less organized in the Netherlands compared with, for instance, Scandinavian countries. Despite (or because of) the wealth of systematic reviews and related guideline recommendations on the organization of stroke services, the local therapists experienced difficulties in critically appraising the research knowledge and guideline documents in terms of their usefulness for their local setting. 15 Together with the multidisciplinary team, we performed an integrated KTA project on organized stroke care by co-creating knowledge that fitted the local circumstances.
A fieldwork approach including participatory action research was used to assist the local therapists in KTA activities regarding organized stroke care. In such an approach, active interaction between researchers and those researched influences the learning processes and the self-reflective capacity of both parties. 16 An integrated KTA framework guided the study and involved researchers, therapists, and other stakeholders in a 2-way knowledge translation and multidirectional learning process (see Tab. 1 for an overview of phases, stakeholders, tools, and products). 17 A mixture of research tools was used to bridge the research-practice gap, comprising literature study, individual and focus group interviews, a pilot study, and expert meetings. All individual and focus group interviews were digitally recorded, and files were verbatim transcribed. Data were subsequently coded and compared with regard to facilitators/barriers and advantages/disadvantages of the service to be put into action. The Atlas-ti software program (Atlas-ti GmbH, Berlin, Germany) was used for qualitative data analysis. 18
Two-Way Knowledge Exchange and Multidirectional Learning Process a
PR=participatory researcher, SR=senior researcher, PTs=physical therapists, OTs=occupational therapists, CCHR=combined clinical and home rehabilitation, GP=general practitioner, ESD=early supported discharge, KTA=knowledge-to-action.
A project team was appointed, consisting of the head of the department, the medical manager of the stroke unit, the participatory researcher, and a senior researcher. A human movement scientist, who also worked as a physical therapist in the stroke rehabilitation team, fulfilled both the role of participatory researcher and that of content and setting expert. A philosopher of science and medicine (senior researcher), who was not involved in local practice, fulfilled the role of reflective questioner and supported the participatory researcher in the conceptualization, analysis, triangulation, and interpretation of the data. Ongoing collaboration took place with the multidisciplinary team and their team manager in terms of consultation, information, and feedback meetings. The Board of Directors of University Medical Center Groningen and health care insurance experts were consulted to answer questions about financial, legislation, and regulatory matters.
Phase 1: Specify Problem
In this phase, the participatory and senior researchers specified the problem of the local team by examining literature about the research-practice gap in general, and more specifically about organized stroke care. They identified the problem not just as a lack of knowledge of local therapists but also as a knowledge production problem. The evidence for well-organized stroke care was widely acknowledged. 15 , 19 However, trials had been undertaken in several countries in various settings, using different names to distinguish well-organized from less-organized ones and selecting different target groups with respect to severity due to stroke. 15 This variability in naming, setting, and target population complicated the translation of the body of evidence summarized in numerous reviews into local improvements. Thus, the poor uptake of evidence on organized stroke care in local practices was attributed to the great diversity in stroke services examined in clinical trials. 15 , 20 , 21
Phase 2: Knowledge Creation
In this phase, the researchers searched for reviews summarizing the evidence produced in clinical trials on organized stroke care and stroke rehabilitation. Two guidelines on stroke management were used as additional knowledge sources. 20 , 21
Review of reviews
PubMed, CINAHL, and The Cochrane Library revealed a great variety of reviews on stroke rehabilitation and organized stroke care services. The researchers selected a total of 16 reviews between January 2003 and September 2013 that were relevant to the identified problem. These reviews had their focus on the organization of stroke rehabilitation in primary and secondary care. 22 – 37 Reviews with a focus on diagnostic procedures and rehabilitation treatments were excluded.
Making research knowledge manageable
The project team asked the researchers to make the diversity of stroke services and related evidence manageable in a user-friendly tool. Informed by distinctions made in the reviews, the researchers ordered the research knowledge in a matrix with 4 quadrants ( Figure ). 22 – 38 They distinguished services in well- and less-organized services and inpatient and outpatient services (see Appendix for definitions of services). 22 , 26 – 31 In addition, they differentiated stroke severity as mild (a), moderate (b), or severe disability (c) and evidence as firm (+), inconclusive (+/−), or no evidence (−). 38 In so doing, they reflected the emerging hierarchy of service organizations and target group descriptions articulated by “stroke unit trialists.” 22
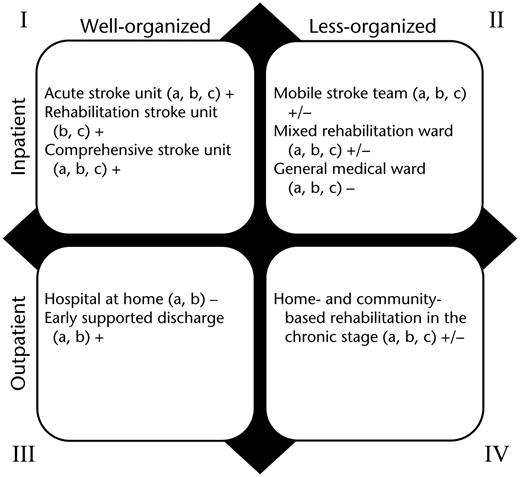
Ordering of well- and less-organized and inpatient and outpatient services. a=mild disability, b=moderate disability, c=severe disability, +=evidence, +/−=inconclusive evidence, −=no evidence.
Phase 3: Tailor Knowledge to Address Identified Problem
In this phase, the project team applied the matrix as an ordering figure to: (1) determine the nature of the local rehabilitation service, (2) explicate the available evidence for the local service, and (3) pinpoint research knowledge that could be used locally for improving home- and community-based services. To address these issues, the researchers explored differences and similarities in target population, content, and implementation environment between the services reviewed and the local service under study.
A rehabilitation stroke unit: a firm evidence base to start with
The project team determined their local service as an evidence-based rehabilitation stroke unit (quadrant I), as their service met the 4 criteria set out in stroke unit reviews. 22 – 25 First, there was a multidisciplinary team that provided stroke care in a dedicated ward; second, the stroke team (including nursing staff) was specialized and trained in stroke rehabilitation; third, routine involvement of caregivers in the rehabilitation process was established in the form of partner groups; and, fourth, new insights and skills in stroke rehabilitation were taught in regular meetings and courses. 22 – 25 Furthermore, the target population of the local service were adult patients with moderate to severe disability who had been admitted to a dedicated department after care in the acute stroke unit of a hospital. The multifaceted problems meant that rehabilitation treatment could not adequately and safely be managed at home. This approach was in line with stroke guidelines recommending that all patients not suitable for transfer home after completion of acute diagnosis and treatment should be treated in a specialist rehabilitation stroke unit. 20 , 21 Research knowledge about rehabilitation stroke units thus served as a firm evidence base (level A) for the target group in the local setting.
Early supported discharge (ESD): a challenge to translate the evidence
Evidence concerning home and community rehabilitation services was inconclusive because of variability across services (quadrant IV). 28 – 30 The project team endorsed ESD as a well-organized and evidence-based cost-saving outpatient alternative to regularly supported discharge (quadrant III). 31 – 37 Early supported discharge involves a multidisciplinary team specialized in stroke rehabilitation that plans and coordinates early discharge from the hospital, postdischarge care, and rehabilitation at home through weekly team meetings, usually followed by a visit from the case manager of the ESD team. 31 Stroke guidelines recommend that patients should be discharged early from stroke unit care only if there is a specialist stroke rehabilitation team able to continue rehabilitation in the community from the day of transfer. 20 , 21
The project team noted that well-organized, specialist home- and community-based stroke services were scarce in the region. Moreover, the greatest benefits from ESD are attributed to patients with mild to moderate disability in acute stroke units, whereas the target group in their local setting are patients with moderate to severe disability treated in a rehabilitation stroke unit. 31 – 36 They concluded that the original evidence on ESD did not exactly fit the circumstances of the target setting. Even so, they argued that the local rehabilitation stroke unit could well profit from the ESD recommendation to shift more—and at an earlier stage—into home-based alternatives. 31 – 33 , 35 , 36 In light of these findings, the idea of an alternative service tailored to patients with moderate and severe disability following stroke surfaced; that is, combined clinical home rehabilitation (CCHR), in which specialist multidisciplinary treatment in the rehabilitation unit could be combined with home treatment at an early stage. The participatory researcher used the matrix to inform the multidisciplinary team about: (1) how to build on the evidence available for stroke rehabilitation units and (2) how to learn from evidence for ESD.
Phase 4: Adapt Knowledge to Local Context
In this phase, the researchers traced and articulated ways of attending to clinical and home rehabilitation of the local team. Therefore, they conducted 2 focus group discussions, each with 8 participants from different disciplines of the multidisciplinary team. The focus groups addressed the question: “How could one learn the most from the advantages or disadvantages of combined clinical and home rehabilitation.” To elaborate on the practical contextual knowledge of the team, the researchers subsequently conducted a second literature review focused on items that the participants addressed as challenging.
Practical knowledge of the team
The participants articulated the greatest advantage of CCHR as being an easier carryover of skills learned in the clinical setting to the home setting. They discussed the carryover problem in terms of “a gap, into which patients and their families threaten to fall after discharge from the rehabilitation unit.” Patients faced the problem of being treated in an institution and then having to master an environment that differed from this institution in various ways. This problem could not be prevented by means of weekend leaves and routine involvement of partners in the rehabilitation process, or even by home visits. Therapists critically reflected on the “artificial state” of their treatments by stressing that activities training in a clinical setting was always an imperfect simulation of the natural setting at home. Therefore, they welcomed CCHR because it made training more “tailor-made” and task- and context-specific. Patient goals could be better set in collaboration with patients and significant others at home, thereby taking problems in real life as a directive for treatment. The added value of CCHR was expressed in a better transition to the home setting rather than in cost savings such as in ESD.
One disadvantage discussed by the participants was the distance that needed to be bridged in order to deliver treatment at home. Travel time made them less employable in the clinical setting, and they doubted whether health insurance companies were willing to pay for such indirect costs. Asking community therapists to deliver home treatment was not an alternative because they lacked specialist expertise in stroke rehabilitation. Fatigue of patients with stroke was a concern that also needed to be considered with respect to travel time. Also, although family members could be actively involved in CCHR, they might not always be able to free themselves from work obligations during home treatment.
Research knowledge from the literature
To build on the practical knowledge of the local team, the researchers conducted a literature review on task- and context-specific training and goal setting. This review confirmed and specified the practical knowledge of the team. Indeed, most patients with stroke had difficulty with generalizing what had been learned in the therapeutic setting to their own living environments. 39 The context in which tasks are learned, therefore, should be as personalized and home-like as possible. Task-specific training enhanced functional outcomes in stroke rehabilitation, where there is increasing evidence available for neural plastic changes. 40 Intensive, meaningful, repetitive task-specific and client-centered treatments that targeted the whole body were advocated in an enriched environment. 40 , 41 Goal setting in close collaboration with patients and their families was considered a key element in rehabilitation treatment. 42 Goals should be meaningful and challenging but achievable and should include both short-term (days/weeks) and long-term (weeks/months) targets and time-bound measurable outcomes. 42 Qualitative studies on the actual use of goals in rehabilitation practice revealed, however, that goals are frequently unattained, modified, or contested. 43 , 44 In rehabilitation, goals are set for the home setting that differ—in terms of spatial and social characteristics—from those in the clinical setting, where people are training for the accomplishment of goals. 44 The research knowledge on task- and context-specific training and goal setting supported the practical knowledge and drives of the therapists and the uptake of CCHR. The therapists explicated these findings in a feedback meeting with the team.
Phase 5: Assess Barriers to Knowledge Use
In this phase, the project team decided in close cooperation with the team to conduct a pilot study with 4 patients with varying cognitive and motor problems poststroke ( Tab. 2 ). Physical therapists and occupational therapists were indicated as best candidates for delivery of CCHR. The participatory researcher assisted the therapists in making CCHR practical. After the pilot study, the researchers assessed facilitators and barriers in the application of CCHR by conducting semistructured individual interviews with 9 therapists and the 4 patients and their caregivers involved in the pilot study. The head of the department and the senior researcher subsequently talked with members of the Board of Directors of University Medical Center Groningen and with regional health insurance experts about the potential of CCHR.
Patient Characteristics a
MRS=Modified Rankin Scale, CCHR=combined clinical home rehabilitation, PT=physical therapist, OT=occupational therapist.
Specification of CCHR
Informed by ESD evidence, the participatory researcher decided in partnership with the therapists to begin with CCHR as early as possible, that is, within 4 weeks after admission to the rehabilitation stroke unit. The literature studies on task- and context-specific training and goal setting made them decide that goals needed to be set in the home setting in close collaboration with the patients and their caregivers. Whole tasks should subsequently be assessed and trained in the home setting and then problematic tasks repeatedly practiced in the clinical setting with a focus on the missing components. Subsequently, the whole tasks had to be trained in the home setting again.
Experiences of therapists and patients and their caregivers
Therapists embraced the alternative: CCHR provided a great deal of insight into the home environment, including the problems their patients had to face. Although they experienced difficulties with restructuring their existing skills, they felt they could offer their patients a more customized treatment. According to one therapist, “CCHR was a lottery ticket for a patient with severe cognitive problems.” This patient showed astonishing improvements when training took place in his own living environment. Patients were satisfied, because they were taught to use, in their own home environment, what they had learned in the clinical setting. Home treatments made family members feel more secure in assisting patients in performing daily activities in the absence of the therapist during weekend leaves.
Most of the goals that were set at home, and subsequently trained for in the clinical setting, were attained. A frequency of two 45-minute home-treatment sessions a week appeared to be enough for goal setting and treatment. The total duration of CCHR ranged from 2 to 5 weeks, in which the total number of home treatments ranged from 2 to 10 sessions, depending on the complexity of problems poststroke. However, starting early (ie, within 4 weeks) became a barrier for some patients and their caregivers. For logistical reasons, the team could not select more than 2 patients for home treatment at the same time; otherwise, too few therapists would then be available for regular treatment in the clinic. Therapists also experienced time pressure in their schedules caused by additional travel time and time to fine-tune activities. As a solution, home treatments were connected to weekend leaves.
Expert consultation
A barrier beyond the control of the therapists involved the organization and finance system of health care services in the Netherlands. The consulted board of directors and health insurance experts foresaw financial and legislative problems were it to be implemented structurally. Dutch inpatient and outpatient therapists work in separate organizational environments with different employment relationships and financing agencies. They suggested involving care financing agencies in the project because legislative procedures and partitioning walls between health-financing systems in primary and secondary care might hamper structural implementation of CCHR. This suggestion implied that the project team had to redefine the problem and integrate practical and contextual knowledge of regional managers, therapists, and financial and policy experts in the local knowledge co-creation process. Several therapists were eager to give content to the new idea.
Phase 6: Redefine Identified Problem
In this phase, the researchers placed the problematic integration of primary and secondary care services in a broader perspective by organizing an expert meeting with 1 local care manager as well as 4 care managers, 1 health insurance expert, 1 general practitioner, and 2 policy makers in the region. Another expert meeting was organized with 6 physical therapists, 5 occupational therapists, and 2 speech therapists treating survivors of stroke in the region. Subsequently, the researchers conducted a qualitative study to gain knowledge of the needs of survivors of stroke and family caregivers in the clinical, postdischarge, and reintegration phases of the rehabilitation process.
Expert meetings
The region had identified active and healthy aging as a major societal challenge. All participants were supportive of a better integration between primary and secondary stroke care services. To meet the demands associated with demographic change in terms of low birthrates, increasing longevity, the related shortage of health care professionals, and increasing pressure on public budgets, the policy makers felt the need to rethink the way stroke services were organized in the regional chain of care. Delivery of stroke care with less fragmentation, close to home, and bridging distances with the help of innovative technology were shared challenges. The physical therapists, occupational therapists, and speech therapists expressed a shortage of knowledge in outpatient services concerning the treatment and multifaceted problems of survivors of stroke as a major concern. The qualitative study revealed that survivors of stroke foregrounded functional recovery in the clinical phase, were confronted with an identity confusion and related mourning process in the postdischarge phase, and longed for recognition and a sense of belonging in the reintegration phase. 45
Reshape problem
Informed by this practical, contextual, and research knowledge, the project team suggested that individual coaching of survivors of stroke and family caregivers rather than multidisciplinary treatment should be pivotal in home- and community-based rehabilitation. The project team decided to reshape the identified therapeutic problem by placing it in a regional policy and multi-stakeholder perspective and then go through the knowledge creation and action cycle again. The therapeutic question “How can therapists improve the transition from the clinical to the home setting with the available evidence on organized stroke care?” was reshaped into a decision-making question: “How do we organize rehabilitation service through to the home environment of survivors of stroke in a sustainable, efficient, and smart way, eventually with the help of e-health technology?” Combined coaching at home (face-to-face) and over distance (screen-to-screen) was articulated as an alternative that might contribute to regional challenges. How the project team addressed multiple organization levels in a second KTA study on organized stroke care and how they managed that therapists remained involved will be presented in the near future.
This case report illustrates the iterative and dynamic process of integrated KTA research aimed at translating evidence, produced in controlled research settings, to complicated implementation environments such as those seen in clinics. To bridge the research-practice gap experienced, we used a participative action approach, thereby treating research and practical contextual knowledge with analytical impartiality. 5 , 12 The lessons learned by doing are discussed below.
Different Translations of Evidence to Local Setting
By articulating similarities and differences in the target population and environments of local and research settings, we learned that evidence produced in clinical trials could help to advance local settings in different ways. Similarities indicate proof of actual practice in local settings, implying that local therapists already worked in an evidence-based manner, as was the case in the local rehabilitation stroke unit described in this case report. Differences indicate that there is a challenge to improve local reality in an evidence-informed way, as we did with evidence for ESD. This finding might imply that therapists need to deviate from original evidence produced in research settings, as was done in CCHR, in order to tailor it to the abilities of patients who are severely disabled poststroke treated in a rehabilitation stroke unit. In most reviewed trials, severity was measured with the Barthel Index. Whether the Barthel Index is a valid instrument for objectifying the multi-facedness of problems of survivors of stroke in their own living environments might be a topic for future research.
Generalizability of Case Studies
Case studies and participatory action research do not have generalizing power, in that we can now recommend how other stroke rehabilitation services can improve their service in a well-organized and evidence-informed manner. This conclusion, however, does not mean that the findings in this KTA project only have local value. We hope to have demonstrated that detailed analysis and description of a bidirectional evidence-informed translation process in one location might have value for stakeholders working in another location. Indeed, such a specification of a local improvement process renders it possible for therapists in other settings to examine what will remain the same and what will change, when they want to improve the organization of their service in an evidence-informed manner. The user-friendly matrix that we developed as an ordering figure for navigating through the different types of services on organized stroke care including available evidence also might facilitate others in improving their local setting in an evidence-informed way.
Lack of Attention to Multiple Organizational Levels
One limitation of this case report is that we did not take broader organizational levels into account from the very beginning of our KTA process. We learned that improving rehabilitation practice with available evidence on organized stroke care is not just a matter of mobilizing its key users but also one of augmenting its material and organizational environment. 7 , 8 Partitioning walls between different financing systems along with stifling legislation and regulatory procedures were detected as main barriers for structural implementation of CCHR. Thus, multiple organizational levels need to be addressed in KTA studies rather than focusing on therapists as the sole site of change. 46 That is why we reshaped our identified problem and started to go through the knowledge creation funnel and action cycle again. The philosophy underlying, and methodology used, in transition management research may prove to be useful in such a multi-actor process. 47
Transformed Terminology and KTA Framework
Translation was conceived in the KTA process as a 2-way knowledge exchange and multidirectional learning process for knowledge “producers” and “users.” 5 , 6 , 12 Conventional KTA frameworks suggest a one-way knowledge transfer by the KTA expert, as is illustrated by the arrows of the action cycle pointing in just one direction. 2 , 5 We welcome the bidirectional arrows of present frameworks that visualize the iterative, dynamic, and multidirectional learning process in KTA work more adequately. 17 Knowledge translation experts may have been too focused on applied and evaluation research, which privileges scientific knowledge over local practical knowledge. 12 As such, they might overlook the multiplicity of KTA work, in particular the production of new knowledge, which arises from the interactions between scientific and practical contextual knowledge. This situation implies that we need to reconsider the terminology in which current KTA frameworks articulate their knowledge creation and KTA activities. Also, the contradiction between knowledge “producers” and knowledge “users” might no longer be appropriate terminology. We argue that evidence-informed improvements of local practices are achieved more easily if the terminology remains equally valued and yet is fluid enough to change shape, to make it adaptable to the requirements of the new surroundings.
Improving rehabilitation practice is quite a different enterprise from proving its effectiveness. 14 Improving settings with the help of research findings from a rather “sterile” evidence base 1 and translating these findings into the complex world of health care delivery is a matter of creatively working with heterogeneous information sources. 3 , 13 , 14 It is an iterative, cyclical, and dynamic translation and transformation process that requires practical and contextually relevant wisdom on the part of all involved, such as researchers, therapists, patients, caregivers, managers, and policy makers.
Project approval was obtained from the Medical Ethical Committee of University Medical Center Groningen (UMCG).
Green , LW , . Making research relevant: if it is an evidence-based practice, where's the practice-based evidence? Fam Pract . 2008 ; 25 ( suppl 1 ): i20 – i24 .
Google Scholar
Tugwell , PS , Santesso , NA , O'Connor , AM , Wilson , AJ ; Effective Consumer Investigative Group . Knowledge translation for effective consumers . Phys Ther . 2007 ; 87 ; 1728 – 1738 .
van Twillert , S , Postema , K , Geertzen , JH , et al. . Improving rehabilitation treatment in a local setting: a case study of prosthetic rehabilitation . Clin Rehabil . 2009 ; 23 : 938 – 947 .
Graham , ID , Logan , J , Harrison , MB , et al. . Lost in knowledge translation: time for a map? J Contin Educ Health Prof . 2006 ; 26 : 13 – 24 .
Bowen , SJ , Graham , ID . From knowledge translation to engaged scholarship: promoting research relevance and utilization . Arch Phys Med Rehabil . 2013 ; 94 : S3 – S8 .
Van de Ven , AH , Johnson , PE . Knowledge for theory and practice . Acad Manage Rev . 2006 ; 31 : 802 – 821 .
Best , A , Terpstra , JL , Moor , G , et al. . Building knowledge integration systems for evidence-informed decisions . J Health Organ Manag . 2009 ; 23 : 627 – 641 .
Glasgow , RE , Green , LW , Klesges , LM , et al. . External validity: we need to do more . Ann Behav Med . 2006 ; 31 : 105 – 108 .
Green , LW , Glasgow , RE . Evaluating the relevance, generalization, and applicability of research: issues in external validation and translation methodology . Eval Health Prof . 2006 ; 29 : 126 – 153 .
Green , LW , Ottoson , JM , Garcia , C , Hiatt , RA . Diffusion theory and knowledge dissemination, utilization, and integration in public health . Annu Rev Public Health . 2009 ; 30 : 151 – 174 .
Hay , MC , Weisner , TS , Subramanian , S , et al. . Harnessing experience: exploring the gap between evidence-based medicine and clinical practice . J Eval Clin Pract . 2008 ; 14 : 707 – 713 .
Kitto , SC , Sargeant , J , Reves , S , Silver , I . Towards a of knowledge translation: the importance of being dis-interested in knowledge translation . Adv Health Sci Educ Theory Pract . 2012 ; 17 : 289 – 299 .
Lettinga , AT , Mol , A . Clinical specificity and the non-generalities of science: on innovation strategies in neurological physical therapy . Theo Med Bioeth . 1999 ; 20 : 517 – 535 .
Mol , A . Proving or improving: on healthcare research as a form of self-reflection . Qual Health Res . 2006 ; 16 : 405 – 414 .
Kalra , L , Langhorne , P . Facilitating recovery: evidence for organized stroke care . J Rehabil Med . 2007 ; 39 : 97 – 102 .
Hennink , M , Hutter , I , Bailey , A . Qualitative Research Methods . London, United Kingdom : Sage Publications ; 2011 .
Google Preview
Straus , SE , Tetroe , J , Graham , ID , eds. Knowledge Translation in Health Care: Moving From Evidence to Practice . 2nd ed. Chichester, United Kingdom : Wiley-Blackwell ; 2013 .
Muhr , T , Friese , S . User's Manual for Atlas.ti 5.0 . 2nd ed. Berlin, Germany : Scientific Software Development ; 2004 .
Walker , MF , Fisher , RJ , Korner-Bitensky , N , et al. . From what we know to what we do: translating stroke rehabilitation research into practice . Int J Stroke . 2013 ; 8 : 11 – 17 .
Intercollegiate Stroke Working Party . National Clinical Guideline for Stroke . 3rd ed. London, United Kingdom : Royal College of Physicians ; 2008 .
Kwaliteitsinstituut voor de Gezondheidszorg CBO . Richtlijn “Diagnostiek, Behandeling en zorg voor Patiënten met een Beroerte.” Utrecht, the Netherlands : Nederlandse Vereniging voor Neurologie ; 2008 .
Stroke Unit Trialists' Collaboration . Organized inpatient (stroke unit) care for stroke . Cochrane Database Syst Rev . 2013 ; 9 : CD000197 .
Foley , N , Salter , K , Teasell , R . Specialized stroke services: a meta-analysis comparing three models of care . Cerebrovasc Dis . 2007 ; 23 : 194 – 202 .
Fuentes , B , Diez-Tejedor , E . Stroke units: many questions, some answers . Int J Stroke . 2009 ; 4 : 28 – 37 .
Seenan , P , Long , M , Langhorne , P . Stroke units in their natural habitat: systematic review of observational studies . Stroke . 2007 ; 38 : 1886 – 1892 .
Langhorne , P , Dey , P , Woodman , M , et al. . Is stroke unit care portable? A systematic review of the clinical trials . Age Ageing . 2005 ; 34 : 324 – 330 .
Shepperd , S , Doll , H , Broad , J , et al. . Early discharge hospital at home . Cochrane Database Syst Rev . 2009 ; 1 : CD000356 .
Legg , L , Langhorne , P ; Outpatient Service Trialists . Rehabilitation therapy services for stroke patients living at home: systematic review of randomised trials . Lancet . 2004 ; 363 : 352 – 356 .
Hillier , S , Inglis-Jassiem , G . Rehabilitation for community-dwelling people with stroke: home or centre based? A systematic review . Int J Stroke . 2010 ; 5 : 178 – 186 .
Aziz , NA , Leonardi-Bee , J , Phillips , M , et al. . Therapy-based rehabilitation services for patients living at home more than one year after stroke . Cochrane Database Syst Rev . 2008 ; 2 : CD005952 .
Fearon , P , Langhorne , P ; Early Supported Discharge Trialists . Services for reducing duration of hospital care for acute stroke patients . Cochrane Database Syst Rev . 2012 ; 9 : CD000443 .
Langhorne , P , Holmqvist , LW ; Early Supported Discharge Trialists . Early supported discharge after stroke . J Rehabil Med . 2007 ; 39 : 103 – 108 .
Rousseaux , M , Daveluy , W , Kozlowski , R . Value and efficacy of early supported discharge from stroke units . Ann Phys Rehabil Med . 2009 ; 52 : 224 – 233 .
Larsen , T , Olsen , TS , Sorensen , J . Early home-supported discharge of stroke patients: a health technology assessment . Int J Technol Assess Health Care . 2006 ; 22 : 313 – 320 .
Langhorne , P , Taylor , G , Murray , G , et al. . Early supported discharge services for stroke patients: a meta-analysis of individual patients' data . Lancet . 2005 ; 365 : 501 – 506 .
Teasell , RW , Foley , NC , Bhogal , SK , et al. . Early supported discharge in stroke rehabilitation . Top Stroke Rehabil . 2003 ; 10 : 19 – 33 .
Brady , BK , McGahan , L , Skidmore , B . Systematic review of economic evidence on stroke rehabilitation services . Int J Technol Assess Health Care . 2005 ; 21 : 15 – 21 .
Langhorne , P . Organisation of acute stroke care . Br Med Bull . 2000 ; 56 : 436 – 443 .
Mulder , T , Hochstenbach , J . Adaptability and flexibility of the human motor system: implications for neurological rehabilitation . Neural Plast . 2001 ; 8 : 131 – 140 .
Arya , KN , Pandian , S , Verma , R , et al. . Movement therapy induced neural reorganization and motor recovery in stroke: a review . J Bodyw Mov Ther . 2011 ; 15 : 528 – 537 .
Combs , SA , Kelly , SP , Barton , R , et al. . Effects of an intensive, task-specific rehabilitation program for individuals with chronic stroke: a case series . Disabil Rehabil . 2010 ; 32 : 669 – 678 .
Playford , ED , Siegert , R , Levack , W , et al. . Areas of consensus and controversy about goal setting in rehabilitation: a conference report . Clin Rehabil . 2009 ; 23 : 334 – 344 .
Levack , WM , Taylor , K , Siegert , RJ , et al. . Is goal planning in rehabilitation effective? A systematic review . Clin Rehabil . 2006 ; 20 : 739 – 755 .
Struhkamp , R . Goals in their setting: a normative analysis of goal setting in physical rehabilitation . Health Care Anal . 2004 ; 12 : 131 – 155 .
Nanninga , CS , Meijering , L , Schönherr , MC , et al. . Place attachment in stroke rehabilitation: a transdisciplinary encounter between cultural geography, environmental psychology and rehabilitation medicine . Disabil Rehabil . 2014 Aug 29 [Epub ahead of print]. doi: 10.3109/09638288.2014.955136 .
Chesla , CA . Translational research: essential contributions from interpretive nursing science . Res Nurs Health . 2008 ; 31 : 381 – 390 .
Loorbach , D , Rotmans , J . The practice of transition management, examples and lessons from four distinct cases . Futures . 2010 ; 42 : 237 – 246 .
Glossary of Stroke Services Ordered in a Matrix
Author notes
Email alerts, citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1538-6724
- Copyright © 2024 American Physical Therapy Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

- < Previous
Home > Communities > School of Medicine & Health Sciences > PT > PT-GRAD > 578
Physical Therapy Scholarly Projects
Physical Therapy for a Female with Acute Stroke: A Case Report
Lisa Grandpre , University of North Dakota
Date of Award
Document type.
Scholarly Project
Degree Name
Doctor of Physical Therapy (DPT)
Physical Therapy
First Advisor
Mark Romanick
Stroke -- therapy; Case Reports
Background and Purpose : Strokes are the 5th leading cause of death and adult disability in the US. Strokes affect each individual differently, some individuals more severely than others. The goal of physical therapists is to come up with the best treatment plan for each individual in order to restore as much function as possible.
Case Description : The patient was a Caucasian female in her 80s who suffered a stroke while in the hospital. She was living in assisted living prior to her hospital stay and was functional in the home only. The passive range of motion in her left extremities was within normal limits, with tone flaccid. We were unable to assess the strength of her left extremities. She required 2-person, maximal assistance for transfers and minimal assistance for static sitting during our early visits.
Intervention : Patient education, therapeutic exercise, bed mobility, balance and transfer training, and wheelchair mobility training were some of this patient's interventions.
Outcomes : The patient had 18 physical therapy sessions. She was able to increase her static standing time from 15 to 20 seconds to 30 to 40 seconds. Her sitting trunk control increased and her bed mobility went from a 2 person maximal assistance to a 1 person maximal assistance by her discharge.
Discussion : Research on acute stroke patients is limited. Most research focuses on subacute and chronic stroke patients. Our patient had minimal improvements after 16 days in the hospital and was discharged to a nursing home with both physical and occupational therapy recommended.
Recommended Citation
Grandpre, Lisa, "Physical Therapy for a Female with Acute Stroke: A Case Report" (2016). Physical Therapy Scholarly Projects . 578. https://commons.und.edu/pt-grad/578
Since May 29, 2018
Included in
Physical Therapy Commons
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Author Corner
- Author Submission Agreement
- About the Library
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Cerebellar Stroke Occupational Therapy and Physical Therapy Management from Intensive Care Unit to Outpatient: A Case Report
Affiliations.
- 1 Physical Therapy Program, School of Health Sciences, Oakland University.
- 2 Rehabilitation Services, Beaumont Hospital, Troy, Mi.
- 3 Physical Therapy Program, School of Health Sciences, Oakland University, Rochester, Mi.
- PMID: 29468104
- PMCID: PMC5812525
- DOI: 10.7759/cureus.1949
Cerebellar stroke increases the risk of extensive physical disability and long-term institutionalization. The purpose of this case report is to describe the 14-month longitudinal rehabilitation management and outcomes from the intensive care unit, inpatient rehabilitation unit and outpatient care of a patient after cerebellar stroke. A goal of this case report is to provide rehabilitation clinicians with a long-term perspective and understanding of the course of recovery for a patient after cerebellar cerebrovascular accident or related injury. A 51-year-old healthy athletic female experienced acute bilateral cerebellar infarcts with subsequent craniotomy to remove infarcted areas. The patient had postoperative hemorrhages and hydrocephalus and was deemed to have a poor prognosis. Multimodal sensory stimulation and early mobility was performed until conventional neuromuscular reeducation interventions could be tolerated. Primary deficits included decreased proximal strength, whole body ataxia, vertical diplopia, dysphagia, difficulty communicating, and emotional lability. Fourteen months after the initial infarcts, the patient was able to reside in her own home with her husband, ambulate, and stand with assistance and perform most activities of daily living with standby or set-up assistance. This patient made significant progress toward safety and mobility and was able to return home despite the early discussion about a poor prognosis and a palliative care consultation. The complex, intensive course of rehabilitation elicited slow, steady, consistent gains. The patient's motivation and family involvement likely facilitated optimum outcomes.
Keywords: cerebellar diplopia; cerebellar stroke; cerebellum; early mobility; icu; multimodal sensory stimulation; occupational therapy; palliative; physical therapy; stroke.
Publication types
- Case Reports
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 13, Issue 8
- Clinical course of a 66-year-old man with an acute ischaemic stroke in the setting of a COVID-19 infection
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-7441-6952 Saajan Basi 1 , 2 ,
- Mohammad Hamdan 1 and
- Shuja Punekar 1
- 1 Department of Stroke and Acute Medicine , King's Mill Hospital , Sutton-in-Ashfield , UK
- 2 Department of Acute Medicine , University Hospitals of Derby and Burton , Derby , UK
- Correspondence to Dr Saajan Basi; saajan.basi{at}nhs.net
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater oxygen requirement, alongside reduced levels of consciousness. A positive COVID-19 throat swab, in addition to bilateral pneumonia on chest X-ray and lymphopaenia in his blood tests, confirmed a diagnosis of COVID-19 pneumonia. A proactive decision was made involving the patients’ family, ward and intensive care healthcare staff, to not escalate care above a ward-based ceiling of care. The patient died 5 days following admission under the palliative care provided by the medical team.
- respiratory medicine
- infectious diseases
- global health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bcr-2020-235920
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is a new strain of coronavirus that is thought to have originated in December 2019 in Wuhan, China. In a matter of months, it has erupted from non-existence to perhaps the greatest challenge to healthcare in modern times, grinding most societies globally to a sudden halt. Consequently, the study and research into SARS-CoV-2 is invaluable. Although coronaviruses are common, SARS-CoV-2 appears to be considerably more contagious. The WHO figures into the 2003 SARS-CoV-1 outbreak, from November 2002 to July 2003, indicate a total of 8439 confirmed cases globally. 1 In comparison, during a period of 4 months from December 2019 to July 2020, the number of global cases of COVID-19 reached 10 357 662, increasing exponentially, illustrating how much more contagious SARS-CoV-2 has been. 2
Previous literature has indicated infections, and influenza-like illness have been associated with an overall increase in the odds of stroke development. 3 There appears to be a growing correlation between COVID-19 positive patients presenting to hospital with ischaemic stroke; however, studies investigating this are in progress, with new data emerging daily. This patient report comments on and further characterises the link between COVID-19 pneumonia and the development of ischaemic stroke. At the time of this patients’ admission, there were 95 positive cases from 604 COVID-19 tests conducted in the local community, with a predicted population of 108 000. 4 Only 4 days later, when this patient died, the figure increased to 172 positive cases (81% increase), illustrating the rapid escalation towards the peak of the pandemic, and widespread transmission within the local community ( figure 1 ). As more cases of ischaemic stroke in COVID-19 pneumonia patients arise, the recognition and understanding of its presentation and aetiology can be deciphered. Considering the virulence of SARS-CoV-2 it is crucial as a global healthcare community, we develop this understanding, in order to intervene and reduce significant morbidity and mortality in stroke patients.
- Download figure
- Open in new tab
- Download powerpoint
A graph showing the number of patients with COVID-19 in the hospital and in the community over time.
Case presentation
A 66-year-old man presented to the hospital with signs of left-sided weakness. The patient had a background of chronic obstructive pulmonary disease (COPD), atrial fibrillation and had one previous ischaemic stroke, producing left-sided haemiparesis, which had completely resolved. He was a non-smoker and lived in a house. The patient was found slumped over on the sofa at home on 1 April 2020, by a relative at approximately 01:00, having been seen to have no acute medical illness at 22:00. The patients’ relative initially described disorientation and agitation with weakness noted in the left upper limb and dysarthria. At the time of presentation, neither the patient nor his relative identified any history of fever, cough, shortness of breath, loss of taste, smell or any other symptoms; however, the patient did have a prior admission 9 days earlier with shortness of breath.
The vague nature of symptoms, entwined with considerable concern over approaching the hospital, due to the risk of contracting COVID-19, created a delay in the patients’ attendance to the accident and emergency department. His primary survey conducted at 09:20 on 1 April 2020 demonstrated a patent airway, with spontaneous breathing and good perfusion. His Glasgow Coma Scale (GCS) score was 15 (a score of 15 is the highest level of consciousness), his blood glucose was 7.2, and he did not exhibit any signs of trauma. His abbreviated mental test score was 7 out of 10, indicating a degree of altered cognition. An ECG demonstrated atrial fibrillation with a normal heart rate. His admission weight measured 107 kg. At 09:57 the patient required 2 L of nasal cannula oxygen to maintain his oxygen saturations between 88% and 92%. He started to develop agitation associated with an increased respiratory rate at 36 breaths per minute. On auscultation of his chest, he demonstrated widespread coarse crepitation and bilateral wheeze. Throughout he was haemodynamically stable, with a systolic blood pressure between 143 mm Hg and 144 mm Hg and heart rate between 86 beats/min and 95 beats/min. From a neurological standpoint, he had a mild left facial droop, 2/5 power in both lower limbs, 2/5 power in his left upper limb and 5/5 power in his right upper limb. Tone in his left upper limb had increased. This patient was suspected of having COVID-19 pneumonia alongside an ischaemic stroke.
Investigations
A CT of his brain conducted at 11:38 on 1 April 2020 ( figure 2 ) illustrated an ill-defined hypodensity in the right frontal lobe medially, with sulcal effacement and loss of grey-white matter. This was highly likely to represent acute anterior cerebral artery territory infarction. Furthermore an oval low-density area in the right cerebellar hemisphere, that was also suspicious of an acute infarction. These vascular territories did not entirely correlate with his clinical picture, as limb weakness is not as prominent in anterior cerebral artery territory ischaemia. Therefore this left-sided weakness may have been an amalgamation of residual weakness from his previous stroke, in addition to his acute cerebral infarction. An erect AP chest X-ray with portable equipment ( figure 3 ) conducted on the same day demonstrated patchy peripheral consolidation bilaterally, with no evidence of significant pleural effusion. The pattern of lung involvement raised suspicion of COVID-19 infection, which at this stage was thought to have provoked the acute cerebral infarct. Clinically significant blood results from 1 April 2020 demonstrated a raised C-reactive protein (CRP) at 215 mg/L (normal 0–5 mg/L) and lymphopaenia at 0.5×10 9 (normal 1×10 9 to 3×10 9 ). Other routine blood results are provided in table 1 .
CT imaging of this patients’ brain demonstrating a wedge-shaped infarction of the anterior cerebral artery territory.
Chest X-ray demonstrating the bilateral COVID-19 pneumonia of this patient on admission.
- View inline
Clinical biochemistry and haematology blood results of the patient
Interestingly the patient, in this case, was clinically assessed in the accident and emergency department on 23 March 2020, 9 days prior to admission, with symptoms of shortness of breath. His blood results from this day showed a CRP of 22 mg/L and a greater lymphopaenia at 0.3×10 9 . He had a chest X-ray ( figure 4 ), which indicated mild radiopacification in the left mid zone. He was initially treated with intravenous co-amoxiclav and ciprofloxacin. The following day he had minimal symptoms (CURB 65 score 1 for being over 65 years). Given improving blood results (declining CRP), he was discharged home with a course of oral amoxicillin and clarithromycin. As national governmental restrictions due to COVID-19 had not been formally announced until 23 March 2020, and inconsistencies regarding personal protective equipment training and usage existed during the earlier stages of this rapidly evolving pandemic, it is possible that this patient contracted COVID-19 within the local community, or during his prior hospital admission. It could be argued that the patient had early COVID-19 signs and symptoms, having presented with shortness of breath, lymphopaenia, and having had subtle infective chest X-ray changes. The patient explained he developed a stagnant productive cough, which began 5 days prior to his attendance to hospital on 23 March 2020. He responded to antibiotics, making a full recovery following 7 days of treatment. This information does not assimilate with the typical features of a COVID-19 infection. A diagnosis of community-acquired pneumonia or infective exacerbation of COPD seem more likely. However, given the high incidence of COVID-19 infections during this patients’ illness, an exposure and early COVID-19 illness, prior to the 23 March 2020, cannot be completely ruled out.
Chest X-ray conducted on prior admission illustrating mild radiopacification in the left mid zone.
On the current admission, this patient was managed with nasal cannula oxygen at 2 L. By the end of the day, this had progressed to a venturi mask, requiring 8 L of oxygen to maintain oxygen saturation. He had also become increasingly drowsy and confused, his GCS declined from 15 to 12. However, the patient was still haemodynamically stable, as he had been in the morning. An arterial blood gas demonstrated a respiratory alkalosis (pH 7.55, pCO 2 3.1, pO 2 6.7 and HCO 3 24.9, lactate 1.8, base excess 0.5). He was commenced on intravenous co-amoxiclav and ciprofloxacin, to treat a potential exacerbation of COPD. This patient had a COVID-19 throat swab on 1 April 2020. Before the result of this swab, an early discussion was held with the intensive care unit staff, who decided at 17:00 on 1 April 2020 that given the patients presentation, rapid deterioration, comorbidities and likely COVID-19 diagnosis he would not be for escalation to the intensive care unit, and if he were to deteriorate further the end of life pathway would be most appropriate. The discussion was reiterated to the patients’ family, who were in agreement with this. Although he had evidence of an ischaemic stroke on CT of his brain, it was agreed by all clinicians that intervention for this was not as much of a priority as providing optimal palliative care, therefore, a minimally invasive method of treatment was advocated by the stroke team. The patient was given 300 mg of aspirin and was not a candidate for fibrinolysis.
Outcome and follow-up
The following day, before the throat swab result, had appeared the patient deteriorated further, requiring 15 L of oxygen through a non-rebreather face mask at 60% FiO 2 to maintain his oxygen saturation, at a maximum of 88% overnight. At this point, he was unresponsive to voice, with a GCS of 5. Although, he was still haemodynamically stable, with a blood pressure of 126/74 mm Hg and a heart rate of 98 beats/min. His respiratory rate was 30 breaths/min. His worsening respiratory condition, combined with his declining level of consciousness made it impossible to clinically assess progression of the neurological deficit generated by his cerebral infarction. Moreover, the patient was declining sharply while receiving the maximal ward-based treatment available. The senior respiratory physician overseeing the patients’ care decided that a palliative approach was in this his best interest, which was agreed on by all parties. The respiratory team completed the ‘recognising dying’ documentation, which signified that priorities of care had shifted from curative treatment to palliative care. Although the palliative team was not formally involved in the care of the patient, the patient received comfort measures without further attempts at supporting oxygenation, or conduction of regular clinical observations. The COVID-19 throat swab confirmed a positive result on 2 April 2020. The patient was treated by the medical team under jurisdiction of the hospital palliative care team. This included the prescribing of anticipatory medications and a syringe driver, which was established on 3 April 2020. His antibiotic treatment, non-essential medication and intravenous fluid treatment were discontinued. His comatose condition persisted throughout the admission. Once the patients’ GCS was 5, it did not improve. The patient was pronounced dead by doctors at 08:40 on 5 April 2020.
SARS-CoV-2 is a type of coronavirus that was first reported to have caused pneumonia-like infection in humans on 3 December 2019. 5 As a group, coronaviruses are a common cause of upper and lower respiratory tract infections (especially in children) and have been researched extensively since they were first characterised in the 1960s. 6 To date, there are seven coronaviruses that are known to cause infection in humans, including SARS-CoV-1, the first known zoonotic coronavirus outbreak in November 2002. 7 Coronavirus infections pass through communities during the winter months, causing small outbreaks in local communities, that do not cause significant mortality or morbidity.
SARS-CoV-2 strain of coronavirus is classed as a zoonotic coronavirus, meaning the virus pathogen is transmitted from non-humans to cause disease in humans. However the rapid spread of SARS-CoV-2 indicates human to human transmission is present. From previous research on the transmission of coronaviruses and that of SARS-CoV-2 it can be inferred that SARS-CoV-2 spreads via respiratory droplets, either from direct inhalation, or indirectly touching surfaces with the virus and exposing the eyes, nose or mouth. 8 Common signs and symptoms of the COVID-19 infection identified in patients include high fevers, severe fatigue, dry cough, acute breathing difficulties, bilateral pneumonia on radiological imaging and lymphopaenia. 9 Most of these features were identified in this case study. The significance of COVID-19 is illustrated by the speed of its global spread and the potential to cause severe clinical presentations, which as of April 2020 can only be treated symptomatically. In Italy, as of mid-March 2020, it was reported that 12% of the entire COVID-19 positive population and 16% of all hospitalised patients had an admission to the intensive care unit. 10
The patient, in this case, illustrates the clinical relevance of understanding COVID-19, as he presented with an ischaemic stroke underlined by minimal respiratory symptoms, which progressed expeditiously, resulting in acute respiratory distress syndrome and subsequent death.
Our case is an example of a new and ever-evolving clinical correlation, between patients who present with a radiological confirmed ischaemic stroke and severe COVID-19 pneumonia. As of April 2020, no comprehensive data of the relationship between ischaemic stroke and COVID-19 has been published, however early retrospective case series from three hospitals in Wuhan, China have indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke. 11 These studies have not yet undergone peer review, but they tell us a great deal about the relationship between COVID-19 and ischaemic stroke, and have been used to influence the American Heart Associations ‘Temporary Emergency Guidance to US Stroke Centres During the COVID-19 Pandemic’. 12
The relationship between similar coronaviruses and other viruses, such as influenza in the development of ischaemic stroke has previously been researched and provide a basis for further investigation, into the prominence of COVID-19 and its relation to ischaemic stroke. 3 Studies of SARS-CoV-2 indicate its receptor-binding region for entry into the host cell is the same as ACE2, which is present on endothelial cells throughout the body. It may be the case that SARS-CoV-2 alters the conventional ability of ACE2 to protect endothelial function in blood vessels, promoting atherosclerotic plaque displacement by producing an inflammatory response, thus increasing the risk of ischaemic stroke development. 13
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14
Arrhythmias such as atrial fibrillation had been identified in 17% of 138 COVID-19 patients, in a study conducted in Wuhan, China. 15 In this report, the patient was known to have atrial fibrillation and was treated with rivaroxaban. The acute inflammatory state COVID-19 is known to produce had the potential to create a prothrombotic environment, culminating in an ischaemic stroke.
Some early case studies produced in Wuhan describe patients in the sixth decade of life that had not been previously noted to have antiphospholipid antibodies, contain the antibodies in blood results. They are antibodies signify antiphospholipid syndrome; a prothrombotic condition. 16 This raises the hypothesis concerning the ability of COVID-19 to evoke the creation of these antibodies and potentiate thrombotic events, such as ischaemic stroke.
No peer-reviewed studies on the effects of COVID-19 and mechanism of stroke are published as of April 2020; therefore, it is difficult to evidence a specific reason as to why COVID-19 patients are developing neurological signs. It is suspected that a mixture of the factors mentioned above influence the development of ischaemic stroke.
If we delve further into this patients’ comorbid state exclusive to COVID-19 infection, it can be argued that this patient was already at a relatively higher risk of stroke development compared with the general population. The fact this patient had previously had an ischaemic stroke illustrates a prior susceptibility. This patient had a known background of hypertension and atrial fibrillation, which as mentioned previously, can influence blood clot or plaque propagation in the development of an acute ischaemic event. 15 Although the patient was prescribed rivaroxaban as an anticoagulant, true consistent compliance to rivaroxaban or other medications such as amlodipine, clopidogrel, candesartan and atorvastatin cannot be confirmed; all of which can contribute to the reduction of influential factors in the development of ischaemic stroke. Furthermore, the fear of contracting COVID-19, in addition to his vague symptoms, unlike his prior ischaemic stroke, which demonstrated dense left-sided haemiparesis, led to a delay in presentation to hospital. This made treatment options like fibrinolysis unachievable, although it can be argued that if he was already infected with COVID-19, he would have still developed life-threatening COVID-19 pneumonia, regardless of whether he underwent fibrinolysis. It is therefore important to consider that if this patient did not contract COVID-19 pneumonia, he still had many risk factors that made him prone to ischaemic stroke formation. Thus, we must consider whether similar patients would suffer from ischaemic stroke, regardless of COVID-19 infection and whether COVID-19 impacts on the severity of the stroke as an entity.
Having said this, the management of these patients is dependent on the likelihood of a positive outcome from the COVID-19 infection. Establishing the ceiling of care is crucial, as it prevents incredibly unwell or unfit patients’ from going through futile treatments, ensuring respect and dignity in death, if this is the likely outcome. It also allows for the provision of limited or intensive resources, such as intensive care beds or endotracheal intubation during the COVID-19 pandemic, to those who are assessed by the multidisciplinary team to benefit the most from their use. The way to establish this ceiling of care is through an early multidisciplinary discussion. In this case, the patient did not convey his wishes regarding his care to the medical team or his family; therefore it was decided among intensive care specialists, respiratory physicians, stroke physicians and the patients’ relatives. The patient was discussed with the intensive care team, who decided that as the patient sustained two acute life-threatening illnesses simultaneously and had rapidly deteriorated, ward-based care with a view to palliate if the further deterioration was in the patients’ best interests. These decisions were not easy to make, especially as it was on the first day of presentation. This decision was made in the context of the patients’ comorbidities, including COPD, the patients’ age, and the availability of intensive care beds during the steep rise in intensive care admissions, in the midst of the COVID-19 pandemic ( figure 1 ). Furthermore, the patients’ rapid and permanent decline in GCS, entwined with the severe stroke on CT imaging of the brain made it more unlikely that significant and permanent recovery could be achieved from mechanical intubation, especially as the damage caused by the stroke could not be significantly reversed. As hospitals manage patients with COVID-19 in many parts of the world, there may be tension between the need to provide higher levels of care for an individual patient and the need to preserve finite resources to maximise the benefits for most patients. This patient presented during a steep rise in intensive care admissions, which may have influenced the early decision not to treat the patient in an intensive care setting. Retrospective studies from Wuhan investigating mortality in patients with multiple organ failure, in the setting of COVID-19, requiring intubation have demonstrated mortality can be up to 61.5%. 17 The mortality risk is even higher in those over 65 years of age with respiratory comorbidities, indicating why this patient was unlikely to survive an admission to the intensive care unit. 18
Regularly updating the patients’ family ensured cooperation, empathy and sympathy. The patients’ stroke was not seen as a priority given the severity of his COVID-19 pneumonia, therefore the least invasive, but most appropriate treatment was provided for his stroke. The British Association of Stroke Physicians advocate this approach and also request the notification to their organisation of COVID-19-related stroke cases, in the UK. 19
Learning points
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is one of seven known coronaviruses that commonly cause upper and lower respiratory tract infections. It is the cause of the 2019–2020 global coronavirus pandemic.
The significance of COVID-19 is illustrated by the rapid speed of its spread globally and the potential to cause severe clinical presentations, such as ischaemic stroke.
Early retrospective data has indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke.
Potential mechanisms behind stroke in COVID-19 patients include a plethora of hypercoagulability secondary to critical illness and systemic inflammation, the development of arrhythmia, alteration to the vascular endothelium resulting in atherosclerotic plaque displacement and dehydration.
It is vital that effective, open communication between the multidisciplinary team, patient and patients relatives is conducted early in order to firmly establish the most appropriate ceiling of care for the patient.
- Cannine M , et al
- Wunderink RG
- van Doremalen N ,
- Bushmaker T ,
- Morris DH , et al
- Wang X-G , et al
- Grasselli G ,
- Pesenti A ,
- Wang M , et al
- American Stroke Assocation, 2020
- Zhang Y-H ,
- Zhang Y-huan ,
- Dong X-F , et al
- Li X , et al
- Hu C , et al
- Zhang S , et al
- Jiang B , et al
- Xu J , et al
- British Association of Stroke Physicians
Contributors SB was involved in the collecting of information for the case, the initial written draft of the case and researching existing data on acute stroke and COVID-19. He also edited drafts of the report. MH was involved in reviewing and editing drafts of the report and contributing new data. SP oversaw the conduction of the project and contributed addition research papers.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Next of kin consent obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Telerehabil
- v.14(1); 2022
Implementing Team-Based Post-Stroke Telerehabilitation: A Case Example
Melissa anderson.
1 Kintinu Telerehab, Quality Living, Inc., Omaha, Nebraska, USA
Brad Dexter
Ana hancock, nealey hoffman, steve kerschke, dipika aggarwal.
2 Department of Neurology, University of Kansas Health System, Kansas City, Kansas, USA
Access to extensive, interdisciplinary rehabilitation following stroke is necessary to optimize recovery. Telerehabilitation is an appropriate model for delivering these services. However, given its relatively recent increase in popularity as a service delivery model, researchers have yet to explore the feasibility of interprofessional coordination and collaboration as a guiding framework for telerehabilitation and the effects of team-based remote service delivery on recovery of body functions and activities. This case example reports the development, implementation, and progression of a post-acute treatment program delivered via telerehabilitation to a woman with left hemorrhagic stroke. As is typical, therapy time alone afforded insufficient practice to exploit neuroplasticity and ensure maintenance and generalization of improved functioning; hence, the team worked collaboratively to encourage interdisciplinary activities outside scheduled treatment sessions. Standardized and informal assessments administered at the start and conclusion of treatment confirmed improved functioning as did the client's progress toward independent living and return to work. Implications for telerehabilitation practices are discussed.
Timely access to extensive rehabilitation is essential for promoting neuroplasticity and optimizing functional recovery after stroke ( Belagaje, 2017 ). As the coronavirus disease 2019 (COVID-19) pandemic persisted in 2020 and 2021, hospital systems had to postpone or cancel many in-person, post-acute rehabilitation services, thus substantially interfering with the application of best practices to post-stroke management ( Buheji & Hassani, 2020 ; Stein et al., 2020 ). In response, telerehabilitation grew as an alternative delivery method for physical therapy (PT), occupational therapy (OT), and speech-language pathology (SLP) services ( American Physical Therapy Association, 2020 ; Buheji & Hassani, 2020 ; Moradi et al., 2021 ; Prabawa et al., 2021 ; Stein et al., 2020 ; Tenforde et al., 2020 ). However, given that remote service delivery has only recently surged in popularity, researchers have yet to explore how reliance on accepted methods of best practice for stroke rehabilitation—such as incorporating a team-based approach to service delivery that incorporates interprofessional care plans and interdisciplinary team meetings ( Careau et al., 2008 ; Clarke & Forster, 2015 ; Heuer et al., 2019 ; Stroke Unit Trialists' Collaboration, 2013 ; Yagura et al., 2005 )—occurs with telerehabilitation. In particular, interdisciplinary coordination of therapeutic activities to implement team-based post-stroke telerehabilitation warrants examination as does the overall efficacy of the service delivery model for achieving clients' long-term goals.
Telerehabilitation can be an effective service delivery method for specific aspects of post-stroke care ( Macoir et al., 2017 ; Tchero et al., 2018 ). For example, Cramer et al. (2019) compared upper extremity improvements for 124 adults with stroke receiving either telehealth or dose- and intensity-matched in-clinic treatment and found comparable improvement across groups. By monitoring exercise program participation by Veterans with chronic stroke receiving PT via telehealth, Miller et al. (2014) documented increases in the variety of exercises and number of repetitions performed. Regarding SLP, Meltzer et al. (2017) delivered either in-clinic or telepractice sessions to 44 adults with aphasia or cognitive-communication disorder secondary to stroke and, apart from communication confidence, found statistically equivalent pre- to post-intervention gains regardless of treatment delivery method.
Documentation of telerehabilitation's usefulness is important from the standpoint of establishing efficacy for individual aspects of post-stroke treatment; however, most people sustaining stroke experience deficits across a range of physical and communicative functions and receive concurrent treatment from an interdisciplinary team of professionals working collaboratively. Indeed, considerable evidence supports the notion that interdisciplinary, team-based approaches to stroke rehabilitation are superior to isolated treatments ( Clarke & Forster, 2015 ; Stroke Unit Trialists' Collaboration, 2013 ; Yagura et al., 2005 ). Such approaches optimize rehabilitation by encouraging professionals to be creative in working collaboratively to meet unique and personalized client goals. Team-based approaches promote the sharing of expertise and professional skills across disciplines to recognize overlapping and supportive treatment opportunities that facilitate functional gains in domains important to a client ( Clarke & Forster, 2015 ; Stroke Unit Trialists' Collaboration, 2013 ).
Recent restrictions to in-person treatment and increased reliance on telerehabilitation secondary to the COVID-19 pandemic give rise to questions about team-based procedures professionals can implement to provide mutually supportive intervention services. The purpose of this case example was to document the development, implementation, and progression of a person's post-acute treatment when delivered by an interdisciplinary team of telerehabilitation specialists. The case serves as an example of PT, OT, and SLP professionals working collaboratively with a client to achieve meaningful progress toward long term goals by incorporating functional therapeutic tasks in a natural environment that provides multiple opportunities for repetitive practice. We received permission to access case information from the Institutional Review Board before initiating any review of treatment records, and the subject of the case example, Dipika Aggarwal 1 , signed a consent form acknowledging her willingness to participate.
CASE DESCRIPTION
Dipika was 37 years old, living independently, and working fulltime as a hospital-based neurologist when she sustained a moderate stroke (NIH Stroke Scale = 11). The etiology was a subarachnoid hemorrhage caused by a ruptured aneurysm at the left middle cerebral artery bifurcation. After neurosurgery and 2 weeks of medical stabilization in an intensive care unit, Dipika transferred to an acute rehabilitation facility for 5.5 weeks of treatment for right hemiplegia and aphasia. She then transferred to a non-hospital, post-acute, inpatient rehabilitation program for an additional 5 weeks of intensive PT, OT, SLP, life path, and counseling services followed by 2 months of daily outpatient PT, OT, and SLP services. An unrelated medical condition requiring surgical intervention then forced return to an acute care hospital. Recovery extended over several weeks, and, when ready to resume therapy for stroke-related deficits, COVID-19 restrictions limited Dipika's treatment options. For the next month, she received 30 minute PT and OT sessions three times per week and a total of two SLP sessions from a home health service provider. Dissatisfaction with progress prompted her to seek services via telerehabilitation as an alternative. She began telerehabilitation services 7 months post-stroke. Initial sessions in each discipline lasted 60 minutes and occurred three times weekly; the frequency and intensity of PT and OT sessions remained unchanged over the next year, whereas SLP sessions gradually declined to 30 minutes every other week. Figure 1 depicts the progression of Dipika's treatment through various medical and rehabilitation facilities and service providers.

Progression of Medical and Rehabilitation Service Provision
Dipika's telerehabilitation team had previously worked on collaborative interdisciplinary teams within an inpatient rehabilitation setting. This experience provided them with substantial training and experience implementing team-based services, and they transferred many skills from their inpatient practice to telerehabilitation operations. However, because limited literature exists about applying an interprofessional approach to remote service delivery, the team engaged in ongoing learning and discussion to refine their communication strategies, meeting formats, and overall efficiency.
The first step pursued by Dipika's clinicians was to perform discipline-specific assessments at the initiation of telerehabilitation services. This served as the basis for developing a “problem list” and establishing preliminary functional goals. Dipika's reduced range of motion, strength, and fine motor coordination in the right upper extremity interfered with performing basic and instrumental activities of daily living; she relied primarily on her nondominant, left arm and hand to perform grooming, dressing, and feeding tasks, and she was dependent on family members for meal preparation and home management. Dipika's decreased stamina, balance problems, and gait abnormalities interfered with walking, and she used a single-point cane for stabilization. Regarding communication, Dipika's struggles with word retrieval limited conversational participation. She also needed support to comprehend and retain lengthy information presented through the auditory or written modality.
The clinical team held a preliminary meeting to share their assessment findings. As a clinician likely to have substantial involvement in Dipika's program, her physical therapist assumed primary ownership of the case and facilitated the 10- to 15-minute meeting to establish a comprehensive treatment plan and identify shared goals. In accordance with suggestions from TeamSTEPPS ® 2.0 (Agency for Healthcare Research and Quality, 2019 ), the structured meeting format encouraged an efficient yet thorough means of sharing of information and developing a treatment plan. The team leader then recorded details about the developed program in an easy-to-access, shared document that served as a guide for future meetings. Specifically, they modified the “I Pass the Baton” tool from TeamSTEPPS ® to one they called, “Pass It On.” Table 1 provides a “Pass It On” template with an explanation of type of content for inclusion in each category and Dipika's information inserted in the right hand column.
Pass It on Content Categories, Explanations, and Case Example Information
The clinical team then met with Dipika to discuss her long-term goals. These included resuming independent living, returning to work, and organizing and hosting a stroke support group. The discipline-specific objectives appearing in Figure 2 served as a means of facilitating achievement of the long-term goals. Scheduled treatment sessions provided opportunities to present instructions and monitor exercise performance and strategy implementation. However, therapy sessions alone afforded insufficient practice to promote neuroplasticity and ensure maintenance and generalization of improved functioning. To address this problem, the treatment team met remotely every two weeks to brainstorm interdisciplinary ways of capitalizing on Dipika's intrinsic motivation, access to materials in her environment, and professional understanding of neuroplasticity concepts to implement therapy-related activities outside scheduled telerehabilitation sessions.

Discipline-specific Objectives to Facilitate Long-term Goal Achievement
As the treatment team leader, Dipika's physical therapist assumed responsibility for keeping the program on track, facilitating communication with all stakeholders, and guiding other programmatic related discussions. He did this during five- to 10-minute check-ins that were part of a larger meeting at which the team reviewed all current and newly scheduled clients. Additionally, the team utilized Microsoft 365 ® applications to support communication, collaboration, information sharing, and accountability; they used Microsoft Teams for instant chat and video calls and the Planner application to assign tasks and offer discussion topics for the bi-weekly meetings. Examples of interdisciplinary activities appropriate for Dipika and the disciplines targeted appear in Table 2 ; these example activities were supplemental to continued engagement in discipline-specific tasks.
Interdisciplinary Activities to Augment Telerehabilitation Sessions
Dipika improved steadily over the one-year course of telerehabilitation services while residing with a family member. Results of standardized and informal assessments administered at the start and conclusion of telerehabilitation appear in Table 3 and provide evidence of improvement. Further evidence was Dipika's resumption of functional activities performed prior to her stroke and consistent with her desire to live independently and return to her previous employment. For example, at 9 months post-stroke, Dipika began assuming responsibility for preparing simple breakfast and lunch meals for herself; one month after that, she returned to performing home management tasks such as doing laundry; and, after another two months, she initiated resumption of work responsibilities by passing continuing education exams and observing neurosurgeries. By the conclusion of telerehabilitation services, Dipika was working remotely two days per week, coordinating and hosting a support group for people with stroke, and preparing to return to independent living.
Standardized and Informal Assessment Results at the Initiation and Conclusion of Telerehabilitation
Growing evidence supports the appropriateness of relying on telerehabilitation for delivering services to people needing intensive treatment over multiple months ( Buheji & Hassani, 2020 ; Cramer et al., 2019 ). Telerehabilitation services for the presented case started seven months post-stroke. Despite the length of time that had elapsed since stroke onset, the client's improvement was substantial and represented important progress toward independent living and work resumption goals. The improvement achieved provides evidence of the effectiveness of telerehabilitation for promoting recovery by people with chronic stroke challenges as well as the value of combining discipline-specific and interdisciplinary activities into a comprehensive treatment program.
Much extant research documenting the benefits of team-based approaches to stroke care relate to acute hospital or inpatient rehabilitation settings (e.g., Stroke Unit Trialists' Collaboration, 2017 ; Yagura et al., 2003 , 2005 ); less information is available about the benefits of interdisciplinary teams on post-acute recovery. However, encouraging professionals to work in an interdisciplinary fashion is likely to increase efficacy regardless of recovery stage because of the reduction in service fragmentation and duplication that results from engagement in team planning. In addition, team-based approaches promote client-centered services that address individualized goals and enhance quality of life ( Clarke, 2010 ; Markle-Reid et al., 2011 ).
Applying an interdisciplinary team approach to telerehabilitation has a similar potential to bolster treatment efficacy as it does for in-person service delivery. A critical factor, however, is that team efforts must extend beyond being merely multidisciplinary; only when team members share comparable status, exhibit mutual respect, and collaborate fully in an interdisciplinary fashion to make and implement treatment decisions are the benefits of integrated team action realized ( Atwal & Caldwell, 2005 ; Clarke & Forster 2015 ). Although this coordination requires time and a commitment to cooperation, substantial benefits result from merging the collective knowledge and specialized skills of diverse rehabilitation professionals. Regarding the case presented herein, the benefit was evident in the incorporation of interdisciplinary activities that encouraged numerous repetitions, served a functional purpose in the client's daily life, and aided her efforts toward further recovery and achievement of long-term goals.
An important aspect of the implemented teamwork was the incorporation of meaningful activities using readily available materials and serving functional purposes within the client's living environment. This represents a potential advantage of telerehabilitation over in-person rehabilitation. Although in-person practitioners may strive to make treatment activities meaningful and personalized, having access to a client's home environment facilitates this process and makes it easy to suggest adaptations and alternative methods of performing difficult tasks ( Temkin et al., 1996 ). For example, instead of practicing stair climbing on an artificial staircase available in a clinic setting, telerehabilitation practitioners use the stairs and railings in a person's dwelling; instead of preparing meals in an adapted kitchen, telerehabilitation practitioners provide meal preparation instruction using tools and equipment available in a client's personal kitchen; and instead of working on reading with generic books or magazines available in a clinic or accessible online, telerehabilitation practitioners use materials a client has and wants to read for leisure or work purposes. The realism and personalization afforded by these types of activities optimize motivation and engagement—two crucial factors given the need for a multitude of repetitions to promote neuroplasticity and maximize recovery.
STUDY LIMITATIONS
Limitations are inherent when using case examples to examine rehabilitation practices or glean evidence about treatment efficacy. Case examples lack the scientific rigor associated with controlling and manipulating variables for hypothesis testing purposes. Furthermore, specific aspects of the case presented herein add to its uniqueness and lessen the appropriateness of generalizing the results. Specifically, the client was highly knowledgeable about stroke recovery and neuroplasticity because of her profession; she may also have had relatively high cognitive reserve in comparison to other people. As such, the telerehabilitation team did not need to expend effort convincing her of the benefit associated with extensive task repetition; unlike what sometimes occurs with other clients, her full participation in treatment never wavered. Also, the client's relative youth, strong family support, and long-term access to rehabilitation services were advantageous for recovery; not all clients have such advantages or resources. Still, despite these caveats, the client's achievements provide a valid example of post-stroke recovery attained with services delivered by a collaborative team of telerehabilitation specialists working in an interdisciplinary fashion.
Telerehabilitation as an alternative to in-person services has, at least in part, gained popularity because of restrictions imposed by the COVID-19 pandemic. Factors such as client and therapist convenience, cost, and evidence of effectiveness are likely to affect the long-term acceptance of telerehabilitation as a preferred service delivery method. A risk to this acceptance is the potential for professionals to work in isolation rather than as an interdisciplinary team. As such, establishing ways in which professionals can work collaboratively and cooperatively when delivering services via telecommunication technologies is critical. Using an interdisciplinary team approach can serve as a tool to maximize recovery by promoting neuroplasticity through activity repetition and encouraging maintenance and generalization of improved functioning to activities occurring outside scheduled treatment sessions.
1 Client's identity revealed at her request.
- Agency for Healthcare Research and Quality (2019, March ). TeamSTEPPS fundamentals course: Module 3. Communication . https://www.ahrq.gov/teamstepps/instructor/fundamentals/module3/igcommunication.html [ Google Scholar ]
- American Physical Therapy Association. (2020). Impact of COVID-19 on the physical therapy profession: A report from the American Physical Therapy Association . American Physical Therapy Association. https://www.apta.org/contentassets/15ad5dc898a14d02b8257ab1cdb67f46/impact-of-covid-19-on-physical-therapy-profession.pdf [ Google Scholar ]
- Atwal, A., & Caldwell, K. (2005). Do all health and social care professionals interact equally: A study of interactions in multidisciplinary teams in the United Kingdom . Scandinavian Journal of Caring Sciences , 19 ( 3 ), 268–273. 10.1111/j.1471-6712.2005.00338.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Belagaje, S. R. (2017). Stroke rehabilitation . Continuum: Lifelong Learning in Neurology , 23 ( 1 ), 238–253. 10.1212/CON.0000000000000423 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buheji, M., & Hassani, A. (2020). Design of lean tele-rehabilitation services for post COVID-19 pandemic . International Journal of Advanced Research in Engineering and Technology , 11 ( 11 ), 1360–1371. 10.34218/IJARET.11.11.2020.123 [ CrossRef ] [ Google Scholar ]
- Careau, E., Vincent, C., & Noreau, L. (2008). Assessing interprofessional teamwork in a videoconference-based telerehabilitation setting . Journal of Telemedicine and Telecare , 14 ( 8 ), 427–434. 10.1258/jtt.2008.080415 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clarke, D. J. (2010). Achieving teamwork in stroke units: The contribution of opportunistic dialogue . Journal of Interprofessional Care , 24 ( 3 ), 285–297. 10.3109/13561820903163645 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clarke, D.J., & Forster, A. (2015). Improving post-stroke recovery: The role of the multidisciplinary health care team . Journal of Multidisciplinary Healthcare , 8 , 433–442. 10.2147/JMDH.S68764 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cramer, S.C., Dodakian, L., Le, V., See, J., Augsburer, R., McKenzie, A., Zhou, R.J., Ghiu, N.L., Heckhausen, J., Cassidy, J.M., Scacchi, W., Smith, M.T., Barrett, A.M., Knutson, J., Edwards, D., Putrino, D., Argawal, K., Ngo, K., Roth, E.J., … Janis, S. (2019). Efficacy of home-based telerehabilitation vs in-clinic therapy for adults after stroke . JAMA Neurology , 76 ( 9 ), 1079–1087. 10.1001/jamaneurol.2019.1604 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heuer, A., Hector, J.R., & Cassell, V. (2019). An update on telehealth in allied health and interprofessional care . Journal of Allied Health , 48 ( 2 ), 140–147. [ PubMed ] [ Google Scholar ]
- Macoir, J., Sauvageau, V.M., Boissy, P., Tousignant, M., & Tousignant, M. (2017). In-home synchronous telespeech therapy to improve functional communication in chronic poststroke aphasia: Results from a quasi-experimental study . Telemedicine and e-Health , 23 ( 8 ), 630–639. 10.1089/tmj.2016.0235 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Markle-Reid, M., Orridge, C., Weir, R., Browne, G., Gafni, A., Lewis, M., Walsh, M., Levy, C., Daub, S., Brien, H., Roberts, J. & Thabane, L. (2011). Interprofessional stroke rehabilitation for stroke survivors using home care . Canadian Journal of Neurological Sciences , 38 ( 2 ), 317–334. 10.1017/S0317167100011537 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Meltzer, J.A., Baird, A.J., Steele, R.D., & Harvey, S. J. (2017). Computer-based treatment of poststroke language disorders: A non-inferiority study of telerehabilitation compared to in-person service delivery . Aphasiology , 32 ( 3 ), 290–311. 10.1080/02687038.2017.1355440 [ CrossRef ] [ Google Scholar ]
- Miller, K., Chumbler, N.R., Carlson, K., & Daggett, V. (2014). Tele-rehabilitation to promote exercise in Veterans post-stroke: An observational pilot study . International Journal of Physical Medicine and Rehabilitation , 2 ( 3 ), 1–5. 10.4172/2329-9096.1000200 [ CrossRef ] [ Google Scholar ]
- Moradi, V., Babaee, T., Esfandiari, E., Lim, S.B., & Kordi, R. (2021). Telework and telerehabilitation programs for workers with a stroke during the COVID-19 pandemic: A commentary . Work , 68 , 77–80. 10.3233/WOR-203356 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prabawa, I.M.Y., Silakarma, D., & Widnyana, M. (2021). Telerehabilitation as a physical therapy solution for the post-stroke patient in COVID-19 pandemic situations: A review . Intisari Sains Medis , 12 ( 1 ), 1–5. 10.15562/ism.v12i1.873 [ CrossRef ] [ Google Scholar ]
- Stein, J., Visco, C.J., & Barbuto, S. (2020). Rehabilitation medicine response to the COVID-19 pandemic. Advance online publication . American Journal of Physical Medicine & Rehabilitation . 10.1097/PHM.0000000000001470 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stroke Unit Trialists' Collaboration. (2013). Organised inpatient (stroke unit) care for stroke . Cochrane Database of Systematic Reviews . 10.1002/14651858.CD000197.pub3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tchero, H., Tabue-Teguo, M., Lannuzel, A., & Rusch, E. (2018). Telerehabilitation for stroke survivors: Systematic review and meta-analysis . Journal of Medical Internet Research , 20 ( 10 ), e10867. 10.2196/10867 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Temkin, A.J., Ulicny, G.R., & Versarovich, S. H. (1996). Telerehab: A perspective of the way technology is going to change the future of patient treatment . Rehab Management , 9 ( 2 ), 28–30. [ PubMed ] [ Google Scholar ]
- Tenforde, A.S., Borgstrom, H., Polich, G., Steere, H., Davis, I.S., Cotton, K., O'Donnell, M., & Silver, J. K. (2020). Outpatient physical, occupational, and speech therapy synchronous telemedicine: A survey study of patient satisfaction with virtual visits during the COVID-19 pandemic . American Journal of Physical Medicine & Rehabilitation . Advance online publication. 10.1097/PHM.0000000000001571 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yagura, H., Miyai, I., Seike, Y., Suzuki, T., & Yanagihara, T. (2003). Benefit of inpatient multidisciplinary rehabilitation up to 1 year after stroke . Archives of Physical Medicine and Rehabilitation , 84 ( 11 ), 1687–1691. 10.1053/S0003-9993(03)00286-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yagura, H., Miyai, I., Suzuki, T., & Yanagihara, T. (2005). Patients with severe stroke benefit most by interdisciplinary rehabilitation team approach . Cerebrovascular Diseases , 20 ( 4 ), 258–263. 10.1159/000087708 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Stroke rehabilitation...

Stroke rehabilitation in adults: summary of updated NICE guidance
Linked practice.
Caring is the invisible piece of the stroke recovery puzzle
- Related content
- Peer review
- Eugene Tang , NIHR clinical lecturer in general practice 1 ,
- Nicola Moran , stroke physiotherapist 2 ,
- Mark Cadman , lay member 3 4 ,
- Stephen Hill , lay member 3 4 ,
- Claire Sloan , health economist 3 ,
- Elizabeth Warburton , consultant stroke physician 3 5
- on behalf of the guideline committee
- 1 Population Health Sciences Institute, Newcastle University, UK
- 2 Belfast Health and Social Care Trust, Northern Ireland
- 3 National Institute for Health and Care Excellence, London
- 4 Public representative
- 5 Cambridge University Hospitals, Cambridge
- Correspondence to E Tang ( eugene.tang{at}newcastle.ac.uk )
What you need to know
Stroke rehabilitation total therapy time should be based on the person’s needs, with the amount increasing to at least three hours a day on at least five days a week
Fatigue is common; use a validated scale for early assessment
Offer vision and hearing assessment
Consider referral to community participation programmes suited to the person’s rehabilitation goals
Introduction
Globally, stroke is the second leading cause of death and the third leading cause of death and disability combined. 1 Around 100 000 people have strokes each year, and around 1.3 million people in the UK have survived a stroke. 2 High quality rehabilitation can minimise the physical, emotional, cognitive, and social impacts for people who have had a stroke and their carers, and yield substantial cost savings to society. 3
The National Institute for Health and Care Excellence (NICE) first published guidance on stroke rehabilitation in adults in 2013. 4 The guidance was updated in October 2023 to include appraisal of new evidence. 5 This guideline summary covers selected new and updated recommendations in the 2023 update, and will focus on those most relevant to primary care and community rehabilitation settings.
Recommendations
NICE recommendations are based on systematic reviews of best available evidence and explicit consideration of cost effectiveness. When minimal evidence is available, recommendations are based on the guideline development group’s experience and opinion of what constitutes good practice. Evidence levels for the recommendations are given in italics in square brackets. Evidence certainty is based on GRADE criteria ( box 1 ).
GRADE Working Group grades of evidence
High certainty—we are very confident that the true effect lies close to that of the estimate of the effect.
Moderate certainty—we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low certainty—our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect.
Very low certainty—we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
Transfer of care from hospital to community
Before the person who has had a stroke is transferred from the hospital into the community, a prompt assessment should be carried out by members of the core multidisciplinary stroke rehabilitation team ( box 2 ). 5 Offer early supported discharge from the hospital to the community when people who have had a stroke can move from a bed to a chair independently, or with assistance, as long as a safe and secure environment can be provided. 4 5 Previously, early supported discharge was recommended for select people, however this recommendation was updated because qualitative research showed that rehabilitation support after hospital is often withdrawn from people who have had a stroke even when they need more rehabilitation or when the person thought it was too early.
Core multidisciplinary stroke rehabilitation team
Stroke rehabilitation, which comprises functional task practice, motor, cognitive, and visual rehabilitation, nutritional support, and communication and swallow therapy, is commenced within acute inpatient care in hospital and continued into the community for as long as it continues to help people who have had a stroke to achieve their treatment goals.
This is delivered by core members of the multidisciplinary team:
Stroke physician(s)
Physiotherapists
Occupational therapists
Speech and language therapists
Orthoptists
Clinical psychologists
Once the person has left hospital after having a stroke, continue their care and rehabilitation for as long as it continues to help them achieve their treatment goals.
[Recommendations based on a mixed methods analysis of qualitative and mostly low quality evidence from randomised controlled trials (including a Cochrane systematic review), and on the guideline committee’s experience and expertise]
Intensity of stroke rehabilitation
Increasing evidence suggests that greater doses and intensity of therapy improve motor function and functional independence measures. Evidence reviews of individual rehabilitation therapies found that intensive physiotherapy of one to two hours a day resulted in improvements in activities of daily living, and people who have had a stroke reported faster recovery, especially within the first six months, compared with usual care.
For people receiving occupational and speech and language therapies, the committee concluded that the number of studies to determine specific minutes of intervention was limited. However, in view of how therapy is delivered (such as joint sessions) and alongside the evidence for physiotherapy, a recommendation was made for total therapy time (inclusive of physiotherapy, occupational, and speech and language therapies) of at least three hours on at least five days a week. This was supported by a health economic analysis of higher intensity physiotherapy compared with standard practice (one to two hours, five days a week compared with <45 minutes, five days a week) showing cost effectiveness, alongside long term health benefits. 5
Offer needs-based rehabilitation to people after stroke. This should be for at least three hours a day, on at least five days of the week, and cover a range of multidisciplinary therapies including physiotherapy, occupational therapy, and speech and language therapy.
Where it is agreed with the person after stroke that they are unable, or do not wish, to participate in rehabilitation therapy for at least three hours a day, on at least five days of the week, ensure that any therapy needed is still offered for a minimum of five days per week.
[Recommendations based on very low and low quality evidence from randomised controlled trials, economic modelling results, and on the guideline committee’s experience and expertise]
Feeling tired with a lack of energy is very common following stroke, 6 and for some patients who have had a stroke, it is the most difficult issue they cope with. For most, fatigue is self-limiting (resolving within a year), however for up to 40% it persists for more than two years. 6 Some patients are also low in mood. Performing an assessment of fatigue, both in the early stages and at a six month review, is a new recommendation driven by feedback from stakeholders and patients. One of three validated scales (fatigue severity scale, fatigue assessment scale, modified fatigue impact scale) was recommended based on published work on validity and reliability.
Consider a standardised assessment of fatigue in people after stroke in the early stage of their rehabilitation programme and at their six month stroke review.
[Recommendations based on validity and reliability studies (as no assess-to-treat studies were identified) and on the guideline committee’s experience and expertise]
Sensory disturbance: vision and hearing
If visual and hearing impairments following a stroke go undetected, it can affect the person’s quality of life and ability to engage with rehabilitation. Visual problems in acute stroke can affect more than half of patients who have had a stroke. 7 Compared with the previous guideline, a stronger recommendation to perform a visual assessment urgently was made because of the potential consequences of undetected vision problems (eg, accidents related to driving, or falls). Screening patients for hearing difficulties within six weeks is a new recommendation.
Offer people who are in hospital after stroke a specialist orthoptist assessment as soon as possible. If this cannot be done before discharge, offer the person an urgent outpatient appointment.
Screen people for hearing problems within the first six weeks after stroke.
Consider the Handicap Hearing Inventory in the Elderly or Amsterdam Inventory Auditory of Disability questionnaires for screening.
During screening, ask the person, and their family members and carers, about any changes to their hearing since the stroke.
Refer people with hearing difficulties for an audiology assessment, in line with NICE’s guideline on hearing loss in adults.
[Based on the experience and opinion of the guideline development group]
Community participation programmes
Involving patients in community participation programmes as part of their rehabilitation is a new recommendation. Examples of programmes include group based physical exercise, art, and music activities. In the evidence review, a wide range of outcomes were assessed including health related quality of life (person and carer), return to work, wellbeing, psychological distress, stroke specific patient reported outcome measures, and discontinuation. Those participating in programmes, broadly, had improved quality of life compared with those who did not, but the extent of the improvement varied substantially across studies.
Consider referring people after stroke, and their families and carers (if appropriate), to community participation programmes that:
are suited to the person’s rehabilitation goals and
take into account their needs, views, and preferences in line with NICE’s guideline on patient experience in adult NHS services.
[Recommendations based on very low and low quality evidence from randomised controlled trials, and on the guideline committee’s experience and expertise]
Implementation
As part of an updated National Stroke Service model, the integrated community stroke service now coordinates the transfer of care from hospital to community settings, and provides needs based stroke rehabilitation in the community, seven days a week. 8 Recommendations around early supported discharge and treatment intensity complement this new service model. Early supported discharge is likely to vary, with some regions not having a dedicated early supported discharge coordinator, and services will need to adapt to improve equitable access for all patients. Increasing the intensity of therapy will have substantial implications for therapists who deliver the programme. A change in how therapists deliver the sessions, such as group work, semi-supervised practice, and use of technology to deliver the session remotely, may be required.
Recommendations related to objective assessment of fatigue will lead to increased use of tools as part of standardised follow-up, alongside more personalised advice and person centred support or signposting. Recommending that all patients receive regular hearing and visual assessments will lead to an increase in inpatient and outpatient referrals to orthoptist and audiology services.
Access to community participation programmes varies across the country. Demand for these programmes will increase, and patients may request healthcare professionals to signpost these programmes, for example through social prescribing link workers. Because of the differences in commissioning and delivery of these programmes at a national scale, including programmes delivered purely by charities through funding from grants, appropriate funding may not meet demand for services.
Future research
The guideline committee prioritised the following for further research:
What is the clinical and cost effectiveness of delivering rehabilitation for seven days a week compared with five days a week for people after a stroke?
What is the clinical and cost effectiveness of more intensive cognitive and psychological therapy compared with usual care for people after a stroke?
For people after stroke with communication difficulties, what is the optimal tool for assessing fatigue?
Guidelines into practice
Think about the last time you had a consultation with a patient who had a stroke. What were the rehabilitation goals and needs of the patient and how did you navigate services locally to meet them?
What community participation groups are available locally for patients?
Further information on the guidance
This guidance was developed by the Guideline Development Team in accordance with NICE guideline methodology ( www.nice.org.uk/media/default/about/what-we-do/our-programmes/developing-nice-guidelines-the-manual.pdf ). A guideline committee (GC) was established by the Guideline Development Team, which incorporated healthcare and allied healthcare professionals (one neurorehabilitation physician, one neuropsychologist, one neurophysiotherapist, one stroke physiotherapist, one stroke physician, one general practitioner, one stroke specialist nurse, two stroke specialist speech and language therapists, two stroke specialist occupational therapists, one third sector representative, two dietitians, one orthoptist, one social worker) and three lay members.
The guideline is available at https://www.nice.org.uk/guidance/ng236 . The GC identified relevant review questions and collected and appraised clinical and cost effectiveness evidence. Quality ratings of the evidence were based on GRADE methodology ( www.gradeworkinggroup.org ). These relate to the quality of the available evidence for assessed outcomes or themes rather than the quality of the study. The GC agreed recommendations for clinical practice based on the available evidence or, when evidence was not found, based on their experience and opinion using informal consensus methods.
The scope and the draft of the guideline went through a rigorous reviewing process, in which stakeholder organisations were invited to comment; the GC took all comments into consideration when producing the final version of the guideline. NICE will conduct regular reviews after publication of the guidance, to determine whether the evidence base has progressed significantly enough to alter the current guideline recommendations and require an update.
How patients were involved in the creation of this article
Two co-authors MC and SH were lay members of the guideline committee. In addition, committee members involved in this guideline update included three lay members who contributed to the formulation of the recommendations summarised here.
Acknowledgments
The members of the Guideline Committee were (shown alphabetically): Sara Ajina (neurorehabilitation physician), Khalid Ali (stroke physician), Jacqueline Benfield (stroke specialist speech and language therapist), Jon Brown (chair), Mark Cadman (lay member), Adele Collins (dietitian), Catherine Ford (neuropsychologist), Richard Francis (third sector representative), Jeanette Grocott (stroke specialist nurse), Stephen Hill (lay member), David Hearnden (social worker), Chandrika Kaviraj (lay member), Nicola Moran (stroke physiotherapist), Rebecca Palmer (stroke specialist speech and language therapist), Sarah Paterson (neurophysiotherapist), Fiona Rowe (orthoptist), Eugene Tang (general practitioner), Elizabeth Taylor (stroke specialist occupational therapist), Lauren Turner (dietitian), Elizabeth Warburton (topic adviser) and Kaye Wood (stroke specialist occupational therapist).
The members of the NICE technical team (shown alphabetically by surname): Amber Hernaman, Bernard Higgins, Sophia Kemmis-Betty, Nancy Pursey, Joseph Runicles, Claire Sloan, David Wonderling, George Wood, and Madeleine Zucker.
Contributorship and the guarantor: All six authors confirm that they meet all four authorship criteria in the ICMJE uniform requirements. ET is the guarantor for this article. The views expressed in this publication are those of the authors and not necessarily those of NICE.
Funding: No authors received specific funding from NICE to write this summary. ET (NIHR clinical lecturer) is funded by the NIHR. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR, NHS, or the UK Department of Health and Social Care.
Competing interests: We declared the following interests based on NICE’s policy on conflicts of interests ( https://www.nice.org.uk/Media/Default/About/Who-we-are/Policies-and-procedures/declaration-of-interests-policy.pdf ): The guideline authors’ full statements can be viewed at https://www.nice.org.uk/guidance/ng236/documents/register-of-interests
Provenance and peer review: commissioned; not externally peer reviewed.
- GBD 2019 Stroke Collaborators
- ↵ Stroke Association. Stroke statistics. https://www.stroke.org.uk/what-is-stroke/stroke-statistics .
- Berdunov V ,
- Quayyum Z ,
- Wittenberg R
- ↵ National Institute for Health and Care Excellence. Stroke rehabilitation in adults: Clinical guideline [CG162]. 2013.
- ↵ National Institute for Health and Care Excellence. Stroke rehabilitation in adults: Clinical Guideline [NG236] 2023. www.nice.org.uk/guidance/ng236 .
- Paciaroni M ,
- Acciarresi M
- Hepworth LR ,
- Cheyne CP ,
- ↵ National Health Service. National service model for an integrated community stroke service. 2022. https://www.england.nhs.uk/wp-content/uploads/2022/02/stroke-integrated-community-service-february-2022.pdf .

Home > Colleges Schools and Departments > WCHP > Physical Therapy > PT Student Works > PT Student Papers > Case Report Papers
Case Report Papers
During the course of two semesters, UNE Doctor of Physical Therapy students who elect the case report track to fulfill the program’s scholarship requirement work with a faculty advisor to gather data about a patient, institution, facility, or other definable unit related to the profession of physical therapy, and write a case report manuscript following the guidelines, format, and standards for a professional journal.
Papers from 2024 2024
Implementing a Mobility Program with a Complex Patient in an Acute Care Setting: A Case Report , Marisa Carbone, Miguel Vidal, Emma Jones, Haley Yarber, Samantha Strout, Akua Obeng, and Elizabeth Cyr
Papers from 2023 2023
The Effectiveness Of The Six Minute Walk Test For Tracking Progress In Patients With Post-COVID Condition: A Case Report , Jason Angellano, Alexander M. Ferreira, Colleen McGonagle, Yurong Ren, and Michael Tran
Papers from 2021 2021
The Rehabilitation Of A 75-Year-Old Male Presenting With A Right Hip Flexor Strain Concomitant With Numerous Psychosocial Factors: A Case Report , Jillian Battista, Megan Chapski, Suma Varanasi, and Jillian Witwicki
Utilizing An Evidence-Based Practice Framework In Non-Operative ACL Rehabilitation - A Case Report , Eric Norman, Michael Madore, Kathryn Magee, Tyler Calimer, and Parker Nally
Lower Extremity Strengthening, Neuromuscular Re-Education And Graded Activity For A Runner With Distal Hamstring Tendinopathy: A Case Report , Tara Oyasato
Soft Tissue Techniques For Upper Quadrant Range Of Motion And Pain In A Breast Cancer Survivor Following Mastectomy: A Case Report , Marissa Paquette
Papers from 2020 2020
Return To Golf In A 71-Year-Old Female After A Mako Robotic-Arm-Assisted Unicompartmental Knee Arthroplasty Surgery: A Case Report , Katelyn Austin
The Creation Of An Algorithm To Assist Survivorship Clinics Identify The Rehabilitation Needs Of Cancer Survivors: An Administrative Case Report , Joseph Connor
Restoring Functional Mobility For A Patient Following A Comminuted Patella Fracture Status Post Open Reduction Internal Fixation: A Case Report , Elaina Cosentino
Graded Motor Imagery And Pain Neuroscience Education For A Middle-Aged Patient With Chronic Low Back Pain: A Case Report , Brandon Drinan
Inpatient Rehabilitation For A 75-Year-Old Female Following A Left-Sided Pontine Infarct: A Case Report , Marisa Flores
Physical Therapy Management Of Gross Function Loss Following Gunshot Wound To Left Hand: A Case Report , Matthew Freeman
Mobilizations And Strengthening For Radiating Hip And Anterior Knee Pain: A Case Report , Thai Ho
The Challenges Of Exercise Selection For A Post-Operative Patient With Severe Deconditioning And Longstanding Neurogenic Claudication: A Case Report , Madison Lostra
Physical Therapy Emphasizing Progressive Weight Bearing And Gait Training Following Chopart Amputation In A Patient With Diabetes: A Case Report , Spenser Lynass
Restoring Functional Mobility In A 51-Year-Old Male Post Intramedullary Limb Lengthening Surgery Following Helicopter Crash: A Case Report , Shawn Novella
Proprioceptive Neuromuscular Facilitation And Overground Gait Training For A Patient Following A Left Central Medullary Stroke: A Case Report , Shelby Stegemann
Physical Therapy Interventions Via Telehealth For A Child With Developmental Delay During The Covid-19 Pandemic: A Case Report , Julie Sullivan
Papers from 2019 2019
Physical Therapy Management Of Low Back Pain In A Young Female With Ankylosing Spondylitis Associated With HLA-B27 Antigen: A Case Report , Jake Adkins
Regaining Independence In Ambulation For A Visually Impaired Patient With Rhabdomyolysis: A Case Report , Brandon Bourgoin
Gait, Strength, And Balance Training For A 43-Year-Old Male Following An Acute Right Middle Cerebral Artery Stroke: A Case Report , Victoria Dwyer
Functional School-Based Physical Therapy Management For A Child With Pallister-Killian Syndrome: A Case Report , Cheryl R. Espinosa
Balance And Strength Interventions For An Older Individual With Peripheral Polyneuropathy: A Case Report , Hanna Geib
Early Mobilization And Functional Mobility Training For A Patient With Triple Vessel Coronary Artery Bypass Grafting: A Case Report , Cody Hall
Barefoot Training In The Rehabilitation Of Stage II Posterior Tibialis Tendon Dysfunction: A Case Report , Matthew Heindel
Restoring Functional Mobility For A Geriatric Patient Following Open Repair Of A Ruptured Abdominal Aortic Aneurysm: A Case Report , Grace Laughlin
Tissue Plasminogen Activator Effects On Stroke And Physical Therapy Outcomes In Acute Care: A Case Report , Lindsey Leboeuf
A Hip Strengthening Protocol For A Patient Following Achilles Repair: A Case Report , Matthew Morris
Combining A Comprehensive Physical Therapy Program And Electrocorpeal Shockwave Therapy For Plantar Fasciitis: A Case Report , Kathryn Piersiak
Treatment Of A Work-Related Superior Glenoid Labral Repair: A Case Report , Alexandra Touri
Functional Mobility In A Patient With Antiphospholipid Antibody Syndrome Following A Femoral Neck Fracture Surgical Repair: A Case Report , McKenna Young
Papers from 2018 2018
Inpatient Physical Therapy Management For A Patient With Chronic Pulmonary Complications Secondary To Multiple Lobectomies: A Case Report , Bayley Archinal
The Treatment Of Pes Anserine Syndrome Using ACL Injury Prevention Exercises: A Case Report , Stephanie Chau
Comprehensive Physical Therapy Management Of A Patient With Decreased Shoulder Function And A History Of Breast, Lung, And Oral Cancer: A Case Report , Andrew Chongaway
Functional Mobility For A Patient With Myelodysplastic Syndrome, Chronic GVHD, And Corticosteroid Use: A Case Report , Alyssa Deardorff
Restoring Functional Mobility In An Adult Patient Secondary To Subtrochanteric Femur Fracture Surgical Repair: A Case Report , Brittany Gray
A Barefoot Running Program For A College Lacrosse Player With Chronic Exertional Compartment Syndrome: A Case Report , Erica Mazzarelli
The Comprehensive PT Management Of A Patient With Chronic Low Back Pain And Lumbar Radiculopathy: A Case Report , Robin McGuire
A 6 Week Balance And Gait Training Program Using The AlterG For A Patient With Cervical Myelopathy After Spinal Decompression Surgery: A Case Report , Palak Patel
Functional Mobility For An Elderly Patient With Amyotrophic Lateral Sclerosis: A Case Report , Gianna G. Pezzano
Inpatient Rehabilitation Of A 99-Year-Old Patient Following A High-Impact Unstable Pelvic Ring Fracture: A Case Report , Julia Pratt
Relieving Low Back Pain And Improving Mobility For An Adult Patient With Progressive Multifocal Leukoencephalopathy: A Case Report , Derek Schwaiger
Mckenzie Approach To Treating Lumbar Radiculopathy With A Lateral Shift: A Case Report , Carly Theriault
The Use Of Medical Therapeutic Yoga On A Patient With Adhesive Capsulitis: A Case Report , Cameron Vallie
Subacute Physical Rehabilitation For A Young Adult With A Hypoxic Brain Injury Resulting In Severe Myoclonic Movements And Ataxia: A Case Report , Chelsea VanDriel
Conservative Management Of A Complete Rupture Of The Long Head Of The Biceps: A Case Report , Ali Woller
Papers from 2017 2017
Physical Therapy For Low Back Pain With A Focus On McKenzie Method For Diagnosis And Treatment: A Case Report , Macey N. Berube
The Use Of Therapeutic Exercises And Manual Stretching For A Patient Following A Total Knee Arthroplasty (TKA) Revision: A Case Report , Nicholas Cebula
Graston Technique Used In The Treatment Of Patellofemoral Pain In An Ultimate Frisbee Player: A Case Report , Patricia Dobrowski
High Intensity Intervals And Gait Training For A Patient With Heart Failure And Parkinson Disease In A Skilled Nursing Facility: A Case Report , Kelly Fritz
Outpatient Vestibular Rehabilitation For A Patient Three Months Post Acoustic Neuroma Resection: A Case Report , Joel Harrison
Outpatient Physical Therapy Management Of A Total Knee Arthroplasty With Severe Contralateral Knee Osteoarthritis: A Case Report , Michael Ikemura
Balance & Fall Prevention Rehabilitation Program For A 77-Year-Old Patient Following A Trimalleolar Fracture: A Case Report , Kathryn Judd
Adult Scoliosis And Chronic Low Back Pain With Land And Aquatic Based Physical Therapy: A Case Report , Thomas Kent
The Effect Of A Stability And Strengthening Program On The Oswestry Disability Index In A 14-Year-Old Patient With Spondylolisthesis: A Case Report , Hormoz Maragoul
Restoration Of Functional Mobility For A Young Adult Patient Following A Severe Motor Vehicle Accident: A Case Report , Zachary Mercier
Utilization Of Task-Oriented Training To Restore Independence In A Patient With Encephalitis In The Intensive Care Unit: A Case Report , Victoria Perez
The Role Of Physical Therapy Interventions For An Elderly Patient Following Surgical Fixation Of A Fracture Of The Femoral Shaft: A Case Report , Ashley Push
Acute Care Physical Therapy Status Post Laparoscopic Loop Sigmoid Colostomy For A Patient With Colorectal Cancer: A Case Report , Elizabeth Race
The Use Of Manual Lumbar Traction And Therapeutic Exercise In The Treatment Of A Patient With Low Back Pain: A Case Report , Kyle Rasmussen
Vestibular Rehabilitation For A Geriatric Patient With Benign Paroxysmal Positional Vertigo Treatment Failure: A Case Report , Clare Roeder
Strength And Balance Training For A 29-Year-Old Female Who Sustained A Multifocal Stroke: A Case Report , Britney Simonton
Physical Therapy On The Function Of A Patient With Stage III Parkinson’s Disease: A Case Report , Kelly Trancygier
The Physical Therapy Management Of A Patient With Chronic Shoulder Dislocations And Chronic Inflammatory Demyelinating Polyneuropathy: A Case Report , Lindsey Umapathy
A Comprehensive PT Program Utilizing An AlterG Treadmill For A Patient With Lower Extremity Fractures And Charcot-Marie-Tooth Disease: A Case Report , Mark Whitsitt
Utilization Of Postural Control Training To Improve Gait Symmetry And Walking Ability In A Patient Following A Lacunar Stroke: A Case Report , Hannah C. Wilder
Papers from 2016 2016
The Use Of Manual Therapy In The Treatment Of A Patient With Chronic Low Back Pain And Sciatica: A Case Report , Elia N. Darazi
Physical Therapy Intervention For A Patient With Temporomandibular Joint Dysfunction Caused By Two Traumatic Events: A Case Study , Elyse Detweiler
Physical Therapy Management Of A Patient With Chronic Knee Pain: A Case Report , Mohamed Elsaid
Physical Therapy Management Of A Patient With Chronic Brainstem Stroke Syndrome To Improve Functional Mobility: A Case Report , Kelley Flahaven
Therapeutic Exercise In The Treatment Of Greater Trochanteric Pain Syndrome S/P Lumbar Discectomy: A Case Report , Sean Jeffrey
Restoring Gait And Functional Mobility For A Patient With An Ischemic Stroke Through Physical Therapy: A Case Report , Colleen Kelly
Functional Training In A Patient With Middle Cerebral Artery Stroke With Multiple Comorbidities: A Case Report , Darien Lewis
Physical Therapy And Cognitive Behavioral Therapy In A Patient With Multiple Co-Morbidities – A Case Report , Jeanine Manubay
Management Of A Patient With Bronchiectasis Using Pulmonary Rehabilitation And Balance Training: A Case Report , Megan Witherow Quarles
Use Of Functional Strengthening, Balance Training, And Stretching In The Treatment Of A Patient Following A T11-L5 Spinal Fusion: A Case Report , Anna Sidloski
Papers from 2015 2015
Management Of A Patient Lumbar Spinal Stenosis and Carotid Aneurysm Using Therapeutic Exercise, Education, And Manual Therapy: A Case Report , Nicholas Adriance
Application Of A Short-Term Aquatic Physical Therapy Program For A Patient With Chronic Low Back Pain And Radiculopathy: A Case Report , Marc Asta
A Progressive Physical Therapy Plan Of Care For A Patient With Charcot-Marie-Tooth Disease Following Myocardial Infarction: A Case Report , Paige Blasco
Balance And Gait Training To Reduce Fall Risk In A Patient With Bilateral Foot And Hand Deformities Secondary To Rheumatoid Arthritis: A Case Report , Kirsten Bombardier
Body Weight Supported Treadmill Training And Overground Gait Training In The In-Patient Setting For An Individual With Chronic Stroke: A Case Report , Stephanie Bordignon
Evaluation And Treatment Of A Patient Diagnosed With Adhesive Capsulitis Classified As A Derangement Using The McKenzie Method: A Case Report , Ashley Bowser
Use Of The Lower Extremity Functional Scale (LEFS) In A Patient After A First Metatarsophalangeal Joint Implant: A Case Report , Courtney Brinckman
Use Of Core Stabilization Exercise And Medical Exercise Therapy In The Treatment Of A Patient With Chronic Post Partum Low Back Pain: A Case Report , Zachary Chaloner
Gait Training, Strength Training, And Pain Management Of A 26 Year Old Female Recovering From A Multiple Sclerosis Exacerbation: A Case Report , Ellen Cox
The Use Of Parkinson’s Disease Specific Rehabilitative Interventions To Treat A Patient With Lewy Body Dementia: A Case Report , Cassandra Dawley
The Effects Of Specific Training On Balance And Ambulation In A Patient With Stage IV Glioblastoma: A Case Report , Matt Denning
Use Of A Task-Oriented Approach In The Physical Therapy Management Of A Patient Following A Posterior Inferior Cerebellar Artery Stroke: A Case Report , Erika Derks
Treatment Of A Patient With Thoracolumbar Scoliosis Utilizing A Regional Interdependence Approach Including Components Of The Schroth Method: A Case Report , Samantha Fisk
Use Of Therapeutic Exercise, Functional Endurance, And Gait Re-training In A Deconditioned Patient With Acute Respiratory Failure: A Case Report , Ellen Forslund
Neuromuscular Strengthening Exercises Following ACL And Meniscal Repair In A 15 Year Old Female Athlete With Generalized Knee Laxity: A Case Report , Alyssa Gardner
The Use Of Manual Therapy And Strengthening Exercises To Improve Plantarflexion Strength And Mobility Following Achilles Tendon Repair: A Case Report , Jason Glikman
Using The Selective Functional Movement Assessment And Regional Interdependence Theory To Guide Treatment Of An Athlete With Back Pain: A Case Report , Gabriella Goshtigian
Neuromuscular Electrical Stimulation And Quadriceps Strength Following Patellar Fracture And Open Reduction Internal Fixation Surgery: A Case Report , Chelsea Hussey
The Role Of Physical Therapy In The Treatment And Discharge Of An Elderly Homeless Patient With Fractures Of The T12-L1 Vertebrae: A Case Report , Matthew Kraft
Restoring Functional Mobility In A Patient With Delayed Onset Of Physical Rehabilitation Following A Hemorrhagic Stroke: A Case Report , Bettie Kruger
Strength And Balance Exercises To Improve Functional Outcomes And Mobility For A Patient With Parkinson’s Disease And Co-morbidities: A Case Report , Nicholas LaSarso
Functional Mobility Management Of A Patient With Adult-Onset Hereditary Proximal Motor Neuropathy Following A Tibial Fracture: A Case Report , Timothy Lira
Use Of Manual Therapy And Sport Specific Re-training In An Adolescent Elite Sprinter With Bilateral Pedicle Stress Fractures: A Case Report , Erika Lopez
The Use Of Postural Reeducation And Strengthening Exercises In The Reversal Of Functional Scoliosis: A Case Report , Cory Marcoux
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Contributors
- Physical Therapy Department
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
- Case Report
- Open access
- Published: 27 March 2024
Effectiveness of physical therapy on physical activity and employment status in kidney transplant recipients in their sixties: a case report with literature review
- Tomoya Yamaguchi ORCID: orcid.org/0000-0002-6536-7001 1 ,
- Hiroki Yabe 2 ,
- Takayuki Sugiyama 3 ,
- Shinsuke Isobe 4 ,
- Yuma Hirano 1 ,
- Hideo Yasuda 4 ,
- Hideaki Miyake 3 , 5 &
- Katsuya Yamauchi 1
Renal Replacement Therapy volume 10 , Article number: 22 ( 2024 ) Cite this article
59 Accesses
Metrics details
Few reports have been published on preoperative and long-term postoperative rehabilitation after kidney transplantation. Poor physical function after kidney transplantation is associated with adverse events; hence, physical function should be improved postoperatively. We report a case in which physical therapy was provided just before the operation and 12 months postoperatively to improve physical performance.
Case presentation
A 64-year-old man, working as a janitor and maintenance worker at a driving school, received a living-donor kidney transplant from his wife. The just before the operation assessment revealed a decline in his physical function, indicating he had become frail. Accordingly, physical therapy was initiated prior to kidney transplantation. Subsequently, his Short Physical Performance Battery score improved from 10 to 12, and his knee extension muscle strength improved from 0.38 to 0.43 kgf/kg, enabling him to resume work. The work functioning impairment scale improved from 13 to 7.
Conclusions
This case reveals that just before the operation and long-term rehabilitation is crucial in enhancing physical activity in kidney transplantation patients. Although this focused rehabilitation approach holds promise, evaluating its efficacy requires the examination of a larger cohort of cases.
Kidney transplantation has a higher return-to-work rate than other kidney replacement therapies. However, complications associated with kidney transplantation include perioperative disuse syndrome, weight changes, and susceptibility to infection because of steroid and immunosuppressive medication. These complications reduce physical activity, function, and exercise tolerance and increase the risk of frailty [ 1 , 2 ], which may preclude return to the workplace and community. Therefore, medical treatment to preserve transplanted kidney function and post-transplant care is required to improve physical activity and function for returning to the community and employment.
Renal rehabilitation guidelines recommend exercise therapy in patients who undergo kidney transplantation (2C) [ 3 ]. In Japan, the overall decline in the available workforce has necessitated the critical inclusion of older people to maintain essential labor pools. Moreover, employment is vital in sustaining health, physical fitness, and cognitive function. Therefore, evaluating work status along with physical function and activity is pivotal for older renal transplant patients. However, previous reports have focused on younger patients aged 40–50 years and have not adequately demonstrated long-term preoperative to postoperative follow-up in older patients or included a comprehensive physical function, activity, and employment assessment. We encountered a case of a patient undergoing hemodialysis and admitted for kidney transplantation who underwent continuous physical therapy just before the operation for up to 12 months postoperatively. This study aimed to evaluate the influence of physical therapy, particularly on the level of activity performed, in a patient undergoing hemodialysis and admitted for kidney transplantation. The physical therapy intervention commenced before surgery and continued for 12 months post-surgery.
Patient profile
The patient was a 64-year-old man on hemodialysis for 4.2 years for end-stage kidney failure due to diabetic kidney disease. He had a medical history of hypertension, paroxysmal atrial fibrillation, and angina pectoris and had undergone surgery for a calcified amorphous tumor of the left ventricular 1 year before transplantation. Before admission, the patient lived with his spouse, was self-caring, and could transport himself to outpatient dialysis. He was fully independent and worked part-time as a janitor and maintenance worker at a driving school for 3 h, 3 days a week.
Assessment of physical function in rehabilitation
Table 1 presents the data obtained on X −3 days.
The preoperative evaluation ( X –4 days) in rehabilitation encompassed the assessment of muscle strength, walking ability, physical performance, cognitive function, muscle mass, frailty, exercise motivation, and employment status (Table 2 ).
Knee extension muscle strength was assessed using a dynamometer (μTas F-1 handheld dynamometer; Anima, Tokyo, Japan) on three occasions, and the maximum values were used. The ratio of knee extension muscle power to body weight was calculated as representative values for lower extremity muscle strength. Grip strength was measured using a Smedley digital hand dynamometer (101A HATS; Tokyo, Japan), and the highest value from the two measurements was considered. Walking ability was assessed by measuring the 10-m walking speed. Physical performance was assessed using the Short Physical Performance Battery, cognitive function was assessed using the Mini-Mental State Examination, muscle mass was determined by calculating the skeletal muscle index, and frailty was evaluated using the Japanese version of the Cardiovascular Health Study criteria. The patient met three Japanese frailty criteria: grip strength, exercise habits, and fatigue. Exercise motivation was assessed through measurements of exercise self-efficacy (SE). He had no exercise routine—his exercise SE was 14/20. Work functioning impairment scale (WFun) score was 13/35. WFun is composed of seven simple questions, each scored between 1 and 5 points, allowing for a total score ranging from 7 to 35 points. In this scale, a lower score is indicative of better work functioning or a better condition.
Methodology of rehabilitation intervention
The patient’s physical therapy goal was to return to the same job and to travel further distances. His rehabilitation started 4 days before surgery. The just before the operation rehabilitation program included an orientation toward early postoperative rehabilitation interventions, assessment of physical function, and self-training instructions using informational brochures. Postoperatively, we followed a rehabilitation program based on previous studies [ 4 ] to reduce disuse syndrome as much as possible. Specifically, orthostatic and gait training was started on day 4, and aerobic exercise using a bicycle ergometer was started on day 10. Additional exercises, such as squats, wall push-ups, and one-leg standing, were gradually introduced to improve strength and balance. Following renal rehabilitation guidelines, we prescribed five 40-min exercise therapy sessions daily, five times per week [ 3 ].
Outpatient intervention
The patient visited the outpatient clinic every 2–4 weeks for medication management, nutritional counseling, and rehabilitation. We used a self-monitoring sheet to record daily physical changes, independent training activities, number of steps, weight, blood sugar, frequent urination, and amount of water consumed. He maintained a diabetes diary before hospitalization. After his discharge, it was integrated into a self-monitoring sheet, which allowed him to continue the ongoing documentation personally. For outpatient rehabilitation, the target number of steps set was based on his continuous step count recorded during hospitalization and was gradually increased. At each visit, the number of steps was recorded, the target was readjusted accordingly, and visual feedback was provided. The number of steps taken was noted using a graph to visually show the degree of goal attainment; the graph was printed on paper and was distributed each time for visual feedback. We assessed his physical condition using a self-recorded sheet by a physical therapist at each visit.
Postoperative treatment and progress
An ABO non-identical living donor kidney transplant was performed with his spouse as the donor. The left donor kidney was then transplanted into the right pelvic cavity. Immunosuppressive therapies included basiliximab, methylprednisolone, tacrolimus, and mycophenolate mofetil. After kidney transplantation, two additional hemodialysis sessions were required because of delayed graft function. A physical activity tracker device (Lifecorder, Kenz, Suzuken Co., Ltd., Nagoya, Aichi, Japan) was given to the patient after surgery and catheter removal, and he was instructed to incrementally increase the step count by 5000 steps per day during hospitalization and by 5% every month after discharge [ 4 , 5 ]. The patient was discharged on day X + 36. The estimated glomerular filtration rate (eGFR) at discharge was 16 mL/min/1.73 m 2 . His weight during the 12 months post-surgery is shown in Fig. 1 . No adverse events associated with kidney function occurred because of the exercise intervention. Physical function during the 12 months post-surgery is shown in Table 2 . At 6 months, the patient resumed work, and the number of workdays increased from three to five. A total of 12 months later, working hours increased from 3 h to 4.5 h. Furthermore, he was able to travel for one week without worrying about his dialysis appointments.
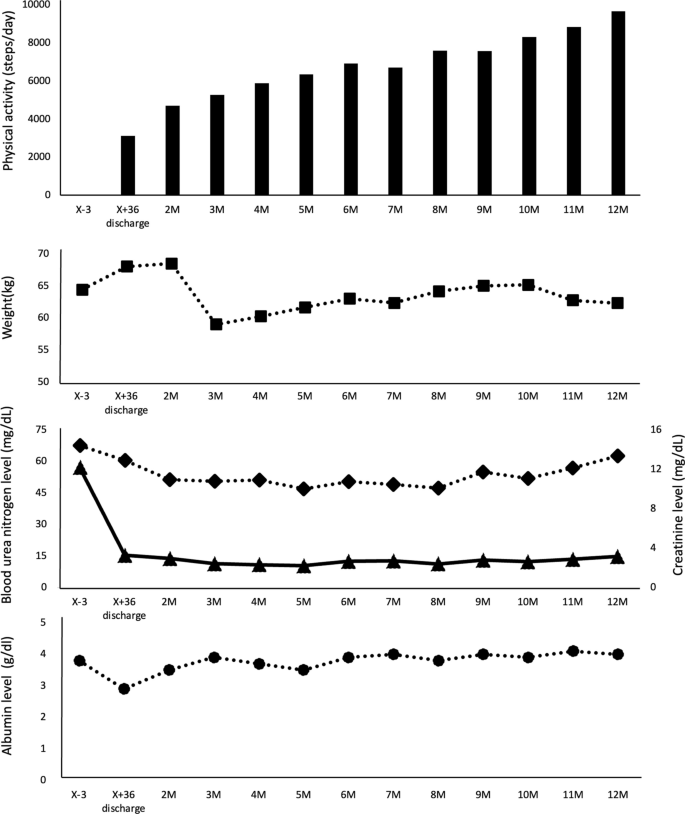
Progress during rehabilitation (physical activity and weight). ◆ , Blood urea nitrogen level; ▲, Creatinine level; ● , Albumin level
Literature review
To our knowledge, there have been three previous studies evaluating physical activity levels (step counts) in renal transplant patients using activity monitors (Table 3 ). In the study conducted by Yamamoto et al. [ 4 ], the effectiveness of early postoperative rehabilitation was compared between a control group receiving usual care and an intervention group undergoing rehabilitation. The intervention group commenced rehabilitation on the sixth day post-surgery and received guidance on physical activity levels for two months post-surgery. While there was no significant difference in step counts between the two groups two months post-surgery, knee extensor strength was substantially higher in the intervention group compared with that of the control group. Furthermore, no adverse events related to exercise intervention on renal function were observed, and estimated glomerular filtration rate (eGFR) exhibited a similar trajectory to that of the control group. In the research by Serper et al. [ 6 ], a randomized controlled trial (RCT) focused on physical activity levels was conducted for three months among renal and liver transplant patients within the first 12 months postoperatively. The intervention group received guidance with a target step count set at 15% above their average step count every two weeks. At the final assessment, there was no considerable difference in actual step counts between the intervention and control groups. However, the odds ratio for achieving the target step count was 2.23, demonstrating the effectiveness of physical activity guidance through monitoring. A study by O'Brien et al. [ 7 ], implemented a 12-month RCT targeting individuals aged 60 and above, and at least 3 months or longer post-transplantation. The intervention group set a target step count by adding 5% to the average step count of the previous month. As a result, there was no discernible difference in step counts between the two groups over the course of 12 months. From these findings, a consensus on the efficacy of improving physical activity levels has not been reached. Moreover, studies focusing on elderly renal transplant patients are limited, and the impact of intervening in physical activity levels from pre- to post-surgery over an extended period on physical and labor functions remains unclear (Table 3 ).
Discussion and conclusions
Following kidney transplantation, physical function declines and frailty is prevalent due to disuse syndrome, complications, and adverse drug reactions associated with surgery and hospitalization [ 3 ]. A previous study has reported that the level of frailty at the time of kidney transplantation surgery is significantly higher, at 20%, compared with 6.9% in the general older population aged ≥ 65 years [ 5 ]. Frailty and poor physical function in patients who undergo kidney transplantation contribute to adverse events, such as prolonged hospital stay, graft dysfunction, and mortality [ 1 , 2 ]. Preventing frailty and physical functional decline in patients who undergo kidney transplantation is crucial for improving postoperative prognosis.
Further, rehabilitation is a critical intervention for patients who undergo kidney transplantation after surgery, preventing frailty and physical function decline. Exercise therapy has been reported to enhance physical function in middle-aged kidney transplant patients. However, most previous studies have focused on short-term interventions in middle-aged patients ≥ 6 months postoperatively, with limited research on the effects of exercise therapy during the early or long-term postoperative periods. The patient in the current case was older and exhibited more preoperative weakness and impaired physical function compared with the patients described in the referenced studies [ 4 , 6 ]. However, the patient’s physical function improved with ongoing long-term interventions initiated in the early postoperative period. These interventions could potentially facilitate long-term kidney rehabilitation and commitment to physical activity from the early postoperative stages, even for relatively older patients.
A previous study has shown that an intervention targeting exercise therapy and physical activity improved exercise tolerance and walking ability without adverse effects on kidney function compared with a non-exercise intervention [ 4 ]. Another RCT conducted among middle-aged patients who underwent kidney transplantation during the stable postoperative phase (2–24 months) has reported that the provision and monitoring of a target number of steps led to an odds ratio of 2.23 for the goal attainment number of steps in the intervention group, compared with that of the control group [ 6 ]. In the present case, the absence of exercise habits before surgery and low SE, which served as an index of motivation to exercise, were evident. Long-term rehabilitation and visual feedback on physical activity using self-monitoring sheets may improve frailty and physical function by enhancing SE, establishing exercise habits, and increasing physical activity. Providing home exercise instructions and self-monitoring, general exercise therapy during hospitalization, and continuation therapy after discharge were influential in our case.
After kidney transplantation, whereas some individuals reintegrate into society due to the improvement of uremia, others face restrictions in employment or working hours due to the complications and side effects of kidney transplantation and medications. Within the framework of Standardized Outcomes in Nephrology—Transplantation, life participation has been identified as a crucial core outcome for patients who underwent kidney transplantation, along with considerations of mortality and infection, followed by the capacity to engage in work [ 8 ]. A previous study has revealed that working patients showed superior subjective health status post-kidney transplantation compared with that of non-working patients, indicating that enhanced physical function is essential for employment [ 9 ]. A 12-month rehabilitation program for patients who underwent kidney transplantation contributed to improved physical and mental quality of life, higher employment rates, and enhanced participation in social activities [ 10 ]. In the present case, the patient worked 3 days per week on non-dialysis days before undergoing kidney transplantation. A total of 6 months after the surgery, he was successfully reemployed, with the frequency of work increasing from 3 to 5 days per week and working hours from 3 h to 4.5 h per day for 12 months, and an improvement in labor function was observed. Consequently, long-term rehabilitation can improve physical function, activity, and frailty, proving effective in physically demanding occupations.
In this case, the limited duration of just before the operation rehabilitation precluded evaluating the patient’s physical activity level before admission. Therefore, it is not easy to refer to preoperative rehabilitation. However, the patient underwent physical therapy evaluation, risk stratification, and intervention during the just before the operation and 12-month postoperative periods. This improved physical function, enhanced physical activity, reduced frailty and allowed him to resume vocational activities. Physical therapists’ active involvement in caring for patients who underwent kidney transplantation helps reintegrate patients with kidney failure into society.
In conclusion, we suggest that the long-term rehabilitation of frail patients who undergo kidney transplantation in their 60 s yields favorable physical function, physical activity, and employment outcomes.
Availability of data and materials
All data in this case are available upon request.
Abbreviations
Knee extension muscle strength
Short physical performance battery
Randomized controlled trial
Skeletal muscle index
Self-efficacy
Work functioning impairment scale
Nastasi AJ, McAdams-DeMarco MA, Schrack J, Ying H, Olorundare I, Warsame F, et al. Pre-kidney transplant lower extremity impairment and post-kidney transplant mortality. Am J Transplant. 2018;18:189–96.
Article CAS PubMed Google Scholar
Quint EE, Zogaj D, Banning LBD, Benjamens S, Annema C, Bakker SJL, et al. Frailty and kidney transplantation: a systematic review and meta-analysis. Transplant Direct. 2021;7:e701.
Article PubMed PubMed Central Google Scholar
De Smet S, Van Craenenbroeck AH. Exercise training in patients after kidney transplantation. Clin Kidney J. 2021;14:ii15-24.
Yamamoto S, Matsuzawa R, Kamitani T, Hoshi K, Ishii D, Noguchi F, et al. Efficacy of exercise therapy initiated in the early phase after kidney transplantation: a pilot study. J Ren Nutr. 2020;30:518–25.
Article PubMed Google Scholar
Exterkate L, Slegtenhorst BR, Kelm M, Seyda M, Schuitenmaker JM, Quante M, et al. Frailty and transplantation. Transplantation. 2016;100:727–33.
Serper M, Barankay I, Chadha S, Shults J, Jones LS, Olthoff KM, et al. A randomized, controlled, behavioral intervention to promote walking after abdominal organ transplantation: results from the LIFT study. Transpl Int. 2020;33:632–43.
O’Brien T, Russell CL, Tan A, Mion L, Rose K, Focht B, et al. A pilot randomized controlled trial using SystemCHANGE™ approach to increase physical activity in older kidney transplant recipients. Prog Transplant. 2020;30:306–14.
Tong A, Manns B, Wang AYM, Hemmelgarn B, Wheeler DC, Gill J, et al. SONG Implementation Workshop Investigators. Implementing core outcomes in kidney disease: report of the Standardized Outcomes in Nephrology (SONG) implementation workshop. Kidney Int. 2018;94:1053–68.
Nour N, Heck CS, Ross H. Factors related to participation in paid work after organ transplantation: perceptions of kidney transplant recipients. J Occup Rehabil. 2015;25:38–51.
Kastelz A, Fernhall B, Wang E, Tzvetanov I, Spaggiari M, Shetty A, et al. Personalized physical rehabilitation program and employment in kidney transplant recipients: a randomized trial. Transpl Int. 2021;34:1083–92.
Download references
Acknowledgements
We thank the patient and all the doctors involved.
Author information
Authors and affiliations.
Department of Rehabilitation Medicine, Hamamatsu University Hospital, 1-20-1 Handayama, Chuo-ku, Hamamatsu City, Shizuoka, 431-3192, Japan
Tomoya Yamaguchi, Yuma Hirano & Katsuya Yamauchi
Department of Physical Therapy, School of Rehabilitation Sciences, Seirei Christopher University, 3453, Mikatabara-chou, Chuo-ku, Hamamatsu City, Shizuka, 433-8558, Japan
Hiroki Yabe
Department of Urology, Hamamatsu University Hospital, 1-20-1 Handayama, Chuo-ku, Hamamatsu City, Shizuoka, 431-3192, Japan
Takayuki Sugiyama & Hideaki Miyake
First Department of Medicine, Hamamatsu University Hospital, 1-20-1 Handayama, Chuo-ku, Hamamatsu City, Shizuoka, 431-3192, Japan
Shinsuke Isobe & Hideo Yasuda
Division of Urology, Kobe University Graduate School of Medicine, 7-5-1 Kusunokicho, Chuo-ku, Kobe City, 650-0017, Japan
Hideaki Miyake
You can also search for this author in PubMed Google Scholar
Contributions
T.Y. investigated physical activity, physical function, and employment status in kidney transplant recipients in their 60s. T.Y., H.Y., and T.S. were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Tomoya Yamaguchi .
Ethics declarations
Ethics approval and consent to participate.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from the patient.
Consent for publication
Written consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yamaguchi, T., Yabe, H., Sugiyama, T. et al. Effectiveness of physical therapy on physical activity and employment status in kidney transplant recipients in their sixties: a case report with literature review. Ren Replace Ther 10 , 22 (2024). https://doi.org/10.1186/s41100-024-00538-y
Download citation
Received : 12 December 2023
Accepted : 17 March 2024
Published : 27 March 2024
DOI : https://doi.org/10.1186/s41100-024-00538-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Employment status
- Kidney transplantation
- Physical activity
- Physical therapy intervention
Renal Replacement Therapy
ISSN: 2059-1381
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Abstract. A man aged 77 years sustained a left-hemisphere stroke with right hemiparesis. After spending 10 days in the hospital, he was referred to an area rehabilitation centre. There he carried out daily physical, occupational and speech therapy, with an emphasis on task-oriented treatment. The patient's upper-extremity motor performance was ...
Physical Therapy for a Female with Acute Stroke: A Case Report Lisa Grandpre University of North Dakota How does access to this work benefit you? Let us know! Follow this and additional works at: https://commons.und.edu/pt-grad Part of the Physical Therapy Commons Recommended Citation Grandpre, Lisa, "Physical Therapy for a Female with Acute ...
Abstract. Post stroke rehabilitation has been consistently reported in physiotherapy as being difficult to manage and limiting to rehabilitation outcome. It is reported that the first few months ...
Combined clinical home rehabilitation—A service that accelerates home rehabilitation of patients admitted to a rehabilitation stroke unit and combines this rehabilitation with treatment by a multidisciplinary team including specialist nursing staff based in a discrete ward or unit exclusively for patients with stroke (ie, as in this case report).
Flahaven, Physical Therapy Management of a Patient with Chronic Brainstem Stroke Syndrome to Improve Functional Mobility: a Case Report 5 97 repetitive task gait training has shown to create short-term improvements in gait for patients 98 post-stroke; however, long-term effects have not proven these improvements are maintained.7 99 Beyaert, Vasa, and Frykberg7 also reported on non-specific ...
This report identifies the impact of a repetitive adapted golf program on the (1) functional fitness skills and (2) balance of adults recovering from stroke as well as any commu-nity resources used by participants. Eleven men and women (M age = 61.5) were re-ferred to the program. Each participated in a group-oriented, collaborative community ...
This proof-of-principle study suggests that the combination of BCI training with goal-directed, active physical therapy may improve the motor abilities of chronic stroke patients despite apparent initial paralysis. References. ... Case report: post-stroke interventional BCI rehabilitation in an indiv... Go to citation Crossref Google Scholar.
CASE 1. A 20 year old man with no past medical history presented to a primary stroke center with sudden left sided weakness and imbalance followed by decreased level of consciousness. Head CT showed no hemorrhage, no acute ischemic changes, and a hyper-dense basilar artery. CT angiography showed a mid-basilar occlusion.
Grandpre, Lisa, "Physical Therapy for a Female with Acute Stroke: A Case Report" (2016). Physical Therapy Scholarly Projects. 578. Background and Purpose: Strokes are the 5th leading cause of death and adult disability in the US. Strokes affect each individual differently, some individuals more severely than others.
Running head: Outcome Measures for Individuals With Stroke Case Report Outcome Measures for Individuals With Stroke: Recommendations From the American Physical Therapy Association Neurology Section Task Force Jane E. Sullivan, Beth E. Crowner, Patricia M. Kluding, Diane Nichols, Dorian K. Rose, Rie Yoshida, Genevieve Pinto Zipp
A stroke occurs when there is a disruption in the blood supply to the brain, leading to brain cell damage or death. The causes of stroke can be categorized into two main types: ischemic stroke and hemorrhagic stroke. 1. Ischemic Stroke Causes: Ischemic stroke is the most common type of stroke and is caused by a blockage
Cerebellar stroke increases the risk of extensive physical disability and long-term institutionalization. The purpose of this case report is to describe the 14-month longitudinal rehabilitation management and outcomes from the intensive care unit, inpatient rehabilitation unit and outpatient care of a patient after cerebellar stroke.
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater ...
Telerehabilitation services for the presented case started seven months post-stroke. Despite the length of time that had elapsed since stroke onset, the client's improvement was substantial and represented important progress toward independent living and work resumption goals. ... Impact of COVID-19 on the physical therapy profession: A report ...
Introduction. Globally, stroke is the second leading cause of death and the third leading cause of death and disability combined.1 Around 100 000 people have strokes each year, and around 1.3 million people in the UK have survived a stroke.2 High quality rehabilitation can minimise the physical, emotional, cognitive, and social impacts for people who have had a stroke and their carers, and ...
Molly also did occupational therapy and physical therapy to get her strength back. Months later, in the fall of 2020, when COVID-19 canceled all marathons, Donald created his own 26.2-mile run in the Chicago suburbs as a fundraiser for stroke research in Molly's honor.
Case Report Papers. During the course of two semesters, UNE Doctor of Physical Therapy students who elect the case report track to fulfill the program's scholarship requirement work with a faculty advisor to gather data about a patient, institution, facility, or other definable unit related to the profession of physical therapy, and write a ...
Background Few reports have been published on preoperative and long-term postoperative rehabilitation after kidney transplantation. Poor physical function after kidney transplantation is associated with adverse events; hence, physical function should be improved postoperatively. We report a case in which physical therapy was provided just before the operation and 12 months postoperatively to ...