- Patient Care & Health Information
- Diseases & Conditions
- Coronavirus disease 2019 (COVID-19)
COVID-19, also called coronavirus disease 2019, is an illness caused by a virus. The virus is called severe acute respiratory syndrome coronavirus 2, or more commonly, SARS-CoV-2. It started spreading at the end of 2019 and became a pandemic disease in 2020.
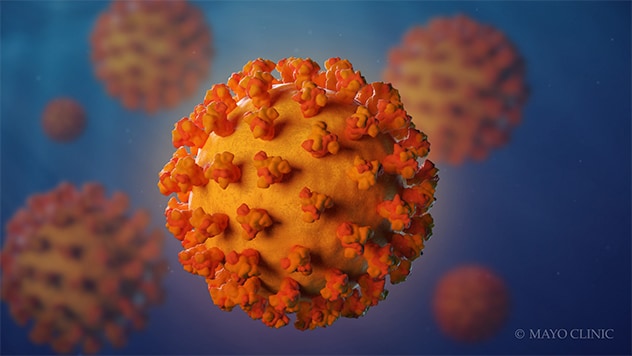
- Coronavirus
Coronaviruses are a family of viruses. These viruses cause illnesses such as the common cold, severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS) and coronavirus disease 2019 (COVID-19).
The virus that causes COVID-19 spreads most commonly through the air in tiny droplets of fluid between people in close contact. Many people with COVID-19 have no symptoms or mild illness. But for older adults and people with certain medical conditions, COVID-19 can lead to the need for care in the hospital or death.
Staying up to date on your COVID-19 vaccine helps prevent serious illness, the need for hospital care due to COVID-19 and death from COVID-19 . Other ways that may help prevent the spread of this coronavirus includes good indoor air flow, physical distancing, wearing a mask in the right setting and good hygiene.
Medicine can limit the seriousness of the viral infection. Most people recover without long-term effects, but some people have symptoms that continue for months.

Products & Services
- A Book: Endemic - A Post-Pandemic Playbook
- A Book: Future Care
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
Typical COVID-19 symptoms often show up 2 to 14 days after contact with the virus.
Symptoms can include:
- Shortness of breath.
- Loss of taste or smell.
- Extreme tiredness, called fatigue.
- Digestive symptoms such as upset stomach, vomiting or loose stools, called diarrhea.
- Pain, such as headaches and body or muscle aches.
- Fever or chills.
- Cold-like symptoms such as congestion, runny nose or sore throat.
People may only have a few symptoms or none. People who have no symptoms but test positive for COVID-19 are called asymptomatic. For example, many children who test positive don't have symptoms of COVID-19 illness. People who go on to have symptoms are considered presymptomatic. Both groups can still spread COVID-19 to others.
Some people may have symptoms that get worse about 7 to 14 days after symptoms start.
Most people with COVID-19 have mild to moderate symptoms. But COVID-19 can cause serious medical complications and lead to death. Older adults or people who already have medical conditions are at greater risk of serious illness.
COVID-19 may be a mild, moderate, severe or critical illness.
- In broad terms, mild COVID-19 doesn't affect the ability of the lungs to get oxygen to the body.
- In moderate COVID-19 illness, the lungs also work properly but there are signs that the infection is deep in the lungs.
- Severe COVID-19 means that the lungs don't work correctly, and the person needs oxygen and other medical help in the hospital.
- Critical COVID-19 illness means the lung and breathing system, called the respiratory system, has failed and there is damage throughout the body.
Rarely, people who catch the coronavirus can develop a group of symptoms linked to inflamed organs or tissues. The illness is called multisystem inflammatory syndrome. When children have this illness, it is called multisystem inflammatory syndrome in children, shortened to MIS -C. In adults, the name is MIS -A.
When to see a doctor
Contact a healthcare professional if you test positive for COVID-19 . If you have symptoms and need to test for COVID-19 , or you've been exposed to someone with COVID-19 , a healthcare professional can help.
People who are at high risk of serious illness may get medicine to block the spread of the COVID-19 virus in the body. Or your healthcare team may plan regular checks to monitor your health.
Get emergency help right away for any of these symptoms:
- Can't catch your breath or have problems breathing.
- Skin, lips or nail beds that are pale, gray or blue.
- New confusion.
- Trouble staying awake or waking up.
- Chest pain or pressure that is constant.
This list doesn't include every emergency symptom. If you or a person you're taking care of has symptoms that worry you, get help. Let the healthcare team know about a positive test for COVID-19 or symptoms of the illness.
More Information
- COVID-19 vs. flu: Similarities and differences
- COVID-19, cold, allergies and the flu
- Unusual symptoms of coronavirus
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
COVID-19 is caused by infection with the severe acute respiratory syndrome coronavirus 2, also called SARS-CoV-2.
The coronavirus spreads mainly from person to person, even from someone who is infected but has no symptoms. When people with COVID-19 cough, sneeze, breathe, sing or talk, their breath may be infected with the COVID-19 virus.
The coronavirus carried by a person's breath can land directly on the face of a nearby person, after a sneeze or cough, for example. The droplets or particles the infected person breathes out could possibly be breathed in by other people if they are close together or in areas with low air flow. And a person may touch a surface that has respiratory droplets and then touch their face with hands that have the coronavirus on them.
It's possible to get COVID-19 more than once.
- Over time, the body's defense against the COVID-19 virus can fade.
- A person may be exposed to so much of the virus that it breaks through their immune defense.
- As a virus infects a group of people, the virus copies itself. During this process, the genetic code can randomly change in each copy. The changes are called mutations. If the coronavirus that causes COVID-19 changes in ways that make previous infections or vaccination less effective at preventing infection, people can get sick again.
The virus that causes COVID-19 can infect some pets. Cats, dogs, hamsters and ferrets have caught this coronavirus and had symptoms. It's rare for a person to get COVID-19 from a pet.
Risk factors
The main risk factors for COVID-19 are:
- If someone you live with has COVID-19 .
- If you spend time in places with poor air flow and a higher number of people when the virus is spreading.
- If you spend more than 30 minutes in close contact with someone who has COVID-19 .
Many factors affect your risk of catching the virus that causes COVID-19 . How long you are in contact, if the space has good air flow and your activities all affect the risk. Also, if you or others wear masks, if someone has COVID-19 symptoms and how close you are affects your risk. Close contact includes sitting and talking next to one another, for example, or sharing a car or bedroom.
It seems to be rare for people to catch the virus that causes COVID-19 from an infected surface. While the virus is shed in waste, called stool, COVID-19 infection from places such as a public bathroom is not common.
Serious COVID-19 illness risk factors
Some people are at a higher risk of serious COVID-19 illness than others. This includes people age 65 and older as well as babies younger than 6 months. Those age groups have the highest risk of needing hospital care for COVID-19 .
Not every risk factor for serious COVID-19 illness is known. People of all ages who have no other medical issues have needed hospital care for COVID-19 .
Known risk factors for serious illness include people who have not gotten a COVID-19 vaccine. Serious illness also is a higher risk for people who have:
- Sickle cell disease or thalassemia.
- Serious heart diseases and possibly high blood pressure.
- Chronic kidney, liver or lung diseases.
People with dementia or Alzheimer's also are at higher risk, as are people with brain and nervous system conditions such as stroke. Smoking increases the risk of serious COVID-19 illness. And people with a body mass index in the overweight category or obese category may have a higher risk as well.
Other medical conditions that may raise the risk of serious illness from COVID-19 include:
- Cancer or a history of cancer.
- Type 1 or type 2 diabetes.
- Weakened immune system from solid organ transplants or bone marrow transplants, some medicines, or HIV .
This list is not complete. Factors linked to a health issue may raise the risk of serious COVID-19 illness too. Examples are a medical condition where people live in a group home, or lack of access to medical care. Also, people with more than one health issue, or people of older age who also have health issues have a higher chance of severe illness.
Related information
- COVID-19: Who's at higher risk of serious symptoms? - Related information COVID-19: Who's at higher risk of serious symptoms?
Complications
Complications of COVID-19 include long-term loss of taste and smell, skin rashes, and sores. The illness can cause trouble breathing or pneumonia. Medical issues a person already manages may get worse.
Complications of severe COVID-19 illness can include:
- Acute respiratory distress syndrome, when the body's organs do not get enough oxygen.
- Shock caused by the infection or heart problems.
- Overreaction of the immune system, called the inflammatory response.
- Blood clots.
- Kidney injury.
Post-COVID-19 syndrome
After a COVID-19 infection, some people report that symptoms continue for months, or they develop new symptoms. This syndrome has often been called long COVID, or post- COVID-19 . You might hear it called long haul COVID-19 , post-COVID conditions or PASC. That's short for post-acute sequelae of SARS -CoV-2.
Other infections, such as the flu and polio, can lead to long-term illness. But the virus that causes COVID-19 has only been studied since it began to spread in 2019. So, research into the specific effects of long-term COVID-19 symptoms continues.
Researchers do think that post- COVID-19 syndrome can happen after an illness of any severity.
Getting a COVID-19 vaccine may help prevent post- COVID-19 syndrome.
- Long-term effects of COVID-19
The Centers for Disease Control and Prevention (CDC) recommends a COVID-19 vaccine for everyone age 6 months and older. The COVID-19 vaccine can lower the risk of death or serious illness caused by COVID-19. It lowers your risk and lowers the risk that you may spread it to people around you.
The COVID-19 vaccines available in the United States are:
2023-2024 Pfizer-BioNTech COVID-19 vaccine. This vaccine is available for people age 6 months and older.
Among people with a typical immune system:
- Children age 6 months up to age 4 years are up to date after three doses of a Pfizer-BioNTech COVID-19 vaccine.
- People age 5 and older are up to date after one Pfizer-BioNTech COVID-19 vaccine.
- For people who have not had a 2023-2024 COVID-19 vaccination, the CDC recommends getting an additional shot of that updated vaccine.
2023-2024 Moderna COVID-19 vaccine. This vaccine is available for people age 6 months and older.
- Children ages 6 months up to age 4 are up to date if they've had two doses of a Moderna COVID-19 vaccine.
- People age 5 and older are up to date with one Moderna COVID-19 vaccine.
2023-2024 Novavax COVID-19 vaccine. This vaccine is available for people age 12 years and older.
- People age 12 years and older are up to date if they've had two doses of a Novavax COVID-19 vaccine.
In general, people age 5 and older with typical immune systems can get any vaccine approved or authorized for their age. They usually don't need to get the same vaccine each time.
Some people should get all their vaccine doses from the same vaccine maker, including:
- Children ages 6 months to 4 years.
- People age 5 years and older with weakened immune systems.
- People age 12 and older who have had one shot of the Novavax vaccine should get the second Novavax shot in the two-dose series.
Talk to your healthcare professional if you have any questions about the vaccines for you or your child. Your healthcare team can help you if:
- The vaccine you or your child got earlier isn't available.
- You don't know which vaccine you or your child received.
- You or your child started a vaccine series but couldn't finish it due to side effects.
People with weakened immune systems
Your healthcare team may suggest added doses of COVID-19 vaccine if you have a moderately or seriously weakened immune system. The FDA has also authorized the monoclonal antibody pemivibart (Pemgarda) to prevent COVID-19 in some people with weakened immune systems.
Control the spread of infection
In addition to vaccination, there are other ways to stop the spread of the virus that causes COVID-19 .
If you are at a higher risk of serious illness, talk to your healthcare professional about how best to protect yourself. Know what to do if you get sick so you can quickly start treatment.
If you feel ill or have COVID-19 , stay home and away from others, including pets, if possible. Avoid sharing household items such as dishes or towels if you're sick.
In general, make it a habit to:
- Test for COVID-19 . If you have symptoms of COVID-19 test for the infection. Or test five days after you came in contact with the virus.
- Help from afar. Avoid close contact with anyone who is sick or has symptoms, if possible.
- Wash your hands. Wash your hands well and often with soap and water for at least 20 seconds. Or use an alcohol-based hand sanitizer with at least 60% alcohol.
- Cover your coughs and sneezes. Cough or sneeze into a tissue or your elbow. Then wash your hands.
- Clean and disinfect high-touch surfaces. For example, clean doorknobs, light switches, electronics and counters regularly.
Try to spread out in crowded public areas, especially in places with poor airflow. This is important if you have a higher risk of serious illness.
The CDC recommends that people wear a mask in indoor public spaces if you're in an area with a high number of people with COVID-19 in the hospital. They suggest wearing the most protective mask possible that you'll wear regularly, that fits well and is comfortable.
- COVID-19 vaccines: Get the facts - Related information COVID-19 vaccines: Get the facts
- Comparing the differences between COVID-19 vaccines - Related information Comparing the differences between COVID-19 vaccines
- Different types of COVID-19 vaccines: How they work - Related information Different types of COVID-19 vaccines: How they work
- Debunking COVID-19 myths - Related information Debunking COVID-19 myths
Travel and COVID-19
Travel brings people together from areas where illnesses may be at higher levels. Masks can help slow the spread of respiratory diseases in general, including COVID-19 . Masks help the most in places with low air flow and where you are in close contact with other people. Also, masks can help if the places you travel to or through have a high level of illness.
Masking is especially important if you or a companion have a high risk of serious illness from COVID-19 .
- COVID-19 travel advice
- COVID-19 vaccines
- COVID-19 vaccines for kids: What you need to know
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Fight coronavirus (COVID-19) transmission at home
- Herd immunity and coronavirus
- How well do face masks protect against COVID-19?
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- COVID-19 and vitamin D
- COVID-19: How can I protect myself?
- Mayo Clinic Minute: How dirty are common surfaces?
- Mayo Clinic Minute: You're washing your hands all wrong
- Goldman L, et al., eds. COVID-19: Epidemiology, clinical manifestations, diagnosis, community prevention, and prognosis. In: Goldman-Cecil Medicine. 27th ed. Elsevier; 2024. https://www.clinicalkey.com. Accessed Dec. 17, 2023.
- Coronavirus disease 2019 (COVID-19) treatment guidelines. National Institutes of Health. https://www.covid19treatmentguidelines.nih.gov/. Accessed Dec. 18, 2023.
- AskMayoExpert. COVID-19: Testing, symptoms. Mayo Clinic; Nov. 2, 2023.
- Symptoms of COVID-19. Centers for Disease Control and Preventions. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed Dec. 20, 2023.
- AskMayoExpert. COVID-19: Outpatient management. Mayo Clinic; Oct. 10, 2023.
- Morris SB, et al. Case series of multisystem inflammatory syndrome in adults associated with SARS-CoV-2 infection — United Kingdom and United States, March-August 2020. MMWR. Morbidity and Mortality Weekly Report 2020;69:1450. DOI: http://dx.doi.org/10.15585/mmwr.mm6940e1external icon.
- COVID-19 testing: What you need to know. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html. Accessed Dec. 20, 2023.
- SARS-CoV-2 in animals. American Veterinary Medical Association. https://www.avma.org/resources-tools/one-health/covid-19/sars-cov-2-animals-including-pets. Accessed Jan. 17, 2024.
- Understanding exposure risk. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/your-health/risks-exposure.html. Accessed Jan. 10, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed Jan. 10, 2024.
- Factors that affect your risk of getting very sick from COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/your-health/risks-getting-very-sick.html. Accessed Jan. 10, 2024.
- Regan JJ, et al. Use of Updated COVID-19 Vaccines 2023-2024 Formula for Persons Aged ≥6 Months: Recommendations of the Advisory Committee on Immunization Practices—United States, September 2023. MMWR. Morbidity and Mortality Weekly Report 2023; 72:1140–1146. DOI: http://dx.doi.org/10.15585/mmwr.mm7242e1.
- Long COVID or post-COVID conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html. Accessed Jan. 10, 2024.
- Stay up to date with your vaccines. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed Jan. 10, 2024.
- Interim clinical considerations for use of COVID-19 vaccines currently approved or authorized in the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html#CoV-19-vaccination. Accessed Jan. 10, 2024.
- Use and care of masks. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html. Accessed Jan. 10, 2024.
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed Jan. 10, 2024.
- People who are immunocompromised. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html. Accessed Jan. 10, 2024.
- Masking during travel. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/masks. Accessed Jan. 10, 2024.
- AskMayoExpert. COVID-19: Testing. Mayo Clinic. 2023.
- COVID-19 test basics. U.S. Food and Drug Administration. https://www.fda.gov/consumers/consumer-updates/covid-19-test-basics. Accessed Jan. 11, 2024.
- At-home COVID-19 antigen tests — Take steps to reduce your risk of false negative results: FDA safety communication. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/safety-communications/home-covid-19-antigen-tests-take-steps-reduce-your-risk-false-negative-results-fda-safety. Accessed Jan. 11, 2024.
- Interim clinical considerations for COVID-19 treatment in outpatients. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/outpatient-treatment-overview.html. Accessed Jan. 11, 2024.
- Know your treatment options for COVID-19. U.S. Food and Drug Administration. https://www.fda.gov/consumers/consumer-updates/know-your-treatment-options-covid-19. Accessed Jan. 11, 2024.
- AskMayoExpert. COVID:19 Drug regimens and other treatment options. Mayo Clinic. 2023.
- Preventing spread of respiratory viruses when you're sick. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/precautions-when-sick.html. Accessed March 5, 2024.
- AskMayoExpert. COVID-19: Quarantine and isolation. Mayo Clinic. 2023.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed Jan. 11, 2024.
- COVID-19 overview and infection prevention and control priorities in non-U.S. healthcare settings. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html. Accessed Jan. 16, 2024.
- Kim AY, et al. COVID-19: Management in hospitalized adults. https://www.uptodate.com/contents/search. Accessed Jan. 17, 2024.
- O'Horo JC, et al. Outcomes of COVID-19 with the Mayo Clinic Model of Care and Research. Mayo Clinic Proceedings. 2021; doi:10.1016/j.mayocp.2020.12.006.
- At-home OTC COVID-19 diagnostic tests. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/home-otc-covid-19-diagnostic-tests. Accessed Jan. 22, 2024.
- Emergency use authorizations for drugs and non-vaccine biological products. U.S. Food and Drug Association. https://www.fda.gov/drugs/emergency-preparedness-drugs/emergency-use-authorizations-drugs-and-non-vaccine-biological-products. Accessed March 25, 2024.
- Coronavirus infection by race
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- COVID-19 variant
- COVID-19: Who's at higher risk of serious symptoms?
- How do COVID-19 antibody tests differ from diagnostic tests?
- Is hydroxychloroquine a treatment for COVID-19?
- Pregnancy and COVID-19
- Sex and COVID-19
- Treating COVID-19 at home
Associated Procedures
- Convalescent plasma therapy
- COVID-19 antibody testing
- COVID-19 tests
- Extracorporeal membrane oxygenation (ECMO)
News from Mayo Clinic
- Mayo Clinic Q and A: Who should get the latest COVID-19 vaccine? Nov. 21, 2023, 01:30 p.m. CDT
- Can you get COVID-19 and the flu at the same time? A Mayo Clinic expert weighs in Oct. 16, 2023, 04:30 p.m. CDT
- At-home COVID-19 tests: A Mayo Clinic expert answers questions on expiration dates and the new variants Sept. 18, 2023, 04:00 p.m. CDT
- Mayo Clinic expert answers questions about the new COVID-19 vaccine Sept. 13, 2023, 04:15 p.m. CDT
- Study identifies risk factors for long-haul COVID disease in adults Sept. 13, 2023, 02:00 p.m. CDT
- Mayo researchers find vaccine may reduce severity of long-haul COVID symptoms Aug. 23, 2023, 04:34 p.m. CDT
- Corticosteroids lower the likelihood of in-hospital mortality from COVID-19 Aug. 04, 2023, 03:00 p.m. CDT
- COVID-19 vaccine administration simplified April 21, 2023, 07:00 p.m. CDT
- Science Saturday: COVID-19 -- the pandemic that's forever changed laboratory testing April 15, 2023, 11:00 a.m. CDT
- Mayo Clinic expert talks about the new omicron variant April 13, 2023, 02:13 p.m. CDT
- Mayo Clinic to ease universal face mask requirement April 04, 2023, 03:05 p.m. CDT
- 'Deaths of Despair' contribute to 17% rise in Minnesota's death rate during COVID-19 pandemic March 13, 2023, 12:00 p.m. CDT
- Rising cases of COVID-19 variant, XBB.1.5 Jan. 09, 2023, 05:15 p.m. CDT
- Bivalent COVID-19 booster approved for children 6 months and older Dec. 09, 2022, 09:33 p.m. CDT
- Mayo Clinic Minute: How to self-care at home when you have COVID-19 Dec. 06, 2022, 05:00 p.m. CDT
- Halloween safety tips from a Mayo Clinic infectious diseases expert Oct. 27, 2022, 02:00 p.m. CDT
- COVID-19, RSV and flu--season of respiratory infections Oct. 26, 2022, 04:30 p.m. CDT
- COVID-19 bivalent booster vaccines for kids 5-11 approved, Mayo Clinic awaits supply Oct. 13, 2022, 04:54 p.m. CDT
- Questions answered about the COVID-19 bivalent booster vaccines Oct. 12, 2022, 03:30 p.m. CDT
- Will the COVID-19 booster be like an annual flu shot? Sept. 12, 2022, 04:30 p.m. CDT
- Mayo Clinic Q and A: Who needs back-to-school COVID-19 vaccinations and boosters? Sept. 04, 2022, 11:00 a.m. CDT
- Q&A podcast: Updated COVID-19 boosters target omicron variants Sept. 02, 2022, 12:30 p.m. CDT
- Mayo Clinic Minute: Back-to-school COVID-19 vaccinations for kids Aug. 15, 2022, 03:15 p.m. CDT
- Mayo Clinic research shows bebtelovimab to be a reliable option for treating COVID-19 in era of BA.2, other subvariants Aug. 15, 2022, 02:09 p.m. CDT
- Mayo Clinic Q and A: New variants of COVID-19 Aug. 04, 2022, 12:30 p.m. CDT
- COVID-19 variant BA.5 is dominant strain; BA.2.75 is being monitored July 28, 2022, 02:30 p.m. CDT
- Mayo Clinic researchers pinpoint genetic variations that might sway course of COVID-19 July 25, 2022, 02:00 p.m. CDT
- Mayo Clinic Q&A podcast: BA.5 omicron variant fueling latest COVID-19 surge July 15, 2022, 12:00 p.m. CDT
- What you need to know about the BA.5 omicron variant July 14, 2022, 06:41 p.m. CDT
- Mayo Clinic Q&A podcast: The importance of COVID-19 vaccines for children under 5 July 06, 2022, 01:00 p.m. CDT
- COVID-19 vaccination for kids age 5 and younger starting the week of July 4 at most Mayo sites July 01, 2022, 04:00 p.m. CDT
- Patients treated with monoclonal antibodies during COVID-19 delta surge had low rates of severe disease, Mayo Clinic study finds June 27, 2022, 03:00 p.m. CDT
- Long COVID and the digestive system: Mayo Clinic expert describes common symptoms June 21, 2022, 02:43 p.m. CDT
- Mayo Clinic Q&A podcast: COVID-19 update June 17, 2022, 01:08 p.m. CDT
- Study finds few COVID-19 patients get rebound symptoms after Paxlovid treatment June 14, 2022, 10:06 a.m. CDT
- Mayo Clinic Minute: What to expect with COVID-19 vaccinations for youngest kids June 08, 2022, 04:35 p.m. CDT
- Mayo Clinic Q&A podcast: Community leaders are key to reaching people underrepresented in research May 26, 2022, 02:00 p.m. CDT
- COVID-19 booster vaccinations extended to kids 5-11 May 20, 2022, 06:10 p.m. CDT
- Mayo Clinic expert shares tips for navigating a return to work with long COVID May 19, 2022, 02:08 p.m. CDT
- Mayo Clinic Q&A podcast: COVID-19 update May 17, 2022, 01:14 p.m. CDT
- FDA limits use of J&J COVID-19 vaccine May 06, 2022, 05:06 p.m. CDT
- Mayo Clinic Q&A podcast: COVID-19 news update April 29, 2022, 12:25 p.m. CDT
- COVID-19 shines a spotlight on laboratory professionals' vital role in health care April 25, 2022, 12:30 p.m. CDT
- Confused about when to get your second COVID-19 booster vaccination? Mayo Clinic expert answers common questions April 11, 2022, 04:30 p.m. CDT
- Mayo Clinic expert shares 5 early care tips for people with long COVID April 07, 2022, 03:30 p.m. CDT
- Mayo Clinic will offer COVID-19 booster for those 50 and older, immunocompromised patients 12 and older April 06, 2022, 02:30 p.m. CDT
- Testing wastewater for COVID-19: The clearest path to understanding community infection April 05, 2022, 03:30 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- COVID-19 vaccines: Get the facts
- How well do face masks protect against coronavirus?
- Post-COVID Recovery
News on coronavirus disease 2019 (COVID-19)
Learn the latest medical news about COVID-19 on Mayo Clinic News Network.
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Registry Operations
- Reporting Guidelines
- COVID-19 Abstraction Guidance
COVID-19 Presentations

COVID-19 Abstraction Guidance by Margaret (Peggy) Adamo, RHIT, CTR
Access the presentation slides (PDF, 1.2 MB)

Coronavirus-Disease 19 (COVID-19) & SARS-CoV-2 Testing by Alison Van Dyke, MD, PhD
Access the presentation slides (PDF, 4.6 MB)

Immunization Courses: Webcasts and Self Study
CDC offers continuing education (CE) for several self-study programs on immunization. These can be accessed in a variety of ways: web-based, video, and webinar.
Most CE from these programs is free and easy to access through the training and CE online system . If needed, assistance with obtaining CE is available.
Click the course name in the table below to see its description, intended audience, format , CE details, and any needed materials and resources. Other details include registration, objectives, and presenters/faculty, etc.
Terms used on this page are defined at bottom of page.
CDC-INFO’s correspondence process has changed. The email box is not actively monitored; please submit questions via the CDC-INFO online form .
Some courses offer continuing education (CE).
CDC’s Training and Continuing Education Online system ( TCEO ) has been the primary system that provides access to CDC educational activities for CE. To improve the learning experience, CDC’s continuing education (CE) process is moving from TCEO to CDC TRAIN .
Beginning January 1, 2024, many activities that offer CE from CDC will be listed in CDC TRAIN . Older modules will continue to use the TCEO system throughout 2024 to provide CE.
If you would like to claim CE or print a certificate, specific instructions are provided within each course to guide you to the appropriate system.
For additional immunization training, see
- 1-hour CDC webinars on current immunization issues
- Other organization’s courses for CMEs, CNEs, CEUs, and CE
Top of Page
Target Audience: Physicians, PAs, Advanced Practice Nurses, RNs, Pharmacists, Health Educators
Description: CDC has created a new, web-on-demand, self-paced module for healthcare providers who will be administering COVID-19 vaccines. This module will provide healthcare providers with information about COVID-19 vaccine Emergency Use Authorization and safety, approved COVID-19 vaccines, and guidelines around vaccine storage, handling, administration, and reporting.
Learning Objectives:
At the conclusion of the session, the participant will be able to:
- Describe storage and handling requirements for COVID-19 vaccines.
- Describe vaccine preparation procedures for COVID-19 vaccines.
- Describe vaccine administration procedures for COVID-19 vaccines.
- Locate current immunization resources to increase knowledge of team’s role in program implementation for improved team performance.
CME: Valid through August 17, 2025
CE Details: https://www2.cdc.gov/vaccines/ed/covid19/covax/
- Describe best practices for effective COVID-19 vaccine administration.
- Address recent COVID-19 recommendations made by the Advisory Committee on Immunization Practices and CDC.
- Implement disease detection and prevention health care services (e.g., smoking cessation, weight reduction, diabetes screening, blood pressure screening, immunization services) to prevent health problems and maintain health.
Continuing Education is no longer available for this series.
CE Details: www.cdc.gov/vaccines/covid-19/training-education/webinars.html
Target Audience: Immunization Providers (Physicians, Nurses, Nurse Practitioners, Pharmacists, Physician’s Assistants, DoD Paraprofessionals, Medical Students, etc.)
Description: The General Best Practice Guidelines for Immunization publication is intended for clinicians and other health care providers who vaccinate patients in varied settings, including hospitals, provider offices, pharmacies, schools, community health centers, and public health clinics. It is organized into the following 10 sections: 1) Timing and Spacing of Immunobiologics; 2) Contraindications and Precautions; 3) Preventing and Managing Adverse Reactions; 4) Vaccine Administration; 5) Storage and Handling of Immunobiologics; 6) Altered Immunocompetence; 7) Special Situations; 8) Vaccination Records; 9) Vaccination Programs; and 10) Vaccine Information Sources.
- Identify valid contraindications for commonly used vaccines.
- Describe the minimum intervals between doses for vaccines routinely used in the United States.
- Describe methods for preventing and managing adverse reactions.
- Describe recommended practices for administration of vaccines.
- Describe proper storage and handling procedures for immunobiologics.
- Identify evidence-based interventions shown to improve vaccination rates among children.
CME: Valid through April 21, 2025.
CE Details: General Best Practice Guidelines for Immunization course #WB4458R
Description: Communication between providers and parents is key to improving HPV vaccination. HPV Vaccine: Same Way, Same Day ™ is a brief, interactive role-play simulation designed to enhance healthcare providers’ ability to introduce the HPV vaccine and address HPV vaccine hesitant parents’ concerns. In this app, you will practice techniques to introduce and discuss the vaccine with parents and patients, including those who may be hesitant to immunize. It is ideal for immunization education and provider training.
Format: Self-paced mobile app available for download from the Google Play store and the Apple iTunes store
MEDSCAPE CME: This CME activity is a roundtable discussion on HPV vaccine developed for distribution on Medscape. It can be accessed at “MedscapeCME” at http://www.medscape.org/viewarticle/768633
Target Audience: This activity is intended for pediatricians, physicians in primary care and family medicine, pediatric nurses, nurse practitioners, and other healthcare professionals involved in the treatment, management, and prevention of human papillomavirus (HPV)-related disease in adolescents and/or young men and women at risk for HPV infection.
Description: CE activity for physicians, nurses, and pharmacists who recommend or provide vaccinations to preteens and teens. The goals of this activity are to increase clinician recognition of the burden of HPV-related disease and to increase understanding of Advisory Committee on Immunization Practices (ACIP) recommendations for HPV disease prevention through vaccination.
- Describe the cancer risks that have been linked to HPV infection
- Apply the ACIP vaccine recommendations for HPV immunization to practice
CE is no longer available for this product .
Target Audience: Immunization Providers (Physicians, Nurses, Nurse Practitioners, Pharmacists, Physician’s Assistants, Dentists, DoD Paraprofessionals, Medical Students, etc.)
Description: HPV vaccination is cancer prevention. While most U.S. adolescents are starting the HPV vaccine series, less than half have finished the HPV vaccine series. Every year that adolescents aren’t vaccinated is another year they are left unprotected against cancer-causing infections. A clinician recommendation plays a critical role in getting parents to accept HPV vaccination for their child.
CDC is looking to you to make an effective recommendation for HPV vaccination for all your 11-12 year old patients. This presentation is intended to support you in making effective recommendations and answering parents’ questions. Provided in this presentation is up-to-date information on HPV infection/disease, HPV vaccine, and ways to successfully communicate with parents about HPV vaccination.
Learning Objectives
- Describe the burden of HPV infection and disease in the United States.
- Define the importance of HPV vaccination in cancer prevention.
- Describe recommendations for HPV vaccination for adolescents and adults.
- Describe the rationale for the routine HPV vaccination at age 11 or 12 years.
- List two components of an effective HPV vaccine recommendation.
- Identify relevant and compelling information to share with parents about HPV vaccine to help inform their decision to vaccinate their child.
- Locate current immunization resources to increase knowledge of the team’s role in program implementation for improved team performance.
CME: Valid through April 12, 2024.
CE Details: HPV course # WD4538
Description: This web-based course is an interactive, self-study program consisting of a series of modules covering all aspects of immunization. The modules provide basic vaccine content, links to resource materials, a comprehensive glossary, and self-tests to assess learning.
Audience: Practicing nurses and nursing students, medical assistants, pharmacists, and other health professionals who provide immunizations. The course is designed for immunization providers who are new to immunization or for those who need a refresher.
Format: Interactive web-based program.
Produced by: The Association for Prevention Teaching and Research, in collaboration with CDC’s National Center for Immunization and Respiratory Diseases.
To View or Order: More information and link to all available modules
Description: The Perinatal Hepatitis B Prevention Program (PHBPP) was established in 1990 by CDC. Orientation and trainings have been provided to coordinators in the past in various formats and venues. This series will combine aspects of both training on the epidemiology of hepatitis B virus and orientation to the PHBHPP in a web-based format. It presents both practice-based and program oriented content on Perinatal Hepatitis B. It addresses an educational need of an importance audience for the prevention of perinatal hepatitis B transmission, the new PHBPP Coordinator. This web-on-demand video will allow both new and experienced coordinators to improve their knowledge of perinatal hepatitis B and program management skills.
The multi-session series presents core knowledge necessary for a PHBPP Coordinator to posses to be successful in their position in concise web-based platform. The creation of this series is a direct result of requests from Coordinators for a web based training course with available continuing education.
- Identify the purpose of the Perinatal Hepatitis B Prevention Program (PHBPP).
- Identify the required PHBPP program objectives.
- Describe the relationship between the PHBPP objectives and the Advisory Committee on Immunization Practices (ACIP) Hepatitis Recommendations.
- Describe 2 activities that can be implemented to achieve the program objectives.
- Identify 3 key program data sources.
- Describe 1 way to use key data sources to improve program outcomes.
CME: CE for this course has expired.
Video, Transcript, and CE Details: Perihepb course # WD2895
Description: Provides guidelines for vaccine-preventable disease surveillance, case investigation, and outbreak control.
Audience: Physicians, infection control practitioners, nurses, epidemiologists, laboratorians, sanitarians, disease reporters, and others who are involved in surveillance and reporting of VPDs.
Format: Archived Webcast
Produced by: CDC
Description: This curriculum is designed for use in medical schools to support immunization instruction. The TIME modules provide ready-to-use instructional materials that can be integrated into existing medical curricula. The modules include vaccine indications and contraindications, immunization schedules, and recommendations on efficient ways to increase vaccination levels.
The materials provide student objectives, learning objectives, key teaching points, and resources.
Audience: Schools of Medicine
Format: Download from Internet
Produced by: The Association for Prevention Teaching and Research (APTR), in collaboration with the University of Pittsburgh School of Medicine and the CDC.
To View or Order: For information and to download a free copy, visit the APTR website
Terms Used on This Page
Broadcasts use streaming video (played as it arrives vs. waiting for entire file to be downloaded) techniques, and you can “tune it in” using something like RealPlayer. CDC’s immunization training broadcasts are offered live. Recorded sessions are archived to be played again if you missed the live session. Broadcasts are scheduled and delivered on demand.
Continuing Education (CE). Certification programs are designed to provide training to individuals, who are required to have and maintain specific levels of knowledge and skills in their job categories, often as a legal requirement to perform their duties. Certification programs may carry credits, and may be prerequisites for licensure. Requirements vary by state and profession. Disclaimer: This is a general definition and not necessarily CDC’s or an organizations’.
Continuing Medical Education (CME) credit. Continuing Nurses Education (CNE). Educational opportunities for physicians and other health professionals (CME), nurses and nurse students (CNE) to earn required continuing professional education credits. Continuing CNE and CME requirements vary from state to state. Disclaimer: This is a general definition and not necessarily CDC’s or an organizations’.
Continuing Education Units (CEU). Certain professions require that practitioners earn a specific number of CEUs per year to ensure that they are up-to-date with current practices in their field. Proof of credits earned is necessary in order to renew a license or certification. The annual number of CEUs required varies by state and profession. Disclaimer: This is a general definition and not necessarily CDC’s or an organizations’.
Training sessions are made available to you whenever you need it. An example is a TV show that can be watched whenever you want.
Podcasting is a form of audio broadcasting on the internet. An audio broadcast can be downloaded on your computer with some music software such as Media Player or iTunes.
Questions and Answers:
Questions submitted during NetConference/webcasts, including faxed and e-mailed questions not answered on-air.
Links to resources discussed during the broadcasts/webcasts.
Streaming Technology:
Data streaming, commonly seen in the forms of audio and video streaming, is when a multimedia file can be played back without being completely downloaded first. An example is watching and listening to videos via YouTube in ‘real time’.
PowerPoint presentations for each segment of the broadcasts/webcasts.
Updates and Clarifications:
Information that has changed since the broadcasts/webcasts, and explanations or clarifications of topics discussed during the webcast.
A webcast is a presentation shown on the web using streaming technology to many listeners/viewers at the same time. You can see it either live or ‘on demand’. Essentially, webcasting is “broadcasting” over the Internet. It does not allow interaction between you and the presenter.
Short for web-based seminar, a webinar is a presentation, lecture, workshop or seminar that is transmitted over the web. A key feature of a webinar is its interactive elements: the ability to give, receive and discuss information.
Please note that some of our training products do not reflect changes in CDC-INFO’s new operating hours. CDC-INFO’s hours of operation are 8:00am to 8:00pm Monday through Friday, Eastern Standard Time (EST). CDC-INFO will be closed overnight (8:00pm to 8:00am EST), Saturdays and Sundays, and on major federal holidays (New Year’s Day, Martin Luther King Day, Memorial Day, Independence Day, Labor Day, Veteran’s Day, Thanksgiving Day, Christmas Day).
- Current Issues in Immunization Webinar (CIIW)
- Netconferences
To receive email updates about this page, enter your email address:
- Vaccines & Immunizations
- ACIP Recommendations
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Clinical presentation and course of COVID-19
Affiliations.
- 1 Department of Infectious Disease, Respiratory Institute, Cleveland Clinic.
- 2 Vice-Chair, Department of Infectious Disease, Respiratory Institute, Cleveland Clinic; Assistant Professor, Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH [email protected].
- PMID: 32371564
- DOI: 10.3949/ccjm.87a.ccc013
Information about the clinical presentation and course of COVID-19 is evolving rapidly. On presentation, cough and fever predominate, but extrapulmonary symptoms are also common; in some patients, loss of sense of smell may be an early but favorable sign. The mortality rate varies widely in different reports but should become clearer as more data are collected. Risk factors for severe disease and death include comorbid conditions such as hypertension, cardiovascular disease, diabetes mellitus, and chronic obstructive pulmonary disease. Other implicated factors include older age, obesity, end-stage renal disease, and a higher neutrophil-lymphocyte ratio.
Copyright © 2020 The Cleveland Clinic Foundation. All Rights Reserved.
- Betacoronavirus / isolation & purification*
- Clinical Deterioration
- Comorbidity
- Coronavirus Infections / diagnosis
- Coronavirus Infections / epidemiology
- Coronavirus Infections / physiopathology
- Coronavirus Infections / therapy
- Multiple Chronic Conditions / epidemiology
- Multiple Organ Failure* / diagnosis
- Multiple Organ Failure* / etiology
- Multiple Organ Failure* / mortality
- Pneumonia, Viral* / diagnosis
- Pneumonia, Viral* / diagnostic imaging
- Pneumonia, Viral* / epidemiology
- Pneumonia, Viral* / etiology
- Pneumonia, Viral* / physiopathology
- Pneumonia, Viral* / therapy
- Radiography, Thoracic / methods
- Risk Assessment / methods
- Risk Factors
- Survival Analysis
- Symptom Assessment / methods*
- Symptom Assessment / statistics & numerical data

Patients with COVID-19 Infection and Stroke have Higher than Expected Mortality, Regardless of the Primary Presentation
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Jintong Liu
- For correspondence: [email protected]
- Info/History
- Preview PDF
Background COVID-19 infection is associated with thrombotic events; however, this phenomenon is poorly understood. Few studies have reported the association between COVID-19 and stroke in the hospital setting. Methods We retrospectively reviewed and characterized all patients who presented to a single, quaternary medical center between March and December 2020 (N=603). COVID-19 positive patients who developed ischemic or hemorrhagic stroke were included in the analysis (N=66). This cohort was compared with patients who were COVID-19 negative at the time of stroke presentation in the same period (N=537). Statistical significance was evaluated using Pearson's Chi squared test with Yates' continuity correction and linear model ANOVA. Results Sixty-six patients had COVID-19 and Stroke. Of these patients, 22 (33.4%) patients initially presented with stroke and 44 (66.7%) initially presented with COVID-19. Patients who presented with COVID-19 and had a stroke during their hospitalization (COVID-first) had worse outcomes than patients presenting to the hospital with stroke whose COVID test became positive later in the hospitalization (stroke-first). Patients who presented with COVID-19 and had a stroke during their hospitalization had an increased rate of acute renal failure (48.9% vs 19.0%, p=0.021) and need for ventilation (60.0% vs 28.6%, p=0.017). Further, in the COVID-first cohort, the use of heparin prior to the stroke event was not associated with mortality or type of stroke (ischemic or hemorrhagic). Conclusion In the early pandemic, patients with COVID-19 infection and stroke had a higher mortality rate compared to COVID-19 negative patients with stroke. Among patients with both COVID-19 and stroke, patients presenting with COVID-19 first had worse outcomes than patients presenting with stroke first. The use of heparin prior to the stroke event was not associated with mortality or type of stroke.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
No funding received.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
This retrospective observational study complies with the US Health Insurance Portability and Accountability Act (HIPPA) of 1996 and was exempted by the Colorado Multiple Institutional Review Board.Submission ID: PAM001-1.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
Dr. Wohlauer had full access to all the data in the study and takes responsibility for its integrity and the data analysis.
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Addiction Medicine (315)
- Allergy and Immunology (617)
- Anesthesia (159)
- Cardiovascular Medicine (2268)
- Dentistry and Oral Medicine (279)
- Dermatology (201)
- Emergency Medicine (369)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (797)
- Epidemiology (11559)
- Forensic Medicine (10)
- Gastroenterology (676)
- Genetic and Genomic Medicine (3558)
- Geriatric Medicine (336)
- Health Economics (614)
- Health Informatics (2295)
- Health Policy (912)
- Health Systems and Quality Improvement (860)
- Hematology (333)
- HIV/AIDS (746)
- Infectious Diseases (except HIV/AIDS) (13132)
- Intensive Care and Critical Care Medicine (755)
- Medical Education (358)
- Medical Ethics (100)
- Nephrology (388)
- Neurology (3339)
- Nursing (191)
- Nutrition (505)
- Obstetrics and Gynecology (650)
- Occupational and Environmental Health (643)
- Oncology (1752)
- Ophthalmology (524)
- Orthopedics (208)
- Otolaryngology (284)
- Pain Medicine (223)
- Palliative Medicine (66)
- Pathology (437)
- Pediatrics (999)
- Pharmacology and Therapeutics (419)
- Primary Care Research (402)
- Psychiatry and Clinical Psychology (3048)
- Public and Global Health (5980)
- Radiology and Imaging (1217)
- Rehabilitation Medicine and Physical Therapy (712)
- Respiratory Medicine (808)
- Rheumatology (367)
- Sexual and Reproductive Health (348)
- Sports Medicine (313)
- Surgery (385)
- Toxicology (50)
- Transplantation (170)
- Urology (142)

Get local news delivered to your inbox!
Subscribe to our Daily Headlines newsletter.

- Copy article link
Stanford researcher to address loss of trust in science and society
- RAVALLI REPUBLIC
- Apr 2, 2024
- ASSOCIATED PRESS, ASHLEY DEUTSCH FOR THE HARTSTONE-ROSE LAB
Researchers will observe how animals’ routines at the Fort Worth Zoo are disrupted during the April 8 total solar eclipse. The moon's shadow will sweep across North America including from Texas to Maine.
Well before the COVID-19 pandemic, Stanford University physician and microbiologist David Relman, M.D., realized research scientists like himself had a growing problem persuading people to trust their studies, results, conclusions, and even their intentions.
The COVID-19 pandemic elevated the problem to a crisis and personally affected him after he questioned the SARS-CoV-2 virus origin views of some of his peers.
Relman will discuss those experiences and potential remedies on April 19 at 7 p.m. at the Hamilton High School Performing Arts Center, 327 Fairgrounds Road. His presentation, “Trust in Science and Scientists: Why is it important, how is it so easily lost, and what will it take to restore it,” is part of a free outreach program sponsored by Rocky Mountain Laboratories (RML). The hour-long presentation is intended for a general audience and will include a brief time for questions.
People are also reading…
- Robbery suspect fatally shot by Hamilton police
- 21 electric buses headed to Bitterroot Valley schools
- Mining exploration company reports 'significant discovery' of gallium in Sheep Creek, something reported last year
- Easter events in the Bitterroot Valley
Bald eagle caught in leg-hold trap near Stevensville released
- Horse flies FedEx from Alabama to Billings to get prosthetic leg in Cody
Hamilton Christian Academy celebrates 60 years
- Kendall Cotton: Make Berkeley Pit great again
- 3 Montanans sentenced for fentanyl distribution in connection to 'Hulk' heroin
- Don 'K' Kaltschmidt: Say 'no' to Final Four
Fire in the Root hosting wildfire-landscaping workshops
- Miss Teen Rodeo Montana hosting fundraiser ahead of year on the road
- Ex-Montana State Bobcat Callahan O'Reilly keeps football dream alive with UFL's St. Louis Battlehawks
- Supreme Court gives AG until Friday to defend ballot statement
- In a major ruling, Montana Supreme Court strikes down 4 elections bills
Stanford researcher Dr. David Relman will give a presentation titled "Trust in Science and Scientists: Why is it important, how is it so easily lost, and what will it take to restore it,” on April 19 at 7 p.m. at the Hamilton High School Performing Arts Center, 327 Fairgrounds Road.
The breakdown in trust between scientists and the rest of society, Relman said, likely has several root causes:
• A general suspicion of so-called elites (of all kinds)
• A widening gulf between haves and have-nots
• The politicization of science in the setting of the increasing political polarization of society
• The inherent uncertainties in scientific findings
• The apparent inconsistencies between results of studies
“But the scientific community has contributed as well,” he said, “through miscommunication and over-interpretation of scientific findings, unaddressed conflicts of interest, lack of transparency about the conduct of science, and through rare but egregious acts of fraud.”
Evidence of the breakdown became more apparent during the pandemic and revealed “dire consequences,” he said. “I felt this personally when I became involved on a regular basis as an invited subject matter expert and guest host in town hall meetings held by my congressperson with her constituents starting in 2020, and heard directly from them.” Things worsened, he said, after he challenged “the prevailing opinion by some scientists about the origin of the pandemic and became a target of angry comments by other scientists and institutions.”
In spring 2021, Relman led an effort asking colleagues to keep an open mind on the origin of the COVID-19 virus, saying it wasn’t clear whether SARS-CoV-2 emerged naturally or from a laboratory accident. He was one of 18 scientists who signed a letter, published in "Science," raising those points.
More concerning than the personal attacks during the pandemic, Relman said, was the breakdown in public health, which for decades had been a core aspect of U.S. society. This breakdown led to broad and unnecessary health harm to thousands of distrusting people.
“In my presentation, I will offer thoughts about how trust might be rebuilt, why it is so important to achieve this, and the costs of failure,” Relman said. “Most importantly, I am eager to hear suggestions from the audience about possible collective actions.”
Relman is no stranger to complicated microbial threat scenarios and illness of unclear origin, according to a 2021 Stanford Medicine news article. He has advised the U.S. government on emerging infectious diseases and potential biological threats. He served as vice chair of a National Academy of Sciences committee reviewing the FBI investigation of letters containing anthrax that were sent in 2001. He chaired another academy committee that assessed “Havana syndrome,” a cluster of poorly explained illnesses in U.S. embassy employees. He is a past president of the Infectious Diseases Society of America.
His research focuses on microbiology, microbe-host interactions, the human microbiome, and biological threats.
“Dr. Relman is simply one of the most respected infectious disease experts in the world,” Dr. Marshall Bloom, RML associate director for scientific management, said. “In addition, he has studied the factors leading to a decline of public trust in scientists and science itself. This decline threatens the very credibility of public health, a dangerous situation already exposing us to the reemergence of diseases like measles.”
- Microbiology
- Scientific Terms
Related to this story
How do animals react during a total solar eclipse researchers notice strange behaviors.
Researchers will observe how animals’ routines at the Fort Worth Zoo are disrupted during the April 8 total solar eclipse. The moon's shadow w…
The Fire in the Root Council regularly offers free community education opportunities and said this time of year is ideal for planning and planting.
Hamilton Christian Academy is celebrating 60 years of educating students with a gala at Hamilton Assembly of God.
A bald eagle found in Stevensville in a leg-hold trap got a new lease on life recently after the iconic raptor was successfully rehabilitated …
Watch Now: Related Video
Trump to attack White House over border policy during Michigan visit
How to watch a solar eclipse safely with a pinhole camera, pope francis appeals for gaza cease-fire and russia-ukraine prisoner swap in easter sunday prayers, floating crane arrives at wreckage of baltimore's collapsed bridge.
- Provided photo
- Notifications
Get up-to-the-minute news sent straight to your device.
News Alerts
Breaking news.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 14, Issue 3
- Influence of COVID-19 pandemic in India on coronary artery disease clinical presentation, angiography, interventions and in-hospital outcomes: a single centre prospective registry-based observational study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-8356-3137 Rajeev Gupta 1 ,
- Krishnakumar Sharma 2 ,
- Raghubir Singh Khedar 1 ,
- Sanjeev Kumar Sharma 3 ,
- Jitender Singh Makkar 3 ,
- Vishnu Natani 3 ,
- Ajeet Bana 3 ,
- Samin Sharma 4
- 1 Medicine , Eternal Heart Care Centre and Research Institute , Jaipur , Rajasthan , India
- 2 Pharmacy , LBS College of Pharmacy, Rajasthan University of Health Sciences , Jaipur , Rajasthan , India
- 3 Cardiology , Eternal Heart Care Centre and Research Institute , Jaipur , Rajasthan , India
- 4 Cardiology , Mount Sinai Health System , New York , New York , USA
- Correspondence to Dr Rajeev Gupta; rajeevgg{at}gmail.com
Objective The study examined the influence of the COVID-19 pandemic in India on variation in clinical features, management and in-hospital outcomes in patients undergoing percutaneous coronary intervention (PCI).
Design Prospective registry-based observational study.
Setting A tertiary care hospital in India participant in the American College of Cardiology CathPCI Registry.
Participants 7089 successive patients who underwent PCI from April 2018 to March 2023 were enrolled (men 5627, women 1462). Details of risk factors, clinical presentation, coronary angiography, coronary interventions, clinical management and in-hospital outcomes were recorded. Annual data were classified into specific COVID-19 periods according to Government of India guidelines as pre-COVID-19 (April 2018 to March 2019, n=1563; April 2019 to March 2020, n=1594), COVID-19 (April 2020 to March 2020, n=1206; April 2021 to March 2022, n=1223) and post-COVID-19 (April 2022 to March 2023, n=1503).
Results Compared with the patients in pre-COVID-19 and post-COVID-19 periods, during the first COVID-19 year, patients had more hypertension, non-ST elevation myocardial infarction (NSTEMI), lower left ventricular ejection fraction (LVEF) and multivessel coronary artery disease (CAD). In the second COVID-19 year, patients had more STEMI, lower LVEF, multivessel CAD, primary PCI, multiple stents and more vasopressor and mechanical support. There were 99 (1.4%) in-hospital deaths which in the successive years were 1.2%, 1.4%, 0.8%, 2.4% and 1.3%, respectively (p=0.019). Compared with the baseline year, deaths were slightly lower in the first COVID-19-year (age-sex adjusted OR 0.68, 95% CI 0.31 to 1.47) but significantly more in the second COVID-19-year (OR 1.97, 95% CI 1.10 to 3.54). This variation attenuated following adjustment for clinical presentation, extent of CAD, in-hospital treatment and duration of hospitalisation.
Conclusions In-hospital mortality among patients with CAD undergoing PCI was significantly higher in the second year of the COVID-19 pandemic in India and could be one of the reasons for excess deaths in the country. These patients had more severe CAD, lower LVEF, and more vasopressor and mechanical support and duration of hospitalisation.
- Coronary intervention
- SARS-CoV-2 Infection
Data availability statement
Data are available upon reasonable request. Data may be obtained from a third party and are not publicly available. The data are available at ACC CathPCI website and are available to site investigators and other researchers upon reasonable request.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2023-078596
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The registry includes patients with coronary artery disease (CAD) before, during and following the COVID-19 pandemic in India.
More CAD deaths during the delta-wave of COVID-19 could partially explain the excess deaths in India during this period.
Data on prehospital pain-to-door time and door-to-balloon time are not available.
Extremely sick patients or those not suitable for coronary angioplasty have not been included.
This single hospital-based study may not be externally valid for the country.
Introduction
The pandemic of COVID-19 led to a large number of deaths at its peak during the years 2020–2022. 1–4 In developed countries, with robust healthcare systems and the availability of high-quality universal mortality statistics, these deaths were carefully enumerated and causes of excess deaths (incident deaths beyond the predicted usual) were provided. 3 It was estimated that while most of the excess deaths were directly related to COVID-19, a significant proportion was due to indirect effects of the pandemic due to non-availability or delays in seeking healthcare for medical emergencies such as acute coronary events, strokes and others. 1 In the UK it was estimated that during the pandemic years about one-third of excessive deaths were due to non-COVID-19 reasons. 5 Similar data are available from the USA and many European countries. 6–8 In India and most developing countries real-time mortality statistics enumerating causes of death are not available. 9 10 In contrast to the official number of less than half a million deaths from COVID-19 in India, some estimates have reported more than 2.5 million deaths during the 2 years when COVID-19 was rampant. 3 11–14 Many of these estimates are based on extrapolations from locally available data. 15–20
The COVID-19 pandemic in India led to severe disruptions in healthcare access, availability and quality of care for patients. 21 Excessive mortality beyond the official data was predicted. 22 In India, a proportion of excess deaths at the height of the COVID-19 pandemic could be due to hospitalisation delays leading to more advanced and complicated presentations in acutely ill patients without COVID-19 with coronary artery disease (CAD) or other cardiovascular, neurological, pulmonary and renal diseases. 23–25 CAD is the most important cause of death in India and delayed presentation following an acute coronary syndrome (ACS) is the most important cause of short-term and long-term mortality. 26 27 A proportion of excess deaths due to COVID-19 in India could have been due to such delays. As part of the American College of Cardiology (ACC) National Cardiovascular Disease Registry (NCDR) we have been systematically collecting data on all patients who undergo percutaneous coronary intervention (PCI) at our hospital. 28–30 To evaluate variations in CAD risk factors, clinical presentation, disease severity and in-hospital outcomes among successive patients who underwent PCI before, during and after the COVID-19 pandemic years in India, we analysed our hospital data.
This single-centre registry-based study has been conducted at Eternal Heart Care Centre & Research Institute, Jaipur (India). The CathPCI Registry at the hospital is part of the ACC-NCDR Centre of Excellence programme. 31 Informed consent was obtained from each participant included in the registry with specific consent for inclusion of anonymised data. The protocol of the study and all the data are available at ACC-NCDR website at: https://cvquality.acc.org/NCDR-Home/registries/hospital-registries/cathpci-registry .
Successive patients who underwent PCI at the hospital over a 60-month period, from April 2018 to March 2023, have been included. Clinical data were prospectively obtained at admission, coronary intervention and hospital discharge and entered into the NCDR database by research assistants. Details of the methodology have been previously reported. 28 Briefly, we obtained details regarding age and sex, risk factors- hypertension, diabetes, dyslipidaemias, tobacco use and chronic kidney disease, other laboratory investigations, clinical presentation (ST-segment myocardial infarction (STEMI) or non-STEMI (NSTEMI)/unstable angina and echocardiographic left ventricular ejection fraction (LVEF). We also recorded angiographic details of the location and extent of CAD and number of stents deployed. Almost all stents deployed (>99%) were drug-eluting. Details of in-hospital management with a specific focus on pharmacological vasopressors (norepinephrine, dopamine, vasopressin, etc), cardiac-support devices (intra-aortic balloon pump and miniature ventricular assist devices (mVAD) and post-discharge medications were also recorded.
In-hospital follow-up were duration of hospitalisation (hours), cardiovascular deaths and all-cause deaths.
Patient and public involvement
Patients were not involved in the study design, conduct, outcome measures or preparation of the manuscript.
Statistical analyses
The patients have been divided into three periods according to Government of India guidelines 32 : Pre-COVID-19 period: first year - April 2018 to March 2019 and second year - April 2019 to March 2020; COVID-19 period: third year - April 2020 to March 2021 and fourth year - April 2021 to March 2022; and Post-COVID-19 period: fifth year - April 2022 to March 2023. Severe restrictions and lockdowns in India started in the last week of March 2020, accordingly, the patients enrolled before 31st March 2020 have been included in pre-COVID-19 period. Lockdowns and restrictions continued for the next 2 years (COVID-19-phase) and were lifted in March 2022 when all restrictions were relaxed and international flights resumed. Therefore, the period from April 2022 to March 2023 has been categorised as post-COVID-19. Data have been downloaded from the ACC-NCDR website 31 and transferred to MS Excel worksheets. Data analyses have been performed using SPSS software (V.23). Continuous variables are reported as mean±1 SD and categorical variables as per cent. Non-normal data are presented as median with 25–75th percentile IQR. Inter-group differences have been determined using analysis of variance for continuous variables, χ 2 test for categorical variables and Kruskal-Wallis test for non-normal data. To identify the magnitude of inter-group difference in clinical presentation, angiographic findings, disease severity, clinical management, duration of hospitalisation and in-hospital outcomes in successive years, we calculated unadjusted; age-sex adjusted; age-sex, risk factors and presentation-adjusted; and multivariate-adjusted (age-sex, risk factors, presentation, left ventricular ejection fraction, extent of CAD, coronary stents, in-hospital therapies including vascular support and duration of hospitalisation) odds ratios (OR) and 95% confidence intervals (CIs) using stepwise logistic regression. The first year (April 2018 to March 2019) was the index. P values<0.05 are considered significant.
7089 successive patients (men 5627, women 1462) who underwent percutaneous coronary intervention from April 2018 to March 2023 have been enrolled. Mean age was 60.4±11 years (men 59.8±11 years, women 61.5±11). There was a significant prevalence of most coronary risk factors ( table 1 ). Previous PCI was in 945 (13.3%) and coronary bypass surgery in 237 (3.3%). Clinical presentation was predominantly as ACS (n=6735, 95.0%) with more NSTEMI/unstable angina (n=3934, 55.5%) compared with STEMI (n=2801, 39.5%). Mean LVEF at admission was 45±11%, about half of the patients had LVEF 30–45%, while low LVEF (<30%) was in 378 (5.3%). Coronary angiography revealed that most patients had disease of the left anterior descending artery (n=5633, 79.5%). Single vessel disease was in 2976 (42.0%), double vessel disease in 2378 (33.5%) and triple vessel disease in 1699 (24.0%). Drug-eluting stents were deployed in almost all with single stents in the majority (4661, 65.1%) and 506 (7.1%) patients had >3 stents. During hospitalisation, pharmacological vasopressor support was in 756 (10.7%) and mechanical support in 244 (3.4%). The deployment of a mVAD or extracorporeal membrane oxygenation was minimal. Median duration of hospital stay was 68.1 hours (IQR 51.1–84.0). There were 99 (1.4%) in-hospital deaths.
- View inline
Baseline characteristics of the study cohort
Clinical characteristics and interventions among PCI patients during successive years of the study in pre-COVID-19, COVID-19 and post-COVID-19 periods are shown in tables 2 and 3 . No difference in mean age or sex distribution is observed. There is no difference in the proportion of young patients <40 years age in various groups ( table 2 ). During COVID-19 years (April 2020 to March 2021 and April 2021 to March 2022) the prevalence of hypertension, diabetes, hypercholesterolaemia, kidney failure (creatinine >2 mg/dL) and previous PCI were more ( table 2 ). Presentation as STEMI was lower in the first year of COVID-19 and greater in the second (p<0.001). Echocardiography at admission revealed lower mean LVEF with a greater presence of very low EF (<30%) in the second year of COVID-19. Angiography revealed a greater prevalence of double and triple vessel disease during the COVID-19 and post-COVID-19 years. Primary PCI for STEMI was lower and pharmaco-invasive therapy was more during the first year of COVID-19. The pharmacoinvasive therapy was deployed according to Indian guidelines. 33 More coronary stents were deployed in the second year of COVID-19 ( table 3 ). The use of pharmacological vasopressors (norepinephrine, dopamine, vasopressin, etc) and mechanical support was also more during the second year of COVID-19. Both the mean and median duration of hospitalisation were significantly greater during the first and second COVID-19 years ( table 3 ).
Characteristics of patients undergoing PCI before, during and after COVID-19
Angiographic characteristics, interventions and outcomes of patients before, during and after COVID-19 pandemic
The incidence of in-hospital deaths in the five successive years was 1.2%, 1.4%, 0.8%, 2.4% and 1.3%, respectively, (χ 2 test, p=0.019) ( figure 1 ). Compared with pre-COVID-19 years, the deaths were lower in the first year of COVID-19 (0.8%) and significantly more during the second year (2.4%). Age and sex-adjusted, age, sex, risk factor and clinical presentation-adjusted and multivariate-adjusted logistic regression for in-hospital deaths at years 2, 3, 4 and 5 compared with the first year are shown in figure 2 . This shows that in the age-sex-adjusted model, compared with the baseline year, deaths were slightly lower in the first year of COVID-19 (age-sex adjusted OR 0.68, 95% CI 0.31 to 1.47) and significantly more in the second year (age-sex adjusted OR 1.97, 95% CI 1.10 to 3.54). The OR for deaths in the second year of COVID-19 increased further following adjustment for risk factors and clinical presentation (OR 2.33, 95% CI 1.28 to 4.22). This variation is completely attenuated following adjustment for age, sex, risk factors, clinical presentation, LVEF, extent of CAD, stents, in-hospital treatments and duration of hospitalisation (OR 1.00, 95% CI 0.52 to 1.94) ( figure 2 ).
- Download figure
- Open in new tab
- Download powerpoint
In-hospital deaths (%) during the pre-COVID-19, COVID-19 and post-COVID-19 years.
Age and sex adjusted; age, sex, risk factor and clinical presentation adjusted; and multivariate-adjusted ORs and 95% CIs for in-hospital deaths in pre-COVID-19 period (year 2), COVID-19 period (years 3 and 4) and post-COVID-19 period (year 5) compared with the baseline pre-COVID-19 year.
This single-hospital-based prospective percutaneous coronary intervention registry in India among patients with ACS from April 2018 to March 2023 shows that there was a doubling of in-hospital deaths during the second phase of COVID-19 (SARS-CoV-2 delta variant wave) 14 as compared with the pre-COVID-19 years. A higher death rate in the second COVID-19 year was associated with patients having more coronary risk factors, STEMI, lower LVEF, multivessel CAD, deployment of >3 coronary stents, higher use of pharmacological and mechanical vasopressor support and longer duration of hospitalisation. These findings suggest more severe cases with complex CAD. We cannot comment on delayed presentation as we do not have data on symptom-to-hospital, door-to-needle or door-to-balloon times.
Studies in the UK, Europe and the USA have reported considerable disruption of acute coronary care and cardiovascular services during the COVID-19 pandemic. 23 24 34–36 This was also associated with delays in seeking care following acute coronary events due to multiple factors including over-burdened ambulance services, less availability of trained emergency care personnel (who were deployed for COVID-19 patient care), greater use of pharmacological therapies for STEMIs and lower use of primary PCI. 35 36 All such data are available for high-income countries with limited data from lower-income countries such as India. 37 38 The present study shows that in the first year of the pandemic in India, there was a slight decline in COVID-19-related deaths suggesting a lack of access to healthcare for patients with ACS due to prolonged lockdowns. 39 40 The patients who reached the hospital were less sick resulting in slightly lower (though not significant) deaths following PCI. On the other hand, during the second wave of the pandemic in India (delta-variant wave in 2021), a doubling of deaths is observed ( figure 2 ). Patients with CAD who underwent PCI at the hospital during the second wave of the pandemic in India were sicker at presentation with more hypertension and diabetes, lower LVEF, more multivessel disease and had a greater need for multivessel stenting and pharmacological and mechanical circulatory support ( table 3 ). This is similar to studies from UK and USA. 24 36 Higher in-hospital deaths during the second wave attenuated after adjustment of these clinical variables. In India, the second COVID-19 wave was associated with a doubling of the pandemic-associated deaths compared with the first and subsequent waves. 41 42 The doubling of deaths following PCI in the present study suggests that many of the excess deaths due to COVID-19 in India could be related to non-COVID-19 reasons. However, the estimation of the excess deaths due to non-COVID-19 reasons in India shall require a comprehensive modelling exercise. More data from across the country are needed to model the contribution of CAD events for excess deaths as there is a large state-level variation in CAD incidence. 43
There are many reasons for variability in CAD deaths during COVID-19 as observed in the present study. Apart from healthcare-seeking delays for acute coronary events, a substantial decline in control of important cardiovascular risk factors (hypertension, hypercholesterolaemia and diabetes), more sedentariness, confined indoor activities and exposure to indoor pollution, mental stress, increased tobacco and alcohol use, etc could be responsible. 44 The biological effects of acute COVID-19 infection on the vascular system (endothelialitis, thrombosis, etc) as well as long-term influence on vascular reactivity and plaque destabilisation are also important. 45 All these factors need more studies.
Limitations of the study include a tertiary care location of the study and our data is not nationally representative. A large number of patients with private health insurance (40%) also suggests a skewed sample and is not representative of India, where only 10–15% have such insurance. 28 We also did not include all the patients with ACS presenting to the hospital as patients who do not undergo PCI were not enrolled in the ACC-NCDR CathPCI Registry. More sick patients or those with severe CAD, not suitable for PCI have not been included. There is no information regarding symptom-to-hospital, door-to-needle or door-to-balloon times and this is an important study limitation. Studies have reported that COVID-19 pandemic led to delayed presentation following ACS. 23 We have no data on geographic, social, economic and other determinants that influence prehospital delays, 27 especially during the COVID-19 pandemic. 36 38 We also do not have data on the status of cardiovascular risk factor control at admission. A low representation of women is also an important limitation, but the data are similar to other Indian CAD registries. 27 The lack of long-term follow-up data is also an important limitation as in-hospital events are likely an underestimate of the true influence of the pandemic on cardiovascular outcomes. 3 On the other hand, this is one of the larger prospective CAD intervention registries from lower-middle income countries. We enrolled patients with CAD before, during and following the COVID-19 pandemic and could identify variations in the characteristics of the patients with CAD and in-hospital outcomes. Standardised and comparable data have been obtained as part of the ACC-NCDR CathPCI Registry.
In conclusion, the present study that used annual data of patients with CAD undergoing PCI shows a lower death rate (possibly related to reduced access to care) during the first year of the COVID-19 pandemic in India and a doubling of in-hospital mortality during the second year. The latter was associated with more severe disease at presentation, more multivessel CAD and greater deployment of coronary stents. These patients also required more pharmacological and mechanical vascular support. COVID-19-like pandemics are likely to recur. Increased cardiovascular mortality as demonstrated in the present study can be ameliorated by multiple health system interventions. 46 Development of well-equipped healthcare infrastructure trained to function during an infectious disease pandemic is required. Strategies include widespread availability of pandemic-proof ambulances and supply chain logistics; well-trained healthcare workers, nurses and clinicians; provision of acute coronary care including invasive care during an epidemic with the deployment of multidisciplinary teams. 46 Technology has a huge role in disease surveillance, monitoring of healthcare workers and managing logistics during such an epidemic. 47 Artificial intelligence-based systems can provide seamless care to the needy. 47 All these initiatives are important to reduce excess deaths from cardiovascular events during infectious disease pandemics.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by Institutional Ethics Committee, Eternal Heart Care Centre & Research Institute, Jaipur, Government of India, Registration No. ECR/615/Inst/RJ/2014/RR-20. Participants gave informed consent to participate in the study before taking part.
- Ioannidis JPA
- COVID-19 Cumulative Infection Collaborators
- COVID-19 Excess Mortality Collaborators
- Schöley J ,
- Aburto JM ,
- Kashnitsky I , et al
- Kashyap R ,
- Schöley J , et al
- Masters RK ,
- Sati P , et al
- Zimmermann LV ,
- Salvatore M ,
- Babu GR , et al
- Deshmukh Y ,
- Tumbe C , et al
- Guilmoto CZ
- Novosad P ,
- Tandel V , et al
- Sharma AK ,
- Baig VN , et al
- Lewnard JA ,
- Narayan T , et al
- Clarke JM ,
- Jain V , et al
- India State-Level Disease Burden Initiative Collaborators
- Sundararaman T ,
- Rajendran P , et al
- Muniyandi M ,
- Aanandh Y , et al
- Kontopantelis E ,
- Webb RT , et al
- Banerjee A ,
- Pasea L , et al
- Li S , et al
- Khedar RS ,
- Gaur K , et al
- Makkar JS ,
- Sharma SK , et al
- Sharma SK ,
- Bana A , et al
- Sharma KK , et al
- ↵ American College of Cardiology’s CathPCI registry . Available : https://cvquality.acc.org/NCDR-Home/registries/hospital-registries/cathpci-registry [Accessed 30 Apr 2023 ].
- ↵ COVID-19 pandemic in India . Available : https://en.wikipedia.org/wiki/COVID-19_pandemic_in_India [Accessed 18 Feb 2024 ].
- Kerkar PG ,
- Alexander T , et al
- Mathieu E ,
- Ritchie H ,
- Rodes-Guirao LR , et al
- Mattiuzzi C ,
- Czeisler MÉ ,
- Marynak K ,
- Clarke KEN , et al
- Zachariah G ,
- Mohanan PP , et al
- Xiao Y , et al
- Mukherjee A ,
- Sharma RK , et al
- Mittal K , et al
- Xavier D , et al
- Kaushik A ,
- Johnson L , et al
- Chen DG , et al
Twitter @rajeevgg
Contributors RG, SKS and SS initiated the study. RG, KS, RSK and VN contributed to project administration, supervision and analyses. SKS, JSM, AB and SS supervised the study conduct and contributed to the study with patient management. RG and KS performed the statistical analyses. RG wrote the first and revised all the subsequent drafts. All the authors reviewed and provided critical inputs to the manuscript. RG is responsible for the overall content and is the guarantor.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
55 templates

8 templates

44 templates

solar eclipse
25 templates

13 templates
philippines
38 templates
Linear COVID-19 Prevention
Free google slides theme and powerpoint template.
Currently, all information concerning preventive measures against COVID-19 is crucial and should be accessible for everybody. Explain them in the form of infographics, since images convey a lot. Edit our linear-style timelines, charts and diagrams to maximize the chances of your message reaching the public.
Features of these infographics
- 100% editable and easy to modify
- 30 different infographics to boost your presentations
- Include icons and Flaticon’s extension for further customization
- Designed to be used in Google Slides, Microsoft PowerPoint and Keynote
- 16:9 widescreen format suitable for all types of screens
- Include information about how to edit and customize your infographics
How can I use the infographics?
Am I free to use the templates?
How to attribute the infographics?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access

- The Power of mRNA
- Responsibility
News Details
Moderna advances multiple vaccine programs to late-stage clinical trials.
Announces next-generation COVID-19 vaccine candidate as fourth respiratory vaccine to successfully meet its Phase 3 endpoints
Expects two more Phase 3 readouts in 2024, including combination vaccine against flu and COVID-19, and vaccine against CMV
Announces positive clinical trial data from three new vaccines against viruses that cause significant burden (Epstein-Barr virus, Varicella-Zoster virus, norovirus) and advances programs toward Phase 3 development
Anticipates U.S. launch of vaccine against RSV following FDA approval and ACIP recommendation in 2024
Announces development and commercialization funding agreement with Blackstone Life Sciences for up to $750 million to advance flu program
"Our mRNA platform continues a remarkable track record across our broad vaccine portfolio. Today, we are excited to share that four vaccines in our pipeline have achieved successful clinical readouts across our respiratory, latent and other virus franchises," said Stéphane Bancel, Chief Executive Officer of Moderna. "With five vaccines in Phase 3, and three more moving toward Phase 3, we have built a very large and diverse portfolio addressing significant unmet medical needs. We are focused on execution to further build momentum across our pipeline and business, and to deliver for patients who are impacted by these infectious diseases."
Portfolio Overview
The vaccine portfolio seeks to address infectious diseases that cause considerable health burdens and includes 28 vaccines addressing respiratory, latent and other pathogens.
Latent and Other Vaccine Portfolio
Moderna is advancing five vaccine candidates against viruses that cause latent infections, all of which are in clinical trials. When latent, a virus is present in the body but exists in a resting state, typically without causing any noticeable symptoms. Latent viruses can reactivate and cause clinical symptoms as a person ages, during times of stress or when immunity is compromised. The capacity for latency is a defining feature of members of the Herpesviridae family, including cytomegalovirus (CMV), Epstein-Barr virus (EBV), herpes simplex virus (HSV) and Varicella-Zoster virus (VZV).
Cytomegalovirus (CMV)
CMV is the most common infectious cause of birth defects in the U.S. and is responsible for several billion dollars in annual healthcare costs. One in 200 babies in the U.S. are born with a congenital CMV infection, and of those affected, one in five will have severe, life-altering health problems. Possible short- and long-term sequelae of CMV infection include microcephaly, chorioretinitis, seizures, sensorineural hearing loss, cognitive impairment and cerebral palsy. There is currently no approved vaccine to prevent congenital CMV.
CMVictory is a pivotal Phase 3 trial evaluating mRNA-1647 against primary CMV infection in women 16 to 40 years of age. The trial is a randomized, observer-blind, placebo-controlled study designed to evaluate the efficacy, safety and immunogenicity of mRNA-1647. The trial is fully enrolled with approximately 7,300 participants from 290 clinical sites globally.
To date, 50 primary infection cases have accrued and are undergoing confirmation. The first interim analysis for the evaluation of vaccine efficacy, which will be triggered when both 81 confirmed per-protocol cases and 12 median months of safety follow-up have occurred, is expected as early as the end of 2024.
Moderna's CMV vaccine candidate mRNA-1647 has advanced to indication expansion studies in adolescents 9 to 15 years of age and adult transplant patients, both of which have begun enrollment.
Epstein-Barr virus (EBV)
EBV is a major cause of infectious mononucleosis (IM) in the U.S., accounting for more than 90% of IM cases annually. Importantly, EBV and IM are associated with a higher lifetime risk of more serious sequelae including certain cancers such as gastric carcinoma, nasopharyngeal carcinoma and multiple types of lymphoma. The lifetime risk of developing multiple sclerosis (MS) is increased by 32-fold after EBV infection. There is currently no approved vaccine to prevent EBV.
Moderna's EBV vaccine candidates are designed to tackle multiple EBV-associated conditions, including prevention of IM (mRNA-1189) and MS and post-transplant lymphoproliferative disorder, a subcategory of lymphoma in solid organ transplant patients (mRNA-1195) . The Phase 1 trial for mRNA-1189 was designed to test the safety, reactogenicity and immunogenicity of four different dose levels in participants 12 to 30 years of age in the U.S. The randomized, observer-blind, placebo-controlled study showed mRNA-1189 was immunogenic and generally well tolerated across all dose levels. The Company is advancing mRNA-1189 toward a pivotal Phase 3 trial.
The Phase 1 trial for mRNA-1195 was designed to test the safety, reactogenicity and immunogenicity of two drug products at four different dose levels in healthy EBV seropositive participants 18 to 55 years of age in the U.S. The randomized, observer-blind, placebo-controlled study is fully enrolled.
Herpes simplex virus (HSV)
Herpes simplex virus type 2 (HSV-2) infects approximately 13% of adults globally and is the primary cause of genital herpes. There are an estimated four billion people globally infected with HSV, of which 491 million cases are HSV-2. Recurrent genital herpes causes a reduction in quality of life, which antivirals (current standard of care) only partially restore. Moderna expects that if an HSV vaccine candidate could deliver similar efficacy as a suppressive antiviral treatment, compliance with recommended therapy and associated quality of life would improve. There is currently no approved vaccine to treat HSV-2.
The first in human, fully enrolled Phase 1/2 trial of mRNA-1608 is designed to test safety and immunogenicity and to establish a proof-of-concept of clinical benefit in adults 18 to 55 years of age with recurrent HSV-2 genital herpes. The randomized 1:1:1:1, observer-blind, controlled study is fully enrolled with 300 participants in the U.S.
Varicella-Zoster virus (VZV)
Herpes zoster, also known as shingles, is caused by reactivation of latent VZV, the same virus that causes chickenpox. Declining immunity in older adults decreases immunity against VZV, allowing reactivation of the virus from latently infected neurons, causing painful and itchy lesions. Herpes Zoster occurs in one out of three adults in the U.S. in their lifetime and the incidence increases at 50 years of age. There is potential to reach a growing and underserved patient population.
Moderna's VZV vaccine candidate mRNA-1468 has initial data available from a Phase 1/2 trial, which was designed to test safety and immunogenicity in healthy adults 50 years of age and older in the U.S. The randomized 1:1:1:1:1, observer-blind, active-controlled study of mRNA-1468 elicited strong antigen-specific T cell responses at one month after the second dose and was generally well tolerated. Results of the first interim analysis support the further clinical development of mRNA-1468 for the prevention of shingles. Additional results from the ongoing Phase 1/2 study will be available later this year, including persistence data. The Company is planning for a pivotal Phase 3 trial. Norovirus
Enteric viruses, including norovirus, are a leading cause of diarrheal diseases, resulting in significant morbidity and mortality worldwide, particularly among young children and older adults. Norovirus is highly contagious and a leading cause of diarrheal disease globally, associated with 18% of all acute gastroenteritis (AGE), resulting in approximately 200,000 deaths per year and substantial healthcare costs. Given the wide diversity of norovirus genotypes, a broadly effective norovirus vaccine will require a multivalent vaccine design. There is currently no approved vaccine to prevent norovirus.
The randomized, observer-blind, placebo-controlled Phase 1 trial was designed to evaluate the safety, reactogenicity and immunogenicity of trivalent (mRNA-1403) and pentavalent (mRNA-1405) norovirus vaccine candidates in 664 participants 18 to 49 years of age and 60 to 80 years of age in the U.S. An interim analysis showed that a single dose of mRNA-1403 elicited a robust immune response across all dose levels evaluated with a clinically acceptable reactogenicity and safety profile. The Company is advancing mRNA-1403 toward a pivotal Phase 3 trial.
Respiratory Vaccine Portfolio
Moderna's approach to ease the global burden of respiratory infections includes vaccine candidates against major causative pathogens, including SARS-CoV-2, respiratory syncytial virus (RSV) and influenza virus. Respiratory infections are a top cause of death in the U.S. and are particularly harmful to the young, immunocompromised, and older adults who experience more severe illness, greater incidence of hospitalization, and greater mortality than younger adults.
Moderna's respiratory pipeline includes Phase 3 trials for investigational vaccines including a next-generation COVID-19 vaccine, an RSV vaccine, a flu vaccine, and a flu and COVID-19 combination vaccine. The pipeline includes three additional flu vaccine candidates with expanded antigen coverage as well as combination vaccine programs.
Moderna continues to address the needs of the endemic COVID-19 market by focusing on public health efforts to increase vaccination coverage rates to reduce the substantial burden of COVID-19 as well as by advancing next-generation vaccines. The Company's mRNA platform can produce variant-matched vaccines on an accelerated time horizon, consistent with recent U.S. Food and Drug Administration (FDA) comments on the timing of potential strain selection for the fall booster season.
A recent announcement of positive interim results from the NEXTCove Phase 3 trial showed that mRNA-1283 elicited a higher immune response against both the Omicron BA.4/BA.5 and original virus strains of SARS-CoV-2 compared to mRNA-1273.222, Moderna's licensed COVID-19 vaccine. mRNA-1283 is designed to be refrigerator-stable and paves the way for a combination vaccine against influenza and COVID-19, mRNA-1083, enhancing the Company's overall respiratory portfolio. This is Moderna's fourth infectious disease vaccine program with Phase 3 data.
Respiratory Syncytial Virus (RSV)
RSV is the leading cause of respiratory illness in young children, and older adults are at increased risk relative to younger adults for severe outcomes. In addition to acute mortality and morbidity, RSV infection is associated with long-term sequelae such as asthma and impaired lung function in pediatric populations, and exacerbation of chronic obstructive pulmonary disease in older adults. Annually, there are approximately two million medically attended RSV infections and 58,000 to 80,000 hospitalizations in children younger than five years old in the U.S. In the U.S., each year there are up to 160,000 hospitalizations and 10,000 deaths in adults 65 years and older due to RSV. Across high-income countries in 2019, RSV caused an estimated 5.2 million cases, 470,000 hospitalizations and 33,000 in-hospital deaths in adults 60 years and older.
Moderna's RSV vaccine candidate, mRNA-1345, is in an ongoing Phase 2/3, randomized, observer-blind, placebo-controlled case-driven trial (ConquerRSV) in adults over 60 years of age. In this study, approximately 37,000 participants from 22 countries were randomized 1:1 to receive one dose of mRNA-1345 or placebo.
Based on positive data from the ConquerRSV trial, Moderna has filed for regulatory approvals for mRNA-1345 for the prevention of RSV-associated lower respiratory tract disease (RSV-LRTD) and acute respiratory disease (ARD) in adults over 60 years of age.
The trial met both its primary efficacy endpoints, with a vaccine efficacy (VE) of 83.7% (95.88% CI: 66.1%, 92.2%; p<0.0001) against RSV-LRTD as defined by two or more symptoms, and a VE of 82.4% (96.36% CI: 34.8%, 95.3%; p=0.0078) against RSV-LRTD defined by three or more symptoms. These data were published in the New England Journal of Medicine in December 2023.
A subsequent analysis from the ConquerRSV study with a longer median follow-up duration of 8.6 months (versus 3.7 months in the primary analysis), with a range of 15 days to 530 days, and including subjects from the Northern and Southern Hemispheres was recently presented at the RSVVW'24 conference . In this supplemental analysis, mRNA-1345 maintained durable efficacy, with sustained VE of 63.3% (95.88% CI: 48.7%, 73.7%) against RSV-LRTD including two or more symptoms. VE was 74.6% (95% CI: 50.7%, 86.9%) against RSV-LRTD with ≥2 symptoms, including shortness of breath and 63.0% (95% CI: 37.3%, 78.2%) against RSV-LRTD including three of more symptoms. The stringent statistical criterion of the study, a lower bound on the 95% CI of >20%, continued to be met for both endpoints.
mRNA-1345 has been granted Breakthrough Therapy designation by the FDA for the prevention of RSV-LRTD in adults over 60 years of age. The Company is awaiting regulatory approvals and the U.S. ACIP recommendation in 2024.
Indication expansion studies for mRNA-1345
mRNA-1345 has the potential to protect all vulnerable populations from RSV. Moderna has initiated multiple Phase 3 expansion studies in adults over 50 years of age to evaluate co-administration and revaccination. Additional trials (Phase 1 - Phase 3) have been initiated for high-risk adults, as well as maternal and pediatric populations. Interim data from these studies could be available as early as 2024.
Influenza (Flu)
Worldwide, influenza leads to 3-5 million severe cases of flu and 290,000-650,000 flu-related respiratory deaths annually. Two main types of influenza viruses (A and B) cause seasonal flu epidemics, and the influenza A viruses lead to most flu-related hospitalization in older adults.
The Company has several seasonal influenza vaccine candidates in clinical development. Moderna's seasonal flu vaccine, mRNA-1010 , demonstrated consistently acceptable safety and tolerability across three Phase 3 trials. In the most recent Phase 3 trial (P303), which was designed to test the immunogenicity and safety of an optimized vaccine composition, mRNA-1010 met all immunogenicity primary endpoints, demonstrating higher antibody titers compared to a currently licensed standard-dose flu vaccine. In an older adult extension study of P303, mRNA-1010 is being studied against high dose Fluzone HD ® ; the trial is fully enrolled. The Company is in ongoing discussions with regulators and intends to file in 2024.
Combination Respiratory Vaccines
Moderna's combination vaccine candidates cover respiratory viruses associated with the largest disease burden in the category. The Phase 3 combination study of the Company's investigational combination vaccine against flu and COVID-19 (mRNA-1083) for adults aged 50 years and older is fully enrolled and data are expected in 2024. mRNA-1083 was granted Fast Track designation by the FDA in May 2023.
Commercial Updates
Respiratory viruses in addition to latent and other viruses represent large unmet or underserved medical needs, and the human and economic costs from these infectious diseases highlight the need for effective vaccines. To help address this need, Moderna expects multiple vaccine product launches in the next few years, each with significant addressable markets.
The 2024 global endemic COVID-19 vaccine market alone is estimated by Moderna to be approximately $10 billion. COVID-19 continues to show a high burden of disease, and while COVID-19 hospitalizations remain high relative to RSV and flu, the risks of Long COVID are also becoming better understood. Moderna is focused on improving education and awareness to increase vaccination rates as Long COVID data suggests even traditionally low-risk groups should be vaccinated. Moderna is also working with health authorities to align the timing of COVID-19 and flu vaccine launches to help improve public health.
For RSV, Moderna estimates the peak annual market to be approximately $10 billion. The Company expects a strong RSV vaccine launch into a large market in 2024. As the only mRNA investigational vaccine with positive Phase 3 data, Moderna's RSV vaccine candidate has a strong profile with consistently strong efficacy across vulnerable and older populations, a well-established safety and tolerability profile, and ease of administration with a ready-to-use, pre-filled syringe formulation, which could relieve some of the burden that falls on pharmacies during the fall vaccination season.
An interim analysis from an ongoing time and motion study evaluating differences in preparation time between a pre-filled syringe (PFS) presentation and vaccines that require reconstitution showed that a PFS presentation could relieve some of the burden that falls on pharmacies during the fall vaccination season. Results from this study suggest that pharmacies may be capable of preparing up to four times as many doses of PFS in an hour compared to vaccines requiring reconstitution.
Moderna estimates flu vaccines represent an approximately $7 billion market in 2024. The market is expected to grow with the rise of more effective vaccines and there is an opportunity to expand the market with next-generation premium flu vaccines as well as combination respiratory vaccines, adding increased value to the health ecosystem.
CMV is expected to be a $2-5 billion annual market. With no vaccine currently on the market and a potential vaccine launch in 2026, Moderna could be the first CMV vaccine in multi-billion-dollar latent vaccine market. In addition, EBV has the potential to address and reduce the burden and cost of EBV infection in multiple populations, while VZV provides the opportunity to enter a large and growing market, which could be $5-6 billion annually. The market for norovirus vaccines is similar to that of rotavirus in pediatrics with opportunity to expand into the adult population, and represents a $3-6 billion annual market.
Moderna's vaccine portfolio targets large addressable markets, with an estimated total addressable market (TAM) of $52 billon for Moderna infectious disease vaccines, which includes a respiratory vaccines TAM of more than $27 billion and a latent and other vaccines TAM of more than $25 billion.
Manufacturing
The Company's manufacturing innovation supports expanding commercialization of a diverse pipeline through efficiency and productivity gains. Its mRNA manufacturing platform enables benefits such as quality, speed, scale and cost efficiency across a footprint that broadly includes the manufacture of plasmid, mRNA, lipid nanoparticles, as well as fill/finish and quality control capabilities.
As the Company continues to build its footprint for the future, it is developing an agile global manufacturing network to meet commercial demand and support its growing pipeline. Pre-clinical through commercial manufacturing occurs at the Moderna Technology Center in Norwood, Massachusetts, which remains central to the Company's network. New facilities being constructed in Australia, Canada and the UK are expected to come online in 2025, and drug product capacity is achieved through a flexible contract manufacturing network. Additionally, the Company has purchased and started build-out of a manufacturing site in Marlborough, Massachusetts, to enable commercial scale of its individualized neoantigen therapy program.
By continuing to pioneer new technologies, including advanced robotics, applying AI and other digital solutions, and driving network and capital efficiency, Moderna's manufacturing network is expected to also drive more predictable cost of sales.
Research and Development Investment Strategy
Today's updates provide further evidence that Moderna's mRNA technology platform is working, and with a rate of success higher than industry standard. Looking ahead, research and development will continue to be the Company's top capital allocation priority.
As Moderna looks to create value through the research and development strategy for its vaccine portfolio, it is taking three prioritization parameters into consideration: pipeline advancement, revenue diversification and risk reduction. As part of its strategy, the funding options Moderna considers are self-funding, project financing and partnerships.
Moderna recently entered into a development and commercialization funding agreement with Blackstone Life Sciences to advance the Company's flu program. As part of the agreement, Blackstone will fund up to $750 million with a return based on cumulative commercial milestones and low-single digit royalties. Moderna expects to recognize the funding as a reduction in research and development expenses and will retain full rights and control of the Company's flu program. This funding does not result in any change to Moderna's 2024 research and development framework spending of approximately $4.5 billion.
About Moderna
Moderna is a leader in the creation of the field of mRNA medicine. Through the advancement of mRNA technology, Moderna is reimagining how medicines are made and transforming how we treat and prevent disease for everyone. By working at the intersection of science, technology and health for more than a decade, the company has developed medicines at unprecedented speed and efficiency, including one of the earliest and most effective COVID-19 vaccines.
Moderna's mRNA platform has enabled the development of therapeutics and vaccines for infectious diseases, immuno-oncology, rare diseases and autoimmune diseases. With a unique culture and a global team driven by the Moderna values and mindsets to responsibly change the future of human health, Moderna strives to deliver the greatest possible impact to people through mRNA medicines. For more information about Moderna, please visit modernatx.com and connect with us on X (formerly Twitter), Facebook, Instagram, YouTube and LinkedIn.
INDICATION (U.S.)
SPIKEVAX (COVID-19 Vaccine, mRNA) is a vaccine indicated for active immunization to prevent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in individuals 18 years of age and older.
IMPORTANT SAFETY INFORMATION
- Do not administer to individuals with a known history of severe allergic reaction (e.g., anaphylaxis) to any component of the vaccine.
- Appropriate medical treatment to manage immediate allergic reactions must be immediately available in the event an acute anaphylactic reaction occurs following administration of the vaccine.
- Postmarketing data demonstrate increased risks of myocarditis and pericarditis, particularly within 7 days following the second dose. The observed risk is higher among males under 40 years of age than among females and older males. The observed risk is highest in males 18 through 24 years of age.
- Syncope (fainting) may occur in association with administration of injectable vaccines. Procedures should be in place to avoid injury from fainting.
- Immunocompromised persons, including individuals receiving immunosuppressive therapy, may have a diminished response to the vaccine.
- The vaccine may not protect all vaccine recipients.
- Adverse reactions reported in clinical trials following administration of the vaccine include pain at the injection site, fatigue, headache, myalgia, arthralgia, chills, nausea/vomiting, axillary swelling/tenderness, fever, swelling at the injection site, and erythema at the injection site, and rash.
- The vaccination provider is responsible for mandatory reporting of certain adverse events to the Vaccine Adverse Event Reporting System (VAERS) online at https://vaers.hhs.gov/reportevent.html or by calling 1-800-822-7967.
- Please see the SPIKEVAX Full Prescribing Information . For information regarding authorized emergency uses of the Moderna COVID-19 Vaccine, please see the EUA Fact Sheet .
Spikevax ® is a registered trademark of Moderna. Fluzone ® is a registered trademark of Sanofi Pasteur. Forward-Looking Statements
This press release contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995, as amended, including statements regarding: the advancement of Moderna's programs under clinical development; the timing for anticipated approvals of vaccine candidates; the efficacy, safety and tolerability of vaccine candidates; the total addressable markets for programs under development; the efficiencies and advantages of Moderna's mRNA platform; future capital allocation and financing efforts; and anticipated spending for R&D in 2024. In some cases, forward-looking statements can be identified by terminology such as "will," "may," "should," "could," "expects," "intends," "plans," "aims," "anticipates," "believes," "estimates," "predicts," "potential," "continue," or the negative of these terms or other comparable terminology, although not all forward-looking statements contain these words. The forward-looking statements in this press release are neither promises nor guarantees, and you should not place undue reliance on these forward-looking statements because they involve known and unknown risks, uncertainties, and other factors, many of which are beyond Moderna's control and which could cause actual results to differ materially from those expressed or implied by these forward-looking statements. These risks, uncertainties, and other factors include, among others, those risks and uncertainties described under the heading "Risk Factors" in Moderna's Annual Report on Form 10-K for the fiscal year ended December 31, 2023, filed with the U.S. Securities and Exchange Commission (SEC), and in subsequent filings made by Moderna with the SEC, which are available on the SEC's website at www.sec.gov . Except as required by law, Moderna disclaims any intention or responsibility for updating or revising any forward-looking statements contained in this presentation in the event of new information, future developments or otherwise. These forward-looking statements are based on Moderna's current expectations and speak only as of the date of this press release.
Moderna Contacts
Media: Chris Ridley Head, Global Media Relations +1 617-800-3651 [email protected]
Investors: Lavina Talukdar Senior Vice President & Head of Investor Relations +1 617-209-5834 [email protected]
SOURCE: Moderna, Inc.
Quick Links
- SEC Filings
- Investor FAQs
- Information Request Form
Investor Email Alerts
To opt-in for investor email alerts, please enter your email address in the field below and select at least one alert option. After submitting your request, you will receive an activation email to the requested email address. You must click the activation link in order to complete your subscription. You can sign up for additional alert options at any time.
At Moderna, we promise to treat your data with respect and will not share your information with any third party. You can unsubscribe to any of the investor alerts you are subscribed to by visiting the ‘unsubscribe’ section below. If you experience any issues with this process, please contact us for further assistance.
By providing your email address below, you are providing consent to Moderna to send you the requested Investor Email Alert updates.
Email Alert Sign Up Confirmation
Investor overview
Press releases
Media Center
Partnerships.
Strategic collaborators
Company culture
People behind the science
Join our team
Innovation Incubator
New venture labs
- Terms of Use
- Privacy Policy
- Contact Moderna
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

Clinical presentation and management of COVID ‐19
Irani thevarajan.
1 Victorian Infectious Diseases Service, Royal Melbourne Hospital, Melbourne VIC
2 University of Melbourne, Melbourne VIC
Kirsty L Buising
Benjamin c cowie.
3 WHO Collaborating Centre for Viral Hepatitis, Doherty Institute, Melbourne VIC
- The rapid spread of severe acute respiratory syndrome coronavirus 2 led to the declaration of a global pandemic within 3 months of its emergence.
- The majority of patients presenting with coronavirus disease 2019 ( COVID ‐19) experience a mild illness that can usually be managed in the community. Patients require careful monitoring and early referral to hospital if any signs of clinical deterioration occur.
- Increased age and the presence of comorbidities are associated with more severe disease and poorer outcomes.
- Treatment for COVID ‐19 is currently predominantly supportive care, focused on appropriate management of respiratory dysfunction.
- Clinical evidence is emerging for some specific therapies (including antiviral and immune‐modulating agents). Investigational therapies for COVID ‐19 should be used in the context of approved randomised controlled trials.
- Australian clinicians need to be able to recognise, diagnose, manage and appropriately refer patients affected by COVID ‐19, with thousands of cases likely to present over the coming years.
In December 2019, a novel coronavirus emerged in Wuhan, Hubei Province, China, leading to a global pandemic. The virus, named severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), causes a clinical syndrome termed coronavirus disease 2019 (COVID‐19).
The first reports of an undiagnosed pneumonia in Wuhan on 8 December 2019 were followed by an alert from China to the World Health Organization (WHO) about a cluster of pneumonia cases on 30 December. Isolation of a novel coronavirus occurred on 3 January 2020. On 30 January, the WHO declared a public health emergency of international concern, and a pandemic was declared on 12 March 2020.
Clinical presentation
Similar to other coronaviruses, SARS‐CoV‐2 is predominantly spread by respiratory droplets, although spread by contact with contaminated fomites also occurs, as does transmission by aerosols in certain circumstances. 1
Based on the experience in China, the typical incubation period of COVID‐19 infection has been estimated to be a median of 5.1 days (95% CI, 4.5–5.8 days), with 97.5% of those who develop symptoms doing so within 11 days of exposure (95% CI, 8.2–15.6 days). This has informed the use of a 14‐day time period for quarantining potentially exposed individuals in an effort to limit onward spread. 2
The recognition of asymptomatic infection has been an area of intense interest in understanding the epidemiology of COVID‐19. The ratio of asymptomatic to symptomatic infection is currently uncertain. Cross‐sectional studies have reported asymptomatic infection in women attending a maternity service in New York (33 of 215 infected, 88% asymptomatic) 3 and in general population testing in Iceland (87 of 10 797 infected, 41% asymptomatic). 4 In such cross‐sectional studies, a proportion of those who were asymptomatic at the time of testing may in fact have been in the pre‐symptomatic phase of infection. In a study conducted in a nursing home in the United States, 48 of 76 residents tested positive, with 27 (56%) being asymptomatic at the time of testing. However, 24 (89%) of these individuals went on to develop symptoms at a median of 4 days (interquartile range [IQR], 3–5 days) after the positive test result. 5
Symptomatic COVID‐19 infection usually presents as a respiratory syndrome, most commonly with fever and cough. 6 , 7
Fever has been reported in up to 99% of people at some time during the course of their illness, but importantly in one cohort, it was reported to be present at the time of hospital presentation in only 44% of patients, and at some time during the hospital admission in 89%. 8 Other common symptoms are cough, dyspnoea, fatigue, anorexia, anosmia, myalgia and sometimes confusion. Diarrhoea may occur in up to 10% of patients. 9 Symptoms reported less frequently (< 5% of cases) include sore throat, rhinorrhoea, headache, chest pain, dizziness, abdominal pain and nausea. 6 , 7
Around 80% of COVID‐19 infections present as a mild respiratory illness in a patient who is ambulatory and can generally be managed outside the hospital. Around 15% typically need hospital care (usually for moderate to severe pneumonia), and another 5% have critical illness requiring more intensive supports. 10
Of those who require hospitalisation, the median time from first symptoms to onset of dyspnoea is 5 days (IQR, 1–10 days), the median time to hospital admission is 7 days (IQR, 4–8 days), and in those who develop more severe manifestations, the median time to acute respiratory distress syndrome is 8 days (IQR, 6–12 days). 6 About a quarter of patients who are hospitalised may need transfer to the intensive care unit (ICU) for the management of complications such as hypoxaemic respiratory failure or hypotension requiring vasopressor support. 11
At presentation to hospital, the most common laboratory feature of COVID‐19 infection is lymphopenia (reported in 70.3% of cases). 6 Radiological imaging may reveal a clear chest, unilateral or bilateral consolidation, or ground glass opacity.
Nasopharyngeal specimens, deep nasal swabs, throat swabs or lower respiratory samples (eg, sputum) sent for molecular detection of SARS‐CoV‐2 by polymerase chain reaction (PCR) are currently the best means of specific diagnosis of COVID‐19 in Australia. Faecal samples may also be PCR positive for COVID‐19 but the role of the oral–faecal route for transmission remains unclear. 12 Patients with more severe disease tend to have higher viral loads in respiratory samples. Mild cases have been shown to clear the virus earlier, with over 90% returning negative PCR test results by day 10 compared with severe cases who more often remain positive beyond day 10. 13 Viral loads appear to be highest early in the illness. Prolonged viral shedding after the onset of symptoms has been described. 14 The virus has also been detected by PCR in asymptomatic patients with comparable viral loads to those still symptomatic. 15
Patients with suspected or confirmed COVID‐19 should be assessed for features of severe disease and risk factors for progression to severe disease. This assists in determining whether a patient can safely be managed in the community or requires referral and admission to a health care facility able to provide acute inpatient care. Current data suggest that older patients and those with comorbidities have increased risk of progression to severe disease and mortality. In a large surveillance report from China including over 44 000 confirmed cases of COVID‐19, the case fatality rate was < 0.5% for patients aged < 50 years, but rose to 8.0% for those in their 70s, and 14.8% in those aged > 80 years. 16 While these surveillance‐based case fatality rates are possibly overestimates, being influenced by under‐recognition of lower severity cases, the impact of increasing age and the presence of comorbidities on risk of severe and fatal illness should be recognised, 8 and such patients should generally be offered more careful monitoring.
Clinical features that have been identified more often in COVID‐19 infected patients who have had a fatal outcome compared with those who survive are: dyspnoea at presentation (70.6% v 24.7%; P < 0.001); lower initial oxygen saturation (median oxygen saturation, 85% [IQR, 75–91%] v 97% [IQR, 95–98%]; P < 0.001); and higher total white blood cell count but lower lymphocyte count at presentation accompanied by a lower lymphocyte count, expressed as a lower lymphocyte percentage (median, 7.1% [IQR, 4.5–12.7%] v 23.5% [IQR, 15.3–31.3%]; P < 0.001). 17 In developing a predictive model, Chinese researchers found four factors independently associated with disease progression during hospitalisation in 208 consecutive patients: presence of comorbidity, age > 60 years, lymphocyte count < 1.0 × 10 9 /L, and elevated lactate dehydrogenase levels. 18
A propensity for deterioration in the second week of illness has been recognised in some cohorts of patients, typically 5–10 days after the onset of symptoms. 19 All patients should be warned about symptoms of concern (such as increasing breathlessness), and early referral for hospital admission should be suggested for any patient with signs of clinical deterioration. Individual circumstances need to be considered when determining the ideal monitoring strategy and site of care for each patient ( Box ).
Assessing disease severity and consideration for setting of care for patients diagnosed with COVID‐19
Adapted from World Health Organization interim guidance, 21 Australasian Society for Infectious Diseases interim guidelines, 20 and National COVID‐19 Clinical Evidence Taskforce living guidelines. 19
General management
It is critically important to ensure optimal infection prevention from the time a patient with suspected COVID‐19 is first assessed until their infection is resolved, irrespective of the site of care. This can present particular challenges for health care staff, who must learn to use personal protective equipment safely, and for patients and their loved ones who must manage the difficulties associated with isolation.
Patients with mild disease (about 80%) 10 can often be managed in the community if they are able to self‐isolate. They must also be capable of monitoring their own condition, be aware of which symptoms should prompt medical review, and be able to escalate any concerns. 19 , 20 , 21 For some patients, a more proactive program of monitoring by phone or telehealth or in‐person monitoring (eg, hospital in the home, regular review by general practitioner, or hospital admission) may be required. Strategies for care should be individualised to suit patient circumstances. Patients whose home environment is not conducive to safe management, or which is unacceptable from an infection prevention perspective, may require admission either to hospital or to alternative safe accommodation. Discussion with public health authorities is essential to ensure that appropriate isolation and follow‐up mechanisms are in place. In the face of high health care demand during the peak of a pandemic, safe management of low risk patients in the community will likely be essential to preserve hospital capacity for the more severely ill.
Patients with moderate or severe illness will generally require admission to hospital. This includes those who are dyspnoeic on minor exertion, tachypnoeic at rest (respiratory rate > 22 breaths/min), hypoxaemic (pulse oximetry [SpO 2 ] < 94% on room air), hypotensive (systolic blood pressure < 100 mmHg), have an acutely altered mental state, or who have extensive pulmonary infiltrates evident on chest imaging. 19 , 20 , 21
Severe illness, indicated by, among other features, a respiratory rate > 30 breaths/min, SpO 2 < 92% on room air 19 , 21 or sustained hypotension, warrants urgent hospitalisation and consideration of the need for intensive care if suitable for a given patient.
Respiratory management
Supplemental oxygen should be administered for patients with SpO 2 < 92%. 19 , 20 Once stabilised, the target SpO 2 range is usually 92–96%. The target will be lower in those with chronic hypercapnoeic respiratory failure (eg, 88–92%). 19 , 20 , 21
Manoeuvres to improve gas exchange should be implemented, such as positioning patients appropriately in bed (on either side with regular turning), elevating the bed head to 30 degrees, encouraging deep breathing every hour while awake, sitting patients out of bed every day when possible, and mobilising when able. For mechanically ventilated patients with persistent hypoxaemia, prone positioning may be effective. 19 , 22
In the setting of progressive hypoxaemia despite low or moderate flow oxygen (via nasal prongs or Hudson mask), high flow oxygen can be considered. Whether high flow oxygen devices (> 10 mL/min) are potentially aerosol‐generating is being studied, but current guidelines 1 , 23 advise that airborne precautions be taken by staff (personal protective equipment including N95/P2 masks) and single rooms where possible.
There are emerging views that the respiratory dysfunction observed in COVID‐19 infections is not uniform. 22 Initial recommendations have focused on consideration of early intubation and mechanical ventilation for patients with acute respiratory distress syndrome due to COVID‐19. 1 , 19 , 20 , 21 Experience from a multicentre Italian COVID‐19 patient cohort suggests that non‐invasive ventilation such as continuous positive airways pressure and bilevel positive airways pressure may also have a role both within and outside ICUs. 24 These non‐invasive ventilation devices are clearly aerosol‐generating and as such should only be used with appropriate precautions in place. 1 , 23 Advice from experts in respiratory medicine or critical care should be sought.
Other management considerations
Empirical antibiotic therapy for bacterial pneumonia should be considered in patients whose illness is severe, where there is evidence of sepsis or septic shock, or where the patient is clinically deteriorating. 19 , 20 Empirical treatment for influenza with a neuraminidase inhibitor should be considered for patients with severe pneumonia (guided by local epidemiology) until influenza PCR results are available. 20 , 21 Empirical antibiotics are not recommended for patients with mild or moderate pneumonia unless there is additional clinical evidence to suggest bacterial infection. De‐escalation of empirical antimicrobial therapy should be undertaken as appropriate, guided by microbiology results (where available) and clinical judgement. 21
Hypovolaemia may be contributed to by reduced oral intake and increased losses, but management requires cautious administration of intravenous fluids with regular assessments given the risk of exacerbating pulmonary oedema in the setting of acute respiratory distress syndrome 19 , 22 and given the possibility of underlying cardiac injury. 25
A range of possible complications related to SARS‐CoV‐2 infection have been reported and their incidence is being monitored. These include thromboembolic events in the lungs 22 and cerebrovascular system, 26 Prophylaxis with anticoagulants for adults with moderate, severe or critical COVID‐19 infection is generally recommended, unless there are contraindications. 19 , 21 Acute cardiac injury presenting with electrocardiogram changes, arrhythmias, left ventricular dysfunction, cardiomyopathy and congestive cardiac failure have also been described, and assessment of baseline electrocardiogram is suggested for patients with moderate or severe COVID‐19 illness. 25 , 27
There is considerable interest in monitoring large patient cohorts and conducting analysis of linked datasets at a population level to establish whether there are any rare or longer term complications or associations of COVID‐19 with other medical conditions. Given the very recent emergence of SARS‐CoV‐2, data are currently limited but it is likely that information will emerge in coming months from populations that have experienced a high attack rate. An example of a rare condition with potential association is paediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2, presenting as hyperinflammatory shock with features similar to atypical Kawasaki disease. 28 Similarly, there is interest in monitoring long term incidence of cardiovascular complications, thromboembolic disease, chronic respiratory dysfunction, renal or neurological disorders, and post‐infectious inflammatory syndromes after COVID‐19, in addition to inspection of large datasets for complications that are as yet unsuspected.
Specific therapies
A range of pharmacotherapies have been proposed as possible treatments for COVID‐19. Early evidence of clinical benefit for some agents has emerged. The WHO interim guidance on the clinical management of COVID‐19 21 asserts that investigational therapeutics should be used only in approved randomised controlled trials. This position is endorsed by the Australasian Society for Infectious Diseases interim guidelines for the clinical management of COVID‐19 in adults, 20 and the Australian guidelines for the clinical care of people with COVID‐19, 19 which state that even where conditional recommendations for use of disease modifying agents are made, whenever possible these should be administered in the context of randomised trials with appropriate ethical approval.
The understandable interest in evaluating potential treatments has led to a large number of clinical trials being registered globally; by late April 2020, over 1100 clinical studies were registered, including over 500 randomised controlled trials. 29
Antimicrobials
Lopinavir–ritonavir.
Lopinavir–ritonavir, a combined antiretroviral agent, was proposed as a potential treatment for severe acute respiratory syndrome in 2003, based on apparent reductions in mortality in preliminary research in Hong Kong. 30 Given its hypothesised role, five of the first 18 patients diagnosed with COVID‐19 in Singapore were administered this agent. 31
On 18 March 2020, a randomised controlled open label trial of lopinavir–ritonavir in 199 hospitalised adults with COVID‐19 in China was published. 32 No benefit was observed in participants treated with the antiviral compared with controls. Nearly 14% of those receiving lopinavir–ritonavir were unable to complete 14 days of treatments owing to adverse events.
Chloroquine and hydroxychloroquine
Chloroquine and hydroxychloroquine are antimalarial agents which also have immunomodulatory properties that led to established indications for use in the treatment of rheumatological conditions. Potential adverse effects include retinal toxicity, QT interval prolongation and other cardiological and dermatological effects.
In early February 2020, chloroquine was reported to inhibit SARS‐CoV‐2 replication in vitro. 33 By mid‐February, treatment of COVID‐19 with chloroquine was being described as a “breakthrough”: a published letter stated that the results of treatment in over 100 patients in China had demonstrated that chloroquine was “superior to the control treatment”, but no data were provided. 34 A small French open label non‐randomised clinical trial examining hydroxychloroquine with or without azithromycin suggested a significant viral load reduction in those receiving therapy; 35 however, concerns have been raised about the design and analysis of the study. 36
Despite the lack of clinical evidence from randomised clinical trials, several institutional and local guidelines, and notable public figures, have supported the potential use of chloroquine or hydroxychloroquine for the treatment of COVID‐19. 37 , 38
However, given the current lack of evidence of clinical benefit and reports of significant limitations of supply of hydroxychloroquine for patients with rheumatological conditions, in March 2020, the Pharmaceutical Society of Australia and the Australasian Society for Infectious Diseases called for immediate cessation of prescribing and dispensing of hydroxychloroquine for indications relating to COVID‐19, outside use in approved clinical trials. 39 , 40
On 5 June 2020, the chief investigators on the RECOVERY trial (comprising over 11 500 patients enrolled from hospitals across the United Kingdom) issued a press release stating that no beneficial effect of hydroxychloroquine had been observed. 41 No difference in 28‐day mortality, duration of admission, or other outcomes were observed between the 1542 patients randomised to hydroxychloroquine and the 3132 patients randomised to usual care. Further details regarding this analysis are awaited.
In January 2020, the first patient diagnosed with COVID‐19 in the US received the investigational nucleotide prodrug remdesivir, supplied on a compassionate basis. 42 Developed as a potential therapy for Ebola, there is in vitro evidence that remdesivir inhibits replication of coronaviruses, including Middle East respiratory syndrome coronavirus and SARS‐CoV‐2. 33 , 43 By late March 2020, four clinical trials to assess the efficacy of remdesivir against COVID‐19 had commenced in the US and two were registered in China. 44 On 29 April, results of the first randomised clinical trial conducted in China were published; 45 while this found no clinical benefit of remdesivir, the trial was underpowered (237 participants) owing to the success of public health measures in controlling COVID‐19 in China. The authors noted a non‐significant numerical reduction in time to clinical improvement in patients commencing treatment earlier in the course of illness.
On 27 May 2020, the first positive results of a randomised double‐blind controlled trial of a treatment for COVID‐19 were published. 46 This international multicentre study reported the preliminary results of 1059 hospitalised patients who received up to 10 days of remdesivir or placebo. Those receiving remdesivir had a significantly shorter median recovery time of 11 days compared with 15 days for those receiving placebo (rate ratio for recovery, 1.32; 95% CI, 1.12–1.55; P < 0.001); no significant difference in mortality was found. Benefit was reported for the group requiring oxygen but not yet requiring invasive or non‐invasive ventilatory support. This new evidence has led Australian national guidelines to adopt a conditional recommendation for use of remdesivir outside of a trial setting where necessary. 19
Combination therapy with interferon beta‐1b, lopinavir–ritonavir and ribavirin
In May 2020, a randomised trial in Hong Kong reported results of a comparison of lopinavir–ritonavir alone ( n = 24) with a combination of lopinavir–ritonavir, ribavirin and subcutaneous interferon beta‐1b ( n = 52). 47 The combination group experienced a faster median time to viral clearance (7 days v 13 days; P < 0.0001) and shorter median length of hospital stay (8 days v 15 days; P = 0.0030) if the combination was commenced in the first 7 days from symptom onset. Importantly, the cohort of patients studied was not particularly unwell, with very few requiring ICU support and no deaths in the group.
Immunomodulatory treatments
Corticosteroids.
Interim guidance from the WHO states that corticosteroids should not be used in routine treatment of COVID‐19. 21 This is based on systematic reviews in the context of severe acute respiratory syndrome and Middle East respiratory syndrome which showed lack of effectiveness, and possible harm. 48
In a study of 138 hospitalised patients with COVID‐19 in Wuhan, 49 72.2% of ICU patients and 35.3% of non‐ICU patients received glucocorticoid therapy. The authors commented that while the dose of methylprednisolone varied depending on disease severity, no effective outcomes were observed.
However, on 22 June 2020, a preliminary report regarding interim findings from the UK RECOVERY trial suggested that low dose dexamethasone (6 mg daily orally or intravenous for 10 days) may substantially reduce mortality in hospitalised patients with COVID‐19 who received supplemental oxygen or mechanical ventilation. 50 In comparing 2104 patients randomised to receive dexamethasone with 4321 randomised to receive usual care, dexamethasone was found to reduce mortality by 35% (rate ratio, 0.65; 95% CI, 0.51–0.82; P < 0.001) among ventilated patients, and for those receiving oxygen without mechanical ventilation, mortality was reduced by 20% (rate ratio, 0.80; 95% CI, 0.70–0.92; P = 0.002). No benefit of dexamethasone was observed among hospitalised patients who did not require respiratory support. While peer review and formal publication of this analysis is awaited, it is likely that these findings will be reflected in national and international guidelines.
Interleukin 6 antagonists
Tocilizumab is a humanised monoclonal antibody which binds to interleukin 6 (IL‐6) receptors, resulting in reduced immune activation and inflammation. It is licensed in Australia for use in autoimmune conditions including rheumatoid arthritis and giant cell arteritis. In addition to complications of immunosuppression including serious infections, adverse effects include hepatotoxicity and gastrointestinal complications. The theory behind use of tocilizumab or other agents that target the IL‐6 pathway (eg, sarilumab) in the context of COVID‐19 is that part of the pathogenesis in some patients may be attributable to an acute inflammatory syndrome or cytokine storm, which is associated with elevated IL‐6 levels. Clinical trials of these agents are currently underway. 44
Other agents
Numerous immunomodulatory agents have been proposed as potential adjunctive treatments for COVID‐19, with a range of different immunological targets including other inflammatory cytokines. These include anakinra (an IL‐1 receptor antagonist), bevacizumab (an antivascular endothelial growth factor agent), and eculizumab (which inhibits terminal complement and prevents formation of the membrane attack complex). 44 , 51 While clinical trials are underway overseas for several proposed agents, no data exist to support their use at this time. 44
Passive immunotherapy
A preliminary, uncontrolled case series of five critically ill Chinese patients with COVID‐19 who received convalescent plasma containing high SARS‐CoV‐2‐specific antibody titres was published on 27 March 2020. 52 While improvement in clinical status was reported following this intervention, the small sample size and uncontrolled nature of the study precludes drawing any conclusions regarding the efficacy of this intervention. Once again, further research is needed.
Holistic care
A global pandemic causes understandable fear and anxiety for many people in the community. For those at particular risk of worse outcomes of infection — older people and those with significant pre‐existing illness or multiple comorbidities — COVID‐19 represents a particular threat. In addition, the health care workforce is under substantial strain and faces a potentially overwhelming challenge in delivering care to patients. Ensuring emotional care for the most vulnerable and those experiencing high levels of stress will be a fundamental determinant of the resilience of our society during this challenge.
For vulnerable and frail patients at particular risk of poor outcomes, it is important to provide personalised care and to develop an understanding of each individual's perspectives and preferences for health management. Involving caregivers and family members in decision making and establishing goals of care is necessary. 21 Discussing goals of care early and, where appropriate, assisting patients to make advance care directives or resuscitation plans early in illness (or before infection) may provide substantial peace of mind and allow families to face the pandemic openly and with unity as they support vulnerable loved ones.
It is essential to ensure that all patients receive the best standard of care irrespective of the setting in which the care is delivered, or of the existence of any proposed limitations to life‐extending interventions. Under no circumstances should the best possible symptom control and compassionate, individualised care be denied any patient affected by COVID‐19.
SARS‐CoV‐2 has caused a global pandemic with a profound public health impact, changing the daily lives of billions of people. It has exposed weaknesses in even strong and well resourced health systems internationally, and the economic impact alone will be staggering.
However, never before has the global community had the tools currently available to address a pandemic threat. A strong commitment to social and public health strategies and communicable disease control will ensure our health system retains the capacity to address COVID‐19, including sufficient hospital and intensive care resources to care for those with severe illness.
Biomedical innovations such as new and rapid point‐of‐care diagnostics, effective specific treatments and preventive vaccines are very high priorities which are rightly attracting substantial attention and funding. In the interim, high quality, evidence‐based clinical care — scaled up to face the pandemic challenge — together with robust public health interventions will save the lives of thousands in Australia, and millions globally.
Competing interests
No relevant disclosures.
Commissioned; externally peer reviewed.
Acknowledgements
We gratefully acknowledge the contributions of Anna Deng, Louis Irving, Ashleigh Qama and Lien Tran to this article.
The unedited version of this article was published as a preprint on mja.com.au on 8 April 2020
Rand Paul announces bipartisan investigation of COVID-19 origins
by JACKSON WALKER | The National Desk

WASHINGTON (TND) — Sen. Rand Paul, R-Ky., on Monday announced the launch of a bipartisan investigation looking into the origins of the coronavirus.
Signing onto the effort is Sen. Gary Peters, D-Mich., who oversees the Senate Homeland Security and Governmental Affairs Committee, Politico first reported . The outlet added the investigation will lead to hearings on an array of scientific safety topic, including the origins of COVID-19.
The senators will also work to increase transparency of how taxpayer funds are used in life science research.
Sen. Paul, who is a physician, has repeatedly engaged in intense exchanges with leading health officials, including Dr. Anthony Fauci. Speaking to The National Desk in 2022, Sen. Paul said Fauci had been “ignoring the immunity you have from acquiring the disease” in pushing for widespread COVID-19 vaccination.
The Bluegrass State Republican also became the first congressman to ever lead a hearing dedicated to gain-of-function research, in which scientists modify a genetic organism. He argued such practices have “historically been supported by tax dollars both domestically and internationally."
In 2024, Republicans remain hard-pressed to learn more about the virus. Democrats, however, continue to defend Fauci, accusing their colleagues across the aisle of politicizing the pandemic, promoting vaccine hesitancy and spreading misinformation.
Rep. Robert Garcia, D-Calif., in July said "there is a complete dismantling of the importance of what vaccines have actually done in this country and how many lives have actually been saved."
Follow Jackson Walker on X at @_jlwalker_ for the latest trending national news. Have a news tip? Send it to [email protected].

IMAGES
COMMENTS
COVID-19 is an infectious disease of the human respiratory system caused by the virus SARS-CoV-2. The disease is almost always mild and causes fever, dry cough, shortness of breath, and fatigue. ... This presentation summarizes important basic information on the current pandemic. It was written for high school and college non-science-major ...
The virus that causes COVID-19 spreads most commonly through the air in tiny droplets of fluid between people in close contact. Many people with COVID-19 have no symptoms or mild illness. But for older adults and people with certain medical conditions, COVID-19 can lead to the need for care in the hospital or death.
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States. COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs ...
COVID-19 is a disease caused by a virus. The most common symptoms are fever, chills, and sore throat, but there are a range of others. Most people make a full recovery without needing hospital treatment. People with severe symptoms should seek medical care as soon as possible. Over 760 million cases and 6.9 million deaths have been recorded ...
Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus will experience mild to moderate respiratory illness and recover without requiring special treatment. However, some will become seriously ill and require medical attention. Older people and those with underlying medical ...
COVID-19 Presentation . Multi-purpose . Premium Google Slides theme and PowerPoint template . The coronavirus outbreak has become one of the most notorious events of the decade, if not the current century. Every bit of information helps a lot, so let us help you create useful and informative presentations about this virus with our latest template.
The clinical presentation of COVID-19 ranges from asymptomatic to critical illness. An infected person can transmit SARS-CoV-2, the virus that causes COVID-19, before the onset of symptoms. Symptoms can change over the course of illness and can progress in severity. Uncommon presentations of COVID-19 can occur, might vary by the age of the ...
A novel coronavirus (CoV) named '2019-nCoV' or '2019 novel coronavirus' or 'COVID-19' by the World Health Organization (WHO) is in charge of the current outbreak of pneumonia that began at the beginning of December 2019 near in Wuhan City, Hubei Province, China [1-4]. COVID-19 is a pathogenic virus. From the phylogenetic analysis ...
For COVID-19, this means staying in the facility or at home for several days. Isolation is used for people with COVID-19 symptoms or who have tested positive for the virus. Being in isolation means being separated from other people, ideally in a medical facility where you can receive clinical care.
If a patient tests negative by Rapid Antigen Test (RAT) FDA recommends. If symptomatic, test at least twice 48 hours apart. A third test might be needed if the patient is concerned they have COVID-19. If asymptomatic, but believe they have been exposed, test with RAT at least 3 times, each 48 hours apart to be considered truly negative.
Coronavirus disease 2019 (COVID-19) is a highly contagious viral illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 has had a catastrophic effect on the world, resulting in more than 6 million deaths worldwide. After the first cases of this predominantly respiratory viral illness were reported in Wuhan, Hubei Province, China, in late December 2019, SARS ...
Scroll down the page to view all COVID-19 articles, stories, and resources from across NIH. You can also select a topic from the list to view resources on that topic. - Any -. Aging. Cancer. Children. Clinical Trials. Immune Responses. Long COVID.
Areas covered. Direct person-to-person respiratory transmission has rapidly amplified the spread of coronavirus. In the absence of any clinically proven treatment options, the current clinical management of COVID-19 includes symptom management, infection prevention and control measures, optimized supportive care, and intensive care support in severe or critical illness.
Coronavirus Presentation templates Raise awareness about one of the hottest topics of the 21st century by downloading and editing our free PPT templates and Google Slides themes about Coronavirus. Filter by. ... The COVID-19 vaccine has improved the pandemic situation. We are gradually returning to our pre-COVID-19 lifestyle.
Free Google Slides theme and PowerPoint template. After a year and a half, has society really learned a lesson about the COVID-19 pandemic? What about in education? These are questions that you can answer by customizing this new template for educational presentations. Teaching and classes in general might be different now, but one thing is ...
COVID-19 Abstraction Guidance by Margaret (Peggy) Adamo, RHIT, CTR. Access the presentation slides (PDF, 1.2 MB) View the presentation recording. Coronavirus-Disease 19 (COVID-19) & SARS-CoV-2 Testing by Alison Van Dyke, MD, PhD. Access the presentation slides (PDF, 4.6 MB) View the presentation recording
Coronavirus Disease (COVID-19): Comprehensive Review of Clinical Presentation. 2021 Jan 15:8:582932. doi: 10.3389/fpubh.2020.582932. COVID-19 is a rapidly growing pandemic with its first case identified during December 2019 in Wuhan, Hubei Province, China. Due to the rampant rise in the number of cases in China and globally, WHO declared COVID ...
Aim: Pharyngodynia, nasal congestion, rhinorrhea, smell, and taste dysfunctions could be the presenting symptoms of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2. The aim was to perform a systematic review of current evidences on clinical presentation of COVID-19, focusing on upper airway symptoms in order to help otolaryngologists identifying ...
The "COVID-19 Vaccine" webinars are 15-30-minute presentations designed to provide health care providers with the most up-to-date information on COVID-19 disease and the vaccines used to fight the virus that causes COVID-19. ... This presentation is intended to support you in making effective recommendations and answering parents ...
Correlation between Clinical Presentation and Clinical Evolution. According to WHO reports, the overall fatality rate for COVID-19 is estimated at 2.3% [ 47 ], but the fatality rate has varied among studies from 1.4% to 4.3% [ 21, 37 ]. In our case series, the overall mortality rate was 2.5%.
Information about the clinical presentation and course of COVID-19 is evolving rapidly. On presentation, cough and fever predominate, but extrapulmonary symptoms are also common; in some patients, loss of sense of smell may be an early but favorable sign. The mortality rate varies widely in differen …
Background COVID-19 infection is associated with thrombotic events; however, this phenomenon is poorly understood. Few studies have reported the association between COVID-19 and stroke in the hospital setting. Methods We retrospectively reviewed and characterized all patients who presented to a single, quaternary medical center between March and December 2020 (N=603). COVID-19 positive ...
Well before the COVID-19 pandemic, Stanford University physician and microbiologist David Relman, M.D., realized research scientists like himself had a growing problem persuading people to trust ...
Studies have reported that COVID-19 pandemic led to delayed presentation following ACS.23 We have no data on geographic, social, economic and other determinants that influence prehospital delays,27 especially during the COVID-19 pandemic.36 38 We also do not have data on the status of cardiovascular risk factor control at admission.
Free Google Slides theme and PowerPoint template. Currently, all information concerning preventive measures against COVID-19 is crucial and should be accessible for everybody. Explain them in the form of infographics, since images convey a lot. Edit our linear-style timelines, charts and diagrams to maximize the chances of your message reaching ...
Announces next-generation COVID-19 vaccine candidate as fourth respiratory vaccine to successfully meet its Phase 3 endpoints Expects two more Phase 3 readouts in 2024, including combination vaccine against flu and COVID-19, and vaccine against CMV Announces positive clinical trial data from three new vaccines against viruses that cause significant burden (Epstein-Barr virus, Varicella-Zoster ...
Clinical presentation. Similar to other coronaviruses, SARS‐CoV‐2 is predominantly spread by respiratory droplets, although spread by contact with contaminated fomites also occurs, as does transmission by aerosols in certain circumstances.1 Based on the experience in China, the typical incubation period of COVID‐19 infection has been estimated to be a median of 5.1 days (95% CI, 4.5-5. ...
WASHINGTON (TND) — Sen. Rand Paul, R-Ky., on Monday announced the launch of a bipartisan investigation looking into the origins of the coronavirus. Signing onto the effort is Sen. Gary Peters, D-Mich., who oversees the Senate Homeland Security and Governmental Affairs Committee, Politico first reported.The outlet added the investigation will lead to hearings on an array of scientific safety ...
The group formed during the 2019-20 academic year and quickly became a place of support and collaboration during the COVID-19 pandemic. Since 2022, the group has worked closely with Laura Cruz at the Schreyer Institute for Teaching Excellence at Penn State to develop and conduct a yearlong research project using evidence-based practices to ...
The John Gokongwei School of Management invites you to a Brown Bag Session on "COVID-19 Blood Collection Volatility in the Philippines: A Data-Driven Disaster Preparedness and Recovery Policy Framework". Our presenter is Joel Patrick D. Caballa, Lecturer at the Department of Quantitative Methods and Information Technology.