
Case Presentation
Statement of ethics, conflict of interest statement, funding sources, author contributions, ischemic stroke in a 29-year-old patient with covid-19: a case report.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Christian Avvantaggiato , Loredana Amoruso , Maria Pia Lo Muzio , Maria Assunta Mimmo , Michelina Delli Bergoli , Nicoletta Cinone , Luigi Santoro , Lucia Stuppiello , Antonio Turitto , Chiara Ciritella , Pietro Fiore , Andrea Santamato; Ischemic Stroke in a 29-Year-Old Patient with COVID-19: A Case Report. Case Rep Neurol 2 September 2021; 13 (2): 334–340. https://doi.org/10.1159/000515457
Download citation file:
- Ris (Zotero)
- Reference Manager
Increasing evidence reports a greater incidence of stroke among patients with Coronavirus disease 2019 (COVID-19) than the non-COVID-19 population and suggests that SARS-CoV-2 infection represents a risk factor for thromboembolic and acute ischemic stroke. Elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events, and advanced age is strongly associated with severe COVID-19 and death. We reported, instead, a case of an ischemic stroke in a young woman during her hospitalization for COVID-19-related pneumonia. A 29-year-old woman presented to the emergency department of our institution with progressive respiratory distress associated with a 2-day history of fever, nausea, and vomiting. The patient was transferred to the intensive care unit (ICU) where she underwent a tracheostomy for mechanical ventilation due to her severe clinical condition and her very low arterial partial pressure of oxygen. The nasopharyngeal swab test confirmed SARS-CoV-2 infection. Laboratory tests showed neutrophilic leucocytosis, a prolonged prothrombin time, and elevated D-dimer and fibrinogen levels. After 18 days, during her stay in the ICU after suspension of the medications used for sedation, left hemiplegia was reported. Central facial palsy on the left side, dysarthria, and facial drop were present, with complete paralysis of the ipsilateral upper and lower limbs. Computed tomography (CT) of the head and magnetic resonance imaging of the brain confirmed the presence of lesions in the right hemisphere affecting the territories of the anterior and middle cerebral arteries, consistent with ischemic stroke. Pulmonary and splenic infarcts were also found after CT of the chest. The age of the patient and the absence of serious concomitant cardiovascular diseases place the emphasis on the capacity of SARS-CoV-2 infection to be an independent cerebrovascular risk factor. Increased levels of D-dimer and positivity to β2-glycoprotein antibodies could confirm the theory of endothelial activation and hypercoagulability, but other mechanisms – still under discussion – should not be excluded.
Coronavirus disease 2019 (COVID-19), caused by the novel coronavirus SARS-CoV-2, is characterized by a wide range of symptoms, most of which cause acute respiratory distress syndrome [1, 2], associated with intensive care unit (ICU) admission and high mortality [3]. On March 11, 2020, the large global outbreak of the disease led the World Health Organization (WHO) to declare COVID-19 a pandemic, with 11,874,226 confirmed cases and 545,481 deaths worldwide (July 9, 2020) [4]. In many cases, the clinical manifestations of COVID-19 are characteristic of a mild disease that may, however, worsen to a critical lower respiratory infection [2]. At the onset of the disease, the most frequent symptoms are fever, dry cough, fatigue, and shortness of breath as the infection progresses may appear signs and symptoms of respiratory failure that require ICU admission [5, 6]. Although acute respiratory distress syndrome is the most important cause of ICU admission for COVID-19 patients, several studies have underlined the presence of neurological symptoms such as confusion, dizziness, impaired consciousness, ataxia, seizure, anosmia, ageusia, vision impairment, and stroke [7, 8]. In particular, the state of hypercoagulability in patients affected by COVID-19 favors the formation of small and/or large blood clots in multiple organs, including the brain, potentially leading to cerebrovascular disease (ischemic stroke but also intracranial hemorrhage) [9, 10 ].
We found an interesting case of stroke following a SARS-CoV-2 infection in a young patient. A 29-year-old woman, during her ICU hospitalization for COVID-19-related pneumonia, was diagnosed with ischemic stroke of the right hemisphere, without other cardiac/cerebrovascular risk factors except hypertension. The young age of the patient and the absence of higher cerebrovascular risk factors make the present case very interesting as it can help demonstrate that COVID-19 is an independent risk factor for acute ischemic stroke. In a case series of 214 patients with COVID-19 (mean [SD] age, 52.7 [15.5] years), neurologic symptoms were more common in patients with severe infection who were older than the others [ 11 ]. New-onset CVD was more common in COVID-19 patients who had underlying cerebrovascular risk factors, such as older age (>65 years) [ 12 ], and very few cases of stroke in patients younger than 50 years have been reported [ 12, 13 ]. Our case seems to be the only one younger than 30 years.
On the night between March 19 and 20, 2020, a 29-year-old woman was referred to our hospital “Policlinico Riuniti di Foggia” due to a progressive respiratory distress associated with a 2-day history of fever, nausea, and vomiting. At presentation, the heart rate was 128 bpm, the blood oxygen saturation measured by means of the pulse oximeter was 27%, the respiratory rate was 27 breaths per minute, and the blood pressure was 116/77 mm Hg. The arterial blood gas test showed a pH of 7.52, pO 2 20 mm Hg, and pCO 2 34 mm Hg. The patient was immediately transferred to the ICU where she underwent tracheostomy and endotracheal intubation for mechanical ventilation due to her severe clinical condition and deteriorated pulmonary gas exchange. The diagnosis of COVID-19 was confirmed by PCR on a nasopharyngeal swab.
The family medical history was normal, and the only known pre-existing medical conditions were polycystic ovary syndrome (diagnosed 3 years earlier), conversion disorder, and hypertension (both diagnosed 2 years earlier). Ramipril and nebivolol were prescribed for the high blood pressure treatment, and sertraline was prescribed for the conversion disorder treatment. Drug therapy adherence was inconstant. The patient had no history of diabetes, cardiac pathologies, strokes, transient ischemic attacks, thromboembolic, or other vascular pathologies.
Laboratory tests showed neutrophilic leukocytosis (white blood cell count 14.79 × 10 3 , neutrophil percentage 89.8%, and neutrophil count 13.29 × 10 3 ), a prolonged prothrombin time (15.3 s) with a slightly elevated international normalized ratio (1.38), and elevated D-dimer (6,912 ng/mL) and fibrinogen levels (766 mg/dL). Other findings are shown in Table 1 .
Laboratory test

This pharmacological therapy was set as follows: enoxaparin 6,000 U.I. once a day, piperacillin 4 g/tazobactam 0.5 g twice a day; Kaletra, a combination of lopinavir and ritonavir indicated for human immunodeficiency virus (HIV) infection treatment, 2 tablets twice a day; hydroxychloroquine 200 mg once a day; and furosemide 250 mg, calcium gluconate, and aminophylline 240 mg 3 times a day. No adverse events were reported.
On April 7, 2020, during her stay in the ICU and after suspension of the medications used for sedation, left hemiplegia was reported. The same day, the patient underwent a computed tomography examination of the head, which showed areas of hypodensity in the right hemisphere due to recent cerebral ischemia.
On April 16, 2020, the patient was oriented to time, place, and person. Central facial palsy on the left side, dysarthria, and facial drop were present, with complete paralysis of the ipsilateral upper and lower limbs. The power of all the muscles of the left limbs was grade 0 according to the Medical Research Council (MRC) scale. Deep tendon reflexes were reduced on the left upper limb but hyperactive on the ipsilateral lower limb, with a slight increase in the muscle tonus. The senses of touch, vibration, and pain were reduced on the left side of the face and body.
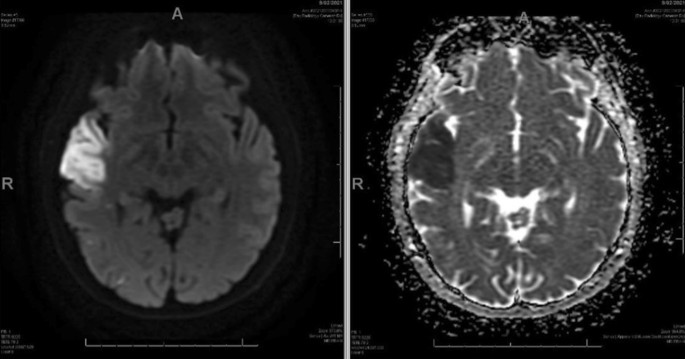
On the same day, the patient underwent magnetic resonance imaging (MRI) of the brain (Fig. 1 a), showing lesions on the right hemisphere affecting the territories of the anterior and middle cerebral arteries. On May 5, 2020, magnetic resonance angiography showed an early duplication of the sphenoidal segment of the right middle cerebral artery, the branches of which are irregular with rosary bead-like aspects (Fig. 1 d, e); on the same day, the second MRI (Fig. 1 b) confirmed the lesions. Computed tomography of the chest (Fig. 1 c) and abdomen (Fig. 1 f), performed 5 days after the MRI of the brain, showed not only multifocal bilateral ground-glass opacities but also a basal subpleural area of increased density within the left lung (4 × 4 × 3 cm), consistent with a pulmonary infarction. In addition, a vascular lesion, consistent with a splenic infarct, was found in the inferior pole of the spleen. Doppler echocardiography of the hearth showed regular right chambers and left atrium and a slightly hypertrophic left ventricle with normal size and kinetics (ejection fraction: 55%). The age of the patient and the absence of serious concomitant cardiovascular diseases place the emphasis on the capacity of SARS-CoV-2 infection to be an independent cerebrovascular risk factor.

Imaging. a April 16, 2020; MRI of the brain: lesions in the right hemisphere affecting the territories of the anterior and the middle cerebral arteries. b May 5, 2020; MRI of the brain: same lesions in the right hemisphere shown in the previous image. d , e May 5, 2020; MRA showed an early duplication of the sphenoidal segment of the right middle cerebral artery, the branches of which are irregular with rosary bead-like aspect and reduction of blood flow in the middle cerebral artery. c April 20, 2020; CT of the abdomen: vascular lesion, consistent with a splenic infarct, found in the inferior pole of the spleen. f April 20, 2020; CT of the chest: basal subpleural area of increased density within the left lung (4 × 4 × 3 cm), consistent with a pulmonary infarction. MRA, magnetic resonance angiography; CT, computed tomography; MRI, magnetic resonance imaging.
The pandemic outbreak of novel SARS-CoV-2 infection has caused great concern among the services and authorities responsible for public health due to not only the mortality rate but also the danger of filling up hospital capacities in terms of ICU beds and acute non-ICU beds. In this regard, the nonrespiratory complications of COVID-19 should also be taken into great consideration, especially those that threaten patients’ lives and extend hospitalization times. Stroke is one of these complications, since a greater incidence of stroke among patients with COVID-19 than the non-COVID-19 population has been reported, and a preliminary case-control study demonstrated that SARS-CoV-2 infection represents a risk factor for acute ischemic stroke [ 14 ].
We found that the reported case is extremely interesting, since the woman is only 29 years old and considering how stroke in a young patient without other known risk factors is uncommon. Not only elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events [ 15 ], but it is also true that advanced age is strongly associated with severe COVID-19 and death. The severity of the disease is directly linked to immune dysregulation, cytokine storm, and acute inflammation state, which in turn are more common in patients who present immunosenescence [6].
Inflammation plays an important role in the occurrence of cardiovascular and cerebrovascular diseases since it favors atherosclerosis and affects plaque stability [ 16 ]. The ischemic stroke of the 29-year-old woman does not appear to be imputable to emboli originating a pre-existing atheromatous plaque, both for the age of the patient and for the absence of plaques at the Doppler ultrasound study of the supra-aortic trunks.
Most likely, COVID-19-associated hypercoagulability and endothelial dysfunction are the causes of ischemic stroke, as suggested by other studies and case reports [ 10, 13, 17 ]. Although the mechanisms by which SARS-CoV-2 infection leads to hypercoagulability are still being studied, current knowledge suggests that cross talk between inflammation and thrombosis has a crucial role [ 18 ]. The release of inflammatory cytokines leads to the activation of epithelial cells, monocytes, and macrophages. Direct infection of endothelial cells through the ACE2 receptor also leads to endothelial activation and dysfunction, expression of tissue factor, and platelet activation and increased levels of VWF and FVIII, all of which contribute to thrombin generation and fibrin clot formation [ 17 ]. The 29-year-old patient showed an increased level of D-dimer, which is a degradation product of cross-linked fibrin, indicating a global activation of hemostasis and fibrinolysis and conforming to the hypothesis of COVID-19-associated hypercoagulability. Endothelial activation and hypercoagulability are also confirmed by positivity to β2 glycoprotein antibodies. Anticardiolipin antibody and/or β2 glycoprotein antibody positivity has been reported in a few studies [ 17, 19, 20 ]. In addition, widespread thrombosis in SARS-CoV-2 infection could also be caused by neutrophil extracellular traps (NETs). Neutrophilia [ 21 ] and an elevated neutrophil-lymphocyte ratio [ 22 ] have been reported by numerous studies as predictive of worse disease outcomes, and recently, the contribution of NETs in the pathophysiology of COVID-19 was reported [ 23 ]. Thrombogenic involvement of NETs has been described in various settings of thrombosis, including stroke, myocardial infarction, and deep vein thrombosis [ 24 ]. The high neutrophil count found in our case does not exclude the hypothesis that NETs are involved in the pathogenesis of ischemic stroke.
Ischemic stroke in young patients without pre-existing cerebrovascular risk factors is very unusual. In this regard, our case of an ischemic stroke, reported in a 29-year-old woman, is very interesting. Although it is not possible to determine precisely when the thromboembolic event occurred, our case of stroke during COVID-19-related pneumonia seems to confirm that COVID-19 is an independent risk factor for acute ischemic stroke. The mechanisms by which coronavirus disease leads to stroke are still under study, but it is clear that hypercoagulability and endothelial activation play a key role. Testing for SARS-CoV-2 infection should be considered for patients who develop neurologic symptoms, but it is equally important to monitor COVID-19 patients during their hospitalization to find any neurological sign or symptom in a timely manner. Our case suggests that discovering neurological deficits in sedated patients promptly can be very difficult; for this reason, sedation in mechanically ventilated patients has to be considered only if strictly necessary. Performing serial laboratory testing and waking up the patient as soon as clinical conditions allow are strategies that should be taken into account.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
No funding was received for the publication of this case report.
All authors agree with the contents of the manuscript and were fully involved in the study and preparation of the manuscript. All authors read and approved the final version of the manuscript. M.A. Mimmo, M.P. Lo Muzio, M. Delli Bergoli, and L. Amoruso collected the data. C. Avvantaggiato wrote the manuscript with support of N. Cinone, L. Santoro, and C. Ciritella. C. Avvantaggiato, A. Turitto, and L. Stuppiello researched and discussed the neurophysiological principles of this study. P. Fiore and A. Santamato supervised the project.

Email alerts
Citing articles via, suggested reading.
- Online ISSN 1662-680X
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Email: [email protected]
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Diseases & Diagnoses
Issue Index
- Case Reports
Guest Medical Editor’s Letter | December 2023
Stroke: Notable Case Reports and Issues
James r. brorson, md.
Associate Professor Department of Neurology The University of Chicago Chicago, IL
Corpus Callosum Stroke: A Rare Localization for an Isolated Cerebral Infarction
Alexis García-Sarreón, MD; Vanessa Cano-Nigenda, MD; Karla Jonguitud, MD; Nicole Somerville-Briones, MD, MSc; and Daniel Aguirre-Fernández, MD
This Month's Issue
Jerome Lisk, MD, FAAN; Paul G. Mathew, MD, DNBPAS, FAAN, FAHS; Nabil Ali, MD; Larry Charleston IV, MD, MSc, FAHS; Roderick C. Spears, MD, FAAN, FAHS; Cynthia E. Armand, MD; Amtul Farheen, MD, FAAN; Justin S. Moon, MD, MPH; and Tamika M. Burrus, MD, FAAN
Katrina Roberto, MD; and Mary Jane Lim-Fat, MD, MSc

Related Articles
Wilmar Jolink, MD, PhD; and Doeschka Ferro, MD, PhD
Fatma Ger Akarsu, MD; Andrea M. Kuczynski, MD, PhD; Gustavo Saponsik, MD, PhD; and Manav V. Vyas, MBBS, MSc, PhD, FRCPC
Sign up to receive new issue alerts and news updates from Practical Neurology®.
Related News
- Case report
- Open access
- Published: 25 August 2015
Case report of a young stroke patient showing interim normalization of the MRI diffusion-weighted imaging lesion
- Ann-Christin Ostwaldt 1 ,
- Tatiana Usnich 2 ,
- Christian H. Nolte 1 , 2 ,
- Kersten Villringer 1 &
- Jochen B. Fiebach 1
BMC Medical Imaging volume 15 , Article number: 33 ( 2015 ) Cite this article
5589 Accesses
2 Citations
Metrics details
In acute ischemic stroke, diffusion weighted imaging (DWI) shows hyperintensities and is considered to indicate irreversibly damaged tissue. We present the case of a young stroke patient with unusual variability in the development of signal intensities within the same vessel territory.
Case presentation
A 35-year-old patient presented with symptoms of global aphasia and hypesthesia of the left hand. MRI demonstrated a scattered lesion in the MCA territory. After rtPA therapy the patient received further MRI examination, three times on day 1, and once on day 2, 3, 5 and 43. The posterior part of the lesion showed the usual pattern with increasing DWI hyperintensity and decreased ADC, as well as delayed FLAIR positivity. However, the anterior part of the lesion, which was clearly visible in the first examination completely normalized on the first day and only reappeared on day 2. This was accompanied by a normalization of the ADC as well as an even further delayed FLAIR positivity.
We showed that interim normalization of DWI and ADC in the acute phase can not only be found in rodent models of stroke, but also in humans. We propose that DWI lesion development might be more variable during the first 24 h after stroke than previously assumed.
Peer Review reports
Acute cerebral ischemia can be visualized with MRI diffusion weighted imaging (DWI) within minutes after its onset [ 1 ]. It has been suggested that in the majority of human stroke patients DWI positive cerebral ischemia indicate irreversible tissue damage leading to infarction [ 2 ]. However, lately reversal of parts of the DWI lesion has been demonstrated in association with early recanalization [ 3 – 5 ]. In animal models the occurrence of interim or sustained normalization of both DWI and apparent diffusion coefficient (ADC) seem to depend on the occlusion times [ 6 , 7 ]. In contrast to DWI, lesions on fluid-attenuated inversion recovery (FLAIR) are usually seen several hours after stroke onset [ 8 ] in humans.
Here we present a case of partial interim normalization of DWI and ADC visualized with serial MRI in a young stroke patient.
A 35 year old female patient was admitted with incomplete global aphasia and a fluctuating slight hypesthesia of the left hand. Her baseline National Institutes of Health Stroke Scale score (NIHSS) was 4 and arterial hypertension was the only vascular risk factor. The patient was repeatedly examined in the MRI 57 min as well as 3.3 h, 5.5 h and 7.6 h after symptom onset, and on the second, third, fifth and 43 rd day post-stroke. These data were obtained from the prospective 1000Plus Study (NCT00715533). The patient gave written informed consent. At baseline, the anterior M2 branch of the right middle cerebral artery (MCA) was occluded. DWI showed a scattered lesion affecting the anterior and posterior part of the right MCA territory and perfusion imaging showed a corresponding deficit. Intravenous rt-PA was administered directly after the first MRI scan. The follow-up examinations showed a patent MCA branch 5.5 h after symptom onset, complete normalization of the perfusion deficit on day 2 and no signs of hemorrhagic transformation. The patient’s symptoms had substantially improved, resulting in a NIHSS of 0 at discharge. Infarct size on FLAIR was 31.76 ml at day 5.
On the first examination 57 min after onset, the anterior part of the lesion was clearly hyperintense on DWI; however, on the second examination at 3.3 h it was not visible any more and did not reappear until day 2 (Fig. 1 ). For a more detailed analysis of this phenomenon, the image datasets for each time point were coregistered and regions-of-interest (ROIs) for both the anterior and the posterior part of the lesion were created on DWI day 5 images. Signal intensities (rSI) were determined relative to the contralateral side, as previously described [ 8 ].
Development of the anterior and the posterior lesion on serial DWI and FLAIR images. The first and second rows show the diffusion-weighted images (DWI) on two slices depicting the lesion development over time from symptom onset. The third and fourth row shows the coregistered fluid-attenuated inversion recovery (FLAIR) images corresponding to the DWI slices
As can be seen in Fig. 2 , DWI and ADC rSI values of the anterior lesion normalized for the time period between 3.3 h and 25 h after symptom onset (Fig. 2a-b ). Also, the fluid-attenuated inversion recovery (FLAIR) rSI values of the anterior lesion were much lower than the values of the posterior lesion and only at day 3 post-stroke did the FLAIR rSI in the anterior lesion reach values substantially different from 1 (Fig. 2c ).
Development of relative signal intensity (rSI) for the anterior and the posterior lesion separately. a + b ) Diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) rSI show the normalization of the anterior lesion and its reappearance at day 2. c ) The fluid attenuated inversion recovery (FLAIR) rSI shows that the anterior part of the lesion is FLAIR positive much later than the posterior part
Conclusions
We demonstrated that the degree and time course of DWI hyperintensities can differ within one lesion in the first day after stroke. To the best of our knowledge, this is the first time that the exact time course of DWI reversal and reappearance was visualized using highly repetitive MRI examinations. Our findings resemble those in rodent models of stroke [ 6 ], where lesions normalized on the DWI and ADC after recanalization and reappeared at day 2 after stroke. In stroke patients, reversible DWI hyperintensities have been demonstrated for very small, mainly embolic lesions [ 9 ]. Also it has been shown that recanalization (either after intraarterial or intravenous thrombolysis) could evoke DWI lesion reversal in some patients, with parts of lesion showing later reappearance [ 3 – 5 ]. Therefore, we hypothesize, that a possible explanation for the interim normalization of a large part of the initial lesion in our case would be the fast recanalization and reperfusion of the tissue. It therefore seems that the baseline DWI lesion contains tissue with benign oligemia and only cell damage which could not be prevented will reveal itself on follow-up examinations. It might well be possible, that an interim normalization as observed in our case is more common in stroke patients. However, this will rarely be observed due to lack of MRI follow-ups in clinical routine.
We conclude that DWI lesion visibility might be more prone to fluctuation and variability during the first 24 h after stroke than previously assumed and baseline DWI may include tissue with benign oligemia. Therefore, during interpretation of DWI one has to keep in mind that an interim normalization can occur and which might delay lesion visualization.
Abbreviations
- Magnetic resonance imaging
Diffusion-weighted imaging
Apparent diffusion coefficient
National Institutes of health stroke scale
Middle cerebral artery
Region-of-interest
Relative signal intensity
Fluid-attenuated inversion recovery
Moseley M, Cohen Y, Mintorovitch J, Chileuitt L, Shimizu H, Kucharczyk J, et al. Early detection of regional cerebral ischemia in cats: comparison of diffusion-weighted and T2-weighted MRI and spectroscopy. Magn Reson Med. 1990;14:330–46.
Article CAS PubMed Google Scholar
Fiehler J, Fiebach JB, Gass A, Hoehn M, Kucinski T, Neumann-Haefelin T, et al. Diffusion-weighted imaging in acute stroke – a tool of uncertain value? Cerebrovasc Dis. 2002;14:187–96.
Article PubMed Google Scholar
Soize S, Tisserand M, Charron S, Turc G, Ben Hassen W, Labeyrie MA, et al. How sustained is 24-h diffusion-weighted imaging lesion reversal? Serial magnetic resonance imaging in a patient cohort thrombolyzed within 4.5 h of stroke onset. Stroke. 2015;46:704–10.
Kidwell CS, Saver JL, Starkman S, Duckwiler G, Jahan R, Vespa P, et al. Late secondary ischemic injury in patients receiving intraarterial thrombolysis. Ann Neurol. 2002;52:698–703.
Sakamoto Y, Kimura K, Iguchi Y, Shibazaki K, Aoki J. Dramatic changes of a DWI lesion in a patient with acute ischemic stroke treated with IV t-PA. J Neuroimaging. 2013;23:228–30.
Neumann-Haefelin T, Kastrup A, de Crespigny A, Yenari MA, Ringer T, Sun GH, et al. Serial MRI after transient focal cerebral ischemia in rats: dynamics of tissue injury, blood–brain barrier damage, and edema formation. Stroke. 2000;31:1965–72.
Li F, Liu KF, Silva MD, Omae T, Sotak CH, Fenstermacher JD, et al. Transient and Permanent Resolution of Ischemic Lesions on Diffusion-Weighted Imaging After Brief Periods of Focal Ischemia in Rats: Correlation With Histopathology. Stroke. 2000;31:946–54.
Cheng B, Brinkmann M, Forkert ND, Treszl A, Ebinger M, Köhrmann M, et al. Quantitative measurements of relative fluid-attenuated inversion recovery (FLAIR) signal intensities in acute stroke for the prediction of time from symptom onset. J Cereb Blood Flow Metab. 2013;33:76–84.
Albach FN, Brunecker P, Usnich T, Villringer K, Ebinger M, Fiebach JB, et al. Complete Early Reversal of Diffusion-Weighted Imaging Hyperintensities After Ischemic Stroke Is Mainly Limited to Small Embolic Lesions. Stroke. 2013;44:1043–8.
Download references
Acknowledgements
This research received funding from the Federal Ministry of Education and Research via the grant Center for Stroke Research Berlin (01EO0801 and 01EO1301).
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
Author information
Authors and affiliations.
Center for Stroke Research Berlin (CSB), Charité Universitätsmedizin Berlin, Hindenburgdamm 30, 12200, Berlin, Germany
Ann-Christin Ostwaldt, Christian H. Nolte, Kersten Villringer & Jochen B. Fiebach
Department of Neurology, Charité Universitätsmedizin Berlin, Hindenburgdamm 30, 12200, Berlin, Germany
Tatiana Usnich & Christian H. Nolte
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ann-Christin Ostwaldt .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
AO was responsible for analyzing and interpreting the imaging data. She generated the figures and drafted the manuscript. TU and CN were the responsible treating physicians of the patients. TU additionally helped analyzing the data. CN was responsible for the data collection on the clinical side and made contributions to interpretation of the results. KV participated in design and coordination of the study and substantially helped in interpreting the results and drafting the manuscript. JF was responsible for conception and design of the study and agree to be accountable for accuracy or integrity of the work. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Ostwaldt, AC., Usnich, T., Nolte, C.H. et al. Case report of a young stroke patient showing interim normalization of the MRI diffusion-weighted imaging lesion. BMC Med Imaging 15 , 33 (2015). https://doi.org/10.1186/s12880-015-0077-9
Download citation
Received : 19 January 2015
Accepted : 14 August 2015
Published : 25 August 2015
DOI : https://doi.org/10.1186/s12880-015-0077-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Acute ischemic stroke
- Time course
- Normalization
BMC Medical Imaging
ISSN: 1471-2342
- General enquiries: [email protected]
- Case report
- Open access
- Published: 15 December 2023
Emotional dysmetria after cerebellar-pontine stroke: a case report
- Rebecca M. Long ORCID: orcid.org/0009-0005-3552-8336 1 , 2 ,
- Michèle DuVal 3 ,
- Bridget Mulvany-Robbins 3 ,
- Amanda N. Wagner 3 &
- Glen C. Jickling 2 , 3
Journal of Medical Case Reports volume 17 , Article number: 544 ( 2023 ) Cite this article
684 Accesses
6 Altmetric
Metrics details
Introduction
Pseudobulbar affect, or emotional dysregulation, commonly occurs following stroke. However, it is frequently missed in cases involving the cerebellum, resulting in a lack of treatment, which can directly impact stroke rehabilitation.
Case presentation
A 63-year-old Caucasian female with no history of mood disorders presented with gait instability, dysarthria, and right sided hemiplegia, secondary to cerebellar and pontine ischemic stroke from a basilar occlusion. She underwent endovascular therapy and her deficits gradually improved. However during recovery she began to develop uncontrollable tearfulness while retaining insight that her emotional expression was contextually inappropriate. She was treated with a selective serotonin reuptake inhibitor with reported improvements in her emotional regulation at one year follow up.
This case highlights cerebellar injury as a potential cause of poorly regulated emotions, or an emotional dysmetria. The recognition of this disorder in patients with cerebellar or pontine strokes is critical, as untreated pseudobulbar affect can impact future stroke rehabilitation.
Peer Review reports
Pseudobulbar affect (PBA) is a dysregulation of emotions that can occur in 17–20% of patients with acute ischemic stroke [ 1 ]. Typical symptoms include crying or laughter that is disproportionate and/or inappropriate to context, not under full voluntary control, and can occur multiple times a day [ 2 ]. Between emotional outbursts, symptoms generally resolve. Unfortunately, PBA is frequently underrecognized and thus physicians may miss opportunities to treat and improve care in patients following stroke [ 3 ]. Early recognition and treatment of PBA can have significant implications on quality of life and patient engagement with rehabilitation, resulting in improved recovery post stroke.
While PBA is commonly associated with damage to the cortex and limbic system, it’s important to emphasize that it can also be a concern in patients with cerebellar and pontine strokes. Emotion is distributed widely across the brain involving cortical and subcortical structures, including the limbic system, brainstem and cerebellum [ 4 ]. PBA can result from injury or dysfunction anywhere along the cortico-ponto-cerebellar pathway [ 5 ]. Other disorders of emotional regulation, including depression and mania, have also been described in the context of cerebellar lesions, as recently reviewed by Frazier et al. [ 6 ], and is also known to occur as cerebellar cognitive-affective syndrome in children following surgical removal of posterior fossa tumours [ 7 ]. Within the cerebellum, the hemispheres are the main regions that contribute to PBA. The cerebellar hemispheres contain numerous tracts that project, via the pons, to and from the dorsolateral and dorsomedial prefrontal cortex, posterior parietal region, cingulate gyrus, and to limbic structures including the septal nuclei and the hippocampus [ 8 ]. The perception and experience of emotion involves this complex network for not only appropriate expression of emotions, but also the detection of emotionally charged stimuli, and assessment of the social context. The cerebellum specifically plays a role in the coordination and control of emotion expression in appropriate social circumstances, and if this coordination is impaired, a poorly measured emotional response, or a dysmetria of emotions, can occur. Emotional and contextual information from the cerebrum is sent to the cerebellum via cortico-ponto-cerebellar connections, and coordinates with the effectors in motor cortex, brainstem, and cranial nerve nuclei to express the perceived emotion [ 9 ]. If this pathway is disrupted, it may result in a discoordination of outward emotional expression, or PBA [ 10 ].
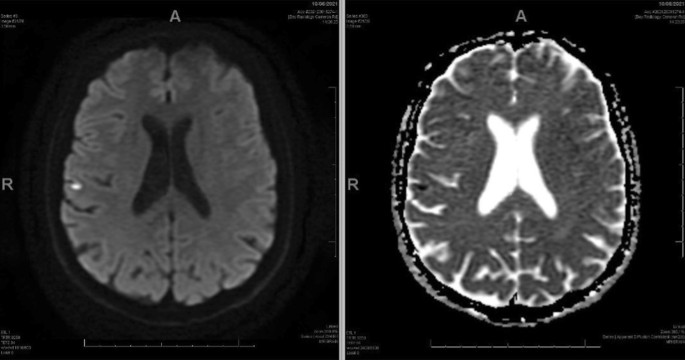
A 63-year-old Caucasian female with diabetes and dyslipidemia presented with sudden onset gait instability, right-sided hemiplegia, and severe dysarthria. She was previously independent, required no additional support and lived in a private home. The symptoms started 1.5 h prior to her presentation. Her NIHSS was 13. Neurovascular imaging revealed a proximal occlusion of her basilar artery, which was successfully recanalized with endovascular therapy five hours after her symptom onset. She regained antigravity strength on the right side, with subsequent brain imaging showing bilateral cerebellar and pontine ischemia (Figs. 1 , 2 ), which was the likely cause of her deficits.
Plain computed tomography brain scan showing ischemia of the lateral right cerebellar hemisphere (arrow)
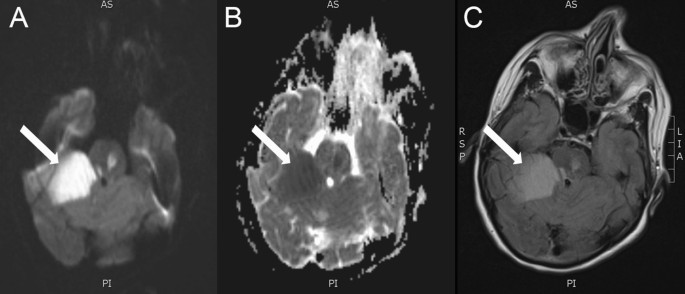
MR Brain with DWI ( A ), ADC ( B ), and FLAIR ( C ) sequences. The white arrows demonstrate a large territory of restricted diffusion in the right cerebellar hemisphere, with an additional focus in the left pons
During her recovery in hospital, she began to experience sudden outbursts of tearfulness in response to routine questions. The tearfulness was often so intrusive, it prevented her from conversing. Additionally, bedside PHQ-9 was completed 7 days after her stroke with a score of 18, suggesting moderately severe depressive symptoms. A diagnosis of PBA was made due to her uncontrollable tearfulness. Interestingly, she was able to recognize that her emotional response was inappropriate given the current context, a feature that is not always present in PBA. She denied any history of depression, anxiety, or other mood disorders. The emotional lability limited her capacity to communicate effectively with clinical staff and engage in rehabilitation as she was unable to control her tearfulness during interactions, which resulted in increased social stress, exacerbating the situation further. She was started on escitalopram 10 mg and noted an improvement in emotional lability over the ensuing weeks, allowing better engagement in her post-stroke rehabilitation.
She was transitioned to a long-term rehabilitation centre for a few months where she continued to improve. At her follow-up visits 1 year later, she still had some residual right sided hemiparesis and right arm and leg ataxia, but her mood and emotion regulation have remained stabilized on escitalopram. She remains fully independent for her basic ADLs and requires minimal assistance with some instrumental ADLs.
Emotion processing occurs across cortical, subcortical, and cerebellar regions within the brain [ 4 , 5 , 6 , 7 , 8 , 9 ], and damage along this pathway can result in varying degrees of emotional impairment. In patients with PBA, their insight into their emotional response may also be affected. While literature and formal investigation is lacking, this impairment of insight can potentially aid in the localization of the lesion along the cortico-ponto-cerebellar pathway, with cortical lesions anecdotally resulting in loss of emotional insight, and lesions of the pons or cerebellum reportingly sparing insight [ 11 ]. This dissociation follows the idea that the cortical and subcortical regions of the brain are more involved in emotional processing and interpretation, while the pons and cerebellum play a role in modulating the motor output. Currently, this relationship has not been fully established, and represents an opportunity for further research. While not supported in the current literature, we speculate that intact cortical and subcortical regions may be required for retained insight, as shown in the current presentation. In a patient with a cerebellar/pontine stroke, the presence of increased emotionality with retained insight may provide clues that uniquely link cortical and subcortical areas with emotional reasoning in the context of PBA. In addition to impacting a person’s interpretation of their resulting emotional state, untreated PBA can have a deleterious impact on post-stroke recovery in other ways, making recognition of PBA in cerebellar stroke critical. The dysmetric expression of emotion often causes patients distress and embarrassment, leading to curtailment of social engagement, and therefore limited participation in rehabilitation and interaction with others. As such, prompt recognition and initiation of treatment can be advantageous in expediting effective rehabilitation practices. Additionally, PBA can exacerbate pre-existing anxiety and depression, further hindering rehabilitation efforts [ 10 ]. While there are no reports on how PBA directly affects the outcome of stroke rehabilitation, it is known that emotional impairment such as depression can complicate and delay stroke rehabilitation [ 12 ]. Further, caregivers report they endure more distress and upsetting experiences than caregivers of non-PBA patients [ 10 ]. Overall, early treatment of PBA can reduce emotional outbursts [ 13 , 14 ] and may help improve stroke outcomes. Antidepressants and dextromethorphan-quinidine are commonly used in the treatment of PBA, with adjunctive cognitive therapy also being of potential benefit [ 15 ].
In conclusion, while PBA can occur in patients with damage to the cortex and limbic system, it can also occur with ischemic stroke of the cerebellum and pons. Here, we suggest that PBA should be considered when emotional dysmetria is identified. Early recognition is important, as prompt treatment can improve quality of life, reduce associated depression and anxiety, and increase engagement in post-stroke rehabilitation. The presented case highlights the role of ischemic injury to the cerebellum and pons as a cause of PBA with retained insight into emotional response. Recognition of PBA in the presented patient permitted early initiation of a selective serotonin reuptake inhibitor, which reduced her emotional lability and aided her participation in post-stroke rehabilitation.
Availability of data and materials
Not applicable.
Gillesie DC, Cadden AP, Lees R, West RM, Broomfield NM. Prevalence of pseudobulbar affect following stroke: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2016;25(3):688–94.
Article Google Scholar
Dark FL, McGrath JJ, Ron MA. Pathological laughing and crying. Aust NZJ Psychiatry. 1996. https://doi.org/10.3109/00048679609065020 .
Work SS, Colamonico JA, Bradley WG, Kaye RE. Pseudobulbar affect: an under-recognized and under-treated neurological disorder. Adv Ther. 2011;28(7):586–601.
Article PubMed Google Scholar
Parvizi J, Coburn KL, Shillcutt SD, Coffey CE, Lauterbach EC, Mendez MF. Neuroanatomy of pathological laughing and crying: a report of the American neuropsychiatric association committee on research. J Neuropsychiatry Clin Neurosci. 2009;21(1):75–87.
Trojsi F, Di Nardo F, D’Alvano G, Caiazzo G, Passaniti C, Mangione A, et al . Resting state fMRI analysis of pseudobulbar affect in amyotrophic lateral sclerosis (ALS): motor dysfunction of emotional expression. Brain Imaging Behav. 2023;17(1):77–89.
Frazier MR, Hoffman LJ, Popal H, Sullivan-Toole H, Olino TM, Olson IR. A missing link in affect regulation: the cerebellum. Soc Cogn Affect Neurosci. 2022;17(12):1068–81.
Article PubMed PubMed Central Google Scholar
Schmahmann JD. Pediatric post-operative cerebellar mutism syndrome, cerebellar cognitive affective syndrome, and posterior fossa syndrome: historical review and proposed resolution to guide future study. Childs Nerv Syst. 2020;36(6):1205–14.
Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain. 1998;121:561–79.
Parvizi J, Anderson SW, Martin C, Damasio H, Damasio AR. Pathological laughter and crying: A link to the cerebellum. Brain. 2001;124(9):1708–19.
Article CAS PubMed Google Scholar
Girotra T, Lowe F, Feng W. Pseudobulbar affect after stroke: a narrative review. Top Stroke Rehabil. 2018;25(8):610–6.
Sacco S, Sarà M, Pistoia F, Conson M, Albertini G, Carolei A. Management of pathologic laughter and crying in patients with locked-in syndrome: a report of 4 cases. Arch Phys Med Rehabil. 2008;89(4):775–8.
Pompili M, Venturini P, Campi S, Seretti ME, Montebovi F, Lamis DA, et al . Do stroke patients have an increased risk of developing suicidal ideation or dying by suicide? An overview of the current literature. CNS Neurosci Ther. 2012;18(9):711–21.
Murai T, Barthel H, Berrouschot J, Sorger D, Yves von Cramon D, Müller U. Neuroimaging of serotonin transporters in post-stroke pathological crying. Psychiatry Res Neuroimaging. 2003;123(3):207–11.
Article CAS Google Scholar
Nadeau SE. Treatment of disorders of emotional comprehension, expression, and emotional semantics. Handb Clin Neurol. 2021;183:283–97.
Kasprisin A. Alternative cognitive therapy for emotional instability (pathologic laughing and crying). Phys Med Rehabil Clin N Am. 2004;15(4):883–917.
Download references
Acknowledgements
We would like to thank the participant for their involvement in the creation and publication of this manuscript.
Author information
Authors and affiliations.
Cumming School of Medicine, University of Calgary, Calgary, Canada
Rebecca M. Long
Neuroscience and Mental Health Institute, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Canada
Rebecca M. Long & Glen C. Jickling
Department of Medicine, Division of Neurology, University of Alberta, Edmonton, Canada
Michèle DuVal, Bridget Mulvany-Robbins, Amanda N. Wagner & Glen C. Jickling
You can also search for this author in PubMed Google Scholar
Contributions
RML and GCJ conceived the article. RML drafted the manuscript. MD, BMR, ANW, and GCJ were involved in patient care. All authors participated in editing and approved the final manuscript.
Corresponding author
Correspondence to Rebecca M. Long .
Ethics declarations
Ethics approval and consent to participate., consent for publication.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
Additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Long, R.M., DuVal, M., Mulvany-Robbins, B. et al. Emotional dysmetria after cerebellar-pontine stroke: a case report. J Med Case Reports 17 , 544 (2023). https://doi.org/10.1186/s13256-023-04294-1
Download citation
Received : 29 September 2023
Accepted : 29 November 2023
Published : 15 December 2023
DOI : https://doi.org/10.1186/s13256-023-04294-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pseudobulbar affect
- Ischemic stroke
- Emotional lability
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Case Report
- Open access
- Published: 01 February 2023
A case report of an ischaemic stroke, caused by a primary cardiac intimal sarcoma
- Joshua Lloyd 1 ,
- Navinee Gilliat 1 ,
- Graeme Porter 1 &
- Francesco Pirone 2
BMC Cardiovascular Disorders volume 23 , Article number: 59 ( 2023 ) Cite this article
1915 Accesses
Metrics details
Intimal sarcomas are an extremely rare type of primary cardiac malignancy. They most commonly present with symptoms of cardiac dysfunction. We present a case of intimal sarcoma identified without any cardiac signs or symptoms. Cardiac sarcomas historically carry a very poor prognosis.
Presentation
A 57-year-old man presented with a sudden onset of left limb weakness and disorientation. MRI brain identified an acute ischaemic stroke in the right anterior temporal lobe. Four months later, he presented again with transient left arm weakness. The patient had a normal cardiovascular examination and ECG. All other initial investigations for cryptogenic stroke were non-contributory. The patient did not initially get an echocardiogram. When this investigation was performed, after his second presentation, a large pedunculated mass was present in his left atrium. This was resected and identified histologically as a primary intimal sarcoma of his left atrium. The patient was treated with post-operative radiotherapy but declined chemotherapy. He recovered well post-operatively but subsequently passed away 14 months after diagnosis.
Conclusions
It is possible for primary cardiac malignancies to present with only symptoms of systemic emboli. For this reason, echocardiography is a crucial investigation in cases of cryptogenic stroke. Some stroke guidelines do not definitively support routine echocardiography. Primary intimal cardiac sarcoma is a very rare condition with a poor prognosis. The literature is limited to case reports and optimal management is with surgical resection where possible. The role of post operative radiotherapy and chemotherapy is uncertain.
Peer Review reports
Even as a broader group, primary cardiac malignancies are rare, with 34 cases per 100 million persons. Cardiac sarcomas make up approximately 65% of primary cardiac malignancies [ 1 ]. Intimal sarcomas appear to be the rarest subtype of sarcoma, with only a small number ever reported in the literature [ 2 , 3 ].
Most commonly this malignancy presents with chest pain, oedema, dyspnoea and palpitations [ 1 , 4 ]. We report a case where the patient presented with purely neurological symptoms, with no clinical clue of his underlying cardiac malignancy. We are aware of only one other case of primary cardiac sarcoma presenting with stroke. In that case it is unclear if there were abnormalities on ECG or cardiovascular examination [ 2 ].
Histologically, intimal sarcoma is identified by poorly differentiated spindle shaped cells that may resemble smooth muscle. These tumours can be difficult to diagnose both histologically and radiologically. This, along with their rarity, mean there are frequently delays in diagnosis [ 5 ]. The incidence of cardiac sarcoma is increasing, so clinicians may be faced with this condition in the future [ 1 ].
Most previous cases have been treated with surgical resection, where possible. There is a possible role for radiotherapy or systemic chemotherapy. Management can be very difficult, with very few previous cases to judge whether radiotherapy or chemotherapy have any benefit. The prognosis of this condition is extremely poor, with mean survival quoted as being between 3 and 12 months [ 2 ].
Case presentation
A fit 57-year-old building inspector presented, by ambulance, with sudden onset left limb weakness and “shaking”, associated with confusion. The symptoms lasted minutes and had resolved before arrival to the Emergency Department. He had a background of homozygous ZZ phenotype alpha-1-antitrypsin deficiency with associated mild bi-basal bronchiectasis and a distant background of a resected melanoma.
Four months later, he presented again with a sudden onset of episodes of left arm weakness. The episodes lasted several minutes, with complete resolution in between, over a period of eight hours. He had no other neurological, cardio-respiratory, or systemic symptoms of note. His neurological and cardio-respiratory examination was normal.

Investigations
The patient’s most recent imaging prior to this presentation was a CT chest from 3 years earlier, which showed mid to lower zone panlobular emphysematous change with associated bronchiectasis and no obvious cardiac abnormality.
At the initial presentation the patient had unremarkable basic bloods. Baseline ECG and 72 h of continuous ECG monitoring demonstrated no atrial fibrillation or other arrhythmia. CT and CTA of head and neck showed normal appearance of intra and extracranial arteries with no significant atherosclerotic disease. MRI brain revealed acute right anterior temporal lobe infarction (Fig. 1 ).
MRI brain at initial presentation
Given the higher incidence of ANCA associated vasculitis in patients with alpha 1 antitrypsin deficiency, a vasculitis screening panel was sent. This was still pending at the time of discharge, but eventually returned as negative.
When the patient re-presented with further episodes of left sided weakness, repeat MRI brain showed a small focus of acute restricted diffusion at the left superior temporal gyrus and gliosis at the site of the previous temporal infarct (Fig. 2 ).
MRI brain at the second presentation
Repeat CTA of head and neck, telemetry and vasculitis screen did not reveal any clear cause for ischaemic stroke. His ECG showed normal sinus rhythm.
Echocardiography was not performed at the patient’s first presentation, based on our interpretation of local guidelines [ 6 , 7 ]. This is explained further in the discussion. When echocardiography was performed at the patient’s second presentation, it revealed a very large pedunculated mobile mass approximately 65 × 35 mm which filled the left atrium and prolapsed through the mitral valve (Fig. 3 ).
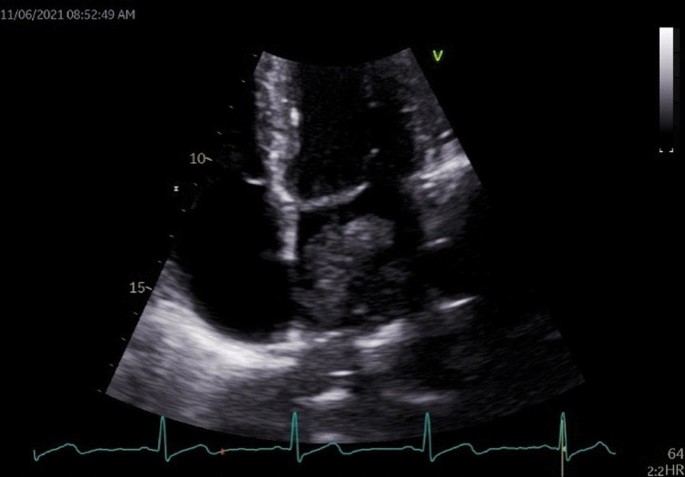
Pedunculated mass within the left atrium
CT chest/abdomen/pelvis subsequently showed a left atrial lesion with extension into bilateral inferior pulmonary veins and left ventricle and several enlarged retro-cardiac lymph nodes. There was no evidence of any other lesion.
The patient underwent a left atrial mass excision on the third day of his second admission. (Fig. 4 ).
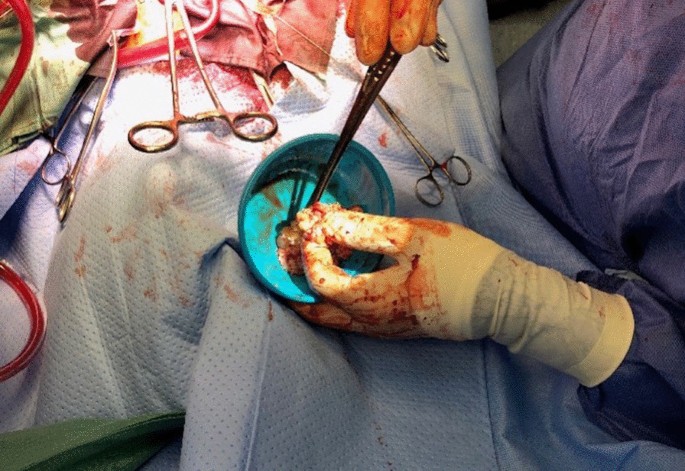
Intra-operative image of the atrial sarcoma, immediately after resection
The histology was reported as 90 mm pleomorphic spindle cell tumour. (Fig. 5 ) Tumour was seen to the inked margin.
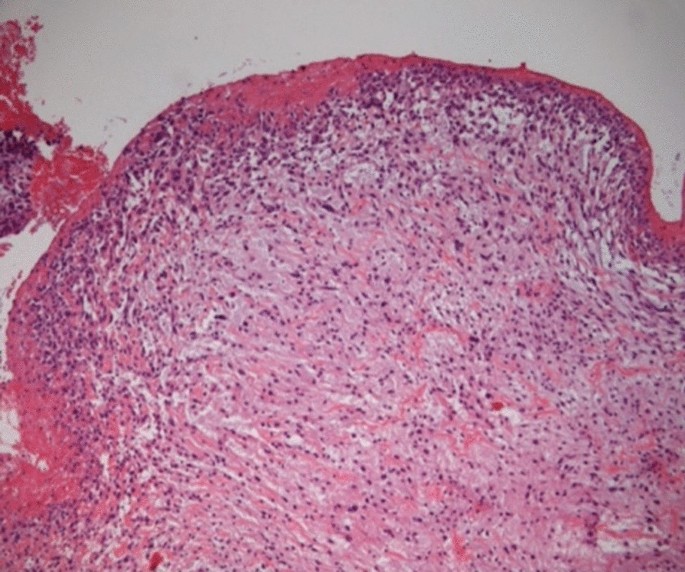
Hematoxylin and eosin staining of a section of the excised mass, at 40 × magnification. Pleomorphic spindle cells within a myxoid background are seen below the eroded endothelial layer, accompanied by a surface fibrinous exudate
He recovered well. He was discharged on the thirteenth post-operative day.
After discussion at the national sarcoma multi-disciplinary meeting, this was felt to be an intimal sarcoma. The patient underwent outpatient post-operative radiotherapy to the sarcoma site. He received 3 months of warfarin and aspirin post operatively and then moved to aspirin monotherapy.
Outcome and follow up
The patient recovered well from this treatment. He returned to work, with a Modified Rankin Score of 0. Three-monthly echocardiographs and CT chest, abdomen and pelvis did not show any evidence of disease recurrence. Despite these reassuring investigations, the patient presented acutely to the emergency department 14 months after his diagnosis with symptoms of a small bowel obstruction. CT of his abdomen identified probable metastatic disease. He passed away several days later in hospital.
Very few cases of primary intimal sarcoma have been previously reported. While previous cases have tended to present with signs of cardiac dysfunction [ 1 , 8 ], this case did not have any signs to indicate his underlying cardiac malignancy.
Other, more common forms of left atrial tumours such as left atrial myxoma are recognized as “high risk” for embolization by consensus [ 9 ]. There are reports of other subtypes of cardiac sarcoma presenting with stroke [ 4 , 10 ]. It is therefore reasonable to consider that our patient’s neurological symptoms were embolic.
This patient had a normal cardiovascular history and examination, as well as normal ECGs and cardiac monitoring. He had no known risk factors for cardiovascular disease. Despite this, he had an underlying primary cardiac malignancy.
Echocardiography was crucial in establishing this diagnosis. Current Royal College of Physicians stroke guidelines recognize the importance of echocardiography in stroke, however in the “Choosing Wisely” section, they say to NOT perform echocardiograms routinely. They suggest selecting patients with history of structural cardiac disease or abnormal physical or ECG findings [ 6 ].Our case did not meet these criteria. The Australasian stroke guidelines, adopted by our institute, suggest echocardiography considering “based on an individual patient factors” [ 7 ]. While you could make an argument that these guidelines support echocardiography, they are not completely clear.
Subsequent to this case, we strongly advocate for performing echocardiography as a first line investigation in cryptogenic stroke, even in the absence of any cardiac signs. This may lead to earlier identification and more successful treatment of these rare cardiac malignancies. We suggest that local clinicians follow guidelines released by the Cardiac Society of Australian and New Zealand. They are more definite with their recommendation for echocardiography. They suggest transthoracic echocardiography for all cryptogenic stroke in people under 60 years-old [ 8 ].
Cardiac sarcomas generally carry a very poor prognosis. One year survival is only 47%. Three-year survival is 21% [ 1 ]. Intimal sarcomas as a subtype appear to have even poorer outcomes, with mean survival between 3 and 12 months [ 2 ]. Treatment with surgical resection and post operative radiotherapy, in our case, led to the patient having a period of good quality of life and no macroscopic evidence of disease. Sadly, he later died due to disease recurrence in the abdomen, 14 months after diagnosis and resection. It is difficult to establish optimal treatment in this disease given its high malignant potential and rarity.
Despite their extreme rarity, the incidence of cardiac sarcomas is increasing. [ 1 ] It is possible clinicians may come across them in the future.
Learning points
In cases of cryptogenic stroke, even in the absence of cardiac symptoms and signs, trans-thoracic echo should be considered.
Cardiac malignant tumours most commonly present with chest pain, dyspnoea and decompensated heart failure. They can present with symptoms of systemic emboli only, with no cardiac history or physical signs.
The management of primary cardiac malignancy is complex and involves a large range of specialist services. Surgical resection, where possible, is the mainstay of treatment.
In general, the prognosis of a primary intimal cardiac sarcoma is poor, based on a small number of case studies.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Oliveira G, Al-Kindi S, Hoimes C, et al. Characteristics and survival of malignant cardiac tumors. Circulation. 2015;132(25):2395–402.
Article Google Scholar
Moeri-Schimmel R, Pras E, Desar I, et al. Primary sarcoma of the heart: case report and literature review. J Cardiothorac Surg. 2020;15(1):1–6.
Ibrahim A, Luk A, Singhal P, et al. Primary intimal (spindle cell) sarcoma of the heart: a case report and review of the literature. Case Rep Med. 2013;2013:1–5.
Barreiro M, Renilla A, Jimenez J, et al. Primary cardiac tumors: 32 years of experience from a Spanish tertiary surgical center. Cardiovasc Pathol. 2013;22(6):424–7.
Ho K, Yatham K, Seno R, Sultan O. A case report of primary cardiac intimal sarcoma presenting with atrial fibrillation and a left atrial mass. Eur Heart J Case Rep. 2021;5(11):ytab410.
Intercollegiate Stroke Working Party. National clinical guideline for stroke, 5th edn. London: Royal College of Physicians; 2016, Choosing Wisely; p. xvii.
Stroke Foundation. Australian and New Zealand Clinical Guidelines for Stroke Management. Melbourne; 2017. Chapter 2, Early assessment and diagnosis; [cited 2022 March 21]; Available from: https://informme.org.au/guidelines/clinical-guidelines-for-stroke-management.
Sasse A, O'Meeghan T, Anscombe R, et al. Appropriateness Guideline for Adult Echocardiography (New Zealand). Wellington: Cardiac Society of Australia and New Zealand; 2017. Stroke - Cardiac source of embolism; [cited 2022 March 21]; p. 12. Available from: https://cardiacsociety.org.nz/wp-content/uploads/Echo-Appropriateness-Guidelines-NZ.pdf.
Ay H, Furie K, Singhal A, et al. An evidence-based causative classification system for acute ischemic stroke. Ann Neurol. 2005;58(5):688–97.
Pickering L, Cox I, Pandha H. Left atrial sarcoma presenting as cerebral infarction. Lancet Oncol. 2001;2(11):705–6.
Article CAS Google Scholar
Download references
Acknowledgements
Dr Michelle Head, Oncologist was involved in reviewing ongoing management and considering the role of chemotherapy. Dr Michael Arendse, Pathologist reviewed and provided description of histology.
Not Applicable.
Author information
Authors and affiliations.
Te Whatu Ora Health New Zealand – Bay of Plenty, 829 Cameron Road, Tauranga South, Tauranga, 3112, New Zealand
Joshua Lloyd, Navinee Gilliat & Graeme Porter
Te Whatu Ora Health New Zealand – Waikato, 183 Pembroke Street, Hamilton, 3204, New Zealand
Francesco Pirone
You can also search for this author in PubMed Google Scholar
Contributions
JL was the major contributor to writing the manuscript and was involved in part of the team caring for the patient. NG was the consultant who the patient was originally admitted under and who organised his initial management and investigation. NG had ongoing role following up the patient. NG contributed to some of the writing of the manuscript. GP reported the echocardiogram and arranged transfer for cardiac surgery. He had a role in the writing of the manuscript. He was part of the patients ongoing follow up. FP was the surgeon who resected the malignancy. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Joshua Lloyd .
Ethics declarations
Ethics approval and consent to participate.
Written informed patient consent. Ethics committee approval Not applicable.
Consent for publication
We have written informed consent from the patient (before he passed away) to publish his case and associated investigations.
Competing Interests
The author’s declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lloyd, J., Gilliat, N., Porter, G. et al. A case report of an ischaemic stroke, caused by a primary cardiac intimal sarcoma. BMC Cardiovasc Disord 23 , 59 (2023). https://doi.org/10.1186/s12872-023-03090-5
Download citation
Received : 14 November 2022
Accepted : 24 January 2023
Published : 01 February 2023
DOI : https://doi.org/10.1186/s12872-023-03090-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Intimal sarcoma
- Case report
- Primary cardiac malignancy
BMC Cardiovascular Disorders
ISSN: 1471-2261
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 13, Issue 8
- Clinical course of a 66-year-old man with an acute ischaemic stroke in the setting of a COVID-19 infection
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-7441-6952 Saajan Basi 1 , 2 ,
- Mohammad Hamdan 1 and
- Shuja Punekar 1
- 1 Department of Stroke and Acute Medicine , King's Mill Hospital , Sutton-in-Ashfield , UK
- 2 Department of Acute Medicine , University Hospitals of Derby and Burton , Derby , UK
- Correspondence to Dr Saajan Basi; saajan.basi{at}nhs.net
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater oxygen requirement, alongside reduced levels of consciousness. A positive COVID-19 throat swab, in addition to bilateral pneumonia on chest X-ray and lymphopaenia in his blood tests, confirmed a diagnosis of COVID-19 pneumonia. A proactive decision was made involving the patients’ family, ward and intensive care healthcare staff, to not escalate care above a ward-based ceiling of care. The patient died 5 days following admission under the palliative care provided by the medical team.
- respiratory medicine
- infectious diseases
- global health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bcr-2020-235920
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is a new strain of coronavirus that is thought to have originated in December 2019 in Wuhan, China. In a matter of months, it has erupted from non-existence to perhaps the greatest challenge to healthcare in modern times, grinding most societies globally to a sudden halt. Consequently, the study and research into SARS-CoV-2 is invaluable. Although coronaviruses are common, SARS-CoV-2 appears to be considerably more contagious. The WHO figures into the 2003 SARS-CoV-1 outbreak, from November 2002 to July 2003, indicate a total of 8439 confirmed cases globally. 1 In comparison, during a period of 4 months from December 2019 to July 2020, the number of global cases of COVID-19 reached 10 357 662, increasing exponentially, illustrating how much more contagious SARS-CoV-2 has been. 2
Previous literature has indicated infections, and influenza-like illness have been associated with an overall increase in the odds of stroke development. 3 There appears to be a growing correlation between COVID-19 positive patients presenting to hospital with ischaemic stroke; however, studies investigating this are in progress, with new data emerging daily. This patient report comments on and further characterises the link between COVID-19 pneumonia and the development of ischaemic stroke. At the time of this patients’ admission, there were 95 positive cases from 604 COVID-19 tests conducted in the local community, with a predicted population of 108 000. 4 Only 4 days later, when this patient died, the figure increased to 172 positive cases (81% increase), illustrating the rapid escalation towards the peak of the pandemic, and widespread transmission within the local community ( figure 1 ). As more cases of ischaemic stroke in COVID-19 pneumonia patients arise, the recognition and understanding of its presentation and aetiology can be deciphered. Considering the virulence of SARS-CoV-2 it is crucial as a global healthcare community, we develop this understanding, in order to intervene and reduce significant morbidity and mortality in stroke patients.
- Download figure
- Open in new tab
- Download powerpoint
A graph showing the number of patients with COVID-19 in the hospital and in the community over time.
Case presentation
A 66-year-old man presented to the hospital with signs of left-sided weakness. The patient had a background of chronic obstructive pulmonary disease (COPD), atrial fibrillation and had one previous ischaemic stroke, producing left-sided haemiparesis, which had completely resolved. He was a non-smoker and lived in a house. The patient was found slumped over on the sofa at home on 1 April 2020, by a relative at approximately 01:00, having been seen to have no acute medical illness at 22:00. The patients’ relative initially described disorientation and agitation with weakness noted in the left upper limb and dysarthria. At the time of presentation, neither the patient nor his relative identified any history of fever, cough, shortness of breath, loss of taste, smell or any other symptoms; however, the patient did have a prior admission 9 days earlier with shortness of breath.
The vague nature of symptoms, entwined with considerable concern over approaching the hospital, due to the risk of contracting COVID-19, created a delay in the patients’ attendance to the accident and emergency department. His primary survey conducted at 09:20 on 1 April 2020 demonstrated a patent airway, with spontaneous breathing and good perfusion. His Glasgow Coma Scale (GCS) score was 15 (a score of 15 is the highest level of consciousness), his blood glucose was 7.2, and he did not exhibit any signs of trauma. His abbreviated mental test score was 7 out of 10, indicating a degree of altered cognition. An ECG demonstrated atrial fibrillation with a normal heart rate. His admission weight measured 107 kg. At 09:57 the patient required 2 L of nasal cannula oxygen to maintain his oxygen saturations between 88% and 92%. He started to develop agitation associated with an increased respiratory rate at 36 breaths per minute. On auscultation of his chest, he demonstrated widespread coarse crepitation and bilateral wheeze. Throughout he was haemodynamically stable, with a systolic blood pressure between 143 mm Hg and 144 mm Hg and heart rate between 86 beats/min and 95 beats/min. From a neurological standpoint, he had a mild left facial droop, 2/5 power in both lower limbs, 2/5 power in his left upper limb and 5/5 power in his right upper limb. Tone in his left upper limb had increased. This patient was suspected of having COVID-19 pneumonia alongside an ischaemic stroke.
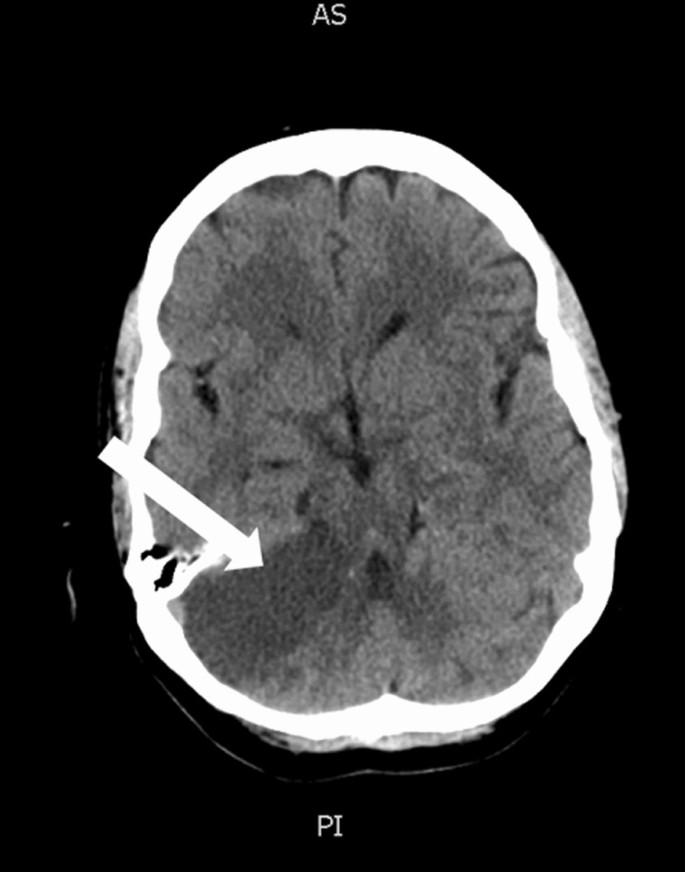
Investigations
A CT of his brain conducted at 11:38 on 1 April 2020 ( figure 2 ) illustrated an ill-defined hypodensity in the right frontal lobe medially, with sulcal effacement and loss of grey-white matter. This was highly likely to represent acute anterior cerebral artery territory infarction. Furthermore an oval low-density area in the right cerebellar hemisphere, that was also suspicious of an acute infarction. These vascular territories did not entirely correlate with his clinical picture, as limb weakness is not as prominent in anterior cerebral artery territory ischaemia. Therefore this left-sided weakness may have been an amalgamation of residual weakness from his previous stroke, in addition to his acute cerebral infarction. An erect AP chest X-ray with portable equipment ( figure 3 ) conducted on the same day demonstrated patchy peripheral consolidation bilaterally, with no evidence of significant pleural effusion. The pattern of lung involvement raised suspicion of COVID-19 infection, which at this stage was thought to have provoked the acute cerebral infarct. Clinically significant blood results from 1 April 2020 demonstrated a raised C-reactive protein (CRP) at 215 mg/L (normal 0–5 mg/L) and lymphopaenia at 0.5×10 9 (normal 1×10 9 to 3×10 9 ). Other routine blood results are provided in table 1 .
CT imaging of this patients’ brain demonstrating a wedge-shaped infarction of the anterior cerebral artery territory.
Chest X-ray demonstrating the bilateral COVID-19 pneumonia of this patient on admission.
- View inline
Clinical biochemistry and haematology blood results of the patient
Interestingly the patient, in this case, was clinically assessed in the accident and emergency department on 23 March 2020, 9 days prior to admission, with symptoms of shortness of breath. His blood results from this day showed a CRP of 22 mg/L and a greater lymphopaenia at 0.3×10 9 . He had a chest X-ray ( figure 4 ), which indicated mild radiopacification in the left mid zone. He was initially treated with intravenous co-amoxiclav and ciprofloxacin. The following day he had minimal symptoms (CURB 65 score 1 for being over 65 years). Given improving blood results (declining CRP), he was discharged home with a course of oral amoxicillin and clarithromycin. As national governmental restrictions due to COVID-19 had not been formally announced until 23 March 2020, and inconsistencies regarding personal protective equipment training and usage existed during the earlier stages of this rapidly evolving pandemic, it is possible that this patient contracted COVID-19 within the local community, or during his prior hospital admission. It could be argued that the patient had early COVID-19 signs and symptoms, having presented with shortness of breath, lymphopaenia, and having had subtle infective chest X-ray changes. The patient explained he developed a stagnant productive cough, which began 5 days prior to his attendance to hospital on 23 March 2020. He responded to antibiotics, making a full recovery following 7 days of treatment. This information does not assimilate with the typical features of a COVID-19 infection. A diagnosis of community-acquired pneumonia or infective exacerbation of COPD seem more likely. However, given the high incidence of COVID-19 infections during this patients’ illness, an exposure and early COVID-19 illness, prior to the 23 March 2020, cannot be completely ruled out.
Chest X-ray conducted on prior admission illustrating mild radiopacification in the left mid zone.
On the current admission, this patient was managed with nasal cannula oxygen at 2 L. By the end of the day, this had progressed to a venturi mask, requiring 8 L of oxygen to maintain oxygen saturation. He had also become increasingly drowsy and confused, his GCS declined from 15 to 12. However, the patient was still haemodynamically stable, as he had been in the morning. An arterial blood gas demonstrated a respiratory alkalosis (pH 7.55, pCO 2 3.1, pO 2 6.7 and HCO 3 24.9, lactate 1.8, base excess 0.5). He was commenced on intravenous co-amoxiclav and ciprofloxacin, to treat a potential exacerbation of COPD. This patient had a COVID-19 throat swab on 1 April 2020. Before the result of this swab, an early discussion was held with the intensive care unit staff, who decided at 17:00 on 1 April 2020 that given the patients presentation, rapid deterioration, comorbidities and likely COVID-19 diagnosis he would not be for escalation to the intensive care unit, and if he were to deteriorate further the end of life pathway would be most appropriate. The discussion was reiterated to the patients’ family, who were in agreement with this. Although he had evidence of an ischaemic stroke on CT of his brain, it was agreed by all clinicians that intervention for this was not as much of a priority as providing optimal palliative care, therefore, a minimally invasive method of treatment was advocated by the stroke team. The patient was given 300 mg of aspirin and was not a candidate for fibrinolysis.
Outcome and follow-up
The following day, before the throat swab result, had appeared the patient deteriorated further, requiring 15 L of oxygen through a non-rebreather face mask at 60% FiO 2 to maintain his oxygen saturation, at a maximum of 88% overnight. At this point, he was unresponsive to voice, with a GCS of 5. Although, he was still haemodynamically stable, with a blood pressure of 126/74 mm Hg and a heart rate of 98 beats/min. His respiratory rate was 30 breaths/min. His worsening respiratory condition, combined with his declining level of consciousness made it impossible to clinically assess progression of the neurological deficit generated by his cerebral infarction. Moreover, the patient was declining sharply while receiving the maximal ward-based treatment available. The senior respiratory physician overseeing the patients’ care decided that a palliative approach was in this his best interest, which was agreed on by all parties. The respiratory team completed the ‘recognising dying’ documentation, which signified that priorities of care had shifted from curative treatment to palliative care. Although the palliative team was not formally involved in the care of the patient, the patient received comfort measures without further attempts at supporting oxygenation, or conduction of regular clinical observations. The COVID-19 throat swab confirmed a positive result on 2 April 2020. The patient was treated by the medical team under jurisdiction of the hospital palliative care team. This included the prescribing of anticipatory medications and a syringe driver, which was established on 3 April 2020. His antibiotic treatment, non-essential medication and intravenous fluid treatment were discontinued. His comatose condition persisted throughout the admission. Once the patients’ GCS was 5, it did not improve. The patient was pronounced dead by doctors at 08:40 on 5 April 2020.
SARS-CoV-2 is a type of coronavirus that was first reported to have caused pneumonia-like infection in humans on 3 December 2019. 5 As a group, coronaviruses are a common cause of upper and lower respiratory tract infections (especially in children) and have been researched extensively since they were first characterised in the 1960s. 6 To date, there are seven coronaviruses that are known to cause infection in humans, including SARS-CoV-1, the first known zoonotic coronavirus outbreak in November 2002. 7 Coronavirus infections pass through communities during the winter months, causing small outbreaks in local communities, that do not cause significant mortality or morbidity.
SARS-CoV-2 strain of coronavirus is classed as a zoonotic coronavirus, meaning the virus pathogen is transmitted from non-humans to cause disease in humans. However the rapid spread of SARS-CoV-2 indicates human to human transmission is present. From previous research on the transmission of coronaviruses and that of SARS-CoV-2 it can be inferred that SARS-CoV-2 spreads via respiratory droplets, either from direct inhalation, or indirectly touching surfaces with the virus and exposing the eyes, nose or mouth. 8 Common signs and symptoms of the COVID-19 infection identified in patients include high fevers, severe fatigue, dry cough, acute breathing difficulties, bilateral pneumonia on radiological imaging and lymphopaenia. 9 Most of these features were identified in this case study. The significance of COVID-19 is illustrated by the speed of its global spread and the potential to cause severe clinical presentations, which as of April 2020 can only be treated symptomatically. In Italy, as of mid-March 2020, it was reported that 12% of the entire COVID-19 positive population and 16% of all hospitalised patients had an admission to the intensive care unit. 10
The patient, in this case, illustrates the clinical relevance of understanding COVID-19, as he presented with an ischaemic stroke underlined by minimal respiratory symptoms, which progressed expeditiously, resulting in acute respiratory distress syndrome and subsequent death.
Our case is an example of a new and ever-evolving clinical correlation, between patients who present with a radiological confirmed ischaemic stroke and severe COVID-19 pneumonia. As of April 2020, no comprehensive data of the relationship between ischaemic stroke and COVID-19 has been published, however early retrospective case series from three hospitals in Wuhan, China have indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke. 11 These studies have not yet undergone peer review, but they tell us a great deal about the relationship between COVID-19 and ischaemic stroke, and have been used to influence the American Heart Associations ‘Temporary Emergency Guidance to US Stroke Centres During the COVID-19 Pandemic’. 12
The relationship between similar coronaviruses and other viruses, such as influenza in the development of ischaemic stroke has previously been researched and provide a basis for further investigation, into the prominence of COVID-19 and its relation to ischaemic stroke. 3 Studies of SARS-CoV-2 indicate its receptor-binding region for entry into the host cell is the same as ACE2, which is present on endothelial cells throughout the body. It may be the case that SARS-CoV-2 alters the conventional ability of ACE2 to protect endothelial function in blood vessels, promoting atherosclerotic plaque displacement by producing an inflammatory response, thus increasing the risk of ischaemic stroke development. 13
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14
Arrhythmias such as atrial fibrillation had been identified in 17% of 138 COVID-19 patients, in a study conducted in Wuhan, China. 15 In this report, the patient was known to have atrial fibrillation and was treated with rivaroxaban. The acute inflammatory state COVID-19 is known to produce had the potential to create a prothrombotic environment, culminating in an ischaemic stroke.
Some early case studies produced in Wuhan describe patients in the sixth decade of life that had not been previously noted to have antiphospholipid antibodies, contain the antibodies in blood results. They are antibodies signify antiphospholipid syndrome; a prothrombotic condition. 16 This raises the hypothesis concerning the ability of COVID-19 to evoke the creation of these antibodies and potentiate thrombotic events, such as ischaemic stroke.
No peer-reviewed studies on the effects of COVID-19 and mechanism of stroke are published as of April 2020; therefore, it is difficult to evidence a specific reason as to why COVID-19 patients are developing neurological signs. It is suspected that a mixture of the factors mentioned above influence the development of ischaemic stroke.
If we delve further into this patients’ comorbid state exclusive to COVID-19 infection, it can be argued that this patient was already at a relatively higher risk of stroke development compared with the general population. The fact this patient had previously had an ischaemic stroke illustrates a prior susceptibility. This patient had a known background of hypertension and atrial fibrillation, which as mentioned previously, can influence blood clot or plaque propagation in the development of an acute ischaemic event. 15 Although the patient was prescribed rivaroxaban as an anticoagulant, true consistent compliance to rivaroxaban or other medications such as amlodipine, clopidogrel, candesartan and atorvastatin cannot be confirmed; all of which can contribute to the reduction of influential factors in the development of ischaemic stroke. Furthermore, the fear of contracting COVID-19, in addition to his vague symptoms, unlike his prior ischaemic stroke, which demonstrated dense left-sided haemiparesis, led to a delay in presentation to hospital. This made treatment options like fibrinolysis unachievable, although it can be argued that if he was already infected with COVID-19, he would have still developed life-threatening COVID-19 pneumonia, regardless of whether he underwent fibrinolysis. It is therefore important to consider that if this patient did not contract COVID-19 pneumonia, he still had many risk factors that made him prone to ischaemic stroke formation. Thus, we must consider whether similar patients would suffer from ischaemic stroke, regardless of COVID-19 infection and whether COVID-19 impacts on the severity of the stroke as an entity.
Having said this, the management of these patients is dependent on the likelihood of a positive outcome from the COVID-19 infection. Establishing the ceiling of care is crucial, as it prevents incredibly unwell or unfit patients’ from going through futile treatments, ensuring respect and dignity in death, if this is the likely outcome. It also allows for the provision of limited or intensive resources, such as intensive care beds or endotracheal intubation during the COVID-19 pandemic, to those who are assessed by the multidisciplinary team to benefit the most from their use. The way to establish this ceiling of care is through an early multidisciplinary discussion. In this case, the patient did not convey his wishes regarding his care to the medical team or his family; therefore it was decided among intensive care specialists, respiratory physicians, stroke physicians and the patients’ relatives. The patient was discussed with the intensive care team, who decided that as the patient sustained two acute life-threatening illnesses simultaneously and had rapidly deteriorated, ward-based care with a view to palliate if the further deterioration was in the patients’ best interests. These decisions were not easy to make, especially as it was on the first day of presentation. This decision was made in the context of the patients’ comorbidities, including COPD, the patients’ age, and the availability of intensive care beds during the steep rise in intensive care admissions, in the midst of the COVID-19 pandemic ( figure 1 ). Furthermore, the patients’ rapid and permanent decline in GCS, entwined with the severe stroke on CT imaging of the brain made it more unlikely that significant and permanent recovery could be achieved from mechanical intubation, especially as the damage caused by the stroke could not be significantly reversed. As hospitals manage patients with COVID-19 in many parts of the world, there may be tension between the need to provide higher levels of care for an individual patient and the need to preserve finite resources to maximise the benefits for most patients. This patient presented during a steep rise in intensive care admissions, which may have influenced the early decision not to treat the patient in an intensive care setting. Retrospective studies from Wuhan investigating mortality in patients with multiple organ failure, in the setting of COVID-19, requiring intubation have demonstrated mortality can be up to 61.5%. 17 The mortality risk is even higher in those over 65 years of age with respiratory comorbidities, indicating why this patient was unlikely to survive an admission to the intensive care unit. 18
Regularly updating the patients’ family ensured cooperation, empathy and sympathy. The patients’ stroke was not seen as a priority given the severity of his COVID-19 pneumonia, therefore the least invasive, but most appropriate treatment was provided for his stroke. The British Association of Stroke Physicians advocate this approach and also request the notification to their organisation of COVID-19-related stroke cases, in the UK. 19
Learning points
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is one of seven known coronaviruses that commonly cause upper and lower respiratory tract infections. It is the cause of the 2019–2020 global coronavirus pandemic.
The significance of COVID-19 is illustrated by the rapid speed of its spread globally and the potential to cause severe clinical presentations, such as ischaemic stroke.
Early retrospective data has indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke.
Potential mechanisms behind stroke in COVID-19 patients include a plethora of hypercoagulability secondary to critical illness and systemic inflammation, the development of arrhythmia, alteration to the vascular endothelium resulting in atherosclerotic plaque displacement and dehydration.
It is vital that effective, open communication between the multidisciplinary team, patient and patients relatives is conducted early in order to firmly establish the most appropriate ceiling of care for the patient.
- Cannine M , et al
- Wunderink RG
- van Doremalen N ,
- Bushmaker T ,
- Morris DH , et al
- Wang X-G , et al
- Grasselli G ,
- Pesenti A ,
- Wang M , et al
- American Stroke Assocation, 2020
- Zhang Y-H ,
- Zhang Y-huan ,
- Dong X-F , et al
- Li X , et al
- Hu C , et al
- Zhang S , et al
- Jiang B , et al
- Xu J , et al
- British Association of Stroke Physicians
Contributors SB was involved in the collecting of information for the case, the initial written draft of the case and researching existing data on acute stroke and COVID-19. He also edited drafts of the report. MH was involved in reviewing and editing drafts of the report and contributing new data. SP oversaw the conduction of the project and contributed addition research papers.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Next of kin consent obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
CASE REPORTS: Thrombolysis in acute retinal ischemia treated with tenecteplase
Article sidebar, main article content.
Central retinal artery occlusion (CRAO), a type of acute retinal arterial ischemia, analogous to an ocular stroke, is a medical emergency that warrants immediate diagnosis and treatment. CRAO usually presents with sudden, painless, monocular vision loss. Ipsilateral carotid artery disease is an important associated finding in these patients. The primary limitation to effective treatment of CRAO is that patients are rarely seen in the acute stage. Moreover, there are no guidelines for effective treatment. We report a patient with right CRAO whose treatment with intravenous thrombolysis with tenecteplase and anterior chamber paracentesis with ocular massage resulted in a good clinical outcome.
Article Details
- American Medical Association

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License .

Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond) 2013;27:688-97.
Biousse V, Nahab F, Newman NJ. Management of acute retinal ischemia: follow the guidelines! Ophthalmology 2018;125:1597-1607.
Dumitrascu OM, Newman NJ, Biousse V. Thrombolysis for central retinal artery occlusion in 2020: time is vision. J Neuroophthalmol 2020;40:333-45.
Burgos AM, Saver JL. Evidence that tenecteplase is noninferior to alteplase for acute ischemic stroke: meta-analysis of 5 randomized trials. Stroke 2019;50:2156-62.
Lee A, Chryssidis S, Thoo S, Chen C. Poster abstracts: AS31-039. Eur Stroke J 2017;2(1_suppl):125-26.
Mac Grory B, Schrag M, Biousse V, et al; American Heart Association Stroke Council; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Hypertension; Council on Peripheral Vascular Disease. Management of central retinal artery occlusion: a scientific statement from the American Heart Association [published correction in Stroke 2021;52:e309]. Stroke 2021;52:e282-94.
Schultheiss M, Härtig F, Spitzer MS, et al. Intravenous thrombolysis in acute central retinal artery occlusion—a prospective interventional case series. PLoS One 2018;13:e0198114.
Préterre C, Godeneche G, Vandamme X, et al. Management of acute central retinal artery occlusion: intravenous thrombolysis is feasible and safe. Int J Stroke 2017;12:720-23.
Nedelmann M, Graef M, Weinand F, et al. Retrobulbar spot sign predicts thrombolytic treatment effects and etiology in central retinal artery occlusion. Stroke 2015;46:2322-4.
Hattenbach LO, Kuhli-Hattenbach C, Scharrer I, Baatz H. Intravenous thrombolysis with low-dose recombinant tissue plasminogen activator in central retinal artery occlusion. Am J Ophthalmol 2008;146:700-6.
Kattah JC, Wang DZ, Reddy C. Intravenous recombinant tissue-type plasminogen activator thrombolysis in treatment of central retinal artery occlusion. Arch Ophthalmol 2002;120:1234-6.
Mames RN, Shugar JK, Levy N, Brasington A, Margo CE. Peripheral thrombolytic therapy for central retinal artery occlusion. CRAO Study Group. Arch Ophthalmol 1995;113:1094.
Schumacher M, Schmidt D, Jurklies B, et al. Central retinal artery occlusion: local intra-arterial fibrinolysis versus conservative treatment, a multicenter randomized trial. Ophthalmology 2010;117:1367-75.e1.
Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. Am J Ophthalmol 2005;140:376-91.
Advertisement
Supported by
Judge Won’t Delay Trump’s Criminal Trial to Wait for Immunity Ruling
The former president had asked the judge to push back his Manhattan criminal trial, slated to begin April 15, until after the Supreme Court decides whether he is immune from prosecution.
- Share full article

By Ben Protess and William K. Rashbaum
The judge overseeing Donald J. Trump’s criminal case in Manhattan rejected his last-ditch bid to delay a trial beyond April 15, removing on Wednesday one of the final obstacles to the first prosecution of a former American president.
Mr. Trump, who is accused of covering up a sex scandal surrounding the 2016 presidential campaign, had asked the judge to delay the trial until after the Supreme Court rules on whether he is immune from prosecution over official acts he took while president. That issue arose in another of his criminal cases, and the Supreme Court is expected to hear arguments this month, but might not rule until June.
The judge in the Manhattan case, Juan M. Merchan, ruled that his trial did not need to wait for the Supreme Court. He denied Mr. Trump’s effort as “untimely,” ruling that he had failed to request the delay by a legal deadline.
The judge said the request’s timing — just weeks before the trial was set to start — also raised “real questions about the sincerity and actual purpose of the motion.”
He added: “The circumstances, viewed as a whole, test this court’s credulity.”
Mr. Trump’s effort was his latest bid to delay his four criminal cases, which are unfolding against the backdrop of his campaign to regain the White House. If Mr. Trump can stall the cases until Election Day, and he wins the presidency, they would likely grind to a halt.
Some of his tactics have paid off. In Florida, where Mr. Trump is accused of mishandling classified documents, a Trump-appointed judge has yet to finalize a trial date. And in Washington, D.C., where a federal special counsel has accused Mr. Trump of plotting to overturn the 2020 election, the Supreme Court has paused the trial while it considers the immunity issue.
In the Manhattan case, Mr. Trump secured a three-week delay, from late March to mid-April, after new investigative records emerged. But Mr. Trump wanted to push back the trial further. His lawyers sought a 90-day delay, or an outright dismissal, blaming prosecutorial misconduct for the last-minute cache of documents.
That accusation carried little weight with Justice Merchan, who recently confirmed the April 15 start date and rebuked Mr. Trump’s legal team.
Mr. Trump’s lawyers, Todd Blanche and Susan R. Necheles, declined to comment.
The Manhattan case stems from a hush-money deal struck with a porn star, Stormy Daniels, in the final days of the 2016 campaign. In a 34-count indictment last year, the Manhattan district attorney, Alvin L. Bragg, accused Mr. Trump of falsifying business records related to the payoff.
Mr. Trump, the presumptive Republican nominee for president, has denied the affair and the charges, which he claims are politically motivated.
The effort to drag out the Manhattan case until after the Supreme Court addressed the immunity issue seemed particularly far-fetched.
The Manhattan district attorney’s office noted that Mr. Trump’s lawyers filed the request only 17 days before the trial was initially scheduled to start, months after they filed other pretrial motions.
Mr. Trump’s lawyers, Justice Merchan noted, had already argued the same issue in federal court in Washington and yet had failed to raise it with him.
The judge also appeared skeptical that the immunity claim had direct bearing on the charges brought by Mr. Bragg.
At a hearing in February, Justice Merchan said that “the issue of the state proceedings I don’t believe is for the Supreme Court.”
In a footnote to Wednesday’s decision, Justice Merchan wrote that Mr. Trump “does not appear to raise a claim of presidential immunity” that applies to the cover-up of the sex scandal.
Ben Protess is an investigative reporter at The Times, writing about public corruption. He has been covering the various criminal investigations into former President Trump and his allies. More about Ben Protess
William K. Rashbaum is a senior writer on the Metro desk, where he covers political and municipal corruption, courts, terrorism and law enforcement. He was a part of the team awarded the 2009 Pulitzer Prize for Breaking News. More about William K. Rashbaum
Our Coverage of the Trump Hush-Money Case
The manhattan district attorney has filed charges against former president donald trump over a hush-money payment to a porn star on the eve of the 2016 election..
Taking the Case to Trial: Trump is all but certain to become the first former U.S. president to stand trial on criminal charges after a judge denied his effort to delay the proceeding and confirmed it will begin on April 15 .
Implications for Trump: As the case goes to trial, the former president’s inner circle sees a silver lining in the timing. But Trump wouldn’t be able to pardon himself should he become president again as he could if found guilty in the federal cases against him.
Michael Cohen: Trump’s former fixer was not an essential witness in the former president’s civil fraud trial in New York that concluded in January. But he will be when he takes the stand in the hush-money case .
Stormy Daniels: The chain of events flowing from a 2006 encounter that the adult film star said she had with Trump has led to the brink of a historic trial. Here's a look inside the hush-money payout .
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Judge expands Trump’s gag order after ex-president’s social media posts about judge’s daughter
Former President Donald Trump speaks during a press conference at 40 Wall Street after a pre-trial hearing at Manhattan criminal court, Monday, March 25, 2024, in New York. A New York judge has scheduled an April 15 trial date in former President Donald Trump’s hush money case. Judge Juan M. Merchan made the ruling Monday.(AP Photo/Frank Franklin II)
- Copy Link copied
NEW YORK (AP) — The judge in Donald Trump’s April 15 hush-money criminal trial declared his family off-limits to the former president’s rancor on Monday, expanding a gag order days after Trump assailed his daughter and made false claims about her on social media.
Manhattan Judge Juan M. Merchan amended a week-old ban on Trump making public statements about witnesses, jurors and others connected with the case after the presumptive Republican nominee lashed out at Loren Merchan, a Democratic political consultant in several posts on his Truth Social platform.
Trump is still free to criticize Merchan and another key figure in the case, Manhattan District Attorney Alvin Bragg, an elected Democrat who’s leading the hush-money prosecution. But under the revised gag order, the D.A.'s family is now off-limits from his rhetoric, too.
“This pattern of attacking family members of presiding jurists and attorneys assigned to his cases serves no legitimate purpose,” Merchan wrote. “It merely injects fear in those assigned or called to participate in the proceedings that not only they, but their family members as well, are ‘fair game,’ for Defendant’s vitriol.”
A violation could result in Trump being held in contempt of court, fined or even jailed.
Trump’s lawyer, Susan Necheles, declined comment. A spokesperson for the district attorney’s office also declined comment.
Trump’s hush-money case, one of four criminal cases against him , centers on allegations that he falsely logged payments to his former lawyer Michael Cohen as legal fees when they were for Cohen’s work covering up negative stories about Trump during the 2016 campaign. That included $130,000 Cohen paid porn actor Stormy Daniels on Trump’s behalf so she wouldn’t publicize her claim of a sexual encounter with him years earlier.
Trump pleaded not guilty last April to 34 counts of falsifying business records , a felony punishable by up to four years in prison, though there is no guarantee that a conviction would result in jail time. He denies having sex with Daniels and his lawyers have said that the payments to Cohen were legitimate legal expenses, not part of any coverup.
Trump touched off a firestorm last Wednesday — the day after the original gag order was issued — when he suggested on Truth Social, without evidence, that Merchan’s rulings were swayed by his daughter’s political consulting interests and wrongly claimed that she had posted a photo on social media showing him behind bars.
Trump complained that the judge was “wrongfully attempting to deprive me of my First Amendment Right to speak out against the Weaponization of Law Enforcement” by Democratic rivals and that Loren Merchan “makes money by working to ‘Get Trump.’”
Trump’s posts put Merchan in an extraordinary position as a judge and a father. Just two weeks before jury selection in the historic first-ever criminal trial of a former president, Trump’s lawyers and prosecutors wrangled in a series of court filings over the bounds of the original gag order and whether Trump had overstepped them.
“It is no longer just a mere possibility or a reasonable likelihood that there exists a threat to the integrity of the judicial proceedings,” Merchan concluded Monday. “The threat is very real. Admonitions are not enough, nor is reliance on self-restraint.”
Merchan responded after prosecutors asked him Friday to “clarify or confirm” the scope of the gag order and to direct Trump to “immediately desist from attacks on family members.”
Assistant District Attorney Joshua Steinglass implored Merchan to “make abundantly clear” to Trump that the gag order protects the judge’s family, Bragg’s family and the family members of all other individuals it covers. He urged Merchan to warn Trump “that his recent conduct is contumacious and direct him to immediately desist.”
Trump’s lawyers fought the gag order and its expansion, citing constitutional concerns about restricting Trump’s speech further while he’s campaigning for president and fighting criminal charges.
On Monday, they said they would soon ask again for Merchan to step aside from the case — promising a court filing in the coming days seeking his recusal based on what they said were “changed circumstances and newly discovered evidence.”
Merchan refused the defense’s demands to exit the case last year when they first made an issue of his daughter’s consulting work and questioned $35 worth of donations he’d made to Democratic causes during the 2020 campaign, including $15 to Biden.
Merchan said then that a state court ethics panel found Loren Merchan’s work had no bearing on his impartiality. He ruled last September that he was certain of his “ability to be fair and impartial” and that Trump’s lawyers had “failed to demonstrate that there exists concrete, or even realistic” reasons for recusal.
Trump’s original gag order, issued last Tuesday, had barred him from either making or directing other people to make public statements on his behalf about jurors or potential witnesses in the hush-money trial, such as his lawyer-turned-nemesis Michael Cohen and porn star Stormy Daniels.
The order, echoing one in Trump’s Washington, D.C., election interference criminal case, also prohibits any statements meant to interfere with or harass the court’s staff, prosecution team or their families. Those prohibitions still apply, along with the newly minted ban on comments about Merchan’s and Bragg’s families.
Merchan, in expanding the gag order, also warned Trump he’ll forfeit his right to see the names of jurors — which are otherwise being kept from the public — if he engages in conduct that threatens their safety or integrity.
“Again, all citizens called upon to participate in these proceedings, whether as a juror, a witness or in some other capacity, must now concern themselves not only with their own personal safety, but with the safety and the potential for personal attacks upon their loved ones,” Merchan wrote. “That reality cannot be overstated.”
Trump special counsel fires back at Cannon order that could disrupt case
Prosecutor says judge’s legal premise on presidential records act ‘is wrong,’ urges her to rule in classified documents case so he can appeal.
Special counsel Jack Smith warned the judge overseeing Donald Trump ’s classified documents case that she is pursuing a legal premise that “is wrong” and said he would probably appeal to a higher court if she rules that a federal records law can protect the former president from prosecution.
In a late-night legal filing Tuesday, Smith’s office pushed back hard against an unusual instruction from U.S. District Judge Aileen M. Cannon — one that veteran national security lawyers and former judges have said badly misinterprets the Presidential Records Act and laws related to classified documents.
Smith’s filing represents the most stark and high-stakes confrontation yet between the judge and the prosecutor, illustrating the extent to which a ruling by Cannon that legitimizes the PRA as a defense could eviscerate the historic case, one of four Trump is facing as he again runs for president. The special counsel repeatedly said that he probably would appeal such a ruling, potentially delaying the classified documents trial well beyond November’s presidential election.
Last month, Cannon ordered defense lawyers and prosecutors in the case to submit hypothetical jury instructions based on two different, and very much contested, readings of the PRA.
In response, Smith said Cannon was pursuing a “fundamentally flawed legal premise” that the law somehow overrides Section 793 of the Espionage Act, which Trump is accused of violating by stashing hundreds of classified documents at Mar-a-Lago, his Florida home and private club, after his presidency ended.
“That legal premise is wrong, and a jury instruction for Section 793 that reflects that premise would distort the trial,” Smith wrote. The Presidential Records Act, he said, “should not play any role at trial at all.”
Sign up for The Trump Trials, our weekly newsletter on Trump's four criminal cases
Smith’s filing was unusual in that prosecutors rarely seek direct confrontations with judges overseeing their case; it makes clear he sees significant potential danger for his prosecution from Cannon’s approach to the PRA issue. How Cannon, a Trump nominee who has been on the bench since late 2020, responds will be critical.
If she rules against Smith, he could appeal. If she retreats from the disputed legal premise, the issue could fade into the background as she decides a pretrial hearing schedule and sets a trial date.
Cannon has been slow to make a number of decisions, even as prosecutors have urged her to move quickly, and it’s possible that on this issue too, she simply takes her time. In the meantime, Trump is scheduled to stand trial starting April 15 in a New York state case accusing him of falsifying business records to cover up a hush money payment during the 2016 election. Two other criminal cases , related to Trump’s alleged efforts to block Joe Biden’s 2020 election victory, are mired in pretrial proceedings and appeals.
Tuesday night’s filing urged Cannon to rule quickly on whether the Presidential Records Act is relevant to the case, so that prosecutors can appeal any such determination to a higher court before the Florida trial, which is delayed from its original late May start date but has not yet been rescheduled.
Smith has said the records act has nothing to do with the national security crimes Trump is accused of committing — a view backed by many legal experts, who have said a ruling in Trump’s favor would open the door for future presidents to claim personal ownership of national defense secrets. Waiting until the trial is underway to rule on the issue, Smith warned, could doom the prosecution’s case before it ever gets to a jury.
“If the Court were to defer a decision on that fundamental legal question it would inject substantial delay into the trial and, worse, prevent the government from seeking review before jeopardy attaches,” he wrote.
Even as he questioned the premise of Cannon’s order, Smith complied, offering proposed jury instructions for the two legal scenarios she outlined. Smith’s proffered language, however, was couched in a kind of lawyerly attack on Cannon’s legal analysis.
“[E]ven if an individual holds a security clearance and has a need to know classified information, the individual’s possession of the classified information is unauthorized if the individual removes the classified information from a secure facility or possesses the information outside of a secure facility,” Smith wrote in the proposed jury instruction.
“I instruct you, however, that, as to a former President, even if he lacks a security clearance, lacks a need to know classified information, and stores information outside of a secure facility, he is authorized to do so if the classified information is contained within a ‘personal record,’ within the meaning of the Presidential Records Act (PRA).”
Trump has pleaded not guilty to 32 charges of violating the Espionage Act, with each count corresponding to a specific classified document that he is alleged to have retained after leaving office, as well as eight additional charges of obstructing government efforts to retrieve the materials. His lawyers argue that the former president had the authority under the PRA to declare even highly classified documents to be his personal records and property.
Prosecutors and legal experts have said such claims badly misstate the law, which says that presidential records belong to the public and are to be turned over to the National Archives and Records Administration at the end of a presidency. Legal experts say Cannon’s focus on jury instructions seems odd at this stage of the process because a trial is not imminent and the judge still has a number of decisions to make in the pretrial proceedings before the instructions are relevant. They also say the premise of Cannon’s orders indulged some mangled interpretations of laws that have been pushed by Trump’s lawyers and supporters.
Trump’s team said in its own late-night filing that Cannon’s assignment is consistent with Trump’s position that the “prosecution is based on official acts” he took as president — not illegal retention of materials.
The judge told lawyers to write jury instructions for two legal interpretations. Legal experts said she could use those instructions to help inform her eventual ruling on a request that Trump made to dismiss the case because the PRA allowed him to designate any presidential record as personal.
In one scenario, Cannon asked them to craft jury instructions that assume the PRA allows presidents to designate any documents as personal at the end of a presidency — which is what Trump’s legal team has argued he had the authority to do. She then said they should also write separate jury instructions predicated on the idea that jurors would be able to determine which of the documents Trump is accused of illegally retaining are personal and which are presidential.
The government has said it is the Espionage Act — not the PRA — that guards classified materials. Trump is not charged with violating the PRA, and prosecutors said throughout their filing that the PRA should not be in those instructions.
“The PRA’s distinction between personal and presidential records has no bearing on whether a former President’s possession of documents containing national defense information is authorized under the Espionage Act, and the PRA should play no role in the jury instructions,” Smith wrote. “Indeed, based on the current record, the PRA should not play any role at trial at all.”
In their proposed jury instructions, Trump’s attorneys leaned into their argument that the former president had the ultimate authority to determine the designation of the documents that he is accused of illegally retaining.
“You heard evidence during the trial that President Trump exercised that authority, at times verbally and at times without using formal procedures, while he was President,” Trump’s legal team wrote in the hypothetical jury instructions . “I instruct you that those declassification decisions are examples of valid and legally appropriate uses of President Trump’s declassification authority while he was President of the United States.”
Cannon held a hearing over a month ago to determine a new date for the classified documents trial. Prosecutors sought a date in early July, while Trump’s lawyers asked to wait until after the election or to start in August at the earliest. The judge has not yet ruled.
She issued her jury instruction order a few days after a different hearing, held March 14, at which she heard arguments on two of Trump’s motions to toss out the case.
One motion said the case should be dismissed because the PRA meant that Trump could simply declare highly classified documents to be his personal property and keep them at Mar-a-Lago. Cannon has not yet ruled on that motion.
Hours after the hearing, she rejected Trump’s other motion to dismiss. It argued that the Espionage Act , which has been used for decades to convict others of improperly possessing classified documents, was too vaguely worded to be used in his indictment.
More on the Trump classified documents indictment
The latest: Federal prosecutors have asked a judge to push back Donald Trump’s classified documents trial in Florida to July 8, probably after the Supreme Court rules on his claim of presidential immunity, while Trump’s lawyers are trying again to delay the trial until after the presidential election.
The case: The criminal investigation looks into whether Trump took government secrets with him after he left the White House and obstructed a subsequent investigation. Trump has pleaded not guilty . Here’s what to know about the classified documents case .
The charges: Trump faces 40 separate charges in the documents case. Read the full text of the superseding indictment against Trump and our top takeaways from the indictmen t .
Can Trump still run for president? While it has never been attempted by a candidate from a major party before, Trump is allowed to run for president while under indictment in four cases — or even if he is convicted of a crime. Here’s how Trump’s indictment could affect the election .
- Trump defends Judge Cannon in fight over classified documents trial April 4, 2024 Trump defends Judge Cannon in fight over classified documents trial April 4, 2024
- Judge Cannon shoots down Trump’s presidential records act claim April 4, 2024 Judge Cannon shoots down Trump’s presidential records act claim April 4, 2024
- Jack Smith puts Judge Aileen Cannon on notice April 3, 2024 Jack Smith puts Judge Aileen Cannon on notice April 3, 2024

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(8); 2023 Aug
- PMC10427890

Post-Stroke Recrudescence: A Case Report and Literature Review
Manogna sagiraju.
1 Internal Medicine, Kempegowda Institute of Medical Sciences, Bangalore, IND
Raghav Prasad
2 Neurology, Kempegowda Institute of Medical Sciences, Bangalore, IND
Milenko Lazarevic
3 Internal Medicine, Swedish Covenant Hospital, Chicago, USA
Post-stroke recrudescence (PSR) is a clinical entity characterized by the acute transient recurrence of previously recovered focal stroke deficits. Various names have been used to describe PSR, which further complicates its diagnosis. Increased awareness of this condition is crucial for preventing inappropriate management and unnecessary testing. Mechanisms proposed for PSR include altered drug response in diseased brain areas and immune activation due to a compromised blood-brain barrier (BBB). Patients with PSR have a distinct vascular risk profile and fewer cardiovascular complications than those with transient ischemic attacks (TIAs). Accurate differentiation of PSR from other conditions that mimic stroke is essential for its appropriate management. Misdiagnosis may lead to unnecessary procedures and prolonged hospitalization. This article presents the case of a 56-year-old female with multiple episodes of PSR that were initially misdiagnosed in the emergency department. The patient had a history of hypertension and ischemic stroke, and her episodes of PSR were often triggered by elevated blood pressure. Future studies should focus on developing validated prediction scores to guide recurrent stroke workup. Enhancing awareness and understanding of PSR can optimize resource allocation and improve patient outcomes.
Introduction
Post-stroke recrudescence (PSR) is an under-recognized clinical entity defined as an acute transient recurrence of previous but recovered focal stroke deficits. It is characterized by the following criteria: transient worsening of residual post-stroke focal neurologic deficits or transient recurrence of previous stroke-related focal neurologic deficits, identifiable stressors, chronic stroke on brain imaging, absence of acute lesions on diffusion-weighted imaging (DWI), and an unlikely alternative diagnosis [ 1 ].
There are several names given to the same clinical entity of PSR, such as recrudescence of old stroke deficits (ROSD) [ 2 ], differential awakening [ 3 ], re-emergence [ 4 ], anamnestic recall [ 5 ], exacerbation of focal neurological deficits [ 6 ], locus minoris resistentiae [ 7 ], and “metabolic insult causing reexpression of old stroke” [ 8 ], which adds to further confusion in terms of diagnosing the condition in clinical practice. Here, we chose PSR because it is concise and clear.
PSR is a relatively common phenomenon, affecting one in 10 patients with transient neurological attacks. In one study, although patients with PSR and transient ischemic attack (TIA) had similar baseline vascular risk factors, patients with PSR had significantly fewer cardiovascular complications during the 90-day follow-up than those with TIA [ 2 ]. Therefore, it is essential to differentiate it from mimics, such as acute stroke, TIA, migraine, and seizure, as these conditions have different management protocols.
The patient in the present case had several episodes of PSR, which were diagnosed differently each time in the emergency department. She also appeared to have elevated blood pressure as a trigger for episodes of PSR. Increased awareness of this condition might have prevented inappropriate diagnosis and testing of this patient.
Case presentation
A 56-year-old Caucasian female with a past medical history of Addison’s disease, stroke, migraine, and hypertension presented with right-sided numbness and weakness.
Her last known well was at 09:00 on that day when she developed numbness in her right lower extremity, which progressed to her right upper extremity and the right side of the face. This was followed by weakness in the same region and slurring of the speech. With these symptoms, she presented to the emergency department at 15:30 am, which made her ineligible for thrombolytic therapy. The patient denied any loss of consciousness, drowsiness, confusion, headache, vision disturbances, vomiting, or fever.
The patient had a documented history of Addison's disease for which she was receiving hydrocortisone. She also had a history of two TIAs in 2016 and an ischemic stroke of the left middle cerebral artery (L MCA) in May 2017, which presented with right-sided weakness and paresthesia.
Since the stroke, she has reported multiple episodes that presented with symptoms similar to those of her prior stroke. The symptoms were equal or inferior in severity as compared to the initial stroke. During these episodes, the patient presented with elevated blood pressure, and following its reduction, her symptoms spontaneously resolved within a couple of hours. These episodes occurred on the following dates: August 15, 2017, May 30, 2018, August 31, 2021, July 26, 2022, and November 11, 2022. The patient's hypertension was treated with enalapril.
Upon arrival at the emergency department, the patient's blood pressure was significantly elevated at 198/110 mmHg and her pulse rate was 110 bpm. The patient had a National Institutes of Health Stroke Scale (NIHSS) of 8. A neurological examination revealed a slight slurring of speech, with the rest of her higher mental functions being normal. Cranial nerve examination revealed facial asymmetry, reduced prominence of the right nasolabial fold, and weakness in the right trapezius and sternocleidomastoid muscles. Motor examination demonstrated reduced power on the right side, with the right upper extremity graded at 3/5 and the right lower extremity graded at 2/5, compared to a normal 5/5 strength on the left side. Reflexes were 2+ in all extremities, and Babinski and Hoffmann's signs were absent. Sensory examination revealed decreased sensation to light touch and vibration on the right side of the body, and hemineglect was absent. The patient exhibited a normal finger-nose-finger test and heel-shin test on the left side, whereas weakness precluded performing these tests on the right side. Right-sided pronator drift was observed. The results of the remaining systemic examinations were unremarkable.
Non-contrast CT of the head demonstrated no signs of acute hemorrhage and showed severe encephalomalacia of the left hemisphere, consistent with a previous L MCA stroke (Figure (Figure1 1 ).

Laboratory investigations included a comprehensive metabolic panel and a complete blood count, which yielded normal results. Electrocardiography (EKG) showed normal sinus rhythm, and chest X-ray appeared normal. Two-dimensional echocardiography (2D echo) did not reveal any significant abnormalities.
Brain MRI showed no evidence of acute infarction but revealed signs of old stroke, that is, hypointensity on fluid-attenuated inversion recovery (FLAIR) and DWI (Figures (Figures2, 2 , ,3) 3 ) with correlates on ADC in the left hemisphere. Electroencephalogram (EEG) demonstrated a normal study with no epileptic foci.

MRI FLAIR: magnetic resonance imaging with fluid-attenuated inversion recovery

MRI DWI: magnetic resonance imaging with diffusion-weighted imaging; ACA: anterior cerebral artery; MCA: middle cerebral artery: PCA: posterior cerebral artery
Upon admission, the patient was initiated on secondary stroke prevention measures and administered a combination of aspirin and dipyridamole. This caused the patient to complain of severe headache. With the patient’s history of migraine, the medication chart was cross-referenced, and the combination drug was stopped and replaced with plain aspirin. The patient reported relief from headaches after discontinuation of the combination drug. Overnight, she experienced complete resolution of neurological symptoms. The patient was subsequently discharged from the hospital.
Several mechanisms have been proposed for PSR. First, there may be altered drug uptake, distribution, and/or metabolism in diseased or abnormal areas of the brain, making the brain more susceptible to sedatives, especially gamma-amino butyric acid (GABA) receptor agonists [ 6 ]. Second, some redundancies in neuronal numbers or circuitry that characterizes the normal state are lost focally in a diseased brain. Even minimal impairment of the remaining functioning neurons may produce an exaggerated response [ 9 ]. Third, another theory based on an animal model states that after an episode of stroke, exposure to central nervous system (CNS) antigens due to compromise of the blood-brain barrier (BBB) or release of antigen into the bloodstream leads to CNS-specific lymphocytes. Later, when the body produces significant systemic inflammation in response to a systemic stressor, CNS-specific lymphocytes can be activated. This can lead to stroke-like symptoms localized to the area of the previous insult [ 5 ].
Certain demographic characteristics were associated with a higher risk of PSR, including being female, being African American, or identifying as belonging to "other" races. Patients with recrudescence also had higher frequencies of diabetes, dyslipidemia, smoking, and more severe neurologic deficits at the time of the initial stroke, indicating that these comorbidities and the severity of stroke may increase vulnerability to PSR [ 1 ].
PSR is characterized by the inability of the brain to adapt to systemic stressors and is always preceded by such stressors. By contrast, only 20% of TIA cases have an identified stressor [ 2 ]. Currently, stressors are categorized into five main groups: systemic inflammation (e.g., fever and infections), hypotension, metabolic factors (e.g., hyponatremia and hypokalemia), chemical insults (benzodiazepines, sedatives, and opioids), and physiological stress (insomnia, fatigue, and excessive sun exposure).
Notably, in the case of the patient discussed here, there appeared to be a correlation between elevated blood pressure and the occurrence of episodes of PSR. Further research is needed to better comprehend the specific stressors and their relationships with PSR, including investigating the potential associations between elevated blood pressure and the occurrence of PSR episodes.
Patients with PSR typically have a history of similar episodes. Thus, a comprehensive history that includes a detailed summary of the symptoms of the patient during the initial stroke is paramount for effectively managing such cases. This becomes especially relevant in cases like that presented here, where the patient's prior history of TIA further complicates the diagnostic process. This information can help determine the typical presentation of PSR symptoms in the patient, which can aid in the diagnosis. In addition, understanding which triggers are more likely to induce symptoms can guide recommendations for the patient to avoid such triggers in the future. Inaccurate identification of PSR as a TIA can lead to unwarranted modifications in patient management. It is imperative to prioritize preventive measures and prompt treatment of infections, hyponatremia, and other medical complications associated with PSR while also exercising caution in the use of benzodiazepines. It is imperative to prioritize preventive measures and prompt treatment of infections, hyponatremia, and other medical complications associated with PSR, while also exercising caution in the use of benzodiazepines.
In this particular patient, thrombolytic treatment was appropriately deferred because she presented outside the thrombolytic window. Fortunately, this decision was favorable. Within a comprehensive stroke center, it has been observed that 21% of patients who received intravenous tissue plasminogen activator (IV tPA) were subsequently determined not to have experienced a stroke [ 10 ]. Although these patients did not exhibit worsened outcomes, it is worth noting that individuals with PSR have a distinct vascular risk profile compared with other conditions that mimic stroke symptoms. Therefore, it is essential to conduct studies that investigate the potential adverse consequences of incorrect initial diagnosis and management of PSR. Given the urgent nature of stroke cases, which necessitates prompt judgment and decision-making, there is a demand for clinical decision-making tools that can assess the likelihood of PSR in patients.
Moreover, such misdiagnoses may lead to a cascade of costly procedures, such as vascular imaging, cardiac ultrasound, Holter monitoring, and blood tests, which not only increases expenses but also prolongs the patient's hospitalization.
In clinical practice, we differentiate TIA from PSR based on the presence of deficits, which are new compared to the old stroke. Data are required on the accuracy of this method as, theoretically, there can be overlap scenarios, where TIA can present with same deficits.
Enhanced awareness regarding the temporal resolution of symptoms and anticipated duration of hospitalization has the potential to optimize resource allocation. This can be facilitated by stressing the differentials to consider when a patient presents with stroke-like symptoms and not only on the recommended initial imaging and treatment of stroke, which will lead to improved outcomes in such patients. Future studies are needed to generate a validated predictor score for this unique phenomenon to identify who may or may not benefit from a recurrent stroke work-up.
Conclusions
PSR is a frequently encountered but often overlooked clinical entity characterized by an acute recurrence of previously resolved stroke deficits. This case report highlights the challenges in diagnosing and managing PSR and the need for increased awareness among healthcare professionals. The patient presented with multiple episodes of PSR, which were initially misdiagnosed in the emergency department, leading not only to unnecessary testing and confusion regarding the appropriate management protocols but also to prescribing a medication that triggered her other coexisting condition, leading to increased discomfort for the patient. Differentiating PSR from other conditions that mimic stroke, such as TIAs, is crucial to avoid inappropriate interventions and provide targeted preventive measures. Understanding the mechanisms underlying PSR, including altered drug responses and immune activation, can aid in the development of effective treatment strategies.
Moreover, the accurate identification of PSR can have important implications for healthcare resource allocation. Misdiagnosis can lead to unnecessary procedures, prolonged hospitalization, and increased costs. By improving the awareness of PSR and its distinct vascular risk profile, healthcare providers can optimize patient care, prioritize preventive measures, and avoid unnecessary interventions. Future research efforts should focus on developing validated prediction scores to identify patients at risk of PSR and to guide appropriate diagnostic workup. Clinical decision-making tools can aid in assessing the likelihood of PSR and support prompt and accurate diagnoses. Ultimately, enhancing the understanding and recognition of PSR will contribute to improving patient outcomes, resource allocation, and cost-effective healthcare delivery.
Acknowledgments
Manogna Sagiraju and Raghav Prasad contributed equally to the work and should be considered co-first authors.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study

IMAGES
VIDEO
COMMENTS
CASE 1. A 20 year old man with no past medical history presented to a primary stroke center with sudden left sided weakness and imbalance followed by decreased level of consciousness. Head CT showed no hemorrhage, no acute ischemic changes, and a hyper-dense basilar artery. CT angiography showed a mid-basilar occlusion.
Case presentation. A 66-year-old man presented to the hospital with signs of left-sided weakness. The patient had a background of chronic obstructive pulmonary disease (COPD), atrial fibrillation and had one previous ischaemic stroke, producing left-sided haemiparesis, which had completely resolved.
In this retrospective study, the case records of 1,287 stroke patients admitted to Al-basher Hospital during a three-year period were reviewed. The stroke patient cohort included 60% men and 40% ...
Abstract. Increasing evidence reports a greater incidence of stroke among patients with Coronavirus disease 2019 (COVID-19) than the non-COVID-19 population and suggests that SARS-CoV-2 infection represents a risk factor for thromboembolic and acute ischemic stroke. Elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events, and advanced age ...
Alzheimer's & Dementia Child Neurology Epilepsy & Seizures Headache & Pain Imaging & Testing Movement Disorders MS & Immune Disorders Neuromuscular Sleep Stroke TBI. Issue Index . 2024 2023 2022 2021 2020 2019 2018 2017 2016 2015 2014 2013 2012 2011 2010 2009 2008 2007 2006 2005. News; Podcasts; Case Reports; Resources . Clinical Care Tools ...
This case report demonstrates the typical clinical presentation of an ICH and demonstrates a multimodal approach that involves not only the standard medical therapy of intracerebral hemorrhage, but also a combination of the various minimally invasive surgical, mechanical and thrombolytic methods in order to safely access and visualize both ...
Presentation of Case. Dr. Scott B. Silverman: A 68-year-old man was admitted to this hospital because of worsening confusion. The patient had a history of hypertension and coronary artery disease ...
Case report. We present a case of a 69 - old patient admitted in the Neurological Ward of "St. George Hospital in Plovdiv in 2015, Bulgaria with right hemiparesis due to ischemic stroke in the basin of the left middle cerebral artery. This was a patient with sensory aphasia and paralysis facials in the right side.
Case. A 44-year-old man with a history of migraines with aura presented with very brief right-sided weakness and a "pins and needles" sensation. The event, which lasted no more than 10 seconds in his estimation and affected his right face, arm, and leg. He staggered because of the momentary hemiparesis, which quickly resolved.
We hereby, report a case of a young adult with large-vessel occlusion due to post-strangulation internal CAD. This case highlights the importance of raising awareness of the possibility of CAD in the presence of any focal neurologic deficit due to strangulation.
The patient was admitted as a case of suspected stroke in the young for workup. Basic laboratory tests, including complete blood count, electrolytes, renal function, liver function, and inflammatory markers, were normal. Electrocardiography showed normal sinus rhythm. His HbA1c was 8% (normal range: 4.80-5.90%),
Stroke should be considered a cause of syncope when persistent and significant neurological changes occur before the episode or during the recovery period. WS, also known as lateral medullary syndrome, is the most prevalent posterior ischaemic stroke syndrome. It commonly results from occlusion of the PICA or one of its branches.
purpose of this case report is to review background, treatments, physical therapy interventions and outcomes of a patient with a sub-acute stroke, treated in an inpatient setting. Case Description: The patient was a 70 year old male with a severe ischemic CVA following surgery to repair an abdominal aortic aneurysm.
This report presents a rare case of a patient admitted to the emergency department because of unilateral paresthesia and clinical suspicion of acute ischemic stroke. Case presentation A 69-year-old Caucasian male patient was examined at the emergency department because of numbness in the left upper and lower extremities.
Background In acute ischemic stroke, diffusion weighted imaging (DWI) shows hyperintensities and is considered to indicate irreversibly damaged tissue. We present the case of a young stroke patient with unusual variability in the development of signal intensities within the same vessel territory. Case presentation A 35-year-old patient presented with symptoms of global aphasia and hypesthesia ...
Introduction Pseudobulbar affect, or emotional dysregulation, commonly occurs following stroke. However, it is frequently missed in cases involving the cerebellum, resulting in a lack of treatment, which can directly impact stroke rehabilitation. Case presentation A 63-year-old Caucasian female with no history of mood disorders presented with gait instability, dysarthria, and right sided ...
Background Intimal sarcomas are an extremely rare type of primary cardiac malignancy. They most commonly present with symptoms of cardiac dysfunction. We present a case of intimal sarcoma identified without any cardiac signs or symptoms. Cardiac sarcomas historically carry a very poor prognosis. Presentation A 57-year-old man presented with a sudden onset of left limb weakness and ...
A PFO has been demonstrated in 10%-26% of healthy adults. 14 In young patients who have had a cryptogenic stroke, however, the prevalence is thought to be much higher, for example, 40% in one study. 15 It is thought that a PFO allows microemboli to pass into the systemic circulation leading to a stroke.
feedback form, stroke audit report/form, time tracker, tracking worksheet, tracking form. You will need to dig into various parts of the patient medical record to find information about the patient to include on this form. You may have a separate form specifically for EMS. a. This case review report can be shared with the following staff: i ...
Exclusion Criteria (contraindications) 3-4.5 hr treatment window. Select all that apply: C1: Elevated blood pressure (systolic > 185 mm Hg or diastolic > 110 mm Hg) despite treatment. C2: Recent intracranial or spinal surgery or significant head trauma, or prior stroke in previous 3 months.
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater ...
TAK has been described worldwide, with an incidence of 0.2-2.6 new cases per million people each year. However, these studies are mainly limited to Asian and Western countries. 6-8 Rarity of the disease and a lack of awareness of the condition are the remaining challenges to the early diagnosis and treatment of the cases. 9 In the case presented here, we describe a patient with an ischemic ...
Central retinal artery occlusion (CRAO), a type of acute retinal arterial ischemia, analogous to an ocular stroke, is a medical emergency that warrants immediate diagnosis and treatment. CRAO usually presents with sudden, painless, monocular vision loss. Ipsilateral carotid artery disease is an important associated finding in these patients.
Post-Stroke Recrudescence: A Case Report and Literature Review Manogna Sagiraju , Raghav Prasad , Milenko Lazarevic 1 . In ter alM d ic ,Kmpgow s uf S B ND2 y ... Open Access Case 1 2 3 Report DOI: 10.7759/cureus.43461 How to cite this article Sagiraju M, Prasad R, Lazarevic M (August 14, 2023) Post-Stroke Recrudescence: A Case Report and ...
The push for a quick decision on one of the former president's most far-fetched claims is an unusual and risky move in a case Judge Aileen Cannon has allowed to become bogged down. Supporters of ...
April 3, 2024. The judge overseeing Donald J. Trump's criminal case in Manhattan rejected his last-ditch bid to delay a trial beyond April 15, removing on Wednesday one of the final obstacles to ...
Abstract. Ischaemic stroke as the initial presentation of systemic malignancy is reported infrequently and is characterised by ischaemic lesions that exceed the vascular territory of a single vessel. There is also a high rate of early stroke recurrence. Several pathophysiological mechanisms are known to cause cerebrovascular complications in ...
Trump's hush-money case, one of four criminal cases against him, centers on allegations that he falsely logged payments to his former lawyer Michael Cohen as legal fees when they were for Cohen's work covering up negative stories about Trump during the 2016 campaign.That included $130,000 Cohen paid porn actor Stormy Daniels on Trump's behalf so she wouldn't publicize her claim of a ...
8 min. Special counsel Jack Smith warned the judge overseeing Donald Trump 's classified documents case that she is pursuing a legal premise that "is wrong" and said he would probably appeal ...
Post-stroke recrudescence (PSR) is a clinical entity characterized by the acute transient recurrence of previously recovered focal stroke deficits. Various names have been used to describe PSR, which further complicates its diagnosis. Increased awareness of this condition is crucial for preventing inappropriate management and unnecessary testing.