An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


What causes medication administration errors in a mental health hospital? A qualitative study with nursing staff
Richard n. keers.
1 Centre for Pharmacoepidemiology and Drug Safety, Division of Pharmacy and Optometry, School of Health Sciences, Manchester Academic Health Sciences Centre (MAHSC), University of Manchester, Manchester, United Kingdom
2 NIHR Greater Manchester Patient Safety Translational Research Centre, MAHSC, University of Manchester, Manchester, United Kingdom
3 Medicines Management Team, Greater Manchester Mental Health NHS Foundation Trust, Park House Hospital, North Manchester General Hospital, Manchester, United Kingdom
Madalena Plácido
Karen bennett.
4 School of Health and Human Sciences, University of Bolton, Bolton, United Kingdom
Kristen Clayton
Petra brown, darren m. ashcroft, associated data.
The dataset used to generate the findings of the study was the complete dataset and not a minimal dataset – the complete dataset was not reduced or adapted for analysis. This qualitative study took place in a single UK mental health hospital with a participant group restricted to nursing staff. Our university research ethics committee (UREC) approval for this study was granted based on the anonymity of participants discussing events that some may consider sensitive. Making the full anonymised interview transcripts publicly or privately available could therefore potentially lead to the identification of participants. Specifically, our ethical approval was based upon statements in the participant information sheets and consent forms that referred to only anonymised quotations from transcripts being used in study outputs; the participants did not consent to their full transcript being made publically available or shared with anyone outside the research team, except to responsible individuals from the University of Manchester, from regulatory authorities or from the participating NHS Trust, where it is relevant to them taking part in the research. The researchers are therefore not permitted to share the anonymised interview transcripts outside the research team unless this is to participants who request their own transcribed interview data privately or to appropriate individuals for regulatory purposes. Please contact the research team for further details if required. Address of the university research ethics department who approved this study: Directorate of Research and Business Engagement Support Services, 2nd Floor Christie Building, University of Manchester, Oxford Road, Manchester M13 9PL.
Medication administration errors (MAEs) are a common risk to patient safety in mental health hospitals, but an absence of in-depth studies to understand the underlying causes of these errors limits the development of effective remedial interventions. This study aimed to investigate the causes of MAEs affecting inpatients in a mental health National Health Service (NHS) hospital in the North West of England.
Registered and student mental health nurses working in inpatient psychiatric units were identified using a combination of direct advertisement and incident reports and invited to participate in semi-structured interviews utilising the critical incident technique. Interviews were designed to capture the participants’ experiences of inpatient MAEs. All interviews were transcribed verbatim and subject to framework analysis to illuminate the underlying active failures, error/violation-provoking conditions and latent failures according to Reason’s model of accident causation.
A total of 20 participants described 26 MAEs (including 5 near misses) during the interviews. The majority of MAEs were skill-based slips and lapses (n = 16) or mistakes (n = 5), and were caused by a variety of interconnecting error/violation-provoking conditions relating to the patient, medicines used, medicines administration task, health care team, individual nurse and working environment. Some of these local conditions had origins in wider organisational latent failures. Recurrent and influential themes included inadequate staffing levels, unbalanced staff skill mix, interruptions/distractions, concerns with how the medicines administration task was approached and problems with communication.
Conclusions
To our knowledge this is the first published in-depth qualitative study to investigate the underlying causes of specific MAEs in a mental health hospital. Our findings revealed that MAEs may arise due to multiple interacting error and violation provoking conditions and latent ‘system’ failures, which emphasises the complexity of this everyday task facing practitioners in clinical practice. Future research should focus on developing and testing interventions which address key local and wider organisational ‘systems’ failures to reduce error.
Introduction
Mental health illness is common and has a significant detrimental impact on societies and national economies [ 1 , 2 ]. Patients with these illnesses are a complex and vulnerable patient group with a high risk of premature mortality [ 3 ]. They are known to have high burdens of physical co-morbidity [ 4 ], do not always access appropriate health care and may suffer inequalities in the care they are provided [ 5 , 6 ].
The use of medicines to treat mental illness is a mainstay of modern practice [ 7 ]. However, psychotropic polypharmacy [ 8 – 10 ], unlicensed psychotropic prescribing [ 11 ], and use of high risk medications such as lithium, depot antipsychotics and clozapine [ 12 ] are common in this population and present unique challenges for safe medication use. To compound the risks to patient safety that these issues create, prescribed medications may frequently change during psychiatric hospital admission [ 13 ] and not all mental health service users may feel involved in decisions about their drug treatment [ 14 ]. The way medicines are managed in hospital settings may also differ to general hospitals; for example in the United Kingdom (UK) patients may receive medication from a trolley located centrally and trained ‘runners’ such as health care assistants may take medication dispensed by nurses to patients on the ward [ 15 , 16 ]. There is also emerging evidence that medicine-related factors may play a role in causing re-admission to mental health hospitals [ 17 , 18 ]. This clearly highlights the importance of studying the quality and safety of medicines use in mental health settings, and there is growing international consensus on this issue [ 19 , 20 ].
A recent systematic review of medication safety in mental health hospitals found that prescribing errors and medication administration errors (MAEs) were common in this setting, and that patients were often harmed by preventable medication related adverse events [ 21 ]. Indeed, MAEs may be the most commonly reported medication error in mental health hospitals [ 22 , 23 ], with direct observation studies finding MAE rates of 3.3–48% of doses administered or omitted [ 24 – 26 ].
Whilst there is emerging evidence of the prevalence and nature of MAEs in mental health hospitals, an in-depth understanding of the underlying causes of these errors remains absent [ 21 ]. This is an important knowledge gap in the current evidence base, as the causes of MAEs in mental health hospitals may be different to general hospitals and a clearer understanding of the underlying causes of MAEs in this specialist setting could inform the design of effective interventions [ 27 ]. To date, available evidence of MAE causation in mental health settings is limited to quantitative analysis of observation data [ 24 – 26 ] (which cannot capture internal mental processes like intention), incident report reviews [ 22 , 23 , 28 ] (which often report limited descriptions of MAE causation) and more general explorations of medicines administration practices [ 15 , 16 ] or related knowledge/competency [ 29 ]. Whilst these studies are useful in identifying some of the important MAE antecedents, including those that might differ to general hospitals (e.g. ‘runners’ [ 22 , 23 ] and disturbed patients [ 22 ]), they do not provide a comprehensive account of the causal chain leading to error, nor how various factors may interconnect under different circumstances to lead to MAEs [ 27 , 30 ]. Therefore, this study aimed to investigate in-depth the underlying causes of MAEs in a mental health National Health Service (NHS) hospital.
Definitions
Medication incidents were included in the study if they met the following definitions. Medication administration errors (MAEs) were defined as ‘a deviation from the prescriber’s order as written on the patient’s chart, manufacturer’s instructions or relevant institutional policies’ [ 27 , 30 ]. Our definition of an MAE encompassed ‘near misses’ that were prevented from reaching the patient by any means [ 31 ]. Our analysis of the underlying causes of MAEs was informed by established human error theory, the components of which are defined later in this manuscript (see ‘Data Analysis’).
Student and registered mental health nurses (RMNs) were recruited between March-July 2015 from one mental health hospital in the North West of England. The hospital had a total of 9 adult inpatient units catering for a variety of mental health illnesses including acute care, intensive care, later life and rehabilitation.
At the time the study was carried out, the study hospital utilised paper-based prescribing and an electronic patient record system. Medicines administration involved patients attending the ward clinic room to receive their medications (except later life wards). Medications were prepared for individual patients sequentially during medication rounds; pre-preparing medications or preparing multiple medications simultaneously for different patients was not recommended. Most oral medicines were authorised to be administered by a single qualified nurse, but in practice a second ‘runner’ (often a trained health care assistant or nurse) was frequently utilised to bring patients to the clinic room or to take medications to the patient directly. A group of ‘high risk’ medications including all injectable medicines (e.g. insulin, depot antipsychotics) and controlled drugs required two authorised members of staff to check and sign for administration; this most often involved two qualified nurses. Student nurses were only permitted to administer medications to patients under the direct supervision of a registered (qualified) nurse.
Recruitment
Both student nurses and RMNs were eligible to participate provided they were working on mental health inpatient units at the time the MAE was made and were willing to discuss the causes of at least one of these incidents that they had been directly involved with. Near misses were included as MAEs as they also provide windows into the safety of systems, and student nurses were considered eligible to take part alongside RMNs in order to provide further diverse perspectives on what factors influence medication administration errors.
Participants were recruited to the study in three ways:
- Nursing staff who recorded MAEs using the local incident reporting system during and up to 6 months before the study began were identified and approached by the research team. This system allowed those reporting incidents to be identified by senior management and medicines safety staff for improvement, quality control and governance purposes,
- Local members of the medicines management team who identified MAEs on their inpatient wards reported these to the research team, who then approached the nursing staff member involved, and
- Members of the research team directly advertised the study to inpatient nursing staff during ward visits and using posters located in clinical ward areas.
Potential participants were then offered information packs (cover letter and participant information sheet) about the study. Anyone then interested in taking part contacted a member of the research team to arrange an interview. Written consent was provided before interviews took place.
Data collection
The interview guide used in this study was adapted for the mental health setting following successful use by the research team investigating the causes of MAEs in UK general hospitals [ 30 ]. The interview guide can be found in the Appendix ( S1 Appendix ). Briefly, participants were asked to provide basic background demographic information before discussing one or more MAEs that either reached or did not reach the patient (near misses) that they were directly involved with. Emphasis was placed on recalling in detail the circumstances of the incident and what the participant thought caused it to happen. The interviews closed with participants providing insights into what they felt could have prevented their error from occurring.
Research team members RNK and MP conducted interviews face-to-face and following a semi-structured format with each participant. Each interview was digitally audio-recorded (with the exception of one interview, where the participant preferred written notes to be made instead) and lasted between 10–42 minutes. Research team members RNK and MP were both trained in qualitative interviewing and co-interviewed 3 participants (with their permission) in order to achieve consistency in interview style.
The design of the interview guide and overall approach to the interviews was based on the critical incident technique (CIT) [ 32 ]. The CIT has been successfully applied to help understand the causes of inpatient prescribing [ 33 ] and medication administration errors [ 30 , 34 ], and facilitates the collection of rich and relevant data from otherwise busy ward staff by focusing on exploring their specific intentions, behaviours and actions when a particular error or near miss occurred [ 35 ].
Data analysis
Interviews were transcribed verbatim. Transcripts were organised and coded using the NVivo computer software program (v10) according to the Framework method [ 36 ]. Framework is a seven step analytical approach designed to be systematic and transparent so that the process of translating raw data into emerging themes is clear [ 37 ]. Data are organised in matrices and summarised in individual cells so they can be reduced and compared across participants without losing context within individual accounts. The stages of analysis are as follows: the interviews are transcribed and researchers become familiar with it; then the data are coded and the conceptual framework is developed before being tested and applied; and finally the data are summarised in matrices and interpreted (e.g. by connecting themes/cases, or by developing typologies). Researchers are free to move between these analytical stages as required to refine concepts [ 36 , 37 ].
The analysis framework was informed by Reason’s model of accident causation [ 38 , 39 ]. Earlier research has applied this model to understand the causes of medication errors [ 27 , 30 , 33 , 40 ], and it has been described in the context of MAE research in detail elsewhere (including summary diagrams of how Reason’s model applies to MAE research) [ 27 , 30 ]. Reason’s model is summarised in Fig 1 . Data were coded as active failures, error/violation provoking conditions and latent (wider organisational) failures, and one author (KB) independently extracted and analysed data for 10 interviews in order to confirm the suitability of the coding framework. Each MAE type (e.g. dose omission) was assigned by the research team [ 30 ]. Active failure assignments were confirmed following review and discussion between RNK and DMA.

Ethical approval
The study was approved by the University of Manchester Research Ethics Committee 2 (submission 15104) and by the research and development department at the participating NHS trust.
Twenty participants described a total of 26 MAEs, including 5 ‘near misses’ that did not reach the patient. No errors resulted in patient harm. A summary of interview participants and the MAEs they described can be found in Table 1 . The majority of errors involved medications used to treat central nervous system (CNS) disorders (n = 21), and most commonly involved either wrong drug (n = 7), wrong patient (n = 5) or wrong dose errors (n = 4). The reported MAEs involved nurses of varying levels of experience post-qualification, with over half occurring when participants had 1 year or less (n = 14, 54%) experience (including 2 student nurse errors) and 7 (27%) when nurses had more than 5 years’ experience. Each error and near miss (active failure) was preceded by combinations of underlying error and violation provoking conditions, as exemplified in Fig 2 that describes the active failures and error provoking conditions underpinning one MAE discussed in this study.
F = female; IM = intramuscular; KBM = knowledge based mistake; M = male; NK = not known, other person prominently involved; NS = not specified; RBM = rule based mistake

Active failures
Sixteen of the MAEs reported by participants involved skill based slips and lapses (n = 13 slips), with the remainder either knowledge (n = 4) or rule based mistakes (n = 1), and violations (n = 1). Some events could not be categorised as active failures as another staff member was more prominently involved (n = 4).
Slips and lapses
Skill based errors often resulted in nurses selecting the wrong product (drug or dosage) or overlooking or misinterpreting important information. One experienced nurse described how she administered co-codamol instead of codeine whilst busy and could only recall that the patient was prescribed co-codamol previously:
“… but the gentleman in question had been on co-codamol since he’d been here, and he’d only just been changed to codeine. So, in my head, I saw the codeine, but because I was that busy I thought, oh he’s been on co-codamol since he’s got here, so that’s why I gave him it [co-codamol].” (N14, > 5 years’ experience)
Knowledge and rule based mistakes
In contrast to skill based errors, knowledge and rule based mistakes involved flawed planning. In one account, a junior nurse was not certain of her knowledge when faced with a novel problem:
“I think because I was newly qualified and it [how to dose ‘when required’ medications over 24 hours] hadn’t really been explained very well, so I thought that they could have two [doses] in a day so, say, today they could have two today, and then two lots tomorrow. But, you have to do it from the time, don’t you…” (N10, < 1 year)
There was one reported violation, which involved the administration of levothyroxine to the wrong patient after a nurse who did not routinely work on the ward in question misidentified a service user using only their name and not their date of birth as recommended in the local policy for medicines administration.
Error and violation provoking conditions
The health care team.
Problems with written and verbal communication were discussed by 11 participants, and commonly led to skill-based errors and mistakes when staff missed, misinterpreted or made assumptions about information whilst working under challenging conditions (such as high workload, noisy environments, and distractions from staff or patients).
Written communication problems concerned prescriptions that were ambiguous because they had parts crossed out or were unclearly written, as well as previous medicines administration records that were not correct or were omitted. Problems with verbal communication were less common (n = 4 errors) but commonly involved communication breakdown between two staff members (e.g. between nurse and ‘runner’ who administered medication to the patient) and the use of using only the patient name for identification.
Three nurses discussed how a close working relationship with colleagues led to errors when working together to administer medications, with one experienced nurse revealing how he made an assumption about which patient was being discussed with his trusted colleague before making a skill based error and administering medication to the wrong patient:
“… I presumed that he [nursing colleague] knew I was talking about somebody else [medication to be administered], […] but I was just working on the assumption that he knew what I was thinking, which is quite strange really. Looking back, with hindsight, it seems stupid, but I suppose when you’re busy and you’re rushing, then it’s just one of those things.” (N11, > 5 years)
Supervision and support were identified as an important barriers to error by participants, as deficiencies in these areas were frequently raised by participants as contributing to their errors or near misses, and by junior staff members in particular (though two examples of different errors occurred despite direct support). Participants discussed making both skill-based and planning errors as a consequence. Lone working was frequently implicated in these errors as this often caused anxiety which distracted participants, added to their workload if there were certain tasks only qualified nurses could perform (e.g. obtaining money from the safe) and gave them limited options for clarification in cases of uncertainty. One recently qualified nurse described how lone working during medicines administration limited her options for clarification which contributed to a knowledge based mistake:
“And, as a newly qualified I was left on my own, like, the only qualified nurse… […] … I wasn’t able to ask another nurse, I wasn’t able to check with them, because I was just on my own. Obviously, the patient was getting really upset and agitated, so I think that was probably another reason why I gave it [dose] a bit early.” (N10, < 1 year)
The individual nurse
The majority of participants highlighted how considerable stress, nervousness (particularly amongst junior nurses) and feelings of pressure to complete tasks contributed to their errors and near misses; these mental states were driven primarily by high workload, low staffing, inexperience, patient acuity and inadequate skill mix and led to inappropriate decision making and skill based errors through lack of concentration or rushing.
Along with undergraduate students, new or recently qualified nursing staff in particular described how their unfamiliarity with certain medications (e.g. depot antipsychotics) and patients contributed to errors. Two nurses commented on how semi-sodium valproate was used “a lot more” (N03, > 5 years) on their wards compared to sodium valproate, which contributed to misidentification of these medicines through prior expectations.
When left on their own, junior nurses reported burdensome feelings of responsibility when working in isolation and questioned their readiness to cope with this role which put further pressure on themselves, causing mental distraction and flawed decision-making.
“I think I was naturally more anxious for that shift anyway because I was the only nurse on [the ward] and it was the first time so you’ve got that…I don’t know if it’s relevant but what I got was getting really anxious, like, what if I can’t manage it, I’ve only been qualified a few months, what if something goes wrong and it comes back on me, I’m looking after 20 patients on my own, I haven’t been qualified long. So I think there was an underlying anxiety as well that maybe I was also distracted by that when I was dispensing the medication which did probably have an effect as well.” (N01, < 1 year)
Greater experience was highlighted as a protective barrier to error by one nurse who commented on how this gave them confidence to challenge patient demands in the interests of safety, rather than trying to respond immediately (and rushing) to meet their requests:
“… I’ve learnt over the years that some things don’t have to be done immediately, you know, you have to prioritise and especially where medicines are concerned, you need to do it right, so if it means taking an extra half hour, then unfortunately I’d just explain to the patient, you’re just going to have to wait half an hour before you can go on your leave.” (N02, < 1 year)
The patient
Patient mental illness, behaviours (e.g. agitation, hostility) and requests contributed to every active failure. One nurse described how a lack of ward staffing meant that patients were not receiving attention and were instead interrupting staff with requests, leading to a skill-based slip:
“… there wasn’t enough staff and the patients obviously weren’t getting probably the attention that they wanted, so they did keep coming [to see staff], because some patients are demanding and they do want a lot of time off staff, which you can’t always give if you’re busy.” (N06, 1–5 years)
Another participant who reported a violation described how a patient’s mental illness meant they did not intervene despite being addressed with the wrong name and given incorrect medications:
“But I remember I think because I was talking to the patient and saying their name, and over and over, and saying how are you doing today, da-da-da, and talking to them, I think the patient was very withdrawn and didn’t really talk too much with me and never really corrected me, I just assumed that that was fine and that that was the [correct] person.” (N20, 1–5 years)
Other participants revealed how persistent demands from often agitated and aggressive patients led to them yielding to these requests despite their own uncertainties, due in part to lack of staff support/lone working and inadequate confidence, experience and/or knowledge. This was exemplified by one account of a wrong drug error involving a depot antipsychotic when the participant was a junior nurse, where patient distraction combined with multi-tasking, workload pressures and a change in prescription contributed to the pathway to error:
“I think I wasn’t familiar with the [depot] chart, because they changed, I let the patient mither [pester] me, she was, like, I want to go [leave the ward], I want to go, can you do it? And I was trying to do two things at once and because it was a depot [antipsychotic administration], it’s outside of your normal medicine round, so I think I was under other pressures and I was, like, oh, just get her depot done and then she can go on her leave, sort of thing, then it’s one less person around my feet asking for something, which is wrong, I can see that now, but at the time, you know, it’s quite easy to get drawn into…and really what I should have done to her was said, you’re just going to have to wait five minutes, just have a seat, let me just go and…and then I think if I’d have just took that extra couple of minutes, I wouldn’t have picked the wrong [medication] card up.” (N02, < 1 year)
The working environment
The majority of participants (n = 17) described working environments that were noisy, chaotic, and/or busy. Some participants used the term “acute” (N15, < 1 year) to describe the ward conditions, which highlighted instances where there were multiple unwell/agitated patients or general disruption present. Many described how patients queued outside the clinic room to receive their medication, creating noise and asking questions of staff. This type of environment led to distractions and interruptions, high workload and rushing, and when combined with other factors led to both skill-based and planning errors as nurses were not able to focus on the medicines administration task.
“Rushed, there were lots of people milling around in the corridor, there were doctors running on and off the ward requesting prescription charts, there were medical students who were doing bloods on another patient in the clinic at the same time, so it was really crowded, it just felt really…just really rushed, I had to get the medication round finished to get on with the rest of the day […] One of the medical students was asking me where the blood bottles and needles were.” (N01, < 1 year)
Distractions and interruptions were implicated in more than half of the incidents reported and the majority resulted in skill-based errors. Their origins were multifactorial, including high workload, patient factors, staff/skills mix issues and other activities taking place during the medication round (e.g. ward rounds).
High perceived workload, inadequate skill mix and particularly low staffing were major themes interconnecting the majority of errors. Low staffing was reported to be common place and appeared chronic in some cases, with causes including sickness, annual leave and wards acting as a staff “donor” (N11, > 5 years) to others requiring personnel. As a result, some staff reported working longer hours or being left on their own as the only qualified nurse during shifts, adversely affecting workload and nurse mental state.
Many participants felt that using agency nurses in response to staff shortages added to their workload and mental burden due to their perceived deficiencies in skill level and lack of familiarity with the ward, its patients and practices. One nurse felt she could not use agency staff for support when faced with a knowledge deficit:
“… which is another issue, agency staff only. They don’t know the ward, they don’t know the patients, so you’re the only qualified with three or four agency staff only, who don’t have the ward, who don’t know the patients. So you can’t rely on them. All you need to do is to rely on yourself, you know?” (N08, 1–5 years)
The medicines
Medicines that sounded and/or looked a-like were discussed as contributory factors to error on four occasions, with three involving mix-ups between semi-sodium and sodium valproate. Four participants also described how storage of multiple pre-prepared depot syringes and other medicines (mainly valproate) next to each other contributed to selection errors.
Nursing staff emphasised how easy it was for them to mistake valproate products for one another, with one more experienced nurse describing how similarities in how they are written contributed to a skill-based slip:
“… because, you know, there’s only the ‘semi’ different and it was the same amount, same dose, you know, the same amount, same times and everything, it [sodium valproate] did look very much, you know, very similar [to semi sodium valproate] …” (N03, > 5 years)
The medicines administration task
Challenging ward conditions appeared to affect the perceptions of nursing staff towards the medicines administration task. Participants described rushing medicines administration in order to carry out other tasks or to prioritise a competing demand (e.g. patient needs), with one experienced nurse reporting doing so because they felt isolated in the clinic room and out of control from the rest of the ward, resulting in medications being given to the wrong patient.
“… the reason that I was hurrying was because I wanted to get out of the clinic. I just wanted to make sure the medication was done and dusted, and then you can get back onto the ward. Because when you’re in the clinic, […] you don’t really know what’s going on, on the ward. And on a ward like [Ward name], it’s…you need to be aware of what’s going on at all times.” (N11, > 5 years)
There was evidence of deficiencies relating to medicine double checking practices as well as patient identification. Although double checking was in place as a defensive barrier to error, MAEs occurred during both single (majority of medicines) and dual practitioner administration (e.g. controlled drugs, student nurses, depots, use of ‘runners’ to administer medication). For dual practitioner errors, examples included cases where either double checking did not take place, both staff members involved made the same mistake or information was miscommunicated between parties. Despite this, one nurse mentioned the protective effects of cross-checking for patient safety:
“Yeah there is [cross checking each other’s work] at times because like say sometimes things [medications] get changed from ward round but only one nurse is in there and then it might not always get handed over, but then it can be a good time for them to hand over that medication might have changed or things like that. It sort of jogs your memory sometimes.” (N18, < 1 year)
Latent (wider organisational) failures
Whilst not identified as frequently as error/violation provoking conditions by participants, latent failures were reported as underpinning the emergence of staffing, skill mix and workload issues. One nurse suggested that the ward shift roster system was partly responsible for low staffing on their unit, and more than one participant commented that it was difficult for managers to identify staff replacements and for agencies to fill staff vacancies leading to skill mix and staffing problems. There were also suggestions that nurses were not allocated ‘protected time’ to administer medications on the ward and that scheduling ward rounds and patient meetings at the same time as medicines administration depleted available staff and increased workload.
To our knowledge, this is the first study to explore the causes of specific MAEs in a mental health hospital using in-depth qualitative interviews. Each MAE was reported to be caused by a combination of local error/violation provoking conditions relating to the patient, the health care team, the working environment, the medicines administration task, the individual nurse and the particular medicines involved, with wider organisational latent failures underpinning the emergence of many of these local conditions.
Implications of findings
This study has brought into sharp focus the complexity of medicines administration on mental health wards and builds significantly on earlier work in the context of patient safety [ 15 , 16 , 21 – 23 , 28 , 29 ]. It is apparent that medicines administration regularly takes place in physically and cognitively demanding circumstances that could compromise defensive barriers and promote the occurrence of MAEs, and we have identified factors influencing the safety of medicines administration processes which are unique to this environment. We gathered in-depth accounts from nurses with different levels of experience who reported making errors across different mental health specialities. Our findings suggest that newly qualified staff might be particularly vulnerable and require additional support as a defensive barrier to help them practise safely and with confidence. The knowledge of the underlying causes of MAEs generated by this study will be an important contributor in the ongoing agenda to enhance mental health service quality [ 41 , 42 ], and in informing the optimisation and evaluation of ward based medicines management services.
Whilst there are some similarities between the findings of our study and in-depth research of MAE causation in general hospitals across areas such as low staffing, interruptions, high workload and task management/double checking deficiencies [ 27 , 30 ], our study has identified more context specific targets such as the impact of lone working and patient-related needs or behaviours (e.g. demands, aggression, lack of engagement).
A number of themes emerged as influential antecedents to multiple errors discussed in this study, and were also found to be linked to other causative factors. These are described below. However, it is important to recognise that whilst each theme might individually be isolated and mitigated to reduce the risk of error, future efforts to develop remedial interventions could consider a multifaceted approach to maximise positive impact as the MAEs in this study were often caused by interacting factors across multiple themes [ 27 , 30 , 43 ].
Low staffing and inadequate skill mix
These themes preceded most MAEs and have emerged as quality measures in mental health with guidance being produced in the UK [ 44 , 45 ]. There are a number of tools available to assess staffing levels [ 46 ] but there remains a need for those tailored to the mental health setting [ 47 , 48 ]. Although the use of temporary staff in the mental health setting is a long-standing issue [ 49 ], with agency staff associated with a high cost burden [ 45 ], our study adds an important perspective to this narrative if nurses consider agency staff as creating problems in the medicines safety context. Mental health organisations are now considering more creative options to manage qualified nursing shortages [ 50 ]. However, the evidence of impact of staffing in relation to medicines safety is limited [ 48 , 51 – 52 ] and further research could therefore measure, understand and mitigate these influential causative factors.
Disruptive and distracting working environments
The busy working environment, and in particular distractions and interruptions, were highly influential in skill-based slips and lapses. These factors feature prominently in earlier studies of error causation in mental health [ 22 , 23 , 28 , 29 ] but our findings add much needed contextual detail, and place more emphasis on patient-led causes of distractions and interruptions compared to evidence from general hospitals [ 27 , 30 ] which could be crucial for the design of remedial interventions [ 53 ].
Individual stress/pressure and task management
This study has emphasised the mental demands of the nursing role and the important influence this has on how nurses prioritise and carry out their duties. Previous studies have highlighted significant workplace stress for mental health nurses [ 54 ] and how mental workload can impact prescribing [ 33 ] and medicines administration safety in general hospitals [ 30 , 55 ]. This indicates a need for more in-depth understanding of how factors such as patient advocacy, risk/benefit judgement and other personal and environmental circumstances affect decision-making in the medicines administration context in mental health. It may be useful to utilise techniques such as observation and hierarchical task analysis to characterise and predict the risks to medicines administration safety for nurses on the mental health ward, as seen in general hospitals [ 56 , 57 ].
Communication
We identified communication deficiencies that were both common to other settings (e.g. illegible prescriptions) but also unique to mental health settings (e.g. between nurses and ‘runners’ [ 22 , 23 , 16 ]). Communication deficiencies appear as frequent contributors to error in incident report studies in mental health hospitals [ 22 , 23 , 28 , 29 ] though detail as to their nature which we identified is rarely provided. Whilst electronic prescribing and medicines administration systems are being introduced to improve medicines safety, there is evidence that nursing documentation discrepancies increase [ 58 ], and to our knowledge there have been no published evaluations of the impact of such systems in the mental health setting to date. Understanding and improving verbal communication between colleagues and with patients during medicines administration in the context of drug safety appears to be a subject of limited research [ 43 , 59 ].
Strengths and limitations
Strengths of this study include a focus on obtaining relevant data by restricting participant accounts to only examples in which they were directly involved. We used established data collection and analysis methods, though we did not triangulate with other methods such as observation which may help distinguish between what people say and what actually occurred. The research team also noted emerging data saturation at approximately the half way point of interviews which may have helped to ensure adequate coverage of the important contributory factors to MAEs.
The possibility of recall and hindsight bias cannot be excluded particularly as we asked participants identified from incident reports to recount events from up to 6 months previously, although the risk was minimised by asking participants to discuss events occurring within recent memory or those they could remember clearly. The risk of social desirability bias [ 60 ] may have been minimised as CIT was used to focus on actual actions and behaviours of participants, and attribution bias [ 61 ] may have also been minimised as the experience of the data collectors was that participants accepted their measure of responsibility for MAEs or near misses, and did not readily blame others.
This study found that MAEs occurring in a UK mental health NHS hospital are each caused by a combination of interconnecting local error provoking conditions and latent ‘systems’ failures. Key antecedents to multiple types of MAE and thus central contributors to error were identified and included low staffing, inadequate skill mix, challenging ward environments (including patient factors), interruptions and distractions and communication problems. Future research efforts should be directed toward developing, testing and evaluating practical interventions designed to target these known causative factors, in order to offer informed recommendations to improve front line clinical services for the benefit of patients through reduced MAE rates.
Supporting information
S1 appendix, acknowledgments.
We would like to thank all the registered and student mental health nurses who agreed to take part in this study.
Funding Statement
This work was supported internally by The University of Manchester and participating NHS trust, no specific grant or funding stream was used. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
Interventions to reduce medication errors in adult medical and surgical settings: a systematic review
Affiliations.
- 1 School of Nursing and Midwifery, Centre for Quality and Patient Safety Research, Institute for Health Transformation, Deakin University, 221 Burwood Highway, Burwood, Victoria 3125, Australia.
- 2 Department of Nursing, The University of Melbourne, Melbourne, Victoria, Australia.
- 3 Melbourne Medical School, The University of Melbourne, Melbourne, Victoria, Australia.
- PMID: 33240478
- PMCID: PMC7672746
- DOI: 10.1177/2042098620968309
Background and aims: Medication errors occur at any point of the medication management process, and are a major cause of death and harm globally. The objective of this review was to compare the effectiveness of different interventions in reducing prescribing, dispensing and administration medication errors in acute medical and surgical settings.
Methods: The protocol for this systematic review was registered in PROSPERO (CRD42019124587). The library databases, MEDLINE, CINAHL, EMBASE, PsycINFO, Cochrane Database of Systematic Reviews and the Cochrane Central Register of Controlled Trials were searched from inception to February 2019. Studies were included if they involved testing of an intervention aimed at reducing medication errors in adult, acute medical or surgical settings. Meta-analyses were performed to examine the effectiveness of intervention types.
Results: A total of 34 articles were included with 12 intervention types identified. Meta-analysis showed that prescribing errors were reduced by pharmacist-led medication reconciliation, computerised medication reconciliation, pharmacist partnership, prescriber education, medication reconciliation by trained mentors and computerised physician order entry (CPOE) as single interventions. Medication administration errors were reduced by CPOE and the use of an automated drug distribution system as single interventions. Combined interventions were also found to be effective in reducing prescribing or administration medication errors. No interventions were found to reduce dispensing error rates. Most studies were conducted at single-site hospitals, with chart review being the most common method for collecting medication error data. Clinical significance of interventions was examined in 21 studies. Since many studies were conducted in a pre-post format, future studies should include a concurrent control group.
Conclusion: The systematic review identified a number of single and combined intervention types that were effective in reducing medication errors, which clinicians and policymakers could consider for implementation in medical and surgical settings. New directions for future research should examine interdisciplinary collaborative approaches comprising physicians, pharmacists and nurses.
Lay summary: Activities to reduce medication errors in adult medical and surgical hospital areas .
Introduction: Medication errors or mistakes may happen at any time in hospital, and they are a major reason for death and harm around the world.
Objective: To compare the effectiveness of different activities in reducing medication errors occurring with prescribing, giving and supplying medications in adult medical and surgical settings in hospital.
Methods: Six library databases were examined from the time they were developed to February 2019. Studies were included if they involved testing of an activity aimed at reducing medication errors in adult medical and surgical settings in hospital. Statistical analysis was used to look at the success of different types of activities.
Results: A total of 34 studies were included with 12 activity types identified. Statistical analysis showed that prescribing errors were reduced by pharmacists matching medications, computers matching medications, partnerships with pharmacists, prescriber education, medication matching by trained physicians, and computerised physician order entry (CPOE). Medication-giving errors were reduced by the use of CPOE and an automated medication distribution system. The combination of different activity types were also shown to be successful in reducing prescribing or medication-giving errors. No activities were found to be successful in reducing errors relating to supplying medications. Most studies were conducted at one hospital with reviewing patient charts being the most common way for collecting information about medication errors. In 21 out of 34 articles, researchers examined the effect of activity types on patient harm caused by medication errors. Many studies did not involve the use of a control group that does not receive the activity.
Conclusion: A number of activity types were shown to be successful in reducing prescribing and medication-giving errors. New directions for future research should examine activities comprising health professionals working together.
Keywords: hospitals; medical order entry systems; medication errors; medication reconciliation; medication therapy management; nurses; patient safety; pharmacists; physicians; systematic review.
© The Author(s), 2020.
Publication types
- Open access
- Published: 25 October 2021
Improving patient safety through identifying barriers to reporting medication administration errors among nurses: an integrative review
- Agani Afaya 1 , 2 ,
- Kennedy Diema Konlan 1 , 2 &
- Hyunok Kim Do 1
BMC Health Services Research volume 21 , Article number: 1156 ( 2021 ) Cite this article
26k Accesses
17 Citations
7 Altmetric
Metrics details
The aim of the third WHO challenge released in 2017 was to attain a global commitment to lessen the severity and to prevent medication-related harm by 50% within the next five years. To achieve this goal, comprehensive identification of barriers to reporting medication errors is imperative.
This review systematically identified and examined the barriers hindering nurses from reporting medication administration errors in the hospital setting.
An integrative review.
Review methods
PubMed, Web of Science, EMBASE, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) including Google scholar were searched to identify published studies on barriers to medication administration error reporting from January 2016 to December 2020. Two reviewers (AA, and KDK) independently assessed the quality of all the included studies using the Mixed Methods Appraisal Tool (MMAT) version 2018.
Of the 10, 929 articles retrieved, 14 studies were included in this study. The main themes and subthemes identified as barriers to reporting medication administration errors after the integration of results from qualitative and quantitative studies were: organisational barriers (inadequate reporting systems, management behaviour, and unclear definition of medication error), and professional and individual barriers (fear of management/colleagues/lawsuit, individual reasons, and inadequate knowledge of errors).
Providing an enabling environment void of punitive measures and blame culture is imperious for nurses to report medication administration errors. Policymakers, managers, and nurses should agree on a uniform definition of what constitutes medication error to enhance nurses’ ability to report medication administration errors.
Peer Review reports
Introduction
Improving patient safety remains an ongoing global health challenge for more than two decades after the beginning of the new wave of attention by the United States (US) Institute of Medicine (IOM) in 1999 report “To err is human” [ 1 , 2 , 3 , 4 ]. In March 2017, the World Health Organisation (WHO), released an article called “Medication Without Harm, WHO Global Patient Safety Challenge”, to gear up the process of change to reduce the impact of patient harm associated with unsafe medication practices by health care practitioners [ 5 ]. The aim of the third WHO challenge released in 2017 was to attain a global commitment, involvement, and prevention strategies to lessen the severity and to prevent medication-related harm by 50% within the next five years [ 5 , 6 , 7 ]. One of the ten leading causes of disability and deaths in the world is the occurrence of adverse events arising due to errors [ 8 ]. In developed countries, approximately one in every ten patients suffers harm while receiving care [ 9 , 10 ] in the hospital with 50% of them being preventable [ 8 ]. It is also estimated that each year, 134 million adverse effects occur in hospitals within developing countries resulting in 2.6 million deaths due to unsafe care [ 8 ].
Medication error (ME) reporting systems represent a central tool for retrospective medication safety risk management in many healthcare organisations as they provide information on the occurred incidents [ 11 ]. However, these systems may become worse if adequate measures are not taken to ensure an enabling environment in reporting MEs [ 12 ]. Nurses are the most significant healthcare workforce in the healthcare sector, primary caregivers, and play a vital role in the prevention and detection of adverse events in patients [ 4 ]. Their roles in reporting medication administration errors (MAEs) are pivotal because they are directly involved in the administration of the vast majority of the medications ordered in hospitals [ 13 ].
MEs are the leading causes of avoidable patient harm in the health care system across the world [ 14 ] and nurses are among the biggest contributors to MEs [ 15 ]. Al-Worafi [ 16 ] revealed that 39% of MEs occur among general practitioners, 38% among nurses, and 23% among pharmacists. Also, Ferrah, Lovell, and Ibrahim [ 17 ], in their systematic review indicated that the prevalence of MEs among nurses is between 16 and 27%. These figures are worrying and therefore nurses reporting MAEs in the health care system will enhance root cause analysis. This will lead to the identification of the specific causes of MEs and therefore provide concrete solutions to reduce medication harm to patients. It is also essential for nurses to report MEs because nurses represent the last safety check in the chain of events in the drug administration process, and are the final safeguard of patient wellbeing [ 14 ].
An integrative review method based on Whittemore and Knafl’s [ 18 ] methodological approach was employed to identify primary studies that focused on barriers to reporting medication administration errors (MAEs) among nurses. Unlike the traditional systematic review, an integrative review utilises a broad focus and allows for the analysis of diverse data sources (qualitative, quantitative, and mixed-method studies) [ 18 ] to inform research and practice. Whittemore and Knafl’s approach strengthens the rigor of an integrative review of nursing evidence and plays a vital role in the development of evidence-based healthcare initiatives. The study was guided by the five steps of Whittemore and Knafl’s which fostered a thorough methodological approach focusing on problem identification, literature search, data evaluation, data analysis, and presentation of study characteristics [ 18 ]. The first step focused on why this review is essential. The second step detailed how the reviewers conducted a robust literature search using the Preferred Reporting Items for Systematic reviews and Meta-Analysis guidelines (PRISMA). The third step detailed how the articles were assessed for rigor using the Mixed Method Appraisal Tool (MMAT) version 2018 [ 19 ]. The last step involved data analysis and presentation of findings from the reviewed articles.
Problem identification
The researchers observed that nurses’ inability to report MAEs is hindered by multiple organisational and individual barriers. Several studies have identified some organisational and individual barriers to reporting MAEs such as; lack of reporting systems, blaming individuals instead of the system, no feedback after reporting MAE, negative response from reporting MAEs, lack of clear definition for ME, and fear of reprimand and punishment [ 20 , 21 , 22 ]. Therefore, the need to systematically synthesize current available studies from a wider international perspective to inform nurses and policymakers on strategies to improve MAE reporting and the prevention of patient harm in health facilities.
Literature search
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework was used for the identification and screening of articles [ 23 , 24 ]. A search of electronic databases (PubMed, Web of Science, EMBASE, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL)) identified articles published between January 2016 to December 2020. To determine the search parameters, the Population, Intervention, Comparison, Outcome (PICO) framework was used. Nurses were the population for this review, the intervention was reporting MAE, there was no comparison, and the outcome was barriers to reporting MAEs. The following keywords and combinations were used: medication error*/medicine error*/drug error*; report*/disclosure; nurs*. The inclusion and exclusion criteria for this review is shown in Table 1 .
Quality appraisal
Two researchers (AA and KDK) independently assessed the quality of all the included studies using the MMAT version 2018 [ 25 ]. Disagreements between the two researchers (AA and KDK) were discussed and a consensus was built with HKD. The MMAT contains methodological quality criteria for appraising qualitative, quantitative, and mixed methods studies. The MMAT evaluates the appropriateness of the study aim, study design, methodology, recruitment of participants, data collection, analysis of data, presentation of results, discussions by authors, and conclusions. The studies were rated as high, moderate, and low in quality. The researchers did not assign the overall quality score as it is discouraged by Hong et al. [ 25 ] but the methodological quality of the studies were assessed in accordance to the guideline provided by Hong et al. [ 25 ].
Data extraction and synthesis
For data extraction, a matrix was developed to extract relevant information from the studies which included information about the authors, study aim, study design, sample size and characteristics, key findings concerning barriers to reporting MAEs among nurses. Two researchers (AA and KDK) were involved in data extraction. Disagreements were resolved through discussion with the third author (HKD). A convergent synthesis design was adopted to integrate results from qualitative, quantitative, and mixed-method studies and transformed them into qualitative findings [ 26 ]. A thematic approach was used to synthesize key findings emerging from included articles in relation to barriers to reporting MAEs among nurses, which were read thoroughly and coded by two of the researchers (AA and KDK). The codes were reviewed, and similar codes were categorized to form descriptive themes. The descriptive themes were assessed to generate meaning beyond the original data leading to the development of new, interpretive analytical themes. The researchers (AA and KDK) synthesized the data independently, discrepancies were discussed (AA, KDK, and HKD), and a consensus was built before finalizing the overarching themes and subthemes.
Study selection
The search of all the electronic databases yielded 10,926 articles. Citations for the articles were imported into Endnote X9 (version 1.19.6) reference manager for screening, removal of duplicates, and storage. Additional articles ( n = 3) were searched from Google Scholar and through manually tracing of relevant literature from the list of references in the included studies. A total of 3726 non-duplicate articles were screened by title and abstract using the standard integrative review process (inclusion and exclusion criteria) (Table 1 ). Following the title and abstract screening, 23 articles were included. Of the remaining 23 sources, 12 articles were excluded following a full-text review. Discrepancies were resolved through discussions and the final articles were agreed on. In addition to the 3 additional articles retrieved from manual tracing of reference list and Google Scholar, finally, a total of 14 studies were included in the review. Figure 1 illustrates the PRISMA flow diagram.
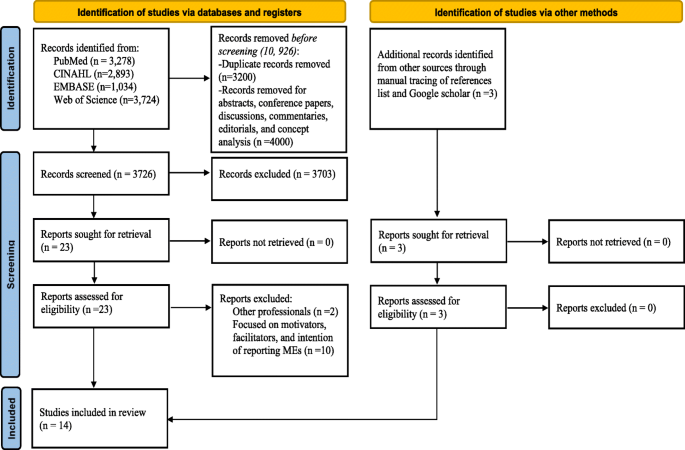
PRISMA 2020 flow diagram
Study characteristics
This review was based on 14 peer-reviewed original publications on barriers to reporting MAEs by nurses in different countries. The study approaches used mainly quantitative descriptive cross-sectional [ 12 ], mixed-method [ 1 ], and qualitative study explorative design [ 1 ]. The cumulative sample size comprised 3299 nurses. The sample size for the quantitative studies ranged from 135 to 548 and the qualitative study involved 23 nurses. Three studies were conducted in Iran [ 27 , 28 , 29 ] and Saudi Arabia [ 13 , 30 , 31 ], and a study each in Malaysia [ 32 ], Jordan [ 33 ], South Korea [ 34 ], Taiwan [ 35 ], United States [ 36 ], Ethiopia [ 37 ], Pakistan [ 38 ] and Turkey [ 39 ]. Two studies utilized a theoretical or conceptual framework. The Theoretical Domains Framework model was utilized by Alrabadi et al. [ 33 ], and the Theory of Planned Behaviour was utilized by Shahzadi et al. [ 38 ] (See Table 2 ).
During the data analysis, two major themes and five subthemes regarding barriers to MAEs reporting emerged. The two major themes included organisational barriers and professional and behaviour-related barriers to reporting ME as shown in Table 3 .
Organisational barriers
Organisational barriers were categorized into three sub-themes of barriers to ME reporting: reporting system, definitions of MEs, and management behaviour. The sub-themes are described below in more detail.
Reporting system
The researchers identified in the studies that there was no clear or proper ME reporting system [ 38 ] therefore making the process of reporting cumbersome, especially the use of the medication incident reporting form which served as a major barrier to reporting MEs [ 33 ]. Some studies documented that ME reporting consumed much time [ 31 , 34 , 36 , 38 , 39 ], whiles Dyab et al. [ 32 ] reported lack of time, tiredness, and heavy workload as barriers to reporting MEs. Rutledge et al. [ 36 ] revealed that the forms used to report MEs are long which posed as a barrier to reporting MEs.
Definitions of medication error
It was indicated in some studies that because there was no precise definition of ME within the hospital [ 28 , 29 , 31 , 37 , 39 ], there were disagreements regarding the definition of ME and what should constitute a reporting event [ 30 , 31 , 37 , 39 ].
Management behaviour
Several studies revealed that reporting MAEs may result in punitive actions by management or negative consequence [ 13 , 27 , 29 , 30 , 31 , 32 , 34 , 36 , 37 ], thereby creating fear among nurses [ 27 , 32 , 34 , 36 , 37 ]. Also, a negative response from the hospital administration was identified by Shahzadi et al. [ 38 ] as a key deterrent to reporting MEs by nurses. Nurses indicated in several studies that they were not given feedback after reporting MAEs [ 13 , 27 , 30 , 32 , 34 , 39 ] which contributed to underreporting of MEs. The researchers also observed that the nursing administration focuses on the individual rather than using the systems approach to solve the problems [ 13 , 27 , 28 , 30 , 31 ] which served as a major barrier to reporting MEs. Nurses indicated that too much emphasis is placed on MEs as a measure of the quality of nursing care [ 28 , 30 , 31 ] therefore impeding error reporting. Nurse’s feared of being blamed by management [ 31 , 32 , 35 , 36 ] if they reported MEs and this served a barrier. Lack of confidentiality in management was also a barrier to reporting MEs [ 32 ].
Professional and behavioural barriers
Under the professional behavioural barriers, two sub-themes were identified: personal reasons, and knowledge of error. The sub-themes are described below in more detail.
Personal reasons/lawsuit
Personal reasons such as criticism from colleagues or other professionals was a barrier to ME reporting [ 34 , 39 ] because they felt they would be embarrassed or discriminated against if they reported MAEs [ 32 ]. Nurses personally felt they could be blamed [ 36 ] if something negative happened to the patient [ 30 ] so they were not encouraged to report MEs. Nurses feared that reporting MEs would negatively impact their job records [ 32 ] or they might lose their job [ 33 , 39 ] which served as an impediment to reporting MEs. A tag on their professional identity or fear of being labelled as incompetent and an inadequate nurse [ 35 ] was also identified as a barrier to ME reporting. One major key factor impeding ME reporting in some studies was the fear of legal actions against nurses by patients or their families [ 13 , 27 , 34 , 36 ]. Forgetting to report ME was another individual barrier to reporting ME [ 29 ].
Knowledge of medication error
Inadequate knowledge of nurses about what constitutes ME [ 33 ] led to underreporting. Nurses did not see the gravity of the ME to warrant reporting [ 31 , 33 , 38 ]. The inability of nurses to identify that an error has occurred hindered reporting of MEs [ 33 , 35 , 38 ]. MAEs that occurred without patient harm did not warrant reporting [ 35 ]. Unawareness of the occurrence of MEs [ 39 ] also led to nurses not reporting MEs.
This study reviewed and synthesized results on barriers to reporting MAEs among nurses. The major barriers include [1] organisational, and [2] professional and behavioural barriers. These are results of studies from different countries ranging from low- middle-, and high-income countries. Therefore, the findings from this review can be vital for the global healthcare communities to improve patient safety as it remains one of the biggest global challenges in healthcare. Most of the studies included in this review were rated as strong, and moderate inferring that the evidence produced from this review has a strong and justified conclusion, meaning that implications can be drawn for nursing research and practice. Also, this study aligns with the WHO `Global Patient Safety Challenge’ emphasizing the promotion and improvement of patient safety actions to reduce severe, preventable medication-related harm by 50% in the next five years [ 7 ]. To develop an effective and robust intervention to improve patient safety, MAE reporting is essential and grounded through the identification of barriers based on the consideration of behavioural change theories [ 40 ]. This information garnered from the key clinical practicing professionals will go a long way to inform policy, healthcare organisations, and other stakeholders on measures to mitigate these barriers and improve patient safety within our healthcare settings across the globe.
The current review found organisational barriers to be the most prominent barrier for nurses not reporting/underreporting MAEs. Barriers such as lack of proper reporting systems, no clear definition of MAEs, and punitive actions against nurses after reporting MAE were identified as organisational barriers to reporting MAEs. Many MAEs go unreported due to the lack of reporting systems or lack of proper reporting systems [ 41 ]. It is imperative to know that if there are no proper reporting systems for MAEs in health facilities, then nurses will find it difficult to duly report errors. Therefore, an established system for reporting MEs in hospitals is important to improving patient safety measures. Established good reporting systems are avenues for collecting vital and sufficient information about MAEs from different reporters [ 41 ]. This information gathered will help reporters understand the factors that influence errors and will therefore subsequently help to prevent their recurrence [ 41 ]. Generally, it is observed that nurses’ failure to report MEs is related to the aftermath consequences they may suffer after reporting depending on the severity of the incidence of injury [ 42 ]. It is observed that some health practitioners fail to report errors due to the intense follow-up investigations on persons that commit these errors rather than the system. Nurses believe that reporting errors negatively impact their future job appraisals and professional development due to the punitive actions taken against them. Non-punitive actions against health care professionals who report errors are recommended to improve patient safety care [ 22 , 42 , 43 ]. Several studies have documented that health professionals who are rewarded and motivated for reporting errors during healthcare are encouraged to further improve on their reporting behaviour which subsequently improves patient safety in the organisation [ 22 , 43 ]. It is also noted that many organisations have been challenged to provide an environment that is free and safe to admit errors and to understand why they occur void of reprisal and punishment [ 44 ].
Criminal prosecution of healthcare professionals in the line of duty remains an astonishing event. Over the years the number of healthcare professionals facing legal actions continues to increase [ 45 ], indicating that healthcare professionals should take strong actions to address these issues. This review revealed that nurses were afraid to report MEs due to possible lawsuits and lack of confidentiality or anonymity in the reporting system. When designing a reporting system, anonymity should be considered to be an important factor [ 22 ] because an anonymous system means a non-punitive reporting culture [ 46 ] and no traceable follow-up procedures after reporting medication incidents [ 47 ]. An anonymous medication error reporting system could help to overcome these barriers of not reporting. A study by Hurley and Berghahn [ 45 ] reported two cases in which nurses were prosecuted for criminal negligence related to MAEs. In order to enhance ME reporting, it is imperative to address systemic issues and problems within the institutions but not the individual.
Inadequate knowledge of nurses about what constitutes ME [ 33 ] and their inability to identify ME necessitating error reporting [ 33 , 35 , 38 ] were barriers to error reporting. Nurses’ knowledge of ME reporting is an important factor that determines the success of the medication reporting system [ 32 ]. It has been recommended that a blend of formal educational seminars (patient safety lectures), and informal educational sessions (lunchtime educational sessions or an online tutorial on using a new reporting system) could improve error reporting [ 43 ]. Therefore, organisations should develop interventional educational programs tailored toward continuous professional education of nurses on MEs reporting systems to improve medication safety. As some studies have found a strong correlation between healthcare workers attending patient safety training workshops and the increased rate of error reporting [ 43 , 48 ].
Limitations
This review had several limitations. First, 12 of the studies included in this review were clustered in Asia, one each in the United States and Ethiopia. These countries captured in this review are not sufficient for the entire world. Second, this study included only published articles in English which might have excluded relevant evidence published in other languages. Third, authors may have unintentionally omitted relevant studies from this review although extensive database and hand searches were conducted. Finally, the review focused on only nurses, and this might have caused the loss of some vital information on studies conducted among other health care professionals such as pharmacists and doctors. That notwithstanding nurses are the final point of drug administration so therefore, this study provides a comprehensive insight into barriers to reporting MAEs among nurses. These findings could help inform policy decision-making in order to improve patient safety through reporting MAEs.
Providing an enabling environment void of punitive measures and blame culture is imperative for nurses to report MEs. The institutionalisation of a proper reporting system for ME reporting provides an avenue to gather data for root cause analysis of errors. This will further enhance a systems approach in dealing with the problems and issues with MEs without focusing on the individual. To minimise the burden on nurses reporting MEs, an effective, non-time consuming, and the uncomplicated anonymous system is required. An open feedback system for motivating or rewarding nurses for reporting MEs is imperative and will therefore increase the rate of MAE reporting. Policymakers, managers, and Nurses should agree on a uniform definition of what constitutes ME to enhance nurses’ ability to report.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Cumulative Index to Nursing and Allied Health Literature
Mixed Methods Appraisal Tool
United States
Institute of Medicine
World Health Organisation
Medication Error
Medication Administration Error
Preferred Reporting Items for Systematic reviews and Meta-Analysis guidelines
Donaldson MS, Corrigan JM, Kohn LT. To err is human: building a safer health system: National Academies Press; 2000.
Amaral RT, Bezerra ALQ, Teixeira CC, de Brito Paranaguá TT, Afonso TC, Souza ACS. Risks and occurrences of adverse events in the perception of health care nurses. Rev Rene. 2019;20:51. https://doi.org/10.15253/2175-6783.20192041302 .
Article Google Scholar
D'Amour D, Dubois CA, Tchouaket E, Clarke S, Blais R. The occurrence of adverse events potentially attributable to nursing care in medical units: cross sectional record review. Int J Nurs Stud. 2014;51(6):882–91. https://doi.org/10.1016/j.ijnurstu.2013.10.017 .
Article PubMed Google Scholar
Liu X, Zheng J, Liu K, Baggs JG, Liu J, Wu Y, et al. Hospital nursing organizational factors, nursing care left undone, and nurse burnout as predictors of patient safety: a structural equation modeling analysis. Int J Nurs Stud. 2018;86:82–9. https://doi.org/10.1016/j.ijnurstu.2018.05.005 .
Article CAS PubMed Google Scholar
Donaldson LJ, Kelley ET, Dhingra-Kumar N, Kieny MP, Sheikh A. Medication without harm: WHO's third global patient safety challenge. Lancet. 2017;389(10080):1680–1. https://doi.org/10.1016/S0140-6736(17)31047-4 .
Stewart D, Thomas B, MacLure K, Wilbur K, Wilby K, Pallivalapila A, et al. Exploring facilitators and barriers to medication error reporting among healthcare professionals in Qatar using the theoretical domains framework: a mixed-methods approach. PLoS One. 2018;13(10):e0204987. https://doi.org/10.1371/journal.pone.0204987 .
Article CAS PubMed PubMed Central Google Scholar
World Health Organization. Medication Without Harm-Global Patient Safety Challenge on Medication Safety.: World Health Organization; 2017 [Available from: https://apps.who.int/iris/bitstream/handle/10665/255263/WHO-HIS-SDS-2017.6-eng.pdf?sequence=1 .
World Health Organisation. Patient Safety: World Health Organisation; 2019 [Available from: https://www.who.int/news-room/fact-sheets/detail/patient-safety .
Stewart D, Thomas B, MacLure K, Pallivalapila A, El Kassem W, Awaisu A, et al. Perspectives of healthcare professionals in Qatar on causes of medication errors: a mixed methods study of safety culture. PLoS One. 2018;13(9):e0204801. https://doi.org/10.1371/journal.pone.0204801 .
Jha AK, Larizgoitia I, Audera-Lopez C, Prasopa-Plaizier N, Waters H, Bates DW. The global burden of unsafe medical care: analytic modelling of observational studies. BMJ Qual Saf. 2013;22(10):809–15. https://doi.org/10.1136/bmjqs-2012-001748 .
Holmström AR, Laaksonen R, Airaksinen M. How to make medication error reporting systems work--factors associated with their successful development and implementation. Health Policy. 2015;119(8):1046–54. https://doi.org/10.1016/j.healthpol.2015.03.002 .
Jember A, Hailu M, Messele A, Demeke T, Hassen M. Proportion of medication error reporting and associated factors among nurses: a cross sectional study. BMC Nurs. 2018;17(1):9. https://doi.org/10.1186/s12912-018-0280-4 .
Article PubMed PubMed Central Google Scholar
Albukhodaah AA. Barriers and perceptions to medication administration error reporting among nurses in Saudi Arabia 2016.
Wondmieneh A, Alemu W, Tadele N, Demis A. Medication administration errors and contributing factors among nurses: a cross sectional study in tertiary hospitals, Addis Ababa, Ethiopia. BMC Nurs. 2020;19(1):4. https://doi.org/10.1186/s12912-020-0397-0 .
Tang FI, Sheu SJ, Yu S, Wei IL, Chen CH. Nurses relate the contributing factors involved in medication errors. J Clin Nurs. 2007;16(3):447–57. https://doi.org/10.1111/j.1365-2702.2005.01540.x .
Al-Worafi YM. Medication errors. Drug Safety in Developing Countries: Elsevier; 2020. p. 59–71, DOI: https://doi.org/10.1016/B978-0-12-819837-7.00006-6 .
Ferrah N, Lovell JJ, Ibrahim JE. Systematic review of the prevalence of medication errors resulting in hospitalization and death of nursing home residents. J Am Geriatr Soc. 2017;65(2):433–42. https://doi.org/10.1111/jgs.14683 .
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53. https://doi.org/10.1111/j.1365-2648.2005.03621.x .
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Improving the content validity of the mixed methods appraisal tool: a modified e-Delphi study. J Clin Epidemiol. 2019;111:49–59.e1.
Bayazidi S, Zarezadeh Y, Zamanzadeh V, Parvan K. Medication error reporting rate and its barriers and facilitators among nurses. J Caring Sci. 2012;1(4):231–6. https://doi.org/10.5681/jcs.2012.032 .
Chiang HY, Pepper GA. Barriers to nurses' reporting of medication administration errors in Taiwan. J Nurs Scholarsh. 2006;38(4):392–9. https://doi.org/10.1111/j.1547-5069.2006.00133.x .
Vrbnjak D, Denieffe S, O'Gorman C, Pajnkihar M. Barriers to reporting medication errors and near misses among nurses: a systematic review. Int J Nurs Stud. 2016;63:162–78. https://doi.org/10.1016/j.ijnurstu.2016.08.019 .
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj. 2015;350(jan02 1):g7647. https://doi.org/10.1136/bmj.g7647 .
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1 .
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed methods appraisal tool (MMAT), version 2018. Registration of copyright. 2018;1148552:10.
Google Scholar
Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health. 2014;35(1):29–45. https://doi.org/10.1146/annurev-publhealth-032013-182440 .
Nourian M, Babaie M, Heidary F, Nasiri M. Barriers of medication administration error reporting in neonatal and neonatal intensive care units. J Patient Safety Qual Improve. 2020;8(3):173–81.
Abdullah HDA, Sameen FY. Barriers that Preventing the Nursing Staff from Reporting Medication Errors in Kirkuk City Hospitals. Kufa Journal for Nursing Sciences. 2017;7(1).
Amrollahi M, Khanjani N, Raadabadi M, Hosseinabadi M, Mostafaee M, Samaei S. Nurses' perspectives on the reasons behind medication errors and the barriers to error reporting. Nursing and Midwifery Studies. 2017;6(3):132–6. https://doi.org/10.4103/nms.nms_31_17 .
Alamrani HH. Nurses' perspectives on causes and barriers to reporting medication administration errors. Health Sci J. 2020;14(2):1–7.
Hammoudi BM, Ismaile S, Abu YO. Factors associated with medication administration errors and why nurses fail to report them. Scand J Caring Sci. 2018;32(3):1038–46. https://doi.org/10.1111/scs.12546 .
Dyab EA, Elkalmi RM, Bux SH, Jamshed SQ. Exploration of Nurses' Knowledge, Attitudes, and Perceived Barriers towards Medication Error Reporting in a Tertiary Health Care Facility: A Qualitative Approach. Pharmacy (Basel). 2018;6(4).
Alrabadi N, Haddad R, Haddad R, Shawagfeh S, Mukatash T, Al-rabadi D, et al. Medication errors among registered nurses in Jordan. J Pharm Health Serv Res. 2020;11(3):237–43. https://doi.org/10.1111/jphs.12348 .
Lee E. Reporting of medication administration errors by nurses in south Korean hospitals. Int J Qual Health Care. 2017;29(5):728–34. https://doi.org/10.1093/intqhc/mzx096 .
Yung HP, Yu S, Chu C, Hou IC, Tang FI. Nurses' attitudes and perceived barriers to the reporting of medication administration errors. J Nurs Manag. 2016;24(5):580–8. https://doi.org/10.1111/jonm.12360 .
Rutledge DN, Retrosi T, Ostrowski G. Barriers to medication error reporting among hospital nurses. J Clin Nurs. 2018;27(9–10):1941–9. https://doi.org/10.1111/jocn.14335 .
Bifftu BB, Dachew BA, Tiruneh BT, Beshah DT. Medication administration error reporting and associated factors among nurses working at the University of Gondar referral hospital, Northwest Ethiopia, 2015. BMC Nurs. 2016;15:43.
Shahzadi S, Afzal MM, Kousar MR, Waqasee MA. Barriers to Reporting Medication Administration Errors among Nurses in Services Hospital Lahore. 2017.
Dirik HF, Samur M, Seren Intepeler S, Hewison A. Nurses' identification and reporting of medication errors. J Clin Nurs. 2019;28(5–6):931–8. https://doi.org/10.1111/jocn.14716 .
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50(5):587–92. https://doi.org/10.1016/j.ijnurstu.2012.09.010 .
Wolf ZR, Hughes RG. Advances in Patient Safety Error Reporting and Disclosure. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008.
Alves MFT, Carvalho DS, Albuquerque GSC. Barriers to patient safety incident reporting by Brazilian health professionals: an integrative review. Cien Saude Colet. 2019;24(8):2895–908. https://doi.org/10.1590/1413-81232018248.23912017 .
Gleeson L, Dalton K, O'Mahony D, Byrne S. Interventions to improve reporting of medication errors in hospitals: a systematic review and narrative synthesis. Res Social Adm Pharm. 2020;16(8):1017–25. https://doi.org/10.1016/j.sapharm.2019.12.005 .
Browne F, Hannigan B, Harden J. A realist evaluation of a safe medication administration education Programme. Nurse Educ Today. 2020;104685:104685. https://doi.org/10.1016/j.nedt.2020.104685 .
Hurley SP, Berghahn MJ. Medication errors and criminal negligence: lessons from two cases. J Nurs Regulat. 2010;1(1):39–43. https://doi.org/10.1016/S2155-8256(15)30365-3 .
Lin YH, Ma SM. Willingness of nurses to report medication administration errors in southern Taiwan: a cross-sectional survey. Worldviews Evid-Based Nurs. 2009;6(4):237–45. https://doi.org/10.1111/j.1741-6787.2009.00169.x .
Force MV, Deering L, Hubbe J, Andersen M, Hagemann B, Cooper-Hahn M, et al. Effective strategies to increase reporting of medication errors in hospitals. J Nurs Adm. 2006;36(1):34–41. https://doi.org/10.1097/00005110-200601000-00009 .
Ramírez E, Martín A, Villán Y, Lorente M, Ojeda J, Moro M, et al. Effectiveness and limitations of an incident-reporting system analyzed by local clinical safety leaders in a tertiary hospital: prospective evaluation through real-time observations of patient safety incidents. Medicine (Baltimore). 2018;97(38):e12509. https://doi.org/10.1097/MD.0000000000012509 .
Download references
Acknowledgments
The authors wish to acknowledge the enormous contribution of Professor Kim Sue of Yonsei University, College of Nursing, in shaping this review.
The study received no funding.
Author information
Authors and affiliations.
College of Nursing, Yonsei University, 50-1, Yonsei-ro, Seodaemun-gu, Seoul, 03722, South Korea
Agani Afaya, Kennedy Diema Konlan & Hyunok Kim Do
School of Nursing and Midwifery, University of Health and Allied Sciences, Ho, Ghana
Agani Afaya & Kennedy Diema Konlan
You can also search for this author in PubMed Google Scholar
Contributions
AA, KDK, and HDK conceived the idea and conceptualized the study. AA and KDK wrote the manuscript. HDK provided expert review in the context of patient safety. All authors read and gave final approval for the final version to be published and agreed to be accountable for all aspects of the work.
Corresponding author
Correspondence to Agani Afaya .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Supplementary Information
Additional file 1..
Search strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Afaya, A., Konlan, K.D. & Kim Do, H. Improving patient safety through identifying barriers to reporting medication administration errors among nurses: an integrative review. BMC Health Serv Res 21 , 1156 (2021). https://doi.org/10.1186/s12913-021-07187-5
Download citation
Received : 23 February 2021
Accepted : 18 October 2021
Published : 25 October 2021
DOI : https://doi.org/10.1186/s12913-021-07187-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Integrative review
- Medication administration error
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
What causes medication administration errors in a mental health hospital? A qualitative study with nursing staff
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Centre for Pharmacoepidemiology and Drug Safety, Division of Pharmacy and Optometry, School of Health Sciences, Manchester Academic Health Sciences Centre (MAHSC), University of Manchester, Manchester, United Kingdom, NIHR Greater Manchester Patient Safety Translational Research Centre, MAHSC, University of Manchester, Manchester, United Kingdom, Medicines Management Team, Greater Manchester Mental Health NHS Foundation Trust, Park House Hospital, North Manchester General Hospital, Manchester, United Kingdom
Roles Data curation, Investigation, Methodology, Writing – review & editing
Affiliation Centre for Pharmacoepidemiology and Drug Safety, Division of Pharmacy and Optometry, School of Health Sciences, Manchester Academic Health Sciences Centre (MAHSC), University of Manchester, Manchester, United Kingdom
Roles Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Writing – review & editing
Affiliations Medicines Management Team, Greater Manchester Mental Health NHS Foundation Trust, Park House Hospital, North Manchester General Hospital, Manchester, United Kingdom, School of Health and Human Sciences, University of Bolton, Bolton, United Kingdom
Roles Conceptualization, Investigation, Project administration, Supervision, Writing – review & editing
Affiliation Medicines Management Team, Greater Manchester Mental Health NHS Foundation Trust, Park House Hospital, North Manchester General Hospital, Manchester, United Kingdom
Roles Conceptualization, Project administration, Supervision, Writing – review & editing
Roles Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Writing – review & editing
Affiliations Centre for Pharmacoepidemiology and Drug Safety, Division of Pharmacy and Optometry, School of Health Sciences, Manchester Academic Health Sciences Centre (MAHSC), University of Manchester, Manchester, United Kingdom, NIHR Greater Manchester Patient Safety Translational Research Centre, MAHSC, University of Manchester, Manchester, United Kingdom
- Richard N. Keers,
- Madalena Plácido,
- Karen Bennett,
- Kristen Clayton,
- Petra Brown,
- Darren M. Ashcroft

- Published: October 26, 2018
- https://doi.org/10.1371/journal.pone.0206233
- Reader Comments
Medication administration errors (MAEs) are a common risk to patient safety in mental health hospitals, but an absence of in-depth studies to understand the underlying causes of these errors limits the development of effective remedial interventions. This study aimed to investigate the causes of MAEs affecting inpatients in a mental health National Health Service (NHS) hospital in the North West of England.
Registered and student mental health nurses working in inpatient psychiatric units were identified using a combination of direct advertisement and incident reports and invited to participate in semi-structured interviews utilising the critical incident technique. Interviews were designed to capture the participants’ experiences of inpatient MAEs. All interviews were transcribed verbatim and subject to framework analysis to illuminate the underlying active failures, error/violation-provoking conditions and latent failures according to Reason’s model of accident causation.
A total of 20 participants described 26 MAEs (including 5 near misses) during the interviews. The majority of MAEs were skill-based slips and lapses (n = 16) or mistakes (n = 5), and were caused by a variety of interconnecting error/violation-provoking conditions relating to the patient, medicines used, medicines administration task, health care team, individual nurse and working environment. Some of these local conditions had origins in wider organisational latent failures. Recurrent and influential themes included inadequate staffing levels, unbalanced staff skill mix, interruptions/distractions, concerns with how the medicines administration task was approached and problems with communication.
Conclusions
To our knowledge this is the first published in-depth qualitative study to investigate the underlying causes of specific MAEs in a mental health hospital. Our findings revealed that MAEs may arise due to multiple interacting error and violation provoking conditions and latent ‘system’ failures, which emphasises the complexity of this everyday task facing practitioners in clinical practice. Future research should focus on developing and testing interventions which address key local and wider organisational ‘systems’ failures to reduce error.
Citation: Keers RN, Plácido M, Bennett K, Clayton K, Brown P, Ashcroft DM (2018) What causes medication administration errors in a mental health hospital? A qualitative study with nursing staff. PLoS ONE 13(10): e0206233. https://doi.org/10.1371/journal.pone.0206233
Editor: Mojtaba Vaismoradi, Nord University, NORWAY
Received: June 1, 2018; Accepted: October 9, 2018; Published: October 26, 2018
Copyright: © 2018 Keers et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The dataset used to generate the findings of the study was the complete dataset and not a minimal dataset – the complete dataset was not reduced or adapted for analysis. This qualitative study took place in a single UK mental health hospital with a participant group restricted to nursing staff. Our university research ethics committee (UREC) approval for this study was granted based on the anonymity of participants discussing events that some may consider sensitive. Making the full anonymised interview transcripts publicly or privately available could therefore potentially lead to the identification of participants. Specifically, our ethical approval was based upon statements in the participant information sheets and consent forms that referred to only anonymised quotations from transcripts being used in study outputs; the participants did not consent to their full transcript being made publically available or shared with anyone outside the research team, except to responsible individuals from the University of Manchester, from regulatory authorities or from the participating NHS Trust, where it is relevant to them taking part in the research. The researchers are therefore not permitted to share the anonymised interview transcripts outside the research team unless this is to participants who request their own transcribed interview data privately or to appropriate individuals for regulatory purposes. Please contact the research team for further details if required. Address of the university research ethics department who approved this study: Directorate of Research and Business Engagement Support Services, 2nd Floor Christie Building, University of Manchester, Oxford Road, Manchester M13 9PL.
Funding: This work was supported internally by The University of Manchester and participating NHS trust, no specific grant or funding stream was used. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Mental health illness is common and has a significant detrimental impact on societies and national economies [ 1 , 2 ]. Patients with these illnesses are a complex and vulnerable patient group with a high risk of premature mortality [ 3 ]. They are known to have high burdens of physical co-morbidity [ 4 ], do not always access appropriate health care and may suffer inequalities in the care they are provided [ 5 , 6 ].
The use of medicines to treat mental illness is a mainstay of modern practice [ 7 ]. However, psychotropic polypharmacy [ 8 – 10 ], unlicensed psychotropic prescribing [ 11 ], and use of high risk medications such as lithium, depot antipsychotics and clozapine [ 12 ] are common in this population and present unique challenges for safe medication use. To compound the risks to patient safety that these issues create, prescribed medications may frequently change during psychiatric hospital admission [ 13 ] and not all mental health service users may feel involved in decisions about their drug treatment [ 14 ]. The way medicines are managed in hospital settings may also differ to general hospitals; for example in the United Kingdom (UK) patients may receive medication from a trolley located centrally and trained ‘runners’ such as health care assistants may take medication dispensed by nurses to patients on the ward [ 15 , 16 ]. There is also emerging evidence that medicine-related factors may play a role in causing re-admission to mental health hospitals [ 17 , 18 ]. This clearly highlights the importance of studying the quality and safety of medicines use in mental health settings, and there is growing international consensus on this issue [ 19 , 20 ].
A recent systematic review of medication safety in mental health hospitals found that prescribing errors and medication administration errors (MAEs) were common in this setting, and that patients were often harmed by preventable medication related adverse events [ 21 ]. Indeed, MAEs may be the most commonly reported medication error in mental health hospitals [ 22 , 23 ], with direct observation studies finding MAE rates of 3.3–48% of doses administered or omitted [ 24 – 26 ].
Whilst there is emerging evidence of the prevalence and nature of MAEs in mental health hospitals, an in-depth understanding of the underlying causes of these errors remains absent [ 21 ]. This is an important knowledge gap in the current evidence base, as the causes of MAEs in mental health hospitals may be different to general hospitals and a clearer understanding of the underlying causes of MAEs in this specialist setting could inform the design of effective interventions [ 27 ]. To date, available evidence of MAE causation in mental health settings is limited to quantitative analysis of observation data [ 24 – 26 ] (which cannot capture internal mental processes like intention), incident report reviews [ 22 , 23 , 28 ] (which often report limited descriptions of MAE causation) and more general explorations of medicines administration practices [ 15 , 16 ] or related knowledge/competency [ 29 ]. Whilst these studies are useful in identifying some of the important MAE antecedents, including those that might differ to general hospitals (e.g. ‘runners’ [ 22 , 23 ] and disturbed patients [ 22 ]), they do not provide a comprehensive account of the causal chain leading to error, nor how various factors may interconnect under different circumstances to lead to MAEs [ 27 , 30 ]. Therefore, this study aimed to investigate in-depth the underlying causes of MAEs in a mental health National Health Service (NHS) hospital.
Definitions
Medication incidents were included in the study if they met the following definitions. Medication administration errors (MAEs) were defined as ‘a deviation from the prescriber’s order as written on the patient’s chart, manufacturer’s instructions or relevant institutional policies’ [ 27 , 30 ]. Our definition of an MAE encompassed ‘near misses’ that were prevented from reaching the patient by any means [ 31 ]. Our analysis of the underlying causes of MAEs was informed by established human error theory, the components of which are defined later in this manuscript (see ‘Data Analysis’).
Student and registered mental health nurses (RMNs) were recruited between March-July 2015 from one mental health hospital in the North West of England. The hospital had a total of 9 adult inpatient units catering for a variety of mental health illnesses including acute care, intensive care, later life and rehabilitation.
At the time the study was carried out, the study hospital utilised paper-based prescribing and an electronic patient record system. Medicines administration involved patients attending the ward clinic room to receive their medications (except later life wards). Medications were prepared for individual patients sequentially during medication rounds; pre-preparing medications or preparing multiple medications simultaneously for different patients was not recommended. Most oral medicines were authorised to be administered by a single qualified nurse, but in practice a second ‘runner’ (often a trained health care assistant or nurse) was frequently utilised to bring patients to the clinic room or to take medications to the patient directly. A group of ‘high risk’ medications including all injectable medicines (e.g. insulin, depot antipsychotics) and controlled drugs required two authorised members of staff to check and sign for administration; this most often involved two qualified nurses. Student nurses were only permitted to administer medications to patients under the direct supervision of a registered (qualified) nurse.
Recruitment
Both student nurses and RMNs were eligible to participate provided they were working on mental health inpatient units at the time the MAE was made and were willing to discuss the causes of at least one of these incidents that they had been directly involved with. Near misses were included as MAEs as they also provide windows into the safety of systems, and student nurses were considered eligible to take part alongside RMNs in order to provide further diverse perspectives on what factors influence medication administration errors.
Participants were recruited to the study in three ways:
- Nursing staff who recorded MAEs using the local incident reporting system during and up to 6 months before the study began were identified and approached by the research team. This system allowed those reporting incidents to be identified by senior management and medicines safety staff for improvement, quality control and governance purposes,
- Local members of the medicines management team who identified MAEs on their inpatient wards reported these to the research team, who then approached the nursing staff member involved, and
- Members of the research team directly advertised the study to inpatient nursing staff during ward visits and using posters located in clinical ward areas.
Potential participants were then offered information packs (cover letter and participant information sheet) about the study. Anyone then interested in taking part contacted a member of the research team to arrange an interview. Written consent was provided before interviews took place.
Data collection
The interview guide used in this study was adapted for the mental health setting following successful use by the research team investigating the causes of MAEs in UK general hospitals [ 30 ]. The interview guide can be found in the Appendix ( S1 Appendix ). Briefly, participants were asked to provide basic background demographic information before discussing one or more MAEs that either reached or did not reach the patient (near misses) that they were directly involved with. Emphasis was placed on recalling in detail the circumstances of the incident and what the participant thought caused it to happen. The interviews closed with participants providing insights into what they felt could have prevented their error from occurring.
Research team members RNK and MP conducted interviews face-to-face and following a semi-structured format with each participant. Each interview was digitally audio-recorded (with the exception of one interview, where the participant preferred written notes to be made instead) and lasted between 10–42 minutes. Research team members RNK and MP were both trained in qualitative interviewing and co-interviewed 3 participants (with their permission) in order to achieve consistency in interview style.
The design of the interview guide and overall approach to the interviews was based on the critical incident technique (CIT) [ 32 ]. The CIT has been successfully applied to help understand the causes of inpatient prescribing [ 33 ] and medication administration errors [ 30 , 34 ], and facilitates the collection of rich and relevant data from otherwise busy ward staff by focusing on exploring their specific intentions, behaviours and actions when a particular error or near miss occurred [ 35 ].
Data analysis
Interviews were transcribed verbatim. Transcripts were organised and coded using the NVivo computer software program (v10) according to the Framework method [ 36 ]. Framework is a seven step analytical approach designed to be systematic and transparent so that the process of translating raw data into emerging themes is clear [ 37 ]. Data are organised in matrices and summarised in individual cells so they can be reduced and compared across participants without losing context within individual accounts. The stages of analysis are as follows: the interviews are transcribed and researchers become familiar with it; then the data are coded and the conceptual framework is developed before being tested and applied; and finally the data are summarised in matrices and interpreted (e.g. by connecting themes/cases, or by developing typologies). Researchers are free to move between these analytical stages as required to refine concepts [ 36 , 37 ].
The analysis framework was informed by Reason’s model of accident causation [ 38 , 39 ]. Earlier research has applied this model to understand the causes of medication errors [ 27 , 30 , 33 , 40 ], and it has been described in the context of MAE research in detail elsewhere (including summary diagrams of how Reason’s model applies to MAE research) [ 27 , 30 ]. Reason’s model is summarised in Fig 1 . Data were coded as active failures, error/violation provoking conditions and latent (wider organisational) failures, and one author (KB) independently extracted and analysed data for 10 interviews in order to confirm the suitability of the coding framework. Each MAE type (e.g. dose omission) was assigned by the research team [ 30 ]. Active failure assignments were confirmed following review and discussion between RNK and DMA.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0206233.g001
Ethical approval
The study was approved by the University of Manchester Research Ethics Committee 2 (submission 15104) and by the research and development department at the participating NHS trust.
Twenty participants described a total of 26 MAEs, including 5 ‘near misses’ that did not reach the patient. No errors resulted in patient harm. A summary of interview participants and the MAEs they described can be found in Table 1 . The majority of errors involved medications used to treat central nervous system (CNS) disorders (n = 21), and most commonly involved either wrong drug (n = 7), wrong patient (n = 5) or wrong dose errors (n = 4). The reported MAEs involved nurses of varying levels of experience post-qualification, with over half occurring when participants had 1 year or less (n = 14, 54%) experience (including 2 student nurse errors) and 7 (27%) when nurses had more than 5 years’ experience. Each error and near miss (active failure) was preceded by combinations of underlying error and violation provoking conditions, as exemplified in Fig 2 that describes the active failures and error provoking conditions underpinning one MAE discussed in this study.
https://doi.org/10.1371/journal.pone.0206233.t001
https://doi.org/10.1371/journal.pone.0206233.g002
Active failures
Sixteen of the MAEs reported by participants involved skill based slips and lapses (n = 13 slips), with the remainder either knowledge (n = 4) or rule based mistakes (n = 1), and violations (n = 1). Some events could not be categorised as active failures as another staff member was more prominently involved (n = 4).
Slips and lapses.
Skill based errors often resulted in nurses selecting the wrong product (drug or dosage) or overlooking or misinterpreting important information. One experienced nurse described how she administered co-codamol instead of codeine whilst busy and could only recall that the patient was prescribed co-codamol previously:
“… but the gentleman in question had been on co-codamol since he’d been here, and he’d only just been changed to codeine. So, in my head, I saw the codeine, but because I was that busy I thought, oh he’s been on co-codamol since he’s got here, so that’s why I gave him it [co-codamol].” (N14, > 5 years’ experience)
Knowledge and rule based mistakes.
In contrast to skill based errors, knowledge and rule based mistakes involved flawed planning. In one account, a junior nurse was not certain of her knowledge when faced with a novel problem:
“I think because I was newly qualified and it [how to dose ‘when required’ medications over 24 hours] hadn’t really been explained very well, so I thought that they could have two [doses] in a day so, say, today they could have two today, and then two lots tomorrow. But, you have to do it from the time, don’t you…” (N10, < 1 year)
Violations.
There was one reported violation, which involved the administration of levothyroxine to the wrong patient after a nurse who did not routinely work on the ward in question misidentified a service user using only their name and not their date of birth as recommended in the local policy for medicines administration.
Error and violation provoking conditions
The health care team..
Problems with written and verbal communication were discussed by 11 participants, and commonly led to skill-based errors and mistakes when staff missed, misinterpreted or made assumptions about information whilst working under challenging conditions (such as high workload, noisy environments, and distractions from staff or patients).
Written communication problems concerned prescriptions that were ambiguous because they had parts crossed out or were unclearly written, as well as previous medicines administration records that were not correct or were omitted. Problems with verbal communication were less common (n = 4 errors) but commonly involved communication breakdown between two staff members (e.g. between nurse and ‘runner’ who administered medication to the patient) and the use of using only the patient name for identification.
Three nurses discussed how a close working relationship with colleagues led to errors when working together to administer medications, with one experienced nurse revealing how he made an assumption about which patient was being discussed with his trusted colleague before making a skill based error and administering medication to the wrong patient:
“… I presumed that he [nursing colleague] knew I was talking about somebody else [medication to be administered], […] but I was just working on the assumption that he knew what I was thinking, which is quite strange really. Looking back, with hindsight, it seems stupid, but I suppose when you’re busy and you’re rushing, then it’s just one of those things.” (N11, > 5 years)
Supervision and support were identified as an important barriers to error by participants, as deficiencies in these areas were frequently raised by participants as contributing to their errors or near misses, and by junior staff members in particular (though two examples of different errors occurred despite direct support). Participants discussed making both skill-based and planning errors as a consequence. Lone working was frequently implicated in these errors as this often caused anxiety which distracted participants, added to their workload if there were certain tasks only qualified nurses could perform (e.g. obtaining money from the safe) and gave them limited options for clarification in cases of uncertainty. One recently qualified nurse described how lone working during medicines administration limited her options for clarification which contributed to a knowledge based mistake:
“And, as a newly qualified I was left on my own, like, the only qualified nurse… […] … I wasn’t able to ask another nurse, I wasn’t able to check with them, because I was just on my own. Obviously, the patient was getting really upset and agitated, so I think that was probably another reason why I gave it [dose] a bit early.” (N10, < 1 year)
The individual nurse.
The majority of participants highlighted how considerable stress, nervousness (particularly amongst junior nurses) and feelings of pressure to complete tasks contributed to their errors and near misses; these mental states were driven primarily by high workload, low staffing, inexperience, patient acuity and inadequate skill mix and led to inappropriate decision making and skill based errors through lack of concentration or rushing.
Along with undergraduate students, new or recently qualified nursing staff in particular described how their unfamiliarity with certain medications (e.g. depot antipsychotics) and patients contributed to errors. Two nurses commented on how semi-sodium valproate was used “a lot more” (N03, > 5 years) on their wards compared to sodium valproate, which contributed to misidentification of these medicines through prior expectations.
When left on their own, junior nurses reported burdensome feelings of responsibility when working in isolation and questioned their readiness to cope with this role which put further pressure on themselves, causing mental distraction and flawed decision-making.
“I think I was naturally more anxious for that shift anyway because I was the only nurse on [the ward] and it was the first time so you’ve got that…I don’t know if it’s relevant but what I got was getting really anxious, like, what if I can’t manage it, I’ve only been qualified a few months, what if something goes wrong and it comes back on me, I’m looking after 20 patients on my own, I haven’t been qualified long. So I think there was an underlying anxiety as well that maybe I was also distracted by that when I was dispensing the medication which did probably have an effect as well.” (N01, < 1 year)
Greater experience was highlighted as a protective barrier to error by one nurse who commented on how this gave them confidence to challenge patient demands in the interests of safety, rather than trying to respond immediately (and rushing) to meet their requests:
“… I’ve learnt over the years that some things don’t have to be done immediately, you know, you have to prioritise and especially where medicines are concerned, you need to do it right, so if it means taking an extra half hour, then unfortunately I’d just explain to the patient, you’re just going to have to wait half an hour before you can go on your leave.” (N02, < 1 year)
The patient.
Patient mental illness, behaviours (e.g. agitation, hostility) and requests contributed to every active failure. One nurse described how a lack of ward staffing meant that patients were not receiving attention and were instead interrupting staff with requests, leading to a skill-based slip:
“… there wasn’t enough staff and the patients obviously weren’t getting probably the attention that they wanted, so they did keep coming [to see staff], because some patients are demanding and they do want a lot of time off staff, which you can’t always give if you’re busy.” (N06, 1–5 years)
Another participant who reported a violation described how a patient’s mental illness meant they did not intervene despite being addressed with the wrong name and given incorrect medications:
“But I remember I think because I was talking to the patient and saying their name, and over and over, and saying how are you doing today, da-da-da, and talking to them, I think the patient was very withdrawn and didn’t really talk too much with me and never really corrected me, I just assumed that that was fine and that that was the [correct] person.” (N20, 1–5 years)
Other participants revealed how persistent demands from often agitated and aggressive patients led to them yielding to these requests despite their own uncertainties, due in part to lack of staff support/lone working and inadequate confidence, experience and/or knowledge. This was exemplified by one account of a wrong drug error involving a depot antipsychotic when the participant was a junior nurse, where patient distraction combined with multi-tasking, workload pressures and a change in prescription contributed to the pathway to error:
“I think I wasn’t familiar with the [depot] chart, because they changed, I let the patient mither [pester] me, she was, like, I want to go [leave the ward], I want to go, can you do it? And I was trying to do two things at once and because it was a depot [antipsychotic administration], it’s outside of your normal medicine round, so I think I was under other pressures and I was, like, oh, just get her depot done and then she can go on her leave, sort of thing, then it’s one less person around my feet asking for something, which is wrong, I can see that now, but at the time, you know, it’s quite easy to get drawn into…and really what I should have done to her was said, you’re just going to have to wait five minutes, just have a seat, let me just go and…and then I think if I’d have just took that extra couple of minutes, I wouldn’t have picked the wrong [medication] card up.” (N02, < 1 year)
The working environment.
The majority of participants (n = 17) described working environments that were noisy, chaotic, and/or busy. Some participants used the term “acute” (N15, < 1 year) to describe the ward conditions, which highlighted instances where there were multiple unwell/agitated patients or general disruption present. Many described how patients queued outside the clinic room to receive their medication, creating noise and asking questions of staff. This type of environment led to distractions and interruptions, high workload and rushing, and when combined with other factors led to both skill-based and planning errors as nurses were not able to focus on the medicines administration task.
“Rushed, there were lots of people milling around in the corridor, there were doctors running on and off the ward requesting prescription charts, there were medical students who were doing bloods on another patient in the clinic at the same time, so it was really crowded, it just felt really…just really rushed, I had to get the medication round finished to get on with the rest of the day […] One of the medical students was asking me where the blood bottles and needles were.” (N01, < 1 year)
Distractions and interruptions were implicated in more than half of the incidents reported and the majority resulted in skill-based errors. Their origins were multifactorial, including high workload, patient factors, staff/skills mix issues and other activities taking place during the medication round (e.g. ward rounds).
High perceived workload, inadequate skill mix and particularly low staffing were major themes interconnecting the majority of errors. Low staffing was reported to be common place and appeared chronic in some cases, with causes including sickness, annual leave and wards acting as a staff “donor” (N11, > 5 years) to others requiring personnel. As a result, some staff reported working longer hours or being left on their own as the only qualified nurse during shifts, adversely affecting workload and nurse mental state.
Many participants felt that using agency nurses in response to staff shortages added to their workload and mental burden due to their perceived deficiencies in skill level and lack of familiarity with the ward, its patients and practices. One nurse felt she could not use agency staff for support when faced with a knowledge deficit:
“… which is another issue, agency staff only. They don’t know the ward, they don’t know the patients, so you’re the only qualified with three or four agency staff only, who don’t have the ward, who don’t know the patients. So you can’t rely on them. All you need to do is to rely on yourself, you know?” (N08, 1–5 years)
The medicines.
Medicines that sounded and/or looked a-like were discussed as contributory factors to error on four occasions, with three involving mix-ups between semi-sodium and sodium valproate. Four participants also described how storage of multiple pre-prepared depot syringes and other medicines (mainly valproate) next to each other contributed to selection errors.
Nursing staff emphasised how easy it was for them to mistake valproate products for one another, with one more experienced nurse describing how similarities in how they are written contributed to a skill-based slip:
“… because, you know, there’s only the ‘semi’ different and it was the same amount, same dose, you know, the same amount, same times and everything, it [sodium valproate] did look very much, you know, very similar [to semi sodium valproate] …” (N03, > 5 years)
The medicines administration task.
Challenging ward conditions appeared to affect the perceptions of nursing staff towards the medicines administration task. Participants described rushing medicines administration in order to carry out other tasks or to prioritise a competing demand (e.g. patient needs), with one experienced nurse reporting doing so because they felt isolated in the clinic room and out of control from the rest of the ward, resulting in medications being given to the wrong patient.
“… the reason that I was hurrying was because I wanted to get out of the clinic. I just wanted to make sure the medication was done and dusted, and then you can get back onto the ward. Because when you’re in the clinic, […] you don’t really know what’s going on, on the ward. And on a ward like [Ward name], it’s…you need to be aware of what’s going on at all times.” (N11, > 5 years)
There was evidence of deficiencies relating to medicine double checking practices as well as patient identification. Although double checking was in place as a defensive barrier to error, MAEs occurred during both single (majority of medicines) and dual practitioner administration (e.g. controlled drugs, student nurses, depots, use of ‘runners’ to administer medication). For dual practitioner errors, examples included cases where either double checking did not take place, both staff members involved made the same mistake or information was miscommunicated between parties. Despite this, one nurse mentioned the protective effects of cross-checking for patient safety:
“Yeah there is [cross checking each other’s work] at times because like say sometimes things [medications] get changed from ward round but only one nurse is in there and then it might not always get handed over, but then it can be a good time for them to hand over that medication might have changed or things like that. It sort of jogs your memory sometimes.” (N18, < 1 year)
Latent (wider organisational) failures.
Whilst not identified as frequently as error/violation provoking conditions by participants, latent failures were reported as underpinning the emergence of staffing, skill mix and workload issues. One nurse suggested that the ward shift roster system was partly responsible for low staffing on their unit, and more than one participant commented that it was difficult for managers to identify staff replacements and for agencies to fill staff vacancies leading to skill mix and staffing problems. There were also suggestions that nurses were not allocated ‘protected time’ to administer medications on the ward and that scheduling ward rounds and patient meetings at the same time as medicines administration depleted available staff and increased workload.
To our knowledge, this is the first study to explore the causes of specific MAEs in a mental health hospital using in-depth qualitative interviews. Each MAE was reported to be caused by a combination of local error/violation provoking conditions relating to the patient, the health care team, the working environment, the medicines administration task, the individual nurse and the particular medicines involved, with wider organisational latent failures underpinning the emergence of many of these local conditions.
Implications of findings
This study has brought into sharp focus the complexity of medicines administration on mental health wards and builds significantly on earlier work in the context of patient safety [ 15 , 16 , 21 – 23 , 28 , 29 ]. It is apparent that medicines administration regularly takes place in physically and cognitively demanding circumstances that could compromise defensive barriers and promote the occurrence of MAEs, and we have identified factors influencing the safety of medicines administration processes which are unique to this environment. We gathered in-depth accounts from nurses with different levels of experience who reported making errors across different mental health specialities. Our findings suggest that newly qualified staff might be particularly vulnerable and require additional support as a defensive barrier to help them practise safely and with confidence. The knowledge of the underlying causes of MAEs generated by this study will be an important contributor in the ongoing agenda to enhance mental health service quality [ 41 , 42 ], and in informing the optimisation and evaluation of ward based medicines management services.
Whilst there are some similarities between the findings of our study and in-depth research of MAE causation in general hospitals across areas such as low staffing, interruptions, high workload and task management/double checking deficiencies [ 27 , 30 ], our study has identified more context specific targets such as the impact of lone working and patient-related needs or behaviours (e.g. demands, aggression, lack of engagement).
A number of themes emerged as influential antecedents to multiple errors discussed in this study, and were also found to be linked to other causative factors. These are described below. However, it is important to recognise that whilst each theme might individually be isolated and mitigated to reduce the risk of error, future efforts to develop remedial interventions could consider a multifaceted approach to maximise positive impact as the MAEs in this study were often caused by interacting factors across multiple themes [ 27 , 30 , 43 ].
Low staffing and inadequate skill mix
These themes preceded most MAEs and have emerged as quality measures in mental health with guidance being produced in the UK [ 44 , 45 ]. There are a number of tools available to assess staffing levels [ 46 ] but there remains a need for those tailored to the mental health setting [ 47 , 48 ]. Although the use of temporary staff in the mental health setting is a long-standing issue [ 49 ], with agency staff associated with a high cost burden [ 45 ], our study adds an important perspective to this narrative if nurses consider agency staff as creating problems in the medicines safety context. Mental health organisations are now considering more creative options to manage qualified nursing shortages [ 50 ]. However, the evidence of impact of staffing in relation to medicines safety is limited [ 48 , 51 – 52 ] and further research could therefore measure, understand and mitigate these influential causative factors.
Disruptive and distracting working environments
The busy working environment, and in particular distractions and interruptions, were highly influential in skill-based slips and lapses. These factors feature prominently in earlier studies of error causation in mental health [ 22 , 23 , 28 , 29 ] but our findings add much needed contextual detail, and place more emphasis on patient-led causes of distractions and interruptions compared to evidence from general hospitals [ 27 , 30 ] which could be crucial for the design of remedial interventions [ 53 ].
Individual stress/pressure and task management
This study has emphasised the mental demands of the nursing role and the important influence this has on how nurses prioritise and carry out their duties. Previous studies have highlighted significant workplace stress for mental health nurses [ 54 ] and how mental workload can impact prescribing [ 33 ] and medicines administration safety in general hospitals [ 30 , 55 ]. This indicates a need for more in-depth understanding of how factors such as patient advocacy, risk/benefit judgement and other personal and environmental circumstances affect decision-making in the medicines administration context in mental health. It may be useful to utilise techniques such as observation and hierarchical task analysis to characterise and predict the risks to medicines administration safety for nurses on the mental health ward, as seen in general hospitals [ 56 , 57 ].
Communication
We identified communication deficiencies that were both common to other settings (e.g. illegible prescriptions) but also unique to mental health settings (e.g. between nurses and ‘runners’ [ 22 , 23 , 16 ]). Communication deficiencies appear as frequent contributors to error in incident report studies in mental health hospitals [ 22 , 23 , 28 , 29 ] though detail as to their nature which we identified is rarely provided. Whilst electronic prescribing and medicines administration systems are being introduced to improve medicines safety, there is evidence that nursing documentation discrepancies increase [ 58 ], and to our knowledge there have been no published evaluations of the impact of such systems in the mental health setting to date. Understanding and improving verbal communication between colleagues and with patients during medicines administration in the context of drug safety appears to be a subject of limited research [ 43 , 59 ].
Strengths and limitations
Strengths of this study include a focus on obtaining relevant data by restricting participant accounts to only examples in which they were directly involved. We used established data collection and analysis methods, though we did not triangulate with other methods such as observation which may help distinguish between what people say and what actually occurred. The research team also noted emerging data saturation at approximately the half way point of interviews which may have helped to ensure adequate coverage of the important contributory factors to MAEs.
The possibility of recall and hindsight bias cannot be excluded particularly as we asked participants identified from incident reports to recount events from up to 6 months previously, although the risk was minimised by asking participants to discuss events occurring within recent memory or those they could remember clearly. The risk of social desirability bias [ 60 ] may have been minimised as CIT was used to focus on actual actions and behaviours of participants, and attribution bias [ 61 ] may have also been minimised as the experience of the data collectors was that participants accepted their measure of responsibility for MAEs or near misses, and did not readily blame others.
This study found that MAEs occurring in a UK mental health NHS hospital are each caused by a combination of interconnecting local error provoking conditions and latent ‘systems’ failures. Key antecedents to multiple types of MAE and thus central contributors to error were identified and included low staffing, inadequate skill mix, challenging ward environments (including patient factors), interruptions and distractions and communication problems. Future research efforts should be directed toward developing, testing and evaluating practical interventions designed to target these known causative factors, in order to offer informed recommendations to improve front line clinical services for the benefit of patients through reduced MAE rates.
Supporting information
S1 appendix..
https://doi.org/10.1371/journal.pone.0206233.s001
Acknowledgments
We would like to thank all the registered and student mental health nurses who agreed to take part in this study.
- 1. The Organisation for Economic Co-operation and Development (OECD). Making Mental Health Count: The Social and Economic Costs of Neglecting Mental Health Care. [Internet]. 2014. Available from: http://www.keepeek.com/Digital-Asset-Management/oecd/social-issues-migration-health/making-mental-health-count_9789264208445-en#.WYGQYvn6EZ8#page2 [Last accessed: 31/05/2018].
- View Article
- PubMed/NCBI
- Google Scholar
- 7. Harris N, Baker J, Gray R, eds. Medicines Management in Mental Health Care. Chichester, UK: Wiley-Blackwell; 2009.
- 12. Taylor D, Paton C, Kapur S. The Maudsley Prescribing Guidelines in Psychiatry, 12 th Ed. Chichester, UK: Wiley Blackwell; 2015.
- 14. National Collaborating Centre for Mental Health and British Psychological Society. Service user experience in adult mental health: Improving the experience of care for people using adult NHS mental health services. [Internet]. 2012. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0079707/ [Last accessed: 31/05/2018].
- 20. World Health Organization and Calouste Gulbenkian Foundation. Improving access to and appropriate use of medicines for mental disorders. [Internet]. 2017. http://www.who.int/mental_health/management/improving_access_medicines_mental_disorders/en/ [Last accessed: 31/05/2018].
- 31. Smetzer JL, Cohen MR. Medication error reporting systems. In: Cohen MR (ed). Medication errors. 2 nd edition. Washington DC, US: American Pharmacists Association; 2007. p513–514.
- 36. Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A., Burgess RG., eds. Analysing Qualitative Data. London, UK: Routledge 1994:172–194.
- 38. Reason J. Human Error. Cambridge, UK: Cambridge University Press; 1990.
- 39. Reason J. Managing the risks of organizational accidents. Aldershot, UK: Ashgate Publishing Limited; 1997.
- 41. The Mental Health Taskforce. The five year forward view for mental health. [Internet]. 2016. https://www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf [Last accessed: 31/05/2018].
- 44. National Institute for Health and Care Excellence. Safe staffing for nursing in adult inpatient wards in acute hospitals. [Internet]. 2014. https://www.nice.org.uk/guidance/sg1 [Last accessed: 31/05/2018].
- 45. Royal College of Nursing. Guidance on safe nurse staffing levels in the UK. [Internet]. 2010. https://www.rcn.org.uk/about-us/policy-briefings/pol-003860 [Last accessed: 31/05/2018].
- 48. Rutter L, Kavanagh J, Fields E. Safe staffing for nursing in inpatient mental health settings: draft evidence review. National Institute for Health and Care Excellence (NICE). [Internet]. 2015. https://www.nice.org.uk/media/default/news/safe-staffing-mental-health-inpatient-evidence-review.pdf [Last accessed: 31/05/2018].
- 60. Sheth JN, Malhotra NKGrimm P. Social desirability bias. In: Sheth JN, Malhotra NK, eds. Wiley international encyclopedia of marketing. John Wiley and Sons Ltd [Internet], 2010. http://onlinelibrary.wiley.com/doi/10.1002/9781444316568.wiem02057/abstract [Last accessed: 31/05/2018].

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Annotated bibliography: an update to: "Understanding ambulatory care practices in the context of patient safety and quality improvement."
Kumar PR, Nash DB. Annotated Bibliography: An Update to “Understanding Ambulatory Care Practices in the Context of Patient Safety and Quality Improvement”. Am J Med Qual. 2020;36(3):185-196. doi:10.1177/1062860620938762.
The outpatient setting is receiving increased attention as a research focus in patient safety. This bibliography provides an annotated list of articles summarizing safety improvement efforts in the ambulatory setting since 2016. Topics explored include safety culture, measurement , team training, test result management, incident reporting, and diagnostic error .
Approaching the evidence basis for aviation-derived teamwork training in medicine. October 28, 2009
Weaving quality improvement and patient safety skills into all levels of medical training: an annotated bibliography. April 23, 2014
The evolving curriculum in quality improvement and patient safety in undergraduate and graduate medical education: a scoping review. February 15, 2023
Health care governance for quality and safety: the new agenda. June 20, 2007
Training in quality and safety: the current landscape. August 27, 2014
Graduate medical education's new focus on resident engagement in quality and safety: will it transform the culture of teaching hospitals? August 6, 2014
Culture change at the source: a medical school tackles patient safety. January 31, 2006
Health care provider use of private sector internal error-reporting systems. November 30, 2005
Development and evaluation of a 1-day interclerkship program for medical students on medical errors and patient safety. January 31, 2007
Developing a tool for assessing competency in root cause analysis. January 21, 2009
Physician burnout and medical errors: exploring the relationship, cost, and solutions received. August 9, 2023
Estimating the hospital costs of inpatient harms. October 31, 2018
Information gaps in newborn care and their potential for harm. May 6, 2015
Medical errors and consequent adverse events in critically ill surgical patients in a tertiary care teaching hospital in Delhi. July 15, 2009
Incident reporting in surgical trainees-revisited. August 13, 2008
Does error and adverse event reporting by physicians and nurses differ? August 27, 2008
The patient who falls: "It's always a trade-off." January 27, 2010
Clinicians' perceptions of opioid error–contributing factors in inpatient palliative care services: a qualitative study. May 22, 2019
Reducing surgical mortality in Scotland by use of the WHO Surgical Safety Checklist. May 8, 2019
Variability in the concentrations of intravenous drug infusions prepared in a critical care unit. August 27, 2008
Factors associated with misdiagnosis of acute stroke in young adults. December 7, 2011
Safe labeling practices to minimize medication errors in anesthesia: 5 case reports and review of the literature. January 31, 2018
Comparison and interpretation of urinalysis performed by a nephrologist versus a hospital-based clinical laboratory. January 18, 2006
Patient safety strategies: are we on the same team? October 3, 2012
Outcomes of daytime procedures performed by attending surgeons after night work. September 2, 2015
What stage are low-income and middle-income countries (LMICs) at with patient safety curriculum implementation and what are the barriers to implementation? A two-stage cross-sectional study. August 9, 2017
Management and patient safety of complex elderly patients in primary care during the COVID-19 pandemic in the UK-Qualitative assessment. April 14, 2021
Integrating principles of safety culture and just culture into nursing homes: lessons from the pandemic. January 12, 2022
Perioperative team-based morbidity and mortality conferences: a systematic review of the literature. October 11, 2023
Fake it 'til you make it: pressures to measure up in surgical training. June 13, 2018
Root cause analysis of transfusion error: identifying causes to implement changes. December 22, 2010
Resident duty hours and resident and patient outcomes: systematic review and meta-analysis. November 16, 2022
Safe opioid prescribing: a prognostic machine learning approach to predicting 30-day risk after an opioid dispensation in Alberta, Canada. June 16, 2021
The use of anatomical side markers in general radiology: a systematic review of the current literature. August 26, 2020
Waking up the next morning: surgeons' emotional reactions to adverse events. December 12, 2012
Rethinking peer review: what aviation can teach radiology about performance improvement. August 31, 2011
Human factors engineering in patient safety. February 19, 2014
Sample to sample carryover: a source of analytical laboratory error and its relevance to integrated clinical chemistry/immunoassay systems. July 5, 2006
Surgical teams' attitudes about surgical safety and the surgical safety checklist at 10 years: a multinational survey. November 17, 2021
Deprescribing: a simple method for reducing polypharmacy. September 6, 2017
Five reasons for optimism on World Patient Safety Day. October 23, 2019
Racial disparities in diagnostic delay among women with breast cancer. August 18, 2021
Experiences of transgender and gender nonbinary patients in the emergency department and recommendations for health care policy, education, and practice. July 21, 2021
Perspectives on perioperative team-based morbidity and mortality conferences: a mixed-methods study. November 29, 2023
Costs and consequences associated with misdiagnosed lower extremity cellulitis. November 23, 2016
Diagnosis is a team sport—partnering with allied health professionals to reduce diagnostic errors: a case study on the role of a vestibular therapist in diagnosing dizziness. July 27, 2016
Using electronic health records to identify adverse drug events in ambulatory care: a systematic review. March 13, 2019
Is WHO's surgical safety checklist being hyped? August 21, 2019
The prescription opioid crisis: role of the anaesthesiologist in reducing opioid use and misuse. July 24, 2019
A prospective study to evaluate awareness about medication errors amongst health-care personnel representing North, East, West Regions of India. March 26, 2014
Mandatory pharmacy residencies: one way to reduce medication errors. April 7, 2010
Seeing systems in health care organizations. September 5, 2007
Using a survey of incident reporting and learning practices to improve organisational learning at a cancer care centre. October 17, 2007
Structural racism in behavioral health presentation and management. May 17, 2023
Improving safety and eliminating redundant tests: cutting costs in U.S. hospitals. September 30, 2009
Community-, healthcare-, and hospital-acquired severe sepsis hospitalizations in the University HealthSystem Consortium. September 2, 2015
Addressing the opioid epidemic in the United States: lessons from the Department of Veterans Affairs. April 5, 2017
Computerized physician order entry of medications and clinical decision support can improve problem list documentation compliance. July 30, 2008
The effect of bedrails on falls and injury: a systematic review of clinical studies. June 11, 2008
Errors and adverse events in otolaryngology. June 14, 2006
Voluntary electronic reporting of laboratory errors: an analysis of 37,532 laboratory event reports from 30 health care organizations. April 18, 2012
Complications of daytime elective laparoscopic cholecystectomies performed by surgeons who operated the night before. November 20, 2013
Patients' experiences and perspectives of patient-reported outcome measures in clinical care: a systematic review and qualitative meta-synthesis. May 11, 2022
Voluntary electronic reporting of medical errors and adverse events. January 18, 2006
Case studies of patient safety research classics to build research capacity in low- and middle-income countries. December 11, 2013
Automation of the I-PASS tool to improve transitions of care. October 23, 2019
Claiming behaviour in a no-fault system of medical injury: a descriptive analysis of claimants and non-claimants. September 6, 2006
Improving nurse-to-patient staffing ratios as a cost-effective safety intervention. August 10, 2005
Peer feedback, learning, and improvement: answering the call of the Institute of Medicine report on diagnostic error. December 7, 2016
Impact of computerised physician order entry (CPOE) on the incidence of chemotherapy-related medication errors: a systematic review. April 7, 2021
Creating a better discharge summary: improvement in quality and timeliness using an electronic discharge summary. May 6, 2009
Incorporation of quality and safety principles in maintenance of certification: a qualitative analysis of American Board of Medical Specialties member boards. September 12, 2018
Early death after discharge from emergency departments: analysis of national US insurance claims data. February 15, 2017
The role of teamwork in the professional education of physicians: current status and assessment recommendations. March 6, 2005
In situ simulation as a tool to longitudinally identify and track latent safety threats in a structured quality improvement initiative for SARS-CoV-2 airway management: a single-center study. February 22, 2023
Utilization of a role-based head covering system to decrease misidentification in the operating room. August 7, 2019
Potassium and phosphorus repletion in hospitalized patients: implications for clinical practice and the potential use of healthcare information technology to improve prescribing and patient safety. February 14, 2007
Building a culture of safety in ophthalmology. November 2, 2016
A framework for evaluating the appropriateness of clinical decision support alerts and responses. September 21, 2011
Specificity of computerized physician order entry has a significant effect on the efficiency of workflow for critically ill patients. April 21, 2005
Outcomes of concurrent operations: results from the American College of Surgeons' National Surgical Quality Improvement Program. October 11, 2017
The clinical transformation of Ascension Health: eliminating all preventable injuries and deaths. June 7, 2006
Differences in safety climate among hospital anesthesia departments and the effect of a realistic simulation-based training program. February 20, 2008
To do no harm - and the most good - with AI in health care. March 13, 2024
Do medical inpatients who report poor service quality experience more adverse events and medical errors? February 13, 2008
Parental misinterpretations of over-the-counter pediatric cough and cold medication labels. July 1, 2009
Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. January 18, 2017
Sustaining the gains: a 7-year follow-through of a hospital-wide patient safety improvement project on hospital-wide adverse event outcomes and patient safety culture. June 10, 2020
Measurement and training of TeamSTEPPS dimensions using the Medical Team Performance Assessment Tool. January 30, 2013
Safety on an inpatient pediatric otolaryngology service: many small errors, few adverse events. May 6, 2009
Planning and implementing a systems-based patient safety curriculum in medical education. August 13, 2008
Reducing medical error in the Military Health System: how can team training help? October 18, 2006
Pharmacy clarification of prescriptions ordered in primary care: a report from the Applied Strategies for Improving Patient Safety (ASIPS) collaborative. February 8, 2006
Using a pediatric trigger tool to estimate total harm burden hospital-acquired conditions represent. July 11, 2018
Association of communication between hospital-based physicians and primary care providers with patient outcomes. January 21, 2009
Controlled trial to improve resident sign-out in a medical intensive care unit. August 30, 2017
A trigger tool fails to identify serious errors and adverse events in pediatric otolaryngology. October 27, 2010
US public opinion regarding proposed limits on resident physician work hours. July 28, 2010
Otolaryngologists' responses to errors and adverse events. July 26, 2006
Computer-assisted bar-coding system significantly reduces clinical laboratory specimen identification errors in a pediatric oncology hospital. February 13, 2008
Annual Perspective
Perspective
Patient Safety Innovations
Ambulatory Safety Nets to Reduce Missed and Delayed Diagnoses of Cancer
Preventing falls through patient and family engagement to create customized prevention plans.
Using morbidity and mortality conferences to drive quality improvement and reduce errors. May 17, 2023
Diagnostic challenges in primary care: identifying and avoiding cognitive bias. June 29, 2022
Patient Safety Primers
The design and conduct of Project RedDE: a cluster-randomized trial to reduce diagnostic errors in pediatric primary care. May 15, 2019
Recommendations from a national panel on quality improvement in obstetrics. April 24, 2019
Quality improvement priorities for safer out-of-hours palliative care: lessons from a mixed-methods analysis of a national incident-reporting database. February 6, 2019
Quality, Value, and Patient Safety in Orthopedic Surgery. October 24, 2018
The STEP-up programme: engaging all staff in patient safety. September 26, 2018
Influences on the adoption of patient safety innovation in primary care: a qualitative exploration of staff perspectives. August 22, 2018
Six Building Blocks: A Team-Based Approach to Improving Opioid Management in Primary Care. June 27, 2018
Exploring and evaluating patient safety culture in a community-based primary care setting. May 16, 2018
The Economics of Patient Safety in Primary and Ambulatory Care: Flying Blind. May 2, 2018
The need for closed-loop systems for management of abnormal test results. April 25, 2018
General internists in pursuit of diagnostic excellence in primary care: a #ProudtobeGIM thread that unites us all. April 18, 2018
Pragmatic insights on patient safety priorities and intervention strategies in ambulatory settings. December 6, 2017
Diagnostic errors in primary care pediatrics: Project RedDE. November 29, 2017
Diagnostic errors: impact of an educational intervention on pediatric primary care. November 8, 2017
Repeat prescribing of medications: a system-centred risk management model for primary care organisations. November 8, 2017
Infection prevention and control in pediatric ambulatory settings. November 1, 2017
Implementing the Comprehensive Unit-Based Safety Program (CUSP) to improve patient safety in an academic primary care practice. October 18, 2017
Identification and characterization of adverse drug events in primary care. October 11, 2017

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
An Annotated Bibliography
For the assignment this week, I chose the topic of Medication Errors to find three reputable sources to cite the information on with an annotated bibliography. The sources I chose from the ProQuest database because I think they have a good reputation in providing peer-reviewed material relevant to the topic I chose. Chang, Y., & Mark, Barbara A, RN,PhD., F.A.A.N. (2009). Antecedents of severe and nonsevere medication errors. Journal of Nursing Scholarship, 41(1), 70-8.
Retrieved from http://search.proquest.com/docview/236343845?accountid=35812 This article focused on ways used to investigate the differences in antecedents for medication errors. Severe and non-severe errors have different antecedents; therefore both the prevention and management strategies must be targeted to the specific type of error that occurred.
Gleason, K. M., Mcdaniel, M. R., Feinglass, J., Baker, D. W., Lindquist, L., Liss, D., & Noskin, G. A. (2010). Results of the medications at transitions and clinical handoffs (MATCH) study: An analysis of medication reconciliation errors and risk factors at hospital admission. Journal of General Internal Medicine, 25(5), 441-7. Retrieved from http://search.proquest.com.ezproxy.apollolibrary.com/nursing/docview/871261424/abstract/13D93A93855F3D5824/4?accountid=35812 This article shows how harm can be prevented or reduced for patients by quickly correcting any errors made through medication administration. Accurate and complete medication histories are preferred for all patients.
Collaboration between physicians, nurses and other health care providers on medication reconciliation is beneficial for a pharmacist. Attention to detail is always expected and more so during shift changes and handoffs of care, therefore reducing the risk of medication errors occurring.
Sarvadikar, A., Prescott, G., & Williams, D. (2010). Attitudes to reporting medication error among differing healthcare professionals. European Journal of Clinical Pharmacology, 66(8), 843-53. Retrieved from http://search.proquest.com.ezproxy.apollolibrary.com/nursing/docview/633059249/abstract/13D9373EFE72C940FE5/1?accountid=35812 These results reflect opposing attitudes about reporting medication errors, among health care.
Related Essays
THE PURPOSE OF THIS ARTICLE IS TO DESCRIBE MANY MEDICATION ERRORS AND HOW TO PREVENT PHARMACIST FROM MAKING THE ERRORS. THE ARTICLE DOCUMENTED FIVE YEARS OF MEDICATION ERROR PREVENTION RESULTS, SUMMARIZING ADHERENCE TO THE ALBERTA CANCER BOARD’S MEDICATION ERROR PREVENTION …
Understanding Pharmacology is vital towards becoming a Medical Assistant. This is to help prevent medical errors and substance abuse. The knowledge of proper administration of medications is important because it protects the patient and the medical professional. Knowing what your …
Berman, A. (2004). Reducing medication errors through naming, labeling, and packaging. Journal of Medical Systems, 28(1), 9-29. doi:http://dx.doi.org/10.1023/B:JOMS.0000021518.60670.10 This article talks about the different names of drugs that are similar and may cause medication errors in the healthcare field. Also, …
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Citing sources
- What Is an Annotated Bibliography? | Examples & Format
What Is an Annotated Bibliography? | Examples & Format
Published on March 9, 2021 by Jack Caulfield . Revised on August 23, 2022.
An annotated bibliography is a list of source references that includes a short descriptive text (an annotation) for each source. It may be assigned as part of the research process for a paper , or as an individual assignment to gather and read relevant sources on a topic.
Scribbr’s free Citation Generator allows you to easily create and manage your annotated bibliography in APA or MLA style. To generate a perfectly formatted annotated bibliography, select the source type, fill out the relevant fields, and add your annotation.
An example of an annotated source is shown below:
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes

Table of contents
Annotated bibliography format: apa, mla, chicago, how to write an annotated bibliography, descriptive annotation example, evaluative annotation example, reflective annotation example, finding sources for your annotated bibliography, frequently asked questions about annotated bibliographies.
Make sure your annotated bibliography is formatted according to the guidelines of the style guide you’re working with. Three common styles are covered below:
In APA Style , both the reference entry and the annotation should be double-spaced and left-aligned.
The reference entry itself should have a hanging indent . The annotation follows on the next line, and the whole annotation should be indented to match the hanging indent. The first line of any additional paragraphs should be indented an additional time.
In an MLA style annotated bibliography , the Works Cited entry and the annotation are both double-spaced and left-aligned.
The Works Cited entry has a hanging indent. The annotation itself is indented 1 inch (twice as far as the hanging indent). If there are two or more paragraphs in the annotation, the first line of each paragraph is indented an additional half-inch, but not if there is only one paragraph.
Chicago style
In a Chicago style annotated bibliography , the bibliography entry itself should be single-spaced and feature a hanging indent.
The annotation should be indented, double-spaced, and left-aligned. The first line of any additional paragraphs should be indented an additional time.
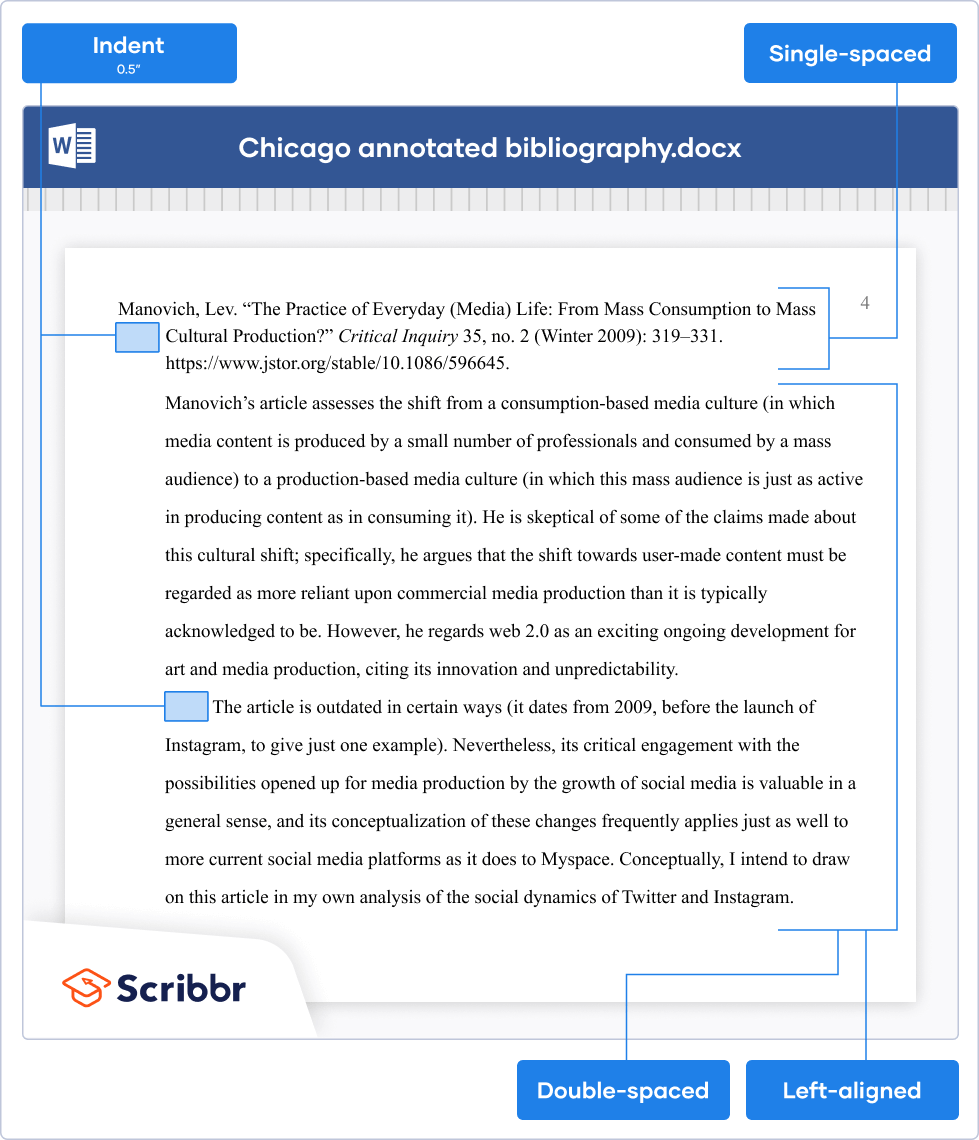
The only proofreading tool specialized in correcting academic writing - try for free!
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Try for free
For each source, start by writing (or generating ) a full reference entry that gives the author, title, date, and other information. The annotated bibliography format varies based on the citation style you’re using.
The annotations themselves are usually between 50 and 200 words in length, typically formatted as a single paragraph. This can vary depending on the word count of the assignment, the relative length and importance of different sources, and the number of sources you include.
Consider the instructions you’ve been given or consult your instructor to determine what kind of annotations they’re looking for:
- Descriptive annotations : When the assignment is just about gathering and summarizing information, focus on the key arguments and methods of each source.
- Evaluative annotations : When the assignment is about evaluating the sources , you should also assess the validity and effectiveness of these arguments and methods.
- Reflective annotations : When the assignment is part of a larger research process, you need to consider the relevance and usefulness of the sources to your own research.
These specific terms won’t necessarily be used. The important thing is to understand the purpose of your assignment and pick the approach that matches it best. Interactive examples of the different styles of annotation are shown below.
A descriptive annotation summarizes the approach and arguments of a source in an objective way, without attempting to assess their validity.
In this way, it resembles an abstract , but you should never just copy text from a source’s abstract, as this would be considered plagiarism . You’ll naturally cover similar ground, but you should also consider whether the abstract omits any important points from the full text.
The interactive example shown below describes an article about the relationship between business regulations and CO 2 emissions.
Rieger, A. (2019). Doing business and increasing emissions? An exploratory analysis of the impact of business regulation on CO 2 emissions. Human Ecology Review , 25 (1), 69–86. https://www.jstor.org/stable/26964340
An evaluative annotation also describes the content of a source, but it goes on to evaluate elements like the validity of the source’s arguments and the appropriateness of its methods .
For example, the following annotation describes, and evaluates the effectiveness of, a book about the history of Western philosophy.
Kenny, A. (2010). A new history of Western philosophy: In four parts . Oxford University Press.
Scribbr Citation Checker New
The AI-powered Citation Checker helps you avoid common mistakes such as:
- Missing commas and periods
- Incorrect usage of “et al.”
- Ampersands (&) in narrative citations
- Missing reference entries
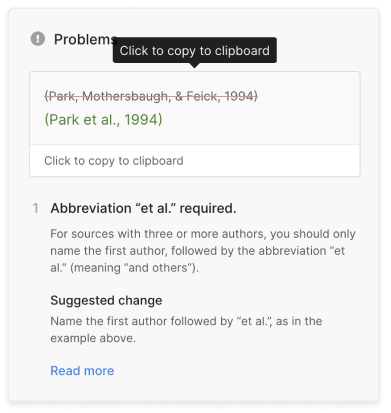
A reflective annotation is similar to an evaluative one, but it focuses on the source’s usefulness or relevance to your own research.
Reflective annotations are often required when the point is to gather sources for a future research project, or to assess how they were used in a project you already completed.
The annotation below assesses the usefulness of a particular article for the author’s own research in the field of media studies.
Manovich, Lev. (2009). The practice of everyday (media) life: From mass consumption to mass cultural production? Critical Inquiry , 35 (2), 319–331. https://www.jstor.org/stable/10.1086/596645
Manovich’s article assesses the shift from a consumption-based media culture (in which media content is produced by a small number of professionals and consumed by a mass audience) to a production-based media culture (in which this mass audience is just as active in producing content as in consuming it). He is skeptical of some of the claims made about this cultural shift; specifically, he argues that the shift towards user-made content must be regarded as more reliant upon commercial media production than it is typically acknowledged to be. However, he regards web 2.0 as an exciting ongoing development for art and media production, citing its innovation and unpredictability.
The article is outdated in certain ways (it dates from 2009, before the launch of Instagram, to give just one example). Nevertheless, its critical engagement with the possibilities opened up for media production by the growth of social media is valuable in a general sense, and its conceptualization of these changes frequently applies just as well to more current social media platforms as it does to Myspace. Conceptually, I intend to draw on this article in my own analysis of the social dynamics of Twitter and Instagram.
Before you can write your annotations, you’ll need to find sources . If the annotated bibliography is part of the research process for a paper, your sources will be those you consult and cite as you prepare the paper. Otherwise, your assignment and your choice of topic will guide you in what kind of sources to look for.
Make sure that you’ve clearly defined your topic , and then consider what keywords are relevant to it, including variants of the terms. Use these keywords to search databases (e.g., Google Scholar ), using Boolean operators to refine your search.
Sources can include journal articles, books, and other source types , depending on the scope of the assignment. Read the abstracts or blurbs of the sources you find to see whether they’re relevant, and try exploring their bibliographies to discover more. If a particular source keeps showing up, it’s probably important.
Once you’ve selected an appropriate range of sources, read through them, taking notes that you can use to build up your annotations. You may even prefer to write your annotations as you go, while each source is fresh in your mind.
An annotated bibliography is an assignment where you collect sources on a specific topic and write an annotation for each source. An annotation is a short text that describes and sometimes evaluates the source.
Any credible sources on your topic can be included in an annotated bibliography . The exact sources you cover will vary depending on the assignment, but you should usually focus on collecting journal articles and scholarly books . When in doubt, utilize the CRAAP test !
Each annotation in an annotated bibliography is usually between 50 and 200 words long. Longer annotations may be divided into paragraphs .
The content of the annotation varies according to your assignment. An annotation can be descriptive, meaning it just describes the source objectively; evaluative, meaning it assesses its usefulness; or reflective, meaning it explains how the source will be used in your own research .
A source annotation in an annotated bibliography fulfills a similar purpose to an abstract : they’re both intended to summarize the approach and key points of a source.
However, an annotation may also evaluate the source , discussing the validity and effectiveness of its arguments. Even if your annotation is purely descriptive , you may have a different perspective on the source from the author and highlight different key points.
You should never just copy text from the abstract for your annotation, as doing so constitutes plagiarism .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Caulfield, J. (2022, August 23). What Is an Annotated Bibliography? | Examples & Format. Scribbr. Retrieved April 2, 2024, from https://www.scribbr.com/citing-sources/annotated-bibliography/
Is this article helpful?

Jack Caulfield
Other students also liked, evaluating sources | methods & examples, how to find sources | scholarly articles, books, etc., hanging indent | word & google docs instructions, what is your plagiarism score.
- Research Paper
- Book Report
- Book Review
- Movie Review
- Dissertation
- Thesis Proposal
- Research Proposal
- Dissertation - Abstract
- Dissertation Introduction
- Dissertation Review
- Dissertat. Methodology
- Dissertation - Results
- Admission Essay
- Scholarship Essay
- Personal Statement
- Proofreading
- Speech Presentation
- Math Problem
- Article Critique
- Annotated Bibliography
- Reaction Paper
- PowerPoint Presentation
- Statistics Project
- Multiple Choice Questions
- Resume Writing
- Other (Not Listed)
Medication Errors: Annotated Bibliography Health, Medicine Paper (Annotated Bibliography Sample)
Write an annotated bibliography accompanied by a brief introduction, literature search criteria, artic;e evaluation criteria, and a refelction on lessons leanrt from working on the annotated bibliography.
Medication Errors: Annotated Bibliography Student's Name Department, University Course Code and Name Instructor's Name Due Date Medication Errors: Annotated Bibliography Medication errors are failures in the treatment process that cause harm or injury to the patient related to their use of a drug. Medication errors are a common cause of preventable harm to patients and increase the financial burden on a health institution (Scott, 2016). Medication errors arise from wrongful prescription, lack of administrative protocols, inadequate patient instruction, or failure to address allergies and known contraindications (Burlingame, 2018). Although all health care professionals can commit medication errors, nurses are especially prone to medication errors in the administration and patient education phases of drug use. As a nurse, I chose medication error as the topic for my annotated bibliography to inform future practice and reduce the likelihood of committing medication errors. The medication error health care problem interests me because nurses can greatly reduce its occurrence in health care settings. The possibility of causing preventable harm to a patient informs my focus on medication error as the healthcare issue I would like to address. Having worked with patients who use several drugs concurrently, I feel that learning more about medication errors can instill confidence in my capability to handle such cases in the future. Literature Search Criteria I found peer-reviewed journal articles based on their relevance to medication error management using the University's library database. I used the search terms "medication error management", "medication safety", and "nursing medication error". Additionally, I filtered the results by discipline to retain nursing articles, and by publication date to retain articles published within the last five years. Finally, I selected the four articles I felt would provide the most information on preventing medication error after reading the abstracts of all articles that satisfied the search parameters. Article Relevance and Credibility Evaluation Criteria All articles that satisfied the search criteria were published in peer-reviewed journals, which ensures their credibility because their findings and claims pass accuracy reviews by panels of nursing experts. I checked article relevance using publication date and article abstracts. I found that all the four articles I chose provided valuable information on medication error management. Annotated Bibliography Burlingame, B. L. (2018). Guideline implementation: Medication safety. AORN Journal, 107(4), 476–487. https://doi.org/10.1002/aorn.12095 Burlingame's article focuses on preventing medication error in the perioperative phases, from prescription to the transition of the patient to home care. The article focuses on strategies delineated in the Association of periOperative Registered Nurses (AORN) Guideline for medication safety. The AORN document emphasizes precaution at all stages of the perioperative process. Burlingame focuses on four phases, namely the prescription phase, administration phase, patient education phase, and transitions of care phase. The guidelines require specific precautions such as designating a healthcare professional to oversee information transfer to the receiving caregiver in transitions of care and to conduct complete education of the patient and caregiver before discharge. Burlingame also demonstrates how the same guidelines apply to other areas of the healthcare center. This article highlights the need for precaution at all stages of the patient's exposure to medication, from prescription to administration and aftercare, hence its inclusion in the annotated bibliography.
Other Topics:
- Epilepsy Awareness Health, Medicine, Nursing Annotated Bibliography Description: Epilepsy is defined as a social and medical condition with unique characteristics of recurrent seizures. It is remarkably distributed across the globe and affects people of all ages. Due to its prevalence, the disorder is now a public health concern, hence a need to understand its prevalence and risk... 12 pages/≈3300 words | 15 Sources | APA | Health, Medicine, Nursing | Annotated Bibliography |
- Skills, Knowledge, and Practice in the Management of Remote Obstetric Emergencies Description: This annotated bibliography contains a collection of evidence that support my project on the acquisition of knowledge and skills in remote obstetric emergencies management. It includes seven articles that are directly focused on obstetric emergencies training and programs, two that focus on the need for maternity... 17 pages/≈4675 words | 14 Sources | APA | Health, Medicine, Nursing | Annotated Bibliography |
- THE RAPEUTIC FASTING AS AN ALTERNATIVE TO INSULIN. Description: Fasting is a therapeutic tool practiced by different cultures and medical systems over time. However, when someone is said to be under Therapeutic fasting, they are believed to have completely abstained from all substances except pure water in an environment of complete rest. ... 3 pages/≈825 words | 1 Source | APA | Health, Medicine, Nursing | Annotated Bibliography |
- Exchange your samples for free Unlocks.
- 24/7 Support
Medication Errors in the Elderly Treatment Annotated Bibliography
Introduction.
Thousands of patients suffer or even die because of dangerous or substandard treatment their doctors prescribe. The patients’ safety is a key to the quality health care system that prioritizes and guarantees medication safety. It is one of the crucial aspects of a patient’s safety during his stay in the hospital. The main objective of every medication is to reduce patients’ suffering, but not to increase it. That is why it is necessary for medical personnel to provide high-quality services and to state the patient’s comfort as their primary concern (Keers, Plácido, Bennett, Clayton, Brown, Ashcroft, 2018). However, as some research shows, medical errors occur occasionally, especially when treating the elderly. The essential factor to adequately treating the elderly without any mistreatment occurring is careful consideration of the medication doses prescribed to a patient because metabolism slows with age. Hence, it takes time for older people’s bodies to take the medication properly. If the medicine is not absorbed in the right way, older people may face side effects, which in combination with poor health conditions may result in the patient’s death.
As practice shows, the cause of most inaccuracies is the human factor which can be either wrongly prescribed medicine or improperly educated nurse (Keers, Plácido, Bennett, Clayton, Brown, Ashcroft, 2018). However, the reason for interruptions may also be the doctor’s confidence in him being right and prescribing the proper treatment. Medication administration errors are often connected to medical personnel’s negligence, inaccuracies, or lack of knowledge. Anyway, similar to all patients, older people require considerate treatment and more attention to their medication prescription. Everybody has the right to quality medical treatment, which is effective, safe, and oriented on people’s needs. It is also essential to provide patients with high-quality treatment because both proper and improper treatment affect the reputation of a particular health care institution. Hence, the medical personnel should be appropriately educated and attentive to the patients and to the treatment he prescribes.
All the articles chosen relate to the problem of medication errors that occur while treating the elderly. They address different aspects of the problem, which allows looking at it from different perspectives. They also contain some statistical data that help to assess the scale of the situation in numbers.
Annotated Bibliography
Raban, M. Z., & Westbrook, J. I. (2013). Are interventions to reduce interruptions and errors during medication administration effective?: A systematic review. BMJ Quality & Safety , 23 (5), 414–421. Web.
The authors present the results of their qualitative research on the connection between interventions and medication administration interruptions and their impact on medication administration errors. The study’s main aim was to find out if interventions to reduce interruptions during medication administration may be considered an effective way to decrease interruptions and medication administration errors. The main methods the authors used during the research were data collecting and analysis. The authors analyzed ten studies from different sources, including MEDLINE, EMBASE, CINAHL, PsycINFO, Cochrane Effective Practice, Organization of Care Groups, Google, and Google Scholar. The information collected by the authors of the research reports quantitative data based on direct observations of interruptions or medication administration errors. Overall, the authors found 626 citations from the searches. Only 10 of the articles met the requirements of the study and were included in the review – eight from North America and two from Europe. However, the present ten sources provided weak confirmation of the authors’ hypothesis mainly due to the small number of statistical data or lack of inter-rater reliability assessments.
The study’s strength concerns the fact that apart from the lack of statistics, the researchers found out that interventions might be an effective way to reduce the ratio of interruptions and errors during medication administration. However, the study’s strength is inseparable from its limitations due to insufficient information on the topic. The majority of sources did not contain any statistical data on the observed sample size and did not assess the reliability of the data. They also used staff from the same medical institutions as observers, which may become the reason for bias.
The generalization of the study findings is complicated because the research was conducted in the United States only, usually in one hospital, in the same wards, and considered the same medical personnel. That is why the present research seems to require further data gathering and analysis in order to provide more factual findings on the topic. However, the current results may be considered quite promising.
Metsälä, E., Viherkoski, U. (2013). Medication errors in elderly acute care – a systematic review. Scandinavian Journal of Caring Sciences , 28 (1), 12–28. Web.
The authors define the main aim of the present research as improving the prerequisites of the old age patients’ medication safety by reviewing statistical data of medication errors in elderly treatment. The methods of the research are data gathering and statistical analysis. The sources of the up-to-date information related to the study’s main objective are Cinahl, Medline, Cochrane, JBI Connect+ databases, and Finnish health care databases Medic and Ohtanen. The overall number of studies the authors selected for the research was 20 – eight from the USA, seven from Europe, three from Taiwan, and one each from Canada and Australia. The results of the study prove that the most medication errors mentioned in the research concerned nursing competence, prescription- and patient-related factors, medication work organization and nursing process, and safety culture.
The strengths of the research concern the fact that the paper provides concrete data on the topic of medication safety of the elderly and the most widespread medication errors occurring during their treatment. The study also offers several practical implications of the results for improving the medication safety of older people. The limitations of the research regard the fact that its timeline is limited to the years 2001-2011. The authors chose the 10-years limit because the treatment of the elderly and the medication administration process evolve fast, and new criteria and data for the analysis emerge. That is why it is almost impossible to regard the results of any study on the field in the long-term perspective. Another limitation of the research concerns the language of the sources because the authors considered those published only in English or Finnish. This approach did not enable them to study medical data published in other languages. It may be regarded as a significant shortcoming, as the analysis of more sources published by scientists from different countries might have resulted in other conclusions and statistical data.
Overall, the present research may be considered a relevant and up-to-date piece of scientific work. Its results may be implemented to reduce the number of medication administration errors in older people’s treatment. However, the research may need further consideration and fact-checking in 5-10 years due to the fast changes that happen in the field of treating the elderly.
Tariq, A., Georgiou, A., & Westbrook, J. (2013). Medication errors in residential aged care facilities: A distributed cognition analysis of the information exchange process. International Journal of Medical Informatics , 82 (5), 299–312. Web.
The present article is qualitative research on the topic of medication safety and medication errors. The aim of the study was to explain the cognitive distribution that defines residential aged care facilities (RACFs) medication ordering and delivery to figure out gaps in the theoretical data that lead to medication errors. The data were collected by conducting ethnographic analysis from May 2011 to September 2011. The qualitative methods of the analysis included minimally instructive direct observations, semi-structured interviews, and artefact analysis. Observations were conducted mainly during day shifts of medical personnel, which is from 7 a.m. to 3 p.m., as, statistically, medication activities are the most intense during that period.
It was established during the research that the majority of medication-related errors in RACF medication ordering and delivery do not attribute to individual care providers. The researchers found out three significant factors medication errors contribute to. First, the design of medication charts complicates the ordering procedure. Then, slow coordination between the participants of medication order and delivery process causes the lack of coherence between GPs, hospitals, and community pharmacies. Finally, using mainly fax and telephone as a prevailing means of communication complicates the process of information exchange between hospitals and pharmacies, as the data updates quickly, and pharmacies need to constantly double-check it.
The strengths of the present research concern the fact that it reveals and enumerates the reasons for medication-related errors and explains the reasons for their appearance. Besides, it provides an accurate assessment of the elements composing the medication ordering and delivery process. However, the researchers single out several limitations of the study, which concern only one organizational setting with established organizational practices. The authors stress that they had no intentions of generalizing the data collected to the population of RACFs. Overall, the present research is important for understanding the process of occurring medication errors, though it may need further consideration.
Westbrook, J. I., Li, L., Lehnbom, E. C., Baysari, M. T., Braithwaite, J., Burke, R., Conn, C., & Day, R. O. (2015). What are incident reports telling us? A comparative study at two Australian hospitals of medication errors identified at audit, detected by staff and reported to an incident system. International Journal for Quality in Health Care , 27 (1), 1–9. Web.
The article in question reveals the quantitative research conducted among the patients of two major academic hospitals in Australia. The study had three main objectives concerning the ratio of medication errors. The first was to compare medication errors identified during audit and observation with medication incident reports. Then, the study needed to determine the difference between the two hospitals regarding the medication error rates and incident report frequency. The third aim was to identify the ratio of prescribing error detections by the staff. The researchers’ methods during the study regarded the comparative analysis of the data on the electronically reported accidents on medication errors that occurred in the two hospitals involved in the research.
The research identified 12 567 medication errors on the whole. However, only 1,3 percent of them were reported. The medical personnel detected 21, 9per percent of all clinically important prescribing errors, but only 6 percent of them were reported. Overall, only 1 of 1000 medication-prescribing errors identified during the research was reported to the incident system. However, only 10 percent of the reported errors had evidence of being reported by the medical personnel. The researchers found no relation between the number of reported medication errors and the actual rate of prescribing errors. However, they established that the first hospital detected errors and reported them to the incident system more often than the second one.
The main strength of the present research is the availability of relevant and reliable data from the studies of the previous years, which enabled the researchers to make quite a precise and concrete conclusion. The study’s limitations concern the fact that the authors relied mainly on documented evidence concerning error detection, which may establish an underestimated ratio of medication errors. As mentioned in the study results, only around 2 percent of them were reported to the incident system. Hence, it is necessary not to rely only on the officially documented data when studying the ratio of the errors related to the medication prescription. Overall, the present study still proves that medical personnel’s lack of reporting medication errors is a significant problem for health care. The insufficient data prevents the therapists from assessing the possible health damage that a particular way of treatment may cause to the patients.
Literature Evaluation
The four present articles address the issue of medication-related errors when treating the patient, the elderly, in particular, and provide scientific data on the topic. Each report deals with different aspects of the issue. Thus, the first study (Raban & Westbrook, 2013) is devoted to the impact of interventions on interruptions and errors during medication administration. However, the research results present weak confirmation of the authors’ hypothesis, mainly due to the limitations, which include the same medication institution for each of the ten studies the authors analyzed. However, even with those limitations, the authors managed to prove that interventions may reduce interruptions which lead to medication administration errors.
The second study (Metsälä & Vaherkoski, 2013) proves that the human factor involving nurse competence as well as work organization and the nursing process are among the key reasons for medication prescription and administration errors. Hence, it is possible to establish the relationship between the competence level of the medical personnel, the work environment, and the medication-related errors. Thus, the more quiet and undisturbed the nurses’ workplace is, and the more skilled nurses are, the fewer medication errors occur. However, this hypothesis may require further consideration and scientific confirmation.
Medication-related work organization presumes not only the process of medication prescription and preparation but the process of medication ordering and delivery as well. The third article (Tariq, Georgiou & Westbrook, 2013) aims to identify gaps in medication-related information exchange between medical institutions in order to figure out the possible limitations that relate to the errors. The results of the authors’ research prove that the main reasons for the work organization-related errors concerning ordering and delivery of medication lie in the lack of information exchange between hospitals, GPs, and pharmacies. The analysis provided by the authors of the research highlights how poor information exchange may result in severe damage to patients’ health conditions. Thus, establishing the proper communication channel between medical institutions will help prevent medication order and delivery errors and
When continuing the description of the medication errors caused by the human factor, the first (Raban & Westbrook, 2013) and the second (Metsälä & Vaherkoski, 2013) studies mention, there is one more aspect to describe. It relates closely not only to the competence of the medical personnel but to the people’s general decency. This aspect is the medication incidents reports made by the doctors and nurses. It is the subject of the fourth study (Westbrook, Li, Lehnbom, Baysari, Braithwaite, Burke, Conn & Day, 2015), which compares the number of medication errors identified during the audit with the number of the reported incidents. The study results reveal the unpleasant truth – the majority of medication error cases remain unreported, which harmfully influences the statistics of the risks a particular treatment carries for patients.
Overall, the results of these four studies supplement each other. They help the people see that the majority of the medication-related errors worldwide are caused either by a human factor or by the unacceptable working conditions of the medication institutions. Hence, it is necessary to educate medical personnel and modify the working environment in order to provide proper health care conditions for the patients. The studies help improve people’s understanding of the nature of medication-related errors by providing numbers, figures, and scientifically confirmed data. The three studies provide a substantial confirmation of their hypothesis that medication errors are caused either by the human factor or the lack of communication between medical institutions and often remain unreported. However, one study (Raban & Westbrook, 2013) on the effectiveness of interventions in reducing interruptions during the medication administration process provides insufficient data and may require further consideration and confirmation.
To summarize, the analyzed studies reveal the problem of improper organization of the healthcare system that causes most medication errors when treating patients. The results of the present studies concern people of all age groups, but it is vital to consider them when treating the elderly. Safe use of medication is essential for people of old age because age alone brings many challenges and health issues that may deteriorate with the improper use of medication. The insufficient data on the influence of improper treatment on older people’s organisms prevent scientists from making proper conclusions concerning possible health outcomes for the patients (Keers, Plácido, Bennett, Clayton, Brown, Ashcroft, 2018). Hence, it is necessary to consider the results of four present studies while treating the elderly in order to avoid possible errors.
The results of the research are also applicable to the work process of nurses, as quite a number of mistakes reported by the four studies regarded the nurse competence and medical proficiency. The present studies may help decrease the number of human factor-related errors and improve the nursing process because they show the importance of attentive medication prescription and preparation and double-checking medication administration. The last one is a standard practice implemented in hospitals, particularly for high-risked drugs (Koyama, Maddox, Li, Bucknall, Westbrook, 2020). The results of the studies may be used to educate and properly train nurses in order to decrease the number of medication administration mistakes.
Keers, R. N., Plácido, M., Bennett, K., Clayton, K., Brown, P., Ashcroft, D. M. (2018). What causes medication administration errors in a mental health hospital? A qualitative study with nursing staff. PLoS One, 13 (10).
Koyama, A. K., Maddox, C-S. S., Li, L., Bucknall, T., Westbrook, J., I. (2020). Effectiveness of double-checking to reduce medication administration errors: A systematic review. BMJ Quality & Safety, 29 (7), 595-603.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, November 20). Medication Errors in the Elderly Treatment. https://ivypanda.com/essays/medication-errors-in-the-elderly-treatment/
"Medication Errors in the Elderly Treatment." IvyPanda , 20 Nov. 2022, ivypanda.com/essays/medication-errors-in-the-elderly-treatment/.
IvyPanda . (2022) 'Medication Errors in the Elderly Treatment'. 20 November.
IvyPanda . 2022. "Medication Errors in the Elderly Treatment." November 20, 2022. https://ivypanda.com/essays/medication-errors-in-the-elderly-treatment/.
1. IvyPanda . "Medication Errors in the Elderly Treatment." November 20, 2022. https://ivypanda.com/essays/medication-errors-in-the-elderly-treatment/.
Bibliography
IvyPanda . "Medication Errors in the Elderly Treatment." November 20, 2022. https://ivypanda.com/essays/medication-errors-in-the-elderly-treatment/.
- Medication Management in Electronic Health Records
- Polypharmacy Among the Elderly Population
- Miami University Hospital: Performance Scorecard
- Improving Patient Outcomes by Reducing Avoidable Interruptions
- The Interruptions of Women’s Workforce
- Risk of Medication Error During Drug Administration
- College Student Work Habits, Interruptions, and Stress
- Root-Cause Analysis and Safety Improvement Plan
- Alarm Fatigue in Health Centers
- Medication Errors and Innovative Interventions
- Medical Errors in Emergency Care for the Elderly
- Aspects of Geriatric Physical Therapy
- Weight Loss in an Elderly Male
- The Activity Theory: Promoting Health Care
- Chronic Anemia Management in the Elderly

IMAGES
VIDEO
COMMENTS
Preventing Medication Errors . An Annotated Bibliography . Biron AD, Loiselle G, Lavoie-Tremblay M. Work interruptions and their contribution to medication administration errors: an evidence review. Worldviews Evid Based Nurs. 2009;6(2):70-86. BACKGROUND: In many surveys, nurses cite work interruptions as a significant
Annotated Bibliography: Medication Errors. When choosing the sources, I used google scholar known for peer-reviewed articles. I used the following keywords during the research; medication errors, medication administration, and medication safety. I ensured that the source was an academic peer-reviewed article which
Annotated Bibliography Alqenae, F., Steinke, D.,&Keers,R.(2020), Prevalence and the nature of medication errors and medication-related harm following discharge from hospital to community settings: A systemic review: An international journal of medical toxicology and drug experience.
5. Recommendations to Improve Medication Errors Reporting Systems. Every medical institution should aim towards implementing methodologies whereby patients are not put at risk due to medication errors. Healthcare organizations should proactively eliminate these by investigating errors that have both occurred and those that may potentially occur.
Systematic reviews examining interventions aimed at reducing medication errors have largely focused on specialty settings, such as patients situated in adult and paediatric intensive care units, emergency departments, and neonatal intensive care and paediatric units. 6-10 Previous relevant systematic reviews relating to testing interventions for reducing medication errors in general hospital ...
An Annotated Bibliography . By . CRICO. Developed for When Things Go Wrong: Voices of Patients and Families [film], Cambridge, MA: CRICO; 2006. This bibliography focuses on the issues around medical errors and adverse events. The selected articles and books are valuable tools in
Medication administration errors (MAEs) are a common risk to patient safety in mental health hospitals, but an absence of in-depth studies to understand the underlying causes of these errors limits the development of effective remedial interventions. This study aimed to investigate the causes of MAEs affecting inpatients in a mental health ...
Background and aims: Medication errors occur at any point of the medication management process, and are a major cause of death and harm globally. The objective of this review was to compare the effectiveness of different interventions in reducing prescribing, dispensing and administration medication errors in acute medical and surgical settings.
Annotated Bibliography • Ammenwerth E, Schnell-Inderst P, Machan C, and Siebert U. The Effect of Electronic Prescribing on Medication Errors and Adverse Drug Events: A Systematic Review. J. Am. Med. Inform. Assoc. 15: 585-600. doi: 10.1197/jamia.M2667 • Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, Spurr C, Khorasani R ...
Background The aim of the third WHO challenge released in 2017 was to attain a global commitment to lessen the severity and to prevent medication-related harm by 50% within the next five years. To achieve this goal, comprehensive identification of barriers to reporting medication errors is imperative. Objective This review systematically identified and examined the barriers hindering nurses ...
Objective Medication administration errors (MAEs) are a common risk to patient safety in mental health hospitals, but an absence of in-depth studies to understand the underlying causes of these errors limits the development of effective remedial interventions. This study aimed to investigate the causes of MAEs affecting inpatients in a mental health National Health Service (NHS) hospital in ...
Annotated Bibliography: Understanding Ambulatory Care Practices in the Context of Patient Safety and Quality Improvement Maria F. Montano, MPH1 Harshal Mehdi, MD, MBA2 ... entry on medication errors in a multispecialty group practice. J Am Med Inform Assoc. 2010;17:78-84. 14. Farber J. Measuring and improving ambulatory surgery patients ...
Safe labeling practices to minimize medication errors in anesthesia: 5 case reports and review of the literature. Citation Text: Prakash S, Mullick P, Kumar A, et al. Safe Labeling Practices to Minimize Medication Errors in Anesthesia. ... Annotated bibliography: an update to: "Understanding ambulatory care practices in the context of patient ...
Annotated bibliography: an update to: "Understanding ambulatory care practices in the context of patient safety and quality improvement." ... A prospective study to evaluate awareness about medication errors amongst health-care personnel representing North, East, West Regions of India. March 26, 2014.
For the assignment this week, I chose the topic of Medication Errors to find three reputable sources to cite the information on with an annotated bibliography. The sources I chose from the ProQuest database because I think they have a good reputation in providing peer-reviewed material relevant to the topic I chose.
like "medication errors," "medication errors in nursing," and "medication errors in critical care." into consideration due to an important safety issue. The J. came up with block charting to allow more time for the nurses delivering care. Finally, the article discusses a team-
Introduction. In this paper, I will be evaluating a literature review research paper that was published in a journal publication. The article titled "A literature review of the individual and system factors that contribute to medication errors in nursing practice" written by Brady et al (2009) is a form of a desk-based review paper that utilizes secondary sources to investigate the extent ...
Published on March 9, 2021 by Jack Caulfield . Revised on August 23, 2022. An annotated bibliography is a list of source references that includes a short descriptive text (an annotation) for each source. It may be assigned as part of the research process for a paper, or as an individual assignment to gather and read relevant sources on a topic.
Medication Errors: Annotated Bibliography Medication errors are failures in the treatment process that cause harm or injury to the patient related to their use of a drug. Medication errors are a common cause of preventable harm to patients and increase the financial burden on a health institution (Scott, 2016).
BMJ Quality & Safety, 29 (7), 595-603. This annotated bibliography, "Medication Errors in the Elderly Treatment" is published exclusively on IvyPanda's free essay examples database. You can use it for research and reference purposes to write your own paper. However, you must cite it accordingly .
Medication Errors Annotated Bibliography.docx. Walden University. NURS 6052. NHS4000_WALCOTTSHANIQUA_Assessment2-Attempt1.edited (2).docx. Capella University. NURS 4000. Annotated Bibliography for Medication Errors DRAFT COPY 11.docx. De Montfort University. HLS NURS2001.
ANNOTATED BIBLIOGRAPHY FOR MEDICATION ERRORS 4 rooted culture and practices of all key participants from ordering to eventual administration to the patients. The major socializations and cultures identified as the main contributors to persistent medical errors are pharmacist reviews, the process of automated distribution and the process of bar ...
An annotated bibliography is a list of citations to books, articles, and documents. Each citation is followed by a brief (usually about 150 words) descriptive and evaluative paragraph, the annotation. The purpose of the annotation is to inform the reader of the relevance, accuracy, and quality of the sources cited.