
- Mission and Vision
- Scientific Advancement Plan
- Science Visioning
- Research Framework
- Minority Health and Health Disparities Definitions
- Organizational Structure
- Staff Directory
- About the Director
- Director’s Messages
- News Mentions
- Presentations
- Selected Publications
- Director's Laboratory
- Congressional Justification
- Congressional Testimony
- Legislative History
- NIH Minority Health and Health Disparities Strategic Plan 2021-2025
- Minority Health and Health Disparities: Definitions and Parameters
- NIH and HHS Commitment
- Foundation for Planning
- Structure of This Plan
- Strategic Plan Categories
- Summary of Categories and Goals
- Scientific Goals, Research Strategies, and Priority Areas
- Research-Sustaining Activities: Goals, Strategies, and Priority Areas
- Outreach, Collaboration, and Dissemination: Goals and Strategies
- Leap Forward Research Challenge
- Future Plans
- Research Interest Areas
- Research Centers
- Research Endowment
- Community Based Participatory Research Program (CBPR)
- SBIR/STTR: Small Business Innovation/Tech Transfer
- Solicited and Investigator-Initiated Research Project Grants
- Scientific Conferences
- Training and Career Development
- Loan Repayment Program (LRP)
- Data Management and Sharing
- Social and Behavioral Sciences
- Population and Community Health Sciences
- Epidemiology and Genetics
- Medical Research Scholars Program (MRSP)
- Coleman Research Innovation Award
- Health Disparities Interest Group
- Art Challenge
- Breathe Better Network
- Healthy Hearts Network
- DEBUT Challenge
- Healthy Mind Initiative
- Mental Health Essay Contest
- Science Day for Students at NIH
- Fuel Up to Play 60 en Español
- Brother, You're on My Mind
- Celebrating National Minority Health Month
- Reaching People in Multiple Languages
- Funding Strategy
- Active Funding Opportunities
- Expired Funding Opportunities
- Technical Assistance Webinars

- Community Health and Population Sciences
- Clinical and Health Services Research
- Integrative Biological and Behavioral Sciences
- Intramural Research Program
- Training and Diverse Workforce Development
- Inside NIMHD
- ScHARe HDPulse PhenX SDOH Toolkit Understanding Health Disparities For Research Applicants For Research Grantees Research and Training Programs Reports and Data Resources Health Information for the Public Science Education

- News and Events
- Improving Health Through Place-Based Interventions

- News Releases
- NIMHD in the News
- Conferences & Events
- Research Spotlights
- E-Newsletter
- Grantee Recognition

Working with Communities to Improve Health
Improving health is not always a matter of prescribing the right medicine. Sometimes the environment needs to change. Many Americans live in neighborhoods that lack safe walking routes, grocery stores, and health facilities.

“Are there places for kids to play? Are there good farmers markets or grocery stores?” asks Irene Dankwa-Mullan, M.D., M.P.H., formerly of NIMHD and now deputy chief health officer of IBM Watson Health. Such features help people in a neighborhood live healthier lives. Along with NIMHD director Eliseo Pérez-Stable, Dr. Dankwa-Mullan wrote an editorial in the April 2016 issue of the American Journal of Public Health , “Addressing Health Disparities Is a Place-Based Issue.”
Efforts to address these problems in particular communities are called “place-based interventions.” Ideally, these interventions come from a collaboration among community members, businesses, and other stakeholders, working together with police, urban planners, and other groups to improve their neighborhood. Community members are involved to make sure the interventions are based on their values.
Examples of place-based interventions include an effort to bring a farmers market to a neighborhood without a grocery store or promoting public safety so that residents feel safe walking on the street. Walking is a simple way to improve health, but there can be many barriers to walking, a fact highlighted in the Surgeon General’s Call to Action on walking .
Place-based interventions have been used successfully in rural areas, disadvantaged urban neighborhoods, and Indian reservations. People who live in such places tend to have particular health problems, such as diabetes and heart disease, and working to change the place-based conditions may help address health disparities.
Communities are complicated, and figuring out the best way to improve the health of all residents in a particular place can be a daunting task. “Part of the issue is that we do not have a best practices model for place-based interventions,” Dr. Dankwa-Mullan says. The editorial in the American Journal of Public Health was part of a new series on best practices for place-based interventions. Through this series, public health professionals will be able to learn how to develop place-based interventions.
One key to success of place-based interventions is involving the community. This is similar to community-based participatory research, a way of doing research in which the community sets priorities, ensuring that communities that are asked to participate in research get answers to the questions that are most important to them.
A research program in Baltimore is looking at bringing healthier food to African Americans who have high blood pressure and mild or moderate chronic kidney disease. The Dietary Approaches to Stop Hypertension (DASH) diet can lower blood pressure without medication. But it can be difficult for people who live in low-income areas with few supermarkets to get the vegetables and other healthy foods that are part of the diet. In the study led by an NIMHD grantee , participants will learn about the DASH diet and receive $30 per week of potassium-rich foods. Researchers will monitor participants’ blood pressure and kidney health to see whether the intervention helps.
In rural Kentucky , another NIMHD grantee is trying to improve health by teaching children about healthy foods and drinks, in cooperation with community organizations and farmers markets.
Another NIH-funded project in Baltimore is exploring alcohol policies that may reduce neighborhood violence. The researchers are examining how the density of liquor stores affects violence among youth.
These studies are not only delivering interventions; they are testing whether the individual interventions work to improve health. “Programs need to have evaluations or metrics of success,” Dr. Dankwa-Mullan says. “We need more research on the impact.” By funding research on place-based interventions, NIMHD hopes to find out the best ways to improve the health of disadvantaged people and reduce health disparities.
- Dankwa-Mullan, I., & Pérez-Stable, E. (2016). Addressing health disparities is a place-based issue . American Journal of Public Health , 106, 637–639. doi: 10.2105/AJPH.2016.303077.
- Johnson, L. A. (1974). The people of East Harlem . New York, NY: Mount Sinai School of Medicine.
- McDermott, W., & Deuschle, K. W. (1970). The people’s health: Anthropology and medicine in a Navajo community . New York, NY: Appleton-Century-Crofts.
Posted May 1, 2017
More Information
Read about what is happening at NIMHD at the News and Events section
NIMHD Fact Sheet
301-402-1366
Connect with Us
Subscribe to email updates

Staying Connected
- Funding Opportunities
- News & Events
- HHS Vulnerability Disclosure
- Privacy/Disclaimer/Accessibility Policy
- Viewers & Players
Community engaged learning brings students, locals together to solve health problems

December 14, 2022 – Over the summer, eight students from Harvard T.H. Chan School of Public Health partnered with organizations and community members from Boston to Nairobi, Kenya to learn about and help address locally identified public health problems. The students—members of the Spring 2022 cohort of Community Engaged Learning Fellows —spoke about their work at a December 6 event at the School.
The students’ projects included working with a Boston health collaborative, a clinic in Uganda, and cobalt miners in the Democratic Republic of Congo, among others. A common thread across the students’ presentations was their effort to draw on community knowledge to develop creative solutions together.
Jen Cruz , PhD ’26, partnered with the Allston Brighton Health Collaborative (ABHC), a public health nonprofit that convenes organizations, health advocates, elected officials, and residents to improve the systems that impact health and wellbeing in Boston’s Allston and Brighton neighborhoods.
Before she worked with ABHC on her fellowship project, Cruz—an Allston resident herself—volunteered for the Collaborative’s vaccine clinic. Since then, she has supported ABHC by serving on its mental wellness and transportation working committees, and plans to join the advisory board in 2023.
In her committee work, Cruz became aware that some of her fellow volunteers were reticent about advocating for their own priorities regarding the Collaborative’s decision-making about programs and policies for marginalized and under-resourced community members. Instead, they sometimes would ask Cruz to speak on their behalf in the hope that her public health expertise would strengthen their input.
“You shouldn’t have to have an MPH or degree in public health to contribute to the conversation, understand what the news is telling you, and make informed decisions about your health,” Cruz said. So, for her fellowship project, Cruz helped develop an educational program aimed at engaging community members as leaders in ABHC’s work.
Erin McGuinness , DrPH ’24, and Yacine Fall , SM ’23—the inaugural recipients of the Global Mental Health Fellowship , which offers students opportunities to partner with organizations outside the U.S. to address mental health issues in their communities—spoke about their work collaborating with the John Cleaver Kelly Clinic in Kabale, Uganda. They worked with the clinic on evaluating its community mental health outreach, including understanding the perspective of community health workers, patients, and families.
Alina Bhojani , SM ’23, and Alya Al Sager , SM ’23, discussed their experience working with Kidogo, a Kenya-based social enterprise building an expanding network of childcare centers in Nairobi’s urban slums. Kidogo supports female entrepreneurs—who they call “Mamapreneurs”—in starting childcare businesses in their own communities. Al Sager and Bhojani worked with Kidogo to tailor its early childhood development program so that Mamapreneurs would be more likely to use it in their centers.
Learning from locals
Under the Community Engaged Learning Fellows program, student cohorts are chosen each spring and fall to help respond to community-identified concerns, striving to balance the service they provide with their learning experience. Jocelyn Chu , director of the program, spoke about the benefits students gain from their field education and practice experiences.
“Public health education has the unique opportunity to incorporate field-based learning and training to sharpen skills in collaborative approaches and community engagement,” Chu said. “With an invitation to take on the posture of a ‘learner in the field,’ we have witnessed transformative learning experiences that have gone on to impact the career trajectories of our fellows.”
Other Spring 2022 Community Engaged Learning Fellows who presented at the December event included:
- Benita Kayembe , SM ’23, investigated the effects of artisanal cobalt mining on miners’ health in the Democratic Republic of the Congo—where up to 60% of the global supply of cobalt is sourced—with a goal of informing policymaking and building programs to improve miners’ quality of life.
- Christian Groth-Hoover , MPH ’23, worked with Massachusetts gun owners on the best means of communicating the dangers of lead exposure from firearms.
- Kaitlin Schroeder , MPH ’23, worked with the Boston Public Health Commission to develop culturally appropriate, community-facing messaging on colorectal cancer detection, which led to more residents getting tested.
– Catherine Seraphin
Photo: Catherine Seraphin

The Role and Potential of Communities in Population Health Improvement: Workshop Summary (2015)
Chapter: 5 how institutions work with communities.
5 How Institutions Work with Communities
The third panel of the workshop considered the role of institutions (academic, government, and private) in working with communities to build capacity and support change. An example of how a university can partner with community-based groups was provided by Jomella Watson-Thompson, an assistant professor in the Department of Applied Behavioral Sciences and the associate director for Community Participation and Research and the University of Kansas (KU) Work Group for Community Health and Development. Renee Canady, the chief executive officer of the Michigan Public Health Institute, discussed achieving collective impact through collaboration from her perspective as a former county health officer. Individual participants then discussed the importance of engaging the private sector as partners, the importance of collecting data with utility in mind, and, again, how to scale community organizing efforts. The discussion was moderated by Melissa Simon, an associate professor in obstetrics and gynecology, general and preventive medicine, and medical social sciences at the Northwestern University Feinberg School of Medicine.
MULTISECTOR PARTNERSHIPS
KU partners with various community-based groups, from grassroots neighborhood-based organizations to state and local departments, to build community capacity to support change and improvement, said Watson-Thompson from KU. Referring to a famous quote from Margaret
Mead—“Never doubt that a small group of thoughtful, committed citizens can change the world. Indeed it is the only thing that ever has.” Watson-Thompson said that such small groups of individuals can be found in neighborhoods, in agencies and universities, and in organizations, including faith communities.
The Power of Partnerships
Watson-Thompson described to the workshop her first personal experience with capacity building, which took place in 1997. A father of four young children in the Ivanhoe neighborhood of Kansas City had become frustrated with the ills in his neighborhood, which included crime, drugs, and vacant housing, and he and his wife began to organize prayer vigils and other activities in the community. The couple then began to work with other groups that had expertise in community organization and mobilizing. The KU Work Group for Community Health and Development 1 provided technical support and training. Seventeen years later, the Ivanhoe Neighborhood Council 2 is still committed to neighborhood improvement. Echoing the comments of other presenters, Watson-Thompson said that a key element in the success of that effort was the provision of adult development (community education, training, and capacity-building activities) to help those in the community come together, solve their own problems, and sustain progress after the technical advisers left.
Watson-Thompson described how more than 100 block leaders came together to develop block-level plans to support change and improvement. These leaders also engaged in multi-sector partnership with academia (the KU Work Group), businesses, government agencies, schools, and residents. The KU Work Group facilitated 117 community changes, which led to improvements in various community outcomes, including housing and crime. Over a 4-year period, there was a 54 percent increase in housing loan applications, a 17 percent decrease in violent crime, and a 20 percent decrease in non-violent crime. After addressing the most pressing needs, the Ivanhoe Neighborhood Council moved on to other community needs, such as parks and farmers markets. This is an example of a general principle in community organizing, Watson-Thompson said: If one person in a community steps up and leads, others will join.
In another multisector partnership, the KU Work Group worked with the Kansas Department of Social and Rehabilitation Services and with community coalitions in 14 Kansas counties to address underage drinking using the Kansas Strategic Prevention Framework State Incentive Grant. Overall,
____________
1 For more information see https://communityhealth.ku.edu (accessed August 15, 2014).
2 See http://www.incthrives.org (accessed August 15, 2014).
Watson-Thompson said, there were 802 program policy changes implemented through engaging 12 sectors of the community, which resulted in a 9.6 percent decrease in self-reported 30-day alcohol use by youth in the 14 counties. This initiative has become a model in Kansas for how to support prevention work, Watson-Thompson said. Another example is the Latino Health for All Coalition, which works to address disparities in cardiovascular disease and diabetes in Kansas City by providing access to healthier foods, safe activities, and health care. The collaborative partnership supported 41 program, policy, and practice changes over the initial 3-year program period. 3
Watson-Thompson said that each of these successful efforts adhered to three key principles for supporting population-level improvement:
- Focus on the outcome. Work with community partners to identify the behaviors that need to be changed at the community and population levels.
- Change the environment. Transform the community conditions to promote health and well-being.
- Support the change process. Take action to assess, plan, act, intervene, evaluate, and sustain.
A Collaborative Action Framework for Population-Level Improvements
To guide the process of working with community partners, the KU Work Group adapted the Institute of Medicine (IOM) Framework for Collaborative Public Health Action in Communities (IOM, 2003, p. 178) (see Figure 5-1 ). All activity is implemented based upon the direction of the community partners, Watson-Thompson said. The key responsibility of the academic partner is to support the ability of other partners to implement these processes (see Table 5-1 ). Watson-Thompson stressed that this is not prescribing the process to the other partners, but rather providing the support so that they can implement and maintain the processes (Fawcett et al., 2010).
Change and improvement in communities is the result of comprehensive interventions. While single-dose (i.e., one-program) interventions are important, Watson-Thompson said that addressing complex and interrelated problems requires an influx of program, policy, and practice changes. When these community- and system-level changes are of suf-
3 A review of collaborative partnerships may be found at http://www.ncbi.nlm.nih.gov/pubmed/10884958 (accessed July 25, 2014).

FIGURE 5-1 Framework for collaborative action for improving health and development. SOURCE: Watson-Thompson presentation, April 10, 2014, adapted from IOM, 2003, Figure 4-1, p. 178.
ficient intensity and penetration, they can achieve population-level outcomes (Fawcett et al., 2003).
Watson-Thompson highlighted several core principles, assumptions, and values that guide the KU Work Group on community and health development. Improvements are directed toward the population and require change both in behaviors of groups of people and in the conditions of the environment. Issues should be determined by those most affected, she said, and attention should be on the broader social determinants of health. Because these are influenced by multiple interrelated factors, single interventions are unlikely to be sufficient. Change requires
TABLE 5-1 Best Processes for Capacity and Change Identified by Watson-Thompson and Others
SOURCE: Watson-Thompson presentation, April 10, 2014, adapted from Fawcett et al., 2010.
engaging diverse groups across sectors as well as collaboration among multiple partners. Finally, she concluded, partners are catalysts for change, building the capacity to address what matters to people in the community.
Challenges and Opportunities for Academic Institutions
In closing, Watson-Thompson said that the community members are the experts and the researchers are co-learners in the process. It is important to build trust and rapport with community partners and to assure early wins to build shared success and empower the community. This requires an infusion of resources and a commitment over time and across people (i.e., across changes in leadership). It is important to stay at the table and to be part of the process and, as noted by others, also to make sure to contribute to the community. Academia is a base for supporting change and improving the community, and it is the collective responsibility of academics working with communities to have collective impact, she concluded. The key aim, Watson-Thompson said, is to have “community-engaged scholarship” where collaborative research, teaching, and public service is integrated.
COLLABORATION AND COLLECTIVE IMPACT
Canady shared her perspectives on collaboration and collective impact based on her prior experiences as health officer for the Ingham County, Michigan Health Department. Collective impact is “long-term
commitments by a group of important actors from different sectors to a common agenda for solving a specific problem,” she said. “Their actions are supported by a shared measurement system, mutually reinforcing activities, and ongoing communication, and are staffed by an independent backbone organization.”
Collaboration is not the same as community engagement, which is not the same as community organizing, which is not the same as collective impact, she said. Citing Edmonson (2012), she explained that collaboration is about convening around programs and initiatives while declaring neutrality, whereas collective impact is more about working together to move outcomes. While collaboration uses data to prove things, collective impact tries to improve things. Collaboration is usually something in addition to what people already do, while collective impact entails integrating practices that get results into everyday work. Finally, collaboration is often about advocating for ideas, while collective impact advocates for what works. As an example, Canady said that when public health practitioners were focused on childhood obesity, the community responded that if children do not live to be 10, it does not matter if they are fat. In other words, violence and safety were the primary concerns of the community, and public health officials needed to shift their focus to address that. As defined by the Leadership Development National Excellence Collaborative, 4 collaborative leadership in public health means that all the people affected by the decision are a part of the process, and the more that power is shared, the more power all of us working together have to use, Canady said.
Authentic Collaboration Between Institutions and Communities
Canady described three spheres of influence in a model of authentic collaboration between institutions and communities: leadership, the community, and the workforce. There is endorsement by leadership; engagement of, or advocacy by, community members who want to create change; and a workforce that is empowered to respond and to challenge the status quo. Collectively, the impact of the three together is greater than that of any one alone. In many cases, Canady noted, one person represents more than one sphere.
As an example, Canady said that in 1998 the Ingham County Health Department received a grant from the W.K. Kellogg Foundation’s Community Voices: Healthcare for the Underserved initiative to increase access to health care through community engagement. As part of its funded work, Ingham County began facilitated dialogues to discuss how
4 See http://www.collaborativeleadership.org (accessed July 24, 2014).
to get community groups, organizations, and neighborhoods to see health department resources as their assets and how to get the health department to view the community’s assets as its greatest resource. Canady characterized these dialogues as emerging out of the need to recognize the “web of mutuality” between health departments and communities. 5 An outgrowth of these dialogues was the establishment of institutions and organizations that began to work with the health department on these issues, including the African-American Health Institute, the Lansing Latino Health Alliance, and others. These exist, Canady said, because the community drove the health department to use its power to establish those entities. Relationships were also established with leadership in the Mayor’s Initiative on Race and Diversity.
Another example of establishing relationships to mobilize community assets for change in Ingham County is the Power of We Consortium (see Figure 5-2 ). Canady described how the directors of different human services agencies met regularly to ensure there was no redundancy in their services. Canady said that likely because of the mutual dialogue and learning they received individually and institutionally, they realized that others should be at the table joining them. Over time, what was called the human services collaborative, was opened up to the community and the Power of We Consortium was formed. The consortium, Canady said, is a network of networks, comprised of 12 issue-based coalitions as well as other community partners and stakeholders which come together once per month to work on issues of common interest and to hold each other accountable.
Canady also described two current activities in Ingham County that are part of a statewide push for public health professionals to partner with community organizers and to view the community as partners rather than as clients. The Building Bridges Initiative is focused on mobilizing community partnerships to identify and solve health problems and on informing, educating, and empowering people about health issues. The Power to Thrive movement is building a shared culture for change and action, bringing together local health departments, the state department of health, and community organizing entities to consider public health issues in a local context. Canady explained that the movement’s goal is to establish a model of synergy that allows for candid and authentic conversations and discussions that move toward action.
5 Canady mentioned Martin Luther King, Jr., and was likely referring to King’s “Letter from Birmingham Jail,” where he discussed the “network of mutuality” in which whatever threat is faced directly by one, indirectly affects all. Available at http://mlk-kpp01.stanford.edu/index.php/resources/article/annotated_letter_from_birmingham (accessed July 16, 2014).

FIGURE 5-2 The Power of We Consortium structure. NOTE: This figure has been updated since Canady presented it at the workshop, courtesy of the Power of We Consortium. SOURCE: Provided by Power of We Consortium, 2014.
Facilitated Dialogue as a Vehicle for Change
Ingham County used facilitated dialogue as a vehicle for change. In implementing this methodology, it was important to establish what a dialogue is and to distinguish it from debate, training, or conversation. In a debate, Canady said, competing factions use persuasion to convince others of the “best” solution. In contrast, dialogue focuses on a common purpose, emphasizing listening, in order to identify multiple, complementary solutions. Training is a unidirectional flow of information, embracing what is known and teaching new solutions. Dialogue is a mutual exchange of information, embracing what is not known and discovering new solutions together. A conversation is a casual, undirected exploration where differences are marginalized. Dialogue, on the other hand, is a vigorous and directed exploration that welcomes differences (without debating them). The philosophy of the facilitated dialogue, Canady said, is that institutions should “get out of the way” and allow the solutions to emerge according to each community’s vision for being healthy and whole.
Melissa Simon, the panel moderator, summarized some of the key points from the panel presentations, and she noted that some of what was discussed circled back to what keynote speaker Manuel Pastor articulated earlier in the day about sharing power to harness more power (see Chapter 2 ). Simon noted that both panelists demonstrated the power of “we,” and how sharing power among partners—be they organizers, academics, social and health service providers, policy makers, youth, fathers or mothers—speaks to the power of communities. This idea of network building from one person to many, helps propel this work and to scale it. Building powerful communities and community partners is an authentic part of creating change by establishing relationships that involve long-term commitment, mutuality, and shared visions and dreams that need to be reinforced and maintained over time.
Simon continued that it is apparent from the presentations that building a new narrative through facilitated dialogue involving a diversity of community partners can be a vehicle for change. This involves breaking down silos and building relationships with people across sectors. It also involves having authentic dialogues with people and moving beyond the surface to listen and learn from another person’s story, she added. Simon also noted that concealed stories (as discussed by Karen Marshall in Chapter 3 ) needed to be heard more widely so they could be part of the dialogue shaping a shared vision for change. Simon added that achieving the kind of change discussed by the presenters may best be accomplished by rethinking how ecosystem partners can use their relationships strategically to amplify and champion this work through understanding that both the community and academic institutions have resources and assets to help each other.
Engaging the Private Sector
A participant stressed the importance of engaging private sector community partners in a meaningful way. Canady concurred and said that inviting small business owners and representatives to the table is important for discussions about fostering personal responsibility (e.g., what can be done structurally in stores to make sure that the healthy choice is the easy choice, rather than one that requires additional effort or resources). She mentioned the California Pay for Success/Social Impact Bond Initiative as an example of meaningful engagement of private partners. 6
6 Private investors fund preventative or interventional social services, and, if the program is a success, the government reimburses the investors with a return on their investment. See http://nonprofitfinancefund.org/pay-for-success (accessed July 24, 2014).
Collecting Data with Utility in Mind
Many participants discussed the challenges of balancing academia’s need for robust data with community members’ weariness with data collection on issues that they think may be obvious (e.g., everyone in the community already knows they have limited access to fresh food). Phyllis Meadows remarked that community members often feel they can tell the researchers the answers to the questions they are researching, but the researchers end up simply describing the community’s problems over and over, in different ways, or gathering data that does not seem useful to the community and does not help them advance.
Watson-Thompson agreed that there is a tension between the data that academic partners need to collect and the interpretation of that work by communities. She reiterated the value of engaging the community at the beginning of the process in identifying the questions that need to be examined, the different ways in which to examine them, and how best to share and use the results. The researcher’s perspective on the types of data that are appropriate may differ from the community’s perspective on what is meaningful or helpful to them. Data are only good if used, so sharing the data in a way that is understandable to the community is also essential. Traditional academic formats may not be an effective approach. The quantitative piece is more meaningful when matched with the qualitative (i.e., the stories). Watson-Thompson suggested that validity testing is needed to determine if what is being presented has meaning and utility for those it is intended to serve. She also noted the need to be bi-directional with learning and information-sharing processes. It is important to engage the community to educate academia about ways in which information can be presented and disseminated that are meaningful to them and to establish a culture of data-informed decision making that matters for both parties or entities involved. Canady added that the publish-or-perish mentality of academia also affects how researchers work with communities (see Chapter 6 for additional discussion on this topic). Simon reiterated the need to build a pipeline of research scientists, academics, and leaders coming from (and hopefully returning to) these communities.
As in other sessions, many participants in this session asked questions about how to take community aspirations and efforts to promote health to scale. Canady responded that although everyone is eager for rapid change, it took time to make the progress seen today, and it will take time to understand and achieve long-term change. The process, when done correctly, is leading toward something, she said. Citing the united
efforts to respond to H1N1 pandemic influenza as an example, she said that agencies, institutions, and organizations have to come together, recognizing that each has its own agenda or self-interest, but understanding that there will be greater benefit from collective effort. As a community, we need to hold ourselves accountable to demonstrate what is different today compared to 6 months ago, 1 year ago, or 3 years ago, Canady said.
Organizing for Better Health Care
A question was raised about the potential role of community organizing in addressing the waste in health care in order to free up resources for population health and health equity. A participant suggested that patients and people in the communities need to push for quality care. Equity comes from quality across all metrics. Another participant said that organizing people around the cost efficiency of hospitals is not particularly interesting for most people, but there is a lot of public anger concerning costs that can be tapped.
This page intentionally left blank.
The Role and Potential of Communities in Population Health Improvement is the summary of a workshop held by the Institute of Medicine Roundtable on Population Health Improvement in April 2014 that featured invited speakers from community groups that have taken steps to improve the health of their communities. Speakers from communities across the United States discussed the potential roles of communities for improving population health. The workshop focused on youth organizing, community organizing or other types of community participation, and partnerships between community and institutional actors. This report explores the roles and potential of the community as leaders, partners, and facilitators in transforming the social and environmental conditions that shape health and well-being at the local level.
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
- Forgot Password?
- Create Account
- User ID: -->
- Password: -->
Our website has detected that you are using an outdated internet browser. Using an outdated browser can limit your ability to use all of the features on our website, including the ability to make purchases and register for meetings. Please upgrade your browser to improve your experience.
- Directories

- Community Benefit
- Disaster Resources
- Diversity & Disparities
- Environment
- Global Health
- Human Trafficking
- Immigration
- Ministry Formation
- Ministry Identity Assessment
- Palliative Care
- Pastoral Care
- Sponsorship
- We Are Called
- Calendar of Events
- Assembly 2024
- Safety Protocols
- Prayers During the Coronavirus Pandemic
- Meditations
- For Patients & Families
- Observances
- For Those Who Work in Catholic Health Care
- For Meetings
- Social Justice
- Calendar of Prayers
- Prayer Cards
- Health Progress Prayer Services
- World Day of the Sick Blessing
- The Angel Gabriel En Route to Mary
- The Annunciation and St. Ann
- The Visitation and Zechariah
- The Magi Set Up Camp
- The Nativity and The Midwives
- 2020 Advent Reflections
- Lent Reflections Archive
- Video & Audio Reflections
- Inspired by the Saints
- The Synod on Synodality
- Bibliography of Prayers
- Hear Us, Heal Us
- 2018 Month of Prayer
- 2017 Month of Prayer
- Links to Other Prayer Resources
- Week of Thanks
- Current Issue
- Prayer Service Archives
- DEI Discussion Guide
- Advertising Rates & Specifications
- Subscription Rates
- Author's Guide
- Submit an Article
- Health Progress 100
- HCEUSA Subject Index
- Periodical Review
- 2023 Christmas Advertising
- Submit story ideas to the editor

- Public Health's Role: Collaborating for Healthy Communities
BY: ROBERT M. PESTRONK, M.P.H., JULIA JOH ELLIGERS, M.P.H. and BARBARA LAYMON, M.P.H.
The Commonwealth Center for Government Studies reports that the moment has come to take a fresh look at traditional practices and relationships and to develop new approaches that will serve our communities better and more efficiently. 1 The center also recommends that hospital governance take oversight for both system-wide community benefit policies and programs and for the hospital's role and priorities in the realm of population health. Although many different solutions are now being proposed, most informed observers are unified on one point: The value and the quality of services should correspond to the size of the investment in the clinical care and public health sectors. 2, 3
Local health departments, too, are being asked to re-examine and reprioritize their approaches to improving the public's health 4 through proof of capacity, 5 continuous improvement of the activities they perform 6 and oversight for the outcomes achieved or desired by the public health and health care sector. 7 The National Association of County and City Health Officials (NACCHO), representing the 2,800 local health departments across the country, sees this time as a true opportunity to improve the public's health.
As collaborative relationships between hospitals and local health departments become the new normal, opportunities abound. The new "community benefit" definition and requirements in the Affordable Care Act (ACA) 8 require hospitals to conduct a community health assessment and produce a community improvement plan. Local health departments are required to produce an assessment and improvement plans. Why not plan and conduct these in a collaborative fashion, making use of the assets, capabilities and capacities which each can offer?
Assessment is a core function of public health. Many local health departments have traditionally conducted community health assessments 9 — approximately 60 percent in the last five years. 10 Many hospitals also have conducted or participated in community health needs assessments related to community benefit programs. Collaborative work will allow local health departments and hospitals around the country to build upon their existing expertise, relationships and experiences to conduct various improvement initiatives partnering together around specific goals.
These efforts to partner around community health assessment and improvement planning span four types of strategies: networking, coordinating, cooperating and collaborating. With such collaboration, community health assessment and improvement activities can be precursors to real gains in population health and an integral part of continuous improvement processes towards that goal.
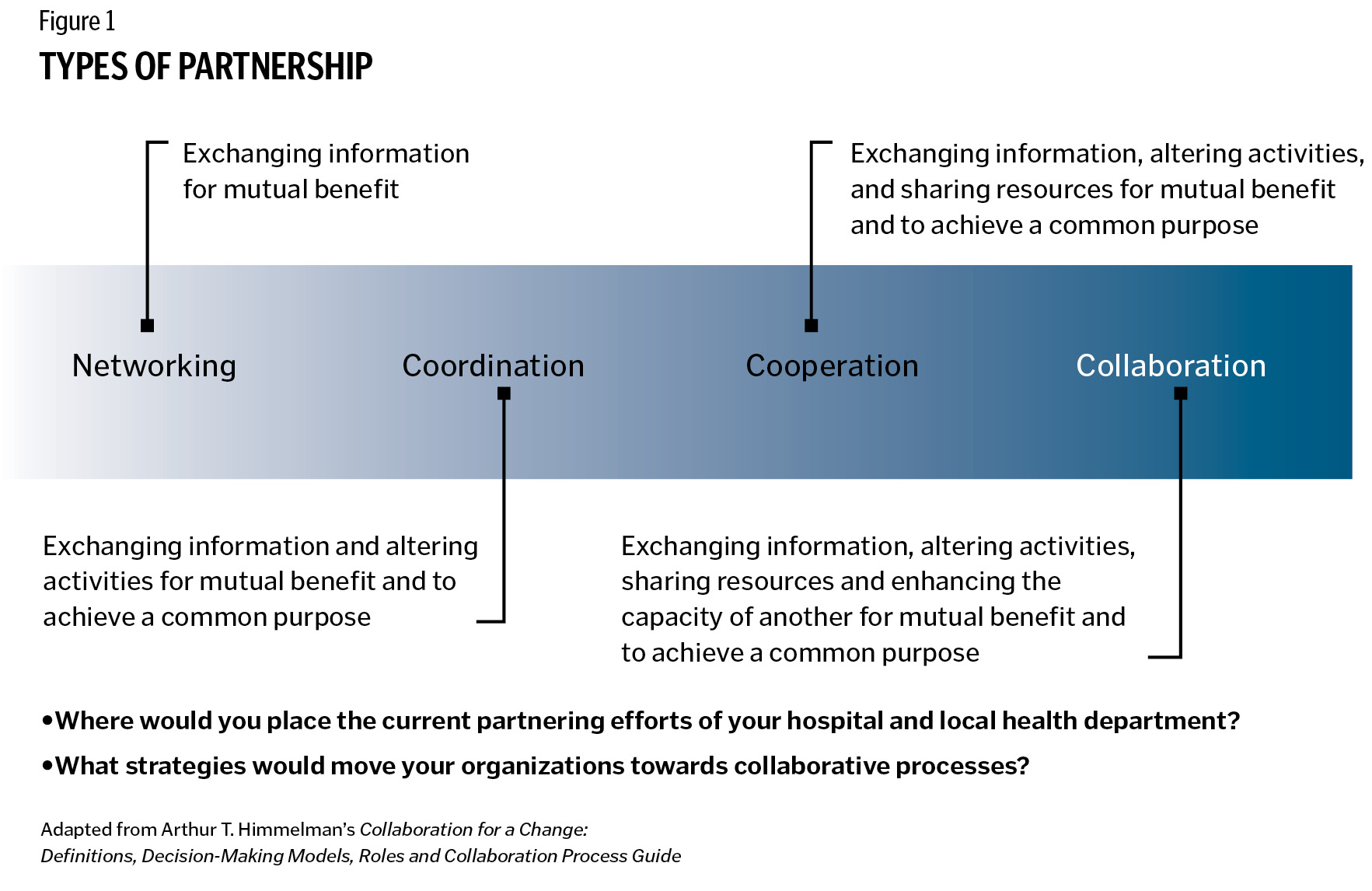
KEYS TO SUCCESSFUL COLLABORATION Over the past year, NACCHO conducted three focus groups with leaders of health departments and nonprofit hospitals across the country to identify what makes community health assessment and improvement collaborations successful between local health departments and hospitals. Common strategies undergirded successful partnerships:
Formalized mechanisms. Communities where local health departments and hospitals work well together have constructed a formalized forum for dialogue. A memorandum of understanding helps clarify the roles and responsibilities of each entity. Further, a written memorandum of understanding helps ensure that collaborative efforts continue even if leadership at either organization changes. In communities where the local health department and hospital do not have a history of working together, a third party can help. In one Florida community, for example, the local health department and hospital used their health planning council to build and strengthen their relationship.
Vision. Successful collaboration is contingent on a shared vision or goal. One focus group participant said, "There's certainly a difference between what is the focus of public health versus individual care and private health care. But in focusing on some of the common goal areas ... that made a big difference."
Another participant pointed out it is important not only to think about what the product and process will look like, but ultimately to determine "what is the end game around the assessment?"
Communication. Frank, open and candid conversations between leaders and staff of local health departments and hospitals enrich relationships between collaboration partners. One local health department representative noted that department staff members learned about the financial and political realities that confront their nonprofit hospital, and their hospital partners learned about the political and financial challenges of governmental public health practice. Shared learning helped develop mutual respect. Together they were more effective in engaging other community organizations and partners.
Neutral convener. When there is more than one hospital in a community, a neutral convener can be helpful to the process of working together. Many local health departments have staff with facilitation skills that can be used to structure and coordinate collaborative assessment and improvement activities involving usually competitive area hospitals. One hospital executive said, "There are times when you have to put down the competition and raise a flag of collaboration, and that's what we've been able to do. I credit that to the health department for being able to put us all around the table and get some work done."
Champions and Leaders. Effective collaboration requires each organization to have champions who will move the effort forward. The champions can arise from formal leaders or other staff members; each background has advantages. A formal organizational leader can motivate and assign work to staff members, while a staff member's interest, energy and enthusiasm can infect leaders and other staff.
A successful collaboration needs support from local health officials and from hospital executives. Focus group participants noted that with leadership on board, their staffs, the community and partner organizations then seem to acknowledge the importance of assessment and improvement work. Several focus group participants commented that hospital executives, in particular, bring a level of prestige to assessment and improvement initiatives.
Attitude. Building trust and positive relationships takes time. A representative of a hospital nonprofit commented, "The hospitals that see the community health improvement process as an opportunity to improve community health, rather than an obligation, tend to be more successful." Challenges arise in any relationship. Focus groups revealed some of them. Competitive hospitals usually can work together on community health assessment processes, even if it's difficult for them to work together on other activities. One focus group member said that in her jurisdiction, competing hospitals pooled their resources to make sure the needs and requirements of the community health needs assessment process were met in a collaborative way. The group also included other health care providers (for example, a rehabilitation center) who helped bring in more data and ideas.
One participant observed that when hospitals are highly competitive, it's sometimes difficult to get them both on the same page, but once you get one hospital on board, other hospitals begin to show interest.
The timetable of the new Internal Revenue Service requirement for hospitals does not necessarily coincide with the timing of health department reporting and planning requirements; however, hospitals and health departments can work together to design a process and data management system that produces results they each can use.
Health department jurisdictions may encompass several hospitals. Hospital market areas may span many local health department jurisdictions. Flexible designs and processes among multiple hospitals and local health departments can overcome jurisdictional boundary issues.
TOWARDS HEALTHIER COMMUNITIES There are many ways that local health departments and hospitals can pool their resources of time, talents, data, knowledge, partner base and funding to support collaborative efforts to achieve healthier communities. Local health departments and hospitals bring complementary strengths in many areas, including:
Data: While local health departments have vital statistics and county mortality and morbidity data on their jurisdictional population, hospitals have data on their patient population. Some local health departments have data specific to census tracks or neighborhoods, data on social determinants of health and data on behavioral risk factors. Further, many health departments have data on the communities' perceptions of quality of life. Some local health departments have conducted forces of change assessments that identify externalities that can have an impact on health, while others have conducted public health system assessments that measure how well local organizations work together to provide essential services. Many local health departments also have collected qualitative data on assets that can be leveraged to solve health problems. When viewed together, data from local health departments and from hospitals provides a more complete picture of a community's health challenges. That picture creates a shared understanding that can inform potential solutions.
Skills and Processes: Many local health departments have skills specific to community health assessment and improvement. Local health departments already have well-established processes for completing community health assessment and improvement processes. In focus groups, several local health department representatives commented that their hospital partners were happy to hear the local health department had a structured process like Mobilizing for Action through Planning and Partnerships (MAPP) 11 that would help them meet their assessment requirements.
Local health departments also may have assessment-related experience in data collection, data analysis, community outreach, facilitation, health education and wellness programs. One advantage of the local health department as facilitator is its ability to find and maintain multiple contacts — many champions — within partner organizations in order to manage details which come up in collaborative efforts. Similarly, hospitals may have processes in place to conduct community health improvement work such as patient education, wellness programs, outreach and other activities that can be natural adjuncts to local health department activity.
Partners: Many local health departments have access to a variety of nontraditional and community partners, working directly with community residents and grassroots organizations. Some have staff members with skills in qualitative methods, such as key-informant interviews and focus groups, whose work provides rich context and explanatory power to quantitative data. Hospitals have partners and board members who bring a certain stature to the work of engaging a community, adding legitimacy and the chance of acceptance for initiatives that may bring far-reaching health changes. A health department executive added that it's important to have the right people in the room who are aware of all the resources available from their organizations.
Health Equity: In the community health dialogue, local health departments bring a public health view regarding the central importance of assuring the conditions where people can be healthy. Hospitals bring experience in the care and treatment of members of marginalized populations, and they bring a needed perspective to the health equity conversation.
Through collaborative community health assessment, local health departments and hospitals have been able to implement well-informed organizational strategic plans and collaborative, overarching community-health improvement plans. Collaborative community health assessments have allowed organizations to identify the needs of specific subpopulations and develop solutions to their unique needs. What's more, other organizations then can align and integrate portions of their strategic plans with a community health improvement plan. Further, collaboration among local health departments, hospitals and other entities have resulted in comprehensive assessments that inform grant proposals, public policy and ways for organizations to work more efficiently and effectively together.
Partnerships between hospitals and local health departments have proven productive in many communities. Better organized systems of care can assure that both treatment and prevention are artful and evidence-based. Designed attention to the unique goals, roles and needs of hospitals and local health departments will benefit from the strengths and assets each partner offers. Communication and dialogue among hospitals, health departments and other local partners can lead to concurrence and a prioritization based on the community's risks to health and remedies to prevent disease. Other benefits include a shared understanding of problems, transparency about efforts to improve health and treat illness and better public support for each partner and the partnership.
Collaborative community health assessment and community health improvement processes should be standard practice everywhere. Effective collaboration will require intent and patience as very different cultures come to know each other better. Leadership in both organizations must encourage the awkward steps that will no doubt precede the more elegant and practiced choreography of effective collaborations.
What will be discovered on the journey is a better command of the role that each entity can play in a re-forming medical and public health system and, more important, better success with their shared mission of population health.
ROBERT M. PESTRONK is executive director for the National Association of County and City Health Officials (NACCHO) in Washington, D.C.
JULIA JOH ELLIGERS is NACCHO's director, assessment, planning and workforce development, Washington, D.C.
BARBARA LAYMON is lead program analyst for assessment and planning within NACCHO's public health infrastructure and systems team, Washington, D.C.
- Lawrence Prybil et al., Governance in Large Nonprofit Health Systems: Current Profile and Emerging Patterns (Lexington, Ky.: Commonwealth Center for Governance Studies, 2012). www.hallrender.com/health_care_law/library/articles/1220/Governance_booklet.pdf .
- Joseph R. Antos, Mark V. Pauly and Gail Wilensky, "Bending the Cost Curve through Market-Based Incentives," New England Journal of Medicine 367 (Sept. 6, 2012), www.nejm.org/doi/full/10.1056/NEJMsb1207996 (accessed 8/3/12).
- Ezekiel Emanuel et al., "A Systemic Approach to Containing Health Care Spending," New England Journal of Medicine 367 (Sept. 6, 2012), www.nejm.org/doi/full/10.1056/NEJMsb1205901 (accessed 8/3/12).
- Institute of Medicine, For the Public's Health: The Role of Measurement in Action and Accountability (Washington, D.C.: National Academy of Sciences, 2010). See more at www.iom.edu/Reports/2010/For-the-Publics-Health-The-Role-of-Measurement-in-Action-and-Accountability.aspx .
- See Public Health Accreditation Board, www.phaboard.org/accreditation-overview/what-is-accreditation/ .
- National Association of County and City Health Officials, Operational Definition of Public Health (Washington, D.C.: NACCHO, 2005), www.naccho.org/topics/infrastructure/accreditation/upload/OperationalDefinitionBrochure-2.pdf .
- IOM, For the Public's Health .
- The Affordable Care Act requires nonprofit hospitals to conduct community health needs assessments. The public health field does not limit community health assessments to identifying needs and therefore are using the term community health assessment, excluding the explicit reference to needs. Community health assessments that are limited to uncovering needs do not comprehensively identify community issues and solutions to addressing problems. Often public health community health assessments include information about community assets and other information about forces, quality of life and how different providers work together to deliver services, which provides a comprehensive illustration on why needs and public health problems exist in a community.
- The National Association of County and City Health Officials, Issue Brief: Collaborating through Community Health Assessment to Improve the Public's Health . December 2011. Downloaded at www.naccho.org/topics/infrastructure/mapp/loader.cfm?csModule=security/getfile&pageID=228716 .
- National Association of County and City Health Officials, 2010 National Profile of Local Health Departments (Washington, D.C.: NACCHO, 2011), www.naccho.org/topics/infrastructure/profile/resources/2010report/upload/2010_Profile_main_report-web.pdf .
- For more information about the MAPP (Mobilizing for Action through Planning and Partnerships) process, visit www.naccho.org/mapp .
Copyright © 2013 by the Catholic Health Association of the United States For reprint permission, contact Betty Crosby or call (314) 253-3477.
Copyright © 2013 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3490.
Back to Top
Also in this Issue
- U.S. Health Care Is Moving Upstream
- Public Health Workers Needed: Educational Programs Grow as Shortage Looms
- Catholic Health Systems Steer the New Course
- A Model Strategy: Targeting Infant Mortality Can Produce Results
1625 Eye Street NW Suite 550 Washington, DC 20006 (202) 296-3993
ST. LOUIS OFFICE
4455 Woodson Road St. Louis, MO 63134 (314) 427-2500
- Social Media
- Focus Areas
- Publications
- Career Center
We Will Empower Bold Change to Elevate Human Flourishing SM
© The Catholic Health Association of the United States. All Rights Reserved.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Finding middle way out of Gaza war

Navigating Harvard with a non-apparent disability

Yes, it’s exciting. Just don’t look at the sun.
Community engaged learning brings students, locals together to solve health problems.

Photo by Catherine Seraphin
Over the summer, eight students from Harvard T.H. Chan School of Public Health partnered with organizations and community members from Boston to Nairobi, Kenya, to learn about and help address locally identified public health problems. The students — members of the spring 2022 cohort of Community Engaged Learning Fellows — spoke about their work at a Dec. 6 event at the School.
The students’ projects included working with a Boston health collaborative, a clinic in Uganda, and cobalt miners in the Democratic Republic of Congo, among others. A common thread across the students’ presentations was their effort to draw on community knowledge to develop creative solutions together.
Jen Cruz , Ph.D. ’26, partnered with the Allston Brighton Health Collaborative (ABHC), a public health nonprofit that convenes organizations, health advocates, elected officials, and residents to improve the systems that impact health and well-being in Boston’s Allston and Brighton neighborhoods.
Before she worked with ABHC on her fellowship project, Cruz — an Allston resident herself — volunteered for the Collaborative’s vaccine clinic. Since then, she has supported ABHC by serving on its mental wellness and transportation working committees, and plans to join the advisory board in 2023.
In her committee work, Cruz became aware that some of her fellow volunteers were reticent about advocating for their own priorities regarding the Collaborative’s decision-making about programs and policies for marginalized and under-resourced community members. Instead, they sometimes would ask Cruz to speak on their behalf in the hope that her public health expertise would strengthen their input.
“You shouldn’t have to have an M.P.H. or degree in public health to contribute to the conversation, understand what the news is telling you, and make informed decisions about your health,” Cruz said. So, for her fellowship project, Cruz helped develop an educational program aimed at engaging community members as leaders in ABHC’s work.
Erin McGuinness , Dr.P.H. ’24, and Yacine Fall , S.M. ’23 — the inaugural recipients of the Global Mental Health Fellowship , which offers students opportunities to partner with organizations outside the U.S. to address mental health issues in their communities — spoke about their work collaborating with the John Cleaver Kelly Clinic in Kabale, Uganda. They worked with the clinic on evaluating its community mental health outreach, including understanding the perspective of community health workers, patients, and families.
Alina Bhojani , S.M. ’23, and Alya Al Sager , S.M .’23, discussed their experience working with Kidogo, a Kenya-based social enterprise building an expanding network of childcare centers in Nairobi’s urban slums. Kidogo supports female entrepreneurs — who they call “Mamapreneurs” — in starting childcare businesses in their own communities. Al Sager and Bhojani worked with Kidogo to tailor its early childhood development program so that Mamapreneurs would be more likely to use it in their centers.
Learning from locals
Under the Community Engaged Learning Fellows program, student cohorts are chosen each spring and fall to help respond to community-identified concerns, striving to balance the service they provide with their learning experience. Jocelyn Chu , director of the program, spoke about the benefits students gain from their field education and practice experiences.
Share this article
You might like.
Educators, activists explore peacebuilding based on shared desires for ‘freedom and equality and independence’ at Weatherhead panel

4 students with conditions ranging from diabetes to narcolepsy describe daily challenges that may not be obvious to their classmates and professors

Lab, telescope specialist details Harvard eclipse-viewing party, offers safety tips
College accepts 1,937 to Class of 2028
Students represent 94 countries, all 50 states
Pushing back on DEI ‘orthodoxy’
Panelists support diversity efforts but worry that current model is too narrow, denying institutions the benefit of other voices, ideas
So what exactly makes Taylor Swift so great?
Experts weigh in on pop superstar's cultural and financial impact as her tours and albums continue to break records.
- Community Engagement is Vital to…
Community Engagement is Vital to Solving Local Health Problems
Date posted:.
Editor's note: This post is part of our series in recognition of PolicyLab's 10th anniversary and our ongoing efforts to chart new frontiers in children's health research and policy. Read the first post here , and check back for more content throughout the year!
As one of PolicyLab’s founding members, I have had the privilege of conducting research in the city of Philadelphia for over 17 years. Philadelphia is recognized as one of the poorest of the 11 largest cities in the U.S. As a consequence, Philadelphia’s children are in relatively poor overall health compared to children in other large cities: ranked highest in obesity, smoke exposure, infant and child mortality, low birth weight births and violent crime, and lowest in on-time high school graduation. Yet these statistics belie a vibrant and diverse community, committed to improving the lives of young children. I know this to be true, since I’ve worked with many community organizations and their leadership on projects to improve the lives of Philadelphia youth.
As a result, I have come to value community-engaged (CE) research in my approach to addressing important child health problems. But what is CE research? The Centers for Disease Control and Prevention has defined community engagement as “the process of working collaboratively with and through groups of people affiliated by geographic proximity, special interest, or similar situations to address issues affecting the well-being of those people.” Therefore, CE research is a collaborative process that involves academic researchers and community members working together to solve vexing health problems that neither is adequately positioned on their own to solve.
Through CE research, community members bring insight and local knowledge of community health problems to the table, while academic researchers bring an understanding of research design and study conduct. Community members help researchers prioritize research questions, identify appropriate research designs and interventions and interpret and disseminate findings to empower the community . This results in research findings that establish generalizable knowledge while being relevant to the context in which they are placed and, therefore, positioned to improve community health. In the lexicon of research phases, it is considered to be a T3 translational study.
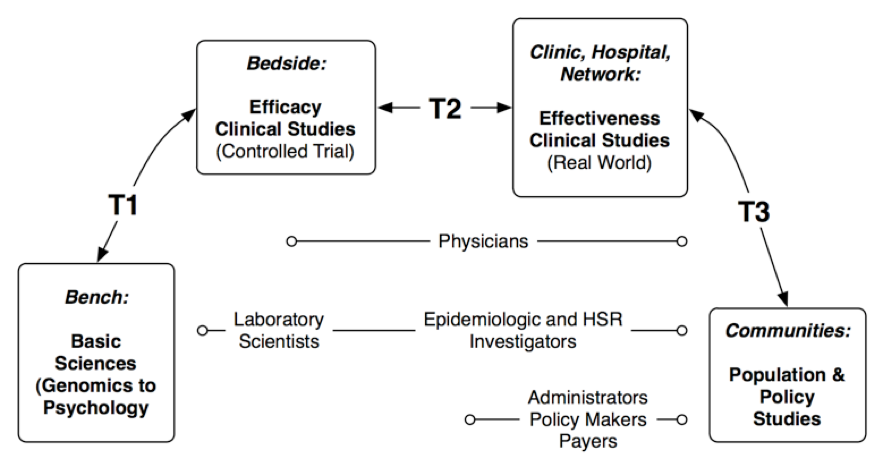
It is exciting to see the growth in CE research since the founding of PolicyLab. Many PolicyLab investigators are turning to CE research designs to address questions of public health importance, including smoking cessation, obesity, school violence, racism, maternal depression and immigrant health to name a few. Understanding the importance of collaborative partnerships to develop sustainable solutions, my colleagues are developing projects that involve the local health department, advocacy organizations, schools and service providers.
Take as an example a project that I’m partnering on with Drs. Marsha Gerdes and Katherine Yun. We are working with members of the city of Philadelphia’s Division of Intellectual disAbility Services , KenCrest and Public Health Management Corporation to study the effects of patient navigation for children with developmental delays who have been referred to Early Intervention . Members of these community organizations have the intimate knowledge of how Philadelphia’s Infant Toddler Early Intervention Program works and are positioned to disseminate our research findings locally. It has been an empowering and fruitful partnership that is only increasing our ability to develop evidence-based sustainable solutions for these youth.
As we mark PolicyLab’s 10 th anniversary and think about charting new frontiers in children’s health policy, I expect that PolicyLab investigators will continue to rely on CE research to address difficult problems and to help improve the lives of Philadelphia’s children. I look forward to partnering with them and with our community partners on this exciting research.
Latest Blog Posts

Q&A: Engaging Communities to Alleviate Period Poverty with Lynette Medley
There are 16.9 million women, girls and all other people who experience a menstrual cycle in the United States living in poverty, many of whom are…
Supporting Early Literacy by Reaching Families Beyond the Exam Room Walls in 200 Words
March marks the celebration of National Reading Month! At PolicyLab and Reach Out and Read Greater Philadelphia (RORGP), we champion the role of…

Eating Disorders Affect Boys and Men Too—Research and Policy Need to Catch Up
A Google image search for “eating disorders” will return countless photos of young girls and women staring miserably at a plate or at the number on a…
Check out our new Publications View Publications
Adolescent Health & Well-Being
Behavioral health, population health sciences, health equity, family & community health.
A collaborative approach to community health issues
Asu college of health solutions celebrates 10 years of health innovation, looks forward.

Sometimes a good idea doesn’t have to be sold, it just needs the chance to be heard.
That’s how the idea behind Arizona State University’s College of Health Solutions revealed itself to Dorothy Sears, the college’s executive director of clinical and community translational science and professor of nutrition.
As the College of Health Solutions celebrates its 10th anniversary, faculty, staff and alumni are reflecting on the history of the school while looking forward to what’s next.
The college was formed in 2012 when a group of separate academic units located across three campuses were brought together under one umbrella to offer students a comprehensive education in health.
In 2017, the new leader of the College of Health Solutions, Deborah Helitzer, was asked by ASU President Michael Crow to reimagine how those separate units could be better aligned to address the ASU Charter. That charter says that ASU must assume, among other things, fundamental responsibility for the overall health of the communities it serves.
With that charge, and a courageous changemaker at the helm, a collaborative process began to better align the college’s mission and structure with the university’s charter.
That idea appealed to Sears, who had a taste of a similar collaborative effort while working on a grant from the National Institutes of Health at a previous institution. The only problem was once that grant ran out, so did the spirit of collaboration.
But a chance meeting with College of Health Solutions Associate Dean and Professor Carol Johnston while Sears was on her way to a scientific conference in Mexico gave her an idea where she could find that collaborative spirit again.
Sears said, “While we flew down together, we just talked, talked and talked waiting for the plane and in line at customs and waiting to get bags. We had so much in common.”
Johnston later invited Sears to come to ASU to give a talk and she fell in love with the place.
“I was seeing the beautiful new facilities, that was the initial attraction; I wasn’t even considering leaving my (previous) institution at that point,” Sears said. “Then meeting (College of Health Solutions) Dean Deborah Helitzer was amazing. I felt like I had landed on another planet.
“Learning how the dean had led a process that resulted in eliminating all the departments in the college, I was like, wooo! This is awesome!”

College of Health Solutions Dean Deborah Helitzer (at podium) leads a visioning exercise shortly after arriving at Arizona State University in 2017.
A new approach to educating health leaders
The evolution of the College of Health Solutions was well underway by the time Sears came on board in 2018.
In 2012, Dr. Keith Lindor, former dean of the Mayo Clinic Alix School of Medicine, was named executive vice provost and founding dean of a newly formed College of Health Solutions. Lindor worked to create a new school for the science of health care delivery and strengthen the university’s partnership with Mayo Clinic.
The new health college also included previously existing academic units such as:
School of Nutrition and Health Promotion.
Department of Biomedical Informatics.
School of Biological and Health Systems Engineering.
Center for Health Innovation and Clinical Trials.
Center for Health Information and Research.
Center for World Health Promotion and Disease Prevention.
Health Care Delivery and Policy Program.
Healthcare Transformation Institute.
Those early years saw the college as a collection of health-related units and faculty with significant domain expertise who were spread out across three ASU campuses. Bringing that collection together to form a unified, integrated college would require significant change – change that might not be popular with everyone.
Julie Liss, now an associate dean and professor in the College of Health Solutions, came to ASU in 2013 as a professor in the former Department of Speech and Hearing Science, said that while some adapted to the change reluctantly, others embraced it.
“Other people were saying, ‘Wow, I’m meeting more people than I’ve ever known in the college, I’m able to do things I had never been able to do before,’” Liss said.
She said that accelerated when Helitzer was named dean of the College of Health Solutions in 2017.
“There were two eras,” Liss said. “The Dean Lindor era was getting all of our building blocks in place. The Dean Helitzer era was figuring out how those blocks could build something bigger, synergistically.”
Accelerating a rocket of change
Helitzer came to ASU from the University of New Mexico where she was the founding dean of the College of Population Health. While there, she led the development and implementation of the country’s first undergraduate degree in population health.
Her innovative work there caught the attention of ASU President Michael Crow. She was charged with leading the process of reimagining how the college could be positioned to best address major health issues in the community.
And she was asked to do it quickly.

Deborah Helitzer
“When President Crow introduced me to the faculty he said, ‘I told her I’m going to put her on a rocket and I’m expecting fast change,’” Helitzer said. “I said, ‘Well, President Crow, if you give me the fuel...' Everyone laughed and said, ‘We’re going to have to watch out for her.’”
In the fall of 2017 Helitzer assembled and led an executive visioning team working to reimagine what the college would become. That visioning project included ideas and input from 300 faculty, staff, administrators, community members and health system representatives. A new vision and structure emerged and Helitzer began leading the implementation of that vision, knocking down barriers to collaboration.
“There was no understanding of each other, no knowledge of each other,” Helitzer said. “The faculty were in the same physical building but didn’t know each other or talk to each other. We’ve worked to create structures to address that and we’re still working on it, but I’ve tried to put us on the path.”
One big idea that came out of the visioning effort is the formation of translational teams.
A unique approach to health solutions
Translational teams , a component of the new college structure, bring together researchers, teaching faculty, clinical and community partners, industry innovators and students with different skills and perspectives. By bringing all kinds of people together, translational teams aim to better understand the different layers of the problem they are trying to solve from the ground up. This translational approach takes advantage of the school’s work to break down barriers that have traditionally stopped faculty and students from different disciplines from working together.
It’s a holistic approach to solving the problems facing health care professionals and the essence of understanding the whole person, rather than specific diseases.
“You can look at the molecular level of a disease or condition,” Johnston said. “Then you can look at the dietary and exercise components. And then you can see how (that solution) can be introduced into a community to promote population health. You have all those fields going on. The translational piece is unique. I never heard of it until we started doing it.”
Translational teams at the College of Health Solutions are working on health problems including:
Autism spectrum disorder.
Cancer prevention and control.
Metabolic health.
Substance abuse.
They are studying the health needs of specific populations, such as women, children and those with significant health disparities, because those groups have special needs that are not experienced by other populations.
In addition to the creation of translational teams, the revisioning process also resulted in a charter for the College of Health Solutions.
That charter reads:
"The College of Health Solutions at Arizona State University is committed to translating scientific health research and discovery into practice. We prepare students to address the challenges facing our populations to stay healthy, improve their health and manage chronic disease. We bring people together to improve the health of the communities we serve, reaching them where they live, learn, work and play throughout the lifespan."
That statement helps to provide direction and focus, as well as some insight into the future of the College of Health Solutions. The college’s charter is directly aligned with the ASU Charter , specifically the last phrase, which mentions community health.
In the coming years, Helitzer sees the college being recognized as leading innovation in the field of health education, just as the university as a whole is recognized for innovation.
She would also like to see the college as having played an integral role in addressing the health needs of the community.
“It is critical that we work with the community to solve their problems, not what we see as their problems, but what they see as their problems,” Helitzer said. “That means our faculty must be nimble and will change or tweak what they’re doing to fit the needs of the community.”
Helitzer related that goal with something she experienced while working on malaria prevention in Africa. She said her group was talking to people about taking steps such as using bed nets and screens and ridding the area of standing water to control mosquitos.
“I remember going to one village and saying we want to help you with this,” she said. “They said, ‘First you get us running water and then we’ll be happy to talk with you about that.’ We worked on getting running water in the area and then they trusted us because that was what they needed. Then we could talk about malaria, which was also a problem for them, but it wasn’t the primary problem.”
Another outcome Helitzer would like to see as a result of the collaborative structure is for the students to gain a broader understanding of what the college has to offer and the many ways they can learn to make an impact.
“I’ve been saying we should have the first-year students have a course, or two semesters, to learn about all of the programs in the college and how we work together,” Helitzer said. “Then they could choose a major, knowing what role it plays in solving health problems.”
Helping students achieve their goals
Students are attracted to the forward-thinking, innovative nature of the College of Health Solutions, offering them a unique path toward meaningful change in health.
Vivienne Gellert, BS medical studies ’17, said her personal experience with health care shaped her views of the system and inspired her to take action. She said her education at the College of Health Solutions helped her reach those goals.
Gellert was badly injured in an automobile accident while she was in high school and saw first hand how frustrating and inefficient the system could be.
“You can ask anyone and they’ll tell you the health care system is broken,” Gellert said. “It’s easy to say that and get super frustrated with it, but at the end of the day, what are you going to do about it? In order to do something about it, we have to do something different and (the College of Health Solutions) prepared me to do just that.”
Gellert’s solution started with putting an argument she used in debate class into action. Her idea was based on connecting with people who are experiencing homeless in downtown Phoenix. The title of that speech was “Give a man your jacket, not your dollar.”
That led to the creation of a nonprofit organization called BakPak while Gellert was still in college. It was designed to directly connect people experiencing homelessness to resources and became the basis for a nonprofit, Elaine, and a company she has since founded named Gellert Health.
She said her education in medical studies helped her carry out her vision. And she said the College of Health Solutions will help countless others achieve their goals as well.
“If you look at some of the graduates of the College of Health Solutions I’ve met, they’re incredible,” Gellert said. “They are going to medical school. They are starting their own companies. They are going to work for companies that are directly touching patients' lives and they’re bringing new knowledge from their education to implement change.
“In the spirit of the 10th anniversary, I think we should take a minute to look at the contributions that the College of Health Solutions has already made to our community. They should feel honored they’re there every day with these students. It’s working.”
The College of Health Solutions will celebrate its 10th anniversary in collaboration with the community at Celebration of Health on Wednessday, Oct. 19, at El Chorro in Paradise Valley, Arizona. Sponsorships and tickets are available and all donations will directly support students through the college’s Student Scholarship Fund.
Top photo: ASU nutrition students make a l ow-sodium, diabetic-friendly Tuscan vegetable soup at the ASU Kitchen Café in the College of Health Solutions in downtown Phoenix. Photo by Charlie Leight/ASU News
More Health and medicine
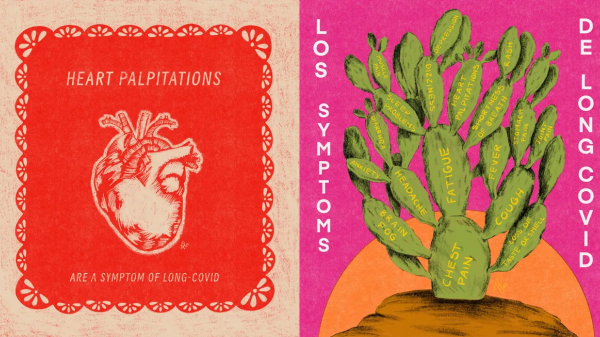
Health communication program brings long COVID awareness to Latinos
After COVID-19 hit the Latino community especially hard, Gilberto Lopez created COVIDLatino, a health communication program designed to share accurate, timely, evidence-based and culturally tailored…
Gates Foundation to fund research on antibiotic resistance
Antibiotic resistance, what happens when germs develop the ability to defeat the drugs designed to kill them, is a growing concern among scientists today. When bacteria become resistant to…
ASU epidemiologist on the rise in US measles cases
The Centers for Disease Control and Prevention issued an alert this month about a rise in measles cases worldwide. And as of March 21, a total of 64 measles cases were reported in 17 states,…
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Jamison DT, Gelband H, Horton S, et al., editors. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd edition. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017 Nov 27. doi: 10.1596/978-1-4648-0527-1_ch14


Disease Control Priorities: Improving Health and Reducing Poverty. 3rd edition.
Chapter 14 community platforms for public health interventions.
Melissa Sherry , Abdul Ghaffar , and David Bishai .

Corresponding author: Melissa Sherry, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, United States; ude.uhj@4yrrehsm .
- Introduction
Community health platforms are the partnerships formed to assess and ensure public health. They provide the context in which outside interventions should be implemented and sustained, and they offer a way to develop and maintain community-centered solutions. Although local boards of health and health departments are the official bodies with the mandate to sustain strong community health platforms, they do not always achieve their full potential ( Bellagio District Public Health Workshop Participants 2016 ). In the absence of an effective government presence, nongovernmental organizations (NGOs) can build community health platforms.
Well-functioning community health platforms can serve as vehicles for health information and advocacy and can convene local resources to support successful public health interventions. Well-designed and well-implemented community health platforms can function as the engine in the public health cycle of convening communities to monitor, review, and act ( figure 14.1 ). These are functional tasks that are best conducted in a partnership among public health professionals, politicians, and community members. Effective partnerships among these parties ensure that health data are collected to answer questions posed by the community, that local health data are shared with the community to guide actions, and that actions marshal all of a community’s human and capital resources as well as public revenue. Then the cycle repeats. A community that has the ability to engage successfully in the cycle shown in figure 14.1 has a platform that can support all types of community health initiatives.
Figure 14.1
Public Health Cycle: Monitor, Review, and Act.
The provision of legal authority for community health platforms can be traced to England’s first health law, the Public Health Act of 1848, which gave cities the option to create local health boards ( Rosen 1958 ; Szreter 1988 ). In the mid-nineteenth century, functional health departments were established throughout Canada, Europe, and the United States before the development of effective medical care and drove the dramatic decline in mortality in the twentieth century ( McKeown, Record, and Turner 1975 ). However, western governments had largely omitted the creation of functioning local health departments when they formed colonies in the Americas, Africa, and Asia; countries that gained independence in the mid-1900s faced an urgent need to catch up. By the late 20th century, the growing recognition that public health and primary care were lagging became the topic of international concern. In 1978, an International Conference on Primary Health Care in Alma-Ata, USSR, attended by nearly all member nations of the World Health Organization and the United Nations Children’s Fund, demonstrated the degree of concern about access to primary health care ( Lawn and others 2008 ). It resulted in the Declaration of Alma-Ata.
Chapter Overview
The Declaration of Alma-Ata asserted that health is a fundamental human right and that community consultation and participation in health care are essential elements of successful programs ( Lawn and others 2008 ; Rohde and others 2008 ). Following the declaration, global health indicators improved despite inadequate adherence to the principles laid out in the declaration. The recent transition from the Millennium Development Goals to the Sustainable Development Goals of the United Nations has renewed attention to strategies that build on local capacity to strengthen community health platforms ( Open Working Group of the General Assembly 2014 ).
This chapter presents a brief review of how the public health cycle supports the sustained success of any of the interventions discussed in the Disease Control Priorities volumes. It offers a typology of the stages of development of community health platforms, as well as a framework for assessing their success. We illustrate four stages of development of community health platforms with four case studies that range from a most developed case in Indonesia to a primitive case of near-paralysis of the state’s efforts in public health. The chapter closes with a discussion of investment opportunities for policy makers who are interested in strengthening community health platforms.
Background and Historical Context
The lack of a clear roadmap to implement community involvement, combined with changes in the global economy, slowed the progress of low- and middle-income countries in achieving the primary health care goals set by Alma-Ata ( Lawn and others 2008 ; Rohde and others 2008 ). The Cold War fostered a culture of development planning that emphasized interventions that were rapidly deployed and easily measured. Health commodities, such as vaccines, oral rehydration solutions, micronutrients, contraceptives, and antibiotics, became the focus of health care systems ( Lawn and others 2008 ; Perry 2013). The emphasis of global health donors on results and short project cycles made the focus on commodities rather than systems more expedient.
The urgency of saving lives in the moment and the truth that the commodities really did save lives perpetuated a stronger emphasis on delivery of medical services and health care goods and a lighter emphasis on communities’ development of Alma-Ata—style platforms. The term vertical was used to define projects focused on getting a selected health commodity or service to households in the most expedient way, typically using a stand-alone organization of staff, vehicles, and capital. The term horizontal was used to define initiatives to build more comprehensive institutions of primary care services and for population-level public health. A short-term focus on vertical programs delivering good health at low cost crowded out attention to building long-term horizontal platforms. The World Development Report 1993 : Investing in Health ( World Bank 1993 ) offered an excellent listing of population-level public health interventions that could be implemented, but it neglected any discussion of how to make them happen, other than by raising money. This report was novel in that it demonstrated for the first time that international health investments could be justified on the basis of having measureable outcomes and effects.
Volume 1 of the first edition of Disease Control Priorities in Developing Countries ( DCP1 ) also offered a comprehensive list of public health policies, with recommendations for developing and financing state capacity in data collection and data analysis ( Mosley, Bobadilla, and Jamison 1993 ). The authors shared aspirations for better policy environments that would be conducive to structural approaches to public health. Volume 2 of the second edition of Disease Control Priorities in Developing Countries (DCP2) explicitly recognized the need for community-driven global health efforts to strengthen health systems and infrastructure and suggested the need to strengthen platforms that would allow communities to hold health systems accountable for improved quality and access to services ( Mills, Rasheed, and Tollman 2006 ). DCP2 also emphasized that a lack of intersectoral action through cross-sector partnerships and the failure of health systems to address community-level barriers to accessing the health system were key constraints for health system strengthening ( Mills, Rasheed, and Tollman 2006 ). However, DCP1, DCP2 , and the World Development Report 1993 did not offer specific recommendations about how to create conducive policy environments that could enable and sustain public health interventions, cross-sectoral partnerships, and community engagement with local health departments ( Macinko, Starfield, and Erinosho 2009 ; Mosley, Bobadilla, and Jamison 1993 ; Rohde and others 2008 ).
The lack of a roadmap for creating community health platforms and cross-sectoral action made room for vertical programming to dominate the policy landscape ( Lawn and others 2008 ; Macinko, Starfield, and Erinosho 2009 ; Rohde and others 2008 ). These vertical programs saved lives, but they left populations vulnerable by failing to create resilient systems in situ that would marshal local political will and local resources to address the root causes of poor population health.
Actions that improve public health are often met with resistance about who will pay for them, because results are often less tangible and urgent than medical interventions. Further, public health actions often threaten the livelihoods of industries and occupations whose harmful aspects are regulated. Resistance is to be expected. Examples of public health actions range from the need to pay for sewers and waterworks to the need to enact and enforce restrictions on tobacco, food labeling, and road safety. Solving these problems is fundamental to public health. Solutions are often political, and vertical approaches are only partial responses.
The inability to sustain a local consensus and to mobilize community buy-in regarding the health risks leads to difficulty in imposing the measures needed to control health threats. Poorly performing public health departments are part of the reason that HIV/AIDS (human immunodeficiency virus/acquired immune deficiency syndrome) and the Ebola virus arose and overwhelmed many health systems.
Essential Public Health Functions
To improve public health functioning, between 1989 and 1994, groups at the Centers for Disease Control and Prevention and the U.S. Public Health Service developed a list of 10 essential public health functions to benchmark the quality of practice in public health agencies ( Dyal 1995 ). The consensus was that country health ministries and regional offices needed to define national-level lists of functions and items deemed essential and that the lists should be country specific ( Bettcher, Sapirie, and Goon 1998 ). Countries and regions have adapted their own priority lists of essential public health functions on the basis of local stakeholder input ( Bishai and others 2016 ). For example, the Pan American Health Organization’s (PAHO) list of Essential Public Health Functions (EPHFs) is as follows ( PAHO 2001 ):
- Monitor health status to identify community health problems.
- Diagnose and investigate health problems and health hazards in the community.
- Inform, educate, and empower people about health issues.
- Mobilize community partnerships to identify and solve health problems.
- Develop policies and plans that support individual and community health efforts.
- Enforce laws and regulations that protect health and ensure safety.
- Link people to needed personal health services and assure the provision of health care when otherwise unavailable.
- Assure a competent public and personal health care workforce.
- Evaluate effectiveness, accessibility, and quality of personal and population-based health services.
- Research for new insights and innovative solutions to health problems.
- Engage in disaster preparedness to reduce the impact of emergencies and disasters on health.
PAHO’s 11 items fall into the same basic cycle of monitor, review, and act shown in figure 14.1 . EPHFs 1 and 2 are for monitoring; EPHFs 3–5 are for reviewing, typically through participatory multistakeholder community engagement; and EPHFs 6–11 are for acting. The best community health platforms successfully make their populations healthy by understanding what constitutes health threats and by sharing this information with community members from multiple sectors. Community health platforms mobilize parts of a coherent solution using the strengths and resources present in the community.
Health Care and Health Facilities
The care of the sick and the delivery of health commodities are integral parts of public health practice and are parts of the work plan of community health platforms. Community health workers can play multiple roles in generating health data ( PAHO 2001 , EPHFs 1–2), informing and mobilizing communities ( PAHO 2001 , EPHFs 3–5), and helping to provide primary care services ( PAHO 2001 , EPHFs 7–9). Many of the interventions discussed in Volume 4 of the third edition of Disease Control Priorities ( DCP3) rely on facilities and community health workers ( Patel and others 2015 ). When community health platforms fulfill their mandate to provide essential public health functions like those mentioned earlier, interventions based in facilities and involving community health workers become integrated and sustained by local support and action.
- Measuring Success in Community Health Platforms
The literature shows that community health platforms that enable participation and engagement lead to improved health outcomes ( Edmunds and Albritton 2015 ; George and others 2015 ; Kenny and others 2013 ; McCoy, Hall, and Ridge 2012 ; O’Mara-Eves and others 2015 ; Rifkin 1996 , 2014 ). Measuring health outcomes associated with community participation can be difficult, but community participation in public health generally leads to improvements in health knowledge, service quality, and health-related outcomes ( Kenny and others 2013 ; Russell and others 2008 ).
The degree to which a community health platform is high functioning lies along a continuum. At one end is development that extends from mere delivery of services. At the other end is facilitation of an active community through an engagement platform whereby communities are informed and enabled to take shared responsibility for addressing their changing health risks and concerns ( Beracochea 2015 ; Cyril and others 2015 ; Dooris and Heritage 2013 ; Draper, Hewitt, and Rifkin 2010 ; George and others 2015 ; McCoy, Hall, and Ridge 2012 ; Raeburn and others 2006 ; Rosato and others 2008 ; Russell and others 2008 ).
The breadth of the literature on community health platforms demonstrates the range of ways that the concept can be applied. Types of platforms described in published and gray literature generally fall into the following categories:
- Health committees
- Community health worker interventions
- Community-based participatory research and health scorecards
- NGOs or academic community partnerships for specific community interventions ( Beracochea 2015 ; Draper, Hewitt, and Rifkin 2010 ; George and others 2015 ; Kenny and others 2013 ; Marmot and others 2008 ; Meier, Pardue, and London 2012 ; Rifkin 1996 ; Tiwari, Lommerse, and Smith 2014 ; UK Aid and DFID/HDRC 2011 ).
The literature also covers concepts of community engagement, participation, and mobilization as they relate to multiple types of community platforms ( Cyril and others 2015 ; Draper, Hewitt, and Rifkin 2010 ; Frumence and others 2014 ; Meier, Pardue, and London 2012 ; Rifkin 1996 , 2014 ; Rosato and others 2008 ; Russell and others 2008 ; UK Aid and DFID/HDRC 2011 ).
The likelihood that community engagement will result in improved health outcomes depends on many factors. Cyril and others ( 2015 ) identified the following components of success: engaging in real power sharing, building collaborative partnerships, providing bidirectional learning, incorporating the voice and agency of beneficiary communities in research protocol, and using multicultural health care workers for intervention delivery. Draper, Hewitt, and Rifkin ( 2010 ) suggested a continuum of process measures for use in evaluating community participation in a health system context ( table 14.1 ). Figure 14.2 summarizes a process of increasing empowerment in the development of community participation.
Example of Process Indicators for Participation.
Figure 14.2
From Passive to Active Community Participation.
- Interventions, Policies, and Effectiveness
Community Health Platform Case Studies
We describe the continuum of developmental stages that low- and middle-income countries move through in their health systems as they improve in their ability to empower communities to take on health challenges. Using themes that emerged from the literature, we identified broad domains of function in the development of community health platforms:
- Level of community engagement: To what extent was the community empowered to engage with the health care system?
- Health-system context and role of the government: Was the health system decentralized? Did local health departments have power to innovate and to work with communities? Was the government a support or a hindrance to community health platforms?
- Breadth of intersectoral partnerships: Was the community able to work with NGOs, community-based organizations, local governments, and other sectors in addition to the health sector? Did this ability predict the comprehensiveness of improvements? Was the community able to influence action across sectors?
- Sustainability: Was the community health platform’s ability to be both scalable and sustainable a key factor in its success and longevity? This category includes the financing strategies and the ability to create lasting change while reducing inefficiencies across the system. Is the community health platform legally recognized?
- Leadership and platform structure that promotes integration across all partners: Who initiated the community’s involvement with the health system? Did the platform create opportunities for shared vision, shared leadership and decision making, and shared financing across sectors?
Identifying Case Studies Demonstrating Community Health Platform Development
Among the countries with recent rapid reductions in mortality under age 5 years, Indonesia and Peru offer informative examples of community health platforms that have been sustainable and high achieving ( Altobelli 2008 ; Blas, Sommerfeld, and Kurup 2011 ; Kowitt and others 2015 ; Rasanathan and others 2012 ; Siswanto 2009 ; Tanvatanakul and others 2007 ; Tiwari, Lommerse, and Smith 2014 ; Westphal and others 2011 ). Table 14.2 shows a staged typology of community health platforms as countries move from low-functioning platforms with little accountability (level 1) to high-functioning platforms that promote intersectoral action (level 4).
Continuum of Functioning, from High to Low, across Functional Domains of Community Health Platforms.
Factors That Support Successful Community Health Platforms
Supportive factors that emerged from the case study review and that contribute to sustainability include government participation, advocacy, cross-sectoral partnerships, and community-owned vetting mechanisms.
Successful community health platforms were developed to fit in the political and cultural context of the local area they served, but they were strengthened by advocacy from NGOs or universities, which also provided technical support for emerging platforms. Support from the government was essential for longer-term sustainability, but strong internal and external advocates from nongovernment sectors helped communities engage with governments and health systems, which led to more formal structures.
Successful community health platforms relied on coordination across sectors to meet health goals, which resulted in reduced duplication of efforts and more efficient use of government funding. Successful platforms also provided a mechanism to vet new projects or accept funding from external donors or NGOs based on the priorities of communities. The ability of platforms to set their own health agenda further reduced duplication of efforts and empowered communities to establish control over their own health priorities.
Case Study: Gerbangmas Movement as a Community Health Platform, Lumajang District, Indonesia, Level 4
Among lower-middle-income countries, Indonesia has achieved the highest reduction in the rate of mortality under age 5 years in recent decades ( Rohde and others 2008 ; Siswanto 2009 ). One component in this success was a network of community health posts ( posyandus ) that involved communities in primary health care. In the 1980s and 1990s, these posts offered limited services, and quality and performance varied ( Blas, Sommerfeld, and Kurup 2011 ; Siswanto 2009 ). After Indonesia decentralized in 2001, district governments were empowered to run district-level health systems.
The experience of Lumajang district in East Java is notable as an example of a health-in-all-policies approach driven by public health and community participation, as well as for its ability to adapt and sustain itself despite political and environmental changes over time. The district health office originally created enriched health posts with three key functions: community education, community empowerment, and community services. The enriched health post hosted activities such as clinical maternal and child health, family planning, nutrition, immunization, diarrhea control, under-five growth stimulation, and early childhood education. Other sectors outside of health care, such as education, became involved ( Blas, Sommerfeld, and Kurup 2011 ; Siswanto 2009 ).
Starting in 2005, with encouragement from the governor, the district health office led subsequent efforts to create the Gerbangmas movement, a platform for communities, the public health sector, and other government sectors to work collaboratively to achieve 21 indicators of concern ( Blas, Sommerfeld, and Kurup 2011 ; Siswanto 2009 ). The more specific objectives were to achieve 14 indicators for human development, 1 indicator for the economy, and 6 indicators for the household environment that together represented the priorities of the government and the community, as well as the religious, education, industry and trade, health, family planning, agriculture, and public works sectors ( Blas, Sommerfeld, and Kurup 2011 ; Siswanto 2009 ). The sectors worked together with support from the district governor, leadership from a local NGO to address family welfare issues, and a funding stream that allowed all sectors to contribute to progress on the chosen indicators.
This movement for community development resulted in improvements in all indicators ( Marmot and others 2008 ). The multisectoral Gerbangmas movement was sustainable and successful, even in the context of a changing economic and government landscape. Although the Gerbangmas movement has experienced numerous changes over time, its central tenants of building a community health platform to lead cross-sector partnerships has remained relevant in Indonesia for the past 15 years. Lessons learned from this case study illustrate important roles for local government, cross-sector partnerships, and leadership.
Heath Systems and Role of Local Government
The development of the Gerbangmas movement stemmed from decentralization of the Indonesian health system, allowing peripheral innovation. The local government offered support and leadership for the initiative, as well as a mechanism for funding. Once the movement was planned and funded, the district health office created a single vehicle through which the communities, the health system, and other sectors could collaborate around common goals without competing for volunteers or resources. The district health office did not dominate the partnership; it included itself as a stakeholder, with leadership provided by a neutral entity.
Partnerships across Sectors
The partnership structure provided clear roles for each sector to develop programs to help achieve the shared indicators. The district PKK (a family welfare semi-governmental NGO consisting of spouses of government officials and community members) helped coordinate and support the partnership across organizations. The funding structure created a common pool of funds from which communities were able to draw for investment in interventions in multiple sectors. Some sectors also contributed funds to achieve action plans. Essentially, the partnership structure of this movement allowed sectors to compete for community dollars in their respective programs, while preventing duplication of efforts and competition across sectors ( Blas, Sommerfeld, and Kurup 2011 ; Siswanto 2009 ).
The district governor mandated that all community empowerment programs use the Gerbangmas movement as an entry point, thereby reducing competition and keeping outside interests (such as those from NGOs) from affecting the success of the partnerships across sectors ( Blas, Sommerfeld, and Kurup 2011 ; Siswanto 2009 ). With the community at the center of the partnership structure, a hierarchy that placed all sectors on equal footing, and a common set of indicators to work toward, the Gerbangmas movement helped sectors work together effectively.
Leadership and Integration
The district health office was the initial champion for the Gerbangmas movement, which eventually assumed the role of the integrated health platform. During the initial scale-up from health posts to enriched health posts, the district health office garnered support from local government and encouraged involvement of other sectors (such as education) while demonstrating the importance of involving other sectors in achieving common health goals. As the health posts evolved into enriched posts, or Gerbangmas health posts ( figure 14.3 ), the district health office took a step back to participate as a member of a team engaging other sectors; an NGO took on a more significant role as an integrator and coordinator of the movement. Part of the significance of an NGO’s heading an integrated platform is that such an organization can be sector neutral, allowing each sector equal weight in achieving agreed-upon goals. Notably, the community itself held power over the management of the programs and the priorities of the Gerbangmas movement.
Figure 14.3
Evolution of Conventional Health Posts to Gerbangmas Health Posts in Lumajang District.
Role of Communities
Community volunteers conducted needs surveys in their respective villages, and maps of community needs were developed on the basis of the data gathered. The community problems in each village were discussed in open forums where members created action plans. Final proposals were drawn up that became the community action plans. Community members had input on the allocation of funds. Financing came from government funding allocation and from financial contributions from the community. Community volunteers also participated in the monitoring and evaluation of activities that had been carried out each year.
District Gerbangmas teams trained subdistrict teams. A training-of-trainers approach helped educate many community volunteers and village staff members on the way to assess community health, facilitate community dialogue about the findings to lead to community involvement in proposing and implementing action plans, and evaluate the results of those plans ( Blas, Sommerfeld, and Kurup 2011 ; Siswanto 2009 ).
Sustainability
Sustainability was supported by an overall structure that included resources, funding, and training from partnering organizations and did not rely on grant funds or external donor dollars ( Blas, Sommerfeld, and Kurup 2011 ; Siswanto 2009 ). In addition, the partnership structure did not depend on the success of any single organization or leader. The largest hurdle to sustainability was the turnover of government officials. Sustainability relied on the new district governor’s approval of the Gerbangmas movement in the subsequent five-year plan. In response, the district government created an official book on the Gerbangmas movement, including write-ups of the success of the movement in the governor’s accountability report. The report covered a summary of the governor’s achievements during his term and included the movement as policy in the district regulation, which was ratified by the district legislative body ( Blas, Sommerfeld, and Kurup 2011 ; Siswanto 2009 ).
Case Study: Local Health Administration Committees, Peru, Level 3
The Peruvian government has legalized, regulated, and institutionalized community participation as a means of ensuring its role in primary health care ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ). Local health administration communities (comunidades locales de administración en salud, or CLAS) are private, nonprofit civil associations that have agreements with the government to receive and administer public funding for the purpose of implementing primary health care services responsive to community needs.
Evolution of Local Health Administration Committees
The path to development of the CLAS movement was a complicated one. The CLAS movement emerged in 1994, following the collapse of the health sector in Peru. Terrorism and hyperinflation were major national challenges, and decentralization was beginning ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ). Rural areas had a strong mistrust of the government; initial efforts to expand primary health care in these areas resulted in further mistrust, because community members often felt mistreated by physicians ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ). When Jaime Freundt became the minister of health in the mid-1990s, he sought reform through a process that involved convening technical experts and community members. As a result, a new form of CLAS was proposed ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ).
In the new CLAS, community members were part of a civil association under the authority of the Peruvian Civil Code. Community members had a formal relationship with the government by electing community representatives to a general assembly that worked with the regional health directorates ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ).
The elected assembly provided a way to demand accountability from health personnel ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ). The CLAS became a platform through which community representatives and volunteers could perform public health roles of community assessment, identifying health priorities across local areas, guiding interventions, and choosing where resources should be allocated. The CLAS structure also allowed communities to control the quality of care and distribution of services. Unlike a community advisory board in which participation is often based on board members’ advising those with the power to make decisions and allocate funding, each CLAS had the power and resources to act as the local health department for its respective community.
The CLAS’s financing came from direct government transfers from general revenue, reimbursements from the government health insurance program for the poor, and in-kind stocks of medicines and supplies from the regional health directorates. Control over allocation of these funds resided in the hands of the CLAS ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ). The CLAS assemblies conducted community assessments for health needs and helped identify unmet health needs to determine how best to tailor primary health care services to local contexts ( Iwami and Petchey 2002 ).
The CLAS movement began as a pilot with 250 health facilities incorporated into the program. Early evaluations showed improved equity, quality, and coverage of health services in CLAS facilities, compared to non-CLAS facilities ( Beracochea 2015 ). Advocates helped demonstrate the positive effects of the model, and in 2007, the Peruvian Congress approved a statute for citizen participation in primary health care at local levels. The passage of this law ensured the sustainability of the CLAS movement and confirmed Peru’s commitment to empowering communities to have some control over their own health care ( Altobelli 2008 ).
CLAS Achievements
The CLAS movement increased the availability of physicians in rural areas; improved access to care for the poor; improved usage rates, especially for children; improved quality in health facilities; and improved connections among people in Peruvian communities ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ). These achievements were the result of the communities’ ability to allocate budgets to attract higher numbers of physicians to areas where they were needed and to provide full or partial fee exemptions based on financial need. In addition, the number of women members of the CLAS general assembly grew substantially ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ).
Heath Systems and Role of Government
One interesting lesson learned from the CLAS movement is that public mistrust of the government can be counteracted through structures for communities to take ownership and oversight of public programs ( Altobelli 2008 ; Beracochea 2015 ; Blas, Sommerfeld, and Kurup 2011 ; Iwami and Petchey 2002 ). The CLAS movement was a key driver in creating transparency, participation, and social control over the health system that built community trust and improved relations between communities and the government ( Altobelli 2008 ). The Ministry of Health, with internal and external champions, was instrumental in helping the CLAS expansion to continue and become law ( Altobelli 2008 ).
In addition to primary health care needs, CLAS began to focus on the development needs of communities through community work plans that used discretionary funds and partnerships with local municipalities to allocate dollars to community-identified development projects ( Beracochea 2015 ). CLAS appears to be well on its way to transitioning from level 3 to level 4 in the typology of table 14.2 ; CLAS is already a community platform for addressing health needs and is broadening its intersectoral reach to partner with additional sectors. The CLAS movement has been spreading through the SEED-SCALE model of sustainability ( Taylor and Taylor 2002 ). Successful models in each region served as training centers and hubs for lateral diffusion of innovations.
Case Study: Community Scorecards in Nine Districts, Uganda, Level 2
Examples of contractor- and donor-driven platforms (level 2 in table 14.2 ) are fairly common in practice, and extensive literature documents this approach. We present a district scorecard program conducted in Uganda in 2004 to promote community oversight of health services at the primary care level.
The goal of the intervention was to strengthen provider accountability through a process that used community organizations as facilitators of village-level meetings to inform communities about the status of health service delivery in their area relative to the standards held in surrounding areas ( Abdul Latif Jameel Poverty Action Lab 2015 ; Björkman and Svensson 2009 , 2010 ). Facilitators encouraged community members to identify areas for improvement in health service provision and to develop action plans that could lead to improvements ( Abdul Latif Jameel Poverty Action Lab 2015 ; Björkman and Svensson 2009 , 2010 ). The intervention sought to create a community-led process of monitoring to ensure that health care workers were performing their assigned tasks ( Abdul Latif Jameel Poverty Action Lab 2015 ; Björkman and Svensson 2009 , 2010 ). The results of the study indicated that, compared to control communities, community-based monitoring improved the quality and quantity of primary care delivered, reduced the number of deaths among children under age 5 years, improved outpatient service use, and improved quality measures such as wait time in primary care ( Abdul Latif Jameel Poverty Action Lab 2015 ; Björkman and Svensson 2009 , 2010 ).
Analysis of Uganda District Scorecards
The example of the district scorecard study in Uganda represented a limited intervention that was driven by outside agencies for the purposes of involving the community in health service improvement. Despite positive outcomes, ongoing success was reliant on ongoing collection of scores from scorecards by third-party entities ( Abdul Latif Jameel Poverty Action Lab 2015 ; Björkman and Svensson 2009 , 2010 ).
Health Systems and Role of Government
In Uganda’s decentralized system, local health unit management committees monitored the day-to-day health service activities of the public dispensaries. The government was not the driver of the interventions and did not have a large role in the improvements to community health, other than through its role in running the committees ( Abdul Latif Jameel Poverty Action Lab 2015 ; BjÖrkman and Svensson 2009 , 2010 ).
Partnerships across sectors were limited in this example. NGOs and community organizations participated in community meetings, but there were few other partnerships across sectors or across government agencies ( Abdul Latif Jameel Poverty Action Lab 2015 ; BjÖrkman and Svensson 2009 , 2010 ).
The community health platform was originally developed by researchers at the University of Stockholm and the World Bank, and the researchers generated the report cards that served as the basis for the program. Local NGOs facilitated program meetings and served as community leaders for the intervention. There was no means for integration across sectors ( BjÖrkman and Svensson 2009 , 2010 ).
The role of communities was to attend meetings where health care provider performance and quality were examined, discuss health care delivery problems that could be improved, and develop action plans for needed changes ( Abdul Latif Jameel Poverty Action Lab 2015 ; BjÖrkman and Svensson 2009 , 2010 ). Although the communities’ ability to hold health care providers accountable was limited, they were able to participate in the improvement process and were given a voice for addressing their concerns.
Because the scorecards—determined to be a crucial piece of this intervention—were not developed by communities or the government, this intervention was scalable and sustainable only as long as researchers continued to provide data, or until a cheaper and more direct way of creating the scorecards was established ( Abdul Latif Jameel Poverty Action Lab 2015 ; BjÖrkman and Svensson 2009 , 2010 ). Without further government and community buy-in to allocate resources to these activities, the district scorecard intervention faced many challenges in scalability and sustainability.
Case Study: Weak Government Platforms for Community Empowerment, Haiti, Level 1
Challenges to development of community health platforms.
Haiti faces many challenges in developing local government engagement of community health platforms. It provides a case study where important lessons can be learned about the role of NGOs and donor agencies in helping promote or hinder development of community health platforms.
Haiti has long suffered from natural disasters, disease outbreaks, poverty and social divisions, political instability, and other social and political inequalities that have led to instability ( Fatton 2006 ; James 2010 ). Numerous NGOs arrived with varying agendas; before the 2010 earthquake, an estimated 8,000–9,000 were working in the country ( Batley and McLoughlin 2010 ; Zanotti 2010 ). Nearly all of the interventions in the education, health, and development sectors were led by NGOs, which provided 70 percent of health care services and 85 percent of education support ( Vaux and Visman 2005 ; Zanotti 2010 ). The flow of funds through NGOs rather than the government weakened the elected government, created instability, and further undermined the accountability and sustainability of the state ( Zanotti 2010 ). After the earthquake, the negligible state capacity that did exist was destroyed, and the vulnerability of the state and subsequent reliance on NGOs, faith-based organizations, and formal providers for care was further exposed ( Hill and others 2014 ).
Given the diversity of NGOs working throughout Haiti, health care delivery was largely inconsistent in quality, quantity, and coordination across the country ( Hill and others 2014 ). The role of the Ministry of Public Health and Population was marginal, and external resources were often allocated according to the priorities of NGOs or donors ( Hill and others 2014 ; Zanotti 2010 ). Ultimately, many of these NGOs did not have local origins, did not understand local context, and did not focus on creating sustainable, responsive platforms where communities could be empowered to address their own health needs ( Zanotti 2010 ).
Analysis of Haiti’s Challenges with Development of Successful Community Health Platforms
Unreliable health services and access to those services promoted health inequities and created a reliance on external entities that created difficulties for communities to voice their own needs ( Hill and others 2014 ). Lack of service integration and coordination led to further fragmentation and duplication of efforts, and Haitians often relied on traditional medicine that was widely available ( Hill and others 2014 ).
Despite the challenges, Haiti’s structure also provides the opportunity for NGOs to develop community health platforms that are responsive and engage local communities. Several NGOs engaged the needs of communities and helped build community capacity in the areas of development, health, and education. Successful NGOs had several factors in common:
- They had local origins in Haiti.
- They had a diverse international network of donors and were not accountable to a single funder or government agency.
- They focused on addressing local needs and the needs of the poorest individuals.
- They shared a vision that tied economy, politics, and human rights ( Zanotti 2010 ).
The weakness of the state and the reliance on NGOs created an environment in which external entities often influenced resource allocation and priority setting. The lack of a focus on Haitian governance and the subsequent lack of health system structure and community input created difficulties for the community to engage meaningfully in the public health process and hampered the creation of sustainable and responsive health care systems. The ability of communities to hold the government accountable for health service access and quality was nearly absent.
Partnership across Sectors
Coordination among health and other sectors has been slow owing to lack of government leadership. However, successful NGOs acknowledged the importance of other sectors in improving health outcomes and worked on issues of sanitation, economic development, and education, in addition to health ( Zanotti 2010 ). NGOs served as providers of services, as well as social advocates pursuing reforms to address poverty and social injustice ( Zanotti 2010 ).
One of the key difficulties that Haiti faces in creating community health platforms is that the country’s leaders are highly influenced by external funding sources. The ability of an NGO to make decisions on the basis of community needs would be much greater if it did not depend on external agencies with specific agendas. Addressing community needs requires flexibility in setting agendas that not all NGOs possess.
Successful NGOs were those that were able to engage communities, to set priorities for community input, and to include communities in identifying problems and developing and delivering solutions. These included, for example, community health workers and health care providers ( Zanotti 2010 ).
One of Haiti’s most significant challenges is creating sustainable solutions in the presence of NGOs that provide the majority of the health-related services in the country. NGOs that can create a platform through which communities can carry out basic public health functions and partner with other sectors to address the social determinants of health represent a way forward. NGOs that can empower communities and provide them with the necessary skills are setting the stage for the sustainability and effectiveness of a future health system.
Strengthening Community Health Platforms
Benefits of strengthening community health platforms.
The reviewed literature and the focal case studies highlight the benefits of and provide a framework for strengthening community health platforms. The benefits arise whether the priority is (a) implementing or scaling up delivery of commodities, services, and programs or (b) building the capacity of communities to identify and address long-standing and emerging public health problems.
The benefits of stronger platforms arise because the more health platforms develop along the continuum in table 14.2 , the better they can carry out the essential public health functions and the cycle of monitoring, reviewing, and acting to achieve solutions. Strength means the capability of health data collection through local surveillance and outbreak investigation. Strength means that public health personnel can find ways to share the data with their communities and to engage communities in developing local solutions that mobilize external resources as well as untapped resources in communities. Strength also means that local public health personnel can facilitate implementation of existing programs and develop modifications in response to emerging issues.
Because only some communities have community health platforms that can effectively carry out essential public health functions, outsiders often develop action plans that can succeed in the absence of these platforms. The unintended consequence of neglecting core strength in community health platforms is the continued building of partial substitutes for what community health platforms ought to be doing. The partial substitutes crowd out the necessary business of building indigenous strength.
Factors That Strengthen Community Health Platforms
Our review found the following identifiable factors that strengthen community health platforms:
- Access to data about health problems and health threats
- The means and will to share data and control with community members
- Achievement of a balance between delivering clinical services and preventing disease in whole populations
- Advocacy to maintain community engagement against pressure to consolidate control.
In some cases, these factors were present fortuitously. However, evidence suggests that the success factors can be present as the result of intention and effort. A commitment to engage community stakeholders cannot be maintained for long simply because of circumstances. However, a widespread political movement toward openness and grassroots engagement can make maintaining a community orientation easier.
Priorities for Investment in Strengthening Community Health Platforms
Effective strategies must come from taking stock of the current position of a community on the development continuum shown in table 14.2 . Tools to measure a community’s performance of essential public health functions have been used extensively in the Americas ( Corso and others 2000 ; PAHO 2001 ; Upshaw 2000 ). Measurement of current strength in public health care services through a performance and quality improvement tool that targets the essential public health functions can help identify areas of emphasis within a district if the measures are provided to the public health staff to help create a performance improvement plan ( Bishai and others 2016 ).
A strategy to develop community health platforms requires a modest investment in a central unit devoted to the quality of public health practice. Quality units are a growing feature in public health departments ( Gunzenhauser and others 2010 ). The best practice for a quality unit is to use measurement of practice as a conversation starter rather than a disciplinary bludgeon. A public health practice quality unit for a central or regional health ministry requires a small investment. The budget should allow a team of district supervisors to make quarterly supervisory visits to specified districts and remain in regular electronic communication. Checklists and protocols for supervisory visits have been developed and are available from several sources. (The library of these resources can be found at http://www.ianphi.org/documents/pdfs/evaluationtool and https://sites.google.com/site/ephfjhu/ .)
Conclusions
Communities vary in their level of sophistication in conducting a cycle of monitoring, reviewing, and acting on the basis of local data and local multisector community-engaged partnerships. Helping communities do this well is a concept that goes back to the foundations of the field of public health. Because good health can exist at low cost with vertical programs that rescue people regardless of their community’s functional level, making the case for investing in community resilience can be challenging. The situation does not need to be an “either-or” option; the way forward ought to be a “both-and” option. Rescuing and building resilience are complementary. Especially where budgets are finite, strong community health platforms can marshal new resources to the service of public health.
Valuing Community Health Platforms
Given the common misinterpretation that cost-effectiveness (as dollars per disability-adjusted life year averted) is the key to understanding an intervention’s value, one might be lulled into thinking that any investment that cannot show its disability-adjusted life years averted is wasteful—perhaps even unethical, given that people are dying of preventable causes every day.
Without initiatives to help community health platforms flourish around the world, the health gains promised by interventions will cost more and deliver less. Communities will miss opportunities to activate partners and resources that can shift health determinants in schools and workplaces and the commerce, transport, and culture sectors. Political will to make changes in public health law enforcement and regulation and to hold governments accountable is a precious resource that community health platforms can nurture and maintain. With the availability of local data, local forums for sharing data, and local multisectoral stakeholder engagement, the solutions will work better and deliver more. This human infrastructure has been neglected for far too long.
A Way Forward for Health Systems
With the Sustainable Development Goals and calls for health system resilience, we are entering a new era in which this neglect of community engagement and capacity is ending ( Bellagio District Public Health Workshop Participants 2016 ). Community health platforms require a respectful trust that people being presented with data about their health problems and evidence about what works to solve the problems will choose wisely. Community health platforms require a recognition that health is too big for the health care sector alone; we need a decision-making forum that includes the education sector, commercial interests, transportation, law enforcement, and media. These partnerships are essential if we are to address upstream social determinants.
Our model of community health platforms is explicitly drawn at the local level. The national and global policy makers have important roles in setting up expectations and tools to support local communities. Fundamentally, human bodies are small objects; most of the time, what makes a body sick (or worse) is a microbe from across the street or a cigarette from the local store or a speeding car with a drunk driver behind the wheel. Protecting a body requires a protector that is close to that body. The emerging burden of noncommunicable diseases caused by health behavior choices, lifestyles, mental health trauma, and injuries underscores the need for local approaches. High-income country data show that noncommunicable disease burdens differ intensely at the scale of a census tract. Modern cities are seeing life-expectancy differentials of 20 years across neighborhoods.
The other advantage of local communities is their sheer number. For a failed state, efforts to work at the national level can remain frustrating for decades. At the local level, one can find failed communities, but one can also find successful communities. One can even find successful communities inside failed states and accomplish at subnational levels what cannot be done when a central government is not prioritizing health.
The model of community health platforms asks local government health officials to play a prominent role as conveners and integrators. Government presence does not suggest that government workers perform all of the roles in the public health cycle. The decisions about who does what emerge from the community, on the basis of its own stock of possible actors and doers. Community health platforms can mobilize resources through volunteers and voluntary activities independent of the budgets of governments and donors.
A Chinese proverb says that the best time to plant a tree was 20 years ago, and the second-best time is today. High-functioning community health platforms are the trees that we wish our ancestors had planted in every community many years ago. Future generations cannot afford to have us spend the next 20 years attending to local epidemics and global pandemics that could have been snuffed out and quickly controlled if all local communities had been performing all of the essential public health functions and engaging their communities in building a culture of health.
- Acknowledgments
The authors gratefully acknowledge helpful comments from Henry Mosley, MD, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States.
World Bank Income Classifications as of July 2014 are as follows, based on estimates of gross national income (GNI) per capita for 2013:
- Low-income countries (LICs) = US$1,045 or less
- lower-middle-income = US$1,046 to US$4,125
- upper-middle-income (UMICs) = US$4,126 to US$12,745
- High-income countries (HICs) = US$12,746 or more.
- Abdul Latif Jameel Poverty Action Lab. 2015. “The Power of Information in Community Monitoring.” J-PAL Policy Briefcase, July. https://www .povertyactionlab .org/sites/default /files/publications /Community%20Monitoring_2.pdf .
- Altobelli L., 2008. “Case Study of CLAS in Peru: Opportunity and Empowerment for Health Equity.” Prepared for Case Studies of Programmes Addressing Social Determinants of Health and Equity, Priority Public Health Conditions–Knowledge Network, World Health Organization (WHO) Commission on Social Determinants of Health, with support from the Alliance for Health Policy and Systems Research, WHO, Geneva.
- Batley R, McLoughlin C. 2010. “Engagement with Non-State Service Providers in Fragile States: Reconciling State Building and Service Delivery.” Development Policy Review 28 (10): 131–54.
- Bellagio District Public Health Workshop Participants. 2016. “Public Health Performance Strengthening at Districts: Rationale and Blueprint for Action.” White paper prepared after the Bellagio Conference, New York City, November 21–25. www .who.int/alliance-hpsr /bellagiowhitepaper.pdf .
- Beracochea E., 2015. Improving Aid in Global Health. New York: Springer.
- Bettcher D W, Sapirie S, Goon E H. 1998. “Essential Public Health Functions: Results of the International Delphi Study.” World Health Statistics Quarterly 51 (1): 44–54. [ PubMed : 9675808 ]
- Bishai D, Sherry M K, Pereira C, Chicumbe S, Mbofana F., and others. 2016. “Development and Usefulness of a District Health Systems Tool for Performance Improvement in Essential Public Health Functions in Botswana and Mozambique.” Journal of Public Health Management and Practice 22 (6): 586–96. [ PMC free article : PMC5933056 ] [ PubMed : 27682727 ]
- BjÖrkman M, Svensson J. 2009. “Power to the People: Evidence from a Randomized Field Experiment on Community-Based Monitoring in Uganda.” Quarterly Journal of Economics 124 (2): 735–69.
- BjÖrkman M, Svensson J. 2010. “When Is Community-Based Monitoring Effective? Evidence from a Randomized Experiment in Primary Health in Uganda.” Journal of European Economic Association 8 (2–3):571–81.
- Blas E, Sommerfeld J, Kurup A S. 2011. Social Determinants Approaches to Public Health: From Concept to Practice. Geneva: World Health Organization.
- Corso L C, Wiesner P J, Halverson P K, Brown C K. 2000. “Using the Essential Services as a Foundation for Performance Measurement and Assessment of Local Public Health Systems.” Journal of Public Health Management and Practice 6 (5): 1–18. [ PubMed : 11067656 ]
- Cyril S, Smith B J, Possamai-Inesedy A, Renzaho A M. 2015. “Exploring the Role of Community Engagement in Improving the Health of Disadvantaged Populations: A Systematic Review.” Global Health Action 8: 29842. [ PMC free article : PMC4685976 ] [ PubMed : 26689460 ]
- Dooris M, Heritage Z. 2013. “Healthy Cities: Facilitating the Active Participation and Empowerment of Local People.” Journal of Urban Health 90 (Suppl 1):74–91. [ PMC free article : PMC3764265 ] [ PubMed : 22125115 ]
- Draper A K, Hewitt G, Rifkin S. 2010. “Chasing the Dragon: Developing Indicators for the Assessment of Community Participation in Health Programmes.” Social Science and Medicine 71 (6): 1102–09. [ PubMed : 20621405 ]
- Dyal W W. 1995. “Ten Organizational Practices of Public Health: A Historical Perspective.” American Journal of Preventive Medicine 11 (Suppl 6):6–8. [ PubMed : 8776135 ]
- Edmunds M, Albritton E. 2015. “Global Public Health Systems Innovations: A Scan of Promising Practices.” AcademyHealth, Washington, DC, and Robert Wood Johnson Foundation, Princeton, NJ.
- Fatton R., 2006. “Haiti: The Saturnalia of Emancipation and the Vicissitudes of Predatory Rule.” Third World Quarterly 27 (1): 115–33.
- Frumence G, Nyamhanga T, Mwangu M, Hurtig A K. 2014. “Participation in Health Planning in a Decentralised Health System: Experiences from Facility Governing Committees in the Kongwa District of Tanzania.” Global Public Health 9 (10): 1125–38. [ PubMed : 25248312 ]
- George A, Scott K, Garimella S, Mondal S, Ved R, Sheikh K. 2015. “Anchoring Contextual Analysis in Health Policy and Systems Research: A Narrative Review of Contextual Factors Influencing Health Committees in Low and Middle Income Countries.” Social Science and Medicine 133 159–67. [ PubMed : 25875322 ]
- Gunzenhauser J, Eggena Z, Fielding J, Smith K, Jacobson D, Bazini-Barakat N. 2010. “The Quality Improvement Experience in a High-Performing Local Health Department: Los Angeles County.” Journal of Public Health Management and Practice 16 (1): 39–48. [ PubMed : 20009643 ]
- Hill P S, Pavignani E, Michael M, Murru M, Beesley M. 2014. “The ‘Empty Void’ Is a Crowded Space: Health Service Provision at the Margins of Fragile and Conflict Affected States.” Conflict and Health 8 (20). [ PMC free article : PMC4210361 ] [ PubMed : 25349625 ]
- Iwami M, Petchey R. 2002. “A CLAS Act? Community-Based Organizations, Health Service Decentralization and Primary Care Development in Peru.” Journal of Public Health Medicine 26 (4): 246–51. [ PubMed : 12546199 ]
- James E C. 2010. “Ruptures, Rights, and Repair: The Political Economy of Trauma in Haiti.” Social Science and Medicine 70 (1): 106–13. [ PubMed : 19836120 ]
- Kenny A, Hyett N, Sawtell J, Dickson-Swift V, Farmer J, O’Meara P. 2013. “Community Participation in Rural Health: A Scoping Review.” BMC Health Services Research 13 64–72. [ PMC free article : PMC3583801 ] [ PubMed : 23414561 ]
- Kowitt S D, Emmerling D, Fisher E B, Tanasugarn C. 2015. “Community Health Workers as Agents of Health Promotion: Analyzing Thailand’s Village Health Volunteer Program.” Journal of Community Health 40 (4): 780–88. [ PubMed : 25744815 ]
- Lawn J E, Rohde J, Rifkin S, Were M, Paul V K, Chopra M. 2008. “Alma-Ata 30 Years On: Revolutionary, Relevant, and Time to Revitalise.” The Lancet 372 (9642): 917–27. [ PubMed : 18790315 ]
- Macinko J S, Starfield B, Erinosho T. 2009. “The Impact of Primary Healthcare on Population Health in Low- and Middle-Income Countries.” Journal of Ambulatory Care Management 32 (2): 150–71. [ PubMed : 19305227 ]
- Marmot M, Friel S, Bell R, Houweling T A, Taylor J S, the Commission on Social Determinants of Health. 2008. “Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health.” The Lancet 372 (9650): 1661–69. [ PubMed : 18994664 ]
- McCoy D C, Hall J. A, Ridge M. 2012. “A Systematic Review of the Literature for Evidence on Health Facility Committees in Low- and Middle-Income Countries.” Health Policy Plan 27 (6): 449–66. [ PubMed : 22155589 ]
- McKeown T, Record R G, Turner R D. 1975. “An Interpretation of the Decline of Mortality in England and Wales during the Twentieth Century.” Population Studies 29 391–422. [ PubMed : 11630508 ]
- Meier B M, Pardue C, London L. 2012. “Implementing Community Participation through Legislative Reform: A Study of the Policy Framework for Community Participation in Western Cape Province of South Africa.” BMC International Health and Human Rights 12 15–29. [ PMC free article : PMC3532148 ] [ PubMed : 22920557 ]
- Mills A, Rasheed F, Tollman S. 2006. “Strengthening Health Systems.” In Disease Control Priorities in Developing Countries, second edition, edited by Jamison D T, Bremen Measham J G, Alleyne A R, Claeson G, Evans M, Jha D B, Mills P, Musgrove A P, editors. . Washington, DC: World Bank Oxford University Press. [ PubMed : 21250309 ]
- Mosley W H, Bobadilla J L, Jamison D T. 1993. “The Health Transition: Implications for Health Policy in Developing Countries.” In Disease Control Priorities in Developing Countries, edited by Jamison D T, Mosley W H, Measham A R, Bobadilla J L, editors. . Washington, DC: World Bank; New York: Oxford University Press. [ PubMed : 21250309 ]
- O’Mara-Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, Thomas J. 2015. “The Effectiveness of Community Engagement in Public Health Interventions for Disadvantaged Groups: A Meta-Analysis.” BMC Public Health 15: 129. [ PMC free article : PMC4374501 ] [ PubMed : 25885588 ]
- Open Working Group of the General Assembly. 2014. “Open Working Group Proposal for Sustainable Development Goals.” A/68/970, United Nations, New York. http://undocs .org/A/68/970 .
- PAHO (Pan American Health Organization). 2001. Public Health in the Americas. Washington, DC: PAHO.
- Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora M E., eds. 2015. Disease Control Priorities (third edition): Volume 9, Mental, Neurological, and Substance Use Disorders. Washington, DC: World Bank. [ PubMed : 27227198 ]
- Perry H B. 2013. “Primary Health Care: A Redefinition, History, Trends, Controversies and Challenges.” White paper, Unpublished.
- Raeburn J, Akerman M, Chuengsatiansup K, Mejia F, Oladepo O. 2006. “Community Capacity Building and Health Promotion in a Globalized World.” Health Promotion International 21 (Suppl 1):84–90. [ PubMed : 17307961 ]
- Rasanathan K, Posayanonda T, Birmingham M, Tangcharoensathien V. 2012. “Innovation and Participation for Healthy Public Policy: The First National Health Assembly in Thailand.” Health Expectations 15 (1): 87–96. [ PMC free article : PMC5060602 ] [ PubMed : 21281413 ]
- Rifkin S B. 1996. “Paradigms Lost: Toward a New Understanding of Community Participation in Health Programmes.” Acta Tropica 61 (2): 79–92. [ PubMed : 8740887 ]
- Rifkin S B. 2014. “Examining the Links between Community Participation and Health Outcomes: A Review of the Literature.” Health Policy and Planning 29 (Suppl 2): ii98–106. [ PMC free article : PMC4202913 ] [ PubMed : 25274645 ]
- Rohde J, Cousens S, Chopra M, Tangcharoensathien V, Black R. and others. 2008. “30 Years after Alma-Ata: Has Primary Health Care Worked in Countries?” The Lancet 372 (9642): 950–61. [ PubMed : 18790318 ]
- Rosato M, Laverack G, Grabman L H, Tripathy P, Nair N.,, and others. 2008. “Community Participation: Lessons for Maternal, Newborn, and Child Health.” The Lancet 372 (9642): 962–71. [ PubMed : 18790319 ]
- Rosen G., 1958. A History of Public Health. Baltimore, MD: Johns Hopkins University Press.
- Russell N, Ingras S, Johri N, Kuoh H, Pavin M, Wickstrom J. 2008. “The Active Community Engagement Continuum.” Project Working Paper, July, ACQUIRE Project, New York, and United States Agency for International Development, Washington, DC. http://www .acquireproject .org/fileadmin/user_upload /ACQUIRE/Publications /ACE-Working-Paper-final.pdf .
- Siswanto E S. 2009. “Community Empowerment through Intersectoral Action: A Case Study of Gerbangmas in Lumajang District.” Jurnal Managemen Pelayanan Keshehatan 12 (1).
- Szreter S., 1988. “The Importance of Social Intervention in Britain’s Mortality Decline c. 1850–1914: A Reinterpretation of the Role of Public Health.” Social History of Medicine 1 (1): 1–38.
- Tanvatanakul V, Vicente C, Amado J, Saowakontha S. 2007. “Strengthening Health Development at the Community Level in Thailand: What Events Should Be Managed?” World Health and Population 9 (1): 65–73. [ PubMed : 18270500 ]
- Taylor D C, Taylor C E. 2002. A Just and Lasting Change: When Communities Own Their Own Futures. Baltimore, MD: Johns Hopkins University Press.
- Tiwari R, Lommerse M, Smith D. 2014. M2Models and Methodologies for Community Engagement. Singapore: Springer.
- UK Aid and DFID/HDRC (Department for International Development, United Kingdom/Human Development Resource Centre). 2011. “Helpdesk Report: Community Engagement in Health Service Delivery.” November 16, DFID, London.
- Upshaw V., 2000. “The National Public Health Performance Standards Program: Will It Strengthen Governance of Local Public Health?” Journal of Public Health Management and Practice 6 (5): 88–92. [ PubMed : 11067666 ]
- Vaux T, Visman E. 2005. Service Delivery in Countries Emerging from Conflict. Report, Centre for International Co-operation and Security, University of Bradford, Bradford, U.K.
- Westphal M F, Zioni F, Almeida M F, Nascimento P R. 2011. “Monitoring Millennium Development Goals in Brazilian Municipalities: Challenges to Be Met in Facing Up to Iniquities.” Cadernos de saude publica 27 (Suppl 2): S155–63. [ PubMed : 21789409 ]
- World Bank. World Development Report 1993: Investing in Health. Washington, DC: World Bank.
- Zanotti L., 2010. “Cacophonies of Aid, Failed State Building and NGOs in Haiti: Setting the Stage for Disaster, Envisioning the Future.” Third World Quarterly 31 (5): 755–71. [ PubMed : 20821882 ]
This work is available under the Creative Commons Attribution 3.0 IGO license (CC BY 3.0 IGO) http://creativecommons.org/licenses/by/3.0/igo . Under the Creative Commons Attribution license, you are free to copy, distribute, transmit, and adapt this work, including for commercial purposes, under the following conditions:
Attribution —Please cite the work as follows: Patel, V., D. Chisholm., T. Dua, R. Laxminarayan, and M. E. Medina-Mora, editors. 2015. Mental, Neurological, and Substance Use Disorders . Disease Control Priorities, third edition, volume 4. Washington, DC: World Bank. doi:10.1596/978-1-4648-0426-7. License: Creative Commons Attribution CC BY 3.0 IGO
Translations —If you create a translation of this work, please add the following disclaimer along with the attribution: This translation was not created by The World Bank and should not be considered an official World Bank translation. The World Bank shall not be liable for any content or error in this translation .
Third-party content —The World Bank does not necessarily own each component of the content contained within the work. The World Bank therefore does not warrant that the use of any third-party-owned individual component or part contained in the work will not infringe on the rights of those third parties. The risk of claims resulting from such infringement rests solely with you. If you wish to re-use a component of the work, it is your responsibility to determine whether permission is needed for that re-use and to obtain permission from the copyright owner. Examples of components can include, but are not limited to, tables, figures, or images.
All queries on rights and licenses should be addressed to the Publishing and Knowledge Division, The World Bank, 1818 H Street NW, Washington, DC 20433, USA; fax: 202-522-2625; e-mail: gro.knabdlrow@sthgirbup .
- Cite this Page Sherry M, Ghaffar A, Bishai D. Community Platforms for Public Health Interventions. In: Jamison DT, Gelband H, Horton S, et al., editors. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd edition. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017 Nov 27. Chapter 14. doi: 10.1596/978-1-4648-0527-1_ch14
- PDF version of this title (7.6M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Tuberculosis. [Major Infectious Diseases. 2017] Review Tuberculosis. Bloom BR, Atun R, Cohen T, Dye C, Fraser H, Gomez GB, Knight G, Murray M, Nardell E, Rubin E, et al. Major Infectious Diseases. 2017 Nov 3
- Review A review of major influences on current public health policy in developed countries in the second half of the 20th century. [J R Soc Promot Health. 2006] Review A review of major influences on current public health policy in developed countries in the second half of the 20th century. Irvine L, Elliott L, Wallace H, Crombie IK. J R Soc Promot Health. 2006 Mar; 126(2):73-8.
- The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. [JBI Database System Rev Implem...] The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. Newell S, Jordan Z. JBI Database System Rev Implement Rep. 2015 Jan; 13(1):76-87.
- Working with NGOs: PAHO's approach. [Glob AIDSnews. 1993] Working with NGOs: PAHO's approach. Hartigan P, Wiseman T. Glob AIDSnews. 1993; (3):17-8.
- Community participation: the keynote of integrated population programmes. [Asian Pac Popul Programme News...] Community participation: the keynote of integrated population programmes. . Asian Pac Popul Programme News. 1984; 13(1):10-1.
Recent Activity
- Community Platforms for Public Health Interventions - Disease Control Priorities... Community Platforms for Public Health Interventions - Disease Control Priorities: Improving Health and Reducing Poverty
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
COMMENTS
Communities are complicated, and figuring out the best way to improve the health of all residents in a particular place can be a daunting task. "Part of the issue is that we do not have a best practices model for place-based interventions," Dr. Dankwa-Mullan says. The editorial in the American Journal of Public Health was part of a new ...
Effective partnerships are essential for community-based solutions for advancing health equity by making it a shared vision and value, increasing the community's capacity to shape outcomes, and fostering multi-sector collaboration. Many different stakeholders can lead or participate in championing and implementing such solutions. These include organizations with a health mission, such as ...
Examining health outcomes in the community can help communities understand how health is connected to other desired objectives, and improving education or housing or employment can also help improve health. ... community groups, and individual community members come together to solve problems that affect the whole community—has the potential ...
Increasingly, 'community engagement' has become a buzzword among a variety of health and human rights organizations and government agencies. It's also the focus of new resources, and capacity building and training efforts. With the increasing use of this term, there are also some confusions on what 'community engagement' actually is.
Identifying strengths early helps community members understand what action they can take and where they fit in the work, he says. "You've got to know you're quick and can dribble before we ...
Yacine Fall (left) and Erin McGuinness describe their experience at a clinic in Uganda. December 14, 2022 - Over the summer, eight students from Harvard T.H. Chan School of Public Health partnered with organizations and community members from Boston to Nairobi, Kenya to learn about and help address locally identified public health problems.
As of 2021, there are more than 1,400 health centers in the United States, serving more than 14,500 service delivery locations; these include organizations designated as Federally Qualified Health Centers (FQHCs) and Health Center Program look-alikes.Health centers serve more than 28 million patients, 58% of whom are members of racial and ethnic minority groups and 68% of whom are at or below ...
Yet all communities can take action—with the help of supportive policies and collaboration across multiple sectors—to directly affect the determinants of health and improve health equity in the community. The work done to improve high school graduation rates, or access to transit, or more affordable housing options works to improve a ...
Simply put, lasting change cannot happen without active community involvement. Community members have important lived experience. They are context experts, and can provide critical insights into the dynamics at play in local communities. 1. Community members: Bring a breadth and depth of local knowledge. They know what solutions will work.
The KU Work Group for Community Health and Development 1 provided technical support and training. ... and capacity-building activities) to help those in the community come together, solve their own problems, and sustain progress after the technical advisers left. ... Phyllis Meadows remarked that community members often feel they can tell the ...
Examining health outcomes in the community can help communities understand how health is connected to other desired objectives, and improving education or housing or employment can also help improve health. ... community groups, and individual community members come together to solve problems that affect the whole community—has the potential ...
Introduction. Community based collaborative approaches leverage the talents, resources and perspectives of diverse organizations and individuals to address large-scale, complex social challenges (Fawcett et al., 2010; Thompson et al., 2016).Collaborations can take a variety of forms such as cooperation, collaboration, informal network, coalition, partnership, strategic alliance or joint ...
Many local health departments also have collected qualitative data on assets that can be leveraged to solve health problems. When viewed together, data from local health departments and from hospitals provides a more complete picture of a community's health challenges. That picture creates a shared understanding that can inform potential solutions.
Over the summer, eight students from Harvard T.H. Chan School of Public Health partnered with organizations and community members from Boston to Nairobi, Kenya, to learn about and help address locally identified public health problems. The students — members of the spring 2022 cohort of Community Engaged Learning Fellows — spoke about their ...
Therefore, CE research is a collaborative process that involves academic researchers and community members working together to solve vexing health problems that neither is adequately positioned on their own to solve. Through CE research, community members bring insight and local knowledge of community health problems to the table, while ...
We worked closely with community-based organizations, led by the Indiana Public Health Association, and together discovered three key learnings that are applicable to any community collaboration ...
A new approach to educating health leaders. The evolution of the College of Health Solutions was well underway by the time Sears came on board in 2018. In 2012, Dr. Keith Lindor, former dean of the Mayo Clinic Alix School of Medicine, was named executive vice provost and founding dean of a newly formed College of Health Solutions.
Community health platforms are the partnerships formed to assess and ensure public health. They provide the context in which outside interventions should be implemented and sustained, and they offer a way to develop and maintain community-centered solutions. Although local boards of health and health departments are the official bodies with the mandate to sustain strong community health ...
How can community members work together to solve health problems? How can schools have more effective health programs with limited funding? There's just one step to solve this.
Question: How can community members work together to solve health problems? How can community members work together to solve health problems? Here's the best way to solve it. Powered by Chegg AI. Step 1. View the full answer. Step 2. Unlock. Step 3. Unlock. Step 4. Unlock. Step 5. Unlock. Step 6.
How can community members work together to solve health problems? There are 2 steps to solve this one. Who are the experts? Experts have been vetted by Chegg as specialists in this subject. Expert-verified. Step 1. Community members can work together to solve health problems by engaging in collaborative efforts th... View the full answer. Step ...