Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 13, Issue 8
- Clinical course of a 66-year-old man with an acute ischaemic stroke in the setting of a COVID-19 infection
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-7441-6952 Saajan Basi 1 , 2 ,
- Mohammad Hamdan 1 and
- Shuja Punekar 1
- 1 Department of Stroke and Acute Medicine , King's Mill Hospital , Sutton-in-Ashfield , UK
- 2 Department of Acute Medicine , University Hospitals of Derby and Burton , Derby , UK
- Correspondence to Dr Saajan Basi; saajan.basi{at}nhs.net
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater oxygen requirement, alongside reduced levels of consciousness. A positive COVID-19 throat swab, in addition to bilateral pneumonia on chest X-ray and lymphopaenia in his blood tests, confirmed a diagnosis of COVID-19 pneumonia. A proactive decision was made involving the patients’ family, ward and intensive care healthcare staff, to not escalate care above a ward-based ceiling of care. The patient died 5 days following admission under the palliative care provided by the medical team.
- respiratory medicine
- infectious diseases
- global health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bcr-2020-235920
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is a new strain of coronavirus that is thought to have originated in December 2019 in Wuhan, China. In a matter of months, it has erupted from non-existence to perhaps the greatest challenge to healthcare in modern times, grinding most societies globally to a sudden halt. Consequently, the study and research into SARS-CoV-2 is invaluable. Although coronaviruses are common, SARS-CoV-2 appears to be considerably more contagious. The WHO figures into the 2003 SARS-CoV-1 outbreak, from November 2002 to July 2003, indicate a total of 8439 confirmed cases globally. 1 In comparison, during a period of 4 months from December 2019 to July 2020, the number of global cases of COVID-19 reached 10 357 662, increasing exponentially, illustrating how much more contagious SARS-CoV-2 has been. 2
Previous literature has indicated infections, and influenza-like illness have been associated with an overall increase in the odds of stroke development. 3 There appears to be a growing correlation between COVID-19 positive patients presenting to hospital with ischaemic stroke; however, studies investigating this are in progress, with new data emerging daily. This patient report comments on and further characterises the link between COVID-19 pneumonia and the development of ischaemic stroke. At the time of this patients’ admission, there were 95 positive cases from 604 COVID-19 tests conducted in the local community, with a predicted population of 108 000. 4 Only 4 days later, when this patient died, the figure increased to 172 positive cases (81% increase), illustrating the rapid escalation towards the peak of the pandemic, and widespread transmission within the local community ( figure 1 ). As more cases of ischaemic stroke in COVID-19 pneumonia patients arise, the recognition and understanding of its presentation and aetiology can be deciphered. Considering the virulence of SARS-CoV-2 it is crucial as a global healthcare community, we develop this understanding, in order to intervene and reduce significant morbidity and mortality in stroke patients.
- Download figure
- Open in new tab
- Download powerpoint
A graph showing the number of patients with COVID-19 in the hospital and in the community over time.
Case presentation
A 66-year-old man presented to the hospital with signs of left-sided weakness. The patient had a background of chronic obstructive pulmonary disease (COPD), atrial fibrillation and had one previous ischaemic stroke, producing left-sided haemiparesis, which had completely resolved. He was a non-smoker and lived in a house. The patient was found slumped over on the sofa at home on 1 April 2020, by a relative at approximately 01:00, having been seen to have no acute medical illness at 22:00. The patients’ relative initially described disorientation and agitation with weakness noted in the left upper limb and dysarthria. At the time of presentation, neither the patient nor his relative identified any history of fever, cough, shortness of breath, loss of taste, smell or any other symptoms; however, the patient did have a prior admission 9 days earlier with shortness of breath.
The vague nature of symptoms, entwined with considerable concern over approaching the hospital, due to the risk of contracting COVID-19, created a delay in the patients’ attendance to the accident and emergency department. His primary survey conducted at 09:20 on 1 April 2020 demonstrated a patent airway, with spontaneous breathing and good perfusion. His Glasgow Coma Scale (GCS) score was 15 (a score of 15 is the highest level of consciousness), his blood glucose was 7.2, and he did not exhibit any signs of trauma. His abbreviated mental test score was 7 out of 10, indicating a degree of altered cognition. An ECG demonstrated atrial fibrillation with a normal heart rate. His admission weight measured 107 kg. At 09:57 the patient required 2 L of nasal cannula oxygen to maintain his oxygen saturations between 88% and 92%. He started to develop agitation associated with an increased respiratory rate at 36 breaths per minute. On auscultation of his chest, he demonstrated widespread coarse crepitation and bilateral wheeze. Throughout he was haemodynamically stable, with a systolic blood pressure between 143 mm Hg and 144 mm Hg and heart rate between 86 beats/min and 95 beats/min. From a neurological standpoint, he had a mild left facial droop, 2/5 power in both lower limbs, 2/5 power in his left upper limb and 5/5 power in his right upper limb. Tone in his left upper limb had increased. This patient was suspected of having COVID-19 pneumonia alongside an ischaemic stroke.
Investigations
A CT of his brain conducted at 11:38 on 1 April 2020 ( figure 2 ) illustrated an ill-defined hypodensity in the right frontal lobe medially, with sulcal effacement and loss of grey-white matter. This was highly likely to represent acute anterior cerebral artery territory infarction. Furthermore an oval low-density area in the right cerebellar hemisphere, that was also suspicious of an acute infarction. These vascular territories did not entirely correlate with his clinical picture, as limb weakness is not as prominent in anterior cerebral artery territory ischaemia. Therefore this left-sided weakness may have been an amalgamation of residual weakness from his previous stroke, in addition to his acute cerebral infarction. An erect AP chest X-ray with portable equipment ( figure 3 ) conducted on the same day demonstrated patchy peripheral consolidation bilaterally, with no evidence of significant pleural effusion. The pattern of lung involvement raised suspicion of COVID-19 infection, which at this stage was thought to have provoked the acute cerebral infarct. Clinically significant blood results from 1 April 2020 demonstrated a raised C-reactive protein (CRP) at 215 mg/L (normal 0–5 mg/L) and lymphopaenia at 0.5×10 9 (normal 1×10 9 to 3×10 9 ). Other routine blood results are provided in table 1 .
CT imaging of this patients’ brain demonstrating a wedge-shaped infarction of the anterior cerebral artery territory.
Chest X-ray demonstrating the bilateral COVID-19 pneumonia of this patient on admission.
- View inline
Clinical biochemistry and haematology blood results of the patient
Interestingly the patient, in this case, was clinically assessed in the accident and emergency department on 23 March 2020, 9 days prior to admission, with symptoms of shortness of breath. His blood results from this day showed a CRP of 22 mg/L and a greater lymphopaenia at 0.3×10 9 . He had a chest X-ray ( figure 4 ), which indicated mild radiopacification in the left mid zone. He was initially treated with intravenous co-amoxiclav and ciprofloxacin. The following day he had minimal symptoms (CURB 65 score 1 for being over 65 years). Given improving blood results (declining CRP), he was discharged home with a course of oral amoxicillin and clarithromycin. As national governmental restrictions due to COVID-19 had not been formally announced until 23 March 2020, and inconsistencies regarding personal protective equipment training and usage existed during the earlier stages of this rapidly evolving pandemic, it is possible that this patient contracted COVID-19 within the local community, or during his prior hospital admission. It could be argued that the patient had early COVID-19 signs and symptoms, having presented with shortness of breath, lymphopaenia, and having had subtle infective chest X-ray changes. The patient explained he developed a stagnant productive cough, which began 5 days prior to his attendance to hospital on 23 March 2020. He responded to antibiotics, making a full recovery following 7 days of treatment. This information does not assimilate with the typical features of a COVID-19 infection. A diagnosis of community-acquired pneumonia or infective exacerbation of COPD seem more likely. However, given the high incidence of COVID-19 infections during this patients’ illness, an exposure and early COVID-19 illness, prior to the 23 March 2020, cannot be completely ruled out.
Chest X-ray conducted on prior admission illustrating mild radiopacification in the left mid zone.
On the current admission, this patient was managed with nasal cannula oxygen at 2 L. By the end of the day, this had progressed to a venturi mask, requiring 8 L of oxygen to maintain oxygen saturation. He had also become increasingly drowsy and confused, his GCS declined from 15 to 12. However, the patient was still haemodynamically stable, as he had been in the morning. An arterial blood gas demonstrated a respiratory alkalosis (pH 7.55, pCO 2 3.1, pO 2 6.7 and HCO 3 24.9, lactate 1.8, base excess 0.5). He was commenced on intravenous co-amoxiclav and ciprofloxacin, to treat a potential exacerbation of COPD. This patient had a COVID-19 throat swab on 1 April 2020. Before the result of this swab, an early discussion was held with the intensive care unit staff, who decided at 17:00 on 1 April 2020 that given the patients presentation, rapid deterioration, comorbidities and likely COVID-19 diagnosis he would not be for escalation to the intensive care unit, and if he were to deteriorate further the end of life pathway would be most appropriate. The discussion was reiterated to the patients’ family, who were in agreement with this. Although he had evidence of an ischaemic stroke on CT of his brain, it was agreed by all clinicians that intervention for this was not as much of a priority as providing optimal palliative care, therefore, a minimally invasive method of treatment was advocated by the stroke team. The patient was given 300 mg of aspirin and was not a candidate for fibrinolysis.
Outcome and follow-up
The following day, before the throat swab result, had appeared the patient deteriorated further, requiring 15 L of oxygen through a non-rebreather face mask at 60% FiO 2 to maintain his oxygen saturation, at a maximum of 88% overnight. At this point, he was unresponsive to voice, with a GCS of 5. Although, he was still haemodynamically stable, with a blood pressure of 126/74 mm Hg and a heart rate of 98 beats/min. His respiratory rate was 30 breaths/min. His worsening respiratory condition, combined with his declining level of consciousness made it impossible to clinically assess progression of the neurological deficit generated by his cerebral infarction. Moreover, the patient was declining sharply while receiving the maximal ward-based treatment available. The senior respiratory physician overseeing the patients’ care decided that a palliative approach was in this his best interest, which was agreed on by all parties. The respiratory team completed the ‘recognising dying’ documentation, which signified that priorities of care had shifted from curative treatment to palliative care. Although the palliative team was not formally involved in the care of the patient, the patient received comfort measures without further attempts at supporting oxygenation, or conduction of regular clinical observations. The COVID-19 throat swab confirmed a positive result on 2 April 2020. The patient was treated by the medical team under jurisdiction of the hospital palliative care team. This included the prescribing of anticipatory medications and a syringe driver, which was established on 3 April 2020. His antibiotic treatment, non-essential medication and intravenous fluid treatment were discontinued. His comatose condition persisted throughout the admission. Once the patients’ GCS was 5, it did not improve. The patient was pronounced dead by doctors at 08:40 on 5 April 2020.
SARS-CoV-2 is a type of coronavirus that was first reported to have caused pneumonia-like infection in humans on 3 December 2019. 5 As a group, coronaviruses are a common cause of upper and lower respiratory tract infections (especially in children) and have been researched extensively since they were first characterised in the 1960s. 6 To date, there are seven coronaviruses that are known to cause infection in humans, including SARS-CoV-1, the first known zoonotic coronavirus outbreak in November 2002. 7 Coronavirus infections pass through communities during the winter months, causing small outbreaks in local communities, that do not cause significant mortality or morbidity.
SARS-CoV-2 strain of coronavirus is classed as a zoonotic coronavirus, meaning the virus pathogen is transmitted from non-humans to cause disease in humans. However the rapid spread of SARS-CoV-2 indicates human to human transmission is present. From previous research on the transmission of coronaviruses and that of SARS-CoV-2 it can be inferred that SARS-CoV-2 spreads via respiratory droplets, either from direct inhalation, or indirectly touching surfaces with the virus and exposing the eyes, nose or mouth. 8 Common signs and symptoms of the COVID-19 infection identified in patients include high fevers, severe fatigue, dry cough, acute breathing difficulties, bilateral pneumonia on radiological imaging and lymphopaenia. 9 Most of these features were identified in this case study. The significance of COVID-19 is illustrated by the speed of its global spread and the potential to cause severe clinical presentations, which as of April 2020 can only be treated symptomatically. In Italy, as of mid-March 2020, it was reported that 12% of the entire COVID-19 positive population and 16% of all hospitalised patients had an admission to the intensive care unit. 10
The patient, in this case, illustrates the clinical relevance of understanding COVID-19, as he presented with an ischaemic stroke underlined by minimal respiratory symptoms, which progressed expeditiously, resulting in acute respiratory distress syndrome and subsequent death.
Our case is an example of a new and ever-evolving clinical correlation, between patients who present with a radiological confirmed ischaemic stroke and severe COVID-19 pneumonia. As of April 2020, no comprehensive data of the relationship between ischaemic stroke and COVID-19 has been published, however early retrospective case series from three hospitals in Wuhan, China have indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke. 11 These studies have not yet undergone peer review, but they tell us a great deal about the relationship between COVID-19 and ischaemic stroke, and have been used to influence the American Heart Associations ‘Temporary Emergency Guidance to US Stroke Centres During the COVID-19 Pandemic’. 12
The relationship between similar coronaviruses and other viruses, such as influenza in the development of ischaemic stroke has previously been researched and provide a basis for further investigation, into the prominence of COVID-19 and its relation to ischaemic stroke. 3 Studies of SARS-CoV-2 indicate its receptor-binding region for entry into the host cell is the same as ACE2, which is present on endothelial cells throughout the body. It may be the case that SARS-CoV-2 alters the conventional ability of ACE2 to protect endothelial function in blood vessels, promoting atherosclerotic plaque displacement by producing an inflammatory response, thus increasing the risk of ischaemic stroke development. 13
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14
Arrhythmias such as atrial fibrillation had been identified in 17% of 138 COVID-19 patients, in a study conducted in Wuhan, China. 15 In this report, the patient was known to have atrial fibrillation and was treated with rivaroxaban. The acute inflammatory state COVID-19 is known to produce had the potential to create a prothrombotic environment, culminating in an ischaemic stroke.
Some early case studies produced in Wuhan describe patients in the sixth decade of life that had not been previously noted to have antiphospholipid antibodies, contain the antibodies in blood results. They are antibodies signify antiphospholipid syndrome; a prothrombotic condition. 16 This raises the hypothesis concerning the ability of COVID-19 to evoke the creation of these antibodies and potentiate thrombotic events, such as ischaemic stroke.
No peer-reviewed studies on the effects of COVID-19 and mechanism of stroke are published as of April 2020; therefore, it is difficult to evidence a specific reason as to why COVID-19 patients are developing neurological signs. It is suspected that a mixture of the factors mentioned above influence the development of ischaemic stroke.
If we delve further into this patients’ comorbid state exclusive to COVID-19 infection, it can be argued that this patient was already at a relatively higher risk of stroke development compared with the general population. The fact this patient had previously had an ischaemic stroke illustrates a prior susceptibility. This patient had a known background of hypertension and atrial fibrillation, which as mentioned previously, can influence blood clot or plaque propagation in the development of an acute ischaemic event. 15 Although the patient was prescribed rivaroxaban as an anticoagulant, true consistent compliance to rivaroxaban or other medications such as amlodipine, clopidogrel, candesartan and atorvastatin cannot be confirmed; all of which can contribute to the reduction of influential factors in the development of ischaemic stroke. Furthermore, the fear of contracting COVID-19, in addition to his vague symptoms, unlike his prior ischaemic stroke, which demonstrated dense left-sided haemiparesis, led to a delay in presentation to hospital. This made treatment options like fibrinolysis unachievable, although it can be argued that if he was already infected with COVID-19, he would have still developed life-threatening COVID-19 pneumonia, regardless of whether he underwent fibrinolysis. It is therefore important to consider that if this patient did not contract COVID-19 pneumonia, he still had many risk factors that made him prone to ischaemic stroke formation. Thus, we must consider whether similar patients would suffer from ischaemic stroke, regardless of COVID-19 infection and whether COVID-19 impacts on the severity of the stroke as an entity.
Having said this, the management of these patients is dependent on the likelihood of a positive outcome from the COVID-19 infection. Establishing the ceiling of care is crucial, as it prevents incredibly unwell or unfit patients’ from going through futile treatments, ensuring respect and dignity in death, if this is the likely outcome. It also allows for the provision of limited or intensive resources, such as intensive care beds or endotracheal intubation during the COVID-19 pandemic, to those who are assessed by the multidisciplinary team to benefit the most from their use. The way to establish this ceiling of care is through an early multidisciplinary discussion. In this case, the patient did not convey his wishes regarding his care to the medical team or his family; therefore it was decided among intensive care specialists, respiratory physicians, stroke physicians and the patients’ relatives. The patient was discussed with the intensive care team, who decided that as the patient sustained two acute life-threatening illnesses simultaneously and had rapidly deteriorated, ward-based care with a view to palliate if the further deterioration was in the patients’ best interests. These decisions were not easy to make, especially as it was on the first day of presentation. This decision was made in the context of the patients’ comorbidities, including COPD, the patients’ age, and the availability of intensive care beds during the steep rise in intensive care admissions, in the midst of the COVID-19 pandemic ( figure 1 ). Furthermore, the patients’ rapid and permanent decline in GCS, entwined with the severe stroke on CT imaging of the brain made it more unlikely that significant and permanent recovery could be achieved from mechanical intubation, especially as the damage caused by the stroke could not be significantly reversed. As hospitals manage patients with COVID-19 in many parts of the world, there may be tension between the need to provide higher levels of care for an individual patient and the need to preserve finite resources to maximise the benefits for most patients. This patient presented during a steep rise in intensive care admissions, which may have influenced the early decision not to treat the patient in an intensive care setting. Retrospective studies from Wuhan investigating mortality in patients with multiple organ failure, in the setting of COVID-19, requiring intubation have demonstrated mortality can be up to 61.5%. 17 The mortality risk is even higher in those over 65 years of age with respiratory comorbidities, indicating why this patient was unlikely to survive an admission to the intensive care unit. 18
Regularly updating the patients’ family ensured cooperation, empathy and sympathy. The patients’ stroke was not seen as a priority given the severity of his COVID-19 pneumonia, therefore the least invasive, but most appropriate treatment was provided for his stroke. The British Association of Stroke Physicians advocate this approach and also request the notification to their organisation of COVID-19-related stroke cases, in the UK. 19
Learning points
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is one of seven known coronaviruses that commonly cause upper and lower respiratory tract infections. It is the cause of the 2019–2020 global coronavirus pandemic.
The significance of COVID-19 is illustrated by the rapid speed of its spread globally and the potential to cause severe clinical presentations, such as ischaemic stroke.
Early retrospective data has indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke.
Potential mechanisms behind stroke in COVID-19 patients include a plethora of hypercoagulability secondary to critical illness and systemic inflammation, the development of arrhythmia, alteration to the vascular endothelium resulting in atherosclerotic plaque displacement and dehydration.
It is vital that effective, open communication between the multidisciplinary team, patient and patients relatives is conducted early in order to firmly establish the most appropriate ceiling of care for the patient.
- Cannine M , et al
- Wunderink RG
- van Doremalen N ,
- Bushmaker T ,
- Morris DH , et al
- Wang X-G , et al
- Grasselli G ,
- Pesenti A ,
- Wang M , et al
- American Stroke Assocation, 2020
- Zhang Y-H ,
- Zhang Y-huan ,
- Dong X-F , et al
- Li X , et al
- Hu C , et al
- Zhang S , et al
- Jiang B , et al
- Xu J , et al
- British Association of Stroke Physicians
Contributors SB was involved in the collecting of information for the case, the initial written draft of the case and researching existing data on acute stroke and COVID-19. He also edited drafts of the report. MH was involved in reviewing and editing drafts of the report and contributing new data. SP oversaw the conduction of the project and contributed addition research papers.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Next of kin consent obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 7: 10 Real Cases on Transient Ischemic Attack and Stroke: Diagnosis, Management, and Follow-Up
Jeirym Miranda; Fareeha S. Alavi; Muhammad Saad
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion, clinical symptoms.
- Radiologic Findings
- Full Chapter
- Supplementary Content
Case 1: Management of Acute Thrombotic Cerebrovascular Accident Post Recombinant Tissue Plasminogen Activator Therapy
A 59-year-old Hispanic man presented with right upper and lower extremity weakness, associated with facial drop and slurred speech starting 2 hours before the presentation. He denied visual disturbance, headache, chest pain, palpitations, dyspnea, dysphagia, fever, dizziness, loss of consciousness, bowel or urinary incontinence, or trauma. His medical history was significant for uncontrolled type 2 diabetes mellitus, hypertension, hyperlipidemia, and benign prostatic hypertrophy. Social history included cigarette smoking (1 pack per day for 20 years) and alcohol intake of 3 to 4 beers daily. Family history was not significant, and he did not remember his medications. In the emergency department, his vital signs were stable. His physical examination was remarkable for right-sided facial droop, dysarthria, and right-sided hemiplegia. The rest of the examination findings were insignificant. His National Institutes of Health Stroke Scale (NIHSS) score was calculated as 7. Initial CT angiogram of head and neck reported no acute intracranial findings. The neurology team was consulted, and intravenous recombinant tissue plasminogen activator (t-PA) was administered along with high-intensity statin therapy. The patient was admitted to the intensive care unit where his hemodynamics were monitored for 24 hours and later transferred to the telemetry unit. MRI of the head revealed an acute 1.7-cm infarct of the left periventricular white matter and posterior left basal ganglia. How would you manage this case?
This case scenario presents a patient with acute ischemic cerebrovascular accident (CVA) requiring intravenous t-PA. Diagnosis was based on clinical neurologic symptoms and an NIHSS score of 7 and was later confirmed by neuroimaging. He had multiple comorbidities, including hypertension, diabetes, dyslipidemia, and smoking history, which put him at a higher risk for developing cardiovascular disease. Because his symptoms started within 4.5 hours of presentation, he was deemed to be a candidate for thrombolytics. The eligibility time line is estimated either by self-report or last witness of baseline status.
Ischemic strokes are caused by an obstruction of a blood vessel, which irrigates the brain mainly secondary to the development of atherosclerotic changes, leading to cerebral thrombosis and embolism. Diagnosis is made based on presenting symptoms and CT/MRI of the head, and the treatment is focused on cerebral reperfusion based on eligibility criteria and timing of presentation.
Symptoms include alteration of sensorium, numbness, decreased motor strength, facial drop, dysarthria, ataxia, visual disturbance, dizziness, and headache.
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
- Open access
- Published: 06 September 2022
Stroke in young adults, stroke types and risk factors: a case control study
- Priscilla Namaganda 1 ,
- Jane Nakibuuka 2 ,
- Mark Kaddumukasa 3 &
- Elly Katabira 4
BMC Neurology volume 22 , Article number: 335 ( 2022 ) Cite this article
9584 Accesses
9 Citations
Metrics details
Stroke is the second leading cause of death above the age of 60 years, and the fifth leading cause in people aged 15 to 59 years old as reported by the World Health Organization global burden of diseases. Stroke in the young is particularly tragic because of the potential to create long-term disability, burden on the victims, their families, and the community at large. Despite this, there is limited data on stroke in young adults, and its risk factors in Uganda. Therefore, we determined the frequency and risk factors for stroke among young adults at Mulago hospital.
A case control study was conducted among patients presenting consecutively to the general medical wards with stroke during the study period September 2015 to March 2016. A brain Computerized Tomography scan was performed to confirm stroke and classify the stroke subtype. Controls were patients that presented to the surgical outpatient clinic with minor surgical conditions, matched for age and sex. Social demographic, clinical and laboratory characteristics were assessed for both cases and controls. Descriptive statistics including frequencies, percentages, means, and standard deviation were used to describe the social demographics of case and controls as well as the stroke types for cases. To determine risk factors for stroke, a conditional logistic regression, which accounts for matching (e.g., age and sex), was applied. Odds ratio (with 95% confidence interval) was used as a measure for associations.
Among 51 patients with stroke, 39(76.5%) had ischemic stroke and 12(23.5%) had hemorrhagic stroke. The mean age was 36.8 years (SD 7.4) for stroke patients (cases) and 36.8 years (SD 6.9) for controls. Female patients predominated in both groups 56.9% in cases and 52.9% in controls. Risk factors noted were HIV infection, OR 3.57 (95% CI 1.16–10.96), elevated waist to hip ratio, OR 11.59(95% CI 1.98–68.24) and sickle cell disease, OR 4.68 (95% CI 1.11–19.70). This study found a protective effect of oral contraceptive use for stroke OR 0.27 95% CI 0.08–0.87. There was no association between stroke and hypertension, diabetes, and hyperlipidemia.
Among young adults with stroke, ischemic stroke predominated over hemorrhagic stroke. Risk factors for stroke were HIV infection, elevated waist to hip ratio and sickle cell disease.
Peer Review reports
Stroke is the second leading cause of death above the age of 60 years, and the fifth leading cause in people aged 15 to 59 years old as reported by the World Health Organization (WHO) global burden of diseases [ 1 ]. The severity of stroke in the young is relatively low in developed countries ranging from 2 -7% in Italy and USA respectively [ 2 , 3 ]. In Africa, on the other hand the prevalence of stroke among young adults is 12.9% in Nigeria [ 4 ], 31% in South Africa [ 5 ], 28.9% in Morocco [ 6 ]. The incidence of ischemic stroke in the young has been increasing globally over the last 2–3 decades. From the Danish National Patient Register, the incidence rates of first‐time hospitalizations for ischemic stroke and transient ischemic attack (TIA) in young adults have increased substantially since the mid 1990s while the incidences of hospitalizations for intracerebral hemorrhage and subarachnoid hemorrhage remained stable during the study period [ 7 ].
In Uganda, literature on stroke in young adults is limited however results of a study done among acute stroke patients admitted to the national referral hospital (Mulago hospital) showed a 30-day mortality of 43.8%. Out of 133 patients, 32 patients (25%) were less than 51 years old. Out of the 56 patients that died, 13 patients (23%) were less than 51 years [ 8 ].
Rapid western cultural adaption (sedentary lifestyle, deleterious health behavior like consumption of tobacco and alcohol and high fat/cholesterol diet) and Human immunodeficiency syndrome/ Acquired immunodeficiency syndrome (HIV/AIDS) that is highly prevalent in Africa has accelerated risk factors and increased the burden of stroke [ 9 ].
Most literature indicates that the traditional risk factors i.e., hypertension, diabetes mellitus and dyslipidemia are still the commonest risk factors with hypertension having the highest frequency. Other risk factors common to the young include smoking, excessive alcohol intake, illicit drug use, oral contraceptive use and migraine [ 10 ].
Although stroke is predominantly a disease of the middle age and the elderly, its occurrence in younger age groups is not rare. Stroke in young adults seems to be increasing and is particularly tragic because of the potential to create long-term disability, burden on the victims, their families, and the community at large such as Uganda. Despite the huge socioeconomic impact of stroke in this age group, there is a scarcity of data regarding stroke in young adults in sub-Saharan Africa including Uganda. Effective stroke prevention strategies in the young require comprehensive information on risk factors and possible causes. Although case reports and etiologic investigations of possible causes of stroke in the young have been identified especially in developed countries, there is limited data on risk factors in Africa Uganda inclusive. Information obtained from this study will fill the knowledge gap in this area of stroke in the young which will inform institutional strategies on prevention and management of stroke in this age group. This study, therefore, seeks to determine the frequency of stroke types and risk factors for this population.
The aims of the study were:
To determine the frequency of stroke types among young adults on the general medical wards in Mulago hospital between September 2015 and March 2016.
To determine the risk factors for stroke (i.e., ischemic, and hemorrhagic stroke) among young adults on the general medical wards in Mulago hospital between September and March 2016.
This was a case control study. Cases were defined as patients with a confirmed diagnosis of stroke by brain computerized tomography (CT) scan that met the inclusion criteria. Controls were defined as patients with minor surgical conditions that met the inclusion criteria. The study was carried out in Mulago hospital which is the national referral hospital in Uganda as well as the teaching hospital of Makerere University College of health sciences. It has a bed capacity of 1500 beds and has both inpatient wards, outpatient departments both for medical and surgical specialties. It has a radiological department with CT scan and highly trained personnel and a well-equipped laboratory. Cases were recruited consecutively from the medical wards specifically on the neurology ward of Mulago hospital. Patients on the neurology ward are managed by physicians that have had additional training in the management of neurological conditions.
Controls were recruited from general surgical outpatient departments from Mulago hospital. They were matched for age and sex. Eligible patients were patients aged 15–45 years, confirmed diagnosis of stroke on brain CT scan and with a written informed consent or assent for patients less than 18 years. These included patients with intracranial hemorrhages and ischemic stroke, none had subarachnoid hemorrhage. Patients were excluded if they were unconscious and with no valid surrogate (next of kin) and HIV positive with opportunistic infections. Patients eligible as control were, patient aged 15–45 years, minor surgical condition, written informed consent or assent for patients less than 18 years. Patients with features of stroke secondary to non-vascular causes like trauma, tumors were excluded as controls. For controls, we chose patients with minor surgical conditions because we wanted controls to be hospital patients but with non-medical conditions that could confound our findings. Such conditions included lacerations, hernias, lipomas, ingrown toenails, circumcision.
Based on the catchment area of Mulago, patients with minor surgical conditions are likely to have similar social economic status and come from similar neighborhoods as would health controls living in the catchment areas as patients with stroke.
The best alternative would have been healthy controls from the neighborhoods of the patients with stroke, but this would have been resource consuming.
The sample size was calculated assuming a prevalence of 62.2% of hypertension among the stroke patients as was indicated in a similar study among the young Thai adults in Bangkok, Thailand (Bandasak et al., 2011) [ 11 ]. We also assumed that the risk for stroke is higher among the hypertensive with an OR of 3. With this sample size, we were powered to detect associations with other risk factors like smoking (OR 2.6) [ 12 ], diabetes (OR 13.2 for black men and 22.1 for black women) [ 13 ].
With these assumptions, a sample size of 51 cases and 51 controls was found sufficient with 80% power and 0.05 level of significance.
Sampling procedure
All young patients admitted on the general medical wards suspected of having stroke were screened and brain CT scan done. Once a diagnosis of stroke was confirmed on CT scan, participants who consented to participate in the study were recruited consecutively, a standardized questionnaire administered by the research team for those patients able to communicate. For patients not able to communicate, consent and information were obtained through the care givers. Controls were selected from the general surgical outpatient clinic using consecutive sampling method. This was done after we had obtained all the cases. These were matched for age and sex until the sample size was accrued.
Information was collected on:
Social demographic characteristics i.e., age, sex, level of education, occupation, religion, history of smoking and alcohol consumption, history of illicit drug use, history of oral contraceptive use.
Clinical examination included general physical examination, blood pressure using a digital blood pressure machine. For patients who were too weak to sit up, blood pressure measurement was taken in supine position. For those able to sit, it was taken in the sitting position. The two blood pressure measurements were taken at an interval of 5 min and the average blood pressure recorded as the final blood pressure.
Physical measurements for the weight and hip were taken using a stretchable tape measure. Waist measurements were taken at the narrowest point-umbilicus and hip measurements at the widest point- buttocks. A waist to hip ratio was obtained and recorded on the questionnaire.
Blood was drawn for laboratory tests; high density lipoprotein, low density lipoprotein (HDL/LDL), fasting blood sugar, full blood count, Hb electrophoresis, prothrombin time/ international normalization ratio (PT/INR), HIV serology, Treponema pallidum hemagglutination (TPHA).
Other information obtained was history and family history of diabetes and hypertension.
The general surgical outpatient clinic runs every Tuesday, and Thursday in Old Mulago hospital Participants were identified at the surgical outpatient clinic. Those matching the age and sex of the cases were recruited, written consent/assent obtained, and questionnaire was administered by the PI. The procedure as explained above was followed for the controls.
Data collection
A pre-tested and standardized questionnaire was used as a data collection tool. The principal investigator administered the questionnaire to the participants in data collection. Data on socio demographics and past medical history was collected.
Results from imaging and laboratory investigations were also recorded into the questionnaire.
Data collected was double entered into the computer using EPI-DATA (version 3.1) software to minimize data entry errors. Data was then backed up and archived in both soft and hard copy to avoid losses. Confidentiality was ensured using code numbers instead of patients’ names. Questionnaires were stored in a lockable cabinet for safety.
Data analysis
Data was analyzed using STATA Version 12 (StataCorp. 2011. Stata Statistical Software: Release 12 . College Station, TX: StataCorp LP). Descriptive statistics were used to describe characteristics of the study participants and the stroke subtypes which included frequencies, percentages, means and standard deviation. To determine factors associated with stroke, a conditional logistic regression, which accounts for matching (e.g., age and sex), was applied. Odds ratio (with 95% confidence interval) was used as a measure for associations. Factors with p -values < 0.2 at a bi-variable analysis were entered into a multiple conditional logistic regression to obtain the adjusted estimates. Factors whose 95% confidence interval for the odds ratio that excludes a 1 or whose p -value < 0.05, were considered statistically significant at the adjusted level. Post-hoc power calculation was performed for the adjusted analysis to check if there was enough power to detect a difference between cases and controls.
Quality control
To ensure quality of results several measures were undertaken, these included:
The questionnaires were pre-tested and standardized before study commenced.
The research team administered the structured, pre- coded and pre-tested questionnaire to enrolled participants on a face-to-face basis and brain CT scans were done by competent and well-trained radiology technicians and interpretation done by a specialist radiologist at the Radiology Department of Mulago hospital.
The questionnaires were checked for completeness at the end of every interview. The two files were compared, and any discordance corrected against data recorded with the questionnaire. The data were then backed up.
Ethical consideration
Written informed consent/ assent was obtained from all participants or their parent/guardian or legal authorized representative to participate in the study. Ethical approval was obtained from Makerere University, school of medicine research and ethics committee (SOMREC) (reference number #REC REF 2015–105).
Confidentiality was ensured using code numbers instead of patients’ names. Questionnaires were stored in a lockable cabinet for safety.
Profile of the study
Enrollment of study participants was carried out between September 2015 to March 2016 in Mulago hospital. The patient flow diagram for cases and controls is as shown in Fig. 1 .
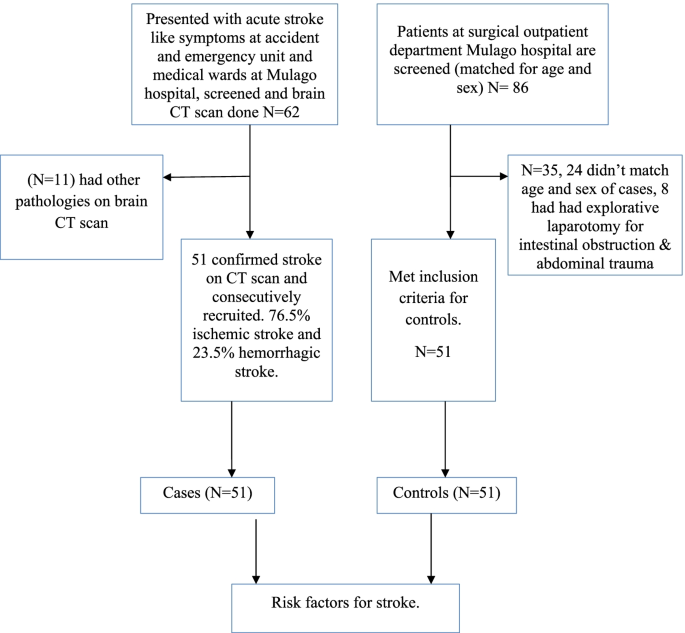
Patient flow diagram
Social demographic characteristics of the study population
A total of 51 cases aged 18 to 45 years and the same number of hospital control matched for age and sex were identified. The mean age of cases was 36.8 years (standard deviation (SD) 7.4) and the control was 36.8 years (SD 6.9). Females predominated in both groups with 56.9% in cases and 52.9% in controls. There was no significant difference in other baseline characteristics between cases and controls except in oral contraceptive use, waist to hip ratio, HIV status and sickle cell disease. Details of the social demographic characteristics are shown in Table 1 .
Clinical characteristics of the study participants
The mean fasting blood sugar was 6.6 (SD 3.9) for cases and 5.3 (SD 0.7) for controls. This was statistically significant with a p value of 0.015. Waist to hip ratio was also statistically significant with a p value of 0.007. Cases with an elevated wait to hip ratio were 14 (27.5%) and controls were 3 (5.9%). Table 2 shows the baseline clinical characteristics of the study participants.
Laboratory characteristics of the study participants
HIV serology and Hb electrophoresis were statistically significant with a p value of 0.076 and 0.023 respectively. 18 patients (35.3%) were reactive for HIV among cases and controls 10 (19.6%). 12 patients (23.5%) had abnormal Hb electrophoresis among cases controls 3 (5.9%). Table 3 shows the laboratory characteristics of the study participants.
Stroke types
Stroke types by social demographic characteristics of cases.
Among 62 patients, who had brain CT scan done, 11 patients had non stroke pathologies (4 had brain abscesses, 7 patients had ring enhancing lesions suggestive of toxoplasmosis). Among 51 patients with stroke confirmed on CT scan, the frequency of ischemic stroke was 76.5% and hemorrhagic stroke was 23.5%.
Most participants with ischemic or hemorrhagic stroke were in the age group 36–45 years. Females predominated in both ischemic and hemorrhagic stroke. Details of the social demographic characteristics by stroke types are shown in Table 4 .
Clinical and laboratory characteristics by stroke types
Majority of patients with hemorrhagic stroke were hypertensive (91.7%) compared to only 25.6% among patients with ischemic stroke. Details of the clinical and laboratory characteristics of the study participants by stroke subtypes are shown in Table 5 .
Risk factors for stroke at univariate analysis
Social demographic characteristics at univariate analysis.
Oral contraceptive use showed a significant difference with an unadjusted OR of 0.27 (95% CI 0.08–0.87) case subjects 23.3% and control subjects 56.5%. Belonging to other religion (seventh day advent, Pentecostal) was statistically significant with a p value of 0.009, OR 0.17. These findings are detailed in Table 6 below.
Clinical characteristics at univariate analysis
There was a significant difference in waist to hip ratio between cases (27.5%) and controls (5.9%), with unadjusted OR 6.85 (CI 1.70–27.62). HIV serology with an unadjusted OR of 2.64 (95% CI 1.03–6.82). Hb electrophoresis with an unadjusted OR of 4.31 (95% CI- 1.15–16.17). Fasting blood sugar with an unadjusted OR of 1.64 (95% CI 1.02–2.62). Details of the above findings are shown in Table 7 below.
Risk factors for stroke at multivariate analysis
At multivariate analysis, HIV serology (OR 3.72, 95% CI 1.16–10.96), waist to hip ratio (OR 11.26 95% CI 1.98–68.24) and sickle cell disease OR 4.78 95% CI 1.11–19.70) were independent risk factors for stroke in young adults. Table 8 shows risk factors at multivariate analysis. None of the patients with HIV met the definition of AIDS as defined by the occurrence of any of the more than 20 life-threatening cancers or “opportunistic infections”, by WHO.
This case–control study showed that the frequency of ischemic stroke was higher than that of hemorrhagic stroke in young Ugandan population. We showed that positive HIV serology, elevated waist to hip ratio and sickle cell disease were independent risk factors for stroke in this population.
This is consistent with several studies that have been done and found ischemic stroke to be more prevalent than hemorrhagic stroke. Studies done in Africa, in Libya reported 77% ischemic stroke and 23% hemorrhagic stroke (these included both intracerebral and subarachnoid hemorrhagic stroke) [ 14 ], in Morocco, 87.3% ischemic stroke and 12.7% hemorrhagic (study did not specify on the subtypes of hemorrhagic stroke) [ 6 ]. In a study from Bosnia and Herzegovina, Subarachnoid hemorrhage was more frequent in young adults compared with older patients (> 45 years of age) (22% vs. 3.5%), intracerebral hemorrhage (ICH) was similar in both groups (16.9% vs. 15.8%), but ischemic stroke (IS) was predominant stroke type in the older group (61% vs. 74%) [ 15 ]. On the other hand, studies focusing on all young stroke patients and including also subarachnoid hemorrhages have found much higher proportion of hemorrhagic strokes in younger vs. older individuals. Population-based studies have reported as low as 57% prevalence for ischemic stroke in those aged > 45, as reported by a recent narrative review [ 16 ]. This difference in occurrence of stroke subtypes could be due to the low prevalence of hypertension in this population in our setting given that hypertension has been reported to be the commonest risk factor for hemorrhagic stroke.
Most previous studies of HIV and stroke have been retrospective, but the prospective studies in Africa and East Africa have reported the importance of HIV as a risk factor for stroke [ 17 ]. A recently published study done in Malawi, with defined cases and population controls and 99% ascertainment of HIV status, reported HIV infection as an independent risk factor for stroke. This study further found that patients who had started standard HIV treatment in the previous six months had a higher risk of stroke (OR 15.6 95% CI 4.21–46.6). This was probably due to an immune reconstitution inflammatory syndrome (IRIS) like process [ 18 ]. A variety of mechanisms have been implicated in the association of HIV and stroke, these include HIV associated vasculopathy, vasculitis which causes abnormality of the intracranial or extracranial cerebral blood vessels and neoplastic involvement. Indirectly through cardioembolic, coagulopathy in association with protein C and protein S deficiency. Some infections are well established causes of stroke, such as Mycobacterium tuberculosi s , syphilis, and varicella zoster virus through increased susceptibility to acquisition or reactivation of these infections [ 19 , 20 ]. Combined antiretroviral therapy (cART) might unmask occult opportunistic infections that subsequently cause a stroke. This possibility should be considered in all patients who have had an acute stroke or have worsening of stroke symptoms after initiation of cART [ 21 ].
An elevated waist to hip ratio (WHR) was associated with 12 times increased risk of stroke among young adults in Mulago hospital compared to individuals with a normal waist to hip ratio. Abdominal obesity (measured as waist–hip ratio) is associated with an increased risk of myocardial infarction, stroke, and premature death [ 22 ]. This agrees with a few studies that have assessed the association of stroke with waist to hip ratio. Aaron et al. 1990, assessed the relation between body fat distribution, and the 2-year incidences of hypertension and stroke in a cohort of 41,837 women aged 55–69 years. Women who developed stroke were 2.1 (95% CI 1.5–2.9) times more likely to have an elevated ratio than those who did not [ 23 ]. Md Habib et al. 2011 assessed high waist to hip ratio as a risk factor for ischemic stroke for overall stroke and he found 64% of the ischemic stroke patient had abnormal WHR in Bangladesh [ 24 ]. Abdominal obesity measured with WHR was an independent risk factor for cryptogenic ischemic stroke (CIS) in young adults after rigorous adjustment for concomitant risk factors in the Revealing the Etiology, Triggers, and Outcome (SECRETO; NCT01934725) study, a prospective case–control study that included patients aged 18–49 years with a first ever CIS at 19 European university centers [ 25 ].
Sickle cell disease was also associated with increased risk of stroke among young adults in Mulago hospital. This agrees with several studies that have associated sickle cell disease with stroke. Ohene et al. 1998 assessed cerebrovascular accidents (CVA) in sickle cell disease, found the highest rates of prevalence of 4.01% and incidence of 0.61 per 100 patient-years. The incidence of hemorrhagic stroke was highest among patients aged 20 to 29 years [ 26 ].
In our study, the unadjusted OR for oral contraceptive use was 0.26 95% CI 0.08–0.87 with a p value of 0.028. This observation at the unadjusted level is significant but could be due to another variable which is a confounder to OC use such as higher socioeconomic status and better control of other possible risk factors.
In our study, we found no association between hypertension and stroke in young adults though it’s an independent risk factor for stroke in the older population. This finding is different from the multinational interstroke study which attributed most strokes among young adults in low- and middle-income countries to hypertension. In that study, only one fifth of the patients were from wealthier African countries where hypertension, diabetes and hypercholesterolemia are likely to occur with higher prevalence than in Mulago hospital [ 27 ]. Other studies have also reported the role of hypertension as a risk factor for stroke in young adults, low physical activity and hypertension were the most important risk factors, accounting for 59.7% and 27.1% of all strokes, respectively among a German nationwide case–control study based on patients enrolled in the SIFAP1 study (Stroke in Young Fabry Patients) 2007 to 2010 and controls from the population-based GEDA study (German Health Update) 2009 to 2010 [ 28 ]. A study that used population-based controls for hospitalized young patients with ischemic stroke demonstrated that independent risk factors for stroke were atrial fibrillation (OR 10.43; cardiovascular disease (OR, 8.01; type 1 diabetes mellitus (OR, 6.72; type 2 diabetes mellitus (OR, 2.31, low high‐density lipoprotein cholesterol (OR, 1.81; current smoking status (OR, 1.81; hypertension (OR, 1.43, and a family history of stroke (OR, 1.37) [ 29 ].
This finding could be explained by the high prevalence of hypertension in the general peri urban Ugandan population among young adults as reported by Kayima et al. 2015. He found a prevalence of 15% (95% CI 14.2 – 19.6%) % for young adults aged 18–44 years [ 30 ].
The study was conducted at Mulago hospital which is a national referral hospital in Uganda situated in central Uganda. Mulago hospital received patients both referred patients from all over Uganda and those from its catchment area. This is generally representative of the whole Ugandan population.
Uganda has a young population and with an HIV prevalence comparable to most countries in Sub-Saharan Africa, so the findings of this study are generalizable to other Sub-Saharan African populations.
Ischemic stroke is more prevalent than hemorrhagic stroke among young adults in Mulago hospital. Independent risk factors for stroke among young adults in Mulago hospital were HIV infection, elevated waist to hip ratio and sickle cell disease. Oral contraceptive use was found to be protective of stroke among young adults in Mulago hospital. There was no significant association between stroke among young adults and hypertension, diabetes, hyperlipidemia, smoking, alcohol use and illicit use.
Study limitations
The sample size was too small to detect all but the strongest associations with common exposures. When designing the study, we based on hypertension as a significant driver for strokes in this population based on other studies done to calculate the sample size, however based on our findings, hypertension was not a big driver of stroke in this population. Secondly the nature of stroke type associated with hypertension is hemorrhagic which were less common in this study. This was an unexpected finding and needs more evaluation.
Consecutive sampling methods has selection bias in which a variable that is associated with the outcome under investigation may occur more frequently or less in those sampled in this period as compared to the general population.
The use of a combined ischemic stroke and intracerebral hemorrhage group may have obscured relationships specific to one group, i.e., the risk factors for stroke were not stratified for type of stroke.
The best alternative for controls would have been healthy controls from the neighborhoods of the patients with stroke, but this would have been resource consuming hence the choice of hospital controls with different medical conditions from cases.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Turner MB. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–245.
PubMed Google Scholar
Griffiths D, Sturm J. Epidemiology and etiology of young stroke. Stroke research and treatment, 2011. 2011.
Google Scholar
Bevan HS, Sharma K, Bradley W. Stroke in young adults. Stroke. 1990;21(3):382–6.
Article CAS Google Scholar
Mustapha AF, Sanya EO, Bello TO. Stroke among young adults at the LAUTECH Teaching Hospital, Osogbo, Nigeria. Nig Q J Hosp Med. 2012;22(3):177–80.
CAS PubMed Google Scholar
Hoffmann M. Stroke in the young: the multiethnic prospective Durban stroke data bank results. J Stroke Cerebrovasc Dis. 1998;7(6):404–13.
Chraa M, Louhab N, Kissani N. Stroke in young adults: about 128 cases. Pan Afr Med J. 2014;17(37).
Tibæk M, Dehlendorff C, Jørgensen HS, Forchhammer HB, Johnsen SP, Kammersgaard LP. Increasing incidence of hospitalization for stroke and transient ischemic attack in young adults: a registry-based study. J Am Heart Assoc. 2016;5(5):e003158. https://doi.org/10.1161/JAHA.115.003158 .
Article PubMed PubMed Central Google Scholar
Kwarisima L, Mukisa R, Nakibuuka J, Matovu S, Katabira E. Thirty-day stroke mortality and associated clinical and laboratory factors among adult stroke patients admitted at Mulago Hospital (Uganda). Afr J Neurol Sci. 2014;33(1):79–86.
Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2(1):43–53.
Article Google Scholar
Katsnelson MJ, Della-Morte D, Rundek T. Stroke in the young. Period Biol. 2012;114(3):347–53.
Bandasak R, Narksawat K, Tangkanakul C, Chinvarun Y, Siri S. Association between hypertension and stroke among young Thai adults in Bangkok, Thailand. Southeast Asian J Trop Med Public Health. 2011;42(5):1241–8 PMID: 22299451.
Bhat VM, Cole JW, Sorkin JD, Wozniak MA, Malarcher AM, Giles WH, Stern BJ, Kittner SJ. Dose-response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke. 2008;39(9):2439–43. https://doi.org/10.1161/STROKEAHA.107.510073 . Epub 2008 Aug 14. PMID: 18703815; PMCID: PMC3564048.
Rohr J, Kittner S, Feeser B, Hebel JR, Whyte MG, Weinstein A, Sherwin R. Traditional risk factors and ischemic stroke in young adults: the Baltimore-Washington Cooperative Young Stroke Study. Arch Neurol. 1996;53(7):603–7.
Radhakrishnan K, Ashok PP, Sridharan R, Mousa ME. Stroke in the young: incidence and pattern in Benghazi. Libya. 1986;73(4):434–8.
CAS Google Scholar
Smajlović D, Salihović D, Ibrahimagić OĆ, Sinanović O. Characteristics of stroke in young adults in Tuzla Canton Bosnia and Herzegovina. Coll Antropol. 2013;37(2):515–9.
Tatlisumak, et al. Nontraumatic intracerebral haemorrhage in young adults. Nat Rev Neurol. 2018;14:237–50. https://doi.org/10.1038/nrneurol.2018.17 .
Article PubMed Google Scholar
O’Donnell M, Yusuf S. Risk factors for stroke in Tanzania. Lancet Glob Health. 2013;1:e241–2.
Benjamin LA, Corbett EL, Connor MD, et al. HIV, antiretroviral treatment, hypertension, and stroke in Malawian adults, a case control study. Neurology. 2016;86:324–33. https://doi.org/10.1212/WNL.0000000000002278 .
Article CAS PubMed PubMed Central Google Scholar
Benjamin LA, Bryer A, Emsley HCA, Khoo S, Solomon T, Connor MD. HIV infection and stroke: current perspectives and future directions. Lancet Neurol. 2012;11(10):878–90. https://doi.org/10.1016/S1474-4422(12)70205-3 .
Lammie GA, Hewlett RH, Schoeman JF, Donald PR. Tuberculous cerebrovascular disease: a review. J Infect. 2009;59:156–66.
Berger JR. AIDS and stroke risk. Lancet Neurol. 2004;3:206–7 [PubMed: 15039031].
Nejtek V, Talari D. Novel Risk Factors for TIA and Stroke in Young Adults. 2016.
Folsom AR, Prineas RJ, Kaye SA, Munger RG. Incidence of hypertension and stroke in relation to body fat distribution and other risk factors in older women. Stroke. 1990;21:701–6.
Khan MH, Chakraborty SK, Biswas RSR. High Waist to Hip Ratio as a Risk Factor for Ischemic Stroke Patients Admitted in a Tertiary Care Hospital. Bangladesh J Anat. 2011;9(1):30–4.
JJaakonmäki N, Zedde M, Sarkanen T, Martinez-Majander N, Tuohinen S, Sinisalo J, SECRETO Study Group. Obesity and the risk of cryptogenic ischemic stroke in young adults. J Stroke Cerebrovasc Dis. 2022;31(5):106380.
Rothman SM, Fulling KH, Nelson JS. Sickle cell anemia and central nervous system infarction: a neuropathological study. Ann Neurol. 1986;20:684–90.
O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischemic and intracerebral hemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–23.
Aigner A, Grittner U, Rolfs A, Norrving B, Siegerink B, Busch MA. Contribution of established stroke risk factors to the burden of stroke in young adults. Stroke. 2017;48(7):1744–51.
Kivioja R, Pietilä A, Martinez-Majander N, Gordin D, Havulinna AS, Salomaa V, Putaala J. Risk factors for Early-Onset ischemic stroke: a Case-Control study. J Am Heart Assoc. 2018;7(21):e009774.
Kayima J, Nankabirwa J, Sinabulya I, Nakibuuka J, Zhu X, Rahman M, Kamya MR. Determinants of hypertension in a young adult Ugandan population in epidemiological transition—the MEPI-CVD survey. BMC Public Health. 2015;15(1):1–9.
Download references
Acknowledgements
We acknowledge the patients of Mulago hospital who gave us consent to obtain this information.
This study was funded with funds from the MEPI-Neurology program under Makerere University. The funding project had no role in the design of the study and collection, analysis, and interpretation of data and no role in writing the manuscript.
Author information
Authors and affiliations.
Kiruddu National Referral Hospital, P.O. Box 6553, Kampala, Uganda
Priscilla Namaganda
Mulago National Referral Hospital, Mulago Hospital Complex, P.O. Box 7272, Kampala, Uganda
Jane Nakibuuka
Department of Medicine, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda
Mark Kaddumukasa
Infectious Diseases Institute, Makerere University, Kampala, Uganda
Elly Katabira
You can also search for this author in PubMed Google Scholar
Contributions
PN– conception, design of work, acquisition, analysis, interpretation of data, drafted and substantively revised the manuscript, JN– analysis, interpretation of data, drafted and substantively revised the manuscript, MK – analysis, interpretation of data, drafted and substantively revised the manuscript, EK– design of work, acquisition, analysis, interpretation of data, drafted and substantively revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Priscilla Namaganda .
Ethics declarations
Ethics approval and consent to participate.
Written informed consent/ assent was obtained from all participants or their parent/guardian or legal authorized representative to participate in the study. Ethical approval was obtained from Makerere University, school of medicine research and ethics committee (SOMREC) (reference number #REC REF 2015–105). All methods and procedures were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Namaganda, P., Nakibuuka, J., Kaddumukasa, M. et al. Stroke in young adults, stroke types and risk factors: a case control study. BMC Neurol 22 , 335 (2022). https://doi.org/10.1186/s12883-022-02853-5
Download citation
Received : 18 March 2022
Accepted : 23 August 2022
Published : 06 September 2022
DOI : https://doi.org/10.1186/s12883-022-02853-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Young adults
- Risk factors
BMC Neurology
ISSN: 1471-2377
- General enquiries: [email protected]
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Amani Baidwan, Kendyl Egizi and Alysha Payne
Darrell Jackson, 81 year old male, came to the Emergency Department at Los Robles Hospital by ambulance after he collapsed in a coffee shop. Upon arrival he presented with left sided weakness, facial drooping, and aphasia. He was diagnosed with an ischemic stroke, right humerus head fracture, and right wrist fracture. The priority of care upon initial presentation to the Emergency Department included a CT scan, frequent monitoring of vital signs, starting a peripheral IV, drawing labs, assessing blood glucose, and an EKG. The nurse in the Emergency Department continuously monitored Mr. Jackson’s neurological status, changes in level of consciousness and signs and symptoms of complications.
After much discussion with the family, consent was given for tissue plasminogen activator (tPA). After tPA was given, Mr. Jackson converted to a hemorrhagic stroke, which is one of many risks associated with administration of tPA. He was His computed tomographic scans (CT) revealed intraparenchymal hematoma in both cerebral hemispheres and a large hemorrhage in the left parietal lobe. In the Intensive care Unit, Mr. Jackson was on a ventilator, had a RASS score of -5 and was only responsive to noxious stimuli. Priority in plan of care included airway management and a CPAP trial to begin weaning protocols. The CPAP trial failed, and a tracheostomy was placed. Mr.Jackson was then transferred to the Progressive Care Unit to continue treatment where the NG tube was removed and a PEG tube was inserted. Mr. Jackson has no known allergies and has a history of hypertension, dementia, Parkinson’s disease, stroke, diabetes, GERD, BPH, hypophosphatemia and anemia.
Collaborative interventions are necessary from all healthcare providers, such as physicians, nurses, physical therapy, occupational therapy, speech therapy, case management and social work, to adequate;y care for Mr. Jackson. Case management has been working closely with the family to provide necessary resources to continue care for Mr. Jackson after discharge from the hospital. Mr. Jackson was discharged home with home health after 3 weeks in the hospital. His condition prior to discharge was as follows: A/O x 3 with mild cognitive deficits, speech impairment and left sided weakness.
Discussion Questions
- What is the difference between an ischemic stroke and hemorrhagic stroke?
- What are some of the risk associated with tissue plasminogen activator (tPA) that the nurse would need to assess for and educate the patient about?
- What are some of the psychological needs the nurse should anticipate for a patient who has experienced a stroke?
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Stroke case study
- Sanaya Batcho
- Kara Kitzmiller
- Emma Overman
Our reason for choosing this disorder
Stroke is the leading cause of disability in the United States. As advanced practice nurses, we anticipate caring for those impacted by strokes in many healthcare settings including emergency rooms, acute care, rehab settings, extended care facilities, and in primary care. Early diagnosis and treatment are imperative in the treatment of a stroke in order to minimize permanent deficits so it is important for advanced practice nurses to be proficient in recognizing clinical manifestations of a stroke. There are also many modifiable risk factors for strokes so advanced practice nurses need to be able to educate patients and families on potential lifestyle changes that can decrease stroke risk.
Explore prestigious scientific journals and award and funding opportunities to advance your research.
Access practice-improvement tools, including guidelines, measures, Axon Registry, and practice management resources.
Learn to effectively advocate on behalf of neurologists and their patients, and access AAN position and policy statements.
Not a member? Continue as a nonmember.
Become a Member
By becoming a member of the AAN, you can receive exclusive information to help you at every stage of your career. Benefits include:
- Online education resources at no additional cost
- Discounts on Annual Meeting registration
- Guidelines and publications including Neurology® journal
- A network of 40,000+ neurologists and neuroscience professionals
- The latest research and news affecting neurology
Join Now See All Benefits
Loading... please wait
We’re experiencing unusually high levels of traffic. Thank you for your patience.
Inpatient Stroke Case Studies
Inpatient e/m case studies.
Case study of a stroke patient at varying visit levels to better understand code selection for inpatient encounters under the revised guidelines for 2024.
67-year-old Female with Stroke
Total time* for Inpatient E/M in 2023
Refer to the following tables for correct code selection when billing based on time for inpatient E/M Services:
*Total time includes non face-to-face time on the date of service
Day 1: Critical Care (99291)
A 67-year-old woman with hypertension and diabetes presents to the emergency department with abrupt onset of left hemiparesis 45 minutes ago.
Pre-evaluation : Discussed presentation and vital signs with ED provider (3 mins).
Face-to-face evaluation : Performed medically appropriate history and exam. She has a dense left hemiparesis and an NIH Stroke Scale score of 8. Thrombolysis safety criteria reviewed (7 mins).
Post-evaluation : Non-contrast head CT, CTA of head and neck, and lab results reviewed in the ED. Case discussed with ED provider and thrombolysis recommended. Consultation documented in the ED (25 mins).
Total time : 35 minutes.
Critical Care Coding
According to the 2024 CPT code set, a provider may bill for critical care when the following requirements are met:
- A critical condition: one that acutely impairs a vital organ system with a high probability of imminent or life-threatening deterioration. This includes, for example, central nervous system failure.
- Direct delivery of critical care: high complexity decision-making to assess, manipulate, and support vital systems to treat organ system failure or prevent further life-threatening deterioration.
- At least 30 minutes of time spent solely in the care of the patient. It does not need to be continuous, and it includes both time at the bedside and time spent on the same floor or unit engaged in work directly related to the patient’s care (e.g., documenting critical care, reviewing test results, discussing care with other providers, obtaining history, or discussing treatments or treatment limitations with surrogates when the patient lacks the capacity to do so).
Specific critical care credentials are not required to bill critical care. Critical care is usually provided in a critical care area such as an intensive care unit or emergency department, but this is not always the case (for example, critical care provided to a deteriorating patient in a non-critical care unit).
Other examples of critical care might include:
- Evaluating a patient with status epilepticus and prescribing anti-epileptic drugs or sedative infusions,
- Evaluating a patient with acute respiratory failure from neuromuscular disease and prescribing plasmapheresis,
- Evaluating a patient with coma after cardiac arrest and discussing prognosis, treatment, and goals of care with surrogates (documenting the patient’s lack of capacity to participate)
Critical care, 30-74 minutes CPT 99291 is justified based on the above documentation, although E&M codes (e.g., 99223) associated with fewer wRVUs and lower reimbursement could be used as well.
Day 2: Subsequent Hospital Inpatient Care
Pre-rounds : Reviewed vitals, labs, and studies (LDL, Hemoglobin A1c, EKG, TTE). Review and document independent interpretation of MRI (8 mins).
On Rounds : Performed medically appropriate history and exam. The patient’s symptoms and findings improved somewhat overnight. Patient counseled about stroke evaluation and secondary prevention (10 mins).
Post-rounds : Order atorvastatin, order diabetes consult for management of diabetes. Document discussion with case management possible need for acute inpatient rehabilitation. Documentation completed (10 mins).
Total time : 28 minutes
In this situation, billing according to MDM would be associated with higher reimbursement.
Day 3: Discharge Day Management (By Primary Service)
Pre-rounds : Reviewed vitals, daily CBC and BMP, nursing notes and PT/OT notes (5 mins).
On Rounds : Performed medically appropriate history and exam. The patient reports continued slight improvement in symptoms and requests counseling on how complementary and alternative medicine might help manage her chronic conditions (15 mins).
Post-rounds : Prescribe antiplatelet agent, antidiabetic medications, and antihypertensives. Prepare discharge paperwork and document discharge summary (15 mins).
Total time : 35 minutes
Discharge Day Management Coding (Inpatient or Observation)
Discharge CPTs are selected based on total (face-to-face and non-face-to-face) time, not MDM:
- 99238: 30 minutes or less
- 99239: 31 minutes or more
Discharge CPTs would be used by the primary attending service (e.g., a Neurohospitalist service). Consulting services would continue to choose Subsequent Day codes based on time or MDM.
Discharge Day Management, 31 minutes or more CPT 99239

Tongue Pressure Resistance Training for Post-Stroke Dysphagia: A Case Study
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Get Permissions
- Cite Icon Cite
- Search Site
Sana Smaoui , Melanie Peladeau-Pigeon , Renata Mancopes , Danielle Sutton , Denyse Richardson , Catriona Steele; Tongue Pressure Resistance Training for Post-Stroke Dysphagia: A Case Study. Folia Phoniatr Logop 2024; https://doi.org/10.1159/000538717
Download citation file:
- Ris (Zotero)
- Reference Manager

Article PDF first page preview
ABSTRACT Purpose: The purpose of this study was to explore the effect of a lingual resistance training protocol on the swallowing function of an individual presenting with dysphagia and reduced tongue pressures following a supratentorial ischemic stroke. Methods: A study involving a lingual resistance training protocol with videofluoroscopy to measure outcomes comparing different parameters to ASPEKT normative reference values at three timepoints: baseline (VFSS A), following a 4-week lead-in period to control for spontaneous recovery (VFSS B), and at the 8-week endpoint of treatment (VFSS C). The study was interrupted due to the COVID-19 pandemic after 1 participant enrollment and is presented as single case study. Results: Isometric tongue pressures: Following the 4-week lead-in, a decline in maximum isometric anterior tongue pressure (MAIP) and regular effort saliva swallow pressures (RESS) was noted, however there was no change in maximum posterior isometric tongue pressures (MPIP). Isometric tongue pressures improved post-treatment, with increases in MAIP, MPIP, and to a lesser degree RESS. Swallowing Function: Impairments in swallowing safety continued between the baseline VFSS A (Penetration-Aspiration Scale score [PAS]=8) and lead-in VFSS B (PAS=5). Swallowing safety improved following the intervention, with PAS scores = 1 at the endpoint VFSS C. Pixel-based measures of swallowing efficiency revealed a reduced frequency of post-swallow total pharyngeal reside following the treatment. Improvements were found in two other swallowing parameters, laryngeal vestibule closure integrity and pharyngeal area at maximum pharyngeal constriction, at the endpoint VFSS. Conclusion: These pilot data suggest improvements in some swallowing parameters as an outcome of intervention.
Individual Login
Institutional login.
- Access via Shibboleth and OpenAthens
- Access via username and password
Digital Version
Email alerts, citing articles via, suggested reading.
- Online ISSN 1421-9972
- Print ISSN 1021-7762
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Email: [email protected]
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Student Case Study: Stroke Symptoms
Stroke symptoms.
Neurosomatic Massage therapy Provides Relief for Chronic Stroke Symptoms: A Case Study
Kim Jackman
Background: Stroke is considered a leading cause of adult disability and despite advances in treating stroke, severe disability remains a common outcome. The most prevalent deficit after stroke is hemiparesis of the contralateral upper limb. Common manifestations of upper extremity motor impairment include muscle weakness or contracture, changes in muscle tone, joint laxity, and impaired motor control. Joint subluxation and muscle contractures can also lead to nociceptive musculoskeletal pain. Little information is available on palliative and symptomatic care for post-stroke patients. !
Case Presentation: A 66 year-old female patient in the chronic stages of stroke recovery was treated bi-weekly for five weeks for symptoms related to an ischemic stoke. The patient presented with neck and shoulder pain and fatigue. The Western Ontario Shoulder Index and a Dynamometer were outcome measures for this study. Most treatment centered on reducing hypertonicity of muscles in the cervical region in order to mobilize the atlas and axis to a neutral position. Hot/cold therapy was used with myofascial release, skin rolling, friction w/fiber and x/ fiber, and decompression and mobilization of the atlanto-occiptital/atlanto-axial joint. Massage therapy was administered by a student near the end of her 2nd of 3 semesters in a 1,278 vocational massage therapy program.!
Results: The results indicated that massage therapy improved chronic neck pain and showed a downward trend in relieving shoulder pain as well as indirectly reducing fatigue and risk for future stroke by mobilizing the atlas and axis vertebrae.!
Discussion: Measurements showed a general increase in the impact her shoulder has on her quality of life. However, individual line-items related to the specific areas worked showed a decrease in impact from shoulder related QoL. A longer study with a larger population is needed to show more definitive results.
Cardiovascular safety of using non-steroidal anti-inflammatory drugs for gout: a Danish nationwide case-crossover study
- Observational Research
- Open access
- Published: 06 April 2024
Cite this article
You have full access to this open access article
- Anne Bech-Drewes ORCID: orcid.org/0000-0003-4370-6997 1 , 2 ,
- Kasper Bonnesen 1 , 2 ,
- Ellen-Magrethe Hauge 2 , 3 &
- Morten Schmidt 1 , 2 , 4
Gout attacks are treated with uric-lowering and anti-inflammatory drugs. In patients with gout, non-steroidal anti-inflammatory drugs (NSAIDs) could be both cardiovascular beneficial, due to their anti-inflammatory actions, and cardiovascular hazardous, due to their prothrombotic, hypertensive, and proarrhythmic side effects. We, therefore, examined the risk of cardiovascular events associated with NSAID use in patients with gout. We conducted a nationwide, population-based case-crossover study of all Danes ≥ 18 years of age with first-time gout during 1997–2020, who experienced a cardiovascular event (myocardial infarction, ischemic stroke, congestive heart failure, atrial fibrillation/flutter, or cardiovascular death) ( n = 59,150). The exposure was use of NSAIDs, overall and according to type (ibuprofen, naproxen, or diclofenac). We used the dates 300, 240, 180, and 120 before the outcome date as reference dates. We used the Mantel–Haenszel method to calculate odds ratios (ORs) with 95% confidence intervals (CIs) of the association between NSAID use and cardiovascular events. NSAID use was overall associated with 12% decreased odds of a cardiovascular event (OR = 0.88, 95% CI: 0.85–0.91). This decreased odds ratio was observed for the use of ibuprofen (OR = 0.92, 95% CI: 0.88–0.97) and naproxen (OR = 0.85, 95% CI: 0.74–0.97), but not for the use of diclofenac (OR = 0.97, 95% CI: 0.90–1.05). Overall, use of NSAIDs was associated with decreased odds of all the individual components of the composite outcome. NSAIDs were not associated with an increased cardiovascular event rate when used in gout patients. Ibuprofen and naproxen appeared to have better cardiovascular risk profiles than diclofenac.
Avoid common mistakes on your manuscript.
Introduction
The prevalence of gout ranges from < 1% to 6.8% depending upon the population studied, making it the most common form of inflammatory arthritis globally [ 1 ]. Gout incidence has recently increased in developed countries [ 2 , 3 , 4 ]. For example, in Denmark, the annual incidence of gout increased by almost 80% between 1995 and 2015 [ 4 ]. Gout is characterized by the presence of monosodium urate crystals in joints or synovial fluid [ 3 ] as well as increased uric acid blood levels (hyperuricemia) [ 1 ]. Gout and hyperuricemia are considered cardiovascular risk factors [ 2 ]. Thus, a meta-analysis found an increased risk of myocardial infarction in patients with gout compared with patients without gout (relative risk = 1.22, 95% confidence interval (CI): 1.16–1.26) [ 5 ]. The increased cardiovascular risk in patients with gout might partly be explained by inflammation and oxidative stress, causing atherosclerotic plaque formation [ 6 , 7 ].
The treatment of gout attacks aims at reducing inflammation, which is done with non-steroidal anti-inflammatory drugs (NSAIDs), low-dose colchicine, and/or glucocorticoids [ 8 ]. The treatment should be individualized with co-existing diseases considered [ 8 , 9 ]. NSAID use has been associated with increased cardiovascular risks, even when used for a short period [ 10 ]. This increased risk is thought to be a complex altered equilibrium between cyclooxygenase (COX)-1 and COX-2 inhibition [ 11 , 12 ]. However, in patients with inflammatory conditions, such as gout, the anti-inflammatory effects of NSAIDs might balance out their cardiovascular hazard. This risk–benefit balance is important for clinical decision-making. However, no study has examined NSAID-associated cardiovascular risks in patients with gout. Using patients as their own control in a case-crossover design, we, therefore, examined the cardiovascular event rate associated with NSAID use in patients with gout.
The Danish Health Service offers comprehensive tax-funded health care to both Danish citizens and legal residents. This includes free access to general practitioners and hospitals as well as partial reimbursement for prescribed medications, including NSAIDs [ 13 ]. Upon birth or immigration, all Danish citizens and legal residents receive a unique Civil Personal Registration number [ 13 ]. This system allows individual-level linkage between Danish registries as well as virtually complete long-term follow-up with accurate censoring at emigration or death [ 13 ].
Study design
We conducted a nationwide, population-based case-crossover study of all patients with gout ≥ 18 years of age from January 1, 1996, to December 31, 2020, who experienced a cardiovascular event [ 14 ]. We identified patients with gout through either a primary, in- or outpatient gout diagnosis or through a filling of an allopurinol prescription. The gout diagnoses were identified via the Danish National Patient Registry [ 15 ]. This registry contains nationwide information on non-psychiatric inpatient contacts since 1977, and on psychiatric inpatient as well as all outpatient and emergency contacts since 1995 [ 15 ]. Gout patients who are solely treated by their general practitioner, however, do not have their gout registered in the Danish National Patient Registry [ 15 ]. We, therefore, also identified patients with gout using filled prescriptions for allopurinol from the Danish National Prescription Registry [ 16 ]. Allopurinol has only few FDA-approved indications besides gout [ 17 ], including prevention of recurrent calcium nephrolithiasis in patients with hyperuricosuria, and preventing of tumor lysis syndrome [ 17 ]. The Danish National Prescription Registry contains nationwide information on filled prescriptions from all community pharmacies since 1995 [ 16 ]. Supplementary Table S1 presents all codes used in the study.
The exposures were the use of NSAIDs, both overall and according to type (ibuprofen, naproxen, or diclofenac) identified via filled prescriptions from the Danish National Prescription Registry [ 16 ]. Because this registry does not contain information on the length of treatment or daily dose, we defined NSAID exposure as two tablets per day no matter the dose [ 18 ]. If a patient filled a new prescription for the same NSAID within a use period plus a 14-day grace period, the use period was extended by the number of days provided by the new prescription. If there went more than 14 days after a use period and a new prescription was filled, the new period of use would start on the day the new prescription. The grace period was added to the use period in both situations ( i.e. , prospective filling of gaps) [ 19 ].
The primary outcome was a cardiovascular event defined as a composite of atrial fibrillation/flutter, congestive heart failure, myocardial infarction, ischemic stroke, and cardiovascular death [ 20 ]. The secondary outcomes included the individual cardiovascular diseases [ 20 ]. Cardiovascular events were identified from the Danish National Patient Registry and the main underlying cause of death from the Danish Register of Causes of Death [ 15 ]. Since 1970, The Danish Register of Causes of Death has contained information on the primary underlying cause and any potential contributory cause(s) of deaths [ 21 ].
Covariables
The Comorbidities were identified using in- and outpatient medical history from the Danish National Patient Registry in the 5 years preceding the occurrence of a cardiovascular event. Every hospital discharge from 1977 and each outpatient clinic visit from 1995 onwards is documented in the registry, assigning one primary diagnosis and possibly multiple secondary discharge diagnoses, categorizing according to the International Classification of Diseases, Eighth Revision until the end of 1993 and thereafter the Tenth Revision [ 15 ]. Generally, the positive predictive values for most of the employed comorbidities were found to be high (> 90) [ 22 ]. Comorbidity burden was categorized according to the Danish Index for Acute Myocardial Infarction (DANCAMI) as no (score: 0), low (score: 1–3), moderate (score: 4–5), or severe (score: ≥ 6) [ 23 ].
Comedication use was defined as a filled prescription registered in the Danish National Prescription Registry within 90 days prior to the occurrence of a cardiovascular event. Comedications, such as statins, are employed as an indirect measure of identifying diagnoses like hyperlipidemia. Importantly, the self-control design controls for time-stable confounders by design. Thus, we presume consistent eating and exercise patterns between the event date and the earliest reference date (i.e., 300 days). As patients with cancer might receive allopurinol to prevent tumor lysis syndrome, we defined individuals as having cancer-related gout if they had either received a cancer diagnosis or filled a prescription for an antineoplastic agent in the 5 years before their gout diagnosis. Table 1 contains the identified comorbidities and comedications.
Statistical analyses
We present continuous variables as medians with interquartile ranges and categorical variables as numbers with percentages. In our self-controlled design, we compared, among individuals expiring a cardiovascular event, the number of individuals using NSAIDs at the day of the event but not at a reference date with the number of individuals using NSAIDs at a reference date, but not at the event date (Fig. 1 ) [ 18 , 24 ]. We used the Mantel–Haenszel method to calculate odds ratios (ORs) with 95% confidence intervals (CIs) of the association between NSAID use and a cardiovascular event [ 24 , 25 ]. As previously applied, we used the dates 300, 240, 180, and 120 before the outcome date as reference dates [ 18 ]. By using fixed outcome and reference dates, rather than fixed windows stacked backwards in time from the outcome and reference dates, we allowed for flexibility when assigning the exposure length after a filled prescription. By having a 120-day gap between the last reference date and the outcome date, compared with only a 60-day gap between the individual reference dates, we secured a 60-day washout window [ 26 ]. As everyone serves as their own control, the self-control design controls for confounding by time-stable variables, such as genetics, by design.
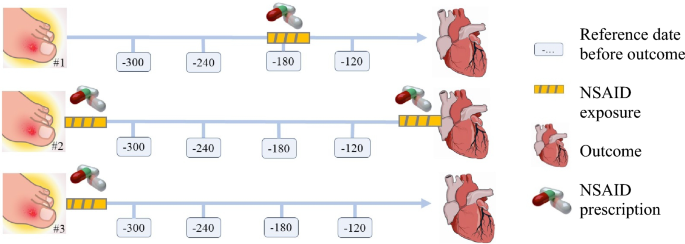
The case-crossover study design. The self-controlled design compares, among individuals experiencing an outcome, the number of individuals exposed to NSAID use at the outcome date, but not at any reference date, with the number of individuals exposed at a reference date, but not at the outcome date. Patient #1 is exposed at the second reference point from the outcome. Patient #2 is exposed at the outcome date. Patient #3 is not exposed at any reference day or outcome date and is dropped from the analysis. Using Mantel–Haenszel method, the odds ratios of being exposed on the outcome date vs. the reference date is calculated by dividing the first pattern with the second pattern
We performed the analyses within subgroups according to sex, age, comorbidity burden, cancer-related gout, and whether gout was identified via a diagnosis or via a filled allopurinol prescription. All analyses were performed using Stata version 17.0 (StataCorp LLC, College Station, TX, USA).
Patient characteristics
We identified 59,150 individuals with either a first-time gout diagnosis (12%) or a filled allopurinol prescription (88%) who experienced a cardiovascular event during follow-up from 1996 to 2020 (Fig. 2 ). The time from gout diagnosis to a cardiovascular event differed whether gout was identified via a diagnosis (median = 924 days, interquartile range: 279–2167) or via a filled allopurinol prescription (median = 1373 days, interquartile range: 462–3032). The average number of filled allopurinol prescriptions in the study period were 13 (median = 5, interquartile range: 2–16). Among the included patients with gout, 68% were males, their median age was 72 years (interquartile range: 62–79), 29% had no comorbidity burden, 27% had a severe comorbidity burden and 8.9% had gout in relation to cancer (Table 1 ). The most common comorbidities were hypertension (38%), other inflammatory diseases (19%), degenerative rheumatic disease (18%), diabetes (16%), chronic pulmonary disease (15%) and chronic kidney disease (9%). The most used drugs were diuretics (52%), beta-blockers (32%), and antiplatelets (29%).
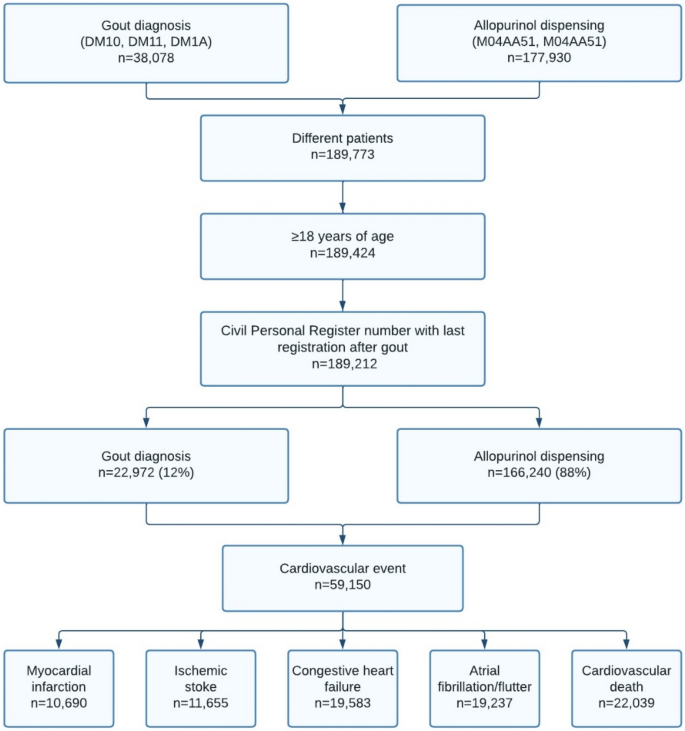
Flowchart of the study populations, 1996–2020
Cardiovascular risks
Compared with when not using NSAIDs, slightly decreased odds of a cardiovascular event were found for use of NSAIDs overall (OR = 0.88, 95% CI: 0.85–0.91), ibuprofen (OR = 0.92, 95% CI: 0.88–0.97), and naproxen (OR = 0.85, CI: 0.74–0.97) (Fig. 3 ). Use of diclofenac was not associated with a cardiovascular event (OR = 0.97, 95% CI: 0.90–1.05).
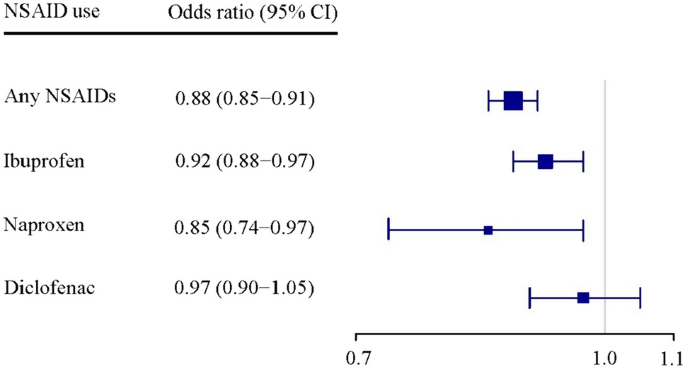
Non-steroidal anti-inflammatory drugs (NSAIDs) and adverse cardiovascular events in patients with gout. Number of disconcordant pairs: 13,564 for any NSAID, 7,658 for ibuprofen, 988 for naproxen, 3,152 for diclofenac. Adverse cardiovascular event is a composite of myocardial infarction, ischemic stroke, congestive heart failure, atrial fibrillation or flutter, and cardiovascular death
Compared with when not using NSAIDs, use of any NSAID was associated with decreased odds of all secondary outcomes, i.e. , myocardial infarction (OR = 0.91, 95% CI: 0.84–0.99), ischemic stroke (OR = 0.88, 95% CI: 0.81–0.95), congestive heart failure (OR = 0.89, 95% CI: 0.83–0.94), atrial fibrillation/flutter (OR = 0.80, 95% CI: 0.75–0.85), and cardiovascular death (OR = 0.60, 95% CI: 0.56–0.65) (Table 2 ). Regarding the type of NSAID, compared with when not using NSAIDs, ibuprofen use was associated with a decreased odds of ischemic stroke (OR = 0.86, 95% CI: 0.77–0.96), atrial fibrillation/flutter (OR = 0.82, 95% CI: 0.75–0.90), and cardiovascular death (OR = 0.67, 95% CI: 0.61–0.74). Naproxen use was associated with a decreased odds of cardiovascular death (OR = 0.53, 95% CI: 0.40–0.71). Diclofenac use was associated with a decreased odds of atrial fibrillation/flutter (OR = 0.83, 95% CI: 0.71–0.96) and cardiovascular death (OR = 0.87, 95% CI: 0.76–0.99) (Table 2 ).
Subgroup analyses
The results remained robust after stratifying by sex (Table 3 ). Interpretation of the age- and comorbidity-stratified results were limited due to low precision (Table 3 ). Compared with a period when not using NSAIDs, use of any NSAIDs was associated with a decreased risk of cardiovascular events when restricting to patients without previous cancer (OR = 0.87, 95% CI: 0.84–0.90) (Table 3 ). The results did not differ notably according to whether gout was defined via a hospital diagnosis or via a filled allopurinol prescription (Table 3 ).
This study examined the cardiovascular risks associated with NSAID use among patients with a first-time gout attack. Our findings indicate that the overall use of NSAIDs in patients with gout was not associated with an increased risk of adverse cardiovascular events. This finding supports the current clinical practice of treating gout with NSAIDs. In fact, the use of particularly ibuprofen and naproxen were linked to a slightly reduced risk of adverse cardiovascular events compared with non-use and, therefore, seem preferable to diclofenac. These results remained robust for various cardiovascular outcomes.
Previous literature
Chronic inflammation has been associated with up to a 70% increased risk of cardiometabolic disorders [ 27 ]. Gout is characterized by low-grade inflammation, which leads to elevated levels of reactive oxygen species, proinflammatory cytokines, endothelial dysfunction, formation of neutrophil extracellular traps, and platelet hyperactivity. All of these factors may contribute to the development of atherosclerosis [ 28 ]. Additionally, hyperuricemia in patients with gout can cause oxidative stress, further damaging the endothelia [ 28 ]. Accordingly, a self-controlled study found that individuals with gout, who experienced a cardiovascular event, had twice the likelihood of having a gout flare in the days leading up the event, indicating that gout flares are linked to a temporary rise in cardiovascular risk [ 29 ]. Moreover, patients with inflammatory diseases are at higher cardiovascular risk due to the presence of traditional risk factors such as sex, hypertension, diabetes, smoking, and others [ 28 ].
Both randomized controlled trials and observational studies have provided evidence that NSAIDs increase the risk of cardiovascular events in general even for short treatment periods and low doses [ 11 , 12 , 18 , 30 ], but data have been lacking in gout patients whose chronic inflammation may alter the risk–benefit balance. We did not find an increased odds of cardiovascular events when using NSAIDs in patients with gout. While the exact mechanism of the neutral or slightly beneficial effect of NSAID use in patients with gout remains unknown, we speculate that it relates to the anti-inflammatory properties of NSAIDs [ 6 , 7 ]. Blocking a central mediator in the inflammation of gout patients (NLRP3 inflammasome) prevents cardiovascular events by activating the cytokine interleukin-1β, which affects the development of atherothrombotic plaques [ 27 , 31 ]. Furthermore, it has been shown that, if left untreated, gout is associated with a two-fold increased risk of coronary heart disease, but treated (allopurinol, colchicine, sulfinpyrazone) the prognosis is comparable to the general population [ 32 ]. These results correspond with the decreased cardiovascular risk associated with NSAID use at time of the event found in our study. Finally, our findings also support previous literature suggesting a more favorable cardiovascular risk profile for the nonselective NSAIDs ibuprofen and naproxen than for the COX-2 selective diclofenac [ 12 ].
Strengths and limitations
The large cohort of patients with frequent use of NSAIDs increased precision and allowed for examinations of associations on individual NSAIDs.
The free access to health care and the virtually complete long-term follow-up reduced the risk of selection bias from selective inclusion of health insurance systems, specific hospitals, or age groups. Using a filled allopurinol prescription, it was possible to locate further cases not diagnosed at a hospital. However, this may also present limitations as it is possible that we have included patients who were treated with allopurinol for other conditions than gout such as tumor lysis syndrome. However, the number treated with allopurinol for such diseases is likely small due to few indications [ 17 ], resulting in only a few non-gout patients included in the study. Even though the study by design only included patients with gout who suffered a cardiovascular event, the study results are considered relevant for gout attacks in general.
As the Danish National Prescription Registry lacks information on in-hospital NSAID use and over-the-counter NSAID sales, we might have misclassified in-hospital NSAID users or over-the-counter ibuprofen users as non-users [ 33 ]. However, in-hospital NSAID use is limited, and during the study period, ibuprofen was the only NSAID available over the counter, constituting approximately 15–25% of total NSAID sales [ 33 ]. This potential misclassification of NSAID, therefore, cannot noteworthy bias effect estimates of the association between NSAID use and cardiovascular events [ 34 ]. Coding of the gout diagnosis has not been validated in the Danish National Patient Registry [ 15 ]. However, we aligned the codes with recommendations from rheumatologists about current and previous coding practices of gout in the hospital setting. To increase completeness, we also identified patients through filled allopurinol prescriptions, which have few indications besides gout . The cardiovascular diagnosis has been validated with a positive predictive value of around 90% for myocardial infarction and ischemic stroke, 80% for heart failure, and 95% for atrial fibrillation [ 35 , 36 ]. Mortality data are complete and accurate [ 13 ].
Even though the self-controlled design is robust to confounding by time-stable co-variables, it may be influenced by time-varying co-variables such as disease severity. The design is further prone to confounding-by-indication, if the patients would use NSAIDs for conditions associated with the outcome (for example using NSAIDs to treat angina). However, the consistency in the results of the individual outcomes indicates that this cannot explain the finding of no increased risk overall.
In patients with gout, we found that NSAID use was not associated with increased cardiovascular risks at the time of a first gout attack. Furthermore, the use of ibuprofen or naproxen seemed to be associated with a lower cardiovascular risk than diclofenac. This information may be taken into consideration when selecting NSAIDs for patients with gout.
Data availability
Not allowed.
Dehlin M, Jacobsson L, Roddy E (2020) Global epidemiology of gout: prevalence, incidence, treatment patterns and risk factors. Nat Rev Rheumatol 16(7):380–390. https://doi.org/10.1038/s41584-020-0441-1
Article PubMed Google Scholar
Kuo CF, Grainge MJ, Zhang W, Doherty M (2015) Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol 11(11):649–662. https://doi.org/10.1038/nrrheum.2015.91
Neogi T, Jansen TL, Dalbeth N, Fransen J, Schumacher HR, Berendsen D et al (2015) Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 74(10):1789–1798. https://doi.org/10.1136/annrheumdis-2015-208237
Article CAS PubMed Google Scholar
Zobbe K, Prieto-Alhambra D, Cordtz R, Hojgaard P, Hindrup JS, Kristensen LE et al (2019) Secular trends in the incidence and prevalence of gout in Denmark from 1995 to 2015: a nationwide register-based study. Rheumatology (Oxford) 58(5):836–839. https://doi.org/10.1093/rheumatology/key390
Schieir O, Tosevski C, Glazier RH, Hogg-Johnson S, Badley EM (2017) Incident myocardial infarction associated with major types of arthritis in the general population: a systematic review and meta-analysis. Ann Rheum Dis 76(8):1396–1404. https://doi.org/10.1136/annrheumdis-2016-210275
Golia E, Limongelli G, Natale F, Fimiani F, Maddaloni V, Pariggiano I et al (2014) Inflammation and cardiovascular disease: from pathogenesis to therapeutic target. Curr Atheroscler Rep 16(9):435. https://doi.org/10.1007/s11883-014-0435-z
Pagidipati NJ, Clare RM, Keenan RT, Chiswell K, Roe MT, Hess CN (2018) Association of gout with long-term cardiovascular outcomes among patients with obstructive coronary artery disease. J Am Heart Assoc 7(16):e009328. https://doi.org/10.1161/JAHA.118.009328
Article PubMed PubMed Central Google Scholar
Mikuls TR (2022) Gout. N Engl J Med 387(20):1877–1887. https://doi.org/10.1056/NEJMcp2203385
Stamp LK, Dalbeth N (2022) Critical appraisal of serum urate targets in the management of gout. Nat Rev Rheumatol 18(10):603–609. https://doi.org/10.1038/s41584-022-00816-1
Schjerning Olsen AM, Fosbøl EL, Lindhardsen J, Folke F, Charlot M, Selmer C et al (2011) Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study. Circulation 123(20):2226–2235. https://doi.org/10.1161/circulationaha.110.004671
Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA et al (2007) Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American heart association. Circulation 115(12):1634–1642. https://doi.org/10.1161/CIRCULATIONAHA.106.181424
McGettigan P, Henry D (2011) Cardiovascular risk with non-steroidal anti-inflammatory drugs: systematic review of population-based controlled observational studies. PLoS Med 8(9):e1001098. https://doi.org/10.1371/journal.pmed.1001098
Article CAS PubMed PubMed Central Google Scholar
Schmidt M, Pedersen L, Sørensen HT (2014) The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol 29(8):541–549. https://doi.org/10.1007/s10654-014-9930-3
Petersen I, Douglas I, Whitaker H (2016) Self controlled case series methods: an alternative to standard epidemiological study designs. BMJ 354:i4515. https://doi.org/10.1136/bmj.i4515
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT (2015) The Danish national patient registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490. https://doi.org/10.2147/CLEP.S91125
Pottegard A, Schmidt SAJ, Wallach-Kildemoes H, Sorensen HT, Hallas J, Schmidt M (2017) Data resource profile: the Danish national prescription registry. Int J Epidemiol. https://doi.org/10.1093/ije/dyw213
Qurie A, Preuss CV, Musa R. Allopurinol. StatPearls. Treasure Island (FL) 2023.
Bonnesen K, Pedersen L, Ehrenstein V, Gronkjaer MS, Sorensen HT, Hallas J et al (2023) Impact of lifestyle and socioeconomic position on the association between non-steroidal anti-inflammatory drug use and major adverse cardiovascular events: a case-crossover study. Drug Saf 46(6):533–543. https://doi.org/10.1007/s40264-023-01298-0
Pazzagli L, Linder M, Zhang M, Vago E, Stang P, Myers D et al (2018) Methods for time-varying exposure related problems in pharmacoepidemiology: an overview. Pharmacoepidemiol Drug Saf 27(2):148–160. https://doi.org/10.1002/pds.4372
Bhala N, Emberson J, Merhi A, Abramson S, Arber N, Baron JA et al (2013) Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet 382(9894):769–779. https://doi.org/10.1016/s0140-6736(13)60900-9
Helweg-Larsen K (2011) The Danish register of causes of death. Scand J Public Health 39(7 Suppl):26–29. https://doi.org/10.1177/1403494811399958
Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sørensen HT (2011) The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish national registry of patients. BMC Med Res Methodol 11:83. https://doi.org/10.1186/1471-2288-11-83
Wellejus Albertsen L, Heide-Jorgensen U, Schmidt SAJ, Grey C, Jackson R, Sorensen HT et al (2020) The Danish comorbidity index for acute myocardial infarction (DANCAMI): development, validation and comparison with existing comorbidity indices. Clin Epidemiol 12:1299–1311. https://doi.org/10.2147/CLEP.S277325
Hallas J, Pottegård A (2014) Use of self-controlled designs in pharmacoepidemiology. J Intern Med 275(6):581–589. https://doi.org/10.1111/joim.12186
Maclure M (1991) The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 133(2):144–153. https://doi.org/10.1093/oxfordjournals.aje.a115853
Mittleman MA, Maclure M, Robins JM (1995) Control sampling strategies for case-crossover studies: an assessment of relative efficiency. Am J Epidemiol 142(1):91–98. https://doi.org/10.1093/oxfordjournals.aje.a117550
Dregan A, Chowienczyk P, Molokhia M (2017) Cardiovascular and type 2 diabetes morbidity and all-cause mortality among diverse chronic inflammatory disorders. Heart 103(23):1867–1873. https://doi.org/10.1136/heartjnl-2017-311214
Hansildaar R, Vedder D, Baniaamam M, Tausche AK, Gerritsen M, Nurmohamed MT (2021) Cardiovascular risk in inflammatory arthritis: rheumatoid arthritis and gout. Lancet Rheumatol 3(1):e58–e70. https://doi.org/10.1016/S2665-9913(20)30221-6
Cipolletta E, Tata LJ, Nakafero G, Avery AJ, Mamas MA, Abhishek A (2022) Association between gout flare and subsequent cardiovascular events among patients with gout. JAMA 328(5):440–450. https://doi.org/10.1001/jama.2022.11390
Schmidt M, Sorensen HT, Pedersen L (2018) Diclofenac use and cardiovascular risks: series of nationwide cohort studies. BMJ 362:k3426. https://doi.org/10.1136/bmj.k3426
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C et al (2017) Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 377(12):1119–1131. https://doi.org/10.1056/NEJMoa1707914
Krishnan E, Pandya BJ, Lingala B, Hariri A, Dabbous O (2012) Hyperuricemia and untreated gout are poor prognostic markers among those with a recent acute myocardial infarction. Arthritis Res Ther 14(1):R10. https://doi.org/10.1186/ar3684
Schmidt M, Hallas J, Friis S (2014) Potential of prescription registries to capture individual-level use of aspirin and other nonsteroidal anti-inflammatory drugs in Denmark: trends in utilization 1999–2012. Clin Epidemiol 6:155–168. https://doi.org/10.2147/CLEP.S59156
Gaster N, Hallas J, Pottegard A, Friis S, Schmidt M (2021) The Validity of Danish prescription data to measure use of aspirin and other non-steroidal anti-inflammatory drugs and quantification of bias due to non-prescription drug use. Clin Epidemiol 13:569–579. https://doi.org/10.2147/CLEP.S311450
Johnsen SP, Overvad K, Sorensen HT, Tjonneland A, Husted SE (2002) Predictive value of stroke and transient ischemic attack discharge diagnoses in the Danish national registry of patients. J Clin Epidemiol 55(6):602–607. https://doi.org/10.1016/s0895-4356(02)00391-8
Sundbøll J, Adelborg K, Munch T, Frøslev T, Sørensen HT, Bøtker HE et al (2016) Positive predictive value of cardiovascular diagnoses in the Danish national patient registry: a validation study. BMJ Open 6(11):e012832. https://doi.org/10.1136/bmjopen-2016-012832
Download references
Open access funding provided by Aarhus University Hospital. For this article, the author(s) disclosed receipt of the following financial support for the authorship, research, or/and publication. Anne Bech-Drewes, Kasper Bonnesen and Morten Schmidt are supported by the Novo Nordic Foundation (grant NNF190C0054908). The funding sources had no role in the design, conduct, analysis, or reporting of the study.
Author information
Authors and affiliations.
Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark
Anne Bech-Drewes, Kasper Bonnesen & Morten Schmidt
Department of Clinical Medicine, Aarhus University, Olof Palmes Allé 43, 8200, Aarhus, Denmark
Anne Bech-Drewes, Kasper Bonnesen, Ellen-Magrethe Hauge & Morten Schmidt
Department of Rheumatology, Aarhus University Hospital, Aarhus, Denmark
Ellen-Magrethe Hauge
Department of Cardiology, Gødstrup Regional Hospital, Aarhus, Denmark
Morten Schmidt
You can also search for this author in PubMed Google Scholar
Contributions
The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. All authors take full responsibility for the integrity and accuracy of all aspects of the work.
Corresponding author
Correspondence to Anne Bech-Drewes .
Ethics declarations
Conflict of interest.
The authors declared no potential conflict of interest concerning the authorship, research, or/and publication of this article. There is no competing interests to declare.
Related congress abstract publications
Abstract for poster presentation at ESC 2023: AM Drewes, K Bonnesen, EM Hauge, M Schmidt. Cardiovascular safety of non-steroidal anti-inflammatory drug use for gout: A Danish nationwide case-crossover study. European Heart Journal, volume 44, issue supplement_2, November 2023, ehad655.2789, http://doi.org/ https://doi.org/10.1093/eurheartj/ehad655.2789 . Abstract 545 for poster presentation at ICPE 2023: AM Drewes, M Schmidt, K Bonnesen, EM Hauge. Cardiovascular safety of non-steroidal anti-inflammatory drug use for gout: A Danish nationwide case-crossover study. Pharmacoepidemiology and Drug Safety, volume 32, issue S1, p. 3–612, 12 October 2023, https://doi.org/ https://doi.org/10.1002/pds.5687 .
Data permission and ethical committee approval
The study was reported to the Danish Data Protection Agency through institutional registration (record number 2014–54-0922, Aarhus University record number 2016–051-000001–811). No ethical committee approval was needed.
Previously online posted pre-publication
The manuscript and the data are not submitted or published elsewhere.
Transparency declaration
The authors affirm that the manuscript is an accurate, honest and transparent account of the study being reported. No aspect of the study has been omitted. Any discrepancies from the study as planned have been explained.
Patient involvement statement
No patient involvement.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 23 kb)
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Bech-Drewes, A., Bonnesen, K., Hauge, EM. et al. Cardiovascular safety of using non-steroidal anti-inflammatory drugs for gout: a Danish nationwide case-crossover study. Rheumatol Int (2024). https://doi.org/10.1007/s00296-024-05584-7
Download citation
Received : 08 January 2024
Accepted : 13 March 2024
Published : 06 April 2024
DOI : https://doi.org/10.1007/s00296-024-05584-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cardiovascular disease
- Non-steroidal anti-inflammatory drugs
- Case-crossover study
- Find a journal
- Publish with us
- Track your research
Influenza Vaccines Linked to Elevated Stroke Risk in Elderly: FDA Study

Some people who received a COVID-19 vaccine were at higher risk of stroke but an analysis found that the risk was connected to influenza vaccination, U.S. Food and Drug Administration (FDA) researchers said in a new study.
The researchers, analyzing data from Medicare, detected an elevated stroke risk among the elderly following receipt of a bivalent COVID-19 vaccine made by Pfizer and Moderna and available from the fall of 2022 to the fall of 2023. There was an elevated risk of nonhemorrhagic stroke or transient ischemic attack in people 85 or older following Pfizer vaccination and people aged 65 to 74 following Moderna vaccination, the researchers found.
But the researchers then looked at which people received an influenza shot at the same time as a COVID-19 shot and saw that the elevated risk only persisted among people who received the vaccines concomitantly.
“This finding suggests that the observed association between vaccination and stroke in the concomitant subgroup was likely driven by a high-dose or adjuvanted influenza vaccination,” Steven Anderson, director of the Office of Biostatistics and Epidemiology at the FDA, and the other researchers wrote.
High-dose influenza vaccines are primarily for the elderly, while adjuvanted influenza vaccines are another type of flu shot.
The researchers also found an elevated risk of nonhemorrhagic stroke among people who received an influenza vaccine and did not get a COVID-19 vaccine, supporting the finding.

“The clinical significance of the risk of stroke after vaccination must be carefully considered together with the significant benefits of receiving an influenza vaccination,” the researchers said, adding later that “more studies are needed to better understand the association between high-dose or adjuvanted influenza vaccination and stroke.”
Limitations include the exclusion of cases with COVID-19 in the 30 days prior to stroke as well as the restriction of the study to vaccinated people. The method researchers used, a self-controlled case series, used vaccinated people as both the primary group and the control group. Researchers counted strokes that occurred within 42 days of vaccination as being possibly linked to vaccination and strokes that happened between 43 days and 90 days after vaccination as unrelated to vaccination.
The paper included stroke cases between Aug. 31, 2022, and January or February 2023, depending on the type of stroke. After exclusions, 11,001 stroke cases were included.
The only conflicts of interest listed by the researchers were that some of them work for Acumen. The paper was funded by the FDA through an agreement for which Acumen is the contractor. “The FDA played a role in the design and conduct of the study; interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The FDA did not play a role in the collection, management, or analysis of the data,” according to the study.
Previous Findings
The CDC later said data from the system suggested the elevated risk stemmed from receiving an influenza vaccine with a COVID-19 shot.
French researchers have said they examined whether receipt of a bivalent vaccine was linked to a higher rate of stroke and other cardiovascular events than the old vaccine versions and found that receipt of the former was actually linked to a lower rate.
Rep. Boebert to Appear on Top of Primary Ballot in New Race

Judge Berates DOJ for Defying Congressional Subpoenas

Europe Warns of ‘Lack of Immune Defenses’ Among Humans If Bird Flu Changes

RFK Jr. Says He'll Appoint Special Prosecutor to Investigate Jan 6 Prosecutions

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Neurol
Acute Ischemic Stroke in COVID-19: A Case-Based Systematic Review
Tissa wijeratne.
1 Neurology & Stroke, Australian Institute for Musculoskeletal Science, Melbourne Medical School, Sunshine Hospital, The University of Melbourne, Parkville, VIC, Australia
2 School of Psychology and Public Health, College of Science, Health and Engineering, La Trobe University, Melbourne, Parkville, VIC, Australia
3 Department of Medicine and Dean's Office, Rajarata University of Sri Lanka, Anuradhapura, Sri Lanka
Carmela Sales
4 Department of Neurology, Australian Institute for Musculoskeletal Science, Level Three, Western Centre for Health Research and Education, Sunshine Hospital, Western Health & University Melbourne, St Albans, VIC, Australia
Leila Karimi
5 Faculty of Social and Political Sciences, Tbilisi State University, Tbilisi, Georgia
Sheila Gillard Crewther
Corona virus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus2 (SARS-CoV-2) is recognized as a global pandemic by WHO 2020 with 5,934 936 infections, 367,166 deaths and affecting over 200 countries as of 30th May 2020. Acute Ischemic Stroke (AIS) in brain is also emerging as an important neurovascular/neurological complication of COVID-19, associated with extreme immune responses leading to dysregulated coagulation system and generalized thrombo-embolic status and increased risk of AIS especially among usually less vulnerable younger adults in this cohort. Thus, in early June 2020, we aimed to review the clinical data on all published cases of COVID-19 and concomitant AIS, with a view to understanding the pertinent clinical, laboratory and imaging features. The neutrophil-lymphocyte ratio (NLR) at time of hospital admission for COVID infection correlates positively with the duration of time before onset of clinical features of AIS. Higher NLR, C-Reactive protein, serum ferritin, D-dimer and fibrinogen levels are associated with poor prognosis of AIS in COVID-19 with 75% of patients dying or being severely disabled at present. Currently it is too early to comment on the long-term outcomes for survivors.
Key Findings
- Acute ischemic stroke is an important, but an under recognized complication of SARS-CoV2 infection, that leaves most recovered patients with significant disabilities as of present stage July 2020 of the pandemic.
- Hypercoagulation markers such as D-dimer are substantially elevated among all patients early in the disease progression.
- Neutrophil to lymphocyte ratio, C-Reactive protein, and Serum Ferritin levels appear to be prognostic markers.
- Patients with higher admission neutrophil-lymphocyte ratios demonstrate a shorter interval between infective symptoms of COVID-19 and the clinical manifestation of Acute Ischemic Stroke.
- Large vessel occlusion is the main etiologic subtype, with only a minority of patients receiving standard of care treatment.
- Seventy five percent of the patients with COVID-19 and Acute Ischemic Stroke died or are still severely disabled.
- The COVID-19 pandemic has created a unique opportunity to advance the whole field of neurorehabilitation based on a better biological and scientific underpinning of precision neurorehabilitation protocols.
Introduction
In December 2019, a novel corona virus associated with a series of acute, atypical respiratory diseases was first detected in Wuhan China. Since then the virus, now known as SARS-CoV2 (Severe Acute Respiratory Syndrome coronavirus two), has spread to over 200 countries and is now recognized as a major world pandemic ( 1 ). As of May 30th 2020, the mortality rate of COVID-19 was reported with the number of confirmed deaths with recorded cases worldwide. Since the pathogenesis of SARS-CoV2 first began to emerge, numerous other clinical system manifestations have been identified.
Neurological manifestations of SARS-CoV 2 infection were first reported in a series of patients in Wuhan, China by Zhou et al. ( 2 ). Acute ischemic stroke (AIS) was diagnosed in 5% of the cases ( 2 ). However, a much lower rate of only 0.9% imaging confirmed AIS i.e., 32/3,556 total patients case number with COVID-19 was reported in New York USA ( 3 ). Subsequent retrospective reports from Europe have also confirmed AIS as a common neurovascular complications of SARS-CoV2 ( 4 , 5 ). Interestingly Oxley et al. noted an increased occurrence of younger SARS CoV2 virus-infected patients with no significant traditional risk factors for AIS, presenting with large vessel occlusion ( 6 ). Putative mechanisms suggested as inducing AIS in association with SARS CoV2 have included systemic inflammation, inflammatory cytokine storm, hyper-coagulability, and imbalances in the classical and alternative Renin Angiotensin System (RAS) in relation to SARS-CoV-2 spike glycoprotein-ACE2 binding related molecular mechanisms ( 3 , 7 – 19 ). The RAS system comprises both a plasma-based RAS regulating cardiovascular system and tissue-based RAS regulating long term changes via a complex hormonal system, endocrine, paracrine, and autocrine in action. Thus, the RAS controls renal, adrenal and cardiovascular systems with important implications on blood pressure control as well as fluid/electrolyte control which are critically important to maintain life being very susceptible to damage by SARS-CoV 2. The inflammatory pathway is core to the various clinical manifestations of SARS-CoV2 infection. Also referred to as the “cytokine storm,” it triggers an upsurge of various inflammatory cytokines such as IL-2, IL-7, IL-10 ( 20 , 21 ), induces a state of lymphocytopenia ( 22 – 24 ) and also activates a spike of acute phase reactants such as CRP and ferritin ( 25 , 26 ).
Various parameters have been proposed to predict prognosis and outcomes among patients with COVID, including the neutrophil to lymphocyte ratio (NLR) ( 27 – 30 ). A metanalysis of six studies involving 1,141 patients has demonstrated that an elevated NLR is associated with severe disease manifestation ( 28 ). The same meta-analysis has also revealed that along with ESR and IL-6, CRP was correlated with increased severity among patients with SARS-CoV2 infection ( 28 ). The role of ferritin as a predictor of mortality among confirmed SARS-CoV2, has also been confirmed in another metanalysis of 10 studies involving more than 1,400 subjects ( 31 ). Furthermore, elevated D-dimer and hyperfibrinogenemia, which are both biomarkers of inflammation and hypercoagulable state, have also been shown to predict the severity of the said infection ( 31 , 32 ). Interestingly, similar biomarkers predict outcomes in stroke ( 33 – 39 ). In particular, it is known that patients who show elevated NLR, ferritin, CRP, D-dimer and fibrinogen have a higher risk for stroke and equate to potentially poorer clinical outcomes ( 33 – 39 ).
To date, despite the theoretical association of inflammatory and procoagulable states linking stroke and SARS-CoV2 infection, there is limited published literature on the actual co-occurrence of both. There is also limited information on the biological markers which may be associated with poor neurological outcomes. Thus, this study aims to describe the clinical characteristics of patients with acute ischemic stroke and concomitant SARS-CoV2 infection. By further analysis of available laboratory data, this will look at the trend of inflammatory biomarkers such as NLR, CRP, serum ferritin, fibrinogen and D-dimer and hospital discharge outcomes.
Currently, there is limited information about the clinical characteristics and specific neurorehabilitation issues of AIS patients with SARS-CoV 2 infection ( 40 – 43 ). However, it is expected that the surge in patient numbers, on-going issues with personal protective equipment (PPE) shortages, and associated health care workers anxiety and stress about the potential of getting infected with COVID-19 (and actual infection of health care workers and mandatory self isolation for 14 days even if these members are demonstrating minimum or no symptoms) will create a significant challenge to traditional neurorehabilitation practices and pathways, at least during the pandemic, possibly for a long time to come. Thus, these circumstances argue a strong case for converting the catastrophe [Complex rearrangement of hospital facilities as part of the preparation for the pandemic has also occasioned significant problems and added resource problems for health care systems across the world ( 44 – 50 ) into an opportunity for revamping of rehabilitation protocols]. Currently evidence is emerging for further expansion of telemedicine type paradigms, with incorporation of tablet based remote monitoring technology (Melbourne Rapid Field visual fields, wearable devices and artificial intelligence) suggesting as the way forward in neurorehabilitation of AIS in COVID19 pandemic era, at least for the foreseeable future ( 43 , 51 – 53 ).
Thus, this systematic review aims to identify and collate the clinical and laboratory features, acute and long term treatment, and outcomes of all published reports on patients with concomitant diagnosis of confirmed SARS-CoV 2 infection and acute ischemic stroke and with a special emphasis on clinical and laboratory features.
The present study was conducted to provide a systematic review of AIS and COVID-19 with respect to definition, prevalence, pathophysiology, clinical characteristics, acute, subacute features, prognostic markers outcomes.
Participants
Information regarding ischemic stroke patients with confirmed SARS-CoV2 infection and radiologically or clinically Confirmed AIS included in published studies from November 2019 to May 30th 2020 using the search strategy detailed below will be considered here.
Types of Studies
All types of studies including qualitative, systematic reviews, meta-analyses, case reports and case series, were included.
Search Methods
Published articles in English and on human subjects that were published from November 2019 until 30th May 2020 were the inclusion criteria for the search. The following search strategy was adopted:
- In the first step MEDLINE, Cochrane and CINAHL databases were searched, followed by title and abstract search.
- In the second step, the keywords were used when searching on Ovid MEDLINE, Cochrane, PubMed, CINAHL, and EMBASE databases.
- In the third step, a manual search was carried out to ensure no study was inadvertently left out.
The keywords used to conduct the search were: Stroke, thrombosis, coronavirus, neurological complication, neurorehabilitation, COVID19, SARS-COV2.
Data Extraction
The Arksey and O'Malley methodological framework was employed in this review ( 54 ).
The bibliographies of individual studies were further hand-searched. Articles were screened by two independent investigators.
4. In the fourth step the secondary analysis was carried out as follows.
Clinical and laboratory data of every patient was extracted. Demographics and details of their respective laboratory details were also investigated. In particular, the following routine laboratory values were of interest to the researchers: NLR, CRP, ferritin, fibrinogen, and D-dimer. Individual patient outcomes were also accounted for and classified as good [with modified Rankin Scores (mRS) of 0, 1, 2, and 3 and poor mRS of 4, 5, 6]. Patients with no available laboratory data and outcomes were excluded in the quantitative analysis.
Search Results
Extensive database search yielded 595 citations, and four studies were added by manual searching. A total of 257 duplicates were excluded resulting in 342 citations. These titles and abstracts were further screened yielding 90 final publications of relevance to consideration of stroke and SARS-COV2 infection, during the second screening process. One publication was non-existent despite being cited by multiple authors in their publications. Further evaluation of the full texts of the 89 studies by two independent neurologists (TW and CS) excluded 74 citations with 15 studies. Three further studies were added from hand-held search by TW and CS with 18 publications that were deemed to be included in this systematic review by all authors.
Year and Country of Study
The studies published from 2019 to 2020, Included literature were originated from North America, Europe, and Asia.
Study Population
This study included all patients with SARS-COV2 infection and a concomitant diagnosis of acute ischemic stroke and/or acute/subacute outcomes where available.
An electronic search performed on May 10 to 30th, 2020 using the identified keywords yielded 342 citations after removal of duplicates. This was further assessed at the title and abstract level which resulted in 90 articles. After full assessment of the full text of each, 18 were deemed relevant to the study, in addition to the three articles which were added from hand-held research. Figure 1 summarizes the search process.

PRISMA Flowchart.
There were 18 articles included in the study consisting of 87 patients from USA, Italy, Turkey, France, Philippines, and United Kingdom. Most of the studies were case reports and case series while three of the included studies were retrospective and prospective cohorts. Table 1 outlines the characteristics of the individual studies.
Characteristics of studies included.
Clinical characteristics of patients are described in Table 2 .
Clinical characteristics of patients described.
The majority of the patients were within the 50–70 age group while almost one-third of the patients were <50 years old. The most common comorbidity was hypertension followed by diabetes, dyslipidemia and less frequently, atrial fibrillation. Mean hematologic parameters are also described. Neurovascular imaging either with magnetic resonance angiography (MRA) or computer tomographic angiography (CTA) was available for 35 patients, of whom the majority presented with anterior circulation, large vessel occlusion. Treatment regimens were also described for the majority of the patients and among whom a significant number received systemic anticoagulation, intravenous thrombolysis and mechanical thrombectomy. Of the 87 patients described, 72 outcomes are available, with almost 75% resulting in poor neurological outcomes of Modified Rankin score (mRS) 4 and above.
Inflammatory and coagulation markers of individual patients were also analyzed. Neurological outcomes were classified as either good (mRS 3 and below) or poor (mRS 4 and above). Respective inflammatory parameters such as neutrophil to lymphocyte ratio, C-reactive protein and serum ferritin were analyzed for each group. The same was performed for coagulation markers such as D-dimer and fibrinogen. Patients with good neurological outcomes had lower mean NLR, CRP and serum ferritin (4.39 ± 1.44, 53.09 ± 92.70 mg/L, 449 ± 482.3 ug/L, respectively), compared to patients with mRS 4 and above (7.51 ± 5.84, 88.69 ± 70.45 mg/L, 1,086 ± 1,220 ug/L, respectively). Similar trends were observed in terms of coagulation markers, with D-dimer and fibrinogen showing levels of 2,509 ± 4,093 ug/L and 4.70 ± 1.70 g/L, respectively, for patients with mRS 3 and below, while values for patients with poor neurological outcomes were 7,223 ± 6,781 ug/L for D-dimer and 6.086 ± 2.69 g/L for fibrinogen respectively. Summary of the said values are plotted in Figures 2A–E .

(A–C) Mean inflammatory markers among patients with stroke and confirmed SARA-CoV2 infections. (D–E) Mean coagulation markers among patients with stroke and confirmed SARS-CoV2 infection.
The relationship between the NLR on admission and the time interval from onset of SARS-CoV2 symptoms to the appearance onset of symptoms of stroke was established. As shown in Figure 3 , patients who have higher NLR at the onset have a shorter time interval between infective symptoms and the occurrence of the ischemic event.

Relationship between NLR and the occurrence of stroke from onset of SARS-CoV2 symptoms.
To date, there is no comprehensive review describing the potential role of inflammatory and coagulation biomarkers in determining the clinical outcomes of patients with SARS-CoV2 infection and concomitant acute ischemic stroke. The data presented will also supplement currently limited information on the occurrence of neurovascular events among patients with SARS-CoV2 infection.
To date a number of theoretical models have been proposed to account for the occurrence of neurovascular events among SARS-CoV2 patients. Most build on the idea of the SARS-CoV2 virus infection inducing inflammation and associated immunological release of cytokines from blood and endothelial cells and the concurrent activation of platelets resulting in micro thrombosis ( 69 ). The depletion of the cardioprotective and neuroprotective ACE-2 receptors throughout the body and on microglia in the brain, as a result of the receptors being the preferential cellular target of the virus invasion, has also been proposed as another neuropathologic mechanism irrespective of age ( 8 ). However, the hypercoagulable state of SARS-COV2 infection as the sole basis of this mechanism is debateable given that vascular workups for cryptogenic stroke have not been detailed in most of the case studies. Furthermore, the increase in “burden of disease” especially in the elderly is likely to be further exacerbated by the expected age-related depletion in ACE-2 receptors resulting in the predominance of the end-organ damaging effects of increasing the ACE-1/Angiotensin II ratio ( 70 – 72 ).
To date, the majority of AIS lesion sites in the patients described in the literature, are related to large vessel occlusion. However, it remains unclear whether this is due to a mechanism related to thrombosis or embolism or the lack of brain imaging. Unfortunately, there are no studies to date, which fully report autopsy findings of the deaths recorded among the stroke patients with SARS-CoV infection. In a different, though recent, study describing the autopsy results of 12 SARS-CoV2 patients in a German center, the majority of cases showed massive venous thromboembolism with no arterial thrombosis being reported ( 73 ). Mechanisms which may contribute to intracranial arterial thrombosis include the cytokine-induced initiation of thrombin formation that triggers the activation of platelets that subsequently result in the development of micro and macrothrombi ( 74 – 87 ). This is worsened by the free conversion of fibrinogen to fibrin and inflammation-induced depletion of physiological anticoagulants such as antithrombin III, tissue factor pathway inhibitor, and the protein C system ( 74 – 88 ). In terms of treatment, while 30 cases were reported to have large vessel occlusion, only 20 mechanical thrombectomies were performed. A comprehensive stroke center in Barcelona, Spain reported an 18 and 23% drop in the number of strokes codes and mechanical thrombectomies during the start of the pandemic, respectively, albeit without any changes in reperfusion and clinical outcomes ( 89 ) The World Stroke Organization recognizes the said difficulties and emphasizes the utility of telemedicine as well as best practice sharing to further optimize and streamline stroke processes ( 90 , 91 ).
While not depictive of the true epidemiologic picture, it is clear that patients with AIS and SARS-CoV2 infection have poor neurologic outcomes of either death or severe disability. Aggarwal et al. ( 92 ) concluded in a point analysis of four studies that patients with a previous history of stroke have a 2.5-fold increase in the odds of severe COVID infection but did not show any significant association with mortality ( 92 ). A retrospective cohort study of ischemic stroke reports a mortality rate close to 50% ( 3 ) while a prospective study involving 10 AIS patients resulted in four deaths ( 55 ) Clearly, more prospective studies involving a larger number of individual patients is necessary to ascertain the true mortality rate in this population.
In this study, there is a trend that patients with good outcomes have lower NLR, CRP, and serum ferritin compared to patients who died or remained critically ill. NLR has been shown to have a good predictive value in assessing patients who are likely to have severe SARS-CoV2 infection ( 30 , 93 – 96 ). In particular, it has been proposed that patients who are older and have NLR values of more than 3 are likely to require intensive care ( 27 ). Yan et al. also predicted that high NLR values on admission is associated with greater odds of complications related to COVID-infection ( 97 ). On the other hand, it is known that high NLR is used as a poor prognosticating factor for patients with cerebral ischemia, intracerebral hemorrhage and post-stroke complications ( 98 – 107 ). The dual consequence of COVID-related lymphopenia along with migration of the neutrophils to the ischemic tissue may contribute to the significant increase in the NLR levels in patients with stroke and concomitant SARS-CoV2 infection ( 107 ).
Another hyperinflammatory biomarker which has been shown to stratify outcomes in patients with SARS-CoV2 infection is CRP. Aside from predicting severity and mortality, it has prognosticating value in determining which patients will eventually require mechanical ventilation ( 108 – 110 ). Published literature noted that elevated CRP is associated with poor outcomes in patients with neurovascular conditions ( 111 , 112 ). There is also evidence to suggest that CRP is not just a “marker” but a “maker” of the atherogenesis ( 110 ). It has been demonstrated in experimental studies that exogenous CRP promotes atherogenesis by promoting the expression of adhesion molecules and cell mediators along with the decrease of arterial vasodilators ( 113 – 115 ). A meta-analysis of nine studies also provides evidence on the dose-dependent relationship of CRP and increased risk of venous thromboembolism ( 112 ). Whether the elevation of CRP is the causative etiology or the sequelae of a multifactorial process linking SARS-CoV2-infection to inflammation, atherogenesis or embolism needs further exploration.
Hyperferritinemia, which implies a heightened state of immunologic reactivity has also been associated with increased mortality in recent publications related to the SARS-CoV2 infection ( 116 ). It signals the activation of the macrophages and the reticuloendothelial system resulting in end-organ damage ( 117 ). Patients with SARS-CoV2 treated for pneumonia with Toculizumab had a marked decrease in the inflammatory markers such as CRP and ferritin, along with significant clinical improvement post-infusion ( 118 ). In patients with acute stroke, this iron storage protein can potentially worsen the iron-dependent oxidative stress in the ischemic penumbra which can lead to further neurologic decline ( 119 ). This is further validated in a study which shows a direct correlation between serum ferritin and markers of neural and blood-brain barrier disruption such as glutamate, interleukin-6, matrix metalloproteinase-9 and cellular fibronectin among patients receiving thrombolysis ( 39 ). The complementary inflammatory sequelae of SARS-CoV2 infection and ischemic stroke is the likely culprit of hyperferritinemia in SARS-CoV2 related strokes.
SARS-CoV2-related coagulopathy is responsible for various thrombotic events linked to mortality. Described as a fibrinolytic “shut-down,” SARS-CoV2 infection promotes a pro and hypercoagulable states resulting in disseminated (intravascular coagulation (DIC), microthrombi and other venous and arterial thrombotic phenomena ( 4 , 120 – 122 ). D-dimer and fibrinogen are both recognized as important biomarkers of the severity of coagulopathy in patients with SARS-CoV 2 infection ( 123 , 124 ). Olive et al. in a retrospective analysis of 21 patients with SARS-CoV infection concludes that D-dimer was associated with increased risk of pulmonary embolism ( 125 ). A similar observation was made in a larger study that suggests that D-dimer levels above 1 μg/mL may help in stratifying patients with poor prognosis at the onset ( 26 ). Fibrinogen increase was also observed among patients with severe SARS-CoV2 related pneumonia compared to mild presentation ( 126 ). The disproportionate increase of these biomarkers, especially at the early stages, warrant screening of thromboembolic events and initiation of thromboprophylaxis ( 124 ). The trend in these coagulation biomarkers are similarly observed in non-COVID related strokes. In the ARISTOTLE trial, patients with AF and increased D-dimer values had higher incidence of stroke, systemic embolism and all-cause mortality ( 127 ). Choi and colleagues also propose that D-dimer can be used as a biomarker for recurrence among patients with previous AF and non-AF related strokes ( 128 ). The EUROSTROKE study likewise confirms the utility of fibrinogen in predicting patients who are at risk for stroke ( 36 ). The said risk is equated to various clinical risks such as smoking, DM, MI, and HDL cholesterol ( 36 ). In this study, we have provided a scaffold on the potential trend between outcomes and coagulation parameters for SARS-CoV2 related strokes. While the most accepted mechanism behind this phenomenon is sepsis-induced disruption of the coagulation system, Iba et al. propose that more complex procoagulant responses resulting in a distinct interaction between the host's immunologic and the coagulation systems ( 124 ).
This study also highlights the occurrence of the ischemic event days to weeks after the onset of SARS-CoV2 symptoms. More importantly, we have established an inverse relationship between the inflammatory biomarker, NLR on admission and the duration between the stroke and the onset of SARS-CoV2 symptoms. This is likely related to the inflammatory burden which triggers a pro-coagulable cascade. Furthermore, Amiral et al. relate this to the alloimmune hypothesis, which has been demonstrated in rodents ( 129 ). The development of auto-antibodies to other ACE-2 receptors such as on the microglia in the brain after the onset of viral infection presumably resulted in the exponential increase in the cytokine storm and significant tissue destruction which may be linked to the delayed onset of the vascular event after the viral prodrome ( 129 ).
Lastly as the COVID-19 pandemic is distressing national health systems worldwide, a tsunami wave of neurorehabilitation needs and challenges regarding the long-term effects of the pandemic must be expected to begin to unfold soon. Thus, we believe that with strong humanity and collaboration across disciplines, this is the time to convert this situation into an opportunity that with vision, creativity, innovation, and use of smart technology can be harnessed with the aim of surviving this global health crisis ( 43 , 130 ).
Stroke is an important neurovascular complication of SARS-CoV2 infection. The aetiopathogenesis of cerebral ischemia is related to the overactivation of immune and hypercoagulable mechanisms. This is supported by the disproportionate increase of biomarkers such as NLR, CRP, serum ferritin, D-dimer and fibrinogen among patients who died or were critically ill. An elevated NLR on admission also implies an increased burden of inflammation at the onset of SARS-CoV infection which may result in early manifestation of cerebral ischemic events.
Author Contributions
TW and LK conceived of the presented idea. TW, SC, and LK developed the theory. TW and CS performed the literature search. TW wrote the manuscript with support from CS, LK, and SC. All four authors approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.

IMAGES
VIDEO
COMMENTS
CASE 1. A 20 year old man with no past medical history presented to a primary stroke center with sudden left sided weakness and imbalance followed by decreased level of consciousness. Head CT showed no hemorrhage, no acute ischemic changes, and a hyper-dense basilar artery. CT angiography showed a mid-basilar occlusion.
Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14
This case scenario presents a patient with acute ischemic cerebrovascular accident (CVA) requiring intravenous t-PA. Diagnosis was based on clinical neurologic symptoms and an NIHSS score of 7 and was later confirmed by neuroimaging.
Dr. Schwamm: The hospital-based response to acute stroke in this case began with the administration of intravenous t-PA, which according to established guidelines, 9 is a class 1, level of ...
Stroke is one of these complications, since a greater incidence of stroke among patients with COVID-19 than the non-COVID-19 population has been reported, and a preliminary case-control study demonstrated that SARS-CoV-2 infection represents a risk factor for acute ischemic stroke .
Figure 1. Neuroimaging from Patients with Acute Ischemic Stroke and Occlusion of the Left Middle Cerebral Artery. A 62-year-old, right-handed, independently functioning man presents 1 hour after a ...
A PFO has been demonstrated in 10%-26% of healthy adults. 14 In young patients who have had a cryptogenic stroke, however, the prevalence is thought to be much higher, for example, 40% in one study. 15 It is thought that a PFO allows microemboli to pass into the systemic circulation leading to a stroke.
Background Stroke is the second leading cause of death above the age of 60 years, and the fifth leading cause in people aged 15 to 59 years old as reported by the World Health Organization global burden of diseases. Stroke in the young is particularly tragic because of the potential to create long-term disability, burden on the victims, their families, and the community at large. Despite this ...
In Uganda, literature on stroke in young adults is limited however results of a study done among acute stroke patients admitted to the national referral hospital (Mulago hospital) showed a 30-day mortality of 43.8%. Out of 133 patients, 32 patients (25%) were less than 51 years old. Out of the 56 patients that died, 13 patients (23%) were less ...
This case study presents a 68-year old "right-handed" African-American man named Randall Swanson. He has a history of hypertension, hyperlipidemia and a history of smoking one pack per day for the last 20 years. ... the doctor must make the diagnosis of an acute ischemic stroke, and the patient must continue to present with neurological ...
IVT has been demonstrated to improve outcomes in patients with acute ischemic stroke within the first 4.5-h. 14, 15, 20-22 In 1996, the Food and Drug Administration (FDA) approved intravenous-tPA (IV-tPA) for treating acute ischemic stroke, based on successful outcomes in the National Institute of Neurological Disorders and Stroke study. 23, 24 ...
Amani Baidwan, Kendyl Egizi and Alysha Payne. Darrell Jackson, 81 year old male, came to the Emergency Department at Los Robles Hospital by ambulance after he collapsed in a coffee shop. Upon arrival he presented with left sided weakness, facial drooping, and aphasia. He was diagnosed with an ischemic stroke, right humerus head fracture, and ...
Patient Case Presentation. Image courtesy of uofmhealthblogs.org. D.B. is a 72 year old African American female who presented to the ED with complaints of headache, altered mental status as evidenced by confusion and lethargy, slurred speech, right sided weakness, and a facial droop. Symptoms were first noted when patient woke up from a nap ...
Stroke case study Creators. Sanaya Batcho; Kara Kitzmiller; Emma Overman; Our reason for choosing this disorder. Stroke is the leading cause of disability in the United States. As advanced practice nurses, we anticipate caring for those impacted by strokes in many healthcare settings including emergency rooms, acute care, rehab settings ...
Due to the multidimensional presentations (size/location of ICH, presence or absence of IVH, etc.) of those with hemorrhagic stroke, we presented this case study in order to pose that a single surgical approach may not be the answer to improving outcomes in comparison to medical management but actually a transition to a multimodal manner that ...
Statements, conclusions, accuracy and reliability of studies published in American Heart Association scientific journals or presented at American Heart Association scientific meetings are solely those of the study authors and do not necessarily reflect the American Heart Association's official guidance, policies or positions.
Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14
Inpatient Stroke Case Studies Inpatient E/M Case Studies. Case study of a stroke patient at varying visit levels to better understand code selection for inpatient encounters under the revised guidelines for 2024. 67-year-old Female with Stroke. Total time* for Inpatient E/M in 2023.
Abstract. ABSTRACT Purpose: The purpose of this study was to explore the effect of a lingual resistance training protocol on the swallowing function of an individual presenting with dysphagia and reduced tongue pressures following a supratentorial ischemic stroke. Methods: A study involving a lingual resistance training protocol with videofluoroscopy to measure outcomes comparing different ...
In one study, the five most frequent stroke mimics were seizure, syncope, sepsis, migraine and brain tumours 12; detailed reviews can be found in Practical Neurology. 13 14. ... Insufficient data, case-by-case risk decision with obstetric team. Unruptured intracranial aneurysm: Small (<10 mm) unsecured unruptured intracranial aneurysm should ...
Neurosomatic Massage therapy Provides Relief for Chronic Stroke Symptoms: A Case Study. Kim Jackman. Abstract. Background: Stroke is considered a leading cause of adult disability and despite advances in treating stroke, severe disability remains a common outcome.The most prevalent deficit after stroke is hemiparesis of the contralateral upper limb.
We conducted a nationwide, population-based case-crossover study of all Danes ≥ 18 years of age with first-time gout during 1997-2020, who experienced a cardiovascular event (myocardial infarction, ischemic stroke, congestive heart failure, atrial fibrillation/flutter, or cardiovascular death) (n = 59,150). The exposure was use of NSAIDs ...
A case study conducted in the US showed that people with high financial status had better stroke treatment options than deprived individuals . ... Stroke studies should be conducted in both male and female subjects to exclude gender bias, and should take account of other confounders like hypertension, diabetes and obesity. ...
The paper included stroke cases between Aug. 31, 2022, and January or February 2023, depending on the type of stroke. After exclusions, 11,001 stroke cases were included.
Acute ischemic stroke (AIS) was diagnosed in 5% of the cases ( 2 ). However, a much lower rate of only 0.9% imaging confirmed AIS i.e., 32/3,556 total patients case number with COVID-19 was reported in New York USA ( 3 ). Subsequent retrospective reports from Europe have also confirmed AIS as a common neurovascular complications of SARS-CoV2 ...