Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State

Patient Case Presentation

Figure 1. Blue and silver stethoscope (Pixabay, N.D.)
Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness. She also noticed other changes about herself, including decreased appetite, insomnia, fatigue, and poor ability to concentrate. The things that used to bring Ms. S.W. joy, such as gardening and listening to podcasts, are no longer bringing her the same happiness they used to. She became especially concerned as within the past two weeks she also started experiencing feelings of worthlessness, the perception that she is a burden to others, and fleeting thoughts of death/suicide.
Ms. S.W. acknowledges that she has numerous stressors in her life. She reports that her daughter’s grades have been steadily declining over the past two semesters and she is unsure if her daughter will be attending college anymore. Her relationship with her son is somewhat strained as she and his father are not on good terms and her son feels Ms. S.W. is at fault for this. She feels her career has been unfulfilling and though she’d like to go back to school, this isn’t possible given the family’s tight finances/the patient raising a family on a single income.
Ms. S.W. has experienced symptoms of depression previously, but she does not think the symptoms have ever been as severe as they are currently. She has taken antidepressants in the past and was generally adherent to them, but she believes that therapy was more helpful than the medications. She denies ever having history of manic or hypomanic episodes. She has been unable to connect to a mental health agency in several years due to lack of time and feeling that she could manage the symptoms on her own. She now feels that this is her last option and is looking for ongoing outpatient mental health treatment.
Past Medical History
- Hypertension, diagnosed at age 41
Past Surgical History
- Wisdom teeth extraction, age 22
Pertinent Family History
- Mother with history of Major Depressive Disorder, treated with antidepressants
- Maternal grandmother with history of Major Depressive Disorder, Generalized Anxiety Disorder
- Brother with history of suicide attempt and subsequent inpatient psychiatric hospitalization,
- Brother with history of Alcohol Use Disorder
- Father died from lung cancer (2012)
Pertinent Social History
- Works full-time as an enrollment specialist for Columbus City Schools since 2006
- Has two children, a daughter age 17 and a son age 14
- Divorced in 2015, currently single
- History of some emotional abuse and neglect from mother during childhood, otherwise denies history of trauma, including physical and sexual abuse
- Smoking 1/2 PPD of cigarettes
- Occasional alcohol use (approximately 1-2 glasses of wine 1-2 times weekly; patient had not had any alcohol consumption for the past year until two weeks ago)

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Common mental health problems: Clinical case scenarios
Published by Ella Stack Modified over 10 years ago
Similar presentations
Presentation on theme: "Common mental health problems: Clinical case scenarios"— Presentation transcript:
Implementing NICE guidance
Depression in adults with a chronic physical health problem
Maternal and child nutrition
Pregnancy and complex social factors
Diabetic Foot Problems
For primary and secondary care settings
and alcohol dependence
Depression Lawrence Pike.
Consulting on the Telephone OOH GP Training Day. Learning Objectives Review our approach to consulting on the phone Address concerns over this format.
Understanding Depression
Presenting Issues Considerations for Counselling and Psychotherapy An Introduction to Counselling and Psychotherapy: From Theory to Practice.
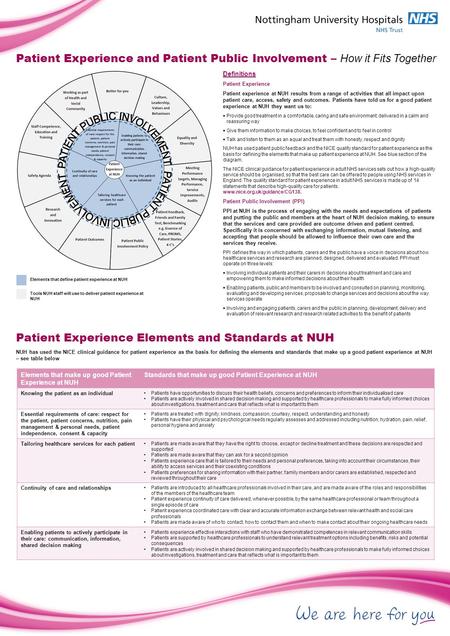
Definitions Patient Experience Patient experience at NUH results from a range of activities that all impact upon patient care, access, safety and outcomes.
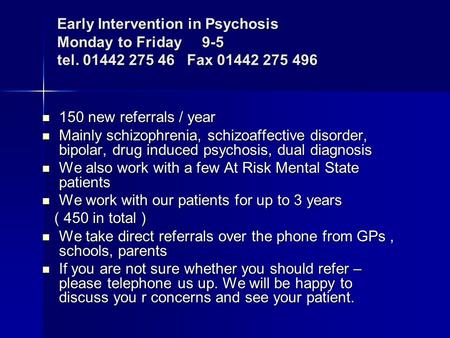
150 new referrals / year 150 new referrals / year Mainly schizophrenia, schizoaffective disorder, bipolar, drug induced psychosis, dual diagnosis Mainly.

TalkingSpace & TalkingHealth The IAPT service, Oxfordshire and Buckinghamshire NHS Foundation Trust Christina Surawy: Oxford Mindfulness Centre, Oxford.
PACIFIC HEADS OF PRISONS CONFERENCE Mental Health Workshop.

The West Cheshire Way Be part of the conversation.. Alison Lee Chief Officer West Cheshire Clinical Commissioning Group Making sure you get the healthcare.
Centre for Emotional Health - Ageing Research Viviana Wuthrich.
Module C: Lesson 4. Anxiety disorders affect 12% of the population. Many do not seek treatment because: Consider the symptoms mild or normal.
Alcohol-use disorders: diagnosis, assessment and management of harmful drinking and alcohol dependence Implementing NICE guidance February 2011 NICE clinical.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.

Mental Health Case Study: Understanding Depression through a Real-life Example
Imagine feeling an unrelenting heaviness weighing down on your chest. Every breath becomes a struggle as a cloud of sadness engulfs your every thought. Your energy levels plummet, leaving you physically and emotionally drained. This is the reality for millions of people worldwide who suffer from depression, a complex and debilitating mental health condition.
Understanding depression is crucial in order to provide effective support and treatment for those affected. While textbooks and research papers provide valuable insights, sometimes the best way to truly comprehend the depths of this condition is through real-life case studies. These stories bring depression to life, shedding light on its impact on individuals and society as a whole.
In this article, we will delve into the world of mental health case studies, using a real-life example to explore the intricacies of depression. We will examine the symptoms, prevalence, and consequences of this all-encompassing condition. Furthermore, we will discuss the significance of case studies in mental health research, including their ability to provide detailed information about individual experiences and contribute to the development of treatment strategies.
Through an in-depth analysis of a selected case study, we will gain insight into the journey of an individual facing depression. We will explore their background, symptoms, and initial diagnosis. Additionally, we will examine the various treatment options available and assess the effectiveness of the chosen approach.
By delving into this real-life example, we will not only gain a better understanding of depression as a mental health condition, but we will also uncover valuable lessons that can aid in the treatment and support of those who are affected. So, let us embark on this enlightening journey, using the power of case studies to bring understanding and empathy to those who need it most.
Understanding Depression
Depression is a complex and multifaceted mental health condition that affects millions of people worldwide. To comprehend the impact of depression, it is essential to explore its defining characteristics, prevalence, and consequences on individuals and society as a whole.
Defining depression and its symptoms
Depression is more than just feeling sad or experiencing a low mood. It is a serious mental health disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities that were once enjoyable. Individuals with depression often experience a range of symptoms that can significantly impact their daily lives. These symptoms include:
1. Persistent feelings of sadness or emptiness. 2. Fatigue and decreased energy levels. 3. Significant changes in appetite and weight. 4. Difficulty concentrating or making decisions. 5. Insomnia or excessive sleep. 6. feelings of guilt, worthlessness, or hopelessness. 7. Loss of interest or pleasure in activities.
Exploring the prevalence of depression worldwide
Depression knows no boundaries and affects individuals from all walks of life. According to the World Health Organization (WHO), an estimated 264 million people globally suffer from depression. This makes depression one of the most common mental health conditions worldwide. Additionally, the WHO highlights that depression is more prevalent among females than males.
The impact of depression is not limited to individuals alone. It also has significant social and economic consequences. Depression can lead to impaired productivity, increased healthcare costs, and strain on relationships, contributing to a significant burden on families, communities, and society at large.
The impact of depression on individuals and society
Depression can have a profound and debilitating impact on individuals’ lives, affecting their physical, emotional, and social well-being. The persistent sadness and loss of interest can lead to difficulties in maintaining relationships, pursuing education or careers, and engaging in daily activities. Furthermore, depression increases the risk of developing other mental health conditions, such as anxiety disorders or substance abuse.
On a societal level, depression poses numerous challenges. The economic burden of depression is significant, with costs associated with treatment, reduced productivity, and premature death. Moreover, the social stigma surrounding mental health can impede individuals from seeking help and accessing appropriate support systems.
Understanding the prevalence and consequences of depression is crucial for policymakers, healthcare professionals, and individuals alike. By recognizing the significant impact depression has on individuals and society, appropriate resources and interventions can be developed to mitigate its effects and improve the overall well-being of those affected.
The Significance of Case Studies in Mental Health Research
Case studies play a vital role in mental health research, providing valuable insights into individual experiences and contributing to the development of effective treatment strategies. Let us explore why case studies are considered invaluable in understanding and addressing mental health conditions.
Why case studies are valuable in mental health research
Case studies offer a unique opportunity to examine mental health conditions within the real-life context of individuals. Unlike large-scale studies that focus on statistical data, case studies provide a detailed examination of specific cases, allowing researchers to delve into the complexities of a particular condition or treatment approach. This micro-level analysis helps researchers gain a deeper understanding of the nuances and intricacies involved.
The role of case studies in providing detailed information about individual experiences
Through case studies, researchers can capture rich narratives and delve into the lived experiences of individuals facing mental health challenges. These stories help to humanize the condition and provide valuable insights that go beyond a list of symptoms or diagnostic criteria. By understanding the unique experiences, thoughts, and emotions of individuals, researchers can develop a more comprehensive understanding of mental health conditions and tailor interventions accordingly.
How case studies contribute to the development of treatment strategies
Case studies form a vital foundation for the development of effective treatment strategies. By examining a specific case in detail, researchers can identify patterns, factors influencing treatment outcomes, and areas where intervention may be particularly effective. Moreover, case studies foster an iterative approach to treatment development—an ongoing cycle of using data and experience to refine and improve interventions.
By examining multiple case studies, researchers can identify common themes and trends, leading to the development of evidence-based guidelines and best practices. This allows healthcare professionals to provide more targeted and personalized support to individuals facing mental health conditions.
Furthermore, case studies can shed light on potential limitations or challenges in existing treatment approaches. By thoroughly analyzing different cases, researchers can identify gaps in current treatments and focus on areas that require further exploration and innovation.
In summary, case studies are a vital component of mental health research, offering detailed insights into the lived experiences of individuals with mental health conditions. They provide a rich understanding of the complexities of these conditions and contribute to the development of effective treatment strategies. By leveraging the power of case studies, researchers can move closer to improving the lives of individuals facing mental health challenges.
Examining a Real-life Case Study of Depression
In order to gain a deeper understanding of depression, let us now turn our attention to a real-life case study. By exploring the journey of an individual navigating through depression, we can gain valuable insights into the complexities and challenges associated with this mental health condition.
Introduction to the selected case study
In this case study, we will focus on Jane, a 32-year-old woman who has been struggling with depression for the past two years. Jane’s case offers a compelling narrative that highlights the various aspects of depression, including its onset, symptoms, and the treatment journey.
Background information on the individual facing depression
Before the onset of depression, Jane led a fulfilling and successful life. She had a promising career, a supportive network of friends and family, and engaged in hobbies that brought her joy. However, a series of life stressors, including a demanding job, a breakup, and the loss of a loved one, began to take a toll on her mental well-being.
Jane’s background highlights a common phenomenon – depression can affect individuals from all walks of life, irrespective of their socio-economic status, age, or external circumstances. It serves as a reminder that no one is immune to mental health challenges.
Presentation of symptoms and initial diagnosis
Jane began noticing a shift in her mood, characterized by persistent feelings of sadness and a lack of interest in activities she once enjoyed. She experienced disruptions in her sleep patterns, appetite changes, and a general sense of hopelessness. Recognizing the severity of her symptoms, Jane sought help from a mental health professional who diagnosed her with major depressive disorder.
Jane’s case exemplifies the varied and complex symptoms associated with depression. While individuals may exhibit overlapping symptoms, the intensity and manifestation of those symptoms can vary greatly, underscoring the importance of personalized and tailored treatment approaches.
By examining this real-life case study of depression, we can gain an empathetic understanding of the challenges faced by individuals experiencing this mental health condition. Through Jane’s journey, we will uncover the treatment options available for depression and analyze the effectiveness of the chosen approach. The case study will allow us to explore the nuances of depression and provide valuable insights into the treatment landscape for this prevalent mental health condition.
The Treatment Journey
When it comes to treating depression, there are various options available, ranging from therapy to medication. In this section, we will provide an overview of the treatment options for depression and analyze the treatment plan implemented in the real-life case study.
Overview of the treatment options available for depression
Treatment for depression typically involves a combination of approaches tailored to the individual’s needs. The two primary treatment modalities for depression are psychotherapy (talk therapy) and medication. Psychotherapy aims to help individuals explore their thoughts, emotions, and behaviors, while medication can help alleviate symptoms by restoring chemical imbalances in the brain.
Common forms of psychotherapy used in the treatment of depression include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and psychodynamic therapy. These therapeutic approaches focus on addressing negative thought patterns, improving relationship dynamics, and gaining insight into underlying psychological factors contributing to depression.
In cases where medication is utilized, selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed. These medications help rebalance serotonin levels in the brain, which are often disrupted in individuals with depression. Other classes of antidepressant medications, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) or tricyclic antidepressants (TCAs), may be considered in specific cases.
Exploring the treatment plan implemented in the case study
In Jane’s case, a comprehensive treatment plan was developed with the intention of addressing her specific needs and symptoms. Recognizing the severity of her depression, Jane’s healthcare team recommended a combination of talk therapy and medication.
Jane began attending weekly sessions of cognitive-behavioral therapy (CBT) with a licensed therapist. This form of therapy aimed to help Jane identify and challenge negative thought patterns, develop coping strategies, and cultivate more adaptive behaviors. The therapeutic relationship provided Jane with a safe space to explore and process her emotions, ultimately helping her regain a sense of control over her life.
In conjunction with therapy, Jane’s healthcare provider prescribed an SSRI medication to assist in managing her symptoms. The medication was carefully selected based on Jane’s specific symptoms and medical history, and regular follow-up appointments were scheduled to monitor her response to the medication and adjust the dosage if necessary.
Analyzing the effectiveness of the treatment approach
The effectiveness of treatment for depression varies from person to person, and it often requires a period of trial and adjustment to find the most suitable intervention. In Jane’s case, the combination of cognitive-behavioral therapy and medication proved to be beneficial. Over time, she reported a reduction in her depressive symptoms, an improvement in her overall mood, and increased ability to engage in activities she once enjoyed.
It is important to note that the treatment journey for depression is not always linear, and setbacks and challenges may occur along the way. Each individual responds differently to treatment, and adjustments might be necessary to optimize outcomes. Continuous communication between the individual and their healthcare team is crucial to addressing any concerns, monitoring progress, and adapting the treatment plan as needed.
By analyzing the treatment approach in the real-life case study, we gain insights into the various treatment options available for depression and how they can be tailored to meet individual needs. The combination of psychotherapy and medication offers a holistic approach, addressing both psychological and biological aspects of depression.
The Outcome and Lessons Learned
After undergoing treatment for depression, it is essential to assess the outcome and draw valuable lessons from the case study. In this section, we will discuss the progress made by the individual in the case study, examine the challenges faced during the treatment process, and identify key lessons learned.
Discussing the progress made by the individual in the case study
Throughout the treatment process, Jane experienced significant progress in managing her depression. She reported a reduction in depressive symptoms, improved mood, and a renewed sense of hope and purpose in her life. Jane’s active participation in therapy, combined with the appropriate use of medication, played a crucial role in her progress.
Furthermore, Jane’s support network of family and friends played a significant role in her recovery. Their understanding, empathy, and support provided a solid foundation for her journey towards improved mental well-being. This highlights the importance of social support in the treatment and management of depression.
Examining the challenges faced during the treatment process
Despite the progress made, Jane faced several challenges during her treatment journey. Adhering to the treatment plan consistently proved to be difficult at times, as she encountered setbacks and moments of self-doubt. Additionally, managing the side effects of the medication required careful monitoring and adjustments to find the right balance.
Moreover, the stigma associated with mental health continued to be a challenge for Jane. Overcoming societal misconceptions and seeking help required courage and resilience. The case study underscores the need for increased awareness, education, and advocacy to address the stigma surrounding mental health conditions.
Identifying the key lessons learned from the case study
The case study offers valuable lessons that can inform the treatment and support of individuals with depression:
1. Holistic Approach: The combination of psychotherapy and medication proved to be effective in addressing the psychological and biological aspects of depression. This highlights the need for a holistic and personalized treatment approach.
2. Importance of Support: Having a strong support system can significantly impact an individual’s ability to navigate through depression. Family, friends, and healthcare professionals play a vital role in providing empathy, understanding, and encouragement.
3. Individualized Treatment: Depression manifests differently in each individual, emphasizing the importance of tailoring treatment plans to meet individual needs. Personalized interventions are more likely to lead to positive outcomes.
4. Overcoming Stigma: Addressing the stigma associated with mental health conditions is crucial for individuals to seek timely help and access the support they need. Educating society about mental health is essential to create a more supportive and inclusive environment.
By drawing lessons from this real-life case study, we gain insights that can improve the understanding and treatment of depression. Recognizing the progress made, understanding the challenges faced, and implementing the lessons learned can contribute to more effective interventions and support systems for individuals facing depression.In conclusion, this article has explored the significance of mental health case studies in understanding and addressing depression, focusing on a real-life example. By delving into case studies, we gain a deeper appreciation for the complexities of depression and the profound impact it has on individuals and society.
Through our examination of the selected case study, we have learned valuable lessons about the nature of depression and its treatment. We have seen how the combination of psychotherapy and medication can provide a holistic approach, addressing both psychological and biological factors. Furthermore, the importance of social support and the role of a strong network in an individual’s recovery journey cannot be overstated.
Additionally, we have identified challenges faced during the treatment process, such as adherence to the treatment plan and managing medication side effects. These challenges highlight the need for ongoing monitoring, adjustments, and open communication between individuals and their healthcare providers.
The case study has also emphasized the impact of stigma on individuals seeking help for depression. Addressing societal misconceptions and promoting mental health awareness is essential to create a more supportive environment for those affected by depression and other mental health conditions.
Overall, this article reinforces the significance of case studies in advancing our understanding of mental health conditions and developing effective treatment strategies. Through real-life examples, we gain a more comprehensive and empathetic perspective on depression, enabling us to provide better support and care for individuals facing this mental health challenge.
As we conclude, it is crucial to emphasize the importance of continued research and exploration of mental health case studies. The more we learn from individual experiences, the better equipped we become to address the diverse needs of those affected by mental health conditions. By fostering a culture of understanding, support, and advocacy, we can strive towards a future where individuals with depression receive the care and compassion they deserve.
Similar Posts

Dating Someone with Bipolar: Understanding, Challenges, and Ways to Navigate the Relationship
Love is a beautiful and unpredictable journey that can take us to the highest peaks of joy and the deepest depths of despair. But what happens when that rollercoaster of emotions is amplified by Bipolar Disorder?…

Understanding the C&P Exam for Bipolar Disorder: A Comprehensive Guide
Imagine living with the constant swing of emotions, from euphoric highs to deep lows, all while trying to navigate daily life. This is the reality for individuals with bipolar disorder, a mental health condition that affects…

Understanding the Meaning behind ‘If Depression Gets the Best of Me’ Lyrics
Imagine a world where emotions are given a voice, where the harrowing depths of depression are laid bare for all to see and understand. In a society that often shies away from discussing mental health openly,…

Understanding Bipolar Hyperfixation: Causes, Symptoms, and Coping Strategies
Do you ever find yourself completely engrossed in a particular activity or interest, to the point where it consumes your thoughts and time? Perhaps you’ve experienced moments of intense fixation on a certain hobby, topic, or…

Finding Major Depressive Disorder Specialists: Where to Get Help for Depression Near You
Imagine waking up every morning weighed down by an overwhelming sense of sadness and despair. You drag yourself out of bed, facing another day filled with emptiness and hopelessness. Your friends and family may struggle to…

The Potential Benefits of Reishi Mushroom for Bipolar Disorder
Living with bipolar disorder can be a rollercoaster of emotions. The extreme highs of mania and the debilitating lows of depression can disrupt daily life and strain relationships. For those searching for alternative approaches to managing…
Home Collections Medical Mental Health Clinical Case Of Mental Health
Best Clinical Case Of Mental Health PPT And Google Slides
Clinical Case Of Mental Health Presentation Slide
Features of the template.
- 100% customizable slides and easy to download.
- Slides are available in different colors
- The slide has 4:3 and 16:9 formats.
- Easy to change the slide colors quickly.
- Appealing Presentation to impress an audience.
- Create feature-rich slide presentations.
- An eye-pleasing color slide helps to give a catchy display.
- Highly compatible with PowerPoint and Google Slides.
- mental health
- Clinical Case Of Mental Health
- Mental Health
- Mental Health Clinical Case
- Clinical Case Of Mental Health Infographics
- Google Slides

666+ Templates
-594.webp)
124+ Templates

Science & Research
182+ Templates

Telemedicine
40+ Templates

320+ Templates

86+ Templates
115+ Templates

43+ Templates
44+ Templates

191+ Templates
You May Also Like These PowerPoint Templates

Module 11: Schizophrenia Spectrum and Other Psychotic Disorders
Case studies: schizophrenia spectrum disorders, learning objectives.
- Identify schizophrenia and psychotic disorders in case studies
Case Study: Bryant
Thirty-five-year-old Bryant was admitted to the hospital because of ritualistic behaviors, depression, and distrust. At the time of admission, prominent ritualistic behaviors and depression misled clinicians to diagnose Bryant with obsessive-compulsive disorder (OCD). Shortly after, psychotic symptoms such as disorganized thoughts and delusion of control were noticeable. He told the doctors he has not been receiving any treatment, was not on any substance or medication, and has been experiencing these symptoms for about two weeks. Throughout the course of his treatment, the doctors noticed that he developed a catatonic stupor and a respiratory infection, which was identified by respiratory symptoms, blood tests, and a chest X-ray. To treat the psychotic symptoms, catatonic stupor, and respiratory infection, risperidone, MECT, and ceftriaxone (antibiotic) were administered, and these therapies proved to be dramatically effective. [1]
Case Study: Shanta
Shanta, a 28-year-old female with no prior psychiatric hospitalizations, was sent to the local emergency room after her parents called 911; they were concerned that their daughter had become uncharacteristically irritable and paranoid. The family observed that she had stopped interacting with them and had been spending long periods of time alone in her bedroom. For over a month, she had not attended school at the local community college. Her parents finally made the decision to call the police when she started to threaten them with a knife, and the police took her to the local emergency room for a crisis evaluation.
Following the administration of the medication, she tried to escape from the emergency room, contending that the hospital staff was planning to kill her. She eventually slept and when she awoke, she told the crisis worker that she had been diagnosed with attention-deficit/hyperactive disorder (ADHD) a month ago. At the time of this ADHD diagnosis, she was started on 30 mg of a stimulant to be taken every morning in order to help her focus and become less stressed over the possibility of poor school performance.
After two weeks, the provider increased her dosage to 60 mg every morning and also started her on dextroamphetamine sulfate tablets (10 mg) that she took daily in the afternoon in order to improve her concentration and ability to study. Shanta claimed that she might have taken up to three dextroamphetamine sulfate tablets over the past three days because she was worried about falling asleep and being unable to adequately prepare for an examination.
Prior to the ADHD diagnosis, the patient had no known psychiatric or substance abuse history. The urine toxicology screen taken upon admission to the emergency department was positive only for amphetamines. There was no family history of psychotic or mood disorders, and she didn’t exhibit any depressive, manic, or hypomanic symptoms.
The stimulant medications were discontinued by the hospital upon admission to the emergency department and the patient was treated with an atypical antipsychotic. She tolerated the medications well, started psychotherapy sessions, and was released five days later. On the day of discharge, there were no delusions or hallucinations reported. She was referred to the local mental health center for aftercare follow-up with a psychiatrist. [2]
Another powerful case study example is that of Elyn R. Saks, the associate dean and Orrin B. Evans professor of law, psychology, and psychiatry and the behavioral sciences at the University of Southern California Gould Law School.
Saks began experiencing symptoms of mental illness at eight years old, but she had her first full-blown episode when studying as a Marshall scholar at Oxford University. Another breakdown happened while Saks was a student at Yale Law School, after which she “ended up forcibly restrained and forced to take anti-psychotic medication.” Her scholarly efforts thus include taking a careful look at the destructive impact force and coercion can have on the lives of people with psychiatric illnesses, whether during treatment or perhaps in interactions with police; the Saks Institute, for example, co-hosted a conference examining the urgent problem of how to address excessive use of force in encounters between law enforcement and individuals with mental health challenges.
Saks lives with schizophrenia and has written and spoken about her experiences. She says, “There’s a tremendous need to implode the myths of mental illness, to put a face on it, to show people that a diagnosis does not have to lead to a painful and oblique life.”
In recent years, researchers have begun talking about mental health care in the same way addiction specialists speak of recovery—the lifelong journey of self-treatment and discipline that guides substance abuse programs. The idea remains controversial: managing a severe mental illness is more complicated than simply avoiding certain behaviors. Approaches include “medication (usually), therapy (often), a measure of good luck (always)—and, most of all, the inner strength to manage one’s demons, if not banish them. That strength can come from any number of places…love, forgiveness, faith in God, a lifelong friendship.” Saks says, “We who struggle with these disorders can lead full, happy, productive lives, if we have the right resources.”
You can view the transcript for “A tale of mental illness | Elyn Saks” here (opens in new window) .
- Bai, Y., Yang, X., Zeng, Z., & Yang, H. (2018). A case report of schizoaffective disorder with ritualistic behaviors and catatonic stupor: successful treatment by risperidone and modified electroconvulsive therapy. BMC psychiatry , 18(1), 67. https://doi.org/10.1186/s12888-018-1655-5 ↵
- Henning A, Kurtom M, Espiridion E D (February 23, 2019) A Case Study of Acute Stimulant-induced Psychosis. Cureus 11(2): e4126. doi:10.7759/cureus.4126 ↵
- Modification, adaptation, and original content. Authored by : Wallis Back for Lumen Learning. Provided by : Lumen Learning. License : CC BY: Attribution
- A tale of mental illness . Authored by : Elyn Saks. Provided by : TED. Located at : https://www.youtube.com/watch?v=f6CILJA110Y . License : Other . License Terms : Standard YouTube License
- A Case Study of Acute Stimulant-induced Psychosis. Authored by : Ashley Henning, Muhannad Kurtom, Eduardo D. Espiridion. Provided by : Cureus. Located at : https://www.cureus.com/articles/17024-a-case-study-of-acute-stimulant-induced-psychosis#article-disclosures-acknowledgements . License : CC BY: Attribution
- Elyn Saks. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Elyn_Saks . License : CC BY-SA: Attribution-ShareAlike
- A case report of schizoaffective disorder with ritualistic behaviors and catatonic stupor: successful treatment by risperidone and modified electroconvulsive therapy. Authored by : Yuanhan Bai, Xi Yang, Zhiqiang Zeng, and Haichen Yangcorresponding. Located at : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851085/ . License : CC BY: Attribution

- Children's mental health case studies
- Food, health and nutrition
- Mental wellbeing
- Mental health
Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and feedback for the user. Use these cases on your own or in classes and training events
Each case study:
- Explores the experiences of a child and family over time.
- Introduces theories, research and practice ideas about children's mental health.
- Shows the needs of a child at specific stages of development.
- Invites users to “try on the hat” of different specific professionals.
By completing a case study participants will:
- Examine the needs of children from an interdisciplinary perspective.
- Recognize the importance of prevention/early intervention in children’s mental health.
- Apply ecological and developmental perspectives to children’s mental health.
- Predict probable outcomes for children based on services they receive.
Case studies prompt users to practice making decisions that are:
- Research-based.
- Practice-based.
- Best to meet a child and family's needs in that moment.
Children’s mental health service delivery systems often face significant challenges.
- Services can be disconnected and hard to access.
- Stigma can prevent people from seeking help.
- Parents, teachers and other direct providers can become overwhelmed with piecing together a system of care that meets the needs of an individual child.
- Professionals can be unaware of the theories and perspectives under which others serving the same family work
- Professionals may face challenges doing interdisciplinary work.
- Limited funding promotes competition between organizations trying to serve families.
These case studies help explore life-like mental health situations and decision-making. Case studies introduce characters with history, relationships and real-life problems. They offer users the opportunity to:
- Examine all these details, as well as pertinent research.
- Make informed decisions about intervention based on the available information.
The case study also allows users to see how preventive decisions can change outcomes later on. At every step, the case content and learning format encourages users to review the research to inform their decisions.
Each case study emphasizes the need to consider a growing child within ecological, developmental, and interdisciplinary frameworks.
- Ecological approaches consider all the levels of influence on a child.
- Developmental approaches recognize that children are constantly growing and developing. They may learn some things before other things.
- Interdisciplinary perspectives recognize that the needs of children will not be met within the perspectives and theories of a single discipline.
There are currently two different case students available. Each case study reflects a set of themes that the child and family experience.
The About Steven case study addresses:
- Adolescent depression.
- School mental health.
- Rural mental health services.
- Social/emotional development.
The Brianna and Tanya case study reflects themes of:
- Infant and early childhood mental health.
- Educational disparities.
- Trauma and toxic stress.
- Financial insecurity.
- Intergenerational issues.
The case studies are designed with many audiences in mind:
Practitioners from a variety of fields. This includes social work, education, nursing, public health, mental health, and others.
Professionals in training, including those attending graduate or undergraduate classes.
The broader community.
Each case is based on the research, theories, practices and perspectives of people in all these areas. The case studies emphasize the importance of considering an interdisciplinary framework. Children’s needs cannot be met within the perspective of a single discipline.
The complex problems children face need solutions that integrate many and diverse ways of knowing. The case studies also help everyone better understand the mental health needs of children. We all have a role to play.
These case has been piloted within:
Graduate and undergraduate courses.
Discipline-specific and interdisciplinary settings.
Professional organizations.
Currently, the case studies are being offered to instructors and their staff and students in graduate and undergraduate level courses. They are designed to supplement existing course curricula.
Instructors have used the case study effectively by:
- Assigning the entire case at one time as homework. This is followed by in-class discussion or a reflective writing assignment relevant to a course.
- Assigning sections of the case throughout the course. Instructors then require students to prepare for in-class discussion pertinent to that section.
- Creating writing, research or presentation assignments based on specific sections of course content.
- Focusing on a specific theme present in the case that is pertinent to the course. Instructors use this as a launching point for deeper study.
- Constructing other in-class creative experiences with the case.
- Collaborating with other instructors to hold interdisciplinary discussions about the case.
To get started with a particular case, visit the related web page and follow the instructions to register. Once you register as an instructor, you will receive information for your co-instructors, teaching assistants and students. Get more information on the following web pages.
- Brianna and Tanya: A case study about infant and early childhood mental health
- About Steven: A children’s mental health case study about depression
Cari Michaels, Extension educator
Reviewed in 2023
© 2024 Regents of the University of Minnesota. All rights reserved. The University of Minnesota is an equal opportunity educator and employer.
- Report Web Disability-Related Issue |
- Privacy Statement |
- Staff intranet
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Sample Case Presentation in Psychiatric Nursing Case Analysis

Because the pros and cons for the use of medicine in psychiatry are not absolutely clear or agreed upon, strong arguments have risen on all sides. The objective of this paper is not to create a division in the clinical practice. Rather, to present an example of how to use a model in the analysis of understanding the patient behavior.
RELATED PAPERS
Jason Wonsley
Estela Orozco Hernández
Hrvatski Ljetopis Za Kazneno Pravo I Praksu
Zoran Buric
Bruce Salzberg MD, FACG
Patricia Bejarano-Muñoz
The Cancer Journal
David Teachey
Chantal Zaouche-Gaudron
Translational vision science & technology
Richard Rosen
New West Indian Guide / Nieuwe West-Indische Gids
Klaas Kramer
AIAA Guidance, Navigation, and Control Conference
Michael Naderhirn
Acta chirurgica iugoslavica
Brandon Johnson
Carmela De Marco
Journal of Ma’alim al-Quran wa al-Sunnah
Mohd Farhan Md Ariffin
Deysi Antuane Saldaña Amaya
Journal of Crohn's & colitis
Marc Ferrante
Bernard Harris
Amadine Haji
Bulletin of the World Health Organization
Don Savigny
Quarterly Journal of the Royal Meteorological Society
Barbara Chimani
Acta pediátrica española
Alfonso Solar Boga
Asian Soil Research Journal
Ebuka Nwankwo
Circulation
Regional Anesthesia and Pain Medicine
Salvatore Meola
Cecilie M Mejdell
See More Documents Like This
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
Mental Health Prevention and Promotion—A Narrative Review
Associated data.
Extant literature has established the effectiveness of various mental health promotion and prevention strategies, including novel interventions. However, comprehensive literature encompassing all these aspects and challenges and opportunities in implementing such interventions in different settings is still lacking. Therefore, in the current review, we aimed to synthesize existing literature on various mental health promotion and prevention interventions and their effectiveness. Additionally, we intend to highlight various novel approaches to mental health care and their implications across different resource settings and provide future directions. The review highlights the (1) concept of preventive psychiatry, including various mental health promotions and prevention approaches, (2) current level of evidence of various mental health preventive interventions, including the novel interventions, and (3) challenges and opportunities in implementing concepts of preventive psychiatry and related interventions across the settings. Although preventive psychiatry is a well-known concept, it is a poorly utilized public health strategy to address the population's mental health needs. It has wide-ranging implications for the wellbeing of society and individuals, including those suffering from chronic medical problems. The researchers and policymakers are increasingly realizing the potential of preventive psychiatry; however, its implementation is poor in low-resource settings. Utilizing novel interventions, such as mobile-and-internet-based interventions and blended and stepped-care models of care can address the vast mental health need of the population. Additionally, it provides mental health services in a less-stigmatizing and easily accessible, and flexible manner. Furthermore, employing decision support systems/algorithms for patient management and personalized care and utilizing the digital platform for the non-specialists' training in mental health care are valuable additions to the existing mental health support system. However, more research concerning this is required worldwide, especially in the low-and-middle-income countries.
Introduction
Mental disorder has been recognized as a significant public health concern and one of the leading causes of disability worldwide, particularly with the loss of productive years of the sufferer's life ( 1 ). The Global Burden of Disease report (2019) highlights an increase, from around 80 million to over 125 million, in the worldwide number of Disability-Adjusted Life Years (DALYs) attributable to mental disorders. With this surge, mental disorders have moved into the top 10 significant causes of DALYs worldwide over the last three decades ( 2 ). Furthermore, this data does not include substance use disorders (SUDs), which, if included, would increase the estimated burden manifolds. Moreover, if the caregiver-related burden is accounted for, this figure would be much higher. Individual, social, cultural, political, and economic issues are critical mental wellbeing determinants. An increasing burden of mental diseases can, in turn, contribute to deterioration in physical health and poorer social and economic growth of a country ( 3 ). Mental health expenditure is roughly 3–4% of their Gross Domestic Products (GDPs) in developed regions of the world; however, the figure is abysmally low in low-and-middle-income countries (LMICs) ( 4 ). Untreated mental health and behavioral problems in childhood and adolescents, in particular, have profound long-term social and economic adverse consequences, including increased contact with the criminal justice system, lower employment rate and lesser wages among those employed, and interpersonal difficulties ( 5 – 8 ).
Need for Mental Health (MH) Prevention
Longitudinal studies suggest that individuals with a lower level of positive wellbeing are more likely to acquire mental illness ( 9 ). Conversely, factors that promote positive wellbeing and resilience among individuals are critical in preventing mental illnesses and better outcomes among those with mental illness ( 10 , 11 ). For example, in patients with depressive disorders, higher premorbid resilience is associated with earlier responses ( 12 ). On the contrary, patients with bipolar affective- and recurrent depressive disorders who have a lower premorbid quality of life are at higher risk of relapses ( 13 ).
Recently there has been an increased emphasis on the need to promote wellbeing and positive mental health in preventing the development of mental disorders, for poor mental health has significant social and economic implications ( 14 – 16 ). Research also suggests that mental health promotion and preventative measures are cost-effective in preventing or reducing mental illness-related morbidity, both at the society and individual level ( 17 ).
Although the World Health Organization (WHO) defines health as “a state of complete physical, mental, and social wellbeing and not merely an absence of disease or infirmity,” there has been little effort at the global level or stagnation in implementing effective mental health services ( 18 ). Moreover, when it comes to the research on mental health (vis-a-viz physical health), promotive and preventive mental health aspects have received less attention vis-a-viz physical health. Instead, greater emphasis has been given to the illness aspect, such as research on psychopathology, mental disorders, and treatment ( 19 , 20 ). Often, physicians and psychiatrists are unfamiliar with various concepts, approaches, and interventions directed toward mental health promotion and prevention ( 11 , 21 ).
Prevention and promotion of mental health are essential, notably in reducing the growing magnitude of mental illnesses. However, while health promotion and disease prevention are universally regarded concepts in public health, their strategic application for mental health promotion and prevention are often elusive. Furthermore, given the evidence of substantial links between psychological and physical health, the non-incorporation of preventive mental health services is deplorable and has serious ramifications. Therefore, policymakers and health practitioners must be sensitized about linkages between mental- and physical health to effectively implement various mental health promotive and preventive interventions, including in individuals with chronic physical illnesses ( 18 ).
The magnitude of the mental health problems can be gauged by the fact that about 10–20% of young individuals worldwide experience depression ( 22 ). As described above, poor mental health during childhood is associated with adverse health (e.g., substance use and abuse), social (e.g., delinquency), academic (e.g., school failure), and economic (high risk of poverty) adverse outcomes in adulthood ( 23 ). Childhood and adolescence are critical periods for setting the ground for physical growth and mental wellbeing ( 22 ). Therefore, interventions promoting positive psychology empower youth with the life skills and opportunities to reach their full potential and cope with life's challenges. Comprehensive mental health interventions involving families, schools, and communities have resulted in positive physical and psychological health outcomes. However, the data is limited to high-income countries (HICs) ( 24 – 28 ).
In contrast, in low and middle-income countries (LMICs) that bear the greatest brunt of mental health problems, including massive, coupled with a high treatment gap, such interventions remained neglected in public health ( 29 , 30 ). This issue warrants prompt attention, particularly when global development strategies such as Millennium Development Goals (MDGs) realize the importance of mental health ( 31 ). Furthermore, studies have consistently reported that people with socioeconomic disadvantages are at a higher risk of mental illness and associated adverse outcomes; partly, it is attributed to the inequitable distribution of mental health services ( 32 – 35 ).
Scope of Mental Health Promotion and Prevention in the Current Situation
Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses ( 18 , 36 – 42 ). There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe mental diseases (e.g., schizophrenia and psychotic illness, and bipolar affective disorders) as well as common mental disorders (e.g., anxiety, depression, stress-related disorders) ( 43 – 46 ). These preventive measures have also been evaluated for their cost-effectiveness with promising findings. In addition, novel interventions such as digital-based interventions and novel therapies (e.g., adventure therapy, community pharmacy program, and Home-based Nurse family partnership program) to address the mental health problems have yielded positive results. Likewise, data is emerging from LMICs, showing at least moderate evidence of mental health promotion intervention effectiveness. However, most of the available literature and intervention is restricted mainly to the HICs ( 47 ). Therefore, their replicability in LMICs needs to be established and, also, there is a need to develop locally suited interventions.
Fortunately, there has been considerable progress in preventive psychiatry over recent decades, including research on it. In the light of these advances, there is an accelerated interest among researchers, clinicians, governments, and policymakers to harness the potentialities of the preventive strategies to improve the availability, accessibility, and utility of such services for the community.

The Concept of Preventive Psychiatry
Origins of preventive psychiatry.
The history of preventive psychiatry can be traced back to the early 1900's with the foundation of the national mental health association (erstwhile mental health association), the committee on mental hygiene in New York, and the mental health hygiene movement ( 48 ). The latter emphasized the need for physicians to develop empathy and recognize and treat mental illness early, leading to greater awareness about mental health prevention ( 49 ). Despite that, preventive psychiatry remained an alien concept for many, including mental health professionals, particularly when the etiology of most psychiatric disorders was either unknown or poorly understood. However, recent advances in our understanding of the phenomena underlying psychiatric disorders and availability of the neuroimaging and electrophysiological techniques concerning mental illness and its prognosis has again brought the preventive psychiatry in the forefront ( 1 ).
Levels of Prevention
The literal meaning of “prevention” is “the act of preventing something from happening” ( 50 ); the entity being prevented can range from the risk factors of the development of the illness, the onset of illness, or the recurrence of the illness or associated disability. The concept of prevention emerged primarily from infectious diseases; measures like mass vaccination and sanitation promotion have helped prevent the development of the diseases and subsequent fatalities. The original preventive model proposed by the Commission on Chronic Illness in 1957 included primary, secondary, and tertiary preventions ( 48 ).
The Concept of Primary, Secondary, and Tertiary Prevention
The stages of prevention target distinct aspects of the illness's natural course; the primary prevention acts at the stage of pre-pathogenesis, that is, when the disease is yet to occur, whereas the secondary and tertiary prevention target the phase after the onset of the disease ( 51 ). Primary prevention includes health promotion and specific protection, while secondary and tertairy preventions include early diagnosis and treatment and measures to decrease disability and rehabilitation, respectively ( 51 ) ( Figure 1 ).

The concept of primary and secondary prevention [adopted from prevention: Primary, Secondary, Tertiary by Bauman et al. ( 51 )].
The primary prevention targets those individuals vulnerable to developing mental disorders and their consequences because of their bio-psycho-social attributes. Therefore, it can be viewed as an intervention to prevent an illness, thereby preventing mental health morbidity and potential social and economic adversities. The preventive strategies under it usually target the general population or individuals at risk. Secondary and tertiary prevention targets those who have already developed the illness, aiming to reduce impairment and morbidity as soon as possible. However, these measures usually occur in a person who has already developed an illness, therefore facing related suffering, hence may not always be successful in curing or managing the illness. Thus, secondary and tertiary prevention measures target the already exposed or diagnosed individuals.
The Concept of Universal, Selective, and Indicated Prevention
The classification of health prevention based on primary/secondary/tertiary prevention is limited in being highly centered on the etiology of the illness; it does not consider the interaction between underlying etiology and risk factors of an illness. Gordon proposed another model of prevention that focuses on the degree of risk an individual is at, and accordingly, the intensity of intervention is determined. He has classified it into universal, selective, and indicated prevention. A universal preventive strategy targets the whole population irrespective of individual risk (e.g., maintaining healthy, psychoactive substance-free lifestyles); selective prevention is targeted to those at a higher risk than the general population (socio-economically disadvantaged population, e.g., migrants, a victim of a disaster, destitute, etc.). The indicated prevention aims at those who have established risk factors and are at a high risk of getting the disease (e.g., family history of psychiatric illness, history of substance use, certain personality types, etc.). Nevertheless, on the other hand, these two classifications (the primary, secondary, and tertiary prevention; and universal, selective, and indicated prevention) have been intended for and are more appropriate for physical illnesses with a clear etiology or risk factors ( 48 ).
In 1994, the Institute of Medicine (IOM) Committee on Prevention of Mental Disorders proposed a new paradigm that classified primary preventive measures for mental illnesses into three categories. These are indicated, selected, and universal preventive interventions (refer Figure 2 ). According to this paradigm, primary prevention was limited to interventions done before the onset of the mental illness ( 48 ). In contrast, secondary and tertiary prevention encompasses treatment and maintenance measures ( Figure 2 ).

The interventions for mental illness as classified by the Institute of Medicine (IOM) Committee on Prevention of Mental Disorders [adopted from Mrazek and Haggerty ( 48 )].
Although the boundaries between prevention and treatment are often more overlapping than being exclusive, the new paradigm can be used to avoid confusion stemming from the common belief that prevention can take place at all parts of mental health management ( 48 ). The onset of mental illnesses can be prevented by risk reduction interventions, which can involve reducing risk factors in an individual and strengthening protective elements in them. It aims to target modifiable factors, both risk, and protective factors, associated with the development of the illness through various general and specific interventions. These interventions can work across the lifespan. The benefits are not restricted to reduction or delay in the onset of illness but also in terms of severity or duration of illness ( 48 ).On the spectrum of mental health interventions, universal preventive interventions are directed at the whole population without identifiable risk factors. The interventions are beneficial for the general population or sub-groups. Prenatal care and childhood vaccination are examples of preventative measures that have benefited both physical and mental health. Selective preventive mental health interventions are directed at people or a subgroup with a significantly higher risk of developing mental disorders than the general population. Risk groups are those who, because of their vulnerabilities, are at higher risk of developing mental illnesses, e.g., infants with low-birth-weight (LBW), vulnerable children with learning difficulties or victims of maltreatment, elderlies, etc. Specific interventions are home visits and new-born day care facilities for LBW infants, preschool programs for all children living in resource-deprived areas, support groups for vulnerable elderlies, etc. Indicated preventive interventions focus on high-risk individuals who have developed minor but observable signs or symptoms of mental disorder or genetic risk factors for mental illness. However, they have not fulfilled the criteria of a diagnosable mental disorder. For instance, the parent-child interaction training program is an indicated prevention strategy that offers support to children whose parents have recognized them as having behavioral difficulties.
The overall objective of mental health promotion and prevention is to reduce the incidence of new cases, additionally delaying the emergence of mental illness. However, promotion and prevention in mental health complement each other rather than being mutually exclusive. Moreover, combining these two within the overall public health framework reduces stigma, increases cost-effectiveness, and provides multiple positive outcomes ( 18 ).
How Prevention in Psychiatry Differs From Other Medical Disorders
Compared to physical illnesses, diagnosing a mental illness is more challenging, particularly when there is still a lack of objective assessment methods, including diagnostic tools and biomarkers. Therefore, the diagnosis of mental disorders is heavily influenced by the assessors' theoretical perspectives and subjectivity. Moreover, mental illnesses can still be considered despite an individual not fulfilling the proper diagnostic criteria led down in classificatory systems, but there is detectable dysfunction. Furthermore, the precise timing of disorder initiation or transition from subclinical to clinical condition is often uncertain and inconclusive ( 48 ). Therefore, prevention strategies are well-delineated and clear in the case of physical disorders while it's still less prevalent in mental health parlance.
Terms, Definitions, and Concepts
The terms mental health, health promotion, and prevention have been differently defined and interpreted. It is further complicated by overlapping boundaries of the concept of promotion and prevention. Some commonly used terms in mental health prevention have been tabulated ( Table 1 ) ( 18 ).
Commonly used terms in mental health prevention.
Mental Health Promotion and Protection
The term “mental health promotion” also has definitional challenges as it signifies different things to different individuals. For some, it means the treatment of mental illness; for others, it means preventing the occurrence of mental illness; while for others, it means increasing the ability to manage frustration, stress, and difficulties by strengthening one's resilience and coping abilities ( 54 ). It involves promoting the value of mental health and improving the coping capacities of individuals rather than amelioration of symptoms and deficits.
Mental health promotion is a broad concept that encompasses the entire population, and it advocates for a strengths-based approach and tries to address the broader determinants of mental health. The objective is to eliminate health inequalities via empowerment, collaboration, and participation. There is mounting evidence that mental health promotion interventions improve mental health, lower the risk of developing mental disorders ( 48 , 55 , 56 ) and have socioeconomic benefits ( 24 ). In addition, it strives to increase an individual's capacity for psychosocial wellbeing and adversity adaptation ( 11 ).
However, the concepts of mental health promotion, protection, and prevention are intrinsically linked and intertwined. Furthermore, most mental diseases result from complex interaction risk and protective factors instead of a definite etiology. Facilitating the development and timely attainment of developmental milestones across an individual's lifespan is critical for positive mental health ( 57 ). Although mental health promotion and prevention are essential aspects of public health with wide-ranging benefits, their feasibility and implementation are marred by financial and resource constraints. The lack of cost-effectiveness studies, particularly from the LMICs, further restricts its full realization ( 47 , 58 , 59 ).
Despite the significance of the topic and a considerable amount of literature on it, a comprehensive review is still lacking that would cover the concept of mental health promotion and prevention and simultaneously discusses various interventions, including the novel techniques delivered across the lifespan, in different settings, and level of prevention. Therefore, this review aims to analyze the existing literature on various mental health promotion and prevention-based interventions and their effectiveness. Furthermore, its attempts to highlight the implications of such intervention in low-resource settings and provides future directions. Such literature would add to the existing literature on mental health promotion and prevention research and provide key insights into the effectiveness of such interventions and their feasibility and replicability in various settings.
Methodology
For the current review, key terms like “mental health promotion,” OR “protection,” OR “prevention,” OR “mitigation” were used to search relevant literature on Google Scholar, PubMed, and Cochrane library databases, considering a time period between 2000 to 2019 ( Supplementary Material 1 ). However, we have restricted our search till 2019 for non-original articles (reviews, commentaries, viewpoints, etc.), assuming that it would also cover most of the original articles published until then. Additionally, we included original papers from the last 5 years (2016–2021) so that they do not get missed out if not covered under any published review. The time restriction of 2019 for non-original articles was applied to exclude papers published during the Coronavirus disease (COVID-19) pandemic as the latter was a significant event, bringing about substantial change and hence, it warranted a different approach to cater to the MH needs of the population, including MH prevention measures. Moreover, the COVID-19 pandemic resulted in the flooding of novel interventions for mental health prevention and promotion, specifically targeting the pandemic and its consequences, which, if included, could have biased the findings of the current review on various MH promotion and prevention interventions.
A time frame of about 20 years was taken to see the effectiveness of various MH promotion and protection interventions as it would take substantial time to be appreciated in real-world situations. Therefore, the current paper has put greater reliance on the review articles published during the last two decades, assuming that it would cover most of the original articles published until then.
The above search yielded 320 records: 225 articles from Google scholar, 59 articles from PubMed, and 36 articles from the Cochrane database flow-diagram of records screening. All the records were title/abstract screened by all the authors to establish the suitability of those records for the current review; a bibliographic- and gray literature search was also performed. In case of any doubts or differences in opinion, it was resolved by mutual discussion. Only those articles directly related to mental health promotion, primary prevention, and related interventions were included in the current review. In contrast, records that discussed any specific conditions/disorders (post-traumatic stress disorders, suicide, depression, etc.), specific intervention (e.g., specific suicide prevention intervention) that too for a particular population (e.g., disaster victims) lack generalizability in terms of mental health promotion or prevention, those not available in the English language, and whose full text was unavailable were excluded. The findings of the review were described narratively.
Interventions for Mental Health Promotion and Prevention and Their Evidence
Various interventions have been designed for mental health promotion and prevention. They are delivered and evaluated across the regions (high-income countries to low-resource settings, including disaster-affiliated regions of the world), settings (community-based, school-based, family-based, or individualized); utilized different psychological constructs and therapies (cognitive behavioral therapy, behavioral interventions, coping skills training, interpersonal therapies, general health education, etc.); and delivered by different professionals/facilitators (school-teachers, mental health professionals or paraprofessionals, peers, etc.). The details of the studies, interventions used, and outcomes have been provided in Supplementary Table 1 . Below we provide the synthesized findings of the available research.
The majority of the available studies were quantitative and experimental. Randomized controlled trials comprised a sizeable proportion of the studies; others were quasi-experimental studies and, a few, qualitative studies. The studies primarily focussed on school students or the younger population, while others were explicitly concerned with the mental health of young females ( 60 ). Newer data is emerging on mental health promotion and prevention interventions for elderlies (e.g., dementia) ( 61 ). The majority of the research had taken a broad approach to mental health promotion ( 62 ). However, some studies have focused on universal prevention ( 63 , 64 ) or selective prevention ( 65 – 68 ). For instance, the Resourceful Adolescent Program (RAPA) was implemented across the schools and has utilized cognitive-behavioral and interpersonal therapies and reported a significant improvement in depressive symptoms. Some of the interventions were directed at enhancing an individual's characteristics like resilience, behavior regulation, and coping skills (ZIPPY's Friends) ( 69 ), while others have focused on the promotion of social and emotional competencies among the school children and attempted to reduce the gap in such competencies across the socio-economic classes (“Up” program) ( 70 ) or utilized expressive abilities of the war-affected children (Writing for Recover (WfR) intervention) ( 71 ) to bring about an improvement in their psychological problems (a type of selective prevention) ( 62 ) or harnessing the potential of Art, in the community-based intervention, to improve self-efficacy, thus preventing mental disorders (MAD about Art program) ( 72 ). Yet, others have focused on strengthening family ( 60 , 73 ), community relationships ( 62 ), and targeting modifiable risk factors across the life course to prevent dementia among the elderlies and also to support the carers of such patients ( 61 ).
Furthermore, more of the studies were conducted and evaluated in the developed parts of the world, while emerging economies, as anticipated, far lagged in such interventions or related research. The interventions that are specifically adapted for local resources, such as school-based programs involving paraprofessionals and teachers in the delivery of mental health interventions, were shown to be more effective ( 62 , 74 ). Likewise, tailored approaches for low-resource settings such as LMICs may also be more effective ( 63 ). Some of these studies also highlight the beneficial role of a multi-dimensional approach ( 68 , 75 ) and interventions targeting early lifespan ( 76 , 77 ).
Newer Insights: How to Harness Digital Technology and Novel Methods of MH Promotion and Protection
With the advent of digital technology and simultaneous traction on mental health promotion and prevention interventions, preventive psychiatrists and public health experts have developed novel techniques to deliver mental health promotive and preventive interventions. These encompass different settings (e.g., school, home, workplace, the community at large, etc.) and levels of prevention (universal, selective, indicated) ( 78 – 80 ).
The advanced technologies and novel interventions have broadened the scope of MH promotion and prevention, such as addressing the mental health issues of individuals with chronic medical illness ( 81 , 82 ), severe mental disorders ( 83 ), children and adolescents with mental health problems, and geriatric population ( 78 ). Further, it has increased the accessibility and acceptability of such interventions in a non-stigmatizing and tailored manner. Moreover, they can be integrated into the routine life of the individuals.
For instance, Internet-and Mobile-based interventions (IMIs) have been utilized to monitor health behavior as a form of MH prevention and a stand-alone self-help intervention. Moreover, the blended approach has expanded the scope of MH promotive and preventive interventions such as face-to-face interventions coupled with remote therapies. Simultaneously, it has given way to the stepped-care (step down or step-up care) approach of treatment and its continuation ( 79 ). Also, being more interactive and engaging is particularly useful for the youth.
The blended model of care has utilized IMIs to a varying degree and at various stages of the psychological interventions. This includes IMIs as a supplementary approach to the face-to-face-interventions (FTFI), FTFI augmented by behavior intervention technologies (BITs), BITs augmented by remote human support, and fully automated BITs ( 84 ).
The stepped care model of mental health promotion and prevention strategies includes a stepped-up approach, wherein BITs are utilized to manage the prodromal symptoms, thereby preventing the onset of the full-blown episode. In the Stepped-down approach, the more intensive treatments (in-patient or out-patient based interventions) are followed and supplemented with the BITs to prevent relapse of the mental illness, such as for previously admitted patients with depression or substance use disorders ( 85 , 86 ).
Similarly, the latest research has developed newer interventions for strengthening the psychological resilience of the public or at-risk individuals, which can be delivered at the level of the home, such as, e.g., nurse family partnership program (to provide support to the young and vulnerable mothers and prevent childhood maltreatment) ( 87 ); family healing together program aimed at improving the mental health of the family members living with persons with mental illness (PwMI) ( 88 ). In addition, various novel interventions for MH promotion and prevention have been highlighted in the Table 2 .
Depiction of various novel mental health promotion and prevention strategies.
a/w, associated with; A-V, audio-visual; b/w, between; CBT, Cognitive Behavioral Therapy; CES-Dep., Center for Epidemiologic Studies-Depression scale; CG, control group; FU, follow-up; GAD, generalized anxiety disorders-7; IA, intervention arm; HCWs, Health Care Workers; LMIC, low and middle-income countries; MDD, major depressive disorders; mgt, management; MH, mental health; MHP, mental health professional; MINI, mini neuropsychiatric interview; NNT, number needed to treat; PHQ-9, patient health questionnaire; TAU, treatment as usual .
Furthermore, school/educational institutes-based interventions such as school-Mental Health Magazines to increase mental health literacy among the teachers and students have been developed ( 80 ). In addition, workplace mental health promotional activities have targeted the administrators, e.g., guided “e-learning” for the managers that have shown to decrease the mental health problems of the employees ( 102 ).
Likewise, digital technologies have also been harnessed in strengthening community mental health promotive/preventive services, such as the mental health first aid (MHFA) Books on Prescription initiative in New Zealand provided information and self-help tools through library networks and trained book “prescribers,” particularly in rural and remote areas ( 103 ).
Apart from the common mental disorders such as depression, anxiety, and behavioral disorders in the childhood/adolescents, novel interventions have been utilized to prevent the development of or management of medical, including preventing premature mortality and psychological issues among the individuals with severe mental illnesses (SMIs), e.g., Lets' talk about tobacco-web based intervention and motivational interviewing to prevent tobacco use, weight reduction measures, and promotion of healthy lifestyles (exercise, sleep, and balanced diets) through individualized devices, thereby reducing the risk of cardiovascular disorders ( 83 ). Similarly, efforts have been made to improve such individuals' coping skills and employment chances through the WorkingWell mobile application in the US ( 104 ).
Apart from the digital-based interventions, newer, non-digital-based interventions have also been utilized to promote mental health and prevent mental disorders among individuals with chronic medical conditions. One such approach in adventure therapy aims to support and strengthen the multi-dimensional aspects of self. It includes the physical, emotional or cognitive, social, spiritual, psychological, or developmental rehabilitation of the children and adolescents with cancer. Moreover, it is delivered in the natural environment outside the hospital premises, shifting the focus from the illness model to the wellness model ( 81 ). Another strength of this intervention is it can be delivered by the nurses and facilitate peer support and teamwork.
Another novel approach to MH prevention is gut-microbiota and dietary interventions. Such interventions have been explored with promising results for the early developmental disorders (Attention deficit hyperactive disorder, Autism spectrum disorders, etc.) ( 105 ). It works under the framework of the shared vulnerability model for common mental disorders and other non-communicable diseases and harnesses the neuroplasticity potential of the developing brain. Dietary and lifestyle modifications have been recommended for major depressive disorders by the Clinical Practice Guidelines in Australia ( 106 ). As most childhood mental and physical disorders are determined at the level of the in-utero and early after the birth period, targeting maternal nutrition is another vital strategy. The utility has been expanded from maternal nutrition to women of childbearing age. The various novel mental health promotion and prevention strategies are shown in Table 2 .
Newer research is emerging that has utilized the digital platform for training non-specialists in diagnosis and managing individuals with mental health problems, such as Atmiyata Intervention and The SMART MH Project in India, and The Allillanchu Project in Peru, to name a few ( 99 ). Such frameworks facilitate task-sharing by the non-specialist and help in reducing the treatment gap in these countries. Likewise, digital algorithms or decision support systems have been developed to make mental health services more transparent, personalized, outcome-driven, collaborative, and integrative; one such example is DocuMental, a clinical decision support system (DSS). Similarly, frameworks like i-PROACH, a cloud-based intelligent platform for research outcome assessment and care in mental health, have expanded the scope of the mental health support system, including promoting research in mental health ( 100 ). In addition, COVID-19 pandemic has resulted in wider dissemination of the applications based on the evidence-based psycho-social interventions such as National Health Service's (NHS's) Mind app and Headspace (teaching meditation via a website or a phone application) that have utilized mindfulness-based practices to address the psychological problems of the population ( 101 ).
Challenges in Implementing Novel MH Promotion and Prevention Strategies
Although novel interventions, particularly internet and mobile-based interventions (IMIs), are effective models for MH promotion and prevention, their cost-effectiveness requires further exploration. Moreover, their feasibility and acceptability in LMICs could be challenging. Some of these could be attributed to poor digital literacy, digital/network-related limitations, privacy issues, and society's preparedness to implement these interventions.
These interventions need to be customized and adapted according to local needs and context, for which implementation and evaluative research are warranted. In addition, the infusion of more human and financial resources for such activities is required. Some reports highlight that many of these interventions do not align with the preferences and use the pattern of the service utilizers. For instance, one explorative research on mental health app-based interventions targeting youth found that despite the burgeoning applications, they are not aligned with the youth's media preferences and learning patterns. They are less interactive, have fewer audio-visual displays, are not youth-specific, are less dynamic, and are a single touch app ( 107 ).
Furthermore, such novel interventions usually come with high costs. In low-resource settings where service utilizers have limited finances, their willingness to use such services may be doubtful. Moreover, insurance companies, including those in high-income countries (HICs), may not be willing to fund such novel interventions, which restricts the accessibility and availability of interventions.
Research points to the feasibility and effectiveness of incorporating such novel interventions in routine services such as school, community, primary care, or settings, e.g., in low-resource settings, the resource persons like teachers, community health workers, and primary care physicians are already overburdened. Therefore, their willingness to take up additional tasks may raise skepticism. Moreover, the attitudinal barrier to moving from the traditional service delivery model to the novel methods may also impede.
Considering the low MH budget and less priority on the MH prevention and promotion activities in most low-resource settings, the uptake of such interventions in the public health framework may be lesser despite the latter's proven high cost-effectiveness. In contrast, policymakers may be more inclined to invest in the therapeutic aspects of MH.
Such interventions open avenues for personalized and precision medicine/health care vs. the traditional model of MH promotion and preventive interventions ( 108 , 109 ). For instance, multivariate prediction algorithms with methods of machine learning and incorporating biological research, such as genetics, may help in devising tailored, particularly for selected and indicated prevention, interventions for depression, suicide, relapse prevention, etc. ( 79 ). Therefore, more research in this area is warranted.
To be more clinically relevant, greater biological research in MH prevention is required to identify those at higher risk of developing given mental disorders due to the existing risk factors/prominent stress ( 110 ). For instance, researchers have utilized the transcriptional approach to identify a biological fingerprint for susceptibility (denoting abnormal early stress response) to develop post-traumatic stress disorders among the psychological trauma survivors by analyzing the expression of the Peripheral blood mononuclear cell gene expression profiles ( 111 ). Identifying such biological markers would help target at-risk individuals through tailored and intensive interventions as a form of selected prevention.
Similarly, such novel interventions can help in targeting the underlying risk such as substance use, poor stress management, family history, personality traits, etc. and protective factors, e.g., positive coping techniques, social support, resilience, etc., that influences the given MH outcome ( 79 ). Therefore, again, it opens the scope of tailored interventions rather than a one-size-fits-all model of selective and indicated prevention for various MH conditions.
Furthermore, such interventions can be more accessible for the hard-to-reach populations and those with significant mental health stigma. Finally, they play a huge role in ensuring the continuity of care, particularly when community-based MH services are either limited or not available. For instance, IMIs can maintain the improvement of symptoms among individuals previously managed in-patient, such as for suicide, SUDs, etc., or receive intensive treatment like cognitive behavior therapy (CBT) for depression or anxiety, thereby helping relapse prevention ( 86 , 112 ). Hence, such modules need to be developed and tested in low-resource settings.
IMIs (and other novel interventions) being less stigmatizing and easily accessible, provide a platform to engage individuals with chronic medical problems, e.g., epilepsy, cancer, cardiovascular diseases, etc., and non-mental health professionals, thereby making it more relevant and appealing for them.
Lastly, research on prevention-interventions needs to be more robust to adjust for the pre-intervention matching, high attrition rate, studying the characteristics of treatment completers vs. dropouts, and utilizing the intention-to-treat analysis to gauge the effect of such novel interventions ( 78 ).
Recommendations for Low-and-Middle-Income Countries
Although there is growing research on the effectiveness and utility of mental health promotion/prevention interventions across the lifespan and settings, low-resource settings suffer from specific limitations that restrict the full realization of such public health strategies, including implementing the novel intervention. To overcome these challenges, some of the potential solutions/recommendations are as follows:
- The mental health literacy of the population should be enhanced through information, education, and communication (IEC) activities. In addition, these activities should reduce stigma related to mental problems, early identification, and help-seeking for mental health-related issues.
- Involving teachers, workplace managers, community leaders, non-mental health professionals, and allied health staff in mental health promotion and prevention is crucial.
- Mental health concepts and related promotion and prevention should be incorporated into the education curriculum, particularly at the medical undergraduate level.
- Training non-specialists such as community health workers on mental health-related issues across an individual's life course and intervening would be an effective strategy.
- Collaborating with specialists from other disciplines, including complementary and alternative medicines, would be crucial. A provision of an integrated health system would help in increasing awareness, early identification, and prompt intervention for at-risk individuals.
- Low-resource settings need to develop mental health promotion interventions such as community-and school-based interventions, as these would be more culturally relevant, acceptable, and scalable.
- Utilizing a digital platform for scaling mental health services (e.g., telepsychiatry services to at-risk populations) and training the key individuals in the community would be a cost-effective framework that must be explored.
- Infusion of higher financial and human resources in this area would be a critical step, as, without adequate resources, research, service development, and implementation would be challenging.
- It would also be helpful to identify vulnerable populations and intervene in them to prevent the development of clinical psychiatric disorders.
- Lastly, involving individuals with lived experiences at the level of mental health planning, intervention development, and delivery would be cost-effective.
Clinicians, researchers, public health experts, and policymakers have increasingly realized mental health promotion and prevention. Investment in Preventive psychiatry appears to be essential considering the substantial burden of mental and neurological disorders and the significant treatment gap. Literature suggests that MH promotive and preventive interventions are feasible and effective across the lifespan and settings. Moreover, various novel interventions (e.g., internet-and mobile-based interventions, new therapies) have been developed worldwide and proven effective for mental health promotion and prevention; such interventions are limited mainly to HICs.
Despite the significance of preventive psychiatry in the current world and having a wide-ranging implication for the wellbeing of society and individuals, including those suffering from chronic medical problems, it is a poorly utilized public health field to address the population's mental health needs. Lately, researchers and policymakers have realized the untapped potentialities of preventive psychiatry. However, its implementation in low-resource settings is still in infancy and marred by several challenges. The utilization of novel interventions, such as digital-based interventions, and blended and stepped-care models of care, can address the enormous mental health need of the population. Additionally, it provides mental health services in a less-stigmatizing and easily accessible, and flexible manner. More research concerning this is required from the LMICs.
Author Contributions
VS, AK, and SG: methodology, literature search, manuscript preparation, and manuscript review. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.898009/full#supplementary-material
Mental Health and Wellbeing Resources for Students at Harvard
We hope that you find these resources to be helpful:
- The Mental Health and Wellbeing Online Learning Module equips students with information and tips on ways to support individual wellbeing, where to seek help when needed, and how to help a friend in need.
- Counseling and Mental Health Services (CAMHS) provides direct support. One example of the resources we provide is the recently launched TimelyCare virtual platform , which offers each student up to 12 telehealth therapy sessions per academic year.
- The Center for Wellness and Health Promotion offers workshops and other services to nurture individual and collective wellbeing.
- The Student Wellbeing at Harvard website offers additional resources and opportunities to help students prioritize and expand wellbeing , engage in the campus community, and find support when needed.
- The Harvard Chan Office for Students also has some resource listings as well
News from the School

Bethany Kotlar, PhD '24, studies how children fare when they're born to incarcerated mothers

Soccer, truffles, and exclamation points: Dean Baccarelli shares his story

Health care transformation in Africa highlighted at conference

COVID, four years in
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
The Science of Siblings
These identical twins both grew up with autism, but took very different paths.

Jon Hamilton
The Science of Siblings is a new series exploring the ways our siblings can influence us, from our money and our mental health all the way down to our very molecules. We'll be sharing these stories over the next several weeks.

These side-by-side photos show identical twins Sam and John Fetters. On the left, the twins on their first day of third grade; on the right, the brothers at home on Martha's Vineyard in March 2024. Family photo; Jodi Hilton for NPR hide caption
Sam and John Fetters, 19, are identical twins at opposite ends of the autism spectrum.
Sam is a sophomore at Amherst College who plans to double major in history and political science. In his free time, he runs marathons.
John attends a special school, struggles to form sentences, and likes to watch Teletubbies and Sesame Street .
Two brothers. Same genes. Different flavors of autism.
To scientists, twins like Sam and John pose an important question: How can a disorder that is known to be highly genetic look so different in siblings who share the same genome?

"That is one of the greatest mysteries right now in research on autism," says Dr. Stephanie Morris , a pediatric neurologist at the Kennedy Krieger Institute in Baltimore.
Solving that mystery could help explain autism's odd mix of nature and nurture, Morris says. It also might help "modify the trajectory" of autistic children experiencing speech and language delays, or difficulty with social communication.
Identical twins on separate paths
Sam and John are spending the weekend with their mom, Kim Leaird, at the family's apartment in West Tisbury, a small town on Martha's Vineyard.
The twins are crowded together on a couch. Even seated, they look tall. Standing, Sam is 6 feet, 5 inches, his brother just an inch shorter.
John lets Sam do most of the talking. He frequently touches his brother, who sometimes takes his hand.
John has "a truly tremendous amount of empathy," Sam says. "He's able to be very supportive."
When Sam and his mother were at odds, John would comfort him. And when Sam ran track and cross country in high school meets, he'd see his brother at the finish line, "jumping up and down because he was so happy."
When John speaks, it's often about Sesame Street characters, including his favorite: Cookie Monster.

Early in life, Sam (left) and John were much more similar than they may seem today. "They both did not wave, they didn't respond to their name, they both had a lot of repetitive movements," says their mother, Kim Leaird. Jodi Hilton for NPR hide caption
Early in life, Sam (left) and John were much more similar than they may seem today. "They both did not wave, they didn't respond to their name, they both had a lot of repetitive movements," says their mother, Kim Leaird.
Why that particular Muppet?
"He likes cookies!" John says.
Early in life, Sam and John were much more similar than they may seem today, Leaird says.
"They both did not wave, they didn't respond to their name, they both had a lot of repetitive movements," she says.
At age 2, neither was speaking. So Leaird enrolled them in an early intervention preschool.

Shots - Health News
At the heart of this cozy coffee shop lies a big sister's love for her little brother.
It worked for Sam.
"He started talking and has never stopped," Leaird says. "It was only then we were like, 'Well, what's going on with John?"
She moved John to a more intensive program. Even so, he didn't begin using words until he was 4.

"The earliest twin studies really helped to debunk this theory that autism was caused by parenting," says Dr. Stephanie Morris, a pediatric neurologist at the Kennedy Krieger Institute in Baltimore. Jodi Hilton for NPR hide caption
"The earliest twin studies really helped to debunk this theory that autism was caused by parenting," says Dr. Stephanie Morris, a pediatric neurologist at the Kennedy Krieger Institute in Baltimore.
And over the next few years, Sam says, it became clear that he and John were on different paths.
"When we were kids, he was really passionate about Sesame Street; I was really passionate about Thomas the Tank Engine," Sam says.
But later, "I started moving to other passions and he just kept being passionate about Sesame Street ," Sam says, "which is totally valid."
What twin studies reveal about autism
When Sam and John were 5, Leaird enrolled them in a study of identical twins with autism.
"I just thought it might be good to see if we could find answers," Leaird says — especially "to help John, if we could."
The family was living in Maryland at the time. So Sam and John were evaluated at Kennedy Krieger Institute , which is known for treating children with developmental disabilities.
Studies like the one involving Sam and John have played a critical role in understanding autism since the 1970s.
"The earliest twin studies really helped to debunk this theory that autism was caused by parenting," Morris says. Under this theory, moms took the brunt of the blame, supposedly for being "cold and distant and detached from their child."
Those studies showed that autism was largely a product of genetics, not parenting.

Have a story about your sibling? Share it with us!
In 2019, a study of 366 pairs of identical twins changed the field again.
The study confirmed earlier research showing that if one twin had autism, there was a 90% chance the other would too.
"However, the level, or the severity in which the twins were manifesting the diagnosis, was incredibly different," Morris says.
The finding suggests that autism symptoms can be greatly influenced by events that happen after conception.
These events could include mutations in dividing fetal cells, or something that causes certain genes to be switched on or off.
Another possibility, Morris says, is that the severity of symptoms is affected by different experiences during pregnancy and in the first few months of life.
"There's something in very very early development that might be unique to one of the twins and not the other," she says. "That could be something as simple as an infection."
A hole in the heart
Both John and Sam were born with anatomical anomalies that required surgery.
Sam had a hernia that needed repair, but it was surgery that could wait until he was 5. John had a hole in his heart that was affecting his growth and had to be fixed when he was still an infant.
Sam's surgery went smoothly. But John developed an infection in the incision surgeons had made in his chest.
The infection was from drug-resistant staph bacteria. So John went back to the hospital and spent a month on powerful antibiotics pumped directly into a vein near his heart.
There's no way to know whether that experience changed the course of John's autism.

How to have a 'grown up' relationship with a sibling
"It's really only later that I thought, well, maybe it was the staph infection and John's environment when he was so little," Leaird says.
Regardless of what causes twins to end up at different places on the autism spectrum, these siblings seem to have a special relationship, Morris says.

When the boys spent a year in the same school, Sam did fine, but John struggled and had some noisy meltdowns. Jodi Hilton for NPR hide caption
When the boys spent a year in the same school, Sam did fine, but John struggled and had some noisy meltdowns.
"I think there's an understanding that 'My twin isn't quite as capable of communicating in the way that they need to, so I'll help them with that,'" she says.
That description fits Sam and John.
When asked to name his favorite episode of Sesame Street , John blurts out a series of words: "Abby makes the seasons change." Sam understands immediately and quickly steps in to explain.
" There's an episode with Abby Cadabby, Rosita and Zoe, where they dance around with the seasons changing," Sam says. "I think that's the one he's referring to."
His brother's keeper
Sam has always looked out for his brother, Leaird says.
When the boys spent a year in the same school, she says, Sam did fine, but John struggled and had some noisy meltdowns.
"Sam would hear him from his classroom, and he would just flee," Leaird says. "He would get up and run to his brother to help him and to translate for him."
Now that Sam is off at college, he worries about his brother, whose limited speech and flapping arms can make him the target of insults and ridicule.
"One of the ways you avoid that is trying to present [as] more neurotypical," Sam says. "I can do that. My brother can't."

Sam has always looked out for his brother. But now that he has moved away for college, he worries about John. Jodi Hilton for NPR hide caption
Sam has always looked out for his brother. But now that he has moved away for college, he worries about John.
Actually being neurotypical isn't something Sam wants for his brother or himself.
"I think I approach the world in interesting ways," Sam says, noting that autism has contributed to his passion for history and running.
John's autism is part of the "amazing and creative world in his head," Sam says, a world that includes Teletubbies and Muppets, as well as people and places.
Even so, Sam wishes his brother could use words the way he does.
"We are identical twins in almost every other way — laugh in the same way, cry in the same way, see the day in the same way, love the same way," Sam says. "He should absolutely have that ability to speak. He should have that. And him not having that is so unfair."
So for now, Sam plans to keep using his own words to help say what his brother can't.

Twin brothers Sam and John take a walk outside their family home on Martha's Vineyard. Jodi Hilton for NPR hide caption
Twin brothers Sam and John take a walk outside their family home on Martha's Vineyard.
- family relationships
- early child development
- identical twins
- Science of Siblings
- twin studies
- autism spectrum disorder
High-potency marijuana highlights the risk of cannabis-induced psychiatric disorders
Anders Gilliand was just 17 years old when he started to lose contact with reality.
“He thought that there were higher beings that were communicating with him to tell him what to do or who he was,” said his mother, Kristin Gilliand, who lives in Nashville.
Her son, who had been using marijuana since he was 14 years old, was diagnosed with schizophrenia, a chronic psychiatric disorder that can include symptoms like delusions, hallucinations and disorganized speech.
He started taking anti-psychotic medication but ultimately stopped because of the side effects he experienced. To try and quell the voices in his head, he began using heroin and died of an accidental drug overdose in 2019 when he was 22.
“If he had never started using cannabis, he might still be here,” said Gilliand, a neuroscientist at Vanderbilt University. While there is a family history of schizophrenia, she believes that her son’s marijuana use led to psychotic episodes and triggered the condition.
Anders was among a growing number of young adults, particularly men, who are at increased risk of developing psychosis from marijuana use. Evidence from separate Danish and British studies , among others, suggest a link between heavy marijuana use and psychiatric disorders such as depression, bipolar disorder and schizophrenia. Researchers believe that high levels of THC — the psychoactive component in the cannabis plant that causes the high — could set off these conditions in people who have a genetic risk. THC levels in marijuana have been getting stronger for decades.

“We’re definitely seeing a rise in cannabis-induced psychosis among teenagers,” said child psychiatrist Dr. Christian Thurstone, an addiction specialist at the University of Colorado School of Medicine in Denver.
Is higher potency marijuana more dangerous?
The more potent the cannabis products, the more likely users are to have adverse effects, said Nora Volkow, director of the National Institute on Drug Abuse.
“Those who consume the highest doses are the ones that are going to have the highest risk of becoming psychotic,” she said.
There’s limited research on adverse effects of high levels of THC, although a European study published in 2020 found that high-potency cannabis products carried a greater risk of hallucinations and delusions compared with lower potency types.
“It seems like there’s an association between cannabis strength and increased risk for psychosis but more work needs to be done there,” said Ziva Cooper, director of the center for cannabis and cannabinoids at UCLA.
As many as half of people with cannabis-induced psychosis may go on to develop either schizophrenia or bipolar disorder, research suggests.
Young adults and teenagers should be especially concerned, Thurstone said
“The studies that we have so far clearly indicate that the risk for psychosis is dose dependent, meaning that the more marijuana somebody’s exposed to especially in adolescence, the greater the risk of developing psychosis, schizophrenia and severe mental illness,” he said.
More news on marijuana and health
- Risks of marijuana and THC on the heart: What you need to know.
- Marijuana use as little as once a month linked to heart risks.
- Marijuana use sent more kids to the ER during the pandemic.
Another issue with higher strength products is the potential for developing cannabis use disorder, or an addiction to marijuana. When people are exposed frequently to higher strengths of cannabis, they may be more likely to develop cannabis use disorder, although further research is still needed to say definitively.
“There’s no longer any scientific debate that marijuana can not just be psychologically addictive or habit forming, but also physically habit forming,” Thurstone said. “It’s a substance that produces tolerance so people have to use more and more to have the same effect.”
About 1 in 10 people who begin using cannabis will become addicted, according to the Centers for Disease Control .
How cannabis potency may be linked to psychosis
Marijuana overactivates molecules in our brain known as cannabinoid receptors, which cause the high. When these brain receptors are stimulated, it can cause difficulty with thinking and problem-solving, as well as impaired memory.
How marijuana use may trigger psychosis isn’t fully understood, although scientists believe it’s interfering with our brains ability to distinguish between what’s going on in our heads versus the real world.
“Marijuana in the 60s, 70s, 80s and early 90s was about 2% to 3% THC,” said Thurstone, who has tracked the rise of high-potency THC products in smoke shops and dispensaries. “Nowadays, with the commercialized products, they are routinely 20 plus percent — so about 10 times more potent.”
Patrick Johnson, assistant store manager at Frost Exotic dispensary in Colorado, has been in the cannabis industry since 2009 and has seen the potency rise firsthand. Johnson said THC levels really started to take off after marijuana became legal for recreational use in Colorado in 2014.
Since then, 24 states, two territories and Washington, D.C. have legalized marijuana for medical and recreational use.
With more people around the country using weed legally, there’s been greater consumer demand for more powerful weed, experts say.
“After recreational [legalization] is when I have personally seen it go from like 19 or 20% up to like 30 or 35%,” Johnson said.
Currently in his shop they carry strains as low as 14% up to 30%. Most customers have a preference for the strong stuff, Johnson said.
One reason that potency has been getting stronger over the years in cannabis products is because customers may build a tolerance to the drug, said Mahmoud ElSohly, professor of pharmaceutics and cannabis researcher at the University of Mississippi. He has been studying this issue in collaboration with the National Institute of Drug Abuse, finding that the average potency has risen from 3% to 15% from 1995 to 2021.
“People keep needing higher and higher potency products to get the degree of high they’re looking for,” he said.
In the past, a joint with 2% THC may have been enough to get most people high, ElSohly said. With heavier usage, many people now have built up a tolerance and may need to smoke multiple joints with 2% THC or buy a single joint with 6% to get a similar feeling.
Is one form of marijuana safer?
Cannabis strength primarily refers to the THC content in the marijuana flower or bud, which is the smokable part of the plant.
While THC levels can be close to 40% in the flower, other products, such as concentrates or oils may contain amounts as high as 95%.
The problem, said UCLA’s Cooper, is that there isn’t yet a widely accepted standard dose like there is with alcohol, so predicting how someone will react to different cannabis products can be difficult.
It’s also challenging to develop a unit dose for inhaled combusted products. While a typical joint may contain between 100 to 200 milligrams of THC, that doesn’t tell the whole story, Cooper said.
How much THC a marijuana smoker is exposed to can vary. How long and how deep are they inhaling? Or how long do they wait in between puffs as a lot of THC is lost to "sidestream" smoke, which comes from the burning end of the joint in between hits.
In comparison, marijuana edibles such as gummies, cookies and brownies are typically 5 to 10 milligrams per dose. There is a movement toward establishing a unit dose for edibles and limiting how much THC can be consumed at once. In New York state, for example, that number is 10 mg per serving.
How high can the THC go?
“I don’t necessarily think it may raise much more,” said Volkow, from the National Institute on Drug Abuse. “There may be a level at which sometimes too much can become aversive so people smoke and get very agitated or paranoid.”
She is optimistic that the THC levels of available marijuana flower will not rise as high as 50%.
There is a limit to how much THC the plant can produce, although manufacturers are finding clever ways to boost the chemical, Cooper said.
“The industry is adding more THC to the plant products,” including infusing pre-rolled cannabis cigarettes with additional THC, she said. “We’re starting to see that people are being exposed to levels of THC we just haven’t seen in the past.
Akshay Syal, M.D., is a medical fellow with the NBC News Health and Medical Unit.
Kate Snow is a senior national correspondent for NBC News and an anchor for NBC Nightly News.
Patrick Martin is a producer in the NBC News Health & Medical Unit.
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

solar eclipse
25 templates

12 templates
north korea

7 templates
21 templates
48 templates
Shared Psychotic Disorder Case Report
Shared psychotic disorder case report presentation, free google slides theme and powerpoint template.
Shared psychotic disorder occurs in people who have a close relationship with individuals who have a diagnosed mental illness and begin to develop psychiatric symptoms themselves. If this is your field of expertise and you want to present the case you have been working on for some time, this abstract style template with illustrations will be a great help to make your information look clear, visual and enjoyable.
Features of this template
- 100% editable and easy to modify
- 29 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access


IMAGES
VIDEO
COMMENTS
Case Vignette Discussion Slides and Case Examples were created as a part of a grant from New York Community Trust to the National Council for Mental Wellbeing to build the capacity of social work students to lead the charge against the opioid epidemic. How To Use The Slides and Case Vignettes. Feel free to use these templates to build your own ...
Free Google Slides theme and PowerPoint template. Treating psychological and psychiatric conditions is quite important, as they affect our health to a large stent. To learn more about them, use this Mental Health Clinical Case presentation and give some info about case reports, using diagrams, tables, maps…. Provide details about the patient ...
Patient Case Presentation. Figure 1. Blue and silver stethoscope (Pixabay, N.D.) Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness.
Depression is a complex and pervasive condition that can deeply impact one's emotional well-being, relationships, and overall quality of life. There are a lot of misconcepts and counter-productive measures, so what we really need is information and awareness. As for you, you can help other professionals by sharing a case report. Explain how you ...
Behavioral Health Case Presentation Template. DO NOT INCLUDE ANY PATIENT IDENTIFIERS. Please note that case consultations do not create or otherwise establish a provider-patient relationship between any Piedmont Health Services or UNC Health clinician. Presenter name: Juan Prandoni, PhD, HSP-PA, LPA. Presenter Clinical Role:
Professional Simple White Gradient Picture Medical Health Minimalist Case Report Psychology Research Brain Mental Health. Case reports are useful to learn about the complexities of the human brain. Present one of such case reports with our Google Slides & PPT template.
1 Common mental health problems: Clinical case scenarios for primary care Support for education and learning ABOUT THIS PRESENTATION: Clinical case scenarios are an educational resource that can be used for individual or group learning. They have been developed to improve the identification, assessment and treatment of common mental health problems such as anxiety or depression within primary ...
The case study will allow us to explore the nuances of depression and provide valuable insights into the treatment landscape for this prevalent mental health condition. The Treatment Journey When it comes to treating depression, there are various options available, ranging from therapy to medication.
This chapter focuses on Stage 2, the empirical - or 'primary research' - aspect of the study, which we conducted using the case study method. We start with an outline of the specific research methods used, after which we provide a descriptive overview of the individual case study sites; we then present our findings, organised according to a number of analytical themes.
Clinical Case Of Mental Health Presentation Slide. Unlock the world of mental health with our illuminating Clinical Example of Mental Health content. Dive into the depths of a real-life case study on mental health and explore a clinical example that sheds light on the journey to recovery. As you navigate through this content, imagine the image ...
Case Study: Bryant. Thirty-five-year-old Bryant was admitted to the hospital because of ritualistic behaviors, depression, and distrust. At the time of admission, prominent ritualistic behaviors and depression misled clinicians to diagnose Bryant with obsessive-compulsive disorder (OCD). Shortly after, psychotic symptoms such as disorganized ...
INTRODUCTION. Case presentation in an academic psychiatry traditionally follows one of the following three formats: 4DP format (ideal and lengthy format; described in the following section), "Case Summary" (CS) (medium format), or "Case Formulation" (CF) (short format), in order of the decreasing length, duration, and the gradual transition from the use of layman terms (in the history ...
Case Presentation Format Continued 5 Risk or Safety Concerns: Suicidal or homicidal ideation or behavior, self-harming behaviors, or reporting issues. Mental Health Assessment: Include this section on the professor's copy only. Present a comprehensive DSM 5 diagnosis, with principle diagnosis listed first.
At the heart of managing this complex condition lies effective communication between mental health professionals and their patients. So, when it comes to presenting a case report on bipolar disorder, creating a workable and engaging slideshow is crucial. With the help of this template, you can tailor a visual narrative that not only enhances ...
Guidelines for Oral Case Presentation The purpose of case presentations is to provide opportunities for interactive group feedback. Prior to our meeting, organize information about the selected client and your experiences with him/her. You may share this information orally or in writing. Please plan to share a brief audio
Mental health. Children's mental health case studies. Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and ...
Clinical case scenarios: Common mental health disorders in primary care (May 2012) Page 5 of 85 . have had symptoms of generalised anxiety disorder (GAD) is also included to provide some insight into their experiences. Common mental health problems . Common mental health problems such as depression, generalised anxiety
Adler James W. Because the pros and cons for the use of medicine in psychiatry are not absolutely clear or agreed upon, strong arguments have risen on all sides. The objective of this paper is not to create a division in the clinical practice. Rather, to present an example of how to use a model in the analysis of understanding the patient behavior.
Need for Mental Health (MH) Prevention. Longitudinal studies suggest that individuals with a lower level of positive wellbeing are more likely to acquire mental illness ().Conversely, factors that promote positive wellbeing and resilience among individuals are critical in preventing mental illnesses and better outcomes among those with mental illness (10, 11).
We hope that you find these resources to be helpful: The Mental Health and Wellbeing Online Learning Module equips students with information and tips on ways to support individual wellbeing, where to seek help when needed, and how to help a friend in need.; Counseling and Mental Health Services (CAMHS) provides direct support. One example of the resources we provide is the recently launched ...
This is a case study of the Colorado Black Health Collaborative (CBHC) Barbershop/Salon Health Outreach Program, a community-based initiative that targeted disproportionate rates of hypertension and other health problems within the African American community . The program, which began as a grassroots operation in 2008 and was formally incorpo-
Sam and John Fetters are identical twins with autism. But Sam is in college, while John still struggles to form sentences. Their experience may shed light on the disorder's mix of nature and nurture.
Anders was among a growing number of young adults, particularly men, who are at increased risk of developing psychosis from marijuana use. Evidence from separate Danish and British studies, among ...
Free Google Slides theme, PowerPoint template, and Canva presentation template. Let us tell you: depression is a serious matter and all help available is much welcome. We have designed this template where you can lay out the details of a clinical case on a depressive disorder. This allows you to share information with other doctors and have ...
February 18, 2024 at 6:29 PM PST. Listen. 4:14. Vaccines that protect against severe illness, death and lingering long Covid symptoms from a coronavirus infection were linked to small increases in ...
A new, approximately 27,500-square-foot community mental health facility would be constructed in its place. Documents state the total cost for that option would be about $22.4 million. In response ...
These slides are meant to help you spread awareness about mental health and its importance. All our infographics revolve around this concept, and thus include on-topic resources. Edit the bar graphs, pie charts, percentages, timelines and circular diagrams with your data. You could even combine this with our Mental Health...
Free Google Slides theme and PowerPoint template. Shared psychotic disorder occurs in people who have a close relationship with individuals who have a diagnosed mental illness and begin to develop psychiatric symptoms themselves. If this is your field of expertise and you want to present the case you have been working on for some time, this ...